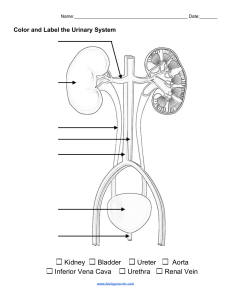
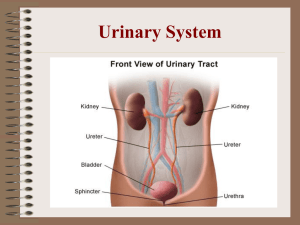
Patho Exam 1 Cell and Genetics Ribosomes: Protein synthesis. Endoplasmic reticulum: Synthesis of protein and transport, and synthesis of lipids. Golgi apparatus: Processing and packaging of proteins. Lysosomes: Digesting cellular substances. Mitochondria: Cellular respiration to produce ATP. Cytoskeleton: “bones and muscle” of the cells. Energy metabolism: Chemical tasks of maintaining cellular functions. Anabolism and catabolism. Anabolism: E-using process; build molecules. Catabolism: E-releasing process; converts carbohydrates, fats & proteins into energy needed for cell function. Passive transport: Diffusion: Movement of solutes from area of greater concentration to area of lesser concentration (down concentration gradient). Do not need energy. • Facilitated Diffusion: A membrane protein facilitates the diffusion. • Passive Diffusion: No protein involved. Substance diffuses across the plasma membrane, oxygen, alcohol, CO2. Osmosis: Is the movement of water down a concentration gradient. Occurs across a semipermeable membrane from a region of higher water concentration to one of lower concentration. Active transport: Transport of a molecule across a plasma membrane against its concentration gradient (up). Always need energy and a membrane protein. Four types of tissues: • Epithelial: Covers most of internal and external body surfaces. Simple squamous epithelium, transitional epithelium, stratified squamous epithelium, simple cuboidal epithelium, simple columnar epithelium, stratified columnar epithelium. • Connective: Binds tissues and organs together. Adipose, cartilage, bone, blood. • Nerve: specialized cells neurons, and glia. • Muscle: Composed of myocytes. Striated, Cardiac, Smooth. Atrophy: Decrease in cellular size. Thymus gland, gonads, disuse atrophy. Hypertrophy: Increase in cell size due to mechanical stimuli. Myocyte enlargement in cardiac hypertrophy. Hyperplasia: Increase in the number of cells. Hepatocytes after removal part of the liver Metaplasia: Replacement of one mature cell by another. Columnar ciliated epithelial cells of the airway by stratified squamous epithelial cells (loss of protective mechanism). Can be reversed if smoking is removed. Dysplasia: Abnormal changes in the size, shape and organization of mature cell. Not a true adaptive change. Does not indicate cancer and may progress to cancer. Epithelial tissue of the cervix. Marfan Syndrome: Autosomal Dominant. Connective tissue disease. Retinal detachment, myopia. Mitral valve prolapse, aortic valve disease, weakness of the aorta. Joint hypermobility, spinal deformities, pigeon chest. Cystic Fibrosis: Autosomal recessive. Mutation in Gene CFTR (Cystic Fibrosis Transmembrane Regulator) on chromosome 7. Test: Sweat test shows elevated chloride. Organs affected by cystic fibrosis: nutrients. Phenylketonuria (PKU): Autosomal recessive. Defect in amino acid metabolism: Inability of the body to convert the essential amino acid phenylalanine to tyrosine (a precursor to melanin). Accumulation leads to mental retardation: elevated phenylalanine is- thought to reduce the IQ. Treatment: Diet restriction of phenylalanine. Tay-Sachs Disease: Autosomal recessive. Accumulation of glycolipids in the brain neurons & retina due to failure of lysosome (enzyme) function. Blindness, seizures, death occurs by 2 to 5 years. Predominately in Eastern Jews population, 1: 30. Cherry red spot on the retina = TaySachs disease. X-linked recessive disease: Usually males more affected because females have another X chromosome to counteract the abnormal gene. Affected males cannot transmit the affected gene to sons but they can to all daughters. Down’s Syndrome/Trisomy 21: Protruding tongue, Flat nasal bridge, Small ears, Single palmar (simian) crease, Mental retardation, Heart problems. Turner Syndrome: Partial or total inactivation of X chromosome. Have 45 chromosomes - 22 pairs of autosomes and 1 sex chromosome - usually the X (missing the second sex chromosome). Short stature and webbing of neck, Lack