[ANESTHESIOLOGY] Preanesthetic Evaluation
Lecturer: Abigail Luna-Gomez MD
Transcriber: Patrick Angelo R. Bautista
References and Legends
nd
• {!} PPT and {"} Chapter 1 - Anesthesiology Manual 2 Ed
th
• {#} Miller’s Anesthesia 8 Ed
•
II.
PATIENT’S PERTINENT HISTORY
The first component of the Preoperative Evaluation of the patient is
that patient’s pertinent history.
• The anesthesiologist selects all of the vital medical conditions
(previous or present, acute or chronic, and treated or untreated)
that will have significant effects on the anesthetic management.
• This is an essential part of the evaluation that reduces
perioperative morbidity or mortality significantly.
• The healthcare provider has the opportunity to think and watch out
for all of the possible events or complications that may arise during
perioperative period, and to prepare necessary interventions
should these problems come.
•
{$} Transcriber’s Note
Table of Contents
I.
Preanesthesia Evaluation
II.
Patient’s Pertinent History
III.
Preoperative Physical Examination for Anesthesia
IV.
The Anesthetic Plan
V.
Conclusion of Preoperative Anesthetic Visit
August 2020
1
1
3
4
5
Parts of the Patient’s Pertinent History
1.
$ Scan the QR Code for the video lecture.
Note: You can use this only if you’re logged in to your FEU-NRMF Moodle
account and have access to the Anesthesiology Course.
I.
PREANESTHESIA EVALUATION
Importance of Anesthetic Evaluation
• Patient Safety
• Provider Safety
American Society of Anesthesiologists (ASA) Task Force Definition:
•
•
•
•
•
•
•
•
•
Systematic process of clinical assessment by the anesthesiologist
that precedes the delivery of anesthesia care for surgery and for
non-surgical procedures.
This applies to all ages who will undergo surgery requiring:
9 General anesthesia
9 Regional anesthesia
9 Monitored anesthesia care
Visit is usually done before the day of surgery.
Patient interview during preanesthetic evaluation includes:
9 Obtaining informed consent
9 Educating the patient
9 Enlightening the possible anesthesia risks and complications of
the anesthetic plan
It also reveals the patient’s current state of health as well as the
patient’s previous medical or surgical problems.
Information gathered in the history and PE will be combined with
the needs of the particular surgical procedure to come up with a
safe and effective delivery of anesthetic plan.
For instance, a proper patient and personnel safety equipment
should be given to cases involving highly communicable diseases.
In this aspect, the preanesthetic evaluation therefore significantly
improves the safety of both the patient and healthcare providers.
Overall, the primary goal of preanesthetic evaluation is:
9 To reduce the patient’s surgical and anesthetic morbidity and
mortality
•
•
•
•
•
•
2.
Brief description of initial symptoms leading to the surgical consult
Diagnostic tests done
Surgical evaluation and presumptive diagnosis
Initial treatments and outcomes
Any changes or significant trends in the vital signs
Significant fluid status and management of the patient
Co-existing Medical Illness
This covers all of the co-existing medical conditions of the patient
using the systemic “Organ System Approach”
• Co-existing cardiac, pulmonary, renal, hepatic, endocrine or
infectious diseases should be given importance.
•
3.
Medication History
Current medications taken by the patient and these includes:
9 Anti-hypertensives
9 Anti-anginas
9 Anti-arrhythmics
9 Anti-coagulants
9 Anti-convulsants
9 Endocrine maintenance medications
• Supplements and other herbal medicines are also noted as some
of these may have effects on coagulation, autonomic, liver and
kidney functions.
•
4.
•
•
•
•
•
5.
$ Scan the QR Code: Preanesthesia Evaluation sample
History of Present Surgical Illness
Allergies and Drug Reactions
These are the unusual, unexpected or unpleasant reactions to
perioperative medications.
These reactions are not that rare and may give rise to complications.
Patients with history of overt allergic reaction will volunteer the
information to the anesthesiologist.
It may be prudent to run down all of the drugs or substances that
will be used intraoperatively that the patient may have missed.
9 Latex from the gloves
9 Medical tapes / adhesives
9 10% Iodine
True allergic reactions
9 Observed when an administered agent (described by the
patient, documented in the medical chart or observed directly)
leads to systemic manifestations such as:
§ Pruritus, hives, facial or oral swelling
§ Shortness of breath, difficulty of breathing, wheezing
§ Vascular collapse
Anesthesia Exposure
The anesthesiologist focuses on the specifics of anesthesia.
The patient is asked for previous to anesthesia whether general or
regional for any previous procedures and the corresponding
reactions and complications if any.
