Autoimmune Polyendocrine Syndromes: Types, Genetics, and Onset
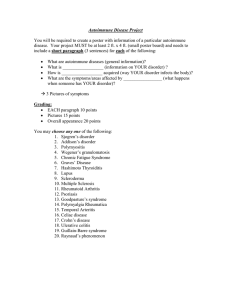
advertisement

Accelerat ing t he world's research. Autoimmune polyendocrine syndromes Biblioteca Medicina Related papers Download a PDF Pack of t he best relat ed papers T ype 1 diabet es and aut oimmune polyglandular syndrome: a clinical review Christ ophe De Block Adrenal Insufficiency Art uro del Mont e Aut oimmune Polyglandular Syndrome T ype II: Epidemiological, Clinical and Immunological Dat a Raouf Hajji, Mnif Fat ma AUTREV-01447; No of Pages 5 Autoimmunity Reviews xxx (2013) xxx–xxx Contents lists available at ScienceDirect Autoimmunity Reviews journal homepage: www.elsevier.com/locate/autrev Review Autoimmune polyendocrine syndromes Maurizio Cutolo ⁎,1 Research Laboratories and Academic Division of Clinical Rheumatology, Department of Internal Medicine, University of Genova Italy, Viale Benedetto XV, 6, 16132 Genova Italy a r t i c l e i n f o Article history: Received 16 July 2013 Accepted 27 July 2013 Available online xxxx Keywords: Autoimmune polyendocrine syndromes (APS) Neuroendocrine immunology (NEI) a b s t r a c t Autoimmune polyendocrine syndromes (APS), also called polyglandular autoimmune syndromes (PGAS), are a heterogeneous group of rare diseases characterized by autoimmune activity against more than one endocrine organs, although non-endocrine organs can be affected. The two major autoimmune polyendocrine syndromes, (type1–type2/APS-1 and APS-2), both have Addison's disease as a prominent component. Further autoimmune polyendocrine syndromes include APS3 and APS4. The major autoimmune polyendocrine syndromes have a strong genetic component with the type 2 syndrome occurring in multiple generations and the type I syndrome in siblings. It is well recognized that more than 20 years may elapse between the onset on one endocrinopathy and the diagnosis of the next, for example, almost 40–50% of subjects with Addison's disease will develop an associated endocrinopathy. The discovery of the polyendocrine autoimmune syndromes offered the possibility to understand autoimmune disorders with particular interest for type 1A diabetes and the neuroendocrine immunology (NEI) is further contributing to understand the links. © 2013 Elsevier B.V. All rights reserved. Contents 1. 2. Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . Autoimmune polyendocrine syndrome type 1 (APS-1) . . . . . . . . . 2.1. Pathogenetic factors . . . . . . . . . . . . . . . . . . . . . 2.2. Onset . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2.3. Diagnosis and treatment . . . . . . . . . . . . . . . . . . . 3. Autoimmune polyendocrine syndrome type 2 (APS-2, Schmidt's syndrome) 3.1. Pathogenetic factors . . . . . . . . . . . . . . . . . . . . . 3.2. Onset . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3.3. Diagnosis and treatment . . . . . . . . . . . . . . . . . . . 3.4. Other polyendocrine syndromes . . . . . . . . . . . . . . . . 4. Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Take-home messages . . . . . . . . . . . . . . . . . . . . . . . . . . . References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1. Introduction The term autoimmune polyendocrine syndromes (APS) comprise several and different conditions in which, however, not all patients necessarily have multiple endocrine disorders, and many have ⁎ Tel.: +39 010 353 7994, +39 335 23 36 21 (mobile); fax: +39 010 353 8885. E-mail address: mcutolo@unige.it. 1 Secretary: +39 010 353 8885. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 0 0 0 0 0 0 0 0 0 0 0 0 0 nonendocrine autoimmune diseases [1]. Interestingly, it is likely that the involved tissues and organs do not share any specific molecule but rather have different molecules that may more or less likely act as targets when the immune system fails to maintain self-tolerance to a variety of molecules. The two major autoimmune polyendocrine syndromes, (autoimmune polyendocrine syndromes type1–type2/APS-1 and APS-2), both have Addison's disease as a prominent component, but exist also APS-3 and APS-4. 