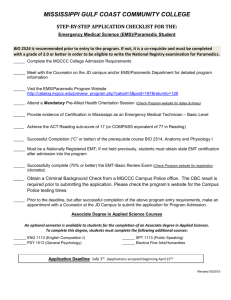
Paramedic/A-EMT/Basic EMT Approved 8.1.2013 1 This book is dedicated to the memory of Dr. Darren Bean, Medical Director for the City of Madison Fire Department, who was instrumental in the development of the ALS system and expanding Dane County EMS. Dr. Bean died on May 10, 2008 while on duty transporting a patient in his capacity as a MedFlight physician. It was Dr. Bean’s vision to have protocols and procedures that were consistent throughout Dane County, and he worked tirelessly with the Dane County ALS Service Providers and Dane County EMS to achieve this goal. In memoriam, we thank Dr. Bean for his vision, energy, and dedication. 2 Table of Contents-Protocols Preliminary Information Overview Acknowledgements Suppositions Authorization General Principles for Medical Care Paramedic Intercept Guidance Medical Transport Destination Physician On Scene Patient Care During Transport Patient Care Standards During Interfacility Transport Radio Report Format Transfer of Care at Hospitals DNR Authorized Pharmaceuticals 6 6 6 6 7 10 11 12 13 14 15 17 18 19 Adult Protocols General Approach to All Adult Patients Abdominal Pain/GI Bleeding Airway Emergencies: Adult Dyspnea Adult Airway Management Rapid Sequence Airway Allergic Reaction Altered Mental Status Behavioral Emergencies/Excited Delirium Bites and Envenomations Cardiac Arrest: General Approach Asystole Pulseless Electrical Activity (PEA) Ventricular Fibrillation/Pulseless Ventricular Tachycardia Post-Resuscitation Care Hypothermia: Therapeutic/Induced Termination of Resuscitation No Resuscitation Indicated Cardiac Arrhythmias: Atrial Fibrillation or Flutter Bradycardia Supraventricular Tachycardia Wide-Complex Tachycardia Polymorphous Ventricular Tachycardia (Torsades de Pointes) Chest Pain 3 20 23 25 30 33 40 43 46 48 50 52 54 56 58 60 63 64 65 67 70 72 75 77 Table of Contents-Protocols Hazardous Material Exposures: Cyanide Toxicity and Smoke Inhalation Nerve Agent/WMD Hypertensive Emergencies Hyperthermia Hypothermia Intravenous Access Obstetrics/Gynecology: Perinatal Emergencies Vaginal Bleeding Childbirth/Labor Overdose and Poisonings: General Approach Tricyclic and Tetracyclic Antidepressant Overdose Cholinergic Poisoning/Organophosphates Antipsychotics/Acute Dystonic Reaction Beta Blocker Toxicity Calcium Channel Blockers Carbon Monoxide Cocaine and Sympathomimetic Overdose Opiate Pain Management—Adult Policy Custody Taser Refusal of Medical Care Refusal of Transport After Treatment Given: Bronchospasm Resolved After Nebulizer Treatment Induced Hypoglycemia—Resolved Sedation/Sedative Agent Use Seizure Shock (Non-Trauma) Stroke—Suspected Syncope Trauma: General Approach to All Patients Burns—Thermal Chest Injuries Head Injuries Eye Injuries Extremity Traumatic Cardiac Arrest Sexual Assault Spinal Immobilization—Indications: 4 81 84 87 89 91 93 95 96 99 102 104 106 107 108 109 110 111 113 114 115 118 119 120 122 123 124 125 128 131 134 137 140 143 144 147 148 151 153 154 Table of Contents-Protocols Pediatric Protocols General Approach to All Pediatric Patients Airway Emergencies: Pediatric Dyspnea Pediatric Airway Management Allergic Reactions—Pediatric Altered Mental Status—Pediatric Apparent Life-Threatening Event (ALTE) Cardiac Arrest: General—Pediatric 159 160 163 166 168 170 171 Cardiac Arrhythmia: Pediatric Bradycardia Pediatric Wide Complex Tachycardia with Pulse Pediatric Narrow Complex Tachycardia (SVT) with Pulse Newborn Resuscitation Overdose, Poisoning, or Ingestion—Pediatric Pain Management—Pediatric Seizure—Pediatric Trauma: Pediatric General Pediatric Burns Pediatric Head Trauma Procedures Pharmaceuticals Abbreviations 176 179 180 183 186 188 191 194 196 200 203 259 316 5 Authorization In accordance with Wisconsin Statute 256 and Chapter 110 of the Wisconsin Administrative Code, effective 8/1/2013 the following medical treatment protocols are authorized by the Medical Director for use in the Dane County EMS System. Changes to these protocols can be made only with authorization of the Medical Director. Michael T. Lohmeier, MD Dane County Medical Director Overview The Dane County EMS Protocols contained within this document are intended to provide and ensure uniform treatment for all patients who receive care from EMS agencies and provider participating in the Dane County EMS System. These protocols apply exclusively to agencies responding to activation of the 911 system within Dane County. Any other use must receive prior approval from the Medical Director of Dane County EMS. While attempts have been made to address all patient care scenarios, unforeseen circumstances and patient care needs will arise. For these instances medical personnel should follow the “General Approach” protocols (or other appropriate protocol), exercise their own judgment, and contact Medical Control for additional physician orders as needed. The patient’s best interest should be the final determinant for all decisions. Acknowledgements The Medical Director wishes to thank the following for their hard work and commitment during the development of these protocols. Dr. Christian Zuver Dr. Lee Faucher Dr. Melissa Schultz Dr. Michael Kim Dr. Suresh Agarwal Dr. Ankush Gosain Melissa Schultz Denise DeSerio Carrie Meier Dane County Medical Advisory Subcommittee Meriter Hospital St. Mary’s Hospital Stoughton Hospital UW Hospital VA Hospital Suppositions □ The term Advanced EMT is considered a licensed EMT – Intermediate Technician. □ For the situation of drug shortages, any alternatives to the drugs listed in the protocols must be approved by medical control before use. □ BIAD – Blindly Inserted Airway Device. Examples include: King LTS-D – LMA - Combitube 6 The following measures shall be applied to help promote prompt and efficient emergency medical care to the sick, ill, injured or infirmed. They shall be utilized by EMS personnel in the field, in the Emergency Department, and when dealing with On-line Medical Control Physicians. 1) The Safety of EMS personnel is paramount. Each scene must be properly evaluated for crew safety and hazards upon arrival and throughout patient care. Assess the need for additional public safety resources as soon as possible after arrival. 2) Proper Personal Protective Equipment and Body Substance Isolation must be utilized according to agency and industry standard. 3) A patient is any person who is requesting and/or in need of medical attention or medical assistance of any kind. 4) A patient care encounter shall be considered any event when subjective or objective signs or symptoms, or a patient complaint, results in evaluation or treatment. 5) All patients in the care of EMS shall be offered transport by ambulance to the nearest appropriate hospital, regardless of the nature of the complaint. In the event a patient for whom EMS has responded to refuses transport to the hospital, a properly executed refusal process must be completed. 6) In accordance with system guidelines, the only appropriate transport destination for EMS patients transported by ambulance is an Emergency Department. Exceptions to this are outlined within the specific protocols. Additional details concerning hospital destination based on clinical criteria are outlined in specific protocols. 7) For all 911 calls, upon initial patient contact, be prepared for immediate medical intervention appropriate for the call level (defibrillation, airway management, drug therapy, etc.) 8) Upon arrival at a scene where an initial EMS crew is rendering patient care, all subsequent arriving EMS crews should immediately engage the on-scene crew. The goal is to determine the status of assessment and seamlessly assist in patient care. 9) Prior to the transfer of care between crews, the provider rendering initial care should directly interface with the provider assuming care, to ensure all pertinent information is conveyed. 10) For all patients in cardiac arrest, call into dispatch with the “patient contact time” at the time of initial patient contact, and with the “first shock time” at the time of initial defibrillation. 11) Try to always obtain verbal consent prior to treatment. Respect the patient’s right to privacy and dignity. Courtesy, concern and common sense will ensure the best possible patient care. Service MD Approval:______ General Principles 1 of 3 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 7 Continued: 12) The provider should generally be able to decide within three (3) minutes after patient contact if advanced life support (ALS) measures will be needed. If identified by EMT Basic or Advanced, ALS should be requested immediately. If identified by Paramedic, ALS measures should be instituted simultaneously with the initial assessment. A comprehensive exam is appropriate after the patient has been stabilized. 13) Generally, initial assessment and therapy should be completed within 10 minutes after patient contact. Except for extensive extrication, or atypical situations, trauma patients should be en route to the receiving facility within 10 minutes and medical patients should be en route to the receiving facility within 20 minutes. Additional therapy, if indicated, should be performed during transport. 14) For all 911 calls where EMTs and Paramedics are in attendance, the Paramedic shall make final patient care decisions. 