Echocardiographic Assessment of Pulmonary Arterial Pressure in Children
advertisement

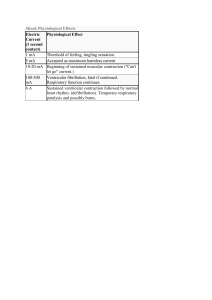
PEDIATRIC CARDIOLOGY EchocardiographicAssessment of PulmonaryArterial Pressure in Children With Complete Right Bundle Branch Block GREGORY L. JOHNSON, MD RICHARD A. MEYER, MD, FACC JOAN KORFHAGEN, RDMS DAVID C. SCHWARTZ, MD, FACC SAMUEL KAPLAN, MD, F&C Lexington, Kentucky Cincinnati, Ohio From the Department of Pediatrics, College of Medicine, University of Cincinnati, Children’s Hospital,Cincinnati,OhioandDepartmentof Ps diaiics, College of Medicine,Universityof Kentuckv MedicalCenter. Lexintion, Kentucky.This w&wassq+rtedI~partbytheAmericar;Hear? Association, SouthwesternOhio Chapter, Cincinnati,Ohioandthe KentuckyHeartAssociation, Louisvllie,Kentucky.hb~script recehredOctober 11,1977; rev&d rnanuscrlptreceivedDecember 6,1977, acoepted December 7,1977. Addressfor reprints:Qe9ory L. Johnson,MD, Deparbnentof Pediatrics,Universityof Kentucky Medical Center, Lexington,Kentucky40506. 1264 June 1978 The time Interval between tricuspid valve closure and pulmonaryvalve openlng,termed the lsovokrmlccontractlontime of the rightventricle,was evaluated echographically In 38 normal children and within 24 hours of cardiac catheterlzatlon in 83 children with congenital heart disease and normal conductlon as assessed with the electrocardilbgram.In the 53 patients with congenital heart disease, lsovolumiccontractiontime was stronglyinfluencedby rfghtventricularaflerload,as defined by pulmonary arterial end-dlastollc pressure (r = 0.87). It was possibleto utilize Isovolumlc contraction time to separate patlents wtth normal or elevated values for pufmonaryarterial end-diastolicpressure.Similar correlations were demonstrated between lsovolumic contraction time and mean pulmonaryarterialpressureand calculatedpulmonaryvascularreststance. Evaluattonof 15 chiklrenwith completerightbundlebranchblockrevealed values for lsovolumlccontractiontime that dld not signtflcantlydiffer from those of patlents with similar pulmonary arterial end-dlastollc pressure but no conductlon abnormalltles. These findings indicate that serial echographic evaluatton of the interval from tricuspid valve closure to pulmonaryvalve openingcan glve an accurate reproducibleassessment of rightventrkxrlarafterloadIn many childrenwtth congenftalheart d&ease and complete right bundle branch block. Obstructive pulmonary vascular disease is a well known potentially lethal complication of many forms of congenital heart disease. In patients at risk of this complication, repeated invasive assessment of pulmonary arterial pressures and pulmonary vascular resistance has frequently been required to determine optimal timing of surgical intervention. Recent that echocardiographic studies by Hirschfeld et al. 112demonstrated measurement of right ventricular systolic time intervals, performed serially and without difficulty, can result in a reasonable noninvasive estimation of pulmonary vascular resistance. In their studies the ratio of the right ventricular preejection period to ejection time, recorded echographically, correlated well with invasively determined values for pulmonary arterial end-diastolic and mean pressure and calculated pulmonary vascular resistance. Because electromechanical delay prolongs the right ventricular preejection period in patients with complete right bundle branch block, the ratio cannot be used to evaluate serial changes in pulmonary vascular dynamics in these patients. Many children have postoperative complete right bundle branch block after correction of their congenital heart lesion. It would be particularly valuable to have a method ofserially evaluating the pulmonary vascular bed noninvasively in these patients. Right ventricular isovolumic contraction time may be defined echographically as the interval from coaptation of the tricuspid valve leaflets to opening of the pulmonary valve. If this interval were found to be relatively independent of the prolongation of the right ventricular pre- The American Journal of CARDIOLOGY Vohme 41 ECHDCARDIDGBAM IN COMPLETE RIGHT BUNDLE BRANCH BLOCK-JOHNSON ETAL. FIGURE 1. Echocardiograms of pulmonary and tricuspid valves of three patients demonstrating pulmonary valve opening and closure and coaptation of tricuspid leaflets. Numbers 235,230 and 220 refer to right ventricular ejection time. ASD = atrial septal defect; MS = mitral stenosis: PHT = pulmonary hypertension; POST-W = postoperative; QPO = interval from the 0 wave to pulmonary valve opening; QT, = interval from the Q wave to tricuspid valve closure: RBBB= right bundle branch blm RICT (rim isovolumic contraction time) = (QPo - QT,); VSD = ventricular septal defect. ejection period induced by electromechanical delay, it could be utilized to evaluate right ventricular afterload in patients with complete right bundle branch block. Additionally, the interval could be utilized in patients without right ventricular conduction abnormalities in whom difficulty in recording pulmonary valve closure precludes use of the preejection period to ejection time ratio to assess right ventricular afterload. The purposes of this study were (1) to evaluate right ventricular isovolumic contraction time echographically in normal children and to establish a range of normal values; (2) to evaluate right ventricular isovolumic contraction time in a large series of children with a variety of congenital heart lesions, including several with coexisting complete right bundle branch block, who were undergoing elective cardiac catheterization; (3) to compare right ventricular isovolumic contraction time with values for pulmonary arterial end-diastolic and mean pressure and calculated pulmonary vascular resistance determined invasively; and (4) to determine the efficacy of using right ventricular isovolumic contraction time in evaluating right ventricular aferload in the presence of complete right bundle branch block. Material and Methods Echocardiograms were performed in 38 normal children aged 1 month to 17 years (median 8 years) without signs of heart disease and within 24 hours of cardiac catheterization in 68 children aged 1 month to 22 years (median 6 years) with congenital heart disease. Fifteen of these 66 children had electrocardiographic evidence of complete right bundle branch block as indicated by a QRS interval greater than 120 msec; the block was temporally related to intracardiac surgery in 14 of the 15. Case material: Echocardiography: Echocardiograms were obtained utilizing a Hoffrel 1OlBor 201 ultrasonoscope. The echographic tracing and electrocardiogram were recorded on a Cambridge multichannel physiologic recorder or a Honeywell model 1856 multichannel recorder. Tracings were recorded at a paper speed of 75 or 125 mm/set with time lines of lo,20 or 40 msec. At a paper speed of 75 mm/set, there was a po- tential error of approximately 5 msec in measurement of time intervals,s which was judged insignificant. An Aerotech 5.0 megahertz nonfocused or a 3.5 or 2.25 megahertz short internal focus transducer was used. In older children, in whom the 2.25 megahertz transducer was used for left ventricular studies, it was frequently helpful to change to a higher frequency transducer to obtain optimal echoes from the right-sided structures. The tricuspid valve was visualized echographically by rotating the transducer medially and inferiorly along the sternum from the aortic region. This position enabled the ultrasonic beam to pass inferiorly through the valve. The ramp was then set to peak at approximately the point of coaptation of the anterior and posterior tricuspid valve 1eailet.s to visualize the point of valve leaflet closure. Similarly, the transducer was robted laterally and slightly superiorly from the aortic area to visualize the pulmonary artery. Occasionally, particularly in older children, it was necessary to move the transducer one interspace superiorly and then rotate it laterally. If the ramp peak was then set at approximately the center of the pulmonary arterial echo, both opening and closure of the pulmonary valve could be visualized. Echographic measurements (Fig. 1): The interval from the Q wave to tricuspid valve closure was measured from the onset of ventricular depolarization, as defined by the Q or R wave of the simultaneous electrocardiogram, to coaptation of the tricuspid valve leaflets. When only the anterior tricuspid leaflet could be accurately visualized, leaflet coaptation was determined to have occurred at the point of transition of the fine anterior leaflet echo to a thicker closed valve echo in early systole. Immediately after valve closure there was a consistent abrupt posterior movement of the valve echo before the gradual anterior movement in systole. The interval Q to pulmonary valve opening was measured from the onset of ventricular depolarization to the point of rapid departure of fine cusp echoes from the thick closed valve echoes recorded