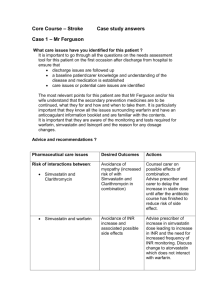
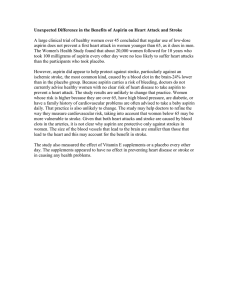
Dr Mere Kende MBBS, MMED (Path), MACTM, MACRRM, MACTM, MAACB Senior Lecturer/Head of Pathology, SMHS, UPNG Define thrombosis Factors promoting/preventing thrombosis Common Anti-thrombotic Drugs Newer anti-thrombotic Drugs Examples of Clinical conditions & use of antithrombotic drugs CLOT THAT FORMS inside vessels (vein or artery) Emboli (thromboembolus)- clot formed in one part of body and lodges in another organ (eg Heart to brain) occlusion of vessel lumina and obstruction of blood supply to distant tissues/organ--ISCHEMIA Factors: ▪ Platelets (ADP & secretions) ▪ Coagulation factors ▪ Damaged vessels (endothelium) ▪ Stasis (venous) Virchow’s Triad ▪ Blood Vessel Damage ▪ Clotting Factors/PLT disorders ▪ Blood Flow Impedance (stasis) Smoking Diabetes High BP High Cholesterol Lack of activity/obesity Poor Diet Family hx of thrombosis Major surgery /orthopaedic Bed-ridden patients Artificial Heart Valves Pregnancy Contains alpha and dense granules & lysosomes Express surface receptors; Gp1b, Gp1b + collagen & VWF---PLT adhesion Secrete PDGF, ADP, histamine, serotonin, betathrombomodulin, thromboxane A2 Injured endothelium- activated, →adheres, aggregates & secretes Thrombin, TXA2 and ADP increased PLT aggregation. Fibrin polymer- stabilises PLT plug Secretary Granules (ADP, serotonin, PAF, Ca++) Arachnidonic/Thromboxane A2 system Surface Receptors (GP IIb/IIIa) cAMP/phosphodiesterase system Thrombin/Fibrinogen linkages Metabolites of arachidonic acid metabolism Synthesis: TXA2 = PLT, PGI2= endothelium TAX2 –vasoconstrictor & PLT aggregator t1/2- 30 seconds PGI2- vasodilator, PLT inhibitor, t1/2- 2mins Normal balance maintained , normal PGI2 & NO activity > TXA2 Cholesterol Plugs Inflammation Smoking Hypertension Thrombi do not form in healthy vessel Normal endothelium prevents coagulation factors from contacting collagen Endothelium secrete anti-thrombotic molecules, eg ▪ ▪ ▪ ▪ Damaged endothelium – pro-thrombotic eg express vWF, ▪ ▪ ▪ ▪ ▪ thrombomodulin (binds ATIII, increase Protein C), plasminogen activators, prostacyclin, heparin-like molecules, & NO PAF, Tissue factor, Plasminogen activator inhibitors, fibronectin & exposes collagen Endothelium maintains balance between anti & pro-coagulant activities Carotid Artery Stenosis STROKE or TIA ▪ Sudden onset of a neurologic deficit ▪ consistent with unilateral cortical ischemia; ▪ weakness & numbness of an extremity, aphasia, dysarthria, or unilateral blindness (amaurosis fugax). ▪ Bruit heard loudest in the mid neck. Aorta Occlusive Disease: ▪ Cramping; pain or tiredness in the calf, leg, or hip while walking (CLAUDICATION). ▪ Diminished femoral pulses. ▪ Tissue loss (ulceration, gangrene) unusual ▪ Cramping; pain or tiredness in the calf only with exercise. (CLAUDICATION) ▪ Reduced popliteal or pedal pulses. ▪ Foot pain at rest, relieved by dependency. ▪ Foot gangrene or ulceration. ▪ Rest pain of the forefoot relieved by dependency ▪ Pain or numbness of the foot with walking. ▪ Ulceration or gangrene of the foot or toes. ▪ Pallor when the foot is elevated. Six P’s — The six P's of acute ischemia include paresthesia, pain, pallor, pulselessness, poikilothermia, and paralysis. The majority of arterial emboli that travel to the extremities originate in the heart, Lower extremities affected more frequently than the upper extremities [6]. Risk factors: ▪ ▪ ▪ ▪ ▪ AF LVF Post-MI Prosthesis Valvular HD Femoral – 28 percent Arm – 20 percent Aortoiliac – 18 percent Popliteal – 17 percent Visceral and other – 9 percent each From: www.uptodate.com ▪ Severe postprandial abdominal pain. ▪ Weight loss with a "fear of eating." Health vessels Healthy Platelet/ Prevent aggregation/activation/secretion/block receptor Block PLT derived chemicals Prevent clotting factors activation Commonly used ▪ Aspirin ▪ Dipyridamole (asasantin) ▪ Clopidogrel (plavix) & ticlopidine Prevention ▪ ▪ ▪ ▪ ▪ ▪ IHD Stroke Heart Valves/Prosthesis AF DVT Thromboembolic Disorders Treatment ▪ Heart Attack ▪ DVT • Aspirin (disprin/aspro) • Indomethacin (indocid) • Ibuprofen (neurofen) • Diclofenac (voltaren) • Piroxicam • Meloxicam • naproxem Inhibition due to Acetylation of PLT COX enzyme in splanchnic circulation Thromboxane A2 (blocks PLT aggregation) Decrease Prostaglandins-anti-inflammatory & analgesic Rapidly destroyed pre-systemically, hence endothelia or systemic COX not affected Oral anti-coagulant dose: 100mg -300mg/day Widely used, cheaper Evidence -very strong in prevention of all vascular events Clopidogrel (plavix): Inhibits ADP receptor on Platelet (blocks activation & aggregation) Dipyridamole: inhibits phosphodiesterase increasing cAMP messenger system (blocks aggregation, granule secretion, dilates coronary vs) Oral tablets Benefit improves when combined with aspirin (asantatin/persantine Clopidogrel still expensive, used with aspirin or if ASA contraindicated 1. Coumarin (warfarin) derivatives via inhibition of activated II, VII, IX, X 2. Heparin and anti-thrombin III complex 3. Protein C and S 4. Ca++ Chelators (Citrate/EDTA/oxalates) Can not be used therapeutically Oral anticoagulant Structurally related to vit K, 4-hydroxycoumarin Prevent formation of active vitamin K from vitamin K epoxide, hence formation of vitamin K-dependent CF (II, IIV, IX, X) Well absorbed via GIT Duration of action: varies considerably Inative (Vitamin K quinol) Active (Vitamin K epoxide) Patient Factors ▪ Age, co-existing illnesses, alcohol, weight changes Drug Interactions ▪ Other anti-thrombotic drugs ▪ Ant-epileptics (enzyme induction) ▪ Antibiotics (enzyme induction) Bleeding Prothrombin Time (PT) INR: ▪ >5-9 risk of spontaneous bleeding, ▪ give vitamin K ▪ >9-Admit for FFP/fresh whole blood or PT concentrate Adjust dosage (1mg-10mg/day) with INR monitoring Vitamin K (phytomenadione) Paediaric (KONAKION) Injection: 2mg/0.2mls Adult (KONAKION) Injection 10mg/ml Tablet 10mg tab Chlorophylous Plants Gut Bacteria Synthetic Present in mast cells Therapeutically: originate from porcine gut or bovine lung Contain –COO- and -SO4 groups MW 20,000 Potency varies with length but standardised in IU numerous negative charged, not absorbed well in GUT/skin Complexes with anti-thrombin III for action Magnifies anti-thrombin III effect 1000x Thrombo-prophylaxis dose: 5000iu tds Treatment Dose: Require higher doses BLEEDING, Low platelet (thrombocytopenia) Osteoporosis, Reversible alopecia aPTT (Factors II, VII, IX, X) Platelet (FBE) Protamine –SO4 (salmon sperm) ▪ injection 1% or 1og/L (5mls) ▪ 1mg neutralises 100IU heparin ▪ Effect immediately reversed Enoxaparin (clexane) Dalteparin, tinzaparin, reviparin, certoparin Longer duration of action Given once daily dose (20,40,60,100,120, 150mg/ml pre-filled syringes Can be administered by patients at home No need for admission eg DVT treatment Regular APTT/platelet monitoring NOT required More reliable dose response relationship Side effect less common Expensive Reversal of bleeding a problem (xa) Low Molecular Weight heparin Unfractionated heparin (20,000 Da) Low Molecular weight heparin (5,000 Da) Action Mostly factor Xa Route of Administration IIa, VIIa, Ixa, XIa, XIIa, Anti-thrombin III SC or IV Absorption from subcut. Route Slow Improved Protein binding Bioavailability (SC) Binds plasma protein 10-30% (low dose) – >90% (higher dose) Less binding >90% Effective half-life Individuals variation Monitoring Elimination Route SC 1.5hr, IV-30mins Extensive APTT Liver & kidneys SC, 4hrs Minimal NOT REQUIRED (anti-Xa) Kidneys SC Newer Drugs ▪ Abciximab ▪ Fibatide ▪ Tirofiban Inhibits GPIIIb/IIa receptor (PLT ) prevent fibrinogen binding & PLT aggregation Not widely available or used abcixmiab is injection only used in ICU/ED Evidence of use not as strong as aspirin Still very expensive Dabigatran (pradaxa)- used in AF to prevent stroke prevention Orally (released 2010) Rivaroxaban (Xarelto) Oral anticoagulant Once daily dose Released 2011 Prevention of DVT patients undergoing knee and hip replacement Also developed for stroke prevention Treatment Arterial Thrombosis ▪ ▪ ▪ ▪ AMI Stroke PE Peripheral arterial thrombosis (limb/GIT/Resp) Venous thrombosis: DVT Anti-inflammatory (ASA) Prophylaxis: ACS Stroke/TIA PE/DVT AF Peripheral Arterial Disease Randomised controlled trials have shown the benefit of warfarin and to a lesser extend aspirin in reducing the incidence of stroke in patients with AF without greatly increasing the risk of hemorrhagic stroke and extracranial hemorrhagic. However, anticoagulant is still under prescribed in patients with AF, particularly in elderly patients ( >75), who stand to benefit most. AF > 