of secondary sex characteristics, underdeveloped breast. Absent ovaries, amenorrhea, sterile. Coarctation of aorta and bicuspid aortic valve. Normal intelligence, but may have difficulty driving, nonverbal problem solving, math. Fluids and Electrolytes Intracellular Compartment (ICF): Consists of fluid contained within all of the billions of cells in the body. Larger of the two compartments, with approximately two thirds of the body water in healthy adults. High concentration of K+. Extracellular Compartment (ECF): Contains the remaining one third of body water. Contains all the fluids outside the cells, including that in the interstitial or tissue spaces and blood vessels. High concentration of Na+ and Cl-. Osmolarity of the extracellular fluid is almost entirely due to Na. Osmolarity of the intracellular fluid is related to many particles and K is the primary electrolyte. If either ECF or ICF changes in concentration, fluid shifts from area of lesser concentration to area of greater concentration. Organs involved in fluid-electrolyte balance: Kidneys, lungs, heart, adrenal glands, parathyroid glands, pituitary gland. Solutions can be classified according to whether they cause cells to shrink: Isotonic: neither shrink nor swell. Hypotonic: swell. Hypertonic: shrink. Antidiuretic Hormone (ADH): Increases water reabsorption into the plasma. Natriuretic Peptide (ANP, BNP): Increases excretion of sodium by the kidneys. Renin Angiotensin Aldosterone System (RAAS): Aldosterone leads to sodium and water reabsorption back into the circulation and excretion of potassium. SODIUM (Na): Major cation in the ECF. 135-145 mEq/L. Primary determent of plasma osmolality. Essential for nerve impulse transmission, muscle contraction and the movement of glucose and amino acids. Hyponatremia: Serum sodium level <135 mEq/L. Sodium deficits cause plasma hypoosmolality and cellular swelling. Sodium imbalances usually are associated with fluid volume imbalances. Most common electrolyte disorder. Older adult population at higher risk. Causes: Pure sodium loss, low intake, diuretics, diaphoresis, GI loss. Early signs are muscle cramps, weakness, and fatigue (heavy exercise). Nervous system is most seriously affected: lethargy, headache can progress to disorientation, confusion, seizures and coma. If leads to loss of ECF and hypovolemia: hypotension, tachycardia, decreased urine output. If dilutional from excess water (hypervolemic hyponatremia), see weight gain, edema, ascites, jugular vein distention. Hypernatremia: Serum sodium level >145 mEq/L. Caused by Cushing syndrome, Renal failure, hyperaldosteronism, Excessive oral sodium ingestion, Hypertonic saline solutions, NPO, Infants, elderly, comatose, Severe burns or fever, Diabetes insipidus Watery diarrhea. Thirst is the early symptom. Decreased urine output, Increased urine osmolality, Increased serum osmolality, Dry skin and mouth, Seizures, Tachycardia. POTASSIUM (K): Major intracellular cation. Normal serum level 3.5-5.0 mEq/L. Concentration maintained by Na+/K+ pump. Essential for transmission and conduction of nerve impulses, normal cardiac rhythms, and skeletal and smooth muscle contraction. Aldosterone, insulin, and epinephrine influence serum potassium levels. Hypokalemia: Potassium level <3.5 mEq/L. Caused by reduced intake of potassium, increased entry of potassium into cells (i.e. hyperinsulinism), steroid administration, Cushing’s syndrome. Increased loss of potassium (GI, Renal; losses: diuretics, diarrhea, vomiting, NG suction). Membrane hyperpolarization causes a decrease in neuromuscular excitability: skeletal muscle weakness, smooth muscle atony, cardiac dysrhythmias. Muscle paralysis with life-threatening respiratory insufficiency (K<2.5mEQ/L). EKG changes: Prolong PR interval, depression of the ST segment, flattening of the t-wave, prominent U wave. Hyperkalemia: Potassium level >5.0 mEq/L. Caused by increased intake, shift of K+ from ICF into ECF (acidosis), decreased renal excretion (potassium sparing diuretics, renal failure, Addison’s disease), cell trauma. CALCIUM (Ca): Serum