15) Prior to the administration of medication, assess for the possibility of medication allergies. If any questions arise in reference to medication allergies, contact on-line Medical Control prior to giving any medications. 16) When caring for pediatric patients, use the Broselow-Luten® weight/length based system to determine medication dosages and equipment sizes. 17) An EMS Patient Care Report will be generated at the conclusion of each patient encounter. Patient care reports should be transmitted to the receiving hospital in accordance with state requirements. 18) For cases that do not exactly fit into a treatment category, refer to the general illness protocol and contact OLMC as needed. 19) Following training and successful competency assessment by their respective agencies, those licensed at the EMT-Basic, Advanced and Paramedic level are authorized to: □ Apply tourniquets □ Utilize pulse oximetry □ Utilize capnography monitoring devices □ Perform blood glucose evaluations □ Perform CPAP □ Place and ventilate blind insertion airway devices (BIAD) □ Place and utilize orogastric tubes via the gastric port of a BIAD □ Acquire and transmit 12 Lead ECGs Individual Agencies must request and receive State of WI approval prior to implementation of these skills. Service MD Approval:______ General Principles 2 of 3 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 8 20) To perform as a Basic EMT/ A-EMT/ Paramedic, personnel must be knowledgeable and proficient in the scope of practice described and taught in the National Scope of Practice Standardized Curriculum, approved by the Wisconsin EMS Unit, and must maintain active state licensure. 21) Members of your service who are credentialed with and function on your service with an RN, PA, or MD license may only practice within the scope of the agency’s license. 22) Perform all procedures as per the Dane County EMS System Procedures manual. If a procedure that is not addressed in the manual is deemed necessary, contact OLMC for orders prior to proceeding. 23) If OLMC gives orders for performance of a procedure that is not covered in the Dane County EMS system Procedures Manual, but is within the providers scope of practice, follow the National Standard Curriculum. 24) For all patients requiring the administration of narcotics or sedative agents, continuous cardiac, oxygen saturation, and ETCO2 monitoring shall be performed. 25) The Poison Control Center should be contacted when handling calls involving poisonous/ hazardous material exposures, overdoses or suspected envenomation. In the event that the Poison Control Center gives recommendations or orders that are not contained within these protocols, EMS providers are authorized to carry out their instructions. The Poison Control Center can be reached at 1.800.222.1222 26) All defibrillators used in the Dane County EMS System must be able to deliver biphasic energy. 27) When using supplemental oxygen in accordance with adult or pediatric treatment protocols, adhere to the following: a) In patients who are non-critical, and have no evidence of respiratory distress, use only the concentration of oxygen needed to achieve oxygen saturation over 93%. Typically this may be accomplished by the use of a nasal cannula. b) For patients with serious respiratory symptoms, persistent hypoxia, or where otherwise specified by protocol, use 100% supplemental oxygen via nonrebreather mask or BVM. Use caution in instances of rising end-tidal CO2. 28) Precautions: Droplet precautions: standard PPE, a standard surgical mask for providers who accompany patients in the back of the ambulance and a surgical mask or NRB O2 mask for the patient. This level of precaution should be utilized when influenza, meningitis, mumps, streptococcal pharyngitis, pertussis, and other illnesses spread via large particle droplets are suspected. Contact precautions: standard PPE, a gown, change of gloves after every patient contact, and strict handwashing precautions. This level of precaution is utilized when multi-drug resistant organisms (ie. MRSA), scabies, zoster (shingles), or other illness spread by contact are suspected. Airborne precautions: standard PPE, N95 mask on EMS personnel and surgical mask or NRB O2 mask on patient. This level is used if tuberculosis is suspected. Service MD Approval:______ General Principles 3 of 3 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 9 Standards Policy Policy: To define the circumstances in which a Paramedic should be requested to intercept with an ambulance not staffed with a Paramedic and to provide guidance for the intercept process. If the Paramedic’s estimated time of arrival is longer than the time it would take to transport the patient to the hospital via BLS ambulance, the patient should be transported without delay. In general BLS should not wait on scene for ALS. Types of Patient Problems that MAY require Paramedic Intercept: a) b) c) d) e) f) g) h) i) j) k) Cardiopulmonary arrest Unconsciousness that does not respond to glucose administration Difficulty breathing/compromised airway Multi-system trauma Chest Pain – suspected cardiac Diabetic with persistent altered level of consciousness Patients with unstable or deteriorating vital signs Active persistent seizures, first seizure, or seizure following head trauma Significant allergic reaction Childbirth complications Any other situation in the opinion of the BLS provider or Medical Control that may benefit from advanced level care. Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 10 Standards Policy All patients should be transported to the hospital of their choice (when operationally feasible) unless the patient is unstable. All patients whose condition is judged to be unstable will be transported to the closest appropriate receiving facility. If several hospitals are within the same approximate distance from the scene. Allow the patient, and/ or patients’ family to select the receiving facility of their choice. For transport destination of Stroke, STEMI, Trauma, or OB (>20weeks) patients, refer to the appropriate protocol. At the time of protocol publication the following centers have appropriate credentialing: Stroke: Meriter St. Mary’s – Madison UW Hospital VA Hospital STEMI: Meriter St. Mary’s – Madison UW Hospital VA Hospital Trauma: UW Hospital OB: Meriter St. Mary’s – Madison Sauk Prairie Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 11 Standards Policy Policy: The control of the scene of an emergency should be the responsibility of the individual in attendance who is the most appropriately trained in providing pre-hospital stabilization and transport. As a representative of the Medical Director of an EMS system, the pre-hospital provider fulfills that role. Occasions will arise when a Physician on the scene will desire to direct prehospital care. A standardized scheme for dealing with these contingencies will optimize the care given to the patient. The Physician desiring to assume care of the patient must: □ Provide documentation of his/her status as a physician (MD or DO) to include a current copy of his/her license to practice medicine in Wisconsin. □ Assume care of the patient and allow documentation of his/her assumption of care on the patient care report. □ Agree to accompany the patient during transport to the hospital. Contact with Medical Control must be established as soon as possible. The Medical Control Physician must agree and relinquish the responsibility of patient care to the physician on-scene, in order for care to be transferred. Orders provided by the Physician assuming responsibility for the patient should be followed as long as they do not, in the judgment of the pre-hospital provider, endanger patient well-being. The prehospital provider may request the Physician to attend to the patient during transport, if the suggested treatment varies significantly from standing orders. If the physician's care is judged by the pre-hospital provider to be potentially harmful to the patient, the provider should: □ Politely voice his/her objection. □ Immediately place the on-scene physician in contact with the Medical Control Physician. When conflicts arise between the physician on scene and the Medical Control Physician, EMS personnel should: □ Follow the directives of the Medical Control Physician. □ Offer no assistance in carrying out the order in question; offer no resistance to the physician performing this care. □ If the physician on scene continues to carry out the order in question, offer no resistance and enlist the aid of law enforcement. All interactions with physicians on the scene must be completely documented in the Patient Care Report, including the name and license number of the on-scene physician. Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 12 Standards Policy The following situation shall require > 1 attendant in the back of an ambulance. Medical or Traumatic cardiac arrest or post-resuscitation care Patients requiring active airway assistance (ETT, BIAD, BVM) Imminent delivery For scenarios not covered above: □ if the provider requests a second attendant. A second attendant is not required if there will be an unacceptable delay in transport. NOTE: Only a student with a current training permit at the appropriate level of care may assist with patient care. Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 13 Standards Policy This policy can ONLY be used if your agency has State approval to provide Interfacility Transport. Although primary responsibility is not for interfacility transports, situations may arise necessitating such transport Regardless of the provider, interfacility transport requires unique skills and capabilities, both in clinical and operational coordination. Adhere to the following standards for all interfacility transports: □ Interfacility transport decisions (including but not limited to transport staffing, equipment and transport destination) should be made on the patient’s medical needs. □ Match provider skills and equipment with patient care needs □ Coordination between hospitals and interfacility transporters is essential before transport is initiated to ensure that patient care is provided at the appropriate level and does not exceed the capabilities of the interfacility transport provider. □ If EMS crewmembers are not capable/skilled in managing devices or medications, or if the devices/medications are not listed in these protocols and must be continued during transport, an adequately trained care provider from the transferring facility whose credentials are acceptable to the transporting agency must accompany the patient during transport. Contact Medical Control with any questions or concerns Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 14 Standards Policy For all patients transported by EMS, radio contact should be made with the receiving facility prior to arrival. When possible, in order to provide sufficient notification of the patient’s condition and estimated time of arrival, radio contact should be made at least 5 minutes prior to arrival. Use the following triage categories and triage levels (colors) to assist the receiving facility in prioritizing incoming calls. TRIAGE CATEGORIES Categories Trauma Medical Red Yellow Green STEMI alert Stroke alert Pediatric Haz‐Mat PNB MD's Orders Definitions indicates patient is a trauma patient indicates patient is a medical patient High acuity of illness or injury, unstable or critical Serious condition, but not critical or unstable Low acuity of illness or injury meets STEMI criteria per Chest Pain protocol meets stroke alert criteria as per Stroke protocol indicates patient is <12 years of age (medical) or less than 18 years of age (trauma) indicates patient was involved in a Haz/Mat incident Cardiopulmonary Arrest Indicates physican orders are needed Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 15 Standards Policy Radio Call to an Emergency Department Begin each transmission with the following: □ Agency name and unit number □ Triage category and triage level (ie. Medical Red, STEMI alert) □ Estimated time of arrival After the receiving facility acknowledges the initial information, give a concise report which includes the following: □ Repeat the triage category and triage level □ Age and gender of patient □ Chief complaint or problem □ Provide pertinent detail as to the following: ~vital signs ~glasgow coma score/level of consciousness ~mechanism of injury (if trauma) ~description of injuries (if trauma) ~treatment provided or under way ~any anticipated delay in transport (ie. extrication) MEDICAL CONTROL CONTACT Contact Medical Control for any additional orders or with questions needed to meet the patient’s needs during on-scene care or transport Any quality concerns involving Medical Control should be forwarded to the Dane County Medical Director for review as soon as possible. Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 16 Standards Policy Once on hospital property, the receiving facility assumes responsibility for all further medical care delivered to EMS transported patients. Dane County EMS personnel are not authorized to follow prehospital protocols after arrival at an Emergency Department and OLMC should not be contacted for orders. Exceptions to this should occur only in the following circumstances: Life-threatening situations such as cardiac arrest, airway emergencies or imminent delivery of a newborn. Continuation of treatment started prior to arrival (ie. Nebulizers, CPAP, IV fluids) When specifically instructed to continue care by the ED physician (when possible document the physician’s name and the time the verbal order was given) To assure all known pertinent information is conveyed to the hospital staff, crews should interface with nursing staff promptly to give a verbal report and written report**. Transporting personnel shall provide to the receiving facility all known pertinent incident, patient identification and patient care information at the time the patient is transferred. In addition turn over all pre-hospital 12 lead EKGs to the ED staff. Patient care reports may be transmitted by physical (paper) means or electronic means. NOTE: ** Administrative Rule 110.34(7) states, “...submit a written report to the receiving hospital upon delivering a patient and a complete patient care report within 24 hours of patient delivery. A written report may be a complete patient care report or other documentation approved by the department and accepted by the receiving hospital.” Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 17 Standards Policy Policy: To clarify State of Wisconsin Do Not Resuscitate: If a patient is found to be wearing a Wisconsin “Do-Not-Resuscitate” DNR bracelet, no resuscitative measure should be undertaken, including compressions, artificial ventilation, defibrillation, or the use of advanced airways. Emergency Provider as appropriate will provide: Clear airway Control bleeding Administer Oxygen Provide pain medication Position for comfort Provide emotional support Splint Emergency Provider will NOT provide: Perform chest compressions Insert advanced airways Administer cardiac resuscitation drugs Provide ventilatory assistance Defibrillate Any other forms must be validated by contacting Medical Control before stopping any resuscitative efforts Service MD Approval:______ Policy Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 18 Authorized Pharmaceuticals Generic Name Trade Name Adenosine Albuterol Amiodarone Aspirin Atropine Calcium Chloride Dextrose (5%, 12.5%, 25%, 50%) Diazepam Diltiazem Diphenhydramine Dopamine DuoDote Kit Epinephrine 1:1,000 Epinephrine 1:10,000 Etomidate Famotidine Fentanyl Glucagon Glucose, Oral Haloperidol Hydroxocobalamin Ipratropium Bromide Ketamine Lidocaine 2% Lorazepam Magnesim Sulfate 10% Mark 1 Kit Methylprednisolone Midazolam Morphine Sulfate Naloxone Nitroglycerin Ondansetron Rocuronium Sodium Bicarbonate 8.4%, 4.2% Succinylcholine Vassopressin Adenocard Proventil Cordarone Route IV/IO Nebulized IV/IO PO IV/IO IV/IO IV/IO Valium, Diastat PR/IM Cardizem IV/IO Benadryl IV/IO/IM Intropin IV/IO IM Adrenaline IM Adrenalin IV/IO Amidate IV/IO Pepcid IV/IO Sublimaze IV/IO/IN GlucaGen IV/IM Glutose PO Haldol IM Cyanokit IV/IO Atrovent Nebulized Ketalar IM Xylocaine IV/IO Ativan IV/IM IV/IO IM Solu‐Medrol IV/IO Versed IV/IM/IN IV/IO Narcan IV/IO/IM/IN Nitrostat, Nitrolingual SL Zofran IV/IO/ODT Zemuron IV/IO IV/IO/Nebulized Anectine IV/IO Pitressin IV/IO 19 Levels P EMT, A, P P EMT, A, P P P A, P P P P P P EMT, A, P P P P P EMT, A, P EMT, A, P P P EMT, A, P P P P P P P P P A, P A, P P P P P P A P M Legend EMT A‐EMT Paramedic Medical Control A P M Scene Safety -Bring all necessary equipment to patients side ‐Demonstrate professionalism and courtesy PPE (consider contact, droplet, or airborne) CARDIAC ARREST Cardiac Arrest Protocol Airway Protocol Vital Signs** General Protocol Initial Assessment BLS Maneuvers Consider Spinal Immobilization If Pediatric Patient – use Broselow Tape Consider supplemental O2 2013 Consider 12 Lead EKG* and/or cardiac monitor IV Protocol if appropriate *** Appropriate PROTOCOL Transport patient per Transport Destination policy M Patient doesn’t fit a protocol or you have exhausted standing protocols? Consult Medical Control M Service MD Approval:______ Pearls RECOMMENDED EXAM: Vital signs, mental status with GCS and location of injury or complaint…..then to specific protocol *12 Lead EKG should be done EARLY on a possible STEMI patient. **Vital signs include Blood Glucose Reading – if any weakness, altered mental status or history of diabetes. Oxygen Saturation and Capnography if condition warrants Nothing by mouth, unless patient is a known diabetic with hypoglycemia and able to self‐administer oral glucose paste or a glucose containing beverage or unless indicated by specific protocol. ***if evidence of dehydration or BP<90mmHg systolic administer 250ml 0.9% NaCl and refer to appropriate protocol. If hypoglycemic refer to altered level of consciousness protocol. Any patient contact which does not result in an EMS transport must have a completed refusal form. Required vital signs on every patient include blood pressure, pulse, respirations, pain‐severity. Pulse oximetry and temperature documentation is dependent on the specific complaint Timing of transport should be based on the patients clinical condition and the transport policy. Never hesitate to consult medical control for patient who refuses Orthostatic vital sign procedure should be performed in situation where volume status is in question. General Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 20 General Approach to All Adult Patients The following measures will serve as the “General Patient Care Protocol—Adult” and apply to the management of all adult patients. All Providers Scene Safety PPE (consider contact, droplet, and/or airborne) Initial assessment (BLS