during diastole. This method was also used when only the posterior pulmonary cusp could be recorded adequately. Right ventricular ejection time was determined as the time from the onset of ventricular ejection to the termination of ejection noted by junction of the fine leaflet echo with the thick closed valve echo. The difference of Q to pulmonary valve opening less Q to tricuspid valve closure was arbitrarily termed right ventricular isovolumic contraction time. Measurements were June 1878 The Amlcan Journal of CARDIOLGGY Vofume 41 1285 EC!lOCARDlOGRAM IN COMPLETE RIGHT BUNDLE BRANCH BLOCK-JOHNSON ET AL. r= -.I9 n = 36 ym 14.5-.04x 0 l m l 16 I l l ee l l l 0 50 I 60 1 70 I SO I 60 I 100 HEART RATE I I IO I 120 Results Normal children: Right ventricular isovolumic contraction time in the 38 normal children ranged from 1 to 20 msec (mean f standard derivation 10.2 f 5.2 msec). There was no correlation (r = -0.05) between values observed and patient age, and only a weak correlation (r = -0.19) between values observed for isovolumic contraction time and heart rate (Fig. 2). Data for normal subjects as well as for study patients were rate-corrected by two separate methods to determine whether rate correction would alter correlation of the isovolumic contraction time with signs of obstructive pulmonary vascular disease. The first of these involved dividing the observed isovolumic contraction time by the square root of the R-R interval. The mean value for this interval in the normal group was 12.9 f 6.5 msec. It has been reported2 that the ratio of right ventricular preejection period to right ventricular ejection time is relatively uninfluenced by heart rate in children. Because the right ventricular isovolumic contraction time is the mechanical component of the right ventricular June 1878 I 140 (bcatr/min.) performed at similar R-R intervals and were made during end-expiration in older children. in the infants with a rapid respiratory rate in whom respiratory monitoring was not available, the shortest R-R intervals were arbitrarily selected to minimize the influence of respiratory variation on the intervals. Five separate complexes were measured and averaged to obtain the final intervals. Hemodynamic measurements: All patients were premedicated with pentobarbital or droperidol before cardiac catheterization and children between 2 and 5 years of age received ketamine anesthesia. Right ventricular and pulmonary arterial pressure curves were measured to the nearest 1 mm Hg. Pulmonary vascular resistance was calculated in units of mm Hg/liter per min per m2 utilizing assumed oxygen consumption in approximately half the patients and measured oxygen consumption using a continuous flow-through system in the remainder. 1288 I 130 ‘TAT FIGURE 2. Correlation between right ventricular isovolumic contraction time (RICT) and heart rate in 38 normal chikken. Sdkl line is the line of regression. n = number of children: r = correlation coefficient. preejection period, the ratio of the right ventricular isovolumic contraction time to the ejection time was also analyzed as an alternative method of eliminating the possible effect of heart rate from our data. The mean value for this ratio in the normal subjects was 0.037 f 0.015. Congenital heart disease without right bundle branch block: In the 53 patients without electrocardiographic evidence of complete right bundle branch block, right ventricular isovolumic contraction time provided excellent separation of those patients with normal pulmonary arterial end-diastolic pressure, all of whom demonstrated values for isovolumic contraction time within the range defined by the normal population, from those with catheterization findings consistent with pulmonary vascular obstructive disease (Fig. 3). The latter group all demonstrated values for isovolumic contraction time greater than 2 standard deviations above the normal range, with the lowest value of 25 msec observed in a patient with pulmonary arterial end-diastolic pressure greater than 20 mm Hg. Although there was considerable scatter in the data, particularly at high values for end-diastolic pressure, a significant positive linear correlation (r = 0.87) was demonstrable between right ventricular isovolumic contraction time and pulmonary arterial end-diastolic pressure. Significant correlations were also demonstrated between isovolumic contraction time and mean pulmonary arterial pressure (r = 0.88) and calculated pulmonary vascular resistance (r = 0.68). Correcting the isovolumic contraction time for heart rate by dividing the observed interval by the square root of the R-R interval also provided excellent separation of patients with normal and elevated values for pulmonary arterial end-diastolic pressure, but the separation was not noticeably improved nor was the correlation coefficient significantly changed (r = 0.85) from The Amerkan Journal of CARDlOLOQY Volume 41 ECHOCARDIOGRAM IN COMPLETE RIGHT BUNDLE BRANCH BLOCK-JOHNSON -CRSEE 80 l Present 0 AS(12) 70 0 PDAIB) 0 COA(5) . ECD A MI (21 t 70 - 60 - 50 - (15) oAbsent (53) (51 60 ^ r” ET AL. 50,P ! 