1568-9972/$ – see front matter © 2013 Elsevier B.V. All rights reserved. http://dx.doi.org/10.1016/j.autrev.2013.07.006 Please cite this article as: Cutolo M, Autoimmune polyendocrine syndromes, Autoimmun Rev (2013), http://dx.doi.org/10.1016/ j.autrev.2013.07.006 2 M. Cutolo / Autoimmunity Reviews xxx (2013) xxx–xxx The major autoimmune polyendocrine syndromes have a strong genetic component with the type 2 syndrome occurring in multiple generations and the type I syndrome in siblings [2]. In addition, patients with APS-1 and APS-2 develop multiple diseases over time and approximately one out of seven relatives of them have an undiagnosed autoimmune disorder (most often hypothyroidism for the type 2 syndrome) [3]. For practical reasons the major pathological conditions associated with both APS-1 and APS-2 are listed in Table 1. 2. Autoimmune polyendocrine syndrome type 1 (APS-1) 2.1. Pathogenetic factors The APS-1 syndrome is almost always inherited in an autosomal recessive manner linked to mutation of the AIRE gene (AIRE: Autoimmune Regulator gene) on chromosome 21 [4,5]. In autoimmune disorders including Addison's disease, patients without the APS-1 syndrome, do not show AIRE mutations suggesting that the gene alterations are not involved in these more common diseases. In contrast, there is evidence that in rare diseases with abnormal T cell development (i.e. T-B-SCID or Omenn syndrome) there are abnormal thymocyte epithelial interaction and deficient thymic AIRE and lack of expression of AIRE dependent “peripheral” molecules such as insulin [6]. It has been hypothesized that mutations of the AIRE gene (i.e. APS-1 syndrome) cause loss of peripheral antigen expression in the thymus and probably decreased deletion of autoreactive T lymphocytes that target such peripheral antigens [7]. Patients with APS-1 express autoantibodies reacting with different autoantigens, and particular patterns of autoantibodies are associated with the syndrome [8]. The presence of anti-adrenal autoantibodies (i.e. 21-hydroxylase) is strongly associated with the development of Addison's disease. In addition, anti-GAD autoantibodies of patients with the APS I syndrome differ from anti-GAD autoantibodies of typical patients with type 1 diabetes in terms of being able to react with GAD on Western blots and inhibit enzymatic activity. Patients expressing multiple anti-islet autoantibodies are at higher risk for progression to diabetes. Table 1 Major pathological conditions associated with both APS-1 and APS-2. Major pathological conditions associated with autoimmune polyendocrine syndrome type 1 Addison's disease Alopecia Asplenism Autoimmune bronchiolitis Autoimmune thyroiditis Chronic active hepatitis Dental enamel and nail dystrophy Major pathological conditions associated with autoimmune polyendocrine syndrome type 2 Alopecia Myasthenia gravis Autoimmune thyroiditis Idiopathic heart block Ectodermal dysplasia Graves' disease Hypogonadism IgA deficiency Keratitis Malabsorption syndrome Pernicious anemia Pure red cell aplasia Type 1 DM (18%) Vitiligo Graves' disease Hypogonadism Stiff-man syndrome Parkinson’s disease IgA deficiency Serositis Celiac disease, dermatitis herpetiformis Pernicious anemia Idiopathic thrombocytopenia Hypophysitis Type 1 DM (50%) Vitiligo APS-1 patients express additional autoantibodies consistent with widespread loss of tolerance to multiple self antigens [8]. Recently 100% of patients with APS-1 have been found to express autoantibodies reacting with interferon-omega and the great majority express autoantibodies reacting with interferon alpha [9]. 2.2. Onset The onset of the disease is usually in infancy. Chronic mucocutaneous candidiasis is often the first condition detected, later complicated by the development of adrenal insufficiency. Interestingly, the etiology of the mucocutaneous candidiasis in the absence of systemic candidiasis in the APS-1 syndrome has been related to anti-cytokine autoantibodies (anti-IL17A, IL17F and IL22) related to Th17 T cells and depressed production of IL17F and IL22 by peripheral blood mononuclear cells through increased IL17 with decreased IL22 also reported [10,11]. The most frequent pathological conditions related to the APS-1 autoimmune polyendocrine syndrome include Addison's disease, hypoparathyroidism and mucocutaneous candidiasis. This condition is also termed as APECED autoimmune polyendocrinopathy-candidiasisectodermal dystrophy [12,13] (Table 1). Other APS-1 associated diseases include autoimmune hepatitis, primary hypothyroidism, a malabsorption syndrome, vitiligo, pernicious anemia, type 1 diabetes, alopecia, primary hypogonadism, cutaneous abnormalities, pulmonary disease, ovarian failure, pericarditis, cerebellar degeneration, encephalopathy, asplenia, esophageal cancer, polyneuropathy, pure red cell aplasia and others [14,15]. 