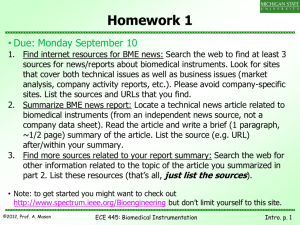
LABORATORY MANUAL PROGRAMME: B.Tech SEMESTER /YEAR: V / III SUBJECT CODE: BM0315 SUBJECT NAME: Biomedical Instrumentation Lab Prepared By: Name: S.P. Angeline Kirubha Designation: A.P (Sr. Gr) DEPARTMENT OF BIOMEDICAL ENGINEERING SCHOOL OF BIOENGINEERING, FACULTY OF ENGINEERING & TECHNOLOGY SRM UNIVERSITY (UNDER SECTION 3 of UGC ACT 1956) KATTANKULATHUR-603203 Tamil Nadu, India LIST OF EXPERIMENTS Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 Sl. No Experiment Page .No 1 Blood Pressure Measurement 1 2 Real time monitoring of Echocardiography 6 3 Working of different types of Diathermy equipments – study 20 3.a Shortwave Diathermy 22 3.b Ultrasound Diathermy 26 3.c Surgical Diathermy 28 4 ECG wave analysis using simulator 32 5 Real time patient monitoring system 35 6 Ultrasound blood flow measurement to identify arteries and 39 veins 7 Respiratory system analysis using Spirometer 41 8 Analysis of ECG abnormal wave pattern using Arrhythmia 47 Simulator 9 EEG wave analysis using simulator 52 10 Auditory system check up using Audiometer 56 11 Heart sound measurement using PCG 61 12 Biotelemetry 65 13 Pacemaker Module 68 14 ECG heart rate alarm system with HRV 73 15 EMG Biofeedback with NCV 78 Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 Ex. No 1 Blood Pressure Measurement Aim: To Measure blood pressure using Sphygmomanometer, semi-automatic blood pressure measuring instrument and automatic blood pressure measuring instrument. Apparatus Required: 1. Cuff 2. Inflator 3. Power supply 4. Stethoscope 5. Sphygmomanometer 6. Semi-automatic bp measuring unit 7. Automatic bp measuring unit THEORY: Blood Pressure Blood pressure is a measurement of the force applied to the walls of the arteries as the heart pumps blood through the body. The pressure is determined by the force and amount of blood pumped, and the size and flexibility of the arteries. Blood pressure is continually changing depending on activity, temperature, diet, emotional state, posture, physical state, and medication use. The ventricles of heart have two states: systole (contraction) and diastole (relaxation). During diastole blood fills the ventricles and during systole the blood is pushed out of the heart into the arteries. The auricles contract anti-phase to the ventricles and chiefly serve to optimally fill the ventricles with blood. The corresponding pressure related to these states are referred to as systolic pressure and diastolic pressure .The range of systolic pressure can be from 90 mm of Hg to 145mm of Hg with the average being 120 mm of Hg. The diastolic pressure typically varies from 60mm of Hg to 90 mm of Hg and the average being 80 mmofHg. PRINCIPLE Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 The upper arm is wrapped with the cuff belt connected to a mercury pressure gauge and air is pumped with a rubber ball to increase cuff pressure about 30 mmHg higher than the systolic blood pressure to block the artery and stop blood flow downstream. Then, the cuff pressure is slowly lowered. The artery opens at the instant when the cuff pressure decreases below the systolic blood pressure and blood begins to flow on and off in synchrony with pulses causing the opening and closing of the artery. The sound emitted by the pulses is named Korotkoff's and continues until the cuff pressure decreases below the systolic blood pressure and the artery ceases the opening and closing. The stethoscope placed closely to the artery downstream of the cuff is used to hear Korotkoff's sound; the blood pressures are measured. Cuff pressure when Korotkoff's sound begins to be heard is defined as the highest blood pressure and that when the sound disappears is defined as the lowest pressure. SPHYGMOMANOMETER Mercury Sphygmomanometer This includes a mercury manometer, an upper arm cuff, a hand inflation bulb with a pressure control valve and requires the use of a stethoscope to listen to the Korotkoff sounds. Relies on the ausculatory technique. Advantages: Regarded as the 'Gold Standard'. It is transportable and is understood by users. Can be used on most patients. Disadvantages: It contains toxic mercury which can lead to maintenance problems, although it is safe in normal useage. Can be prone to observer bias. Semi-automated device This includes an electronic monitor with a pressure sensor, a digital display, an upper arm cuff and a hand bulb. The pressure is raised manually using the hand bulb. The device automatically deflates the cuff and displays systolic and diastolic values. Pulse rate may also be displayed. Is battery powered and uses the oscillometric technique. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 Advantages: Is mercury-free, lightweight and compact. There is no observer bias and it is portable and easy to use. Disadvantages: It was originally designed for home use and may not be suitable for all patients, particularly those with arrhythmias. May be difficult to calibrate. Some cuffs cannot be washed or decontaminated. Automated device This includes an electronic monitor with a pressure sensor, a digital display and an upper arm cuff. An electrically driven pump raises the pressure in the cuff. Devices may have a user-adjustable set inflation pressure or they will automatically inflate to the appropriate level, about 30 mmHg above the predicted systolic reading. On operation of the start button the device automatically inflates and deflates the cuff and displays the systolic and diastolic values. Pulse rate may so be displayed. Devices may also have a memory facility that stores the last measurement or up to 10 or more previous readings. It is battery powered and uses the ocillometric technique. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 Block Diagram: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 Tabulation: S.No Patient Sphygmomanometer Semi Automated Automated Name Systolic Diastolic (mmHg) (mmHg) 1 X 2 Y 3 Z 4 A Systolic Diastolic (mmHg) (mmHg) Pulse Systolic Diastolic Pulse (bpm) (mmHg) (mmHg) (bpm) Result: Thus the blood pressure measurements are done using mercury sphygmomanometer, semi automated and automated devices for human. Ex. No 2 Real time monitoring of Echocardiography Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 Aim: To acquire real time ECG of 12 lead ECG system and analyse the signals. ECG is a transthoracic interpretation of the electrical activity of the heart over time captured and externally recorded by skin electrodes. It is a noninvasive recording produced by an electrocardiographic device. OBJECTIVES: Understand and be able to identify the different deflections seen in an electrocardiogram, a trace of the heart’s electrical activity. COMPONENTS REQUIRED: S.NO DESCRIPTION 1 ECG sensor with leads (electrode patches) RANGE QUANTITY 10 lead 1 No 2 Computer interface 1 No 3 PC 1 No 4 Gel some Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 8 DIAGRAM: Leads: Graphic showing the relationship between positive electrodes, depolarization wavefronts (or mean electrical vectors), and complexes displayed on the ECG. In electrocardiography, the word lead (pronounced /lid/) refers to the signals transmitted and received between two electrodes. The electrodes are attached to the patient's body, usually with very sticky circles of thick tape-like material (the electrode is embedded in the center of this circle). Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 9 ECG leads record the electrical signals of the heart from a particular combination of recording electrodes which are placed at specific points on the patient's body. PLACEMENT OF ELECTRODE: Ten electrodes are used for a 12-lead ECG. They are labeled and placed on the patient's body as follows: ELECTRODE LABEL (in the ELECTRODE PLACEMENT USA) RA On the right arm, avoiding bony prominences. LA In the same location that RA was placed, but on the left arm this time. RL On the right leg, avoiding bony prominences. LL In the same location that RL was placed, but on the left leg this time. V1 In the fourth intercostal space (between ribs 4 & 5) to the right of the sternum (breastbone). V2 In the fourth intercostal space (between ribs 4 & 5) to the left of the sternum. V3 Between leads V2 and V4. V4 In the fifth intercostal space (between ribs 5 & 6) in the midclavicular line (the imaginary line that extends down from the midpoint of the clavicle (collarbone). Horizontally even with V4, but in the anterior axillary line. (The anterior V5 axillary line is the imaginary line that runs down from the point midway between the middle of the clavicle and the lateral end of the clavicle; the lateral end of the collarbone is the end closer to the arm.) V6 Horizontally even with V4 and V5 in the midaxillary line. (The midaxillary line is the imaginary line that extends down from the middle of the patient's armpit.) Unipolar vs. bipolar leads There are two types of leads—unipolar and bipolar. Bipolar leads have one positive and one negative pole. In a 12-lead ECG, the limb leads (I, II and III) are bipolar leads. Unipolar leads have only one true pole (the positive pole). The negative pole is a "composite" pole made up of Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 signals from lots of other electrodes. In a 12-lead ECG, all leads besides the limb leads are unipolar (aVR, aVL, aVF, V1, V2, V3, V4, V5, and V6). Limb leads In both the 5- and 12-lead configuration, leads I, II and III are called limb leads. The electrodes that form these signals are located on the limbs—one on each arm and one on the left leg.The limb leads form the points of what is known as Einthoven's triangle. • Lead I is the signal between the (negative) RA electrode (on the right arm) and the (positive) LA electrode (on the left arm). • Lead II is the signal between the (negative) RA electrode (on the right arm) and the (positive) LL electrode (on the left leg). • Lead III is the signal between the (negative) LA electrode (on the left arm) and the (positive) LL electrode (on the left leg). Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 Augmented limb leads Leads aVR, aVL, and aVF are 'augmented limb leads'. They are derived from the same three electrodes as leads I, II, and III. However, they view the heart from different angles (or vectors) because the negative electrode for these leads is a modification of 'Wilson's central terminal', • Lead aVR or "augmented vector right" has the positive electrode (white) on the right arm. The negative electrode is a combination of the left arm (black) electrode and the left leg (red) electrode, which "augments" the signal strength of the positive electrode on the right arm. • Lead aVL or "augmented vector left" has the positive (black) electrode on the left arm. The negative electrode is a combination of the right arm (white) electrode and the left leg (red) electrode, which "augments" the signal strength of the positive electrode on the left arm. • Lead aVF or "augmented vector foot" has the positive (red) electrode on the left leg. The negative electrode is a combination of the right arm (white) electrode and the left arm (black) electrode, which "augments" the signal of the positive electrode on the left leg. The augmented limb leads aVR, aVL, and aVF are amplified in this way because the signal is too small to be useful when the negative electrode is Wilson's central terminal. Together with leads I, II, and III, augmented limb leads aVR, aVL, and aVF form the basis of the hexaxial reference system, which is used to calculate the heart's electrical axis in the frontal plane. aVR = -(I + II)/2 aVL = I - II/2 aVF = II - I/2 PRINCIPLE: An electrocardiogram (ECG or sometimes EKG) is a reading of the electrical activity of the heart The potentials originated in the individual fibers of heart muscle are added to produce the ECG wave form , the ECG reflects the rhythmic electrical depolarization and repolarization of the myocardium(heart muscle ) associated with the contractions of the atria and ventricles. There are electrical signals that can be detected from two different types of cardiac muscle, the auto rhythmic fibers that make up the electrical conduction system of the heart and the cardiac muscles that produce muscle contractions. The signals are detected by electrodes that measure electrical potential between different points on the body. A typical ECG is taken using 10 wires Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 and is referred to as a 12 lead ECG. Electrodes are place on each limb and are referred to as augmented limb leads and 6 precordial leads are placed directly on the chest. The final lead is the ground lead and is generally placed on the right leg, although it can be placed anywhere on the body. The ground is used as a point of reference. In the ECGs that you will record in class, we will use 3 leads. The leads will be placed on the inside of the forearms near the elbow joint and the ground lead will be placed on the right wrist. STANDARD ECG : The electrical conduction system of the heart consists of the sinoatrial node (SA node), located in the superior wall of the right atrium, which is the heart’s primary pacemaker. These fibers automatically produce an electrical signal at a particular pace that is conveyed to atrioventricular node (AV node), located in the medial wall of the right atrium. The signal from the AV node travels to the atrioventricular bundle and the right and left bundle branches, located in the interventricular septum. From the septum, the signal travels to the Purkinje fibers, which project along the outer walls of the ventricles. Not only does the signal travel through the autorhythmimc fibers that make up the electrical conduction system, but the electrical signal travels through gap junctions to the cardiac muscles, where electrical impulses lead to cardiac muscle contractions. The ECG is the electrical activity of the heart as it is displayed on an oscilloscope. It has 5 different wave deflections: P. Q, R, S and T. In general, ECGs are useful for detecting abnormal rhythms caused by damage to the autorhythmic fibers or abnormal levels of electrolytes such as potassium, sodium or calcium. They are often not as useful in detecting damage to cardiac muscle. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 The P. Q, R, S and T deflections and intervals between indicate the following: The P wave represents the electrical signal produced by the SA node in the right atrium and the propagation of that impulse to the AV node and to the cardiac muscles of the atria. The PR/PQ interval runs from the beginning of the P wave to the beginning of the QRS complex. During this interval includes what is mentioned in the P wave as well as the contraction produced by the atrial cardiac muscles. Atrial contraction occurs during the flat part of the interval. The QRS complex represents the depolarization of the ventricles. Reflected in this is the movement of the electrical signal down the AV bundle, right and left bundle branches, Purkinje fibers and the propagation of that signal to the cardiac muscles of the ventricles. Because of the greater muscle mass of the ventricles, the signal is much larger than the P wave. Also during this time you have repolarization of the atrial cardiac muscles, however the electrical signal is masked by the large depolarization produced by the ventricular muscles. The ST interval represents the contraction of the ventricles. It is measured from the junction of where QRS ends and the T wave begins. The T wave represents the repolarization of the ventricles. The absolute refractory period occurs during the ST interval and extends to the apex of the T wave. The relative refractory period the latter half of the T wave. The QT interval runs from the beginning of the QRS complex to the end of the T wave. This represents the time it takes for depolarization and repolarization of the ventricles. This interval will vary with heart rate. Typical times for segments of an ECG Segment time (ms) P/Q interval 120-200 QRS complex 60-100 ST interval 80-120 Q/T interval 300-440 Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 Bipolar Limb Leads Unipolar Limb Leads: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 Unipolar Chest Leads Right Leg Drive Circuit ECG – Recording Setup Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 ECG Recorder Experimental procedure: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 1) Choose one member of your group to be the subject and apply the electrode patches as described in the experimental setup. 2) Record the ECG of your subject at rest. The subject should be sitting, relaxed, and breathing at a normal rate. You may want to record rate of breathing (optional) to compare how it changes under the other conditions. Record the required interval times. 3) Record the ECG of your subject after three minutes of deep, slow breathing that is done in a supine or sitting position. Try to get the breathing rate down to 5 breaths or less a minute. Record the breathing rate. Record the required interval times. 4) Record the ECG of your subject after three minutes of mild exercise. You may choose jogging in place or choose some other type of exercise for that length of time. Record the breathing rate. Record the required interval times. Analysis: 1) Choose three representative ECG traces and measure the intervals that are listed in the chart above for the three different conditions. Your ECG Lab worksheet has a table for you to record this information. 2) Calculate an average for the intervals. 3) Calculate heart rate and the average heart rate under the three different conditions. Tabulation : Parameters (mv) I II III avR avL avF V1 Max In LEAD R amp (µv) R’ amp (µv) P amp (µv) P’ amp (µv) T amp (µv) T’ amp (µv) Q amp (µv) S amp (µv) Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 1 ST elevation (mm) ST Depression (mm) ST Slope (mv/ sec) QR Time (m/ sec) Interpretation Report:Parameters Rate Observatio Normal n limits Indications Average Heart Rate(bpm) Heart Variation Median PR Interval(ms) P wave amp/ P duration(ms) QRS Width(ms) QRS&(deg)+ T axis QTC(ms) ST elev(mm) ST depr(mm) Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 Max T-wave Rhythm Conduction Ischemia Infarction Hypertrophy Other Abnormality RESULT:Thus the real time ECG is recorded and the signal is analysed for the subject Ex. No 3 Working of different types of Diathermy equipments – study AIM: Heat energy is applied to the painful area which speeds up the cellular metabolism and increases the blood flow APPARATUS REQUIRED: *Shortwave diathermy unit. *Pad electrodes. *Ultrasound diathermy unit. *Surgical diathermy unit. DESCRIPTION: Diathermy involves heating deep muscular tissues. When heat is applied to the painful area, cellular metabolism speeds up and blood flow increases. The increased metabolism and Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 circulation accelerates tissue repair. The heat helps the tissues relax and stretch, thus alleviating stiffness. Heat also reduces nerve fiber sensitivity, increasing the patient's pain threshold. There are three methods of diathermy. In each, energy is delivered to the deep tissues, where it is converted to heat. The three methods are: • Shortwave diathermy: The body part to be treated is placed between two capacitor plates. Heat is generated as the high-frequency waves travel through the body tissues between the plates. Shortwave diathermy is most often used to treat areas like the hip, which is covered with a dense tissue mass. It is also used to treat pelvic infections and sinusitis. The treatment reduces inflammation. Most machines function at 27.33 megahertz. • Ultrasound diathermy: In this method, high-frequency acoustic vibrations are used to generate heat in deep tissue. • Surgical diathermy:The use of electrocautery for coagulation or cauterization, as for sealing a blood vessel, resulting in local tissue destruction Diathermy is also used in surgical procedures. Many doctors use electrically heated probes to seal blood vessels to prevent excessive bleeding. This is particularly helpful in neurosurgery and eye surgery. Doctors can also use diathermy to kill abnormal growths, such as tumors, warts, and infected tissues. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 A. SHORTWAVE DIATHERMY (SWD) Aim: To study the working of Shortwave Diathermy Theory: Short Wave diathermy current is a high frequency alternating current. The heat energy obtained from the wave is used for giving relief to the patient. Its frequency is 27,120,000 cycles per second and the wavelength is 11 metre. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 A shortwave diathermy unit is a device designed to generate radiofrequency radiation and transfer it,via cables and electrodes, to the area to be treated. The units can be operated in either a continuous wave or pulsed mode but both produce heat in deep tissue. TWO FORMS OF SHORTWAVE DIATHERMY: The units can be operated in either ¾ Continuous mode ¾ Pulsed mode Two basic types of electrodes (applicators) are in use: Capacitor-type Inductor type. In the first case tissue heating is basically due to the radiofrequency electric field, while for the inductive electrodes (coils), heating occurs by a combination of electric field effects and currents induced in the tissue by the magnetic field. The heating profile of the two mechanisms is somewhat different. These devices are capable of generating a sufficiently high level of radiation that there may be cause for concern for the safety of the gonads and, in the case of pregnant patients, the foetus. Improper use of the machine may result in burns and/or scalds and deep tissue or organ damage. It must be noted that the level of radiation present in the vicinity of a diathermy unit may be increased by the presence of nearby metallic objects or other units or by reflection from the wall. Care must be taken to ensure that the shortwave radiation does not cause interference with other equipment. SWD is most commonly used for thermotherapy at a frequency of 27.12 MHz. WORKING OF SHORT WAVE DIATHERMY: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 Shortwave diathermy heats the tissue by causing oscillations of electromagnetic energy of high frequencies. The physiologic effects of temperature occur at the site of the application and in distant tissue. Circuit diagram of shortwave diathermy The local effects occur due to the elevated local temperature which is associated with increased local blood flow, capillary dilatation and capillary permeability. It results in higher level tissue metabolism and more rapid transfer of nutritional ingredients to the end organs and tissues. It promotes faster healing. Short wave heat increases connective tissue elasticity, reduces muscle spasm, and sedates the nerve endings to change the pain threshold. Distant changes from the heated target location include reflex vasodilatation and reduction of muscle spasm, increase in body temperature, respiratory and pulse rates and decreased blood pressure. Diathermy increases white blood cell concentration in the area of chronic inflammation . TREATMENT: Before administering the treatment the operator should: • ensure that the thermal sensitivity of the patient is not impaired by analgesics, • ensure that the patient has removed all metallic objects (rings, watches, metal rimmed glasses, etc.) from the treatment area, • Remove towelling or clothing from the treatment area, Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 • ensure that the skin is dry, • ensure that if the patient is wearing a hearing aid, it is removed, ask the patient to report immediately any symptoms experienced during the treatment except 'a mild, comfortable warmth, • ensure that the cables are correctly connected to both the machine and the applicator, not rest the applicator or cables over metal surfaces, align the applicator accurately to ensure an appropriate pattern of heating, • ensure that the testes are not directly irradiated and that care is taken to minimize indirect irradiation, • ensure that the cables leading to the applicator are not placed in the vicinity of the patient's non targetted tissue, • ensure that the chair or other patient support is not metallic and that other large metallic objects are kept at least three metres from the electrodes and cables. After activating the unit the operator should: • remain at least 1 m from the electrodes and 0.5 m from the cables during treatment, • ensure that the patient maintains the correct position and remains cooperative, • not leave the patient during the treatment, unless the patient has been supplied with an emergency • cut-off switch and the patient is reliable, • not allow the patient to touch the unit, • ensure that no other person is in the vicinity of the unit or of the applicator during the treatment, inaccordance with the administrative controls established by the user. TREATMENT TIME: Initial Stage :5-10 minutes Moderate Stage :10-20 minutes Severe State :20-30 minutes ADAVANTAGES: 1. Relaxation of the muscles Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 2. Effective in bacterial infections 3. Relief of pain DISADVANTAGES: 1. Burns 2. Scalds (Boils) 3. Overdose 4. Shock 5. Electric Sparking 6. Faintness Result:The working principle of shortwave Diathermy is studied B. ULTRASOUND DIATHERMY Aim:To study the working of Ultrasound Diathermy Theory:Ultrasound is sound above the limits of human hearing. The therapeutic effects of ultrasound result from the conversion of sound to heat energy. Ultrasound diathermy typically employs frequencies between 0.8 and 1 MHz. Ultrasound diathermy is considered a deep heating modality in that most absorption occurs far beneath the skin. It is most commonly used to treat tendonitis and bursitis, musculoskeletal pain, degenerative arthritis, and contractures. Maximal heating may be limited by deep tissue factors and not by skin tolerance. Ultrasound may be applied directly by placing the applicator on the skin, or indirectly by immersing the body part and applicator in a water-filled container. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 Because of the importance of appropriate technique and inherent dangers, ultrasound diathermy should be applied by a trained attendant and the devices are not appropriate for unsupervised home use. It's an electromagnetic wave different from sound waves. The frequencies of waves employed for medical purposes are between 5,00,000 and 3,000,000 cycles/sec. GENERATION OF ULTRASONIC WAVES: Ultrasonic waves are generated by vibration of a Crystal mounted on a special head. Block diagram of ultrasonic diathermy unit Ultrasound provides therapeutic benefit via thermal (continuous ultrasound) and nonthermal (pulsed ultrasound) effects . CIRCUIT DESCRIPTION:Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 The heart of the system is timed oscillator which produce the electrical oscillation of required frequency. The oscillator output is given to the power amplifier which derives the piezoelectric crystals to generate ultrasound waves. Power amplification is achieved by replacing the transistor in a typical LC tuned colpitt oscillator by 4 power transistors placed in a bridge configuration. The delivery of the ultrasounds power to a patient is to be done for a given time. This is controlled by incorporating a timer to switch on the circuit. The timer can be mechanically spring loaded type or an electronic one, allowing time settings from 0 to 30 minutes. Procedure: 1. The required time and frequency are set for treatment. 2. The ultrasound crystal will be kept on the portion of body which has to be treated. Result:The study of Ultrasound Diathermy working principle is studied. C. SURGICAL DIATHERMY Aim: To study the working of surgical diathermy Theory: Surgical diathermy apparatus comprising a power source, an active electrode for operation on a patient, at least one circuit means for attachment to the patient, interconnection means operatively interconnecting power source with active electrode and at least one circuit means, each circuit means comprising a respective capacitive neutral plate for attachment to the patient, a transformer interconnecting power source to capacitive neutral plate, and a compensator comprising a potential amplifier transformer-coupled by transformer in series between power source and capacitive neutral plate, said respective amplifier being operated to inject a voltage through the transformer which is substantially equal to the potential drop across the capacitive reactance of the capacitive neutral plate. Block diagram of surgical diathermy Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 2 PRINCIPLE: Pertaining to the treatment of disease by manipulative and operative methods. MONOPOLAR SURGICAL DIATHERMY: Localized heating of tissue without muscle twitch or spasm can be effected by passing a large alternating current of high frequency through parts of the body. This is surgical diathermy or electrosurgery. If the power is sufficient, the temperature reached causes coagulation of the blood or even disintegration of the tissue due to boiling. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 This technique is employed in a controlled manner during surgery to seal small blood vessels by coagulation, and to cut through layers of tissue. Cutting and coagulation is achieved by applying electric current to the tissues via small handheld probes (electrodes). The current flows out of the body (usually) through a very large electrode placed on the skin at some remote site (e.g. on the thigh). At this electrode (the indifferent electrode) the current density is very low, so little heating occurs. However, at the hand-held electrode the density is very high due to its small contact area, and so great heat is developed. Surgical diathermy is a special electrical unit generating a high frequency current which produces heat when passed through tissues.Depending upon the speed of the current and the resulting heat, a diathermy unit can achieve the following results: 1. Cutting with high Speed or intensity. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 2. Coagulation (cooking compared to burning due to heated needle in electrocautery). (a) If weak, epilation. (b) If strong, coagulation producing destruction. 3. Desiccation ensues by passing medium current through a mono-terminal electrode at a slight distance from the surface which produces sparking heat and results in drying up the tissues • Coagulation o Produced by interrupted pulses of current (50-100 per second) o Square wave-form • Cutting o Produced by continuous current o Sinus wave-form. Diathermy currents may be generated by valve or transistor circuits and may include a range of protection and monitoring systems. The frequencies used are typically in the range 0.5 to 3 MHz and so it is difficult to achieve true earth-free operation due to the capacitance between the patient and earth, and the capacitance of the leads of monitoring equipment. The system described above is monopolar, whereas bipolar systems are available in which the heating currents only flow between the two tips of special forceps. These are useful for fine work and when the patient has a pacemaker which might malfunction in the presence of the very large circulating high- frequency current. BIPOLAR SURGICAL DIATHERMY As an alternative to the conventional (monopolar) surgical diathermy, in which the electrical current flows from a small active probe through the body to a large indifferent electrode, the path of the current can be constrained to pass only through the tissue being treated. This is achieved using a special forceps in which the two halves of the instrument are insulated from one another and in effect one half becomes the source of the current and the other the destination, thus replacing the active and indifferent electrodes mentioned above. Bipolar diathermy has the advantage that electric currents do not pass through parts of the body which are not being treated and also it is possible to be much more precise with the quantity of tissue being coagulated. For instance, a small blood vessel gripped between the jaws of the forceps will be coagulated, whereas tissue next to other parts of the forceps will not be heated at Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 all. It is useful in microsurgery, but is often called for in other applications, particularly where there may be interference with the action of a cardiac pacemaker by the stray diathermy currents arising with monopolar systems. Most modern diathermy machines can support the use of bipolar probes without modification. Older types are generally unsuitable since the