concentration 8.5 to 10.5 mg/dl. Necessary for structure of bones and teeth, blood clotting, hormone secretion, cell receptor function, plasma membrane stability, transmission of nerve impulses, muscle contraction. Rigidly controlled by parathyroid hormone (PTH removes calcium from the bone when levels are low), vitamin D (maintains plasma levels by increasing absorption from the intestine), and calcitonin (Removes calcium from ECF acting on bone and kidney). Hypocalcemia: Serum calcium level less than 8.5 mg/dl. Caused by inadequate oral intake, lactose intolerance, Low vitamin D, Malabsorption syndromes (Crohn’s disease), renal failure, diarrhea, hyperphosphatemia, hypoparathyroidism (common when removal of thyroid glands, surgeon also removes parathyroid by mistake). Manifestations: Chvostek’s sign is twitching of facial nerve in response to a tap on the nerve. Trousseau’s sign is spasm of forearm on obstruction of its blood supply. Tetany, muscle twitching and arrythmias. Hypercalcemia: Serum calcium > 10.5 mg/dl. Caused by excessive intake of calcium and or vitamin D, thiazide diuretics, hyperparathyroidism, malignant neoplasm. Tachycardia in early phase and Bradycardia in late phase. EKG changes: shortened ST segment; widened T wave. Polyuria: Increase urine output leading to dehydration. Formation of renal calculi. PHOSPHATE (PO4): Normal value 2.5-4.5 mg/dl. Like calcium, most phosphate is also located in the bone. Provides energy for muscle contraction. Parathyroid hormone, vitamin D3, and calcitonin act together to control phosphate absorption and excretion. Hypophosphatemia: Caused by Intestinal malabsorption, Vitamin D deficiency, long term alcohol abuse, malnutrition, respiratory alkalosis, hyperparathyroidism. Muscle pain and weakness. Mental changes: irritability, confusion, numbness, coma, convulsions. Hyperphosphatemia: Caused by increased intake, decreased renal excretion, Hypoparathyroidism. Primarily related to low serum calcium levels (caused by high phosphate levels) similar to the results of hypocalcemia. MAGNESIUM (Mg): Serum concentration 1.5 to 2.5 mEq/L. Increases neuromuscular excitability. Hypomagnesemia: Caused by malnutrition, gastric suction, malabsorption syndromes, Alcoholism. Anorexia, neuromuscular irritability, increased reflexes, depression, disorientation. Hypermagnesemia: Caused by renal insufficiency or failure, excessive intake of magnesium-containing antacids. Lethargy and drowsiness, hypotension, muscle weakness, decreased deep tendon reflexes, decrease respirations, bradycardia. Acid-Base Balance Acid-base balance is determined by the hydrogen ion concentration in body fluids. Involves three systems: Chemical buffer system (HCO3-H2CO3), Kidneys (HCO3), Lungs (CO2). normal pH (7.35-7.45). The most important plasma-buffering systems are the carbonic acid (H2CO3) – bicarbonate (HCO3) pair. Normally there are 20 parts of bicarbonate (base) to 1 part of carbonic acid (acid). Bicarbonate and carbonic acid can increase or decrease, but the ratio must be maintained to maintain the pH. When the pH is altered, two systems can compensate: The respiratory system compensates by increasing ventilation to expire carbon dioxide (CO2) or by decreasing ventilation to retain carbon dioxide. The renal system compensates by producing acidic or alkaline urine (regulating the amount of bicarbonate (HCO3-) and H+ retained or excreted). It is a slow compensatory mechanism. The normal PaCO2 is 35 to 45 mm Hg. Increasing ventilation increases pH by eliminating CO2. Decreasing ventilation decreases pH by retaining CO2. HCO3 normal value is between 21-28 mEq/L. Kidney regulates pH of ECF If pH is low: Elimination of H+ in urine, Reabsorption of HCO3, Production of new HCO3. Metabolic Acidosis: Caused by Diabetic Ketoacidosis, overdose of ferrous sulfate, renal failure (uremia), severe diarrhea, pancreatic fistulas, excessive acetazolamide or ammonium chloride. Symptoms: Headache, decreased BP, Hyperkalemia, muscle twitching, warm flushed skin, nausea, vomiting, diarrhea, confusion, Kussmaul Respirations (compensatory