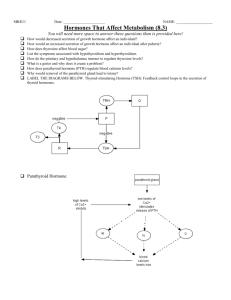
Week1–EndocrinologyI Defineendocrine,autocrine&paracrine,targetcell,hormone ● Endocrine–hormonesthataresecretedintothebloodstream&transportedtotargetcellswheretheyproducetheirphysiological effect ● Autocrine–hormonethatissecretedintoextracellularfluid&actsuponthecellthatproducesit ● Paracrine–ahormonethatexertsitseffectsoncellsnearitssecretionsite(excludesneurotransmitters),butnotthecellthat producedit ○ Actswithintheorganitisproduced ● TargetCell–hormonesthataffectonlythesecellsb/ctheyhavespecificreceptorsthatwillbindthehormone ● Hormones–Chemicalmessengersthataresecretedfromtheendocrineglandortissue Describe&giveexamplesofnegative&positivefeedbackloops ● Sinceendocrineshavetendenciestoover-secreteitshormone,itwillhavemoreofaneffectonthetargetorgan ● Negativefeedbackloops=targetglandhormonesactonendocrineglandstostimulateorinhibittheirproduction(E.g.T4caninhibit theTRHfromthehypothalamusorTSHfromtheanteriorpituitary) ● Positivefeedbackloops=↑edlevelsoftargetglandhormonesstimulatesendocrineglandstosecretemore(E.g.estradiolstimulates anteriorpituitarytosecreteLHforovulation) ● Iftoomuchfunctionoccurs,usuallysomefactorsareassociatedw/thefunctionfeedbackonthe“control”glandtoreducehormone secretion Discusstherelationshipb/wthenervous&endocrinesystems ● Thehypothalamusisaportionofthebrainthatmaintainsthebodiesinternalbalance(homeostasis) ● Thehypothalamusisthelinkb/wtheendocrine&nervoussystems.Thehypothalamusproduces,releasing&inhibitinghormones, whichstoptheproductionofotherhormonesthroughoutthebody. ○ Importantforgrowth,reproduction,metabolism,etc. DescribeAminehormones&identifymembersofthisclassification ● Hormonesthatarederivedfromtheaminoacidtyrosine&includeadrenaline ● Theyincludetwothyroidhormones(thyroxine[T4]&triiodothyronine[T3]),hormonesoftheadrenalmedulla(adrenaline& noradrenaline)aswellasmelatonin(producedbypinealgland) Identifycommonpeptide&proteinhormones ● Thesehormonesareeithersmallpeptidesorproteinswhicharesynthesizedontheribosomesofendocrinecells ● Adrenocorticotropichormone(ACTH)&melanocytestimulatinghormone(MSH)arecommon&comefromasingleprohormone ● Calcitonin,amylin&angiotensinareothercommonones Describethesynthesis&releaseofpeptide&proteinhormones 1) Synthesizedontheribosomesofendocrinecellsaslargerproteinsknownaspreprohormones&thencleavedtoprohormonesby enzymesinthegranularendoplasmicreticulum(ER)ofthecell 2) TheprohormoneisthenpackagedintosecretoryvesiclesbytheGolgiapparatus 3) Itisthencleavedtobecomethefinalhormone&leftoverpeptides a) Botharereleasedbyexocytosisinresponsetospecificstimuli b) Insomecases,theotherpeptidesmayhaveeffectsontargetcells Identifycommonsteroidhormones ● Cholesterolisthemostcommonsteroidhormone,&alltheothershaveasimilarchemicalstructure&actuallyderivedfrom cholesterolitself ● OthercommononesincludeAldosterone,Cortisol,Corticoids,etc Describethesynthesis&releaseofsteroidhormones ● Someendocrinessynthesizetheirowncholesterol,butitismostlyderivedfromp lasmalipoproteinsthataremadeintheliver& circulatetheblood ● Steroidhormonesarehighlylipidsoluble&oncesynthesized,candiffuseacrosstheplasmamembrane&enterthebloodstream ○ Therefore,largequantitiesofsteroidhormonesarenotstoredwithinthesynthesizingcellbuttheirprecursorsare ● Uponappropriatestimulation,enzymesinthesecellscan,withinminutes,causethechemicalconversiontothefinalhormones readyforsecretion Discusstransport&deliveryofhormonestotargetcells