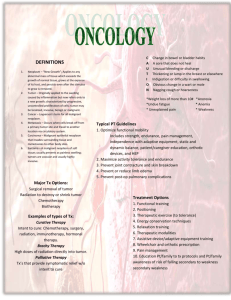
Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN MEDICAL AND SURGICAL NURSING Oncology Nursing Lecturer: Mark Fredderick R. Abejo RN, MAN Oncology (from the Ancient Greek onkos - meaning bulk, mass, or tumor, and the suffix -logy - meaning "study of") is a branch of medicine that deals with tumors (cancer). A medical professional who practices oncology is an oncologist.Oncology is concerned with: The diagnosis of any cancer in a person Therapy (e.g., surgery, chemotherapy, radiotherapy and other modalities) Follow-up of cancer patients after successful treatment Palliative care of patients with terminal malignancies Ethical questions surrounding cancer care Screening efforts: o of populations, or o of the relatives of patients (in types of cancer that are thought to have a hereditary basis, such as breast cancer. A. Characteristics of Normal Cells The Biology of Normal Cells 1) Have limited cell division 2) Undergo Apoptosis 3) Show specific morphology 4) Perform specific differentiated functions 5) Adhere tightly together 6) Non migratory 7) Grow in orderly and well regulated manner 8) Are euploid * Normal cell growth (cell cycle) consists of 5 intervals or phases * Differentiation – refers to the process whereby cells develop specific structures and functions in order to specialize in certain tasks * Apoptosis – cell suicide, normal event. * Cellular adaptation a. Hypertrophy – refers to an increase in size of normal cells b. Atrophy – refers to the shrinkage of cell size c. Hyperplasia – refers to an increase in the number of normal cells d. Metaplasia – refers to a conversion from the normal patters of differentiation of one type of cell into another type of cell not normal for that tissue. Replacement of other mature cell. e. Dysplasia – refers to an alteration in the shape, size, appearance and distribution of cells (reversible) f. Anaplasia – refers to disorganized, irregular cells that have nor structure and have loss of differentiation; the result is always malignant (undifferentiated cell) Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN B. Evolution of Cancer Cells 1. Cancer – refers to a disease whereby cells mutate into abnormal cells that proliferate abnormally Neoplasia – refers to an abnormal cell growth or tumor - a mass of new tissue functioning independently and serving no useful purpose 2. Invasion – occurs when cancer cells infiltrate adjacent tissue surrounding the neoplasm 3. Metastasis – occurs when malignant cells travel through the blood or lymph system and invade other tissues and organs to form a secondary tumor C. Characteristics of malignant cells 1. Rapid cell division and growth: regulation of the rate of mitosis is lost 2. No contact inhibition: cells do not respect boundaries of other cells and invade their tissue areas 3. Loss of differentiation: cells lose specialized characteristics of function for that cell type and revert back to an earlier, more primitive cell type 4. Ability to migrate (metastasize): cells move to distant areas of the body and establish new site malignant lesions (tumors) 5. Alteration in cell structure: differences are evident between normal and malignant cells with respect to cell membrane, cytoplasm and overall cell shape 6. Self-survival a. may develop ectopic sites to produce hormones needed for own growth b. can develop a connective tissue stroma to support growth c. May develop own blood supply by secreting angiotensin growth factor to stimulate local blood vessels to grow into tumor D. Epidemiology of Cancer 1. Incidence of cancer a. Cancer affects every age group though most cancer and cancer deaths occur in people older than 65 years of age b. Cancer ranks 3rd as the cause of morbidity in the Philippines c. Highest incidence of all cancer is prostate cancer d. Highest cancer incidence in males in order of frequency: prostate cancer, lung cancer and colorectal cancer e. Highest cancer incidence in females in order of frequency: breast cancer, lung cancer and colorectal cancer Common sites of cancer and their sites of metastasis Cancer Type 1. Brain Cancer 2. Breast cancer 3. Colon cancer 4. Lung cancer 5. Prostate cancer Sites of Metastasis Central Nervous System Brain Liver Regional lymph nodes Vertebrae Brain Liver Lung Lymph nodes Ovaries Bone Brain Liver Lymph