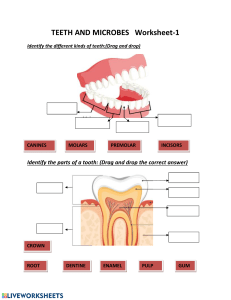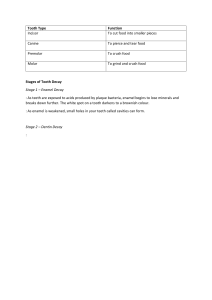
Propaedeutics of Dental disease Topic 10 By: Shakiba Motevalli Nikdad Dousthagh Introduction The purpose of the examination of any patient is to establish a diagnosis of based on a thorough analysis of complaints, anamnesis and objective examination. Examination of the patient, as a rule, begins with a survey, clarification of complaints and history of the disease, suffered and concomitant diseases, allergic status. Survey data allow the laundry from the very beginning to assume the correct diagnosis (preliminary) and outline further methods of examination. They find out the complaints and history of the disease. During the survey, it is necessary to establish trusting contact with the patient, determine his neuropsychiatric status, intelligence and, on this basis, analyze complaints, the course of the disease. The doctor with leading questions should help the patient to present his medical history. Methods of examination of the patient These reaserches methods are divided into basic and additional. • The basic (main) ones consist of clarifying complaints, collecting anamnesis, including the development of a real disease, carried out earlier treatment, its effect.. An objective examination of the patient includes an external examination of the face and neck, palpation examination of the perimaxillary soft tissues, organs and bones of the head and brain parts of the skull, determination of opening functions and closing of the mouth, palpation of the oral cavity and its components, palpation and percussion of the teeth. • Additional ones include various instrumental and laboratory research methods. The main methods • Examination of the oral cavity They begin with examining the vestibule of the mouth with closed jaws and relaxed lips, raising the upper and lowering the lower lip or pulling the cheek with a dental mirror. First of all, the red border of the lips and the corners of the mouth are examined. On the inner surface of the lip, as a rule, an insignificant bumpy surface is determined, due to localization in the mucous layer of small salivary glands. Then, using a mirror, examine the inner surface of the cheeks. It's pale yellow nodules with a diameter of 1 - 2 mm, sometimes visible only when the mucous membrane is pulled. At the level of the upper second large molars (molars) there are papillae, on which the excretory ducts of the parotid salivary glands open. After examining the oral cavity, the gums are examined. Normally, it is pale pink, tightly covers the neck of the tooth. The gingival papillae are pale pink and occupy the interdental spaces. A groove is formed at the place of the dentogingival junction. Due to the development of the pathological process, the gingival epithelium begins to grow along the root, forming a clinical, or periodontal pocket. The condition of the formed pockets, their depth, the presence of tartar is determined using an angled bulbous probe or a probe with notches applied every 2–3 mm. Examination of the gums allows you to determine the type of inflammation (catarrhal, ulcerative necrotic, hyperplastic), the nature of the course (acute, chronic, in the acute stage), prevalence (localized, generalized nose), severity (mild, moderate, severe gingivitis or periodontitis) inflammation. There may be an increase in the size of the gingival papillae due to their swelling, when a significant part of the tooth is covered. Then proceed to the examine of the oral cavity itself. First of all, a general examination is performed, paying attention to the color and moisture content of the mucous membrane. Normally it is pale pink. however, it may become hyperemic, edematous, and sometimes takes on a whitish hue, which indicates the phenomenon of para- or hyperkeratosis. Inspection of the tongue begins with determining the condition of the papillae, especially if there are complaints of changes in sensitivity or burning and soreness in any areas. Coating of the tongue may be observed due to a slower rejection of the outer layers of the epithelium. Such a phenomenon may be a consequence of a violation of the activity of the gastrointestinal tract, and possibly pathological changes in the oral cavity in candidiasis. Sometimes there is an increased desquamation of the papillae of the tongue in some area (more often at the tip and lateral surface). This condition may not disturb the patient, but pain may occur from irritants, especially chemical ones. With atrophy of the papillae of the tongue, its surface becomes smooth as if polished, and due to hyposalivation, it becomes sticky. Separate areas, and sometimes the entire mucous membrane can be bright red or crimson. This condition of the tongue is observed in pernicious anemia and is called Günther's glossitis. Hypertrophy of the papillae may also be noted, which, as a rule, does not cause concern to the patient. Hypertrophy of the papillae of the tongue is often combined with hyperacid gastritis. When examining the tongue, it should