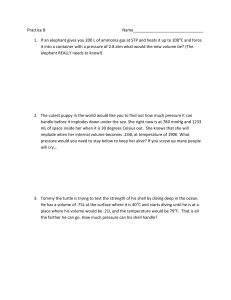
Notes Slide 1 Slide 2 Slide 3 What’s New in Diving Medicine Eric Johnson, MD NAUI #22649 D rector Emergency Services, Teton Val ey Hosp tal, Dr ggs, ID Past President, WMS Notes Slide 4 Sources of Info: • Divers Alert Network – www.diversalertnetwork.org • UHMS Dive Agencies: PADI, NAUI – www.uhms.org • Other Web Site: • • • • Slide 5 What’s New ? • • • • • • • Slide 6 http://scuba-doc.com http://faculty.washington.edu/ekay/ http://www.scubamed.com/divmed.htm www.wms.org Let’s review some data… Never forget the basics. Medical updates. Diving techniques. Equipment Targeted populations Travel. UHMS Website Notes Slide 7 Slide 8 Slide 9 Notes Slide 10 Slide 11 Slide 12 Notes Slide 13 Slide 14 Spontaneous Pneumothorax Slide 15 Notes Slide 16 Slide 17 Slide 18 Notes Slide 19 Slide 20 Slide 21 Notes Slide 22 Slide 23 Slide 24 Notes Slide 25 Slide 26 Slide 27 Notes Slide 28 Slide 29 Medical updates • Asthma – Good publication by UHMS & DAN • Seizures…unchanged, but being challenged • Diabetes: – Used to be always a “NO” – New guidelines and data. Slide 30 Epilepsy and recreational scuba diving : an absolute contraindication or can there be exceptions? A call for discussion. Epilepsia. 2007 May;48(5):851-8 We suggest that people with epilepsy who wish to engage in diving, and the physicians who certify fitness to dive, should be provided with all the available evidence. Those who have been entirely seizure-free on stable antiepileptic drug therapy for at least 4 years, who are not taking sedative antiepileptic drugs and who are able to understand the risks, should then be able to consider diving to shallow depths, provided both they and their diving buddy have fully understood the risks. Notes Slide 31 Pollock NW, Uguccioni DM, Dear GdeL, eds. Diabetes and recreational diving: guidelines for the future. Proceedings of UHMS/DAN 2005 June 19 Workshop. Durham, NC:Divers Alert Network; 2005. Slide 32 Guidelines for Recreational Diving with Diabetes • Selection and Surveillance • Age ≥18 years (≥16 years if in special training program) • Delay diving after start/change in medication – - 3 months with oral hypoglycemic agents (OHA) - 1 year after initiation of insulin therapy • No episodes of hypoglycemia or hyperglycemia requiring intervention from a third party for at least one year • No history of hypoglycemia unawareness • HbA1c ≤9% no more than one month prior to initial assessment and at each annual review – - values >9% indicate the need for further evaluation and possible modification of therapy Slide 33 New Diabetes & Diving Guidelines • No significant secondary complications from diabetes • Physician/Diabetologist should carry out annual review and determine that diver has good understanding of disease and effect of exercise – - in consultation with an expert in diving medicine, as required • Evaluation for silent ischemia for candidates >40 years of age – - after initial evaluation, periodic surveillance for silent ischemia can be in accordance with accepted local/national guidelines for the evaluation of diabetics • Candidate documents intent to follow protocol for divers with diabetes and to cease diving and seek medical review for any adverse events during diving possibly related to diabetes Notes Slide 34 Diabetes & Diving Scope of Diving • Diving should be planned to avoid - depths >100 fsw (30 msw) - durations >60 minutes - compulsory decompression stops overhead environments (e.g., cave, wreck penetration) situations that may exacerbate hypoglycemia (e.g., prolonged cold and arduous dives) • Dive buddy/leader informed of diver’s condition and steps to follow in case of problem • Dive buddy should not have diabetes Slide 35 Diabetes & Diving Glucose Management on the Day of Diving • General self-assessment of fitness to dive • Blood glucose (BG) ≥150 mg·dL-1 (8.3 mmol·L-1), stable or rising, before entering the water - complete a minimum of three pre-dive BG tests to evaluate trends 60 minutes, 30 minutes and immediately prior to diving - alterations in dosage of OHA or insulin on evening prior or day of diving may help • Delay dive if BG - <150 mg·dL-1 (8.3 mmol·L-1) - >300 mg·dL-1 (16.7 mmol·L-1) Slide 36 Diabetes & Diving • Rescue medications - carry readily accessible oral glucose during all dives - have parenteral glucagon available at the surface • If hypoglycemia noticed underwater, the diver should surface (with buddy), establish positive buoyancy, ingest glucose and leave the water • Check blood sugar frequently for 12-15 hours after diving • Ensure adequate hydration on days of diving • Log all dives (include BG test results and all information pertinent to diabetes management) Notes Slide 37 Plasma glucose response to recreational diving in novice teenage divers with insulin requiring diabetes mellitus. N.W . POLLOCK1, D.M. UGUCCIONI2, G.DeL. DEAR1,2, S. BATES3, T.M. ALBUSHIES4, S.A. PROSTERMAN5. 