HormonesTransportinBlood ● Water-solublehormones(adrenaline,noradrenaline&peptides)arecarriedintheplasmainadissolvedstatetotheirtargetorgan(s) ● Thesteroid&thyroidhormonesARENOTverywater-soluble&circulateinthebloodb oundtoplasmaproteins ○ Someoftheseproteinsarespecificallyforthetransportofthehormone;otherplasmaproteins(albumin)cancarryalmost anylipid-solublehormone HormoneDeliverytoTargetCell ● Mostofalipid-solublehormoneisboundtoitsplasmaproteinbutasmallamountexistsasfree,unboundhormonedissolvedin plasma ○ Itisonlythefreehormonethatcancrosscapillarywalls&affectitstargetorgan ○ Thereexistspecificproteintransporterswhichfacilitatethepassageofthesehormonesthroughcapillaryendothelium ○ Ex.specificbindingsitesforT3&T4havebeenidentifiedinplasmamembrane,cellnuclei&mitochondriaofvariousorgans &itispossiblethattheentryofthyroidhormonesisdrivenbythee quilibriumb/wtheextracellular&intracellularthyroid hormonebindingprotein Identifymechanismsofthebodythatmetabolize&clearhormonesfromcirculation ● Forproteinhormones–theyaresecretedtoperipheralcirculationasamixofisoforms.Theseheterodimerichormonesconsistof aminoacidchains&N-linkedglycosylationsiteswheremultipleoligosaccharideresiduescanbeadded ○ Glycosylationaddsahighproportionofsialicacid-enrichedcarbohydrates&alessernumberofsulphatedresiduesto proteinmolecules ● Deglycosylation&p roteolysisarethemajormechanismsofinactivation&clearanceofspecificglycoproteinhormones ● Terminals ialicacidresiduesaretypicallyremovedbyplasmaglycosidases ● Hepaticcellsthenrecognizethe“expose”hormone&peptidebondsb/waminoacidsbecomesusceptibletoenzymaticattack ○ Note:thelessglycosylated/acidicisoformsofproteinhormonesexhibitashorterhalf-lifeinsystemiccirculationthantheir moreacidiccounterparts ○ Mostacidicisoforms(degreeofsialylation&sulphation)aremorepotentstimulatorsoftargetorgans. Describephasic(surge-like),episodic(pulsatile),circadian&cyclicmodesofhormonesecretion ● Phasic(surge-like):suddenchange(aboltofalargeamountofhormone) ● Episodic(pulsatile):topreventdesensitizationfromoccurringundernormalconditions.Theyaresecretedinspurtsratherthan continuously ● Circadian:rhythmsthatfollowa24fourpattern ● Cyclic:itoccursinacycle,whetheramonthorday ● Circannualmodes:yearly/seasonally ○ Note:thegreatestreleaseofgrowthhormoneoccursduringtheearlysleepperiod Definesynergistic,permissive&antagonisteffectsofhormoneactions ● Synergistic–Whentwohormonesworktogether,theireffectscanbeadditiveorcomplementary.Twoormorehormoneswork togethertoproduceaparticularresult ○ Ex.epinephrine&norepinephrine–produceinadditiveaffectintheheartastheyeachseparatelyproducesan↑ incardia ratewhichbecomesevengreateratthesameconcentrationswhentogether ● Permissive–h asanaccommodatingeffectontheactionofasecondhormonewhenitenhancestheresponsivenessofatarget organtothesecondhormone,orwhenit↑ estheactivityofthesecondhormone ○ Ex.PTHtoVitaminD3 ● Antagonistic–w orksagainsteachother ○ Ex.insulin&glucagononadiposetissue ■ Insulinpromotestheformationoffatwhileglucagonpromotesfatbreakdown Describetheeffectsofhormoneconcentrationontargettissues ● Effectsofhormonesareverydependentonconcentration–whenconcentrationsarehigh,theireffectsmaybedifferent ○ Pharmacologicaldosesofhormones,especiallysteroidscanhaveverydamagingsideeffects ○ PrimingEffects:variationsinhormoneswithinnormalrangecanaffectresponsivenessoftargetcellsduetotheeffectof polypeptide&glycoproteinhormonesonthenumberoftheirreceptorproteinsintargetcell. Morereceptorsmaybe