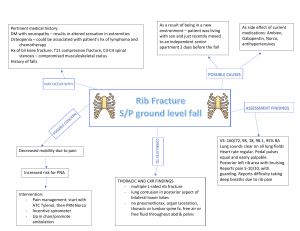
V.N.KARAZIN KHARKIV NATIOONAL UNIVERSITY MEDICAL FACULTY DEPARTMENT OF PEDIATRICS CASE HYSTORY The patient’s_ Sophia ,10 years old ___________ Name, surname, age Diagnosis _______acute_bronchitis________ Student of 5th course _Sahil ___ Group____528__ Date of giving the history for checking up_3/04/2022________________ Teacher’s signature_____ natalia rybak I. PASPORT PART 1. Patient’s surname, first name, second name Sophia 2. Age, date of the birth_10 years old ,16/04/2010 3. Sex (male, female) 4. Date of admission__2/03/2022_ II. PATIEN’S COMPLAINS Ask the patient about the causes of his (her) visit. 1 General complains (temperature, chill, appetite, thirst, weakness, mood)_ _she complains of cough ,fever ,difficulty in breathing , weakness, chills ,pain in muscles and lungs. Complains of diseases in other systems and organs: NERVOUS SYSTEM: ability to work ________yes____, mood_ yes__________, memory_yes___________, attention__good___________, sleep____sleep_apnea_________________ headache: location__in frontal part of head _, character cough headace intensity___mild _, permanent or periodic; accompanying symptoms: pulsation, burning, pressing; dizziness___yes___ tics _vocal tics _convulsion____yes________ hypo -, hyperstesia_____no__ disorders of feeling and speech organs____no__ MUSCULAR-BONE SYSTEM: pain in the muscles__sever pain muscular spasms_____yes______________muscular weakness__yes_____________ pain in the joints (SLIDA)_____mild_stiffness______________________________________ movements of the joints limited ____no___________, redness and swelling of the skin above joints______no__ pain in vertebral column____yes_ RESPIRATORY SYSTEM: sneeze___yes___________, congestion ___yes__________ changing of voice_yes________ cough (dry or moist, deep or superficial, time of appearance_moist,superficial,morning or at night mainly, duration, specific sings)__3 to 10 days with mucus ,pain during cough . _ sputum ( amount_____small_______,character_purulent_mucous,odorless______________ ________________, color____yellow-grey______________, impurity)____yes_______________________________ pain in the chest____yes____, dyspnea (inspiratory, expiratory, mixed)_____mixed_______ CARDIOVASCULAR SYSTEM heart pain (character___yes___________ location__left_midclavicular_region___________, irradiation to the left arm, neck, back)______yes____dyspnea__yes__palpitation__tactile_fermitus_normal______ edema localization _peripheral_____________time of appearance__while coughing _________________ 2 DIGESTIVE SYSTEM abdominal pain (localization____yes______________ intensity_normal__________, irradiation_______no________ time of appearance__while breathing _, connection with eating____pain while swolling _, connection of pain with the act defecation___yes____ dyspeptic disorders: the thirst, difficulty swelling, regurgitation, heartburn, eructation, nausea, vomiting; disorders of defecations: diarrhea(rate, consistence of feces, color, smell, impurity) _________no______, constipation (rate, consistence of feces)_________no_____, disorders of appetite_____no_ URORENAL SYSTEM: pain in the lumbar region: (characteristic, radiate, time ) _mild pain ,during coughing and breathing _, pain in the lower part of abdomen_____yes__, changes of urination (painfulness, rate )__no___, ratio of day time and nocturnal urination)______no__ color of urine______normal ENDOCRINE SYSTEM: Changes of voice yes_ disturbance of the hair growth___no_ (alopecia, hypertrichosis). changes of skin (excessive sweating, dryness)___no_______________________, disorders of growth ______no__ body mass (malnutrition, obesity)__obesity disorders of mensis_____no_ III. HYSTORY DISEASES Development of diseases is described in chronological order. The probably causes of the diseases. Development of symptoms. Previous investigations. Information about treatment, its effectiveness. __ firstly she complains about pain in chest ,coughing for long days and mild fever ,so after diagnosis she had acute bronchitis .hes_sputum cough leading to pneumonia which further lead to acute bronchitis. On examination ,lung auscultation has wheezing sound . IV. PAST HYSTORY Physical and psychomotor development in early childhood. When he go to the kinder-garden or school, school