2.3. Diagnosis and treatment The diagnosis of APS-1 is usually made with two or three of the following conditions: mucocutaneous candidiasis, hypoparathyroidism and/or adrenal insufficiency (or autoantibodies against CYP450c21, 21 hydroxylase) [16]. Since the different components of disease develop over years to decades, surveillance is mandatory for other associated autoimmune disorders. Especially under the age of 30 years surveillance is suggested if more than one of the following conditions is identified: chronic or recurring mucocutaneous candidiasis, hypoparathyroidism, adrenal insufficiency, chronic gastrointestinal disease characterized by obstipation, diarrhea or steatorrhea, vitiligo, alopecia, keratoconjunctivitis or urticaria-like erythema [17]. Consideration for AIRE gene mutational analysis should be entertained (if possible) in the presence of those associations. Usually, sudden hypercalcemia in hypoparathyroid individuals may signal the beginning of adrenal insufficiency [18]. Symptoms of diarrhea, malabsorption with failure to thrive in children and/or obstipation may be identified. These symptoms may be due to the underlying endocrine disease (e.g. diarrhea with the hypocalcemia of hypoparathyroidism) or may be a manifestation of a new disorder. Treatment of course, will in part depend upon the autoimmune disorder identified and aggressive therapy of oral candidiasis is indicated in order to prevent the late complication of epithelial carcinoma [19]. Recently, the presence of cardiac failure in APS-1 has been successfully cured with calcium, calcitriol and hydrocortisone supplementation, since hypocalcemia and hypocortisol state are curable causes of myocardial dysfunction and subsequent congestive cardiac failure [20]. 3. Autoimmune polyendocrine syndrome type 2 (APS-2, Schmidt's syndrome) 3.1. Pathogenetic factors Differently from APS-1, genetic abnormalities underlie disease susceptibility for autoimmune polyendocrine syndrome type 2 (APS-2) and consist primarily of alleles of genes within the major histocompatibility Please cite this article as: Cutolo M, Autoimmune polyendocrine syndromes, Autoimmun Rev (2013), http://dx.doi.org/10.1016/ j.autrev.2013.07.006 M. Cutolo / Autoimmunity Reviews xxx (2013) xxx–xxx complex [21]. The primary association of APS-2, similar to many autoimmune conditions appears to be with class II HLA alleles (immune response genes) and in particular with DQ2 and DQ8. Therefore, APS-2 is has been found strongly associated with human leukocyte (HLA) haplotypes with DR3/DQ2 (DQ2:DQA1*0501, DQB1*0201) and DR4/DQ8 (DQ8:DQA1*0301, DQB1*0302) and with DRB1*0404 [22–24]. In multiplex Addison's disease families, 95% of DR3 haplotypes have HLA-B8 compared to approximately 50% of control U.S. DR3 haplotypes. Several of the diseases of the type 2 syndrome are associated with HLA antigens HLA-DR3 or HLA-DR4 [22,25]. Primary adrenal insufficiency in type 2, but not in type 1 APS, is strongly associated with both HLADR3 and HLA-DR4 [25]. The association of HLA markers with disease can correlate with inheritance of a common HLA-haplotype within families, but haplotypes with DR3 are often introduced into the family by more than one relative. Other HLA-B8 and DR3 associated illnesses include selective IgA deficiency, juvenile dermatomyositis, and dermatitis herpetiformis, alopecia, scleroderma, autoimmune thrombocytopenia purpura, hypophysitis, metaphyseal osteopenia, serositis and premature ovarian failure (16%) [26,27]. Even though signs and symptoms of disease may be absent, patients with multiple disorders should be screened every few years with measurement of anti-islet antibodies, 21-hydroxylase autoantibodies and transglutaminase autoantibodies, a