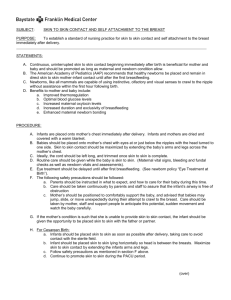
CHAPTER 15: POSTPARTUM ADAPTATIONS Puerperium period: ● Begins after delivery of placenta and lasts 6 weeks Reproductive system adaptations Uterine involution ● How the uterus returns to its normal size ● Involves 3 retrogressive processes ○ Contraction of muscle fibers to reduce those previously stretched during pregnancy ○ Catabolism, which shrinks enlarged individual myometrial cells ○ Regeneration of uterine epithelium from the lower layer of the decidua after the upper layers have been sloughed off and shed during lochial discharge ● The uterus weighs 1,000g after birth ○ After 1 week: shrinks 50% ● During the first 12 hours postpartum the uterus is located at the umbilicus ● Afterpains = primary mechanism preventing hemorrhage from placental site Lochia ● Vaginal discharge; Involution and restoration of endometrium is reflected here ○ RIGHT AFTER BIRTH: bright red ● Three stages of lochia 1- Lochia rubra : deep red mixture; occurs first 3-4 days 2- Lochia serosa: pinkish brown ; 3-10 days PP 3- Lochia alba: creamy white / light brown ; days 10-14 ● Offensive odor = infection like endometritis Cervix is now shaped like a slit instead of a circle Perineum ● Often bruised and edamatous for the first 1-2 days after birth ● Comfort measures to relieve pain: ice packs, warm water, witch hazel, sprays, baths. Pelvic floor ● Pelvic floor dysfunction is one of the most common complications following a NVD ○ Women should do pelvic floor exercises to improve muscle tone ○ Can lead to urinary incontinence Cardiovascular changes ● During pregnancy heart is displaced upward to the left ○ This reverses during involution ● Cardiac output is higher duringp regnancy then declines to normal within 3 months PP ● Blood volume (inc during pregnancy) drops to normal within 4 weeks PP ● HEMATOCRIT STAYS THE SAME ; IF ACUTE DECREASE = SUSPECT HEMORRHAGE Urinary system changes ● After birth women who revoeved anesthetics have trouble feeling sensation to void ○ These women are at risk for ■ Incomplete emptying ■ Bladder distention ■ Difficulty voiding ■ Urinary retention Urinary retention ● Can displace the uterus from midline to the right- which inhibits the uterus from contracting properly ● If the uterus cannot contract properly : risk for post partum hemorrhage ● Urinary retention = major cause of uterine atony ○ Frequent voiding of small amounts <150mL suggest retention with overflow GI system changes ● Decreased bowel tone and sluggish bowels ● Constipation is common - stool softener is usually prescribed Musculoskeletal system changes ● Increased ligament laxity, weight gain, and carpal tunnel revert ● Permanent increase in shoe size ● Fatigue and distorted body image ● Good body mechanics is important to avoid back pain ● Loss of muscle tone in abdomen - can be improved with exercises Integumentary system adaptations ● Pigmentation on abdomen (linea nigra) fades ● Pigmentation on face (melasma) fades ● Hair loss- temporary ● Stiae gravidarum fades into silver lines ● Excessive sweating is common - reassure that this is common and change clothes at night to prevent chilling Respiratory system changes ● Discomforts, shortness of breath, and rib aches are relieved Endocrine system changes ● Estrogen and progesterone drop quickly with delivery of placenta ○ Dec estrogen = related to breast engorgment & excessive diuresis ● Hcg levels are non existent after 1 week ● hPL undetectable after 1 day ● Prolactin will decline after 2 weeks if the women is not breast feeding Weight loss ● Weight gain and postpartum weight retention = inc risk for obesity ● breast feeding can help but is usually not sufficient to return to prepregnant weight ● Lifestyle interventions: exercise and dietary changes Sexual changes ● Problems that occur are usually related to sexual drive, arousal, orgasmic disorders, and uncomfortable intercourse Global health ● The issues of disrespect and abuse during and after childbirth and the need for respectful maternity care are key elements that need to be addressed to improve outcomes. ● Bleeding and infections = most common cause of death after child birth Lactation and Breastfeeding All components must be present for sucessful breastfeeding 1. Periodic motions of infants jaw 2. Undulation of tongue 3. Breast milk ejection reflex Along with: 1. Proper positioning 2. Latching on 3. Sucking 4. Swallowing ● AAP reccomends exclusive breastfeeding for 6 months ○ Introduce complementary foods and continue breast feeding for 1 year + ○ This reccomendation is standard of care today Breast changes Hormones: ● Estrogen stimulates growth of milk collection (ductal) system ● Progesterone stimulates growth of milk production system ● Prolactin triggers synthesis and secretion of MILK after birth ● Oxytocin helps milk eject from alveoli to the nipple ● Synthesis of ESTROGEN, PROGESTERONE, AND PROLACTIN hormones = creates colostrum ○ Has protein and carb but NO milk fat ● Each breast gains nearly 1lb by term ● Nipple stimulation = increases prolactin levels ● Sucking = stimulates prolactin and oxytocin production *Gold standard to initiate breastfeeding = SKIN TO SKIN CONTACT WITHIN FIRST HOUR * ● Newborn instinct to crawl up to breast is termed BREAST CRAWL ● “Let-down reflex” ○ Occurs immediately before or during breast feeding ○ Tingling sensation in breasts ENGORGMENT 🙁 Distention and swelling of breast tissue as a result in increase blood supply and lymph ● Usually peaks 3-5 days postpartum IF MILK IS NOT REMOVED: ● Alveolar space can become overdistended causeing tender swollen breats HOW CAN THIS OCCUR: 1. Infrequent feeding 2. Ineffective emptying of the breasts HOW TO RESOLVE ENGORGMENT: 1. Frequent empyting of the breasts 2. Warm compress before feedings TREATMENTS TO REDUCE PAIN FROM ENGORGMENT 1. Heat / cold application 2. Cabbage leaf compresses 3. Breast massage / milk expression 4. Ultrasound 5. Breast pumping 6. Antiinflammatorys (ibuprofen) Supressing lactation ● No universal guideline on most appropriate approach, can implement: 1. 