indifferent connection to the machine is at earth potential, or is capacitively coupled to earth. An ideal bipolar diathermy current generator should be fully isolated from earth so that there will be no tendency for diathermy currents to circulate in the body to find other routes to earth. This is difficult to achieve at the frequencies used (1-3 MHz). Result:The study of surgical diathermy is thus performed in a subject. Ex. No 4 ECG wave analysis using simulator Aim: To stimulate ECG signal and to analyze the signals in Time and Frequency domain. Apparatus Required: ECG machine, conducting gel, leads Theory: The electrocardiogram is an instrument which records to electrical activity of heart. Electrical signals from the heart, characteristically placed the normal mechanical functions and monitoring of these signal has great clinical significance. Electrographs are used in authorization laboratories, coronary care units and for routine diagnostic applications in cardiology. The diagnostically useful frequency range is usually accepted as 0.05-150hz. The interface of non-biological origin can be handled by using modern differential amplifier Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 which are capable of providing excellent rejection capabilities CMMR of the order of 100- 200db with 5KΩ unbalance in the lead is a desirable feature of ECG machine. The instability of the baseline originating from the chane of the contact impedance, demands the application of the automatic baseline stabilizing circuit. A minimum of two paper feeds is necessary(20-50 per sec) for ECG reading. The lead selector switch is used to drive the required lead configurations and it to dc coupled amplifiers. Einthoven Triangle: It starts the vector sum of the projection of the frontal phase cardiac to vector to the 3 axis of the Einthoven triangle will be zero. Lead 1: Left arm and right arm Lead 2: Left leg and right leg Lead3: Left and right arm Block diagram explanation: The potentials are picked up by the patients electrode are taken to the lead selection switch. In the lead selector, the electrodes are selected two by two according to the lead program. By capacitive coupling the lead is connected to differential pre amplifiers to avoid problem with small dc voltage the way originate from polarisation. The output of the power amplifier is fed to the pen motor which deflect the writhing on the paper. Bipolar Leads: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 ECG is recorded by using two electrodes such that the final trace corresponds to the difference of electrical potentials existing between them, they are called standard leads and have been universally accepted. They are also called as einthoven lead. Unipolar Lead: If the electrode is placed close to the heart , higher potentials can be obtained, that normally available at limbs. ECG is recorded between a single exploratory electrode and the central a potential corresponding to the centre of the body. The combination of several electrodes tied terminal, which has reference electrode is obtained by together at one point, it is of 2 types 1 Limb lead 2 Pericordial leads LEAD 1 WAVE AMP(V) TIME(s) FREQUENCY POWER P QRS T HEART RATE: LEAD 2 WAVE AMP(V) TIME(s) FREQUENCY POWER P QRS T HEART RATE: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 LEAD 3 WAVE AMP(V) TIME(s) FREQUENCY POWER P QRS T HEART RATE: Result: The ECG physiograph was recorded and analyzed. Ex. No 5 Real time patient monitoring system AIM:- To display ECG, EEG and EMG signals along with pulse rate using patient monitor. Apparatus Required: Display, leads and electrodes. THEORY: Patient monitoring systems are used for measuring automatically the value of the patient’s important physiological parameters during a surgical operation. The patient is deprived of several manual reaction mechanisms which normally restores abnormalities in his physical conditions or alert other people. Harm done to the patient can be prevented. BLOCK DIAGRAM EXPLANATION: ECG: The biopotential generated by muscles of heart results in ECG. The voltage difference at any two sites due to electrical activity of the heart is called “lead”. There are basically two leads; i) Unipolar leads ii) Bipolar leads Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 UNIPOLAR LEAD: There are two types, one is limb lead in which two of the limb leads are tied together and recorded with respect to the third. The other one is pericardial lead which employs an exploring electrode to record the potential of the heart action on the chest at six different positions. BIPOLAR LEAD: ECG is recorded by using two electrodes such that the final trace corresponding to the difference of electrical potential existing between these two are called standard leads. EEG: The recorded representation of bio-electric potential generated by the neuron activity of the brain is called EEG. Modern machines make the use of computerised EEG signal processing. FREQUENCY ANALYSER: It takes the low EEG wave mathematically , analyses them and breaks them into their component frequencies. Hence EEG signal is converted into simplified waveform called spectrum. COMPRESSED ANALYSER: The amplitude changes result in power of resulting frequency spectrum. COMPRESSED SPECTRUM ARRAY: In this format a series of computer smoothed spectral array are stretched vertically at several intervals. The origin of plot shifts vertically with time which produces dimensional graph. DSA: It displays power spectrum. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 SAMPLING RATE: Signal with high band width requires sampling to be carried out at high rate. A high sampling rate necessitates a large memory to store all the data. A sampling channel memory display system has sampling rate of 256 samples and multiple channel displays work as 100 samples. PULSE RATE: The pulse rate can be felt by placing the finger tip over the radial artery in the wrist. The pulse pressure and waveform are indicated for blood pressure and flow. The pulse gives a measure of pulse wave velocity which can be recorded and compared with ECG signal. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 The method used for detection of pulse changes are: a) Electrical impedance change b) Strain gauge c) Optical changes OBSERVATION TABLE: CASE I: ECG (bpm) NIBP (mmHg) SYS. TEMP. ( F) SPO2 % TEMP. ( F) SPO2 % DIA. CASE II: ECG (bpm) NIBP (mmHg) SYS. DIA. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 3 CASE III: ECG (bpm) NIBP (mmHg) SYS. TEMP. ( F) SPO2 % DIA. RESULT: Display of EEG, ECG, and EMG signals along with respective waveforms is studied and verified using the patient monitoring system. Ex. No 6. Ultrasound blood flow measurement to identify arteries and veins AIM: To measure the ultrasound blood flow inorder to identify arteries and veins. APPARATUS REQUIRED: • Power supply • Transmitter • Receiver • Power supply • Speaker PRINCIPLE OF WORKING: The principle of ultrasound blood flow measurement is the visualization and measurement of blood flow velocity by the shift in frequency of a continuous ultrasonic wave.The sensor used here is piezoelectric crystal.This sensor acts both as the transmitter and receiver.The ultrasonic waves transmitted by the transmitter are reflected by the motion of blood and is received by the receiver but here the received frequency is Doppler shifted.The Doppler frequency shift is a measure of the size and direction of the flow velocity. It is based on the analysis of echo signals Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 from the erythrocytes in the vascular structures. The relationship between blood velocity and frequency is given by V=(Δf.C)/(2fcosθ) Where v=blood flow velocity C=velocity of sound in blood f=transmitted frequency θ=angle of inclination of the incident wave to the direction of flow PROCEDURE: The sensor which is ultrasonic transducer is non-invasively placed on the subject’s wrist. This sensor has the transmitter and receiver. The transmitted signal gets Doppler shifted. Because of the Doppler effect, the frequency of these echo signals changes relative to the frequency to which the probe transmits. The incident ultrasound is scattered by the blood cells and the scattered wave is received by the receiver. This frequency shift is proportional to the velocity of the scatterers. Alteration in frequency occurs first as the ultrasound arrives at the scatterer and second as it leaves the scatterer. This Doppler shifted frequency wave can be viewed in the Cathode Ray Oscilloscope by properly connecting the output of the speaker to the CRO probes. To any one channel the probes are connected and the time period and offset are adjusted to get the Doppler frequency shifted wave with appropriate amplitude. The output wave can thus be traced out. Also when the output of the receiver is connected to the speaker we will be able to Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 listen to the sound of the blood flow in arteries and veins. RESULT: Thus arteries and veins are identified with ultrasound blood flow meter. Ex. No 7 Respiratory system analysis using Spirometer Aim : To record the changes in pulmonary volume and capacities by using spirometer. Apparatus required: ¾ Peak flow meter ¾ Mouth piece ¾ USB cable ¾ Computer. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 Theory : Spirometry is the most common of the Pulmonary Function Tests (PFTs), measuring lung function, specifically the measurement of the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is an important tool used for generating pneumotachographs which are helpful in assessing conditions such as asthma, pulmonary fibrosis and cystic fibrosis. The spirometry test is performed using a device called a spirometer, which comes in several different varieties. Most spirometers display the following graphs, called spirograms: • a volume-time curve, showing volume (liters) along the Y-axis and time (seconds) along the X-axis • a flow-volume loop, which graphically depicts the rate of airflow on the Y-axis and the total volume inspired or expired on the X-axis • Forced Vital Capacity (FVC): The basic forced volume vital capacity (FVC) test varies slightly depending on the equipment used. Generally, the patient is asked to take the deepest breath they can, and then exhale into the sensor as hard as possible, for as long as possible. It is sometimes directly followed by a rapid inhalation (inspiration), in particular when assessing possible upper airway obstruction. Sometimes, the test will be preceded by a period of quiet breathing in and out from the sensor (tidal volume), or the rapid breath in (forced inspiratory part) will come before the forced exhalation. During the test, soft nose clips may be used to prevent air escaping through the nose. Filter mouthpieces may be used to prevent the spread of microorganisms, particularly for inspiratory maneuvers. • Turbine Transducer: The transducer which is used in spirometry is turbine transducer. It converts the flow of air, breathed by the patient, against a frictionless rotating vane into an electrical signal which is used to produce relevant plots. Block diagram: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 Procedure : ¾ Sit on the edge of your chair if possible, or sit up as far as you can in bed. ¾ Hold the incentive spirometer in an upright position. ¾ Place the mouthpiece in your mouth and seal your lips tightly around your lips. ¾ After each set of 10 deep breaths, practice coughing to be sure your lungs are clear. If you have an incision, support your incision when coughing by placing a pillow firmly against it. ¾ Load the patient’s details ie. Name, age, sex, height, weight, patient ID, etc. ¾ Click onto the FVC (Forced Vital Capacity) graph on the window; the forced expiration followed by forced inspiration will be recorded here. ¾ Click onto the SVC (Slow Vital Capacity) graph on the window; the SVC, being the maximum volume of air that can be exhaled slowly after a slow maximum inhalation will be recorded here. ¾ Click onto the MVV (Minute Ventilatory Volume) graph on the window; the measure of the maximum amount of air that can be inhaled and exhaled in one minute will be recorded here. ¾ Save the recorded values and analyse them using respective software. SPIROMETRY GRAPHS: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 FIG 1. FVC GRAPH Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 FIG 2. SVC GRAPH FIG 3. MVV GRAPH SIPROMETRY RESULTS: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 FVC RESULT Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 SVC RESULTS MVV RESULTS Result : Thus the changes in pulmonary volume and capacities are recorded using spirometer and analysed for a subject. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 Ex. No 8 Analysis of ECG abnormal wave pattern using Arrhythmia Simulator Aim:To record the changes in amplitude for a subject having arrhythmia. Theory The (ECG-A-S) is significantly and exclusively brought into existence to serve and poor and needy who reside in remote places, where proper medical facilities are not persistent. The (ECGA-S) system brings about the measuring certain of the patient’s normal and abnormal ECG parameters like Brachycardia, Tachycardia, Atrial fibrillation, Ventricular fibrillation. The main purpose of using a solar energy is to truly fulfill the purpose of the (ECG-A-S). The remote locations which could not even provide sufficient medical facilities cannot afford to bring about a regular power supply either. Thus the use of solar potential will surely bring in the demand for the same. It consists of an efficient solar panel which receives the incident solar energy and converts into electrical potential. The energy thus produced can be either saved for direct usage or can be used for charging a battery, which in turn can be used to power the biomedical equipment (the simple ECG Arrhythmia). Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 4 ECG ARRHYTHMIA SIMULATOR: ECG Arrhythmia simulator is used for gathering physiological data (ECG) of organism under normal condition and processing the signals over time to find various heart blocks. ECG Arrhythmia simulator is an important technique for biomedical research and clinical medicine. Various grades of heart block can be measured in ambulatory subjects and proper diagnosis can be physician. Biomedical research in ECG Arrhythmia simulator is currently with producing patient monitoring equipment for the detection of ECG arrhythmias. To make comparative evaluations of the widely differing specification, it is necessary to be able to simulate such arrhythmias while retaining control of both number and frequency of abnormal beats and the Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 degree of deviation from normality. This enables not only the counting circuits of such monitoring equipment, but also the threshold levels below which an ECG complex is considered abnormal, to be tested. The similar described is designed for this purpose and utilizes pulse-shaping techniques together with appropriate logic control circuitry and powered using solar energy via battery which is a major advantage in using in rural areas. The most common symptom of arrhythmia is an abnormal awareness of heartbeat, termed palpitations. These may be infrequent, frequent, or continuous. Some of these arrhythmias are harmless but many of them predispose to adverse outcomes. These abnormalities in the functioning of the heart invariably manifest themselves in ECG waveform. Arrhythmia could be classified by rate (Normal, Tachycardia, Bradycardia), or mechanism (Automaticity, Fibrillation). It is also appropriate to classify by site of origin like Atrial, junctional arrhythmias, Atrio-ventricular, ventricular, heart blocks. Power supply is connected to the simulator. A simulator is a device which is an imitation of the real time record of ECG. All the abnormality and normal ECG waveforms are stored in it. DIFFERENT ECG WAVEFORMS NORMAL ECG WAVEFORM BRACHYCARDIA TACHYCARDIA Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 ATRIAL FIBRILLATION VENTRICULAR FIBRILLATION Each heart beat originates as an electrical impulse from a small area of tissue in the right atrium of the heart called the sinus node. The impulse initially causes both of the atria to contract, then activates the atrioventricular (or AV) node which is normally the only electrical connection between the atria and the ventricles , which can be called as main pumping chambers. The impulse then spreads through both ventricles via the Bundle of His and the Purkinje fibres causing a synchronised contraction of the heart muscle, and thus, the pulse. In adults the normal resting heart rate ranges from 60 to 80 beats per minute. The resting heart rate in children is much faster Bradycardia (Brad) A slow rhythm, beats less than 60 beats/min, is called bradycardia. This may be caused due to a pause in the normal activity of the sinus node or by blocking of the electrical impulse on its way from the atria to the ventricles. There is a long RR interval in bradycardia Tachycardia (Tach) Any resting heart rate faster than 100 beats/minute is called as tachycardia. Increased heart rate is a normal response to physical exercise or emotional stress. Inverted QRS waveform is obtained with short RR intervals in tachycardia. Atrial Fibrillation (A-fib) Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 Atrial fibrillation affects the upper chambers of the heart, known as the atria. Atrial fibrillation may be due to serious underlying medical conditions. It is not typically a medical emergency. P wave and T wave is fibrillated or lost in fibrillation. Ventricular Fibrillation (V-fib) Ventricular fibrillation occurs in the ventricles (lower chambers) of the heart; it is always a medical emergency. If left untreated, ventricular fibrillation can lead to death within minutes. When a heart goes into V-fib, effective pumping of the blood stops. Vfib is considered a form of cardiac arrest. No amplitude and frequency could be seen in Vfib as it is an irregular waveform. There is no FFT obtained. Thus the different abnormal ECG waveforms are monitored using ECG-A-S in remote areas using the mobile unit (ECG-A-S). It is also possible to connect an alarm to the ECG-A-S or setting up threshold limits over the parameters. Thus when the patient’s ECG parameters exceed or cross over the preset limits, then the sensors alarms and alert the attention towards the patient, and this entire set up is possible to be connected to a solar panel so that it can work even in the absence of electricity or even during night. Result:The abnormal changes in amplitude for a subject having arrhythmia is verified and recorded. Ex. No 9 EEG wave analysis using simulator Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 AIM: To measure and record the amplitude and time taken for the different alpha , theta, beta and gamma EEG waves. APPARATUS REQUIRED: 1. EEG stimulator 2. Connecting probes 3. Biokit physiograph 4. PC THEORY: Electroencephalography (EEG) is the recording of electrical activity along the scalp produced by the firing of neurons within the brain. In conventional scalp EEG, the recording is obtained by placing electrodes on the scalp with a conductive gel or paste. Electrode locations and names are specified by the International 10–20 system for most clinical and research applications. Each electrode is connected to one input of a differential amplifier (one amplifier per pair of electrodes); a common system reference electrode is connected to the other input of each differential amplifier. These amplifiers amplify the voltage between the active electrode and the reference. A typical adult human EEG signal is about 10µV to 100 µV in amplitude when measured from the scalp and is about 10–20 mV when measured from subdural electrodes. EEG WAVE PATTERNS: DELTA WAVE: Delta is the frequency range up to 4 Hz. It tends to be the highest in amplitude and the slowest waves. It is seen normally in adults in slow wave sleep. It is also seen normally in babies. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 THETA WAVE: Theta is the frequency range from 4 Hz to 7 Hz. Theta is seen normally in young children. It may be seen in drowsiness or arousal in older children and adults; it can also be seen in meditation. ALPHA WAVES: Alpha is the frequency range from 8 Hz to 12 Hz. Hans Berger named the first rhythmic EEG activity he saw, the "alpha wave. It emerges with closing of the eyes and with relaxation, and attenuates with eye opening or mental exertion. The posterior basic rhythm is actually slower than 8 Hz in young children. BETA WAVES: Beta is the frequency range from 12 Hz to about 30 Hz Beta activity is closely linked to motor behaviour and is generally attenuated during active movements. It is the dominant rhythm in patients who are alert or anxious or who have their eyes open. Since an EEG voltage signal represents a difference between the voltages at two electrodes, the display of the EEG for the reading encephalographer may be set up in one of several ways. The representation of the EEG channels is referred to as a montage. BIPOLAR MONTAGE: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 Each channel (i.e., waveform) represents the difference between two adjacent electrodes. The entire montage consists of a series of these channels. For example, the channel "Fp1-F3" represents the difference in voltage between the Fp1 electrode and the F3 electrode. The next channel in the montage, "F3-C3," represents the voltage difference between F3 and C3, and so on through the entire array of electrodes. REFERENTIAL MONTAGE: Each channel represents the difference between a certain electrode and a designated reference electrode. There is no standard position for this reference; it is, however, at a different position than the "recording" electrodes. Midline positions are often used because they do not amplify the signal in one hemisphere vs. the other. Another popular reference is "linked ears," which is a physical or mathematical average of electrodes attached to both earlobes or mastoids. AVERAGE REFERNTIAL MONTAGE: The outputs of all of the amplifiers are summed and averaged, and this averaged signal is used as the common reference for each channel. LAPLACIAN MONTAGE: Each channel represents the difference between an electrode and a weighted average of the surrounding electrode. When analog (paper) EEGs are used, the technologist switches between montages during the recording in order to highlight or better characterize certain features of the EEG. With digital EEG, all signals are typically digitized and stored in a particular (usually referential) montage; since any montage can be constructed mathematically from any other, the EEG can be viewed by the electroencephalographer in any display montage that is desired. TABULAR COLUMN: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 AMPLITUDE(V) WAVES TIME(S) FREQUENCY(Hz) POWER ALPHA BETA THETA DELTA PROCEDURE: 1. From the EEG stimulator input is given to the biokit physiograph. 