maneuvers and consider c-spine immobilization) Establish patent airway Provide Supplemental oxygen to maintain SpO2 ≥ 93 %, or if any respiratory signs or symptoms present Obtain, record and monitor vital signs Perform a 12-lead ECG if chest pain, abdominal pain above the umbilicus or ischemic equivalent symptoms Record and monitor continuous O2 saturation and Capnography (if available) if condition warrants Record Blood Glucose Level if any weakness, altered mental status or history of diabetes Nothing by mouth, unless patient is a known diabetic with hypoglycemia and is able to self-administer oral glucose paste, or a glucose containing beverage: Glucose paste 15 g or other oral glucose agent (e.g. orange juice) if patient alert enough to self administer oral agent Transport patient to nearest appropriate Emergency Department Minimize on-scene time when possible Advanced EMT Consider IV 0.9% NaCl TKO/KVO or IV lock If evidence of dehydration (tachycardia, dry mucous membranes, poor skin turgor) or hypovolemia, administer boluses of 0.9% NaCl at 250 ml (up to 500 ml total if no hypotension) If BP<90 mmHg systolic, administer boluses of 0.9% NaCl at 250 ml until systolic BP>90 mmHg, max individual dose 2 L ▪ Contraindicated if evidence of congestive heart failure (e.g. rales) ▪ If Hypoglycemic (Blood glucose < 70 mg/dL) with IV access: 21 o Dextrose 12.5-25g or D10W 100ml Repeat Dextrose once if blood glucose <70 mg/dL after 10 minutes If Hypoglycemic (Blood glucose < 70 mg/dL) without IV access Glucose paste 15 g or other oral glucose containing agent (e.g., orange juice) if patient alert enough to self administer oral agent If unable to take oral glucose administer Glucagon 1 mg IM Paramedic When condition warrants (specified as “Full ALS Assessment and Treatment “ in individual protocols) Advanced airway/ventilatory management as needed Perform cardiac monitoring IV 0.9% NaCl TKO/KVO or IV lock If evidence of dehydration (tachycardia, dry mucous membranes, poor skin turgor) or hypovolemia, administer boluses of 0.9% NaCl at 250 ml (up to 500 ml total if no hypotension) If BP<90 mmHg systolic, administer boluses of 0.9% NaCl at 250 ml until systolic BP>90 mmHg, max individual dose 2 L Contraindicated if evidence of congestive heart failure (e.g. rales) If Hypoglycemic (Blood glucose < 70 mg/dL) with IV access: o Dextrose 12.5g-25g IV or D10W 100mL IV Repeat Dextrose 12.5-25 g once if blood glucose <70 mg/dL after 10 minutes If Hypoglycemic (Blood glucose < 70 mg/dL) without IV access Glucose paste 15 g or other oral glucose containing agent (e.g., orange juice) if patient alert enough to self administer oral agent If unable to take oral glucose administer Glucagon 1 mg IM Contact Medical Control with any additional orders or questions 22 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Signs and Symptoms Pain Tenderness Nausea Vomiting Diarrhea Dysuria Constipation Vaginal Bleeding/Discharge Pregnancy Other Symptoms: Fever, Headache, Weakness, malaise, myalgias, cough, Headache, rash, mental status change Differential Pneumonia or PE Liver (hepatitis, CHF) Peptic Ulcer disease / Gastritis Gallbladder MI Pancreatitis Kidney Stone Abdominal Aneurysm Appendicitis Bladder/prostate disorder Pelvic Spleen enlargement Diverticulitis Bowel obstruction Gastroenteritis Medical Protocol History: Age Past Medical/surgical history Medications Onset Provocation Quality Region / Radiation / Referred Severity 1‐10 Time Fever Last meal eaten Last bowel movement Menstrual history (pregnancy) General Approach to All Adult Patients A IV Protocol A 2013 Blood Pressure <90mmHg >90mmHg A Normal saline bolus 500 ml (max 2L) A Nausea and/or vomiting No Yes P If severe Ondansetron (Zofran) 4 mg IV/IM/ODT P Consider Chest Pain Protocol Pain Control Protocol Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Neck, Heart, Lung, Abdomen, Back, Extremities, Neuro Nothing by mouth If pain is above the umbilicus, perform 12‐Lead EKG, refer to CHEST PAIN PROTOCOL if indicated Abdominal pain in women of childbearing age should be treated as ectopic pregnancy until proven otherwise The diagnosis of abdominal aneurysm should be considered with abdominal pain in patients over 50 Repeat vital signs after each bolus Appendicitis may present with vague, peri‐umbilical pain which migrates to the RLQ over time Increased initial NS Bolus of 500ml approved by Medical Advisory subcommittee to accommodate volume loss from GI bleed. Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 23 Abdominal Pain/GI Bleeding All Providers General Patient Care Protocol—Adult Nothing by mouth If pain is above the umbilicus, perform 12-lead EKG, refer to Chest Pain Protocol if indicated. Advanced EMT Consider IV Protocol Consider Fluid Bolus-500ml NS (max 2 liters) Paramedic Full ALS Assessment and Treatment For Patients with severe nausea or vomiting: Ondansetron (Zofran), 4 mg IV/IM/Oral Disintegrating Tablet (ODT) Refer to Pain Management Protocol if indicated Contact Medical Control for any additional orders or questions 24 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Signs and Symptoms Shortness of breath Pursed lip breathing Decreased ability to speak Increased respiratory rate and effort Wheezing, rhonchi Use of accessory muscles Fever, cough Tachycardia Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 25 2013 Pearls RECOMMENDED EXAM: Mental Status, HEENT, Skin, Neck, Heart, Lungs, Abdomen, Extremities, Neuro * Online Medical Control if age >50, HR >150 or History of Coronary Artery Disease **CPAP – start at 5cm of H2O and titrate up to maximum 15cm of H2O for effect ***Nitro contraindication use of Phosphodiesterase-5 (PDE-5) inhibitor within last 24 hours (Viagra, Levitra); 48 hours (Cialis) Position Patient for Comfort If cardiac origin a possibility and no contraindication, administer Aspirin 324 mg PO Medical Protocol History: Asthma; COPD – chronic bronchitis, emphysema, CHF Home treatment (oxygen, nebulizer) Medications (theophylline, steroids, inhalers) Toxic exposure, smoke inhalation Differential Asthma Anaphylaxis Aspiration COPD (Emphysema, Bronchitis) Pleural effusion Pneumonia Pulmonary embolus Pneumothorax Cardiac (MI and CHF) Pericardial tamponade Hyperventilation Inhaled toxin (Carbon Monoxide, etc) Drowning/Near Drowning Foreign body obstruction Carbon monoxide poisoning Legend EMT A‐EMT Paramedic A P M Medical Control A P M General Approach to all Adult Patients Airway Adult Protocol Assess Airway Patency Breathing Adequacy APNEA INSUFFICIENT SUFFICIENT RR <10 or >20 VS, SpO₂, EtCO₂ Consider CPAP Procedure Consider Airway Adult Protocol Supplemental O₂ NO Reassess VS, RR, SpO₂, EtCO₂ Wheezing? History of CHF, rales, peripheral edema, HTN, pink sputum NO YES A IV Protocol YES Albuterol 2.5mg/3ml Ipratropium 0.5mg/2.5ml Repeat Albuterol x2 (max 3 doses) A 2013 Acute Bronchospasm Consider CPAP Procedure** SpO₂ <93% YES NO EtCO₂ >45 Medical Protocol Fatigue Altered LOC Airway Obstruction Procedure OBSTRUCTION Pulmonary Edema SEVERE P MethylPrednisolone 125mg IV P SEVERE NO Improvement P No Speaking Little/no air movement ASA 324mg PO 12 Lead EKG Epinephrine 1:1,000* 0.3mg IM IV Protocol SEVERE Magnesium Sulfate 2g IV in 100ml D5 over 20 min. P A AWAKE and following commands Consider CPAP Procedure** Consult Medical Control A AWAKE and following commands P M Nitroglycerin 0.4mg SL every 3 minutes if SBP >90mmHg and no PDE*** M Ondansetron 4mg IV/IO Morphine 5‐10mg IV if SBP >150mmHg Dopamine 5‐20mcg/kg/min if SBP <90mmHg Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 26 P Airway Emergencies: Adult Dyspnea All Providers General Patient Care Protocol—Adult Supplemental oxygen to maintain SPO2 > 93% Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer if wheezing or history of Asthma/COPD. Albuterol may be repeated to a maximum of 3 administrations. If symptoms Severe (not speaking, little or no air movement) consider Epinephrine 1:1000, 0.3mg IM, if available OLMC if Age >50, HR>150 or History of CAD Perform obstructed airway procedures per BLS standards. Consider CPAP if available and symptoms are moderate to severe If history of Asthma or COPD, Start at 5cm of H2O and titrate up to maximum 10 cm of H20 for effect If cardiac origin a possibility and no contraindication, administer Aspirin 324 mg PO Advanced EMT Consider IV Protocol if indicated Acute Pulmonary Edema Suspected (History of CHF, peripheral edema elevated SBP) Nitroglycerin 0.4 mg SL every 3 min: o Contraindicated if SBP <90 mmHg o Contraindicated if use of a Phosphodiesterase-5 (PDE-5) inhibitor within last 24 hours (Viagra, Levitra); 48 hours (Cialis) Aspirin 324 mg PO Consider CPAP if symptoms moderate/severe: o Start at 5cm of H2O and titrate up to maximum 15 cm of H20 for effect 27 Paramedic Full ALS Assessment and Treatment Observe for signs of impending respiratory failure: Refer to Airway Management Protocol if indicated: Hypoxia (O2 sat < 90%) not improved with 100% O2 Poor ventilatory effort Altered mental status/decreased level of consciousness Inability to maintain patent airway Acute Bronchospasm (wheezing with or without history of Asthma or COPD) Mild Symptoms: Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer if not already given May repeat Albuterol (Proventil) PRN for continued wheezing Moderate Symptoms: As for mild symptoms, additionally: Methylprednisolone (Solumedrol) 125 mg IV if wheezing persists after 