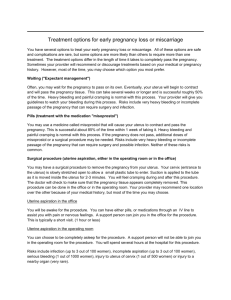
Obstetrics Overview: Hospital Structure, Care, and Procedures
advertisement

1. The structure of obstetrical hospital. Specificity of each unit and service. The structure of an obstetrical hospital can vary depending on the size and type of hospital. However, in general, it includes the following units and services: Labor and delivery unit: This unit is responsible for the management of labor and delivery. It typically includes delivery rooms, operating rooms for caesarean sections, and recovery rooms. Medical personnel such as obstetricians, nurses, and anesthesiologists work in this unit. Antenatal care unit: This unit provides care for pregnant women before labor and delivery. It includes services such as prenatal visits, ultrasounds, and prenatal testing. Obstetricians, midwives, and nurses work in this unit. Neonatal unit: This unit provides care for newborns who require specialized medical attention, such as premature babies or those with medical conditions. It typically includes neonatal intensive care units (NICUs) with specialized medical equipment and staffed by neonatologists, nurses, and respiratory therapists. Postpartum unit: This unit provides care for women and newborns after delivery. It includes services such as breastfeeding support, postpartum checkups, and newborn care education. Obstetricians, midwives, and nurses work in this unit. Obstetric emergency unit: This unit provides emergency care for pregnant women experiencing complications such as preterm labor, bleeding, or preeclampsia. It typically includes operating rooms and staffed by obstetricians, anesthesiologists, and nurses. In addition to these units, an obstetrical hospital may also have services such as a fertility clinic, genetic counseling, and social work services. The hospital may also offer educational classes for expectant parents, such as childbirth education and parenting classes. 2. Antenatal care, pre-conceptional counseling and care. Antenatal care, also known as prenatal care, is the medical care provided to pregnant women during their pregnancy to monitor the health of both the 1|Page mother and the developing fetus. It involves a series of regular checkups and tests that are designed to identify and address any potential health problems that may arise during pregnancy. Antenatal care aims to promote a healthy pregnancy, reduce the risk of complications, and ensure the safe delivery of the baby. Pre-conceptional counseling and care refer to the medical care and advice given to women before they become pregnant to ensure that they are healthy and prepared for pregnancy. This includes counseling on nutrition, exercise, and lifestyle changes that may be necessary to optimize health and fertility. Preconceptional care also involves identifying and addressing any underlying medical conditions that may pose a risk during pregnancy, such as diabetes, high blood pressure, or thyroid disease. Antenatal and pre-conceptional care typically involve a team of healthcare professionals, including obstetricians, midwives, and nurses. The care provided may include: Regular checkups and tests to monitor the health of the mother and fetus, including ultrasound scans, blood tests, and urine tests. Counseling on nutrition, exercise, and lifestyle changes. Screening for medical conditions that may pose a risk during pregnancy, such as diabetes, high blood pressure, and thyroid disease. Education on childbirth preparation, breastfeeding, and newborn care. Support for mental health issues that may arise during pregnancy, such as anxiety or depression. Referral to specialists, such as a genetic counselor, if needed. Antenatal and pre-conceptional care are critical components of ensuring a healthy pregnancy and delivery. Pregnant women are encouraged to seek early and regular medical care to optimize the health outcomes for both themselves and their babie 3. Safe motherhood. Epidemiology of obstetrics: maternal morbidity and mortality, perinatal morbidity and mortality. 2|Page Safe motherhood is a global public health initiative that aims to reduce maternal and perinatal mortality and morbidity. Maternal morbidity refers to the health complications that occur during pregnancy, childbirth, or in the postpartum period, while maternal mortality refers to the death of a woman during pregnancy or within 42 days of delivery. Perinatal morbidity and mortality refer to the health complications and death of the fetus or newborn during the pregnancy, childbirth, or within the first week of life. The epidemiology of obstetrics focuses on the incidence, distribution, and determinants of maternal and perinatal morbidity and mortality. According to the World Health Organization (WHO), approximately 830 women die from preventable causes related to pregnancy and childbirth every day, with the majority of these deaths occurring in low-income countries. The leading causes of maternal mortality include severe bleeding, infections, high blood pressure during pregnancy, and unsafe abortions. Perinatal morbidity and mortality also remain significant public health issues. Factors that contribute to perinatal morbidity and mortality include maternal age, low socioeconomic status, poor maternal nutrition, inadequate prenatal care, and complications during pregnancy and childbirth. Prevention and management of maternal and perinatal morbidity and mortality require a comprehensive approach that includes access to quality antenatal care, skilled attendance at birth, emergency obstetric care, and postpartum care. Implementation of evidence-based interventions such as proper nutrition, prevention and treatment of infections, and timely management of complications can reduce maternal and perinatal morbidity and mortality. 4. Audit in obstetrics. Medico- legal aspects of obstetries practice. Audit in obstetrics is the process of reviewing and evaluating the quality of care provided to pregnant women and their newborns, with the aim of identifying areas for improvement and implementing changes to improve outcomes. This 3|Page includes the assessment of the clinical practice, decision-making, and care provided during pregnancy, labor, delivery, and postpartum periods. The process of audit involves the following steps: Defining standards of care: This involves developing guidelines and protocols for the care of pregnant women and their newborns, based on best available evidence. Measuring practice against standards: This involves collecting data on the care provided and comparing it with the established standards of care. Identifying areas of improvement: This involves analyzing the data collected to identify areas of care that need improvement. Implementing changes: This involves making changes to the care provided, based on the findings of the audit, and evaluating the impact of these changes. Medico-legal aspects of obstetric practice refer to the legal implications of obstetric care. These include issues related to malpractice, negligence, informed consent, and confidentiality. Obstetricians must ensure that they provide care in accordance with established standards of care and adhere to legal and ethical principles. They should also maintain accurate and complete medical records and ensure that patient confidentiality is protected. In addition, obstetricians must ensure that patients are fully informed about the risks and benefits of any interventions or treatments and obtain their informed consent before proceeding. Failure to obtain informed consent or providing substandard care can result in legal action being taken against the obstetrician. As such, it is important for obstetricians to have a thorough understanding of the legal and ethical issues related to obstetric practice. It is important to discuss with a healthcare provider the most appropriate method of contraception for individual needs and circumstances. 4|Page 5. Medical termination of pregnancy in different trimesters, procedures. Medical termination of pregnancy (MTP) is the use of medications to end a pregnancy. It can be done in different trimesters using different procedures: First trimester (up to 12 weeks): MTP can be done using medications such as mifepristone and misoprostol, which are taken orally or vaginally. These medications work by blocking the hormone progesterone, which is needed for the pregnancy to continue. This causes the lining of the uterus to break down and the cervix to soften and open, leading to the expulsion of the embryo/fetus. Second trimester (13-24 weeks): MTP in the second trimester is more complex and usually requires hospitalization. It can be done using medications such as mifepristone and misoprostol, but at higher doses and for a longer duration. Another option is to have a surgical abortion, which involves dilation and curettage (D&C) or dilation and evacuation (D&E) procedures. Third trimester (after 24 weeks): MTP in the third trimester is not allowed except in cases of severe fetal abnormalities or if the mother's life is at risk. In these cases, labor induction or caesarean section may be done to end the pregnancy. It's important to note that MTP should only be performed by a trained healthcare provider in a safe and legal setting. Counseling before and after the procedure is also crucial to ensure the woman's physical and emotional wellbeing. 6. Anatomy and physiology of female reproductive system. The female reproductive system consists of internal and external structures. The internal structures include the ovaries, fallopian tubes, uterus, cervix, and vagina. The external structures include the mons pubis, labia majora and minora, clitoris, and Bartholin's glands. The ovaries are the female gonads responsible for producing eggs and hormones, such as estrogen and progesterone. Each ovary is located on either 5|Page side of the uterus and is connected to the uterus by the fallopian tubes. The fallopian tubes, also known as oviducts, are a pair of tubes that transport eggs from the ovaries to the uterus. Fertilization typically occurs in the fallopian tubes. The uterus is a muscular organ that houses and nourishes a developing fetus during pregnancy. The lower part of the uterus is called the cervix, which is the opening to the vagina. The vagina is a muscular canal that connects the cervix to the external genitalia. It serves as the birth canal during childbirth and also functions in sexual intercourse and menstruation. The external structures of the female reproductive system include the mons pubis, which is the fatty tissue that covers the pubic bone; the labia majora and minora, which protect the clitoris and vaginal opening; the clitoris, which is a highly sensitive organ involved in sexual arousal; and the Bartholin's glands, which secrete lubricating fluid during sexual activity. Overall, the female reproductive system is a complex and intricately regulated system responsible for the production of female gametes, hormones, and the nourishment and protection of a developing fetus during pregnancy. 7. Endocrinology in relation to reproduction. Endocrinology plays a critical role in female reproduction, as it regulates the menstrual cycle, ovulation, and pregnancy. The female reproductive system is under the control of the hypothalamic- pituitary-gonadal (HPG) axis, which regulates the production of hormones that control the menstrual cycle and ovulation. The hypothalamus produces gonadotropin-releasing hormone (GnRH), which 6|Page stimulates the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH and LH then act on the ovaries to stimulate the development and maturation of follicles, which contain eggs. As the follicles mature, they produce estrogen, which triggers the thickening of the uterine lining and prepares it for potential implantation. Once a follicle reaches maturity, it releases an egg during ovulation. If the egg is fertilized by sperm, it implants in the uterine lining and pregnancy begins. The fertilized egg then produces human chorionic gonadotropin (hCG), which signals to the ovaries to continue producing estrogen and progesterone, which maintain the uterine lining and support the developing fetus. If the egg is not fertilized, it disintegrates and the corpus luteum, which is the remaining structure of the mature follicle, stops producing estrogen and progesterone. This leads to the shedding of the uterine lining during menstruation, which starts a new menstrual cycle. Other hormones that play a role in female reproduction include prolactin, which stimulates milk production after childbirth, and oxytocin, which triggers uterine contractions during labor and delivery. 8. The placenta and the membranes: development, structure, function. The placenta and the membranes play a crucial role in fetal development and pregnancy. The development of the placenta and membranes begins at fertilization, when the fertilized egg implants into the uterine lining. The placenta is an organ that develops in the uterus during pregnancy and is responsible for providing oxygen, nutrients, and waste elimination for the developing fetus. It also produces hormones that are essential for maintaining the pregnancy, such as human chorionic gonadotropin (hCG), estrogen, and progesterone. 7|Page The structure of the placenta consists of a fetal side and a maternal side, separated by a layer of tissue called the placental membrane. The fetal side is covered in small, branching structures called chorionic villi, which allow for exchange of gases, nutrients, and waste products between the fetal and maternal blood supplies. The maternal side is composed of blood vessels and tissues that supply oxygen and nutrients to the developing fetus. The membranes refer to the sac that surrounds the developing fetus and contains the amniotic fluid. The amniotic sac is composed of two layers: the chorion and the amnion. The chorion forms the outer layer of the sac and contains the chorionic villi that develop into the placenta. The amnion is the innermost layer of the sac and contains the amniotic fluid, which acts as a cushion and protects the developing fetus. Overall, the placenta and membranes are essential for fetal development and play a crucial role in maintaining a healthy pregnancy. 9. Physiological changes during pregnancy: genital and extragenital. During pregnancy, the female body undergoes significant physiological changes to accommodate the developing fetus and prepare for childbirth. These changes can be divided into genital and extragenital changes. Genital Changes: Uterus: The uterus increases in size as the fetus grows, and its weight increases from about 70 grams to about 1 kilogram at term. The uterus also undergoes rhythmic contractions throughout pregnancy to prepare for labor. 8|Page Cervix: The cervix softens, lengthens, and thins out (effaces) in preparation for childbirth. This process is known as cervical ripening. Vagina: Increased blood flow to the vagina can cause it to become swollen, and hormonal changes can cause the vagina to produce more mucus. Ovaries: Ovulation ceases during pregnancy, and the ovaries stop producing estrogen and progesterone. Extragenital Changes: Cardiovascular system: Blood volume increases by about 50% during pregnancy, and the heart rate and cardiac output increase to accommodate the increased demand. Blood pressure may also decrease slightly in the first and second trimesters. Respiratory system: The respiratory rate increases, and oxygen consumption also increases to support the fetus. Renal system: The kidneys increase in size and produce more urine, and the glomerular filtration rate increases. Gastrointestinal system: Hormonal changes can cause constipation and heartburn, and the growing uterus can push the stomach and intestines upward, causing discomfort and indigestion. Musculoskeletal system: The center of gravity shifts forward as the uterus grows, which can cause back pain and changes in posture. Hormonal changes also loosen the ligaments in the pelvic area in preparation for childbirth. Overall, these changes are essential for a healthy pregnancy and successful childbirth, but they can also cause discomfort and complications, which require proper management and monitoring by healthcare professionals. 10. Application of different diagnostic methods in obstetrics (physical examination, auscultation, palpation, laboratory, ultrasonography). Different diagnostic methods are used in obstetrics to evaluate the health of both the mother and the fetus during pregnancy. Here are some of the 9|Page commonly used diagnostic methods: Physical examination: This involves a general assessment of the mother's health and physical condition. The obstetrician checks the mother's weight, blood pressure, and heart rate, and also performs a pelvic exam to check the size and position of the uterus and to evaluate the cervix. Auscultation: This involves listening to the fetal heartbeat using a fetal doppler or a fetoscope. It is usually done during routine prenatal visits and is a noninvasive way to monitor the fetal heart rate. Palpation: This involves feeling the mother's abdomen to assess the size and position of the fetus. The obstetrician can also determine the presentation (e.g. head-down or breech) of the fetus through palpation. Laboratory tests: These include blood and urine tests to monitor the mother's health and to detect any conditions that may affect the pregnancy, such as gestational diabetes or preeclampsia. Ultrasonography: This is a non-invasive imaging technique that uses highfrequency sound waves to create images of the fetus and the mother's reproductive organs. It is used to monitor fetal growth, evaluate the placenta and amniotic fluid, and to detect any abnormalities or complications during pregnancy. Other diagnostic methods that may be used in obstetrics include fetal monitoring (to assess the fetal heart rate and detect any signs of distress), amniocentesis (to test for chromosomal abnormalities or other genetic conditions), and magnetic resonance imaging (MRI) (to evaluate fetal and maternal health in more detail). The specific diagnostic methods used will depend on the individual patient and the specific concerns or conditions that are being monitored or evaluated. 11. Methods of obstetrical examination. Obstetrical examination involves a series of physical and medical assessments to monitor the health of the mother and fetus during pregnancy. Some of the methods of obstetrical examination include: Physical examination: This involves assessing the general health of the mother, 10 | P a g e including blood pressure, weight, and any symptoms or complaints she may have. Obstetrical history: This involves obtaining information about the mother's past obstetrical and medical history, including previous pregnancies, deliveries, miscarriages, and medical conditions. Pelvic examination: This involves examining the size and shape of the pelvis to assess the likelihood of a vaginal delivery. The cervix and vaginal walls are also examined for any abnormalities. Ultrasonography: This is a non-invasive imaging technique that uses sound waves to produce images of the fetus and uterus. It is used to assess fetal growth, development, and well-being. Fetal monitoring: This involves monitoring the fetal heart rate using a fetal Doppler or electronic fetal monitor. It is used to assess fetal well-being during pregnancy and labor. Laboratory tests: These include blood tests, urine tests, and other diagnostic tests that are used to screen for medical conditions that may affect pregnancy, such as gestational diabetes, preeclampsia, and infections. Non-stress test: This is a test that is used to assess fetal well-being during pregnancy. It involves monitoring the fetal heart rate in response to fetal movement. Biophysical profile: This is a combination of fetal monitoring and ultrasonography that is used to assess fetal well-being in high-risk pregnancies. Amniocentesis: This is a diagnostic test that involves withdrawing a small amount of amniotic fluid from the uterus using a needle. The fluid is then analyzed for genetic abnormalities or other medical conditions. Chorionic villus sampling (CVS): This is a diagnostic test that involves taking a small sample of the placenta to test for genetic abnormalities or other medical conditions. 12. Diagnosis of pregnancy in 1*. 200 and 3" trimesters. Diagnosis of pregnancy in the first trimester is usually based on the presence of 11 | P a g e clinical signs and symptoms, as well as laboratory tests. The most common signs of pregnancy in the first trimester include a missed period, nausea and vomiting, breast tenderness, and fatigue. Pregnancy tests that detect the presence of human chorionic gonadotropin (hCG) in urine or blood are also reliable indicators of pregnancy. In the second trimester, pregnancy can be diagnosed by a combination of clinical examination, such as abdominal palpation and ultrasound imaging. Fetal movements can also be felt by the mother during this trimester, which is another sign of a viable pregnancy. In the third trimester, diagnosis of pregnancy is typically confirmed by the presence of a fetus on ultrasound imaging, as well as fetal movements and a growing uterus. The mother may also experience more physical symptoms such as back pain, shortness of breath, and difficulty sleeping. 13. Differential diagnosis of pregnancy. Differential diagnosis of pregnancy involves the identification of conditions that have similar symptoms to pregnancy. Some of the conditions that may present with symptoms similar to pregnancy include: Pseudocyesis: This is also known as false pregnancy. It is a condition where a woman experiences symptoms of pregnancy, but she is not actually pregnant. Ectopic pregnancy: This is a condition where the fertilized egg implants itself outside the uterus, usually in the fallopian tube. It can cause symptoms similar to pregnancy, but it is a life-threatening condition that requires immediate medical attention. Hydatidiform mole: This is a type of gestational trophoblastic disease that occurs when the cells that are supposed to form the placenta develop into abnormal cells. It can cause symptoms similar to pregnancy, but it requires immediate medical attention. Ovarian cyst: This is a fluid-filled sac that develops on the ovaries. It can cause 12 | P a g e abdominal discomfort, bloating, and irregular menstrual periods, which may be mistaken for pregnancy. Fibroids: These are non-cancerous growths that develop in the uterus. They can cause abdominal pain, heavy menstrual bleeding, and a feeling of fullness in the abdomen, which may be mistaken for pregnancy. Urinary tract infection: This is a bacterial infection that affects the urinary system. It can cause symptoms such as frequent urination, painful urination, and lower abdominal pain, which may be mistaken for pregnancy. Menopause: This is a natural process that occurs when a woman stops ovulating and menstruating. It can cause symptoms such as hot flashes, mood swings, and irregular menstrual periods, which may be mistaken for pregnancy. 14. Signs and symptoms of pregnancy in chronological order. Here are some common signs and symptoms of pregnancy in chronological order: Missed period: This is often the first sign of pregnancy, occurring around 4 weeks after the last menstrual period. Nausea and vomiting: Often called morning sickness, this can occur any time of the day and usually starts around 6 weeks of pregnancy. Fatigue: Feelings of exhaustion are common in early pregnancy due to increased levels of progesterone. Breast changes: The breasts may become sore, swollen, or tender around 6-8 weeks of pregnancy. Frequent urination: As the uterus expands, it can put pressure on the bladder, causing frequent trips to the bathroom, usually around 6-8 weeks of pregnancy. Food cravings and aversions: Changes in hormones can lead to specific food cravings or aversions, often beginning around 8-10 weeks of pregnancy. Mood swings: Hormonal changes during pregnancy can cause mood swings, ranging from happiness to sadness or irritability, often starting in the first trimester. Braxton Hicks contractions: These "practice" contractions can start as early as 13 | P a g e the second trimester. Fetal movement: Around 16-25 weeks of pregnancy, the fetus may start moving and kicking, which can be felt by the mother. Shortness of breath: As the uterus expands, it can put pressure on the diaphragm, causing shortness of breath, typically in the third trimester. It's important to note that not all women experience every symptom, and some may experience none at all. Additionally, some symptoms may occur at different times or in a different order than listed above. 15. Normal duration of pregnancy: time limits for early and late abortions, preterm. term and post-term labor. Estimation of expected delivery date. The normal duration of pregnancy is around 40 weeks or 280 days, calculated from the first day of the last menstrual period. This is divided into three trimesters, each lasting approximately 12-14 weeks. Early abortion refers to the termination of pregnancy before 12 weeks of gestation. Late abortion refers to the termination of pregnancy between 12 and 24 weeks of gestation. Preterm labor is defined as the onset of labor before 37 weeks of gestation. Term labor is defined as labor that occurs between 37 and 42 weeks of gestation. Post-term labor refers to labor that occurs after 42 weeks of gestation. The expected delivery date can be estimated using several methods, including the last menstrual period, ultrasound measurement of the fetal crown-rump length, and measurement of the fundal height. The most commonly used method is the last menstrual period, with the expected delivery date calculated by adding 280 days to the first day of the last menstrual period. Ultrasound measurements and fundal height measurements can also be used to estimate the gestational age and expected delivery date. 16. Fetus-in-utero: attitude, lie, presentation, position. 14 | P a g e Fetus-in-utero refers to the position of the fetus within the uterus during pregnancy. There are several terms used to describe the position of the fetus: Attitude: This refers to the position of the fetal head and limbs in relation to the fetal body. The normal attitude is the fetal head flexed forward onto the chest, with the arms crossed over the chest and the legs flexed at the hip and knee joints. Lie: This refers to the orientation of the fetus in relation to the mother's longitudinal axis. The two possible lies are longitudinal lie (fetal spine is parallel to the mother's spine) and transverse lie (fetal spine is perpendicular to the mother's spine). Presentation: This refers to the fetal body part that is closest to the birth canal. There are three main types of presentation: cephalic (head-first), breech (bottomfirst), and shoulder (transverse) presentation. Position: This refers to the specific location of the fetal presenting part in relation to the mother's pelvis. There are four positions for each presentation: occiput anterior (OA), occiput posterior (OP), sacrum anterior (SA), and sacrum posterior (SP). It is important to determine the attitude, lie, presentation, and position of the fetus during pregnancy to ensure a safe and successful delivery. This can be done through obstetrical examination, including ultrasound imaging. 17. Fetal length, weight at different ages, nutrition, circulation and its changes at birth. Fetal growth and development occur throughout the pregnancy, and the fetus undergoes many changes in size, weight, and circulation. During the first trimester, the fetus is approximately 3 inches long and weighs about 1 ounce. By the end of the second trimester, the fetus is around 14 inches long and weighs around 2 pounds. In the third trimester, the fetus continues to grow and gain weight rapidly, with an average length of around 20 inches and a weight of around 7-8 pounds at term. 15 | P a g e Nutrition is essential for fetal growth and development, and the fetus receives all its nutrition through the placenta. The mother's diet and nutritional status can affect fetal growth, and it is essential for pregnant women to maintain a healthy diet and receive proper prenatal care. The fetal circulation is unique in that it is adapted to the low oxygen environment of the uterus. The fetus receives oxygen and nutrients from the placenta through the umbilical vein, which carries oxygenated blood to the liver and then to the heart. The oxygenated blood is then distributed to the body through the aorta. Deoxygenated blood is carried back to the placenta through the umbilical arteries. At birth, the fetal circulation undergoes significant changes. The umbilical cord is clamped and cut, and the lungs take over the role of oxygenation. Blood flow to the lungs increases, and the foramen ovale and ductus arteriosus, which allow blood to bypass the lungs in utero, close. These changes result in the establishment of the adult circulatory system. 18. Fetal skull from obstetrical perspective: structure, sutures, fontanelles. diameters, adaptation to the birth canal. The fetal skull is an important aspect to consider in obstetrics as it determines the ability of the fetus to pass through the birth canal during delivery. Here are some key points regarding the fetal skull: Structure: The fetal skull is made up of several bones that are not yet fused together. This allows for some flexibility and molding of the skull during delivery. Sutures: The areas where the fetal skull bones meet are called sutures. These sutures are made up of fibrous tissue and allow for some movement of the skull bones during delivery. Fontanelles: The areas where several skull bones meet and form a "soft spot" are called fontanelles. The anterior fontanelle is the larger of the two and is often used to assess the position of the fetal head during delivery. 16 | P a g e Diameters: There are several diameters of the fetal skull that are important to consider during delivery. The biparietal diameter (BPD) is the distance between the two parietal bones and is the most commonly used measurement to estimate fetal head size. The occipitofrontal diameter (OFD) is the distance between the occipital and frontal bones, and the suboccipitobregmatic diameter (SOD) is the distance between the occipital bone and the bregma (an anatomical landmark on the skull). Adaptation to the birth canal: The fetal skull is designed to adapt to the shape of the birth canal during delivery. This is accomplished through a combination of molding (changes in the shape of the skull bones) and descent (movement of the fetal head through the birth canal). The position of the fetus (i.e. occiput anterior, occiput posterior) can also affect how the skull adapts to the birth canal. 19. Female pelvis from obstetrical perspective: bony structure, inlet, cavity. outlet, diameters, axis, joints, external diameters. The female pelvis is a bony structure that supports the weight of the upper body and protects the pelvic organs. It is divided into two parts: the greater pelvis and the lesser pelvis. The greater pelvis is located above the pelvic brim (or inlet) and is wider than the lesser pelvis, which is located below the pelvic brim. The pelvic brim is an imaginary line that separates the two parts of the pelvis. The pelvic cavity, which is located in the lesser pelvis, is where the fetal head passes during delivery. It has an inlet, a cavity, and an outlet. The inlet is the upper opening of the pelvic cavity and is defined by the pelvic brim. The cavity is the space between the inlet and the outlet, and the outlet is the lower opening of the pelvic cavity. The diameters of the pelvic inlet are important in determining whether a fetus can pass through the pelvis during delivery. The main diameters are the 17 | P a g e anteroposterior diameter (from the sacral promontory to the pubic symphysis), the transverse diameter (the widest part of the pelvic inlet), and the oblique diameters (from one iliopectineal eminence to the opposite sacroiliac joint). The pelvic joints are important for allowing the pelvis to expand during delivery. The sacroiliac joints connect the sacrum to the ilium, while the pubic symphysis connects the two pubic bones. The external diameters of the pelvis are also important in determining whether a fetus can pass through the pelvis during delivery. The main external diameters are the interspinous diameter (the distance between the two ischial spines), the intertuberous diameter (the distance between the two ischial tuberosities), and the bispinous diameter (the distance between the two anterior superior iliac spines). Overall, the shape and size of the female pelvis play a crucial role in the successful delivery of a fetus. 20. Diagnosis of prelabour and labour. Definitions of normal and abnormal labour. Prelabour is the time period before the onset of true labour. It is characterized by contractions that do not result in cervical dilation. The diagnosis of prelabour is based on the absence of cervical changes and the presence of irregular contractions. Labour is defined as the process by which the fetus is expelled from the uterus. The diagnosis of labour is based on the presence of regular, painful contractions that result in cervical dilation and effacement. The onset of labour is typically diagnosed when the woman's contractions become regular and increase in intensity, leading to progressive cervical dilation and effacement. Normal labour is defined as labour that progresses spontaneously, without 18 | P a g e complications, and results in the safe delivery of a healthy baby. Abnormal labour is defined as labour that is prolonged, obstructed, or associated with complications that may put the mother or baby at risk. Prolonged labour is defined as labour that lasts longer than 18-24 hours in primigravidas or longer than 12-14 hours in multigravidas. Obstructed labour is defined as labour in which the fetus cannot pass through the birth canal due to a mechanical obstruction, such as cephalopelvic disproportion or malposition of the fetus. Other factors that may be considered abnormal in labour include failure of cervical dilation, failure of descent of the fetal head, abnormal fetal heart rate patterns, and maternal exhaustion or distress. These factors may require medical intervention to ensure a safe delivery for both the mother and the baby. 21. Causes of onset of labour. The onset of labor is a complex process that is not fully understood, but there are several factors that are believed to contribute to it. These include: Hormonal changes: As the pregnancy progresses, the levels of certain hormones, such as oxytocin and prostaglandins, increase in the mother's body. These hormones play a role in stimulating uterine contractions and preparing the cervix for delivery. Fetal factors: As the fetus grows and develops, it puts increasing pressure on the uterus and cervix. This pressure can also help to stimulate contractions and initiate labor. Maternal factors: Maternal factors, such as physical activity, stress, and dehydration, can also play a role in initiating labor. For example, physical activity can help to stimulate contractions by increasing blood flow to the uterus. Placental factors: Towards the end of pregnancy, the placenta may begin to deteriorate, which can trigger the release of hormones that stimulate labor. Genetic factors: There is some evidence to suggest that genetic factors may play 19 | P a g e a role in the onset of labor. For example, certain genes have been linked to an increased risk of preterm labor. 22. Contractile system of myometrium. The contractile system of the myometrium is composed of smooth muscle cells that are arranged in multiple layers with various orientations. During pregnancy, the uterus undergoes significant changes in structure and function in preparation for labor and delivery. Hormones such as estrogen and progesterone play a critical role in these changes by modulating the contractile properties of the myometrium. The myometrium contains specialized cells known as pacemaker cells that generate spontaneous electrical impulses, which propagate through gap junctions to neighboring smooth muscle cells. These electrical impulses trigger the release of calcium ions from intracellular stores, which activate the contractile machinery of the smooth muscle cells and lead to contraction of the myometrium. During labor, the myometrium undergoes a series of coordinated contractions that gradually increase in frequency, duration, and intensity. These contractions are stimulated by a variety of factors, including hormonal changes, mechanical stretch of the uterus, and neural signals from the fetus. The coordinated contractions of the myometrium are essential for the expulsion of the fetus and placenta during delivery. 23. Stages of labour. Normal duration of labour. Labor is typically divided into three stages: 20 | P a g e First stage of labor: This stage starts with the onset of regular uterine contractions and ends with complete cervical dilation at 10 centimeters. The first stage is further divided into a latent phase and an active phase. The latent phase can last for several hours or even days, during which the cervix gradually thins and begins to dilate. The active phase typically lasts for several hours and is characterized by more rapid cervical dilation and stronger contractions. Second stage of labor: This stage begins once the cervix is fully dilated and ends with the delivery of the baby. During this stage, the mother is encouraged to push with each contraction to help move the baby down the birth canal and out of the body. Third stage of labor: This stage begins after the baby is delivered and ends with the delivery of the placenta. During this stage, the uterus continues to contract to help detach the placenta from the uterine wall and push it out of the body. The normal duration of labor varies widely, but for first-time mothers, the first stage of labor typically lasts around 12-14 hours, while subsequent labors may be shorter. The second stage of labor usually lasts between 20 minutes to 2 hours, and the third stage usually lasts around 5-30 minutes. However, these durations can be affected by factors such as the mother's age, the size and position of the baby, and the use of medical interventions. It's important to note that every woman's labor experience is unique and there is no "right" or "wrong" way for labor to progress as long as both the mother and baby are healthy. 24. Mechanism of labour for occipito-anterior position. The mechanism of labor for occipito-anterior position refers to the movements that the fetal head undergoes as it descends through the birth canal during a normal vaginal delivery. Here are the steps of the mechanism of labor for occipito-anterior position: Engagement: The widest diameter of the fetal head (the biparietal diameter) passes through the maternal pelvic inlet, and the head becomes fixed in the 21 | P a g e pelvic cavity. Descent: The head moves further down the birth canal as a result of uterine contractions and maternal pushing efforts. Flexion: As the head descends, it encounters resistance from the soft tissues of the pelvic floor. To negotiate this resistance, the fetal head flexes forward, so that the chin comes into contact with the fetal chest. Internal rotation: Once the fetal head reaches the pelvic floor, it rotates 45-90 degrees so that the occiput (back of the head) faces the maternal symphysis pubis. This is known as "internal rotation." Extension: After internal rotation, the fetal head begins to extend, so that the chin is lifted up towards the pubic bone. Restitution: Once the head is delivered, it will rotate back to its original position, aligning itself with the shoulders. External rotation: After restitution, the shoulders descend into the pelvis in a transverse position. Once the shoulders reach the pelvic outlet, they rotate 90 degrees to align with the anteroposterior diameter of the outlet. Expulsion: The rest of the body follows the shoulders, and the baby is born. The normal duration of labor varies, but is generally considered to be around 1218 hours for first- time mothers and 6-8 hours for subsequent deliveries. However, labor can be longer or shorter than these time frames and still be considered normal as long as progress is being made and the mother and baby are tolerating labor well. 25. Mechanism of labour for occipito-posterior position. Occipito-posterior position is a fetal position during childbirth where the baby's head is facing towards the mother's abdomen rather than her spine. This position is also called the posterior position, and it occurs in about 10-20% of births. It is associated with prolonged labor, more difficult vaginal delivery, and increased rates of cesarean section. The mechanism of labor for the occipito- posterior position is different from that of the occipito-anterior position, and it is generally more difficult. During the first stage of labor, the fetus may rotate to the occipito-posterior position due to various factors such as a small maternal pelvis, weak 22 | P a g e contractions, or fetal anomalies. In this position, the fetal head enters the maternal pelvis with the occiput facing towards the mother's sacrum instead of towards the pubic bone. As the fetus descends into the birth canal, the occipito-posterior position causes the head to extend and rotate further back towards the mother's spine. This can lead to pressure on the mother's sacrum and tailbone, causing more intense back pain and longer pushing phases. The fetus may also have difficulty navigating the curves of the birth canal, leading to slower progress and increased likelihood of assisted delivery. During the second stage of labor, the fetal head typically rotates to a more favorable position, such as occipito-anterior, before delivery. However, in some cases, the fetus may remain in the occipito- posterior position, making delivery more difficult. In these cases, the healthcare provider may need to use special techniques such as forceps or vacuum extraction to assist with delivery. 26. First stage of labour: physiology, clinical course and management. The first stage of labor is the period of time between the onset of true labor contractions and the full dilation of the cervix. It is divided into two phases: the latent phase and the active phase. During the latent phase, the cervix begins to efface (thin out) and dilate (open up) slowly. Contractions become more frequent and regular, but are typically mild and irregular. This phase can last for several hours or even days. During the active phase, the cervix continues to dilate more rapidly, typically at a rate of 1 cm per hour. Contractions become stronger, longer, and closer together, typically every 3-5 minutes. This phase can last for several hours, but typically lasts between 3-8 hours for first-time mothers. Management during the first stage of labor includes frequent monitoring of fetal 23 | P a g e heart rate, maternal vital signs, and uterine contractions. Pain relief options such as epidurals, nitrous oxide, and non- pharmacologic methods like breathing techniques and position changes may be offered to the mother. In some cases, oxytocin (Pitocin) may be used to augment or induce labor if progress is slow or if there are concerns for fetal or maternal well-being. If progress is slow or there are concerns for the safety of the mother or baby, a cesarean delivery may be recommended. Immediate postpartum period: This period lasts from delivery to 2 hours after birth. During this time, the mother is monitored closely for signs of hemorrhage, uterine atony, and other complications. Early puerperium: This period lasts from 2 hours to 24 hours after birth. The mother is monitored for vital signs, uterine involution, and lactation. She is also assessed for any signs of infection or other complications. Late puerperium: This period lasts from 24 hours to 6 weeks after birth. The mother is monitored for continued uterine involution, lactation, and the resumption of menstruation. She is also assessed for any signs of postpartum depression or other emotional disturbances. Management during the puerperium includes monitoring for complications, such as hemorrhage, infection, or thromboembolism, as well as providing education and support for breastfeeding and infant care. Mothers are also encouraged to practice good self-care, including getting adequate rest, eating a healthy diet, and engaging in light exercise. 27. Lactation: physiology, stimulation ailments. Lactation is the process of producing and secreting milk from the mammary glands of the breasts. It is essential for providing nutrition to newborn infants and promoting their growth and development. The physiology of lactation is complex and involves the interaction of hormones, nerves, and breast tissue. 24 | P a g e During pregnancy, hormonal changes stimulate the development of the breast tissue and prepare it for lactation. The hormone prolactin, produced by the pituitary gland, stimulates milk production in the mammary glands, while the hormone oxytocin, also produced by the pituitary gland, causes the let-down reflex, which is the release of milk from the mammary glands. After delivery, the baby's suckling stimulates the release of prolactin, which maintains milk production, and oxytocin, which causes the milk to be released from the mammary glands. Frequent and effective breastfeeding is important for maintaining milk production and ensuring that the baby is well-nourished. Several factors can affect lactation, including stress, fatigue, hormonal imbalances, and certain medications. In some cases, lactation may be difficult or even impossible, and formula feeding may be necessary. Stimulation ailments, such as mastitis and engorgement, can also affect lactation. Mastitis is an inflammation of the breast tissue that can cause pain, swelling, and fever. Engorgement is the overfilling of the mammary glands with milk, which can cause discomfort and difficulty breastfeeding. Treatment for both conditions includes rest, warm compresses, and antibiotics for mastitis. Gentle massage, warm compresses, and frequent breastfeeding can help relieve engorgement. 28. Second stage of labour: physiology, clinical course and management, The second stage of labor is the stage of active pushing and delivery of the baby. It begins when the cervix is fully dilated and ends with the delivery of the baby. Physiology: During this stage, the uterus contracts to push the baby down the birth canal, while the mother actively pushes to help deliver the baby. The contractions become stronger and closer together, and the mother experiences an urge to push as the baby moves lower in the birth canal. The pelvic floor muscles also play a significant role in the second stage of labor. The pelvic floor muscles need to relax to allow the baby to pass through the birth canal, and the mother needs 25 | P a g e to use these muscles to push effectively. Clinical course and management: The second stage of labor can last anywhere from a few minutes to a few hours, depending on the position and size of the baby and the mother's pushing effort. During this stage, the mother is encouraged to push with each contraction and rest in between contractions to conserve energy. The healthcare provider will monitor the baby's heart rate and the mother's vital signs and may guide the mother through different positions to help facilitate delivery. If progress is slow, the healthcare provider may assist with forceps or a vacuum extraction to help deliver the baby. In some cases, the healthcare provider may recommend a cesarean section if there are concerns about the safety of the baby or mother. After the baby is delivered, the healthcare provider will clamp and cut the umbilical cord and may administer medication to help the uterus contract and reduce bleeding. The baby will be assessed for breathing and overall health, and the mother will continue to have her vital signs monitored. 29. Third stage of labour: physiology, clinical course and management. The third stage of labor is the delivery of the placenta and membranes after the baby is born. During the third stage, the uterus continues to contract, causing the placenta to separate from the uterine wall and be expelled through the vagina. Physiology: During the third stage, the contraction of the uterus prevents bleeding and causes the separation of the placenta from the uterine wall. The contractions help to decrease the size of the uterus, which helps expel the placenta and membranes. Clinical course: The third stage of labor typically lasts about 5-30 minutes, with an average of 10-15 minutes. The signs that indicate the onset of the third stage of labor are a change in the shape of the uterus, a lengthening of the umbilical 26 | P a g e cord, and a gush of blood. The healthcare provider may use controlled cord traction, gentle pulling on the umbilical cord to assist in the delivery of the placenta. Management: Active management of the third stage of labor involves giving a uterotonic agent such as oxytocin, which helps the uterus to contract and expel the placenta more quickly, reducing the risk of postpartum hemorrhage. Controlled cord traction is performed to help deliver the placenta. The healthcare provider will also check the placenta and membranes to ensure that they are complete and no fragments are left inside the uterus. If fragments are left, it can increase the risk of infection and bleeding. 30. Mother and fetal monitoring in labour. Apgar score. Immediate post partum neonatal care. Mother and fetal monitoring during labor is essential to identify any potential problems and intervene promptly. There are several ways to monitor both the mother and fetus during labor, including: Maternal vital signs: Blood pressure, heart rate, and respiratory rate should be monitored at regular intervals during labor. Fetal heart rate monitoring: This can be done through intermittent auscultation or continuous electronic fetal monitoring (EFM). Intermittent auscultation involves listening to the fetal heart rate with a stethoscope or handheld Doppler device at specific intervals, while EFM uses a device that is strapped to the mother's abdomen to continuously monitor the fetal heart rate. Uterine contractions: The frequency, duration, and strength of uterine contractions can be monitored using a tocodynamometer, which measures changes in the abdominal girth. Cervical dilation: The progress of cervical dilation can be assessed by performing vaginal examinations. The Apgar score is a standardized method of evaluating the physical condition of 27 | P a g e a newborn immediately after delivery. The score is based on five parameters: heart rate, respiratory effort, muscle tone, reflex irritability, and skin color. Each parameter is scored from 0 to 2, and the scores are added up to give a total score ranging from 0 to 10. A score of 7 or higher is considered normal, while a score of 3 or lower indicates that the newborn requires immediate medical attention. Immediate postpartum neonatal care includes a thorough physical examination of the newborn to assess for any abnormalities or signs of distress. The newborn's vital signs, including temperature, heart rate, and respiratory rate, are also monitored. The newborn may receive preventive measures such as eye prophylaxis and vitamin K administration. The mother and newborn are typically kept together to promote bonding and initiate breastfeeding, unless there are medical reasons for separation. 31. The puerperium: physiology, clinical course and management. The puerperium is the period following childbirth during which the mother's body returns to its pre- pregnancy state. It usually lasts for 6 weeks but can be shorter or longer depending on individual circumstances. During this time, the uterus undergoes involution, which is the process of returning to its pre-pregnancy size and location. Physiologically, the puerperium is characterized by changes in hormone levels, particularly a decrease in estrogen and progesterone levels. The breasts produce milk for lactation, and there is a gradual decrease in the amount of lochia, which is the vaginal discharge consisting of blood, mucus, and tissue debris. Clinically, the puerperium is characterized by the following stages: Immediate postpartum period: This period lasts from delivery to 2 hours after birth. During this time, the mother is monitored closely for signs of hemorrhage, 28 | P a g e uterine atony, and other complications. Early puerperium: This period lasts from 2 hours to 24 hours after birth. The mother is monitored for vital signs, uterine involution, and lactation. She is also assessed for any signs of infection or other complications. Late puerperium: This period lasts from 24 hours to 6 weeks after birth. The mother is monitored for continued uterine involution, lactation, and the resumption of menstruation. She is also assessed for any signs of postpartum depression or other emotional disturbances. Management during the puerperium includes monitoring for complications, such as hemorrhage, infection, or thromboembolism, as well as providing education and support for breastfeeding and infant care. Mothers are also encouraged to practice good self-care, including getting adequate rest, eating a healthy diet, and engaging in light exercise. 32. Lactation: physiology, stimulation ailments. Lactation is the process of producing and secreting milk from the mammary glands of the breasts. It is essential for providing nutrition to newborn infants and promoting their growth and development. The physiology of lactation is complex and involves the interaction of hormones, nerves, and breast tissue. During pregnancy, hormonal changes stimulate the development of the breast tissue and prepare it for lactation. The hormone prolactin, produced by the pituitary gland, stimulates milk production in the mammary glands, while the hormone oxytocin, also produced by the pituitary gland, causes the let-down reflex, which is the release of milk from the mammary glands. After delivery, the baby's suckling stimulates the release of prolactin, which maintains milk production, and oxytocin, which causes the milk to be released from the mammary glands. Frequent and effective breastfeeding is important for maintaining milk production and ensuring that the baby is well-nourished. Several factors can affect lactation, including stress, fatigue, hormonal imbalances, and certain 29 | P a g e medications. In some cases, lactation may be difficult or even impossible, and formula feeding may be necessary. Stimulation ailments, such as mastitis and engorgement, can also affect lactation. Mastitis is an inflammation of the breast tissue that can cause pain, swelling, and fever. Engorgement is the overfilling of the mammary glands with milk, which can cause discomfort and difficulty breastfeeding. Treatment for both conditions includes rest, warm compresses, and antibiotics for mastitis. Gentle massage, warm compresses, and frequent breastfeeding can help relieve engorgement. 30 | P a g e 31 | P a g e 33. Breech presentation: etiology, varieties, diagnosis and prognosis for delivery. ETIOLOGY:1. Prematurity: It is the most common cause of breech presentation. Factors preventing spontaneous version: (a) Breech with extended legs, (b) Twins, (c) Oligohydramnios, (d) Congenital malformation of the uterus such as septate or bicornuate uterus, (e) Short cord, relative or absolute, (f) Intrauterine death of the fetus. 2. Favorable adaptation: (a) Hydrocephalus- big head can be well accommodated in the wide fundus, (b) Placenta previa, (c) Contracted pelvis, (d) Cornu-fundal attachment of the placenta-minimizes the space of the fundus where the smaller head can be placed comfortably. 3. Undue mobility of the fetus: (a) Hydramnios, (b) Multiparae with lax abdominal wall. Fetal abnormality: Trisomies 13, 18, 21, anencephaly and myotonic dystrophy due to alteration of fetal muscular tone and mobility. Recurrent breech: On occasion, the breech presentation recurs in successive pregnancies. When it recurs in three or more consecutive pregnancies, it is called habitual or recurrent breech. The probable causes are congenital malformation of the uterus, septate or bicornuate, and repeated cornu-fundal attachment of the placenta. VARIETIES There are two varieties of breech presentation. • Complete • Incomplete Complete (Flexed breech): The normal attitude of full flexion is maintained. Thighs are flexed at hips and legs at knees. The presenting part consists of two buttocks, external genitalia and two feet. It is commonly present in multi-parae (10%). Incomplete: This is due to varying degrees of extension of thighs or legs at the podalic pole. Three varieties are possible: 32 | P a g e • Breech with extended legs (Frank breech): In this condition, thighs are flexed on the trunk and legs are extended at the knee joints (Fig. 26.10). The presenting part consists of the two buttocks and external genitalia only. It is commonly present in primigravidae, about 70%. The increased prevalence in primigravida is due to a tight abdominal wall, good uterine tone and early engagement of breech. Footling presentation (25%): Both thighs and legs are partially extended bringing the legs to present at brim. Knee presentation: Thighs are extended but the knees are flexed, bringing the knees down to present at the brim. The latter two varieties are not common. Clinical varieties: In an attempt to find out the dangers inherent to breech, breech presentation is clinically classified as: Uncomplicated It is defined as one where there is no other associated obstetric complications apart from the breech, prematurity being excluded. Complicated--When the presentation is associated with conditions which adversely influence the prognosis such as prematurity, twins, contracted pelvis, placenta previa, etc. It is called complicated breech. Extended legs, extended arms, cord prolapse or difficulty encountered during breech delivery should not be called complicated breech but are called complicated or abnormal breech delivery. DIAGNOSIS OF BREECH PRESENTATION Clinical. Sonography ULTRASONOGRAPHY is most informative. (1) It confirms the clinical diagnosisespecially in primigravidae with engaged frank breech or with tense abdominal wall and irritable uterus. (2) It can detect fetal congenital abnormality and also congenital anomalies of the uterus. (3) Type of breech (complete or incomplete. (4) It measures biparietal diameter, gestational age and estimated weight of the fetus. (5) It also localizes the placenta. (6) Assessment of liquor volume (important for ECV). (7) Attitude of the head - flexion or hyperextension (important for decision making at the time of delivery). CT and MRI can be used to assess the pelvic capacity in addition to all the above-mentioned information. 