2. The physiograph kit is connected to the PC using RS232. 3. For the respective alpha, beta , theta and delta waves the amplitude and time are noted. 4. The FFT is performed for the respective waves and the values are noted. Result: Thus the EEG waves are studied and the amplitude and time for each waveforms are noted for a subject. Ex. No 10 Auditory system check up using Audiometer AIM: To plot audiogram of the subject using air conduction pure tone audiometer EQUIPMENTS REQUIRED: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 a) b) c) d) e) f) g) Sine wave generator 0 to 10KHz White noise generator L‐R selector Audio Amplifier – 2 Nos. Level Indicator Log Battery Charger THEORY: The human ear has three main sections, which consist of the outer ear, the middle ear, and the inner ear. Sound waves enter the outer ear and travel through the ear canal to the middle ear. The ear canal channels the waves to the eardrum, a thin, sensitive membrane stretched tightly over the entrance to the middle ear. The waves cause the eardrum to vibrate. It passes these vibrations on to the hammer, one of three tiny bones in the ear. The hammer vibrating causes the anvil, the small bone touching the hammer, to vibrate. The anvil passes these vibrations to the stirrup, another small bone which touches the anvil. From the stirrup, the vibrations pass into the inner ear. The stirrup touches a liquid filled sack and the vibrations travel into the cochlea, which is shaped like a shell. Inside the cochlea, there are hundreds of special cells attached to nerve fibers, which can transmit information to the brain. The brain processes the information from the ear and this distinguishes between different types of sounds. Air and bone conduction: Air conduction, by definition, is the transmission of sound through the external and middle ear to the internal ear. Bone conduction, on the other hand, refers to the transmission of sound to the internal ear mediated by mechanical vibration of the cranial bones and soft tissues. The most important diagnostic differential from the standpoint of the functional hearing tests is the relationship between air and bone Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 conduction acuity. Clinical observation has shown that hard‐of‐hearing patients with middle ear disease have normal hearing by bone conduction, whereas patients with inner ear involvement have decreased or diminished bone–conduction.It has been concluded from clinical observations that approximately 60dB loss is the maximal air conduction impairment to be anticipated with middle ear defect. Therefore, if the air conduction loss in a patient with apparently typical middle ear pathology exceeds 60 dB, it is likely that inner ear impairment is superimposed on the middle ear lesion. BLOCK DIAGRAM: BLOCK DIAGRAM DESCRIPTION: Sine wave generator Sine wave generator is used to generate a signal representing the periodic value of a given mathematical function, especially sine waveform, the range here is 0‐ 10 KHz and the output ranges from 2V Pk to Pk. White noise generator A white noise generator produces a sound that is random in character which sounds like a rushing waterfall or wind blowing through trees. White noise is a random signal with a flat power spectral Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 5 density. In other words, the signal contains equal power within a fixed bandwidth at any center frequency. Audio amplifier Audio amplifier is an electronic amplifier that amplifies low power audio signals to a required level. The audio amplifier used in this application has a frequency range of 0‐10KHz. Level Indicator The level indicator displays the level of sound in decibels it has LEDs which indicates the sound level given to the subject. L‐R selector The L‐R selector is used to select the ear in which the subject wishes to determine the threshold of hearing. PROCEDURE: 1) To plot audiogram of the subject using air conduction pure tone audiometer a) b) c) d) e) f) g) h) i) j) k) Connect the modules as per the block diagram. Switch ON the battery. Adjust masking level to a suitable level so that it does not cause discomfort to the subject Put L, R switch in L position. Keeping x1, x10 switch and set frequency in steps of 100Hz. Adjust output dB level till the subject hears the sound. Note the frequency and output dB level from DSO and level indicator respectively. Repeat the above mentioned procedure for different set of frequencies. Put L, R switch in R position Repeat the above mentioned procedure for the right ear. Plot the graph of frequency versus output dB level for L, R. TYPICAL AUDIOGRAM Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 -10 0 Sound Level in dB +10 +20 +30 +40 +50 +60 +70 +80 200 500 1K 2K 3K 4K 5K 6K 7K 8K 9K 10K 11K Frequency in Hz Left Ear Response Right Ear Response L + R Ear Response TABULAR COLUMN Frequency Decible(dB) Left Right Left & Right GRAPH Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 -20 -15 (dB) -10 200 -5 400 600 --------------Æ Frequency 800 1000 RESULT: The graph of frequency verses output dB level gives audiogram of the subject. Ex. No 11 Heart sound measurement using PCG Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 AIM The basic aim of phonocardiograph is to pick up the different heart sounds, filter out the heart sounds and to display or record them. APPARATUS REQUIRED • Power supply • Digital storage oscilloscope • Head phone • Phonocardiograph THEORY A Phonocardiogram or PCG is a plot of high fidelity recording of the sounds and murmurs made by the heart with the help of the machine called phonocardiograph, or "Recording of the sounds made by the heart during a cardiac cycle". The sounds are thought to result from vibrations created by closure of the heart valves. There are at least two: the first when the atrioventricular valves close at the beginning of systole and the second when the aortic valve closes at the end of systole. It allows the detection of sub audible sounds and murmurs, and makes a permanent record of these events. In contrast, the ordinary stethoscope cannot detect such sounds or murmurs, and provides no record of their occurrence. The ability to quantitate the sounds made by the heart provides information not readily available from more sophisticated tests, and provides vital information about the effects of certain cardiac drugs upon the heart. It is also an effective method for tracking the progress of the patient's disease. Heart sounds are classified into four groups on the basis of their mechanism of origin, they are 1. Valve closure sound 2. Ventricular filling sound 3. Valve opening sounds and 4. Extra cardiac sounds Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 HEART SOUNDS First heart sound Second heart sound BLOCK DIAGRAM AMPLIFIER TRANSDUCER AMPLIFIER PCG DISPLAY BUFFER OUT LEVEL 5 FILTERS AMPLIFIER AMPLIFIER AUDIO (DSO) MICROPHONE Valve closure sound Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 These sounds occur at the beginning of systole (first heart sound) and the beginning of diastole (second heart sound). The first heart sound is due to the closure of mitral and tricuspid valves associated with myocardial contraction. And the second heart sounds is due to the closure of the aortic and pulmonary valves. The first heart sounds are low frequency vibrations occur approximately 0.05s after the onset of the QRS complex of the ECG, the first heart sounds last for (0.1 to 0.12s) and the frequency ranges 30-50Hz.The second heart sound is due to the vibrations set up by the closure of semilunar valves. These sounds start approximately ( 0.03 to 0.05)s after the end of T wave of the ECG, this lasts for (0.08 to 0.14)s and have a frequency up to 250Hz. Ventricular filling sounds These sounds occur either at the period of rapid filling of the ventricles (third heart sound) or during the terminal phase of ventricular filling. These sounds are inaudible. Third heart sound starts at (0.12 to 0.18) s after the onset of the second heart sound.it last approximately (0.04 to 0.08) s. The frequency is about 10 to 100 Hz. Valve opening sounds These sounds occur at the time of opening of the atria ventricular valves and semi lunar valves. The fourth heart sound starts approximately (0.12 to 0.18) s after the onset of the P wave. The sound last for (0.03 to 0.06)s. And the frequency is 10 to 50 Hz. Extra cardiac sounds These sounds occur in late systole or early diastole and are believed to be caused by thickened pericardium which limits ventricular distensibility. Murmurs are sounds related to non-laminar flow of blood in the heart and the great vessels. They are distinguished from the basic heart sounds such that they have noisy character having long duration and with high frequency components up to 1000 Hz. OBSERVATION TABLE: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 Period: Peak-peak value: SL.NO: HEART SOUNDS AMPLITUDE 1.First heart sound . 2.Second heart sound PROCEDURE 1. Switch on the main power supply. 2. Connect the transducer and microphone. 3. The heart beat is sensed by keeping the sensor on the chest position. 4. Press the acquire button in DSO, when a proper signal is formed. 5. Press the stop button to freeze the signal. 