sensitive thyrotropin assay, and measurement of serum B12 levels [28,29]. Several autoantibodies are both disease specific (i.e. antiacetylcholine receptor antibodies in myasthenia gravis and antiTSH receptor antibodies in Graves' disease) and causal [30]. Other autoantibodies such as anti-thyroid autoantibodies including antithyroid peroxidase, formerly termed anti-microsomal, and antithyroglobulin are as frequent among patients and relatives as to be of little predictive value. Similarly, many individuals may show antibodies to parietal cells, H+/K+ adenosine triphosphatase of the stomach and intrinsic factor, but the autoantibodies may not correlate well with abnormal gastric acid secretion or development of pernicious anemia [31–33]. Further autoantibodies associated with the type 2 syndrome include anti-melanocytic, anti-adrenal and anti-gonadal autoantibodies [34,35]. Finally, antibodies to specific receptors are characteristic of given disorders for example anti-acetylcholine receptor antibodies of myasthenia gravis, and oocyte sperm receptor autoantibodies associated with oophoritis. 3.2. Onset It is recognized that more than 20 years may elapse between the onset on one endocrinopathy and the diagnosis of the next, for example, almost 40–50% of subjects with Addison's disease will develop an associated endocrinopathy. However, a distinction must be made for subjects with isolated thyroid disease who have no family history of polyglandular syndrome type 2, since relatively frequent in the general population. As matter of fact, individuals have a relatively low probability of developing additional autoimmune disorders in comparison with individuals with rare autoimmune disorders such as Addison's disease or myasthenia gravis. Interestingly, initiating factors for the type 2 syndrome and its component illnesses are not completely established except for celiac disease (wheat protein gliadin), the insulin autoimmune syndrome (i.e. methimizole), myasthenia gravis, type 1A diabetes (rarely congenital rubella), Graves' disease (rarely anti-CD52 monoclonal treating patients with multiple sclerosis) and hypothyroidism (interferon therapy associated with thyroid autoimmunity and diabetes) [36–39]. 3 3.3. Diagnosis and treatment APS-2 is the most common autoimmune polyendocrine syndrome and includes Addison's disease, Graves' disease (thyrotoxicosis), primary hypothyroidism, primary hypogonadism, hypopituitarism, IgA deficiency, insulin-dependent or type 1A diabetes mellitus (IDDM), Parkinson's disease, myasthenia gravis, celiac disease, vitiligo, serositis, stiff-man syndrome, alopecia, pernicious, and autoimmune thyroiditis [1,21,27]. Generally, individuals with a single autoimmune disease are at increased risk for the development of a second disease compared to the general population and often patient individuals with APS-2 syndrome will develop autoimmunity sequentially over a period of many years. In addition, patients often will not have polyglandular failure at the onset of clinical symptoms of the initial autoimmune disease, conversely, the possible development of sequential autoimmune diseases should be expected after a polyglandular disease. Interestingly, controversy exists regarding the screening tests that should be employed and the frequency of testing performed when expecting an autoimmune diseases. For example, in patients affected by type 1diabetes, the routine screening for thyroid disease with biochemical assays should be performed (i.e. TSH assay) [40]. Again, the screening for celiac disease within the APS-2 patients is controversial, since the disease is expected in the diabetic population and many of these patients are asymptomatic at the time of the diagnosis [41]. Increased concentrations of transglutaminase autoantibodies are associated with a positive celiac biopsy [42]. Data on anti-pituitary autoimmunity have recently identified: IgG4 hypophysitis, anti-Pit1 combined pituitary deficiencies and recognition of predictive pituitary antibody staining pattern [43]. In order to finalize the diagnosis of APS-2, once a second autoimmune disease is identified, a further extensive screening is suggested with the intention to identify the further disease at an early stage. Therefore, the screening for autoantibodies associated with diabetes (i.e. IA-2, insulin and GAD), thyroid disease (i.e. TG and/or TPO), Addison's disease (21-hydroxylase), celiac disease (transglutaminase) and autoimmune hepatitis (cytochrome P450 enzymes) may discover an associated autoimmune disease not yet clinically evident. Treatment of the APS-2 syndrome is obviously related to the specific disease manifestation with a some further suggestions [1,21,27]. 