formedintargetcellinresponsetothis(up-regulationofreceptors) ○ Desensitization&Downregulation:prolongedexposuretohighconcentrationofpolypeptidehormoneshasbeenfoundto desensitizethetargetcells.Thisisduetothedownregulationofreceptors&itcausesbycontinuousexposureofthetarget cellstothehormone ● Topreventthis,hormonesaresecretedinspurts(pulsatilesecretion). HormonesintheSameChemicalCategory: ● Bindingishighlyspecific ● Hormonesbindtoreceptorsw/ahighaffinity ● Hormonesbindtoreceptorsw/alowcapacity;saturatingthereceptorsw/hormonemolecules DiscusstheMechanismsofActionforofAmine&Peptide/ProteinHormones Non-SteroidAction( amineorpeptide)hormonesarep olarhormones&bindtoreceptorsonplasmamembranewheretheyexerttheir effectsthroughs econdmessengersystems ● Catecholamines,polypeptides&glycoproteinscannotpassthroughtheplasmamembrane ● Hormonesarelikemessengerswheretheintracellularmediatorsofthehormonesactioncanbesecondmessengers ○ Secondmessengersareapartofsignal-transductionmechanisms ○ Extracellularsignals(hormones)aretransducedintointracellularsignals(secondmessengers) ■ Examples:adenylatecyclase,phospholipaseC&tyrosinekinasearesecondmessengers. AdenylateCyclase–CyclicAMP(cAMP) ● EffectsofmanypolypeptideglycoproteinhormonesaremediatedbycAMP ● Whenhormonebindstoreceptorprotein,itcausesdissociationofsubunitfromthecomplexofG-proteins,thesubunitmoves throughmembraneuntilitreachesenzymeadenylatecyclase ● TheG-proteinssubunitbinds&activatestheenzymes,whichcatalyzesthereactionw/cytoplasmofthecell. ○ ATPcAMP+PPi ● Thisreactioncausesan↑ inintracellular[cAMP] ● cAMPactivatesinactiveenzymeincytoplasm,proteinkinase,byattachingtoitsregulatorysubunit,causingittodissociatefromits catalyticsubunit,whichtoobecomesactive ○ ↑incAMPproductioncauses↑ ofproteinkinaseenzymeactivity ● InactivationofcAMPmustberapidlydoneforittofunctioneffectively&isaccomplishedbyphosphodiesterase ● Cyclicguanosinemonophosphate(cGMP)functionsasasecondmessengeraswell PhospholipaseC–Ca2+ ● ConcentrationofCa2+incytoplasmiskeptverylowbyactivetransportercarriers(calciumpumps)inplasmamembrane ● [Ca2+]isreducedtooneten-thousandthofitsconcentrationintheextracellularfluid ● EndoplasmicreticulumcontainsCapumpstotransportCa2+fromcytoplasmtocisternae ○ WhenmusclesarecontractedCa2+couplesw/electricalexcitationofthemusclecelltomechanicallycontractmuscle ● Stimulationofalpha-1-adrenergicreceptorsbyepinephrineactivatesthetargetcellviaCa2+secondmessenger ○ ThisactivatestheenzymeinplasmamembranephospholipaseC,thesubstrateoftheenzymeissplitintoIP3(inositol triphosphate)&DAG(diacylglycerol)–bothofwhichactassecondmessengers ■ IP3leavestheplasmamembrane&diffusesthroughcytoplasmtoendoplasmicreticulumwherereceptorproteins forIP3locate ■ ThebindingcausesspecificCa2+channelstoopen,todiffuseCa2+intocytoplasm,whichbindsaproteincalled calmodulin,activatingit&inturn,activatesproteinkinaseenzymes Note:proteinkinaseenzymes areenzymesthatregulatethebiologicalactivityofproteinsbyphosphorylationofspecificaminoacidsw/ATP. TyrosineKinaseSecondMessengerSystems: ● Insulinpromoters’glucose&aminoacidtransport&stimulatesglycogen,fat,&proteinsynthesisinitstargetorgans(liver,skeletal muscles&adiposetissue) ● ThegrowthfactorsincludingEGF(epidermalgrowthfactor)&PDGF(platelet-derivedgrowthfactor),IGF(insulin-likegrowthfactor) areautocrineregulators ○ Inthecaseofinsulin&growthfactors,thereceptorproteinislocatedintheplasmamembrane&isanenzymecalled