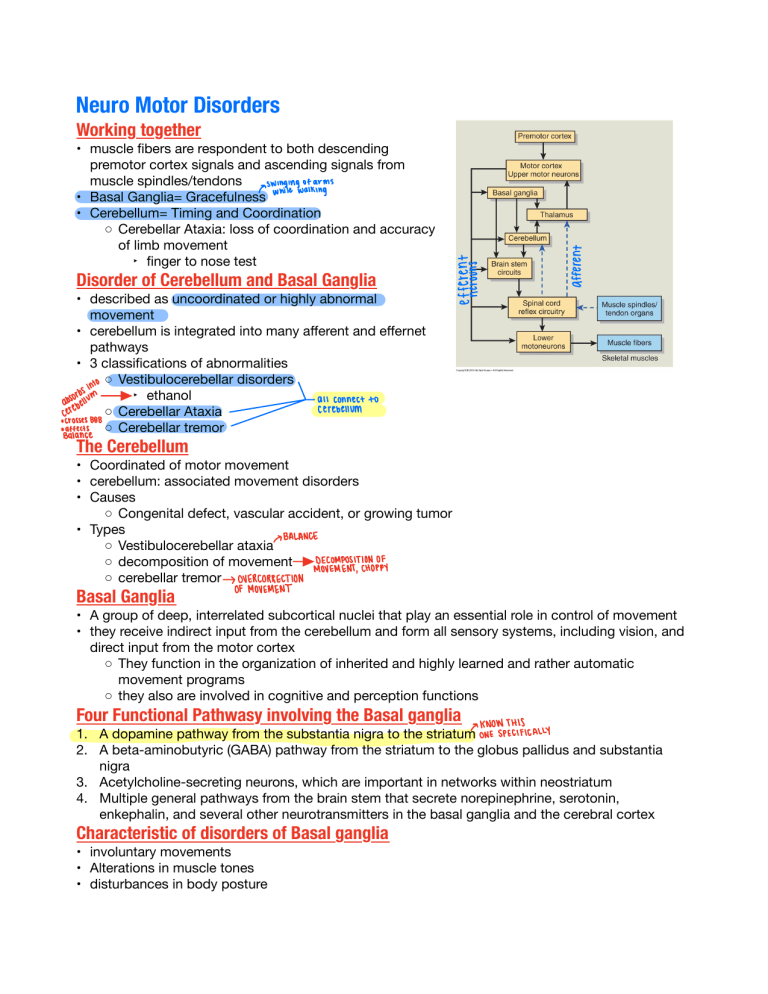
Neuro Motor Disorders Working together • muscle bers are respondent to both descending premotor cortex signals and ascending signals from muscle spindles/tendons MY'hitentiatiings • Basal Ganglia= Gracefulness • Cerebellum= Timing and Coordination ◦ Cerebellar Ataxia: loss of coordination and accuracy of limb movement ‣ nger to nose test Disorder of Cerebellum and Basal Ganglia • described as uncoordinated or highly abnormal movement • cerebellum is integrated into many a erent and e ernet pathways • 3 classi cations of abnormalities ◦ Vestibulocerebellar disorders ‣ ethanol anconnectto cerebellum ◦ Cerebellar Ataxia ssesooo ◦ Cerebellar tremor ÉÉ É Itis Ente The Cerebellum • Coordinated of motor movement • cerebellum: associated movement disorders • Causes ◦ Congenital defect, vascular accident, or growing tumor • Types BALANCE ◦ Vestibulocerebellar ataxia ◦ decomposition of movement Decomposition of MOVEMENTCHOPPY ◦ cerebellar tremor OVERCORRECTION OFMovement Basal Ganglia • A group of deep, interrelated subcortical nuclei that play an essential role in control of movement • they receive indirect input from the cerebellum and form all sensory systems, including vision, and direct input from the motor cortex ◦ They function in the organization of inherited and highly learned and rather automatic movement programs ◦ they also are involved in cognitive and perception functions Four Functional Pathwasy involving the Basal ganglia KNOW THIS 1. A dopamine pathway from the substantia nigra to the striatumonespecifically 2. A beta-aminobutyric (GABA) pathway from the striatum to the globus pallidus and substantia nigra 3. Acetylcholine-secreting neurons, which are important in networks within neostriatum 4. Multiple general pathways from the brain stem that secrete norepinephrine, serotonin, enkephalin, and several other neurotransmitters in the basal ganglia and the cerebral cortex Characteristic of disorders of Basal ganglia • involuntary movements • Alterations in muscle tones • disturbances in body posture lithium cancauseParkisonlikesymptoms dehydration an SIGNSISYMPTOMS snuffle of fingers Parkinson's Disease cant holditems functions motor De nition fidgeting hands i muscle smiling • a degenerative disorder or basal ganglia function that results in variable combinations of tremor, rigidity, bradykinesia, and postural changes Characteristics • progressive destruction of the nigrostriatal pathway, with subsequent reduction in striatal concentrations of dopamine Clinical Syndrome communication • Parkinsonism- dopamine depletion results from degeneration of the dopamine nigrostriatal system Pathophysiology PRICEY IneREAL DOPAMINE Housey betweenhere and pathogenesis •I Idiopathic destruction of neuronal cells in sunstantia nigra • decreased dopamine stores 2 • breakdown of dopaminergic nigrostriatal pathway 3 4• imbalance between EXCITATORY and INHIBITORY pathways, more excitatory Also hasAcetylcholine EXCITATORY •5 Resulting in abnormal movements A◦ resting tremor B◦ increased muscle tone (rigidity) C◦ slow movement (bradykinesia) D◦ postural changes • Slowly progressive, tremor often begins in hands, then 6 generalized How Parkinson Drugs Work • Act of 2 Pathways ◦ Increase functional ability of under active dopaminergic thoughcellsarebreakingdownwecana concentrationof system even bcuzreceptors dopamine arestillthere ‣ Carbidopa/Levodopa increase dopamine Dopa a cross not ‣ Dopamine agonist- stimulate dopamine receptors but Balone combo in ‣ Monoamine Oxidase Inhibitors (MAOI) - slow n inside nonce converts breakdown of dopamine me y form ntoactive ◦ Reduce excessive excitatory cholinergic neurons ‣ Benztropine- lessen tremors and