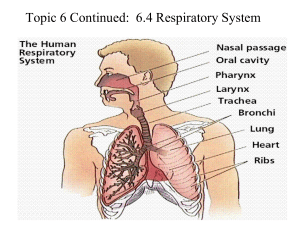
NNPD1013 & NNBB1234: PULMONARY VENTILATION dr farah fauzi | fakulti sains kesihatan 1 Objectives • Overview of respiration • Stages of respiration: pulmonary ventilation • Control of pulmonary ventilation • Factors affecting ventilation 2 The Goal of Respiration The ultimate mission of the respiratory system to make oxygen available to body tissues for cell metabolism. This mission is carried out in several stages of respiration. 5 Stages of Respiration A. External Respiration (ventilation & gas exchange) 6 B. Gas Transport C. Internal Respiration Stages of Respiration 1, 2 1 2 3 4 3 4 7 Cellular Respiration 10 Pulmonary Ventilation Gas Exchange Gas Transport Internal Respiration Pulmonary Ventilation 11 Pulmonary Ventilation Ventilation refers to the flow of air in and out of the lungs (alveoli). This process can be categorised into minute ventilation and alveolar ventilation. 12 Pulmonary Ventilation Minute ventilation = the amount of air entering lungs per minute Alveolar ventilation = the amount of gas that reaches the alveoli and takes part in gas exchange 13 Pulmonary Ventilation Lungs Alveoli 14 Pulmonary Ventilation Inhalation brings in air into the lungs, inflating the alveoli. Exhalation drives air out of the lungs and deflating the alveoli. O2 CO2 15 Pulmonary Ventilation Unlike the heart, the lungs are not innervated with nerves. The inflation and deflation of the lungs during breathing depends solely on movement of respiratory muscles, i.e. diaphragm and intercostal muscles and special characteristics of the lung tissue. 16 Respiratory Muscles § Diaphragm § External intercostal muscles 17 Diaphragm • Innervated by phrenic nerve. • Contracts (inhalation) à descends and flattens. § increasing the vertical volume of thoracic cavity • Relaxes (exhalation) à dome-shaped § decreases the volume of thoracic cavity 18 Ext. Intercostal muscles • Muscles between the ribs. • Innervated by intercostal nerve. • Contraction (inhalation) à elevates the ribs upward and outward § increases thoracic volume • Relaxation (exhalation) à depresses the ribs § decreases thoracic volume 19 Respiratory Muscles The cycle of contraction and relaxation of the diaphragm and intercostals muscles cause the volume of thoracic cavity to change. Changes in the thoracic volume create different pressures in the lungs (intrapulmonary pressure) that ultimately result in inhalation and exhalation. 20 Physics of Gas and Volume 21 Respiratory Muscles • Contraction of respiratory muscles à thoracic volume ▲, P▼ • Relaxation of respiratory muscles à thoracic volume ▼, P▲ 22 Physics of Air Flow 23 Pressure Differences The pressure differences between atmosphere and intrapulmonary drives air flow. 760 mmHg 760 mmHg contraction 757 mmHg INHALATION 24 relaxation 763 mmHg EXHALATION The Balloon Lung Model The lungs are just a pair of air bags. They expand as a result of air flowing in, and not the other way round! 25 Control of Ventilation 26 Although we can consciously control our breathing, most of the time we do not, especially during sleep. So, what controls our breathing ? 27 Control of Ventilation Ventilation is controlled at two levels: § Involuntary (brain stem; respiratory centers) § Voluntary (cerebral cortex) 28 Control of Ventilation The respiratory centers are located in the: § medulla oblongata (medullary respiratory center) § pons (pontine respiratory center) 29 Medullary respiratory group The respiratory centers in the medulla oblongata are two group of neurons; the dorsal group (DRG) and ventral group (VRG). The DRG is involved in generating a normal breathing rhythm (eupnea), while the VRG is mostly involved in forced breathing. Both DRG and VRG innervates the respiratory muscles. DRG VRG 30 DRG and VRG innervations 31 Medullary Respiratory Center • DRG generate impulse to begin inhalation. • Signals sent to respiratory muscles via efferent nerves to stimulate contraction. • Diaphragm: phrenic nerve • Intercostal muscles: intercostal nerve 34 Control of Eupnea Inspiratory neurons depolarise (‘on’) Inspiratory neurons repolarise (‘off’) Impulse sent to diaphragm and intercostal muscles Impulse ceases Contraction of respiratory muscles Relaxation of respiratory muscles INHALATION EXHALATION 35 Pontine Respiratory Group The pneumotaxic centre and apneustic centre of the PRG modifies the output of the MRC. Not essential for basic rhythm of breathing, but important in fine-tuning breathing rhythm during singing, talking, exercising, laughing, etc 36 Pontine Respiratory Group Pneumotaxic center - tachypnea Apneustic center - apnea 37 Voluntary Control of Breathing • Motor cortex of the frontal lobe. • Breath-holding, smelling, meditation. • Signals are relayed down from the motor cortex directly to the phrenic and intercostal nerves, bypassing the respiratory centers. • Respiratory centers can override the voluntary control if levels of blood gases are compromised. 38 Factors Affecting Ventilation 39 Factors Affecting Ventilation Factors that can affect airflow in and out of lungs: § § § § 40 Resistance in airway Lung compliance Pulmonary surfactant Elastic recoil Airway resistance Any condition that narrows or obstruct the airways, making it difficult for air to flow in and out of the lungs: § asthma § emphysema § bronchitis asthma emphysema 41 Lung compliance The ability of lungs to expand easily when we inhale. Low lung compliance will need more effort to inhale. Decreased compliance can be seen in: § scarring of lung tissue (TB, asbestosis) § lack of pulmonary surfactant 42 Pulmonary surfactant Pulmonary surfactant is an ‘oily’ coating inside the alveoli to help loosen water surface tension in the alveoli. Surfactant is made up of secretions rich in lipids and proteins, secreted by type II pneumocytes. surfactant alveolar fluid alveolar air 44 Alveoli are moist. During exhalation alveoli deflate and can become ‘sticky’, making it hard to re-expand.. Having pulmonary surfactant solves this ‘stickiness’ problem! 45 Pulmonary surfactant • reduce surface tension • prevent alveoli collapse during exhalation • bind to pathogens, debris • prevent excessive moisture in the alveoli Helps to maintain lung compliance by allowing the lungs to expand easily after exhalation 46 PULMONARY SURFACTANT INSUFFICIENCY Newborn respiratory distress syndrome or “blue baby” is common in premature infants (<35 wk), due to insufficient surfactant production. 47 Elastic recoil Alveoli contain elastic fibers enabling them to stretch during inhalation and recoil during exhalation. Elastic recoil gives lungs the passive ability to deflate easily during exhalation. 48 Elastic recoil If elastic recoil is compromised, exhalation will be DIFFICULT 49 Loss of Recoil in Emphysema • Alveoli damage à loss of elastic fibers. • Loss of elastic recoil à air trapped in alveoli. • Less air is exhaled out, less fresh air can enter lungs. • Causing low O2 levels in the blood 50 Summary The act of breathing highly depends on the coordinated actions of the respiratory centers and muscles to generate pressure differences in the lungs and hence, create air flow. Apart from damaged lung structures, breathing process can also be compromised by diseases affecting respiratory nerves and muscles. 56