3.4. Other polyendocrine syndromes The third type of autoimmune polyendocrine syndromes (APS type 3) involves the same disorder of endocrine glands as type 2 but usually without any defect of adrenal cortex. If the autoimmune endocrine gland disorder does not fulfill the criteria of APS 1–3, the disease may be categorized as autoimmune polyendocrine syndrome type 4 [44]. Further syndromes are reported in the following Table 2. 4. Conclusions The discovery of the polyendocrine autoimmune syndromes offered the possibility to understand autoimmune disorders with particular interest for type 1A diabetes [52]. As matter of fact the early evidence that type 1A diabetes should be considered as an autoimmune disorder came from its association with spontaneous Addison's disease [53]. On the other side, the first demonstration of cytoplasmic islet cell autoantibodies occurred in patients with polyendocrine autoimmunity [54]. Moreover, the relationships observed between the different polyendocrine autoimmune disorders suggest that as the disease pathogenesis is understood and antigen-specific therapies are developed, the improved knowledge of pathogenesis and improvements in therapy will be applicable to several autoimmune diseases. The science of neuroendocrine immunology (NEI) is approaching systematically from long time the intriguing relationships that characterize the polyendocrine autoimmune syndromes [55–57]. Please cite this article as: Cutolo M, Autoimmune polyendocrine syndromes, Autoimmun Rev (2013), http://dx.doi.org/10.1016/ j.autrev.2013.07.006 4 M. Cutolo / Autoimmunity Reviews xxx (2013) xxx–xxx Table 2 Other polyendocrine syndromes. Other polyendocrine syndromes IPEX (Immune Dysfunction Polyendocrinopathy X-linked) The IPEX syndrome is a very rare disorder that presents in neonates with fatal autoimmunity and has multiple different names reflecting endocrinopathy, allergic manifestations, intestinal destruction and immune dysregulation [45]. Thymic tumor diseases Thymomas and thymic hyperplasia are associated with a series of autoimmune diseases and the most common are myasthenia gravis and red cell aplasia. In addition, Graves' disease, type 1 diabetes, and Addison's disease may also be associated with thymic tumors [46]. POEMS syndrome POEMS (Polyneuropathy, Organomegaly, Endocrinopathy, M-protein, Skin changes) patients usually are characterized by a sensory motor polyneuropathy, diabetes mellitus (50%), primary gonadal failure (70%), and a plasma cell dyscrasia with sclerotic bony lesions [47]. Insulin autoimmune syndrome (Hirata syndrome) The insulin autoimmune syndrome, associated with Graves' disease and methimazole therapy (or other sulfhydryl containing medications) is of particular interest due to a remarkably strong association with a specific HLA haplotype (DR4-positive individuals with DRB1*0406) [48]. Adult Combined Pituitary Hormone Deficiency (CPHD) Very rare disease. The pituitary-specific transcription factor Pit-1/GHF1 regulates the expression of PRL, GH, and TSH beta genes through binding to specific regions of the promoters of these genes. Mutations of the Pit-1 gene have been shown to be responsible for a syndrome of combined pituitary hormone deficiency (CPHD), including complete GH and PRL deficiencies and central hypothyroidism [49]. Kearns–Sayre syndrome From the first description by Kearns and Sayre in 1958, this syndrome, a complex mitochondrial encephalomyopathy, has been diagnosed in several hundred patients [50]. DIDMOAD syndrome (also termed Wolfram syndromes 1 and 2) Wolfram syndrome 1 (WS1) is an autosomal recessive disorder characterized by diabetes insipidus, diabetes mellitus, optic atrophy, and deafness (DI DM OA D syndrome) associated with other