Alterations in Oxygenation: Pediatric Respiratory Disorders
advertisement

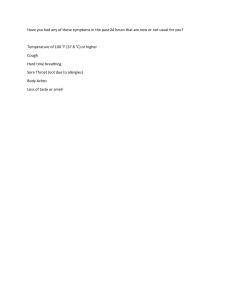
Alterations in oxygenation LEANNE ASHLEY D. BONIFACIO, RN, MN divisions of the respiratory system UPPER RESPIRATORY TRACT • • • • • LOWER RESPIRATORY TRACT Nose Paranasal sinuses Pharynx Larynx Epiglottis • Bronchi • Bronchioles • Alveoli presentation title 3 R E S P I R AT O RY T R A C T D I F F E R E N C E S I N CHILDREN Frontal and sphenoidal sinuses do not develop until 6 to 8 years of age Tongues are large in proportion to the mouth Infants have small nares and are obligate nose breathers Airway is smaller in diameter and shorter in length Airway structures have greater laxity Have large occiputs when compared with an adult a. Infant’s large occiput has caused flexion of the head and subsequently caused the base of the tongue to obstruct the upper airway. b.Placing a towel under the shoulders and neck allowing more extension of the head and an opening of the upper airway relieves the obstruction. physical assessment of a child with a respiratory disorder Cough ▪ Initiated by stimulation of the nerves of the respiratory tract mucosa. ▪ Clears excess mucus or foreign bodies from the respiratory tract or as a response to gastric contents refluxed into the airway. ❑ Paroxysmal coughing - series of expiratory coughs after a deep inspiration. Rate & Depth of Respirations ▪ Tachypnea - often is the first indicator of respiratory distress in young children ▪ Assess not only the rate but also the depth and quality of respirations and other vital signs Retractions ▪ Created when the child must inspire more forcefully than normal to inflate their lungs because of an airway obstruction or stiff, noncompliant lungs. Restlessness ▪ Children hypoxia or can infants become who have anxious and restless. ▪ May be one of the first signs of airway obstruction or the respiratory obstruction is becoming acute. Cyanosis ▪ Can indicate hypoxia. ▪ Not always an accurate indication of the degree of airway difficulty. Clubbing of Fingers ▪ A change in the angle between the fingernail and nail bed because of increased capillary growth in the fingertips. Adventitious Sounds o Rhonchi - vibrations produced as air is forced past an obstruction, such as mucus in the nose or pharynx. o Stridor - harsher, strident sound on inspiration if the obstruction is at the base of the tongue or in the larynx. o Wheezing - expiratory whistle sound if an obstruction is in the lower trachea or bronchioles. o Rales - fine crackling sounds if the alveoli become fluid filled. Chest Diameter ▪ “Pigeon breast” - elongated anteroposterior diameter of the chest due to chronically trapped air in lung alveoli (hyperinflation). common disorders of the respiratory system in children 15 i. UPPER RESPIRATORY TRACT CHOANAL ATRESIA ➢ Congenital obstruction of the posterior nares by an obstructing membrane or bony growth, which prevents a newborn from drawing air through the nose and down into the nasopharynx 17 Cause & risk factors • Exact cause is unknown. • Thought to be a combination of genetic and environmental factors. • More common in females. • Higher risk if the birth parent takes certain thyroid medications during pregnancy • There are also potential links between choanal atresia and high pre-pregnancy intake of vitamin B12, zinc, and niacin. 18 19 Most common anomaly associated with choanal atresia presentation title SIGNS & SYMPTOMS • Chest retracts unless the child is breathing through mouth or crying. • Difficulty breathing following birth, which may result in cyanosis (bluish discoloration), unless infant is crying. • Inability to nurse and breathe at same time. • Inability to pass a catheter through each side of the nose into the throat. 20 Management & interventions ➢Assist in resuscitation if indicated. ➢Monitor vital signs closely. ➢Aid in providing supplemental oxygen. ➢Give intravenous (IV) fluid as ordered to maintain their glucose and fluid level until surgery can be performed. ➢Surgery is the only definitive treatment to correct the obstruction and restore airflow. 21 ACUTE NASOPHARYNGITIS ➢Also known as the “common cold” ➢ It is the most frequent infectious disease in children ➢Incubation period is typically 2 to 3 days 22 Cause & risk factors ▪ Viruses: rhinovirus, respiratory syncytial virus (RSV), adenovirus, parainfluenza viruses, influenza viruses ▪ Children who are in ill health from some other cause, or who have a compromised immune system, are more susceptible. 