nodes Pancreas Spinal cord Bladder Bone Liver Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN External factors causing CANCER 1. Chemical Carcinogens- over 1,000 chemicals are known to be carcinogenic • Alcoholic beverages (Liver, esophagus, mouth, breast colon) - serves as a promoter in cancers of the liver and esophagus - when combined with tobacco, the risks for other cancers are even higher • Anabolic Steroid (Liver) • Arsenic (Lung; Skin) • Asbestos (Lung; peritoneum) • Benzene (Leukemia) Diesel exhaust (Lung) Hair dyes (bladder) Pesticides (Lungs) Sunlight (Skin; eyes) Tobacco (Lungs; esophagus; mouth; pharynx; larynx) smokeless tobacco (snuff and chewing tobacco) increases the risk of oral and esophageal cancers * long-term exposure to secondhand smoke increases the risk for lung and bladder cancers 2. Physical Carcinogens – Radiation – Chronic Irritation- GERD 3. Viral Carcinogens - some viral infections tend to increase risk of cancer Ex: Epstein Barr Genital herpes Papillomavirus Hepatitis B Human cytomegalovirus 4. Dietary Factors - diets in high fat, low in fiber and those containing nitrosamines found in preserved meats and pickled foods promote certain cancers such as colon, breast, esophageal and gastric Personal factors causing CANCER 1. Immune Functions 2. Age a. Increased risk for people over age of 65 b. Factors attributed to cancer in elderly include hormonal changes, altered responses and the accumulation of free radicals c. Age has been identified as the single most important factor related to the development of cancer 3. Gender a. certain cancers are more commonly seen in specific genders ex: breast cancer –more common in female colon cancer – more common in males 4. Genetic Risk - 15% of cancers may be attributed to a hereditary component Ex: Breast, colon, lung, ovarian and prostate cancers 5. Race – can affect any population - African-Americans experience a higher rate of cancer than any other racial or ethnic group CARCINOGENESIS: Transformation of Normal Cells into Cancer Cells 1. Initiation – occurs when carcinogen damages DNA - carcinogenesis cause changes in the structure and function of the cell at the genetic or molecular level. This damage may be reversible or may lead to genetic mutations if not repaired; however the mutations may lead immediately to cancer 2. Promotion – occurs with additional assaults to the cell, resulting in further geneticdamage 3. These genetic events result in a malignant conversion 4. Progression – the cells are increasingly malignant in appearance and behaviour and develop into an invasive cancer with metastases to distant body parts Comparison of the Characteristics of Normal and Cancer Cells Characteristic Mitotic cell division Normal Cells Mitotic division lead to 2 daughter cells Appearance 1. Cells of same type homogeneous in size, shape, and growth 2. Cells cohesive, form regular pattern of expansion 3. Uniform size to nucleus 4. Have characteristic pattern of organization Cancer Cells Mitosis leads to multiple daughter cells that may or may not resemble the parent. Multiple mitotic spindles 1. cells larger and grow more rapidly than normal; pleomorphic 2. Cells not as cohesive; irregular patterns of expansion 3. Larger, more prominent nucleus 4. Lack characteristic pattern of organization of host cell Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN 5. Mixture of stem cells (precursors) and well-differentiated cells 5. Anaplastic, lack of differentiated cell characteristics, specific functions Growth pattern 1. do not invade adjacent tissue 2. Proliferate in response to specific stimuli 3. Grow in ideal conditions (ex: nutrients, oxygen, space, correct biochemical environment) 4. Exhibit contact inhibition 5. Cell birth equals or is less than cell death 6. Stable cell membrane 7. Constant or predictable growth rate 8. Cannot grow outside specific environment (ex: breast cells grow only in breast) 1. invade adjacent tissues 2. Proliferation in response to abnormal stimuli 3. Grow in adverse conditions such as a lack of nutrients 4. Do not exhibit contact inhibition 5. Cell birth exceeds cell death 6. Loss of cell control a result of cell membrane changes 7. Growth rate erratic 8. Able to break off cells that migrate through bloodstream or lymphatics or seed to distant sites and grow in other sites