1Center for Hyperbaric Medicine and Environmental Physiology, Department of Anesthesiology, Duke University Medical Center, Durham, NC 27710; 2Divers Alert Network, Durham, NC, 27710; 3Golisano Children’s Hospital, Rochester, NY; 4Concord Pediatrics, CPPA, Concord, NH; 5University of the Virgin Islands, St. Thomas. • Pollock NW , Uguccioni DM, Dear GdeL, Bates S, Albushies TM, Prosterman SA. Plasma glucose response • to recreational diving in novice teenage divers with insulin-requiring diabetes mellitus. • Med 2006; 33(2):125-133. Undersea Hyperb • • • • • • • A growing number of individuals with insulin-requiring diabetes mellitus (IRDM) dive, but data on plasma glucose (PG) response to diving are limited, particularly for adolescents. W e report on seven 16-17 year old novice divers with IRDM participating in a tropical diving camp who had recent at least moderate PG control (HbA1c 7.3±1.1%) (mean ± SD). PG was measured at 60, 30 and 10 min predive and immediately following 42 dives. Maximum depth (17±6 msw) and total underwater times (44±14 min) were not extreme. Pre-dive PG exceeded 16.7 mmol⋅L-1 (300 mg⋅dL-1) in 22% of dives. Males had significantly higher pre-dive levels (15.4±5.6 mmol⋅L-1 [277±100 mg⋅dL-1] vs. 12.8±2.9 mmol⋅L-1 [230±52 mg⋅dL-1], respectively) and greater pre-post-dive changes (-4.3±4.4 mmol⋅L-1 [-78±79 mg⋅dL-1] vs. -0.5±4.3 mmol⋅L-1 [-9±77 mg⋅dL-1], respectively). Post-dive PG was <4.4 mmol⋅L-1 [<80 mg⋅dL-1] in two dives by two different males (3.4 and 3.9 mmol⋅L-1 [61 and 70 mg⋅dL-1]). • The impact of purposeful elevation of PG to protect against hypoglycemia during diving remains to be determined. • No symptoms or complications of hypoglycemia were reported. These data show that in a closely monitored situation, and with benign diving conditions, some diabetic adolescents with good control and no secondary complications may be able to dive safely. Slide 38 Medical Issues: Remote DCS TX Slide 39 New Text on Medical Fitness to Dive…from Best Publishing Notes Slide 40 Flying After Diving • Single NO-DECO Dive = 12 hour preflight surface interval recommended. • Multiple dives in a day or Multiple Days of Diving = preflight SI of 18 hours. • I use the 24 hour rule!!! Slide 41 Slide 42 Diving Techniques & Equipment • Equipment: – Improved design – Better safety gear • Redundent air sources • Communication • Navigation – Improved “algorithms” for dive computers. Notes Slide 43 Dive Techniques • Buoyancy…always important! • Reverse Dive profiles: – The workshop finds no reason for the diving communities to prohibit reverse dive profiles for no-decompression dives less than 40 msw (130 fsw) and depth differentials less than 12 msw (40 fsw). • Ascent Rate: • Slower appears better, but being tested. • -30 fpm or slower • Rule of Halves: Slide 44 The National Association of Underwater Instructors (NAUI) recently recommended the “rule of halves:” NAUI now recommends for table-based norequired decompression dives in excess of 40 fsw, divers should halve the distance to the surface from the dive’s deepest depth and make a 1- minute safety stop, followed by a 2-minute safety stop in the 15 fsw zone. For dives shallower than 40 fsw, the standard 3-minute safety stop should be completed. Emphasis in the diving community is still to slowly ascend, 30 feet per minute (fpm) or slower. Divers should halve the distance to the surface from the dive’s deepest depth and make a 1- minute safety stop, followed by a 2-minute safety stop in the 15 fsw zone Slide 45 Targeted Groups: -Kids -Technical Divers Notes Slide 46 Don’t forget getting there? • Travel Med concerns – Immunizations – Malaria and other “bugs” – Safety – TSA • Dive accidents – How to get yourself out? • Most common cause of dive trip injury? Slide 47 Slide 48 THANK YOU!!! Notes Slide 49 If needed, Please resuscitate the person next to you!!!