TyrosineKinase(akinaseenzymewhichaddsaphosphatespecificallytotyrosineaminoacids) ● Insulinreceptorconsistsoftwoalpha&twobetasubunits ○ Alphaunitsintheextracellularsideofplasmamembrane&containtheligandbindingsite&thebetaunitsintheplasma membrane Wheninsulinbindstoalphaunits,thebetaunitsarestimulatedtophosphorylateeachinaprocesscalledautophosphorylationwhich activatesthetyrosinekinaseactivity. ● Activatedinsulinreceptorphosphorylatessubstrateproteinswhichactivateavarietyofsignalingmolecules ● Thesecauseinsertionoftransportcarrierproteinsfromglucoseintoplasmamembranewhichpromotetheuptakeofplasmaglucose intotissuecells[lowersplasmaglucose]. DiscusstheMechanismsofActionforofSteroid/ThyroidHormones Unlikewater-solublehormones,thelipophilic&thyroidhormonesdonottraveldissolvedintheaqueousportionofplasma;theyusecarrier proteins.Theydissociatefromthesecarrierproteinsonceclosetotargetcell&diffusethroughtheplasmamembrane. Receptorsoflipophilichormonesarecalledn uclearhormonereceptors(NHR)&functionastranscriptionfactorsbyactivatinggenetic transcription.TheymustfirstbeactivatedbybindingtotheirhormoneligandssothatitcanbindtoaspecificregionofDNAcalledthe hormone-responseelement(HRE).NREhastworegions/domains:(1)aligand(hormone)-binddomain&(2)aDNA-bindingdomain. SteroidHormoneModeofAction: ● Non-genomicactionofsteroidsmayoccurincytoplasmoftargetcells&involvetheactivationofsecond-messengersystems ● Stimulategenetictranscription( genomicaction)&takessometimetowork ○ Thereceptorsareinthecytoplasm,orsometimesunboundreceptorscanbefoundinnucleus ○ Whencytoplasmicreceptors(NREs)bindtotheirspecifichormoneligands,theymovetothenucleuswheretheir DNA-bindingdomainsbindtothespecifichormone-responseelementoftheDNA ○ Thehormone-responseelementofDNAconsistsoftwohalf-sites(dimer)&sincetheyarethesameitisahomodimer ○ 1steroid-receptorboundtoonehormoneattachesasingleunittoonehalf-sitethenthesamefortheother. ■ Theactivatedreceptorsstimulatetranscriptionofgenes(hormonalregulation) Whensteroidhormoneligandbindstoitsnuclearreceptorprotein(NRP),itchangesthereceptorstructurewhichcauses: a) Removalofagroupofproteins(heatshockproteins) b) Recruitmentofcoactivatorproteins&preventionofcorepressorproteins. ThyroidHormoneMechanismofAction: MajorhormonessecretedbythyroidglandisThyroxine&ittravelsthroughbloodw/acarrierproteinTBH(thyroxine-bindingglobulin) ● CarrierproteinshavehigheraffinityforT4thanT3,thereforetheamountofunboundT3is10XgreaterthanT4 ● OnlyfreeT3&T4canenterthetargetcells(boundonesserveasreservoir) ● Oncefree,T4passesintotargetcell,itisconvertedtoT3 ● Thyroid-hormonereceptors(THR)arelocatedinthenucleus&boundtoDNA. Thethyroidhormoneresponseelement: ● Hastwohalfsitesbutthethyroidhormonereceptor(TR)forT3onlybindstooneofthehalfsites ● TheotherhalfsitebindstothereceptorforVitaminA(RXR) ○ Createsheterodimer Identifythetargetofthefollowinghypothalamicreleasing/inhibitingfactors:TRH,CRH,GHRH,somatostatin TRH:stimulatessecretionofTSH(Thyroid-stimulatinghormonewhichisresponsibleforproducing&secretingT4&T3. CRH:stimulatessecretionofACTH(Adrenocorticotropichormone)whichstimulatesadrenalcortextosecretegluco-corticoidssuchascortisol. GHRH:secretedbyhypothalamusthatstimulatestheanteriorpituitarytosecretegrowthhormone,whilesomatostatinfromhypothalamus inhibitssecretion. Identifythehormonesoftheanteriorpituitary 1) GrowthHormone(GH,orsomatotropin) a) Promotesmovementofaminoacidsintocells&incorporationofaminoacidsintoproteins(promotesoveralltissue&organ growth) 2) Thyroid-stimulatingHormone(TSHorThyrotropin) a) Stimulatesthyroidglandtoproduce&secreteT4&T3 3) AdrenocorticotropicHormone(ACTH,orcorticotropin) a) Stimulatesadrenalcortextosecretegluco-corticoids,suchascortisol 4) Follicle-stimulatingHormone(FSH,folliculotropin) a) Stimulatesgrowthofovarianfolliclesinfemales&theproductionofspermcellsintestesofmales 5) LuteinizingHormone(LH,orluteotropin) a) w/FSH,collectivelycalledgonadotropichormones b) Stimulatesovulation&stimulatessecretionofmalesexhormones(testosterone). 6) Prolactin(PRL) a) Stimulationofmilkproduction b) Lactation c) Supportswaterregulation&electrolytebalance Describethegeneraleffectsofgrowthhormone ● Growthhormonecausesgrowthofalmostalltissuesofthebodythatarecapableofgrowing ● Causescellsto↑ insize,↑edmitosis&specificdifferentiationofcertaintypesofcellssuchasbonegrowthcells&earlymusclecells ● Deficienciesingrowthhormonesecretionmaybecongenitalortheymayoccurslowly,orsuddenly,atanytimeinlife Describetheregulationofgrowthhormonesecretion ● Growthhormonesecretionisregulatedbygrowthhormonereleasinghormone(GHRH)&growthhormoneinhibitinghormone (GHIG,SRIF) ○ Thesearesecretedbythehypothalamus&transportedtotheanteriorpituitaryglandthroughthe hypothalamic-hypophysealportalvessels ○ Someofthesamesignalsthatinitiatefeedingsalsostimulatethesecretionofgrowthhormone Describetheeffectsofgrowthhormoneonthemetabolismofproteins,fattyacids&glucose GrowthHormoneProteinMetabolism: ● ↑estherateofproteinsynthesisthroughamechanismnotfullyunderstood ● Italsoenhancesthetransportofaminoacidsintothecell ● Evenintheabsenceofhighconcentrationofaminoacids,growthhormones↑ RNAtranslationwhichstimulateproteinsynthesis GrowthHormoneFattyAcidMetabolism: ● Growthhormonenotonly↑ esthemobilizationoffattyacidsfromadiposetissue,itenhancestheconversionoffattyacidsto acetyl-CoA ○ Fatisutilizedforenergypreferentiallyovercarbohydrates&proteins ● Ifanexcessivequantityofgrowthhormone&largeamountsoffatarebeingmobilized,excessamountsofacetoaceticacidare formedintheliver&aconditioncalledketosisdevelops. GrowthHormoneGlucoseMetabolism: ● GrowthHormonescausean↑ inbloodglucoselevelswhichtriggersthereleaseofinsulinfromthepancreas ● Decreasestheutilizationofglucosebysuppressingglucoseuptake&glucoseoxidation&stimulatesglycogenesis Discusshowgrowthhormoneimpactslong-bonegrowth ● GHstimulatesallaspectsoftheprocessesofepiphysealcartilage&longbonegrowth.GHstimulatesosteoblaststolaydownmore newbonewhichleadstoathickeningofthebone ● GHstimulatesthelivertoproduceIGF-1,whichwilltraveltothetargetsite&isamajorcontributortotheproductionofcartilage& bone Definetherelationshipb/wgrowthhormones&theinsulin-likegrowthfactor ● Theliverproduces&secretesIGF-1inresponsetoGHstimulation ● IGF-1servesasamediatorforsomeofGH’sactions.AmajortargetofIGF-1isthecartilagewhereIGF-1stimulatescelldivision& growth Discusshowinsulin-likegrowthfactorscanactinendocrine,autocrine&paracrinemanner ● Endocrine:Itisproducedbytheliver&cantraveltootherorgansintheblood ● Autocrine:ItcanbeproducedbythecellswhichrequiretheIGF-1 ● Paracrine:Itcanbeproducedinmanycells&canactonthetissuesinwhichitisproduced Describecommonpathologiesassociatedw/inappropriategrowthhormonesecretion ● Gigantism:ExcessiveGHproduction ● Acromegaly:ExcessiveGHproductionaftertheepiphysealdiscshavesealed(doesn’tcause↑inheight,but↑edgrowthofsoft