Function 1. have specific, designated purpose 2. Contribute to the overall well-being of the host 3. Function in specific, predetermined manners (ex: cells in the thyroid secrete thyroid hormone) 1. serve no useful purpose 2. do not contribute to the well-being of the host; parasitic, actually feed off host without contributing anything 3. If cells function at all, they do not function normally or they may actually cause damage (ex: lung cancer cells secrete ACTH and cause excessive stimulation of adrenal cortex) Other 1. develop specific antigens, characteristic of the particular cell formed 2. Chromosomes remain constant throughout cell division 3. Complex metabolic and enzyme pattern 4. Cannot invade, erode, or spread 5. cannot grow in present of necrosis or inflammation 1. develop antigens completely different from a normal cell 2. chromosomal aberrations 3. have more primitive and simplified metabolic and enzyme pattern 4. invade, erode and spread 5. grow in presence of necrosis and inflammatory cells such as lymphocytes and macrophages 6. exhibit periods of latency that vary from tumor to tumor 7. have own blood supply and supporting stroma Metastasis - ability of cancer cells to spread from the original site of the tumor to distant organs Stages: 1. Detachment * tumor cell loses cohesiveness and it has increasing motility * tumor cell detaches from the primary tumor and create defects in the basemement membranes with resulting stromal invasion and spread into circulation 2. Migration * Cancer cells migrate via the lymph or blood circulation or by direct extension * The lymphatic system provides the most common pathway for the initial spread of malignant cancer cells * The blood vessels carry cancer cells from the primary tumor to the capillary beds of the lungs, liver and bones * Direct tumor extension of tumors to adjacent tissues also occurs Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN 3. Dissemination * Cancer cells are established at the secondary site which may result from entrapment due to the size of the tumor clump, adherence to cells at the new through specific interactions, or by binding to exposed basement membrane 4. Angiogenesis * Vascularization of the tumor The Immune System and Cancer Two critical components of the immune response 1. the ability to recognize a pathogen as foreign 2. the ability to mount a response to eliminate the pathogen * T-cell lymphocyte, macrophages, and antigens recognize cancers cells as non-self and destroy them Immune Surveillance Theory – proposes that immune responses, particularly cell-mediated, provide a defense against cancer cells by recognizing the antigens on the surface of some neoplastic cells as foreign - they are killed by cytotoxic T cells that have receptors for specific tumor antigens and by interferonactivated natural killer (NK) lymphocytes and macrophages - macrophages phagocytize the pathogen and present it as antigen to T and B lymphocytes Failure of Immune Defenses - the immune system may be unable to recognize cancer cells as foreign or to mount an immune response due to the following: a. it’s immature, old or weak b. malnutrition or chronic ailment c. cancer cells escape detection because they resemble normal cells. Others produce substances that shield them from recognition or they may be coated with fibrin d. use of immunosuppressive drugs which can suppress immune system Classification of Neoplasms 1. Benign – from latin word “benigunus”- kind 2. Malignant a Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN Characteristic Speed Growth Mode of Growth Capsule Cell characteristics Recurrence Benign Neoplasm Grows slowly Usually continues to grow throughout life unless surgically removed May have periods of remission Grows by enlarging and expanding Always remains localized; never infiltrates surrounding tissues Malignant Neoplasm Usually grows rapidly Tends to grow relentlessly throughout life Rarely, neoplasm may regress spontaneously Almost always contained within a fibrous capsule Capsule does not prevent expansion of neoplasm but does prevent growth by infiltrations Capsule advantageous because encapsulated tumor can be removed surgically Usually well differentiated Mitotic figures absent or scanty Anaplastic cells absent Cells function poorly in comparison with normal cells from which they