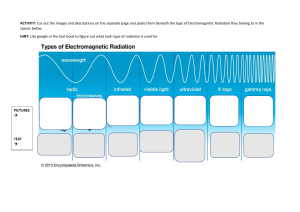
lOMoARcPSD|16207318 2 Oncology - Nursing notes bs nursing (Southwestern University PHINMA) StuDocu is not sponsored or endorsed by any college or university Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 Notes of Zairra Oncology • Risk Factor increase the odds of developing cancer Theories on Cancer: Misused Overused Unused Terms: ·Cancer Number 1 Killer Have 1 nucleus (generally) Except osteoclast (many nuclei) Neoplastic Disorder Undergo mitosis ·Neoplasm Have APOPTOSIS new tissue growth Cell could detect abnormal DNA or ·Mitosis chromosomes --> cell can commit suicide Have CONTACT INHIBITION cell division Cells stop replicating at a specific rate ·Metastasis if the quantity is too much to avoid spread of cancer cells in the body overpopulation Uncontrolled proliferation of cancer With function Characteristics of Cancerous Cells cells Cancer cells continue to grow and divide ·Benign Variations in size and shapes of cells (-oma) Nucleus that is larger and darker than Example: Adenoma normal Maturation of normal cells --> small nucleus • Malignant Abnormal number of chromosomes (-carcinoma) arranged in a disorganized fashion Cluster of cells without a boundary Example: Adenocarcinoma • Stable cells growth in # prn (cell growth when damaged) Example: Liver cells are able to Tissues: group of cells regenerate Organ: group of tissues • Labile cells Abnormal cells > abnormal tissue > abnormal organ > tumor growth in # is continuous Abnormal organs do not have a function Example: Lung cells (are always “Pseudo-organ” replacing cells) Two types of tumor Benign • Differentiation Harmless specialization Can become malignant Differentiated Cell Must still be removed cell with a specific function Slow growth Without metastasis Undifferentiated Cell Encapsulated cell with no function; abnormal Non-invasive: cells are within the • Risk Factor tumor will increase the odds of developing Malignant cancer Harmful Rapid growth With metastasis Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 -Causes of metastasis Circulatory spread Lymphatic spread Unencapsulated Invasive -Tumor cells are spread -Could enter circulation (circulatory spread) Could reach more places than lymphatic spread -Could enter the lymph (lymphatic spread) Cell of origin --> daughter cells Normal cells produce normal daughter cells. (It may produce abnormal cells via mutation) Abnormal cells produce abnormal daughter cells which continues the lineage WARNING SIGNS OF CANCER C A U T I O CAUTIONUS change in bowel and bladder function (habits) • Subjective data a sore that doesn’t heal • Subjective data unusual bleeding thickening or lump in breast or elsewhere indigestion N U S obvious change in warts or mole Inherently objective but comparison will come from the patient which can be considered as subjective nagging cough or hoarseness of voice STAGING Numerical Staging Stage 1: Limited (local) Stage 2: Limited (regional) Stage 3: Extensive local and regional spread Stage 4: Distant metastasis Stage 5: DOES NOT EXIST TNM Staging T – tumor (size) T0 – no tumor Tx – tumor cannot be identified (tumor may be behind an organ; hidden tumor) Tis – In situ (not proliferative) T1 - < 2 cm T2 ¬- < 5 cm T3 - > 5 cm T4 - > 5 cm (with metastasis) N – nodes (number of lymph nodes involved) N0 – no lymph nodes Nx – lymph node cannot be identified N1 – nodes 4 N2 – nodes > 4 Important lymph nodes • Cervical – neck • Supra-clavicular – collarbone • Axillary – armpits • Inguinal – groin • Mediastinal • Aortic Lymph Nodes • Canal system: -Edema (extremities) --> elevation of extremity --> absorption by lymph nodes --> jugular vein --> heart --> kidneys M – metastasis (with or without) M0 – no metastasis Mx – metastasis cannot be identified M1 – with metastasis T0N0M0 – no cancer unexplained anemia sudden weight loss Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 Ann-Arber (process comes in the exam, not the name) Stage 1 – only 1 lymph node involved Radiation therapy Stage 2 – two or more lymph nodes involved, 1 side Reference point: diaphragm Radiation therapy Stage 3 – two or more lymph nodes involved, both sides Reference point: diaphragm Chemotherapy and radiation therapy Stage 4 – extralymphatic (outside of lymph nodes) Chemotherapy and radiation therapy DIAGNOSTICS