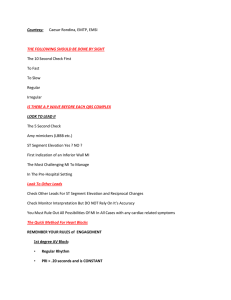
Cardiac Conduction Disorders Atrial fibrillation, atrial flutter, heart blocks, ventricular arrhythmias, ICDs and Pacemakers Dysrhythmias & Conduction Problems Related to CAD, MI & Cardiac Surgery Dysrhythmias • Atrial Fibrillation • Atrial Flutter • Premature Ventricular Contractions • VT • VF • PEA • Asystole Conduction Problems • 1st Degree AV Block • 2nd Degree AV Block Types I and II Premature Atrial Complexes • Rhythm – regular/irregular • If there are > 30 PACs/hour or if there is a run of >20 PACs CO is affected, risk for death and stroke rises 60% and there is a 2.7fold increase in the development of AF • Rate- normal • Take apical pulse for a full minute for any irregular pulse • Clues & Causes – no clear cause, no health risks • In most cases PACs are not a sign of heart disease. Common in CM • Treatment – Lifestyle changes for risk factors • No smoking, loose weight if overweight, heart healthy diet, exercise regularly, limit alcoholic drinks to a maximum of 1 drink/day for women and 2 drinks/day for men (varies with individual) • Nursing Implications • If patient is symptomatic (presyncope, syncope, angina, dyspnea) expect treatment with calcium channel blockers or beta blockers . Premature Atrial Complexes Rhythm: Irregular Rate: >150 (depends on AV conduction) Cues & Causes • CAD, HTN, mitral or tricuspid valve disease, PE, CM, pericarditis, hypoxia, hyperthyroidism • Emotional triggers, exhaustion, caffeine, sleep deprivation, hormonal, alcohol, surgery or medical procedures Atrial Fibrillation Treatments • Control rate • Rhythm conversion • Prevent thrombus formation • Surgical ablation Nursing Implications • Assess patient for SOB, decreased energy, fatigue, “feeling beats” especially in neck or temple region (palpitations), chest pain, light headedness, syncope, decreased ability to exert • Anticoagulant therapy • Bridges Atrial Fibrillation Atrial Fibrillation • Treatment • Anticoagulants • to prevent embolization • Beta-Blockers • to block the effects of certain hormones on the heart and slow the heart rate • Calcium Channel Blockers • to help slow the heart rate by blocking the number of electrical impulses that pass through the AV node into the ventricles • Digoxin to help slow the heart rate by blocking the number of electrical impulses that pass through the AV node into the ventricles • Electrocardioversion • is a procedure in which electric currents are used to reset the heart’s rhythm back to a regular pattern • Catheter or Radiofrequency Ablation • is a procedure which works by scarring or destroying tissue in your heart to disrupt faulty electrical signals causing the arrhythmia Atrial Fibrillation & Anticoagulants • Coumadin/ Warfarin • Newer Anticoagulant Drugs • Dibigatran (Pradaxa ®) • Direct thrombin inhibitor • No routine lab tests or diet restrictions • 150 mg orally twice a day (check renal function) • Riaroxaban (Xarelto ®) • Factor Xa inhibitor • 20 mg orally once daily • Apixaban (Eliquis ®) • Factor Xa inhibitor • 5 mg orally twice daily Atrial Flutter • Rhythm: Regular or regularly irregular • Rate: 75-150 (depends on A-V conduction) • Atrial rate 200-300 • Ventricular rate varies depending on A-V ratio • Cues & Causes • PE, thyrotoxicosis, ischemic heart disease, hypoxia, quinidine toxicity, post cardiac surgery • Treatment • Control rate • Rhythm conversion • Prevent thrombus formation • Surgical ablation successful in 80-90% cases • Nursing indications Atrial Flutter Premature Ventricular Contraction • Rhythm • Rate • Clues & Causes • Treatment • Nursing Implications Premature Ventricular Contraction Ventricular Tachycardia • Rhythm • Rate • Clues & Causes • Treatment • Nursing Implications Ventricular Tachycardia Ventricular Fibrillation • Rhythm • Chaotic • Rate • None, non discernable • Cues & Causes • • • • No P, P-R interval, atrial rate or QRS duration Ischemic heart disease, cardiomyopathy, myocarditis ST elevation with BBB in V1-V3 = Brugada Syndrome < 40 • Treatment • CPR, precordial thump, defibrillation, medications • Nursing Implications • Assess patient NO palpable pulses • ABC • Call code/ask for AED Arrhythmias Don’t Delay Defibrillation Antiarrhythmic drugs Sudden death V fib, pulseless, V tach, asystole Decrease CO Blocks, atrial arrhythmias, PVC’s Prophylactic Beta blockers, antiarrhythmics V fib: Epinephrine Amniodarone/Lidocaine Vasopressin • Rhythm • Regular • Rate • 60-100 1st Degree Heart Block • Cues & Causes • P waves normal; PR interval > 0.20 seconds in sinus rhythm of some sort; QRS interval < 0.12 seconds • May be normal finding in people without cardiac history/athletes • AV node injury/ischemia, medications, rheumatic heart disease, hyperkalemia, MI, digoxin toxicity • Treatments • Treat the cause • Nursing Indications • Patient may be asymptomatic • Monitor with MI 2nd Degree Heart Block Types I & II • Rhythm: • Mobitz Type I/Wenckebach: Irregular • Mobitz Type II: Irregular • Rate • Mobitz Type I/Wenckebach: varies, slow, atrial rate greater than ventricular rate • Mobitz Type II: varies, slow, atrial rate greater than ventricular rate • Cues & Causes • Mobitz Type I/Wenckebach: P waves normal/ plot through; PR lengthens with each cycle until a QRS drops then shorter again; QRS usually 0.10 seconds or less but is periodically dropped • Mobitz Type II: P waves normal/plot through; PR WNL or slightly prolonged; QRS usually 0.10 or greater and periodically absent after P waves • Anterior MI (LCA supplied), Type II from myocarditis • Treatments • Pacemaker placement • Nursing Indications • May rapidly progress to complete HB without warning • Patient response to dysrhythmia is related to ventricular response, assess for low BP, SOB, pulmonary congestion, decreased LOC nd 2 Degree AV Block • Rhythm: Atrial regular & ventricular regular • Rate: Atrial rate that of underlying rhythm; ventricular rate 40-60if originated in AV node; 20-40 if originates in ventricular muscle 3rd Degree Heart Block • Cues & Causes • P waves normal; PR interval varies; NO relationship between P waves and QRS complexes; QRS depend on where they originate • Acute MI (inferior) • Treatments • Atropine • Temporary pacemaker & permanent pacemaker • Nursing Indications • Assess patient and determine affect rhythm has on BP & RR • Prepare for pacemaker insertion • Often patient on BR has adequate perfusion rd 3 Degree AV Block • Digitalis • Prolonged PR interval with sagging ST depression • Hyperkalemia • Tall, pointy T waves Miscellaneous Effects on ECG • Severe hyperkalemia • Widened QRS complexes • Hypokalemia • Flattened T waves, prominent U wave • Hypercalcemia • Shortened, almost non-existent ST segment • Hypocalcemia • Prolonged ST segment, causing prolonged QT interval Pacemakers • Used to increase heart rate (contraction) with symptomatic bradycardia, 2nd degree block type 2, 3rd degree heart block • They electrically stimulate heart muscle (to initiate depolarization)…hopefully a resultant contraction will occur • They are small generators Pacemakers • Types • Temporary • Transthoracic, Transvenous, Epicardial • Permanent (programmed) • Transvenous, Epicardial • Transcutaneous • Atrial, ventricular or dual chamber pacing • Settings • Demand (synchronous) • Fixed rate (asynchronous) How to Identify Pacemaker Rhythms • A three-letter code identifies the type of pacemaker in use. The first letter refers to the chamber paced, the second is the chamber sensed, and the third is the response to the sensed events. • There can be a fourth letter for rate response features (R) • VVI (ventricular pacing both chambers, inhibited) • DDD pacemakers pace atrium and ventricles, dual triggered • Pacing can involve the ventricle, the atrium or both. All paced rhythms have a spike, a thin vertical line, immediately preceding the paced beats • If the ventricle is paced, the resultant QRS will be wide, resembling ventricular beats • Malfunctions in pacing, capturing and sensing Pacemakers • Failure to Pace • Is noted when the pacemaker spike is not evident on the ECG • Failure to Capture • Is successful depolarization of the atria and/or ventricles by an artificial pacemaker • Pacer spike is noted on ECG but not followed by P waves or QRS complexes • Assess patient for fatigue, bradycardia, hypotension • Battery failure? • Output set too low? • Failure to sense • Is when the pacemaker doesn’t sense patient’s rhythm and starts an electrical impulse ALWAYS WORRY IF THE RATE DROPS BELOW THE SET RATE Pacemakers • Nursing care and considerations • Perioperative • Postoperative care • Monitor incision • Most common complication is electrode displacement • Immobilize arm to allow wires to imbed • ROM to prevent frozen shoulder • Transthoracic • Patient education/teaching • Check pulse daily • ID card • Avoid microwaves/MRI’s • Avoid contact sports Pacemakers • Signs & Symptoms of malfunction • Presyncope/syncope • Weakness • Arrhythmia, palpitations, tachycardia/bradycardia • Dyspnea • Constant twitching of muscles in chest or abdomen • Frequent hiccups • Angina, chest pain • Confusion, extreme drowsiness Pacemakers • Common Causes of Malfunction • Battery depletion • Loose or broken wire between heart and pacer • Lead dislodgment or gets pulled out • Electronic circuit failure • Electrolyte imbalance • Electromagnetic interference (generators, medical equipment) • Cyber attack • Change in condition that requires pacemaker reprogramming Note: Keep cell phone on opposite side of where pacer is placed Implantable Cardioverter Defibrillator (ICD) ICD • Can detect life threatening arrhythmias and then cardioverts, defibrillates and/or paces and records ECG • Last for about 5-7 years • The newer subcutaneous ICD delivers the energy at the left sternum from sites near the left axilla • Can be set for • Low energy pacing therapy • Anti tachycardia pacing • Cardioversion therapy • Defibrillation therapy Nursing Management (After Permanent Electronic Device Insertion) • ECG assessment • CXR • Nursing assessment • CO and hemodynamic stability • Incision site • Signs of ineffective coping • Level of knowledge and education needs of family and patient ICD • Discharge teaching • Postoperative complications • Follow up appointments • No lifting more than 5 pounds • No contact sports, strenuous exercise or swimming, bicycling, bowling, vacuuming (above shoulder activities) • Battery life • No driving for at least one month and up to 6 months if implanted for previous VT, VF • Electrical interference issues: • Cell/mobile devices (keep at least 6 inches/15 cm away from implantation site • Security systems and held metal detectors (airports) • Medical equipment (MRI, MRA not recommended • Power generators (keep at least 2 feet/0.6 meters away) • MP3 player headphones devices (keep at least 6 inches/15 cm away from implantation site) • End of life issues Cardiogenic Shock Heart attack as a cause of cardiogenic shock: Damaged heart muscle results in reduced force of contractions, reduced stroke volume, and reduced cardiac output.