success. _his physical development is normal ,well good during school 3 Previous infection and somatic diseases._______he living in a polluted place due to poor family history so he had asthma __ Information about surgical operations___no_____ Information about tuberculin sensitivity (Manty tests result)____no_____________ Information about prophylactic vaccination _____________negative___________ reactions on vaccination__no____ The child’s hygienic regime___living in polluted area Family history: presence in family heredity diseases, alcoholism, psychiatric diseases, cancer. Family material status and living conditions. _____________he have 3 sister ,only one person who earn money ,so his family condition is not good Lives in polluted area . Allergic history: presence of allergic diseases in child, his parents; presence of unusual reactions on the food, plants, smells, insects, animals and so on. __________allergy to pollen Epidemiological anamnesis: presence of contact with the infectious patients for the last 3 weeks, epidemiological surroundings in child's establishment which is visited by a child. Contact in the family with venereal diseases (syphilis, gonorrhea, AIDS) tuberculosis _____________no such history _ V. OBJECTIVE EXAMINATION General condition of the child: satisfactory, moderate, severe, very severe (choose). Patient’s feeling satisfactory, no satisfactory reaction to others: adequate, negative (choose). Position on the bed: active, passive, compelled __________________________________________________________________. Consciousness: clear, stupor, sopor, coma, excitement (choose). PHYSICAL DEVELOPMENT OF CHILD Estimations of all parameters are provided with percentile tables: average, above the average, less than average, excessive, low, extremely excessive and extremely low. Weight)___12___(kg)___________height___1.35_____(cm),_________________ ____ BMI_____10.3kg/m2_________________________________________________ ________ head circumference___55___ (cm), chest circumference _57______(cm). CONCLUSION: physical development satisfactory, delay, biology acceleration 4 Average but accelerating __________________________________________________________________ ________________________________________________________________ NERVOUS SYSTEM Psychomotor development speech__no___________, sensory: vision__no__ hearing__yes________ skin sensibility__________ (parastesia, hyperstesia, anesthesia), olphactory function normal____________ taste function___normal_____________ , intellect activity__normal_____________, motor activity____abnormal__________________, (Corresponds or not to age) Stigmatic of embriogenesis (micrognatia, macrognathia, low or asymmetrical located ears, deformation of earlobes, low growth of the hair on the forehead, falling or sinking down of the eyelid, torticollis, a significant amount creases on the neck, protrusions umbilicus, polydactyly, brachidactyly, arachnodactyly, syndactyly, overlapping, camptodactyly) _______no________________________ vegetative innervation’s according the result of demographic investigation ( white or red) Abnormalities of gait___________no____________________________________ Coordination (is checked with Romberg’s position (posture is stable or not)_________________________no____________________________________ __________________________________________________________________ __ finger–nose test (presence or absence of distaxia)_____no______________________ heel-knee test________________no________________________________________ Presence of pathological symptom or not: Kernig’s, Brudsinsky’s upper, Brudzinsky’s lower, rigidity of occipital muscles_______yes___________ SKIN, SUBCUTANEUS TISSUE Color of skin: usually color, pink, pale-pink, pale, yellow, gray, cyanotic (acrocyanosis, perioral cyanosis, periorbital cyanosis, cyanosis of the nasolabial triangle)(choose). Rash on the skin: primary lesions: macula, patch, papule, plaque, nodule, tumor, vesicle, bulla, pustule (choose); secondary: pigmentation, crust, fissure, erosion, ulcer, scar, lichenification, hemorrhagic rash (choose); localization: quantity: excess itching: No Temperature of skin: moderate warm, cold, hot, Dryness or moistness: moderate moist, moist (indicate location)__moist_in_chest__________ __________________________________________________________________ dry (indicate location)___dryness_in_chest__________________________________________ Elasticity: normal, decreased, increased. 