lecture-6-anxiety-disorders-panic-attacks-agoraphobia-ocd-panic-disorders
advertisement

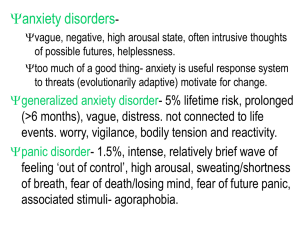
lOMoARcPSD|8913128 Lecture 6 - Anxiety disorders: panic attacks, agoraphobia, OCD, panic disorders Mental Health and Disorder (University of Lincoln) Studocu is not sponsored or endorsed by any college or university Downloaded by Molemela godfrey (molemela9623@gmail.com) lOMoARcPSD|8913128 Lecture 6 – Anxiety Disorders Anxiety is… - Ubiquitous, functional and normal emotional state that everyone experiences Disorders are typically diagnosed whenever the anxiety has a significant impact on a person’s day-to-day functioning It on a continuum and is BOTH a normal emotional AND a diagnosable disorder Anxiety vs Fear - Anxiety is a negative mood state characterised by bodily symptoms of physical tension and apprehension about the future (can be good in small amounts) Fear is an immediate alarm reaction to danger that can protect us e.g. fight vs flight They differ in psychological and physiological processes Panic Attacks - In the DSM-5 Is an “abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which four (or more) of the following symptoms occur: 1. Palpitations, pounding heart 2. Sweating 3. Trembling 4. Sensations of shortness of breath 5. Feelings of choking 6. Nausea, abdominal distress 7. Chills or heat sensations 8. Fear of losing control or going crazy 9. Fear of dying Comorbidity: - Very high rates seen between individuals in co-occurrence of anxiety related disorders All show features of anxiety, fear and panic Downloaded by Molemela godfrey (molemela9623@gmail.com) lOMoARcPSD|8913128 - Share the same vulnerabilities in terms of biological and psychological factors Differ in terms of trigger and may be patterns of the attacks Shared vulnerabilities include: Biological vulnerabilities (heritable contribution to negative affect) – “glass half empty”, irritable and driven Specific psychological vulnerability (e.g. physical sensations are potentially dangerous) – anxiety about health, non-clinical panic Generalized psychological vulnerability (sense that events are uncontrollable/unpredictable) – tendency toward lack of self-confidence, low self esteem and the inability to cope Biological factors - - Genetics: there is a heritability of tendency to panic or be tense, uptight and anxious, however there is no single gene and it is a complex trait. In combination with stress confers vulnerability Neurochemical contribution: reduced GABA activity produces anxiety in animal models. Drugs which increase GABA function are anxiolytic. Noradrenaline in the locus coreruleus may be important in panic disorders. Antidepressants which affect the NA are helpful. OCD may involve a neurotransmitter imbalance of serotonin (5HT), and SSRI antidepressants help many patients. The Behavioural Inhibition System (BIS) - Suggests that the conflict generation enter the behavioural inhibition system, where there are anti-anxiety drugs, which leads to the resolving of conflict e.g increased attention. The Fight vs Flight Response - - Gets the body ready to fight or run away. Once a threat is detected, your body responds automatically. These changes happen for good reasons, but may be experienced as uncomfortable when they happen in safe situations. Dry mouth, sweaty palms, tense muscles, cold hands, vision change, bladder urgency are some examples. Downloaded by Molemela godfrey (molemela9623@gmail.com) lOMoARcPSD|8913128 Psychological factors Anxiety – sense of control or uncontrollability and the role of early childhood/parental style is important Panic – condition and external and internal cues are key factors. Anxiety and OCD related disorders: - Generalised anxiety disorder (GAD) – most prevalent in 30-44 years Panic disorder and agoraphobia – more prevalent in 45-59 years Specific phobia – most prevalent in 45-59 years Social anxiety disorder (social phobia) – prevalent in 30-44 years OCD – prevalent in 30-44 years. Generalised Anxiety Disorder (GAD) Physical symptoms include: over-awareness of autonomic activity, gastro-intestinal, respiratory, cardiovascular, genito-uninary, CNS changes, muscle tensions Psychological symptoms include: fearful anticipation, irritability, lack of concentration, noise sensitivity, restlessness, insomnia, loss of libido DSM-5 Features of GAD include: 1) Excessive anxiety and worry, occurring more days than not for atleast 6 months 2) The individual finds it difficult to control the worry 3) The anxiety and worry are associated with atleast three or more symptoms, but only 1 in children: Restlessness, easily fatigued, difficulty concentrating, irritability, muscle tension, sleep disturbance 4) The anxiety, worry or physical symptoms cause clinically significant distress or impairment in social, occupational or other important functioning areas 5) The disturbance is not due to the direct physiological effects of a substance or better explained by any other mental disorder Panic Disorder - Recurrent experiences of sudden, inexplicable and overwhelming apprehension Sudden onset of attacks, approx. duration 10 minutes Brevity and severity distinguishes it clearly from other anxiety disorders Emotional: feeling of extreme terror, sense of impending doom Physical: sweating, palpitations, dizziness Cognitive: “catastrophic misinterpretation” 60% of those who have panic attacks have nocturnal panic attacks, where EEG shows they occur in the deepest stage of sleep, which links to anxiety around letting go. Isolated sleep paralysis is an Downloaded by Molemela godfrey (molemela9623@gmail.com) lOMoARcPSD|8913128 example, which occurs before waking or going to sleep (links to PTSD) and is more prevalent in African Americans. Two types of panic disorder: 1) Unexpected (uncued) can happen spontaneously 2) Expected (cued) – sometimes you can identify the trigger event Panic disorder genetics: a higher concordance rate for MZ twins than DZ twins, also 30% of close relatives with panic attack disorder also experience later in life. DSM-5 Criteria for Panic Disorder without agoraphobia: A. Both (1) and (2): (1) recurrent unexpected Panic Attacks (2) at least one of the attacks has been followed by 1 month (or more) of one (or more) of the following: (a) persistent concern about having additional attacks (b) worry about the implications of the attack or its consequences (e.g., losing control, having a heart attack, "going crazy") (c) a meaningful change in behavior related to the attacks B. Absence of Agoraphobia. C. The Panic Attacks are not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition (e.g., hyperthyroidism). D. They are not better accounted for by any other mental disorder. Agoraphobia - Is the most common phobia Is the fear of entering unfamiliar situations, e.g anxious when away from home, in crowds and situations where they cannot leave easily Symptoms generally the same as for other anxiety disorders, however other symptoms such as depression, depersonalisation and obsessive thoughts are more common. The “housebound housewife” stereotype, as women are twice as likely to suffer DSM-5 Criteria for agoraphobia: A) Marked fear or anxiety about two or more of the following: public transport, open spaces, enclosed spaces, standing in line or being in a crowd, being outside the house alone B) The individual fears or avoids these situations due to thoughts that escaping might be difficult or help might not be available in the event of developing panic like symptoms C) Agoraphobic situations always provoke fear D) The situations are actively avoided, require a companion and are endured with anxiety E) The fear of anxiety is out of proportion to the actual danger posed by agoraphobic situations F) The fear, anxiety or avoidance is persistent, typically lasting 6+ months G) The fear, anxiety or avoidance causes clinically significant distress or dysfunction in important everyday life Downloaded by Molemela godfrey (molemela9623@gmail.com) lOMoARcPSD|8913128 H) If another medical condition is present, this fear is clearly excessive I) It is not better explained by another mental disorder The cognitive model of panic (Clark and Wells) suggests: An internal or external trigger -> threat is perceived -> leads to anxiety At the point of anxiety, there are body and mental symptoms and catastrophic misinterpretations that act as safety behaviours. Phobias - Have the same core symptoms as generalised panic disorder, but these symptoms only occur in specific situations or in response to specific stimuli Typically a persistent and disproportionate fear for a situation or object that presents little danger to the person Two characteristics of phobic disorders include: 1) The individual avoids circumstances that provoke anxiety, and 2) they experience anticipatory anxiety prior to the situation There are 4 major subtypes of phobias – blood/injection, situational, natural environment and animal types. Before the DSM-IV there was no meaningful classifications of phobias. Most prevalent phobias include: snakes, heights, flying, enclosures, illness. People often have several phobias Females more likely than males 4:1 ratio The DSM-5 Criteria for Phobias: A) Marked fear or anxiety about a specific object or situation lasting 6+ months B) The phobic object almost always prokes immediate fear or anxiety and is avoided C) The fear or anxiety is out of proportion to actual danger posed by the specific object or situation D) The fear, anxiety or avoidance causes clinically significant distress or impairment in social, occupational or other functioning areas E) It is not better explained by other mental disorders Types of phobia - Around 30% of 1st degree relatives have same/similar phobias Distinct from panic disorders – they never have an attack outside the phobic object Social phobia (fear of situations in which one is exposed to the scrutiny of others and may do something to cause embarrassment) Agoraphobia Both social phobia and agoraphobia are associated with high levels of social withdrawal, isolation and depression Obsessive Compulsive and Related Disorders - OCD was previously classified in the DSM-IV as an anxiety disorder DSM-5 has now put it in its own class along with hoarding disorder, body dysmorphia Prevalent of 1.6% Downloaded by Molemela godfrey (molemela9623@gmail.com) lOMoARcPSD|8913128 - - - OCD is characterised by distressing intrusive thoughts and obsessions about the potential harm to self or other and unwanted repetitive safety behaviours (compulsions) that function to neutralise the harm For example, compulsions keep anxiety at bay by “preventing” something bad from happening e.g “I might have left the gas on and the house will blow up” (obsession) “I check the hob several times to ensure it is off (compulsion) Differs from obsessive compulsive personality who actually enjoy the behaviours, OCD leads to distress. Cognitive and motor patterns include: cognitive obsessions, ruminations, cognitive rituals, compulsive motor rituals and compulsive avoidances There are four main compulsion categories: counting, checking, cleaning and avoidance There are no gender differences A genetic incidence of 5-7% in people whose parents had OCD DSM-5 Criteria for OCD: A) Presence of obsessions, compulsions, or both B) The obsessions or compulsions are time-consuming e.g take more than an hour a day, or cause clinically significant distress or impairment to functioning C) The disturbance is not due to the effects of medical, substance or not better explained Obsessions/intrusive thoughts reported by nonclinical samples include - Harming (e.g to jump out of a window, in front of a car, wishing someone would die) Contamination or disease (e.g dirt is always on hands, may have caught a disease) Inappropriate or unacceptable behaviour (e.g idea of swearing, hoping someone doesn’t succeed) Treatments of anxiety disorders: - Drug treatments are no more effective than placebo CBT which aims to change the misperceptions or irrational beliefs, for example: Phobia – dispute beliefs about phobic object, behavioural experiments > exposure Panic disorder – reinterpret bodily symptoms > exposure GAD – reinterpret ambiguous stimuli, likelihood of a negative event > exposure Summary of anxiety disorders: Extremely complex, often comorbidity, biological and psychological vulnerabilities Panic and anxiety combine to create different related disorders, such as GAD, panic disorder and agoraphobia, OCD. Disorders can be differentiated by their triggers being more or less internally or externally driven Downloaded by Molemela godfrey (molemela9623@gmail.com)