arise If neoplasm arises in glandular tissue, cells may secrete hormones Unusual when surgically removed Never contained within a capsule Absence of capsule allows neoplastic cells to invade surrounding tissues Surgical removal of tumor difficult Metastasis Effect of Neoplasm Never occur Not harmful to host unless located in area where it compresses tissue or obstructs vital organs Does not produce cachexia (weight loss, debilitation, anemia, weakness, wasting) Prognosis Very good Tumor generally removed surgically Grows by infiltrating surrounding tissues May remain localized (in situ) but usually infiltrates other tissues Usually poorly differentiated Large numbers of normal and abnormal mitotic figures present Cells tend to be anaplastic Cells too abnormal to perform any physiologic functions Occasionally a malignant tumor arising in glandular tissue secretes hormnes Common following surgery because tumor cells spread into surrounding tissues Very common Always harmful to host Causes death unless removed surgically or destroyed by radiation or chemotherapy Causes disfigurement, disrupted organ function, nutritional imbalances May result in ulcerations, sepsis, perforations, hemorrhage, tissue slough Almost always produces cachexia, which leaves person prone to pneumonia, anemia, and other conditions Depends on cell type and speed of diagnosis Poor prognosis if cells are poorly differentiated and evidence of metastatic spread exists Good prognosis indicated if cells still resemble normal cells and there is no evidence of metastasis Classification of cancer according to tissue of origin 1. Carcinoma - refers to a tumor that arises from epithelial tissue; the name of the cancer identifies location example: basal cell carcinoma 2. Sarcoma - refers to a tumor arising from supportive tissues; the name of the cancer identifies the specific tissue affected example: osteosarcoma 3. Adenocarsinoma – from glandular tissue. example: lungs, ovaries Tissue of Origin Connective Tissue Bone Fibrous tissue Adipose tissue Epithelial Tissue Glandular Surface Benign Neoplasms Malignant Neoplasms Osteoma Fibroma Lipoma Osteosarcoma Fibrosarcoma Liposarcoma Adenoma Papilloma Adenocarcinoma Squamous cell carcinoma Hematopoietic Erythrocytes Granulocytes Lymphatic tissue Erythroleukemia Leukemia Hodgkin’s disease, malignant lymphoma Lymphocytes Plasma cells Lymphocytic leukaemia Multiple myeloma Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN Cancer Prevention and Control 1. Prevention – involves measures to avoid or reduce exposure to carcinogens - activities are aimed at interventions before pathologic change has begun 2. Screening – helps to identify high-risk populations and individuals 3. Early Detection – involves finding a precancerous lesion or a cancer at its earliest, most treatable stage - also called secondary prevention - methods a. inspection b. palpation c. use of tests or procedures Approaches to Cancer prevention 1. Education 2. Regulation – prohibit the sale of tobacco and alcohol to minors, limiting smoking in public places, imposing excise taxes, regulating the use of manufactured carcinogens such as asbestos, and prohibiting carcinogens in foods 3. Host modification - aims to alter the body’s internal environment to decrease the risk of or to reverse a carcinogenic process Cancer Prevention 1. Skin: Avoid exposure to sunlight 2. Oral: Annual oral examination 3. Breast: Monthly BSE from age 20 4. Lungs: Avoid cigarette smoking; annual chest x-ray 5. Colon: DRE for person over age 40. Rectal biopsy, proctosigmoidoscopic examination, Guiac stool examination for persons age 50 and above 6. Uterus: annual Pap’s smear from age 40 7. Basic: annual physical examination and blood examination Dietary Recommendations against cancer 1. Avoid obesity 2. Cut down on total fat intake 3. Eat more high fiber foods – raw fruits and vegetables, whole grain cereal 4. Include food rich in vitamin A and C in daily diet 5. Include cruciferous vegetables in the diet: brocolli, cabbage, cauliflower, brussel sprouts 6. Be moderate in the consumption of alcoholic beverages 7. Be moderate in the consumption of salt-cured, smoked-cured and nitrate-cured foods Recommendations of the American Cancer Society for Early Cancer Detection 1. For detection of breast cancer a. Beginning at age 20, routinely perform