be remembered that the root of the tongue on the right and left has pink or bluish-pink lymphoid tissue. In the same place, the pattern of veins is sometimes clearly visible due to their varicose expansion, but this symptom has no clinical significance. When examining the tongue, pay attention to its size. With an increase in size, the time of manifestation of this symptom (congenital or acquired) should be determined. It is necessary to distinguish macroglossia from edema. The tongue may be folded in the presence of a significant number of longitudinal folds, however, patients may not be aware of this, since in most cases this does not bother them. Folding is manifested when the tongue is straightened. Patients take them for cracks. The difference is that with a crack, the integrity of the epithelial layer is broken, and with a fold, the epithelium is not damaged. Teeth Examination When examining the oral cavity, it is necessary to examine all the teeth, and not just the one that, in the opinion of the patient, is the cause of pain or discomfort. An examination of all teeth on the first visit is necessary in order to make a treatment plan, giving the highest improvement of the oral cavity. It is important that during the examination all changes in the tissues of the tooth are detected. It is recommended to develop a certain inspection system. For example, the inspection should always be done from right to left, starting with the maxillary teeth (molars) and then looking at the mandibular teeth from left to right. Inspection of teeth is carried out using a set of tools; the most commonly used dental mirror and probe (necessarily sharp). The mirror allows you to examine poorly accessible areas and direct the beam of light to the desired area, and the probe checks all the depressions, pigmented areas, etc If the integrity of the Enamel is not broken, then the probe slides freely over the surface of the tooth, not lingering in the depressions and folds of the enamel. In the presence of a carious cavity in the tooth (invisible to the eye), a sharp probe lingers in it. The contact surfaces of the teeth should be examined carefully, since it is not easy to differentiate an existing cavity from healthy chewing surface, while such a cavity can be detected by probing. Probing helps to determine the presence of softened dentin, the depth of the carious cavity, communication with the tooth cavity, the location of the holes of the canals, and the presence of pulp in them. Tweezer Probe The color of the tooth may be important in making a diagnosis. The teeth are usually white in color with many shades (from yellow to bluish). However, regardless of the shade, the enamel of healthy teeth is characterized by a special transparency. In a number of conditions, the enamel loses its luster characteristic and becomes dull. So, the beginning of the carious process is a change in the color of the enamel, the appearance of cloudiness first, and then a white carious spot. Depulped teeth lose their normal enamel luster, they acquire a grayish tint. A similar discoloration, and sometimes more intense, is observed in teeth in which pulp necrosis has occurred. After pulp necrosis, the color of the tooth can change dramatically. The color of the tooth can also change under the influence of external factors: smoking (dark brown color), metal fillings (tooth staining in dark color), chemical treatment of the canals (orange color after the resorcinol-formalin method). Pay attention to the shape and size of the teeth. It is known that some forms of dental anomalies (Hatchinson's teeth, Fournier's teeth) are characteristic of certain diseases. Percussion - tapping on the tooth - is used to determine periodontal conditions. A probe handle are tapped on the cutting edge or chewing surface of the tooth. If there is no inflammation in the periodontium, percussion is painless. In the presence of an inflammatory process in the periodontium from blows that do not cause discomfort in healthy teeth, pain occurs. When conducting percussion, the blows should be light and uniform. Percussion should begin with obviously healthy teeth, so as not to cause severe pain and to enable the patient to compare the sensation in a healthy and affected tooth. Distinguish between vertical percussion, when the direction of the blows coincides with the axis of the tooth, and horizontal, when the blows have a lateral direction. The mobility of the teeth is determined with tweezers by rocking. The tooth has physiological mobility, which is normally almost imperceptible. However, if the periodontium is damaged and there is exudate in it, pronounced tooth mobility occurs. There are three degrees of mobility: I degree - displacement in the weight of the tubular-oral direction II degree - displacement in the vestibular-oral and lateral directions III degree - displacement and along the axis of the tooth (in the vertical direction). The examination of the teeth is carried out regardless of certain complaints of the patient and their condition