33 | P a g e 34. Mechanism of breech delivery MECHANISM OF LABOR IN BREECH PRESENTATION SACROANTERIOR POSITION: In the mechanism of breech delivery, the principal movements occur at three places-buttocks, shoulders and the head. The first two successive parts to be born are bigger but more compressible while the head because of nonmolding due to rapid descent, presents difficulties. Each of the three components undergo cardinal movements as those of normal mechanism Buttocks • The diameter of engagement of the buttock is one of the oblique diameters of the inlet. The engaging diameter is bitrochanteric (10 cm or 4*) with the sacrum directed toward the iliopubic eminence. When the diameter passes through the pelvic brim, the breech is engaged. * Descent of the buttocks occurs undthe anterior Duttock touches the pelvIc floor. interna rotation of the anterior buttock occurs throuch 178th of a circle blacing it behind the symbhysis pubis. * Further descent with lateral flexion of the trunk occurs until the anterior hip hinges under the symphysis pubis which is released first followed by the posterior hip. * Delivery of the trunk and the lower limbs follow. * Restitution occurs so that the buttocks occupy the original position as during engagement in oblique diameter. Shoulders: * Bisacromial diameter (12 cm or 4 3/4") engages in the same oblique diameter as that occupied by the buttocks at the brim soon after the delivery of the breech. 34 | P a g e * Descent occurs with internal rotation of the shoulders bringing the shoulders to lie in the anteroposterior diameter of the pelvic outlet. 'The trunk simultaneously rotates externally through 1/8th of a circle. * Delivery of the posterior shoulder followed by the anterior one is completed by anterior flexion of the delivered trunk. * Restitution and external rotation: Untwisting of the trunk occurs putting the anterior shoulder toward the right thigh in LSA and left thigh in RSA. External rotation of the shoulders occurs to the same direction because of internal rotation of the occiput through 1/8th of a circle anteriorly. The fetal trunk is now positioned as dorsoanterior Head: * Engagement occurs either through the opposite oblique diameter as that occupied by the buttocks or through the transverse diameter. The engaging diameter of the head is suboccipitofrontal (10 cm). * Descent with increasing flexion occurs. * Internal rotation of the occiput occurs anteriorly, through 1/8th or 2/8th of a circle placing the occiput behind the symphysis pubis. * Further descent occurs until the subocciput hinges under the symphysis pubis. * Head is born by flexion-chin, mouth, nose, forehead, vertex and occiput appearing successively. The expulsion of the head from the pelvic cavity depends entirely upon the bearing-down efforts and not at all on uterine contractions. Sacronosterior position: In sacroposterior position, the mechanism is not substantially modified. The head has To rotate 3/8th of circle to bring the occiput behind the symphysis pubis. 35. Antenatal management of breech presentation. Place of external cephalic version in modern obstetrics. Antenatal management in breech presentation consists of: Identificationofthecomplicatingfactorsrelatedwithbreechpresentation. Externalcephalicversion,ifnotcontraindicated. 35 | P a g e Formulation of the line of management, if the version fails or is contraindicated. Identification of complicating factor: It can be detected by clinical examination, supplemented by sonography. Sonography is particularly useful to detect congenital malformations of the fetus, the precise location of the placental site and congenital anomalies of the uterus. External Cephalic Version (ECV): There are protagonists and antagonists to external version. As such, in an institution or to an individual where the perinatal mortality in vaginal breech delivery is appreciably high, there is enough justification for its use. The success rate of version is about 65%. Cardiotocography (CTG) should ideally be done before and after the procedure. Time of version: ECV has been considered from 36 weeks onward. While version in the early weeks is easy but chance of reversion is more. Late version may be difficult because of increasing size of the fetus and diminishing volume of liquor amnii. However, the use of uterine relaxant (tocolysis) has made the version at later weeks less difficult. It minimizes chance of reversion and should fetal complications develop, it can be effectively tackled by cesarean section. Hypertonus or irritable uterus can be overcome with the use of tocolytic drugs. 36. Management of vaginal breech delivery. FIRST STAGE: The management protocol is similar to that mentioned in normal labor. The following are the important considerations. Spontaneous onset of labor increases the chance of successful vaginal delivery. Vaginalexaminationisindicated— (a)attheonsetoflaborforpelvicassessment,(b)soonafter rupture of the membranes to exclude cord prolapse. An intravenous line is sited with Ringer’s solution, oral intake is avoided, blood is sent for group and cross matching (considering the chance of CS). Adequate analgesia is given, epidural is preferred. Fetal status and progress of labor are monitored. Oxytocin in fusion may be used for augmentation of labor. 36 | P a g e Indications of Cesarean Section (CS): (a) Cases seen for the first time in labor with presence of complications; (b) Arrest in the progress of labor; (c) Nonreassuring FHR pattern (Fetal distress); (d) Cord presentation or prolapse. SECOND STAGE: There are three methods of vaginal breech delivery: Spontaneous(10%):Expulsion of the fetus occurs with very little assistance. This is not preferred. Assisted breech:The delivery of the fetus is by assistance from the beginning to the end.This method should be employed in all cases (see below). Breech extraction(partial or total):When part or the entire body of the fetus is extracted by the obstetrician. It is rarely done these days as it produces trauma to the fetus and the mother. Indications are: (a) Delivery of the second twin after IPV (see p. 242, 665), (b) Cord prolapse, (c) Extended legs arrested at the cavity or at the outlet. 37. Assisted breech delivery and extraction of breech. Steps: The patient is brought to the table when the anterior buttock and fetal an usarevisible. She is placed in lithotomy position when the posterior buttock distends the perineum. To avoid aortocaval compression, the woman is tilted laterally (15°) using a wedge under the back. Antisepticc leaning is done, bladder is emptied with an “in and out” catheter. Pudendal block is done along with perineal infiltration if not epidural has been used earlier. Episiotomy: It should be made in all cases of primigravidae and selected multiparae. Its advantages are—(a) to straighten the birth canal which especially facilitates the delivery of breech with extended legs where lateral flexion is inadequate; (b) to facilitate intravaginal manipulation and for forceps delivery, (c) to minimize compression of the aftercoming head. The best time for episiotomy is when the perineum is distended and thinned by the breech as it is “climbing” the perineum. 37 | P a g e The patient is encouraged to bear down as the expulsive forces from above ensure flexion of the fetal head and safe descent. The “no touch to the fetus” policy is adopted until the buttocks are delivered along with the legs in flexed breech and the trunk slips up to the umbilicus. Soon after the trunk up to the umbilicus is born. The following are to be done: (a) The extended legs (in frank breech) are to be decomposed by pressure on the knees (popliteal fossa) in a manner of abduction and flexion of the thighs (b) The umbilical cord is to be pulled down and to be mobilized to one side of the sacral bay to minimize compression. There may be transient abnormality in cord pulsation at this stage which has got no prognostic significance. An attempt of hasty delivery for this reason alone should be avoided. (c) If the back remains posteriorly, rotate the trunk to bring the back anteriorly (sacro anterior). (d) The baby is wrapped with a sterile towel to prevent slipping when held by the hands and to facilitate manipulation, if required. Delivery of the arms: The arms are delivered one after the other only when one axilla is visible, by simply hooking down each elbow with a finger. It is immaterial as to which arm is to be delivered first. Delivery of the aftercoming head: (a) Burns-Marshall method (Fig. 26.17): The baby is allowed to hang by its own weight. The assistant is asked to give suprapubic pressure with the flat of hand in a downward and backward direction, the pressure is to be exerted more toward the sinciput. When the nape of the neck is visible under the pubic arch, the baby is grasped by the ankles with a finger in between the two. When the mouth is cleared off the vulva, there should be no hurry. Mucus of the mouth and pharynx is cleared by mucus sucker. The trunk is depressed to deliver rest of the head. (b) Forceps delivery: Forceps can be used as a routine. The head must be in the cavity. The advantages are—(a) delivery can be controlled by giving pull directly on the head and the force is not transmitted through the neck, (b) flexion is better maintained and (c) mucus can be sucked out from the mouth more effectively. The head should be brought as low down as possible by allowing the baby to hang by its own weight aided by suprapubic pressure. When the occiput lies against the back of the symphysis pubis, an assistant raises the legs of the 38 | P a g e child as much to facilitate introduction of the blades from below. Too much elevation of the trunk may cause extension of the head. The head should be delivered slowly (over 1 minute) to reduce compression-decompression forces as that may cause intracranial bleeding. (c) Malar flexion and shoulder traction (modified Mauriceau-Smellie-Veit technique): The technique is named after the three great obstetricians who described the use of the grip independently. The baby is placed on the supinated left forearm (preferred) with the limbs hanging on either sides. The assistant gives suprapubic pressure during the period to maintain flexion. Thereafter, the fetus is carried in upward and forward direction toward the mother’s abdomen releasing the face, brow and lastly, the trunk is depressed to release the occiput and vertex. 38. Face presentation: etiology, varieties, mechanism of labour, diagnosis and prognosis for delivery. Etiology: The cause of extreme extension of the head is not clear in all the cases. The following are the factors which are often associated. Maternal: (1) Multiparity with pendulous abdomen, (2) Lateral obliquity of the uterus especially, if it is directed to the side toward which the occiput lies, (3) Contracted pelvis is associated in about 40% cases. Flat pelvis favors face presentation, (4) Pelvic tumors. Fetal: (1) Congenital malformations (15%)—(a) The most common one is anencephaly. The almost nonexistent neck with absence of the cranium makes it easy to feel the facial structure even with semi- extended head, (b) Congenital goiter prevalent in endemic areas, (c) Dolichocephalic head with long anteroposterior diameter, (d) Congenital bronchocele. (2) Twist of the cord several turns round the neck. (3) Increased tone of the extensor group of neck muscles. Mechanism : MENTOANTERIOR 60–80% (LMA OR RMA) 39 | P a g e The principal movements are like those of corresponding occipitoanterior position. The exceptions are increasing extension instead of flexion and delivery by flexion instead of extension of the head. Engagement: The diameter of engagement is the oblique diameter—right in LMA, left in RMA, with the mentum related to one iliopubic eminence and the glabella to the opposite sacroiliac joint. The engaging diameter of the head is submentobregmatic 9.5 cm (3 3/4") in fully extended head or submentovertical 11.5 cm (4 1/2") in partially extended head. Engagement is delayed because of long distance between the mentum and biparietal plane (7 cm). Descent with increasing extension occurs till the chin touches the pelvic floor. Internal rotation—Internal rotation of the chin occurs through 1/8th of a circle anteriorly, placing the mentum behind the symphysis pubis. Further descent occurs till the submentum hinges under the pubic arch. Delivery of the head—The head is born by flexion delivering the chin, face, brow, vertex and lastly the occiput. The diameter distending the vulval outlet is submentovertical—11.5 cm (4 1/2"). Restitution occurs through 1/8th of a circle opposite to the direction of internal rotation. External rotation occurs further 1/8th of circle to the same side of restitution so that ultimately the face looks directly to the left thigh in LMA and right thigh in RMA. This follows delivery of the anterior shoulder followed by the posterior shoulder and the rest of the trunk by lateral flexion. MENTOPOSTERIOR (20–25%) (RMP OR LMP): The cardinal movements in the mechanism of mento- posterior positions are like those of occipitoposterior position. The salient differentiating features are—(1) In the mentoposterior position, anterior rotation of the mentum occurs in only 20– 30% cases. (2) In the rest (70–80%), incomplete anterior rotation, non rotation or short posterior rotation of the mentum occurs. Arrest occurs in all these positions with average size pelvis and fetalhead. Unlike persistent occipitoposterior, where occasional face-to-pubis delivery occurs, there is no possibility of spontaneous delivery in persistent mentoposterior. This is because the relatively short neck cannot clear off the total length of the sacrum (12 cm). As such the thorax is thrust in, resulting bregmaticosternal diameter (18 cm or 7") to occupy the pelvis. As a result, the labor becomes inevitably obstructed. 40 | P a g e Diagnosis VAGINAL EXAMINATION The diagnostic features are palpating the mouth with hard alveolar margins, nose, malar eminences, supraorbital ridges and the mentum (Fig. 26.26). In early labor, because of high head and sausage shaped bag of membranes, the parts are not clearly defined. In late labor, the parts are often obscured due to edema. It is often confused with breech presentation. The distinguishing features are—(1) the mouth and the malar eminences are not in a line; but in breech, the anus and the ischial tuberosities are in one line, (2) sucking effect of mouth, (3) hard alveolar margins and (4) absence of meconium staining on the examination fingers. The mentum and the mouth should be clearly identified to exclude brow presentation and to identify the position. The examination should be conducted gently, as there is chance of injury to the eyes. Assessment of the pelvis should be done as a routine. SONOGRAPHY/RADIOGRAPHY: This should be done to confirm the diagnosis, to exclude bony congenital malformation of the fetus and to note the size of the baby. 39. Brow presentation: etiology. varieties, mechanism of labour, diagnosis and prognosis for delivery. CAUSES: The causes of persistent brow are more or less the same as those of face presentation. The position is commonly unstable and converts to either vertex or face presentation. DIAGNOSIS: Antenatal diagnosis is rarely made. The findings are more or less like those of face presentation. The cephalic prominence and the groove between it and the back are less prominent. The head feels very big and is nonengaged. Vaginal examination: The position is to be confirmed on vaginal examination by palpating supraorbital ridges and anterior fontanel. If the anterior fontanel is on mother’s left, with the sagittal suture in transverse pelvic diameter, it is left 41 | P a g e frontum transverse position. In late labor, the landmarks may be obscured by caput formation. Sonography is confirmatory and also helps in excluding bony congenital malformation of the fetus. MECHANISM OF LABOR: Diameter of engagement is through the oblique diameter with the brow anterior or posterior. As the engaging diameter of the head is mentovertical (14 cm), there is no mechanism of labor in an average size baby with normal pelvis. However, if the baby is small and the pelvis is roomy with good uterine contractions, delivery can occur in mentoanterior brow position. The brow descends until it touches the pelvic floor. Internal rotation and descent occur till the root of the nose hinges under the symphysis pubis. The brow and the vertex are delivered by flexion followed by extension to deliver the face. The mechanism is more or less the same as face-to-pubis delivery. Usual restitution and external rotation occur. There is no mechanism in posterior brow position. TRIAL OF LABOR: Brow presentation when transitory, trial of labor may be permissible. Correction of brow with felexion to occiput presentation or complete extension to a face presentation occurs. In such a situation, though rare, trial of labor may be possible. COURSE AND PROGNOSIS: In case of persistent brow presentation, there is a chance of obstructed labor. It is an important cause of rupture of uterus in multiparae. On occasion (10%), there may be spontaneous conversion of brow into face or vertex presentation. MANAGEMENT During pregnancy: If the presentation is diagnosed during pregnancy and there is no other contraindications for vaginal delivery, nothing is to be done. Contracted pelvis and congenital malformation of the fetus are to be excluded. Spontaneous correction into face is likely to occur. Elective cesarean section: Cases with persistent brow presentation are delivered by elective cesarean section. During labor: (1) In uncomplicated cases, if spontaneous correction to either vertex or face fails to occur early in labor, cesarean section is the best method of treatment. (2) Manual Correction to face with full dilatation of cervix is seldom practiced nowadays. (3) Craniotomy—If the labor becomes obstructed and the baby is dead, craniotomy is done. Rupture 42 | P a g e of the uterus should be excluded. 40. Transverse and oblique lies: etiology, varieties, mechanism of labour, diagnosis and prognosis for delivery. ETIOLOGY: The causes are—(1) Multiparity— lax and pendulous abdomen, imperfect uterine tone and extreme uterine obliquity are the responsible factors. (2) Prematurity—center of the gravity lies almost in the middle of the body. (3) Twins—it is more common for the second baby than the first one to be in transverse position. (4) Hydramnios. (5) Contracted pelvis. (6) Placenta previa. (7) Pelvic tumors. (8) Congenital malformation of the uterus—arcuate or subseptate and (9) Intrauterine death. ABDOMINAL EXAMINATION Inspection: The uterus looks broader and often asymmetrical, not maintaining the pyriform shape. Palpation: The fundal height is less than the period of amenorrhea. Fundalgrip—Fetalpole(breechorhead) is not palpable. Lateralgrip—(a)Soft,broadandirregular breech is felt to one side of the midline and smooth, hard and globular head is felt on the other side. The head is usually placed at a lower level on one iliac fossa. (b) The back is felt anteriorly across the long axis in dorsoanterior or the irregular small parts are felt anteriorly in dorsoposterior. Pelvicgrip—Thelowerpoleoftheuterus is found empty. This, however, is evident only during pregnancy but during labor, it may be occupied by the shoulder. Auscultation: FHS is heard easily much below the umbilicus in dorsoanterior position. FHS is, however, located at a higher level and often indistinct in dorsoposterior position. Ultrasonography or radiography confirms the diagnosis. VAGINAL EXAMINATION During pregnancy, the presenting part is so high that it cannot be identified properly but one can feel some soft parts. 43 | P a g e Management: ANTENATAL: External cephalic version should be done in all cases beyond 35 weeks provided there is no contraindication as mentioned in breech presentation (see p. 440). If the lie fails to stabilize even at 36th week, the case is to be managed as outlined in unstable lie. If version fails or is contraindicated: Thepatientistobeadmittedat37thweek,becauseriskofearlyruptureofthemembrane sand cord prolapse is very much there. Elective cesarean section is the preferred method of delivery. Vaginaldeliverymaybeallowedinadeadorcongenitallymalformed(smallsize)fetus.Th e labor may be allowed to continue under supervision till full dilatation of the cervix, when the baby can be delivered by internal version. LATE LABOR: Baby alive—There is hardly any scope of external version in late labor because of invariable rupture of the membranes and drainage of liquor. If the baby is mature and the fetal condition is good, it is preferable to do cesarean section in all cases. Internal version—In a singleton fetus, the risk of internal version is high. Not only it might inflict injury to the uterus (rupture uterus) but also the fetal mortality is increased to the extent of about 50%. In modern obstetric practice, internal version is not recommended except in the case of second twin. Babydead— Cesareansectioneveninsuchcases,ismuchsaferinthehandsofthosewhoare not conversant with destructive operations. Internal version should not be done. 41. Vomiting in pregnancy The vomiting is related to the pregnant state and depending upon the severity, it is classified as: (i) Simple vomiting of pregnancy or milder type (ii) Hyperemesis gravidarum or severe type. SIMPLE VOMITING (Syn: morning sickness, emesis gravidarum): The patient complains of nausea and occasional sickness on rising in the morning. Slight 44 | P a g e vomiting is so common in early pregnancy (about 50%) that it is considered as a symptom of pregnancy. It may, however, occur at other times of the day. The vomitus is small and clear or bile stained. It does not produce any impairment of health or restrict the normal activities of the women. The feature disappears with or without treatment by 12–14th week of pregnancy. High level of serum human chorionic gonadotropin, estrogen and altered immunological states are considered responsible for initiation of the manifestation, which is probably aggravated by the neurogenic factor. Management: Assurance is important. Taking of dry toast or biscuit and avoidance of fatty and spicy foods are enough to relieve the symptoms in majority. Supplementation with vitamin B1 100 mg daily is helpful. If the simple measures fail, antiemetic drugs — trifluoperazine (Espazine) 1 mg twice daily is quite effective. Promethazine and ondansetron can be used. Patient is advised to take plenty of fluids (2.5 L in 24 hours) and fruit juice. HYPEREMESIS GRAVIDARUM DEFINITION: It is a severe type of vomiting of pregnancy which has got deleterious effect on the health of mother and/or incapacitates her in day-to-day activities. The adverse effects of severe vomiting are—dehydration, metabolic acidosis (from starvation) or alkalosis (from loss of hydrochloric acid), electrolyte imbalance (hypokalemia) and weight loss. DIAGNOSIS: The pregnancy is to be confirmed first. Thereafter, all the associated causes of vomiting (enumerated before) are to be excluded. Ultrasonography is useful not only to confirm the pregnancy but also to exclude other, obstetric (hydatidiform mole, multiple pregnancy), gynecological, surgical or medical causes of vomiting MANAGEMENT The principles in the management are: Maintenance of hydration To control vomiting To correct the fluids and electrolytes imbalance To correct metabolic disturbances (acidosis or alkalosis) To prevent the serious complications of severe vomiting Care of pregnancy. Hospitalization: Whenever a patient is diagnosed as a case of hyperemesis gravidarum, she is admitted. Surprisingly, with the same diet and drugs used at 45 | P a g e home, the patient improves rapidly. The relatives may be too sympathetic or too indifferent. Drugs : 1) Antiemetic Drugs - Promethazine 25mg Metoclopramide 2)Hydrocortisone 100 mg IV drip 3) Nutritional supplementation 42. Hypertensive disorders 43. Preeclampsia DEFINITION: Preeclampsia is a multisystem disorder of unknown etiology characterized by development of hypertension to the extent of 140/90 mm Hg or 46 | P a g e more with proteinuria after the 20th week in a previously normotensive and nonproteinuric woman. SYMPTOMS: Preeclampsia is principally a syndrome of signs and when symptoms appear, it is usually late. Mild symptoms: Slight swelling over the ankles which persists on rising from the bed in the morning or tightness of the ring on the finger is the early manifestation of edema due to preeclampsia. Gradually, the swelling may extend to the face, abdominal wall, vulva and even the whole body Alarming symptoms: The following are the ominous symptoms, which may be evident either singly or in combination. These are usually associated with acute onset of the syndrome. (1) Headache — either located over the occipital or frontal region, (2) Disturbed sleep, (3) Diminished urinary output— Urinary output of less than 400 mL in 24 hours is very ominous, (4) Epigastric pain—acute pain in the epigastric region associated with vomiting, at times coffee color, is due to 47 | P a g e hemorrhagic gastritis or due to subcapsular hemorrhage in the liver, (5) Eye symptoms—there may be blurring, scotomata, dimness of vision or at times complete blindness. Vision is usually regained within 4–6 weeks following delivery. The eye symptoms are due to spasm of retinal vessels (retinal infarction), occipital lobe damage (vasogenic edema) or retinal detachment. Reattachment of the retina occurs following subsidence of edema and normalization of blood pressure after delivery. HOSPITAL MANAGEMENT Rest: Admission in hospital and rest is helpful for continued evaluation and treatment of the patient. While in bed patient should be in left-lateral position as much as possible, to lessen the effects of vena caval compression. Rest — (1) increases renal blood flow → diuresis, (2) increases uterine blood flow → improves placental perfusion, and (3) reduces the blood pressure. However completed bed rest is not essential. Diet: The diet should contain adequate amount of daily protein (about 100 g). Usual salt intake is permitted. Fluids need not be restricted. Total calorie approximate 1,600 cal/day. Diuretics: The diuretics should not be used injudiciously, as they cause harm to the baby by diminishing placental perfusion and by electrolyte imbalance. The compelling reasons for its use are—(1) Cardiac failure, (2) Pulmonary edema, (3) Along with selective antihypertensive drug therapy (diazoxide group) where blood pressure reduction is associated with fluid retention, (4) Massive edema, not relieved by rest and producing discomfort to the patient. The most potent diuretic commonly used is furosemide (Lasix) 40 mg, given orally after breakfast for 5 days in a week. 48 | P a g e 44. Spontancous abortion: definition, classification, common causes, mechanism and stages, misscd abortion, septic abortion, management. DEFINITION: Abortion is the expulsion or extraction from its mother of an embryo or fetus weighing 500 g or less when it is not capable of independent survival. The etiology of miscarriage is often complex and obscure. The following factors (embryonic or parental) are important: Genetic Endocrine and metabolic Anatomic Infection Immunological Thrombophilias Environmental Others Unexplained MECHANISM OF MISCARRIAGE: In the early weeks, death of the ovum occurs first, followed by its expulsion. In the later weeks, maternal environmental factors are involved leading to expulsion of the fetus which may have signs of life but is too small to survive. Before 8 weeks: The ovum, surrounded by the villi with the decidual coverings, is expelled out intact. Sometimes, the external os fails to dilate so that the entire mass is accommodated in the dilated cervical canal and is called cervical miscarriage. 49 | P a g e Between 8 weeks and 14 weeks: Expulsion of the fetus commonly occurs leaving behind the placenta and the membranes. A part of it may be partially separated with brisk hemorrhage or remains totally attached to the uterine wall. Beyond 14th week: The process of expulsion is similar to that of a “mini labor”. The fetus is expelled first followed by expulsion of the placenta after a varying interval. COMMON CAUSES OF MISCARRIAGE: First trimester: (1) Genetic factors (50%). (2) Endocrine disorders (LPD, thyroid abnormalities, diabetes). (3) Immunological disorders (autoimmune and alloimmune). (4) Infection. (5) Unexplained. Second trimester: (1) Anatomic abnormalities—(a) Cervical incompetence (congenital or acquired). (b) Müllerian fusion defects (bicornuate uterus, septate uterus). (c) Uterine synechiae. (d) Uterine fibroid. (2) Maternal medical illness. (3) Unexplained. MISSED MISCARRIAGE DEFINITION: When the fetus is dead and retained inside the uterus for a variable period, it is called missed miscarriage or early fetal demise. SEPTIC ABORTION DEFINITION: Any abortion associated with clinical evidences of infection of the uterus and its contents is called septic abortion. Although clinical criteria vary, abortion is usually considered septic when there are: (1) rise of temperature of at least 100.4°F (38°C) for 24 hours or more, (2) offensive or purulent vaginal discharge and (3) other evidences of pelvic infection such as lower abdominal pain and tenderness. GENERAL MANAGEMENT: Hospitalization is essential for all cases of septic abortion. The patient is kept in isolation. To take high vaginal or cervical swab for culture, drug sensitivity test and Gram stain. Vaginal examination is done to note the state of the abortion process and extension of the infection. 50 | P a g e Overall assessment of the case and the patient is leveled in accordance with the clinical grading. Investigation protocols as outlined before are done. Principles of management are: (a) To control sepsis. (b) To remove the source of infection. (c) To give supportive therapy to bring back the normal homeostatic and cellular metabolism. (d) To assess the response of treatment. 45. Recurrent miscarriage: definition, etiology, investigation, management. RECURRENT MISCARRIAGE DEFINITION: Recurrent miscarriage is defined as a sequence of three or more consecutive spontaneous abortion before 20 weeks. Some, however, consider two or more as a standard. It may be primary or secondary (having previous viable birth). A woman procuring three consecutive induced abortions is not a habitual aborter. 51 | P a g e INVESTIGATIONS FOR RECURRENT MISCARRIAGE A thorough medical, surgical and obstetric history with meticulous clinical examination should be carried out to find out the possible cause or causes as mentioned previously. Careful history taking should include—(i) The nature of previous abortion process. (ii) Histology of the placenta or karyotyping of the conceptus, if available. (iii) Any chronic illness. Diagnostic tests: (1) Blood-glucose (fasting and postprandial), VDRL, thyroid function test, ABO and Rh grouping (husband and wife), toxoplasma antibodies IgG and IgM. (2) Autoimmune screening—lupus anticoagulant and anticardiolipin antibodies (3) Serum LH on D2/D3 of the cycle. (4) Ultrasonography—to detect congenital malformation of uterus, polycystic ovaries and uterine fibroid. (5) Hysterosalpingography in the secretory phase to detect—cervical incompetence, uterine synechiae and uterine malformation. (6) This is supported by 52 | P a g e hysteroscopy and/or laparoscopy. (7) Karyotyping (husband and wife). (8) Endocervical swab to detect chlamydia, mycoplasma and bacterial vaginosis. 46. Antepartum haemorrage: etiological classification. DEFINITION: It is defined as bleeding from or into the genital tract after the 28th week of pregnancy but before the birth of the baby (the first and second stage of labor are thus included). The 28th week is taken arbitrarily as the lower limit of fetal viability. The incidence is about 3% amongst hospital deliveries. 47. Placenta praevia: definition, etiology, types, differential diagnosis, management at different stages of pregnancy prog1nosis for delivery. PLACENTA PREVIA DEFINITION: When the placenta is implanted partially or completely over the lower uterine segment (over and adjacent to the internal os) it is called placenta previa. Etiology: Dropping down theory: The fertilized ovum drops down and is implanted in the lower segment. Poor decidual reaction in the upper uterine segment may be the cause. Failure of zona pellucida to disappear in time can be a hypothetical possibility. This explains the formation of central placenta previa. 53 | P a g e Persistence of chorionic activity in the decidua capsularis and its subsequent development into capsular placenta which comes in contact with decidua vera of the lower segment can explain the formation of lesser degrees of placenta previa. Defective decidua, results in spreading of the chorionic villi over a wide area in the uterine wall to get nourishment. During this process, not only the placenta becomes membranous but encroaches onto the lower segment. Such a placenta previa may invade the underlying decidua or myometrium to cause placenta accreta, increta or percreta. DIFFERENTIAL DIAGNOSIS Placenta previa is at times confused with other causes of bleeding occurring in later months of pregnancy. The most common one from which it has to be differentiated is bleeding from premature separation of a normally situated placenta (abruptio placentae). The local cervical lesions (polyps, carcinoma) can easily be differentiated by a speculum examination. However, both the conditions can co-exist. Management: AT HOME: (1) The patient is immediately put to bed. (2) To assess the blood loss—(a) inspection of the clothing soaked with blood (b) to note the pulse, blood pressure and degree of anemia (3) Quick but gentle abdominal examination to mark the height of the uterus, to auscultate the fetal heart sound and to note any tenderness on the uterus (4) Vaginal examination must not be done. Only inspection is done to see whether the bleeding is present or absent and to put a sterile vulval pad. TRANSFER TO HOSPITAL: Arrangement is made to shift the patient to an equipped hospital having facilities of blood transfusion, emergency cesarean section and neonatal intensive care unit (NICU). ‘Flying Squad ’service is ideal for transfer of such type of patients. An intravenous Ringer’s solution drip should be started and is kept running during transport. Patient should be accompanied by two or three persons fit for donation of blood, if necessary. ADMISSION TO HOSPITAL: All cases of APH, even if the bleeding is slight or absent by the time the patient reaches the hospital, should be admitted. The reasons are: (1) All the cases of APH should be regarded as due to placenta previa unless proved otherwise. (2) The bleeding may recur sooner or later and none can predict when it recurs and how much she will bleed. 54 | P a g e 48. Abruptio placentae: definition, etiology, types, differential diagnosisS, management at different stages of pregnancy prognosis for delivery. ABRUPTIO PLACENTAE (Syn: Accidental Hemorrhage. Premature Separation of Placenta) DEFINITION: It is one form of antepartum hemorrhage where the bleeding occurs due to premature separation of normally situated placenta. Types: 1) Revealed : Following separation of the placenta, the blood insinuates downwards between the membranes and the decidua. Ultimately, the blood comes out of the cervical canal to be visible externally. This is the most common type. 2) Concealed : The blood collects behind the separated placenta or collected in between the membranes and decidua. The collected blood is prevented from coming out of the cervix by the presenting part which presses on the lower segment. 3) Mixed : In this type, some part of the blood collects inside (concealed) and a part is expelled out (revealed). Usually one variety predominates over the other. This is quite common. DIFFERENTIAL DIAGNOSIS: (a) Revealed type: There may be occasional diagnostic difficulty with placenta previa. The differentiating points have been given previously in tabulated form (Table 19.1). Confusion with the indeterminate causes of APH is difficult to eliminate (b) Mixed or concealed type: This variety is often confused with — (i) rupture uterus (ii) rectus sheath hematoma (iii) appendicular or intestinal perforation (iv) twisted ovarian tumor (v) volvulus (vi) acute hydramnios (vii) tonic uterine contraction. MANAGEMENT OF ABRUPTIO PLACENTAE 55 | P a g e Early detection and effective therapy of preeclampsia and other hypertensive disorders of pregnancy. Needle puncture during amniocentesis should be under ultrasound guidance. Avoidance of trauma—specially forceful external cephalic version under anesthesia. To avoid sudden decompression of the uterus— in acute or chronic hydramnios, amniocentesis is preferable to artificial rupture of the membranes. To avoid supine hypotension the patient is advised to lie in the left lateral position in the later months of pregnancy. Routine administration of folic acid from the early pregnancy — of doubtful value. 56 | P a g e 49. Postpartum haemoIrage: ctiological classification. ♦ Atonic ♦ Traumatic ♦ Retained tissues ♦ Blood coagulopathy (Thrombin) ♦ Atonic uterus (80%): Atonicity of the uterus is the commonest cause of postpartum hemorrhage. With the separation of the placenta, the uterine sinuses, which are torn, cannot be compressed effectively due to imperfect contraction and retraction of the uterine musculature and bleeding continues. The following are the conditions, which often interfere with the retraction of the uterus as a whole and of the placental site in particular. — Grand multipara—Inadequate retraction and frequent adherent placenta contribute to it. Associated anemia may also probably play a role. — Overdistension of the uterus as in multiple pregnancy, hydramnios and big baby (>4 kg). Imperfect retraction and a large placental site are responsible for excessive bleeding. — Malnutritionandanemia(<9.0g/dL)— Evenslightamountofbloodlossmaydevelopclinical manifestations of postpartum hemorrhage. — Antepartum hemorrhage (Both placenta previa and abruption): The causes of excessive bleeding are mentioned in Chapter 19 p. 282. — Prolongedlabor(>12hours):Poorretraction,infection(amnionitis),dehydrationareim portant factors (Tone). — Anesthesia:Depthofanesthesiaandtheanestheticagents(ether,halothane)maycaus eatonicity. — Initiation or augmentation of delivery by oxytocin:Post delivery uterine atonicity is likely unless the oxytocin is continued for at least one hour following delivery. — Malformation of the uterus: Implantation of the placenta in the uterine septum of a septate uterus or in the cornual region of a bicornuate uterus may cause excessive bleeding. — Uterine fibroid causes imperfect retraction mechanically. — Mismanaged third stage of labor:This includes—(a)Too rapid delivery of the baby preventing the uterine wall to adapt to the diminishing contents, (b) 57 | P a g e Premature attempt to deliver the placenta before it is separated, (c) Kneading and fiddling the uterus, (d) Pulling the cord. All these produce irregular uterine contractions leading to partial separation of placenta and hemorrhage, (e) Manual separation of the placenta increases blood loss during cesarean delivery. — Placenta:Morbidly adherent(accreta,percreta),partially or completely separated and/orretained (constriction ring uterus) cause PPH. — Precipitate labor:In rapid delivery,separation of the placenta occurs following the birth of the baby. Bleeding continues before the onset of uterine retraction. Bleeding may be due to genital tract trauma also (see p. 420). — Other causes of atonic hemorrhage are: t Obesity (BMI > 35) t Previous PPH t Age (>40 yrs) t Drugs: Use of tocolytic drugs (ritodrine), MgSO4, Nifedipine. — Traumatic(20%):Trauma to the genital tract usually occurs following operative delivery;even after spontaneous delivery. Blood loss from the episiotomy wound is often underestimated. Similarly, blood loss in cesarean section amounting to 800–1000 mL is most often ignored. Trauma involves usually the cervix, vagina, perineum (episiotomy wound and lacerations), paraurethral region and rarely, rupture of the uterus occurs. The bleeding is usually revealed but can rarely be concealed (vulvovaginal or broad ligament hematoma). Retained tissues: Bits of placenta, blood clots cause PPH due to imperfect uterine retraction. Combination of atonic and traumatic causes. Thrombin: Blood coagulation disorders, acquired or congenital, are less common causes of postpartum hemorrhage. The blood coagulopathy may be due to diminished procoagulants (washout phenomenon) or increased fibrinolytic activity. The firmly retracted uterus can usually prevent bleeding. The conditions where such disorders may occur are abruptio placentae, jaundice in pregnancy, thrombocytopenic purpura, severe preeclampsia, HELLP syndrome or in IUD. Specific therapy following coagulation screen including recombinant activated factor VII (rF VIIa) may be given. 50. Atonic postpartum haemorrage: etiology, diagnosis and management. Etiology - Above question Diagnosis : In atonic hemorrhage, the uterus is found flabby and becomes hard on massaging. However, both the atonic and traumatic cause may coexist. Even 58 | P a g e following massive blood loss from the injured area, a state of low general condition can make the uterus atonic. The effect of blood loss depends on—(a) Predelivery hemoglobin level, (b) degree of pregnancy induced hypervolemia and (c) speed at which blood loss occurs. Alteration of pulse, blood pressure and pulse pressure appears only after class 2 hemorrhage (20–25% loss of blood volume). On occasion, blood loss is so rapid and brisk that death may occur within a few minutes. 59 | P a g e 51. Retaincd and morbid adherent placenta as causes of postpartum haemorrhages, their types, diagnosis and management. DEFINITION: The placenta is said to be retained when it is not expelled out even 30 minutes after the birth of the baby (WHO 15 minutes). CAUSES: There are three phases involved in the normal expulsion of placenta: (1) Separation through the spongy layer of the decidua, (2) Descent into the lower segment and vagina, (3) Finally its expulsion to outside. Interference in any of these physiological processes, results in its retention. — Placenta completely separated but retained is due to poor voluntary expulsive efforts. — Simpleadherentplacentaisduetouterineatonicityincasesofgrandmultipara,overdist ension 60 | P a g e of uterus, prolonged labor and uterine malformation or due to bigger placental surface area. The commonest cause of retention of non-separated placenta is atonic uterus. — Morbid adherent placenta—partial or rarely, complete. — Placentaincarceratedfollowingpartialorcompleteseparationduetoconstrictionring( hour- glass contraction), premature attempts to deliver the placenta before it is separated. DIAGNOSIS: The diagnosis of retained placenta is made by an arbitrary time (15 minutes) spent following delivery of the baby. Features of placental separation are assessed. The hour- glass contraction or the nature of adherent placenta (simple or morbid) can only be diagnosed during manual removal. Management PERIOD OF WATCHFUL EXPECTANCY — Duringtheperiodofarbitrarytimelimitofhalfanhour,thepatientistobewatchedcarefu llyfor evidence of any bleeding, revealed or concealed and to note the signs of separation of placenta. — The bladder should be emptied using a rubber catheter. — Any bleeding during the period should be managed as outlined in third stage bleeding. RETAINED PLACENTA: t Separated t Unseparated t Complicated Placenta is separated and retained—To express the placenta out by controlled cord traction. Unseparated retained placenta (apparently uncomplicated): Manual removal of placenta is to be done under general anesthesia as described earlier. PLACENTA ACCRETA (Syn: Morbid adherent placenta) Placenta accreta is an extremely rare form in which the placenta is directly anchored to the myometrium partially or completely without any intervening decidua. The diagnosis is made only during attempted manual removal when the plane of cleavage between the placenta and the uterine wall cannot be made out. Ultrasound imaging, color Doppler and MRI have all been valuable in the diagnosis of placenta accreta, increta and percreta during pregnancy. 61 | P a g e MANAGEMENT: t Multidisciplinary team approach in management is to be done. In partial placenta accreta (focal) → Remove the placental tissue as much as possible. Effective uterine contraction and hemostasis are achieved by oxytocic and if necessary by intrauterine plugging. In cases following cesarean delivery bleeding areas are oversewed. If the uterus fails to contract, an early decision of hysterectomy may have to be taken and this is preferable in multiparous women. t In total placenta accreta, hysterectomy is indicated in parous women, while in patients desiring to have a child, conservative attitude may be taken. This consists of incising the uterus above the placental attachment and clamping and cutting the umbilical cord as close to its base as possible and leaving behind the placenta, which is expected to be autolyzed in due course of time. Appropriate antibiotics should be given. Any attempt of placental separation risks massive hemorrhage and ends in hysterectomy in 100% of cases. Uterine artery embolization or therapy with methotrexate has been done for conservation of the uterus. t In a rare case, placenta accreta may invade the bladder. In that case, try to avoid placental removal. It may need hysterectomy and partial cystectomy. 52. Manual removal of placentae: indications, prerequisites, procedure. Step–I: The operation is done under general anesthesia. In extreme urgency where anesthetist is not available, the operation may have to be done under deep sedation with 10 mg diazepam given intravenously. The patient is placed in lithotomy position. With all aseptic measures, the bladder is catheterized. Step–II: One hand is introduced into the uterus after smearing with the antiseptic solution in cone shaped manner following the cord, which is made taut by the other hand (Fig. 28.1). While introducing the hand, the labia are separated by the fingers of the other hand. The fingers of the uterine hand should locate the margin of the placenta. Step–III: Counter pressure on the uterine fundus is applied by the other hand placed over the abdomen. The abdominal hand should steady the fundus and guide the movements of the fingers inside the uterine cavity until the placenta is completely separated. 62 | P a g e Step–IV: As soon as the placental margin is reached, the fingers are insinuated between the placenta and the uterine wall with the back of the hand in contact with the uterine wall. The placenta is gradually separated with a sideways slicing movement of the fingers, until whole of the placenta is separated. Step–V: When the placenta is completely separated, it is extracted by traction of the cord by the other hand. The uterine hand is still inside the uterus for exploration of the cavity to be sure that nothing is left behind. Step–VI: Intravenous methergine 0.2 mg is given and the uterine hand is gradually removed while massaging the uterus by the external hand to make it hard. After the completion of manual removal, inspection of the cervicovaginal canal is to be made to exclude any injury. Introduction of the hand into the uterus in a cone shaped manner following the taut umbilical cord. The placenta is separated by (A) keeping the back of the hand in contact with the uterine wall with slicing movements of the hand Step–VII: The placenta and membranes are inspected for completeness and be sure that the uterus remains hard and contracted. Difficulties: (1) Hour-glass contraction leading to difficulty in introducing the hand, (2) Morbid adherent placenta which may cause difficulty in getting to the plane of cleavage of placental separation. In such a case placenta is removed gently in fragments using an ovum forceps. Complications: (1) Hemorrhage due to incomplete removal, (2) Shock, (3) Injury to the uterus, (4) Infection, (5) Inversion (rare), (6) Subinvolution, (7) Thrombophlebitis, (8) Embolism. In such cases placenta is removed in fragments using an ovum forceps or a flushing curette. 53. Contracted pelvis in obstetrics: parent pelvic types and their obstetrie 63 | P a g e outcomes. 64 | P a g e 54. Contracted pclvis in obstetrics: etiology, types of contacted pelvis and their obstetric outcomes, diagnosis, mechanism of labour. prognosis for vaginal delivery. ETIOLOGY OF CONTRACTED PELVIS: Gross degree of contracted pelvis is nowadays a rarity. Severe malnutrition, rickets, osteomalacia and bone tuberculosis affecting grossly the pelvic architecture are now rarely met in clinical practice. Instead, minor variation in size and/or shape of the pelvis is commonly found which is often overlooked until complication arises. Common causes of contracted pelvis are: (1) Nutritional and environmental defects — Minor variation: Common Major: Rachitic and osteomalacic — rare (2) Diseases or injuries affecting the bones of the pelvis — fracture, tumors, tubercular arthritis; spine — kyphosis, scoliosis, spondylolisthesis, coccygeal deformity; lower limbs — poliomyelitis, hip joint disease. (3) Development defects — Naegele’s pelvis, Robert’s pelvis; high or low assimilation pelvis. FLAT PELVIS (Figs 24.5A to C) In the flat pelvis, the head finds difficulty in negotiating the brim and once it passes through the brim, there is no difficulty in the cavity or outlet. The head negotiates the brim by the following mechanism: The head engages with the sagittal suture in the transverse diameter. Head remains deflexed and engagement is delayed. If the anteroposterior diameter is too short, the occiput is mobilized to the same side to occupy the sacral bay. The biparietal diameter is thus placed in the sacrocotyloid diameter (9.5 cm or 8.5 cm) and the narrow bitemporal diameter is placed in the narrow conjugate. If lateral mobilization is not possible, there is a chance of extension of the head leading to brow or face presentation. Engagementoccursbyexaggeratedparietalpresentationsothatthesupersubparietaldiameter (8.5 cm), instead of the biparietal diameter (9.5 cm), passes through the pelvic brim. Molding may be extreme and often there is an indentation or even a fracture of one parietal bone. However, the caput that forms is not big. Once the head negotiates the brim, there is no difficulty in the cavity and outlet and normal mechanism follows. 65 | P a g e GENERALLY CONTRACTED PELVIS: In this type of pelvis the shape remains unaltered, but all the diameters in the different planes—inlet, cavity and outlet— are shortened. There is difficulty from the beginning to the end. 55. Cephalopelvie disproportion: definition, diagnosis, trial labour. DEFINITION: Disproportion, in relation to the pelvis, is a state where the normal proportion between the size of fetus to the size of the pelvis is disturbed. The disparity in the relation between the head and the pelvis is called cephalopelvic disproportion. DIAGNOSIS OF CEPHALOPELVIC DISPROPORTION (CPD) AT THE BRIM The presence and degree of cephalopelvic disproportion at the brim can be ascertained by the following: Clinical — (a) Abdominal method; (b) Abdominovaginal (Muller-Munro Kerr) Imaging pelvimetry (see above) Cephalometry — (a) Ultrasound; (b) Magnetic Resonance Imaging; (c) X-ray Abdominovaginal method (Muller-Munro Kerr): This bimanual method is superior to the abdominal method as the pelvic assessment can be done simultaneously. Muller introduced the method by placing the vaginal finger tips at the level of ischial spines to note the descent of the head. Munro Kerr added placement of the thumb over the symphysis pubis to note the degree of overlapping. 66 | P a g e TRIAL LABOR Definition: It is the conduction of spontaneous labor in a moderate degree of cephalopelvic disproportion, in an institution under supervision with watchful expectancy, hoping for a vaginal delivery. Every arrangement should be made available for operative delivery, either vaginal or abdominal, if the condition so arises. Aims: A trial labor aims at avoiding an unnecessary cesarean section and at delivering a healthy baby. The phrase “trial” was used originally to test for pelvic adequacy but subsequently its use has been extended to test numerous factors other than the pelvic capacity. For example, the trial is conducted to test the integrity of the scar in a woman with prior cesarean delivery when she goes into labor. 56. Cesarean section: its place and trends in modern obstetries, indications, contraindications, types and complications. 67 | P a g e DEFINITION: It is an operative procedure whereby the fetuses after the end of 28th weeks are delivered through an incision on the abdominal and uterine walls. TYPES OF OPERATIONS: Lower segment Classical or upper segment Lower segment cesarean section (LSCS): In this operation, the extraction of the baby is done through an incision made in the lower segment through a transperitoneal approach. It is the only method practiced in present day obstetrics and unless specified, cesarean section means lower segment operation. The operation done through an extraperitoneal approach to the lower segment in infected cases is obsolete. Classical: In this operation, the baby is extracted through an incision made in the upper segment of the uterus. Its indications in present day obstetrics are very much limited and the operation is only done under forced circumstances such as: Lowersegmentapproachisdifficult:(1)Denseadhesionsduetopreviousabdominalope ration (2) severe contracted pelvis (osteomalacic or rachitic) with pendulous abdomen. 68 | P a g e Lower segment approach is risky: (1) Big fibroid on the lower segment—blood loss is more and contemplating myomectomy may end in hysterectomy (2) carcinoma cervix—to prevent dissemination of the growth and postoperative sepsis (3) repair of high VVF (4) complete anterior placenta previa with engorged vessels in the lower segment—risk of hemorrhage. Perimortem cesarean section: It is done to have alive baby(rare). Perimortem section is an extreme emergency procedure. Classical section is done in a woman who has suffered a cardiac arrest. The infant may survive if delivery is done within 10 minutes of maternal death. 57. Operative vaginal delivery. Obstetric forceps: varieties, indications, prerequisites, low forceps operation, dangers and complications. 69 | P a g e Operative vaginal delivery refers to any delivery process which is assisted by vaginal operations. Delivery by forceps, ventouse and destructive operations are generally included. FORCEPS Obstetric forceps is a pair of instruments, especially designed to assist extraction of the fetal head and thereby accomplishing delivery of the fetus. VARIETIES OF OBSTETRIC FORCEPS: Ever since either Peter I or Peter II of the Chamberlen family invented the forceps around AD 1600, more than 700 varieties were invented or modified. Most of them are of historical interest only. But only three varieties are commonly used in present day obstetric practice (Figs 37.7A to D). These are: Long-curved forceps with or without axis-traction device Short-curved forceps Kielland’s forceps The basic construction of these forceps is the same in that each consists of two halves (blades) articulated by a lock. Low forceps operation STEPS: The operation consists of the following steps: Identification of the blades and their application 70 | P a g e Locking of the blades Traction Removal of the blades 58. Operative vaginal delivery. Ventouse: indications, prerequisites, procedure, dangers and complications. 71 | P a g e Ventouse is an instrumental device designed to assist delivery by creating a vacuum between it and the fetal scalp. The pulling force is dragging the cranium while in forceps, the pulling force is directly transmitted to the base of the skull. Procedure : Step I: Application of the cup: The largest possible cup is to be selected. The cup is introduced after retraction of the perineum with two fingers of the other hand. The cup is placed against the fetal head nearer the occiput (flexion point) with the “knob” of the cup pointing towards the occiput. Traction over this flexion point either by ventouse or forceps facilitates flexion and presents the smaller diameter to the pelvis The pressure is gradually raised at the rate of 0.1 kg/cm2 per minute until the effective vacuum of 0.8 kg/cm2 is achieved in about 10 minutes time. The scalp is sucked into the cup and an artificial caput succedaneum (chignon) is produced. The chignon usually disappears within few hours. 72 | P a g e Step II: Traction Traction must be at right angle to the cup Traction should be synchronous with the uterine contractions Traction is released in between uterine contractions Traction should be made using one hand along the axis of the birth canal. The fingers of the other hand are to be placed against the cup to note the correct angle of traction, rotation and advancement of the head Operative vaginal delivery(forceps ventouse) should be abandoned, where there is nodescent of the presenting part with each pull or when delivery is not imminent after three pulls with correctly applied instruments by an experienced operator. On no account, traction should exceed 30 minutes. COMPLICATIONS: Neonate: (1) Superficial scalp abrasion (2) sloughing of the scalp and (3) cephalhematoma—due to rupture of emissary veins beneath the periosteum. Usually it resolves by one or two weeks (4) subaponeurotic (subgaleal) hemorrhage (not limited by suture line as it is not subperiosteal) (5) intracranial hemorrhage (rare) (6) retinal hemorrhage (no long-term effect) and (7) jaundice. Maternal: The injuries are uncommon but may be due to inclusion of the soft tissues such as the cervix or vaginal wall inside the cup. However, failure rate is high. The sequential use of ventouse and forceps increases the risk of trauma both to the mother and the neonate. Outlet forceps may be used following failure of ventouse. 59. Destructive operations: types indications and procedures. The destructive operations are designed to diminish the bulk of the fetus so as to facilitate easy delivery through the birth canal. In modern obstetric practice, virtually there is hardly any place for destructive operations. Some commonly performed operations are discussed here. There are four types of operations: Craniotomy Evisceration Decapitation Cleidotomy 73 | P a g e CRANIOTOMY DEFINITION: It is an operation to make a perforation on the fetal head, to evacuate the contents followed by extraction of the fetus. INDICATIONS: Cephalicpresentationproducingobstructedlaborwithdeadfetus:Thisisthemostcom mon indication of craniotomy in the referral hospitals of the developing countries. Hydrocephaluseveninalivingfetus:Thisisapplicablebothfortheforecomingandtheaft er- coming head (see p. 470). Interlocking head of twins. PROCEDURES: Preliminaries: The preliminary preparations are the same as mentioned in p. 642. The operation is to be done under general anesthesia. Actual steps Step I: The two fingers (index and middle) are introduced into the vagina and the finger tips are to be placed on proposed site of perforation. However, when the suture line cannot be defined because of big caput, the perforation should be done through the dependent part. Sites of perforation: Vertex: On the parietal bone either side of the sagittal suture. Suture is avoided to prevent collapse of the bone thereby preventing escape of the brain matter. Face:Through the orbit or hard palate. Brow: Through the frontal bone. Step II: The Oldham’s perforator with the blades closed is introduced under the palmar aspect of the fingers protecting the anterior vaginal wall and the adjacent bladder (as shown in Figs 37.20A and B) until the tip reaches the proposed site of perforation. Step III: By rotating movements the skull is perforated. During this step, an assistant is asked to steady the head per abdomen in a manner of first pelvic grip. After the skull is perforated, the instrument is thrust up to the shoulders and the handles are approximated so as to allow separation of the sharp blades for about 2.5 cm. Alternative to Oldham’s perforator, similar procedure could be performed using a sharp-pointed Mayo’s scissors. 