monthly breast self-examination b. Women ages 20-39 should have breast examination by a healthcare provider every 3 years c. Women age 40 and older should have a yearly mammogram and breast self-examination by a healthcare provider 2. For detection of colon and rectal cancer a. all persons age 50 and older should have a yearly fecal occult blood test b. digital rectal examination and flexible sigmoidoscopy should be done every 5 years c. Colonoscopy with barium enema should be done every 10 years 3. For detection of uterine cancer a. yearly papanicolao (Pap) smear for sexually active females and any female over age 18 b. At menopause, high-risk women should have an endometrial tissue sample 4. For detection of prostate cancer a. beginning at age 50, have a yearly digital rectal examination b. beginning at age 50, have a yearly prostate-specific antigen (PSA) test American Cancer Society’s seven warning signs of cancer (uses acronym CAUTION US): 1. Change in bowel or bladder habits 2. A sore that does not heal 3. Unusual bleeding or discharge 4. Thickening or lump in breast or elsewhere 5. Indigestions or difficulty in swallowing 6. Obvious change in wart or mole 7. Nagging cough or hoarseness 8. Unexplained Anemia 9. Sudden loss of weight Diagnostic tests of Cancer 1. Biopsy/cytology a. Histologic and cytologic examination of specimens are performed by the pathologist on tissues collected by needle aspiration of solid tumors, exfoliation from epithelial surface, and aspiration of fluid from blood or body cavities b. Tissues may be obtained by excisional biopsy, incisional biopsy, and needle biopsy c. By examination of these tissues, the name, grade, and stage of the tumor can be identified Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN 2. Papanicolao Test (Pap Smear) Class I: Normal Class II: Inflammation Class III: Mild to moderate dysplasia Class IV: Probably malignant Class V: Malignant 3. Ultrasound 4. MRI 5. X-rays 6. CT scan 7. Radiographic techniques 8. Antigen Skin test 9. Laboratory tests a. Alpha-feto-protein b. HCG c. Prostatic Acid Phosphatase (PSA) d. Carcinoembroyenic antigens (CEA) 10. Endoscopic examination 11. Monoclonal antibodies Tumor markers 1. Tumor markers are protein substances found in the blood or blody fluids 2. Are released either by the tumor itself, or by the body as a defense in response to the tumor (called host response) 3. Tumor markers are derived from the tumor itself. And include the ff: a. Oncofetal antigens, present normally in fetal tissue, may indicate an anaplastic process in tumor cells; carcinoembyonic antigen (CEA) and alpha-fetoprotein (AFP) are examples of oncofetal antigens. b. Hormones are present in large quantities in the human body; however, high levels of hormones may indicate a hormone-secreting malignancy; hormones that may be utilized as tumor markers include the antidiuretic hormone (ADH), calcitonin, catecholamines, human chorionic gonadotropin (HCG), and parathyroid hormone (PTH) c. Isoenzymes that are normally present in a particular tissue may be released into bloodstream if the tissue is experiencing rapid, excessive growth as the result of tumor; are examples include neuron-specific enolase (NSE) and prostatic acid phosphatase (PAP) d. Tissue-specific proteins identify the type of tissue affected by malignancy; an example of a tissue-specific protein is the protastic-specific antigen (PSA) utilized to identify prostate cancer 4.Host-response tumor makers include the following: a. C-reactive protein b. Interleukin-2 c. Lactic dehydrogenase d. Serum Ferritin e. Tumor necrosis factor Staging Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN 1. The TNM tumor system is utilized for classifying tumors a. T indicates the tumor size 1) T0 indicates no evidence of tumor 2) T is indicates tumor in situ 3) T1,T2,T3,T4 indicate progressive degrees of tumor size and involvement b. N indicates lymph node involvement 1) N0 indicates no abnormal lymph nodes detected 2) N1a, N2a indicate regional nodes involved with increasing degree from N1a to N2a, no metastases detected 3) N1b, N2b, N3b indicate regional lymph nodes involvement with increasing Degree from N1b to N3b, metastasis suspected 4) Nx indicates inability to assess regional nodes c. M indicates distant metastases 1) M0 indicates no evidence of distant metastasis 