is fixed from right to left, first on the upper, then on the lower jaw. Use a mirror and a sharp probe to allows you to establish the integrity of the enamel or detect a cavity, mark its depth and size, as well as communication with the tooth cavity. Pay attention to the color of the teeth. The grayish and cloudy color of the tooth enamel may indicate pulp necrosis. The shape and size of the teeth are also important, including dental anomalies: Hutchinson's teeth, Fournier's, which may indicate general diseases and hereditary signs of pathology. While examining the teeth, their percussion is performed, mobility is determined with tweezers, the presence of supernumerary or milk teeth in a permanent bite, the eruption of the lower wisdom teeth, and the nature of the closing of the teeth are noted. Examine the gingival tubercles, determine the condition of the periodontium. The instrument is tapped on the cutting or chewing surface of the tooth (vertical percussion) and on the vestibular surface of the tooth (horizontal percussion). If pain is noted during percussion, this indicates the presence of an apical or marginal infection in the periodontium. They also perform palpation of the teeth, which allows to establish their mobility and soreness. Having captured the crown of the tooth with dental tweezers, the degrees of mobility are noted - I, II and III. With the help of a dental probe, gingival pockets, their depth, bleeding during probing, discharge from the pockets and their nature are determined. With tooth mobility, it should be clarified whether there is a localized process or a diffuse periodontal lesion, as well as to show oncological alertness. Pathological mobility of a row of teeth, combined with pain on percussion, may be one of the symptoms of osteomyelitis of the jaw.. The results of the examination of the teeth are recorded in a special scheme (dental formula), where milk teeth are denoted by Roman numerals, permenant teeth by Arabic. It is currently customary to designate the number teeth according to the international classification. The clinical examination of the patient should include a range of diagnostic methods and investigations. The type and size of them depend on the nature of the disease or injury of the maxillofacial region and the conditions of the examination (in the clinic or hospital), as well as the level of equipment of the medical institution Additional Methods • Additional research methods. • Electrodontodiagnostics (EDI). • Rentgendiagnostics (intraoral, panoramic). • Functional chewing tests, dental thermometry. • Laboratory research methods. Rules for filling • out a medical history Pulp tests definition Pulp tests play an important role in diagnosis of the status of pulp. Pulp tests are usually done before restorative treatment pulp that is non-vital is indicated for endodontic treatment. Pulp Vitality Testing: Assessment of the pulp's blood supply • Pulp Sensibility Testing: assessment of the pulp's sensory response • Pulp Sensitivity : condition of the pulp being very responsive to a stimulus. Pulp sensibility tests includes: *Electrical pulp test (EDI) *Thermal test *Bite test • Electrical pulp test (EDI): *this test is used for evaluation of condition of the pulp by electrical excitation of neural element within the pulp. *the pulp tester is an instrument which uses the graduation of electrical current to excite a response from the pulp tissue. *a positive response indicates the vitally of the pulp, no response indicates pulp necrosis (the probe can be placed in contact with natural teeth) Working method: *Before testing, clean, dry, and isolate the teeth, then place a small amount of tooth-paste or other conductor on the electrode. Be sure to follow your manufacturer's instructions for establishing an electrical circuit and to ensure accurate measurement with your instrument. *Starting with the adjacent tooth first, place one of the electrodes (black) on patient finger and other electrode (red) on the tooth to complete the electrical circuit then apply little electrical current and increase it slowly. *Turn on the device and slowly increase the electircal current and ask patient to tell you when he fails pain. Each tooth should be tested 2-3 times and the results are compared. If the results are not definitive, test the adjacent tooth and tooth on opposite arch. If patient feels pain then tooth is vital, if no pain is felt then tooth is not-vital. Use another technique in combination with electrical pulp testing to reach a reliable diagnosis. Thermal test : Thermal testing, which involves the application of either hot or cold stimuli to the tooth, is the most common form of sensibility test Types of thermal test: 1) Heat Test Starting with the adjacent tooth first, place hot instrument (e.g., burnisher) or hot material (e.g., heated gutta-percha) over the cervical third of the tooth, so that conductivity to pulp is fast. Three conditions exist: *Patient feels immediate pain, that last for 1-3 seconds after removal of the heated