Recurrent Pregnancy Loss & Stillbirth: Causes & Treatment
advertisement

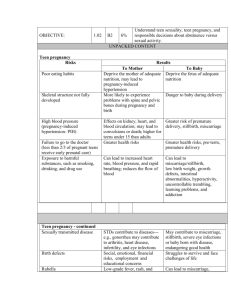
Recurrent Pregnancy LossStillbirth DOÇENT DOKTOR ZİYA KALEM İSTİNYE ÜNİVERSİTESİ LİV BAHÇEŞEHİR HASTANESİ Miscarriage is the most common complication of pregnancy. American Society for Reproductive Medicine defines recurrent pregnancy loss (RPL) as two or more failed pregnancies, not necessarily consecutive. 5% of couples attempting pregnancy will experience two miscarriages, and 1% of couples will experience three or more losses. Despite a comprehensive evaluation, a cause for RPL can be discerned in less than half of cases. In general, a patient and her partner with unexplained RPL have a 75% chance of a successful future pregnancy, The subsequent loss rate for a patient with antiphospholipid antibody syndrome may exceed 90% in an untreated pregnancy. RPL is more likely to occur in couples with similar reproductive histories, including a prior stillbirth, an anomalous fetus, a delayed conception, a family history of recurrent miscarriage, a preterm birth, or a previous child with growth restriction The limited number of bona fide causes includes structural chromosome rearrangements and monogenetic abnormalities, certain uterine anomalies, antiphospholipid antibody syndrome, and severe endocrine disorders Genetic Abnormalities Genetic Abnormalities MATERNAL AGE–RELATED ANEUPLOIDY Maternal age is strongly associated with the risk for both SAB and aneuploidy Cytogenetic alterations are identified in 50% to 60% of spontaneous abortion (SAB) specimens. Common karyotypic abnormalities include autosomal trisomy (60%), monosomyX (20%), and polyploidy (20%). The risk for trisomy in a clinically recognized pregnancy increases from about 2% to 3% for women in their twenties to 25% or more for women in their forties A large prospective Danish cohort study tracking 634,272 women through 1,221,546 pregnancies found SAB rates of less than 12% for women 20 to 29 years old, 15% for those 30 to 34 years old, 24.6% for those 35 to 39 years old, 51% for those 40 to 44 years old, and 93.4% for those older than 44 years. Women who have had ovarian deficiency, either as a result of surgery or as a congenital abnormality, have an increased risk for trisomy 21. Theories for nondisjunction have been proposed. - Absent or reduced recombination events - Abnormal chiasma position or function - Premature separation of sister chromatids - Chronic oxidative stress - Abnormalities in folate metabolism - Progressive shortening of oocyte telomere length ROBERTSONIAN AND RECIPROCAL TRANSLOCATIONS Approximately 3% to 5% of couples who experience RPL have a balanced structural chromosome rearrangement, as opposed to the rate of 0.2% in the general population In couples with RPL; 50% had balancedreciprocal translocations, 24% were robertsonian translocations, and 12% were mosaic for a female sex chromosome abnormality The remaining 14% had other types of rearrangements including pericentric and paracentric inversions Balanced rearrangements are known to predispose to errors in meiosis, resulting in abnormal offspring or RPL. Live birth rate for carriers of a reciprocal balanced translocation was 63% and 69% among those with a robertsonian translocation. There is no clear evidence to suggest a difference in risk for RPL between a maternal or paternal carrier, although men more often present with infertility. SINGLE-GENE DISORDERS Most examples of known single-gene causes of RPL are associated with second-trimester miscarriage. Lethal multiple pterygium syndromes are a collection of autosomal recessive and X-linked recessive disorders that are associated with fetal death at 14 to 20 weeks (arthrogryposis, hydrocephalus, hydrops, cystic hygromas, dental anomalies and cutaneous manifestations, chondrodysplasia punctata type 2, Rett syndrome, oral-facialdigital type 1, Aicardi syndrome, and Goltz syndrome.). MALE GENETIC FACTORS The paternal genome is equally important in fertilization, embryologic development, and placental function. USE OF ASSISTED REPRODUCTIVE TECHNOLOGIES An argument has been proffered that patients with RPL could benefit from ART, including in vitro fertilization (IVF) with or without preimplantation genetic screening (PGS) for