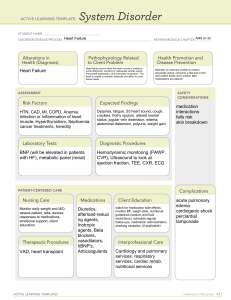
Cardiac CLINICAL MANIFESTATION OF SYSTEMIC VENOUS CONGESTION o Peripheral and periorbital edema, weight gain due to edema, ascites, hepatomegaly, neck vein distention o Dependent edema: lower extremities, genitalia, or generalized INTERVENTIONS TO DECREASE CARDIAC DEMAND FOR CHD Regulate thermal environment: Warm room o Decrease cold stress in infants- shivering requires a great deal of energy Prevent and treat infections o Infection leads to increased BMR, as does fever o Rigorous aseptic technique at all times Maximize chest expansion o HOB at 45 degrees Provide rest o Decreased environment stimulation o Schedule periods of uninterrupted rest CHD DEFECT THAT DECREASES PULMONARY BLOOD FLOW (CYANOTIC) o ASD, VSD (Large) RAPS HEART DEFECT THAT INCREASES PULMONARY BLOOD FLOW (ACYONOTIC) Abnormal connection between the two sides of the heart: either the septum or the great vessels Examples: Atrial Septal Defect (ASD), Ventricular Septal Defect (VSD), Patent Ductus Arteriosus (PDA) Increased blood volume on the right side of the heart o Increased pulmonary blood flow, Decreased systemic blood flow SYMPTOMS OF CONGESTIVE HEART FAILURE IN CYANOTIC HEART DEFECTS o Clinically, patients have hypoxemia and can appear cyanotic. SECONDARY PROBLEMS OF CYANTOIC HEART DEFECTS Characteristic harsh, systolic murmur from pulmonary stenosis & VSD Tet Spells: Acute episodes of cyanosis and hypoxia o O2 requirements exceed blood supply due to obstructed pulmonary blood flow o Place child in knee to chest position to decrease venous return from legs and increase systemic vascular resistance, thus diverting more blood into pulmonary artery o Children will assume this position on their own if old enough Clubbing Poor growth Risk for emboli, loss of consciousness, sudden death TETRALOGY OF FALLOT FOUR STRUCTURAL DEFECTS o Right ventricular hypertrophy, aortic arch (overriding), pulmonic stenosis, septal defect: VSD LARGE WHEN DO YOU NOT GIVE DIGOXIN o not given if pulse is below 90 to 110 beats/minute in infants and young children or below 70 beats/min in older children), auscultate apical pulse for full minute before administering COARCTATION OF THE AROTA-HOW OFTEN SHOULD WE GET VITALS?*** o 4 point blood pressure (UE, LE); NURSING/PATIENT INTERVENTIONS FOR RELIEVING CYANOSIS, TACHYCARDIA, AND TACHYPNEA Medication to Improve cardiac function (increased contractility and decrease afterload) Remove accumulated fluid and sodium (decrease preload) Decrease cardiac demands Improve tissue oxygenation and decrease oxygen consumption o Decrease O2 demand and oxygen supplementation CLOSURE OF THE DUCTUS ARTERIOSUS DO? • Closure in presence of increased oxygen, closing this stops: Blood is recirculated through lungs and returned to LA & LV= Increased workload of on the left side heart. HYPERLIPIDEAMIA-HIGH LEVEL LABS CAN PREVENT CARDIOVASCULAR DISEASE? o Universal screening ages 9-11 WHAT TO WATCH FOR WHEN PT HAS HYPERKALEMIA: o most immediate threat-MUST WATCH FOR ARRHYTHMIAS) (Acute Renal Failure Complication) WHAT DOES A CHEST X-RAY SHOW? o provides information on heart size and pulmonary blood flow patterns GI TREATMENT FOR GER (GERD) Management: depends on severity, avoidance of certain foods, upright positioning while feeding, small, frequent feedings, thickened feedings, H-2 receptor antagonists (Zantac, Tagamet, Pepcid), proton pump inhibitors (Nexium, Prevacid, Prilosec, Protonix) Nissen Fundoplication: surgery-passage of gastric fundus behind the esophagus