2) M1, M2, M3 indicate ascending degrees of distant metastasis and includesdistant lymph nodes Different Modalities for Cancer 1. Surgical interventions 2. Chemotherapy 3. Radiation therapy 4. Immunotherapy 6. Bone Marrow transplantation Surgical Intervention 1. Preventive surgery- removal of precancerous lesions or benign tumors 2. Diagnostic surgery- biopsy 3. Curative surgery- removal of an entire tumor 4. Reconstructive surgery – improvement of structures and function of an organ 5. Palliative surgery – relief of distress in signs and symptoms; retardations of metastasis Common Nursing Techniques and Procedures A. Radiation therapy 1. Is used to kill a tumor, reduce the tumor size, relieve obstruction, or decrease pain 2. Causes lethal injury to DNA, so it can destroy rapidly multiplying cancer cells, as well as normal cells 3. Can be classified as internal radiation therapy (bachytherapy) or external radiation therapy (teletherapy) B. The client undergoing brachytheraphy ( internal radiation) 1. Sources of internal radiation a. Implanted into affected tissue or body cavity b. Ingested as a solution c. Injected as a solution into the bloodstream or body cavity d. Introduced through a catheter into the tumor 2. Side effects of internal radiation a. Fatigue b. Anorexia c. Immunosuppression d. Other side effects similar to external radiation 3. Priority nursing diagnoses: Impaired tissue integrity; fatigue; anxiety; risk for infection; Social isolation; Imbalanced nutrition: less than body requirements 4. Client education a. Avoid close contact with others until treatment is completed b. Maintain daily activities unless contraindicated, allowing for extra rest periods as needed c. Maintain balanced diet; may tolerate food better if consumes small, frequent meals d. Maintain fluid intake ensure adequate hydration (2-3 liters/day) e. If implant is temporary, maintain bedrest to avoid dislodging the implant. f. Excreted body fluids may be radioactive; double-flush toilets after use g. Radiation therapy may lead to bone marrow suppression 5. Nursing management of client receiving internal radiation a. Exposure to small amounts of radiation is possible during close contact with persons receiving internal radiation: understand the principles of protection from exposure to radiation: time, distance, and shielding 1) Time: minimize time spent in close proximity to the radiation source; a common standard is to limit contact time to 30 minutes total per 8-hour shift; minimum distance of 6 feet used when possible 2) Distance: maintain the maximum distance possible from the radiation source 3) Shielding: use lead shields and other precautions to reduce exposure to radiation b. Place client in private room c. Instruct visitors to maintain at least a distance of 6 feet from the client and limit visitors to 10-30 minutes d. Ensure proper handling and disposal of body fluids, assuring the containers are marked appropriately e. Ensure proper handling of bed linens and clothing f. In the event of a dislodged implant, use long-handled forceps and place the implant into a lead container; never directly touch the implant g. Do not allow pregnant woman to come into any contact with radiation Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN h. If working routinely near radiation sources, wear a monitoring device to measure exposure i. Educate client in all safety measures 6. Evaluation: client demonstrates measures to protect others from exposure to radiation, identifies interventions to reduce risk of infection, remains free from infection, achieves adequate fluid and nutritional intake activities of daily living (ADLs) at level of ability The client undergoing external radiation therapy (teletheraphy) 1. The radiation oncologist marks specific locations for radiation treatment using a semipermanent type of ink a. Treatment is usually given 15-30 minutes per day, 5 day per week, for 2-7 weeks b. The client does not pose a risk for radiation exposure to other people 2. side effects of external radiation therapy a. Tissue damage to target area (erythema, sloughing, hemorrhage) b. Ulcerations of oral mucous membranes c. Gastrointestinal effects such as nausea, vomiting, and diarrhea d. Radiation pneumonia e. Fatigue f. Alopecia g. Immunosuppression 3.Priority nursing diagnoses: risk for