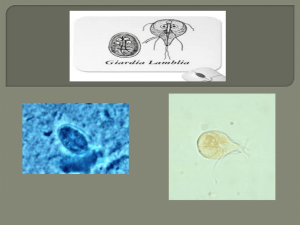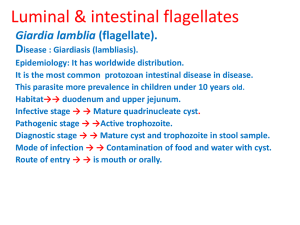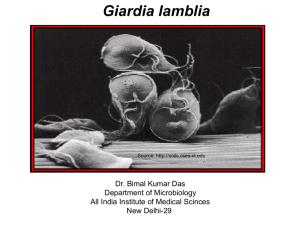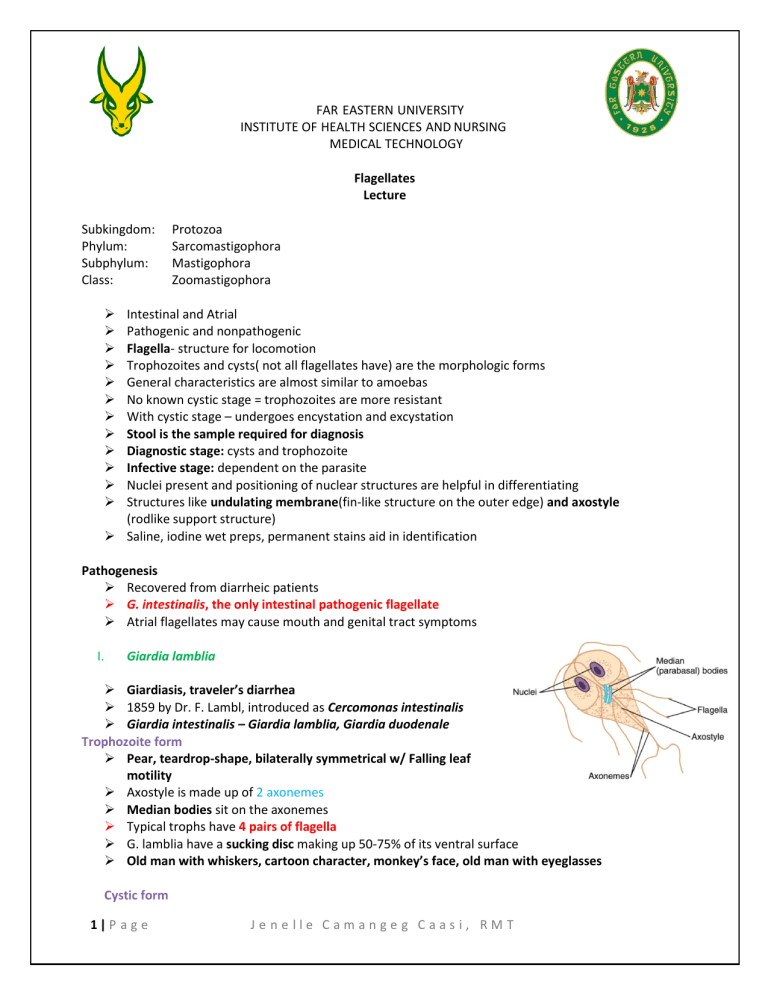
FAR EASTERN UNIVERSITY INSTITUTE OF HEALTH SCIENCES AND NURSING MEDICAL TECHNOLOGY Flagellates Lecture Subkingdom: Phylum: Subphylum: Class: Protozoa Sarcomastigophora Mastigophora Zoomastigophora Intestinal and Atrial Pathogenic and nonpathogenic Flagella- structure for locomotion Trophozoites and cysts( not all flagellates have) are the morphologic forms General characteristics are almost similar to amoebas No known cystic stage = trophozoites are more resistant With cystic stage – undergoes encystation and excystation Stool is the sample required for diagnosis Diagnostic stage: cysts and trophozoite Infective stage: dependent on the parasite Nuclei present and positioning of nuclear structures are helpful in differentiating Structures like undulating membrane(fin-like structure on the outer edge) and axostyle (rodlike support structure) Saline, iodine wet preps, permanent stains aid in identification Pathogenesis Recovered from diarrheic patients G. intestinalis, the only intestinal pathogenic flagellate Atrial flagellates may cause mouth and genital tract symptoms I. Giardia lamblia Giardiasis, traveler’s diarrhea 1859 by Dr. F. Lambl, introduced as Cercomonas intestinalis Giardia intestinalis – Giardia lamblia, Giardia duodenale Trophozoite form Pear, teardrop-shape, bilaterally symmetrical w/ Falling leaf motility Axostyle is made up of 2 axonemes Median bodies sit on the axonemes Typical trophs have 4 pairs of flagella G. lamblia have a sucking disc making up 50-75% of its ventral surface Old man with whiskers, cartoon character, monkey’s face, old man with eyeglasses Cystic form 1|P a g e Jenelle Camangeg Caasi, RMT Colorless, smooth cyst wall Retracted cytoplasm = clearing zone, achieved through formalin preservation 4 nuclei, 4 median bodies seen in iodine wet prep/permanent stains Diagnostic specimen of choice: Stool, multiple samples = cysts and trophs Duodenal aspirations, SI biopsies are also collected. String test/ Enterotest, RT-PCR EIA, ELISA, Direct fluorescence, Giardia Western immunoblotting Life Cycle 1. Giardia cysts can contaminate food, water, and surfaces, and they can cause giardiasis when swallowed in this infective stage of their life cycle. Infection occurs when a person swallows Giardia cysts from contaminated water, food, hands, surfaces, or objects. 2. When Giardia cysts are swallowed, they pass through the mouth, esophagus, and stomach into the small intestine where each cyst releases two trophozoites through a process called excystation. The Giardia trophozoites then feed off and absorb nutrients from the infected person. 3. Giardia trophozoites multiply by splitting in two in a process called longitudinal binary fission, remaining in the small intestine where they can be free or attached to the inside lining of the small intestine. 4. The Giardia trophozoites then move toward the colon and transform back into cyst form through a process called encystation. The Giardia cyst is the stage found most commonly in stool. 5. Both Giardia cysts and trophozoites can be found in the stool of someone who has giardiasis and may be observed microscopically to diagnose giardiasis. Giardia cysts are immediately infectious when passed in the stool or shortly afterward, and the cysts can survive several months in cold water or soil. Epidemiology Worldwide in streams, lakes, other water sources Most common intestinal parasite especially among children Cysts are resistant to routine chlorination Transmitted through eating contaminated fruits and vegetables Oral-anal sexual practices, fecal-oral route Higher risks: Day care center kids, poor sanitary households, drinking contaminated water in endemic areas, unprotected sex esp in homosexual men. Reservoir hosts: Beavers, muskrats, water voles, domestic sheep, cattle, and dogs and can transmit it directly to humans. Clinical Symptoms Only known pathogenic intestinal flagellate Asymptomatic carrier Mild diarrhea, abdominal