1st nebulizer treatment Consider CPAP if symptoms moderate to severe Start at 5cm of H2O and titrate up to maximum 10 cm of H20 for effect Severe Symptoms (not speaking, little or no air movement): As above, additionally: Epinephrine 0.3 mg 1:1000 IM OLMC if age >50, HR>150 or history of CAD Magnesium Sulfate 2 g IV in 100 ml D5W over 10 min Do not use if CHF or history of Renal Failure Acute Pulmonary Edema Suspected (History of CHF, peripheral edema elevated SBP) Nitroglycerin 0.4 mg SL every 3 min: Contraindicated if SBP <90 mmHg Contraindicated if use of a Phosphodiesterase-5 (PDE-5) inhibitor within last 24 hours (Viagra, Levitra); 48 hours (Cialis) Aspirin 324 mg PO Consider CPAP if symptoms moderate/severe: Start at 5cm of H2O and titrate up to maximum 15 cm of H20 for effect 28 If SBP > 150 consider Morphine Sulfate 5-10 mg IV For Hypotension (systolic BP <90 mmHg): Consider Dopamine infusion at 5-20 mcg/kg/min titrated to maintain SBP >90 mmHg If severe nausea or vomiting: Ondansetron (Zofran) 4 mg IV/IO/ODT For bronchospasm (wheezing) associated with Acute Pulmonary Edema: Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer May repeat Albuterol (Proventil) PRN for continued wheezing Consider Airway Management Protocol Drowning/Near Drowning Full ALS Assessment and Treatment Spinal Immobilization if indicated Protect from heat loss Patients may develop delayed onset respiratory symptoms: Consider CPAP for patients with significant dyspnea or hypoxia Start at 5cm of H2O and titrate up to maximum 15 cm of H20 for effect Airway Protocol as needed Refer to appropriate protocol if cardiac arrest present Contact Medical Control for any additional orders or questions Acute Bronchospasm: Contact Medical Control prior to Epinephrine administration if: Age > 50 years Heart Rate >150 History of Coronary Artery Disease 29 A P M Legend EMT A‐EMT Paramedic Medical Control Supplemental Oxygen A P M Assess ABC’s -Respiratory Rate ‐Effort ‐Adequacy Pulse Oximetry ADEQUATE Maintain SPO2 >93% Basic Maneuvers First ‐open airway ‐suction ‐nasal or oral airway INADEQUATE Awake and Protecting Airway Altered, Apneic SUCCESSFUL Consider CPAP OBSTRUCTION BIAD OR P RSA x2 Success < 2 attempts P Airway Obstruction Procedure x2 Resume BVM NO M P Percutaneous Cricothyrotomy (surgical airway) Simultaneously Contact Medical Control M P LEMON Look externally Evaluate with the 3:3:2 rule Mallampati classification Obstruction Neck Mobility Transport to Closest Facility M Consult Medical Control M Pearls If capnography is available it is expected to be used with all methods of intubation. Document results If an effective airway is being maintained by BVM with continuous pulse oximetry values of >93%, it is acceptable to continue with basic airway measures instead of using a Blind insertion device or intubation. For the purposes of this protocol a secure airway is when the patient is receiving appropriate oxygenation and ventilation An intubation attempt is defined as passing the laryngoscope blade or endotracheal tube past the teeth or inserted into the nasal passage Ventilatory rate should be 10‐12 per minute to maintain an ETCO2 of 35‐45. Avoid hyperventilation Quality assurance should always be completed after the use of blind insertion device or intubation Maintain C‐spine immobilization for patients with suspected spinal injury Do not assume hyperventilation is psychogenic – use oxygen, not a paper bag. Sellick’s and or BURP ( Backwards, Up, Rightward Pressure) maneuver should be used to assist with difficult intubations Consider Endotracheal Introducer (Bougie) for incompletely visualized airway. Hyperventilation in deteriorating head trauma should only be done to maintain an ETCO2 of 30‐35 Gastric tube placement should be considered in all intubated patients if available It is important to secure the endotracheal tube well and consider c‐collar to better maintain ETT placement Suction all debris, secretions from the airway if necessary Service MD Approval:______ Airway Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 30 2013 Post Placement Management Gastric Decompression GOOD AIR EXCHANGE NO AIR EXCHANGE NO CHEST RISE YES Confirm Airway Placement ETCO2 and Exam Continue BVM Maintain SpO₂ >93% SUCCESS Airway Protocol BVM UNSUCCESSFUL Airway Emergencies: Adult Airway Management All Providers General Patient Care Protocol—Adult Supplemental oxygen to maintain SPO2 > 93% If suspicion of trauma, maintain C-spine immobilization. Suction all debris, secretions from the airway if necessary Consider CPAP if protecting airway and awake If history of Asthma or COPD, Start at 5cm of H2O and titrate up to maximum 10 cm of H20 for effect If no history of Asthma or COPD, Start at 5cm of H2O and titrate up to maximum 15 cm of H20 for effect Perform Basic Airway Maneuvers: open airway, nasal/oral airway; BVM if needed. BVM: Ventilate once every 5-6 seconds (10-12 times/minute) If signs of airway obstruction refer to appropriate protocol If patient does not respond to above measures or deteriorates consider advanced airway placement Monitor oxygen saturation and end-tidal CO2 continuously Advanced EMT Consider IV Protocol if indicated Paramedic Full ALS Assessment and Treatment Follow algorithm if invasive airway intervention is needed (BIAD/ETT): Apnea Decreased level of consciousness with respiratory failure (i.e. hypoxia [O2 sat < 93%] not improved by 100% oxygen, and/or respiratory rate < 8) Poor ventilatory effort (with hypoxia not improved by 100% oxygen) Unable to maintain patent airway Follow appropriate procedure (Video Laryngoscopy, King LTS-D, Direct Laryngoscopy, etc) 31 Following placement of the ETT/BIAD confirm proper placement: Observe for presence of alveolar waveform on capnography Assess for absence of epigastric sounds, presence of breath sounds, and chest rise and fall Record tube depth and secure in place using a commercial holder if applicable Utilize head restraint devices (i.e. “head-blocks”) or rigid cervical collar and long spine board as needed to help secure airway device in place Capnography/ETCO2 Monitoring Digital capnography (waveform) is the system standard for ETCO2 monitoring. Only in the event digital capnography is not available due to on-scene equipment failure, is continuous colorimetric monitoring of ETCO2 an acceptable alternative. Continuous ETCO2 monitoring is a MANDATORY component of invasive airway management. If ETCO2 monitoring cannot be accomplished by either of the above methods, the invasive device MUST be REMOVED, and the airway managed non-invasively. If an alveolar waveform is not present with capnography (i.e. flat line), briefly check the filter line coupling to assure it is securely in place then remove the ETT or BIAD and proceed to the next step in the algorithm. 32 Under no circumstances should transport be delayed for Rapid Sequence Airway (RSA) if the additional time to perform the procedure is greater than the transport time. P x2 2 PARAMEDICS ARE REQUIRED AT ALL TIMES Simultaneously Contact Medical Control P x2 Airway Protocol Unsuccessful PreOxygenate (T-5 minutes) 100% O₂ x 5 minutes 8 vital capacity breaths with 100% O₂ (BVM/NRB) 2013 Pearls Indications: Age >18 unless specific permission given prior to procedure by Medical Control Need for invasive airway management in the setting of an intact gag reflex or inadequate sedation to perform non‐ pharmacologically assisted airway management (apnea, decreased LOC with respiratory failure, poor ventilatory effort (with hypoxia not improved by 100% O2), Unable to maintain patent airway by other means, Burns with suspected significant inhalation injury) Contraindications: Medication sensitivities Inability to ventilate via BVM Suspected Hyperkalemia Myopathy or neuromuscular disease History of Malignant Hyperthermia Recent crush injury or major burn (>48 hours after injury) End Stage Renal Disease Recent Spinal Cord Injury (72 hours – 6 months) Airway Protocol Service MD Approval:______ Preparation (T-8 minutes) IV, O₂, EKG, SpO₂, BP Check Laryngoscope, ETT, stylet, syringes Check rescue airway device Meds drawn up and labeled PreTreatment (T-3 minutes) Cricoid Pressure / Sellick’s maneuver Lidocaine 1.5mg/kg IV/IO IF head injured (max 150mg) Paralysis and Induction (T+0 minutes) Etomidate 0.3 mg/kg (max 20mg) Succinylcholine 2 mg/kg (max 200mg) Placement with Proof (T+ 30 seconds) ETCO₂ (continuous), Auscultation Secure Device SUCCESSFUL UNSUCCESSFUL Post Placement Airway Management (T+ 60 seconds) Morphine 3 mg IV/IO and Midazolam 3 mg IV/IO Repeat x2 if necessary Rocuronium 1mg/kg IV/IO IF transport time >10 minutes Continue BVM Maintain SpO₂ >93% Airway Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 33 Airway Emergencies: Rapid Sequence Airway Under no circumstances should transport be delayed for RSA if the additional time to perform the procedure is greater than the transport time. 2 PARAMEDICS ARE REQUIRED AT ALL TIMES All Providers General Patient Care Protocol—Adult Preoxygenate with 100% oxygen Basic Airway maneuvers: open airway, nasal and/or oral airway; BVM Paramedic Full ALS assessment and treatment Simultaneously contact OLMC Assess for Indications: Age ≥18 unless specific permission given prior to procedure by medical control Need for invasive airway management in the setting of an intact gag reflex or inadequate sedation to perform non pharmacologically assisted airway