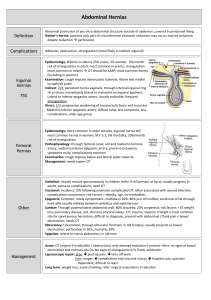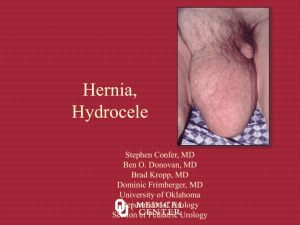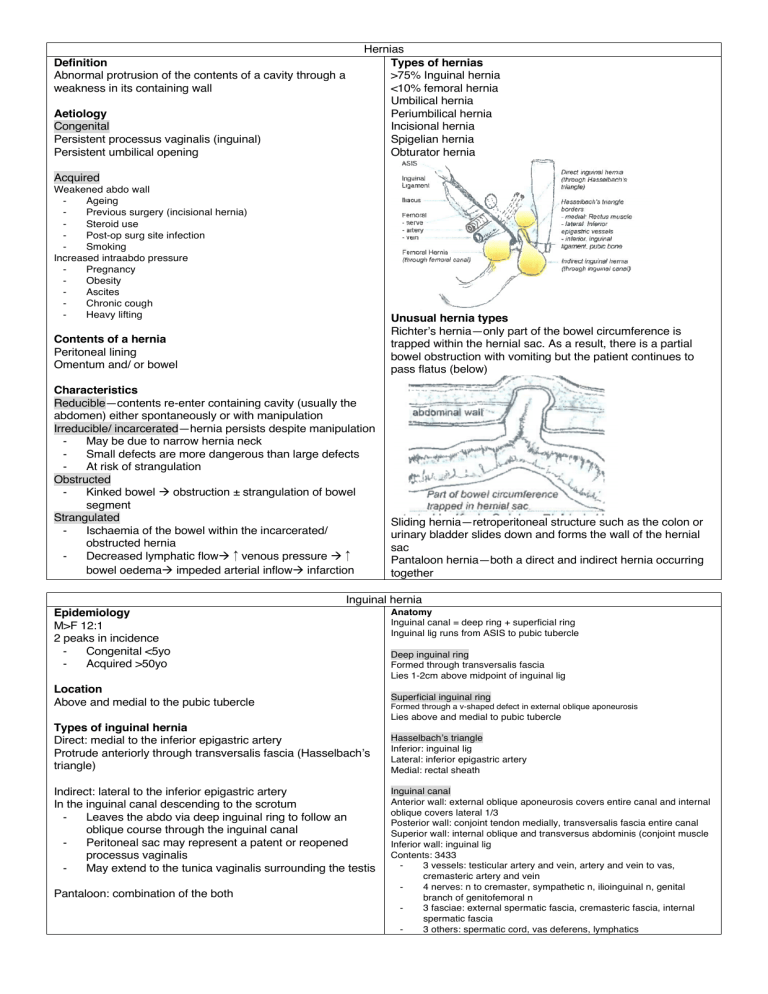
Definition Abnormal protrusion of the contents of a cavity through a weakness in its containing wall Aetiology Congenital Persistent processus vaginalis (inguinal) Persistent umbilical opening Hernias Types of hernias >75% Inguinal hernia <10% femoral hernia Umbilical hernia Periumbilical hernia Incisional hernia Spigelian hernia Obturator hernia Acquired Weakened abdo wall Ageing Previous surgery (incisional hernia) Steroid use Post-op surg site infection Smoking Increased intraabdo pressure Pregnancy Obesity Ascites Chronic cough Heavy lifting Contents of a hernia Peritoneal lining Omentum and/ or bowel Unusual hernia types Richter’s hernia—only part of the bowel circumference is trapped within the hernial sac. As a result, there is a partial bowel obstruction with vomiting but the patient continues to pass flatus (below) Characteristics Reducible—contents re-enter containing cavity (usually the abdomen) either spontaneously or with manipulation Irreducible/ incarcerated—hernia persists despite manipulation May be due to narrow hernia neck Small defects are more dangerous than large defects At risk of strangulation Obstructed Kinked bowel à obstruction ± strangulation of bowel segment Strangulated Ischaemia of the bowel within the incarcerated/ obstructed hernia Decreased lymphatic flowà↑venous pressure à↑ bowel oedemaà impeded arterial inflowà infarction Sliding hernia—retroperitoneal structure such as the colon or urinary bladder slides down and forms the wall of the hernial sac Pantaloon hernia—both a direct and indirect hernia occurring together Inguinal hernia Epidemiology M>F 12:1 2 peaks in incidence Congenital <5yo Acquired >50yo Location Above and medial to the pubic tubercle Anatomy Inguinal canal = deep ring + superficial ring Inguinal lig runs from ASIS to pubic tubercle Deep inguinal ring Formed through transversalis fascia Lies 1-2cm above midpoint of inguinal lig Superficial inguinal ring Formed through a v-shaped defect in external oblique aponeurosis Lies above and medial to pubic tubercle Types of inguinal hernia Direct: medial to the inferior epigastric artery Protrude anteriorly through transversalis fascia (Hasselbach’s triangle) Indirect: lateral to the inferior epigastric artery In the inguinal canal descending to the scrotum Leaves the abdo via deep inguinal ring to follow an oblique course through the inguinal canal Peritoneal sac may represent a patent or reopened processus vaginalis May extend to the tunica vaginalis surrounding the testis Pantaloon: combination of the both Hasselbach’s triangle Inferior: inguinal lig Lateral: inferior epigastric artery Medial: rectal sheath Inguinal canal Anterior wall: external oblique aponeurosis covers entire canal and internal oblique covers lateral 1/3 Posterior wall: conjoint tendon medially, transversalis fascia entire canal Superior wall: internal oblique and transversus abdominis (conjoint muscle Inferior wall: inguinal lig Contents: 3433 3 vessels: testicular artery and vein, artery and vein to vas, cremasteric artery and vein 4 nerves: n to cremaster, sympathetic n, ilioinguinal n, genital branch of genitofemoral n 3 fasciae: external spermatic fascia, cremasteric fascia, internal spermatic fascia 3 others: spermatic cord, vas deferens, lymphatics Clinical features Lump, usually not symptomatic until exacerbated by any condition that ↑intraabdo pressure Chronic cough Obesity Constipation When exacerbated, cause dragging/ aching sensation Operative management Congenital inguinal repair should be done asap due to increased risk of incarceration, strangulation and testicular ischaemia Symptomatic adult hernias should be repaired Indirect inguinal hernia Usually asymptomatic in the morning then symptoms develop throughout the day as the hernia moves down the canal If deep ring defect, it behaves like a direct hernia Direct inguinal hernia Abdo wall lump appears immediately on standing Diagnosis Clinical exam Remember to stand the patient Presence of cough impulse Reduction into its opening defect Once reduced, location of deep ring can be determined USS/ CT if equivocal dx/ obstruction suspected Differentiation of direct vs indirect often done intraoperatively Conservative management for elderly with significant morbidities Open inguinal hernia