NURU 432 Exam 2 Study Guide- Potter Chapters 34, 44, 46, 47, & 50
Potter Chapter 34 Sexuality
1. Know about the male reproductive tract and structures involved in male sterilization.
In male sterilization, or vasectomy, the vas deferens, which carries the sperm away from
the testicles, is cut and tied (p. 710).
2. What patient education should you provide a teen patient who is not partaking in safe
sex behaviors?
It’s imperative that sexually active adolescents be screened for STIs, even when they
have no symptoms. The annual physical examination of a sexually active adolescent
includes a thorough sexual history and a careful examination of the genitalia so that STIs
are not missed (p. 157).
Adolescent birth rates continue to decline due to improvements in contraceptive use,
the use of long-acting reversible contraception, and safe sex practices (p. 157).
When necessary, help to identify risky sexual behaviors, such as unprotected sex or
multiple sexual partners. Ensure that these young adults have adequate sexual health
education regarding birth control and the prevention of sexually transmitted infections
(STIs) (p. 162).
3. Know about the human papillomavirus vaccine (HPV) including its intended audience,
purpose, side effects, etc.
Human papillomavirus (HPV) is the most common sexually transmitted infection in the
United States. An estimated 50% to 75% of sexually active men and women acquire HPV
at some point in their lives, with 14 million new infections occurring annually. HPV is
spread through direct contact with warts, semen, and other body fluids from others who
have the disease. The HPV vaccination provides safe, effective, and lasting protection
against the HPV infections that most commonly cause cancer (p. 711).
4. Know about human immunodeficiency virus (HIV) including how it is transmitted, stages,
and possible treatment.
HIV infection is a bloodborne pathogen and is present in most body fluids. Transmission
occurs when there is an exchange of body fluid. Primary routes of transmission include
contaminated intravenous (IV) needles, anal intercourse, vaginal intercourse, oral-genital
sex, and transfusion of blood and blood products (p. 711).
HIV progresses in three stages: HIV progresses in three stages. Then he or she enters the
clinical latency phase; at this time there are no symptoms of infection. The last stage,
acquired immunodeficiency syndrome (AIDS), happens when a person begins to show
symptoms of the disease (p. 711).
Potter Chapter 44 Pain Management
5. What is the best way to assess a patient’s pain?
Ask them! Pain is subjective. Numeric scale, faces scale.
One of the major challenges of pain is that as a nurse you cannot see or feel a patient’s
pain. It is purely subjective. No two people experience pain in the same way, and no two
painful events create identical responses or feelings in a person. The International
Association for the Study of Pain (IASP) defines it as “an unpleasant, subjective sensory
and emotional experience associated with actual or potential tissue damage, or
described in terms of such damage” (p. 1060).
Clenching the teeth, facial grimacing, holding or guarding the painful part, and bent
posture are common indications of acute pain (p. 1063).
6. What are common side effects of opioid analgesics? What education would you provide
your patient taking this medication?
A common side effect of opioids is opioid-induced constipation (OIC) (p. 754).
The most common side effects of opioids include nausea, vomiting, constipation, and
memory and thought changes. To reduce side effects, patients should take the lowest
dose of an opioid needed to manage pain (p. 1083).
7. What are the different types of pain? Know examples and symptoms of each.
Acute/Transient pain is protective, usually has an identifiable cause, is of short duration,
and has limited tissue damage and emotional response (p. 1063).
Chronic pain is not protective and thus serves no purpose, but it has a dramatic effect on
a person’s quality of life (p. 1064).
Not all patients with cancer experience pain. Cancer pain can be relieved often with
simple interventions in 90% of patients (Burchum and Rosenthal, 2019). Some patients
with cancer experience acute and/or chronic pain.
Idiopathic pain
nociceptive pain (somatic and visceral) somatic musculoskeletal pain visceral- visceral
organs.
neuropathic pain (nerve pain) burning electrical.
8. In a group of patients experiencing pain, which one would you see first?
When setting priorities in pain management, consider the type of pain the patient is
experiencing and the effect that it has on function and quality of life. The primary goal
often is to decrease pain to help the patient improve function. Any episode of acute pain
is a priority because of its potential effects on physical and psychological function.
Unstable patients (p. 1077).
9. What are examples of nonpharmacological pain management interventions and when
would they be appropriate to use?
In the case of moderate to severe acute pain, nonpharmacological therapies should not
be used in place of pharmacological therapies. A number of nonpharmacological
interventions are available for lessening pain.
Evidence-based therapies include acupuncture and massage, osteopathic and
chiropractic manipulation, cognitive-behavioral intervention, meditative movement and
mind-body interventions, and dietary and self-management approaches to pain
management. Cognitive-behavioral interventions change patients’ perceptions of pain,
alter pain behavior, and provide patients with a greater sense of control. Distraction,
prayer, mindfulness, relaxation, guided imagery, music, and biofeedback are examples of
therapies frequently initiated by nurses (p. 1079).
10. If your patient comes out of surgery with a patient-controlled analgesia (PCA), what
patient education should you provide regarding the dosing?