management: Apnea Decreased level of consciousness with respiratory failure (i.e. hypoxia [O2 sat < 90%] not improved by 100% oxygen, and/or respiratory rate < 8) Poor ventilatory effort (with hypoxia not improved by 100% oxygen) Unable to maintain patent airway by other means Burns with suspected significant inhalation injury Preoxygenate 100% oxygen at 15L/min for at least 5 min or 8 Vital Capacity (deep) breaths with 100% O2 Only assist ventilations with BVM if patient’s ventilations are inadequate or if hypoxemic (O2 Saturation < 93% on supplemental oxygen) Assisted ventilations increase risk of aspiration during laryngoscopy Patients cannot have any contraindications to succinylcholine or other RSA drugs: Inability to ventilate via BVM Suspected Hyperkalemia 34 Myopathy or neuromuscular disease History of Malignant Hyperthermia Recent crush injury or major burn (>48 hours after injury) End Stage Renal Disease Recent Spinal Cord Injury (72 hours-6 months) Procedure Preparation (T-8 minutes): Monitoring (continuous ECG, SpO2, Blood Pressure) 2 Patent IV’s required (IO is acceptable) Functioning laryngoscope and BVM with highflow O2 Endotracheal Tube(s), stylet, syringe(s) LEMON Look externally Evaluate with the 3:3:2 rule Mallampati classification Obstruction Neck Mobility BIAD(s) and appropriate syringe(s) Alternative/rescue airway (LMA and surgical airway kit) immediately available All medications drawn up and labeled (including post procedure sedation) Suction: on and functioning End-Tidal CO2 device on and operational (colorimetric immediately available as a back up only) Assess for difficult airway—LEMON Preoxygenation (T-5 minutes): 100% oxygen via NRB for 5 minutes or 8 Vital Capacity breaths (Deep breaths) via NRB or BVM. Minimize BVM to decrease gastric distention and risk of vomiting/aspiration. Pretreatment (T-3 minutes): Evidence of head injury or stroke: Lidocaine 1.5 mg/kg IV/IO (max 150 mg) Begin cricoid pressure/Sellick’s maneuver Paralysis and Induction (T + 0 minutes): Etomidate 0.3 mg/kg IV/IO (max dose 20 mg) Succinylcholine 2 mg/kg IV/IO (max dose 200 mg) Placement with Proof (T + 30 seconds): Place BIAD or ETT Confirm with: End Tidal CO2 waveform 35 Auscultation Physical findings Secure device, note position Post-Placement Airway Management (T + 60 seconds): Sedation Morphine Sulfate 3 mg IV/IO AND Midazolam 3 mg IV/IO after tube confirmed with ETCO2 (check BP prior to administration): May repeat X 2 as needed for sedation If additional paralysis needed and transport time is > 10 minutes consider: Rocuronium 1 mg/kg IV/IO (long acting paralytics mandates sedation as above) Contact Medical Control for any additional orders or questions 36 SIMULTANEOUSLY CONTACT MEDICAL CONTROL Preparation (T-8 minutes) Monitoring (continuous ECG, Sp02, Blood Pressure) 2 patent IVs Functioning Laryngoscope and BVM with highflow O2 Endotracheal tube(s), stylet, syringe(s) BIAD(s) and appropriate syringe(s) Alternative/Rescue Airway (LMA and surgical airway kit) immediately available All medications drawn up and labeled (including post-procedure sedation) Suction--turned on and functioning End Tidal CO2 device on and operational (colorimetric immediately available as back-up only) Assess for difficult airway--LEMON Preoxygenate 100% O2 x 5 minutes (NRB) or 8 VC breaths with 100% O2 (BVM/NRB) Pretreatment (T-3 minutes) Evidence of head injury or stroke Lidocaine 1.5 mg/kg IV/IO (max 150 mg) Begin cricoid pressure/Sellick’s maneuver Paralysis and Induction (T=0) Etomidate 0.3 mg/kg (max 20 mg) Succinylcholine 2 mg/kg (max 200 mg) Placement with Proof (T+30 seconds) Place BIAD/ETT Confirm with: --End Tidal CO2 waveform --Auscultation --Physical Findings Secure Device, note position Post-Placement Management (T+1 minute) Sedation: Morphine 3 mg IV/IO AND Midazolam 3 mg IV/IO, repeat X2 as needed. If additional paralysis needed and transport time > 10 minutes: Rocuronium 1 mg/kg IV/IO 37 Airway Emergencies: Failed Airway When in failed airway scenario, immediate transport to the nearest emergency department is required Simultaneously Contact Medical Control All Providers General Patient Care Protocol—Adult If ventilation ineffective with single person BVM, place nasal and/or oral airway and begin two-person BVM. Attempt ventilation with BVM and oral and/or nasal airway: Acceptable air exchange: Continue with BVM, rapid transport indicated Monitor oxygen saturation, end tidal carbon dioxide and cardiac parameters continuously If unable to ventilate effectively with basic airway maneuvers using BVM and patient has no gag reflex, place advanced airway. Paramedic Full ALS Assessment and Treatment Simultaneously notify OLMC Failed Intubation/BIAD Attempt ventilation with BVM and oral and/or nasal airway: Acceptable air exchange: Continue with BVM, rapid transport indicated Monitor oxygen saturation, end tidal carbon dioxide and cardiac parameters continuously Unacceptable air exchange: Place BIAD (if not previously attempted) Acceptable air exchange: 38 Monitor oxygen saturation, end tidal carbon dioxide and cardiac parameters continuously No air exchange: Can’t intubate/place advanced airway/can’t ventilate situation Percutaneous Cricothyrotomy (Surgical Airway) 39 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Onset and location Insect sting or bite Food allergy / exposure Medication allergy / exposure New clothing, soap, detergent Past history of reactions Past medical history Medication history Medical Protocol Differential Urticaria (rash only) Anaphylaxis (systemic effect) Shock (vascular effect) Angioedema (drug induced) Aspiration / Airway obstruction Vasovagal event Asthma or COPD CHF Signs and Symptoms Itching or hives Coughing / wheezing Respiratory distress Chest or throat constriction Difficulty swallowing Hypotension or shock Edema General Approach to All Adult Patients Mild Reaction Hives / Rash Only No respiratory component IV Protocol Epinephrine 1:1000 Auto‐Injector * 0.3mg Epinephrine 1:1000 IM A A Albuterol 2.5mg/3ml & Ipratropium 0.5mg/2.5ml** P Diphenhydramine 50 mg IV/IM/IO P Famotidine 20 mg in 100 ml D5W P P Albuterol 2.5mg/3ml & Ipratropium 0.5mg/2.5ml A IV Protocol P Diphenhydramine 50 mg IV/IM/IO P Famotidine 20 mg in 100 ml D5W P P A Pearls RECOMMENDED EXAM: Mental Status, Skin, Heart, Lungs *Contact Medical Control: prior to administering epinephrine in patients who are >50 years of age, have a history of cardiac disease, or if the patients heart rate is >150. Epinephrine may precipitate cardiac ischemia. These patients should receive a 12 Lead EKG Famotidine, IV piggyback over 15 minutes (if not already given) **May repeat Albuterol PRN for continued wheezing – max 3 doses The shorter the onset from symptoms to contact, generally the more severe the reaction A *0.3mg 2013 A Moderate Reaction Dyspnea, Wheezing, Chest Tightness Severe Reaction Evidence of Impending Respiratory Distress or Shock A IV Protocol P Diphenhydramine 50 mg IV/IM/IO P Famotidine 20 mg in 100 ml D5W P P P Methylprednisolone 125 mg IV/IO Imminent Cardiac Arrest *** P Epinephrine 1:10,000 0.5mg IV P M Simultaneously Contact Medical Control M *** Severe bradycardia, unresponsive, no obtainable blood pressure or radial pulse A P Continued Severe Symptoms Epinephrine Infusion: MP Mix 2mg (1:1000) in 250ml NS Start at 2mcg/min (max 10mcg/min) PM Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 40 Allergic Reaction All Providers General Patient Care Protocol—Adult Assist patient in self-administration of previously prescribed epinephrine auto-injector (Epi-Pen) If wheezing present: Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer May repeat Albuterol PRN for continued wheezing (max 3 doses) Mild Reaction (Itching/Hives) Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment Consider Diphenhydramine (Benadryl) 50 mg IV/IM/IO Consider Famotidine 20 mg in 100 ml D5W, IV Piggyback over 15 min Moderate Reaction (Dyspnea, Wheezing, Chest Tightness) As for mild symptoms, additionally: All Providers Albuterol (Proventil) 2.5 mg/3 ml and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer, if not already given May repeat Albuterol PRN for continued wheezing (max 3 doses) Advanced EMT Consider IV Protocol Paramedic Diphenhydramine (Benadryl) 50 mg IV/IM/IO (if not already given) Famotidine 20 mg in 100 ml D5W, IV Piggyback over 15 min (if not already given) 41 Severe Systemic Reaction (SBP <90mmHg, Stridor, Severe Respiratory Distress) As for moderate symptoms, additionally: All Providers Epinephrine 1:1000, 0.3 mg IM (OLMC for approval if age>50, HR>150, history of CAD) Albuterol (Proventil) 2.5 mg/3 ml via nebulizer May repeat PRN for continued wheezing (max 3 doses) Advanced EMT Consider IV Protocol Consider Fluid Bolus-500cc NS (max 2 liters) Paramedic Diphenhydramine (Benadryl) 50 mg IV/IM/IO (if not already given) Famotidine 20 mg in 100 ml D5W, IV Piggyback over 15 min (if not already given) Methylprednisolone (Solumedrol) 125 mg IV/IO Imminent Cardiopulmonary Arrest (severe bradycardia, unresponsive, no obtainable blood pressure or radial pulse) Paramedic As for severe systemic reaction, additionally: Epinephrine 1:10,000, 0.5 mg IV Cardiac Arrest Paramedic Refer to the appropriate protocol based on presenting rhythm In the setting of cardiac arrest, the following items should be performed in the post-resuscitative phase, when time allows: Albuterol (Proventil) 2.5 mg/3 ml