to encircle the distal esophagus INFLAMMATORY BOWEL DISEASE o TREATMENT o Goal is to induce and maintain remission: 5-ASAs (mesalamine, olsalazine, and balsalazide in mild u.c., corticosteroids for severe ulcerative colitis and Crohn’s disease, immunomodulators such as azathioprine and 6-MP o Nutritional support: small, frequent meals, high-calorie, high-protein foods, mouth care, enteral feedings or NG tube feeds may be needed, TPN (education) o Surgical interventions o Nursing Care: managing diet, coping with stress, adjusting to remissions and exacerbations, preparing family for possibility of surgery o SYMPTOMS o Ulcerative colitis (UC) (limited to colon and rectum) inflammation of the bowel with ulceration, bleeding, and edema, strictures o Crohn’s disease (involves any part of the GI tract) mouth sores, skip lesions, ulcerations, fibrosis, adhesions, stiffening of the bowel wall, stricture formation, fistulas of bowel, bladder, vagina or skin CROHN DISEASE o WHAT IS IT?: IBD of any part of the GI tract o CLINICAL MANIFESTATIONS: mouth sores, skip lesions, ulcerations, fibrosis, adhesions, stiffening of the bowel wall, stricture formation, fistulas of bowel, bladder, vagina or skin OBJECTIVE MANIFESTATION OF PYLORIC STENOSIS o Forceful vomiting—can indicate pyloric stenosis CLINICAL MANIFESTATION OF BILARY ATRESIA o Clinical Manifestations: if jaundice persists beyond 2 weeks old, especially if direct (conjugated) serum bilirubin is elevated, suspect BA., urine may be dark, and the stools often become progressively acholic or gray (no bile),pruritis, poor weight gain. GU KNOW ASSESSMENT FINDINGS FOR UROSEPSIS o febrile UTI coexisting with systemic signs of bacterial illness; urinary pathogens in blood VESICOURETERAL REFLUX-TEST TO CONFIRM DIAGNOSIS o Voiding cystourethrogram (VCUG): Study done usually 3-6 weeks after active infection has resolved UNDESCENDED TESTICLE (CRYPTORCHISM); Not painful, does not interrupt urination o PARENT EDUCATION: Preventing infection of orchipexy, pain management, Avoid rigorous activity for 2 weeks teach to not strain themselves (hard for 1-2 year old) o Orchiopexy: surgical treatment between 1 & 2 years of age if the testis doesn’t descend spontaneously (protects from damage from body heat excess) LAB FINDINGS FOR ACUTE GLOMERULONEPHRITIS o Elevated BUN/Creatinine, Decreased serum albumin; INFECTION SO CS/URINALYSIS PRIMARY MANIFESTATIONS OF RENAL FAILURE o severe reduction in GFR, elevated BUN, and significant reduction in renal blood flow. Principal feature is oliguria and hypertension. o Hyperkalemia (most immediate threat-MUST WATCH FOR ARRHYTHMIAS) o Hypertension—monitor every 4 to 6 hours o Anemia—transfusion if hemoglobin drops below 6 g/dL o Seizures—related to hypertension, hyponatremia, and hypocalcemia o Cardiac failure with pulmonary edema—associated with hypervolemia—TX=reduce fluid volume, sodium restriction, diuretics o Tendency to develop: Water intoxication, Hyponatremia PREDISPOSITION FOR FEMALES AND UTI’s o Short urethra in girls-predisposition- (recommend cotton underwear for girls) MINIMAL CHANGE NEPHROTIC SYNDROME: See pages 19 ACUTE GLOMERULONEPHRITIS • MANIFESTATIONS OF IMPROVEMENT: Accurate I&O—monitor urine output—**increase in output is often first indication of improvement** COMPLICATION OF NEPHROTIC SYNDROME o WHAT DO YOU ASSESS TO DETECT EARLY SIGN OF COMPLICATION Edema & massive protenuria HYDROCELE • WHEN DO WE DO TREATMENT?: Requires surgery if not spontaneously resolved at a year PT HAS FEVER, DYSURIA, FLANK