rigidity • Dopamine is a BLOCKSRECEPTORS neurotransmitter both haptic inhibitory and excitatory. In 419ft regard to Parkinson's by go increased dopamine we or inhibit uncoordinated movements TROPINE vest ionaboutBenz vest ionaboutCARBIDOPAILEVADOPA Drawbacks to Medication yclemesseswith • ON and OFF Phenomenon sleepcuptake drug • Frequent unpredictable uctuations in motor movements during the day • ON period dyskinesia (peak level of drug on blood) • OFF period bradykinesia (low drug level) • Possible need for Deep Brain Stimulation ◦ Implantation of electrodes, connects to a generator and delivers electrical stimulation to block the abnormal nerve activity that causes tremor 1mV Parkinson's Curable? • • • • not yet manage symptoms it is a progressive disease current research looking at Stem Cell Therapy Multiple Sclerosis VERY PROGRESSIVE • A demyelinating disease of the CNS • Most common non-traumatic cause of neurologic disability among young and middle aged adults • characterized by exacerbations and remissions over many years in several di erent sites in the cns • Initially, there is normal or near-normal neurologic function between exacerbations • as the disease progresses, there is less improvement between exacerbations and increasing neurologic dysfunction De nition • A degenerative disorder of demyelination of the CNS whitechanges tograymatter Characteristics • in ammation and destruction of mostly that white matter of the CNS myelin, the PNS is psread with no injury • onset age of 20-30 years old, women 2x as likely as men- unknown why Risk Factors ruststatistics • Northern European Ancestry, uncommon in Asian, African, Continental American Ancestries • Family History (10-20% increase in risk) • Human Leukocyte Antigen HLA-DR2 haptotype relatedtogenotype Pathogenesis can turnsonimmunesystem gogetscreenedforityantigenresponsetoproteinbacteriacoldillnessanything that • Immune-mediated disorder that occurs in people who are genetically susceptible • an immune response to a protein in the CNS CNS Pathophysiology of nerve bers in the white matter of the brain, spinal cord, and optic nerve 1•• Demyelination signal conduction abnormalities- block or slowed speed 2 • demyelinated patches are visible throughout the- white matter- PLAQUES or LESIONS 3 • it is theorized that lesions have proteolytic enzymes, macrophages, lymphocytes and plasma cells 4 • key precursor is in 5 ammation Signs and Symptoms demyelination net • Symptoms vary depending on location and extent of lesion t • Common problem areas ◦ optic nerve (vision)PERKEY YINING'T614 ◦ Corticobulbar tracts (Speech and swallowing) ◦ Spinocerebellar tracts (balance) ◦ Medical Longitudinal fasciculus (eye muscle movement)EYEDEVIATION ofeye nomusiecontraction muscle right eyeshiftstoleftor where cant find isat thenose correction over normalflarein except inbabies FLAREout How is it treated • Currently NO CURE • Treatment based on course of disease ◦ relapsing-remitting ◦ secondary progressive ◦ primary progressive macrophages myelinated ton de igo nto getting oligits ◦ progressive relapsing • Corticosteroids are the main treatment lessinflammation • Other Drugs Classes systemsuppression tolittleleadtoimmune ◦ interferon Beta A: immune system cytokine booster ◦ Glatiramer Acetate: synthetic polypeptide that stimulate myelin growth and acts as myelin decoy blocking T cells ◦ Natalizumab: suppresses givencanmake leukocyte entry into CNS ptmoreopentoinfection Spinal Cord Injury oftheaxon opens upfor tea tore macrophages forrepair outifnothingto enzymes repairinflamation De nition • SCI represents damage to the neural pathway of the spinal cord • PRIMARILY A DISORDER OF YOUNG PEOPLE 29-42 • Motor vehicle crash, falls, violence (gunshot/stabbing), or recreational sports Characteristics • Most SCI involve damage to the vertebral column or ligaments as well as the spinal cord ◦ Recall-> a erent sensory neurons and frombreakagedownwardsgetsinjuredto orsome sortofimpact lower motor neurons communicate with CNS ◦ Injury will commonly involve both sensory cz.cznerve connects plexus and motor function changes todiaphram breakage can Clinical Syndrome ingpiectith't • Immediate response is referred to as SPINAL SHOCK ◦ Flaccid paralysis with loss of tendon re exes below the level of injury and loss of bowel and bladder function. It includes loss of systemic vasomotor tone • Depends on level of Injury ----------->>>>>>>> sympathetic nervous system Pathophysiology of SC injury 1.Initial injury at time of incident & irreversible 2. Small hemorrhages in gray matter of cord 3. Edematous changes in the white matter that lead to necrosis of neural tissue 4. The severity of injury depends on the mechanical way it happened: a. Compression divingfallingheadfirst b. Stretch overextending c. Shear/Laceration d. Dislocation of Vertebrae e. Contusions bruising AFTER 1.Secondary injury promotes the spread of the initial injury 2. Recall Spinal Shock a. loss of vasomotor tone b. loss of neural re exes below the level of injury 3. Release of vasoactive agents & cellular fromprimar enzymes (in ammation) leads to inflammation sendary torepair will cause actually demyelination & necrosis in neural tissue demyelination 4. Vessel trauma & hemorrhage causing ischemia, increased vascular permeability, and edema 3 Important Changes in SCI • • • • Similar bu di erent SPINAL SHOCK: T6 and up NEUROGENIC SHOCK: T5 and up AUTONOMIC DYSREFLEXIA: T6 and up Spinal Shock "T6 and Above" • Flaccid paralysis with loss of tendon re exes below the level of injury and loss of bowel and bladder function, It includes loss of systemic vasomotor tone. • Can last for hours, days, or weeks • Usually if re exes return/recover by the time patient gets to hospital, neuromuscular changes are reversible (good sign) IFoccursrightawaynormally thesefunctionsback good signthattheywillget ◦ Common in football players or boxing ghters • If re exes do not return ->> hypotension and bradycardia may manifest Neurogenic Shock • Spinal Cord Injury above T5 • imbalance between sympathetic and parasympathetic stimuli • more parasympathetic innervation causing massive vasodilation (LOW BP) and decreased tissue perfusion lossofconnectiontoorgansthatsend • medical EMERGENCYsignal brainaboutHypotension to and Autonomic Dysre exia "T6 and Above" • Better known as Autonomic Hyperre exia- an acute episode of exaggerated sympathetic re ex response • occurs in people with injuries at T6 and above, in which CNS control of spinal re exes is lost • Does not occur until spinal shock is resolved and autonomic re exes return • occurs 6months to 1 year after initial injury exageratedsympatheticresponse Characteristics THINKFIGHT • Massive sympathetic response "think ght response" ◦ Mild to severe hypertensionvery THR3BP ◦ skin pallor, pale and cool BELOWINJURY ◦ goosebumps (Piloerection) VASOCONSTRICTION • Baroreceptors (blood pressure sensors) are innervated by cranial nerves and will stimulate a severe vagal response slowing of heart rate VAGUS (bradycardia) in the presence of sustained NERVEX hypertension canSlowHRsoslowPt • Emergency cangointocardiacarrest • Treatment: remove stimuli initiating the hyperre exia oftenhasissuesw bladder overfilling Stimuli d • Usually a full bladder but can also be: ◦ Visceral distention of rectum (constipation) ◦ Stimulation of pain receptors (pressure ulcers) ◦ Visceral contractions ‣ ejaculation ‣ bladder spasm ‣ uterine contractions