5 The thickness of subcutaneous tissue on lateral surface of abdomen on the umbilical level ____cm, on subscapular place ___ cm, internal surface of thigh ___cm, on the middle of third of foream ___ cm. Development of subcutaneus fat is: sufficiently, poor, excessively developed Distribution of subcutaneous fat: uniform, deposits __________________________________________________________________ Tissue turgor: satisfactory, decreased, increased (choose). Edema: present or not, location___peripheral_____________________________________________ Lymphatic nodes Groups: occipital anterior posterior cervical submandibular: supraclavicular_ undercavicular axillary, cubital, inguinal (describe their localization, quantity, size, shape, , adhesion of nodes between themselves, elastic or dense, painfulness, skin temperature above nodes) MUSCULAR SYSTEM Degree of development of muscle mass: low, middle, good; symmetrical or asymmetrical (choose). Palpation of muscles: painless, painfulness; consistent (density, moderate density, soft) Muscular strength: muscular strength of fingers of hand_weak____________, __________hands, ____weak________forearms,___weak_______ arm, ________upper shoulders (sufficient, reduced, presence weakness of muscles; symmetrical or not) Muscular tone: is sufficient or presence of atonia, hypotonia, hypertonia (indicate location)___hypotonia____ ________ SCELETAL SYSTEM Inspection of head: size:55 cms circumference shape: Normal symmetry: Normal, presence craniotabes or not. Teeth state: caries presence or not Posture state: normal, lordosis, kyphosis, scoliosis, kyphoscoliosis (choose). Estimation of chest: shape (norm, deformation) enlarged Extremities: O-form, X-formed, feet deformation, flat foot, norm foot Estimation of joints: check all group of joints___normal___________________________ Pathological changes : location___________deformation_______yes_____________, size_____changes _____________, edema____no_______________, redness__no__________, hot skin_____yes_________, painfulness during palpation__yes_________, during active movement limited in mobility______yes________, during passive movements limited in mobility __________yes__________________ RESPIRATORY SYSTEM Nasal breathing: free, congestion. 6 Nasal secret: character (aqueous, mucous, mucous-purulent, purulent); quantity (insignificant, moderate, significant), impurity (absent or blood impurity); smell (absent, rotten)_ Voice: normal, hoarse, snuffing, aphonic. Cough during examination: dry, productive, less productive; superefficient or deep; short – or long- termed; accompanied with vomiting or not; specific cough (whooping, barking, brassy) Sputum during examination: absent, quantity (significant, insignificant); consistency (watery, viscous); character (mucous, mucous-purulent, purulent, bloody); smell (absent, stinking); presence of blood (the excretion which looks like pink foam, red color, like compact clots, dark red ). Type of breathing (thoracic, abdominal, mixed; corresponds to age or not) Assess respiration rhythm: rhythmic, arrhythmic, Cheyne – Stoke’s, Biot’s, Cussmaul’s respiration. Respiratory rate: normal, tachypnea, bradypnea. The breathing rate in children Age Norm 3-4 years 30-35 5-10 years 20-25 Over 12 years 16-20 Patient’s breathing rate Character of dyspnea: absent, inspiratory, expiratory, mixed; participation of additional muscles in respiration (are present or not) suprasternal fosse__no________nasal flaring___yes___________ retraction of intercostals space______________________no______________________________________ PALPATION OF CHEST Superefficient palpation of chest: painless, painfulness during superefficient palpation (indicate location)_left_ventricular_region________________________________________ _ Assess of vocal fremitus: in norm – middle strength, the same on the symmetrical parts; decreased or increased (indicate location)_left_midclavicular_region________________________ __________________________________________________________________ Deep palpation of chest: painless, painfulness during deep palpation (indicate location____________painful during deep palpation, Resistance