Biopsy – confirmatory test -Tissue sample taken --> microscopy (cytologic study) -Even if positive in all of CAUTIONUS, it does not mean that you have cancer -Types of biopsy Aspiration • Needle is inserted in body cavity to aspirate tissue sample Incision • Scalpel is used to remove tissue sample Excision • Whole mass removed • Possibly curative -Considerations •Invasive •Need consent •Anesthesia •Sedation • Cancer has pain o Pain is usually felt at the later part • Bone Cancer: most painful cancer • REASON OF PAIN MNEMONIC (COD) o Compression Ex: Nerve compression o Obstruction Ex: Organ obstruction o Destruction Ex: Destruction of bone • Pain management o Relaxation with guided imagery o Massage Massage around the tumor; not on the tumor o Alternating warm and cold compress Could be only one; could be both (alternating) o Medication Mild pain • Tylenol Analgesic • NSAIDs Anti-inflammatory & analgesic Severe pain • Sulfates Codeine sulfate Morphine sulfate Does Cancer have a cure? CXR – lung cancer Mammography – breast cancer Pap smear – cervical cancer • Indefinite yes • CURE mnemonic o C – chemotherapy o U – Upera (Surgery) o R – Radiation o E – Emotional support • Chemotherapy o Anti-neoplastic medications o Spreads throughout the body o Internal (common) Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 o External Topical administration of chemotherapy o Hazardous o Duration of Administration: 3 – 6 months, preferably Sometimes extended up to 8 months (physician’s discretion) • If benefits outweigh the risks o Mode of Action: kills cancer cells o Lacks specificity Can kill normal cells - produce side effects o More likely to kill cancer cells than normal cells o Attracted to rapidly dividing cells o Side Effects: (NANDA) N-nausea and vomiting (common side effect) A-alopecia N-neutropenia: decreased neutrophils • < 500 count •makes patient immunocompromised D-diarrhea A-anemia o Nursing Considerations: (CHEMO) C -caring • N/V --> anti-emetics o Ideally given before chemotherapy as prophylaxis • Diarrhea --> IVF o To counteract dehydration due to diarrhea H– handling • Never by a pregnant nurse o Teratogenic o Easily absorbed (if splashed on skin) • Goggles, mask, gown, gloves – for chemotherapy o Cap, goggles, mask, gown, gloves – to prevent cross contamination • Dispose in hazardous container o Spill kit E– education • Avoid large crowds o Immunocompromised due to neutropenia • Avoid fiber o To prevent aggravation of fluid loss due to diarrhea M– monitoring • Monitor lab values o Uric acid levels Normal: < 7 mg Abnormal: > 7mg Allopurinol o Platelet count Dictates what kind of bleeding Normal: 150,000 – 450,000 Bleeding tendencies present: 50,000 and below Spontaneous bleeding: 20,000 and below O– observation • Alopecia o Inform client that this is temporary Best way to alleviate altered body image o Offer wig (and even makeup) Before alopecia •To minimize obvious/major changes (especially if during alopecia) • Phlebitis o Change access (transfer to another vessel) • Radiation Therapy o High energy waves (High-dose radiation) Low-dose radiation – risk factor for cancer High-dose radiation – treatment for cancer o Localized (generally) o Internal Brachytherapy – radiation is injected o External (common) Teletherapy o Hazardous o Duration of Administration: as ordered o Mode of Action: reduce the size of tumor o Side Effects: F– fatigue (most common side effect) A– alopecia S– skin changes (discoloration) T– taste alterations o Types of Radiation Internal Radiation • Patient is a source of radiation o Teratogenic Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 • Radiation is inserted inside the body o Liquid or solid form • Sealed o Solid form – cesium/iridium Example: colorectal cancer – cesium inserted next to colon o Patient is radioactive, but excreta are not • Unsealed o May be spread o Liquid form – via IV/oral route o Patient AND excreta are radioactive Flush toilet three (3) times • Nursing Considerations o Private room – because patient is radioactive o Place caution on the door o Wear a dosimeter film Like a watch – tells radiation level Could be dosimeter badge o Wear a lead shield before entering room Lead – element designed to repel radiation o 1 nurse: 1 patient o Limit exposure to 30 minutes o No pregnant nurse o No visitors below 16 y/o