chromosomal abnormalities commonly found in abortus specimens. Although the use of ART is appealing for couples with unexplained RPL who are desperate for a successful outcome, the prognosis for live birth in subsequent pregnancy without any intervention is approximately 75% Thrombophilias There are two types of thrombophilia putatively associated with RPL THROMBOPHILIAS Inherited thrombophilias • Factor V Leiden • Prothrombin gene mutation • Other Antiphospholipid antibody syndrome INHERITED THROMBOPHILIAS The possible link between inherited thrombophilias and adverse obstetric outcomes has become a highly debated issue. Researchers and clinicians hypothesized that women or possibly fetuses with a genetic predisposition to thromboembolism could have thrombosis of the uteroplacental circulation and resultant complications such as preeclampsia, placental abruption, growth restriction, or fetal loss. The early literature suggested a causal relationship between pregnancy loss and FVL. A meta-analysis of 31 studies reported a modest link between FVL and first-trimester SAB, with an OR of 2.01 (95% CI, 1.13 to 3.58) but a stronger association with late (> 19 weeks) nonrecurrent fetal loss (OR = 3.26; 95% CI, 1.82 to 5.83). A large case-control study of patients with recurrent stillbirths beyond 22 weeks showed an even stronger association with FVL (OR = 7.83; 95% CI, 2.83 to 21.67) Dudding and Attia conducted a meta-analysis of the link between FVL and adverse pregnancy events and noted no association with first-trimester miscarriage but a strong association with two or more second- or third-trimester fetal losses (OR =10.7; 95% CI, 4.0 to 28.5 Prospective studies have not proven causality between inherited thrombophilia and miscarriage, so screening and treatment are no longer recommended ANTIPHOSPHOLIPID ANTIBODY SYNDROME The antiphospholipid antibody syndrome (APS) is defined by both clinical and laboratory criteria The clinical criteria include a history of deep venous or arterial thrombosis and characteristic obstetric complications including RPL Laboratory criteria include the presence of medium to high titers of IgG/IgM anticardiolipin antibodies, IgG/IgM anti-β2 - glycoprotein-1 antibodies at levels in the 99th percentile or higher, or a lupus anticoagulant on two or more occasions at least 12 weeks apart. At least one clinical criterion and one laboratory criterion must be present for definitive diagnosis. Persistently high levels of aPLs appear to be associated with obstetric complications, including fetal loss after 9 weeks’ gestation, abruption, severe preeclampsia, and intrauterine growth restriction, in about 15% to 20% of affected patients. Between 5% and 15% of women with recurrent SAB have documented aPL, compared with 2% to 5% in the general obstetric population. In patients with strictly defined APS, the pregnancy failure rate in untreated pregnancies is up to 90%, with 52% of miscarriages occurring early (< 10 weeks) and 38% occurring late (> 10 weeks). TREATMENT OF ANTIPHOSPHOLIPID ANTIBODY SYNDROME AND INHERITED THROMBOPHILIAS Proposed interventions include low-molecular-weight heparin (LMWH), unfractionated heparin, aspirin (81 and 325âmg), prednisone, and intravenous immunoglobulin (IVIG). The combination of heparin and aspirin modestly increased the likelihood of a live birth compared with aspirin alone Endocrine Disorders Three endocrine disorders are reported to be associated with RPL. THYROID DISEASE Autoimmune thyroid disease is the most common cause of hypothyroidism, with a reported prevalence of 5% to 20% among pregnant women. Normal maternal thyroid function is important for trophoblast function and maintenance of early pregnancy. Antithyroid antibodies are more common in women with RPL. Nonrandomized studies have suggested that levothyroxine therapy may decrease SAB rates in euthyroid, thyroid-antibody positive women and in those with subclinical hypothyroidism. A recent Cochrane Database Review recommends treating women with subclinical hypothyroidism to reduce the risk for miscarriage LUTEAL PHASE DEFECT A luteal phase defect (LPD) is described as a failure to develop fully mature secretory endometrium The prevalence of LPDs among patients with early RPL is reported to be up to 35%. Studies