repair Day case, but admission for complications 5cm incision in groin area Intestines are placed into their correct position by excising the hernial sac near the spermatic cord and repairing the weak area The weak area is then strengthened with a synthetic mesh (tension free lichtenstein repair) Post op care Patient should not drive or operate machinery for 24h Routinely, patient will be prescribed painkillers but not abx Avoid heavy lifting for 6-8 weeks Epidemiology F>M 30% of all hernia repairs in women and <15 of all hernia repairs in men More common >70yo Location Below and lateral to pubic tubercle Lap herniorrhaphy Indications: bilateral hernias, recurrent hernias Both techniques listed below require the use of mesh and are considered tension free repairs Totally extraperitoneal repair Transabdominal preperitoneal patch repair Complications of repair Scrotal haematoma Wound infection Urinary retention Chronic pain/ paraesthesia in the scrotum (labium majora in females) from damage to the ilio-inguinal nerve Testicular atrophy caused by inadvertent damage to the testicular artery Recurrence <1% rate Due to poor operative technique Conditions like chronic cough, constipation or bladder outlet obstruction also contribute to recurrence Risks of procedure General risks of surgery and GA: N/V, sore throat, cardiac, resp, DVT/ PE risks depending on comorbidities Risks specific to procedure Damage to blood vesselsà bleeding, haematoma (require repeat operation) Testicular atrophy (<1%) when testicular artery is damaged Infection of the wound or mesh (abx, removal of mesh if infected) Nerve damage à chronic pain in groin that may resolve after the operation but may persist Recurrence (1%) Femoral hernia Anatomy Femoral △ Superior: inguinal lig Lateral: medial border of sartorius muscle Medial: medial border of adductor longus Floor: iliacus, psoas, pectineus, adductor longus Roof: superficial fascia, great saphenous vein Contents: (VAN medial to lateral) fem vein, fem artery, fem n Clinical features Small lump immediately below the inguinal lig and just lateral to its medial attachment to the pubic tubercle Cough impulse rarely detected due to narrow neck of hernial sac Due to narrow neck, more likely to strangulate but localising signs usually absent 30% present with bowel obstruction DDx Fen canal lipoma Saphena varix (SFJ varices) Fem lymph node Fem artery aneurysm Fen artery pseudoaneurysm (post angiography) Sarcoma (leio/ rhabdomyosarcoma) Open Lichtenstein tension free repair Utilises a patch of non-absorbable mesh to strengthen the posterior wall of the inguinal canal Local anaesthesia + sedation or general anaesthesia Femoral canal Anterior: inguinal lig Medial: lacunar lig Lateral: fem vein Post: pectineal lig Contents: lymph node (Cloquet’s node) and fat Management All fem hernias should be surgically repaired Other hernias Umbilical hernia Spigelian hernia True umbilical hernia Defect between lateral border of the rectus abdominis and Always congenital linea semilunaris Through umbilical cicatrix Hernial sac comes to lie interstitially between the layers of May close spontaneously by 3y of age internal and external oblique and transversus abdominis Following this, there is little likelihood of improvement and Difficult to diagnose surgical repair should be considered Usually requires imaging—CT Should be surgically repaired after 3yo Direct surgical repair indicated Periumbilical Always acquired Not through the umbilicus itself Common in obese patients and multiparous women Occasionally strangulate Assess case by case basis risk vs benefit for surgery Incisional hernia Up to 10% of laparotomy incisions eventually herniate Predisposing factors Post op wound infection Abdo obesity Poor muscle quality (smoking, anaemia) Multiple operations through the same incision Poor choice of incision Inadequate closure technique Clinical features Lump and defect: vary from small (more dangerous) to complete defects Incisional hernias may be asymptomatic at presentation but tend to progressively enlarge May cause strangulation (rare) Management Repair indicated for pain or strangulation Mesh used for larger defects (>4cm) Obturator hernia Defect through obturator canal (lateral pelvis into thigh) Causes medial thigh pain in cutaneous distribution of the obturator nerve Very challenging to diagnose – CT required High risk of obstruction