6. Finally measure the peak to peak voltage and time period by using the measure button. RESULT: Thus by using a Phonocardiograph, different heart sounds have been identified, displayed and recorded. Ex. No 12 Biotelemetry Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 AIM: To understand the transmission and reception of biological signal using a telemetry system EQUIPMENTS REQUIRED: ECG Amplifier Low Pass Filter – 2 Nos. FM Modulator FM Transmitter FM Receiver FM Demodulator Charger Battery – 2 Nos. Electrodes THEORY: Telemetry is a system of sending data, usually measurements, over a distance. Telemetric data may be physical, environmental or biological. Telemetry is typically used to gather data from distant, inaccessible locations, or when data collection would be difficult or dangerous for a variety of reasons. In telemetry, specialized instruments carry out measurements of physical quantities, and store or transmit the resulting signal, often after some initial signal processing or conversion. Biotelemetry is the electrical measuring, transmitting, and recording of qualities, properties, and actions of organisms and substances, usually by means of radio transmissions from a remote site. There are single channel and multi channel telemetry systems. For a single channel system, a miniature battery operated radio transmitter is connected to the electrodes of the subject. This transmitter broadcasts the biopotential over a limited range to a remotely located receiver, which detects the radio signals and recovers the signal for further processing. In this situation there is a negligible connection or stray capacitance between the electrode circuit and rest of the system. The receiving system can even be located in a room separate from the subject. BLOCK DIAGRAM: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 BLOCK DIAGRAM DESCRIPTION: ECG Amplifier ECG has amplitude of only about 1 mV, so to detect it an amplifier is required. The ECG amplifier used here has a Gain of 1000 and CMRR of more than 80dB. Low Pass Filter A low-pass filter allows low-frequency signals but attenuates (reduces the amplitude of) signals with frequencies higher than the cutoff frequency. When the ECG is amplified, the noise is amplified too, and often swamps the ECG signal. The noise is usually of a higher frequency than the ECG. So the noise can be reduced by low-pass filtering. FM Modulator Modulation is used to embed a message (voice, image, data, etc.) on to a carrier wave for transmission. A bandlimited range of frequencies that comprise the message (baseband) is Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 translated to a higher range of frequencies. The bandlimited message is preserved, i.e. every frequency in that message is scaled by a constant value. Here the incoming ECG signal is modulated at around 110MHz. The modulated ECG signal is given to the FM Transmitter. FM Transmitter FM Transmitter sends a signal (typically 4-20mA) from a process location to a central location for control and monitoring. Here FM transmitter transmits the modulated ECG signal. FM Receiver A receiver receives its input through an antenna. It receives the modulated signal from the transmitter. The receiver then passes on the information to the FM Demodulator where the ECG signal is demodulated to obtain the original ECG signal. FM Demodulator Demodulation, in radio is the technique of separating a transmitted audio frequency signal from its modulated radio carrier wave. Here the modulated ECG signal is demodulated at a frequency of around 100Hz and the original ECG signal is recovered. PROCEDURE: Connect the modules as per the block diagram. Switch ON the battery. Connect the ring electrodes to the subject. View the transmitted signal on the DSO. The various outputs from each of the modules can be viewed on the DSO by connecting the output banana pin to the desired module. RESULT: Thus we understand the transmission and reception of biological signal using a telemetry system. Ex. No 13 Pacemaker Module AIM: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 6 To understand the working of an external pacemaker and the various modules included in it. EQUIPMENTS REQUIRED: a) Oscillator b) Refra Generator –2 Nos. c) Pulse width control d) Amplitude Control e) Paced output f) Synch Generator g) QRS Detector h) QRS Filter i) ECG Amp Pacemaker j) Patient Simulator k) Electrodes l) Charger m) Battery THEORY: A pacemaker is an electronic device equipped with a battery, electronic circuits and memory that generates electronic signals (pacing pulses), which are carried along insulated wires (leads) to the heart to make the muscle beat at a normal rhythm. Bradycardia, a heartbeat that slows to an unhealthy rate, is the most frequent reason for a pacemaker. There are three basic types of temporary or permanent pacemakers, and each may work on demand, constantly or according to the heart's activity. Pacemakers are also of internal and external type. Internal pacemakers are mostly used for permanent heart damages are surgically implanted beneath the skin near the chest or abdomen with its output leads connected directly to the heart muscle. The external pacemakers are mostly used for temporary heart irregularities and are placed outside the body in the form of a wrist watch or in the pocket, from which one wire will go into the heart through the vein. Pacemakers may also be of single-, dual-, or triple chambered. Demand Pacemakers Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 When the heart's rate is too slow or it misses a beat, demand pacemakers, which monitor the heart's activity, will send an electrical pulse to set the heart back to a more normal rhythm. Fixed-rate Pacemakers Fixed-rate pacemakers discharge steadily, regardless of the heart's natural electrical activity. Rate-responsive Pacemakers Rate-responsive pacemakers have sensors that adjust automatically to changes in your physical activity. They are designed to raise or lower the heart rate to meet the body's needs. Here we consider demand pacers having circuitry that analyze the ECG (as detected by the pacer's electrodes). If a QRS is detected, the internal clock is reset thereby delaying the time until when the next pulse is due (i.e. the escape cycle length). The escape interval (the time between the last intrinsic beat and the paced beat) is equivalent to the rate at which the pacemaker is set to activate. Once the pacemaker begins pacing, it will not stop until the intrinsic heart rate climbs above the paced rate. BLOCK DIAGRAM: BLOCK DESCRIPTION: Oscillator An oscillator produces a repetitive electronic signal, often a sine wave or a square wave. The oscillator synchronises with the synch generator. If an R wave is detected the oscillator circuit is reset. In the absence of R wave, the oscillator circuit starts and delivers pulses at a paced rate till Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 the heart rate climbs above the paced rate. The output voltage is 5V and a 10msec pulse. the oscillator has rate control knob on the top panel. Refractory Generator The refractory generator is a non-retrigerrable monostable multivibrator which generates a 250ms delay following an output pulse or a sensed R-wave during which the amplifier in the sensing circuit will not respond to outside signals. The input is a pulse of 0-5V (Min 1msec) and output is pulse of 0-5V (250msec). Pulse Width Control The pulse width circuit is a basic RC network which determines the duration of the pulse delivered to the heart. The pulse width control has a range of 0.1- 2.1 msec and output of 5V. Amplitude Control The output of the pulse width control is given to the amplitude control which controls the amplitude of the delivered pulses. Paced output The paced output delivers the pulse to the heart, the duration and amplitude being controlled by the pulse width control and amplitude control. The output also goes to the ECG amplifier as a feedback signal. ECG Amp. Pacemaker The input to the ECG amplifier is from the Paced output which gives ECG signal as the feedback and it is amplified here. QRS Filter The Demand type pacemaker works on the presence or absence of R wave hence a QRS filter is used to selectively filter the QRS wave. The QRS Filter used here is a Bandpass Filter having limits from 22Hz to 45Hz with a gain of 10. QRS Detector With the presence of an R wave, the QRS detector will generate a pulse. The input voltage is 1V Pk –Pk and output voltage is 5V. It has a frequency range of 15-30Hz. Synch Generator Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 The Synch Generator synchronises with the QRS Detector and in presence of an R wave it resets the oscillator circuit. In the absence of R wave it allows the oscillator to deliver pulses at its preset rate. Patient Simulator The Patient Simulator simulates the abnormal heart condition- Bradycardia, Tachycardia and AV Block. Front Panel a) It has 3 buttons to simulate any of the three conditions mentioned above. b) A control knob to limit the rate of simulating heart conditions. c) Control the threshold of the simulating conditions. Top Panel The top panel of the Simulator has the sketch of the heart. Red and Yellow LEDs arranged in various regions of the heart. The flashing of the Red LEDs indicates the simulated abnormal heart condition. Once the Green LED flashes it signifies the pacemaker has taken over. Output pin connectivity to the DSO to view the paced output. Back Panel Feedback to the paced output through banana pins. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 PROCEDURE: 1. Connect the modules as per the block diagram. 2. Select one of the abnormal conditions in the Pacemaker Simulator and keep holding the button for simulating the condition. 3. The Paced output leads detect this abnormality and the output is given as a feedback to the ECG Amplifier. 4. As a normal QRS wave is not detected, the Oscillator is now triggered and the Pacemaker takes over and Green LEDs flash. 