• Since patients under general anesthesia are unconscious and may
not be aware of other vital information, obtaining information from
different helpful sources such as:
9 Previous anesthetic records
9 History from attending physicians / family members / relatives
•
•
Preanesthetic Evaluation | 1 of 5
Previous Anesthesia Records
The anesthesia record presents an overview of the patient’s
condition during the intraoperative event.
• Aside from the vital signs of the patient, fluid balance
management, interventions, type of anesthesia technique used,
manner of induction and complications are shown in detail.
• Medical records that may help the current anesthesiologist in the
pre-anesthetic evaluation of the following:
9 Response to sedative / analgesic pre-medications and
anesthetic agents
9 Note of difficulty of mask ventilation, the method of
laryngoscopy used, the size and type of laryngoscope blade
and endotracheal tube used
9 Note of difficulty of needle insertion, the technique used during
regional anesthesia and its outcome
9 Note of difficulty of insertion / placement of vascular access
and invasive monitoring
9 Perianesthetic complications
5.1
•
6.
Family History
It is important to take note of adverse anesthetic reactions or
outcomes among family members and relatives.
• This gives the anesthesiologist a chance to identify any familial
disease that may arise from exposure to certain anesthetic agents
and make necessary preparations / interventions.
• “Has anyone in your family or relatives experienced unusual or
serious reactions upon exposure to anesthesia”
• The predisposition to have Malignant Hyperthermia (MH) is a
familial disease which is present in some parts of the Philippines.
9 MH is a rare life-threatening anesthetic emergency with high
morbidity and mortality rates.
9 It manifests upon exposure to triggering factors such as volatile
anesthetics and succinylcholine.
•
7.
Social History
7.1
Perioperative Cigarette Smoking Risk
A study conducted by the American College of Surgeons National
Surgical Quality Improvement Program (2011) found out that
smokers had a higher mortality and increased rates of all types of
cardiorespiratory and septic complications.
There is a strong association between smoking and major adverse
surgical events that affects perioperative outcomes.
Cigarette, electronic cigarette (vape smoking) and tobacco:
9 Nicotine
§ Targets the sympathetic nervous system that causes
hypertension and tachycardia.
§ Impairs the ciliary motility, increases mucus production,
decrease clearing of secretions which makes the bronchial
tree irritable
9 Carbon monoxide
§ Displaces oxygen from the molecule of hemoglobin
producing a shift in the oxygen-dissociation curve to the left
which limits the oxygen availability to the tissues leading to
tissue ischemia.
Other effects of smoking:
9 Weak immune function
9 Delayed wound healing
9 Abnormal bone metabolism
9 Direct effect on the CNS which disturbs the pain perception
and opioid dose requirements
Last smoking history:
9 Patient is advised to stop smoking 2 months (8 weeks) prior
to an elective procedure to minimize wound-related and postoperative cardiopulmonary complications.
•
•
•
•
•
Illicit Substance Abuse
Can pose a threat upon exposure to anesthesia.
The type and degree of drug abuse, the time of last intake and
duration of abuse (acute vs. chronic) must be considered to avoid
deleterious outcomes that affects cardiovascular, pulmonary,
central nervous system, renal and hepatic system.
• Anesthetic management must be planned cautiously.
Marijuana
• Most popular recreational drug from the plant of Cannabis sativa.
• A hallucinogenic agent that can be smoked or be taken orally.
• If this is combined with anesthetic drug like diazepam, it increases
the sedative effect that enhance the depression of CNS.
• In addition, it also affects the cardiovascular system which also
enhances myocardial depression.
• Therefore, a potentiation drug interaction occurs between
anesthetic agents and cannabinoids.
Cocaine
• AKA the “rock” (cracked cocaine), the most serious health
concern worldwide extracted from the plant Erythroxylon coca.
• It is extremely addictive that it can be smoked, injected, snorted
and ingested orally.
• Cocaine interferes presynaptic uptake of sympathomimetic
neurotransmitters (norepinephrine, serotonin, dopamine) that
causes a euphoria due to free catecholamines.
• However, a patient under regional anesthesia may have both:
9 Hypertension due to peripheral vasoconstriction
9 Hypotension which may lead to cardiac dysrhythmias or
myocardial dysfunction
Club drugs
• Such as Lysergic acid (LSD), Phencyclidine (PCP),
3,4-Methylenedioxmethamphetamine (MDMA) – Ecstasy
• When taken orally, it causes:
9 Auditory, visual, tactile hallucinations
9 Distortions of body image, environment, reality
9 Anxiety and a “fear of going crazy”
• These drugs stimulate the sympathetic nervous system by causing
increase in blood pressure, heart rate and body temperature.
