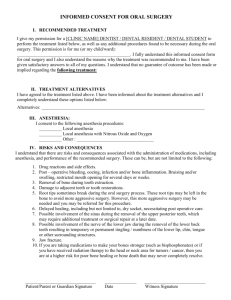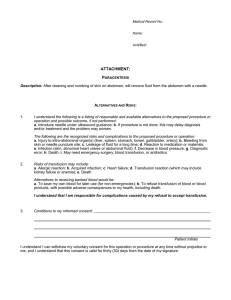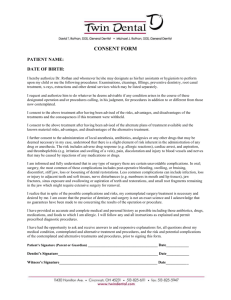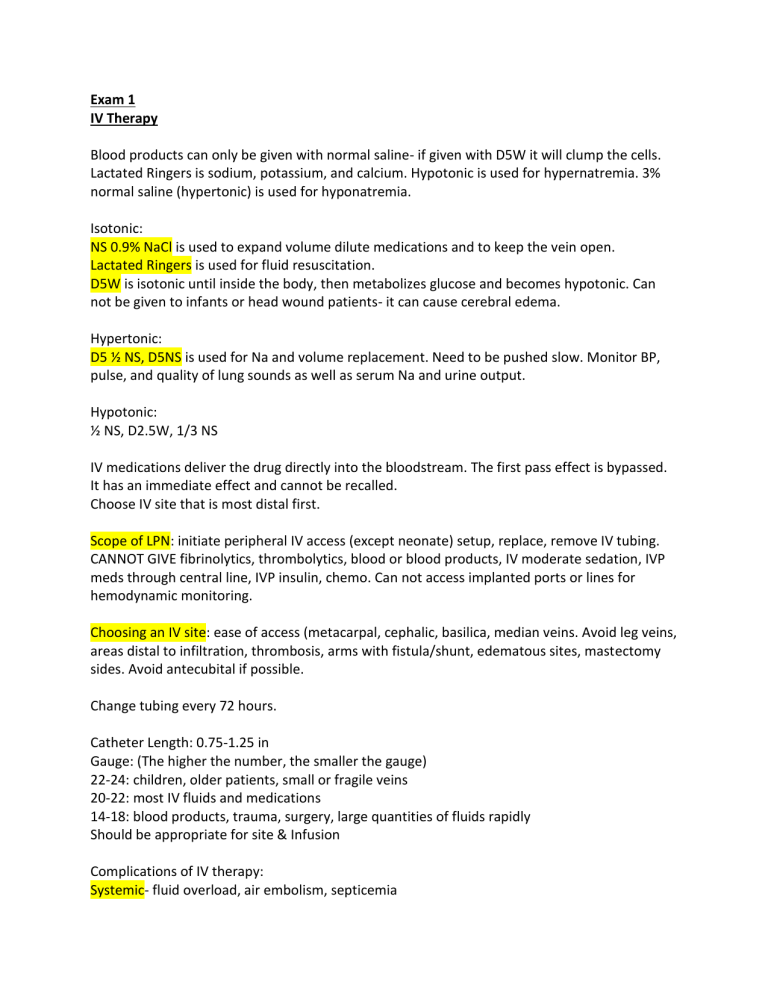
Exam 1 IV Therapy Blood products can only be given with normal saline- if given with D5W it will clump the cells. Lactated Ringers is sodium, potassium, and calcium. Hypotonic is used for hypernatremia. 3% normal saline (hypertonic) is used for hyponatremia. Isotonic: NS 0.9% NaCl is used to expand volume dilute medications and to keep the vein open. Lactated Ringers is used for fluid resuscitation. D5W is isotonic until inside the body, then metabolizes glucose and becomes hypotonic. Can not be given to infants or head wound patients- it can cause cerebral edema. Hypertonic: D5 ½ NS, D5NS is used for Na and volume replacement. Need to be pushed slow. Monitor BP, pulse, and quality of lung sounds as well as serum Na and urine output. Hypotonic: ½ NS, D2.5W, 1/3 NS IV medications deliver the drug directly into the bloodstream. The first pass effect is bypassed. It has an immediate effect and cannot be recalled. Choose IV site that is most distal first. Scope of LPN: initiate peripheral IV access (except neonate) setup, replace, remove IV tubing. CANNOT GIVE fibrinolytics, thrombolytics, blood or blood products, IV moderate sedation, IVP meds through central line, IVP insulin, chemo. Can not access implanted ports or lines for hemodynamic monitoring. Choosing an IV site: ease of access (metacarpal, cephalic, basilica, median veins. Avoid leg veins, areas distal to infiltration, thrombosis, arms with fistula/shunt, edematous sites, mastectomy sides. Avoid antecubital if possible. Change tubing every 72 hours. Catheter Length: 0.75-1.25 in Gauge: (The higher the number, the smaller the gauge) 22-24: children, older patients, small or fragile veins 20-22: most IV fluids and medications 14-18: blood products, trauma, surgery, large quantities of fluids rapidly Should be appropriate for site & Infusion Complications of IV therapy: Systemic- fluid overload, air embolism, septicemia Local- infiltration (most common), hematoma, clotting/obstruction, phlebitis/thrombophlebitis Infiltration signs: redness around the site, swelling/puffy/hard skin around the site, pain, IV not working, cool skin temp around site. Phlebitis (inflammation of the vein) signs: pain, redness, swelling, heat around the site. Hemoglobin of 7 Hematocrit of 20 is when they start to give blood products Volume expanders Crystalloids: inexpensive, maintenance fluids, initial resuscitations, restore 3rd space loss, short intravascular half-life. (Normal saline, lactated ringers) Colloids: increase plasma volume, less peripheral edema, smaller volumes needed for resuscitation, longer half-life (blood products) Type and crossmatch are done every 3 days. The body can build antibodies with every transfusion. Platelets and plasma are straw colored BEFORE transfusion: type and crossmatch, educate patient, consent, verify (product and duration), gather supplies. Get baseline vitals, pre medicate if ordered (Tylenol/benedryl). Verify product (2 RNs): medical order, consent, patient ID number, patient name, blood group/type, expiration, inspect for clots. Do not give blood if fever is present. Blood transfusion is a 2 RN procedure. Only RN can administer. Must be given within 30 minutes of obtaining. Start slow at 5mL/ min, then increase after 15 minutes if no reaction. Nurse must stay in room for first 15 minutes. Check vitals after 15 minutes then Q1H Blood must be transfused within 4 hours. Monitor for 1-hour signs and symptoms of delayed reaction. If a reaction is suspected, do not throw away tubing. Can use tubing for two units of blood. Transfusion reactions Febrile nonhemolytic: women who have had multiple births (RH-) and patients with multiple transfusions. S/S chills followed by fever. Develops at end of transfusion or within two hours post. Acute hemolytic reaction: occurs when patient gets wrong