of available treatments, including ovulation induction and progesterone supplementation, intended to reduce the rate of RPL, have conflicting results. A Cochrane Review did show that progesterone supplementation was beneficial in women with a history of three or more consecutive pregnancy losses (OR = 0.38; 95% CI, 0.2 to 0.7). For a patient with RPL and an LPD accompanied by hyperprolactinemia, bromocriptine is a treatment option that appears to improve live birth rates POLYCYSTIC OVARIAN SYNDROME Initial reports suggested that polycystic ovarian syndrome (PCOS) was associated with recurrent miscarriage, but causal links between hyperandrogenism, hyperinsulinemia, and RPL have been difficult to establish. Those patients with overt diabetes clearly have up to a threefold increased risk for spontaneous pregnancy loss, so women with risk factors should be screened by routine measures and treated accordingly Uterine Malformations and Endometrial Abnormalities Women with müllerian tract anomalies appear to have an increased risk for RPL. the prevalence of congenital uterine anomalies is 16.7% among women with three or more miscarriages The various theories proposed to account for the association between uterine anomalies and RPL include decreased vascularity in the septum, increased inflammation, and a reduction in sensitivity to steroid hormones Although reductions in RPL with surgical correction have been reported in several large series, there have been no prospective randomized trials to validate this intervention The presence of myomas, submucous myomas that distort the uterine cavity have been suggested as causes of recurrent miscarriage and reduced IVF success rates. Other uterine defects, such as Asherman syndrome and polyps, have been posited as causes of recurrent SAB, and descriptive series suggest improvement in pregnancy outcomes after hysteroscopic resection Environmental Factors CAFFEINE ALCOHOL OBESITY Other Factors Associated with Recurrent Pregnancy Loss IMMUNOLOGIC PROCESSES There are conflicting data with regard to the role of immunologic mechanisms in RPL. Maternal antipaternal lymphocytoxic antibodies (i.e.,blocking antibodies) acted to shield the placenta from a maternal immune response. Researchers proposed that excessive human leukocyte antigen (HLA) sharing or an abnormally high HLA conformity by prospective parents would lead to the absence of such antibodies This, in turn, would expose placental antigens to a more cytotoxic maternal immune response CELIAC DISEASE Celiac disease is known to affect other target organs, including the liver, thyroid, skin, and reproductive tract Epidemiologic studies suggest an association between celiac disease and adverse reproductive outcomes, including RPL, low birth weight, preterm birth, and infertility OTHER INFECTIOUS AND INFLAMMATORY PROCESSES Although Chlamydia trachomatis, Ureaplasma urealyticum, Mycoplasma hominis, human cytomegalovirus, adeno-associated virus, rubella, herpesviruses, and human papillomaviruses have been identified more frequently in genital tract cultures from women with RPL, there are no data establishing an association between chronic genital tract carriage of bacteria and recurrent SAB, or data indicating that empiric treatment offers benefit. The presence of bacterial vaginosis during the first trimester of pregnancy has been repeatedly reported as a risk factor for secondtrimester pregnancy loss. Inherited Bleeding Disorders Maintaining hemostatic balance is critical for implantation and pregnancy maintenance Adverse reproductive outcomes including RPL have been reported in patients with bleeding disorders , including heritable and acquired deficiencies of fibrinogen or factor XIII deficiency An increased risk for miscarriage is reported in patients with deficient or defective fibrinogen, including diagnoses of afibrinogenemia, hypofibrinogenemia, and dysfibrinogenemia Evaluation of Patients with Recurrent Pregnancy Loss history physical examination laboratory assessment (genetic, anatomic, endocrine, and hematologic studies) parental karyotypes, karyotyping of miscarriage specimens, and assessment of the placental pathology for trophoblast inclusions or chronic inflammatory processes appear to be reasonable diagnostic studies Stillbirth