cramps, anorexia, flatulence to tenderness of epigastric region, steatorrhea, and malabsorption syndrome. Fat soluble vitamin deficiencies, hypoproteinemia with hypogammaglobulinemia, folic acid deficiencies, and structural changes in intestinal villi 2|P a g e Jenelle Camangeg Caasi, RMT Incubation period: 10-36 days. Px with intestinal diverticuli or an IgA deficiency are susceptible to reoccurring infections. Hypogammaglobulinemia may predispose to Giardia and achlorhydria. Treatment CDC: • • • FDA: • • Metronidazole Tinidazole Nitazoxanide Tinidazole Nitazoxanide Prevention and Control Proper water treatment Good personal hygiene Proper cleaning and cooking of food Avoidance of unprotected oral-anal sex Portable water purification systems II. Chilomastix mesnili Nonpathogenic Trophozoite form Pear-shaped, stiff rotary motility in a directional manner( corkscrew motility) Have 4 flagella, 3 of it seldom stain extends upto anterior end. Has a rudimentary mouth called cytostome Cystic form Lemon-shaped, clear hyaline knob for cysts Diagnosis Diagnostic stage: Freshly passed liquid stool = Trophs Formed stool = Cysts Iodine wet preparation demonstrates organisms features clearly Infections are asymptomatic Epidemiology Cosmopolitan in warm climates. Poor sanitary conditions and personal hygiene Mode of transmission Hand-to-mouth contamination/contaminated food/drink with infective cyst III. Dientamoeba fragilis Initially classified as an ameba because of pseudopodia. Amoeboflagellate Trophozoite form Irregular and roundish in shape, motility is seen on freshly passed stool by broad hyaline pseudopodia Stain of choice: Iron hematoxylin No known cyst stage 3|P a g e Jenelle Camangeg Caasi, RMT Diagnostic identification of D. fragilis is through the exhibition of Hakansson phenomenon when the parasite is mounted in water preparations. Method of choice for diagnosis: Stool examination Unknown mode of transmission Unproven theory for MOT is: transmission with the eggs of E. vermicularis and A. lumbricoides D. fragilis were identified in patients infected with E. vermicularis in a several studies At risk demographics include: children, homosexual men, semicommunal groups, and institutionalized people. Clinical Manifestations: Mode of transmission: fecal-oral, oral-anal routes, person-toperson routes Infected patients may experience diarrhea and abdominal pain, may also include bloody or mucoid stools, flatulence, nausea, or vomiting, weight loss, and fatigue. Some patients experience diarrhea alternating with constipation, low grade eosinophilia, and pruritus. Treatment: • Iodoquinol is the treatment of choice for such infections • Tetracycline is the acceptable alternative • Paromomycin (Humatin) is another alternative if both aforementioned treatments are inappropriate. Prevention and control • Maintaining personal hygiene and sanitary public conditions aid in preventing in this infection; avoidance of unprotected homosexual practices also helps minimize infections. IV. Trichomonas hominis Pear-shaped with jerky motility with the assistance of full-body length undulating membrane. Equipped with a costa, rod-like structure at the undulating membrane base. The troph is supported by an axostyle that extends beyond the posterior of the body. Cone-shaped cytostome cleft may also be present Troph has 3-5 flagella and no known cystic stage Stool examination is the method of choice for T. hominis recovery Epidemiology Found worldwide in cosmopolitan warm and temperate climates Children in warm climates are at a higher risk of contracting infection 4|P a g e Jenelle Camangeg Caasi, RMT MOT: Ingestion of trophozoites, contaminated milk may be suspected to harbor the parasite, fecal-oral transmission may also occur With patients suffering from achlorhydria, the contaminated milk may shield the parasite when it is ingested Treatment is not indicated because T. hominis is nonpathogenic. V. Enteromonas hominis Trophozoite form: Oval in shape and exhibits jerky motility. May also been in a form of half-circle, flattened on one side. 4 flagella present in the anterior