• Overdose with these medications can cause seizures, respiratory
depression, coma and eventually death.
• Patients scheduled for surgery with history of taking “club drugs”
within 24 hours will likely have autonomic dysregulation.
9 Erratic swings of BP with increased HR
9 Predisposes the patient to the following:
§ Risk of cardiomyopathy
§ Coronary and cerebral vasospasm
8.
Alcohol abuse each have its own anesthetic implications.
Obtaining an accurate history of alcohol aids to identify patients
who have greatest risk for postoperative complications.
• There is a great degree of unpredictability of effect of the
medications used in anesthesia for these patients even at clinical
doses and should therefore be adjusted accordingly.
• Example: Acute intoxication of alcohol
9 The requirement for an IV anesthetic to put this patient to sleep
will be less than a normal healthy patient.
• Postoperative morbidity complications of alcohol abuse:
9 Infection
9 Need of ventilatory support
9 Bleeding disorders
9 End-organ failure
9.
•
•
•
7.2
•
•
Alcohol Abuse
•
•
•
•
•
NPO “Non Per Orem” Status / Last Oral Intake
Preoperative fasting
9 Period of time before a surgery or a procedure when patients
are advised not to take any oral intake of solids and liquids so
as to prevent perioperative pulmonary aspiration.
Perioperative pulmonary aspiration
9 Presence of gastric contents in the lungs after induction of
anesthesia, during procedure or surgery or immediate
postoperative period
The 6-8 hours on NPO is observed in anesthesia practice for all
patients undergoing anesthesia to allow sufficient time for gastric
emptying to prevent aspiration during anesthesia.
During induction of anesthesia, the patient is rendered
unconscious and the protective reflexes of the airway are taken out
as well as the tone of the GIT sphincters.
This leaves the airway defenseless for secretions / gastric contents.
Aspiration of gastric contents, even if minimal, may result in
morbidity or mortality due to aspiration pneumonia.
Preanesthetic Evaluation | 2 of 5
10.
•
Review of Systems
4.
This part uncovers subjective findings that the patient may have
failed to mention but may point to dysfunction or disease.
9 General (including activity level): conscious, coherent,
oriented to time, place and person
9 Respiratory: shortness of breath, orthopnea, dyspnea
9 Cardiovascular: palpitations, chest heaviness
9 Renal: dysuria, hematuria, polyuria
9 GIT: hematemesis, melena, hematochezia
9 Hematologic: gum bleeding, nose bleeding
9 Neurologic: numbness, weakness in all extremities
9 Endocrine: excessive sweating, polydipsia
9 Psychiatric: visual and auditory hallucinations
9 Orthopedic: limitation of movement
9 Dermatologic: active skin dermatoses, pruritus
PREOPERATIVE PHYSICAL
EXAMINATION FOR ANESTHESIA
III.
The second component of the Preoperative Evaluation is the PE.
The preoperative PE must be aligned from the history gathered
and must focus on systems affected upon delivery of anesthesia.
• Patient’s baseline findings on vital signs, airway assessment,
examination of cardiorespiratory systems and other systems play a
crucial role during the perioperative anesthesia period.
• The following are the parts of the PE and its focus in anesthesia.
•
•
1.
•
2.
•
•
•
•
•
3.
General Survey
•
5.
6.
•
7.
8.
9.
The examination should focus on airway evaluation and the
predictors of difficult ventilation or difficult intubation.
• The most common classification used for airway evaluation is the
Mallampati Scoring
Back / Spine
Examination includes inspection for gross deformities and active
skin dermatoses that may be a contraindication for regional
anesthesia and palpation of the lumbar spine to assess ease or
difficulty of lumbar puncture.
Neurological Examination
Preoperative Tests are included for the purpose of identification
and verification of a disease or disorder that may affect during
perioperative anesthetic care and formulation of anesthetic plans
and alternatives for the proposed procedure.
• This part of the preanesthetic evaluation is often used to determine
fitness for surgery and anesthesia and to identify patients at high
risk of postoperative complications.
•
•
$ Scan the QR Code: Mallampati Classification
•
•
•
•
9.2
Uvula not visualized
No structures seen
only soft tissues
Figure 38-3. Mallampati classification: class I, soft palate, fauces, entire
uvula, pillars; class II, soft palate, fauces, portion of uvula; class III, soft
palate, base of uvula; class IV, hard palate only.