hyperventilation). Metabolic Alkalosis: Caused by increased bicarbonate administration, excess loss of acid via kidneys or GI (Severe Vomiting), Hypokalemia, Hypochloremia. Symptoms: Confusion, compensatory Hypoventilation, Nausea, and severe vomiting. Respiratory Acidosis: Caused by hypoventilation, acute disorders of ventilation, weakness of respiratory muscles, COPD, Pulmonary fibrosis, sepsis, burns, fever. Symptoms: Hypoxia, skin and mucosa cyanotic or pale, hyperkalemia, disorientation, headache, dysrhythmia. Respiratory Alkalosis: Caused by Hyperventilation. Anxiety, pain, sepsis, fever, salicylate toxicity, encephalitis. Symptoms: numbness or tingling in the face, hands and feet. Tinnitus, lethargy, seizures, hypokalemia, tachycardia. Mixed Acidosis or Alkalosis: Results when 2 or more primary acid-base disorders are present simultaneously. Example: COPD + diarrhea = respiratory acidosis + metabolic acidosis. Renal System Kidneys receive 25% of cardiac output during rest; reduced during physical or emotional response. Uremia indicates urea in blood. Azotemia also indicates high levels of urea (no S&S). Creatinine is a product of creatine metabolism by the muscle. It is filtered by the kidneys and not reabsorbed in the renal tubule. Creatinine levels in the blood and urine are used to measure glomerular filtration rate (GFR). In CKD, as GFR declines and plasma creatinine increases. Glomerular filtration rate (GFR) describes the flow rate of filtered fluid through the kidney. Glomerular filtration rate is the best test to measure your level of kidney function and determine the stage of kidney disease. Urinary Tract Obstruction: Interference with the flow of urine at any site along the urinary tract. The obstruction can be caused by an anatomic or functional defect. Can lead to renal failure (post-renal failure). Caused by renal calculi, a neurogenic bladder (no mechanical, CNS or PNS), cancerous tumors. Hydroureter – Accumulation of urine in the ureter. Hydronephrosis – Enlargement of the renal pelvis and calyces. Ureterohydronephrosis - abnormal enlargement of the ureter and kidney. Upper Urinary Tract Obstruction: Results in dilation of the ureter, renal pelvis, calyces and renal parenchyma due to backing up of the urine. Causes: congenital abnormalities, inflammation, tumors, metabolic conditions, kidney stones-calculi or urinary stones (most common). Renal stones-Calculi: Related to super-saturation of one or more salts in the urine, precipitation of the salts and growth: Urine becomes concentrated with insoluble materials. Crystals form from these materials and then consolidate, forming calculi. Calculi remain in the renal pelvis and damage or destroy kidney tissue or they may enter the ureter. If obstruct urine flow may cause hydronephrosis. Gender: Men > Women (men: up to 20%, women: 5-10%). Fluid intake: Persons who do not consume adequate fluids: DEHYDRATION. Diet- Excessive vitamin D and calcium ingestion. Lack of Exercise: IMMOBILITY. Four types of kidney stones: Calcium stones (i.e., oxalate or phosphate): 70-80% Struvite stones: infection. Uric acid stones: excrete excessive uric acid in the urine. Cystinuric stones. Symptoms: Dull aching flank pain: Renal Colic. May travel from lower back to sides and then pubic region and genitalia. Nausea, vomiting, hematuria. Diagnosis: Kidney ultrasound, 24-hour urine collection to retrieve and analyze calculi. Blood tests – to rule out causes/ Treatment: 90% are small and pass naturally with vigorous hydration (>3 L day). Drug therapy: Antimicrobials, Analgesics, Antiemetics. Remove calculi: Lithotripsy (breaks the stone in fragments). Lower Urinary Tract Obstruction: May involve the bladder, bladder neck, prostate, or urethra. Symptoms are related to alterations in urine excretion. neurogenic bladder (neurologic disorders) and/or anatomic alterations (urethral stricture, prostate enlargement, pelvic organ prolapse, obstruction of the bladder or urethra, low bladder wall compliance). Symptoms: Daytime voiding frequency, Nocturia, Incomplete bladder emptying. Tumors: Renal tumors