74 | P a g e Step IV: With the fingers brain matter is evacuated. The idea is to make the skull collapse as much as possible. Step V: When the skull is found sufficiently compressed, the extraction of the fetus is achieved either by using a cranioclast or by two giant volsella. Giant volsella are used to hold the incised skull and scalp margins. Step VI: The traction is now exerted in the same direction as like that mentioned in forceps operation. Step VII: After the delivery of the placenta, the uterovaginal canal must be explored as a routine for evidence of rupture uterus or any tear. DECAPITATION DEFINITION: It is a destructive operation whereby the fetal head is severed from the trunk and the delivery is completed with the extraction of the trunk and that of the decapitated head per vaginum. INDICATION: (1) Neglected shoulder presentation with dead fetus where neck is easily accessible. (2) Interlocking head of twins. PROCEDURES: Preliminaries — The preliminaries to be followed are the same as outlined earlier. The operation is done under general anesthesia. Actual Steps Step I: If the fetal hand is not prolapsed, bring down a hand. A roller gauze is tied on the fetal wrist and an assistant is asked to give traction towards the side away from the fetal head to make the neck more accessible and fixed. Step II: Two fingers of the left hand (middle and index) are introduced with the palmar surface downwards and the finger tips are to be placed on the superior surface of the neck—the proposed site of decapitation. Step III: The decapitation hook with knife is to be introduced flushed under the guidance of the fingers placed into the vagina, the knob pointing towards the fetal head. The hook is pushed above the neck and rotated to 90° so as to place the knife firmly against the neck. The internal fingers, in the meantime, are placed on the under surface of the neck to guard the tip of the hook. Step IV: By upward and downward movements of the hook with knife, the vertebral column is severed (evident by sudden loss of resistance). The rest of the soft tissue left behind may be severed by the same instrument or by embryotomy scissors. While removing the decapitation hook—it is to be pushed up; rotated to 75 | P a g e 90° and then to take out under the guidance of the internal fingers. The decapitated head is pushed up and the trunk is delivered by traction on the prolapsed arm. Step V: Delivery of the decapitated head—Any of the following methods may be usually effective: By hooking the index finger into the mouth By holding the severed neck with giant vulsellum (Fig. 42.33) and delivery of the head as that of aftercoming head in breech Using forceps. Step VI: Routine exploration of the uterovaginal canal to exclude rupture of the uterus or any other injury. EVISCERATION The operation consists of removal of thoracic and abdominal contents piecemeal through an opening on the thoracic or abdominal cavity at the most accessible site. The object is to diminish the bulk of the fetus which facilitates its extraction. If difficulty arises, the spine may have to be divided (spondylectomy) with embryotomy scissors. The indications are: (1) Neglected shoulder presentation with dead fetus; the neck is not easily accessible and (2) fetal malformations, such as fetal ascites or hugely distended bladder or monsters. CLEIDOTOMY The operation consists of reduction in the bulk of the shoulder girdle by division of one or both the clavicles. The operation is done only in dead fetus (anencephaly excluded) with shoulder dystocia. The clavicles are divided by the embryotomy scissors or long straight scissors introduced under the guidance of left two fingers placed inside the vagina. 60. Abnormal uterine action: definition, classification, etiology. Any deviation of the normal pattern of uterine contractions (as mentioned in page 138) affecting the course of labor is designated as disordered or abnormal uterine action. 76 | P a g e ETIOLOGY: As the physiology of normal uterine contraction is not fully understood, the cause of its disordered action remains obscure. However, the following clinical conditions are often associated: (1) Prevalent in first birth, especially with elderly women; (2) Prolonged pregnancy; (3) Overdistension of the uterus (twins and fibroids); (4) Emotional factor (anxiety, stress); (5) Constitutional factor (obesity); (6) Contracted pelvis and malpresentation; (7) Injudicious administration of sedatives, analgesics and oxytocics; (8) Premature attempt at vaginal delivery (induction of labor or ARM) or attempted instrumental vaginal delivery under light anesthesia. 77 | P a g e 61. Uterine inertia: clinical features. prognosis for mother, child and delivery. management. Uterine inertia is the common type of abnormal uterine contraction but is comparatively less serious. It may complicate any stage of labor. It may be present from the beginning of labor or may develop subsequently after a variable period of effective contractions. EFFECTS ON THE MOTHER AND FETUS: Maternal exhaustion and/or fetal distress are unusual and appear late. MANAGEMENT: Case is reassessed to exclude cephalopelvic disproportion or malpresentation. Place of cesarean section: (1) Presence of contracted pelvis (2) Malpresentation (3) Evidences of fetal or maternal distress. Vaginal delivery — (A) General measures: (1) To keep up the morale of the patient. Maternal stress, pain and anxiety appear to inhibit uterine contractions through release of endogenous catecholamines. (2) Posture of the woman is changed. Supine position is avoided. (3) To empty the bladder, catheterization is made. (4) To maintain hydration by infusion of Ringer’s solution. (5) Adequate pain relief. (B) Active measures: Acceleration of uterine contraction can be brought about by low rupture of the membranes followed by oxytocin drip. The drip rate is gradually increased until effective contractions are set up. The drip is to be continued till 1 hour after delivery. 78 | P a g e 62. Inco-ordinate uterine action: varieties, clinical features, prognosiS for mothe child and delivery, management. 63. Injures to the birth canal: vulval, perineal, vaginal, cervical, their etiology, diagnosis and management. Maternal injuries following childbirth process are quite common and contribute significantly to maternal morbidity and even to death. 79 | P a g e VULVA Lacerations of the vulval skin posteriorly and the paraurethral tear on the inner aspect of the labia minora are the common sites. Paraurethral tear may be associated with brisk hemorrhage and should be repaired by interrupted catgut sutures, preferably after introduction of a rubber catheter into the bladder to prevent injury of the urethra. PERINEUM While minor injury is quite common especially during first birth, gross injury (third and fourth degree) is invariably a result of mismanaged second stage of labor. Overall risk is 1% of all vaginal deliveries. CAUSES: Perineal injury (mainly the third and fourth degree) results from (i) over stretching and/ or (ii) rapid stretching of the perineum especially when the perineum is inelastic VAGINAL Isolated vaginal tears or lacerations without involvement of the perineum or cervix are not uncommon. These are usually seen following instrumental or 80 | P a g e manipulative delivery. In such cases, the tears are extensive and often associated with brisk hemorrhage. TREATMENT: Tears associated with brisk hemorrhage require exploration under general anesthesia with a good light. The tears are repaired by interrupted or continuous sutures using chromic catgut No. “0”. In case of extensive lacerations, in addition to sutures, hemostasis may be achieved by intravaginal plugging by roller gauze, soaked with glycerin and acriflavine. The plug should be removed after 24 hours. Selective arterial embolization may also be done if bleeding persists. CERVIX Minor degree of cervical tear is invariable during first delivery and requires no treatment. Extensive cervical tear is rare. It is the commonest cause of traumatic postpartum hemorrhage. Left lateral tear is the commonest. DIAGNOSIS: Excessive vaginal bleeding immediately following delivery in presence of a hard and contracted uterus—raises the suspicion of a traumatic bleeding. Exploration of the uterovaginal canal under good light not only confirms the diagnosis but also helps to know the extent of the tear. TREATMENT: Only deep cervical tear associated with bleeding should be repaired soon after delivery of the placenta. Repair should be done under general anesthesia, in lithotomy position with a good light. 64. Rupture of the uterus: etiology, pathology, diagnosis, prophylaxis, treatment. 81 | P a g e DEFINITION: Disruption in the continuity of the all uterine layers (endometrium, myometrium and serosa) any time beyond 28 weeks of pregnancy is called rupture of the uterus. 82 | P a g e PATHOLOGY TYPES: Pathologically, it is customary to distinguish between complete and incomplete rupture depending on whether the peritoneal coat is involved or not. So far from the treatment point of view, it matters little. In incomplete rupture, the peritoneum remains intact. Incomplete rupture usually results from rupture of the lower segment scar or extension of a cervical tear into the lower segment with formation of a broad ligament hematoma. Complete rupture usually occurs following disruption of the scar in upper segment. It may also be due to spontaneous rupture of both obstructive and nonobstructive type. FETUS AND PLACENTA: In incomplete rupture, both the fetus and placenta remain inside the uterine cavity or part of the fetus may occupy in between the layers of broad ligament. In complete rupture, the fetus with or without the placenta usually escapes out of the uterus. The uterus remains contracted. Blood loss is not much unless major vessels are affected. 83 | P a g e PROPHYLAXIS: The following guidelines are helpful to prevent or to detect at the earliest the tragic occurrence of rupture uterus: The at-risk mothers, likely to rupture, should have mandatory hospital delivery. These are— (a) Contracted pelvis. (b) Previous history of cesarean section, hysterotomy or myomectomy. (c) Uncorrected transverse lie. (d) Grand multiparity. (e) Known case of hydrocephalus. General anesthesia should not be used to give undue force in external version. Undue delay in the progress of labor in a multipara with previous uneventful delivery should be viewed with concern and the cause should be sought for. Judicious selection of cases with previous history of cesarean sections for vaginal delivery (VBAC) Judicious selection of cases and careful watch are mandatory during oxytocin infusion either for induction or augmentation of labor. There is hardly any place of internal podalic version in singleton fetus in present day obstetrics. It should never be done in obstructed labor as an alternative to destructive operation or cesarean delivery. Attempted forceps delivery or breech extraction through incompletely dilated cervix should be avoided. Destructive vaginal operations should be performed by skilled personnel and exploration of the uterus should be done as a routine following delivery. 84 | P a g e Manual removal in morbid adherent placenta—should be done by a senior person. TREATMENT: Resuscitation Laparotomy Depending upon the state of the clinical condition, either resuscitation is to be done followed by laparotomy or in acute conditions, resuscitation and laparotomy are to be done simultaneously. 65. Birth injures to the newborn (head, bones etc.): classification, etiology and predisposing factors. treatment. Birth injuries is an impairment of the infant’s body function or structure due to adverse influences that occurred at birth. Injury commonly occurs during labor or 85 | P a g e delivery. Birth injuries may be severe enough to cause neonatal deaths, still births or number of morbidities. 86 | P a g e 66. Abnormal puerperium: varictics, clinical features, diagnosis and management. Varieties : 1) Puerperal pyrexia 2) Puerperal Sepsis PUERPERAL PYREXIA DEFINITION: A rise of temperature reaching 100.4°F (38°C) or more (measured orally) on two separate occasions at 24 hours apart (excluding first 24 hours) within first 10 days following delivery is called puerperal pyrexia. 87 | P a g e PUERPERAL SEPSIS (Syn: Puerperal infection) DEFINITION: An infection of the genital tract which occurs as a complication of delivery is termed puerperal sepsis. Puerperal pyrexia is considered to be due to genital tract infection unless proved otherwise. commonly due to—(i) endometritis, (ii) endomyometritis, or (iii) endoparametritis or a combination of all these when it is called pelvic cellulitis. CLINICAL FEATURES Local infection Uterine infection Spreading infection LOCAL INFECTION (WOUND INFECTION): (1) There is slight rise of temperature, generalized malaise or headache, (2) The local wound becomes red and swollen, (3) Pus may form which leads to disruption of the wound. When severe (acute), there is high rise of temperature with chills and rigor. UTERINE INFECTION Mild—(1) There is rise in temperature (>100.4°F) and pulse rate (>90), (2) Lochial discharge becomes offensive and copious, (3) The uterus is subinvoluted and tender. Severe—(1) The onset is acute with high rise of temperature, often with chills and rigor, (2) Pulse rate is rapid, out of proportion to temperature, (3) Often there is breathlessness, coughs, abdominal pain and dysuria, (4) Lochia may be scanty and odorless, (5) Uterus may be subinvoluted, tender and softer. There may be associated wound infection (perineum, vagina or the cervix). SPREADING INFECTION (EXTRAUTERINE SPREAD) is evident by presence of pelvic tenderness (pelvic peritonitis), tenderness on the fornix (parametritis), bulging fluctuant mass in the pouch of Douglas (pelvic abscess). 88 | P a g e General care: (i) Isolation of the patient is preferred especially when hemolytic Streptococcus is obtained on culture, (ii) Adequate fluid and calorie are maintained by intravenous infusion (IV), (iii) Anemia is corrected by oral iron or if needed by blood transfusion, (iv) An indwelling catheter is used to relieve any urine retention due to pelvic abscess. It also helps to record urinary output, (v) A chart is maintained by recording pulse, respiration, temperature, lochial discharge, and fluid intake and output. (vi) Antibiotics: Ideal antibiotic regimen should depend on the culture and sensitivity report. Pending the report, gentamicin (2 mg/kg IV loading dose, followed by 1.5 mg/kg IV every 8 hours) and clindamycin (900 mg IV every 8 hours) should be started. Metronidazole 0.5 g IV is given at 8 hours interval to control the anaerobic group. The treatment is continued until the infection is controlled for at least 7–10 days. Surgical treatment: There is little role of major surgery in the treatment of puerperal sepsis. Perineal wound—The stitches of the perineal wound may have to be removed to facilitate drainage of pus and relieve pain. The wound is to be cleaned with sitz bath several times a day and is dressed with an antiseptic ointment or powder. Retaineduterineproductswithadiameterof3cmorlessmaybedisregardedandleftalon e. Otherwise surgical evacuation after antibiotic coverage for 24 hours should be done to avoid the risk of septicemia. Cases with septic pelvic thrombophlebitis are treated with IV heparin for 7–10 days. 89 | P a g e Pelvic abscess should be drained by colpotomy under ultrasound guidance. Wounddehiscence:Dehiscenceofepisiotomyorabdominalwoundfollowingcesarean section is managed by scrubbing the wound twice daily, debridement of all necrotic tissue and then closing the wound with secondary suture. Laparotomy has got limited indications. Maintenance of electrolyte balance by intravenous fluids along with appropriate antibiotic therapy usually controls the peritonitis. Hysterectomy is indicated in cases with rupture or perforation, having multiple abscesses, gangrenous uterus or gas gangrene infection. Ruptured tubo-ovarian abscess should be removed. Necrotizing fasciitis is rare but fatal complication of wound infection (abdominal, perineal, vaginal), involving muscle and fascia. Treatment includes: Rehydration, wound scrubbing, debridement of all necrotic tissues, and use of high dose broad-spectrum (IV) antibiotics. 90 | P a g e 91 | P a g e 67. Pregnancy in Rh-negative mothers. Haemolytic disease of fetus and newborn. Rh-negative mothers may develop antibodies against Rh-positive fetal blood cells during pregnancy, which can lead to hemolytic disease of the fetus and newborn (HDFN). This occurs because the Rh antigen is present on the surface of red blood cells and is inherited genetically. An Rh-negative mother who carries an Rhpositive fetus is at risk for developing antibodies against the Rh antigen, which can cross the placenta and attack the fetal red blood cells. If the mother is Rh-negative and the father is Rh-positive, there is a 50% chance that the fetus will be Rh-positive. The risk of sensitization to Rh factor increases with each pregnancy, as the mother's immune system is exposed to more Rhpositive fetal blood cells. HDFN can cause anemia, jaundice, and in severe cases, brain damage or death in the fetus or newborn. The severity of HDFN depends on the level of maternal antibodies, the number of fetal red blood cells destroyed, and the gestational age at which the disease occurs. To prevent HDFN, Rh-negative mothers are given Rh immune globulin (RhIg) during pregnancy and within 72 hours after delivery or any other event that may have caused mixing of the maternal and fetal blood, such as miscarriage or abortion. RhIg works by binding to any Rh-positive fetal cells in the mother's bloodstream before her immune system has a chance to develop an immune response. If HDFN is suspected, the fetus can be monitored for signs of anemia using ultrasound and fetal blood sampling. In severe cases, intrauterine blood transfusions may be necessary to treat the anemia. After delivery, the newborn may require phototherapy or exchange transfusions to treat jaundice and prevent brain damage. 68. Anaemia in pregnancy: possible types, diagnosis, complications. prognosis, treatment. Anemia in pregnancy is a common medical condition that occurs when the number of red blood cells or hemoglobin levels are below normal range. There are several possible types of anemia in pregnancy, including iron deficiency 92 | P a g e anemia, folate deficiency anemia, and vitamin B12 deficiency anemia. Iron deficiency anemia is the most common type of anemia in pregnancy. It occurs when there is insufficient iron available for the body to produce enough red blood cells. This type of anemia is typically caused by inadequate intake of iron-rich foods or poor absorption of iron. Folate deficiency anemia and vitamin B12 deficiency anemia are less common but can also occur during pregnancy. The diagnosis of anemia in pregnancy is made through a blood test that measures the levels of hemoglobin and hematocrit. Symptoms of anemia in pregnancy may include fatigue, weakness, pale skin, shortness of breath, and dizziness. Untreated anemia in pregnancy can lead to several complications, including preterm labor, low birth weight, and postpartum hemorrhage. In severe cases, anemia can also increase the risk of fetal and maternal mortality. Treatment for anemia in pregnancy typically involves iron supplements or other nutritional supplements to address the specific type of anemia. In severe cases, blood transfusions may be necessary. It is also important to identify and treat any underlying medical conditions that may be contributing to the anemia. With proper diagnosis and treatment, the prognosis for anemia in pregnancy is generally good. However, it is important for pregnant women to receive regular prenatal care and to follow their healthcare provider's recommendations for nutrition and supplementation to prevent and manage anemia during pregnancy. 69. Heart diseases in pregnancy: prognosis, pregnancy management. Heart diseases in pregnancy can increase the risk of complications for both the mother and the fetus. Some common heart diseases that can affect pregnancy include congenital heart disease, rheumatic heart disease, mitral stenosis, aortic stenosis, and pulmonary hypertension. Prognosis for heart diseases in pregnancy depends on the severity of the disease and the extent of cardiac dysfunction. Women with mild or moderate disease usually have a good prognosis if managed appropriately. However, those with severe heart disease may be at risk of heart failure, arrhythmias, and even maternal mortality. Pregnancy management for women with heart disease should involve a multidisciplinary approach, including an obstetrician, a cardiologist, and a 93 | P a g e maternal-fetal medicine specialist. The management plan should be tailored to the individual woman's specific heart disease and the severity of her symptoms. Management strategies for heart diseases in pregnancy may include close monitoring of maternal and fetal health, medication to manage symptoms and prevent complications, and possible interventions such as cardiac surgery or catheterization. In some cases, induction of labor or cesarean delivery may be recommended to reduce the stress on the mother's heart during delivery. Women with heart diseases in pregnancy require careful monitoring before, during, and after delivery to ensure the best possible outcome for both the mother and the baby. 70. Tuberculosis in pregnancy: risk factors, diagnosis, prognosis, management. Tuberculosis (TB) is a bacterial infection caused by Mycobacterium tuberculosis that primarily affects the lungs but can also affect other organs in the body. TB in pregnancy can be a serious health issue for both the mother and the baby. Risk factors for TB in pregnancy include living in an area with a high prevalence of TB, close contact with a person with active TB, immunocompromised status, and poverty. Diagnosis of TB in pregnancy can be challenging as the symptoms of TB are similar to those of pregnancy, such as cough, fever, and weight loss. Diagnostic tests for TB include chest X-ray, sputum culture, and tuberculin skin test. However, some diagnostic tests may not be safe for pregnant women, and the timing of testing may need to be carefully considered. The prognosis of TB in pregnancy depends on several factors, including the severity of the infection, the timing of diagnosis, and the effectiveness of treatment. TB can cause complications during pregnancy, such as preterm labor, low birth weight, and maternal mortality. Management of TB in pregnancy involves a multidisciplinary approach with a team of obstetricians, pulmonologists, and infectious disease specialists. The treatment of TB in pregnancy is similar to that in non-pregnant patients, but some anti-TB medications may be contraindicated or require dosage adjustments in pregnancy. Close monitoring of the mother and the fetus is crucial during the treatment period. 94 | P a g e 71. Diabetes: risk factors, diagnosis, prognosis, management. Diabetes is a metabolic disorder characterized by high blood glucose levels. During pregnancy, diabetes can occur in two forms: pre-existing diabetes or gestational diabetes. Risk factors for pre-existing diabetes in pregnancy include having type 1 or type 2 diabetes before pregnancy, a family history of diabetes, obesity, and being over 35 years old. Risk factors for gestational diabetes include being overweight or obese, having a family history of diabetes, and being over 25 years old. Diagnosis of pre-existing diabetes in pregnancy is usually made before pregnancy or during the first trimester through blood glucose testing. For gestational diabetes, screening is typically done between 24 and 28 weeks of pregnancy through a glucose challenge test, followed by a glucose tolerance test if the initial test is abnormal. Complications of diabetes in pregnancy can include preterm labor, preeclampsia, stillbirth, and delivery complications such as shoulder dystocia. Poorly controlled diabetes during pregnancy can also lead to health problems for the mother, such as diabetic retinopathy and nephropathy. Management of diabetes in pregnancy involves careful monitoring of blood glucose levels and insulin therapy as needed to maintain normal levels. A healthy diet and regular exercise are also important components of diabetes management during pregnancy. Close monitoring of the pregnancy through frequent ultrasounds and non-stress tests may also be necessary to ensure the health and well-being of both the mother and baby. 72. 72. Viral hepatitis's: risk factors, diagnosis, prognosis, management. Viral hepatitis is a group of infectious diseases caused by hepatitis viruses A, B, C, D, and E. Here are the risk factors, diagnosis, prognosis, and management of viral hepatitis: Risk Factors: • Exposure to contaminated blood and body fluids • Injection drug use • Unprotected sex with an infected partner • Travel to or residence in an area where hepatitis is prevalent • Sharing personal items such as razors or toothbrushes with an 95 | P a g e infected person • Healthcare workers who come into contact with infected blood or body fluids Diagnosis: • Blood tests to detect the presence of viral antibodies and antigens • Liver function tests to evaluate the liver's health • Imaging tests such as ultrasound, CT scan or MRI to examine the liver • Liver biopsy may be done to obtain a sample of liver tissue for further analysis Prognosis: • The prognosis of viral hepatitis varies depending on the type of virus and the extent of liver damage. • Acute hepatitis may resolve on its own, but chronic hepatitis may lead to serious complications such as liver cirrhosis, liver failure, and liver cancer. Management: • Treatment options for viral hepatitis depend on the type of virus and the extent of liver damage. • Antiviral medications such as interferon, ribavirin, and direct-acting antivirals are used to treat hepatitis B and C. • Supportive care such as rest, adequate nutrition, and avoiding alcohol and certain medications that can damage the liver. • Vaccines are available to prevent hepatitis A and B. It is important to seek medical attention if you suspect you have viral hepatitis, as early diagnosis and treatment can improve outcomes. 73. Syphilis in pregnancy: risk factors, diagnosis, prognosis, management. Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. It can be transmitted from an infected mother to her fetus during pregnancy, leading to congenital syphilis. The following are the risk factors, diagnosis, prognosis, and management of syphilis in pregnancy: Risk factors: • Being sexually active with a partner who has syphilis • Previous history of syphilis or other sexually transmitted infections • Unprotected sex • Intravenous drug use 96 | P a g e • Living in an area with a high prevalence of syphilis Diagnosis: Syphilis can be diagnosed through blood tests, such as the Venereal Disease Research Laboratory (VDRL) test or the Rapid Plasma Reagin (RPR) test. If the results are positive, further testing is needed to confirm the diagnosis, such as the Treponema pallidum particle agglutination (TPPA) test or the fluorescent treponemal antibody absorption (FTA-ABS) test. Prognosis: If left untreated, syphilis in pregnancy can lead to serious complications, such as stillbirth, preterm birth, low birth weight, and congenital syphilis. Congenital syphilis can cause deformities, neurological problems, and developmental delays in the baby. Management: Treatment of syphilis in pregnancy involves antibiotics, such as penicillin. Penicillin is safe for use in pregnancy and is the only recommended treatment for pregnant women with syphilis. Treatment should be started as early as possible to prevent transmission of the infection to the fetus. If the fetus is infected, treatment may need to be continued after delivery. Regular monitoring of the mother and fetus is also important to ensure that the infection is treated effectively and to detect any complications. 74. Urinary tract infection in pregnancy (pyelonephritis, asymptomatic bacteriuria): risk factors. diagnosis, prognosis, management. Urinary tract infections (UTIs) are common during pregnancy, especially in the second and third trimesters. Two common types of UTIs during pregnancy are asymptomatic bacteriuria (ASB) and pyelonephritis. Risk factors for UTIs in pregnancy include: • Previous history of UTIs • Diabetes mellitus • Kidney problems • Urinary tract abnormalities • Sexual activity • Use of a diaphragm for contraception Diagnosis of UTIs in pregnancy involves a urine culture to detect the presence of bacteria in the urine. Pregnant women should be screened for ASB during their 97 | P a g e first prenatal visit, and those who test positive should be treated with antibiotics to prevent the development of pyelonephritis. Pyelonephritis is a more serious type of UTI that can cause kidney damage and preterm labor. Symptoms of pyelonephritis may include fever, chills, flank pain, nausea, and vomiting. It is typically treated with a course of antibiotics, and hospitalization may be required for severe cases. Prognosis for UTIs in pregnancy is generally good with appropriate treatment. However, if left untreated, UTIs can lead to serious complications for both the mother and baby. Preventive measures for UTIs during pregnancy include drinking plenty of water, practicing good hygiene, and urinating frequently. Pregnant women should also avoid holding in urine for extended periods and should empty their bladder completely when urinating. 75. HIV/AIDS in pregnancy: risk factors, diagnosis, prognosis, management. HIV (human immunodeficiency virus) is a viral infection that can be transmitted from mother to child during pregnancy, childbirth, or breastfeeding. It is important for pregnant women to know their HIV status, as timely interventions can significantly reduce the risk of mother-to-child transmission. Risk factors for HIV/AIDS in pregnancy include unprotected sexual activity with an infected partner, sharing needles or syringes, and being from a high-prevalence region. Diagnosis of HIV in pregnancy involves routine testing, typically at the first prenatal visit and again in the third trimester for high-risk women. Rapid HIV testing may also be used during labor and delivery for women who do not know their HIV status. The prognosis for HIV-positive mothers and their babies has significantly improved with the use of antiretroviral therapy (ART) during pregnancy and delivery, as well as prophylactic medication for the baby. With appropriate interventions, the risk of mother-to-child transmission can be reduced to less than 1%. Management of HIV/AIDS in pregnancy involves close monitoring by a healthcare provider experienced in managing HIV-positive pregnant women. ART is the 98 | P a g e mainstay of treatment, and it is important to adhere to the treatment regimen to reduce the risk of transmission to the baby. In addition, elective caesarean section delivery may be recommended to further reduce the risk of transmission. Breastfeeding may also need to be avoided or limited depending on the mother's viral load and other factors. 76. General surgery and acute abdomen during the pregnancy. Pregnancy itself does not increase the risk of general surgical conditions or acute abdomen, but pregnancy can affect the presentation, diagnosis, and management of these conditions. Some common general surgical conditions that can occur during pregnancy include appendicitis, cholecystitis, pancreatitis, bowel obstruction, and hernias. The diagnosis of these conditions in pregnant women can be challenging due to changes in anatomy and physiology that occur during pregnancy. For example, the appendix may be located higher in the abdomen due to the upward displacement of the uterus, making it difficult to diagnose appendicitis based on typical clinical signs and symptoms. Additionally, the enlarged uterus may compress the intestines, causing symptoms that can mimic bowel obstruction. Management of these conditions in pregnant women should be tailored to the individual patient and the severity of the condition. In general, surgical intervention should be considered if the condition is life-threatening or if conservative management fails. Surgery during pregnancy carries a higher risk of complications, such as preterm labor, fetal distress, and miscarriage, but these risks must be balanced against the potential risks of delaying or avoiding surgery. In cases of acute abdomen, the immediate management includes stabilization of the mother and fetus, and expedited diagnosis to initiate appropriate management. Surgery may be necessary to manage acute abdomen, but nonsurgical management such as antibiotics may be used for some conditions like acute cholecystitis. In summary, general surgical conditions and acute abdomen can occur during pregnancy and may require surgery or other interventions. Careful diagnosis and management that considers the unique physiology and anatomy of pregnancy are important to ensure optimal outcomes for both the mother and fetus. 99 | P a g e 77. Multiple pregnancy: diagnosis, prognosis and management. Multiple pregnancy refers to the presence of more than one fetus in the uterus. It can result from the fertilization of multiple eggs by multiple sperm (fraternal or dizygotic twins) or from the division of a single fertilized egg (identical or monozygotic twins). Diagnosis of multiple pregnancy is usually made by ultrasound, which can detect the presence of more than one gestational sac and confirm the number of fetuses. Prognosis for multiple pregnancy depends on several factors, including the number of fetuses, gestational age, and presence of any complications such as preterm labor or preeclampsia. Multiple pregnancy is associated with a higher risk of complications such as preterm delivery, low birth weight, and fetal growth restriction. The risk of these complications increases with the number of fetuses. Management of multiple pregnancy involves close monitoring for complications and may require more frequent prenatal visits, ultrasounds, and specialized care. In some cases, interventions such as cerclage (a stitch to keep the cervix closed), bed rest, or medications may be recommended to prevent preterm labor or other complications. In cases where the risk to the mother or fetuses is high, delivery may be recommended earlier than in a singleton pregnancy. In general, the management of multiple pregnancy is individualized based on the specific circumstances of each pregnancy. 78. Post-term pregnancy: diagnosis, prognosis and management. Post-term pregnancy is defined as a pregnancy that goes beyond 42 completed weeks of gestation. The diagnosis is made by accurately determining the gestational age through ultrasound or by calculating the last menstrual period. The prognosis of post-term pregnancy can be associated with increased risk of adverse outcomes for both the mother and the baby. The longer the pregnancy goes beyond the due date, the greater the risk of fetal distress, stillbirth, meconium aspiration syndrome, and other complications such as shoulder dystocia, macrosomia, and prolonged labor. For the mother, post-term pregnancy 100 | P a g e can increase the risk of cesarean delivery, perineal trauma, and postpartum hemorrhage. The management of post-term pregnancy depends on several factors, including the overall health of the mother and fetus, the bishop score, and the presence or absence of fetal distress. Induction of labor is generally recommended after 41 weeks of gestation to reduce the risk of complications. The methods used to induce labor can vary, but commonly include the use of prostaglandins or oxytocin. Cesarean delivery may be necessary if there is fetal distress, failed induction, or other indications for operative delivery. Close monitoring of both the mother and the baby is crucial during the management of post-term pregnancy. 79. Diseases of the fetus and newborn: asphyxia neonatorum, respiratory distress. jaundice. convulsions. Asphyxia neonatorum is a condition in which the newborn baby is not getting enough oxygen. It can be caused by a variety of factors such as prolonged labor, compression of the umbilical cord, or preterm birth. Symptoms include a low heart rate, pale or blue skin, weak or absent breathing, and low muscle tone. Treatment may include resuscitation with oxygen, ventilation, and medication to support the baby's heart rate and blood pressure. Respiratory distress syndrome (RDS) is a common problem in premature infants where the lungs have not fully developed. It is caused by a lack of surfactant, a substance that keeps the air sacs in the lungs open, and leads to difficulty breathing. Symptoms include rapid breathing, flaring of the nostrils, grunting sounds, and a bluish tinge to the skin. Treatment may include oxygen therapy, mechanical ventilation, and medication to stimulate the production of surfactant. Jaundice is a common condition in newborns where the baby's skin and eyes appear yellow due to high levels of bilirubin in the blood. It is often harmless but can be a sign of more serious conditions such as blood type incompatibility or liver disease. Treatment may include phototherapy, in which the baby is exposed to special lights that help break down the bilirubin, or exchange transfusion, in which some of the baby's blood is replaced with donor blood. Convulsions in newborns can be caused by a variety of factors such as brain injury, infection, or metabolic disorders. Symptoms include uncontrolled movements, staring, and changes in breathing and heart rate. Treatment may 101 | P a g e include medication to stop the seizures and treat the underlying cause. In all cases, early detection and appropriate management are crucial for the best possible outcome for the baby. 80. 80. Perinatal infections: common sites, causes, mode, prevention, investigations, treatment. Perinatal infections are infections that can occur during pregnancy or in the neonatal period. These infections can have serious consequences for the health of the mother, the developing fetus, and the newborn. Common perinatal infections include group B streptococcus (GBS), cytomegalovirus (CMV), toxoplasmosis, syphilis, rubella, and herpes simplex virus (HSV). Common sites and causes of perinatal infections: • Maternal genital tract: GBS, chlamydia, gonorrhea, HSV, human papillomavirus (HPV), trichomoniasis • Placenta and fetal membranes: CMV, toxoplasmosis, syphilis • Amniotic fluid: GBS, E. coli, other bacteria, Candida albicans, Ureaplasma urealyticum • Fetal bloodstream: GBS, syphilis, CMV • Neonatal respiratory tract: Group B streptococcus, E. coli, Haemophilus influenzae, Chlamydia trachomatis, Ureaplasma urealyticum, respiratory syncytial virus (RSV) Mode of transmission: • Vertical transmission: from mother to fetus or newborn during pregnancy, delivery, or breastfeeding. • Horizontal transmission: from person to person through contact with infected body fluids or contaminated objects. Prevention: • Routine screening and treatment of maternal infections during pregnancy • Vaccination of the mother before pregnancy to prevent certain infections (e.g., rubella, hepatitis B) • Prevention of exposure to infectious agents through safe sex practices, good hygiene, and avoiding contact with infected individuals • Adequate prenatal care to detect and manage infections promptly Investigations: 102 | P a g e • • • Treatment: • • • • jaundice) Maternal blood tests (e.g., syphilis, HIV, CMV, rubella, toxoplasmosis) Amniocentesis (for diagnosis of fetal infections) Ultrasound (for detection of fetal abnormalities) Antibiotics for bacterial infections (e.g., GBS, syphilis) Antivirals for viral infections (e.g., acyclovir for HSV) Antifungals for fungal infections (e.g., candidiasis) Supportive care for neonatal complications (e.g., respiratory distress, 81. Anatomy of female reproductive system. The female reproductive system includes a complex network of organs, glands, and hormones that work together to produce, transport, and nourish female reproductive cells and support fetal development during pregnancy. The main organs of the female reproductive system include: • Ovaries: two small, almond-shaped organs that produce and release eggs (ova) into the fallopian tubes • Fallopian tubes: two thin tubes that transport eggs from the ovaries to the uterus and are the site of fertilization • Uterus: a muscular organ that is the site of fetal development during pregnancy • Cervix: the lower part of the uterus that connects to the vagina • Vagina: a muscular canal that connects the cervix to the outside of the body and serves as the birth canal during delivery • Vulva: the external genital organs, including the labia, clitoris, and vaginal opening. Other important structures and glands in the female reproductive system include the mammary glands (breasts), which produce milk to nourish newborns, and various glands that produce and regulate hormones such as estrogen and progesterone. 82. Physiology of female reproductive system: hypothalamus as the main neuroendocrine gland; pituitary gland (adenohypophysis). 103 | P a g e The female reproductive system is regulated by a complex interplay of hormones, neurotransmitters, and other signaling molecules. The hypothalamus and the pituitary gland, located in the brain, play important roles in this regulation. The hypothalamus produces gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH) into the bloodstream. These hormones, in turn, act on the ovaries to regulate the menstrual cycle and ovulation. FSH stimulates the growth and maturation of ovarian follicles, which contain the eggs. LH triggers ovulation, the release of a mature egg from the ovary. After ovulation, the empty follicle transforms into the corpus luteum, which produces progesterone, a hormone that prepares the uterus for pregnancy. If fertilization does not occur, the corpus luteum eventually disintegrates, leading to a drop in progesterone levels, which triggers menstruation. If fertilization does occur, the fertilized egg implants in the uterus and produces human chorionic gonadotropin (hCG), a hormone that maintains the corpus luteum and prevents menstruation. In addition to the hypothalamus-pituitary-ovarian axis, other hormones such as estrogen, progesterone, and testosterone also play important roles in the female reproductive system. Estrogen is responsible for the development of female secondary sex characteristics and helps regulate the menstrual cycle, while progesterone prepares the uterus for pregnancy and helps maintain a healthy pregnancy. Testosterone is produced in small amounts in the ovaries and contributes to female sexual function and libido. 83. 83. Ovarian steroidogenesis: hormones and their actions. Ovarian steroidogenesis refers to the process by which the ovaries produce steroid hormones, primarily estrogens and progesterone. This process is regulated by the hypothalamic-pituitary-ovarian axis. The main hormones involved in ovarian steroidogenesis are follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are produced by the anterior pituitary gland. FSH stimulates the growth and maturation of ovarian follicles, which contain the developing oocytes. LH stimulates the production of testosterone by the theca cells within the follicles. 104 | P a g e The granulosa cells within the follicle convert testosterone to estradiol, which is the most potent form of estrogen. The levels of estrogen increase as the follicle matures, and it reaches its highest levels just prior to ovulation. After ovulation, the remaining follicle forms the corpus luteum, which secretes progesterone. Progesterone helps to prepare the uterus for implantation and maintenance of a fertilized egg. The levels of estrogen and progesterone are also regulated by feedback mechanisms between the ovaries, pituitary gland, and hypothalamus. High levels of estrogen and progesterone inhibit the secretion of FSH and LH, which in turn decreases the production of estrogen and progesterone. This helps to maintain a balance between these hormones during the menstrual cycle. Overall, ovarian steroidogenesis is a complex process that involves the interaction of multiple hormones and regulatory mechanisms. It is essential for the normal functioning of the female reproductive system and plays a critical role in the menstrual cycle, pregnancy, and other aspects of female health. 84. 84. Physiology of menstruation and normal menstrual cycle. Menstruation is a cyclic process that occurs in women during their reproductive years, typically from menarche (first menstrual period) to menopause. The menstrual cycle is regulated by the complex interplay of various hormones, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, and progesterone. The menstrual cycle can be divided into three phases: the follicular phase, the ovulatory phase, and the luteal phase. 1. Follicular Phase: This phase begins on the first day of menstruation and lasts for approximately 14 days. During this phase, FSH is secreted by the pituitary gland, which stimulates the growth and maturation of several ovarian follicles. The follicles produce estrogen, which causes the lining of the uterus (endometrium) to thicken in preparation for implantation of a fertilized egg. 2. Ovulatory Phase: This phase occurs around day 14 of the menstrual cycle. LH is secreted by the pituitary gland, which triggers the release of a mature egg (ovulation) from the dominant follicle. 3. Luteal Phase: This phase begins after ovulation and lasts for approximately 14 days. The ruptured follicle (now called the corpus luteum) produces progesterone, which causes the endometrium to become more vascular 105 | P a g e and glandular in preparation for implantation of a fertilized egg. If fertilization does not occur, the corpus luteum degenerates, and the levels of estrogen and progesterone decrease, leading to the shedding of the endometrium and the onset of menstruation. This menstrual cycle is typically 28 days long, but can vary from woman to woman. The duration of the menstrual cycle and the amount of bleeding can also vary. 85. 85. Application of diagnostic methods in gynaecology (general and systemic examination; abdominal examination; gynaecological examination). Diagnostic methods play a crucial role in the diagnosis and management of various gynecological conditions. The following are some of the commonly used diagnostic methods in gynecology: 1. General and systemic examination: This includes a thorough evaluation of the patient's medical history, vital signs, and physical examination of other body systems to identify any underlying medical conditions that may impact gynecological health. 2. Abdominal examination: This involves palpation of the abdomen to assess the size, shape, and tenderness of the uterus, ovaries, and other pelvic structures. 3. Gynecological examination: This is a comprehensive examination of the female genitalia, including the vulva, vagina, cervix, uterus, and ovaries. It is performed to detect any abnormality in the structure or function of these organs. 4. Imaging studies: Imaging studies such as ultrasound, MRI, and CT scans are used to visualize the internal structures of the female reproductive system and detect any abnormalities. 5. Laboratory tests: Laboratory tests such as blood tests, urine tests, and cervical cytology are used to evaluate the hormonal status, detect infections, and diagnose gynecological conditions such as cervical cancer. 6. Biopsy: Biopsy involves the removal of a tissue sample from the cervix, uterus, or ovaries for further analysis to diagnose conditions such as cervical dysplasia, endometrial cancer, or ovarian cancer. 7. Endoscopy: Endoscopy involves the use of a thin, flexible tube with a 106 | P a g e light and camera to visualize the internal structures of the female reproductive system. It is used to diagnose conditions such as endometriosis, pelvic inflammatory disease, and fibroids. Overall, the appropriate use of diagnostic methods is crucial in identifying and managing gynecological conditions and improving women's health outcomes. 86. 86. Application of diagnostic methods in gynaecology (cytohormonal evaluation, uterine aspiration cytology and endometrial biopsy. aspiration of pouch of Douglas, hormonal tests) In gynecology, various diagnostic methods can be used to evaluate different aspects of female reproductive health. Here are some examples of diagnostic methods used in gynecology: 1. Cytological evaluation: This includes Pap smear, uterine aspiration cytology, and endometrial biopsy. These methods help to detect abnormal cells in the cervix, uterus, and endometrium, which may indicate cancer or pre-cancerous conditions. 2. Hormonal evaluation: Hormonal tests are used to evaluate the levels of hormones such as estrogen, progesterone, and follicle-stimulating hormone (FSH). These tests help to diagnose hormonal imbalances, such as polycystic ovary syndrome (PCOS) and menopause. 3. Ultrasonography: This diagnostic method uses high-frequency sound waves to produce images of the uterus, ovaries, and other pelvic structures. It can help to detect conditions such as fibroids, ovarian cysts, and endometriosis. 4. Magnetic resonance imaging (MRI): This imaging technique uses a strong magnetic field and radio waves to produce detailed images of the body. It is particularly useful in detecting pelvic masses and evaluating the extent of endometriosis. 5. Laparoscopy: This is a surgical diagnostic method that involves inserting a small camera through a small incision in the abdomen to view the pelvic structures. It is used to diagnose conditions such as endometriosis, pelvic inflammatory disease (PID), and ovarian cysts. 6. Hysteroscopy: This is a diagnostic method that involves inserting a small camera through the cervix to view the inside of the uterus. It is used to diagnose conditions such as uterine fibroids, polyps, and adhesions. 7. Aspiration of pouch of Douglas: This diagnostic method is performed 107 | P a g e by aspirating fluid from the pouch of Douglas, which is located behind the uterus. It is used to diagnose conditions such as pelvic inflammatory disease (PID) and endometriosis. Overall, the choice of diagnostic method depends on the specific condition being evaluated and the preferences of the healthcare provider and patient. 87. 87. Ultrasonography in gynaecology. Transvaginal ultrasound is a commonly used diagnostic tool in gynecology. It involves the insertion of a transducer probe into the vagina to obtain images of the pelvic organs, including the uterus, ovaries, and cervix. Ultrasound can be used for a variety of purposes in gynecology, including: 1. Evaluation of pelvic pain or abnormal vaginal bleeding 2. Assessment of ovarian cysts or tumors 3. Monitoring of follicular development during fertility treatments 4. Confirmation of pregnancy and evaluation of fetal growth and development 5. Detection of uterine fibroids or polyps 6. Identification of the location and cause of an ectopic pregnancy 7. Guiding procedures such as hysteroscopy, biopsy, or aspiration Transabdominal ultrasound may also be used to evaluate the pelvic organs, but it is less commonly used in gynecology compared to transvaginal ultrasound. 88. 88. Radiological investigation in gynaecology. Radiological investigations are commonly used in gynecology for diagnosis, treatment planning, and monitoring of various conditions. Some of the common radiological investigations used in gynecology include: 1. X-ray: Plain radiographs (X-rays) may be useful in evaluating bony pelvis anatomy, assessing the position and size of intrauterine contraceptive devices (IUDs), and detecting calcifications in ovarian teratomas. 2. Ultrasound: Ultrasound is the most common imaging modality used in gynecology. It is a safe and non-invasive technique that uses high-frequency sound waves to generate images of the internal organs. Ultrasound is used to diagnose and monitor pregnancy, identify and locate pelvic masses, evaluate the 108 | P a g e size and shape of the uterus and ovaries, assess the thickness and vascularity of the endometrium, and guide certain procedures such as oocyte retrieval for in vitro fertilization. 3. Hysterosalpingography: Hysterosalpingography is a type of X-ray that involves the injection of a contrast medium through the cervix into the uterine cavity and fallopian tubes. This allows visualization of the shape and contour of the uterine cavity and fallopian tubes, and may be used to diagnose uterine abnormalities and tubal blockages. 4. Magnetic resonance imaging (MRI): MRI uses a magnetic field and radio waves to produce detailed images of the internal organs. It is useful in diagnosing certain gynecologic conditions such as uterine fibroids, adenomyosis, and endometrial cancer. MRI can also be used to guide certain procedures, such as uterine artery embolization for fibroids. 5. Computed tomography (CT): CT uses X-rays and computer technology to generate cross-sectional images of the body. It is less commonly used in gynecology than ultrasound and MRI, but may be useful in evaluating complex pelvic masses or identifying bony abnormalities. 6. Positron emission tomography (PET) scan: PET scans use a radioactive tracer to produce images of the body. They may be used in the diagnosis and staging of gynecologic cancers. The choice of radiological investigation will depend on the specific clinical scenario, the suspected diagnosis, and the availability of resources. 89. 89. Endoscopy in gynaecology (colposcopy, hysteroscopy, laparoscopy). Endoscopy is an important diagnostic and therapeutic tool in gynecology. It involves the use of specialized instruments to visualize and access internal organs, such as the cervix, uterus, and ovaries. There are several types of endoscopic procedures used in gynecology, including colposcopy, hysteroscopy, and laparoscopy. Colposcopy is a procedure that allows a gynecologist to closely examine the cervix, vulva, and vagina for signs of abnormal tissue. A colposcope is used to magnify the area and a special solution is applied to the area to highlight any abnormal tissue. Biopsies may be taken during the procedure to confirm the diagnosis. Hysteroscopy involves the insertion of a thin, flexible tube with a camera 109 | P a g e (hysteroscope) through the vagina and cervix into the uterus. This allows for visualization of the inside of the uterus and can help diagnose and treat conditions such as abnormal bleeding, fibroids, and polyps. During the procedure, instruments can be inserted through the hysteroscope to remove tissue or perform other treatments. Laparoscopy is a minimally invasive surgical procedure that involves the insertion of a thin, flexible tube with a camera (laparoscope) through a small incision in the abdomen. This allows for visualization of the ovaries, fallopian tubes, and other pelvic organs. Laparoscopy can be used to diagnose and treat a variety of conditions, including endometriosis, ovarian cysts, and ectopic pregnancy. During the procedure, instruments can be inserted through other small incisions to perform surgical procedures as needed. Overall, endoscopy in gynecology is a valuable tool for diagnosing and treating a variety of gynecological conditions. 90. Components contributing to determination of sex. Clinical diagnosis of sex. The determination of sex in humans is determined by the combination of sex chromosomes received from the parents. Females have two X chromosomes (XX) while males have one X and one Y chromosome (XY). The presence of the Y chromosome in males triggers the development of testes which produce testosterone and other androgens. These hormones lead to the development of male genitalia and secondary sexual characteristics. In females, the absence of Y chromosome results in the development of ovaries and the production of estrogen. Clinically, the determination of sex can be achieved through several ways, including physical examination, genetic testing, and imaging studies. Physical examination includes the evaluation of external genitalia, breast development, and distribution of body hair. Genetic testing involves the analysis of chromosomes obtained from a blood sample or amniotic fluid during pregnancy. Imaging studies such as ultrasound may also be used to evaluate the presence of internal reproductive organs. In cases of ambiguous genitalia or disorders of sexual development, a multidisciplinary approach involving endocrinologists, geneticists, and urologists may be required for a comprehensive diagnosis. 110 | P a g e 91. Physiological pubertal changes and development of secondary sex characters related to age. Adolescence problems (precocious puberty, delayed puberty). Puberty is a stage of development during which physical and physiological changes occur that lead to sexual maturity. In females, puberty is characterized by the onset of menstruation and the development of secondary sexual characteristics such as breast development, pubic and underarm hair growth, and widening of the hips. The timing of puberty varies among individuals but generally occurs between the ages of 8 and 13 years. Precocious puberty refers to the onset of puberty before the age of 8 years in girls. It can be caused by various factors such as tumors in the brain, ovaries or adrenal glands, or genetic abnormalities. Delayed puberty, on the other hand, refers to the absence of pubertal development by the age of 13 years in girls. It can be caused by hormonal imbalances, genetic disorders, or chronic illnesses such as malnutrition. Adolescence is a time of significant physical, emotional, and social changes. Adolescents may experience a range of issues such as acne, body image concerns, mood swings, and risk-taking behaviors. It is important for adolescents to receive appropriate support and guidance during this time to promote healthy development and prevent negative outcomes such as substance abuse or mental health problems. In terms of clinical management, the treatment of precocious puberty and delayed puberty depends on the underlying cause. For precocious puberty, treatment may involve medications to suppress the hormones responsible for early onset of puberty or surgical removal of the tumor causing the hormonal imbalance. For delayed puberty, treatment may involve hormonal therapy to stimulate pubertal development. Adolescents experiencing emotional or behavioral problems may benefit from psychological counseling or other forms of support. 