40- 2 nQ : 40k Y JO- 2 30 - 20 - r=.87 IO #&gLA b . 01 a/” “S 53 y= 1.06(x)+2.82 r= .SI A l 1 I 6 16 “’ I 24 I I 32 40 I 40 I5 “=1.31(x1-1.67 1 56 RICT (msec) 01’ FIGURE 3. Correlation between ri&t ventricular isovolumic contraction time (RICT)and pulmonary arterial end-diastolic pressure (PA& in 53 chilcken with congenital heart disease but without complete rtght bundle branch block. Solid Me is the line of regression. AS = aortlc stenosis; COA = coarctation of the aorta; ECD = endocardial cushion defect; MI = mitral insufficiency; n = number of patients; PDA = patent ductus arteriosus; VSD = ventricular septal defect. results observed utilizing the uncorrected data. Similar findings were demonstrated in the correlations between the rate-corrected interval and mean pulmonary arterial pressure (r = 0.86) and calculated pulmonary vascular resistance (r = 0.65). Comparison of pulmonary arterial end-diastolic pressure with the ratio of right ventricular isovolumic contraction time to right ventricular ejection time yielded results similar to those utilizing isovolumic contraction time alone (r = 0.87). Similar correlations were observed between this ratio and mean pulmonary arterial pressure (r = 0.85) and calculated pulmonary vascular resistance (r = 0.71). Patients with congenital heart disease and right bundle branch block: In all patients with complete right bundle branch block and normal pulmonary arterial end-diastolic pressure, values for right ventricular isovolumic contraction time were within the range defined by the normal population. These values observed were not notably different from those in patients with similar pulmonary arterial end-diastolic pressures and normal intraventricular conduction (Fig. 4). As in the patients with normal conduction, elevation of the pulmonary arterial end-diastolic pressure prolonged right ventricular isovolumic contraction time in the patients with complete right bundle branch block, and the interval clearly separated patients with normal pressures from those with pressures indicative of hypertensive ’ 8 I 16 1 24 RICT I I I I 32 40 40 56 lmsecl FIGURE 4. Ccrrelation between rtght ventricular isovolumic contraction time (RICT)and pulmonary arterial enddlastolic pressure (PA& in 15 children with congenital heart disease and complete rtght bundle branch block (CRBBB) compared with that observed in 53 children without complete right bundle branch block. SolId and dashed lines are regression lines in children with and without complete right bundle branch block, respectively. pulmonary vascular disease. A linear correlation relating isovolumic contraction time and pulmonary arterial end-diastolic pressure in patients with complete right bundle branch block was demonstrable (r = 0.81), and there was no statistically significant difference between this regression equation and that relating isovolumic contrastion time and pulmonary arterial end-diastolic pressure in patients without complete right bundle branch block. Similar correlations were demonstrable relating right ventricular isovolumic contraction time in patients with complete right bundle branch block to mean pulmonary arterial pressure (r = 0.84) and calculated pulmonary vascular resistance (r = 0.86). The correlation between right ventricular isovolumic contraction time and pulmonary arterial end-diastolic pressure in patients with complete right bundle branch block was not notably improved by correction of the observed interval for heart rate (F = 0.82) or by evaluation of the isovolumic contraction time to ejection time ratio (r = 0.86). Discussion Isovolumic contraction time has classically been defined as that phase of the preejection period from closure of the atrioventricular valve to onset of ventricular ejection.s*4 Although opening of the pulmonary valve June 1979 The Amwkan Joumal of CARDIOLOGY