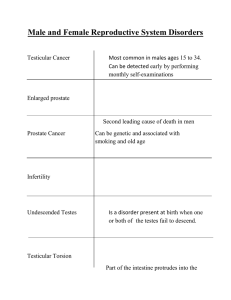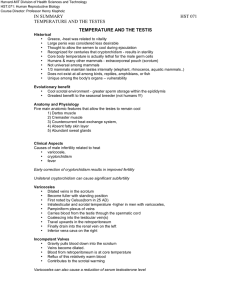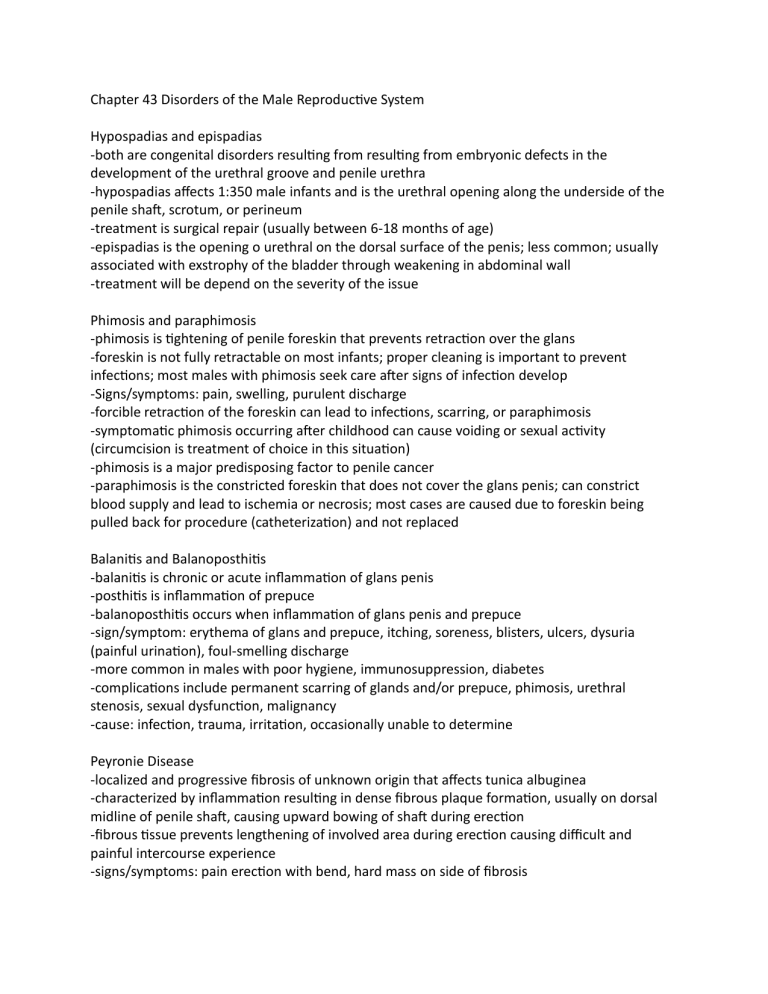
Chapter 43 Disorders of the Male Reproductive System Hypospadias and epispadias -both are congenital disorders resulting from resulting from embryonic defects in the development of the urethral groove and penile urethra -hypospadias affects 1:350 male infants and is the urethral opening along the underside of the penile shaft, scrotum, or perineum -treatment is surgical repair (usually between 6-18 months of age) -epispadias is the opening o urethral on the dorsal surface of the penis; less common; usually associated with exstrophy of the bladder through weakening in abdominal wall -treatment will be depend on the severity of the issue Phimosis and paraphimosis -phimosis is tightening of penile foreskin that prevents retraction over the glans -foreskin is not fully retractable on most infants; proper cleaning is important to prevent infections; most males with phimosis seek care after signs of infection develop -Signs/symptoms: pain, swelling, purulent discharge -forcible retraction of the foreskin can lead to infections, scarring, or paraphimosis -symptomatic phimosis occurring after childhood can cause voiding or sexual activity (circumcision is treatment of choice in this situation) -phimosis is a major predisposing factor to penile cancer -paraphimosis is the constricted foreskin that does not cover the glans penis; can constrict blood supply and lead to ischemia or necrosis; most cases are caused due to foreskin being pulled back for procedure (catheterization) and not replaced Balanitis and Balanoposthitis -balanitis is chronic or acute inflammation of glans penis -posthitis is inflammation of prepuce -balanoposthitis occurs when inflammation of glans penis and prepuce -sign/symptom: erythema of glans and prepuce, itching, soreness, blisters, ulcers, dysuria (painful urination), foul-smelling discharge -more common in males with poor hygiene, immunosuppression, diabetes -complications include permanent scarring of glands and/or prepuce, phimosis, urethral stenosis, sexual dysfunction, malignancy -cause: infection, trauma, irritation, occasionally unable to determine Peyronie Disease -localized and progressive fibrosis of unknown origin that affects tunica albuginea -characterized by inflammation resulting in dense fibrous plaque formation, usually on dorsal midline of penile shaft, causing upward bowing of shaft during erection -fibrous tissue prevents lengthening of involved area during erection causing difficult and painful intercourse experience -signs/symptoms: pain erection with bend, hard mass on side of fibrosis -diagnosis is based on history, physical exam, doppler US may be used to assess cause -treatment: surgical intervention or may possibly have spontaneous resolution Erectile Dysfunction (ED) An erection is a neurovascular process of many steps: erection itself is under control of parasympathetic nervous system and ejaculation occurs under control of sympathetic nervous system. -ED is the persistent inability to achieve and maintain an erection sufficient to permit intercourse -cause: physical (blood flow to and from the penis), psychogenic (depression, anxiety), or organic (neurogenic, hormonal, vascular, drug induced, penile related issues), common in males with diabetes -diagnosis: history, including medication/drug use, physical exam, lab tests to rule out organic causes -treatment: depends on cause but could include medication, psychosexual therapy, vacuum constriction devices, surgical treatment Priapism -involuntary erection lasting longer than 4 hours -true urologic