instrument, indicate vital pulp. *Patient feels immediate severe pain, that last for several minutes after removal of the heated instrument indicate irreversibily inflammed pulp. *Patient feels nothing, indicate non-vital pulp. Methods of the heat test: *The easiest method is to directed theworm air to the exposed surfaces of the tooth and noted the patient response. *If the higher temperature is needed to illicit a response , then other option is needed i.e heated stopping sticks hot burnisher, hot water ect. can be used *Heated gutta percha sticks is most commonly used method for heat test.Tooth is coated with a lubricant such as petroleum jelly to prevent gutta percha from adhering to the tooth surface.The heated gutta percha is applied at the junction of cervical and middle third of the facial surfaces of tooth and patient response is noted. * The other methods of heat testingfrictional heat produced by rotating polishing rubber disk , deliver warm water from syringe (especially useful of teeth with the porcelain or full coverage restoration.) 2)Cold Test Start with adjacent tooth first, place an ice stick on the cervical area of the tooth where enamel is thin, so that conductivity to pulp is fast. Three conditions exist : *Patient feel immediate pain, that lasts for 1-3 seconds after removal of the ice stick., Indicate vital pulp *Patient feel immediate severe pain, that lasts for several minutes after removal of the ice. Indicate irreversibly inflammed pulp *Patient feels nothing, indicate non-vital pulp Methods of application : *Isolation the tooth with rubber dam this is mandatory with all types, it recommended when uses icesticks due to melting ice run to the adjacent teeth and gingival result false positive result. *Spraying cold air directed to the isolated tooth *Application of cotton pellete saturated with ethyl-chloride *Spray of ethyl chloride after isolation the tooth with rubber dam.(The ethyl chloride evaporated so rapidly that it absorbs heat and thus , cools the tooth). Bite test : • This test helps if patient complains of pain on mastication Patient feel pain on biting if pulp necrosis has reached to PDL space or periapical area, or there is vertical fracture in the tooth. symptoms associated with incomplete fractures of posterior teeth. Bite tests can be performed using orange wood sticks, cotton wool rolls, rubber abrasive wheels such as Berlew wheels, or the head of number 10 round bur in a handle of cellophane tape. When using orange wood sticks to determine cracks, the patient is asked to bite on individual cusps separately. This helps to isolate the fractured cusp. • • X-ray (intraoral, panoramic): 1. Panoramic : Panoramic radiography is an extraoralradiography modality that provides two-dimensional information about the teeth and the maxillofacial skeleton. The Panoramic Radiograph is a combination of series of individual images which are combined to form a single Radiograph, The patient is made to stand in the middle of the X-Ray Machine and the X-ray tube head rotates around the head of the patient 360 degrees taking multiple images and a software stitches them together to form a single Radiograph showing the .Maxilla, mandible and other supporting structures Indications Indications for panoramic radiography imaging are : *Periodontal disease with simultaneous evaluation of all teeth and the extent of periodontal bone defects. *Orthodontic evaluation including presence of teeth germs, developmental stage of the dentition and the presence of retained, supernumerary or impacted teeth. *Impacted third molars *Dental age estimation *Lesions such as tumors, cysts, and other bone diseases that cannot be entirely imaged by periapical radiographs *Mandibular trauma *Implant planning Materials/instruments : Lead apron Bite piece Chin support Cotton roll (optional) Single use protective sleeve Disinfectant solution spray Step stool Panoramic machine Camera (optional) Ruler (optional for TMJ tomography) Way of Patient preparation : • Instruct the patient to remove all metallic objects including removable orthodontic appliances, removable prostheses, piercings, glasses, necklaces, hearing aids and hair pins to prevent artefacts from the radiographed site.When the local legislation mandates the use of a lead apron during X-ray exposure, a lead apron with the longer side on the patient’s back or a two-sided apron is used. If the patient’s guardian accompanies the patient during the exposure, he/she should also wear a lead apron. • Advantages : 1.Better patient acceptance. . Patients can easily stand or sit during the panoramic X-ray examination that can be performed once 2.Easier for the dentist and staff. Dentists can now consistently open up the contacts between the posterior teeth simply by adjusting the panoramic positioning light, compared to setting up a sensor in a holder, placing it in the patient’s mouth, aiming the X-ray machine, and repeating .several of these steps for each of the subsequent bitewing exposures 3.Faster. The panoramic technique requires fewer steps than traditional dental X-rays. Dentists or staff members can turn on the machine, have the patient bite into the groove in the bite block, and seconds later have images ready for viewing 4.More diagnostic 5.Less radiation exposure 6.Less infection control. Using the panoramic machine requires no gloves and virtually no between-procedure cleaning or infection control — only replacement of the bite block sleeve, which the patient removes Disadvantages : 1. Images are not as sharp as Intraoral radiograph, as it is made up of multiple stitched images the sharpness and clarity are reduced. Due to the reduced sharpness and clarity, it cannot be used to diagnose caries. 