via nebulizer May repeat PRN for continued wheezing (max 3 doses) Diphenhydramine (Benadryl) 50 mg IV/IO (if not already given) Famotidine 20 mg in 100 ml D5W, IV Piggyback over 15 min (if not already given) Methylprednisolone (Solumedrol) 125 mg IV/IO (if not already given) Contact Medical Control for any additional orders or questions Epinephrine Infusion: Mix 2 mg (1:1000) in 250 ml NS Start at 2 mcg/min, maximum 10 mcg/min 42 A P M Legend EMT A‐EMT Paramedic Medical Control A P M General Approach to All Adult Patients Blood Glucose Glucose <70 A IV Protocol Glucose >70 A A A A Consider other causes: Head injury, OD/toxic ingestion, stroke, hypoxia, hypothermia No Improvement in Altered Mental Status P Improved Assess Cardiac Rhythm P 12 Lead EKG A M Consider *Naloxone 2mg IV/IO/IN**/IM Every 3 minutes (max 8mg) 2013 Consider Oral Glucose 15g if awake and no risk of aspiration If no IV, Glucagon 1mg IM if unable to use glucose Dextrose 12.5‐25g Or D10W 100mL IV A Differential Head Trauma CNS (stroke, tumor, seizure, infection) Cardiac (MI, CHF) Hypothermia Infection (CNS or other) Thyroid (hyper/hypo) Shock (septic, metabolic, traumatic) Diabetes (hyper/hypo) Toxicologic or Ingestion Acidosis/Alkalosis Environmental exposure Pulmonary (hypoxia) Electrolyte abnormality Psychiatric disorder Medical Protocol Signs and Symptoms Decreased mental status Lethargy Change in baseline mental status Bizarre behavior Hypoglycemia (cool/ diaphoretic skin) Hyperglycemia (warm, dry skin, fruity breath, kussmaul respirations, signs of dehydration Irritability History: Known Diabetic, Medic alert tag Drugs, drug paraphernalia Report of illicit drug Use or toxic ingestion Past medical history Medications History of Trauma Change in condition Changes in feeding or sleep habits Contact Medical Control IV bolus 250 ml x1 If clinically hypovolemic (orthostatic hypotension/dry mucous membranes) A M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro. Pay special attention to the head exam for signs of bruising or other injury. * Naloxone (Narcan) can be administered in 0.4 mg increments titrated to respiratory drive and level of consciousness ** for Intranasal administration A-EMT should administer 0.5mg per nare, total of 1mg and then proceed with additional doses as needed. (Paramedics may give 1 mg per nare) Be aware of AMS as presenting sign of an environmental toxin or Hazmat exposure and protect personal safety It is safer to assume hypoglycemia than hyperglycemia if doubt exists. Recheck blood glucose after Dextrose or glucagon Do not let alcohol confuse the clinical picture. Alcoholics frequently develop hypoglycemia and may have unrecognized injuries Low glucose (<70), normal glucose (70‐120), high glucose (>250) Consider restraints if necessary for patients and/or personnel's protection per the restraint protocol Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 43 Altered Mental Status All Providers General Patient Care Protocol—Adult Blood Glucose If hypoglycemic (Blood glucose < 70mg/dL) Glucose paste 15 g or other oral glucose agent (e.g. orange juice) if patient alert enough to self-administer If hypoglycemic and unable to take oral glucose: Consider Glucagon 1mg IM If Stroke suspected, see Stroke Protocol If Head Injury suspected, see Trauma/Head Injury Protocol If severely agitated and/or violent see Behavioral Emergencies Protocol If cardiac arrhythmia present see appropriate Cardiac Arrhythmia Protocol Advanced EMT Consider IV Protocol If Drug (narcotic) overdose suspected: Naloxone (Narcan) 2 mg IV/IO every 3 minutes (maximum 8 mg) ▪ Naloxone (Narcan) can be administered in 0.4 mg increments titrated to respiratory drive and level of consciousness ▪ If IV access has not been established, Naloxone (Narcan) 2 mg IM or 0.5 mg per nare IN (total 1.0mg per administration) ● If hypoglycemic Dextrose 12.5g-25g IV or D10W 100mL IV ▪ May repeat as needed every 5-10 minutes to blood glucose >100 mg/dL If Clinically hypovolemic (orthostatic hypotension / dry mucous membranes) IV bolus 250ml x1. Paramedic ● Full ALS Assessment and treatment ● If hypoglycemic (Blood glucose < 70 mg/dL) with IV access: Dextrose 12.5g-25g IV or D10W 100mL IV May repeat as needed every 5-10 minutes to blood glucose >100 mg/dL ● If hypoglycemic (Blood glucose < 70 mg/dL) without IV access: 44 Glucose paste 15 g or other oral glucose agent (e.g. orange juice) if patient alert enough to self administer ● If hypoglycemic and unable to take oral glucose: Glucagon 1 mg IM ● If Drug (narcotic) overdose suspected: Naloxone (Narcan) 2 mg IVP every 3 minutes (maximum 8 mg) ▪ Naloxone (Narcan) can be administered in 0.4 mg increments titrated to respiratory drive and level of consciousness ▪ If IV access has not been established, Naloxone (Narcan) 2 mg IM or IN via mucosal atomizer device Note: Patients presenting with altered mental status, who respond to Narcan are not candidates for informed refusal. Due to the relatively short half-life of Narcan, these patients are at risk for return of symptoms. These patients should be transported to the emergency department, regardless of an apparently normal mental status. Contact Medical Control for any additional orders or questions 45 A P M Legend EMT A‐EMT Paramedic Medical Control (Excited Delirium) A P M History: Situational crisis Psychiatric illness/medications Injury to self or threats to others Medic alert tag Substance abuse / overdose Diabetes Signs and Symptoms Anxiety, agitation, confusion Affect change, hallucinations Delusional thoughts, bizarre behavior Combative / violent Expression of suicidal / homicidal thoughts Scene Safety Medical Protocol Differential See altered mental status differential Alcohol intoxication Toxin / substance abuse Medication effect / overdose Withdrawal syndromes Depression Bipolar (manic‐depressive) Schizophrenia Anxiety disorders General Approach to All Adult Patients Remove patient from stressful environment Use verbal calming techniques (reassurance, calm, establish rapport) GCS and Pupil Assessment on all patients Paramedics should be considered EARLY NEVER restrain in the PRONE position 2013 Go to appropriate protocol: Altered Mental Status Protocol Overdose / Toxic Ingestion Protocol Head Trauma Protocol Service MD Approval:______ Check glucose if any suspicion of hypoglycemia Altered Mental Status Protocol <70 >70 Restraint Procedure * Haloperidol 5mg IM if <60kg or 10mg IM if >60kg** Lorazepam 1‐2mg IM (can be combined with Haloperidol) P A P IV Protocol A 250 ml bolus (max 2L total) If Cocaine/Sympathomimetic toxicity suspected: M Lorazepam 1mg IV/IM Repeat 1mg IV/IM if needed If patient refuses care Contact Medical Control P M P OR M P Ketamine 4mg/kg IM P M Pearls RECOMMENDED EXAM: Mental Status, Skin, Heart, Lung, Neuro SAFETY FIRST! * Never retrain or transport in prone position **Avoid if recent history of MAO inhibitor use (ie. Phenelzine, Transylcypomine) Consider Haloperidol for patients with history of psychosis Do not overlook the possibility of associated domestic violence or child abuse If patient in excited delirium suffers cardiac arrest, follow appropriate cardiac arrest protocol. All patients who receive either physical or chemical restraint MUST continuously be observed by ALS personnel on scene or immediately upon their arrival. Any patient handcuffed or restrained by law enforcement, law enforcement must ride in ambulance Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 46 Behavioral Emergencies/Excited Delirium Strongly Consider Paramedic Assistance All Providers General Patient Care Protocol—Adult Apply physical restraints if needed to ensure patient/crew safety. Adhere to procedure on Physical Restraint of Agitated Patients when this process is deemed necessary Blood Glucose Measurement-if < 70 mg/dl, refer to Altered Mental Status Protocol Assess and treat for hyperthermia Advanced EMT Consider IV Protocol Paramedic When Chemical or Physical restraints are used, perform Full ALS Assessment and Treatment For patients with severe agitation compromising patient/crew safety, or for patients who continue to struggle against physical restraints: Haloperidol (Haldol) 5 mg IM if, 60 kg or 10mg IM if >60 kg Avoid if recent history of MAO inhibitor use (e.g. Phenelzine, Tranylcypromine) Lorazepam (Ativan) 1-2 mg IM (can be combined in same syringe as Haldol) If concerns for Excited Delirium: 250 ml bolus Normal Saline IV – x4 (2L max) If cocaine/sympathomimetic toxicity strongly suspected: Lorazepam (Ativan) 1 mg IV/IM Repeat Lorazepam (Ativan) 1 mg IM/IV if adequate sedation not achieved on initial dose Note: NEVER restrain or transport in prone position! Contact Medical Control for all refusals or non-transports Contact Medical Control for any additional orders or questions Paramedics - Ketamine 4 mg/kg IM with Medical Control Permission 47 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Type of bite/sting Description or bring creature/ photo with patient for identification Time, location, size of bite/sting Previous reaction to bite/sting Domestic vs. wild Tetanus and rabies risk Immunocompromised patient Signs and Symptoms Rash, skin break, wound Pain, soft tissue swelling, redness Blood oozing from the bite/ wound Evidence of infection Differential Animal bite Human bite Snake bite (poisonous) Spider bite (poisonous) Insect sting/bite (bee, wasp, ant, tick) Infection risk Rabies risk Tetanus risk