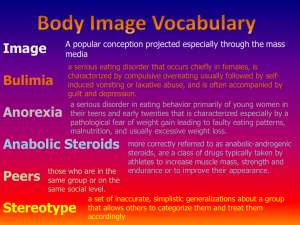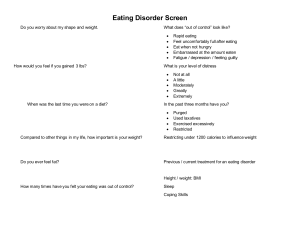
EATING DISORDER ➢ Type of mental illness that involves unhealthy thoughts and behavior towards, weight and body. I. Introduction An eating disorder is more than just about food. It is a type of mental illness that involves unhealthy thoughts and behavior towards food, weight and body shape. II. Core Content of the Chapter Terminology: 1. Pica – Ingestion of non-nutritive and non-edible substances. 2. Ruminating – Repeated regurgitation and rechewing of food. 3. Feeding disorder – It is the failure to eat adequately. 4. Binge – Eating of unusual large amount of food in a relatively short period of time. 5. Purge – To eliminate food by inducing vomiting, enema, laxative and diuretics. 6. Emaciated – A person made excessively thin by the lack of nutrition. 7. Bulimia – A disorder characterized by binge eating, over concerned with body shape and weight. 8. Anorexia – A disorder characterized by restrictive eating resulting in emaciation, disturbance in body image and intense fear of becoming obese. 9. Obesity – It is the consumption of more calories than what the body needs. Etiology: 1. Biological factor – A person with a mother or sister who has had anorexia nervosa are likely to develop the disorder. 2. Psychological factor – A person with eating disorder tends to be perfectionist, with unrealistic expectation of themselves and others. 3. Family factor – Some person with eating disorder belongs to overprotective family 4. Social factor – A person who are into relationship that they need to be thin to be continually accepted. 5. Cultural pressures – In westernized country where female are pressured to be thin to be accepted. 6. Media factor – People who are happy and successful are almost always portrayed by actors or models who are young, thin and toned. 7. Lifestyle – People who are socialites, dancers, models, gymnast, actress, entertainers and male homosexuals. 8. Physical and sexually abused – Person who usually survived tends to have eating disorders. NURSING DIAGNOSIS: ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ Alteration in health maintenance Altered nutrition: less than body requirement Altered nutrition: more than body requirement Anxiety Body image disturbances Ineffective family coping: compromised Ineffective individual coping Self-esteem disturbances ANOREXIA NERVOSA - Refusal to eat The relentless pursuit of thinness Weight phobia Causes: ➢ Serotonin – something to do in mood; appetite, pain ➢ Dominant Mother – “Do no” ➢ Disturbances in the hypothalamus – regulate sexual arrives, eating habits Characteristics: ➢ Obsessive ➢ Underweight – 15% normal weight; 200 to 400 calorie/day ➢ Adolescent ➢ Introvert/low self esteem ➢ Denies disorder – denial ➢ Deceitful vomiting, enema, diuretics, laxatives – manipulate induce vomiting ➢ Perfectionist ➢ Suicidal, sleeps 2 – 3 hours ➢ People pleaser – to family “mama”: One need to please everybody (purge) ➢ Dichotomous thinking – thinking the opposite of what the look like the think they are fat Effects: ➢ Emaciated – not enough nutrients ➢ Constipation – not enough water ➢ Decrease libido – no energy ➢ Dry skin/ falling hair – decrease nutrients ➢ Amenorrhea – imbalanced hormone ➢ Electrolyte imbalances – lack of food; decrease vitamin K so, Check intake before medication; Correct electrolyte imbalances before medication. ➢ Susceptible to infection ➢ Death due to cardiac arrest – lack of potassium; feed first proceeding to any psychotropic drugs; correct electrolyte imbalances Behavior: ➢ Adolescent and young est female child are often affected. ➢ They use denial, don’t accept that they have problem. They are more difficult to treat. ➢ 10-20% die and half of them are suicidal. ➢ They eat in social functioning but purge themselves. But avoids social functions gradually. ➢ As a child, they are chubby or overweight ➢ A perfect girl, ideal, conscientious, hardworking and people pleasers ➢ A person with low tolerance to changers and cannot adjust to new situation. Dependent to family. ➢ Focus in losing weight. ➢ Depress, irritable, withdraws and decrease libido, ➢ As disorder progresses they become deceitful, stubborn, hostile and manipulative. Nursing Care ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ Convey warmth sincerity (Trust) Monitor input and output (Purge) Listen (Afraid to show emotions) Be honest (Distrustful) Set Limits (manipulative) Teach patient about the disorder (Denial) Avoid long science (Rejection) Be consistent (Trust) Daily height taking (not facing the scale) Involve family treatment Positive reinforcement (weight gained) Nursing management: 1. 2. 3. 4. Use reinforcement to help patient gain weight. Acceptance and nonjudgmental Listen to the patient Be honest 5. 6. 7. 8. 9. 10. 11. 12. Avoid long silence Close observation Weigh patient not facing the weighing scale. Set limits Let them participate in the planning process. Teach them about their illness. Be consistent Involve family in the treatment How to establish eating pattern: 1. 2. 3. 4. 