variable clinical manifestations. The causative gene for WS1 (WFS1) encoding wolframin maps to chromosome 4p16.1. Recently, another causative gene, CISD2, has been identified in patients with a type of Wolfram syndrome (WS2) resulting in early optic atrophy, diabetes mellitus, deafness, decreased lifespan, but not diabetes insipidus [51]. Take-home messages • Autoimmune polyendocrine syndromes (APS—types 1/2/3/4) include several and different conditions in which, however, not all patients necessarily have multiple endocrine disorders, and many have nonendocrine autoimmune diseases. • The most frequent pathological conditions related to the APS-1 autoimmune polyendocrine syndrome include Addison's disease, hypoparathyroidism and mucocutaneous candidiasis. • APS-2 is the most common autoimmune polyendocrine syndrome and includes Addison's disease, Graves' disease (thyrotoxicosis), primary hypothyroidism, primary hypogonadism, hypopituitarism, IgA deficiency, insulin-dependent or type 1A diabetes mellitus (IDDM), Parkinson's disease, myasthenia gravis, celiac disease, vitiligo, serositis, stiff-man syndrome, alopecia, pernicious, and autoimmune thyroiditis. • The science of neuroendocrine immunology (NEI) is investigating from long time the complex relationships between immune system and polyendocrine syndromes. References [1] Michels AW, Gottlieb PA. Autoimmune polyglandular syndromes. Nat Rev Endocrinol 2010;6:270–7. [2] Barker JM. Clinical review: type 1 diabetes-associated autoimmunity: natural history, genetic associations, and screening. J Clin Endocrinol Metab 2006;91:1210–7. [3] Eisenbarth GS, Wilson PW, Ward F, Buckley C, Lebovita H. The polyglandular failure syndrome: disease inheritance, HLA type, and immune function. Ann Intern Med 1979;91:528–33. [4] Lindmark E, Chen Y, Georgoudaki AM, Dudziak D, Lindh E, Adams WC, et al. AIRE expressing marginal zone dendritic cells balances adaptive immunity and T-follicular helper cell recruitment. J Autoimmun 2013;42:62–70. [5] Aaltonen J, Björses P, Sandkuijl L, Perheentupa J, Peltonen L. An autosomal locus causing autoimmune disease: autoimmune polyglandular disease type I assigned to chromosome 21. Nat Genet 1994;8:83–7. [6] Lindh E, Rosmaraki E, Berg L, Brauner H, Karlsson MC, Peltonen L, et al. AIRE deficiency leads to impaired iNKT cell development. J Autoimmun 2010;34:66–72. [7] Villasenor J, Benoist C, Mathis D. AIRE and APECED: molecular insights into an autoimmune disease. Immunol Rev 2005;204:156–64. [8] Perniola R, Falorni A, Clemente MG, Forini F, Accogli E, Lobreglio G. Organ-specific and non-organ-specific autoantibodies in children and young adults with autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED). Eur J Endocrinol 2000;143:497–503. [9] Meloni A, Furcas M, Cetani F, Marcocci C, Falorni A, Perniola R, et al. Autoantibodies against type I interferons as an additional diagnostic criterion for autoimmune polyendocrine syndrome type I. J Clin Endocrinol Metab 2008;93:4389–97. [10] Puel A, Doffinger R, Natividad A, Chrabieh M, Barcenas-Morales G, Picard C, et al. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J Exp Med 2010;207:291–7. [11] Alimohammadi M, Bjorklund P, Hallgren A, Pontynen N, Szinnai G, Shikama N, et al. Autoimmune polyendocrine syndrome type 1 and NALP5, a parathyroid autoantigen. N Engl J Med 2008;358:1018–28. [12] Kisand K, Lilic D, Casanova JL, Peterson P, Meager A, Willcox N. Mucocutaneous candidiasis and autoimmunity against cytokines in APECED and thymoma patients: clinical and pathogenetic implications. Eur J Immunol 2011;41:1517–27. [13] Kisand K, Peterson P. Autoimmune polyendocrinopathy candidiasis ectodermal dystrophy: known and novel aspects of the syndrome. Ann N Y Acad Sci 2011;1246:77–91. [14] Bialkowska J, Zygmunt A, Lewinski A, Stankiewicz W, Knopik-Dabrowicz A, Szubert W, et al. Hepatitis and the polyglandular autoimmune syndrome, type 1. Arch Med Sci 2011;7:536–9. [15] Oliva-Hemker M, Berkenblit GV, Anhalt GJ, Yardley JH. Pernicious anemia and widespread absence of gastrointestinal endocrine cells in a patient with autoimmune polyglandular syndrome type I and malabsorption. J Clin Endocrinol Metab 2006;91:2833–8. [16] Reato G, Morlin L, Chen S, Furmaniak