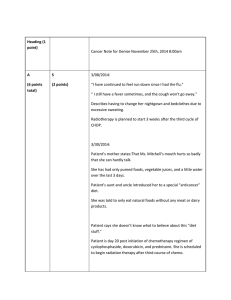
Lecturer: Abrar Alhebshi Name: Jack Nelson DOB: 22/7 (age 48) Physician: J. Phelps, MD ADMISSION DATABASE BED # 3 DATE: 9/22 TIME: TRIAGE STATUS (ER ONLY): □ Red □ Yellow □ Green □ White 0900 Initial Vital Signs TEMP: RESP: 37 ℃ HT: SAO2: 22 bpm WT (kg): B/P: PULSE: 180 cm 97.5 LAST TETANUS 120/80 LAST ATE 90 bpm LAST DRANK 1 year ago 11 PM this AM CHIEF COMPLAINT/HX OF PRESENT ILLNESS PRIMARY PERSON TO CONTACT: Name: Mary Nelson Home #: 555-444-5689 Work #: 555-453-5689 ORIENTATION TO UNIT: □ Call light □Television/telephone □ Bathroom □ Visiting □ Smoking □ Meals □ Patient rights/responsibilities “My wife insisted that I come see someo ne, The yesterday pain w a s sothat bad I was afraid I was having a PERSONAL ARTICLES: (Check if retained/describe) □ Contacts □ R □ L □ Dentures □ Upper □ Lower □ Jewelry: □ Other: eyeglasses NKA (no known allergies) VALUABLES ENVELOPE: no □ Valuables instructions “ heart attack ALLERGIES: Meds, Food, IVP Dye, Seafood: Type of Reaction INFORMATION OBTAINED FROM: □ Previous record □ Responsible party □ Patient □ Family PREVIOUS HOSPITALIZATIONS/SURGERIES S/p R knee arthroplasty 5 years ago Signature Home Medications (including OTC) Codes: A Sent home Dose Frequency Medication Aspirin 325 mg □ Yes Do you take all medications as prescribed? PATIENT/FAMILY HISTORY □ □ □ □ □ □ □ □ □ qd □ □ □ □ □ □ □ □ □ Cold in past two weeks Hay fever Emphysema/lung problems TB disease/positive TB skin test Cancer Stroke/past paralysis Heart attack (Father) Angina/chest pain Heart problems (Mother) □ No If yes, type: Frequency: Route: Date last used: / / this AM C C Not brought in Patient Understanding of Drug yes If no, why? High blood pressure Arthritis Claustrophobia Circulation problems Easy bleeding/bruising/anemia Sickle cell disease Liver disease/jaundice Thyroid disease Diabetes RISK SCREENING □ Yes □ No Have you had a blood transfusion? □ Yes □ No Do you smoke? If yes, how many pack(s)? 1/day for 18 years □ No Does anyone in your household smoke? □ Yes □ Do you drink alcohol? □ Yes No If yes, how often? How much? When was your last drink? □ No Do you take any recreational drugs? □ Yes Jack Nelson B Sent to pharmacy Time of Last Dose Code □ Kidney/urinary problems □ Gastric/abdominal pain/heartburn ( Patient) □ Hearing problems □ Glaucoma/eye problems □ Back pain □ Seizures □ Other FOR WOMEN Ages 12–52 Is there any chance you could be pregnant? If yes, expected date (EDC): Gravida/Para: ALL WOMEN Date of last Pap smear: Do you perform regular breast self-exams? ALL MEN Do you perform regular testicular exams? □ Yes □ No □ Yes □ No □ Yes □ No Lecturer: Abrar Alhebshi Client name: Jack Nelson, DOB: 7/22, Age: 48, Sex: Male, Education: Bachelor dgree Occupation: Retail manager of local department store Hours of work: M–F, works consistently in evenings and on weekends as well Household members: Wife age 42, 2 sons ages 10 and 16 all in good health Ethnic background: Caucasian, Referring physician: Patricia Phelps, MD (family practice) Patient history: Mr. Nelson has been experiencing increased dysphagia, heartburn, regurgitation, coughing with meals over last month, previously only at night but now almost constantly. Physical exam: General appearance: Obese 48-year-old white male in mild distress Heart: Regular rate and rhythm, heart sounds normal HEENT: Noncontributory Neurologic: Oriented x 4 Extremities: No edema; normal strength & sensations Skin: Warm, dry Chest/lungs: Clear Abdomen: No distention. BS normal Nutrition Hx: General: Patient relates that he has gained almost 16 kg since his knee surgery. He attributes this to a decrease in ability to run and has not found a consistent