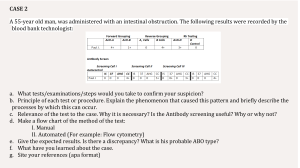
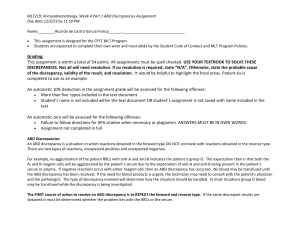
REPORT SHEET Activity No. 6 REVERSE BLOOD TYPING (Tube Method) REVIEW QUESTIONS: 1. When hemolysis is present in the final solution, what does it indicates? Explain. Hemolysis: lysis or rupture of erythrocytes. Hemolysis as an Indicator of Antigen-Antibody Reactions red cell hemolysis observed in the tube is also an indicator of the reactivity of an antigen and antibody in vitro. If the complement system is activated by an immune complex, hemolysis of the red cells along with agglutination can occur. The final steps in the process of complement activation initiate the membrane attack complex, causing membrane damage. As a consequence of this damage, intracellular fluid is released to the reaction environment. The red cell button is often smaller compared with the red cell button present in other tubes. A pinkish to reddish supernatant is observed after the tubes have been centrifuged. For grading a tube with hemolysis, an H is traditionally used when this phenomenon is observed. Some red cell antibodies characteristically display hemolysis in vitro, such as antibodies to the Lewis system antigens and anti-Vel, which are discussed in later chapters.3 It is important to recognize hemolysis as an antigen-antibody reaction. Hemolysis is detected in vitro using fresh serum samples. Serum has active complement proteins. Because anticoagulants bind calcium, which is necessary for complement activation, plasma samples do not demonstrate complement activation. Reference: Harmening, D. (2012), Modern blood banking and transfusion practices, Chapter 6 The ABO Blood Group System, 6th ed., (pp.121-123) F. A. Davis Company 2. When do ABO discrepancies occur? How can this be resolved? ABO discrepancies occur when unexpected reactions are obtained in the forward and/or reverse grouping. These can be due to problems with the patient’s serum (reverse grouping), problems with the patient’s RBCs (forward grouping), or problems with both the serum and cells. The unexpected reaction(s) may be due to an extra positive reaction or a weak or missing reaction in the forward and reverse grouping. All ABO discrepancies must be resolved prior to reporting a patient or donor ABO group. Categories of ABO Discrepancies: ABO discrepancies may be arbitrarily divided into four major categories: group I, group II, group III, and group IV discrepancies. Group I Discrepancy: Associated with unexpected reactions in the reverse grouping due to weakly reacting or missing antibodies. One of the reasons for the missing or weak isoagglutinin’s is that the patient has depressed antibody production or cannot produce the ABO antibodies. Common populations Resolutions • Newborns - Determine the patient’s diagnosis, age and • Elderly patients immunoglobulin levels. • Patient with Leukemia or Lymphoma • Patients on immunosuppressive drugs • Patients with immunodeficiency diseases • Patients with bone marrow transplant Reverse group reaction is to be enhanced. Incubate the patients serum with the reagent cells at room temperature for 15 minutes. - If no reaction, incubate the mixture at 4degree Celsius for 5 minutes with autologous control. - Note that, auto control and a O cell control must be run concurrently this is to rule out presence of cold autoantibody. Group II Discrepancy: are associated with unexpected reactions in the forward groupings due to missing or weak antigens. This group of discrepancies is probably the least frequently encountered. Causes Resolutions • Subgroups of A or B Acidify Anti-B typing reagent at pH 6.0, the acidified • Leukemia and Lymphoma sera or ES-4 monoclonal anti-B clone at pH levels of • Excess antigen of blood group soluble substances 6.5 to 7.0 would agglutinate only “true B antigen” and • Acquired A or B antigens. not the “acquired B antigen. Group III Discrepancy: These discrepancies between forward and reverse groupings are caused by protein or plasma abnormalities and result in rouleaux formation or pseudoagglutination. Causes Resolutions • Elevated levels of plasma globulins as seen in Cell grouping can usually be accomplished by washing cases of Multiple Myeloma, Waldenstrom's the patient’s RBCs several times with saline. macroglobulinemia Performing a saline replacement technique will free the and Hodgkin's lymphoma cells in the case of rouleaux formation in the reverse • Elevated levels of fibrinogen type. • Use of plasma expanders such as dextran • Wharton's jelly in cord blood samples washing cord cells six to eight times with saline should alleviate spontaneous rouleaux due to Wharton’s jelly Group IV Discrepancy: These discrepancies between forward and reverse groupings are due to miscellaneous problems Causes Resolutions • Cold reactive autoantibodies in which RBCs are The polyagglutination is to be confirmed by lectin so heavily coated with antibody that they seeds spontaneously agglutinate, independent of the specificity of the reagent antibody. The patients showing polyagglutinibility should be • Circulating RBCs of more than one ABO group transfused only as washed red cells and not the plasma due to RBC transfusion or marrow/stem cell containing whole blood, since the plasma contains antitransplant T • Unexpected ABO isoagglutinins • Unexpected non-ABO alloantibodies - Harmening, D. (2012), Modern blood banking and transfusion practices, 6th ed., (p. 136142) F. A. Davis Company 3. What are the common sources of technical errors that will result in ABO discrepancies? Technical errors can also cause ABO discrepancies. Exa `mples include blood sample and test tube labeling errors, failure to add reagents, or the addition of incorrect reagents or sample. Serum and antiserum should always be added first, followed by the patient or reagent RBCs to avoid both reagent contamination and potential omission of either patient sample or reagent. Results must be recorded immediately after obtaining them to avoid transcription errors. Always examine reagent vials concurrently while performing ABO testing and quality control testing for possible contamination. Resolution If initial testing was performed using RBCs suspended in serum or plasma, repeat testing of the same sample using a saline suspension of RBCs can usually resolve the ABO discrepancy. It is important to make sure all technical factors that may have given rise to the ABO discrepancy are reviewed and corrected. It is also essential to obtain adequate information regarding the patient’s age, diagnosis, transfusion history, medications, and history of pregnancy. If the discrepancy persists and appears to be due to an error in specimen collection or identification, a new sample must be drawn from the patient and all RBC and serum testing repeated. When a discrepancy is encountered, all results must be recorded, but interpretation of the ABO type must be delayed until the discrepancy is resolved. If the blood is from a potential transfusion recipient, it may be necessary to administer group O, Rh-compatible RBCs before the discrepancy is resolved. In general, when investigating ABO discrepancies, always remember that RBC and serum grouping reactions are very strong (3+ to 4+) and the weaker reactions typically represent the discrepancy. Harmening, D. (2012), Modern blood banking and transfusion practices, 6th ed., (p. 136 F. A. Davis Company