Epidemiology Stillbirth, defined as fetal death at 20 weeks or more of gestation, is one of the most common adverse pregnancy outcomes. It has been estimated that 98% of all stillbirths occur in low- and middle-income countries Maternal age and parity are significant risk factors for stillbirth. There is a U-shaped relationship between maternal age and stillbirth The peak risk period was 37 to 41 weeks. The risk for stillbirth at 37 to 41 weeks for women 35 to 39 years old was 1 in 382 ongoing pregnancies, and for women 40 years or older it was 1 in 267 ongoing pregnancies. Stillbirth rates are lowest for women with one prior pregnancy (4.87 per 1000 births). Multiple gestation and use of assisted reproductive technologies (ART) are also risk factors for stillbirth. The stillbirth rate is 2.8-fold higher for twins and 4.8-fold higher for triplet and higher-order pregnancies compared with singletons Compared with spontaneously conceived singleton pregnancies, singleton pregnancies from in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) procedures had more than four times the risk for stillbirth (odds ratio [OR] = 4.44; 95% CI, 2.38 to 8.28) In most studies, previous stillbirth is associated with an increased recurrence rate of stillbirth (10-fold increased risk for subsequent stillbirths). Previous cesarean delivery as a risk factor for stillbirth is controversial In pregnancy, obesity increases the risk for hypertension and diabetes and is an independent risk factor for stillbirth Pre-pregnancy obesity was associated with a 3.5- to 4.6-fold increased risk for stillbirth after 37 weeks’ gestation. Smoking, another modifiable risk factor, has been associated with a 36% increase in the odds of stillbirth (OR = 1.36; 95% CI, 1.27 to 1.46). Alcohol use, illicit drug use, low maternal education level, and lack of or inadequate prenatal care have all been associated with increased stillbirth rates Pathogenesis INFECTION Infection is believed to be associated with approximately 10% to 20% of stillbirths in developed countries. Infectious agents may result in stillbirth by producing direct fetal infection, placental dysfunction, or severe maternal illness. The most common is an ascending infection from the vagina into the space between the maternal decidua and the maternal chorion. Maternal systemic infections may also spread hematogenously and reach the fetus through the placental villi (villitis). These types of infections typically involve the fetal liver. Syphilis, which is increasingly uncommon in the United States, is still responsible for some stillbirths, especially in endemic areas. Treponema pallidum, the causative agent, can cross the placenta and infect the fetus after 14 weeks’ gestation, with risk for fetal infection increasing with gestational age. Other spirochetal diseases causing stillbirth include leptospirosis and Lyme disease. Bacterial pathogens implicated in stillbirth include Escherichia coli, group B streptococci, Ureaplasma urealyticum, Mycoplasma hominus, Bacteroides species, Gardnerella, Mobiluncus species, and various enterococci, which produce ascending infection. Malaria may be a cause of stillbirth in women who contract a first infection during pregnancy. Other, less common organisms associated with fetal death include Toxoplasma gondii and Listeria monocytogenes. When parvovirus is responsible for stillbirth, themechanism is most often destruction of erythropoietic tissue leading to severe anemia and hydrops. Other viral pathogens include enteroviruses, such as coxsackieviruses and echoviruses, as well as cytomegalovirus (CMV). MATERNAL MEDICAL CONDITIONS Hypertensive Disorders Hypertensive disorders of pregnancy complicate 10% to 16% of pregnancies and is a significant cause of stillbirth. 