replacement for exercise. Patient states that he plays with his children on the weekends but that is the most exercise that he receives. He is worried about his family history of heart disease, which is why he takes an aspirin each day. He has not really followed any diet restrictions. Relates that his schedule has been increasingly busy so that he order pizza or stop for fast food 1–2 times per week instead of cooking. He states that he loves fatty food, soft drinks, lemon juice and fatty snacks such as chips, French fries, cookies and popcorn. However, pt. states that he has been experiencing difficulty eating & swallowing such snacks over the last month. Food allergies/intolerances/aversions: spicy & citrus foods seem to make the pain worse Previous nutrition therapy? no Food purchase/preparation: Wife or eats out Vitamin intake: none Dx: pt. Dx 3 days ago with GERD & mild dysphagia (level 3), pH monitoring and barium esophagram support diagnosis of gastroesophageal reflux disease with negative biopsy for H. pylori. Endoscopy indicates no ulcerations or lesions in the esophagus but mild esophageal dysphagia present with adequate chewing ability. Tx plan: 24-hour pH monitoring, decrease aspirin to 75 mg daily, Consult to dietitian. Lecturer: Abrar Alhebshi NAME: Jack Nelson AGE: 48 PHYSICIAN: P. Phelps, MD DOB: 7/22 SEX: M ****************************************CHEMISTRY***************************************** DAY: DATE: TIME: LOCATION: Admit 9/22 NORMAL Albumin Total protein Prealbumin Transferrin Sodium Potassium Chloride PO4 Magnesium Osmolality Total CO2 Glucose BUN Creatinine Uric acid Calcium Bilirubin Ammonia (NH3 ) ALT AST Alk phos CPK LDH CHOL HDL-C VLDL LDL LDL/HDL ratio Apo A Apo B TG T4 T3 HbA1C 3.5–5 6–8 16–35 250–380 (women) 215–365 (men) 136–145 3.5–5.5 95–105 2.3–4.7 1.8–3 285–295 23–30 70–110 8–18 0.6–1.2 2.8–8.8 (women) 4.0–9.0 (men) 9–11 0.3 9–33 4–36 0–35 30–120 30–135 (women) 55–170 (men) 208–378 120–199 55 (women) 45 (men) 7–32 130 3.22 (women) 3.55 (men) 101–199 (women) 94–178 (men) 60–126 (women) 63–133 (men) 35–135 (women) 40–160 (men) 4–12 75–98 3.9–5.2 UNITS 4.9 7.2 33 350 g/dL g/dL mg/dL mg/dL 144 4.5 102 3.8 2.0 278 28 110 9 0.7 mEq/L mEq/L mEq/L mg/dL mg/dL mmol/kg/H2 O mEq/L mg/dL mg/dL mg/dL mg/dL 9.1 0.8 30 22 156 100 300 220 H 45 130 mg/dL mg/dL mol/L U/L U/L U/L U/L U/L mg/dL mg/dL mg/dL mg/dL mg/dL mg/dL 178 H mg/dL mcg/dL mcg/dL % Lecturer: Abrar Alhebshi NAME: Jack Nelson AGE: 48 PHYSICIAN: P. Phelps, MD DOB: 7/22 SEX: M ****************************************HEMATOLOGY************************************** DAY: DATE: TIME: LOCATION: Admit 9/22 NORMAL WBC RBC HGB HCT MCV RETIC MCH MCHC RDW Plt Ct Diff TYPE ESR % GRANS % LYM SEGS BANDS LYMPHS MONOS EOS Ferritin ZPP Vitamin B12 Folate Total T cells T-helper cells T-suppressor cells PT 4.8–11.8 4.2–5.4 (women) 4.5–6.2 (men) 12–15 (women) 14–17 (men) 37–47 (women) 40–54 (men) 80–96 0.8–2.8 26–32 31.5–36 11.6–16.5 140–440 0–25 (women) 0–15 (men) 34.6–79.2 19.6–52.7 50–62 3–6 24–44 4–8 0.5–4 20–120 (women) 20–300 (men) 30–80 24.4–100 5–25 812–2,318 589–1,505 325–997 11–16 UNITS 5.6 5.2 103/mm3 106/mm3 14.0 g/dL 40 % 85 m3 % pg g/dL % 103/mm3 28 32 mm/hr % % % % % % % mg/mL mol/mol ng/dL g/dL mm3 mm3 mm3 sec Lecturer: Abrar Alhebshi Case Questions: Understanding the Disease and Pathophysiology Q: In the etiology of gastroesophageal reflux disease, what factors affect LES pressure? Factors that potentially affect LES pressure include the hormones gastrin, estrogen, and progesterone; the presence of abdominal fat or obesity, hiatal hernia; the presence of scleroderma, smoking, or some medications including NSAID; and nutritional factors. Foods high in