emergency because prolonged erection causes ischemia and fibrosis of erectile tissue -2 subtypes: a. ischemic (low flow, veno-occlusive): severe pain and medical emergency as little to no cavernous blood flow present b. nonischemic (high flow, arterial): penis is not fully rigid or painful, caused by unregulated arterial inflow -potential causes: sickle cell or neoplasm for children ages 5-10, medications, sickle cell in adults, leukemia, stroke -diagnosis: based on clinical findings, doppler studies of penile blood flow -treatment: analgesics, sedation, hydration, ice packs, possible aspiration/irrigation of corpus cavernosum Penile cancer -squamous cell cancer of penis, average age at diagnosis is 60yrs, if diagnosed early, very curable -more common in uncircumcised males -risk factors: age, poor hygiene, smoking, STI infection (HPV types 16 and 18), UV radiation exposure (for psoriasis); cause is unknown -Signs/symptoms: small lump or ulceration, if phimosis is present, may also exhibit painful swelling, purulent drainage, difficulty with urination, palpable inguinal lymph nodes -diagnosis: physical exam and biopsy, US, CT and MRI may also be used -treatment: depends on size, stage, location and invasiveness; surgery for invasive cancer (penectomy with lymph node removal), local resection of superficial lesions Cryptorchidism -undescended testes (one or both testicles fail to move down into scrotal sac) -testes may remain in lower abdomen, at point of descent in the inguinal canal, or upper scrotum due to histological abnormalities: delay in germ cell development, changes in spermatic tubules or deduced Leydig cells. (These changes become progressive if the testes remain undescended) -most common congenital disorder of GU system affecting males, with higher number seen in premature births -Primary (one or both fail to descend at birth) and Secondary (testes was in scrotum, but pulled back into suprascrotal position after surgical procedure (hernia repair) -Can lead to infertility, increased risk for testicular cancer, and testicular torsion -Treatment: surgical intervention to place testes in scrotal sac Disorders of scrotum and testes (Fig 43-6, pg 1104 and fig 43-7, pg 1105) a. Hydrocele: collection of fluid in scrotum without obvious inguinal hernia; congenital hydrocele can be seen shortly after birth and usually resolves within first 2 year of life; acute hydrocele in children and adults may develop after local injury, testicular torsion, epididymitis or orchitis, STD or testicular cancer. Treatment may include surgical drainage, or removal of cause. Chronic hydrocele usually does not require treatment unless mobility is affected. b. Hematocele: accumulation of blood between the parietal and visceral tunica vaginalis; often associated with a hydrocele; scrotal skin appears purple or dark red; may be seen after abdominal surgery, scrotal trauma, bleeding disorder or testicular tumor. c. Spermatocele: painless, sperm-containing cyst that forms at end of epididymis; can be singular or multiple; if enlarges and causes pain, surgical removal may be necessary d. Varicocele: varicosity of veins supplying blood from testes due to incompetent valves and reflux into pampiniform plexus veins; rarely seen before puberty; signs/symptoms include heaviness in left scrotal area, feeling of “bag of worms” on scrotal palpation in standing position; treatment: surgical ligation or sclerosis (to improve fertility, relief of heaviness sensation or cosmetic) e. Testicular torsion: twisting of spermatic cord and loss of blood supply to ipsilateral testicle; MEDICAL EMERGECC;; early diagnosis and treatment are imperative for testicle