9.2% of stillbirths were associated with hypertensive disorders. Diabetes Mellitus Diabetes mellitus (DM) affects 2% to 5% of all pregnancies and is associated with about 4% of stillbirths. The rate of stillbirth was 1.5% in diabetic pregnancies, five times that seen in the nondiabetic population, with the majority occurring between 34 and 40 gestational weeks. Thyroid Disease Maternal hyperthyroidism in pregnancy is rare, occurring with a prevalence of 0.05% to 0.2%. Graves disease, the most common cause of hyperthyroidism, results in fetal or neonatal thyrotoxicosis in about 1% of cases because of the transplacental passage of thyroid-stimulating immunoglobulins, and it is associated with an increased stillbirth rate of 7% Hypothyroidism, both overt and subclinical, is relatively common, occurring in about 2.5% of pregnancies. Overt hypothyroidism places women at increased risk for pregnancy-induced hypertension,51 SGA infants,51 and stillbirth with a rate of 12/1000 to 20/1000. An increased stillbirth rate has been noted in euthyroid women with high serum antithyroid peroxidase (TPO) antibody concentrations, as seen in Hashimoto thyroiditis. Systemic Lupus Erythematosus Systemic lupus erythematosus (SLE) has an overall prevalence of less than 1%, with a stillbirth rate of 40 to 150 per 1000. Cause of stillbirth is neonatal lupus erythematosus with congenital atrioventricular (AV) block. Antiphospholipid antibodies are present in over a third of patients with SLE and are associated with an increased risk for thrombosis and damage to the uteroplacental vasculature. fetal death was more common in those with antiphospholipid antibodies (38%) than in those without antibodies (16%) Renal Disease The association of renal disease with stillbirth depends on the severity of renal impairment and the presence of hypertension. There is a positive linear relationship between maternal creatinine levels and stillbirth rates. Intrahepatic Cholestasis of Pregnancy Intrahepatic cholestasis of pregnancy (ICP), the most common form of noninfectious liver disease occurring in pregnancy, has been associated with an increased stillbirth rate of 12 to 30/1000 affected pregnancies ICP is characterized by pruritus and an elevation in serum bile acid concentration, but the exact mechanism of the associated stillbirth is unknown. Thrombophilias Antiphospholipid antibody syndrome (APS) is an autoimmune disorder characterized by the presence of antiphospholipid antibodies, thrombosis, and obstetric complications. The mechanism of pregnancy loss remains uncertain, but placental inflammation, thrombosis, and decidual vasculopathy are involved. The role in stillbirth of heritable coagulopathies or thrombophilias that involve deficiencies or abnormalities in anticoagulant proteins or an increase in procoagulant proteins is unclear. CONDITIONS RELATED TO THE FETUS Red Cell Alloimmunization More than 50 different red cell antigens have been reported to be associated with hemolytic disease of the fetus and newborn. Maternal alloimmunization to non-RhD antigens continues to contribute to the occurrence of stillbirth. Platelet Alloimmunization Chromosomal Abnormalities Structural Anomalies Fetomaternal Hemorrhage Fetal Growth Restriction Umbilical Cord Pathology Umbilical cord abnormalities account for 3% to 15% of stillbirths. Velamentous insertion of the umbilical cord occurs when vessels insert on the membranes rather than on the placenta. It may cause stillbirth if it leads to a vasa previa Umbilical cord occlusion results in cessation of blood flow to the fetus. The mechanisms whereby cord accidents could lead to stillbirth include intermittent disruption of blood flow such as cord prolapse, fetal blood loss through cord hemorrhage, intrinsic cord abnormalities, and entanglement of the cords in the case of monochorionic twins Umbilical cord torsion has been reported as a cause of fetal death and is seen most frequently at the fetal end of the cord. Umbilical cord abnormalities accounted for 10% of possible or probable causes of death and were more common in stillbirths of greater than 32 weeks’ gestation. Diagnosis and Evaluation A complete postmortem evaluation is recommended in all cases of stillbirth Autopsy has been found to provide information on a cause of death in over 30% of cases Genetic evaluation should be offered in all cases of stillbirth An abnormal fetal karyotype has been noted in 6% to 13% of all stillbirths tested Prevention of Stillbirth Improved treatment of maternal medical disorders such as diabetes and hypertension has clearly decreased the risk for stillbirth in these situations. The risk for stillbirth associated with APS is decreased with treatment (prophylactic heparin or lowmolecularweight heparin and low-dosage aspirin).