may be small, benign tumors that are difficult to detect, or they may be larger malignant tumors that usually arise from the proximal tubule epithelial cells. Bladder tumors are common; they are the fifth most common malignancy. Renal Cell Carcinoma: Most common renal neoplasm (85%). Risk factors for RCC: tobacco, obesity, and long-term analgesic. Clinical Manifestations: Hematuria (most common), Flank pain, Palpable flank mass, Weight loss. Diagnosis through ultrasound, intravenous pyelography, Ct scan/MRI, Renal angiography. Bladder Tumors: Transitional cell carcinoma (most common). Clinical manifestations: painless hematuria. Most common in males older than 60 years and smokers. Urinary Tract Infections (UTI): Inflammation of the urinary epithelium caused by bacteria anywhere along the urinary tract. Most common bacteria is E. coli. Bacteria usually enter through the urethra. Risk Factors: Age extremes, sexually active women, indwelling catheter, lower urinary tract obstruction, diabetes mellitus, immunosuppression, spinal cord injury. Subjective symptoms include urgency, frequency, dysuria, lower abdomen/suprapubic pain, low back pain. Objective Symptoms include Nocturia, hematuria, pyuria, bacterial growth evident in urine culture. Pharmacologic therapy with antibiotics, urinary antiseptics, antispasmodics, antiinflammatory. Acute Cystitis: Is an inflammation of the bladder wall usually caused by an ascending bacterial infection (E. coli most common). More common in females due to shorter urethra, childbirth, anatomic proximity of the urethra to the rectum. Occur in men secondary to epididymitis, prostatitis, renal calculi. Urethritis: Is an inflammation of the urethra caused by staphylococci, E. coli, pseudomonas, and streptococci. Although inflammatory symptoms are similar to gonorrheal urethritis, sexual contact is not the cause. Urosepsis: Is caused by gram-negative bacteria. May result from an indwelling urinary catheter or an untreated urinary tract infection. Pyelonephritis: Presence of an infection (E. coli most common) of one or both upper urinary tracts (ureter, renal pelvis, and parenchyma) Common Causes: UTI, Kidney Stones, Vesicoureteral reflux, Pregnancy, Neurogenic Bladder, Instrumentation, Female Sexual trauma. Fever/Chills, Tachycardia and tachypnea, Flank or back pain/Tender costal vertebral angle (CVA), Abdominal, often colicky, discomfort, Nausea and vomiting, General malaise or fatigue, Burning, urgency, or frequency of urination, Nocturia. Glomerular Disorders: Affects the glomerulus and change the filtration properties of the kidney. In all types of glomerulonephritis, the epithelial (podocyte) layer is disturbed which changes the membrane permeability. Acute Glomerulonephritis: glomerular inflammation that can be caused or not by immune mechanisms. Immune injury: Deposition of circulating antigen-antibody immune complexes into the glomerulus (type III hypersensitivity) and reaction of antibodies in situ against antigens within the glomerulus (type II hypersensitivity). Nonimmune injury is related to ischemia, HTN, DM, SLE, toxins, vascular disorders and infection. Acute glomerulonephritis usually occurs after 7-12 days of infection with group A B-hemolytic streptococci and is caused by deposition of immune complexes. Proteinuria (varying degrees based on the specific disease). Albumin (macroalbuminuria) as the major protein. Hematuria with red blood cell casts. Renal Failure. Edema. Oliguria. Antibiotics such as penicillin to treat underlying infection that may be contributing to ongoing antigen-antibody responses Corticosteroids. Nephrotic Syndrome: Massive proteinuria, specifically defined as 3.5 g or more of protein per day. The protein excretion is caused by glomerular injury. Causes hypoproteinemia (hypoalbuminemia) which in return diminishes oncotic pressure resulting in edema. Compensatory synthesis of proteins by the liver causes Hyperlipidemia. Serum albumin < 3 g/dl. Nephritic Syndrome: Hematuria and red blood cell casts in urine. Proteinuria also occurs but is less severe than in nephrotic