of chest: satisfactory, decreased, increased. PERCUSSION OF LUNG Comparative percussion: vesicular resonance over both side of lung; decreased of resonance; dull sound, tympanic (indicate location) _subclavicular_region,_vocal fermittus_____________________ 7 Topographical percussion: upper borders of lung on anterior side (in norm over 10 yr.o. 2-4 cm above clavicle): 5cms above clavicle upper borders of lung on posterior side (in norm on level of spinal process of VII cervical vertebrae): on level of spinal process of Vlll cervical vertebrae width of Kroning’s area (in norm over 10 yr.o. 3-5 cm) ___6 cm__________________; inferior borders of lung on mediaclavicular, medioaxillaris, scapular lines (complete tab.1); excursion of lung (in norm 2-4 cm)_____normal___________________ Table 1 The inferior borders of lung in children Line The side Midclavi сular Middle axillary Right Left Right Scapular Left Right Left Age of the child Till 10 years More than 10 years VI rib VI rib VII – VIII rib VIII rib IX rib IX – X rib X rib patient VIII rib X rib X rib AUSCULTATION OF LUNG Characteristic of breath sound over trachea (in norm bronchial breath sound)_abnormal____________________________ over I-II intercostals space and over interscuapular area (in norm broncho-vesicular breath sound)_____abnormal________________________________________________ __ over lung (in norm vesicular breath sound) ___________________abnormal____________ diminished breath sound) (indicate location) Near the right midclavicular absence of breath sound: No amphoric breath sound ( indicate location): Left scapular region. adventitious respiratory sounds: coarse crackles, fine crackles, low pitch wheezes, high pitch wheezes crepitation, plural rub (indicate location, quantity, phase of respiration( during inhalation or exhalation), disappearance after cough up or not Plural rub near middle axillary during exhalation __________________________________________________________________ Bronchophony: not changed, increased –on one side or both side CARDIOVASCULAR SYSTEM Inspection a heart area: Cardiact hump (in norm absent); Precardiac activity (presence or not) carotid pulsation (present or not); neck vein enlargement pulsation in epigastric area (present or not). Palpation 8 Assess of pulse on radial artery: rate (normal, tachycardia, bradycardia) ( tab.2); rhythm (regular-regula, regula –iregula, iregula-iregula); size (normal high, low, weak, alternating pulse); tension (pulse normal pressure, hard, soft); filling (satisfactory, full, less filling). Table 2 Pulse rate in children Age Pulse rate 3 years 105-100 4 100-105 5 98-100 6 90-95 7 85 - 90 8-9 80-85 10-11 78-84 12 75-82 13-14 72-80 patient Palpation of apex beat: location (tab.3), extension (in norm area of apex beat is not more than 1x1 cm, in older children – 2x2 cm)__left medioclavicular line ________________, force (moderate, increased, decreased)____increased Table 3 Location of apex beat in children Border Till 2 years 2-7 years 7-12 years Above 12 years Patient Right IV –V intercostal 1 cm lateral to space 1-2 cm left lateral to the left medioclavicular medioclavicular line line 7-12 years – on 0,5 cm to the left middle from the medioclavicular left line medioclavicular line Percussion of heart: determination of relative and absolute dullness of heart (tab.4, tab.5) Table 4 Borders of relative heart dullness and transversal heart distance Age Right Till 2 years 2-7 years 7-12 years Above 12 years The right Inwards from In the middleLines, closer to parasternal line the right side between thethe latter, after parasternal line right some yearsparasternal andright 9 right line Upper II rib sternalparasternal line II intercostal III rib space III rib or III intercostal space Left 2 cm outwards 1 cm outwards 0,5 cm outwardOn the left from left from left from mediaclavicle mediaclavicule mediaclavicule mediaclavicle line or 0,5 cm line line line inwards Transversal 6-9 cm 8-12 cm 9-14 9-14 heart distance Table 5 Borders of absolute heart dullness and transversal heart distance Age Till 2 years 2-7 years 7-12 years Right Left sternal line Left sternal line Left line Above years sternalLeft sternal line 12 Patient Upper II intercostal III rib III intercostalIV rib space space Left Closer to the On the left Closer to theLeft