fat, chocolate, spearmint, peppermint, alcohol, and caffeine have been noted to decrease LES pressure. Q: What risk factors (habits) do the patient present with that might contribute to his diagnosis? (Be sure to consider lifestyle, medical, and nutritional factors). Weight gain, high-fat diet, lack of physical activity, smoking, and the use of nonsteroidal anti-inflammatory drugs (aspirin) on a daily basis. NCP steps 1. Nutrition assessment (5 categories): Age, gender, smoker/or not, Dx, c/o (s/s) (medical Hx, surgeries), family Hx, medications a. Client History: 48 years old male, smoker, Dx with GERD 3 days ago, c/o (S/S) dysphagia level3, heartburn, regurgitation, coughing over last month, PMH of gastric pain, R knee Appetite, food intake, food quality, food supply, wt change, physical and activity, nutritional supplements arthroplasty 5 years ago, family Hx of heart attack heart problems. On Aspirin qd b. Food/Nutrition- Related History: Good appetite, high calories intake especially from fatty or fast food, no meal preparations, sedentary or light active lifestyle, weight gain in the last 5 years. recently, pt. has mild difficulty swallowing c. Anthropometric Measurements: Q. Assess this patient’s available anthropometric data. Does his BMI contribute to his diagnosis? BMI = 30, Mr. Nelson has Grade I obesity. Obesity has been correlated with GERD and is thought to increase intra-abdominal pressure. IBW= (Ht (cm) -150 )\2.5 x 2.7 + 48.2= 80.6 kg ABW= 0.25x(actual wt-Ideal wt)+Ideal wt = 84.8 ~ 85 kg Calculation of energy and nutrient requirements: Q. Calculate energy, macronutrient and fluid requirements for Mr. Nelson. Identify the formula/calculation method you used. Lecturer: Abrar Alhebshi Mifflin= (10XWt) + (6.25XHt) – (5 X Age) + 5 REE: (10X 84.8) + (6.25X180) – (5X48) + 5 =1738 kcal PA (1.3): 2259.4 kcal TEF10% of PA: 225.94 kcal TEE :2484.9 kcal =2500 kcal All macronutrients % should be converted to grams: CHO →50-60% , Fat→ 25 -35% , Protein→15% 1- Protein ( 15% ): 375 kcal = 93.75 g/day 2- Fat (25%): 625 kcal \9= 69.4 g/day 3- CHO(remaining calories): TEE- (kcal from protein + kcal from fat) = 1500 kcal/day (÷4)= 375 g/day or percentage of CHO (60%)= Fluids: 1 ml / 1kcal = 2500 kcal = 2500 ml d. Biochemical Data, Medical Tests, and Procedures Q. Are there any other abnormal labs that should be addressed to improve Mr. Nelson’s health? (please write the Reason for Abnormality) Abnormal Lab Indications (Reason for Abnormality/ Nutritional Implication) Lipid profile (↑ Chol. & Obesity BMI >30, dyslipidaemia, high saturated fat intake, he is at TG) high risk for heart disease e. Nutrition-Focused Physical Findings: Obese male in mild distress ****************************************************************************************** 2. Nutrition Diagnosis: Problem.....related to....Etiology......as evidenced by....S/S Q. Identify this patient nutrition problems and complete the PES statement (at least one statement). Intake domain: Excessive energy intake related to frequent consumption of fast foods (e.g. fried meals and popcorn) as evidenced by typical daily high calories intake compared to recommended intake of 2500 kcal and a BMI of 30, lab findings of chol and TG, wt gain Excessive fat intake and excessive saturated fat intake........ Recently: Inadequate oral intake related to difficulty swallowing as evidence by coughing with meals, regurgitation & patient diet history Clinical domain Obesity class 1 related to excessive energy intake and physical inactivity as evidenced by BMI of 30, abnormal lipid profile. Recently: Swallowing difficulty or dysphagia related to GERD as evidence by (S/S) coughing with meals, regurgitation & difficulty eating hard snacks over the last month Altered GI function....... Lecturer: Abrar Alhebshi Behavioural–environmental domain Food and nutrition-related knowledge deficit as evidenced by undesirable food choices Undesirable food choices related to knowledge deficit and busy schedule prompting frequent fast food consumption as evidenced by fried foods, cookies, and eating fast food 1–2 times per week Physical inactivity related to inability to find consistent replacement to previous physical activity of running following knee arthroplasty as evidenced by patient stating that he has little to no exercise, pt high BMI , obese ************************************************************************************* 3. Nutrition Intervention (4 categories): a. Food/ Nutrition Delivery, (Provide this patient with 1 day menu plan using exchange list) Q. For each of the PES statements that you have written, establish an ideal goal and an appropriate intervention. Goal: reach a more desirable BMI between 25 and 30 (or IBW), Modify meals and snacks to reduce GERD & dysphagia symptoms Intervention: (how much cal, type of diet , how many grams ) Provide 2500 kcal/day dysphagia advanced diet contains ....g proteins,....g CHO,.....g fat b. Nutrition Education & c. Counseling, (you have to explain in your own words) Q: Are there specific foods that may contribute to GERD? Summarize the current recommendations for nutrition therapy in this disease. Q: What food items should be allowed/avoided regarding Mr. Nelson swallowing ability? Give him an example of one meal menu. Q. What nutrition education should this patient receive prior to discharge? There has been very limited research that addresses how foods may contribute to GERD. The treatment goals include restricting foods that lower LES pressure. To reduce gastric acidity, black and red pepper, coffee (both caffeinated and decaffeinated), and alcohol are avoided, because all have been identified as stimulants for gastric acid production. Likewise, meals of larger quantity tend to produce more acid, delay gastric emptying, and increase the risk of reflux. Thus, smaller, more frequent meals may be indicated. Foods that lower LES pressure should also be restricted. These include chocolate, mint, and foods with a high fat content. Furthermore, any food the client identifies as irritating should be avoided. If the patient is obese, weight reduction should be a component of the plan for nutrition therapy. Regarding his dysphagia status, patient should avoid very hard, sticky, or crunchy items such as..... & foods allowed are most regular foods and tender, moist meats Q. Do any lifestyle issues need to be addressed with this patient? Explain. Q. What other components of lifestyle modification would you address in order to help in treating his disorder? Lecturer: Abrar Alhebshi Discussion about home meal preparation and reduce fatty food intake and smoking. Discussion of the role of smoking in GERD should be addressed. Referrals to assist with smoking cessation can be made within the health care team. The client should remain upright during and immediately after meals. Client should avoid eating or drinking anything for up to 3 hours prior to retiring in the evening. Client may also benefit from smaller meals prior to bedtime. The head of the client’s bed may also be elevated at night to assist with nighttime reflux ****************************************************************************** 4. Nutrition Monitoring and Evaluation: Q. What tools are necessary to follow up this patient? Food records, weekly measurements of weight, nutrient intake reports, resolution of vomiting episodes, swallowing progression.