92. Normal menstrual cycle and menstrual cycle irregularities. The menstrual cycle is the series of changes that occur in the female reproductive 111 | P a g e system, leading to the preparation of the uterus for pregnancy. A typical menstrual cycle lasts for 28 days, although it can vary from 21 to 35 days in adult women. It can be divided into three phases: the follicular phase, ovulation, and the luteal phase. During the follicular phase (days 1-14), the anterior pituitary gland secretes follicle-stimulating hormone (FSH), which stimulates the development of follicles in the ovaries. These follicles produce estrogen, which causes the endometrium to thicken in preparation for implantation. As the follicles mature, they produce increasing amounts of estrogen, which results in a surge of luteinizing hormone (LH), triggering ovulation. Ovulation occurs around day 14, when the mature follicle releases an egg into the fallopian tube. The egg is then available for fertilization by sperm. During the luteal phase (days 15-28), the remaining follicular cells form the corpus luteum, which produces progesterone. This hormone helps to maintain the thickened endometrium in preparation for implantation. If fertilization occurs, the developing embryo releases human chorionic gonadotropin (hCG), which maintains the corpus luteum and progesterone production. If fertilization does not occur, the corpus luteum degenerates, leading to a drop in progesterone and menstruation. Menstrual cycle irregularities can occur due to a variety of factors, including hormonal imbalances, stress, weight changes, medications, and medical conditions. Some examples of menstrual cycle irregularities include: 1. Amenorrhea: the absence of menstrual periods. It can be primary (no period by age 16) or secondary (absence of periods for more than three months in a woman who previously had regular cycles). 2. Dysmenorrhea: painful menstrual periods. 3. Menorrhagia: heavy menstrual bleeding. 4. Oligomenorrhea: infrequent menstrual periods (less than eight periods per year). 5. Polymenorrhea: frequent menstrual periods (more than 12 periods per year). 6. Irregular cycles: cycles that vary in length by more than seven to nine days. Treatment for menstrual cycle irregularities depends on the underlying cause. Hormonal imbalances can be treated with hormonal therapy, such as oral contraceptive pills. Non-hormonal treatments, such as nonsteroidal antiinflammatory drugs (NSAIDs), can help with pain relief. In some cases, lifestyle 112 | P a g e changes, such as weight loss or stress reduction, may also be recommended. 93. Amenorrhoea: definition and classification. Amenorrhea is a medical term that refers to the absence of menstrual bleeding. It is classified into two main types: primary amenorrhea and secondary amenorrhea. Primary amenorrhea is defined as the absence of menstrual bleeding by the age of 16 in the absence of secondary sexual characteristics, or by the age of 14 in the presence of secondary sexual characteristics. Secondary amenorrhea is defined as the absence of menstrual bleeding for more than 3 months in women who have previously had regular menstrual cycles, or for more than 6 months in women who have previously had irregular menstrual cycles. It can be caused by various factors such as pregnancy, menopause, hormonal imbalances, thyroid disorders, eating disorders, excessive exercise, stress, medications, and certain medical conditions. 94. Hypergonadotropic primary amenorrhoea. Turner's syndrome: aetiology, clinical symptoms, investigations, management. Hypergonadotropic primary amenorrhea refers to the absence of menstruation in females beyond the age of 16 years, in association with elevated levels of folliclestimulating hormone (FSH) and luteinizing hormone (LH). Turner syndrome is a genetic disorder that affects females, characterized by the absence or abnormality of one of the two X chromosomes. Aetiology: Turner syndrome is caused by a random error during the formation of reproductive cells, resulting in the loss or alteration of the X chromosome. This condition can also be inherited in rare cases. Clinical symptoms: • Short stature • Absent or incomplete development of secondary sexual characteristics • Infertility • Heart abnormalities 113 | P a g e • Kidney abnormalities • Thyroid problems • Hearing difficulties • Learning disabilities Investigations: • Karyotyping to detect chromosomal abnormalities • Pelvic ultrasound to evaluate the presence of ovaries and uterus • Hormonal assays to determine levels of FSH, LH, estrogen, and other hormones • Echocardiography to evaluate heart function • Renal ultrasound to evaluate kidney function Management: • Growth hormone therapy may be used to treat short stature • Estrogen replacement therapy may be used to induce puberty and develop secondary sexual characteristics • Fertility treatments such as egg donation or surrogacy may be an option for women with Turner syndrome who wish to have children • Treatment of associated medical conditions such as heart or kidney problems 95. Eugonadotropic primary amenorrhoea. Testicular feminizing syndrome: aetiology, clinical symptoms, investigations, management. Eugonadotropic primary amenorrhea is a condition in which a woman does not begin menstruating by the age of 16, despite the presence of normal ovaries and normal levels of pituitary gonadotropins (follicle-stimulating hormone (FSH) and luteinizing hormone (LH)). One of the causes of eugonadotropic primary amenorrhea is the testicular feminization syndrome, also known as Androgen insensitivity syndrome (AIS). AIS is an X-linked recessive disorder in which a genetic male (XY) has an inability to respond to androgens, resulting in the development of female external genitalia and breasts during puberty. The testes remain in the abdomen or inguinal canal, and most individuals with AIS have a female gender identity. Clinical symptoms of AIS include primary amenorrhea, normal or tall stature, absence of pubic or axillary hair, and lack of development of secondary sexual characteristics, such as widening of the hips, due to the inability to respond to 114 | P a g e androgens. Investigations for AIS include a karyotype analysis, which typically shows a 46,XY pattern, and testing for serum testosterone and gonadotropins. Individuals with AIS have high levels of testosterone and gonadotropins due to the inability of the testes to respond to feedback inhibition by androgens. Management of AIS involves psychological support and hormone replacement therapy with estrogen and progesterone to induce and maintain menstruation and to prevent osteoporosis. Gonadectomy may also be considered in individuals with complete androgen insensitivity syndrome to reduce the risk of gonadal tumors. 96. Hypogonadotropic primary amenorrhoea: causes, clinical features. investigations and management. Hypogonadotropic primary amenorrhea refers to a condition where menstruation does not occur in women due to a lack of ovarian function, caused by a deficiency in gonadotropin-releasing hormone (GnRH) secretion by the hypothalamus or a deficiency in pituitary gonadotropin secretion. Causes of hypogonadotropic primary amenorrhea can include: 1. Genetic disorders such as Kallmann syndrome or Prader-Willi syndrome 2. Acquired conditions such as hypothalamic-pituitary tumors or traumatic brain injury 3. Anorexia nervosa or other eating disorders Clinical features of hypogonadotropic primary amenorrhea can include the absence of menstruation, lack of development of secondary sexual characteristics, and low levels of estrogen. Investigations for hypogonadotropic primary amenorrhea typically involve measuring hormone levels, such as follicle-stimulating hormone (FSH), luteinizing hormone (LH), and estradiol, and performing imaging studies, such as MRI of the brain, to identify any underlying structural abnormalities. Management of hypogonadotropic primary amenorrhea involves addressing the underlying cause, such as hormone replacement therapy to replace deficient estrogen levels or surgical removal of a tumor. In some cases, fertility treatment may also be necessary. 115 | P a g e 97. Secondary amenorrhoea: aetiology. classification, investigations and treatment. Secondary amenorrhea refers to the absence of menstruation for at least 3 months in women who have previously had regular menstrual cycles. The causes of secondary amenorrhea can be classified into different categories, including hormonal disorders, structural abnormalities, medications, and systemic diseases. Hormonal disorders that can cause secondary amenorrhea include thyroid dysfunction, hyperprolactinemia, and ovarian insufficiency. Structural abnormalities such as uterine adhesions, tumors, and scarring from surgeries can also lead to secondary amenorrhea. Certain medications such as hormonal contraceptives and antipsychotics can cause temporary amenorrhea, while systemic diseases such as chronic kidney disease and liver disease can also affect menstrual cycles. Investigations for secondary amenorrhea may include blood tests to assess hormone levels, imaging studies such as ultrasound or MRI to evaluate the reproductive organs, and in some cases, biopsy of the endometrial tissue to rule out malignancy. Treatment of secondary amenorrhea depends on the underlying cause. Hormonal imbalances can often be corrected with medications such as synthetic thyroid hormones, estrogen and progesterone replacement therapy, or medications to suppress prolactin production. Structural abnormalities may require surgical intervention, while discontinuation of offending medications or management of underlying systemic diseases may be necessary for some cases. 98. Adrenogenital syndrome: aetiology, clinical symptoms, investigations, Management. Adrenogenital syndrome, also known as congenital adrenal hyperplasia, is a genetic disorder caused by an enzyme deficiency in the adrenal gland that leads to a deficiency of cortisol and/or aldosterone, and an overproduction of androgens. This condition can affect both males and females. Aetiology: Adrenogenital syndrome is caused by a genetic defect that results in the impaired production of enzymes involved in the synthesis of cortisol and/or aldosterone in the adrenal gland. The most common form of adrenogenital syndrome is caused 116 | P a g e by a deficiency of the enzyme 21-hydroxylase. Clinical symptoms: The clinical features of adrenogenital syndrome depend on the severity of the enzyme deficiency and the level of androgen excess. In females, the excess androgens can lead to the development of male secondary sexual characteristics, such as a deepened voice, facial hair growth, and clitoromegaly. In males, the condition may cause precocious puberty, with early onset of pubic hair, enlargement of the penis, and accelerated growth. Both males and females may experience infertility, menstrual irregularities, and acne. In severe cases, lifethreatening adrenal crises may occur. Investigations: Diagnosis of adrenogenital syndrome is based on clinical features and confirmed by laboratory tests, including measurement of serum electrolytes, cortisol, aldosterone, and androgens, and genetic testing. Management: Treatment for adrenogenital syndrome involves hormone replacement therapy to replace deficient hormones and reduce androgen levels. This therapy typically involves the use of glucocorticoids and mineralocorticoids to replace cortisol and aldosterone, respectively. In some cases, surgical interventions may be necessary to correct genital abnormalities or remove tumors associated with the condition. Regular monitoring and management of electrolyte imbalances and adrenal crises are also important aspects of care for individuals with adrenogenital syndrome. 99. Hirsutism: endocrinology, causes, clinical features. investigations and management. Hirsutism is a medical condition characterized by excessive hair growth in women in a male pattern distribution, such as on the face, chest, back, or abdomen. It is usually caused by an excess of androgen hormones in the body, which can be produced by the ovaries, adrenal glands, or both. The causes of hirsutism can be divided into two main categories: non-endocrine and endocrine. Non-endocrine causes include genetic predisposition, ethnicity, and medication side effects. Endocrine causes include polycystic ovary syndrome (PCOS), adrenal gland disorders such as congenital adrenal hyperplasia, and tumors that produce androgen hormones. Clinical features of hirsutism include excessive hair growth in a male pattern 117 | P a g e distribution, acne, and oily skin. Other signs of androgen excess may be present, such as irregular periods, infertility, or deepening of the voice. Investigations for hirsutism include measurement of androgen hormone levels in the blood, such as testosterone, dehydroepiandrosterone sulfate (DHEAS), and androstenedione. An ultrasound of the ovaries may also be performed to evaluate for the presence of ovarian cysts or PCOS. Management of hirsutism involves treating the underlying cause, if possible, as well as addressing the cosmetic concerns of excessive hair growth. Treatment options may include medications that block androgen production or action, such as oral contraceptives, anti-androgen medications, or glucocorticoids. Hair removal methods, such as shaving, waxing, or laser hair removal, may also be used to manage the cosmetic effects of hirsutism. 118 | P a g e 119 | P a g e 100. Polycystic ovarian discase: actiology. clinical symptoms. investigations, management. Polycystic ovarian disease (PCOD), also known as polycystic ovarian syndrome (PCOS), is a hormonal disorder that affects women of reproductive age. It is characterized by multiple small cysts in the ovaries and an excess production of androgens (male hormones) by the ovaries. - The exact cause of PCOD is unknown, but it is believed to be influenced by genetics and insulin resistance. The clinical symptoms of PCOD include irregular menstrual cycles, heavy or prolonged periods, acne, hirsutism (excessive hair growth on the face and body), weight gain, and difficulty getting pregnant. Women with PCOD may also have higher levels of insulin, which can lead to an increased risk of developing type 2 diabetes. The diagnosis of PCOD is made based on a combination of clinical symptoms, physical examination, and laboratory investigations. The Rotterdam criteria are commonly used to diagnose PCOD, which includes the presence of at least two of the following: irregular periods, excess androgen production, and polycystic ovaries seen on ultrasound. The management of PCOD involves a combination of lifestyle modifications, medications, and surgery (in some cases). Lifestyle modifications include weight loss, regular exercise, and a healthy diet. Medications that are commonly used to manage PCOD include oral contraceptives (to regulate menstrual cycles), antiandrogen medications (to reduce hair growth and acne), and medications to improve insulin sensitivity (to reduce the risk of diabetes). In cases where lifestyle modifications and medications are not effective, surgery may be considered. Ovarian drilling is a surgical procedure that is sometimes used to treat PCOD. It involves making small incisions in the ovaries and using heat or a laser to destroy a small portion of the ovarian tissue. This can help to reduce androgen production and restore ovulation. 120 | P a g e 101. Hyperprolactinemia: aetiology. clinical symptoms, investigations, management. Hyperprolactinemia is a medical condition in which there is an abnormally high level of the hormone prolactin in the blood. It can be caused by various factors including prolactinoma (a benign tumor of the pituitary gland that produces prolactin), other tumors that affect the pituitary gland or hypothalamus, medications (such as antipsychotics, antidepressants, or certain blood pressure medications), hypothyroidism, chronic kidney disease, or stress. The clinical symptoms of hyperprolactinemia in women include amenorrhea (absence of menstrual periods), galactorrhea (abnormal lactation or breast discharge), infertility, and reduced libido. In men, it can cause reduced libido, impotence, and gynecomastia (breast enlargement in men). The diagnosis of hyperprolactinemia is made by measuring the level of prolactin in the blood. A single elevated level of prolactin does not necessarily indicate hyperprolactinemia, as prolactin levels can vary throughout the day and can be elevated by stress or certain medications. Therefore, repeat testing may be necessary to confirm the diagnosis. The management of hyperprolactinemia depends on the underlying cause. Treatment may include medications such as dopamine agonists (which can decrease prolactin secretion), surgery to remove pituitary tumors, or radiation therapy to shrink tumors. Patients with hyperprolactinemia should be followed closely by an endocrinologist or gynecologist to monitor prolactin levels and adjust treatment as necessary. 102. Asherman syndrome: causes, clinical symptoms, investigations, management. Progesterone challenge test. Asherman syndrome, also known as intrauterine adhesions or synechiae, is a condition characterized by the presence of adhesions or scar tissue within the 121 | P a g e uterine cavity. This can lead to menstrual abnormalities, infertility, and recurrent miscarriages. Causes: The most common cause of Asherman syndrome is previous uterine surgery, such as dilation and curettage (D&C), myomectomy, or cesarean section. Other possible causes include endometrial infections, radiation therapy, or uterine tuberculosis. Clinical Symptoms: Women with Asherman syndrome may experience menstrual abnormalities, such as decreased or absent periods, pelvic pain or discomfort, infertility, and recurrent miscarriages. Investigations: The diagnosis of Asherman syndrome can be made through a combination of medical history, physical examination, and imaging studies, such as hysterosalpingography (HSG), hysteroscopy, and ultrasound. A progesterone challenge test may also be performed to evaluate the endometrial response to progesterone. Management: The treatment of Asherman syndrome involves the removal of adhesions and restoration of normal uterine function. This is usually achieved through hysteroscopic surgery to remove the scar tissue and promote the regrowth of healthy endometrial tissue. Hormonal therapy, such as estrogen and progesterone supplementation, may also be used to support endometrial growth and prevent the formation of new adhesions. In severe cases, surrogacy or adoption may be considered as alternative options for pregnancy. 103. Premature menopause: actiology, pathophysiology, clinical features, investigations and management. Premature menopause, also known as premature ovarian insufficiency or premature ovarian failure, is a condition in which the ovaries of a woman under 122 | P a g e 40 years of age stop functioning properly, leading to infertility and menopausal symptoms. The exact cause of premature menopause is not always clear, but it can be caused by genetic factors, autoimmune diseases, viral infections, chemotherapy or radiation therapy, and surgical removal of ovaries. Clinical features of premature menopause include irregular or missed periods, hot flashes, night sweats, vaginal dryness, decreased libido, mood swings, and difficulty sleeping. Investigations for premature menopause may include hormone level testing (e.g., follicle-stimulating hormone, luteinizing hormone, estradiol, and progesterone), genetic testing, pelvic ultrasound, and bone density testing. Management of premature menopause may involve hormone replacement therapy to relieve symptoms and prevent long-term health problems associated with low estrogen levels (e.g., osteoporosis, heart disease). Counseling and support groups may also be helpful in coping with the emotional aspects of premature menopause, such as infertility and the loss of reproductive potential. 104. Sheehan's syndrome: causes. clinical symptoms, investigations. management. Sheehan's syndrome is a rare condition that occurs when there is damage to the pituitary gland during or after childbirth. This can lead to a deficiency of one or more hormones produced by the pituitary gland, including prolactin, growth hormone, thyroid-stimulating hormone, adrenocorticotropic hormone, folliclestimulating hormone, and luteinizing hormone. The causes of Sheehan's syndrome are related to severe bleeding during or after childbirth, which can cause a drop in blood pressure and restrict blood flow to the pituitary gland. This can result in the death of pituitary gland cells, leading to hormone deficiencies. 123 | P a g e The clinical symptoms of Sheehan's syndrome can vary depending on which hormones are affected, but common symptoms include failure to lactate, loss of pubic and underarm hair, fatigue, weight gain, hypotension, and menstrual irregularities. Investigations for Sheehan's syndrome may involve blood tests to measure hormone levels and imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to evaluate the pituitary gland. Management of Sheehan's syndrome typically involves hormone replacement therapy to address the hormone deficiencies. This may include medications such as cortisol, thyroid hormone, estrogen, and progesterone. Regular monitoring of hormone levels and symptom control is also important to manage the condition effectively. 105. Menorrhagia: causes, clinical symptoms, investigations, management. Menorrhagia refers to abnormally heavy or prolonged menstrual bleeding. It is a common gynecological problem that can significantly impact a woman's quality of life. The causes of menorrhagia can be varied, including hormonal imbalances, structural abnormalities, and underlying medical conditions. Some of the common causes of menorrhagia are: • Hormonal imbalances, such as anovulation, perimenopause, or thyroid disorders • Uterine fibroids or polyps • Adenomyosis (a condition where the inner lining of the uterus grows into the muscle wall) • Endometriosis (a condition where the inner lining of the uterus grows outside of the uterus) • Intrauterine device (IUD) use • Blood clotting disorders 124 | P a g e • Medications such as anticoagulants or hormonal contraceptives • Cancer or precancerous conditions of the uterus, cervix, or ovaries Clinical symptoms of menorrhagia can include: 1. Excessive bleeding that lasts longer than seven days 2. Needing to change sanitary protection every hour or more frequently 3. Passing clots that are larger than a quarter 4. Anemia symptoms such as fatigue, weakness, or shortness of breath 5. Pain during intercourse or menstruation 6. Interference with daily activities Investigations for menorrhagia may include: Blood tests to assess hormonal imbalances or blood clotting disorders Pelvic ultrasound to check for fibroids, polyps, or other structural abnormalities Endometrial biopsy to assess the thickness and composition of the lining of the uterus Hysteroscopy to visualize the inside of the uterus and take a tissue sample if necessary The management of menorrhagia depends on the underlying cause and the severity of the bleeding. Treatment options may include: Hormonal therapies, such as oral contraceptives or progesterone supplements, to regulate the menstrual cycle and reduce bleeding Nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and bleeding Tranexamic acid, a medication that reduces bleeding by promoting blood clotting Surgical interventions, such as endometrial ablation or hysterectomy, may be considered for severe or refractory cases. In some cases, lifestyle modifications such as maintaining a healthy weight, avoiding alcohol and smoking, and managing stress may also help in managing menorrhagia. 125 | P a g e 106. Menorrhagia: therapeutic measures (conservative treatment, hormone therapy). Menorrhagia is a condition characterized by abnormally heavy or prolonged menstrual bleeding. There are various treatment options available for managing menorrhagia, including conservative measures and hormone therapy. Conservative treatments for menorrhagia include: Nonsteroidal anti-inflammatory drugs (NSAIDs): These drugs can help reduce menstrual bleeding and relieve menstrual cramps. NSAIDs work by inhibiting prostaglandin production, which is responsible for menstrual cramps and heavy bleeding. Tranexamic acid: This medication helps reduce bleeding by preventing the breakdown of blood clots. Iron supplementation: Menorrhagia can lead to iron-deficiency anemia due to excessive blood loss. Iron supplements can help replace the lost iron and improve anemia. Herbal remedies: Certain herbs such as ginger, cinnamon, and turmeric have been found to have anti-inflammatory and anticoagulant properties, which can help reduce menstrual bleeding. Hormone therapy for menorrhagia includes: Combined oral contraceptives: These are the most commonly used hormonal therapy for menorrhagia. They work by preventing ovulation and regulating the menstrual cycle, thereby reducing menstrual bleeding. Progestin-only contraceptives: These contraceptives contain only progestin hormone and are used to regulate the menstrual cycle and reduce menstrual bleeding. Gonadotropin-releasing hormone (GnRH) agonists: These medications work by suppressing the production of estrogen and progesterone, which reduces menstrual bleeding. Levonorgestrel-releasing intrauterine system (LNG-IUS): This is a small, T-shaped device that is inserted into the uterus to release the hormone levonorgestrel. The LNG-IUS can help reduce menstrual bleeding and cramping. In some cases, surgical interventions such as endometrial ablation or hysterectomy may be necessary to manage menorrhagia that does not respond to 126 | P a g e conservative or hormonal treatments. 107. Types of surgical treatment of menorrhagia. Surgical treatment of menorrhagia may be necessary in cases where conservative measures or hormonal therapy have been unsuccessful or are not appropriate for the patient. There are several types of surgical procedures that can be performed to treat menorrhagia, including: Endometrial ablation: This is a minimally invasive procedure in which the lining of the uterus is destroyed or removed. It can be done with various methods such as thermal ablation, microwave ablation, or radiofrequency ablation. This procedure can be done as an outpatient procedure with minimal recovery time. Hysterectomy: This is the surgical removal of the uterus and may be recommended for women who have completed their family or for those who have other medical conditions that make the uterus unsuitable for continued use. It can be performed through an abdominal or vaginal approach. Myomectomy: This is a surgical procedure to remove fibroids from the uterus. It is often recommended for women who wish to preserve their fertility and have large fibroids or multiple fibroids that cannot be treated with medication. Uterine artery embolization: This is a minimally invasive procedure in which the blood supply to the uterus is blocked to shrink the fibroids and reduce bleeding. The choice of surgical procedure depends on various factors such as the age of the patient, her desire for future fertility, the size and location of the fibroids, and the severity of the symptoms. The risks, benefits, and alternatives of each procedure should be discussed with the patient before deciding on the most appropriate treatment. 108. DUB: pathogenesis, classification, pathological anatomy. DUB stands for Dysfunctional Uterine Bleeding, which is abnormal uterine 127 | P a g e bleeding not associated with any organic pathology. It is a diagnosis of exclusion, meaning that other causes of abnormal uterine bleeding such as fibroids, polyps, endometrial hyperplasia, and malignancy should be ruled out first. The pathogenesis of DUB is not completely understood, but it is thought to be related to hormonal imbalances that affect the normal cycle of menstruation. This can result in irregular or heavy bleeding, or bleeding that occurs outside of the normal menstrual cycle. DUB can be classified as ovulatory or anovulatory. Ovulatory DUB occurs when there is an imbalance in the normal hormonal cycle of ovulation, resulting in abnormal bleeding. Anovulatory DUB occurs when ovulation does not occur, leading to an imbalance in hormonal levels that can cause irregular, heavy, or prolonged bleeding. Pathologically, DUB can present with various findings, such as endometrial hyperplasia, atrophy, or polyps. However, many cases may show no significant pathology on examination. Investigations for DUB may include a detailed history and physical examination, including a pelvic examination and a Pap smear. Blood tests may be ordered to assess hormonal levels, such as thyroid function and estrogen and progesterone levels. Imaging studies, such as transvaginal ultrasound, may also be performed to evaluate the uterine and endometrial thickness and to exclude any other underlying pathology. Management of DUB depends on the underlying cause and the severity of symptoms. Conservative treatments may include medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), oral contraceptive pills, or progestins to regulate menstrual cycles and reduce bleeding. In cases of anovulatory DUB, cyclic progestin therapy can be particularly effective. In more severe cases, surgical interventions such as dilation and curettage (D&C), endometrial ablation, or hysterectomy may be necessary to control symptoms and prevent further bleeding. 128 | P a g e 109. Puberty menorrhagia: causes, clinical symptoms, investigations. management. Pubertal menorrhagia refers to heavy or prolonged menstrual bleeding that occurs during puberty, which is the time when the menstrual cycle starts in girls. The causes of pubertal menorrhagia can be related to hormonal imbalances, blood clotting disorders, structural abnormalities of the uterus or cervix, or certain medications. Clinical symptoms of pubertal menorrhagia may include heavy bleeding that lasts for more than seven days, needing to change pads or tampons every hour or two, passing large blood clots, feeling weak or dizzy, and experiencing fatigue or shortness of breath. Investigations for pubertal menorrhagia may include a complete blood count to check for anemia, blood clotting tests to rule out bleeding disorders, and imaging studies such as ultrasound or MRI to assess the uterus and ovaries for structural abnormalities. The management of pubertal menorrhagia depends on the underlying cause. Hormonal treatments such as combined oral contraceptives, progestin-only pills, or intrauterine devices (IUDs) may be prescribed to regulate the menstrual cycle and reduce bleeding. In some cases, medications such as tranexamic acid or nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce bleeding. If structural abnormalities are identified, surgical procedures such as hysteroscopy, dilation and curettage (D&C), or myomectomy may be necessary to treat the underlying condition. In severe cases, hysterectomy may be considered as a last resort. 110. Premenopausal menorthagia: causes. clinical symptoms, investigations. management. Premenopausal menorrhagia refers to heavy menstrual bleeding in women who 129 | P a g e have not yet reached menopause. It can be caused by a variety of factors, including hormonal imbalances, uterine fibroids, adenomyosis, endometrial polyps, and bleeding disorders. Clinical symptoms of premenopausal menorrhagia include prolonged or heavy menstrual bleeding, passing large blood clots, anemia, and menstrual cycles shorter than 21 days or longer than 35 days. Investigations may include blood tests to assess iron levels and screen for bleeding disorders, ultrasound to assess the uterus and ovaries, and hysteroscopy or endometrial biopsy to evaluate the lining of the uterus. Management of premenopausal menorrhagia depends on the underlying cause. Treatment may include nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce menstrual bleeding, hormonal therapy such as birth control pills or progesterone to regulate menstrual cycles, and surgical procedures such as endometrial ablation or hysterectomy for more severe cases. 111. Metropathia haemorragica: aetiology: pathological anatomy, clinical features, investigations and management. Metrorrhagia is abnormal uterine bleeding that occurs at irregular intervals, usually between menstrual periods. The term "metropathia haemorrhagica" is used to describe excessive and prolonged bleeding, often with clots, that is not associated with any specific pathology. Here is an overview of the condition: Aetiology: The exact cause of metropathia haemorrhagica is not fully understood, but it is thought to be related to hormonal imbalances or changes in the uterine lining. It is more commonly seen in women who are approaching menopause, but can occur in women of any age. Pathological anatomy: The uterine lining (endometrium) may be thicker than usual, and there may be 130 | P a g e areas of bleeding within it. Clinical features: The main symptom of metropathia haemorrhagica is irregular, heavy bleeding between periods. This may be accompanied by cramping or pain in the lower abdomen. Women with metropathia haemorrhagica may also experience fatigue and weakness due to the loss of blood. Investigations: The diagnosis of metropathia haemorrhagica is made by ruling out other possible causes of abnormal uterine bleeding. Tests may include blood tests to check hormone levels, imaging studies such as ultrasound or MRI, and a biopsy of the uterine lining. Management: The treatment of metropathia haemorrhagica depends on the severity of symptoms and the underlying cause of the bleeding. In many cases, the bleeding can be managed with hormonal therapies such as birth control pills or progesterone. In more severe cases, surgical treatment such as dilation and curettage (D&C) or hysteroscopy may be necessary to remove any abnormal tissue in the uterus. In rare cases, a hysterectomy (removal of the uterus) may be necessary if other treatments are not effective. 112. Ovulatory DUB: irregular ripening and irregular shedding. Ovulatory dysfunctional uterine bleeding (DUB) is a type of abnormal uterine bleeding that occurs due to irregular ripening of the endometrium and irregular shedding during the menstrual cycle. It is commonly caused by hormonal imbalances, particularly in estrogen and progesterone levels. During a normal menstrual cycle, the endometrium thickens and matures in preparation for a potential pregnancy. If fertilization does not occur, the endometrium is shed as menstrual bleeding. In ovulatory DUB, the endometrium may not mature and ripen properly due to hormonal imbalances, resulting in 131 | P a g e irregular shedding and abnormal bleeding patterns. Symptoms of ovulatory DUB may include heavy bleeding, irregular periods, prolonged bleeding, or bleeding between periods. It can be diagnosed through a variety of investigations, including blood tests to assess hormone levels, pelvic ultrasound to evaluate the thickness and appearance of the endometrium, and endometrial biopsy to examine the tissue for abnormalities. Management of ovulatory DUB may involve hormonal treatments, such as combined estrogen-progestin therapy or progestin-only therapy, to regulate the menstrual cycle and reduce bleeding. In some cases, surgical intervention may be necessary, such as endometrial ablation or hysterectomy. 113. Postmenopausal bleeding: aetiology, clinical features, investigations and management. Postmenopausal bleeding refers to vaginal bleeding that occurs 12 or more months after a woman's last menstrual period. It is considered abnormal and requires further evaluation. The following are the aetiology, clinical features, investigations, and management of postmenopausal bleeding: Aetiology: Atrophic vaginitis or endometrial atrophy Endometrial hyperplasia or cancer Cervical or vaginal cancer Trauma or infection Hormonal therapy Coagulation disorders Clinical features: Vaginal bleeding occurring 12 or more months after the last menstrual period Blood may be light or heavy, intermittent or continuous Associated symptoms may include pelvic pain, discharge, or postcoital bleeding 132 | P a g e Investigations: Transvaginal ultrasound to measure endometrial thickness Endometrial biopsy or curettage to obtain a tissue sample for pathological evaluation Hysteroscopy to visualize the uterine cavity and obtain biopsies or remove any abnormal growths Blood tests to assess hormone levels and check for any coagulation disorders Management: Treatment depends on the underlying cause Hormonal therapy may be used to treat atrophic vaginitis or endometrial hyperplasia Surgery may be required for endometrial or cervical cancer In some cases, no treatment may be necessary if the bleeding is due to a benign cause such as atrophic vaginitis It is important to promptly evaluate postmenopausal bleeding to rule out any serious underlying conditions, especially cancer. 114. Biology of the vagina, Natural defence mechanism of the vagina against infection. Flora of the female genital tract. The vagina is a muscular tube that extends from the vulva to the cervix of the uterus. It has a complex microenvironment that is regulated by hormones and a diverse microbial ecosystem, collectively known as the vaginal flora. The vaginal flora comprises a variety of microorganisms, including bacteria, fungi, and viruses. Lactobacillus species, particularly Lactobacillus crispatus, Lactobacillus jensenii, and Lactobacillus iners, are the dominant species of bacteria in the healthy vaginal flora. These bacteria produce lactic acid, which helps to maintain an acidic environment (pH 3.5 to 4.5) that inhibits the growth of pathogenic organisms. The natural defence mechanisms of the vagina include: Acidic environment: As mentioned above, the vaginal pH is maintained at an 133 | P a g e acidic level that inhibits the growth of pathogenic organisms. Mucus secretion: The vaginal epithelium secretes mucus that forms a barrier against invading pathogens. Antimicrobial peptides: The vaginal epithelium also produces antimicrobial peptides that have broad-spectrum activity against bacteria, fungi, and viruses. Hormonal regulation: The vaginal environment is regulated by hormones, particularly estrogen, which promotes the growth of Lactobacillus species and maintains the integrity of the vaginal epithelium. Immune cells: The vaginal mucosa contains immune cells, including macrophages, dendritic cells, and T cells, which help to detect and eliminate invading pathogens. Overall, the complex microenvironment of the vagina plays an important role in maintaining vaginal health and preventing infections. 115. Inflammatory lesions of the vulva: skin infections. Inflammatory lesions of the vulva can have various causes, including infections. Skin infections of the vulva can be caused by bacteria, viruses, fungi, or parasites. Some common examples include: Bacterial infections: Bacterial infections of the vulva can cause folliculitis, which is an inflammation of the hair follicles. Other bacterial infections include cellulitis, which is a deep skin infection that can cause redness, swelling, and warmth in the affected area, and abscesses, which are collections of pus that can form in the skin or deeper tissues. Viral infections: Viral infections of the vulva include genital warts, which are caused by the human papillomavirus (HPV), and herpes simplex virus (HSV), which can cause painful sores. Fungal infections: Fungal infections of the vulva can cause itching, burning, and soreness. The most common type of fungal infection is a yeast infection, which is caused by the overgrowth of Candida species. Parasitic infections: Parasitic infections of the vulva include pubic lice, which are tiny insects that can attach to pubic hair and cause itching and redness. The natural defense mechanism of the vagina against infection includes the normal flora of the female genital tract. The normal flora consists of bacteria that 134 | P a g e help maintain a healthy environment by producing lactic acid, which helps to maintain an acidic pH that prevents the growth of harmful bacteria. Lactobacillus is the most common type of bacteria found in the normal flora of the vagina. In addition, the vagina is lined with a layer of cells that produce mucus, which helps to keep the vagina moist and traps harmful bacteria and other pathogens, preventing them from entering the body. 116. Sexually transmitted diseases of the vulva; molluseum contagiosum, condylomata acumintata, herpes genitalis (aetiology, symptoms and signs, diagnosis and treatment). Sexually transmitted diseases (STDs) of the vulva include molluscum contagiosum, condylomata acuminate, and herpes genitalis. Here is an overview of each: Molluscum contagiosum: This is a viral infection caused by the molluscum contagiosum virus. It typically causes small, raised, round, pink or skin-colored bumps on the vulva. The bumps may have a dimpled center and can be itchy. Treatment options include cryotherapy, curettage, or topical agents like cantharidin, imiquimod, or podophyllotoxin. Condylomata acuminate: This is a viral infection caused by human papillomavirus (HPV). It leads to the formation of warty growths on the vulva and perianal area. The growths may be flat or raised, cauliflower-like, and can cause itching, burning, or bleeding. Treatment options include cryotherapy, surgical excision, or topical agents like podophyllin, imiquimod, or trichloroacetic acid. Herpes genitalis: This is a viral infection caused by the herpes simplex virus (HSV). It can cause painful blisters or ulcers on the vulva, vagina, or perianal area, along with flu-like symptoms such as fever and swollen lymph nodes. Herpes is a recurrent infection, meaning it can come back after treatment. Antiviral medications like acyclovir, valacyclovir, or famciclovir can help manage symptoms and reduce the frequency and severity of outbreaks. It's important to practice safe sex and get regular STD testing to prevent and detect these infections early. 135 | P a g e 117. Trichomoniasis: aetiology, symptoms and signs, diagnosis and treatment. Trichomoniasis is a sexually transmitted infection caused by a parasite called Trichomonas vaginalis. Here are some details regarding its aetiology, symptoms, diagnosis and treatment: Aetiology: Trichomoniasis is caused by a single-celled parasite called Trichomonas vaginalis, which is usually transmitted through sexual contact. Symptoms and signs: Many people with trichomoniasis do not have any symptoms. However, common symptoms can include: Vaginal discharge that may be frothy, green or yellow in color Vaginal itching or soreness Pain or discomfort during sexual intercourse or urination Strong vaginal odor Diagnosis: Trichomoniasis can be diagnosed by a healthcare provider through a physical exam, review of symptoms and laboratory tests. Laboratory tests may include a microscopic examination of vaginal discharge or a DNA test. Treatment: Trichomoniasis can be treated with antibiotics, such as metronidazole or tinidazole, which are usually given in a single dose. Sexual partners should also be treated to prevent re-infection. It is important to complete the entire course of antibiotics, even if symptoms improve before the medication is finished. It is also recommended to avoid sexual contact until the infection has cleared. 118. Candidiasis: actiology, symptoms and signs, diagnosis and treatment, 136 | P a g e Candidiasis is a fungal infection caused by the yeast Candida. The most common species that cause candidiasis is Candida albicans. Here are the details of its aetiology, symptoms and signs, diagnosis, and treatment: Aetiology: Candidiasis can occur due to several factors, such as weakened immune system, hormonal changes, antibiotic use, diabetes, pregnancy, and tight-fitting clothing. It can also be transmitted sexually. Symptoms and signs: The symptoms of candidiasis can vary depending on the location and severity of the infection. The most common symptom is itching and burning sensation in the affected area. Other symptoms include redness, swelling, and soreness. In women, candidiasis can also cause vaginal discharge and pain during sex. In severe cases, the infection can spread to other parts of the body and cause fever and chills. Diagnosis: Diagnosis of candidiasis is usually based on the symptoms and physical examination. The healthcare provider may also take a sample of the affected area and examine it under a microscope to confirm the presence of Candida. In some cases, a culture may be done to determine the specific type of Candida causing the infection. Treatment: The treatment of candidiasis involves antifungal medications. Topical antifungal creams and ointments can be used for mild infections, while oral antifungal medications are used for more severe infections. Over-the-counter medications such as miconazole and clotrimazole are effective for treating vaginal candidiasis. For recurrent infections, long-term treatment may be required. It is also important to identify and address any underlying conditions that may be contributing to the infection. Additionally, practicing good hygiene and avoiding tight-fitting clothing can help prevent the infection from recurring. 119. Chlamydiasis: aeriology, symptoms and signs, diagnosis and treatmen Chlamydia is a sexually transmitted bacterial infection caused by the bacterium Chlamydia trachomatis. It can infect both men and women, and is often 137 | P a g e asymptomatic, meaning that infected individuals may not experience any symptoms. Symptoms in women may include abnormal vaginal discharge, burning or pain during urination, lower abdominal pain, and pain during sexual intercourse. In men, symptoms may include discharge from the penis, burning or pain during urination, and swollen or tender testicles. Diagnosis is usually made through a urine test or swab of the affected area. Treatment typically involves a course of antibiotics, such as azithromycin or doxycycline. It is important to note that even if symptoms are not present, Chlamydia can still be transmitted to sexual partners, and untreated infections can lead to serious complications such as pelvic inflammatory disease, infertility, and ectopic pregnancy. Therefore, regular STI screening and safe sexual practices are important for preventing and managing Chlamydia infections. 120. Bacterial vaginosis: aetiology, symptoms and signs, diagnosis, treatment Bacterial vaginosis (BV) is a common vaginal infection caused by an overgrowth of certain types of bacteria in the vagina. The exact cause of BV is not fully understood, but it is thought to result from an imbalance in the normal vaginal flora, which allows harmful bacteria to multiply and thrive. Symptoms of BV include a thin, gray or white vaginal discharge with a strong fishy odor, itching, and burning during urination. However, many women with BV may not experience any symptoms at all. Diagnosis of BV is usually made based on a combination of symptoms and laboratory tests. A healthcare provider will perform a pelvic exam to check for vaginal discharge and may take a sample of the discharge for laboratory testing. A "whiff test" may also be performed in which a sample of discharge is mixed with potassium hydroxide (KOH) solution and examined for the characteristic fishy 138 | P a g e odor. Treatment for BV usually involves a course of antibiotics, either as an oral medication or a vaginal cream or gel. Commonly prescribed antibiotics for BV include metronidazole and clindamycin. Sexual partners of women with BV may also need to be treated to prevent reinfection. In addition to antibiotics, certain lifestyle changes may help prevent BV. These include avoiding douching, using condoms during sexual activity, and avoiding the use of scented products on the genital area. 121. Non-specific vaginal infections: aetiology, symptoms and signs, diagnosi and treatment. Non-specific vaginal infections refer to vaginal infections that are not caused by a specific pathogen such as bacteria, fungi, or viruses. Instead, they are caused by imbalances in the vaginal microbiome, which can lead to overgrowth of certain bacteria or other microorganisms. Here is a brief overview of non-specific vaginal infections: Aetiology: Non-specific vaginal infections can be caused by a variety of factors, including: Hormonal changes Antibiotic use Poor hygiene Sexual activity Use of scented products or douching Stress Symptoms and signs: The symptoms of non-specific vaginal infections can vary depending on the severity of the infection, but may include: Vaginal discharge Vaginal itching or burning 139 | P a g e Pain or discomfort during sex Pain or discomfort during urination Foul odor Diagnosis: Diagnosis of non-specific vaginal infections is usually made based on a combination of symptoms, physical examination, and laboratory tests. Your healthcare provider may perform a pelvic exam and take a sample of vaginal discharge for laboratory testing to rule out other causes of vaginal infections. Treatment: Treatment of non-specific vaginal infections typically involves restoring the balance of the vaginal microbiome. This may include: Probiotics: Probiotic supplements or foods can help restore healthy bacteria in the vagina. Antibiotics: Your healthcare provider may prescribe antibiotics if the infection is severe or does not respond to probiotics. Avoiding irritants: Avoid using scented products, douching, or other irritants that can disrupt the vaginal microbiome. Overall, it's important to maintain good hygiene practices and to seek medical care if you experience any symptoms of a vaginal infection. 122. 122. Oestrogen deficiency vaginitis: vulvovaginitis in children and senile vaginitis. Oestrogen deficiency vaginitis is a type of vaginitis that occurs due to decreased levels of estrogen hormone. It can occur in two age groups: prepubertal girls and postmenopausal women. In prepubertal girls, oestrogen deficiency vaginitis can occur due to lack of estrogen production in the body or due to an abnormality in the tissues that respond to estrogen. The symptoms may include vaginal itching, burning, discharge, and pain during urination or intercourse. In postmenopausal women, the vaginal tissues become thinner, drier, and less elastic due to decreased estrogen levels, which can lead to senile vaginitis. 140 | P a g e Symptoms may include vaginal dryness, itching, burning, and pain during intercourse. Treatment for oestrogen deficiency vaginitis involves restoring estrogen levels. In prepubertal girls, this may involve topical estrogen cream or tablets, while in postmenopausal women, estrogen replacement therapy may be used. Other treatments may include lubricants or moisturizers to relieve symptoms. It is important to note that any vaginal symptoms should be evaluated by a healthcare provider to determine the underlying cause and appropriate treatment. 123. Secondary vaginitis and are forms of vaginitis. Secondary vaginitis refers to inflammation of the vaginal wall that is caused by an underlying medical condition or factor, such as a bacterial or fungal infection, hormonal imbalances, or an allergic reaction. Treatment typically involves identifying and addressing the underlying cause of the inflammation. There are many forms of vaginitis, including: Bacterial vaginosis: an overgrowth of bacteria in the vagina that can cause discharge, odor, and irritation. Candidiasis (yeast infection): an overgrowth of yeast in the vagina that can cause itching, burning, and discharge. Trichomoniasis: a sexually transmitted infection caused by a parasite that can cause itching, burning, and discharge. Atrophic vaginitis: inflammation of the vaginal wall due to decreased estrogen levels, which can occur during menopause or after certain medical treatments. Chemical vaginitis: inflammation of the vaginal wall due to exposure to irritants, such as soaps, perfumes, or douches. Mixed vaginitis: a combination of different types of vaginitis, such as bacterial vaginosis and yeast infection occurring together. 141 | P a g e 124. Acute cervicitis: aetiology, symptoms and signs, diagnosis and treatment. Acute cervicitis refers to inflammation of the cervix that develops rapidly and typically presents with symptoms. Here's more information on the aetiology, symptoms and signs, diagnosis, and treatment of acute cervicitis: Aetiology: Infections with various microorganisms, including bacteria, viruses, fungi, and parasites, are the most common cause of acute cervicitis. The most frequent bacterial pathogens are Chlamydia trachomatis, Neisseria gonorrhoeae, and Mycoplasma genitalium, while viral causes include human papillomavirus (HPV), herpes simplex virus (HSV), and cytomegalovirus (CMV). Other causes of acute cervicitis can include chemical irritants, allergic reactions, and trauma to the cervix. Symptoms and signs: Symptoms of acute cervicitis can include vaginal discharge (which may be yellow, green, or gray and have a foul odor), vaginal bleeding or spotting (particularly after intercourse), pain or discomfort during sex, and pain or discomfort in the lower abdomen or pelvis. Signs of acute cervicitis can include redness, swelling, and tenderness of the cervix, as well as the presence of discharge or bleeding. Diagnosis: A physical exam, including a pelvic exam, is typically performed to evaluate for signs of inflammation or infection of the cervix. Tests that may be used to diagnose acute cervicitis include a Pap smear to evaluate for abnormal cervical cells, cultures of cervical secretions to identify the type of microorganism causing the infection, and blood tests to screen for certain sexually transmitted infections. Treatment: The treatment for acute cervicitis depends on the underlying cause of the 142 | P a g e inflammation or infection. Antibiotics are typically used to treat bacterial infections, while antiviral medications may be used to treat viral infections. Treatment may also involve the use of anti-inflammatory medications to reduce pain and swelling. Sexual partners may need to be treated as well to prevent reinfection. 125. Chronic cervicitis: actiology, symptoms and signs. diagnosis and treatment. Chronic cervicitis refers to long-standing inflammation of the cervix, which may be caused by several factors including infection, trauma, or an allergic reaction. Some common causes of chronic cervicitis include sexually transmitted infections (such as chlamydia or gonorrhea), bacterial infections (such as Group B streptococcus), and exposure to chemicals or irritants. Symptoms of chronic cervicitis may include vaginal discharge, discomfort or pain during sex, bleeding between periods, and pelvic pain. However, some women may not experience any symptoms. Diagnosis of chronic cervicitis involves a physical examination and a pelvic exam. A healthcare provider may collect samples of cervical discharge for laboratory testing to identify any potential bacterial or fungal infections. Additionally, a Pap smear may be performed to check for any abnormal cervical cells that could be indicative of cervical cancer. Treatment for chronic cervicitis depends on the underlying cause. Antibiotics may be prescribed for bacterial infections, antifungal medication may be prescribed for fungal infections, and antiviral medication may be prescribed for viral infections. In some cases, topical corticosteroids may be used to reduce inflammation. It is important to complete the full course of any prescribed medication, even if symptoms improve, to ensure the infection is fully treated. Prevention measures for chronic cervicitis include practicing safe sex and using 143 | P a g e barrier methods, such as condoms, to reduce the risk of sexually transmitted infections. It is also important to maintain good hygiene practices and avoid exposure to irritants or chemicals that can cause inflammation. Regular gynecologic check-ups and Pap smears can also help identify and treat any cervical abnormalities early on. 126. Endometritis and pyometra: causes, clinical forms, symptoms and sings diagnosis and management Endometritis and pyometra are two conditions that involve inflammation of the endometrium, or the lining of the uterus. They can have different causes, symptoms, and treatments. Endometritis is an inflammation of the endometrium that can be caused by infections such as bacterial, viral, or fungal. It can also occur as a result of retained products of conception after childbirth, miscarriage, or abortion. Symptoms of endometritis include lower abdominal pain, abnormal vaginal bleeding, fever, and foul-smelling vaginal discharge. Diagnosis is made through a pelvic exam, imaging tests, and cultures of the vaginal discharge. Treatment may involve antibiotics, anti-inflammatory medications, or surgical intervention if necessary. Pyometra, on the other hand, is a rare but serious condition that occurs when the uterus becomes filled with pus. It can be caused by infection or hormonal imbalances, and is most commonly seen in postmenopausal women. Symptoms of pyometra include fever, abdominal pain, abnormal vaginal discharge, and a feeling of fullness or pressure in the pelvic region. Diagnosis is made through a pelvic exam, imaging tests, and analysis of the vaginal discharge. Treatment typically involves antibiotics, and may also include drainage of the pus or surgical removal of the uterus in severe cases. It is important to seek medical attention promptly if you experience any symptoms of endometritis or pyometra, as both conditions can lead to serious complications if left untreated. 144 | P a g e 127. Pelvic inflammatory discase (PID): aetiology, pathological anatomy of acute salpingitis, staging. symptoms and signs of acute PID, diagnosis and differential diagnosis. Pelvic inflammatory disease (PID) is an infection of the female reproductive organs, including the uterus, fallopian tubes, and ovaries. It is usually caused by sexually transmitted infections, such as chlamydia and gonorrhea, although it can also result from other types of bacteria. The pathological anatomy of acute salpingitis in PID is characterized by inflammation and edema of the fallopian tubes, which can lead to scarring and blockage. In severe cases, pus may accumulate in the tubes, leading to pyosalpinx or even rupture. The symptoms and signs of acute PID include lower abdominal pain, fever, vaginal discharge, painful urination, and painful sexual intercourse. Diagnosis is based on a combination of clinical findings, laboratory tests, and imaging studies. The differential diagnosis includes other conditions that can cause similar symptoms, such as endometriosis, ovarian cysts, and ectopic pregnancy. The staging of PID is based on the severity and extent of the infection, as well as the presence of complications such as abscess formation or sepsis. Treatment typically involves a course of antibiotics to clear the infection, as well as pain management and supportive care. In some cases, surgery may be necessary to remove abscesses or repair damage to the reproductive organs. 128. Medical treatment of acute PID. The medical treatment of acute PID involves the use of antibiotics to eliminate the bacterial infection. The choice of antibiotics depends on the severity of the infection, the suspected or identified causative organisms, and any allergies the 145 | P a g e patient may have. In general, a combination of two antibiotics is used to ensure effective treatment and to reduce the risk of antibiotic resistance. The antibiotics are usually given intravenously (IV) in the hospital setting for severe cases, or orally for milder cases that can be managed on an outpatient basis. Some commonly used antibiotics for the treatment of acute PID include: Cefoxitin Cefotetan Ceftriaxone Doxycycline Clindamycin Metronidazole Patients with severe or complicated PID may require longer courses of antibiotics and close monitoring to ensure resolution of the infection and to prevent complications such as abscess formation or infertility. In addition to antibiotics, pain management and supportive care may be needed to manage symptoms such as fever and abdominal pain. It is also important to screen sexual partners and treat any other STIs to prevent reinfection. 