blood. Most dangerous and potentially life threatening. S/S fever, chills, SOB. Emergency Allergic reaction: patients who have antibodies that react with proteins in the transfused blood components. S/S urticaria (hives) and generalized itching within minutes. Usually mild and can give antihistamines. Nursing management of blood transfusion reaction: stop transfusion immediately, assess patients’ vital signs, O2, heart/lung sounds, and possible mental changes, notify provider, notify blood bank, send blood and tubing back to blood bank. Perioperative care Diuretics: during anesthesia may cause respiratory depression resulting from an associated electrolyte imbalance. Corticosteroids: can cause cardiovascular collapse if discontinued suddenly Phenothiazines: may increase the hypotensive action of anesthetics. Interactions between a patient with diabetes mellitus undergoes surgery. Informed consent must be in writing. Consent MUST be obtained by physician. Patients signature must be witnessed by professional staff member. The nurse clarifies the information provided, verifies the presence of the patient’s or designee’s signature, and may be asked to sign as a witness. If at any point the patient requests additional information, or if the nurse feels that the patient may not understand, the nurse notifies the physician. The nurse ascertains that the consent form has been signed before administering psychoactive premedication, because consent is not valid if it is obtained while the patient is under the influence of medications that can affect judgment and decision-making capacity. Circulating nurse: works with surgeons, anesthesia, and other HCP to plan the best course of action for the patient. They manage the OR and protect the patients’ health and safety, activities of the surgical team, checking OR conditions, and continually assessing patient for signs of injury and implementing appropriate interventions. Also, must verify consent and if not obtained, surgery may not commence. They insure cleanliness, proper temp, humidity, lighting, safe equipment, and availability of supplies. They are responsible for ensuring that the second verification of the surgical procedure and site takes place and is documented. Unrestricted zone: street clothes Semi restricted zone: scrubs Restricted zone: sterile Phase 1: PACU, coming from OR, vitals every 5-10 minutes. Waiting on wake from anesthesia Phase 2: out of PACU, waking up enough to eat and drink, take out IV, help get dressed, bathroom Phase 3: discharge Gerontologic considerations: They have a decline in physiologic reserve that weakens the normal response to stressors, acute illness, anesthesia, and surgery. Risks include delirium, hypothermia, positioning injury, DVY, electrolyte imbalance, and circulatory compromise. Slow circulation and hypotension predispose the patient to thrombus formation and emboli. Lower doses of anesthesia are required in older adults due to decreased tissue elasticity and reduced lean tissue mass. Wound healing: First: surgical incision, straight lines Second: like pressure ulcer, take out necrotic tissue, can’t pull it together Third: lots of swelling, can’t close for few days, deep wounds, can be sutured later Post op care: Assess airway, respirations; patient at risk for ineffective airway clearance every 15 minutes. Assess VS every 4 hours or as needed, other indicators of cardiovascular status; patients at risk for decreased cardiac output related to shock or hemorrhage. Assess pain every 4 hours or per protocol. Dehiscence: would pops open. Call HCP asap Evisceration: pops open and bowel comes out. Put in low fowlers, sterile moist dressing placed on top, call HCP asap Mobility Osteoporosis: more common in women. Risk factors include: using corticosteroids for more than 3 months, alcohol intake, family history, inadequate calcium and vitamin d, low BMI, malabsorption disorders, men over 60, postmenopausal women, sedentary lifestyle. Can be