Preoperative Tests
•
9.1
Only base of uvula
visualized
The anesthesiologist determines the quality of the pulses as a
baseline for comparison intra-operatively, as well as the visibility
and palpability of the veins, at times an additional vascular access
is needed in the operating room.
A focused neurologic exam is performed to find any deficits that
may affect general and regional anesthesia techniques.
• More importantly, the neurologic exam is performed to obtain a
baseline, to determine any improvement or deterioration of
function in patients who will undergo neurosurgical procedures.
•
Soft palate, uvula,
and fauces seen –
tonsillar pillars not
visualized
Extremities
•
Head and Neck
Soft palate, uvula,
fauces and tonsillar
pillars are visualized
Abdomen
In the examination of the abdomen, the anesthesiologist gives
importance to any findings that may point to an increase in
intraabdominal pressure.
• Patients with an increase in IAP presents with numerous
anesthetic implications, depending on the level of pressure.
• These implications may translate to morbidity or even mortality if
not addressed properly.
• An example is the decrease in lung volumes and capacities in
patients with massive ascites.
9 These patients are more prone to desaturation and hypoxia
upon induction of anesthesia.
Indicates if patient is in or not in cardiorespiratory distress and
must state the degree of severity cardiorespiratory distress.
Height: cm | Weight: kg | BMI: kg/m2
Blood pressure in mmHg
Heart rate in beats per minute
Respiratory in cycle per minute
Pain score (level of pain) using 1-10 scale
9 0 – no pain; 10 – severe pain
The examination gives focus on the baseline findings of lung
expansion, chest rise, breath and heart sounds in search for any
abnormal findings that may warrant further preoperative testing.
•
•
Vital Signs
Chest and Lungs
•
•
Selection and Timing of Preoperative Tests
Surgeons and anesthesiologists and even patients request a full
panel of laboratory testing prior to surgery.
A lot of which may not give any important information that may
cause or prevent perioperative morbidity or mortality.
The ASA Task Force updated report (March 2012) on the
preanesthesia evaluation recommends that preoperative tests
should not be ordered routinely.
Routine test: defined as a test required in the absence of a
specific clinical indication.
Indications for routine testing must be based from:
9 Medical records
9 Physical examination
9 Patient interview
9 Type of surgical invasiveness
Indicated test: defined as a test that is requested for a specific
clinical purpose, for example, patients who are taking warfarin,
warrants a detailed coagulation studies
Hemoglobin / Hematocrit
A routine preanesthesia hemoglobin or hematocrit is not indicated.
Indications for hemoglobin and hematocrit includes:
9 Surgical invasiveness
9 History of anemia
9 Patients with liver disease
9 Bleeding / hematologic disorders
9 Extremes of age
Preanesthetic Evaluation | 3 of 5
Electrocardiogram
ECG is indicated for patients with:
9 Cardiocirculatory disease
9 Respiratory disease
9 Type of surgical invasiveness
• ECG abnormalities are common in older patients with multiple
cardiac risk factors as well.
9.3
•
9.4
•
Chest Radiographs
Preanesthesia chest radiographs are considered in patients with:
9 History of smoking
9 Recent upper respiratory infection
9 Chronic obstructive pulmonary disease (COPD)
9 Cardiac disease
Pulmonary Diagnostic Examinations
Pulmonary function tests, arterial blood gas monitoring
May guide anesthesiologists in planning and choosing the ideal
anesthetic for the patient.
• Clinical characteristics to consider include:
9 Surgical invasiveness
9 Interval from last evaluation
9 Resolved or symptomatic asthma or COPD
9 Scoliosis with restrictive function
9 Patients with critical illness
Class 1
Class 2
Class 3
9.5
•
•
10.
Class 4
Cardio-Pulmonary Evaluation
Not a “Clearance”
This is a referral by the surgeon, anesthesiologist or at times even
the patient himself to an internist, for the evaluation of the cardiac
and pulmonary status and the risk assessment of the patient for
the planned procedure.
• At present, there are a lot of cardio-pulmonary evaluation indices
and classifications being used in practice. Some examples are:
9 Goldman Multifactorial Risk Index
9 Eagle’s Cardiac Risk Index
9 AHA Cardiac Risk Classification
9 AHA Perioperative Risk Assessment
• When applicable other organ systems may be evaluated too, such
as an endocrinology clearance for patients with diabetes, thyroid
or adrenal diseases.
• The American Society of Anesthesiologists (ASA) has its own
physical status evaluation tool and this is what the Philippine
Society of Anesthesiologists (PSA) follow.