129. Antibiotics therapy of PID. Antibiotic therapy is a key component of the treatment of pelvic inflammatory disease (PID). The choice of antibiotics depends on the severity of the infection, the causative organisms, and the patient's medical history and allergies. Broadspectrum antibiotics are typically used to provide coverage for a range of potential pathogens. Commonly used antibiotics for PID include: Ceftriaxone: This is a third-generation cephalosporin that is often used in 146 | P a g e combination with doxycycline or azithromycin to cover for gonorrhea and chlamydia infections. Doxycycline: This is a tetracycline antibiotic that is often used in combination with ceftriaxone or azithromycin to cover for gonorrhea and chlamydia infections. Azithromycin: This is a macrolide antibiotic that is often used in combination with ceftriaxone or doxycycline to cover for gonorrhea and chlamydia infections. Metronidazole: This is an antibiotic that is effective against anaerobic bacteria and is often used in combination with other antibiotics to treat PID. The duration of antibiotic therapy varies depending on the severity of the infection and the response to treatment. In general, treatment is continued until symptoms have resolved and there is evidence of clinical improvement. It is important to complete the full course of antibiotics to ensure that the infection is completely eradicated and to prevent the development of antibiotic-resistant bacteria. 130. Surgical treatment of acute PID. Surgical treatment of acute PID is reserved for cases where there is an abscess, a ruptured tubo-ovarian abscess, or the patient does not respond to medical therapy. The surgical approach may involve laparoscopy or laparotomy. The goal of surgical treatment is to drain any abscess, remove any infected tissue, and improve fertility if necessary. Laparoscopy is the preferred surgical approach for acute PID as it is less invasive and allows for quicker recovery. During laparoscopy, small incisions are made in the abdomen, and a laparoscope is used to view the pelvic organs. Any abscesses can be drained, and infected tissue can be removed using instruments inserted through the incisions. Laparotomy is a more invasive surgical approach that involves making a larger incision in the abdomen to access the pelvic organs. This approach is typically reserved for cases of severe infection, where there is a risk of rupture of the abscess or other complications. The surgical goals of laparotomy are the same as those of laparoscopy, but the recovery time is longer. 147 | P a g e In addition to surgery, antibiotics may be continued after surgery to ensure complete eradication of the infection. Follow-up appointments with a healthcare provider are important to monitor recovery and prevent future episodes of PID. 131. Pelvic inflammatory disease (PID): pathological anatomy of chronic PID, symptoms and signs of chronic PID, diagnosis and differential diagnosis. Chronic pelvic inflammatory disease (PID) is a condition that develops when acute PID is not adequately treated or resolved. It is characterized by chronic inflammation of the pelvic organs, including the uterus, fallopian tubes, ovaries, and surrounding tissues. The pathological anatomy of chronic PID shows fibrosis, adhesions, and scarring of the pelvic organs and tissues. The fallopian tubes may be occluded or distorted, which can lead to infertility or ectopic pregnancy. Symptoms of chronic PID may include pelvic pain, abnormal vaginal discharge, painful intercourse, and irregular menstrual bleeding. However, some women may have no symptoms at all. Chronic PID can also be asymptomatic and discovered incidentally during an infertility workup. Diagnosis of chronic PID is made based on the clinical history, physical examination, and imaging studies such as transvaginal ultrasound or MRI. Laparoscopy may also be used to confirm the diagnosis and evaluate the extent of pelvic adhesions and damage. Differential diagnosis of chronic PID includes other conditions that cause chronic pelvic pain and infertility, such as endometriosis, adenomyosis, uterine fibroids, and ovarian cysts. Management of chronic PID involves a combination of medical and surgical interventions. Antibiotics may be prescribed to treat any active infection and prevent further spread. Surgery may be necessary to remove adhesions, restore 148 | P a g e patency to the fallopian tubes, or remove damaged organs such as the uterus or ovaries. In some cases, in vitro fertilization (IVF) may be necessary to achieve pregnancy. 132. Surgical treatment of chronic PID. Surgical treatment of chronic PID may be necessary in cases where there are complications such as tubo-ovarian abscesses, pelvic adhesions or blockages in the fallopian tubes. The surgical procedures may include: Salpingectomy: Removal of the fallopian tubes, which may be necessary in cases of severe damage or blockage. Salpingostomy: Creation of an opening in the fallopian tube to drain an abscess. Oophorectomy: Removal of the ovaries, which may be necessary if they are severely damaged or infected. Hysterectomy: Removal of the uterus, which may be necessary in severe cases of chronic PID that do not respond to other treatments and where fertility is no longer desired. Surgical treatment is generally reserved for cases that are unresponsive to medical treatment or have complications that require intervention. It is important to note that surgical treatment may have implications for fertility and should be discussed with the patient beforehand. 149 | P a g e 150 | P a g e 133. PROGNOSIS AND END RESULTS OF PID. ANS. PID has a high morbidity; about 20% of affected women become infertile, 40% develop chronic pelvic pain, and 1% of those who conceive have an ectopic pregnancy. 134. PROPHYLAXIS OF PID. ANS. Essential steps in prevention are : • Community- based approach to increase public health awareness. • Prevention of sexually transmitted infection with the knowledge of healthy and safer sex. • Liberal use of contraceptives. • Routine screening of high risk population. 135. TUBERCULOSIS OF GENITAL TRACT. ANS. The causative organism is Mycobacterium tuberculosis of human type. Genital TB is always secondary to primary infection and spreads mostly by the route of hematogenous spread from the lungs (50%) and LNs. M/c affected organ is the FT (m/c ampulla). Fallopian tubes : Starts by interstitial salpingitis of ampullary region and then can spread medially causing destruction of muscles. Walls get thickened, calcified and fibrous. Fimbria are everted and the abdominal ostium usually remains patent. Gives a ‘tobacco pouch appearance’. Perisalpingitis can be seen. Uterus : Infection from tubes. Cornual ends mostly affected due to dual blood supply. Endometrial ulceration may lead to Asherman’s synd. Cervix, ovaries, vulva and vagina are rarely affected. Diagnosis and investigations : Blood tests, Mantoux test, CXR, diagnostic uterine curettage. Clinical diagnosis : Suspect in case of unexplained infertility or amenorrhea, recurrent PID episodes not responding to ABs. presence of pelvic mass with nodules in the POD. Symptoms & signs : infertility; menstrual abN which includes menorrhagia, 151 | P a g e amenorrhea or oligomenorrhea; c/c pelvic pain; vaginal discharge; constitutional symps like wt. loss, malaise, anorexia, pyrexia, anemia. On p/v examination: vulvar or vaginal ulcer, thickening of tubes may be felt. D/d : Pyogenic tubo-ovarian mass; Pelvic endometriosis; Adherent ovarian cyst; C/c disturbed ectopic pregnancy. Rx : chemo – anti-TB chemo therapy is treatment of choice. Surgery in case of no response to chemo, tubercular pyosalpinx, ovarian abscess or pyometra, persistent menorrhagia and/or c/c pelvic pain. Type of Sx: ideal is total hysterectomy with B/L salpingo-oopherectomy. 136. MYOMAS OF UTERUS: ETIOLOGY, PATHOLOGICAL ANATOMY, C/F, DIAGNOSIS & D/d. Ans. ETIOLOGY : It arises from neoplastic single smooth muscle cell (myocyte) of myometrium. Thus each myoma is monoclonal. The stimulus can be chromosomal abnormality or by polypeptide growth factors. Myoma is a predominantly estrogren dependent tumour. TYPES : Mostly located in the body of uterus. A) Body (corporeal) myomas : 1. Interstitial or intramural (75%) 2. Subperitoneal or subserous (15%) i) Subserous ii) Broad ligament (pseudo) iii) Wandering (parasitic) 3. Submucous (5%) i) Sessile ii) Pedunculated (polyp) B) Cervical myomas : 1. Anterior 2. Posterior 3. Central 4. Lateral C/F : symptoms – 152 | P a g e ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ Majority asymp (75%) AUB (30%): menorrhagia, metrorrhagia. Dysmenorrhea Dyspareunia Subfertility Pressure syms (bladder, ureter and rectum) Recurrent pregnancy loss (miscarriage, PTL) Lower abd or pelvic pain Abd enlargement Signs✓ Palpation- feel is firm, more toward hard; well defined margins; nodular surface; restricted mobility from above downwards but ccan be moved side to side. ✓ Percussion- swelling is dull on percussion. ✓ Pelvic examination- Bimanual examination reveals uterus is irregularly enlarged by the swelling felt per abd. DIAGNOSIS : o TVS o Colour doppler o Saline infusion sonography o Hysteroscopy o HSG o MRI o Uterine curettage o Laparoscopy D/D : a) b) c) d) e) f) Pregnancy Adenomyosis Myohyperplasia Ovarian tumor TO mass Full bladder 153 | P a g e 137. SECONDARY CHANGES: DEGENRATIONS AND OTHER COMPLICATIONS OF MYOMAS. Ans.: Degenerations occur as the tumor grows outside its blood supply. A. Hyaline degeneration- m/c (65%). B. Cystic degeneration- common in interstitial fibroids. Formed by liquefaction of areas with hyaline changes. C. Myxomatous degeneration is common (15%)- occurs mainly in central part of myoma. Smooth muscle cells undergo myxomatous changes. D. Fatty degeneration- fat globules are mainly deposited in muscle cells. E. Calcific degeneration- usually involves subserous fibroids with small pedicle. Precipitation of calcium carbonate and phosphate within the tumor. Womb stone appearance when complete tumor is coverted in calcific mass. F. Red degeneration (carneous change) G. Atrophy H. Necrosis I. Infections J. Vascular changes K. Sarcomatous changes COMPLICAIONS : H’ge Torsion of subserous pedunculated fibroid Polycythemia Persistent menorrhagia, metrorrhagia → severe anemia Severe infections leading to peritonitis or septicemia. Sarcoma (rare) 154 | P a g e 138. INDICATIONS FOR TREATMENT OF MYOMAS. Ans.: Indications for myomectomy : ▪ Persistent uterine bleeding despite medical therapy. ▪ Excessive pain or pressure symptoms. ▪ Size >2 weeks, woman desirous to have a baby. ▪ Unexplained infertility with distortion of the uterine cavity. ▪ Recurrent pregnancy wastage due to fibroid. ▪ Rapidly growing myoma during follow-up. ▪ Subserous pedunculated fibroid Indications for emergency surgery for fibroid : ▪ Torsion of a subserous pedunculated fibroid. ▪ Massive intraperitoneal haemorrhage following rupture of veins over subserous fibroid. ▪ Uncontrolled infected fibroid. ▪ Uncontrolled bleeding fibroid. 139. MEDICAL TREATMENT OF MYOMAS. Ans.: As a temporary palliation, various drugs are used to minimize blood loss and correct anemia when a definite surgery cannot be undertaken for certain periods. Antiprogesterones—Mifepristone (RU 486) is very effective to reduce fibroid size and also menorrhagia. It may produce amenorrhea. It reduces the size of the fibroid significantly. A daily dose of 25–30 mg is recommended for 3 months. 5 mg daily dose is also found effective. Long-term therapy is avoided as it causes endometrial hyperplasia. Asoprisnil is used with success. It is a selective progesterone receptor modulator. It does not cause endometrial hyperplasia. Danazol—can reduce the volume of a fibroid slightly. Because of androgenic side effects, danazol is used only for a period of 3–6 months. Danazol administered daily in divided doses ranging from 200-400 mg for 3 months minimizes blood loss or even produce amenorrhea by its antigonadotropin and androgen agonist actions. Levonorgestrel-releasing Intrauterine System (LNG-IUS) reduces blood loss and uterine size. However, this is not recommended when the uterine size is >12 weeks or there is distortion of uterine cavity. 155 | P a g e GnRH agonists—Drugs commonly used are goserelin, luporelin, buserelin or nafarelin. Mechanism of action is sustained pituitary down regulation and suppression of ovarian function. Optimal duration of therapy is 3 months. Addback therapy may be needed to combat hypestrogenic symptoms. GnRH antagonists—Cetrorelix or ganirelix causes immediate suppression of pituitary and the ovaries. They do not have the initial stimulatory effect. Benefits are same as that of agonists . Onset of amenorrhea is rapid. Prostaglandin synthetase inhibitors—These are used to relieve pain due to associated endometriosis or degeneration of the fibroid. They cannot improve menorrhagia due to fibroids. Non-hormonal options : Tranexamic acid; aromatase inhibitors; prostaglandin synthetase inhibitos (PSI). 140. SURGICAL TREATMENT OF MYOMAS. Myomectomy is a surgical procedure performed to remove uterine fibroids, also known as myomas. Myomectomy is typically performed on women who want to preserve their uterus and have future pregnancies. Here is some information on indications, types, techniques, and complications of myomectomy: Indications: • Fibroids causing heavy menstrual bleeding and anemia • Fibroids causing pressure and pain in the pelvis • Infertility associated with fibroids • Fibroids causing recurrent miscarriage Types of myomectomy: 1. Abdominal myomectomy: This is the traditional approach to myomectomy and involves making a large incision in the abdomen to access the uterus. 2. Laparoscopic myomectomy: This is a minimally invasive approach that involves making small incisions in the abdomen and using a laparoscope (a thin, lighted tube with a camera) to guide the surgery. 3. Hysteroscopic myomectomy: This is a minimally invasive approach that involves accessing the uterus through the cervix and using a hysteroscope (a thin, lighted tube with a camera) to guide the surgery. 156 | P a g e Techniques: • Open surgery (abdominal myomectomy) involves making a large incision in the abdomen and accessing the uterus to remove the fibroids. • Laparoscopic surgery involves making small incisions in the abdomen and using specialized surgical instruments to remove the fibroids. • Hysteroscopic surgery involves accessing the uterus through the cervix and using a hysteroscope to remove the fibroids. Complications: • Bleeding • Infection • Injury to adjacent organs such as bladder, bowel or blood vessels • Scarring • Adhesion formation • Uterine rupture during subsequent pregnancies It is important to discuss the risks and benefits of myomectomy with your doctor to determine the most appropriate treatment for your individual case. 141. 142. ENDOMETRIOSIS Ans.: Presence of functioning endometrium (glands and stroma) in sites other than uterine mucosa is called endometriosis. Theories of etiology : I. Retrograde menstruation (Sampson’s theory). II. Coelomic metaplasia (Meyer & Ivanoff) III. Direct implantation 157 | P a g e IV. V. VI. VII. Lymphatic theory (Halban) Vascular theory Genetic and immunological factors Environment theory Sites : I. Abdominal II. Extra-abdominal III. Remote Common sites - Ovaries • Pelvic peritoneum • Pouch of Douglas • Uterosacral ligaments • Rectovaginal septum • Sigmoid colon • Appendix • Pelvic lymph nodes • Fallopian tubes Rare and remote sites - Umbilicus Abdominal scar Episiotomy scar Lungs Pleura Ureter Kidney Arms Legs Nasal mucosa CF : ➢ Dysmenorrhea ➢ abN menstruation ➢ Infertility ➢ Dyspareunia ➢ c/c pelvic pain ➢ abd pain ➢ Other Symptoms The symptoms are related to the organ involved. Urinary—frequency, dysuria, back pain or even haematuria Sigmoid colon and rectum—painful defecation (dyschezia), diarrhea, constipation, rectal bleeding or even melena Chronic fatigue, perimenstrual symptoms (bowel, bladder) Haemoptysis (rarely), catamenial chest pain Surgical scars—cyclical pain and bleeding Diagnosis – Clinical diagnosis, serum marker CA 125, Imaging (TVS, MRI, CT, Colonoscopy), Laparoscopy (gold std). D/d – ✓ C/c pelvic infection ✓ Ovarian endometrioma (chocolate cysts) ✓ Rupture of chocolate cyst Treatment – can be preventive or curative. 158 | P a g e Options : Expectant Management (observation only) Medical Therapy: • Hormones • Others Surgery: • Conservative • Definitive Combined Therapy: • Medical and Surgical 143. MEDICAL MANAGEMENT OF ENDOMETRIOSIS. Ans.: The aim of the hormonal treatment is to induce atrophy of the endometriotic implants. The drugs used are combined estrogen and progestogen (oral pill), progestogens, danazol and GnRH analogues. All the drugs are used continuously to produce amenorrhea and as such individualization of the dose is required. Combined estrogen and progestogen - It causes endometrial decidualization and atrophy . It may induce amenorrhea. It relieves dysmenorrhea. Progestogens – High doses may suppress ovulation and induce amenorrhea. Oral route is commonly used. Levonorgesteral-releasing-IUCD - reduces dysmenorrhea, pelvic pain, dyspareunia and menorrhagia significantly. It is specially useful for rectovaginal endometriosis. Danazol - started from the day 5 of the menstrual cycle. The dose (600–800 mg daily) is variable and depends upon the extent of the lesions but should be adequate enough to produce amenorrhea. The patient should use barrier methods of contraception to avoid virilization of a female fetus in accidental pregnancy. GnRH analogues - When used continuously act as medical oophorectomy, a state of hypoestrinism and amenorrhea. The goal is to maintain a reduced level of serum estrogen (30–45 pg/mL) so that growth of endometriosis is suppressed. 144. SURGICAL TREATMENT OF ENDOMETRIOSIS. Ans.: Can be conservative and definitive : Conservative - planned to destroy the endometriotic lesions in an attempt to improve the symptoms (pain, subfertility) and at the same time to preserve the reproductive function. Laparoscopy is commonly done to destroy endometriotic lesions by excision or 159 | P a g e ablation by electrodiatherapy or by laser vaporization. Conservative surgical treatment in minimal to mild endometriosis (ablation plus adhesiolysis) improves the fertility outcome. Laparoscopic uterosacral nerve ablation (LUNA) is done when pain is very severe. Definitive surgery - It is indicated in women with advanced stage endometriosis where there is: (i) No prospect for fertility improvement. (ii) Other forms of treatment have failed. (iii) Women with completed family. Definitive surgery means hysterectomy with bilateral salpingo-oophorectomy along with resection of the endometrial tissues as complete as possible 145. ADENOMYOSIS. Ans.: Adenomyosis is a condition where there is ingrowth of the endometrium, both the glandular and stromal components, directly into the myometrium. Pathological anatomy : Characterized by the extension of endometrial glands and stroma beneath the endometrial—myometrial interface (EMI). As the submucosa is absent, endometrial glands lie in direct contact with the underlying myometrium. It forms nests, deep within myometrium. Subsequently, threre is myometrial hyperplasia around the endometriotic foci. Symptoms :➢ Menorrhagia (70%) ➢ Dysmenorrhea (30%) ➢ Dyspareunia ➢ Frequency of urination ➢ Infertility Signs :➢ Abd exm → A hypogastric mass arising out of the pelvis and occupying the midline. The size usually does not exceed 14 weeks pregnant uterus. ➢ Pelvic examination → Reveals uniform enlargement of the uterus. Diagnosis :➢ TVS ➢ Color doppler 160 | P a g e ➢ MRI Treatment :➢ Surgical management:→ (A) Conservative surgery: • Adenomyomectomy • Uterine mass reduction (Laparotomy or laparoscopy). (B) Hysterectomy (parous and aged women). ➢ There is little place of hormone therapy. Treatment with progestins or cyclic estrogen and progestin have got little benefit. Levonorgestrel– releasing-IUS is found to improve the menorrhagia and dysmenorrhea. Danazol—loaded (300–400 mg) intrauterine device (IUD) is also found to improve the symptoms of menorrhagia and dysmenorrhea. 146. Prophylaxis of endometriosis. Endometriosis is a chronic condition in which the tissue that normally lines the inside of the uterus (endometrium) grows outside of it, causing pain, inflammation, and sometimes infertility. Unfortunately, there is no known way to completely prevent endometriosis from developing. However, there are some measures that may help reduce the risk of developing the condition or help manage the symptoms: ✓ Maintain a healthy weight. ✓ Manage stress. ✓ Avoid environmental toxins. ✓ Consider hormonal birth control: Hormonal birth control methods such as birth control pills, patches, or hormonal IUDs can help reduce the risk of developing endometriosis by preventing ovulation and reducing the growth of endometrial tissue outside the uterus. ✓ Surgical options: In some cases, surgery may be recommended to remove endometrial tissue and prevent its growth. This is typically done through laparoscopic surgery and may be helpful in reducing pain and other symptoms. 161 | P a g e 147. Acute abdomen: definition, causes. Acute abdomen in obstetrics refers to the sudden onset of severe abdominal pain in pregnant women, which may be accompanied by other symptoms such as vaginal bleeding, fever, and contractions. Acute abdomen in obstetrics is a medical emergency that requires prompt evaluation and treatment, as it may indicate a serious underlying condition that requires urgent intervention. Some of the common causes of acute abdomen in obstetrics include: 1. Ectopic pregnancy: This is a pregnancy that develops outside the uterus, typically in the fallopian tube. An ectopic pregnancy can cause an acute abdomen and requires prompt medical attention. 2. Miscarriage: A miscarriage is the loss of a pregnancy before the 20th week. It can cause an acute abdomen and is often accompanied by vaginal bleeding. 3. Placental abruption: This is a serious condition in which the placenta partially or completely separates from the uterus before the baby is born. Placental abruption can cause an acute abdomen, vaginal bleeding, and can be life-threatening for both the mother and the baby. 4. Uterine rupture: This is a rare but serious condition in which the uterus tears during pregnancy or labor. Uterine rupture can cause an acute abdomen, severe vaginal bleeding, and can be life-threatening for both the mother and the baby. 5. Ovarian torsion: This is a condition in which the ovary twists on itself, which can cause an acute abdomen and severe pain. Ovarian torsion is rare but can occur during pregnancy. 6. Acute appendicitis: Although rare, acute appendicitis can occur during pregnancy and can cause an acute abdomen. 162 | P a g e 148. Follicular hematomas, corpus luteal haematomas, torsion and rupture of ovarian tumours, torsion of myomas: symptoms and sings, diagnosis and management. Ans.: Follicular hematomas and corpus luteal hematomas are both related to the ovary. A follicular hematoma occurs when bleeding occurs within a developing follicle in the ovary, while a corpus luteal hematoma occurs when there is bleeding into a corpus luteum, which is the structure that forms after the release of an egg from the ovary. These hematomas can present with symptoms such as abdominal pain, bloating, and vaginal bleeding. Diagnosis is made through ultrasound imaging, and management typically involves observation and pain management. Ovarian tumors can also cause torsion or rupture, leading to symptoms such as sudden, severe abdominal pain, nausea, and vomiting. Diagnosis is made through imaging such as ultrasound or CT scan, and management may involve surgery to remove the affected ovary and tumor. Torsion of myomas, or fibroids, can also present with sudden, severe abdominal pain and can be diagnosed through imaging such as ultrasound. Management may involve surgery to remove the affected fibroid or the uterus if necessary. Overall, early diagnosis and appropriate management are important in these gynecological conditions to prevent complications and promote recovery. 149. Ectopic gestation: incidence, aetiology, classification, pathological anatomy. 163 | P a g e Ectopic pregnancy refers to the implantation of a fertilized egg outside the uterine cavity, most commonly in the fallopian tube. It is a potentially lifethreatening condition that requires prompt diagnosis and treatment. The incidence of ectopic pregnancy is approximately 1-2% of all pregnancies, and the most common risk factors include previous pelvic inflammatory disease, previous ectopic pregnancy, tubal surgery, assisted reproductive technology, and smoking. Ectopic pregnancies can be classified based on their location, with the most common being tubal ectopic pregnancy. Other locations include the ovary, cervix, abdominal cavity, and cesarean scar. Pathologically, ectopic pregnancy is characterized by the presence of chorionic villi outside the uterine cavity. The implantation of the fertilized egg outside the uterus can lead to a range of complications, including tubal rupture, hemorrhage, and shock. Diagnosis of ectopic pregnancy typically involves a combination of clinical evaluation, ultrasound imaging, and laboratory tests, including serial serum betahCG measurements. Treatment options depend on the location and severity of the ectopic pregnancy, as well as the patient's clinical condition. Options may include medical management with methotrexate or surgical management with laparoscopy or laparotomy. 150. Tubal pregnancy: pathological anatomy, clinical symptoms, physical signs, diagnostic investigations, differential diagnosis, management. Tubal pregnancy, also known as ectopic pregnancy, is a type of pregnancy where the fertilized egg implants outside of the uterus, most commonly in the fallopian tube. Pathological anatomy: 164 | P a g e • • The fertilized egg implants and grows in the fallopian tube, which is not designed to support a developing embryo. As the embryo grows, the tube may rupture, causing internal bleeding. Clinical symptoms: • • • • Abdominal pain, often on one side Vaginal bleeding Missed menstrual period Signs of shock (if the tube ruptures), including lightheadedness, fainting, rapid heart beat, and low blood pressure. Physical signs: • • • Tenderness and pain on one side of the abdomen or pelvis Abnormal vaginal bleeding An enlarged or mass-like structure felt on pelvic exam. Diagnostic investigations: • • • Transvaginal ultrasound: This is the most common method for diagnosing tubal pregnancy. It uses high-frequency sound waves to create an image of the pelvic organs. Blood tests: Measuring the levels of the hormone human chorionic gonadotropin (hCG) can help diagnose ectopic pregnancy. Laparoscopy: This is a minimally invasive surgical procedure where a small camera is inserted through a small incision in the abdomen to visualize the pelvic organs and confirm the diagnosis. Differential diagnosis: • • • • Miscarriage Ovarian cyst rupture Appendicitis Pelvic inflammatory disease. Management: 165 | P a g e • • • Treatment depends on the location of the ectopic pregnancy, the size of the embryo, and the overall health of the patient. In some cases, medication (such as methotrexate) can be used to stop the growth of the embryo and cause it to be reabsorbed by the body. If the ectopic pregnancy is large or has caused significant internal bleeding, surgery (such as a salpingectomy or salpingostomy) may be necessary to remove the embryo and repair any damage to the fallopian tube. 151. Unruptured ectopic gestation: definition, symptonis and sings, diagnosis. treatment. Unruptured ectopic gestation, also known as tubal pregnancy, refers to an ectopic pregnancy that has not yet ruptured. Symptoms and signs of an unruptured ectopic gestation are similar to those of a ruptured ectopic pregnancy, but they may be less severe. These symptoms may include vaginal bleeding, abdominal or pelvic pain, and shoulder pain. However, in some cases, an unruptured ectopic pregnancy may have no symptoms and may be detected only during routine prenatal care or ultrasound. Diagnosis of an unruptured ectopic pregnancy may involve transvaginal ultrasound to visualize the gestational sac outside the uterus, as well as blood tests to monitor pregnancy hormone levels. Treatment of an unruptured ectopic pregnancy typically involves medical management with methotrexate, a medication that stops the growth of the pregnancy and allows the body to reabsorb it. In some cases, surgery may be necessary if the pregnancy is large or if there is a risk of rupture. Close monitoring is also important to ensure that the pregnancy is resolving and that there are no complications. 166 | P a g e 152. Surgically administered medical treatment of ectopic pregnancy: criteria for metotrexate treatment, technique, advantages and disadvantages. prognosis Surgically administered medical treatment of ectopic pregnancy involves the use of methotrexate, a medication that stops the growth of rapidly dividing cells, to treat ectopic pregnancy that is not ruptured or has minimal bleeding. The criteria for methotrexate treatment include: 1. The size of the gestational sac: The gestational sac should be less than 4 cm in diameter and the embryo should be less than 3.5 cm. 2. The level of human chorionic gonadotropin (hCG): The hCG level should be less than 5000 mIU/mL, and should not have risen by more than 10% over 48 hours. 3. The absence of fetal cardiac activity: Methotrexate is not effective in treating ectopic pregnancies where there is fetal cardiac activity. The technique for methotrexate treatment involves a single or multiple injections of the medication into the muscle or directly into the gestational sac under ultrasound guidance. The medication stops the growth of the pregnancy, and the body then reabsorbs the tissue over time. Advantages of methotrexate treatment include: 1. It is a non-invasive treatment option and does not require surgery. 2. It preserves the woman's fertility. 3. It has a high success rate, with success rates of up to 90% reported in studies. Disadvantages of methotrexate treatment include: 1. It may cause side effects such as nausea, vomiting, and abdominal pain. 2. It may require multiple injections over several weeks. 3. It may not be effective in all cases, particularly in cases of larger or more advanced ectopic pregnancies. 4. It requires close monitoring of the woman's hCG levels and symptoms. The prognosis for women who receive methotrexate treatment for ectopic pregnancy is generally good, with a high success rate and low rate of 167 | P a g e complications. However, close monitoring is necessary to ensure that the pregnancy is resolving appropriately and to identify any potential complications. 153. Interstitial pregnancy: pathological anatomy, clinical symptoms, physical signs, diagnostic investigations, differential diagnosis, treatment. Interstitial pregnancy is a rare type of ectopic pregnancy that occurs when the fertilized egg implants within the interstitial portion of the fallopian tube as it enters the uterine wall. It represents approximately 2-4% of all ectopic pregnancies and carries a high risk of maternal morbidity and mortality. The clinical presentation of an interstitial pregnancy is similar to that of a tubal pregnancy and includes lower abdominal pain, vaginal bleeding, and amenorrhea. However, in some cases, the symptoms may be less severe, and the diagnosis may be delayed. On physical examination, the uterus may be enlarged, and adnexal mass may be palpable on bimanual examination. However, the diagnosis of interstitial pregnancy is usually made with the help of diagnostic imaging, such as transvaginal ultrasound or magnetic resonance imaging (MRI). In transvaginal ultrasound, a gestational sac located in the interstitial portion of the tube, separate from the uterine cavity, is considered diagnostic of interstitial pregnancy. MRI may provide additional information on the extent of the pregnancy and the involvement of adjacent structures. The treatment of interstitial pregnancy depends on the severity of symptoms, the size of the gestational sac, and the desire for future fertility. Options include expectant management, medical management with methotrexate, and surgical management with laparotomy or laparoscopy. Expectant management may be an option in cases of small gestational sacs with low levels of human chorionic gonadotropin (hCG) and stable clinical condition. 168 | P a g e However, this approach carries a risk of rupture and severe bleeding, and close monitoring is necessary. Medical management with methotrexate is an effective option in selected cases. The criteria for methotrexate treatment include a hemodynamically stable patient, a gestational sac with a diameter of less than 3.5 cm, an ectopic mass that is not growing, and a low level of hCG. Methotrexate is administered by injection and works by stopping the growth of the ectopic pregnancy. Surgical management is necessary in cases of rupture, unstable clinical condition, or failure of medical management. Laparoscopy is the preferred method for surgical management of interstitial pregnancy, as it allows for better visualization and preservation of fertility. The prognosis for interstitial pregnancy depends on the timing of diagnosis and appropriate treatment. Delay in diagnosis or inappropriate management can result in severe bleeding, damage to the fallopian tube, and the need for a hysterectomy. Early diagnosis and appropriate management can result in a successful pregnancy outcome and preservation of fertility. 154. Cervical pregnancy: clinical symptoms, physical signs, diagnostic investigations, treatment. Cervical pregnancy is a rare form of ectopic pregnancy that occurs when the fertilized egg implants in the cervical canal instead of the uterine cavity. It is a lifethreatening condition that requires prompt diagnosis and management. Clinical symptoms of cervical pregnancy may include vaginal bleeding, abdominal pain, and cramping. Physical examination may reveal a soft and enlarged cervix, and ultrasound imaging can help confirm the diagnosis. Diagnostic investigations for cervical pregnancy may include transvaginal ultrasound, hysteroscopy, and magnetic resonance imaging (MRI). 169 | P a g e Treatment for cervical pregnancy usually involves the removal of the fetus and placenta to prevent severe bleeding and infection. This can be done using several approaches, including suction curettage, dilatation and curettage (D&C), or hysteroscopy. In some cases, a cervical cerclage may be placed to prevent future cervical pregnancies. It is important to note that cervical pregnancy is a high-risk condition, and complications can include severe bleeding, infection, and damage to the cervix or uterus. Women who have had a cervical pregnancy should receive close monitoring and follow-up care to ensure their health and fertility. 155. Abdominal pregnancy: pathological anatomy, clinical features, diagnosis, treatment. Abdominal pregnancy is a rare form of ectopic pregnancy where the fertilized egg implants in the abdominal cavity outside the uterus. It accounts for less than 1% of all ectopic pregnancies. Here are some of the clinical features, diagnosis, and treatment options for abdominal pregnancy: Clinical features: • • • • Lower abdominal pain Vaginal bleeding Absence of fetal parts felt on vaginal examination Abdominal mass Diagnosis: • • • Ultrasound imaging to confirm the location of the pregnancy Elevated serum beta-hCG levels MRI (magnetic resonance imaging) may also be used to confirm the diagnosis Treatment: 170 | P a g e Abdominal pregnancy is considered a life-threatening condition that requires prompt intervention. Treatment options include: 1. Surgical removal of the pregnancy: • • • This is the preferred treatment option for abdominal pregnancy. The surgical approach will depend on the location of the placenta and its attachment to surrounding organs. In some cases, a hysterectomy may be necessary to remove the placenta completely. Medical management: • • • In some cases, methotrexate (a chemotherapy drug) may be used to stop the growth of the pregnancy and dissolve the placenta. This approach is only used in cases where the pregnancy is small and not well-attached to surrounding organs. Close monitoring is required to ensure the success of the treatment. Expectant management: • • This approach involves close monitoring of the patient's condition and waiting for the pregnancy to naturally terminate. It is only used in cases where the pregnancy is small, the patient is stable, and the risk of bleeding is low. Overall, the prognosis for abdominal pregnancy is generally poor, with a high risk of maternal morbidity and mortality. Early diagnosis and prompt intervention are essential for the best possible outcome. 171 | P a g e 156. Ovarian pregnancy: pathological anatomy, clinical features. diagnosis, treatment. Ovarian pregnancy is a rare form of ectopic pregnancy in which the fertilized egg implants in the ovary. It is estimated to occur in approximately 1 in 7,000 to 1 in 40,000 pregnancies. Pathological anatomy: The implantation of the fertilized egg occurs within the ovary, and as the pregnancy progresses, a gestational sac is formed. The ovary may enlarge, and there may be hemorrhage into the ovarian tissue. Clinical features: The clinical presentation of an ovarian pregnancy is similar to that of other forms of ectopic pregnancy, including abdominal pain, vaginal bleeding, and a positive pregnancy test. However, the symptoms may be milder than in tubal ectopic pregnancy, and the diagnosis may be delayed. Diagnosis: The diagnosis of ovarian pregnancy is made based on clinical suspicion, ultrasound findings, and laboratory tests. Ultrasound may show a gestational sac within the ovary, and serum beta-human chorionic gonadotropin (beta-hCG) levels may be elevated. Treatment: The treatment of ovarian pregnancy is typically surgical, with the removal of the affected ovary (oophorectomy) being the most common approach. In some cases, conservative surgery, such as partial oophorectomy, may be attempted in order to preserve ovarian function. In rare cases, medical management with methotrexate may be attempted, although this is not typically the first-line treatment for ovarian pregnancy. The prognosis for ovarian pregnancy is generally good, particularly when diagnosed and treated promptly. However, there is a risk of ovarian damage or loss, and fertility may be affected in some cases. Close follow-up is typically recommended after treatment. 172 | P a g e 157. Genital prolapse: aetiology, classification, clinical symptoms, investigations, differential diagnosis, management and prophylaxis. Genital prolapse is a condition where there is descent of one or more of the pelvic organs, including the uterus, vagina, bladder, or rectum, from their normal anatomical position. Aetiology: Genital prolapse is primarily caused by weakness or damage to the muscles, ligaments, and fascia that support the pelvic organs. Factors that increase the risk of genital prolapse include pregnancy, childbirth, menopause, aging, obesity, chronic coughing, heavy lifting, and chronic constipation. Classification: Genital prolapse can be classified according to the organs involved, as well as the severity of the condition. The organs involved can include the uterus (uterine prolapse), vagina (vaginal prolapse), bladder (cystocele), and rectum (rectocele). The severity of the condition is typically classified into four grades, with grade I being the mildest and grade IV being the most severe. Clinical symptoms: The symptoms of genital prolapse can vary depending on the organs involved and the severity of the condition. Common symptoms include a sensation of pressure or fullness in the pelvic area, a feeling of something protruding from the vagina, urinary incontinence or urgency, constipation, difficulty with bowel movements, and discomfort or pain during intercourse. Investigations: The diagnosis of genital prolapse is usually made based on a pelvic examination. Further investigations may include a cystoscopy, to evaluate the bladder, and a proctoscopy, to evaluate the rectum. Imaging studies, such as ultrasound, MRI or CT scan, may be necessary in cases of complex prolapse or if malignancy is suspected. Differential diagnosis: 173 | P a g e Other conditions that may present with similar symptoms include urinary tract infections, cystitis, bladder cancer, rectal prolapse, uterine fibroids, and ovarian cysts. Management and prophylaxis: Treatment options for genital prolapse depend on the severity of the condition and the organs involved. Conservative treatment measures may include estrogen replacement therapy may improve minor degree prolapse in postmenopausal women, pelvic floor muscle exercises (kegel exercises), lifestyle modifications, and pessaries. In more severe cases, surgery may be necessary. Type of operation depends upon the organ which is prolapsed. Prophylaxis includes maintaining a healthy weight, regular exercise, avoiding heavy lifting, and treating chronic conditions such as constipation and chronic coughing. Pelvic floor muscle exercises can also be done to prevent genital prolapse. 158. Retroversion of the uterus: aetiology, symptoms, diagnosis, treatment. Retroversion of the uterus, also known as tilted or tipped uterus, is a condition in which the uterus is tilted backward instead of forward. The cause of retroversion of the uterus is often unknown, but it can be congenital or acquired as a result of conditions such as endometriosis, fibroids, pelvic inflammatory disease, or pregnancy. In many cases, retroversion of the uterus is asymptomatic and does not require treatment. However, some women may experience symptoms such as lower back pain, painful intercourse, urinary incontinence, or difficulty inserting tampons. 174 | P a g e Diagnosis of retroversion of the uterus can be done through a pelvic exam or imaging studies such as ultrasound or MRI. Corrective treatment : Pessary and surgical. Pessary is less commonly used in present day gynaecologic practice. Usually, Hodge-Smith pessary is used. The pessary acts by stretching the uterosacral ligaments so as to pull the cervix backwards. The principle of surgical correction is ventro-suspension of the uterus by plicating the round ligaments of both the sides extraperitoneally to the under surface of the anterior rectus sheath . This will pull the uterus forwards and maintains it permanently in the same position. Women with retroversion of the uterus can take steps to prevent symptoms from occurring or worsening, such as practicing good posture, doing exercises to strengthen the pelvic floor muscles, and avoiding heavy lifting. 159. Acute inversion of the uterus: aetiology, pathological anatomy, symptoms, diagnosis and treatment. Acute inversion of the uterus is a rare but serious obstetric emergency that occurs when the uterus turns inside out and prolapses into or beyond the vagina. The aetiology of acute inversion of the uterus includes the following factors: 1. 2. 3. 4. Over traction of the uterus during the third stage of labor Fundal pressure during the third stage of labor Abnormal attachment of the placenta Uterine anomalies or tumors The symptoms of acute inversion of the uterus include sudden, severe abdominal pain, shock, and heavy vaginal bleeding. The uterus may be palpable as a mass protruding from the vagina. In some cases, the uterus may be completely inverted and not palpable. 175 | P a g e Diagnosis of acute inversion of the uterus is usually made based on clinical presentation and physical examination findings. A pelvic examination will reveal a prolapsed uterus, which is usually a rounded, smooth mass protruding from the vagina. Imaging tests such as ultrasound may be used to confirm the diagnosis and rule out other causes of uterine prolapse. Immediate treatment of acute inversion of the uterus is necessary to prevent severe bleeding and shock. Treatment includes replacement of the uterus to its normal position. This can be done manually, by applying pressure to the fundus while the patient is under general anesthesia. In some cases, the use of tocolytic drugs may be necessary to relax the uterus and facilitate replacement. If conservative measures fail, surgery may be necessary to reposition the uterus. 160. Chronic inversion of the uterus: actiology. pathological anatomy, symptoms, diagnosis and treatment. Chronic inversion of the uterus is a rare condition that occurs when the uterus remains partially or completely inverted after delivery. The causes of chronic inversion of the uterus may include incomplete or improper management of acute inversion, uterine tumors, Senile inversion following high amputation of the cervix. It is probably due to cervical atony and incompetence and congenital abnormalities of the uterus. The pathological anatomy of chronic inversion of the uterus may vary depending on the severity and duration of the condition. The uterus may be partially or completely inverted, and there may be varying degrees of prolapse of the cervix and vagina. The condition may also be associated with the formation of adhesions or scar tissue, which can further complicate treatment. Symptoms of chronic inversion of the uterus may include pelvic pain, vaginal discharge, and abnormal bleeding. In some cases, the prolapsed uterus may be visible or palpable through the vaginal opening. Chronic inversion of the uterus 176 | P a g e can also lead to infertility or difficulty conceiving, as well as other complications such as infections and bowel or bladder dysfunction. Diagnosis of chronic inversion of the uterus may involve a physical exam, imaging studies such as ultrasound or magnetic resonance imaging (MRI), and possibly a hysteroscopy or laparoscopy to evaluate the uterine tissue and confirm the diagnosis. Treatment of chronic inversion of the uterus typically involves surgical intervention. The goal of treatment is to restore the uterus to its normal position and function, while minimizing the risk of complications such as bleeding or infection. The specific approach to treatment may vary depending on the severity and duration of the condition, as well as the presence of any associated complications. In some cases, a hysterectomy may be necessary to fully resolve the condition. Conservative surgery: Rectification may be done abdominally (Haultain’s operation — after cutting the posterior ring of the cervix) or vaginally (Spinelli‘s operation — after cutting the anterior ring of the cervix). 161. Non-neoplastic enlargements of the ovary (follicular cysts. lutein cysts of the ovary, polycystic ovarian syndrome): aetiology. pathological anatomy, symptoms, diagnosis and treatment. Non-neoplastic enlargements of the ovary include follicular cysts, lutein cysts of the ovary, and polycystic ovarian syndrome (PCOS). Follicular cysts arise from the unruptured follicles in the ovary. Normally, a follicle ruptures during ovulation, releasing an egg. If this does not occur, the follicle may continue to grow and form a cyst. Most of these cysts are asymptomatic, but in some cases, they can cause pelvic pain, pressure, or bloating. Diagnosis is usually made through ultrasonography, and most follicular cysts will resolve on their own without treatment. 177 | P a g e Lutein cysts of the ovary are another type of functional cyst that can form after ovulation. These cysts can grow to several centimeters in size and may cause abdominal pain, bloating, or irregular menstrual bleeding. Like follicular cysts, most lutein cysts will resolve on their own without treatment. PCOS is a common hormonal disorder that affects women of reproductive age. It is characterized by multiple small cysts on the ovaries, irregular menstrual cycles, and high levels of androgens (male hormones) in the body. Women with PCOS may also experience weight gain, acne, and excess hair growth. Diagnosis is made through a combination of clinical symptoms, physical examination, and laboratory tests. Treatment options include lifestyle modifications, such as weight loss and exercise, and medications to regulate ovulation and hormone levels. In general, non-neoplastic enlargements of the ovary are benign and can be managed conservatively. However, in rare cases, these cysts can become large or twisted, causing severe pain or other complications. In these instances, surgical intervention may be necessary. 162. Parovarian cysts: pathological anatomy, symptoms, diagnosis and treatment. Parovarian cysts, also known as paraovarian cysts or hydatid cysts of Morgagni, are fluid-filled sacs that develop from the remnants of the Wolffian duct and the Mullerian ducts, which are structures that form during embryonic development. They are typically small and benign, and most women with parovarian cysts do not experience any symptoms. However, if the cyst grows larger, it may cause symptoms such as pelvic pain, discomfort, or a feeling of heaviness in the lower abdomen. Parovarian cysts can be diagnosed using imaging techniques such as ultrasound, CT scans, or MRI. In some cases, a doctor may perform a laparoscopy to visualize the cyst directly and determine its size and location. The treatment for parovarian cysts usually depends on the size of the cyst and the severity of symptoms. Small 178 | P a g e cysts that do not cause any symptoms may not require any treatment and can be monitored with regular check-ups. Larger cysts or cysts that cause symptoms may require surgical removal, which is typically done using laparoscopy or laparotomy. In summary, parovarian cysts are small, benign cysts that develop from the remnants of embryonic ducts. They can cause symptoms such as pelvic pain and discomfort, and can be diagnosed using imaging techniques. Treatment may include monitoring, or surgical removal if the cyst is large or causes symptoms. 163. Ovarian tumours: epidemiology, pathology, classification. Ovarian tumors are neoplasms that arise from the ovary. They can be benign (non-cancerous) or malignant (cancerous). Ovarian tumors are relatively common and can affect women of all ages, although they are more common in women over the age of 50. The majority of ovarian tumors arise from the epithelial cells that cover the surface of the ovary. These tumors are known as epithelial ovarian tumors and account for approximately 90% of all ovarian tumors. Other types of ovarian tumors include germ cell tumors, which arise from the cells that give rise to eggs, and sex cord-stromal tumors, which arise from the cells that produce hormones. Ovarian tumors can be classified as benign, borderline (also known as low malignant potential), or malignant. Benign ovarian tumors are non-cancerous and do not spread to other parts of the body. Borderline tumors have some features of cancer, but they do not invade surrounding tissue or spread to other parts of the body. Malignant ovarian tumors are cancerous and can spread to other parts of the body. The symptoms of ovarian tumors can vary depending on the type of tumor and whether it is benign or malignant. Common symptoms of ovarian tumors include abdominal pain, bloating, and a feeling of fullness or pressure in the abdomen. 179 | P a g e Other symptoms may include changes in bowel or bladder habits, abnormal vaginal bleeding, and weight loss. Diagnosis of ovarian tumors typically involves a combination of imaging studies, such as ultrasound or CT scans, and blood tests to measure tumor markers. If an ovarian tumor is suspected, a biopsy may be performed to confirm the diagnosis. Treatment for ovarian tumors depends on the type of tumor and whether it is benign or malignant. Benign ovarian tumors may not require treatment, but may be surgically removed if they are causing symptoms. Borderline tumors may also be surgically removed, but may require additional treatment such as chemotherapy. Malignant ovarian tumors typically require surgical removal and may also require chemotherapy and/or radiation therapy. 164. Characteristics of borderline ovarian tumours. Borderline ovarian tumors, also known as ovarian tumors of low malignant potential (LMP), are a group of tumors that exhibit some characteristics of both benign and malignant tumors. These tumors have the potential to recur and metastasize, but they do not invade the surrounding tissue as deeply as malignant tumors. Borderline ovarian tumors are relatively uncommon, accounting for approximately 10-15% of all ovarian tumors. Histologically, borderline ovarian tumors show an abnormal growth pattern of the cells that line the inside of the ovary. They often have papillary projections, which can be seen under a microscope. The cells have abnormal nuclei and mitotic figures, but they do not exhibit the stromal invasion seen in true malignant tumors. Borderline ovarian tumors can present with similar symptoms as other ovarian tumors, including abdominal pain, bloating, and irregular menstrual cycles. However, they are often detected incidentally on imaging studies or during surgery for other conditions. 180 | P a g e The treatment of borderline ovarian tumors involves surgical removal of the affected ovary and any other involved tissues. Chemotherapy may be recommended in certain cases. The prognosis for patients with borderline ovarian tumors is generally good, with a 5-year survival rate of over 90%. However, follow-up monitoring is necessary, as recurrence and metastasis can occur. 165. Epithelial tumours: pathological anatomy, symptoms and sings, diagnosis and differential diagnosis, treatment. Epithelial tumors are a type of ovarian tumor that arise from the surface epithelium of the ovary. They account for the majority of ovarian tumors and can be benign, borderline, or malignant. Pathological anatomy: Epithelial tumors are classified into serous, mucinous, endometrioid, clear cell, transitional cell, and undifferentiated subtypes based on their histology. They are characterized by the presence of cystic or solid masses on the ovary. Symptoms and signs: Epithelial tumors may present with symptoms such as abdominal distension, pelvic pain, abnormal vaginal bleeding, and urinary frequency or urgency. However, many cases are asymptomatic and are detected incidentally on imaging studies. Diagnosis and differential diagnosis: Diagnosis of epithelial ovarian tumors is made through imaging studies such as ultrasound or CT scan, as well as blood tests to measure tumor markers such as CA-125. A biopsy or surgical removal of the tumor may be necessary to confirm 181 | P a g e the diagnosis. Differential diagnosis includes other types of ovarian tumors, such as germ cell tumors and stromal tumors, as well as other conditions that may cause similar symptoms. Treatment: Treatment of epithelial ovarian tumors depends on the stage and grade of the tumor as well as the patient's age and overall health. Surgery is the mainstay of treatment and involves removal of the tumor and affected ovary and fallopian tube. Chemotherapy may be recommended for advanced or high-grade tumors, and targeted therapy may be used for tumors that express certain molecular markers. 166. Teratoma: types, pathological anatomy, symptoms and sings, diagnosis and differential diagnosis, treatment. Teratoma, also known as a dermoid cyst, is a type of ovarian tumour that arises from germ cells, which are the cells that give rise to eggs. There are two main types of teratomas: mature and immature. Mature teratomas, also called benign teratomas or dermoid cysts, are the most common type of teratoma. They are composed of mature tissues from all three embryonic layers (ectoderm, mesoderm, and endoderm), and may contain hair, teeth, bone, and other tissue types. Mature teratomas are usually asymptomatic and are often discovered incidentally on imaging studies. If they cause symptoms, it is usually due to their size, which can cause abdominal pain or discomfort. Diagnosis is typically made through imaging studies, such as ultrasound or CT scan. Treatment is surgical removal, which is curative. Immature teratomas are rare and are composed of immature or embryonic tissues. They are more likely to be cancerous or malignant, and tend to occur in 182 | P a g e younger women. Symptoms are similar to those of mature teratomas, but may also include hormonal disturbances. Diagnosis is made through imaging studies and biopsy. Treatment involves surgical removal of the tumour, along with chemotherapy and radiation therapy in some cases. 183 | P a g e 184 | P a g e 167. Feminizing tumours of the ovary: pathology, clinical features, diagnosis and treatment. Ans: Granulosa cell and theca cell: ⚫ Granulosa theca cell cancers include ovarian tumors, which consist of granulosa cells, theca cells, and fibroblasts in variable combinations. ⚫ Granulosa cells in the sex cords produce sex steroids and several peptides needed for folliculogenesis and ovulation. ⚫ They also give rise to granulosa theca cell tumors (GCT), which form about 5 percent of ovarian neoplasms and are the commonest sex cord-stromal tumors of the ovary (70 percent). Pathology: Attempts to explain the etiology of sex cord-stromal tumors resulted in two theories. The first one suggests the origin of these neoplasms from the genital ridge mesenchyme. The second theory suggests that these tumors originate from precursors within the mesonephric and coelomic epithelium. However, the exact pathophysiology has not been elucidated so far. • diagnosis: Gross appearance ⚫ Tumours vary in size, from tiny spots to large masses, with an average of 10 cm in diameter. ⚫ Tumours are oval and soft in consistency. ⚫ On cut-section, histology reveals reticular, trabecular areas with interstitial haemorrhage and Call–Exner bodies-small cyst like spaces interspersed within a Graafian follicle. Tumour marker Inhibin, a hormone, has been used as biomarker for granulosa cell tumours. Treatment: Surgery 185 | P a g e ⚫ Surgery (unilateral oophorectomy) is the primary treatment for early stage GCT tumors. Stage I (confined to the ovary) is the most common presentation and surgery is mostly curative. ⚫ As with other tumors of mesenchymal origin, lymphadenectomy has not been considered to play a role in the management of these patients. ⚫ Adjuvant therapies, traditionally chemotherapy, are given in cases of high stage disease (Stage Ic or higher) ⚫ Since overproduction of estradiol from the tumor is a feature of granulosa cell tumors, accompanying uterine pathology is common. ⚫ The process of addressing atypical hyperplasia or endometrial carcinomas subsequently would lead to computerized tomography, hysterectomy, and resection of a unilateral adnexal tumor. Chemotherapy Endocrine therapies ⚫ Endocrine therapies were initially introduced with the rationale of interrupting hormone receptor signaling to achieve antitumor effect in a mechanism that is analogous to what is done in the treatment of hormone receptor positive breast cancer. ⚫ Initial regimens included tamoxifen, and later progestins, in order to modulate estrogen receptor function. ⚫ Later, regimens added gonadotropin-releasing hormone agonists to suppress ovarian function. Radiation therapy 168. Virilizing tumours: pathology, clinical features, diagnosis, treatment. Ans: Sertoli-Leydig cell and Hilus cell : ⚫ Sertoli leydig cell tumor (arrhenoblasteras or androblastomas) 186 | P a g e androgen secreting tumor ⚫ Less frequent ⚫ It generally occurs in women under 30 years of age. ⚫ These tumors are comprised of Sertoli cells which are normally found in testes and Leydig cells which secrete testosterone. The clinical manifestations: ⚫ include the onset of amenorrhea, loss of breast tissue, virilizing effects, such as hirsutism, deepening of the voice, clitoromegaly, and a defeminizing ⚫ change in body habitus to a muscular build. ⚫ diagnosis is by the exclusion of virilizing adrenal tumors and the identification of a tumor in one ovary. Treatment is by the excision of the affected ovary. 