diagnosed by Xray, bone mineral density scan, and DEXA studies. Prevention and treatment: calcium intake, vitamin d, exercise, and eliminate/decrease alcohol, caffeine, and tobacco. Can occur in children with spina bifida, adolescent athletes, and pregnancy. Calcitonin spray helps preserve bone density (spray in every other nostril daily) Fractures: Hip fracture: one leg shorter than the other and foot rotated out. Risks: increased age, women, history of osteoporosis, decreased estrogen, increased falls Nursing priorities: hydration, respiratory support, circulation checks, pain control, prevention of immobility complications. History of chronic conditions and complications. Buck’s traction is skin traction to the lower leg. The pull is exerted in one plane when partial or temporary immobilization is desired. It is used as a temporary measure to overcome muscle spasms and promote immobilization of hip fractures in adult patients waiting for more definitive treatment such as surgery. The nurse monitors for complications of skin traction, which can include skin breakdown, nerve damage, and circulatory impairment. Hip surgery nursing considerations: first 24-48 hours pain relief, prevention of complications, and neurovascular checks are most important. The nurse should encourage deep breathing, dorsiflexion and planter flexion exercises every 1-2 hours. Compression stockings and anticoagulants are used to prevent VTE. The most comfortable position is on the uninjured side with a pillow between the legs. Cast care: The main concern following the application of a cast is assessment and prevention of neurovascular dysfunction or compromise. Assessments should be performed at least every hour for the first 24 hours and every 1-4 hours thereafter. Assessment includes peripheral circulation, peripheral pulses, capillary refill, edema, color, temperature of the skin, motion (weakness or paralysis) sensation (paresthesia) of the extremity- assessing the fingers/toes of the effected extremity and comparing it with those of the opposite extremity. 5 P’s: pain, pallor, pulselessness, paresthesia, and paralysis. Elevate the extremity above the level of the heart during the first 24-48 hours to help augment the flow of fluid, control edema and enhance arterial perfusion. Handle drying cast with palms to prevent indentation Compartment syndrome: when swelling spreads internally due to the compression of cast/restriction device. Tell-tale signs are uncontrolled pain, even with analgesics. Bivalve the cast immediately, then fasciotomy. Systemic complications include infection due to necrotic tissue, renal failure, hyperkalemia, metabolic acidosis. Venous thrombosis: mainly effects patients who refuse to be mobile. Prevention- dorsiflexion and planter flexion of affected limb, compression hose, ROM of unaffected limb Fat embolism: more common in long bone fractures. Symptoms usually occur 12-72 hours post injury. Triad signs: petechia at site, hypoxemia (extreme SOB with O2 sat 60 or less), and neurological compromise. Osteomyelitis: infection of the bone. Manifestations- sudden onset with blood borne infection, fever/chills, irritability or lethargy in young children, localized pain swelling, and warmth. In children, most commonly affects the long bones of the legs and upper arms. Adults- bones that make up the vertebrae. Diabetics may develop osteomyelitis in their feet if they have foot ulcers. Can be diagnosed by CT, MRI, Xray, radioisotope bone scan, ESR, WBC count, wound and blood cultures. Treated with IV abx, wound irrigation with abx, surgery (bone graft, sequestrectomy, microvascular bone transfer, muscle flap) Neurovascular checks are important. Nursing management: relieving pain (immobilize with splint, elevate, handle gently, analgesics); improving physical mobility (no weight bearing activity) controlling the infectious process (monitor response to the abx therapy and observe IV site for phlebitis, infection and infiltration).