48hrs -give warfarin 3 wks before then continue for 4weeks after CV If urgent CV –give heparin then warfarin Give aspirin or clopidogrel CVA 3rd leading cause of death in Western World Incidence~ 1-2:1,000/yr Uncommon <40yrs, increases 10:1000 in >75yrs CVA 85% ischaemic vs 15% hemorrhage (see diagram below) Anti-platelet Therapy ▪ Aspirin ▪ Clopidogrel (plavix/iscover) ▪ Ticlopidine ▪ Dipyridamole (persantin) ▪ Asasantin SR (aspirin/dipyridamole) well evaluated drug with benefit (IST/CAST*) Dosage (160-300mg/day) Start within 48hrs of ischaemic stroke Prevents 10 deaths for every 1000 strokes treated Benefits shown irrespective of age, AF, BP, subtypes or CT findings Should be started even if CT is not available Long term Low dose (100mg/day) Rx protects stroke *IST-ischaemic stroke trial & CAST-Chinese Acute Stroke trial ▪ Enoxaparin (clexane) –synthetic, long acting ▪ Not routinely recommended ▪ Risk: benefit ratio narrow, ill-defined, & depend of pathophysiology and subtypes ▪ Only low dose 5,000u/day with aspirin has shown benefit in cases with profound leg weakness to prevent DVT Streptokinase- not approved ▪ ?benefit huge thrombus in large arteries (carotids) rTPA (recombinant) ▪ Benefit if administered within 3hrs of onset ▪ Risk: benefit low; increased Risk of bleeding ▪ Need CT within 3hrs; no practical Aspirin 160-300mg/day ▪ Most studied ▪ Least expensive ▪ Most effective with combined therapy (see below) Clopidogrel 75mg/day /Tioclopidine ▪ More effective than aspirin ▪ Similar side effects ▪ Expensive, not widely available Dipyridamole SR 200mg daily or early release q6h Dipyridamole & Clopidogrel ▪ Benefit greater if combined with aspirin ▪ Use if aspirin is contraindicated ▪ Expensive (clopidogrel) Benefits of preventive therapy only demonstrated in preventing emboli secondary to heart disorders eg AF/prosthetic valves Not recommened for brain ischaemia secondary non-cardiogenic cause until further research data Very high risk of thromboembolism Warfarin treatment advised Aspirin/dipyridamole only in selected patienst Keep INR much higher 2.5-3 Intensity of treatment depends on age, other risk factors, types of valve lesions, etc 1st generation prosthetic valves have higher risk of thromboembolism than newer types Any valve disease with AF requires anticoagulant prophylaxis (warfarin) Treatment usually guided by echo/TOE findings eg type valve lesion, presence of thrombus, heart failure, age of patient, and co-existing risk factors Aspirin alone if warfarin not possible Keep INR 2.5-3 Treatment is life long Minor sugery (dental procedures/skin biopsy/endoscopic biopsy) ▪ Stop warfarin for 1-3 days ▪ Ensure INR 1.5-2.0 before surgery ▪ Heparin not needed ▪ Resumption possible on the same day High risk of bleeding Discontinue warfarin 4-5 days Keep INR down to 1.0 Risk of thrombosis start heparin to prolong aPTT to ~2x control and then to normal during operation Start heparin /warfarin as soon as possible after operation Warfarin contraindicated especially in 1st trimester and before delivery Unfractionated heparin-choice Newer low molecular heparin does not cross placenta may be used but limited data Acute AMI – within 4 hours of pain - thrombolysis for STEMI and no contra-indications Start aspirin and clopidogrel early, continue long term Heparin use after rTPA use Warfarin only when AF /severe HF Aspirin and clopidogrel used long term Dipyridamole combined with aspirin or if allergic to aspirin Over anti-coagulation Assessed prior to commencing treatment Avoid unless benefit> risk of complications Ensure adequate instruction/follow-up Anti-dote available Age>75 Co-existing organ disease Non-compliance Distance from clinic Use with other anti-thrombolytics PUD Severe hypertension (systolic>180) PT/INR (warfarin) APTT (heparin) Platelets (heparin) ISI Patient’s PT Mean Normal Time INR= ISI= International sensitivity ratio. Mean normal PT is generated from samples from local healthy subjects or commercially available standard. The exact value of ISI dependents on the thromboplastin used in the PT method. Vitamin K Protamine SO4 Transfusion/FFP YH, Lip & AD Blann; ABC of AntiThrombolytic Therapy, BMJ 2003 Current Medical Diagnosis & Treatment 2008 Lullmann, Color Atlas of Pharmacology 2000 , 2nd Edition https://sites.google.com/site/generalpathologylecturenotes/