169. Complications of ovarian tumours. Ans: Complications of ovarian cancer may include bowel obstruction, perforated colon, urinary problems, fluid in the membranes of the lungs, and bone pain. • Infection You have a higher risk of developing an infection after surgery. Symptoms may include fever, chills, sweats, cough, shivering, or swelling or redness around the incision. Vaginal Bleeding After your procedure, you might experience some vaginal bleeding, similar to a light period, typically for a few days to a few weeks. • Blood Clots You may be at risk for developing a blood clot in your pelvis or legs. To help prevent this, your medical team will encourage you to get up and walk around as soon as possible after your operation. You may also be given injections to thin your blood or be asked to wear special stockings. • Bleeding in the Abdomen or Pelvis You’ll likely lose some blood during surgery, and there’s a small chance you could bleed internally afterward. • 187 | P a g e Leg Swelling If your surgeon removes your lymph nodes, you may experience fluid buildup in your legs or, rarely, in your genital area. Tell your doctor if this occurs. • Bladder or Bowel Issues When surgeons operate on the pelvis or abdominal area, there’s a risk of damaging the bladder or bowel. • Colostomy Bag or Catheter During ovarian cancer debulking surgery (a technique to remove as much of the tumor as possible), your surgeon may remove part of the colon or bladder. Afterward, you may need to wear a colostomy bag to collect stool or a catheter to remove urine. These fixes are usually temporary. • Infertility If you have surgery to remove both your ovaries, you won’t be able to get pregnant. Your doctor can tell you about possible ways to preserve your fertility or other options. • Early Menopause Having your ovaries removed during surgery results in menopause if you haven’t already gone through it. • 170. Diagnosis of ovarian tumours. Ans: •Pelvic exam. During a pelvic exam, your doctor inserts gloved fingers into your vagina and simultaneously presses a hand on your abdomen in order to feel (palpate) your pelvic organs. The doctor also visually examines your external genitalia, vagina and cervix. * Imaging tests. Tests, such as ultrasound or CT scans of abdomen and pelvis, may help determine the size, shape and structure of ovaries. * Blood tests. Blood tests might include organ function tests that can help determine overall health. blood test for tumor markers that indicate ovarian cancer. For example, a cancer antigen (CA) 125 test can detect a protein that's often found on the surface of ovarian cancer cells. These tests can't tell whether you have cancer, but they may provide clues about diagnosis and prognosis. * Surgery. Sometimes doctor can't be certain of your diagnosis until you undergo 188 | P a g e surgery to remove an ovary and have it tested for signs of cancer. * Genetic testing. testing a sample of your blood to look for gene changes that increase the risk of ovarian cancer. Knowing you have an inherited change in your DNA helps your doctor make decisions about your treatment plan. You may wish to share the information with your blood relatives, such as your siblings and your children, since they also may have a risk of having those same gene changes. 171. Treatment of ovarian tumours. Ans: SURGERY ⚫ The type of operation you have depends on your cancer and if it's spread. Ovarian cancer is more treatable if it’s diagnosed early. ⚫ If your cancer is in the early stages (has not spread outside of your ovaries), you may have surgery to remove: * both ovaries and the fallopian tubes (bilateral salpingo-oophorectomy) * the opening to your womb from your vagina (cervix) and your womb (abdominal hysterectomy) ⚫ If the cancer has spread to other parts of your body, you may need more surgery to remove as much of it as possible. ⚫ This surgery may include removing parts of the bowel. Chemotherapy ⚫ Chemotherapy is medicine that kills cancer cells. ⚫ It may be given before and after surgery, or it may be used on its own. ⚫ It may also be used for ovarian cancer that has come back. Radiotherapy Radiotherapy uses high-energy rays of radiation to kill cancer cells. You may have radiotherapy for ovarian cancer to: * treat advanced cancer if other treatments are not right for you * help with symptoms, such as bleeding, pain or discomfort Targeted therapies 189 | P a g e ⚫ Targeted therapies are medicines that only target things that help cancer cells to grow or survive. ⚫ They may be an option for advanced ovarian cancer that has come back. Hormone therapy ⚫ Some ovarian cancers need the hormone oestrogen to grow. ⚫ Hormone treatments can block the production of oestrogen to stop some cancers from growing. ⚫ These medicines are rarely used. 172. Ovarian cancer: pathology, spread, staging, clinical features, stagin, staging investigations, management, results. Metastatic carcinomas. Ans: Pathology Histology of ovarian tumours presents wide variations and poses the greatest clinical challenge. These may be grouped as follows: ⚫ Epithelial ovarian cancers account for 80–90% of ovarian cancers. ⚫ Nonepithelial cancers account for 10–20%. These include malignancies of: (i) germ cell origin, (ii) sex cord stromal cell origin, (iii) metastatic cancers and (iv) rare malignancies like lipoid cell tumours, sarcomas Metastatic Carcinomas ⚫ Ovarian metastases are commonly from the primary growth in the gastrointestinal tract, notably the pylorus, colon and, rarely, the small bowel; they occasionally occur from the gall bladder and pancreas. ⚫ They may also occur in late carcinoma of the breast, as seen in 30% of all autopsy material from breast cancer. ⚫ Carcinomas of the corpus (10%) and cervix (1%) also metastasize to the ovary owing to the close relationship of their lymphatic drainage. 190 | P a g e ⚫ Carcinoma of the corpus is 10 times more likely to metastasize to the ovary than the cervix. P ⚫ The reason for this is that the ovarian lymphatics drain the corpus directly whereas the cervical metastases tend to bypass the ovarian lymphatics and travel by way of the hypogastric and aortic glands. Clinical Features ⚫ The clinical features are not specific in early stages, resulting in late diagnosis in 70% cases. A woman with a malignant ovarian tumour is either an adolescent or of menopausal or postmenopausal age of low parity. ⚫ A family history of breast or ovarian tumour may be relevant. ⚫ Initially, the woman is asymptomatic. The tumour however grows rapidly and develops symptoms. ⚫ Abdominal discomfort and pain, abnormal or postmenopausal bleeding and an abdominal lump are the characteristic features. ⚫ Weight loss, cachexia and anaemia are the symptoms and signs of advanced stage of cancer. ⚫ The malignant ovarian tumours are often bilateral, solid and present with ascites. ⚫ The only benign tumours that cause ascites (Meigs’ syndrome) are ovarian fibroma, Brenner tumour and rarely granulosa cell tumour. ⚫ The tumours are often fixed in the late stage and intraperitoneal metastasis may be palpable abdominally. ⚫ The vaginal examination may reveal fixed nodules in the pouch of Douglas, apart from adnexal masses felt separate from the uterus. ⚫ Unilateral nonpitting oedema of the leg, pleural effusion and enlarged liver are suggestive of advanced stage of the disease. ⚫ Peritoneal tuberculosis mimics ovarian cancer with raised CA-125. Investigations ⚫ The investigations to confirm the diagnosis and nature of the tumour are 191 | P a g e described in the chapter dealing with benign ovarian tumours. Further, to confirm or refute malignancy: ✓ CT and MRI indicate the extent of the tumour spread. ✓ Tissue markers mentioned earlier suggest the histological nature of the tumour, as well as decide the duration of postoperative chemotherapy or need for radiotherapy. ✓ CA-125 is raised in epithelial tumours. ✓ Barium meal, barium enema and breast examination are required when metastatic tumour is suspected. X-ray of chest and liver scan are required to detect metastatic growth. ✓ Ultrasound shows a solid tumour with echogenic or cystic areas, a thick capsule with papillary projectors and a thick septum measuring more than 5 mm in a malignant tumour. ➢ The tissue markers are useful during chemotherapy to decide the response and the duration of therapy in postoperative follow-up. ➢ Fine-needle aspiration cytology (FNAC) and ascetic fluid cytology yield a high false-negative report. ➢ CT and MRI diagnose dermoid, endometriosis and extent of spread of ovarian malignancy as well as assess lymph node involvement. ➢ Since these only pick up lymph nodes enlarged more than 1 cm, some employ lymphography if CT and MRI give negative lymph node involvement, because lymphography can pick up nodes as small as 5 mm. ➢ Since debulking surgery is undertaken even in advanced stages, diagnostic laparoscopy has lost its importance. Management ✓ Laparotomy and maximal reduction is the primary and gold standard treatment in all ovarian malignant tumours. ✓ Surgical staging is followed by definitive surgery or debulking followed by chemotherapy or radiotherapy. 192 | P a g e ✓ Surgical staging involves systemic exploration of the undersurface of the diaphragm, liver, stomach, bowel and omentum. ✓ The para-aortic lymph nodes should be palpated. 3Ascitic fluid or peritoneal wash should be collected in heparinized bottles for cytology. ✓ The ovaries and uterus should be studied and definitive surgery planned. ✓ Debulking. Optimal debulking surgery is now considered the standard treatment for all stages of ovarian cancer. ✓ The reasons for this recommendation are as follows: ➢ Despite well-developed chemotherapy available, recurrence is common. ➢ Debulking reduces the amount of chemotherapeutic drugs, reduces resistance to the drugs and improves the blood flow to the residual tumour, thus allowing the chemotherapeutic drugs to reach the tumour tissue. ➢ The incidence of recurrence is therefore less and disease-free interval prolonged. ➢ Reduces ascites and symptoms. ➢ Borderline malignancy. Total abdominal hysterectomy and bilateral salpingooophorectomy (TAH and BSO) should be done in older women, and conservative ovariotomy in young women, provided peritoneal wash is negative. ➢ Frozen section may give false-negative report due to freezing. ➢ Instead, lately, imprint cytology of the specimen gives 90% sensitivity and 80% specificity, takes 20 min, is simple and less expensive. ➢ No postoperative chemotherapy is required, but follow-up is mandatory in young women. ➢ In a young woman, conservation of uterus allows IVF and donor egg use. Stages I and II. The operable cases (Stages I and II) : should undergo total hysterectomy and bilateral salpingooophorectomy with omentectomy. ✓ Advanced and inoperable case (Stages III and IV) will benefit from debulking surgery and removal of the tumour. 193 | P a g e ✓ Postoperative chemotherapy and radiotherapy improve the survival and quality of life. ✓ The purpose of maximal debulking surgery is to reduce the amount of malignant tissue to be subjected to chemotherapy and relieve the woman of her symptoms. ✓ The response to chemotherapy improves with smaller residual tissue and thus remission period and survival is enhanced. ✓ Pre-operative cisplatin followed by surgery is lately employed. Lymphadenectomy. Lately some oncologists believe additional lymphadenectomy improves the survival. ✓ The lymph nodes mainly involved are para-aortic lymph nodes. ✓ Postoperative chemotherapy and radiotherapy depend upon the staging and the type of tumour. ✓ The duration of chemotherapy is judged by the level of tissue markers. Interval Surgery ✓ Some advanced and bulky tumours are initially treated by chemotherapy for three cycles. ✓ This is followed by debulking surgery and postoperative chemotherapy as dictated by tissue marker. ✓ Laparoscopic surgery is lately undertaken by expert laparoscopists. The disadvantages of laparoscopy are as follows: ➢ Possibility of spillage during surgery with recurrence. ➢ Port-site metastasis in 1–1.5% cases. Use of endospecimen bag, lavage and use of intraperitoneal chemotherapy may reduce the risk. Second-Look Surgery The following is the role of second-look surgery: ➢ To detect the presence of any residual tumour following a planned course of chemotherapy and decide if further chemotherapy is required. ➢ With the availability of tissue markers for vast majority of ovarian tumours in the follow-up, the importance of second-look surgery is losing ground and 194 | P a g e surgical morbidity is also eliminated. ➢ Besides, microscopic residual tumours may not be detected (false-negative findings) at laparoscopy ✓ Following a 3–6 month course of chemotherapy in an inoperable case, secondlook surgery may enable TAH and BSO or debulking procedure. ✓ In a recurrent tumour. ✓ Instead of laparotomy, second-look laparoscopy is another alternative. ✓ Combination of surgery, radiotherapy and chemotherapy has improved the salvage rate and quality of life considerably. ✓ The terminal stages require analgesics and sedation. ◆ Recurrent tumour. If the tumour recurs following treatment, the following options are applicable depending upon the type of tumour, size and its histology. ✓ Second-look surgery and removal of the lesion—for a single-site recurrence. ✓ Chemotherapy—for visceral metastasis. ✓ Radiotherapy—preferably for nodal metastasis. ✓ Intraperitoneal chemotherapeutic drug may be instilled in a small residual tumour, at the end of surgery. ✓ The trial with chemotherapeutic drugs intraperitoneally is on. ✓ Stem cell therapy may have a role in future. ✓ Dysgerminoma and granulosa cell tumour respond well to both chemotherapy and radiotherapy. ✓ In a young woman, fertility-retaining surgery of unilateral ovariotomy (if unilateral) is followed by chemotherapy rather than radiotherapy which destroys the other ovary. ✓ In the older woman, hysterectomy and bilateral removal of ovaries may be followed by radiotherapy. 195 | P a g e result: 196 | P a g e 173. Erosion of cervix uteri (congenital erosion, erosion associated with chronic cervicitis. hormonal erosion): definition, pathology, symptoms and sings, differential diagnosis, treatment Ans: Definition ⚫ Cervical ectopy is a condition where the squamous epithelium of the ectocervix is replaced by columnar epithelium, which is continuous with the endocervix. Etiology ⚫ Congenital ⚫ Acquired Congenital ⚫ At birth, in about one-third of cases, the columnar epithelium of the endocervix extends beyond the external os. ⚫ This condition persists only for a few days until the level of estrogen derived from the mother falls. ⚫ Thus, the congenital ectopy heals spontaneously. Acquired Hormonal: ⚫ The squamocolumnar junction (SCJ) is not static and its movement, either inwards or outwards is dependent on estrogen. ⚫ When the estrogen level is high, it moves out so that the columnar epithelium extends onto the vaginal portion of the cervix replacing the squamous epithelium. ⚫ This state is observed during pregnancy and amongst ‘pill users’. The squamocolumnar junction returns back to its normal position after 3 months following delivery and little earlier following withdrawal of ‘pill’. 197 | P a g e Infection: ⚫ The role of infection as the primary cause of ectopy has been discarded. ⚫ However, chronic cervicitis may be associated or else the infection may supervene on an ectopy because of the delicate columnar epithelium which is more vulnerable to trauma and infection. Pathogenesis ⚫ In the active phase of ectopy, the squamocolumnar junction moves out from the os. ⚫ The columnar epithelium of the endocervix maintains its continuity while covering the ectocervix replacing the squamous epithelium. ⚫ The replaced epithelium is usually arranged in a single layer (flat type) or may be so hyperplastic as to fold inwards to accommodate in the increased area—a follicular ectopy. ⚫ At times, it becomes heaped up to fold inwards and outwards—a papillary ectopy. ⚫ Underneath the epithelium, there are evidences of round cell infiltration and glandular proliferation. ⚫ The features of infection are probably secondary rather than primary. ⚫ The columnar epithelium is less resistant to infection than the squamous epithelium. ⚫ During the process of healing, the squamocolumnar junction gradually moves up towards the external os. ⚫ The squamous epithelium grows beneath the columnar epithelium until it reaches at or near to its original position at the external os. ⚫ Alternatively, the replacement is probably by squamous metaplasia of the columnar cells. ⚫ The possibility of squamous metaplasia of the reserve cells is also likely During the process, the squamous epithelium may obstruct the mouth of the underlying glands (normally not present in ectocervix) → pent up secretion → 198 | P a g e retention cyst → nabothian follicle. ⚫ Alternatively, the epithelium may burrow inside the gland lumina. ⚫ This process of replacement by the squamous epithelium is called epidermidization. Clinical Features Symptoms: The lesion may be asymptomatic. However, the following symptoms may be present. ⚫ ™Vaginal discharge—The discharge may be excessively mucoid. It may be mucopurulent, offensive and irritant in presence of infection; may be even blood-stained due to premenstrual congestion. ⚫ Contact bleeding specially during pregnancy and ‘pill use’ either following coitus or defecation may be associated. ⚫ ™Associated cervicitis may produce backache, pelvic pain and at times, infertility. Signs: Internal examination reveals: „ Per speculum—There is a bright red area surrounding and extending beyond the external os in the ectocervix. ⚫ The outer edge is clearly demarcated. ⚫ The lesion may be smooth or having small papillary folds. ⚫ It is neither tender nor bleeds to touch. ⚫ On rubbing with a gauze piece, there may be multiple oozing spots (sharp bleeding in isolated spots in carcinoma). ⚫ The feel is soft and granular giving rise to a grating sensation. Differential Diagnosis The diagnosis is confused with: Ectropion: The lips of the cervix are curled back to expose the endocervix. This may be apparent when the lips of the cervix are stretched by the bivalve speculum. Early carcinoma: It is indurated, friable and usually ulcerated which bleeds to touch. Confirmation is by 199 | P a g e biopsy. Primary lesion (chancre): The ulcer has a punched-out appearance. Tubercular ulcer: There is indurated ulcer with caseation at the base. Biopsy confirms the diagnosis. Management Guidelines: All cases should be subjected to cytological examination from the cervical smear to exclude dysplasia or malignancy Symptomatic cases ⚫ Detected during pregnancy and early puerperium, the treatment should be withheld for at least 12 weeks postpartum. In pill users, the ‘pill’ should be stopped and barrier method is advised. ⚫ Persistent ectopy with troublesome discharge should be treated surgically by— (i) thermal cauterization, (ii) cryosurgery, and (iii) laser vaporization ⚫ All the methods employed are based on the principle of destruction of the columnar epithelium to be followed by its healing by the squamous epithelium. 174. Ectropion of the cervix: definition, pathology, symptoms and sings, treatment. Ans: EVERSION (ECTROPION) : ⚫ In chronic cervicitis, there is marked thickening of the cervical mucosa with underlying tissue edema. ⚫ These thickened tissues tend to push out through the external os along the direction of least resistance. 200 | P a g e ⚫ The entity is most marked where the cervix has already been lacerated. ⚫ In such conditions, the longitudinal muscle fibers are free to act unopposed. ⚫ Due to this, the lips of the cervix curl upwards and outwards to expose the red looking endocervix so as to be confused with ectopy . ⚫ As a result the SCJ lies extermal to the cervical os. 175. Cervical polypi: pathology, symptoms and sings. differential diagnosis, treatment. Ans: MUCOUS POLYP ⚫ The most common type of benign uterine polyp is mucous one. ⚫ It may arise from the body of the uterus or from the cervix Risk factors: Hormone replacement therapy, tamoxifen therapy, diabetes, hypertension, obesity, and increased patient age are the important risk factors. Pathogenesis Body A part of the thick endometrium projects into the cavity and ultimately attains a pedicle. Naked eye appearance: It shows a small polyp size of about 1–2 cm, looks reddish and feels soft. The pedicle may at times be long enough to make the polyp protruded from the cervix. Benign: Mucous Fibroid Placental Malignant: De novo 201 | P a g e Secondary changes of benign polyp Symptoms The patients are usually in reproductive period. The chief complaints are: ⚫ Intermenstrual bleeding, often continuous, specially in fibroid polyp arising from the body Colicky pain in the lower abdomen due to uterine contraction in an effort to expel the polyp out of the uterine cavity. ⚫ Excessive vaginal discharge which may be offensive ⚫ Sensation of something coming down when the polyp becomes big distending the vagina ⚫ It may remain asymptomatic also. Signs General examination reveals varying degrees of anemia. Per vaginam ⚫ The uterus may be bulky. ⚫ The cervix may be patulous and the tip of the polyp is felt or else, the polyp is felt distinctly outside the external os. Speculum examination: It reveals the size and color of the polyp which is usually pale; may be hemorrhagic. ⚫ Whereas, the attachment of the pedicle to the cervix can be visualized but attachment higher up may be at times difficult to locate. Investigations ⚫ Transvaginal sonography (TVS), the polyp is seen as an echogenic mass. ⚫ Saline infusion sonography (gold standard), the polyp 202 | P a g e is seen as a echogenic mass much better compared to TVS? ⚫ Hysteroscopy—to visualize the uterine polyp and simultaneously polypectomy could be done. ⚫ Hysterography—to detect the filling defect in a fibroid polyp. ⚫ Examination under anesthesia and exploration of the uterine cavity by curette or ovum or ring forceps can help in diagnosis of an uterine polyp. ⚫ In all cases, following polypectomy histological examination should be done. ⚫ Sound test—to differentiate a fibroid polyp from chronic inversion, sound test is done. ⚫ If an uterine sound is passed all round between the pedicle and the dilating cervical canal, it is a polyp. ⚫ In complete chronic inversion, the sound cannot be passed. PLACENTAL POLYP ⚫ A retained bit of placental tissue when adherent to the uterine wall gets organized with the surrounding blood clots. Clinical Features ⚫ There is history of recent childbirth or abortion. Irregular bleeding per vaginam and offensive vaginal discharge are present dated back to the pregnancy events. MANAGEMENT OF A POLYP ⚫ Endometrial polyp may be removed by doing hysteroscopy and resection. ⚫ It can also be removed by uterine curettage or using ring or ovum forceps. In cases of recurrence and patients who have completed the family, hysterectomy is justified. ⚫ The causes of recurrence of polyps are: (1) Incomplete removal; 203 | P a g e (2) Persistence of the cause leading to polyp formation; (3) Malignancy. ⚫ Cervical polyps are removed by twisting of the pedicle. ⚫ The base of the pedicle should be cauterized to prevent recurrence. ⚫ Hysteroscopy is useful to locate the postion, size, and the base of the polyp. ⚫ Submucous fibroid polyps can be resected out hysteroscopically as an outpatient basis ⚫ Endometrial polyps that cause infertility, postmenopausal bleeding or abnormal uterine bleeding should be removed hysteroscopically under direct vision. ⚫ It is superior to blind avulsion. ⚫ After the polyp is removed, endometrium is curetted to rule out coexisting pathology (5%). Histology ⚫ Histologically the polyp may be adenomatous (80%), cystic, fibrous, vascular and fibromyomatous. ⚫ There may be ulceration of the dependent portion of the polyp. Malignant change of an endometrial polyp is extremely rare (0.5%). ⚫ Big Fibroid Polyp Lying in the Vagina One should be sure that it is a polyp and not uterine inversion or fibroid with inversion. Diagnosed polyp: Removal of polyp by morcellement (piecemeal) followed by trans fixation suture on the pedicle and removal of the redundant pedicle distal to the ligature. Associated with chronic uterine inversion—The incision is made close to the fibroid and to enucleate it. ⚫ When hysterectomy is indicated, the polyps of such type are expected to be infected and are to be removed first. 204 | P a g e ⚫ Antibiotics are to be administered. ⚫ The general condition of the patient is to be improved and hysterectomy should be done at a later date. ⚫ The polyps should be sent for histological examination after its removal. 176. Dysplasia and cervical intraepithelial neoplasia (CIN): pathological anatomy, clinical features, diagnosis, treatment. Screening for cancer (Pap test). Ans: pathology: The process of carcinogenesis starts at the ‘transformation zone’ (TZ). The zone is not static but in a dynamic state. Two mechanisms are involved in the process of replacement of endocervical columnar epithelium by squamous epithelium. ⚫ By squamous metaplasia of the subcolumnar reserve cells ⚫ Squamous epidermidization by ingrowth of the squamous epithelium of the ectocervix under the columnar epithelium. diagnosis: ⚫ Cytologic screening (Scheme-3): Exfoliative cytology (Papanicolaou and Traut, 1943) has become the gold standard for screening. The smear should contain cells from SCJ, TZ, and the endocervix. Ayre’s spatula and an endocervical brush is used for the purpose. Cells are spread on a single slide and fixed immediately. ⚫ High risk HPV-DNA (HR HPV-DNA) testing is useful in cervical screening ⚫ Visual inspection with acetic acid (VIA) 205 | P a g e ⚫ Colposcopy ⚫ Cervicography ⚫ Biopsy with or without colposcopy treatment: TREATMENT OF CIN Preventive Definitive ⚫ Preventive: HPV vaccines, Prevention of HPV Infection. ⚫ Definitive Treatment ⚫ The treatment modalities depend on: Age of the patient, Desire for reproduction, Risk factors present, Degree of dysplasia Facilities available for follow up such as colposcopy and/or cytology. ⚫ Local ablative methods Cryotherapy Cold coagulation Electrodiathermy Laser vaporization ⚫ Excisional methods Large loop (electrosurgical) excision of transformation zone (LLETZ). Cone excision—using a knife or laser. Hysterectomy—abdominal or vaginal. screening for cancer: 206 | P a g e 177. Carcioma of the cervix: actiology, epidemiology, predisposing risk factors, pathology, staging, clinical features, diagnosis and differential diagnosis, treatment ans: 207 | P a g e Epidemiology: In India, the prevalence is more amongst the comparatively younger age group. Carcinoma cervix is rare in women who are sexually not active (nuns, virginal women). Male circumcision is only partially protective against cervical carcinogenesis. Pathology: The site of the lesion is predominantly in the ectocervix (80%) and the rest (20%) are in the endocervix. Naked Eye Exophytic: These arise from the ectocervix and form friable masses almost filling up the upper vagina in late cases. Ulcerative: The lesion excavates the cervix and often involves the vaginal fornices. Infiltrative: These are found in endocervical growth. They cause expansion of the cervix, so that it becomes barrel-shaped. Histopathology The most common variety is squamous cell carcinoma (75–80%) either welldifferentiated or moderately or poorly differentiated. These arise from the ectocervix. The sources of the squamous epithelium which turn into malignancy are—squamocolumnar junction, squamous metaplasia of the columnar epithelium. 208 | P a g e : diff diag: DIFFERENTIAL DIAGNOSIS The growth needs to be differentiated from: Cervical tuberculosis Syphilitic ulcer Cervical ectopy Products of conception in incomplete abortion Fibroid polyp treatment: The types of treatment employed for the invasive 209 | P a g e carcinoma are as follows: Primary surgery Primary radiotherapy Chemotherapy Combination therapy. 178. Cancer cervix and pregnancy. Ans: CARCINOMA OF CERVIX AND PREGNANCY: Incidence of invasive carcinoma of the cervix is about one in 2500 pregnancies. Diagnosis is often late. Cone biopsy may be necessary for confirmation. Complications of cone biopsy include: Hemorrhage, abortion, preterm labor, and infection. ⚫ LEEP has no superiority over cone biopsy. Management ⚫ The following points are taken into consideration before actual management: (A) Period of gestation, (B) survival of the fetus and (C) wishes of the patient, and (D) histology.A. Patient with microinvasive carcinoma may be followed up to term. Patient is revaluated following delivery and treated as in the nonpregnant state. B. Advanced stage: In the first trimester, treatment : modality is the same as in the nonpregnant state (chemoradiation). In late pregnancy, following maturity, fetus is delivered by classical cesarean section. Subsequent treatment with either radical surgery or radiotherapy or chemoradiation is the same as in the nonpregnant state. Prognosis Clinical stage of the disease is the single most important prognostic factor. Stage for stage survival outcome appears to be no different between pregnancy and nonpregnant state. 210 | P a g e 179. Endometrial carcinoma: predisposing factors, pathology, staging, clinical features, differential diagnosis, treatment and results. ans: predisposing factors:estrogen: persistent stimulation of endometrium, age, parity, late menopause, corpus cancer syndrome, obesity, unopposed estrogen stimultion, unopposed estrogen replacement therapy, polycystic ovarian disease, tamoxifen, family history, fibroid, endometrial hyperplasia. Pathology: naked eye: a) localised b) diffuse Microscopic appearances: The following varieties are noted: Adenocarcinoma (endometrioid 80%) (Fig. 24.11) Adenocarcinoma with squamous elements Papillary serous carcinoma (5–10%) (virulent) Mucinous adenocarcinoma (1–2%) Clear cell adenocarcinoma (< 5%) Secretory carcinoma (1%) Squamous cell carcinoma Mixed carcinoma Undifferentiated carcinoma (1–2%). Endometrial carcinoma are of two types based upon biological and histological behavior clinical features: Symptoms: Postmenopausal bleeding (75%) which may be slight, irregular or continuous. The bleeding at times may be excessive. In premenopausal women, there may be irregular and excessive bleeding. At times, there is watery and offensive discharge due to pyometra. Pain is not uncommon. It may be colicky due to uterine contractions in an attempt to expel the polypoidal growth. Few patients (< 5%) remain asymptomatic. In late cases there may be pelvic pressure, pain or ⚫ abnormal bleeding. 211 | P a g e 180. Strategies to reduce the incidence of genital tract malignancies ans: There have been advances in strategies evolved to reduce the incidence of genital cancers. The following are notable amongst these: 1. The role and value of periodic ‘Pap smear’ tests is well-established in reducing the incidence of invasive carcinoma of the cervix. 2. Evaluation of abnormal Pap tests with colposcopy directed biopsies enables the diagnosis of intraepithelial cancers and diagnosis of early invasive cancer of the cervix. (secondary prevention) 3. The practice of preferring total over subtotal hysterectomy for benign diseases (fibroids, adenomyosis, abnormal uterine bleeding—AUB) protects against risk of future cervical stump carcinoma estimated to occur in 1–2% of cases. 4. Early diagnosis of sexually transmitted diseases (STDs) and their eradication. Herpes and HPV infections render an individual prone to cancer of vulva and the cervix. Barrier contraceptives protect against STD as well as cervical cancer. (primary prevention) 5. HPV vaccine is now available which may eradicate lower genital tract malignancies in young women. The available vaccine is type specific and therefore, protective in only 60–70%. 6. The treatment of cervical dysplasia by CO2 laser/conization for CIN lesions will reduce the incidence of cancer cervix. 7. Addition of progestogens to oestrogens in hormone replacement therapy (HRT) reduces the risks of uterine endometrial cancer. 8. Thorough investigation of a woman with postmenopausal bleeding often brings to light early unsuspected endometrial/ovarian/tubal cancers. 9. The practice of routine removal of both ovaries when performing hysterectomy for benign conditions after the age of 50 years is a prophylaxis against risk of future ovarian cancer. Prophylactic oophorectomy in a genetically predisposed woman is recommended, though premature menopause remains the risk. This also reduces breast cancer by 50%. 10. Early diagnosis of ovarian cancer is the primary objective for long-term 212 | P a g e survival, though this is not obtained as of today. Seventy-five per cent tumours are advanced when diagnosed. 11. Oral combined pills reduce the incidence of uterine and ovarian cancer by 40– 50%. The effects last for 10 years after stoppage of oral pills. Barrier contraceptives prevent cervical cancer. 12. Gene study can select women at high risk for cancer. 13. Evaluation of adnexal masses with scans, Doppler velocimetric studies and CA125 tumour marker to diagnose ovarian cancer. 14. Hysteroscopy/laparoscopy/selective biopsies of suspicious lesions. 15. Routine mammography for all women over the age of 40 years, earlier whenever clinical examination reveals a doubtful lump, or in women with strong family history of breast cancer. 181. Menopause and climacteric: detinition, demography, age. Pathophysiology and hormone levels of climacteric. Anatomical changes of menopause. ans: Menopause is defined as the time of cessation of ovarian function resulting in permanent amenorrhoea. It takes 12 months of amenorrhoea to confirm that menopause has set in, and therefore it is a retrospective diagnosis.Climacteric is the phase of waning ovarian activity, and may begin 2–3 years before menopause and continue for 2–5 years after it. The climacteric is thus a phase of adjustment between the active and inactive ovarian function and occupies several years of a woman’s life, and it involves physical, sexual and psychological adjustments. Demography ⚫ Sixty million women in India are above the age of 55 years. With women living longer than before, a majority would spend one-third of their life in the postmenopausal stage. ⚫ The health problems cropping up during this period and related to oestrogen deficiency of menopause are now obvious and better understood. It is important therefore to address all these menopause-related diseases and apply 213 | P a g e prophylactic measures so that these women can lead an enjoyable and healthy life. An average Indian woman now lives up to 65 years of age, whereas in developed countries a lifespan up to 80 years is possible. Age Menopause sets in when the follicular number falls below 1000. Menopause normally occurs between the ages of 45 and 50 years, the average age being 47 years. It is not uncommon, however, to see a woman menstruate well beyond the age of 50. This delayed menopause may be related to good nutrition and better health. Late menopause is also common in women suffering from uterine fibroids and those at high risk of endometrial cancer. Menopause setting before the age of 40 is known as premature menopause.Menopausal age is not related to menarche, race, socioeconomic status, number of pregnancies and lactation, or taking of oral contraceptives. It is however directly associated with smoking and genetic disposition. Smoking induces premature menopause. Pathophysiology During climacteric, ovarian activity declines. Initially, ovulation fails, no corpus luteum forms and no progesterone is secreted by the ovary. Therefore, the premenopausal menstrual cycles are often anovulatory and irregular. Later, Graafian follicles also fail to develop, oestrogenic activity is reduced and endometrial atrophy leads to amenorrhoea. Cessation of ovarian activity and a fall in the oestrogen and inhibin levels cause a rebound increase in the secretion of FSH and LH by the anterior pituitary gland. The FSH level may rise as much as 50-fold and LH 3–4 fold. Menopausal urine has become an important commercial source of human menopausal gonadotropin (hMG). With further advancing years, gonadotropin activity of the pituitary gland also ceases, and a fall in FSH level eventually occurs. Hormone Levels There is 50% reduction in androgen production and 66% reduction in oestrogen at menopause. The oestrogen level may remain low at 10–20 pg/mL. Some oestrogen comes from the ovary, but most of it is oestrone (E1) derived from peripheral conversion of androstenedione secreted by the ovary, and its level varies between 30 and 70 pg/mL. The ovary also secretes a small amount of testosterone which causes mild hirsutism at menopause. The FSH appears in high concentration in the urine (more than 40 IU/l). E2/E1 ratio maintained over 1 in the premenopausal period is reduced to less than 1 in the menopausal age, causing an oestrogen deficiency state. Oestrogen level of over 40 pg/mL exerts bone and cardiotrophic effect, but the level below 20 pg/mL may predispose to osteoporosis and ischaemic heart disease. Low level of growth hormone causes 214 | P a g e ovarian failure. Risk factors for menopause-related diseases are as follows: ◆ Early menopause. ◆ Surgical menopause or radiation. ◆ Chemotherapy especially alkalytic agents. ◆ Smoking, caffeine, alcohol. ◆ Family history of menopausal diseases (genetic). ◆ Drugs related such as GnRH, heparin, corticosteroids and clomiphene (antioestrogen) when given over a prolonged period (over 6 months) can lead to oestrogen deficiency. ◆ Diabetes Anatomical Changes ⚫ The genital organs undergo atrophy and retrogression. ⚫ The ovaries shrink and their surfaces become grooved and furrowed. ⚫ The tunica albuginea thickens. ⚫ The menopausal ovary measures less than 2 3 1.5 3 1 cm in size (8 mL in volume) as seen on ultrasound. ⚫ Fifteen years later, it should not measure more than 2 mL. ⚫ The plain muscle in the fallopian tube undergoes atrophy, cilia disappear from the tubal epithelium and the tubal plicae are no longer prominent. ⚫ The uterus becomes smaller through atrophy of its plain muscle, so that the connective tissues are more conspicuous. ⚫ The endometrium is represented by only the basal layer with its compact deeply stained stroma, and a few simple tubular glands. ⚫ The lymphoid tissue and the functional layer disappear. ⚫ It is common for the endometrial glands to dilate before menopause sets in, and cystic glandular hyperplasia reported in some premenopausal women causes metropathia haemorrhagica, with irregular heavy bleeding. ⚫ The pre-existing fibromyoma gradually shrinks. ⚫ The cervix becomes smaller and its vaginal portion is represented by a small 215 | P a g e ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ ⚫ prominence at the vaginal vault. The cervical stenosis and pyometra are not uncommon. The vaginal fornices gradually disappear as the cervix shrinks after the menopause. The vagina becomes narrow and its epithelium becomes pale, thin and dry and gets easily infected causing senile vaginitis. The vulva atrophies and the vaginal orifice narrow and this can cause dyspareunia. The skin of the labia minora and vestibule becomes thin, pale and dry, and there is considerable reduction in the amount of fat contained in the labia majora. The pubic hair is reduced and becomes grey. The red patches seen around the urethra and introitus are caused by senile vulvitis, and a urethral caruncle may be produced. The pelvic cellular tissue becomes lax and the ligaments that support the uterus and vagina lose their tone, and these conditions predispose to prolapse of the genital organs, stress incontinence of urine and faecal incontinence. Apart from the atrophy of the genital organs, general disturbances that develop are almost certainly caused by alterations in the endocrine balance maintained during the childbearing period. Fat is deposited around the breasts, hips and abdomen. Although the mammary glandular tissue atrophies, deposition of fat often makes the breasts more pendulous. Whereas, glandular tissue constitutes 30% of the breast volume, it is reduced to only 5% after the menopause. The skin wrinkles and hair grow around the chin and lips. Hypertension, cardiac irregularities and tachycardia are at times noticed after menopause. Arthritis and osteoporosis of the vertebral bones, upper end of the hip joint and wrist are related to oestrogen deficiency after menopause. Tooth decay, keratoconjunctivitis and cataract are related to menopausal oestrogen deficiency 216 | P a g e 182. Menopausal symptoms. Investigations. Ans: In majority, apart from cessation of menstruation,no more symptoms are evident. In some women, symptoms appear. The important symptoms and the health concerns of menopause: ⚫ Vasomotor symptoms ⚫ urogenital atrophy ⚫ Osteoporosis and fracture ⚫ Cardiovascular disease ⚫ Cerebrovascular diseases ⚫ Psychological changes ⚫ Skin and hair ⚫ Sexual dysfunction ⚫ Dementia and cognitive decline. Vasomotor symptoms: ⚫ The characteristic symptom of menopause is ‘hot flush’. ⚫ Hot flush is characterized by sudden feeling of heat followed by profuse sweating. ⚫ There may also be the symptoms of palpitation, fatigue and weakness. The physiologic changes with hot flashes are perspiration and cutaneous vasodilation. ⚫ Both these two functions are under central thermoregulatory control. ⚫ Low estrogen level is a prerequisite for hot flash. ⚫ Hot flash coincides with GnRH pulse secretion with ⚫ increase in serum LH level. Genital and urinary system: 217 | P a g e ⚫ Steroid receptors have been identified in the mucous membrane of urethra, bladder, vagina and the pelvic floor muscles. ⚫ Estrogen plays an important role to maintain the epithelium of vagina, urinary bladder and the urethra. ⚫ Estrogen deficiency produces atrophic epithelial changes in these organs. ⚫ This may cause dyspareunia and dysuria. Dyspareunia: Estradiol deficiency leads to vaginal dryness or atrophy. ⚫ Estrogen replacement reverses atropic changes. ⚫ It can be given orally or vaginally. ⚫ 17 β-estradiol tablet or conjugated equine estrogen (CEE) cream is effective in relieving symptoms. Risks of endometrial hyperplasia is less with vaginal tablets than that of cream. ⚫ Vaginal lubricants (water soluble) and moisturisers (K-Y jelly) are commonly used. Vagina: Minimal trauma may cause vaginal bleeding. ⚫ Dyspareunia, vaginal infections, dryness, pruritus and leucorrhea are also common. ⚫ The urinary symptoms are urgency, dysuria and recurrent urinary tract infection and stress incontinence. Sexual dysfunction: Estrogen deficiency is often associated with decreased sexual desire. ⚫ This may be due to psychological changes (depression anxiety) as well as atrophic changes of the genitourinary system. ⚫ Skin and hair: There is thinning, loss of elasticity and wrinkling of the skin. ⚫ Skin collagen content and thickness decrease by 1–2% per year. ‘Purse string’ wrinkling around the month and ‘crow feet’ around the eyes are the characteristics. ⚫ Estrogen receptors are present in the skin and maximum are present in the facial skin. 218 | P a g e ⚫ Estrogen replacement can prevent this skin loss during menopause. ⚫ After menopause, there is some loss of pubic and axillary hair and slight balding. ⚫ This may be due to low level of estrogen with normal level of testosterone. ⚫ Psychological changes: There is increased frequency of anxiety, headache, insomnia, irritability, dysphasia and depression. Osteoporosis and fracture: Following meno-pause there is decline in collagenous bone matrix resulting in osteoporotic changes. ⚫ Bone mass loss and microarchitectural deterioration of bone tissue occurs primarily in trabecular bone (vertebra, distal radius) and in cortical bones. ⚫ Bone loss increases to 5% per year during menopause. Detection of osteoporosis: Computed tomography (CT) and specially the dualenergy X-ray absorptiometry (DEXA) are reliable methods to assess the bone mineral density. Cardiovascular and cerebrovascular effects: vascular atherosclerotic changes, vasoconstriction and thrombus formation. Risks of ischemic heart disease, coronary artery disease and strokes are increased. 183. Management of menopause. HRT: drugs, dosage and route of administration. Cardioprotective effect of HRT. Treatment of osteoporosis. ans: Hormone Therapy (HT) The HT is indicated in menopausal women to overcome the short-term and longterm consequences of estrogen deficiency. Indications of Hormone Therapy ✓ Relief of menopausal symptom ✓ Relief of vasomotor symptoms ✓ Prevention of osteoporosis 219 | P a g e ✓ To maintain the quality of life in menopausal years. ◆ Special group of women to whom HT should be prescribed: ✓ Premature ovarian failure ✓ Gonadal dysgenesis ✓ Surgical or radiation menopause. HT and Osteoporosis ⚫ HT prevents bone loss and stimulate new bone formation. ⚫ HT increases BMD by 2–5% and reduces the risk of vertebral and hip fracture (25–50%). ⚫ Estrogen is found to play a direct role, as receptors have been found in the osteoblasts. ⚫ Women receiving HT should supplement their diet with an extra 500 mg of calcium daily. Total daily requirement of calcium in postmenopausal women is 1.5 g. ⚫ HT is thought to be cardiovascular protective. ⚫ LDL on oxidation produces vascular endothelial injury and foam cell (macrophage) formation. ⚫ These endothelial changes ultimately lead to intimal smooth muscle proliferation and atherosclerosis. ⚫ Estrogen prevents oxidation of LDL, as it has got antioxidant properties. In postmenopausal women, there is some amount of insulin resistance and hyperinsulinemia. ⚫ Hyperinsulinemia induces atherogenesis. ⚫ Estrogen improve glucose metabolism. ⚫ Dose: interval may be modified as daily for initial 2–3 months then it may be changed to every other day for another 2–3 months and then every third day for the next 2–3 months. ⚫ It may be stopped thereafter if symptoms are controlled. 220 | P a g e ⚫ Oral estrogen regime: CEE, 0.3 mg or 0.625 mg is given daily for woman who had hysterectomy. ⚫ ‰Estrogen and cyclic progestin: For a woman with intact uterus, estrogen is given continuously for 25 days and progestin is added for last 12–14 days. ‰Continuous estrogen and progestin therapy: ⚫ Continued combined therapy can prevent endometrial hyperplasia. ⚫ There may be irregular bleeding with this regimen. ‰Transdermal administration ⚫ Subdermal implants ⚫ Transdermal patch: It contains 3.2 mg of 17 β- estradiol, releasing about 50 µg of estradiol in 24 hours. ⚫ Physiological level of E2 to E1 is maintained. ⚫ It should be applied below the waist line and changed twice a week. ⚫ Skin reaction, irritation and itching have been noted with their use. ⚫ Vaginal cream ⚫ Progestins ‰Tibolone: Tibolone is a steroid (19-nortestosterone derivative) having weak estrogenic, progestogenic and androgenic properties. It prevents osteoporosis, atrophic changes of vagina and hot flashes. ⚫ It increases libido. ⚫ Endometrium is atrophic. ⚫ A dose of 2.5 mg per day is given. ‰Testosterone: Androgen replacement in women with hypoactive sexual desire disorder (HSDD) is found beneficial. ⚫ It improves mood, bone, muscle mass and quality of life. ⚫ Short-term use is suggested. Parathyroid hormone (PTH): Recombinant PTH (teriparatide) is given by injection 221 | P a g e (SC) to prevent osteoporosis and fracture. ⚫ It increases the number of osteoblast cells and their activity and reduces apoptosis of osteoblast cells. ⚫ PTH is safe and well-tolerated. ⚫ At low daily doses (20 µg/day, SC) teriparatide, its anabolic effects predominate. Side effects are leg cramps, nausea and headache. ⚫ Use for more than 2 years is not recommended. Duration of HT Use ⚫ Generally, use of HT for a short period as long as the benefits outweigh the risks. ⚫ Individual woman need counseling with annual or semiannual review. Reduction of dosage should be done as soon as possible. ⚫ Menopausal women should maintain optimum nutrition, ideal body weight and perform regular exercises. ⚫ Individual woman should be informed with updated knowledge as regard the relative merits and possible Progress in Hormone Therapy ⚫ Low Dose HT: Women with intact uterus with 0.3 mg CEE and MPA 1.5 mg is found effective to control the vasomotor symptoms. ⚫ Similarly 1 mg of estradiol and norethisterone acetate 0.5 mg orally, are also effective and have significant bone sparing effect. ⚫ Progestogen is added in the HT to minimize the adverse effects of estrogen. ⚫ Hormone therapy should be used with lowest effective dose and for the short period of time as possible. ⚫ Dose interval may be modified before stopping the therapy. ⚫ To minimize the systemic adverse effects of progestogen, LNG-IUS is being used. 222 | P a g e ⚫ It is primarily used as a contraceptive. ⚫ Estrogen component is delivered by oral or by transdermal route or as an implant. ⚫ A small size LNG-IUS has been developed that releases 10 µg LNG per day. ⚫ This reduced size LNG-IUS is suitable for the postmenopausal women as the size of the uterus is also small. 184. Oestrogen: actions, preparations, indications, contraindications, side effects. Ans:Natural estrogens are 18-carbon atom steroids. Estradiol is the most active natural estrogen in human uses. • Natural • Synthetic Natural (a) It is available in the form of water soluble conjugated estrogen as Premarin [conjugated equine estrogen (CEE)]. It is obtained from the urine of pregnant mares. It is available as tablets 0.3 mg, 0.625 mg, and 1.25 mg and as injection of 20 mg ampoules for IM or IV injection. (b) Estradiol valerate used for priming the endometrium in donor oocyte program. 223 | P a g e Synthetic � Oral � Injectable � Cream/gel � Pessary � Implant � Patch Oral: This is the best route for synthetic preparations. • Ethinyl estradiol (Lynoral): 0.01 mg and 0.05 mg daily is commonly used • Estradiol valerate: 1–2 mg • CEE: 0.3 or 0.625 mg • Estriol succinate (Evalon): 1–2 mg. Injectable: � Estradiol ester as progynon depot (Schering): 10 mg ampoule.� Estradiol benzoate or dipropionate: 1 mg and 5 mg ampoule. Cream: � Vaginal cream–dienestrol (0.1 mg/g), Estriol (1 mg/g). �Percutaneous cream delivers 3 mg of estradiol in each daily 5 g applicator of cream. Gel: 17β-estradiol gel, 1 mg to be applied once daily over the skin of the lower trunk. Pessary: Dienestrol or estradiol acetate pessary (inserted for 90 days). Implants: � Subcutaneous implants of 50 mg and 100 mg of 17β-estradiol effect lasts for 6 months. Transdermal patch: It contains 17β-estradiol releasing about 0.05–0.1 mg of estradiol in 24 hours. Patch should be applied below the waist line and changed twice a week. Therapy • Replacement therapy • Pharmacotherapy Replacement therapy Ovarian hypofunction:Estrogen daily × 21 days followed by norethisterone or medroxyprogesterone 5 mg × last 10 days. • Cyclic or continuous therapy in the form of estradiol or conjugated estrogens • Postmenopausal hormone replacement therapy (HRT) in a symptomatic women „ To reduce vasomotor symptoms „ To prevent osteoporosis „ To prevent cardiovascular disease. Pharmacotherapy Oral contraception 224 | P a g e Vaginitis Senile or atrophic vaginitis—either vaginal cream or oral estrogens may be equally effective. Vulvovaginitis in childhood, foreign body in the vagina or sexual assault—low dose of oral estrogen or vaginal cream helps in increasing the vaginal defence. Intersex state ⚫ In Turner’s syndrome (45, XO) or gonadal dysgenesis (46, XY), estrogen therapy is helpful for the growth and development of the secondary sexual characters. ⚫ In androgen insensitivity syndrome (46, XY), after gonadectomy supplementary estrogen therapy is indicated to prevent regression of the breast development, osteoporosis and cardiovascular complications. ⚫ The estrogen is used cyclically as ethinyl estradiol 0.01 mg twice daily for 25 days. ⚫ However, in prolonged use, progestogen in the form of medroxyprogesterone acetate 10 mg daily is added from day 16–25, to minimize the adverse effects of estrogen. ⚫ Alternatively, a combined oral ‘pill’ may be prescribed. Dysfunctional uterine bleeding (DUB) ⚫ The estrogen in pharmacological doses causes rapid growth of endometrium. ⚫ As such, acute bleeding can be stopped by oral conjugated estrogen in a dose of 10 mg a day. ⚫ The bleeding usually stops within 24 hours. ⚫ Alternatively, 25 mg may be given intravenously every 4 hours for 3 doses. Delayed puberty ⚫ If the breast development fails to start even at the age of 14, 10 µg of estrogen daily may be of help. ⚫ In cases of irregular bleeding or when the breast development is welladvanced, progestogens may be added Cervical mucus hostility ⚫ To improve the quality of the cervical mucus in infertility, low dose of estrogen 225 | P a g e (ethinyl estradiol 0.01 mg) may be given cyclically, from day 1–14. An Adjunct with Clomiphene Therapy In cases of hypoestrogenic state with hypomenorrhea, small dose of estrogen is of help to improve the quality of the cervical mucus. Genuine stress incontinence (GSI) in postmenopausal women to improve the tone of collagen tissue. Adverse Effects Minor ailments are: ™Nausea, vomiting Breast tenderness Breakthrough bleeding Weight gain. Major effects include: Increased incidence of endometrial carcinoma, thromboembolism, cerebral thrombosis, and hemorrhage. To minimize breakthrough bleeding and prevent endometrial carcinomas and vascular complications, progestogens should be combined with estrogen therapy. CONTRAINDICATIONS OF ESTROGEN THERAPY • Undiagnosed genital bleeding • History of venous thromboembolism • Active liver disease • Severe hypertension • Organic heart disease • Estrogen dependent neoplasia (breast) 185. Progesterone: actions, preparations, classification, therapeutic applications, contraindications, side effects. ans: Progesterone is the natural hormone produced by the theca cells of the corpus luteum and the placenta. ⚫ It is metabolized in the liver and excreted in the urine as sodium pregnanediol glucuronide. Natural progesterone is not active orally and is given only by intramuscular injection in an oil base. 226 | P a g e ⚫ Progesterone acts on target tissues only when the latter are primed with oestrogen, as oestrogen produces progesterone receptors. ⚫ A large number of synthetic compounds which can be taken orally have been marketed in recent years. Preparations Progestogens are synthetic compounds belonging to two main groups—the oestrone or 19-norprogestins which are structurally similar to testosterone and pregnane or 17-acetoxy compound structurally similar to progesterone. The oestrone compounds are mainly incorporated in oral contraceptive pills, and pregnane compounds used in pregnancy and AUB. Classification ✓ Pure progesterone—Oral and vaginal micronized progesterone have no adverse effect on lipid profile. ✓ Pregnane (derived from progesterone molecule), lynestrenol (allyloestrenol), medroxyprogesterone, megestrol acetate. ✓ Estrane (derivative of testosterone)—Norethisterone, norethandriol (first generation). ✓ Gonane—Levonorgestrel, norgestrel (second generation). They reduce the level of SHBG, have androgenic, anti-E effect. ✓ Third-generation progesterone (desogestrel, gestodene, norgestimate). These are less androgenic and cause less metabolic disorders, but increase the risk of thrombosis. ✓ Hybrid drospirenone (3 mg equivalent to 25 mg spirinone) now used in oral pills for acne and PCOS. ✓ Yasmin contains 30 µg of EE2 (21 days), Janya contains 20 µg EE2 for 24 days in a cycle. ✓ Hybrids (drospirenone) have anti-androgens, antimineral corticosteroid effect; are used in premenstrual tension; causes hyperkalaemia by decreasing potassium excretion in the urine, less water retention and weight gain. ✓ These have no influence on lipid profile and have a very good control on menstrual cycles. 227 | P a g e ✓ Micronized progesterone—Oral tablet (100 mg) causes vomiting, giddiness and liver damage. ✓ Micronized vaginal tablet (100 mg) is without these oral side effects, but causes vaginal irritation. ✓ Progestogens are administered: ✓ Orally—Singly or with oestrogen ✓ Intramuscular injection monthly, three-monthly as contraceptives. ✓ Implants—Norplant (contraceptives). ✓ IUCD impregnated with levonorgestrel (Progestasert, Mirena). ✓ Vaginal tablet and rings. ✓ Skin patches. ✓ Crinone 8% (90 mg) vaginal gel is a micronized progesterone in dilute emulsion system. Therapeutic Applications ⚫ Pure progesterone as injection in oil or micronized vaginal or oral capsules are used in threatened and recurrent abortions, and in corpus luteal phase deficiency (CLPD). ⚫ High doses of injections are used in advanced endometrial cancer. ⚫ Contraception—Oral in combination with oestrogen, minipills and injectables are used as contraceptives. ⚫ Implants (Norplant) are effective over 5 years. ⚫ IUCDs impregnated with progesterones are available (Mirena). Mirena is effective for 5 years. ✓ Abnormal uterine bleeding. ✓ Dysmenorrhoea, premenstrual tension syndrome. ✓ Endometriosis. Though danazol is the drug of choice, owing to the cost and hirsutism, progestogens continue to be employed in endometriosis. 228 | P a g e ✓ Endometrial ablation in AUB. Prior to the TCRE (transcervical resection of endometrium), endometrial shrinkage is achieved by progestogens given over 4 to 6 weeks. ✓ Amenorrhoea. Progesterone challenge test—A single injection of 100 mg progesterone will induce withdrawal bleeding if endometrium is primed by oestrogen. Oral tablets also work. (Primolut-N 5 mg tid 3 3 days) ✓ Post-coital pill—Levonorgestrel 0.75 mg tablet given within 72 h of unprotected coitus and repeated 12 h later will prevent pregnancy in 98% cases. ✓ With oestrogen in HRT. ✓ Postponement of menstruation—5 mg norethisterone tid for 4 to 5 days or longer will delay onset of menstruation (starting 3 days prior to anticipated period). ✓ Allyl progesterone is used in abortions ✓ Progestogens are used as ‘add back’ therapy with GnRH to prevent osteoporosis and allow prolonged GnRH therapy. Contraindications ✓ Undiagnosed vaginal bleeding. ✓ Breast cancer, breast tumour. ✓ Thromboembolism. Side Effects ✓ Nausea, vomiting. ✓ Headache, mastalgia, water retention, cramps in the legs, weight gain. ✓ Hirsutism in androgen-related compounds. ✓ Depression. ✓ Increased low-density lipoproteins and cardiovascular accidents. ✓ Deep venous thrombosis, pulmonary embolism with desogestrel and gestodene. ✓ Breast tumours, cancer. 