tissues&coarseningoftheskin) ● Dwarfism:InadequatesecretionofGH;targetcellsareinsensitivetoGHb/cofamutationinthegenethatcodesfortheGHreceptor Identifytheendocrinehormonessecretedbythethyroidgland ● Thyroxine(T4)&triiodothyronine(T3) Discusshowthyroidhormonesecretionisregulated ● Thyroidhormonesecretionisregulatedbythyroidstimulatinghormone(TSH)&thyrotropinreleasinghormone(TRH) Describethemicroanatomyofthethyroid&formationbythyroglobulin ● Thethyroidglandconsistsofnumeroussacscalledthyroidfollicles.Eachfollicleconsistsoffollicularcellssurroundedbyafluid (colloid)thatcontainsthyroglobulin Discussiodidetrapping,organification&formationofT3&T4 ThyroidfolliclesaccumulateIodidefromtheblood&secreteitintothecolloid.Oncethere,itisoxidized&attachedtoatyrosineresidue withintheprotein,thyroglobulin(1iodinetotyrosineproducesMIT,2iodinetotyrosineproducesDIT).Withinthecolloid,enzymesmodify thestructureofMIT&couplethemtogether.(2DIT=T3orT4,1DIT&1MIT=T3).Atthispoint,theT3orT4arestillattachedtothe thyroglobulin,untilTSHisstimulated,wheretheyarethenhydrolyzedfromthyroglobulin&areabletobesecretedintotheblood. Describesecretionofthyroidhormones Thethyroidhormonesarestoredinlargequantitiesinthefollicularfluid,enoughforseveralmonths. Eachthyroglobulinmoleculewillhave about30thyroxinemolecules&afewtriiodothyroninemolecules.Atthetimeofreleasethehormonesareenzymaticallysplitfromthe thyroglobulinbyproteases.Thehormonesdiffusethroughthebaseofthethyroidcellintothesurroundingcapillariesasfreehormones. Identify&characterizeconditionsresultinginhyper-&hypo-secretionofthyroidhormones Hyperthyroidism:autoimmunedisorder,autoantibodiesbindTSHreceptorsonthyroidglandfollicularcellscausingagrowthofthethyroid (goiter)&causesexcessivesecretionofthethyroidhormones.Grave’sdiseaseisanotherhyperthyroiddisease,&cancausesymptomssuchas heatsensitivity,palpitations,bulgingoftheeyes,excessiveperspirationetc. Hypothyroidism:Deficiencyiniodineinthedietcanleadtoagoiter(enlargedthyroid).Lackofiodineinthedietreducesthenegative feedbackinhibitionofTSHsecretion,resultinginexcessivesecretionofTSH&stimulatestheformationofanenlargedthyroid(goiter). Symptomsincludefatigue,impairedhairgrowth,intolerancetocold,dryskin,GIproblems,depression&anxiety. Describethephysiologicaleffectsofthyroidhormones ● Excessivethyroidhormonesecretioncancausesomeonetobenervous&emotional,impotenceinmales ● Lackofthyroidhormonescanleadtodepression&anxiety,lossoflibido IdentifyanatomicalregionsofADHsynthesis&secretion ● ADHisproducedinneuroncellbodiesofthesupraoptic&paraventricularnucleiinthehypothalamus&secretedbytheposterior pituitary DiscusshowsecretionofADHisregulated ● ThesecretionofADHiscontrolledbyneuroendocrinereflexes ● Secretionisstimulatedbyosmoreceptorneuronsinthehypothalamusinresponsetoariseinplasmaosmolality ● ADHsecretionisinhibitedbysensoryinputfromstretchreceptorsintheleftatriumoftheheartwhicharestimulatedwhenthereis ariseinbloodvolume DescribetheeffectsofADHonwaterreabsorptioninthekidney ● ADHstimulateswaterretentioninthekidneyssothatlesswaterisexcretedintheurine ● Whenbloodvolume↑ es,ADHisinhibitedsowatermaybeexcretedintheurine DiscusstheeffectofADHonperipheralbloodvessels ● ADHcausescontractionofthesmoothmuscles&constrictionofbloodvessels(vasoconstriction)to↑ bloodpressure ● Conversely,ADHinhibitionwillleadtovasodilation Describediabetesinsipidus ● DiabetesinsipidusisadeficiencyofADH,causingan↑ inthedrinkingofwater ● Bloodglucoselevelsarenormal&thereisnoglucoseintheurine