•
•
ASA Physical Status Classification (Updated 2014)
Class 1
A normal healthy patient
Class 2
A patient with mild systemic disease and no functional
limitations
Class 3
A patient with moderate to severe systemic disease that
results in some function limitation
Class 4
A patient with severe systemic disease that is a
constant threat to life and functionally incapacitating
Class 5
A moribund patient who is not expected to survive 24
hours with or without surgery
Class 6
A brain-dead patient whose organs are being harvested
“E”
If the procedure is an emergency, the physical status is
followed by an “E”
Class 5
Class 6
ASA Classes and Examples
Healthy, non-smoking, no or minimal alcohol use
Mild diseases only without substantive functional
limitations. Examples include but not limited to:
• Current smoker
• Social alcohol drinker
• Pregnancy
• Obesity (30 < BMI < 40)
• Well controlled DM / HTN
• Mild lung disease
Substantive functional limitation; ≥1 moderate to severe
diseases. This includes (but not limited to):
• Poorly controlled DM / HTN
• COPD
• Morbid obesity (BMI >40)
• Active hepatitis
• Alcohol dependence or abuse
• Implanted pacemaker
• Moderate reduction of ejection fraction
• ESRD undergoing regular hemodialysis
• Premature infant PCA <60 weeks
• History (>3 months) of MI, CVA or CAD / stents
Examples include (but not limited to):
• Recent (<3 months) MI, CVA, TIA or CAD/ stents
• Ongoing cardiac ischemia/ severe valve dysfunction
• Severe reduction of ejection fraction
• Sepsis, DIC, ARD or ESRD not undergoing regular
hemodialysis
Examples include (but not limited to):
• Ruptured abdominal aneurysm / thoracic aneurysm
• Massive trauma
• Intracranial bleed with mass effect
• Ischemic bowel in the face of significant cardiac
pathology or multiple organ system dysfunction
A declared brain-dead patient for organ donor purposes
IV.
•
•
•
•
•
THE ANESTHETIC PLAN
In the formulation of an anesthetic plan, the anesthesiologist
should take into consideration of all of the following factors:
9 The age of patient
9 Physical status of patient
9 The type of surgery or procedure to be performed
9 The skill and requirement of the surgeon
9 The skill and preference of the anesthesiologist
9 The patient’s preference and wishes
After considering all of these factors, the anesthesiologist decides
which technique is safest for the patient and most effective for the
procedure.
Good communication is very important between the surgeon and
anesthesiologist at this point.
Multidisciplinary preoperative conferences (with the surgeon,
anesthesiologist, other attending physicians and the patient and
his family) are held when necessary to discuss important aspects
of the procedure which includes the possible complications, risks
and outcomes.
This is held to address concerns, to manage expectations, to
answer questions that may be present and to ensure that every
member of the team including the patient is on-board.
$ See next page for the Algorithm
Preanesthetic Evaluation | 4 of 5
Figure 38-1 Mechanisms by which preoperative evaluation can help
influence and improve perioperative care.
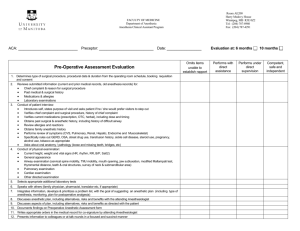
V.
•
•
•
•
•
CONCLUSION OF PREOPERATIVE
ANESTHETIC VISIT
The anesthesiologist summarizes pertinent findings from the
history, physical exam and laboratory testing on the Pre-Anesthetic
Evaluation Form to be inserted in patient’s chart / medical record.
The anesthesiologist orders additional laboratory or diagnostic
tests that are necessary and that will contribute in the perioperative
evaluation and management
The anesthesiologist writes the pre-anesthesia medication orders.
The goals of giving preoperative medications are the ff:
9 To decrease anxiety
9 To provide analgesia
9 To decrease oral secretions
9 To decrease the risk of aspiration
9 To control sympathetic stimulation (increased HR and BP)
The anesthesiologist gives instructions to the patient.
9 Instructions on placing the patient on NPO / fasting status
9 Instructions on which maintenance medications should be
continued or discontinued (anti-hypertensives, oral
hypoglycemic, etc.)
9 Instructions on giving premedications. The patient is not
allowed to ambulate after giving premedications due to the
sedative and autonomic effects of the drugs.
9 Other instructions given for special procedures.
The anesthesiologist and the patient ratify the Informed Consent.
Consent stated that the anesthesiologist explained the
management plan, including the possible risks and outcomes, and
the patient has understood and accepted the management.
$ No proofreading. Use at your own risk.
No samplex attached. Good luck!
Preanesthetic Evaluation | 5 of 5