preservation and fertility; commonly seen in adolescents (possibly due to increasing weight of testicle after puberty and contraction of cremaster muscles); Signs/symptoms: severe pain, tachycardia, nausea and vomiting; Treatment: surgical repair within 6 hours of torsion Epididymitis -acute (< 6 weeks) or chronic (> 6 weeks) inflammation of epididymis -cause/risk factors: infectious (bacterial, UTI, STIs, enterovirus or adenovirus), noninfectious (trauma, surgery (ie vascectomy), medications), postinfectious -signs/symptoms: gradual onset of posterior testicular pain, swelling, inflammation and radiation to lower abdomen -Diagnosis: physical exam; elevated serum white blood cells, UA/culture with bacteriuria and pyuria; doppler US may show increased blood flow affected testes -Treatment: CSAIDS (for inflammation), bedrest, scrotal elevation and support (ie folded washcloth under scrotum), observation for fever/systemic infection, treat cause (antibiotics, antivirals, antifungals, etc) Orchitis -acute inflammation of testes secondary to infection (majority d/t viral mumps infection) -primary infection may be in GU tract (cystitis, urethritis, prostatitis) and travel to epididymis / testes through vas deferens or lymphatics; may be caused by STI -signs/symptoms: enlarged testis, tenderness, scrotal skin erythema, edema, induration of scrotum -Diagnosis: physical exam, UA/culture, urethral culture if STI suspected -Treatment: supportive treatment (bedrest, scrotal elevation, heat or cold therapy), treat infectious cause -spermatogenesis is irreversibly impaired in 30% of testes damaged by mumps orchitis Ceoplasms: a. Scrotal cancer -benign scrotal tumors are common and often do not require treatment -scrotal carcinoma is rare -linked to exposure to tar, soot, oils; scrotal squamous cell carcinomas are linked to poor hygiene, chronic inflammation, HPV and exposure to photochemotherapy -signs/symptoms: small tumor or wart like growth that eventually ulcerates; high likelihood of metastasis to lymph nodes -treatment: surgical removal as does not respond well to chemo or irradiation b. Testicular cancer -most common cancer in males between 15-35 -90% of tumors are germ cell tumors -Seminoma (thought to arise from seminiferous epithelium of testes, most likely to produce uniform population of cells) and nonseminoma (embryonal carcinoma, teratroma, choriocarcinoma, and yoke cell carcinoma derivitives) -cause: unknown; but risk factors: cryptorchidism, genetics, disorders of testicular development -sign/symptoms: slight enlargement of testicle with general aching/heaviness to lower abdomen or groin (can metastasize before tumor is barely palpable) -diagnosis: thorough urologic history and physical exam, US, CT and MRI, tumor markers (alpha fetoprotein, beta HCG) -Stages of tumor-node-metastasis (TCM): a. Stage I: tumor confined to testes, epididymis, or spermatic cord b. Stage II: tumor spread to retroperitoneal lymph nodes below diaphragm c. Stage III: metastases outside of retroperitoneal nodes above diaphragm -treatment: orchiectomy, chemo or irradiation may be necessary if mets present -potential side effects of treatment: retrograde ejaculation, failure to ejaculate, infertility (sperm bank recommended prior to beginning of treatment) Prostatitis -inflammatory disorder of prostate gland (may be spontaneous (post catheterization) or secondary to diseases of GU system a. Acute bacterial: a. Caused by ascending urethral infections or intraprostatic reflux (BPH, STI, GU infection, immunocompromised b. s/s: pelvic pain, urinary symptoms (urgency, dysuria, retention), systemic symptoms (fever, chills, nausea, emesis, malaise), painful