infection; impaired skin integrity; social isolation; disturbed body image; anxiety; fatigue 4. Client education exam for external radiation a. Wash the marked area of the skin with plain water only and pat skin dry; do not use soaps, deodorants, lotions, perfumes, powders or medications on the site during the duration of the treatment; do not wash off the treatment site marks b. Avoid rubbing, scratching, or scrubbing the treatment site; do not apply extreme temperatures (Heat or Cold) to the treatment site ; if shaving, use only an electric razor c. Wear soft, loose-fitting over the treatment area d. Protect skin from sun exposure during the treatment and for at least 1 year after the treatment is completed; when going outdoors, use sun-blocking agents with sun protector factor (SPF) of at least 15 e. Maintain proper rest, diet, and fluid intake as essential to promoting health and repair of normal tissues f. Hair loss may occur; choose a wig, hat, or scarf to cover and protect head (refer to care of client with alopecia later in chapter) 5. Nursing management of the client receiving external radiation a. Monitor for adverse side effects of radiation b. Monitor for significant decreases in white blood cell counts and platelet counts c. Client teaching (refer to later sections for management of immunosuppression, thrombocytopenia 6. Evaluation; client identifies interventions to reduce risk of infection, remains free from infection, achieves adequate fluid and nutritional intake, participates in activities of daily living (ADLs) at level of ability, and maintains intact skin. The Client Undergoing a Bone Marrow Transplant (BMT) 1. BMT – used in the treatment of leukemias, usually in conjunction with radiation or chemotherapy a. Autologous BMT – the client is infused with own bone marrow harvested during remission of disease b. Allogenic BMT – the client is infused with donor bone marrow harvested from a healthy individual 2. The bone marrow is usually harvested from the iliac crest, then frozen and stored until transfusion 3. Before receiving the BMT, the client must first undergo a phase of immunosuppressive therapy to destroy the immune system, infection, bleeding, and death are major complications that can occur during this conditioning phase 4. After immunosuppression, the bone marrow is transfused intravenously through a central line 5. Side of BMT a. malnutrition b. infection related to immunosuppression c. bleeding related to thrombocytopenia 6. Priority Nursing Diagnoses a. Risk for infection b. Risk for hemorrhage c. Risk for imbalanced nutrition d. Social isolation e. Anxiety 7. Nursing Management of client undergoing a bone marrow transplant a. Monitor for graft-versus-host disease b. Provide private room for the hospitalized client; client will be hospitalized for 6-8 weeks c. Encourage contact with significant others by using telephone, computer, and other means of communication to reduce feelings of isolation d. Refer to management for imbalanced nutrition, immunosuppression and thrombocytopenia 8. Evaluation: client evaluates understanding of risks and participates in activities that reduce risk of infection, hemorrhage, and malnutrition; client demonstrates effective coping mechanisms Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN The Client Undergoing other therapeutic interventions 1. Immunotherapy/biologic response modifiers (BMR) a. Enhances the person’s own immune responses in order to modify the biologic processes resulting in malignant cells b. Currently considered experimental in use c. Monoclonal antibodies: antibodies are recovered from an inoculated animal with a specific tumor antigen, then given to the person with that particular cancer type; the goal is: destruction of the tumor d. Cytokines: normal growth-regulating molecules possessing antitumor abilities 1) Interleukin-2(IL-2) increases immune response effective and destroys abnormal cells 2) Interferons are substances produced by cells to protect them from viral infection and replication; interferon-alpha 2b is most commonly used 3) Hematopoietic growth factors such as granulocyte colony- stimulating factor (G-CSF) and erythropoietin, balance the suppression of granulocytes and erythrocytes resulting from chemotherapy e. natural killer cells (NK cells) : exert a spontaneous cytotoxic effect on