left medioclavicular left parasternal medioclavicular line parasternalline line (outside) (outside) Transversal 2-3 cm 4 cm 5-5,5 cm 5-5,5 cm heart distance Auscultation of heart Characteristic of the heart sound in all point of auscultation ( loudness, rhythm, clearness ), abnormal sound: split S1, split S2 paradoxical, widened, fixed, aortic ejection click, pulmonary ejection click, opening snap; murmurs (intensity, time of appearance (early systolic, later systolic, diastolic early, diastolic later, mid diastolic, continuous), duration (long, short), configuration (crescendo, decrescendo, crescendo - decrescendo), quality (harsh, rumbling, scratchy, grunting, blowing, squeaky, musical), irradiation, dependence from the body position, I point ( mitral valve) : loud crescendo & long II point (aortic valves): loud intense and long 10 III point (pulmonary valve): loud rumbling and short IV point (tricuspid valve): short during diastole V point : Towards the right parasternal line Extracardial murmur: Present pericardium frictium: No pleuropericardium friction: no Blood pressure: assess according formula systolic blood pressure : 110mm/Hg diastolic blood pressure 60mm/Hg ( in norm for children older 1 year systolic min - 90 + 2 x n (n is age in years) max - 100 + 2 x n (n is age in years) diastolic:1/2-1/3 of systolic) DIGESTIV SYSTEM Inspection Inspection of oral cavity: mucous membrane of cheeks, palate, gums, pharynx, throat (color – pink, hyperemia (indicate place): Hypermic tonsils dry or moist, tonsils : Moist __________________________________________________________________ Tongue: coated tongue follicles, fissures, geographical tongue, covered : Coated red tongue. Inspection of abdomen: shape: normal and size: normal symmetrical or not, participation in breathing: Active condition of the umbilicus: Normal visible peristaltic present or not, hernia: No umbilical vein visuals or not: No Examination of the perianal area: gaping anus: Normal mucosal prolapse of the rectum: Normal fissures of the anus. Palpation of abdomen Superficial palpation of abdomen: soft abdomen, abdominal distension (indicate place) : soft abdomen with no distention. muscular tenderness and rigidity: Absent painfulness a (epigastric, right subcostal area, left subcostal area, right lateral area, left lateral area, right iliac area, left iliac area), local infiltration (indicate place): pain in the Epigastricum and subcostal areas. meteorism: No Deep palpation of large intestine: sigmoid colon is painless or painfulness; the width: 2Cms (in normal about 1-2 cm), soft or density, mobile or not, grumbling is absent or present; cecum is painless or painfulness, the width is: 2 cms (in norm the size is 3-3,5 cm), mobile or not, soft or density, grumbling is absent or present; ascending part of the colon, transverse colon is placed: grumbling Present (in norm above umbilicus or 12 cm lower than it), painless or painfulness; the width: 2cms (in normal about 2- 2,5 cm), soft or density, mobile or not; descending part of colon: grumbling is absent or present. Symptom of Shchotkin- Blumberg: positive or negative. Palpation of the liver: liver is not palpated, palpated lower than rib in 2cm, shape of edge acute or rounded, consistency soft or density, condition of surface smooth or nodule; 11 The palpation of spleen: spleen is not palpated, palpated lower then left rib in cm, shape, condition of surface, tenderness); The symptoms of gallblager (positive or negative): Ker’s: negative, Ortner’s: negative, Murphy: negative Mussi–Georgievsky: No Palpation of pancreas painless or painfulness in point of Desjardin: No MayoRobson: No Abdominal percussion: Percussion sound : tympanic; weakened, increased, absent; Percussion of sizes of liver by Kurlov’s method ( tab.6) Table 6 The sizes of liver by Kurlov’s method Line of Age of the child (years) Patient measurement 1-3 3-7 7-12 Over 12 Right midclavicular size Anterior median size Left coastal arch or right angel bisector size 5cm 6 cm 8 cm 10 cm 4 cm 5cm 7cm 9cm 3 cm 4 cm 6 cm 8 cm Free fluid in abdominal cavity (fluid wave, fluctuation are present or not) Auscultation of abdomen: is present of grumblings or not Characteristics of stool: Frequency :( more then 3 day per day, 3 time per day, 3 time per week, less than 3 time per week); consistent (type according Bristol’s stool chart, tab.7) Type2 color of feces: brown black, impurity of feces (blood red, dark red), mucus, fat. Table.7 Bristol stool chard Type of stool Characteristic Type1 Separate hard lump, like nuts ( hard to pass ) Type-2 Sausage shaped but lumpy Type-3 Like sausage a but with cracks on it surface Type -4 Like or sausage or snake, smooth and soft Type-5 Soft blobs with clear –cut edges (passed easily) Type-6 Fluffy pieces with ragged edges, a mushy stool Type-7 Watery, no solid pieces 12 URINAL SYSTEM Diuresis: urination rate ____normal__________________________________________ (ratio day time and night time, in norm 2:1), volume of urine__normal______________ (1-10 years – V=600 + 100 (n-1) n – is age in yr., more than 10 years -1500 ml), volume of single act of urination___80 ml________1500ml____________________ (tab.8), painful difficult urination___no__________________________________ involuntary urination____no_____________________________________________. Table 8 Average volume of single act of urination Age Volume in ml 5 years 100 6-10 age 150 Senior school age 250 Patient Bimanual palpation of kidneys: are palpated or not, palpation suprapubical part of abdomen: painless or painfulness)___painless____________________________________ __________________________________________________________________ Pasternatsky’s symptom negative or positive, one the one or both sides) ENDOCRINE SYSTEME Palpation of thyroid gland: enlargemed or not : Enlarged surface smooth or nodule, consistency soft or nodule, painless or painfulness Estimation of sexual development: in girls: Ax :0 Р : No Ма : No Ме: No Menarche with __________ years in boys: Ax ____ Р _______ F ________ L _______ V ________ Formula for estimation of sexual development in girls: Ax : No Р : No Ма: No Ме: No Ax (axilla)- growth of hair in the axilla P (pubic) - pubic hair Ma – development of mammary glands Me - becoming the menstrual function: Me 0 - no menstruation, Me 1 - 1-2 menstruation at the time of examination, 2 - irregular menstruation, 3 – regular menstruation Formula for estimation of sexual development in boys: Ax ____ Р _______ F ________ L _______ V ________ ❌ 13 Ax (axilla)- growth of hair in the axilla P (pubic) - pubic hair F (face) – growth of hair on the face: F0 – absence of hair on the face, F1 - pilosis on the upper lip, F2 - coarse hair on the upper lip and the appearance of hair on the chin, F3 - a common hair on the upper lip and chin, the beginning of the growth of whiskers, F4-5 - fusion zones pilosis L (larynx) - the growth of the thyroid cartilage: L0 - no signs of growth, L1 protrusion of the cartilage begins, L2 - distinct protrusion (Adam's apple). V (voice) - changes in voice: V0 - child's voice, V1 - mutation of the voice (voice cracking), V3 - male timbre of voice. VI. PRELIMINARY DIAGNOSIS Curator must choose the complaints, information from history diseases, past history, pathological finding during physical examination and make preliminary diagnosis On the base of patient’s complaints (list them) __coughing,pain,_speech_problem,_fever,_pain_in_back,_weakness,headache chest pain _,abnormal sleep ,fatigue tension urination abnormal ____ on base of information from of history diseases (write them) _____after treating pneumonia it appeared again and become more severe and turns to form bronchitis .____________________________________________________________ on base of past history (write them) _past history of asthma ,living condition is not good .lives in polluted area , allergy with pollens which leads to pnemonia which further leads to acute bronchitis .________ On base of objective examination (list all abnormality symptom) _1) Distant heart sounds observed. 2) Diminished breath sounds. 