People below 16 y/o are still rapidly growing External Radiation • Patient is not a source of radiation • Radiation can be felt o Instruct client to avoid exposure to sunlight o Avoid restrictive clothing To avoid skin irritation o Wash area with lukewarm water Cold water causes vasoconstriction --> decreased tissue perfusion Hot water irritates skin o Rinse with hand, not washcloth Washcloth promotes friction o Dry with patting, not rubbing motion MEDICATIONS • Hormonal Medications (hormone sensitive tumors) o To decrease size of tumors because some tumors are hormone-sensitive o Drugs T– Tamoxifen (most important drug) A– Arimidex D– Diethylstilbestrol • Vinca Alkaloids (anti-mitosis) o Drugs V– Velban O- Oncovin (most important drug) N-Navelbine • Alkylating Agents (DNA replication antagonist) o Drugs A– Altretamine B - Busulfan (most important drug) O– Oxaliplatin •Immunomodulator (immune manipulation) o So that the immune system kills the cancer cells o Cytokines --> stimulates immune cells to attack foreign bodies o Drugs Interleukins: destroy cancer cells • Chemo counterpart Interferons: slows down growth • Radiation counterpart tumor Monoclonal antibodies: antibodies that attack cancer cells Kinds of Cancer TESTICULAR CANCER • Concepts Testicles: germinal epithelium Produce sperm cells Produce testosterone • Note: Men have low amounts of estrogen • RISK FACTORS Age: 15 – 40 y/o Teach males to do self-examination starting at 15 y/o Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 Undescended testicles Testicles located first at the abdomen --> descends during development (9 months) Cryptorchidism • MANIFESTATIONS Initially painless Irregularities in Testicular Self-Exam Self-exam should be done after a shower • Due to body’s cooling mechanism Testicles should be smooth Self-exam is not confirmatory Self-exam must be done every month on a specific date Painless testicular mass “Heavy Pull” Due to mass Late: Pain • Bone pain • Back pain Gynecomastia • Tumor impairs testosterone production • Note: Tumor impairs sperm production (can cause infertility) • MANAGEMENT Pain management Mild pain • Tylenol Severe pain • Morphine sulfate • Codeine sulfate Chemotherapy Radiation Surgery: Orchiectomy Types of Orchiectomy • Unilateral: only one testicle Still fertile • Bilateral: both testicles Avoid lifting heavy objects Risk for herniation • Intestines may drop into the scrotum – inguinal hernia PROSTATE CANCER • Concepts Testes produce sperm cells Prostate produces seminal fluid • RISK FACTORS Age: more than 50 y/o STDs Heavy metal exposure • MANIFESTATIONS Irregularities – Digital Rectal Exam Highly suggestive; not confirmatory Painless post-coital bleeding (+) PSA – Prostate-Specific Antigen Highly suggestive; not confirmatory Late: Pain • Lumbar Pain • Leg Pain • MANAGEMENT Pain Management Chemotherapy Radiation therapy Surgery: TURP (Transurethral Resection of the Prostate) Using a Resectoscope Bleeding is normal Hematuria is normal Subject patient to CBI (Continuous Bladder Irrigation) • Use a solution to wash out debris • Dilutes salt in the body o Precipitates hyponatremia Watch out for: •Cerebral Edema •Increased Intercranial Presssure o Triad signs of ICP Hypertension Bradycardia Bradypnea CERVICAL CANCER • Concept: Tumor squeezes the neighboring structures • RISK FACTORS HPV Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) cervix and lOMoARcPSD|16207318 Multiple sex partners HPV can be spread Early intercourse 16 y/o Smoking • MANIFESTATIONS Painless vaginal bleeding Painless vaginal discharge (Vesicovaginal) Fistula formation ->leakage of feces and urine Mucous membranes are stuck into each other Two mucous membranes become connected >> a hole is formed >> fluids are being shared • “It’s like I’m peeing through my vagina” Late: Pain • Lumbar Pain • Leg Pain • Pelvic Area Pain • MANAGEMENT Chemotherapy Radiation Therapy Surgery: Hysterectomy BREAST CANCER • Concept: Lobules: produce milk in response to prolactin • RISK FACTORS Chest X-Ray Family History Nulliparity Early Menarche Late Menopause • MANIFESTATIONS Painless breast mass Irregularities in BSE (Breast SelfExam) BSE should be done every month; 7-10 days after the menses • During a bath To assess left breast, raise left arm; assess with right hand • Outer to inner or outer to inner motion