229 | P a g e ✓ Medroxyprogesterone acetate causes bone loss. ✓ Increase in LDL and decrease in HDL. 186. Androgens (danazol, gestrinone): actions, preparations, indications, side effects. Ans: Danazol: ⚫ Danazol is an isoxazole derivative of 17-alpha ethinyl testosterone. ⚫ It has got both androgenic and anabolic properties. ⚫ It is strictly antigonadotropin but acts as an androgen agonist 230 | P a g e Mode of Action The mechanism of action is complex and includes the following: ⚫ ™Acting on the hypothalamo-pituitary-gonadal axis → depression of frequency of GnRH pulses →suppression of pituitary FSH and LH surge. ⚫ There is, however, no change in the basal gonadotropin level. ⚫ Due to this reason the word 'pseudomenopause' seems misnomer; while the estrogen level is reduced but unlike menopause, the gonadotropins remain ⚫ static in base levels. ⚫ Reduces the liver synthesis of sex hormone-binding globulin (SHBG) and as such, free testosterone is increased which in turn has got direct action on endometrial atrophy. ⚫ Acts directly on the ovaries, inhibiting the enzymes responsible for steroidogenesis. ⚫ Estrogen level is low. ⚫ Binds with steroid receptors on the endometrium and also in the ectopic endometrial sites. ⚫ Immunologic effects of danazol include decrease in serum immunoglobulins (Igs), interleukin-1 (Il-1) and tumor necrosis factor (TNF) production. This effect helps in the regression of endometriosis. The net result is production of an hypoestrogenic and hyperandrogenic state. Precautions It should be commenced in the early follicular phase of the menstrual cycle. Barrier method of contraception should be used to avoid being administered during early pregnancy following accidental ovulation. There is a chance of virilization of the female offspring. It is contraindicated in liver disease. Dose Depending upon the indication and response, the dose varies from 200–800 mg daily orally. Side Effects 231 | P a g e The side effects are mostly related to hypoestrogenic and androgenic activity. However, most of these effects revert back to normal soon following stoppage of the therapy. It is recommended that the patient should discontinue the treatment, if they develop hirsutism or hoarseness of voice. Gestrinone Gestrinone is a derivative of 19-norethisterone. It is an androgen-agonist and progesterone agonist-antagonist. It markedly reduces SHBG levels and thus increases the free testosterone. It reduces the secretion of FSH and LH. It has a much longer half-life and the dose required to produce equivalent results, is much smaller than danazol. Dose 2.5 mg twice weekly starting on first day of cycle with second dose 3 days later, repeated on same two days preferably at same time each week. Side Effects This are the same to those of danazol but usually less marked 187. Antioestrogens (clomiphene citrate, tamoxifen): mode of actions, indications, contraindications, side effects. Ans: Clomiphene ✓ Clomiphene citrate is a nonsteroid triphenylethylene compound with a structure similar to that of stilbestrol. ✓ The commercially available form is a mixture of two isomers, enclomiphene—a potent antiestrogen and zuclomiphene—a weak antiestrogen. Mode of Action 232 | P a g e ✓ In the hypothalamus, clomiphene citrate binds to estrogen receptors, occupies the nuclear site for a long time (weeks). ✓ The negative feedback of endogenous estrogen is thus prevented. ✓ The frequency of pulsatile GnRH secretion is thereby increased which in turn results in rise of pulse frequency of both LH and FSH. ✓ Antiestrogenic effects are observed at the level of cervix and endometrium. Indications ✓ Anovulatory infertility where other factors have been excluded. ✓ Induction of ovulation—the ideal case is one of normogonadotropicnormoprolactinemic disorders of ovulation. ✓ Assisted reproductive techniques in producing superovulation. ✓ Male infertility with defective spermatogenesis due to hypogonadotropic hypogonadism. Mode of Administration Adjuvant drugs: Adjuvant drugs are used when there is failure with clomiphene therapy. Contraindications ✓ Patients who are hypogonadotropic and hypoestrogenic. ✓ Presence of cystic ovaries. Side Effects ✓ These include visual disturbances, headache, hot flashes, breast tenderness, abdominal discomfort, loss of hair, rashes, ovarian enlargement and multiple pregnancy. ✓ Hyperstimulation syndrome is less likely. Results ✓ While successful induction can be achieved by 90%, pregnancy rate is about 50%. ✓ The reduced pregnancy rate may be due to its antiestrogenic effect on endometrium cervical mucus and the oocyte. 233 | P a g e ✓ There may be the presence of other factors for infertility including luteal phase defect (LPD) and luteinized unruptured follicle (LUF). ✓ Chance of multiple pregnancy ranges 0–5%. Aromatase Inhibitors ⚫ It inhibits the enzyme aromatase in the granulosa cells of ovarian follicles. It suppresses estrogen synthesis. ⚫ Letrozole, 2.5 mg given from D3 to D7 increases the release of gonadotropins from the pituitary and stimulates development of ovarian follicle. ⚫ Letrozole suppresses ovarian estradiol secretion and reduces estrogen induced negative feedback. ⚫ As a result, levels of FSH rises. ⚫ Intraovarian androgens are increased which increase FSH sensitivity. ⚫ As opposed to clomiphene, it has no peripheral antiestrogenic effects on the endometrium and the cervical mucus. ⚫ Half-life of letrozole is 45 hours. ⚫ Letrozole is used either as a firstline therapy (alternative to clomiphene) or in clomiphene-resistant women with anovulatory infertility. ⚫ Pregnancy rates are comparable or better than that of clomiphene. ⚫ Multiple pregnancy rates are low (monofollicular development). ⚫ However risk of fetal congenital malformations with letrozole, needs authentication with randomized prospective trials. ⚫ Anastrozole, another aromatase inhibitor is found to be effective in reducing the growth of pelvic endometriosis and in pain relief. ⚫ Aromatase inhibitors are primarily used for the treatment of breast cancer in postmenopausal women. Tamoxifen (SERMs) ⚫ Tamoxifen [Selective estrogen receptor modulators (SERMs)], is similar to clomiphene both structurally and functionally. 234 | P a g e ⚫ It has got both estrogen antagonist and agonist effects. ⚫ It is a competitive inhibitor to estrogen at the receptor site. ⚫ Antiestrogenic function of raloxifene is more selective in uterus and breasts. ⚫ It decreases antithrombin III and increases the SHBG level (agonist action). Venous thromboembolism (VTE) is increased. ⚫ It can be used for induction of ovulation in doses of 20 mg per day for 5 days, in cases of intolerance to clomiphene. ⚫ It is widely used for the treatment of benign breast diseases. ⚫ In postmenopausal breast carcinoma, it is given in doses of 10 mg twice daily for 2 years as an adjuvant therapy. ⚫ It is effective both in estrogen receptor positive and negative cases. ⚫ In recurrent endometrial carcinoma, it inhibits the binding of estradiol to the estrogen receptor. ⚫ Tamoxifen increases the progesterone receptors. ⚫ A dose of 20–40 mg per day has been used. ⚫ Low grade tumors and hormone receptor positive tumors have got better response. Raloxifene therapy (60 mg a day) is effective in regression of endometriosis. Side Effects Hot flashes, vaginal dryness, risks of thromboembolism and risks of endometrial carcinoma on prolonged use. 188. Antiprogesterone (mifiprestone): contraindications, side effects. therapeutic applications, Ans: Mifepristone RU486 ⚫ It is a competitive antagonist of progesterone and glucocorticoid receptors ⚫ It is a derivative of 19-nortestosterone. ⚫ It binds competitively to progesterone receptors and nullifies the effect of endogenous progesterone. 235 | P a g e ⚫ As a result, there is an increased release of prostaglandins from the endometrium, resulting in menstrual bleeding or termination of early pregnancy. ⚫ Three important biochemical characters of RU 486 are high affinity for progesterone receptors, long half-life and active metabolites. Uses Therapeutic abortion: It is an effective abortifacient upto 7 weeks. Combination of prostaglandins as vaginal pessary 48 hours after RU 486, increases its efficacy. Dose Tab 200 mg (1 tab = 200 mg) orally, followed immediatly or upto 72 hours later by misoprostol 400 µg (PGE1) oral or 800 mg vaginal pessary, sublingual or buccal. Success rate is 95–100%. Emergency contraception: A single dose of 10 mg is to be taken on 27th day of the cycle irrespective of the day and number of intercourse. Efficiency is 95– 100%. Induction of labor: Mifepristone has been used for cervical ripening. It is given orally. Uterine fibroids: Mifepristone therapy (5–50 mg daily) for 12 weeks is given. Shrinkage of leiomyomas volume occurs by about 50%. It reduces the symptoms (pain relief) also. Endometriosis: A dose of 50 mg/day for 6 months is found to reduce pelvic pain and the extent of spread. Ectopic pregnancy: Injection of mifepristone into the ectopic pregnancy (unruptured sac) is used as a medical management. Cushing’s syndrome: As it blocks the glucocorticoid receptors. Side Effects ✓ Minor side effects are nausea, vomiting, headache and cramp. ✓ There is risk of ongoing pregnancy (failure of medical induction of abortion) in about 1% of cases. ✓ Evacuation of the uterus should be done for such a failure. ✓ Other side effects are: Vasomotor symptoms (40%), endometrial hyperplasia (due to unopposed estrogen effect). ✓ Asoprisnil, a SPRL is found to avoid estrogen deficiency symptoms. 236 | P a g e Contraindications • Age >35 years • Heavy smoker • Adrenal insufficiency • Corticosteroid therapy. 189. Antiandrigens (ciproterone acetate, spironolactonc, flutamide. finasteride): therapeutic applications, dosages, side effects. Ans: Antiandrogens ⚫ Cyproterone acetate ⚫ Spironolactone ⚫ Flutamide ⚫ Finasteride Cyproterone Acetate ✓ Cyproterone acetate is an hydroxyprogesterone (17-OHP)]. antiandrogenic progestogen [17- ✓ It inhibits gonadotropin secretion and also acts as a competetive androgen receptor antagonist. ✓ It decreases 5α-reductase activity and reduces LH secretion. ✓ It induces hepatic enzymes and increases the metabolic clearance of plasma androgens. ✓ It also acts as a potent progestogen having agonist effects on progesterone receptors. Uses It is used in the idiopathic hirsutism or hyper-androgenic state. Dose ⚫ Cyproterone acetate, 2 mg is most frequently used in combination with ethinyl estradiol. 237 | P a g e ✓ Available preparation (COCs) containing cyproterone acetate, 2 mg and ethinyl estradiol, 35 µg may be given from day 5 for 21 days. Treatment It is to be continued for at least 6 months. Side effects ⚫ Weight gain, loss of libido, mastalgia. ⚫ Spironolactone: It is an androgen receptor antagonist. ⚫ It is an antialdosterone diuretic. ⚫ It also inhibits androgen biosynthesis from ovary and adrenal. • Inhibits 5α-reductase activity • It competes with androgen at the receptor sites. Dose ✓ The dose varies from 25–150 mg per day. ✓ This may produce hyponatremia and hyperkalemia for which initial monitoring of serum potassium and creatinine is necessary at doses above 100 mg per day. Important side effects Menstrual irregularity (DUB), fatigue, diuresis, and electrolyte imbalance (hyperkalemia). Flutamide ✓ It is a non steroidal androgen receptor antagonist. ✓ It blocks the androgen receptor sites. ✓ Dose of 250 mg daily for 6 months is optimum. ✓ Important side effects are dry skin, decreased libido and hepatotoxicity. Finasteride ⚫ It inhibits 5α-reductase activity. A dose of 5 mg daily is effective for hirsutism without any side effects. ⚫ Ketoconazole inhibits the enzyme for androgen synthesis. ⚫ A dose of 200 mg daily is adequate to reduce the level of androgens. ⚫ Dexamethasone and for other antiandrogens 238 | P a g e 190. Pituitary hormones: therapeutic uses, side effects. ans: Pituitary Hormones Gonadotropins The anterior pituitary gland secretes follicle-stimulating hormone (FSH), LH and prolactin. Therapeutic Uses Therapeutic uses of gonadotropins are: ⚫ Induction of ovulation in anovulatory infertility. ⚫ Those who fail to respond to clomiphene are treated with FSH and LH. ⚫ Infertility caused by pituitary hypofunction also needs this therapy. ⚫ The dose is adjusted according to ultrasonic findings of follicular growth and E2 level. ⚫ The treatment is started on the second day of the cycle and continued until ovulation occurs. ⚫ Induction of multiple ovulation using hyperstimulation protocols for infertile women going through ART as in in vitro fertilization, GIFT, zygote intrafallopian transfer (ZIFT) and ICSI ⚫ Hypogonadotrophic hypogonadism in males. ⚫ Cryptorchism. ⚫ In primary and secondary amenorrhoea caused by pituitary failure in hypogonadotropic hypogonadism. ⚫ hCG is used in CLPD, infertility and early abortions ⚫ No teratogenicity is reported. ⚫ 250 µg recombinant hCG is equal to 5000 IU of hCG with less local side effects. Side Effects The side effects are: 239 | P a g e ✓ Hyperstimulation syndrome. ✓ Multiple pregnancy in 10%. ✓ Local reaction at the site of injection, fever, arthritis. Anti-FSH and anti-LH are in the process of being developed as contraceptives. 191. Gonadotropin-releasing hormones and its analogues: praparations, clinical uses, side effects. ans: Gonadotropin Releasing Hormone (GnRH) ⚫ The GnRH is also named as luteinizing hormone releasing hormone (LHRH). ⚫ GnRH is a decapeptide and is concerned with the release, synthesis and storage of both the gonadotropins (follicle-stimulating hormone (FSH) and LH) from the anterior pituitary. ⚫ The divergent patterns of FSH and LH in response to a single GnRH are due to modulating influence of the endocrine environment specially the feedback effects of steroids on anterior pituitary gland. ⚫ GnRH is secreted by the arcuate nucleus of the hypothalamus in a pulsatile fashion. ⚫ Developmentally, these neurons originated from the olfactory area. ⚫ The half-life of GnRH is very short (2–4 minutes). ⚫ This is due to the cleavage of amino acid bonds between 5–6, 6–7 and 9–10 in circulation. ⚫ GnRH is secreted into the portal circulation in pulsatile fashion. ⚫ This pulse secretion varies in frequency and amplitude at different phases of menstrual cycle. ⚫ GnRH stimulates anterior pituitary for synthesis, storage and secretion of 240 | P a g e gonadotropins. ⚫ There is decrease in receptor sensitivity when gonadotroph cells (adenohypophysis) are exposed to GnRH stimulation continually. ⚫ This is called ‘down regulation’. ⚫ On the contrary, intermittent exposure of GnRH to gonadotrophs, increase the receptor sensitivity. ⚫ This is called ‘up-regulation’. ⚫ This variable response of anterior pituitary gonadotrophs to GnRH have been utilized in different clinical situation to get therapeutic benefits. uses: GnRH agonists are useful in: Suppression of spontaneous ovulation as part of controlled ovarian hyperstimulation, which is an essential component in in vitro fertilisation(IVF). Typically, after GnRH agonists have induced a state of hypoestrogenism, exogenous FSH is given to stimulate ovarian follicle, followed by human chorionic gonadotropins (hCG) to trigger oocyte release. GnRH agonists routinely used for this purpose are: buserelin, leuprorelin, nafarelin, and triptorelin.[8] • Final maturation induction after having performed controlled ovarian hyperstimulation. Usage of GnRH agonist for this purpose necessitates using a GnRH antagonist instead of a GnRH agonist for suppression of spontaneous ovulation, because using GnRH agonist for that purpose as well inactivates the axis for which it is intended to work for final maturation induction. • Treatment of cancers that are hormonally sensitive and where a hypogonadal state decreases the chances of a recurrence. Thus they are commonly employed in the medical management of prostate cancer and have been used in patients with breast cancer. • • Delaying puberty in individuals with precocious puberty. Delaying puberty pending treatment decisions in children with gender dysphoria. • 241 | P a g e Management estrogenproduction. • of female disorders that are dependent on Women with menorrhagia, endometriosis, adenomyosis, or uterine fibroids may receive GnRH agonists to suppress ovarian activity and induce a hypoestrogenic state. • Suppressing sex hormone especially transgender women. • levels in transgender people, Severe cases of hyperandrogenism, such as in congenital adrenal hyperplasia. • As part of the pharmacologic treatment of paraphilic disorders in sexual offenders or men with a high risk of sexual offending. • side effects: Common side effects of the GnRH agonists and antagonists include symptoms of hypogonadism such as hot flashes, gynecomastia, fatigue, weight gain, fluid retention, erectile dysfunction and decreased libido. Long term therapy can result in metabolic abnormalities, weight gain, worsening of diabetes and osteoporosis. 192. Bromocriptine: therapeutie applications, doses, side effects. Ans: Bromocriptine Bromocriptine, a synthetic ergot derivative (lysergic acid derivative of ergoline) and a powerfuldopamine agonist. It suppresses prolactin while promoting the secretion of gonadotropins. It thus induces menstruation, ovulation and promotes pregnancy. It also suppresses lactation. ⚫ Bromocriptine is available as parlodel, proctinal, cabergoline, serocrip tablets. ⚫ Pergolide is now also available as a vaginal tablet and intramuscular injection by the name parlodel-LAR (glycolipid microspheres). 242 | P a g e Contraindications Hypertension, cardiovascular disease. Therapeutic Applications Bromocriptine’s therapeutic uses are: ✓ Suppression of lactation—2.5–5 mg daily orally. ✓ Cyclical mastalgia. ✓ Anovulatory infertility caused by hyperprolactinaemia ✓ Treatment of microadenoma and preoperatively in macroadenoma to shrink the tumour prior to surgery. In infertility due to hyperprolactinaemia, 70% to 90% ovulate and menstruation is established, 70% pregnancy rate is also encouraging. If pregnancy follows, the treatment should be discontinued,mthough no teratogenic effect is reported in the fetus. In pregnancy, the level of prolactin rises and the followup is mainly by fundus examination which suggests optic nerve pressure by the tumour. Bromocriptine can be continued during pregnancy if the tumour appears to increase in size as suggested by fundus examination. Cabergoline is safe during pregnancy. Dose The dose starts with 1.25 mg at bedtime and gradually increases to 2.5 mg bid or more as required. The effect lasts 12 h. In those who cannot tolerate the oral drug or in resistant cases, the vaginal tablet or cream is to be used daily. Alternately, the long-acting tablet in the name of cabergoline (dostinex) is available. Starting with an initial dose of0.25 mg twice weekly, the dose is gradually built up to 1 mg twice weekly. It acts at a D2 receptor site.Parlodel-LAR monthly intramuscular injection, used in the initial dose of 50 mg increasing to 100 mg if necessary, causes acute reduction in prolactin level by 30% to 80%, reduction in tumour volume by 25% with minimal side effects.Quinagolide 25–150 µg daily in divided doses followed by maintenance dose 75 µg daily. Side Effects The side effects are seen in 10%: ⚫ Nausea, vomiting; the patient is advised to take the tablet at night. ⚫ Hypotension and dizziness due to postural hypotension. ⚫ Nasal congestion, headache, constipation. 243 | P a g e Results The drugs normalize prolactin level in 86% of idiopathic hyperprolactinaemia and 77% in microadenoma. The macroadenoma shrinks in 70%. Some require surgery. 193. Physiology of conception. Ans: Factors Essential for Conception ⚫ Healthy spermatozoa should be deposited high in the vagina at or near the cervix (male factor). ⚫ The spermatozoa should undergo changes (capacitation, acrosome reaction) and acquire motility (cervical factor). ⚫ The motile spermatozoa should ascend through the cervix into the uterine cavity and the fallopian tubes. ⚫ There should be ovulation (ovarian factor). ⚫ The fallopian tubes should be patent and the oocyte should be picked up by the fimbriated end of the tube (tubal factor). ⚫ The spermatozoa should fertilize the oocyte at the ampulla of the tube. ⚫ The embryo should reach the uterine cavity after 3–4 days of fertilization. ⚫ The endometrium should be receptive (by estrogen, progesterone, IGF-l, ⚫ cytokines, integrins) for implantation, and the corpus luteum should function adequately. PHYSIOLOGICAL CONSIDERATION ⚫ Due to anovulation, infertility is the rule prior to puberty and after menopause. ⚫ But it should be remembered that the girl may be pregnant even before menarche and pregnancy is possible within few months of menopause. ⚫ Conception is not possible during pregnancy as the pituitary gonadal axis is suppressed by hCG and hence, no ovulation. ⚫ During lactation, infertility is said to be relative. ⚫ Despite the fact that the patient is amenorrheic during lactation, ovulation and 244 | P a g e conception can occur. ⚫ However, in fully lactating women (breastfeeding 5–6 times a day and spending 60 minutes in 24 hours), pregnancy is unlikely up to 10 weeks postpartum. 194. Vaginismus: definition, aethiology, pathogenesis, symptoms and sings,treatment. ans: Vaginismus Definition Vaginismus is defined as the psychogenically mediated involuntary spasm of the vaginal muscles including the levator ani muscles and/or the thigh adductor muscles. This results in inability of penetrative sexual intercourse. Etiology Primary: Nothing has entered into the woman’s vagina ever. However, the vagina is normal anatomically and physiologically. The cause is mostly psychosexual in origin. There is often presence of a subconscious fear of sexual intercourse (sexual phobias). Secondary: Vaginismus usually appear after childbirth or any other event in life. There is usually some local painful lesions. Such lesions include vulvitis, lacerations of the hymen, tender scar on the perineum or narrow vaginal introitus. The entity is usually transient and is relieved, when the cause is removed. Clinical Presentation The woman with vaginismus avoids vaginal examination and smear. She might present with painful sexual intercourse or with infertility. Diagnosis While diagnosis of the secondary one is not so difficult but to find out the cause of the primary one, examination under anesthesia may be required. If the two fingers can 245 | P a g e be easily introduced through the vaginal introitus, the caliber of the vagina is proved normal. Treatment primary Secondary Primary: The following guidelines are prescribed : ⚫ Psychodynamic therapy: Main causes of fear are removed. To educate and to gain confidence of the husband and wife. This may take time. ⚫ Behavioral therapy: Dilatation of the vaginal introitus digitally followed by introduction of gradually increasing size of the dilators is to be done. Plastic vaginal trainers (pseudopenises) with graduated sizes can help her to remove her fear. This will gain her confidence that her vagina is anatomically of normal caliber. ⚫ Vaginal dilators: Daily introduction of the dilators (pseudopenises) for 1–2 weeks and to keep it inside for 10–15 minutes is enough before she is allowed to attempt coital act. ⚫ Surgery: A classic case of vaginismus needs no surgery. However, surgery may be required, if the hymen is found tight—hymenectomy or Fenton’s operation (operation to enlarge the introitus), if the introitus is narrow Secondary: The local lesion is to be treated medically or surgically. 195. Dyspareunia: definition, causes, investigations and treatment. 246 | P a g e Ans: Dyspareunia Definition Dyspareunia means that the coital act is difficult and or painful. Apareunia is inability to practice coitus. The two are most often interchangeable. Dyspareunia is the most common sexual dysfunction. Etiology: Male causes: The following male factors are responsible: ⚫ Impotence ⚫ Premature ejaculation ⚫ Congenital anatomic defect of the penis ⚫ Lack of technique of coital act. Female causes Depending upon the site of pain, the dyspareunia may be either: ⚫ Superficial or entrance ⚫ Vaginal ⚫ Deep. Superficial: Any lesion of the lower part of the labia minora or around the fourchette may be responsible. Causes of Superficial Dyspareunia Norrow introitus Tough hymen Bartholin's gland cysts Tender perineal scar Vulvar infection Urethral pathology Vulvar vestibulitis syndrome Vaginal: Burning pain along the barrel of vagina either during or following intercourse is the presenting complaint. Common causes are: 247 | P a g e ⚫ Vaginitis ⚫ Vaginal septum ⚫ Tender scar—following gynecologic operation or ⚫ delivery ⚫ Secondary vaginal atresia ⚫ Tumor ⚫ Vaginal atrophy (menopause). Deep: The patient experiences pain while the penis penetrates deep into the vagina. As the vagina is insensitive to pain, deep dyspareunia usually results from pathology of paravaginal tissues or other pelvic organs. Such lesions are: ⚫ Endometriosis, specially on rectovaginal septum ⚫ Chronic cervicitis ⚫ Chronic PID ⚫ Retroverted uterus—mostly acquired and fixed ⚫ Prolapsed ovary in the pouch of Douglas. Treatment Treatment depends upon the cause. Too often, sex education of both the partners relieves the symptom. The infective lesions of the vulva and or vagina are to be treated. Tender scar on the perineum or the vagina is to be excised. The treatment of vaginismus has been mentioned earlier. 196. Infertility and sterility: issues involved, theoretical considerations. Psychological problems in infertulity. Ans: 248 | P a g e ⚫ Infertility is defined as a failure to conceive within one or more years of regular unprotected coitus. ⚫ Primary infertility denotes those patients who have never conceived. Secondary infertility indicates previous pregnancy but failure to conceive subsequently. ⚫ Fecundability is defined as the probability of achieving a pregnancy within one menstrual cycle. In a healthy young couple, it is 20%. ⚫ Fecundity is the probability of achieving a livebirth within a single cycle. 197. Male infertility: spermatogenesis and its endocrine control. Causes, classification of infertility, investigations, treatment of male infertility. Ans: Male Infertility The treatment of male is indicated in: (i) Extreme oligospermia; (ii) Azoospermia; (iii) Low volume ejaculate and (iv) Impotency. ⚫ Management is often difficult and unsatisfactory. To improve spermatogenesis the following measures may be helpful. ⚫ General care: Improvement of general health, reduction of weight in obese, avoidance of alcohol and heavy smoking. ⚫ Medications that interfere spermatogenesis should be avoided. ⚫ In hypogonadotropic-hypogonadism, the disorders of spermatogenesis can be treated with the following therapy with varying success. ✓ hCG 5000 IU intramuscularly once or twice a week is given to stimulate endogenous testosterone production. ✓ hMG or pure FSH (75–150 IU) is added to hCG when there is no sperm in the ejaculate with hCG alone. ✓ Dopamine agonist (cabergoline) is given in hyperprolactinemia to restore 249 | P a g e normal prolactin and testosterone level. This improves libido, potency and fertility. ✓ Pulsatile GnRH therapy in infertile male with GnRH deficiency (Kallmann’s syndrome) is effective. ✓ It is administered by minipump infusion. ✓ Target is to maintain normal adult 'male' LH levels. ✓ Cases with hypogonadotropic hypogonadism may also respond with GnRH therapy. Hypergonadotropic-hypogonadism, no form of medical treatment can improve fertility in men . ✓ Treatment options available are insemination with donor sperm or adoption when no sperm is available. IVF with ICSI may be done in cases with severe oligospermia. ✓ Clomiphene citrate 25 mg orally daily for 3 months is given. It increases serum level of FSH, LH and testosterone. ✓ Presence of antisperm antibodies in the male and its significance is unclear. Currently intrauterine insemination (lUI) is the choice of treatment for such cases Leukocytospermia: Genital tract infection needs prolonged course of antibiotics. ✓ Generally doxycycline or erythromycin is given for a period of 4–6 weeks, depending on the response. ✓ However, leukocytospermia does not always predict infection and it may not have any effect on fertility. Retrogradeejaculation:Phenylephrine(D-adrenergic agonist) is used to improve the tone of internal urethral sphincter. ✓ Sperm may be recovered from the neutralized urine. Processed spermatozoa could be used for lUI. Teratospermia, asthenospermia: Specific causes are unknown. No treatment is available. Donor insemination (AID) is the option. Genetic abnormality: Artificial insemination with donor sperm (AID) is the option as no other treatment is available. 250 | P a g e Surgical ✓ When the patient is found to be azoospermic and yet testicular biopsy shows normal spermatogenesis, obstruction of vas must be suspected. ✓ This should be corrected by microsurgery—vasoepididymostomy or vasovasostomy. ✓ After vasovasostomy patency is obtained in about 80% of cases and pregnancy rate is about 50%. ✓ Surgery for varicocele for improvement of fertility is not helpful. Hydrocele is corrected by surgery. ✓ Orchidopexy in undescended testes should be done between 2–3 years of age to have adequate spermatogenesis in later life. Impotency ✓ Psychosexual treatment may be of help. ✓ Hyperprolactinaemia needs further investigation and treatment. ✓ For erectile dysfunction sildenafil (25–100 mg) or tadalafil (10–20 mg) is currently advised. ✓ A single dose (depending on response) is given orally one hour before sexual activity. ✓ In unresponsive cases, artificial insemination is to be thought of use. Assisted Reproductive Technology (ART) for Male Infertility Prospect of male infertility has improved significantly with the advent of ART. ✓ IUI, TESE, PESA, MESA and intracytoplasmic sperm injection (ICSl) are now the treatment available for infertile males. 198. Female infertility: Aetiology, investigations. Ans: aetiology: Ovulation disorders Ovulating infrequently or not at all accounts for most cases of infertility. Problems with the regulation of reproductive hormones by the hypothalamus or the 251 | P a g e pituitary gland or problems in the ovary can cause ovulation disorders. * Polycystic ovary syndrome (PCOS). PCOS causes a hormone imbalance, which affects ovulation. PCOS is associated with insulin resistance and obesity, abnormal hair growth on the face or body, and acne. It's the most common cause of female infertility. * Hypothalamic dysfunction. Two hormones produced by the pituitary gland are responsible for stimulating ovulation each month — follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Excess physical or emotional stress, a very high or very low body weight, or a recent substantial weight gain or loss can disrupt production of these hormones and affect ovulation. Irregular or absent periods are the most common signs. * Primary ovarian insufficiency. Also called premature ovarian failure, this is usually caused by an autoimmune response or by premature loss of eggs from your ovary, possibly as a result of genetics or chemotherapy. The ovary no longer produces eggs, and it lowers estrogen production in women under age 40. * Too much prolactin. The pituitary gland can cause excess production of prolactin (hyperprolactinemia), which reduces estrogen production and can cause infertility. This can also be caused by medications you're taking for another condition. Damage to fallopian tubes (tubal infertility) Damaged or blocked fallopian tubes keep sperm from getting to the egg or block the passage of the fertilized egg into the uterus. Causes of fallopian tube damage or blockage can include: * Pelvic inflammatory disease, an infection of the uterus and fallopian tubes due to chlamydia, gonorrhea or other sexually transmitted infections * Previous surgery in the abdomen or pelvis, including surgery for ectopic pregnancy, in which a fertilized egg implants and develops somewhere other than the uterus, usually in a fallopian tube Endometriosis Endometriosis occurs when tissue that typically grows in the uterus implants and grows in other places. This extra tissue growth — and the surgical removal of it — can cause scarring, which can block fallopian tubes and keep an egg and sperm from uniting. Endometriosis can also disrupt implantation of the fertilized egg. The condition also seems to affect fertility in less-direct ways, such as damage to the sperm or egg. Uterine or cervical causes 252 | P a g e Several uterine or cervical causes can interfere with the egg implanting or increase the risk of miscarriage: * Benign polyps or tumors (fibroids or myomas) are common in the uterus. Some can block fallopian tubes or interfere with implantation, affecting fertility. However, many women who have fibroids or polyps do become pregnant. * Problems with the uterus present from birth, such as an unusually shaped uterus, can cause problems becoming or remaining pregnant. * Cervical stenosis, a narrowing of the cervix, can be caused by an inherited malformation or damage to the cervix. * Sometimes the cervix can't produce the best type of mucus to allow the sperm to travel through the cervix into the uterus. Unexplained infertility In some cases, the cause of infertility is never found. A combination of several minor factors in both partners could cause unexplained fertility problems. Although it's frustrating to get no specific answer, this problem can correct itself with time. But you shouldn't delay treatment for infertility. INVESTIGATIONS: * Ovulation testing. An at-home, over-the-counter ovulation prediction kit detects the surge in luteinizing hormone (LH) that occurs before ovulation. A blood test for progesterone — a hormone produced after ovulation — can also document that you're ovulating. Other hormone levels, such as prolactin, also might be checked. * Hysterosalpingography. During hysterosalpingography (his-tur-o-sal-ping-GOGruh-fee), X-ray contrast is injected into your uterus and an X-ray is taken to check for problems inside the uterus. The test also shows whether the fluid passes out of the uterus and spills out of your fallopian tubes. If any problems are found, you'll likely need further evaluation. * Ovarian reserve testing. This testing helps determine the quality and quantity of eggs available for ovulation. Women at risk of a depleted egg supply — including women older than 35 — might have this series of blood and imaging tests. * Other hormone testing. Other hormone tests check levels of ovulatory hormones as well as thyroid and pituitary hormones that control reproductive processes. * Imaging tests. A pelvic ultrasound looks for uterine or fallopian tube disease. Sometimes a sonohysterogram, also called a saline infusion sonogram, or a hysteroscopy is used to see details inside the uterus that can't be seen on a 253 | P a g e regular ultrasound. Depending on your situation, rarely your testing might include: * Laparoscopy. This minimally invasive surgery involves making a small incision beneath your navel and inserting a thin viewing device to examine your fallopian tubes, ovaries and uterus. A laparoscopy can identify endometriosis, scarring, blockages or irregularities of the fallopian tubes, and problems with the ovaries and uterus. * Genetic testing. Genetic testing helps determine whether there any changes to your genes that may be causing infertility. 199. Tubal infertility: tests for tubal patency, newer diagnostics techniques, management of tubal infertility. Ans: tubal infertility: is female infertility caused by diseases, obstructions, damage, scarring, congenital malformations or other factors which impede the descent of a fertilized or unfertilized ovum into the uterus through the Fallopian tubes and prevents a normal pregnancy and full term birth. Tubal factors cause 25-30% of infertility cases. Tubal factor is one complication of Chlamydia trachomatis infection in women. Tests for tubal patency: x Dilatationandinsufflationtest(DI) x Hysterosalpingography(HSG) x Salineinfusionsonography x Hysterosalpingocontrastsonography(Hycosy) x Sonohysterosalpingography x Laparoscopyandchromopertubation x Falloposcopy x Salpingoscopy Diagnosis: In the presence of biologic effects of progesterone in the early luteal phase: x Sonography: Persistence of echo-free dominant follicle beyond 36 hours after LH peak. x Laparoscopy: Failure to observe a stigma of ovulation. x Ovarian biopsy: 254 | P a g e Conclusive proof is determination of ovum amidst the structure of corpus luteum. Management: For women with infections of mild to moderate severity, parenteral and oral therapies are prescribed . Typical antibiotics used are cefoxitin or cefotetan plus doxycycline, and clindamycin plus gentamicin. An alternative parenteral regimen is ampicillin/sulbactam plus doxycycline. Once infection has been eliminated, surgery may be successful in opening the lumen of the fallopian tubes to allow a successful pregnancy and birth. 255 | P a g e 256 | P a g e 200. Anovulation: tests of ovulation (basal body temperature, endometrial biopsy, fern test, ultrasound, hormonal study). Management of anovulation. The ovarian activity is totally dependent on the gonadotropins and the normal secretion of gonadotropins depends on the pulsatile release of GnRH from hypothalamus. As such, ovarian dysfunction is likely to be linked with disturbed hypothalamo-pituitaryovarian axis either primary or secondary from thyroid or adrenal dysfunction. Thus, the disturbance may result not only in anovulation but may also produce oligomenorrhea or even amenorrhea. Other causes of anovulation are: Polycystic ovarian syndrome, elderly women and women with premature ovarian failure A. Basal body temperature (BBT) Observation:There is “biphasic pattern” of temperature variation in ovulatory cycle. If pregnancy occurs, the rise of temperature sustains along with absence of the period. In anovulatory cycle, there is no rise of temperature throughout the cycle Clinical importance: Maintenance of BBT chart during investigation is of help in determining ovulation and timing of post-coital test, endometrial biopsy, cervical mucus or vaginal cytology study for ovulation. It also helps the couple to determine the most fertile period, if the cycle is irregular B. Endometrial biopsy Endometrial tissues to detect ovulation (endometrial sampling) can easily be obtained as an outpatient procedure using instruments such as Sharman curette or Pipelle endometrial sampler. Dilatation and curettage is, however reserved in cases where bulk endometrial study is required as in endometrial tuberculosis. Findings: Evidences of secretory activity of the endometrial glands in the second half of the cycle give not only the diagnosis of ovulation but can predict the functional integrity of the corpus luteum. Subnuclear vacuolation is the earliest evidence appearing 36–48 hours following ovulation. Cause: The secretory changes are due to the action of progesterone on the estrogen primed endometrium. C. Fern test – during the midcycle, the cervical mucus is obtained by a platinum loop or pipette and spread on a clean glass slide and dried. When seen under low power microscope, it shows characteristic pattern of fern formation. It is due tohigh sodium chloride, low protein content in the mucus, high estrogen in the midmenstrual phase prior to ovulation. After ovulation with increasing 257 | P a g e progesterone, the ferning disappears completely after 21st day. Thus, the presence of ferning even after 21st day suggests anovulation and its disappearance is presumptive evidence of ovulation D. Ultrasound Ultrasound has now become the standard and indispensable proce dure for monitoring maturation of the Graafian follicle and in de tecting imminent ovulation in IVF, IUI and in timing intercourse. This requires daily ultrasonic visualization of ovaries from the 10th to 16th day of the menstrual cycle. It is noninvasive, accurate and safe. Apart from follicular study for ovulation, pelvic pathology if any can be picked up and endometrial thickness measured. The follicle grows at the rate of 1-2 mm daily to reach 20 mm or more when follicular rupture and ovulation occur at midcycle. The sudden disappearance of the follicle, presence of free fluid in the pouch of Douglas and growth of corpus luteum are evident. Endometrial thickness of 8-10 mm is the normal response of endometrium to progesterone. A lesser thickness indicates corpus luteal phase deficiency (CLPD). E. hormonal study • Plasma concentration – of progesterone rises after ovulation and reaches the peak of 15 ng/mL at mid-luteal phase (22-23rd day) and then declines as the corpus luteum degenerates. A low level of the plasma progesterone below 5 ng/mL at mid-luteal phase, suggests corpus LPD and prompts hormonal therapy. • LH – surge from the anterior pituitary gland occurs about 24 hours prior to ovulation Radioimmunoassay of the morning sample of urine and blood gives the LH results in 3 hours. Not only does the LH surge help in predicting ovulation, but the approximate time of ovulation can be gauged and ruits around this time can improve the chances of conception Ganging the time of ovulation has therapeu uc applications in IVF and in artificial insemination. I kits are now available. • Hyperprolactinemia – It is seen in pituitary adenoma, hyperplasia, hypothyroidism and with the usage of drugs, Le, metoclopramide, cimettdine, methyldopa. Hyperprolactinemia (more than 25 ng/ ml) will require X-ray of pituitary lossa or CT scan, and it fundus examination to exclude a neoplasm. Macroadeno mas may require surgery. Microadenomas and hyperprolac 258 | P a g e tinaemia respond to Bromocriptine and allied drugs (sce chapter on Hormonal Therapy). • FSH – Raised FSH level is seen in ovarian failure. Low FSH level indicates pituitary dysfunction and anovulation. Normal FSH level in the preovulatory phase is 1-8 mlL ml nd LH level at ovulation is 1-5 mit /mL FSH level 251l/ml clomiphene on day 3 fails ovulation, • Thyroid Tests – These should be done especially in case of by perprolacti naemia Hypothyroidism with raised TSH level is related to hyperprolactinaemia. Ovarian reserve or premature failure includes both qualitative and quantitative estimation of FSH LH. Management of anovulation • Clomiphene Citrate • Letrozole 2.5 mg (nonsteroidal aromatase inhibitor) • In PCOD, ovulation is ideally induced with a combination of CC and h MG • GnRH • Prednisolone • Hyperprolactinemia • Laparoscopic Ovarian Drilling – In women with PCOD in whom induction of ovulation with medical line of treatment fails, laparoscopic ovarian drilling of follicles with monopolar cautery/laser has yielded satisfactory results. 201. Newer reproductive technologies: In-vitro fertilization (IVF), gamete intratallopian transfer (GIFT) technique, micro-assisted fertilization (MAF) technique, MESA amd PESA. 202. i. IVF. This is the most commonly done ART procedure. It involves ovulation induction, oocyte retrieval and fertilization of the oocytes in the laboratory: embryos are then cultured for 3-5 days followed by their transfer to the endometrial cavity (ET). Indications 259 | P a g e ⎯ Idiopathic or unexplained male and female infertility. ⎯ Immunological factor in male and female. ⎯ Blocked fallopian tubes or failed tubal surgery. ⎯ Failed intrauterine or fallopian insemination. ⎯ Mild endometriosis. ⎯ Abnormal semen findings. ⎯ Donor semen or sperm. ii. GIFT. This involves ovarian stimulation and egg retrieval, followed by laparoscopically guided transfer of a mixture of two ova and 50.000 sperms into each of the fallopian tubes. This procedure came with a big bang and popularity, however, is no longer in use. Indications ⎯ Unexplained infertility. ⎯ Failed IUI. ⎯ Male infertility. ⎯ Immunological factor in male. ⎯ Immunological factors in the cervix. ⎯ Donor semen required (rare). iii. Epididymal or testicular aspiration or biopsy. ⎯ This is the latest technology employed in azoospermia caused by blocked vas. The former can be done under local anaesthesia, but testicular biopsy requires general anaesthesia. ⎯ Cryopreservation of semen of the husband and embryos for future fertility is required if the man has to undergo radiation or chemotherapy for malignancy. Alternately, epididymal or testicular aspiration technique is employed. In the latter situation, repeat aspiration can be avoided and sperms cryopreserved. ICSI now supersedes zonal tech- niques because of following reasons: ⎯ It is more successful in improving fertility. ⎯ Spermatozoa as well as spermatids can be employed. Histopathology and karyotype study is possible. ⎯ Cryopreservation saves cost and stress of repeated perfor mance in each cycle. 260 | P a g e ⎯ The low success rate is attributed to older age of the woman undergoing the procedure. Because of the cost and stress of the procedure, women opt for these only if other methods fail. ⎯ We have come a long way in male infertility from initial donor insemination, artificial insemination of washed semen to IVF and ICSI with improved success. 202. Peritoneal disorders: causes, investigations and treatment. GOOGLE ANS Peritonitis is a serious condition that starts in the abdomen. That's the area of the body between the chest and the pelvis. Peritonitis happens when the thin layer of tissue inside the abdomen becomes inflamed. The tissue layer is called the peritoneum. Peritonitis usually happens due to an infection from bacteria or fungi. There are two types of peritonitis: • Spontaneous bacterial peritonitis. This infection is caused by bacteria. It can happen when someone has liver disease, such as cirrhosis, or kidney disease. • Secondary peritonitis. Peritonitis can happen due to a hole, also called a rupture, inside an organ in the abdomen. Or it can be caused by other health conditions. Symptoms of peritonitis include: • Belly pain or tenderness. • Bloating or a feeling of fullness in the abdomen. • Fever. • Upset stomach and vomiting. • Loss of appetite. • Diarrhea. • Reduced urine. • Thirst. • Not able to pass stool or gas. • Feeling tired. • Confusion. If you get peritoneal dialysis, peritonitis symptoms also may include: 261 | P a g e • • Cloudy dialysis fluid. White flecks, strands or clumps — which are called fibrin — in the dialysis fluid. Causes The two main types of peritonitis are primary spontaneous peritonitis, an infection that develops in the peritoneum; and secondary peritonitis, which usually develops when an injury or infection in the abdominal cavity allows infectious organisms into the peritoneum. Both types of peritonitis are life-threatening. The death rate from peritonitis depends on many factors, but can be as high as 40% in those who also have cirrhosis. As many as 10% may die from secondary peritonitis. The most common risk factors for primary spontaneous peritonitis include: Liver disease with cirrhosis. Such disease often causes a buildup of abdominal fluid (ascites) that can become infected. Kidney failure getting peritoneal dialysis. This technique, which involves the implantation of a catheter into the peritoneum, is used to remove waste products in the blood of people with kidney failure. It's linked to a higher risk of peritonitis due to accidental contamination of the peritoneum by way of the catheter. Common causes of secondary peritonitis include: • • • • • • • A ruptured appendix, diverticulum, or stomach ulcer Digestive diseases such as Crohn's disease and diverticulitis Pancreatitis Pelvic inflammatory disease Perforations of the bowel, stomach, intestine, gallbladder, or appendix Surgery Trauma to the abdomen, such as an injury from a knife or gunshot wound Noninfectious causes of peritonitis include irritants such as bile, blood, or foreign substances in the abdomen, such as barium. Primary peritoneal cancer is rare cancer that forms in a thin layer of tissue lining your abdomen (belly). This tissue is called the peritoneum • Primary peritoneal cancer starts inside the cells that make up the peritoneum. 262 | P a g e • Secondary peritoneal cancer starts elsewhere in your body and spreads to the peritoneum. Symptoms in the early stages, they may include: • • • • • • • Abdominal and/or pelvic pain. Abnormal vaginal bleeding or discharge. Bloating or sense of fullness in the abdomen or pelvis. Bowel changes (increased constipation and/or gas) or rectal bleeding. Frequent urination. Indigestion, loss of appetite or feeling full before you finish eating. Unintended weight gain or weight loss. As peritoneal cancer grows, additional symptoms may develop, including: • • • • • Fatigue. Fluid buildup in the abdomen (called ascites). Nausea or vomiting. Shortness of breath (dyspnea). Swelling of your legs. Diagnostic tests for peritonitis may include: • Blood and urine tests • Exploratory surgery • patients who have a combination of abdominal pain and a clouding of the peritoneal fluid, which is caused by a buildup of infection-fighting white blood cells. • Blood tests: These look for a chemical made by certain cancer cells called CA-125. The level of this chemical may be high in people with peritoneal cancer. Blood tests may also look for increased levels of a protein called HE4, which may also be produced by peritoneal cancer cells. • Imaging tests: Ultrasound, MRI or CT scan look for tumors. But peritoneal cancer can be hard to see using these tests. • Laparoscopy: Your provider can perform a laparoscopy to make a diagnosis. This procedure involves several very small incisions in the abdomen. During the procedure, they can do a biopsy to take a sample of abnormal tissues. 263 | P a g e • • These tissues are then examined under a microscope by a pathologist to identify if cancer is present. Paracentesis: If you have ascites, your provider may take a sample of abdominal fluid for testing. Providers often perform peritoneal paracentesis during a laparoscopy. Pelvic exam: An exam of your vagina, cervix, uterus, fallopian tubes, ovaries, and rectum to look for any abnormal areas or lumps. Treatment If you're diagnosed with peritonitis, you'll be admitted to a hospital. Typically, you'll immediately start receiving intravenous antibiotics or antifungal medications to treat the infection. Additional supportive treatments will be necessary if organ failure from sepsis develops as a complication of the infection. Such treatments may include intravenous fluids, drugs to maintain blood pressure, and nutritional support. Treatment of peritoneal cancer depends on the stage of cancer, where the primary tumor started, how far it has spread, and the patient's overall health. In some cases, we might use surgery to remove as much of the cancer as possible. Chemotherapy and radiation therapy are also options for certain patients. 203. Unexplained infertility: causes, investigations and treatment. Unexplained infertility is defined when no obvious cause for infertility has been detected following all standard investigations. These include semen analysis, ovulation detection, tubal and peritoneal factors, endocrinopathy, and PCT. Overall incidence is 10–20%. With expectant management about 60% of couples with unexplained infertility will conceive within a period of 3 years. IVF and ET may be an option for those who fail to respond The incidence is extremely variable and largely dependent on the magnitude of the indepth investigation protocol extended to the couple. The reported incidence varies from 10–30%. About 40% of these couples become pregnant within 3 years without having any specific treatment. Therapy: The prospect of spontaneous conception decreases with increasing age of the woman and the duration of infertility. The recommended treatment for unexplained infertility are induction of ovulation, lUI, Superovulation combined 264 | P a g e with lUI and Assisted Reproductive Technology (see below). Combined factor: The faults detected in both the partners should be treated simultaneously and not one after the other. Sperm dysfunction and its biological function are now detected on computerassisted semen analysis (CASA). Abnormal acrosome reaction and sperm–oocyte fusion defects have been identified by CASA and male infertility problems better understood. It has been observed that 20% of such unexplained infertile couples succeed in having a baby in due course of waiting. Perhaps newer and advanced technology in this field may yield a better pregnancy rate of 40–50% in future, albeit at a high cost 204. Birth control and problems of overpopulation. Demographic problems in India and in Russia. Today, as ever, there is a pressing need for limiting the family size at a personal level and for the control of population at a national level. The need of birth control at a personal level has arisen through increased cost of living, scarcity of accommodation, a desire for better education of children in the present competitive world, and an overall desire for an improved standard of living. The population in India has been growing rapidly. The socio-economic problems of overpopulation are too well known to be discussed here. World population is also a major problem with more than 6.3 billion living on this earth and 26 children born every second. Reproductive health and medical grounds are now the other considerations for birth control. It is reckoned that a woman below 20 years is not physically grown to produce a child. If she does reproduce, she becomes a high-risk case during pregnancy and labour, and is likely to deliver a low birth weight (LBW) newborn. Spacing birth, 3 years apart, is considered beneficial for both the mother and the child. Birth control is thus seen as a woman’s health measure. A multiparous woman from a low-income group generally suffers from malnutrition and is also predisposed to prolapse, stress incontinence, chronic cervicitis and cancer of the cervix. The spacing of childbirth and limiting the number of pregnancies are strongly desirable for this reason. The previous two caesarean sections is indication of a repeat caesarean section in a subsequent pregnancy which exposes the woman to further surgical risks. In India, it is customary to suggest sterilization operation at the time of the third caesarean section, and sometimes during the second caesarean section. Other indications for sterilization include the mentally retarded woman and the one 265 | P a g e suffering from serious psychiatric disorders like schizophrenia. A woman who has given birth to a child with a genetic disorder needs genetic counselling and may be advised against future pregnancy There has always been a need felt for avoiding unwanted pregnancies and restricting family size among the married couples. Such a desire and need has always been higher among women than men. The risks associated with repeated and unwanted pregnancies have serious long-term effects on the health of women and at times the entire family. Nowadays, there is a pressing need for limiting the family size at a personal level and for the control of population at the national level. The need of birth control at a personal level has arisen through an increased cost of living, scarcity of accommodation, a desire for better education of children in the present competitive world and an overall desire for an improved standard of living. There are following three approaches to limiting family size: • Contraceptives - prevent fertilization • Emergency contraception - prevents implantation • Medical termination of pregnancy (MTP) – abortion Benefits of fertility control are interrelated. Benefits are improved quality of life, better health, less physical and emotional stress of life, better education, job, and economic opportunities. Benefits are enjoyed by the couple, the children, other family members, the community and the country Contraception and fertility control are not synonymous. Fertility control includes both fertility inhibition (contraception) and fertility stimulation. While the fertility stimulation is related to the problem of the infertile couples, the term contraception includes all measures, temporary or permanent, designed to prevent pregnancy due to the coital act. Birth control can be done by contraceptive method – A method or a system which allows intercourse and yet prevents conception is called a contraceptive method. METHODS OF CONTRACEPTION 1. Natural methods: • Abstinence during the fertile phase. • Withdrawal method (coitus interruptus). • Breastfeeding (lactational amenorrhoea method [LAM]). 266 | P a g e 2. Barrier contraceptives: • Condoms by male and females. • Spermicidal agents • Diaphragm, or the cervical cap in the vagina, use of a female condom. • Hormones which alter the cervical mucous and prevent entry of sperms into the cervical canal. 3. 4. 5. 6. 7. 8. Intrauterine contraceptive devices (IUCDs). Suppression of ovulation with hormones hormonal contraceptives. Interceptive agents (postcoital contraception). Immunological methods. Suppression of spermatogenesis in males. Surgical sterilization. Problems of overpopulation • Depletion of Natural Resources • Accelerated Habitat Loss • Amplified Climate Change and Global Warming • Loss of Biodiversity • Depreciation of Fresh Water • Lower Life Expectancy and Diminished Quality of Life • Emergence of New Pandemics and Epidemics • Intensive Farming Practices • Rise in Unemployment, Crime Rate, and Violence Demographic problems in India According to the 2022 edition of the United Nations World Population Prospects (WPP), India is projected to surpass China as the world’s most populous country in 2023. India is currently at a stage of demographic transition with a substantial percentage of the youth population. with fertility rates down to as low as 1.19 ⎯ Unfulfilled Educational Requirements ⎯ Low Human Development Parameters ⎯ Jobless Growth ⎯ Absence of Proper Policies 267 | P a g e ⎯ Rise in the Share of Elderly Population Demographic problems in Russia Some of the objective reasons for Russia's demographic problems reflect historical dynamics: the number of women of childbearing age is falling, and the average age at which women are having children is rising steadily in modernized, urban, well-educated populations Recent demographic trends in Russia have caused widespread public concern. Russia is experiencing unusually high death rates from nonnatural causes, many related to alcoholism. Life expectancy, especially among working-age males, has dropped precipitously. The Russian fertility rate has declined to among the world's lowest, while its abortion rate is the highest. As a result, for the first time in Russian history, the annual number of deaths has exceeded the number of births (see Figure 1). Compounding these challenges, the population is aging rapidly—a trend that will accelerate over the next two decades—and immigration continues to increase, posing thorny political and social problems for a nation historically accustomed to a net outflow of people. 205. Contraception: definition and classification. A method or a system which allows intercourse and yet prevents conception is called a contraceptive method. METHODS OF CONTRACEPTION 1. Natural methods: • Abstinence during the fertile phase. • Withdrawal method (coitus interruptus). • Breastfeeding (lactational amenorrhoea method [LAM]). 2. Barrier contraceptives: • Condoms by male and females. • Spermicidal agents • Diaphragm, or the cervical cap in the vagina, use of a female condom. • Hormones which alter the cervical mucous and prevent entry of sperms into the cervical canal. 3. Intrauterine contraceptive devices (IUCDs). 268 | P a g e 4. 5. 6. 7. 8. Suppression of ovulation with hormones hormonal contraceptives. Interceptive agents (postcoital contraception). Immunological methods. Suppression of spermatogenesis in males. Surgical sterilization. a) Temporary Methods – ⎯ Intrauterine Contraceptive Devices (IUCDs) b) Steroidal Contraception’s – ⎯ Combined Oral Contraceptives (Pills) ⎯ Progestogen only Contraceptions ⎯ Emergency Contraception (EC) c) Sterilization ⎯ Couple Counseling ⎯ Male Sterilization ⎯ Female Sterilization d) Barrier Methods ⎯ Condom (Male) ⎯ Female Condom (Femidom) ⎯ Diaphragm ⎯ Vaginal Contraceptives ⎯ Fertility Awareness Method ⎯ Contraceptive Counseling and Prescription ⎯ Sterilization Counseling e) Ongoing Trials ⎯ Transcervical Sterilization ⎯ Male Contraception Methods 206. Natural methods of family planning. 