3,) Hyperinflation. the preliminary BASIC DIAGNOSIS can be suspected A physical examination will often reveal decreased intensity of breath sounds, wheezing, rhonchi, and prolonged expiration. Most physicians rely on the presence of a persistent dry or wet cough as evidence of bronchitis. CONCOMINAT DIAGNOSIS CAN BE SUSPECTED A comcomitant can only br made the oxygen levels in your blood or by calculating yhe functional capacity of the lung via chest X rays and blood test preliminary so the patient had acute bronchitis. VII. PLAN OF ADDITIONAL INVESTIGATION Choose laboratory and instrumental methods of investigation, which are necessary for conformation of the clinical diagnosis, and those which are obvious for all patients: 1. Complete blood analysis, 2. General examination of urine, 3. Feces analysis on the helminthes eggs 4. Analysis on enterobiosis 14 Prescribes additional laboratory and instrumental investigations of different system corresponding to suspected diseases: Respiratory system: blood test for estimation immune system: IgE, IgA, IgM, IgG, T-, B- lymphosytes, X-ray investigation of lung, bronchoscope, functional respiratory test (spirography, pneumotachmeter, peak flow meter), analysis of sputum, analysis of pleural punctuate; consultation of ETN specialists, immunologist. Cardiovascular system: biocemical blood test (proteins, lipids, electrolyte balance, blood coagulation test, antistreptolysin- O titer ( ASO titer), C-reactive protein (high sensitivity), presence in blood LE-cells, immunologic examination, measurement of blood pressure, electrocardiography, phonocardiography, ultrasound examination of heart, doplerography, roengenography of chest and joints, contrast angiography, biopsy skin, synovial capsule of joints, rheumatoid nodules. Digestive system: stool test (coprogram), bacteriological investigation of feces, occult blood feces analysis, elastasa-1, test biochemical blood tests: blood analysis on liver function (bilirubun’s, protein’s changing, AlAt, AsAt; fibrinogen, protrombin; determination serum markers of hepatitis B and C; pancreas enzyme level blood test, glucose; determination urine amilasa level; presence a bile pigments in urine: pH meter, esophagogastroduodenoscopy with folloing determination H. Pylory, rectoromanoscopy, colonoscopy, irrigography, ultrasound diagnostic of liver, pancreas, gallblager, computer thomography, Urorenal system: renal function blood test (urea, creatinin, rest nitrogen); Nechyporenko urin test, Zimnytsky urine test, bacteriological investigation of urine, retrograde pyelography, ultrasound investigation of kidneys, urine bladder, contrast rengenography of kidneys, computer thomography, cystoscopy. Blood system: general blood analysis with counts of reticulosytis, determination of osmotic resistances of erytrosytes, determination of hematocryt, examination of blood coagulation, cloth retraction, counts trombosyts, prothrombin and heparin index, coagulogram, tromboelastogram, ultrasound investigation of liver and spleen, sternal punction, roentgengoraphy of bones, lymphatic nodes punctuation; consultation of hematologist. Endocrine system: hormones blood level concentration (for example hormones of thyroid glands); glucemic profile, examination of urine sugar content, 17ketorsteroid concentration, examination of basal metabolism, ultrasound investigation of thyroid gland, suprarenal gland, ovariec, roentgenography of skull, a skeleton, roentgenography of Turkish saddle; consultation of endocrinologist. Nervous system: electroencephalography, ultrasound investigation of brain, computer tomography, consultation of neurologist. Assessment of laboratory investigations The results of additional investigations (with interpretation): Clinical blood test (CBC) RBC__normal ______Hb__11 gram/dl 15 WBC increased Neutrophils: Rised band segm__ eos____increased __ lymph__________ mon______ESR: Rised PL __rised Conclusion _as it is seen from the blood test the amount of wbc and neutrophil is abnormal _,in her past history she had asthma due to which her immune system was not strong _,and also she had inflammation which lead to coughing for long days and lead to acute bronchitis. _____________________________ Clinical urine test Amount ___normal __Gravity ___normal_____Ph____acidic___Protein______no___Glucose ____no___ Ketones ___no_____Epithelium _pale yellow skin colour___________________ Leucocytes____raised___Erythrocytes_____normal___Casts______absent____ Crystals ___absent_______ Mucous ______absent ____Bacteria ______absent_________ Conclusion : Urine test corresponds to normal value . _ _Treatment : humidifier, breathing in steam, and drinking plenty of liquids like water or broth,eliminate irritants .. Amoxicillin is generally considered the first-line treatment for bronchitis Acetaminophen or ibuprofen for fever and mild pain. 16