A patient needs to understand the PCA and be physically able to locate and press the
button to deliver a dose. Family members and visitors must be instructed not to “push
the button” for the patient (a dangerous action known as “PCA by proxy”), as this
bypasses the safety feature of PCA, which requires an awake patient to activate the
device. In particular situations, when patients are unable to activate the PCA device, a
carefully selected family member or nurse may be authorized to activate the device
based on specific criteria (p. 1086).
• Teach how to use the PCA before procedures so that patient understands how to use it
after awakening from anesthesia or sedation. Include demonstration of use of pump.
• Instruct patient in the purpose of PCA, emphasizing that patient controls medication
delivery.
• Explain that the pump reduces risk of overdose.
• Reinforce instruction as needed with teach-back.
{ Extra: Nurses need to understand the medications available for pain relief, indications
for use and pharmacological effects, and risks for addiction. Reassure patients that
treatment of pain is necessary to aid recovery and that nonpharmacological strategies
can be used to augment the effectiveness of analgesics, healing, and pain relief (p.
1082). A person’s response to an analgesic is highly individualized (p. 1084). }
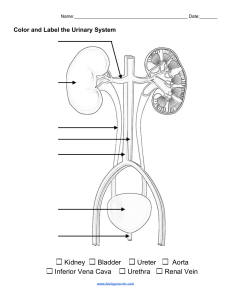
Potter Chapter 46 Urinary Elimination
11. What are signs and symptoms and causes of dysuria?
Pain with urination = dysuria. Burning upon urination (p. 1152).
12. What are the different types of urinary incontinence? Know the characteristics and
possible nursing interventions for each. (P. 1152)
Reflex Urinary Incontinence: Involuntary loss of urine occurring at somewhat
predictable intervals when patient reaches specific bladder volume related to spinal cord
damage between C1 and S2
Urge or Urgency Urinary Incontinence: Involuntary passage of urine often associated
with strong sense of urgency related to an overactive bladder caused by neurological
problems, bladder inflammation, or bladder outlet obstruction
- In many cases bladder overactivity is idiopathic; cause is not known
- Caused by involuntary contractions of the bladder associated with an urge to
void that causes leakage of urine
Stress Urinary Incontinence: Involuntary leakage of small volumes of urine associated
with increased intraabdominal pressure related to either urethral hypermobility or an
incompetent urinary sphincter (e.g., weak pelvic floor muscles, trauma after childbirth, radical
prostatectomy)
Result of weakness or injury to the urinary sphincter or pelvic floor muscles
Underlying result: urethra cannot stay closed as pressure increases in the bladder as a
result of increased abdominal pressure (e.g., a sneeze or cough)
Urinary Incontinence Associated with Chronic Retention of Urine (Overflow Urinary
Incontinence): Involuntary loss of urine caused by an overdistended bladder often related to
bladder outlet obstruction or poor bladder emptying because of weak or absent bladder
contractions
Functional Incontinence: Loss of continence because of causes outside the urinary tract
Usually related to functional deficits such as altered mobility and manual dexterity,
cognitive impairment, poor motivation, or environmental barriers
Direct result of caregivers not responding in a timely manner to requests for help with
toileting
Transient Incontinence: Incontinence caused by medical conditions that in many cases
are treatable and reversible
13. What is urinary retention? What are possible nursing interventions if your patient is
experiencing this?
Involuntary accumulation of urine in bladder as result of loss of muscle tone. Signs and
symptoms include inability to void, restlessness, and bladder distention. It appears 6-8
hours after surgery. Intermittent catheterization is used to measure PVR when
ultrasound or a bladder scanner is unavailable or as a way to manage chronic urinary
retention (p. 1166).
Running warm water, holding warm wash cloth, changing positions, giving them privacy.
14. Know about the signs and symptoms of benign prostatic hypertrophy (BPH) including
patient education.
Hypertrophy of the prostate gland is frequently seen in older men. This hypertrophy
enlarges the gland and places pressure on the neck of the bladder. As a result, urinary
retention, frequency, incontinence, and UTIs occur. In addition, prostatic hypertrophy
results in difficulty initiating voiding and maintaining a urinary stream and does not
always indicate a malignancy (p.180).
15. Know about common causes and risks for developing a urinary tract infection (UTI)?
Escherichia coli, a bacterium commonly found in the colon, is the most common
causative pathogen in correlation with UTI’s. The risk for a UTI increases in the presence
of an indwelling catheter, any instrumentation of the urinary tract, urinary retention,
urinary and fecal incontinence, and poor perineal hygiene practices (p. 1152).
16. What is CAUTI? What are risk factors for developing CAUTI?
Catheter-associated urinary tract infection (CAUTI). The major risk factors for CAUTI’s are
the presence of an indwelling urinary catheter and the length of its use (p. 1152).