23 SIGNS & SYMPTOMS • Nasal congestion • Sore throat • Low-grade fever • Cough • Cervical lymph nodes • Watery rhinitis may be swollen and • Difficulty palpable breathing 24 Management & interventions ➢No specific treatment. ➢ Encourage increased fluid intake. ➢Remove nasal mucus via a bulb syringe ➢Emphasize before feeding (for infants) as needed. importance of hand hygiene. ➢Administer antipyretics for fever as ordered. ➢Educate parents regarding use of ➢Administer nasal saline drops/spray ➢ Place the child in a semi-Fowlers position using pillows to facilitate lung expansion. cool-mist vaporizers. ➢Caution parents not to give Aspirin for children below 18 years of age : Reye’s syndrome 25 TONSILLITIS ➢Inflammation of the tonsils, two oval-shaped pads of tissue at the back of the throat. ❖ Frequent tonsillitis: •More than 7 episodes in 1 year •More than 5 episodes a year during a 2-year period •More than 3 episodes a year during a 3-year period 26 Cause & risk factors • Most often caused by a viral infection (rhinovirus, adenovirus, respiratory syncytial virus or RSV) • Can also be caused by bacterial infection (group A streptococcus) o Risk factors: • Between ages 5 and 15 years • Crowded environments • Poor hand hygiene • Not able to complete the whole course of antibiotic (bacterial tonsillitis) 27 SIGNS & SYMPTOMS ▪ Red, swollen tonsils ▪ White or yellow coating or patches on the tonsils ▪ Sore throat ▪ Difficult or painful swallowing ▪ Enlarged, tender glands (lymph nodes) in the neck ▪ A scratchy, muffled or throaty voice ▪ Bad breath ▪ Stomachache ▪ Neck pain or stiff neck ▪ Headache ▪ Fever 28 ❑ In young children who are unable to describe how they feel, signs of tonsillitis may include: ▪ Drooling ▪ Refusal to eat Management & interventions ➢Encourage rest and plenty of sleep. ➢Provide adequate fluids. ➢Provide comforting foods and beverage. ➢Prepare a saltwater gargle. ➢Instruct parents to keep child away from irritants. ➢Medications: antipyretics, analgesics, antibiotics (if caused by bacterial infection) ➢Surgery: Tonsillectomy 29 Nursing interventions post-op (tonsillectomy) • Place the child prone or side-lying position. • Apply an ice collar postoperatively and administer pain medication as ordered. • Encourage the caregiver to remain at the bedside. • Give small amounts of clear fluids or ice chips when child is fully awake • Discourage the intake of: milk, ice cream, pudding, orange juice, lemonade. • Assess for subtle signs of hemorrhage. • Teach and demonstrate breathing exercises. • Have suction equipment available at the bedside - done only during an airway obstruction 30 presentation title CROUP ➢Inflammation of the larynx, trachea, and major bronchi. ➢Causes swelling in the airways and problems breathing. 31 Cause & risk factors Viruses that are known to cause croup are: • Children between 6 months and • Parainfluenza virus 3 years of age • Most common in boys • Respiratory syncytial virus (RSV) • Family history of croup or recurrent croup • Influenza virus • Adenovirus • Enteroviruses Risk factors: 32 SIGNS & SYMPTOMS • Barking cough (croupy cough) • Mildly elevated temperature Signs of severe croup include: • Inspiratory stridor • Marked retractions Fatigue Diminished breath sounds Hypoxia Cyanosis • Nasal flaring 33 Management & interventions ▪ Do not elicit a gag reflex in any child with a croupy, barking cough and provide comfort to prevent crying. ▪ Provide measures for a child to remain calm using distraction, toys, etc., while monitoring for respiratory changes. ▪ Place child in semi-upright position. ▪ Provide supplemental oxygen as ordered. ▪ Educate importance of proper hand hygiene and keeping child away from anyone that’s sick. Medications: • Inhaled bronchodilators – epinephrine, albuterol • Corticosteroids – dexamethasone • Antipyretics as needed 34 presentation title pharyngitis ➢ Infection and inflammation of the throat. ➢ More commonly known as sore throat. ➢ Although rare, streptococcal infections can lead to acute rheumatic fever and glomerulonephritis if not treated. 35 Cause & risk factors • Either bacterial or viral in origin oViral: rhinovirus, influenza, adenovirus, coronaviruses, and parainfluenza oBacterial: Group A β-hemolytic streptococcus (most frequently involved in bacterial pharyngitis in children) • May occur as a result of a chronic allergy Risk factors: • being between 5 to 15 years of age • close contact with infected individuals • being in small spaces with large groups of people • immunosuppression 36 SIGNS & SYMPTOMS ❖ Viral Pharyngitis: ❖Streptococcal Pharyngitis: • Markedly erythematous (bright red) back of the throat and palatine tonsil • Enlarged tonsils • White exudate in the tonsillar crypts • Petechiae on the palate • Child typically appears ill • Fever • Sore throat • Headache • Stomach ache • Difficulty swallowing • Scarlatiniform rash may develop • Sore throat • Fever • Rhinorrhea • Cough • General malaise • regional lymph nodes may be enlarged • Erythema in the back of the pharynx and the palatine arch • Exudate may or may not appear on the tonsils. 37 Viral pharyngitis resulting in visible redness 38 A case of strep throat Management & interventions ▪ Encourage warm salt water gargles. ▪ Encourage adequate oral hydration. ▪ Encourage rest. ▪ Ice collar may be applied to severe sore throats. ▪ Instruct child / parent to perform proper mouth care. ▪ Avoid exposure to environmental pollutants ▪ Instruct caregivers on the compliance of antibiotic treatment. Medications: Oral analgesic Antibiotics (penicillin, cephalosporin) – bacterial etiology 39