end Posterior end may come together to resemble a small tail structure. Binucleated cyst form of this parasite is more common, with the nucleus appearing on opposite ends; quadrinucleated cyst may also be present. Cystic form: Cysts are protected by a well-defined cell wall The size range of this parasite overlaps with Endolimax nana Stool examination is the method of choice in recovery of this parasite, but difficult to identify due to small size. Primary cause of contraction is the ingestion of infected cysts. Treatment is not indicated since this is nonpathogenic. VI. Retortamonas intestinalis Ovoid shape with jerky motility as a trophoizoite Fine delicate ring of chromatin granules may be visible on the nuclear membrane. Lemon to pear-shaped cyst Two fused fibrils resembling a bird’s beak appearance Stained stool appearance is the best sample to examine Existence has been documented in warm and temperate climates MOT: Ingestion of infected cysts Psych hospitals and crowded conditions residences have reported to contract this parasite VII. Trichomonas tenax Trophozoite is described as being oval to pear-shaped T. tenax trophozoite is equipped with five flagella An undulating membrane that extends two thirds of the body length A small anterior cytostome is located next to the axostyle, opposite the undulating membrane. No known cystic stage T. tenax trophozoites survive in the body as mouth scavengers Smallest Trichomonas T. tenax trophozoite is mouth scrapings. Microscopic examination of tonsillar crypts and pyorrheal pockets Tartar between the teeth and gingival margin of the gums are the primary areas of the mouth that may also potentially harbor this organism. 5|P a g e Jenelle Camangeg Caasi, RMT MOT: the use of contaminated dishes and utensils, as well as introducing droplet contamination through kissing VIII. Trichomonas vaginalis Persistent urethritis, persistent vaginitis, infant Trichomonas vaginalis infection are most common associated with this parasite. ovoid, round, or pearlike in shape with rapid jerky motility accomplished with the aid of the organism’s 4-6 flagella No known cystic stage T. vaginalis trophozoites reside on the mucosal surface of the vagina in infected women. The growing trophozoites multiply by longitudinal binary fission and feed on local bacteria and leukocytes. trophozoites thrive in a slightly alkaline or slightly acidic pH the prostate gland region and the epithelium of the urethra is the most common site as for males MOT: sexual intercourse may also migrate through a mother’s birth canal and infect the unborn child. T. vaginalis is known to be transferred via contaminated toilet articles or underclothing. Sharing of douche supplies, as well as communal bathing, are also potential routes of infection. Persistent or recurring urethritis is the condition that symptomatic men experience as a result of a T. vaginalis infection Involvement of seminal vesicles, higher parts of the urogenital tract, and prostate may occur in severe cases of infection. Release a thin, white urethral discharge that contains the T. vaginalis trophozoites. Persistent vaginitis, found in infected women, is characterized by a Foul smelling, greenish-yellow liquid vaginal discharge after an incubation period of 4 to 28 days. Burning, itching, and chafing may also be present. Red punctate lesions may be present upon examining the vaginal mucosa of infected women. Urethral involvement, dysuria, and increased frequency of urination are among the most commonly experienced symptoms. Cystitis is less commonly observed but may occur. T. vaginalis has been recovered from infants suffering from both respiratory infection and conjunctivitis. T. vaginalis trophozoites migrating from an infected mother to the infant through the birth canal and/ or during vaginal delivery. T. vaginalis infections is the avoidance of unprotected sex. In addition, the prompt diagnosis and treatment of asymptomatic men is also essential. There is evidence to suggest a connection between T. vaginalis infections and cervical carcinoma. 6|P a g e Jenelle Camangeg Caasi, RMT