17. What are the correct steps to inserting an indwelling urinary catheter in a female
patient? What are some troubleshooting tips if there is no urine return? (Essentials
Collection- Inserting an Indwelling Catheter in a Female Patient)
18. What are the correct steps to inserting an indwelling urinary catheter in a male patient?
(Essential Collection- Inserting an Indwelling Catheter in a Male Patient)
19. What are the correct steps when performing an indwelling urinary catheter? (Essential
Collection- Irrigating a Urinary Catheter)
Potter Chapter 47 Bowel Elimination
20. What are the different divisions of the large intestine? Know their location in order and
role in elimination.
The large intestine is divided into the cecum, ascending colon, transverse colon,
descending colon, sigmoid colon, and rectum. The colon has three functions: absorption,
secretion, and elimination. The rectum is the final part of the large intestine. Normally
the rectum is empty of fecal matter until just before defecation (p.1199).
21. What is the proper positioning of a patient on a bed pan?
22. What orders should the nurse anticipate if the patient is having black stool? What are
nursing considerations and patient education?
Melena: Abnormal black, sticky stool containing digested blood that is indicative of
gastrointestinal bleeding.
23. What procedure is commonly performed on children who experience frequent soiling
episodes? What patient education should be provided?
24. What are risk factors for developing increased peristalsis? What are common signs and
symptoms?
Emotional stress. If peristalsis is abnormally fast, there is less time for water to be
absorbed, and the stool will be watery (p. 1199).
25. Know the basic characteristics of each of the anal sphincters and role in elimination.
The body expels feces and flatus from the rectum through the anus. Contraction and
relaxation of the internal and external sphincters, which are innervated by sympathetic
and parasympathetic nerves, aid in the control of defecation (p. 1199).
Potter Chapter 50 Perioperative Nursing Care
26. Be able to identify and describe the three phases of perioperative nursing.
Perioperative nursing includes a registered nurse’s planned patient-centered approach in
providing care to patients preoperatively, intraoperatively, and postoperatively (p. 1321).
27. What are the various classifications of surgical procedures? What are examples of each?
Major: Involves extensive reconstruction or alteration in body parts; poses great risks to
well-being [ie. Coronary artery bypass, colon resection, removal of larynx, resection of
lung lobe]
Minor: Involves minimal alteration in body parts; designed to correct deformities;
involves minimal risks to well-being. [ie. Cataract extraction, facial plastic surgery, tooth
extraction ]
Elective: Performed on basis of patient’s choice; is not essential and is not always
necessary for health [ie. Bunionectomy; facial plastic surgery; hernia repair; breast
reconstruction ]
Urgent: Necessary for patient’s health; often prevents development of additional
problems (e.g., tissue destruction or impaired organ function); not necessarily
emergency [ie. Excision of cancerous tumor; removal of gallbladder for stones; vascular
repair for obstructed artery (e.g., coronary artery bypass) ]
Emergency: Must be done immediately to save life or preserve function of body part [ie.
Repair of perforated appendix or traumatic amputation; control of internal
hemorrhaging]
Diagnostic: Surgical exploration performed to confirm diagnosis; often involves removal
of tissue for further diagnostic testing [ie. Exploratory laparotomy (incision into
peritoneal cavity to inspect abdominal organs); breast mass biopsy]
Ablative: Excision or removal of diseased body part [ie. Amputation; removal of
appendix or an organ such as gallbladder (cholecystectomy)]
Palliative: Relieves or reduces intensity of disease symptoms; does not produce cure [ie.
Colostomy; debridement of necrotic tissue; resection of nerve roots]
Reconstructive/restorative: Restores function or appearance to traumatized or
malfunctioning tissues [ie. Internal fixation of fractures; scar revision]
Procurement for transplant: Removal of organs and/or tissues from a person
pronounced brain dead or from living donors for transplantation into another person [ie.
Kidney, heart, or liver transplant]
Constructive: Restores function lost or reduced as result of congenital anomalies [ie.
Repair of cleft palate; closure of atrial septal defect in heart]
Cosmetic: Performed to improve personal appearance [ie. Blepharoplasty for eyelid
deformities; rhinoplasty to reshape nose]
28. What are the American Society of Anesthesiologists (ASA) Physical Status classifications?
Be able to define each and provide examples.
ASA I: A normal healthy patient
ASA II: A patient with mild systemic disease
ASA III: A patient with severe systemic disease
ASA IV: A patient with severe systemic disease that is a constant threat to life
ASA V: A moribund patient who is not expected to survive without the operation
ASA VI: A patient declared brain dead whose organs are being removed for donor
purpose
29. In a group of patients who underwent a surgical procedure, which one would you see
first?
?????
30. What are common side effects of anesthesia on the urinary system? What would you
include in your nursing assessment?
?????
31. If you are taking care of a postoperative patient, what patient education should you
provide regarding prevention of respiratory complications and why?
After anesthesia, a patient’s tongue causes the majority of airway obstructions. Ongoing
assessment of airway patency is crucial even during phase III recovery. Patients remain in
a side-lying position until airways are clear. Continue to assess respiratory status and
breath sounds (p. 1347).
32. Know the Universal Protocol guidelines of patients undergoing surgery during patient
preparation.
????