PAIN, URGENECY, AND HEMATRUA-WHICH TEST WILL BE PERFORMED? Acute pyelonephritis – clean catch, catheterization, urinalysis Dipstick o Quick and inexpensive Microscopic urinalysis Culture & Sensitivity testing determines susceptibility to antibiotics Clean-catch specimen is preferred, U-bag for collection from child Specimen obtained by catheterization or suprapubic needle aspiration has more accurate results o May be necessary when clean-catch specimen cannot be obtained Imaging studies for suspected obstruction o IVP or abdominal CT scan WHAT IS PHIMOSIS? o Phimosis: Narrowing or stenosis of the opening of the foreskin that prevents retraction of the foreskin MANIFESTATIONS OF HYPOSPADIAS Urethral opening is located below the glans penis or anywhere along the ventral surface Mild: meatus just below the tip of the penis Most severe: meatus on perineum Chordee: ventral curvature of penis accompanies severe form DIALYSIS-WHY WOULD A CHILD SEEM DEPRESSED OR ANGRY?: Loss of control? *** o Boredom, dietary and fluid restrictions, school absence Endocrine THERAPEUTIC MANAGEMENT OF ADRENAL HYPERPLASIA o Administration of clucocorticoids to suppress high secretions of ACTH and adrenal androgens to maintain the timing of normal pubertal development. Cortisone, increase during episodes of stress. Gender assignment ??? CLINICAL MANIFESTATIONS OF ADRENAL HYERPLASIA Inherited disorder of the adrenal glands that affects both genders Inability to properly produce cortisol, and sometimes aldosterone o Also can possibly produce an excess of androgen hormones Main cause of ambiguous genitalia in children o Early puberty, growth concerns Manifestations: Reaches puberty early and hirsutism NURSING INTERVENTIONS FOR DKA PATIENTS Child admitted to the ICU Priority is venous access for administration of fluids, electrolytes and insulin—prompt and adequate fluid therapy! (ALWAYS START 0.9% SALINE FIRST) Weigh child, Monitor vital signs Place on cardiac monitor, administer oxygen Blood glucose and ketone levels determined CLINICAL MANIFESTATIONS FOR TYPE 1 DM o Polyphagia, polyuria, polydipsia, weight loss, enuresis, nocturia, irritability, shortened attention span, hyperglycemia, ketoacidosis, frequent infections, poor wound healing, blurred vision, dry skin, flushed skin, headache, fatigue DIABETES INSIPIDUS-WHAT IS IT?: Undersecretion of ADH, vasopression; manifests as enuresis and insatiable thiirst o TREATMENTS: daily hormone replacement of vasopressin CLINICAL MANIFESTATIONS OF CUSHING SYDROME o Hyperglycemia, bruising, striae, decreased immune response, poor wound healing, periorbital edema OTHER NURSING CARE FOR TRACHEOESOPHAGEL FISTULA o Maintain a patent airway, prevent PNA, gastric or blind pouch decompression, supportive therapy, surgical repair – suction if necessary; supine head elevation 30 degrees o Frothy saliva (excessive amounts) CLEFT LIP/PALATE: Feeding is highest priority o PREOP CARE: Alternative feeding systems (syringe); off bottle, depends on surgeon o POSTOPERATIVE CARE: protecting operative site (petroleum jelly), elbow immobilizers (7-10 days), syringe feedings, analgesia, upright or infant seat, avoid suction and objects in the mouth o NURSING INTERVENTIONS: See above? OMPHALOCELE (NOT IN POWERPOINTS) o NURSING INTERVENTION: (WET STERILE GUAZE); prevents infection and fluid loss keeping intestines moist o WILL ALWAYS HAVE MORE THAN ONE DEFECT: Intestines, liver, etc. Usually have accompanying congenital defect such as cardiovascular or genitourinary defect