269 | P a g e • Natural family planning is a form of birth control that doesn't involve pills or devices. As a result, it doesn’t have side effects. FERTILITY AWARENESS METHOD • With these methods, you track your fertility, which is when you are most likely to get pregnant a) Rhythm Method – The method is based on identification of the fertile period of a cycle and to abstain from sexual intercourse during that period. The methods to determine the approximate time of ovulation and the fertile period include— (a) recording of previous menstrual cycles (calendar rhythm) (b) noting the basal body temperature chart (temperature rhythm) and (c) noting excessive mucoid vaginal discharge (mucus rhythm). Users of temperature rhythm require abstinence until the third day of the rise of temperature. Users of mucus rhythm require abstinence on all days of noticeable mucus and for 3 days thereafter. b) Coitus Interruptus (Withdrawal) – Coitus Interruptus (Withdrawal) (Table 30.12) It is the oldest and probably the most widely accepted contraceptive method used by man. It necessitates withdrawal of penis shortly before ejaculation. c) Breastfeeding, Lactational Amenorrhea (LAM) – Prolonged and sustained breastfeeding offers a natural protection of pregnancy. This is more effective in women who are amenorrheic than those who are menstruating. When the women is full breastfeeding, a contraceptive method should be used in the 3rd postpartum month and with partial or no breastfeeding, she should use it in the 3rd postpartum week d) Fertility awareness-based methods are: (1) Natural contraception (rhythm method, coitus interruptus, and LAM) (2) Barrier method (condoms, diaphragm, and spermicides) 207. Barrier contraceptives. These methods prevent sperm deposition in the vagina or prevent sperm penetration through the cervical canal. The objective is achieved by mechanical devices or by chemical means which produce sperm immobilization, or by combined means. Types of Barrier Methods 270 | P a g e a) Mechanical • Male — Condom • Female — Condom, diaphragm, cervical cap b) Chemical • (Vaginal contraceptives) • Creams — Delfen (nonoxynol-9, 12.5 %) • Jelly — Koromex, Volpar paste • Foam tablets— Aerosol foams, T or Contab, Sponge (Today) c) Combination • Combined use of mechanical and chemical methods CONDOM (MALE) ❖ Condoms are made of polyurethane or latex ❖ It is the most widely practised method used by the male ❖ Protection against sexually transmitted disease (STD) is an additional advantage FEMALE CONDOM (FEMIDOM) ❖ It is a pouch made of polyurethane which lines the vagina and also the external genitalia. It is 17 cm in length with one flexible polyurethane ring at each end. Inner ring at the closed end is smaller compared to the outer ring. Inner ring is inserted at the apex of the vagina and the outer ring remains outside. It gives protection against STIs cytomegalovirus (CMV) [HIV, hepatitis B virus (HBV)] and pelvic inflammatory disease DIAPHRAGM ❖ It is an intravaginal device made of latex with flexible metal or spring ring at the margin ❖ The device is introduced up to 3 hours before intercourse and is to be kept for at least 6 hours after the last coital act. ❖ Ill fitting and accidental displacement during intercourse increase the failure rate VAGINAL CONTRACEPTIVES 271 | P a g e ❖ Spermicides are available as vaginal foams, gels, creams, tablets, and suppositories. Usually, they contain surfactants like nonoxynol–9, octoxynol or benzalkonium chloride. The cream or jelly is introduced high in the vagina with the help of the applicator soon before coitus ❖ Vaginal Contraceptive Sponge (Today) It is made of polyurethane impregnated with 1 g of nonoxynol-9 as a spermicide Nonoxynol-9 acts as a surfactant which either immobilizes or kills sperm. It releases spermicide during coitus, absorbs ejaculate and blocks the entrance to the cervical canal. The sponge should not be removed for 6 hours after intercourse. Its failure rate (HWY) is about—parous women: 32–20, nulliparous 16-9. 208. Intrauterine contraceptive devices: classification, indications, Contrindications, technique of insertion, mechanism of action, complications and advantagees. IUCD is an effective, reversible and long-term method of contraception, which does not require replacement for a long period and does not interfere with sexual activity. The device is commonly made of polyethylene which is impregnated with barium sulphate to render it radiopaque so that the presence or absence of the device in the pelvis can be easily detected by radiograph or ultrasound. CLASSIFICATION a) The device is classified as open, when it has got no circumscribed aperture of more than 5 mm so that a loop of intestine or omentum cannot enter and become strangulated if, accidentally, the device perforates through the uterus into the peritoneal cavity. Lippes loop, Cu-T, Cu-7, Multiload and Progestasert are examples of open devices. b) If closed devices, like Grafenberg ring and Birnberg bow, accidentally enter the abdominal cavity, they have the potential of causing strangulation of the gut; and hence are obsolete. c) The device may be nonmedicated as Lippes loop or medicated (bioactive) by incorporating a metal copper, in devices like Cu T-200, Cu T-380A, Multiload-250, Multiload-375 272 | P a g e d) Hormone containing IUDs either releasing progesterone (progestasert) or levonorgestrel (LNGIUS) has also been introduced. INDICATIONS of IUCD • As a contraceptive • Postcoital contraception (emergency contraception) • Following intrauterine procedure such as adhesiolysis and septal resection prevents development of Asherman syndrome (to be used after removing the copper) • Hormonal IUCD (Mirena) in menorrhagia and dysmen- orrhoea, and hormonal replacement therapy in meno- pausal women • In a woman on Tamoxifen for breast cancer, Mirena can be used to counteract endometrial hyperplasia Contraindications for Insertion of IUCD (1) Presence of pelvic infection current or within 3 months; (2) Undiagnosed genital tract bleeding; (3) Suspected pregnancy; (4) Distortion of the shape of the uterine cavity as in fibroid or congenital uterine malformation; (5) Severe dysmenorrhea; (6) Past history of ectopic pregnancy; (7) Within 6 weeks following cesarean section; (8) Sexually transmitted infections (STIs): Current or within 3 months; (9) Trophoblastic disease; (10) Significant immunosuppression. Additionally for Cu-T are: (11) Wilson disease, and (12) Copper allergy. For LNGIUS are: (13) Hepatic tumor or hepatocellular disease (active); (14) Current breast cancer and (15) Severe arterial disease TECHNIQUE OF INSERTION (1) History-taking and examinations (general and pelvic) to exclude any contraindication of insertion. (2) Patient is informed about the various problems, the device is shown to her and consent is obtained. (3) The insertion is done in the outpatient department, taking aseptic precautions without sedation or anesthesia. To reduce cramping pain Ibuprofen [Nonsteroidal anti-inflammatory drug (NSAID)] may be given (200–400 mg) 30 minutes before insertion. (4) Placement of the device inside the inserter—the device is taken out from the sealed packet (1) The patient empties her bladder and is placed in lithotomy position. Uterine size and position are ascertained by pelvic examination. (2) Posterior vaginal speculum is introduced and the vagina and cervix are cleansed by antiseptic 273 | P a g e lotion. (3) The anterior lip of the cervix is grasped by Allis forceps. A sound is passed through the cervical canal to note the position of the uterus and the length of the uterine cavity. The appropriate length of the inserter is adjusted depending on the length of the uterine cavity. (4) The inserter with the device placed inside is then introduced through the cervical canal right up to the fundus and after positioning it by the guard, the inserter is withdrawn keeping the plunger in position. Thus, the device is not pushed out of the tube but held in place by the plunger while the inserter is withdrawn (withdrawal technique in Figure 30.2). (5) The excess of the nylon thread beyond 2–3 cm from the external os is cut. Then the Allis forceps and the posterior vaginal speculum are taken off. No-touch’ insertion technique includes: (i) Loading the IUD in the inserter without opening the sterile package. The loaded inserter is now taken out of the package without touching the distal end. (ii) Not to touch the vaginal wall and the speculum while introducing the loaded IUD inserter through the cervical canal MECHANISM OF ACTION Several mechanisms are responsible for the contraceptive effect of an IUCD. • The presence of a foreign body in the uterine cavity renders the migration of spermatozoa difficult. • A foreign body within the uterus provokes uterine contractility through prostaglandin release and in- creases the tubal peristalsis so that the fertilized egg is propelled down the fallopian tube more rapidly than in normal and it reaches the uterine cavity before the development of chorionic villi and thus is unable to implant. • The device in situ causes leucocytic infiltration in the endometrium. The macrophages engulf the fertilized egg if it enters the endometrial tissue. • Copper T elutes copper which brings about certain enzymatic and metabolic changes in the endometrial tissue which are inimical to the implantation of the fertilized ovum. • Progestogen-carrying device causes alteration in the cervical mucus which prevents penetration of sperm, in addition to its local action. It also causes endometrial atrophy. It prevents ovulation in about 40%. ADVANTAGES 274 | P a g e • Inexpensive: Cu-T distributed free of cost through government channel • Simplicity in techniques of insertion and most cost effective of all methods • Prolonged contraceptive protection after insertion (5–10 years) and suitable for the rural population of developing countries • Systemic side effects are nil. Suitable for hypertensives, breastfeeding women and epileptics • Reversibility to fertility is prompt after removal DISADVANTAGES • Require motivation • Limitation in its use • Adverse local reactions manifested by menstrual abnormalities, pelvic inflammatory devices (PID), pelvic pain and heavy periods. Side effects are less with third generation of intrauterine devices (IUDs) • Risk of ectopic pregnancy 209. Hormonal contraceptive agents: combined oral pills. Their mechanism of action, benefits, side effects, contraindications. The combined oral steroidal contraceptives is the most effective reversible method of contraception. In the combination pill, the commonly used progestins are either levonorgestrel, or norethisterone, or desogestrel and the estrogens are principally confined to either ethinylestradiol or mestranol (3-methyl ether of ethinyl estradiol). MECHANISM OF ACTION – The combined oral pill suppresses pituitary hormones, FSH and LH peak and through this suppression prevents ovulation. At the same time, progestogen causes atrophic changes in the endometrium and p t-events nidation. Progestogen n also acts on the cervical mucus making it thick and tenacious a impenetrable by sperms. OCP also increases the tubal motility, so the fertilized egg reaches the uterine cavity) before the endometrium is receptive for implantation BENEFITS a) Use of OCP results in regular cycles and average blood loss during menstruation. It is helpful in women with menorrhagia and polymenorrhoea. It also relieves dysmenorrhoea and premenstrual tension. 275 | P a g e b) It prevents anaemia by reducing the menstrual blood loss. c) It lowers the incidence of benign breast conditions such as fibrocystic disease. d) It reduces the incidence of functional ovarian cyst (50%). e) Reduce incidence of malignancies. Both ovarian and endometrial malignancies are less common among regu- lar users of OCP. The incidence of ovarian malignancy is reduced by 40% and uterine malignancy by 50% if taken for 1 year, this protective effect lasts as long as 10 years after stoppage of use of OCPs. The incidence of PID is reduced, though it does not reach the same low level as seen with the barrier method. This protective effect is due to the thick cervical mucus caused by progestogen, preventing the microorganisms entering into the uterine cavity. f) Reduced incidence of ectopic pregnancy is due to suppression of ovulation and reduction in PID. g) It protects against rheumatoid arthritis. h) Reduces the risk of anorectal cancer by 30%-40%. i) It is useful in acne, Polycystic Ovarian Disease (PCOD) and endometriosis. SIDE EFFECTS • Intermenstrual spotting is common in the first 3 months. Amenorrhea lasting more than 6 months requires investigations. • Genital tract candidiasis. Oral pills are associated with monilial (candidial) vaginitis. • No documented association is seen with carcinoma of cervix; however, dysplasia is more frequent. • No adverse effect has been noted on uterine fibroids, and it is oestrogen singly that increases their size. • Breast. The combined pills should not be offered to a woman suffering from cancer of the breast. • Pituitary adenoma was attributed to the use of the pill but its exact role in its development is not clear and doubtful. • Breast milk amount in lactating woman who chooses to use OCPs is reduced. • Liver. Adenomas have been reported and though they are benign rarely a rupture of a hepatoma can be fatal. Because the hormones are 276 | P a g e • • • • • • metabolized in the liver, chronic liver diseases and recent jaundice contraindicate the use of pills. Gall bladder function may be adversely affected. Carbohydrate metabolism. Carbohydrate tolerance may be reduced. Therefore, combined oral pills are contrain- dicated or given cautiously to a diabetic woman. Lipid metabolism. Oestrogen increases the high-density lipoprotein (HDL) and lowers low-density lipoprotein (LDL). Headache, migraine, depression, irritability, increased weight and lethargy can occur due to progestogen. Thromboembolic disorders. Pulmonary embolism and cerebral thrombosis, both venous and arterial, are 7-10 times more frequent in the pill users than in the nonusers in the first year of use. Sickle cell anaemia patients can develop thrombosis and crisis. A woman who wears contact lenses should be warned of oedema and irritation of eyes (thrombosis of optic vessels) it is a relative contraindication. CONTRAINDICATIONS TO THE USE OF OCPS a) Cardiac disease, hypertension, smoker older than 35 b) Diabetes. c) History of thrombosis, myocardial infarction, sickle cell anaemia, severe migraine. d) Chronic liver diseases such as cholestatic jaundice of pregnancy, cirrhosis of liver, adenoma, porphyrias. e) Breast cancer, gall bladder disease. f) Gross obesity. g) Patient on enzyme-inducing drugs such as and antiepileptics except sodium valproate. rifampicin, h) 4-6 weeks prior to a planned surgery. i) Lactating woman. 210. Hormonal contraceptive agents: POP (indications, contrindications, side effects, advantages. 277 | P a g e POP is devoid of any estrogen compound. It contains very low dose of a progestin in any one of the following form— levonorgestrel 75 µg, norethisterone 350 µg, desogestrel 75 µg, lynestrenol 500 µg or norgestrel 30 µg. It has to be taken daily from the first day of the cycle. MECHANISM OF ACTION – It works mainly by making cervical mucus thick and viscous, thereby prevents sperm penetration. Endometrium becomes atrophic, so blastocyst implantation is also hindered. In about 2% of cases ovulation is inhibited and 50 percent women ovulate normally. ADVANTAGES – (1) Side effects attributed to estrogen in the combined pill are totally eliminated (2) No adverse effect on lactation and hence can be suitably prescribed in lactating women and as such it is often called ‘Lactation Pill’ (3) Easy to take as there is no ‘On and Off’ regime (4) It may be prescribed in patient having (medical disorders) hypertension, fibroid, diabetes, epilepsy, smoking, and history of thromboembolism (5) Reduces the risk of PID and endometrial cancer. DISADVANTAGES – (1) There may be acne, mastalgia, headache, breakthrough bleeding, or at times amenorrhea in about 20–30% cases (2) All the side effects, attributed to progestins may be evident (3) Simple cysts of the ovary may be seen, but they do not require any surgery (4) Failure rate is about 0.5–2 per 100 women years of use. Failure is more in young compared to women over 40. Women using drugs that induce liver microsomal enzymes to alter a metabolism (mentioned above) should avoid this method of contraception. CONTRAINDICATIONS – (i) Pregnancy, (ii) unexplained vaginal bleeding, (iii) recent breast cancer, (iv) arterial disease and (v) thromboembolic disease 211. Hormonal contraceptive agents: depot injections (drugs, dosage, route of administration, indications, advantagcs and disadvantages). • Depot Injections of Progesterone. Although not very popular in India depot injections of progesterone (Depot medroxyprogesterone acetate, DMPA; norethisterone enanthate NET-EN) are two commonly used intramuscular injections of progesterone. • In fact, in more than 125 countries these are available in the Family Planning Pro- grams. Ease of administration, repeating action at 2-3 monthly intervals and high efficacy have made this mode of administration of contraceptives very popular. 278 | P a g e • To overcome the inconvenience of daily compliance, depot injections of progestogens have been developed. • DMPA is given in a microcrystalline aqueous suspension and NET-EN in a castor oil solution, both by deep intramuscular injec- tion (subcutaneous preparation of DMPA is also available in 104 mg). • Menstrual irregularity though common 18 accepted by puerperal woman as physiological. The injection should be started within a month of delivery in a non- lactating woman and during the third month in a lactating woman because ovulation is delayed up to at least 10 weeks in lactating mothers. Pregnancy rate is 0.4 per 100 woman- years for DMPA and 0.6 per 100 woman-years for NET-EN. • The injection should be administered within 7 days of menstruation with a grace period of 2 weeks for DMPA and 1 week for NET-EN for a repeat injection. Action lasts 12-14 weeks of the first injection for DMPA and 8-9 weeks for NET-EN. Advantages • Injections are easy to administer and there is no worry over 'missing pill'. They are long-acting and reversible. • The compliance is good and the woman remains under regular medical supervision. • The side effects on lipid and carbohydrate metabolism are avoided. DMPA is least androgenic. • It is suited to lactating women. • The incidence of PID, ectopic pregnancy and functional ovarian cysts is low, so also endometrial cancer. • Avoids oestrogenic side effects. • Can be given to a woman with sickle cell anaemia. • Return of fertility is slightly delayed in DMPA group com- pared to NET, but 80% conceive within a year (5 months for DMPA and 3-4 months for NETEN). • Independent of coitus. • They turn out to be more cost-effective for mass usages. 279 | P a g e Disadvantages • Once administered, the side effects, if any, need to be toler- ated until the progestogenic effect of the injection is over. • Menstrual irregularities are common in the form of amenorrhoea or irregular bleeding. Amenorrhoea is reported in 20%-50% users of DMPA at the end of 1 year and are more common with DMPA than NET. Heavy and irregular bleeding is reported in 1%-2% users and is more common with the use of NET. • Do not prevent STD and HIV. • There is a delay in return of fertility but 80% are expected to conceive by end of 1 year. With DMPA, ovula- tion returns in 5 months, and with NET within 3 months of the last injection. • The side effects in the form of weight gain, depression. bloated feeling and mastalgia can occur with injectable progestogen. • Prolonged DMPA use, by virtue of antioestrogenic action, may reduce bone density mass and induce osteopenia. • Contraindicated in breast cancer. • It does increase LDL but does not adversely affect the blood pressure. • It may decrease libido, cause dry vagina. Because of risk of osteopenia, this contraceptive is contraindicated in adolescents, and should not be used for more than 2 years in others. Lately, subcutaneous injections are under development to enable self-administration by the woman. Once-a-Month Injections. Once-a-month intramuscular injections of combined oestrogen and progestogen are available in some countries. These are as follows: • MESIGYNA - (1/2 mL containing NET 50 ing with oestra- diol valerate 5 mg) is given by deep intramuscular injec- tion once a month with 3 days. The low failure rate of 0.4% at the end of 1 year is encouraging. • CYCLOFEM AND LUNELLE - 1/2 mL contains 25 mg DMPA and oestradiol cypionate 5 mg. The failure rate is 0.2% at the end of 1 year. The menstrual irregularity is less than with progestogen-alone injections. • MARVELON - Desogestrel 150 mcg with EE 30 mcg. 280 | P a g e • FEMOVAN - Gestodene 75 mcg with EE, 30 mcg. • ANAFERTIN - Dihydroxyprogesterone acetophenide 75 mg + estradiol enanthate 5 mg. 212. Hormonal contraceptive agents: subdermal implants (drugs, route of administration, contraindications, advantages and disadvantages). Implants are inserted subcutaneously over the anterior abdominal wall using local anesthesia. 17 β-estradiol implants 25 mg, 50 mg or 100 mg are available and can be kept for 6 months. This method is suitable in patients after hysterectomy. Implants maintain physiological E2 to E1 ratio. In the quest to find alternative routes of giving hormonal contraceptives, subdermal implants were discovered. With this method, the progestogens are delivered into general circulation with a slow and sustained release manner with lesser side effects. There are two types of subdermal implants, biodegradable and nondegradable. Once im- planted they release drug slowly over a period of 1-5 years depending upon the implant. • The subdermal implant has no nuisance value of continuous compliance which often adversely affects motivation. Besides, being nonoral it avoids hepatic first-pass effect and thus, reduces systemic side effects. • Norplant I. Norplant I was the first subdermal implant introduced for contraception containing six silastic capsules, it has now been withdrawn from the market and replaced by a single rod implant. • Norplant II (Jadelle) was the second implant system introduced for contraception. It consisted of two rods each containing 70 mg LNG with a daily release of 50 provides contraception for 3-5 years. mcg and The implants suppress ovulation in 50% of the cycles but the main mechanism of action is suppression of endometrium. INSERTION OF IMPLANTS. • The implants are inserted on the first day of the menstrual cycle or within 5 days of abortion, and 3 weeks after the delivery. The woman needs to use barrier contraception or abstain in the first 7 days after insertion. • It takes 5-10 minutes to insert under local anaesthesia. It is best inserted on the medial aspect of the upper arm. The capsules are nonbiodegradable, so 281 | P a g e they need removal at the end of its use or earlier, if side effects are intolerable. • The insertion and removal is made easier using a single rod system called Implanon (40 x 2 mm), which contains 68 mg etonogestrel and does not require an incision to insert. It releases 30 mcg of the hormone daily and is effective for 3 years. There has been no failure to date. It prevents ovulation and is reversible within 1 month of removal. • With the use of Implanon, amenorrhoea is common at the end of 1 year. Acne is reduced and it has no effect on bone density. ADVANTAGES • They are long-acting with sustained effect-compliance is good. • Coital-independent with no 'nuisance of daily oral or frequent injections. • Pregnancy rate varies between 0.2 and 1.3 per 100 woman- years. The failure rate is higher in obese women weighing more than 70 kg. • Systemic side effects are few and the first-pass effect on the liver avoided. • Return of fertility is prompt (within 4-12 weeks). • Can be used by lactating mothers and women older than 40 years. DISADVANTAGES • Breakthrough bleeding, irregular cycles, amenorrhoea occur as seen with other progesterone only contraceptives. • Other side effects of progestogens are seen. • Ectopic pregnancy is reported in 1.3%. • Local infection at the site of insertion may occur. • Requires insertion and removal with nonbiodegradable implants; however, it is a minor surgical procedure. • The implants are expensive. • Infertility may be seen in a few cases after the removal of implant. 282 | P a g e 213. Hormonal contraceptive agents: silastie vaginal rings (mechanism of action, advantages and disadvantages). • Another route which has been tested and found suitable for delivery of hormonal contraceptive is in the form of contra- ceptive vaginal rings. • In an attempt to reduce the side effects of systemic hormonal contraception and the surgical method of insertion of implants, silastic vaginal rings carrying progestogens in different doses have been tried. • The ring is 50-75 mm in diameter and 5-9 mm thick. • The ring currently available contains LNG released at a rate of 20 mcg of hormone daily. • The ring needs a change after 3 months. • Another ring which contains both oestrogen and progesterone is available in the market by the name of NuvaRing containing 11.7 mg etonogestrel and 2.7 mg ethinvloestradiol. • NuvaRing is effective for 1 month. • Advantage of NuvaRing is that incidence of breakthrough bleeding and spotting is less compared to vaginal ring containing only progesterone. Failure rate is 13 per 100 woman-vears. Recently, a lot of research is going on in this field, some progestin-containing rings (3-keto desogestrel 10 mg) have been left in for 5 months at a time. The pregnancy rate with this is reported to be woman-years (WHO, 1985). A ring releasing 30 meg LE with either 120 mcg desogestrel or 650 meg norethister one is under trial. per 100 Other rings are as follows: a) NuvaRing - 120 meg etnogestrel + 15 mcg EE, daily release can be removed during intercourse but not for more than 3 hours at a time b) Nestorone 150 mcg progesterone +15 meg EE, effect tive for 1 year: failure rate is 1.2 per 100 womanseats. ADVANTAGES • Self insertion and removal good compliance. • Other advantages of progestogen contraceptives. 283 | P a g e • Quick reversibilis. DISADVANTAGES • Expensive. Rs 700 per ring per cycle • Local irritation is felt by few vaginitis • Expulsion can occur especially in woman with vaginal prolapse. • Systemic side effects of progestogens have been noted in some women, 214. Hormonal contraccptive agents: skin patches (route of administration, mcchanism of action, side effects, contraindications). • Hormonal Patch (Ortho-Evra). Another route of hormonal contraceptives which has been tested in clinical practice is a skin patch impregnated in hormone. A Ortho Evra Hormonal patch releases 6.00 mg norelgestromin (NGMN) and 0.75 mg EE. A patch lasts 7 days. Three patches are required in each cycle followed by 1-week patch-free inter- val. The patch should be applied within 5 days of menses over the buttocks or abdomen but not over the breasts. • The failure rate is 1-2.8 per 100 woman-years. Compliance of 90% is reported. The breakthrough bleeding (18%). skin reaction (20%) and breast discomfort are the side effects. The other symptoms are headache, nausea and mastalgia. The site of patch should be changed often and is contraindicated in obese women. • Although found popular among women in rich countries, its popularity is low in India. Because of sweating, excessive heat the patch may get displaced decreasing its effectiveness. 215. Postcoital contraception. EMERGENCY CONTRACEPTION (EC) – Hormones, IUD, Antiprogesterone and 284 | P a g e Others Indications of emergency contraception: Unprotected intercourse, condom rupture, missed pill, delay in taking POP for more than 3 hours, sexual assault or rape and first time intercourse, as known to be always unplanned. Risk of pregnancy following a single act of unprotected coitus around the time of ovulation is 8% HORMONES • Morning-after pill: This is not true contraception, but has rightly been called interception, preventing conception in case of accidental unprotected exposure around the time of ovulation. Drugs commonly used are levonorgestrel ethinyl estradiol 2.5 mg. The drug is taken orally twice daily for 5 days, beginning soon after the exposure but not later than 72 hours. • Levonorgestrel (E. Pills) 0.75 mg, two doses given at 12 hours interval, is very successful and without any side effects. The two tablets (1.50 mg) can be taken as a single dose also. The first dose should be taken within 72 hours (Fig. 30.11) may be taken upto 120 hours. • No fetal adverse effects has been observed when there is failure of emergency contraception. However, induced abortion should be offered to the patient, if the method fails. • Other - Levonorgestrel (POP), Copper IUDs (gold standard), Ulipristal acetate (SPRM), Ethinyl estradiol 50 μg + Norgestrel 0.25 mg (COC), Mifepristone RU 486 (PA) MODE OF ACTION: The exact mechanism of action remains unclear. The following are the possibilities: • Ovulation is either prevented or delayed when the drug is taken in the beginning of the cycle. • Fertilization is interfered. • Implantation is prevented (except E. Pills) as the endometrium is rendered unfavorable. • Interferes with the function of corpus luteum or may cause luteolysis. DRAWBACKS: Nausea and vomiting are much more intense with estrogen use. Antiemetic (meclizine) should be prescribed COPPER IUD 285 | P a g e • Introduction of a copper IUD within a maximum period of 5 days can prevent conception following accidental unprotected exposure. This prevents implantation. Failure rate is about 0–1%. It is the gold standard method to be offered to all women for EC. • ADVANTAGE: It can be kept in place for 10 years if desired as a regular method of contraception. Postcoital contraception is only employed as an emergency measure and is not effective if used as a regular method of contraception. Combined hormonal regimen (Yuzpe method) is equally effective. Two tablets of Ovral (0.25 mg levonorgestrel and 50 µg ethinyl estradiol) should be taken as early as possible after coitus (< 72 hours) and two more tablets are to be taken 12 hours later. Oral antiemetic (10 mg metoclopramide) may be taken 1 hour before each dose to reduce the problem of nausea and vomiting. ANTIPROGESTERONE • Antiprogesterone (RU 486-Mifepristone) binds competitively to progesterone receptors and nullifies the effect of endogenous progesterone. • Dose: A single dose of 100 mg is to be taken within 17 days of intercourse. Implantation is prevented due to its anti-progesterone effect. Pregnancy rate is 0–0.6%. • Ulipristal acetate as an EC is superior to levonorgestrel. It is a progesterone receptor modulator. A single dose 30 mg, to be taken orally as soon as possible or within 120 hours of coitus. It acts by suppressing follicular and endometrial growth. It delays ovulation and inhibits implantation. It should not be prescribed in women with severe hepatic dysfunction nor with severe asthma 216. Surgical male and female sterilization. VASECTOMY Vasectomy consists of dividing the vas deferens and disrupting the passage of sperms. It is done through a small incision in the scrotum, under local anesthesia. The sterility is not immediate. The sperms are stored in the reproductive tract for up to 3 months. The couple must therefore abstain from intercourse during this period or use some other methods of contraception such as condoms. Approximately, 20 ejaculates clear the semen of all sperms. Two semen analysis reports must confirm the absence of sperms before the man can be declared 286 | P a g e sterile. No-scalpel technique has been now adopted. One single incision is made with a special forceps and skin stitch is not required. Clips and plugs can be applied over the vas instead of cutting. Vasectomy is cheaper than tubectomy Reversible inhibition of sperm under guidance (RISUG) has been experimented by All India Institute of Medical Sciences and Indian Institute of Technology in India. A polymer gel is injected into the vas. Reversibility is possible by flushing the vas with sodium bicarbonate. This technique is under trial. COMPLICATIONS • Local pain, skin discolouration, bleeding, haematoma formation (1%-2%). • Infection (1%), trauma to the testicular artery causing gangrene, rare. • Antibody formation and autoimmune disease (10%). Failure rate of 0.15 per 100 woman-years at the end of 1 year. • Granuloma formation in 0.1%-3% cases. Spontaneous recanalization. • Formation of spermatocele. • Decreased libido or impotency are mainly psychological in origin and occur in men who were not properly motivated. • Does not prevent HIV, STD. ADVANTAGES • It is an outpatient procedure. • Local anaesthesia is adequate. • It is a minor surgical procedure and the man can resume duty after rest of 1 or 2 days. • Libido not affected. No evidence of prostate cancer. REVERSIBLE INHIBITION OF SPERM UNDER GUIDANCE (RISUG) NEWER TECHNIQUES New nonsclerotic occlusive copolymer of styrene maleic anhydride (SMA) - lowers pH of semen and alters sperm transportation and morphological changes in the sperms. This copolymer is injected in the lumen of vas deferens under ultrasound guidance with the help of a fine hypoder- mic needle. Its action begins immediately and action can be reversed subsequently by injection of another copolymer which neutralizes its action. Chemical sclerosing agents such as 90% ethanol, 3.6% formaldehyde, silver 287 | P a g e nitrate, hydrogen peroxide, acetic acid can eliminate the need of surgery, are effective and easily administered. However, the consequence of intravascular injection and excessive destruction of the vas by even a slight increase of instillation can be disastrous and the procedure is irreversible. Occlusive plugs and intravasal devices are still in the experimental stage. PLUGS A device called 'SHUG' consists of two flexible silicon plugs connected by a nylon thread which lies outside the vas. This thread prevents migration of plugs and allows easy removal through a small incision. Contraindications to vasectomy are as follows: • Local skin infection • Varicocele, hernia • Undescended testis FEMALE STERILIZATION (TUBECTOMY, TUBAL STERILIZATION) Tubal ligation can be done at any time convenient to the patient. Postpartum sterilization is done within the first week of delivery when the patient is already hospitalized. Interval sterilization is done when the woman is not pregnant or any time after 6 weeks of delivery. Tubec- tomy can also be combined with caesarean section. INDICATIONS Apart from multiparity and the need of permanent method of family planning, sterilization may be advisable in women with medical diseases. Indications are as follows: • Multiparity • Three caesarean deliveries • Medical diseases making a subsequent pregnancy high risk. • Psychiatric problems • Breast cancer • Eugenic - repeat fetal malformations, haemophilia, Rh incompatibility, Wilson disease. Tay-Sachs disease and Marfan syndrome. The interval surgery should preferably be done soon after menses to avoid the potential risk of pregnancy in the postovulatory period. 288 | P a g e CONTRAINDICATIONS • Woman younger than 25 years (as directed by the Government of India). • Parity less than two children (as per the Government rule). • Local infection. METHODS OF STERILIZATION 1. Laparotomy - sterilization is performed during caesarean section and during gynecological surgery. • Pomeroy method • Madlener method • Irving method • Aldridge method • Cornual resection • Uchida method • Fimbriectomy 2. Mini-laparotomy - The operation is performed through a small incision less than 2.5 cm in length. Because of its simplicity and ease of doing operation this procedure is advocated for routine sterilization especially in a smaller set up. • Pomeroy • Madlener • Aldridge • Uchida • Fimbriectomy 3. Vaginal route – Vaginal tubal ligation is not popular because of higher morbidity and because of relatively more difficulty in performing the procedure. The pouch of Douglas is opened after placing patient in a lithotomy position, the fallopian tube is hooked out with finger or Babcock and tubectomy performed. It is associated with risk of pelvic infection, higher failure rate and it is more difficult to perform. It is mainly combined with the Manchester repair operation for prolapse of uterus. 4. Laparoscopy – Silastic ring, bipolar cautery, Filshie – This technique has become the most commonly used technique of tubal sterilization. Laparoscopic sterilization is carried out under local or general anesthesia. A small sub umbilical incision is made and pneumoperitoneum created by 289 | P a g e inserting a Veress needle and introducing CO2. CO2 is safer than air and nitrous oxide which can cause air embolism and accidental ex- plosion, respectively. With the patient in the head low position, the trocar and cannula are inserted through the incision and an operating laparoscope introduced after removing the trocar Each fallopian tube is picked up near the isthmic end (2-3 cm away) and it clipped/banded (silastic bands) (Filshie, Hulka band, silastic ring) or cauterization of a segment of the tube done with a bipolar cautery. The gas is allowed to escape at the end of the procedure and the instruments are removed. A subcuticular skin stitch completes the operation. The failure rate with this technique is 0.6 per 100 woman-years. 5. Hysteroscopy – Chemical agents, Essure clip. – In this technique during hysteroscopy either a chemical agent or some plug is introduced in the cornual of the fallopian tube. The technique of using sclerosing agents and quinacrine has been abandoned because of high failure rate, and other complications such as uterine perforation, burn injury and infection. 217. Contraception for adolescents. In India, many girls get married at an early age and become mothers. They need counselling regarding spacing and delaying the birth of the next child. Unmarried adolescents are exposed to the risk of unwanted pregnancy and unsafe abortion, as well as the possibility of acquiring AIDS and sexually transmitted infections. Family planning and contraception become impor tant health care issues amongst adolescents. Although sex education will provide benefit, many will require contraceptive guidance and provision of a suitable contraception. BARRIER METHOD • It is the best method in young girls. Apart from providing contraceptive method, it can prevent transmission of infections from one partner to the other. • If the man refuses to use condoms, a married woman can use Today sponge with spermicidal cream. A recently married woman may find barrier method cumbersome in the initial stages. 290 | P a g e • The adolescent should receive informed knowledge on 'unsafe period' when ovulation occurs, and be provided with emergency contraception such as LNG, two tablets. This is because periodic abstinence is difficult amongst the young couples. IUCD • While IUCD may not be a suitable contraceptive device in the unmarried and recently married nulliparous women, it is a long-term coitalindependent method suited to young parous women, provided no contraindi- cation exists for its use. It is one of the best methods for spacing childbirth. Progesterone copper device is recommended if the woman has heavy periods with dysmenorrhoea. HORMONAL CONTRACEPTIVES • COC pills can be safely prescribed to adolescents. One must remember the possibility of breast cancer at a later date if the young nulliparous woman younger than 24 years of age takes COC for more than 4 years. • POPs are not preferred over COC, because of the irregu- lar bleeding, amenorrhoea, a higher failure rate and osteo- penia. • Three-monthly injections or implants, skin patches and vaginal rings may be acceptable to young married adolescents, and side effects tolerated. Occasional failure may be backed up with MTP facilities. • Sterilization should not be offered to young couples. The Government of India has passed a law that the surgical procedure should not be performed in a woman younger than 25 years with two or less children and the child less than 2 years old. youngest • MTP and emergency contraception should form the backup procedures in these girls. 218. Lactational amenorrhoea. Regular breastfeeding with at least one feed at night is shown to prevent pregnancy for initial 6 months after delivery, with a failure rate of only 0.5%-1.5%. 291 | P a g e This occurs due to prolactin preventing LH surge and ovulation. There- after, the protective effect wears off. Apart from the beneficial effects of lactation on the newborn, it is advocated as the natural method of family planning in the first 6 months after childbirth. Beyond 6 months of breastfeeding, prolactin level falls and ovulation can occur. It is the frequency rather than the duration of feed that decides an ovulation in a nursing mother. Prolonged and sustained breastfeeding offers a natural protection of pregnancy. This is more effective in women who are amenorrheic than those who are menstruating. The risk of pregnancy to a woman who is fully breastfeeding and amenorrheic is less than 2% in the first 6 months. Otherwise, the failure rate is high (1–10%). Thus during breastfeeding, additional contraceptive support should be given by condom, IUCD or injectable steroids where available to provide complete contraception. When the women is full breastfeeding, a contraceptive method should be used in the 3rd postpartum month and with partial or no breastfeeding, she should use it in the 3rd postpartum week. Fertility awareness based methods are: (1) Natural contraception (rhythm method, coitus interruptus, and LAM) (2) Barrier method (condoms, diaphragm, and spermicides) 219. Contraception for women over the age of 35 years. CONTRACEPTION FOR WOMEN OLDER THAN 35 YEARS Women older than 35 years constitute 20% of the contra- ceptive users, and selection of the proper contraception is an essential component of family planning counselling. A woman after the age of 35 years may become obese, hypertensive and diabetic. She is likely to suffer AUB. The choice depends upon the suitability, contraindication and side effects. STERILIZATION • When considering a permanent method of sterilization, one should weigh the risk of surgical procedure against the number of years a woman needs contraceptive protection. In a woman nearer the menopause with a fewer years of fertility, surgical procedure may not be a wise proposition, and temporary methods will be cost-effective as well as safe, with emergency contraception and MTP as a back-up method. 292 | P a g e LOW-DOSE COC PILLS • They are safe, if the woman is thin, nonsmoker without any medical disease up to the age of 15 years. • Although POPs may be safer than COC, its adverse effect on bone density and occurrence of osteoporosis must be borne in mind if given over a prolonged period. Besides, they cause irregular bleeding, and the risk of breast cancer increases. • IUCD may be suitable and effective. If the woman suffers from menorrhagia, Mirena may be inserted and is effective for 5 years. • Desogestrel and gestodene cause thromboembolism and are contraindicated in elderly women. 220. Contraception for woman with medical disease. • The risk of pregnancy should be weighed against the risk of any contraception in a woman with medical disorder. While prescribing a family planning method, due consideration and counselling related to side effects is necessary. • If the risk is negligible, sterilization provides the perma- nent method to prevent a pregnancy. Vasectomy would be ideal, with no risk to the woman. • IUCD is carefully considered in cardiac and diabetic women, because of the possibility of pelvic infection. • COC is contraindicated in a hypertensive, cardiac and diabetic women, as well as a woman with breast cancer, liver disease and previous thromboembolism. An epileptic woman and a woman on antitubercular drugs such as rifa- mycin may face a higher failure rate due to interaction with rifamycin and antiepileptic drugs except sodium val- proate. • Similarly POP is contraindicated in liver diseases, vascular disorders and breast cancer. It is safe in sickle cell anaemia. • Emergency contraception (LNT tablets) is safe in a woman with medical disorders. • Contraception for a Woman with Psychiatric Disorder. 293 | P a g e • If a woman is considered unfit to bear children, and permanent method considered, a written opinion regarding psychiatric problem should be obtained. The written consent should be obtained from the husband or guardian. as the psychiatric patient may not be mentally aware of the nature of sterilization. • Emergency contraception is no bar to a woman with a medical disorder, as only two tablets are given in 24 hours. 221. Medical termination of pregnancy in India and in Russia. The MTP Act permits the wilful termination of pregnancy before the age of fetal viability (20 weeks' gestation) for well-defined indications. It has to be performed by recognized medical practitioners in a recognized place approved by the competent authority under the Act. INCIDENCE It has been estimated that the total number of abortions performed globally is approximately 46 million annually; of these, 26 million take place in countries where abortions are legalized. In India, 6.7 million MTPs take place annu- ally. However, exact incidence remains unknown. In women undergoing MTP, 40% pregnancies are unplanned and 25% are unwanted. Despite the law, 40%-50% of abortions are unsafe terminations of pregnancy done by unqualified persons under unhygienic conditions. GROUNDS FOR PERFORMING MTP The MTP Act has permitted termination of pregnancy for following indications: 222. Grounds for perfornming MTP. MEDICAL GROUNDS When the continuation of pregnancy is likely to (i) endan- ger the life of the pregnant women or (ii) cause grievous injury to her physical and/or mental health, as in cases of severe hypertension, cardiac disease, diabetes, psychiatric illnesses, genital and breast cancer. 294 | P a g e EUGENIC GROUNDS When ultrasound shows a malformed embryo or fetus or there is a substantial risk of the child being born with serious physical or mental abnormalities. For example, hereditary disorders, congenital malformation in previous offspring with a high risk of recurrence in subsequent child- birth/Rh-isoimmunization, teratogenic drugs and maternal rubella posing risk of anomalies in the fetus. Chorion villus biopsy, cordocentesis and sonographic evaluation of the fetus have contributed significantly in identifying the fetuses at risk. HUMANITARIAN GROUNDS In cases when the pregnancy is caused by rape or incest. SOCIAL GROUNDS When: (i) in the actual or reasonably foreseeable future, her [environment (social or economic) might lead to risk of injury to her mental or physical health. (ii) pregnancy resulting from failure of contraceptive device or method. The written consent of the patient on a specially prescribed form is necessary before undertaking the procedure. The written consent of the legal guardian must be obtained in case the woman is younger than 18 years or she is mentally ill, even if she is older than 18 years. 223. The persons who can perform the MTP and the place for performing 222 MTP. WHO CAN PERFORM MTP? Only doctors who have been registered and authorized by the District Health Authorities for the purpose of carrying out MTP can carry out MTP. Generally for carrying out the first-trimester MTP, opinion and signature of one doctor is sufficient. However, for the termination of pregnancy between 12 and 20 weeks, opinion of two certified doctors is must. THE PLACE FOR PERFORMING MTP The Act stipulates that MTP can be performed only at: (i) a hospital established and maintained by the government, (ii) a place recognized and approved by the government, under this Act. • Abortion services are provided under this Act at these centres under strict confidentiality. 295 | P a g e • The identity of the person is treated as a statutory personal matter. • Ultrasonic scanning plays an important role in confirm- ing uterine pregnancy, estimating gestational age, detect- ing malformed embryo and sometimes in performing MTP under ultrasonic guidance. 224. Indications of the MTP act. Methods of MTP. Indications of MTP are as follows: • Maternal medical disorders • Fetal conditions • Rape, incest • Failure of contraceptives • Social grounds METHODS OF MTP There are different methods adopted for termination of the first- and secondtrimester pregnancies. Methods of the first-trimester MTP • Menstrual regulation • Dilatation and suction evacuation • Cervical softening before dilatation and suction evacuation • Medical methods Methods of the second-trimester MTP • Prostaglandins given vaginally, intraamniotic, extra amniotic or intramuscular • Surgical evacuation • Extraovular instillation of drugs such as ethacridine lactate • Extrauterine methods The above methods are used singly or in combination. The oxytocic drugs stimulate myometrial activity and shorten the induction-abortion interval in the second trimester. Similarly, the use of prostaglandins (gel, supposi- tory) a few hours before the procedure helps to attain a gradual softening and atraumatic dilatation of the cervix, facilitating further dilatation and evacuation procedures. 296 | P a g e 225. First trimester MTP: surgical methods, medical methods ⎯ 6-8 weeks pregnancy – Medical abortion, menstrual regulation ⎯ 8-12 weeks pregnancy – Suction evacuation, medical methods ⎯ 12-14 weeks pregnancy – Extra amniotic drugs, intramuscular prostaglandins, vaginal misoprostol SURGICAL METHODS Menstrual Regulation Menstrual regulation consists of aspiration of the contents of the uterine cavity by means of a disposable plastic cannula (Karman's cannula). It has an attached plastic 50 mL syringe capable of creating a vacuum of 65 cm Hg. It has a simple thumb-operated pressure control valve and a piston-locking handle. It is independent of electricity, is por table and washable. It is effective when carried out on preg nancy within 12 days of the last menstrual period (LMP). A paracervical local anaesthetic block or preoperative sedative alone usually suffices but sometimes in an apprehensive pa tient, general anaesthesia may be necessary. The occasional complications encountered include failure to evacuate leading to continuation of pregnancy incomplete evacuation, haemorrhage, cervical laceration, perforation, infection and anaesthetic complications. If pregnancy was not confirmed by ultrasound, an ectopic pregnancy may be missed. A failure to evacuate is due to following reasons: 1. Too early a pregnancy. 2. Ectopic pregnancy. 3. Uterus bicornuate, aspiration being carried out in a non- pregnant horn. Rh anti-D globulin 50 mcg im, should be given to an Rh-negative nonimmunized woman with pregnancy less than 12 weeks. Medical Abortion Of late termination of early pregnancy (less than 19-63-days) is being carried out with the use of mifepristone (RU (86) and misoprostol. This method avoids need for a surgical method such as menstrual regulation. In India termination of pregnancy up to 49 days has been permitted for the use of a medical method. In a 297 | P a g e confirmed pregnancy the woman is initially given a tablet of mifepristone contain ing 200 mg of drug, followed by vaginal administration of 800 mcg of misoprostol. In most cases, abortion is successful within few hours after administration of misoprostol. Most women experience continuation of bleeding for a period of 714 days. A repeat ultrasound after 14 days is carried out to check for any retained products or possible continuation of pregnancy. Some patients may require suction evacuation for heavy bleeding after medical abortion. Prophylactic antibiotics are given for a period of 48 hours to 5 days. TERMINATION OF PREGNANCY BETWEEN 8 AND 12 WEEKS VACUUM EVACUATION (SUCTION EVACUATION) Vacuum evacuation is the most efficient method of terminating pregnancy up to 12 weeks of gestation. It has gained rapid acceptance worldwide. The operation can be generally undertaken under local anaesthetic, paracervical block, coupled with some sedation if necessary. Apprehensive patients may need general anaesthesia. The procedure involves examination of the patient in the operation theatre observing full aseptic precautions. The gestation size and the position of the uterus are carefully assessed. After administering a paracervical block, the cervix is held with an Allis vulsellum forceps and dilated by means of Hegar's or some other metal dilators until adequate dilation is achieved te permit in reduction of the suction cannula of the appropriate size (diameter corresponding to the weeks of gestation) into the uterine cavity (Fig. 20.2). When the procedure is completed, a grating sensation is felt all around the uterine cavity, no further tissue is aspirated and the internal os begins se gr the Karman cannula which may also reveal a blood-stained froth. Vacuum aspiration as a method of MTP has a very low failure rate (<15%). Complications such as incomplete evacuation, infection, uterine perforation and excessive bleeding occur in less than 2% of cases. The mortality is less than 2 per 100,000 procedures, Nonimmunized Rh-negative mothers must receive 100 mcg of anti-D immunoglob after undergoing MTT Failure to end pregnancy is due very early pregnancy, unrecognized ectopic pregnancy pregnancy in a rudimentary hom. Preoperative ultrasound is useful in preventing these complications. MEDICAL METHODS Prostaglandins and RU 486 have been extensively used as medical methods of 298 | P a g e MTP in early pregnancy. Acting singl they are not as effective as when used in combination. The medical method avoids hospitalization ne the prolonged observation, occasional need of surgical temination (fail ure) and the cost of the drugs are some of the disadvantages. Prostaglandins Prostaglandin Injections (Prostin, Carboprost-prostaglandin Fod 250 mcg given im, every 3 hours up to a maximum of 10 doses has been found to be effective in initiating the process of abortion. It has not been popular in the first trimester because of an unacceptably high incidence of incomplete abortion (20% ) requiring surgical intervention to complete the procedure, and the high rate of smpleasant side effects such as nausea, vomiting, diarrhoea, cramping abdominal pain, brunchospasm and mild fever at times Mifepristone (Mifeges! - RU486) First invented in France, in 1980, RU 186 stands for Roussel Urlaf 186 (boratory number It is a synthetic steroid, a derivative of 19-nortestosterone. with antiprogestogenic effect. It also has antiglucocorticoid and weak antiandrogenic action. By competing with progester- one receptors, it reduces the endometrial glandular activity accelerais degenerative changes and increases stromal action, thereby causing sloughing of endometrium. It thus prevents ut disturbs implantation of the fertilized ovum through luteolysis, It also causes uterine contractions, softens and slightly dilates the cervix. The protocol is as follows: • Witten consent for MTP is required. • Blood group Rh. Hb, urine albumin • Ultrasound is done to confirm uterine pregnancy and duration, and exclude ectopic pregnancy Day 1: 200 mg of mifepristone given as a single dose the woman is observed for half an hour and then allowed to go home. Ann-D globulin given to an Rhnegative woman Day 3: 800 mcg of oral misoprostol (prostaglandin) administered unless abortion has occurred. Sublingual or vaginal misoprostol is also used but a stronger action of a sublingual route can cause uterine rupe in a scarred uterus, Puhe and BP are observed for 2 hours, if all is well patient is allowed to go home. Nowadays, misoprostol (PGE) vaginal tablet of 400 mcg is inserted instead of oral 299 | P a g e tablet. Day 14: Follow-up to confirm abortion has occurred; if not, surgical MTP is done. The bleeding usually starts within few hours of taking mifepristone, and abortion occurs in about a week CONTRAINDICATIONS • IUCD in situ- IUCD should be removed before medical termination to avoid the risk of perforation. • Suspected ectopic pregnancy - ultrasound should be done before termination. • Hypertension, anaemia, glaucoma, cardiovascular disease, smoker, asthmatic. • A woman on anticoagulant (coagulopathy) and glucocortscoid therapy. Allergy, porphyria, seizures (adrenal failure). • Previous uterine scar scar rupture can occur with misoprostol • Fibroid uterus. • Lactating woman - Since the drugs are secreted in the milk, leading to diarrhoea in infants. Lactation may be stopped temporarily. • Gestation period should not exceed 63 days (preferably 49 days). ADVANTAGES • Easily stored in room temperature Shelf life: 3 years • Cheap • Easy administration Not contraindicated in patients with asthma. COMPLICATIONS • Adrenal failure • Headache, malise, skin rash, fever, nausea vomiting, danboe • Failure to abort. 1% • Misoprostol causes Möbius syndrome in the fes (congenital facial palsy, limb defects, bladder extrophy. hydrocephalus). Therefore, termination of pregnancy is strongly recommended if medical termination fails. • It takes longer time for termination compared to Surgical termination and longer follow-up of 2 weeks is necessary. 300 | P a g e • Surgery is required in case of failure or is incomplete. In case the woman starts bleeding profusely emergency surge cal evacuation is required. Therefore, emergency surgical backup is a must for medical termination of pregnancy • The subsequent menstruation may be de Lived by 10-14 days • Sublingual misoprostol is as effective as vaginal pessary, but side effects are more severe than with oral tablets and vaginal pessaries. • If vomiting occurs soon after oral misoprostol, repeat the dose. Vaginal pessary is safe. Alternative protocols used are as follows: • 200 mg of oral mifepristone followed by 800 meg vaginal misoprostol on the third day. • 200 mg mifepristone and 1 mg tablet of prostaglandin E, analogue, gemeprost vaginally – pregnancy failure is reported in 0.2% -2.3% cases. • Methotrexate 50 mg intramuscular or oral followed 5-7 days later by 800 mcg vaginal misoprostol (repeat misoprostol 24 hours later, if required). • Epostane - A progesterone-blocking agent is adminis- tered in doses of 200 mcg every 6 hours for 7 days. Misoprostol alone for termination of pregnancy between 8 and 12 weeks: • For termination of pregnancies between 8 and 12 weeks, misoprostol alone has been used extensively. Several dosages regime have been employed with a variable success rate. In most cases induction-abortion interval may last 24 hours or longer with a risk of incomplete abortion or excessive bleeding. MEDICAL VERSUS SURGICAL METHODS FOR TERMINATION OF EARLY PREGNANCY • While choosing between medical and surgical methods for termination of early pregnancy, there is not much difference in terms of safety and efficacy of two methods. However, surgical method has inherent risk of complications such as perforation of uterus, infection and excessive bleeding during the procedure. 301 | P a g e 226. Late sequels of MTP Late sequelae of MTP include following: • Pelvic Inflammatory Disease (PIB) - chronic pelvic pain. • Infertility caused by tubal infection and blockage. • Incompetent os following trauma to the cervix; this may lead to preterm births and recurrent mid-trimester abortions. • Adherent placenta in the subsequent pregnancy, • Asherman syndrome. • Ectopic pregnancy as a result of PID. • Cervical ectopic pregnancy caused by trauma. • Intrauterine Growth Restriction (IUGR). • Rh-isoimmunization if anti-D has not been administered after the MTP to nonimmunized Rh-negative mothers. • Psychological problems, if MTP was done without proper counselling, and there is a feeling of regret, especially if infertility follows the procedure. 302 | P a g e