Higher breast is the affected breast Women’s breasts are normally asymmetrical Peau d’orange (dimpling similar to the skin of an orange) Men can have breast cancer Men have worse breast cancer Common sites of breast cancer: Upper outer Axillae Below the nipple line • TYPES OF BREAST CANCER Non-invasive breast cancer Stays in the mammary duct Reason why breast cancer is common in women Invasive breast cancer Spreads outside Men have it worse because men do not have mammary ducts >> immediately invasive • MANAGEMENT Position patient in Semi-Fowler’s position Most comfortable position 30 – 45 degrees angle of the head of the bed Chemotherapy Radiation Therapy Administer Tamoxifen as ordered Surgery: Lumpectomy • Removal of the lump Mastectomy • Also a lumpectomy • Removal of lump + breast tissues MRM (Modified Radical Mastectomy) • Also a mastectomy • Removal of lump + breast tissues + axillary lymph node + nipple COMPLICATIONS • Fluid shifting is possible >> edema >> lymphedema o Right breast removal >> right arm has edema >> elevate Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 LUNG CANCER To maximize lung compliance • Concepts: “I go in with oxygen as I go out with carbon dioxide.” “I go in with microorganisms as I go out with microorganisms.” • Tumor prevents exit of microorganisms >> energy is needed to be used >> blood vessels become semi-permeable >> WBCs enter respiratory tract to destroy microorganisms (this process requires energy and the semi-permeability of blood vessels) Anatomical structures: trachea >> bronchi >> bronchioles >> alveoli (gas exchange occurs here) • RISK FACTORS Chest X-Ray Radon: colorless, odorless gaseous chemical Usually on the ground or soil Smoking • MANIFESTATIONS Wheezes Due to constricted airway to Hemoptysis Due to intense coughing Fever Weakness and Fatigue Due to energy expenditure caused by the use of energy to make blood vessels semi-permeable Shortness of breath Pulmonary edema Due to semi-permeability of blood vessels • MANAGEMENT Priority: AIRWAY Oxygen as ordered High-Fowler’s position Pneumonectomy • Removal of entire lung Post Op: Key Concepts • Pleural cavity usually has negative pressure • Surgical procedures cause fluid shifting >> fluid in pleural cavity >> positive pressure • One lung >> difficulty breathing >> lung occupies the space left by the removed lung >> Mediastinal Shift >> Tracheal Deviation >> not good • After a pneumonectomy, CTT (Chest Tube Thoracostomy) is contraindicated • Positive pressure in the affected chest is the desired outcome • Do not allow patient to lie on side of unaffected chest LARYNGEAL CANCER Dyspnea Due to obstruction of airway Cough Compensatory mechanism expel foreign bodies Bronchodilators as ordered Chemotherapy Radiation Therapy Surgery: Lobectomy • Removal of lung lobe • Left lung – 2 lobes • Right lung – 3 lobes • RISK FACTORS Smoking Alcohol Pollutants Radiation Frequent neck radiation • MANIFESTIONS Feeling of a lump in throat Dysphagia: difficulty in swallowing Weight loss Due to impairment of eating because of dysphagia Dyspnea: difficulty breathing Due to obstruction Cough Lump stimulates cough reflex Hemoptysis due to excessive cough >> injury Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 • MANAGEMENT Aspiration precaution Lump in the throat causes impairment of movement of food in the throat High-Fowler’s while feeding • Do not let patient eat while lying down High-Fowler’s even while not eating • To maximize lung expansion Epiglottis opens lower esophageal sphincter closes Otherwise, reflux occurs Food is in the stomach >> pyloric sphincter opens after 2 – 4 hours NOTE: Pyloric sphincter may also open or close depending on the pressure on the duodenum • RISK FACTORS Oxygen as ordered Alternative Routes for Food Total Parenteral Nurtrition NGT Gastrostomy Jejunostomy Surgery: Laryngectomy Total Laryngectomy – if tumor occupies a big amount of the larynx Cordal Stripping – if superficial tumor Spicy foods Highly seasoned food Smoking Alcohol Carcinogens Overcooked food – Benzopyrene Preservatives – Nitrosamine Peanut – Afflatoxin • MANIFESTATIONS Tumor is near LES >> LES does not close >> Difficulty swallowing • Oral fluids are needed to pass food Post-Op: Total Laryngectomy tracheostomy is permanent Assess gag and cough reflexes • To assess laryngeal nerve