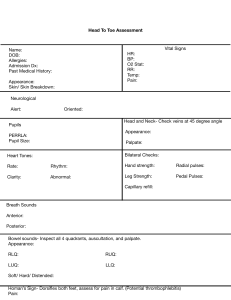
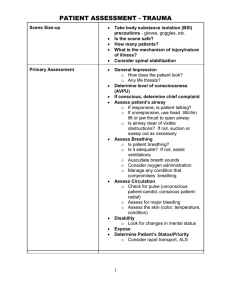
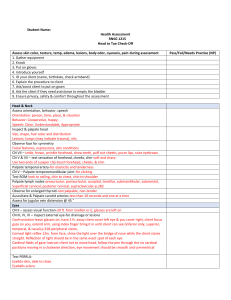
Head-to-Toe Assessment Equipment Checklist Basic equipment includes: Gloves Thermometer Blood pressure cuff Watch Scale Height wall ruler Tape measure, Penlight Stethoscope Additional equipment for more comprehensive examinations would include, Otoscope Ophthalmoscope Reflex hammer Tongue depressor Sterile sharp object (like toothpick or pin) Sterile soft object (like cotton ball) Something for the patient to smell (like an alcohol swab) How to Conduct a Head-to-Toe Assessment Step 1: Establish Trust When beginning an assessment, “establishing a personal relationship of trust and respect between the patient and the nurse is vital.” It is important throughout an assessment to assess how the patient is doing, and make sure they are properly draped and comfortable. You'll want to introduce yourself to the patient and explain the assessment process Step 2: Confirm the patient’s ID Step 3: Note The patient's Appearance and Status During an assessment, the first thing that should be noted is the patient’s overall appearance or general status. This includes level of alertness, state of health/comfort/distress, and respiratory rate. This is done even prior to taking vital signs. Step 4: Assess the ABCs Prior to starting a detailed assessment, you'll want to assess the ABC's - airway, breathing, and circulation. Usually, the assessment begins with the least invasive to most invasive, allowing time for the patient to become more comfortable with the examiner. It also increases the likelihood that the examiner will not forget a system during the exam. Step 5: Look for Abnormalities Differentiating normal from abnormal is an important skill. Some examples of major abnormal findings are changes in normal respiratory rate that indicates respiratory distress, or a change in skin color such as pallor that may indicate anemia or jaundice that typically indicates liver problems. Generally, the human body is bilaterally symmetrical. When you are examining a patient, make note of any unusual asymmetry. If a patient is weaker on one side than another, or has a limited range of motion, or one side seems limper or otherwise different from the other side, there could be an underlying neurological or musculoskeletal issue. The Order of a Head-to-Toe Assessment Assessment Area: General Status Vital signs Heart rate Blood pressure Temperature Pulse oximetry Respiratory rate Pain Assessment Tasks: Assess pain using the appropriate pain scale for the patient Assessment Area: Head, Ears, Eyes, Nose, Throat (HEENT) Observe head tilt Inspect skull and scalp Inspect facial features Palpate head and scalp Auscultate temporal arteries if appropriate Observe the color of lips and moistness Inspect teeth and gums Assess buccal mucosa and palate Examine Tongue Examine at uvula Examine tonsils Palpate nose and assess symmetry Check Septum and inside nostrils Verify patency of nares Check patient’s sense of smell Palpate sinuses Assess patient hearing with whisper test Tuning Fork test (Weber’s test, Rinne test) Look inside ear Assess ear discharge and tympanic membrane Check conjunctive and sclera Assess eye symmetry PERRLA Check vision with Snellen Chart Check six cardinal positions of the gaze Assessment Tasks: Check for size, shape, symmetry, lesions, trauma Check for thickening, hardness, and tenderness Observe for masses, webbing, and skinfolds Assessment Area: Neck Palpate lymph nodes: o Parotid and retropharyngeal (tonsillar) o Submandibular o Submental o Sublingual (facial) o Superficial anterior Cervical o Superficial posterior cervical o Preauricular and postauricular o Sternocleidomastoid o Occipital o Supraclavicular Observe and palpate trachea and neck Check for Jugular Venous Distention Check neck range of motion Check shoulder shrug with resistance Assessment Tasks: Check for symmetry, tenderness, shape Check thyroid for size, shape, configuration, tenderness, nodules Assessment Area: Respiratory Inspect the chest Perform direct and indirect percussion on the chest Listen to lung sounds front and back Assess respiratory expansion level Ask about coughing Palpate thorax Assessment Tasks: Observe chest for size, shape, symmetry, color, superficial venous patterns, and prominence of ribs Evaluate respirations for rate and rhythm Palpate for thoracic expansion, tactile fremitus Listen for intensity, pitch, duration, and quality of breath sounds Assessment Area: Cardiac Palpate the carotid and temporal pulses bilaterally Auscultate the five areas of the heart Inspect the precordium Assessment Tasks: Assess for murmurs Listen for heart rate, rhythm, S1 and S2 Assessment Area: Abdomen Inspect abdomen Listen to 4 quadrants of the abdomen for bowel sounds Palpate 4 quadrants of the abdomen for pain/tenderness Percuss the 4 quadrants of the abdomen Ask about problems with bowel or bladder Assessment Tasks: Check for skin characteristics, venous patterns, symmetry, surface motion Check for masses, hernia, separation of the muscles Listen for bruits Check for tone, liver borders Assessment Area: Pulses Palpate pulses in arms/legs/feet including: o Brachial (in infants) o Radial o Femoral o Posterior tibial o Dorsalis pedi Assessment Tasks: Ensure pulse are palpable and present Assessment Area: Extremities Assess range of motion and strength in arms/legs/ankles Assess sharp and dull sensation on arms/legs Check capillary refill on fingernails/toenails Palpate each joint in the hand and write Assessment Tasks: Check for muscle tone, warmth, tenderness, swelling, and crepitus Check for alignment, size, deformities, contour and symmetry Assessment Area: Skin Check skin turgor Check for lesions, abrasions, rashes Check for tenderness, lumps, lesions Check if the patient is pale, clammy, dry, cold, hot, flushed Assessment Tasks: Check for moisture, temperature, texture, turgor, elasticity Check for color, distribution, density Identify pigmentation, length, redness, swelling, pain, growths Assessment Area: Neurological Test cranial nerves I through XII Evaluate balance using the Romberg test Evaluate coordination and fine motor skills Test primary sensory responses Oriented x3 Assess gait Assess superficial and deep tendon reflexes Check the Glasgow Coma Scale score Assessment Tasks: Gait: posture, rhythm, sequence of stride and arm movements Check for superficial touch and superficial pain response FAQs: What 4 techniques are used in a head-to-toe assessment? o How do you do a head-to-toe assessment? o To perform a thorough head-to-toe assessment, it is recommended that you start with an overall inspection of the patient and then move to the head, ears, eyes, nose and throat. Then, move your way down the body systematically. You will need to include the four techniques of inspection, palpation, percussion, and auscultation throughout the assessment. What is the purpose of a head-to-toe assessment? o The four techniques that are used for physical assessment are inspection, palpation, percussion, and auscultation. The purpose of a head-to-toe assessment is to get a baseline understanding of your patient. This assessment can be used in case there is an emergency or a change in their physical or emotional behavior. It also can be used to help diagnose a disease or illness. What should the nurse begin by assessing when performing a head-to-toe assessment? o This will depend on the patient. Typically, the first thing a nurse should do is look or inspect. Use your eyes to look at your patient’s skin, breathing, and outward appearance before moving on to more invasive aspects of the assessment. However, it is best to start at the head for a systematic top-to-bottom approach.