syndrome. It occurs primarily with infectionrelated glomerulonephritis. The classic diagnosis of nephritic syndrome is poststreptococcal glomerulonephritis. Proteinuria (less then nephrotic), hematuria, hypertension and edema. Treatment is high dose corticosteroids. Renal Failure: Occurs when renal function is impaired to 25% the normal function. Renal failure is classified into acute and chronic. Acute Renal Failure: Sudden decline in kidney function with a decrease in glomerular filtration and urine output with accumulation of nitrogenous waste products as demonstrated by an elevation in plasma creatinine and BUN. Usually follows trauma to the kidneys or overwhelming physiologic stress (e.g. burns, septicemia, nephrotoxic drugs and chemicals, severe shock, etc.) that decreases blood flow to the glomeruli or to the nephrons. o Prerenal Failure: Inadequate kidney perfusion. Heart failure, MI, Hypovolemia, burns, dehydration, diuretic overuse, trauma or tumor. Oliguria (<400ml/24 h). o Intrarenal Failure: Acute tubular necrosis (ATN): destruction of tubular epithelial cells (most common cause of intrarenal failure). Hypotension and nephron toxic drugs. Infections: Glomerulonephritis/Pyelonephritis. Causes renal capillary swelling and cellular proliferation. Oliguria. o Postrenal Failure: Occurs with urinary tract obstructions that affect the kidneys bilaterally. Bladder obstruction, Anti-cholinergic drugs, Autonomic nerve dysfunction, Tumors, Calculi: Ureteral obstruction (both) or urethral obstruction, Benign Prostatic hyperplasia (BPH) or tumor of the prostate. Oliguria. Chronic Renal Failure: Progressive inability, over months to years, of the kidneys to respond to changes in body fluids and electrolyte composition with an inability to produce sufficient urine. Gradual loss of nephron units. Kidneys adapt to loss of nephron mass and alterations may not show until renal function declines more than 75%. Stages: • I Normal (GFR >90 mL/min) • II Mild (GFR 60-89 mL/min) • III Moderate (GFR 30-59 mL/min) • IV Severe (GFR 15-29 mL/min) • V End stage (GFR less than 15) Urinary incontinence: Known as involuntary urination. Leakage of urine. Risk factors: Pregnancy, childbirth, menopause. Urge Incontinence: Due to an overactive bladder. Strong sudden need to urinate. Stress incontinence: Weakened pelvic floor (loss of urine during laughing, sneezing or coughing) Tx: Kegel exercises. Overflow Incontinence: Loss of urine with over distention of bladder. The bladder does not empty completely (example: enlarged prostate-BPH-). Functional Incontinence: Due to medications or health problems. Mental impairment keeps the person from making it to the toilet on time (during dementia, immobility). Musculoskeletal Bone Function: Mechanical support, protects organs, calcium metabolism, hematopoiesis. Joints: Where two bones meet. Synarthrosis immoveable (Cranium), Diarthrosis completely moveable (shoulder), Amphiarthrosis slightly moveable (vertebrae). Skeletal Muscle: Body movements, muscle tone, stabilize joints, maintain body temperature. Strains: Trauma to muscle or tendon. May involve tissue tear or ruptures. Inflammation. Sprains: Stressing or tearing the ligaments. Trauma to a joint. Inflammation. Avulsion: Complete separation of a tendon or ligament from its bony attachment site. Joint Dislocation: Subluxation (incomplete dislocation). Trauma. Popping noise, marked pain, swelling, loss of range of motion. Fractures: It is a break in the continuity of a bone. Pain, loss of function, deformity of the affected area, abnormal mobility. Reduction, immobilization, therapy. Complications include compartment syndrome and fat emboli. Bone Healing: Hematoma formation, Fibrocartilaginous callus formation, bony callus formation, remodeling phase. Hip Fracture: Maintain leg and hip in proper alignment and prevent internal or external rotation and extreme hip flexion. Turn the client to the unaffected side. AVOID HIP flexion greater than 90 degrees and avoid low chairs when out of bed. Neurovascular assessment of affected extremity. Check color, pulses, capillary