specific cancer cells; they also secrete cytokines and provide a resistance to metastasis 2. Gene therapy a. Current use in investigational b. Increases susceptibility of cancer cells to the destruction by other treatments; insertion of specific genes enhances ability of client’s own immune system to recognize and destroy cancer cells 3. Photodynamic theory a. Used to treat specific superficial tumors such as those of the surface of bladder, bronchus, chest wall, head, neck and peritoneal cavity b. Photofirin, a photosensitizing compound, is administered intravenously where it is retained by malignant tissue c. Three days after injection, the drug is activated by a laser treatment which continue for 3 more days d. The drug produces a cytotoxic oxygen molecule (singlet oxygen) e. During intravenous administration, monitor for chills, nausea, rash, local skin reactions, and temporary photosensitivity f. Drug remains in tissues 4-6 weeks after injection; direct or indirect exposure to sun activates drug, resulting in chemical sunburn; educate client to protect skin from exposure to sun Oncologic Emergencies: Diagnosis and Management 1. Spinal Cord Compression a. Occurs secondary to pressure from expanding tumors b. Early symptoms include back and leg pain, coldness, numbness, tingling, paresthesias, progression leads to bowel and bladder dysfunction, weakness, and paralysis c. Early detection is essential: investigate all complaints of back pain or neurological changes d. Treatment is aimed at reducing tumor size by radiation and/or surgery to relieve compression and prevent irreversible paraplegia; may receive corticosteroids to reduce cord edema e. Nursing interventions include early recognition of symptoms, neurological checks and medication administration 2. Superior vena cava syndrome a. Compression or obstruction of the superior vena cava (SVC) b. Usually associated with cancer of the lungs and lymphomas c. signs and symptoms are the result of blockage of venous circulations of head, neck, and upper trunk d. Early signs and symptoms are periorbital edema and facial edema e. Symptoms progress to edema of neck, arms, and hands, difficulty swallowing, shortness of breath f. Late signs and symptoms are cyanosis, altered mental status, headache, and hypotension g. Death may occur if compression is not relieved h. Treatment included high-dose radiation to shrink tumor and relieve symptoms i.Nursing interventions include: a. Monitoring vital signs b. providing oxygen support c. preparing tracheostomy if necessary d. initiating seizure precautions e. administering corticosteroids to reduce edema 3. Disseminated intravascular coagulopathy (DIC) a. Severe disorder of coagulation, often triggered by sepsis, whereby abnormal clot formation occurs in the microvasculature; this process depletes the clotting factors and platelets, allowing extensive bleeding to occur tissue hypoxia occurs as a result of the blockage of blood vessels from the clots b. Signs and symptoms are related to decreased blood flow to major organs (tachycardia, oliguria, dyspnea) and depleted clotting factors (abnormal bleeding and hemorrhage) c. Treatment includes anticoagulants to decrease stimulations of coagulation and transfusion of one or more of the following: 1) fresh frozen plasma (FFP) 2) cryoprecipitate 3) platelets 4) packed RBC d. Nursing interventions include assessing client, monitoring for bleeding, applying pressure dressings to venipuncture sites, and preventing risk of sepsis e. Mortality for clients experiencing DIC is greater than 70% despite aggressive treatment Medical and Surgical Nursing Oncology Nursing Lecture Notes Prepared by: Mark Fredderick R. Abejo RN, MAN 4. Cardiac tamponade a. Pericardial effusion secondary to metastases or esophageal cancer can lead to compression of heart, restricting heart movement and resulting in cardiac tamponade b. Signs and symptoms are related to cardiogenic shock or circulatory collapse: anxiety, cyanosis, dyspnea,hypotension, tachycardia,tachypnea,impaired levels of consciousness, and increased central venous pressure c. Pericardiocentesis is performed to remove fluid from pericardial sac d. Nursing interventions 1) administering oxygen 2) maintaining intravenous line 3) Monitoring vital signs 4) hemodynamic monitoring 5) administration of vasopressor agents