J, Rees SB, Masiero S, et al. Premature ovarian failure in patients with autoimmune Addison's disease: clinical, genetic, and immunological evaluation. J Clin Endocrinol Metab 2011;96:E1255–61. [17] Husebye ES, Perheentupa J, Rautemaa R, Kämpe O. Clinical manifestations and management of patients with autoimmune polyendocrine syndrome type I. J Intern Med 2009;265:514–29. [18] Perheentupa J. APS-I/APECED: the clinical disease and therapy. In: Eisenbarth GS, editor. Autoimmune Polyendocrine Syndromes. Philadelphia: W.B. Saunders Company; 2002. p. 295–320. [19] Ahonen P, Myllarniemi S, Kahanpaa A, Perheentupa J. Ketoconazole is effective against the chronic mucocutaneous candidosis of autoimmune polyendocrinopathycandidosis-ectodermal dystrophy (APECED). Acta Med Scand 1986;220:333–9. [20] Wani AI, Farooqui KJ, Bashir MI, Mir SA, Lone AA, Masoodi SR. Autoimmune polyglandular syndrome type 1 with reversible dilated cardiomyopathy: complete recovery after correction of hypocalcemia and hypocortisolemia. J Pediatr Endocrinol Metab 2013;26:373–6. [21] Michels AW, Eisenbarth GS. Autoimmune polyendocrine syndrome type 1 (APS-1) as a model for understanding autoimmune polyendocrine syndrome type 2 (APS-2). J Intern Med 2009;265:530–40. [22] Rottembourg D, Deal C, Lambert M, Mallone R, Carel JC, Lacroix A, et al. 21Hydroxylase epitopes are targeted by CD8 T cells in autoimmune Addison's disease. J Autoimmun 2010;35:309–15. [23] Myhre AG, Undlien DE, Lovas K, Uhlving S, Nedrebo BG, Kristian JF, et al. Autoimmune adrenocortical failure in Norway: autoantibodies and HLA class II associations related to clinical features. J Clin Endocrinol Metab 2002;87:618–23. [24] Gombos Z, Hermann R, Kiviniemi M, Nejentsev S, Reimand K, Fadeyev V, et al. Analysis of extended human leukocyte antigen haplotype association with Addison's disease in three populations. Eur J Endocrinol 2007;157:757–61. [25] Maclaren NK, Riley WJ. Inherited susceptibility to autoimmune Addison's disease is linked to human leukocyte antigens-DR3 and/or DR4, except when associated with type 1 autoimmune polyglandular syndrome. J Clin Endocrinol Metab 1986;62:455–9. [26] Reato G, Morlin L, Chen S, Furmaniak J, Smith BR, Masiero S, et al. Premature ovarian failure in patients with autoimmune Addison's disease: clinical, genetic, and immunological evaluation. J Clin Endocrinol Metab 2011;96:E1255–61. [27] Ballarini A, Lee-Kirsch MA. Genetic dissection of autoimmune polyendocrine syndrome type 2: common origin of a spectrum of phenotypes. Ann N Y Acad Sci 2007;1110:159–65. [28] Schilling RF. Who has vitamin B12 deficiency? Proc Assoc Am Physicians 1996;108:68–70. [29] Baker PR, Nanduri P, Gottlieb PA, Yu L, Klingensmith GJ, Eisenbarth GS, et al. Predicting the onset of Addison's disease: ACTH, renin, cortisol, and 21hydroxylase autoantibodies. Clin Endocrinol (Oxf) 2012;76:617–24. [30] Sanders J, Oda Y, Roberts S, Kiddie A, Richards T, Bolton J, et al. The interaction of TSH receptor autoantibodies with 125I-labelled TSH receptor. J Clin Endocrinol Metab 1999;84:3797–802. [31] Wenzlau JM, Gardner TJ, Frisch LM, Davidson HW, Hutton JC. Development of a novel autoantibody assay for autoimmune gastritis in type 1 diabetic individuals. Diabetes Metab Res 2011;27:887–90. Please cite this article as: Cutolo M, Autoimmune polyendocrine syndromes, Autoimmun Rev (2013), http://dx.doi.org/10.1016/ j.autrev.2013.07.006 M. Cutolo / Autoimmunity Reviews xxx (2013) xxx–xxx [32] Karlsson FA, Burman P, Loof L, Mardh S. Major parietal cell antigen in autoimmune gastritis and pernicious anemia is the acid producing HK-ATPase of the stomach. J Clin Invest 1988;81:475–9. [33] De Block CE, De Leeuw IH, Van Gaal LF. High prevalence of manifestations of gastric autoimmunity in parietal cell antibody-positive type 1 (insulin-dependent) diabetic patients. The Belgian Diabetes Registry. J Clin Endocrinol Metab 1999;84:4062–7. [34] Myhre AG, Halonen M, Eskelin P, Ekwall O, Hedstrand H, Rorsman F, et al. Autoimmune polyendocrine syndrome type 1 (APS I) in Norway. Clin Endocrinol (Oxf) 2001;54:211–7. [35] Soderbergh A, Winqvist O, Norheim I, Rorsman F, Husebye ES, Dolva O, et al. Adrenal autoantibodies and organ-specific autoimmunity in patients with