refill, movement and sensation. Use antiembolism stockings and encourage the client to flex and extend the feet to reduce the risk of DVT. Intracapsular: Femoral head is broken within the joint capsule. Femoral head and neck received decreased blood supply and heal slowly. Extracapsular: Fracture is outside the joint capsule. Fracture can occur at the greater trochanter or can be a subtrochanteric fracture. Osteoporosis: Density or mass of bone is reduced. Results in increased porosity of the skeleton. Predisposes to bone fractures: PATHOLOGIC FRACTURES. Remodeling cycle is disrupted leading to an imbalance in the coupling process. Usually takes about 4 months for the remodeling process, it can take 2 years with osteoporosis. Osteoclast > Osteoblast. Risk Factors include genetics, diet (high phosphorus, low calcium), hormonal, lifestyle. Clinical Manifestations include pain, bone deformity, pathologic fractures, lost of height , Kyphosis, Dowager’s bump. Postmenopausal Osteoporosis: Estrogen deficiency. Hormonal replacement therapy suppresses cytokines that include osteoclast activity. Promotes apoptosis of osteoclast and inhibits apoptosis of osteoblasts and osteocytes. Adverse effects of HRT include breast cancer risk, thromboembolism and cardiovascular disease. Osteomyelitis: Infection of the bone (Staphylococcus Aureus most common). Other causes are group B strep, poor wound healing, bites, trauma, total joint replacements. Symptoms of infection (swelling, redness, warmth, tenderness, inflammation). Puss accumulation, leads to necrosis and death. Treatment with antibiotics, pain control. Osteoarthritis: A degenerative joint disease characterized by loss of articular cartilage. Hypertrophy and spurring of bone and erosion of cartilage. Risk factors: Trauma, long term mechanical stress, increased age, joint trauma, obesity. Overuse. Pathophysiology: Cartilage becomes thin and may be absent in areas. Underlying bone is unprotected and becomes sclerotic (dense and hard): PAIN. Osteophytes (spur-like bony projections) grow outward and alter the bone contours and joint anatomy: Bouchard and Heberden nodes. Synovitis (inflammation of the synovial membrane) and joint effusion (later on). Clinical Manifestations: Dull, aching pain in the affect joint relieved by rest. Crepitus with movement: Grinding of joints. Edema and stiffness of affected joint, limited motion. Location: ASYMMETRIC. Rheumatoid Arthritis: Chronic, inflammatory disease that causes degeneration of connective tissue primarily in the joints. Systemic, autoimmune disease. Women more than men: 3:1. Cause: Unknown, combination of genetic, environmental, hormonal factors. Pathophysiology: First tissue affected is the synovial membrane (synovium) became inflamed: synovitis first sign. As a result of synovitis, Pannus occurs: abnormal layer of fibrovascular tissue or granulation tissue (thickened synovial tissue). HLA-DR4: surface receptor in the cell that activate the immune system to attack. The immune system attacks the synovium and synovitis occurs. Manifestations: Boutonniere Deformity – jammed finger or central slip extensor tendon injury. Caused by rupture of the central portion of the extensor tendon at its insertion into the middle phalanx. Neck Swan deformity. General symptoms of inflammation. Joint tenderness and stiffness, worse in the morning. Diagnosis: Morning stiffness lasting for at least 1 hour and persisting over 6 weeks. Arthritis swelling or effusion of three or more joints persisting over 6 weeks. SYMMETRIC arthritis with simultaneous involvement of corresponding joints on both sides of the body. Rheumatoid nodules. Gout: Increased levels of uric acid and urate crystals deposit in kidneys and joints. Primaryinability to clear purine (metabolic) Secondary- from diet. Clinical Manifestation: Pain, “Big toe” (podagra). Hyperuricemia. Caused by either overproduction or underexcretion of uric acid. Approximately 50% of the initial attacks occur in the metatarsophalangeal joint of the great toe. 1000 times more likely to develop renal stones than general population.