2. 3. 4. 5. Wear a tight supportive bra 24 hrs daily Apply ice for 15-20 min every other hour No sexual stimulation Do not squeeze breasts and express milk Avoid hot showers Return of ovulation and menses ● Differs for women who breast feed vs. those who do not breastfeed Nonlactating women: menses may resume within 7-9 weeks; majority is 3 months Breastfeeding women: can return anytime depending on frequency and duration Cultural considerations ● Somali women stay home for 40 days ● Somali and arab breast feed for extended periods of time Vietnamese women ● Postpartum = cold state ○ Warm water for hygeine, stimulation of lactation, warm foods, staying indoors. Parental attatchment Attachment is the formation of a relationship between a parent and a newborn through a process of physical and emotional interactions. Attachment between a woman and her newborn has lifelong implications Influences on attatchment: Oxytocin 1. Skin to skin contact 2. Breastfeeding 3. Eyecontact 4. Social vocalizations 5. Maternal and milk odor 6. Newborn massage ● Minimize parent-newborn seperation through ○ kangaroo care (facilitating skin to skin contact) ○ Breastfeeding ○ Parent participation in care Maternal psychological changes ● * Perinatal mood disorders are one of the most common complications during post partum * From mild to severe: 1. Maternal “baby blues” 2. Postpartum depression 3. Psychosis Maternal “Baby Blues” ● Short lived ● Mild depressive symptoms, anxiety, irritability, mood swings, loss of appetite, trouble sleeping, tearfulness, inc sensitivity and fatigue ● Peak PP 4-5 days; usually resolve by day 10 Rubins phases for adjusting to maternal role 1. Taking in phase ● Immediately after birth when mother needs sleep and depends on others ● Characterized by dependent behavior ● They spend time recounting their labor experience to others. Such actions help the mother integrate the birth experience into reality; the pregnancy is over and the newborn is now a unique individual, separate from herself. ● “he has my nose” or “his fingers are long like his father’s” ● Lasts 1-2 days 2. Taking hold phase ● ● ● ● ● ● Dependent and independent behavior 2-3 day postpartum May last several weeks Concerned about her own health and infants condition Wants to care for baby by herself Requires reassurance 3. Letting go phase ● woman reestablishes relationships with other people. She adapts to parenthood in her new role as a mother ● More confidence BAM STAGES 1. Commitment, attachment to the unborn baby, and preparation for delivery and motherhood during pregnancy 2. Acquaintance/attachment to the infant, learning to care for the infant, and physical restoration during the first 2 to 6 weeks following birth 3. Moving toward a new normal 4. Achievement of a maternal identity through redefining self to incorporate motherhood (around 4 months); the mother feels self-confident and competent in her mothering and expresses love for and pleasure interacting with her infant PARTNERS ● We must role in supporting a partner’s transition to parenthood by keeping partners informed about birth and postpartum routines, reporting on their newborn’s health status, and reviewing infant development. They can also contribute by creating participative space for new partners during the postpartum period. Engrossment Partners developing bond with the newborn characterized by 7 behaviors: 1. Visual awareness of the newborn—the partner perceives the newborn as beautiful. 2. Tactile awareness of the newborn—the partner has a desire to touch or hold the newborn and considers this activity pleasurable. 3. Perception of the newborn as perfect—the partner does not “see” any imperfections. 4. Strong attraction to the newborn—the partner focuses all their attention on the newborn when in the room. 5. Awareness of distinct features of the newborn—the partner can distinguish the newborn from others in the nursery. 6. Extreme elation—the partner feels a “high” after the birth of the child. 7. Increased sense of self-esteem—the partner feels proud, “bigger,” more mature, and older after the birth of the child Three stage role development of partners 1. Expectations a. Preconceptions about what having a baby will be like 2. Reality a. Feelings change from elated to sad and frustration when they realize having a baby isnt what they thought 3. Transition to mastery a. he partner makes a conscious decision to take control and be at the center of the newborn’s life regardless of preparedness. b. Similar to mothers “letting-go” phase