Volume 4f 1287 ECHOCARDIOGRAM IN COMF’LETE RIGHT BUNDLE BRANCH BLOCK-JOHNSON visualized echographically has generally been thought to coincide with the onset of right ventricular ejection, the exact timing of closure of the tricuspid valve and its relation to right ventricular events has been controversial. However, it was recently demonstrated with phonocardiographic-echocardiographic techniques5-7 that coaptation of the tricuspid valve leaflets visualized echographically corresponds with the second group of high frequency vibrations in the first heart sound, that is, with tricuspid valve closure. By convention, isovolumic contraction time of the left ventricle has been measured from the phonocardiographic mitral valve closure to the onset of left ventricular ejection (determined from the rapid upstroke of the carotid pulse tracing, and then corrected for the time delay of pulse transmission).It appears reasonableto propose that the echographic correlate of the corresponding period in the right ventricle could be defined by the coaptation of the tricuspid valve leaflets and the point of initial opening of the pulmonary valve. Echographic right ventricular isovolumic contraction time as an assessment of pulmonary arterial end-diastolic pressure: In the present study, the echographic right ventricular isovolumic contraction time thus defined was evaluated in children with and without conduction abnormalities affecting the right ventricle to determine whether the interval could provide the same assessmentof the status of the pulmonary vascular bed afforded by evaluation of the right ventricular preejection period to right ventricular ejection time ratio and, if so, whether this interval could be used to assesspulmonary vascular disease in the presence of right ventricular conduction abnormalities. Our results confirm that right ventricular isovolumic contraction time, evaluated echographically, provides excellent separation of patients with normal pulmonary arterial pressures from those with pressures indicative of hypertensive pulmonary vascular disease. Although a highly significant linear correlation was demonstrated between isovolumic contraction time and pulmonary arterial diastolic and mean pressures, as well as with calculated pulmonary vascular resistance, there was considerable scatter in the data, and one should not attempt to extrapolate precise hemodynamic data from echographic evaluation of the isovolumic contraction time. We believe that the principal utility of our data will be in the serial evaluation of patients at risk of developing pulmonary vascular changes as a result of their congenital heart lesion, particularlyin patients in whom technical difficulty in echographically defining pulmonary valve closure precludes use of the right preejection period to right ventricular ejection time ratio. Effect of right bundle branch block: In patients with complete right bundle branch block, values for right ventricular isovolumic contraction time were not significantly different from values in patients with similar indexes of pulmonary vascular disease but without right ventricular conduction abnormalities. Isovolumic contraction time appears to provide a noninvasive method of serially evaluating the pulmonary 1268 June 1978 The American Journal ol CARDIOLOGY ET AL. vascular bed in this group of patients. In our patients the presence of incomplete right bundle branch block was usually an index of right ventricular hypertrophy, and these patients were not separately evaluated. Among children, complete right bundle branch block usually is not a sign of generalized conduction system disease but is presumably secondary to an isolated, often surgically induced, proximal lesion. Leech and Brooks (personal communication) found that in these patients, right ventricular isovolumic contraction time is normal, but that in the presence of normal afterload, the interval is often prolonged in patients with generalized conduction system disease and distal or arborization block. It would follow that, without a high degree of suspicion regarding the site of the block, the method cannot be applied to all instances of complete right bundle branch block. If these findings are confirmed, the usefulness of the echographic evaluation of isovolumic contraction time in assessing the status of the pulmonary vascular bed would be limited somewhat by these considerations, particularly in adult patients. Effect of heart rate: An unexpected finding