damage High-Fowler’s position • To maximize lung compliance Mech vent as ordered Watch out for • Hemorrhage o Use a penlight Maintain surgical drains Refer to speech therapist GASTRIC CANCER Tumor is near Pyloric Sphincter >> Pyloric Sphincter does not close Heartburn (pyrosis) • Food goes up Vomiting • Area Postrema (vomiting center of the brain) is stimulated Diffused type of cancer Satiety: feeling of fullness Hematemesis • Due to injured tumors drenched in Hydrochloric Acid Melena • Due to injured tumors drenched in Hydrochloric Acid • Bleeding in the upper GI >> blood is processed >> darkened stools Pain Initially, generalized abdominal pain Later on, pain is focused in the middle • Concepts Anatomical structures: esophagus, lower esophageal sphincter, stomach, fundus, pylorus, pyloric sphincter Hydrochloric Acid in the stomach Swallowing >> epiglottis closes >> food goes towards the stomach >> lower • MANAGEMENT esophageal sphincter opens Avoid carcinogens Avoid smoking Avoid alcohol Small frequent feeding Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 Administer antacids as ordered Blood transfusion as ordered Chemotherapy Radiation Therapy Surgery: Total gastrectomy: removal of the entire stomach •Achlorhydria: absence of hydrochloric acid (due to absence of stomach in total gastrectomy) •Anastomosis: surgical connection of two structures •Hydrochloric Acid + Food = Chyme (an acidic substance) o Duodenal cells are able to produce alkaline substances o Considerations: Goal is to delay gastric emptying Low residue diet Fluids only after meals (PC) Lie flat on bed after meals (PC) Antispasmodics to delay gastric emptying Solid foods are preferred over wet food •Lubrication increases gastric emptying COLON CANCER •Achlorhydria >> duodenal cells produce acidic substances >> food is Concepts Jejunum: maximum absorption of digested nutrients • Diet as tolerated Colon: maximum absorption of fluids Parts of the colon: Billroth I (gastroduodenostomy) Appendix Billroth II (gastrojejunostomy) Cecum Ascending colon – stool is in liquid form Post-Op Transverse colon – stool is semisolid NPO 1-3 days depending on peristalsis Descending colon – stool is in solid form • Because surgery was performed Sigmoid Rectum directly on the stomach • Ask patient about flatus • RISK FACTORS o Best way to determine GI function More than 50 y/o Advance from NPO to sips of water >> Polyps if tolerated, soft diet Family History Inflammatory Bowel Disease (IBD) Monitor for electrolyte imbalances Crohn’s Disease Administer IVF and electrolytes as Ulcerative Colitis ordered Administer TPN as ordered • MANIFESTATIONS Watch out for: Blood in the stools •Dumping Syndrome (Increased Tumor is injured because of the flow of Gastric Motility): food is dumped feces o Manifestations: Red blood (Lower GI bleeding) Increased peristalsis Anemia Hyperactive bowel sounds Weight loss Impaired fluid absorption >> fluid Diarrhea volume deficit Abdominal cramping Vomiting Palpitations (and tachycardia) Complete bowel obstruction Diaphoresis Tumor in Ascending Colon (AC) Fluid is not absorbed properly >> Diarrhea Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 Tumor in Descending Colon (DC) Only soft feces are passed Ribbonlike Stool >> • METASTASIS Lymphatic spread Circulatory spread • MANAGEMENT Watch out for: Peritonitis Perforation • Board-like abdomen • Pain • Fever • Dullness upon percussion Intestinal Obstruction Urinary obstruction (clot-induced) Tumor bleeds >> blood clot formation >> urethra is blocked >> urinary obstruction >> UTI >> renal failure • MANAGEMENT Chemotherapy Radiation therapy Surgery: Cystectomy (bladder removal) Ureters are connected to the: • Ileum o Ileal conduit • Colon o Colon conduit MULTIPLE MYELOMA Chemotherapy Radiation Therapy Surgery: Bowel Resection with Colostomy • Concepts Petroleum jelly gauze is given to cover Cancer of the plasma stoma Plasma produces immunoglobulins Watch out for bleeding Plasma contains hematopoietic stem Note color of stoma cells • Normal color: red/pink Hematopoietic stem cells >> becomes RBCs, WBCs, Plasma Watch out for pouch leakage AC – liquid stools Too much plasma >> bone marrow is TC – semiformed stools squeezed DC – solid stools Abnormal plasma attacks the bone >> contains calcium, purine >> causing hyperuricemia, osteoporosis, hypercalcemia