5. Once the abnormal condition is removed the Paced output leads detect this change, the oscillator is reset and the Pacemaker stops functioning. RESULT: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 Hence the working of a Pacemaker along with its various modules is studied. Ex.No 14 ECG Heart rate alarm system with HRV AIM: To understand the various modules of an ECG heart rate alarm system with heart rate variability. EQUIPMENTS REQUIRED: a) ECG Amplifier b) QRS Filter c) QRS Detector d) Refra Generator e) Synch Generator f) F to V Converter g) High Alarm h) Low Alarm i) DVM j) HRV k) Audio Buzzer l) Battery m) Charger n) Electrodes THEORY: Heart rate is the number of heartbeats per unit time - typically expressed as beats per minute (bpm) .The measurement of heart rate is used to assist in the diagnosis and tracking of medical conditions. The R wave to R wave interval (RR interval) is the inverse of the heart rate. Normally, heart rate varies depending on the person's age and activity. The term "arrhythmia” refers to abnormally fast or slow heart rates and to irregular heart rhythms. Arrhythmias are Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 usually diagnosed with an electrocardiogram (ECG). A heart rate that's faster than normal is called tachycardia. Tachycardia may reduce the heart's pumping ability and may require treatment. Sometimes tachycardia is due to an abnormality of the heart's electrical circuits, while other times it may be due to abnormally high adrenaline levels as seen, for example, after surgery. A heart rate that's slower than normal is called bradycardia. Bradycardia may be associated with certain congenital heart defects or may develop by itself before birth or after heart surgery. In some more serious cases if the heart rate is very slow, an artificial pacemaker may be needed. Heart rate variability (HRV) is a physiological phenomenon where the time interval between heart beat varies. HRV analysis is based on measuring variability in heart rate; specifically, variability in intervals between R waves - “RR intervals”. These RR intervals are then analyzed by spectral or some other form of mathematical analysis (e.g., chaos, wavelet theories). BLOCK DIAGRAM: BLOCK DIAGRAM DESCRIPTION: ECG Amplifier Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 ECG has amplitude of only about 1 mV, so to detect it an amplifier is needed. The ECG amplifier used here has a Gain of 1000 and CMRR of more than 80dB. QRS Filter Heart rate is the number of heartbeats per unit time - typically expressed as beats per minute (bpm). The R wave to R wave interval (RR interval) is the inverse of the heart rate. Hence a QRS filter is used to selectively filter the QRS wave. The QRS filter used here is a Bandpass Filter having limits from 22Hz to 45Hz with a gain of 10. QRS Detector With the presence of an R wave, the QRS detector will generate a pulse. The input voltage is 1V Pk –Pk and output voltage is 5V. It has a frequency range of 15-30Hz. Refractory Generator The refractory generator is a non-retrigerrable monostable mutivibrator which generates a 250msec delay following an output pulse or a sensed R-wave during which the amplifier in the sensing circuit will not respond to outside signals. The input is a pulse of 0-5V (min 1msec) and output is pulse of 0-5V (250msec). Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 Synch Generator The synch generator generates a synchronous pulse with the incoming wave. The input is a pulse of 0-5V (< 200msec) and output is pulse of 0-5V (100msec). HRV Module It is the analysis of variations in the instantaneous heart rate time series using the beat to beat RR intervals is known as heart rate variability analysis. These RR intervals are then analyzed by spectral or some other form of mathematical analysis (e.g., chaos, wavelet theories). Such mathematical analysis generates multiple parameters; typically 20-30. HRV analysis has been shown to provide an assessment of cardio vascular diseases. F-V Converter The output of synch generator is frequency hence it is converted into voltage for detection of an increase or decrease of the heart rate. The input pulse width is of 100msec and output voltage is 1V/100 pulse per minute. High Alarm & Low Alarm The modules high alarm and low alarm are calibrated at a certain rate. These are analog comparators which compare the incoming signal to the fixed rate. The high alarm and low alarm modules are calibrated using DVM at a fixed rate of 90 pulses/min and 60 pulses/min respectively. In case of the value being more than/less than the fixed rate the high alarm/low alarm triggers the audio buzzer. The input and output for High Alarm is 0-2.5V DC and 0-5V Pulse (100msec) respectively. The input and output for Low Alarm is 0-2.5V DC and 0-5V Pulse (100msec) respectively DVM The output of the High Alarm and Low Alarm is given to the DVM which gives the numerical display of the voltage. Audio Buzzer The audio buzzer generates an audio beep when the heart rate increases or decreases beyond the specified limits. The frequency of buzzer is 1 kHz and minimum input voltage is 5V. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 PROCEDURE: 1. Connect the modules as per the block diagram. 2. Connect the electrodes to the subject. 3. Switch ON the battery. 4. Observe the heart rate on the DVM. 5. If the heart rate deviates from the normal range the audio buzzer generates an audio beep. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 7 RESULT: Thus we understand the various modules of an ECG heart rate alarm system with heart rate variability. Ex. No 15 EMG Biofeedback with NCV AIM: To understand the EMG system and also calculate the Nerve Conduction Velocity I) a) EMG BIOFEEDBACK: EQUIPMENTS REQUIRED: a) EMG Amplifier b) High Pass Filter c) General Amplifier d) Audio Amplifier e) Level Indicator Linear f) Electrodes g) Battery h) Charger THEORY Electromyography (EMG) is a test of a muscle’s electrical activity. It is used to test how a muscle responds to signals from the nerves responsible for muscle movement, called motor nerves. An EMG may also include a test of how fast the motor nerve conducts impulses. This is Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 8 called a nerve conduction study (NCS) or nerve conduction velocity (NCV) test. Nerve Conduction Velocity (NCV) measures the speed of conduction of impulses through a nerve. The impulses being measured are artificially supplied by a stimulating electrode placed on the skin over the nerve. Electrical activity in the nerve being stimulated is measured by recording electrodes placed on the skin at various distances from the stimulating electrode. The distance between the stimulating and recording electrodes and the time taken for an electrical impulse to travel between the electrodes are used to calculate the nerve conduction velocity. Nerve conduction tests have two parts – testing motor and sensory nerve testing. Nerve conduction velocity studies are performed to evaluate and document a variety of sensory and motor neuropathological conditions in patients with a suspected diagnosis of nerve dysfunction. Nerve dysfunction can be manifested in decreased signal amplitude, slowed conduction velocity or increased latency. Proximal and distal nerve segments may be tested separately to help identify and localize the cause of the patient’s condition. Additional tests are sometimes used to evaluate the results of treatment. Although the stimulation of nerves is similar with all NCV studies, the characteristics of motor, sensory, and mixed NCS are different. • Motor NCV studies are performed by applying electrical stimulation at various points along the course of a motor nerve while recording the electrical response from appropriate muscle. Response parameters include amplitude, latency, configuration, and motor conduction velocity. • Sensory NCV studies are performed by applying electrical stimulation near a nerve and recording the response from a distant site along the nerve. Response parameters include amplitude, latency, configuration, and sensory conduction velocity. BLOCK DIAGRAM: Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 8 BLOCK DIAGRAM DESCRIPTION: EMG Amplifier The amplitude of the EMG signal depends upon the type and placement of electrodes used and the degree of muscular exertion. Generally EMG signals range from 0.1 to 0.5mV which is a weak signal hence it has to be amplified. This amplification is done by the EMG amplifier. Here the gain of the EMG amplifier is 1000 and the output is1 V pk to pk per mV of input. High Pass Filter A high-pass filter, allows high frequencies well but attenuates frequencies lower than the filter's cutoff frequency. The actual amount of attenuation for each frequency is a design parameter of the filter. It is sometimes called a low-cut filter. Here the HPF has a cut off frequency of 70Hz and a Minimum input voltage 1V Pk to Pk Audio Amplifier Audio amplifier amplifies low power audio signals to a required level. Audio amplifier used in this application has a frequency range of 0-10KHz. Level Indicator Linear The level indicator displays the level of contraction of the muscle. PROCEDURE: 1. Connect the modules as per the block diagram. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 8 2. Switch ‘ON’ the battery 3. Connect the subject to EMG amplifier through Ring electrodes. 4. Observe the output in the level indicator. I) b) EMG NERVE CONDUCTION VELOCITY EQUIPMENTS REQUIRED: a) Monostable multivibrator. b) Amplitude control c) High voltage generator d) EMG amplifier e) High pass filter f) Charger g) Battery BLOCK DIAGRAM: BLOCK DIAGRAM DESCRIPTION: Monostable multivibrator A monostable multivibrator is an electronic circuit used to implement a variety of simple twostate systems such as oscillators, timers and flip-flops. In the monostable multivibrator one of the states is stable, but if the other is not then the circuit will flip into the unstable state for a determined period, but will eventually return to the stable state. Such a circuit is useful for creating a timing period of fixed duration in response to some external event. This circuit is also known as a one shot multivibrator. Amplitude control Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 8 The amplitude control controls the amplitude of the triggering pulse from the monostable mutivibrator. High voltage generator For the calculation of nerve conduction velocity an external high volt stimulus is required which is provided by the high voltage generator that produces an output voltage of 100V. EMG Amplifier The amplitude of the EMG signal depends upon the type and placement of electrodes used and the degree of muscular exertion. Generally EMG signals range from 0.1 to 0.5mV which is a week signal hence it has to be amplified. This amplification is done by the EMG amplifier. Here the gain of the EMG amplifier is 1000 and the output is1 V peak to peak per mV of input. High Pass Filter A high-pass filter, or HPF, allows high frequencies well but attenuates frequencies lower than the filter's cutoff frequency. The actual amount of attenuation for each frequency is a design parameter of the filter. It is sometimes called a low-cut filter or bass-cut filter. Here the HPF has a cut off Frequency 70Hz and a Minimum input voltage 1V Pk to Pk. PROCEDURE: 1. 2. 3. 4. Connect the modules as per the block diagram. Connect the ring electrodes to the subject. Give the stimulus using the electrode of the high voltage generator to the subject’s elbow The settings for the DSO are Trigger: External Edge: Rising Edge Mode: Normal Mode 5. Press trigger switch and observe the waveform on the DSO. 6. Calculate nerve conduction velocity by measuring distance between stimulator electrodes and amplifier electrode and measuring time from oscilloscope reading. Nerve conduction velocity = distance /time. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 8 RESULT: Hence the working of EMG Biofeedback System and calculation of Nerve Conduction Velocity is understood and performed. Biomedical Instrumentation Lab Manual Biomedical Engineering Department, School of bioengineering, SRM University Page 8