in our study was that right ventricular isovolumic contraction time was minimally affected by heart rate, and correction of the interval for heart rate did not appreciably change its usefulness in evaluating the status of the pulmonary vascular bed. Because the isovolumic contraction time was found to normally be exceedingly short (mean value in the normal group 10 msec), it may be that the changes associated with changing heart rate are not sufficient to produce the type of changes seen with increased right ventricular afterload. Similarly, division of the isovolumic contraction time by right ventricularejection time, an intervalthat is significantly correlated with heart rate,2 did not improve our data. Effect of right ventricular contractile state, preload and afterload: The principal determinants of the duration of left ventricular isovolumic contraction time have been described as (1) contractile state of the myocardium; (2) preload, or left ventricular end-diastolic volume or pressure; and (3) afterload, or aortic impedance.3vsContractile state of the right ventricular myocardium is difficult to assess;however, none of our patients demonstrated clinical findings of right heart failure at the time of study. Until further data regarding the effect of right ventricular myocardial contractility on right ventricular isovolumic contraction time are available, we believe that any attempt to utilize echocardiographic systolic time intervals to assess right ventricular afterload (pulmonary vascular resistance) in patients in whom right heart failure is suspected should be viewed with extreme caution. Similarly, the effects of preload on the isovolumic contraction time were not evaluated in our study; however, right ventricular end-diastolic pressure was less than 10 mm Hg in all patients in whom this measurementwas available. Despite the potential effect of these factors, our study demonstrates that right ventricular isovolumic contraction time, determined echographically, is significantly affected by right ventricularafterload in patients with a wide variety of congenital heart defects. Volume 41 ECHOCARDIOGRAM Implications: Much additional work is necessary to define more completely factors that can influence right ventricular isovolumic contraction time. Our study may provide an accurate reproducible method of noninvasively defining this interval. In our patient group, marked prolongation of the interval was consistent with the presence of pulmonary hypertension, and this correlation was not affected by the presence of complete right bundle branch block. The serial evaluation of the interval would appear to afford a reasonably accurate IN COMPLETE RIGHT BUNDLE BRANCH BLOCK-JOHNSON ET AL. assessment of the pulmonary vascular bed in selected pediatric patients, particularly those with conduction abnormalities that preclude use of the right ventricular preejection period to right ventricular ejection time ratio. As further experience is gained, serial echographic assessment of right ventricular isovolumic contraction time should enhance the clinical management and reduce the need for repeated cardiac catheterization in many children prone to develop hypertensive pulmonary vascular disease. References 1. Hlrschfeld S, Meyer R, Schwartz DC, et al: Measurement of right and left systolic time intervals by echocardiography. Circulation 51:304-309,1975 2. Hlrschfeld S, Meyer R, Schwartz DC, et al: The echocerdiographic assessment of pulmonary artery pressure and pulmonary vascular resistance. Circulation 52642-650, 1975 3. Welaaler AM, Lewis RP, Lelghtcn RF: The systolic time intervals as a measure of left ventricular performance in man. In, Progress in Cardiology, Vol 1 (Vu PN, Goodwin JF, ed). Philadelphia, Lea & Feblger, 1972, p 155 4. Spcdlck SH, Kuman S: lsovolumic contraction period of the left ventricle. Am Heart J 76:498-503, 1968 5. 6urggrafGW, Cralge E: The YgF first heart sound in complete heart phono-echocardlographic correlations. Circulation 50: 17-24, 6. Walder W, Cralge E: The first heart soundand ejection sounds: echo-phonocardlographic correlation with valvular events. Am J Cardiol35:346-356, 1975 7. Mllner S, Meyer RA, VenablesAW, et al: Mitral and tricuspid valve closure in congenital heart disease. Circulation 53513-518. 1976 8. Wallace AG, MitchellJH, Skinner NS, et al: Duration of the phases of left ventricular systole. Circ Res 12:6 1 l-6 19, 1963 June 1978 The American Journalcf CARDIOLOGY Volume 41 1269