ejaculation, hematospermia, painful defecation, cloudy, malodorous urine c. diagnosis: DRE, thick discharge upon prostatic massage d. Treatment: treat symptoms and antibiotics if necessary b. Chronic bacterial: a. More difficult to treat as it is caused by E Coli or other gm neg Enterobacteriaceae. b. s/s: possible history of acute bacterial prostatitis, relapsing UTIs, irritative or obstructive urologic symptoms, some may be asymptomatic. c. diagnosis: UA, positive leukocytosis and bacterial culture of prostatic fluid d. treatment: long term antibiotic treatment or transurethral resection of prostate (TURP) c. Inflammatory: a. Cause: unknown b. s/s: pain along penis, testicles and scrotum; painful ejaculation, low back pain, rectal pain, decreased libido or ED c. diagnosis: DRE, elevated leukocyte count and abnormal inflammatory cells in prostatic fluid d. treatment: symptom control (sitz bath, CSAIDS, medication for irritative urinary symptoms); if UA normal: DRE with prostate massage -> if inflammation presentpatient prescribe abx and instructions to ejaculate every 3 days d. Coninflammatory: a. Cause: unknown (possible bladder neck obstruction causing reflux) b. s/s and diagnosis: same as inflammatory c. treatment: symptom control (sitz bath, CSAIDS, medication for irritative urinary symptoms); if UA normal: DRE with prostate massage -> if inflammation does not present just instructions to ejaculate every 3 days (no abx) Benign Prostatic Hyperplasia (BPH) -prostate gland is enlarged but not cancerous -2 growth periods: early puberty (doubles in size) and around age 25 (gland growth may impinge urethra and obstruct flow) -characterized by formation of large, discreet lesions in periurethral region of prostate (Fig 43-8, pg 1109) -Cause: not well understood; risk factors include: over age 40, family hx of BPH, obesity, cardiovascular disease, type 2 DM, lack of physical exercise, ED; higher estrogen levels in males who had testicles removed before puberty or elevated DHT levels causing continued growth of prostate gland -s/s: increased prostate size, weak urinary stream, postvoid dribbling, urinary frequency, nocturia, pain after ejaculation or urination, urinary incontinence -diagnosis: patient experience (interview), physical exam with DRE, UA, serum PSA, US, cystoscopy -treatment: lifestyle changes (reducing fluid intake at night, avoid/reduce caffeine/alcohol intake, avoid antihistamine/decongestants/diuretics/antidepressants, bladder training, pelvic floor muscle exercises, prevent/treat constipation), medication, minimally invasive procedures or surgery (TURP) -complications: ED, incontinence, bladder neck contractures Prostate Cancer -most common nonskin cancer in US; disease of aging -development is a multistep process involving genes that control cell differentiation and growth -Primary adenocarcinomas are commonly multicentric and located in peripheral zones of prostate; Mets to lung reflects lymphatic spread through the thoracic duct and dissemination from prostatic venous plexus; Mets to bone usually found in vertebral column, ribs and pelvis -risk factors: age, race, heredity (increased risk with first and second degree relative), male hormone levels and environmental factors (high fat diet, processed meat/cheeses) -s/s: early stage asymptomatic; when symptoms occur-likely due to locally advanced (urgency, frequency, nocturia, hesitancy, dysuria, hematuria, blood on ejaculate) or metastatic disease -> bone (low back pain, pathologic fracture) or weight loss, anemia, SOB -Diagnosis: serum PSA, DRE, transrectal US -Treatment: surgery radiation, hormonal manipulation, chemo has limited effectiveness