Addison's disease. Clin Endocrinol (Oxf) 1996;45:453–60. [36] Norris JM, Barriga K, Hoffenberg EJ, Taki I, Miao D, Haas JE, et al. Risk of celiac disease autoimmunity and timing of gluten introduction in the diet of infants at increased risk of disease. JAMA 2005;18(293):2343–51. [37] Coles AJ, Wing M, Smith S, Coraddu F, Greer S, Taylor C, et al. Pulsed monoclonal antibody treatment and autoimmune thyroid disease in multiple sclerosis. Lancet 1999;354:1691–5. [38] Schreuder TC, Gelderblom HC, Weegink CJ, Hamann D, Reesink HW, Devries JH, et al. High incidence of type 1 diabetes mellitus during or shortly after treatment with pegylated interferon alpha for chronic hepatitis C virus infection. Liver Int 2008;28:39–46. [39] Badra G, Waked I, Selmi C, Saleh SM, El Shaarawy A, Lotfy M. Serum islet cell autoantibodies during interferon alpha treatment in patients with HCV-genotype 4 chronic hepatitis. Clin Dev Immunol 2006;13:11–5. [40] Reghina AD, Albu A, Petre N, Mihu M, Florea S, Fica S. Thyroid autoimmunity in 72 children with type 1 diabetes mellitus: relationship with pancreatic autoimmunity and child growth. J Pediatr Endocrinol Metab 2012;25:723–6. [41] Bakker SF, Tushuizen ME, Stokvis-Brantsma WH, Aanstoot HJ, Winterdijk P, van Setten PA, et al. Frequent delay of coeliac disease diagnosis in symptomatic patients with type 1 diabetes mellitus: clinical and genetic characteristics. Eur J Intern Med 2013;24:456–60. [42] Liu E, Li M, Bao F, Miao D, Rewers MJ, Eisenbarth GS, et al. Need for quantitative assessment of transglutaminase autoantibodies for celiac disease in screeningidentified children. J Pediatr 2005;146:494–9. 5 [43] Lupi I, Manetti L, Raffaelli V, Lombardi M, Cosottini M, Iannelli A, et al. Diagnosis and treatment of autoimmune hypophysitis: a short review. J Endocrinol Invest 2011;34: e245–52. [44] Schneller C, Finkel L, Wise M, Hageman JR, Littlejohn E. Autoimmune polyendocrine syndrome: a case-based review. Pediatr Ann 2013;42:203–8. [45] Kobayashi I, Kubota M, Yamada M, Tanaka H, Itoh S, Sasahara Y, et al. Autoantibodies to villin occur frequently in IPEX, a severe immune dysregulation, syndrome caused by mutation of FOXP3. Clin Immunol 2011;141:83–9. [46] Sherer Y, Bardayan Y, Shoenfeld Y. Thymoma, thymic hyperplasia, thymectomy and autoimmune diseases (review). Int J Oncol 1997;10:939–43. [47] Li J, Zhou DB. New advances in the diagnosis and treatment of POEMS syndrome. Br J Haematol 2013;161:303–15. [48] Paiva ES, Pereira AE, Lombardi MT, Nishida SK, Tachibana TT, Ferrer C, et al. Insulin autoimmune syndrome (Hirata disease) as differential diagnosis in patients with hyperinsulinemic hypoglycemia. Pancreas 2006;32:431–2. [49] Pellegrini-Bouiller I, Bélicar P, Barlier A, Gunz G, Charvet JP, Jaquet P, et al. A new mutation of the gene encoding the transcription factor Pit-1 is responsible for combined pituitary hormone deficiency. J Clin Endocrinol Metab 1996;81:2790–6. [50] Maceluch JA, Niedziela M. The clinical diagnosis and molecular genetics of Kearns– Sayre syndrome: a complex mitochondrial encephalomyopathy. Pediatr Endocrinol Rev 2006;4:117–37. [51] Rigoli L, Di Bella C. Wolfram syndrome 1 and Wolfram syndrome 2. Curr Opin Pediatr 2012;24:512–7. [52] Husebye ES, Anderson MS. Autoimmune polyendocrine syndromes: clues to type 1 diabetes pathogenesis. Immunity 2010;32:479–87. [53] Kenna AP. Addison's disease and diabetes mellitus. Arch Dis Child 1967;42:319–21. [54] Bottazzo GF, Florin-Christensen A, Doniach D. Islet-cell antibodies in diabetes mellitus with autoimmune polyendocrine deficiencies. Lancet 1974;2:1279–83. [55] Cutolo M, Sulli A, Straub RH. Estrogen metabolism and autoimmunity. Autoimmun Rev 2012;11:A460–4. [56] Cutolo M, Otsa K, Uprus M, Paolino S, Seriolo B. Vitamin D in rheumatoid arthritis. Autoimmun Rev 2007;7:59–64. [57] Straub RH, Bijlsma JW, Masi A, Cutolo M. Role of neuroendocrine and neuroimmune mechanisms in chronic inflammatory diseases—the 10-year update. Semin Arthritis Rheum. 2013 May 31. doi:pii:S0049-0172(13)000644.10.1016/j.semarthrit.2013.04.008 [Epub ahead of print]. Please cite this article as: Cutolo M, Autoimmune polyendocrine syndromes, Autoimmun Rev (2013), http://dx.doi.org/10.1016/ j.autrev.2013.07.006