5. Sit with the patient during meals and snack time Offer CHON and CHO food patient prefers Adhere to the treatment program Observe patient after meals/snacks Be aware they hide or discard food Medication: Antidepressant after electrolyte imbalance is corrected. First is to correct electrolyte imbalances Then give “Anti-depressant” (SSRI [BECAUSE SHOWS LESS SIDE EFFECTS] or mood elevators) 1st line of meds to give because the show less effects; if not progressing; TCA tricyclic anti-depressant; MAO Inhibitors Prozac, Zoloft, Paxil – (2 to 4 weeks’ full effect) (2 weeks, wash out period) If pregnant, start with lowest milligram – causes cleft palate Do not overlap drugs (can cause death) Wait for wash out period before starting another meds Side Effect ➢ Nausea (Administer w/ meals) ➢ Diarrhea (low dosage/ hydration) – how many times ➢ Insomnia (adjust time of intake) – not to disturb sleep – check patter of sleep ➢ Dry mouth (Waller/candy) - let the doctor know Drug Interaction 1. TCA – toxic sa blood 2. MAO – fatal 3. Lithium – increase serotonergic effect (check lithium average first before and it should be normal) Side Effect: drooling, slow movement - check for lithium level if abnormal don’t give. 4. Antipsychotic – increase EPS abnormal involuntary movement scales (AIMS) Therapy: ➢ Individual Therapy – denial ➢ Family Therapy – Strict mother ➢ Group Therapy – 10 or less person BULIMIA NERVOSA “diet- binge- purge disorder” Effect: ➢ Eating a large amount of food in a short period of time ➢ A binge – purge eating disorder – continue eating even mot hungry Tension and Cravings Binge Eating Purging to avoid weight gain Cause: ➢ Increase Serotonin ➢ Lack of care from family (Rebelling from family) Characteristics: ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ Dental Problem Vomiting Use and abuse of laxatives, pills and diuretics Increase peristalsis Rectal bleeding Constipation Nursing care: Strict Diet Shame and Disgust ➢ Hoarding ➢ Binge can be controlled at times by the patient. ➢ After an episode they become guilty for uncontrolled urge and purges by cleansing. ➢ Aware of the disorder and ashamed ➢ 8,000 calories in 2 hours or 50, 000 calories in a day ➢ Russell’s sig- old and new scars (knuckles) Obsessive compulsive Normal/over weight Late adolescent, earl adulthood Extrovert/low self esteem Behavior: ➢ Late adolescent and early adulthood ➢ Occurs after a period of dieting. ➢ Belongs to a family that places great value on one’s appearance ➢ They try to be thin to be accepted. ➢ Extrovert, low self-esteem and self-destructive. ➢ Depress, perfectionist, ashamed, feeling of emptiness, highly dependent on the approval of others to maintain self-esteem. ➢ They feel unworthy, cannot talk about their feelings, with deeply buried anger ➢ Uncontrolled impulses. 1. Accept patient as worthwhile person 2. Encourage patient to discuss positive qualities about themselves 3. Inform patient to approach a nurse when they feel urge to binge 4. Encourage group activity Nursing management: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Use reinforcement to help patient gain weight. Acceptance and nonjudgmental Listen to the patient Be honest Avoid long silence Close observation Weigh patient not facing the weighing scale. Set limits Let them participate in the planning process. Teach them about their illness. Be consistent Involve family in the treatment Medications: Antidepressant ➢ Selective Serotonin Reuptake Inhibitors (SSRI), less side effect - Mood elevators - Tofranil or Prozac - Note: 2-4 weeks full effect Therapy: ➢ Family Therapy ➢ Behavioral Therapy Patient with this kind oof disorder is willing to be treated so they cooperate CHARACTERISTIS OF ANOREXIC FROM THE BOLIMIC CLIENT: Appearance Age Family Character Awareness ANOREXIC: Decrease normal weight or underweight 14-18 years old, they are younger. Rigid/controlled BULIMIC: Normal weight or overweight 15-25 years old, they are older More conflicts, violent Introvert/isolates Extrovert/sexually active/on drugs/stealing Denies Aware of the disorder Side Effects of Stabilization: ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ ➢ abdominal discomfort edema constipation food swelling of fingers feels bloated immediate weight gain craving for particular diarrhea digestive distress OBESITY Etiology: 1. Lack of adequate variety of food to eat. 2. Side effects of steroids. 3. Compulsive eating. Types of obesity: 1. Developmental – obese since childhood. 2. Reactive – maladaptive, occur later, used as coping styles when in stress. NURSING MANAGEMENT: 1. 2. 3. 4. 5. Assess suicidal thoughts Assess depression. Provide one on one session. Provide activity. Provide group activity. Other Eating disorders and related problems: ➢ PICA - behavior occurs between 2-3 yrs. and at least one month. Possible cause: MR, neglect, poor family supervision ➢ ANOREXIA ATHLETICA - Obsessed with exercise and engaged in it beyond the requirements for good health. ➢ MUSCLE DYSMORPHIA (bigorexia) - a disorder opposite anorexia. Client worry excessively that they are too small, undeveloped and frail muscles. ➢ ORTHOREXIA NERVOSA - a pathological fixation on eating “proper, pure or superior” food. ➢ NIGHT EATING SYNDROME - lack of appetite for breakfast because client is preoccupied eating late in the day or night. ➢ NOCTURNAL SLEEP-RELATED - a client who eats while asleep. ➢ RUMINATING SYNDROME - a client eats, swallows and regurgitates food back into the mouth, chewed and swallowed. ➢ GOURMAND SYNDROME - an obsession with fine food including its purchase, preparation, presentation and consumption. ➢ PRADER-WILLI SYNDROME - a congenital problem usually associated with M.R which includes incessant eating. Mental- retardation