BLADDER CANCER • Concepts Bladder is the reservoir of urine Bladder contracts >> urine is released Tumor makes bladder think that it is full (of urine) • RISK FACTORS Smoking Chemical Exposure Radiation Bones contain: • Calcium >> bone is attacked o Calcium is released in the blood >> hypercalcemia o Decreased calcium in the bones >> osteoporosis • Purine >> bone is attacked >> uric acid is released in the blood >> hyperuricemia Bones contain Bence Jones Protein • MANIFESTATIONS >> not filtered >> present in urinalysis Urgency • RISK FACTORS Frequency Dysuria: difficulty in urinating Age: 60+ Painless hematuria – most frequent Radiation exposure manifestation Chemical exposure Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 • MANIFESTATIONS • MANAGEMENT Infection precaution Decreased RBCs Observe aseptic technique for all Decreased WBCs procedures Decreased Platelets Isolate patient Note: Leukemia has worse decrease of blood components •Reverse isolation: prevents patient Risk for fractures from being infected by others Renal calculi •Reverse isolation: positive air Kidneys compensate for hypercalcemia pressure >> calcium oxalate stones formed >> •Direct isolation: negative air pressure urinary tract obstruction >> renal failure so that air comes in •Direct or Reverse – room must be end • MANAGEMENT of the hallway Chemotherapy Radiation therapy Limit exposure Bone marrow transplant • Limit visitation hours/visitors LEUKEMIA • Concepts Hematopoietic stems cells are no longer producing useful RBCs and Platelets >> drop of blood components Bone marrow produces RBCs, WBCs, Platelets In leukemia, blood components produced are abnormal or useless RBCs – cannot carry oxygen WBCs – does not fight infection Platelets – does not prevent clotting • RISK FACTORS Smoking Chemical exposure Family history • MANIFESTATIONS Decreased RBC Anemia Paleness Weakness and fatigue Shortness of breath Decreased WBC Client is immunocompromised >> risk for infection AVOID!!! • Fresh fruits • Fresh vegetables • Fresh flowers Monitor temperature Anticipate administration of oral antibiotics for infection • Injections are not allowed due to bleeding tendencies Bleeding Precaution Watch out for • Nadir: point of lowest platelet Avoid • Exposure to sharps • IV fluids • IV medications •Acetylsalicylic Aspirin platelet/platelet aggregator • NSAIDs – gastric irritants – anti- Fatigue Promote rest Assist client with ambulation Schedule activities (plan activities) Packed RBC as ordered • Only time to use injection Decreased Platelet Risk for bleeding Presence of bruises Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) lOMoARcPSD|16207318 Non-Hodgkin’s HODGKIN’S DISEASE • Concepts Cancer of the lymph nodes Lymphatic system is a canal system for fluids Fluids >> lymph nodes >> jugular vein Lymphatic system helps in immune function >> lymphocytes Reed Sternberg cells or Owl’s eyes: hallmark tumor of Hodgkin’s Disease Multiple nuclei instead of only one Instead of lymphocytes Phases of Hodgkin’s Disease Lymphocyte Predominant • More normal cells than abnormal cells Nodular Sclerosis • Equal number of abnormal cells • Cells are separated • Without RSB cells • Late detection False Negative at first • Poor prognosis • Risk: HIV • Risk: Burkitt’s lymphoma • Chemotherapy • Radiation Therapy • Deadlier DIFFERENTIATION OF BLOOD CANCERS normal and • MULTIPLE MYELOMA Abnormal plasma Bone marrow to bone affected >> decreased bone density Mixed Cellularity Blood cancer • Equal number of normal and Chemotherapy abnormal cells Radiation therapy • Normal and abnormal cells have mixed • HODGKIN’S Abnormal lymphocytes Lymphocyte Depletion Lymph nodes are affected >> presence of • More abnormal cells than normal RSB Blood cancer cells Blood cancer Chemotherapy • MANIFESTATIONS Radiation therapy Painless lymphadenopathy Risk for infection • LEUKEMIA Cough Abnormal HSC B-symptoms (suggestive of Hodgkin’s to Bone marrow to blood affected >> be extralymphatic) decreased blood components Fever Blood cancer Night sweats Chemotherapy Weight loss Radiation therapy Hodgkin’s vs Non-hodgkin’s Hodgkin’s • With RSB cells • Early detection • Better prognosis • Risk: Bimodal age 15-30 y/o or more than 50 y/o • Chemotherapy • Radiation Therapy Downloaded by ALMIRA LOPEZ (nur_alopez@metro.edu.ph) NOTESBYZAIRRA