2. It cannot be used to determine interdental bone loss due to the same factors (low sharpness) and also the cahnges in Periodontal ligament are misleading. 3. In most Panoramic radiographs the anterior segment (mandibular) is either overlapped or blurry and not clear. 2. Intraoral: There are 4 methods of intraoral radiography: • radiography of periapical tissues according to the isometric projection rule Isometric imaging is used to assess periapical tissues, however, they give distortions in magnitude, which can lead to over- or under-diagnosis. • interproximal Interproximal radiographs show teeth, periapical tissues, marginal areas of both jaws. • shooting in bite or occlusion Occlusal radiography allows you to get a picture of the site of the alveolar process. Most often, this projection will give an idea of the cortical plate of the alveolar process from the vestibular and lingual sides, including the thickness of the periosteum. In another plane, one can judge more accurately about the pathology: cysts, impacted teeth, jaw fracture lines, the presence of a foreign body (calculus) in the submandibular and sublingual salivary glands. Occlusal images are produced in addition to the previous ones • radiography from an increased focal length with a parallel beam of rays Long-focus radiography is performed on devices. having a more powerful X-ray tube and a long localizer cone. The method is used mainly to display the marginal sections of the alveolar processes, the structure of bone tissue, the shape of the roots and the presence of destructive changes around them. Medical Record According to the record, one can judge the effectiveness and correctness of the treatment. This section is filled in at the reception desk and when the patient first visits the polyclinic. All subsequent sections are completed by the physician. The column <<Diagnosis" is filled in by the attending physician as the final diagnosis after collecting an anamnesis, examination and, if necessary, additional research methods. In some cases, the diagnosis may be clarified or even replaced, but the date must be indicated. However, in all cases, the diagnosis should be specified in accordance with existing classifications. In the column <<Development of the present disease" it is necessary to indicate the appearance of the first signs of the disease, the nature of the course, treatment and its effectiveness. The results of laboratory and OTHER methods of research should be entered in the card. A special section of the map is devoted to the preparation of a treatment plan. This is important to do on the first visit to the patient, which allows for a complete and comprehensive treatment. The presence of a treatment plan is also necessary because the patient, for whatever reason, may go to another doctor. In the Diary section, a brief but clear entry is made about the patient's condition and the result of the treatment. Medical record as a legal and scientific document in the course of The information is stored in the registry for 5 years, and then it is archived. For the convenience of recording the result of the examination of the teeth, special schemes (dental formula) are used. • There are several such schemes. In Russia, a scheme is used in which the horizontal line indicates whether the teeth belong to the upper or lower jaw, and the vertical line indicates whether the teeth belong to the right or left side. At the same time, permanent teeth are usually denoted by Arabic numerals: Laboratory Research methods Laboratory research with a diagnostic need includes a large number of different methods carried out both in a clinic and in a hospital. In a polyclinic, their use is limited. As a rule, they produce general blood and urine tests, determination of their glucose content, cytological and morphological studies. In basic dental and general clinics and other studies can also be additionally carried out. Before the operation in the clinic, the doctor must refer the patient for a blood test for RW, HIV infection, the presence of hepatitis A, B, C viruses, and, if necessary, other blood tests, urine, feces. Before operations in a hospital, in addition to the above methods, laboratory tests are mandatory: they determine the blood group and Rh factor, the glucose content in blood and urine, and coagulation parameters Thanks for your attention