Medical Protocol General Approach to All Adult Patients Irrigate/Cleanse wound with 0.9% NaCl (remove any large debris) Remove stinger if wasp/bee (if easily removed) Mark edematous area with pen and note time Immobilize affected part and remove distal jewelry Refer to Pain Control Protocol if there is significant pain If there is allergic reaction refer to Allergic Reaction Protocol A M Contact Medical Control IV Protocol If SBP<90mmHg, consider 500 ml bolus NS (total 2L) P M If no improvement from 2L fluid bolus Dopamine infusion at 5‐20mcg/kg/min titrated to maintain SBP>90mmHg A Service MD Approval:______ P Pearls RECOMMENDED EXAM: Mental Status, Skin, Extremities (location of injury), and a complete Neck, Lung, Heart, Abdomen, Back, and Neuro exam if systemic effects are noted. Human bites have higher infection rates than animal bites due to normal mouth bacteria Carnivore bites are much more likely to become infected and all have risk of rabies exposure Cat bites may progress to infection rapidly due to a specific bacteria (pasteurella multicoda) Snake bites: amount of envenomation is variable, generally worse with larger snakes and early in spring, if no pain or swelling envenomation is unlikely, it is NOT necessary to take the snake to the ED with the patient. Black widow spider bites tend to be minimally painful, but over a few hours, muscular pain and severe abdominal pain may develop (spider is black with red hourglass on belly) Brown recluse spider bites are minimally painful to painless. Little reaction is noted initially but tissue necrosis at the site of the bite develops over the next few days (brown spider with fiddle shape on back). An alternative to bringing the offender to the Emergency Department would be to take a picture of the animal/insect Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 48 Bites and Envenomations All Providers General Patient Care Protocol—Adult Irrigate/Cleanse wound with 0.9% NaCl (remove any large debris) Remove stinger if wasp/bee (if easily removed) Mark edematous area with pen and note time Immobilize affected part and remove distal jewelry Attempt to identify what caused bite and bring to Emergency Department if dead (use caution when handling dead snakes as envenomation has occurred secondary to reflex motor movement) – an alternative is taking a picture of the animal/insect. Refer to Allergic Reaction Protocol as indicated Transport to closest appropriate facility Advanced EMT Consider IV Protocol For hypotension (SBP<90 mmHg) consider 500 ml IV 0.9% NaCl fluid boluses up to 2L. Paramedic Full ALS Assessment and Treatment For hypotension (SBP<90 mmHg) not improved with fluid boluses up to 2L 0.9% NaCl, or when fluid boluses are contraindicated: Dopamine infusion at 5-20 mcg/kg/min titrated to maintain SBP>90 mmHg Contact Medical Control for any additional orders or questions 49 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Signs and Symptoms Unresponsive Apneic Pulseless History: Events leading to arrest Estimated downtime Past Medical History Medications Existence of terminal illness Signs of lividity, rigor mortis DNR Differential Medical or Trauma Vfib vs Pulseless Vtach Asystole Pulseless electrical activity (PEA) Withhold Resuscitation Cardiac Protocol General Approach to All Adult Patients Criteria for Death/No Resuscitation Indicated YES Call “patient contact” to dispatch when you arrive at patients side Continue compressions until Defib pads in place and monitor charged. YES Adequate Bystander CCR or CPR? NO 2013 AT ANY TIME Return of spontaneous circulation ‐> Go to Post Resuscitation Protocol Immediately perform compressions at a rate of 100 compressions per minute for 2 minutes Stop compressions for rhythm analysis (<5seconds) If VT or VF (or AED advises shock) DEFIBRILLATE (call 1st shock to dispatch) If PEA/Asystole – (or AED advises no shock) do NOT shock Go to appropriate Protocol and Resume compressions A IV Protocol A Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status Immediately after defibrillation, resume chest compressions with a different operator compressing. Do not pause for post‐shock rhythm analysis. Stop compressions only for signs of life (patient movement) or rhythm visible through compressions on monitor or pre‐defibrillation rhythm analysis every 2 minutes and proceed to appropriate protocol CCR is indicated in ADULT patients that have suffered cardiac arrest of a presumed cardiac nature. It is not indicated in those situations where other etiologies are probable (OD, drowning, hanging, etc.) In these instances CPR is indicated CCR is not to be used on individuals less than 18 years of age. Successful resuscitation requires planning and clear role definition In the event a patient suffers cardiac arrest in the presence of EMS, the absolute highest priority is to apply the AED/Defibrillator and deliver a shock immediately if indicated. Reassess airway frequently and with every patient move. DO NOT INTERRUPT CHEST COMPRESSIONS! Designate a “code leader” to coordinate transitions, defibrillation and pharmacological interventions. “Code Leader” ideally should have no procedural tasks. Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 50 Cardiac Arrest: General Approach General CCR is indicated in ADULT patients that have suffered cardiac arrest of a presumed cardiac nature. It is not indicated in those situations where other etiologies are probable (overdose, drowning, hanging etc.). In these instances CPR is indicated. CCR is not to be used on individuals less than 18 years of age. Successful resuscitation requires planning and clear role definition. In the event a patient suffers cardiac arrest in the presence of EMS (EMS witnessed Cardiac Arrest), the absolute highest priority is to apply the AED/Defibrillator and deliver a shock immediately if indicated. Reassess airway frequently and with every patient move. DO NOT INTERRUPT CHEST COMPRESSIONS! Designate a “code leader” to coordinate transitions, defibrillation and pharmacological interventions. “Code Leader” should ideally not have any procedural tasks. If the “code leader” is needed for a specific task, a new leader must be designated. All Providers General Patient Care Protocol (including blood glucose) Check responsiveness and check for a carotid pulse Call “patient contact” to dispatch when you arrive at the patient’s side If adequate bystander compressions ongoing, continue compressions until monitor pads in place and monitor charged. Stop compressions for rhythm analysis (< 5 sec) If VT or VF (or AED Advises Shock), defibrillate Call “first shock” time to dispatch If PEA/Asystole, go to appropriate protocol and resume compressions Immediately after defibrillation, resume chest compressions with a different operator compressing. Do not pause for post-shock rhythm analysis. Stop compressions only for signs of life (patient movement) or rhythm visible through compressions on monitor or pre-defibrillation rhythm analysis every 2 minutes If compressions are not being performed upon arrival or if compressions are not deemed adequate, immediately perform compressions at a rate of 100 compressions per minute for 2 minutes. Advanced EMT Consider IV Protocol Paramedic See Protocol based on presenting rhythm 51 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Past Medical History Medications Events leading to arrest End stage renal disease Estimated downtime Suspected hypothermia Suspected Overdose DNR Signs and Symptoms Pulseless Apneic No electrical activity on ECG No auscultated heart tones Differential Medical or Trauma Hypoxia Potassium (hypo/hyper) Drug Overdose Acidosis Hypothermia Device (lead) error Death Cardiac Protocol Cardiac Arrest Protocol Withhold Resuscitation YES Criteria for Death / No resuscitation NO AT ANY TIME Return of spontaneous circulation ‐> Go to Post Resuscitation Protocol A IV Protocol P P Termination of Resuscitation Protocol Epinephrine 1mg IV/IO every 3‐5 minutes 2013 5 cycles of CPR unless arrest witnessed by AED equipped personnel A P Consider Correctable Causes Hypoxia – secure airway and ventilate Hypoglycemia – Dextrose 12.5‐25g or D10W 100ml IV/IO Hyperkalemia – Sodium bicarbonate 1mEq/kg IV/IO ‐ Calcium Chloride 1g IV/IO Hypothermia – Active Rewarming Calcium Channel and B-Blocker OD – Glucagon 3mg IV/IO Calcium Channel Blocker OD – Calcium Chloride 1g IV/IO (avoid if patient on Digoxin/Lanoxin) Tricyclic antidepressant OD – Sodium Bicarbonate 1mEq/kg IV/IO Possible Narcotic OD – Naloxone 2mg IV/IO YES P After 20 Minutes Criteria for Discontinuation NO Pearls RECOMMENDED EXAM: Mental Status When Asystole is seen on the cardiac monitor, confirmation of the rhythm shall include a printed rhythm strip as well as interpretation of the rhythm in more than one lead. Low amplitude Vfib or PEA may be difficult to distinguish from asystole when using only the cardiac monitor for interpretation. Continue Epinephrine and correctable causes M Consult Medical Control M Service MD Approval:______ Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 52 Cardiac Arrest: Asystole Note: When Asystole is seen on the cardiac monitor, confirmation of the rhythm shall include a printed rhythm strip, as well as interpretation of the rhythm in more than one lead. Low amplitude V-Fib or PEA may be difficult to distinguish from asystole when using only the cardiac monitor for interpretation. All Providers Follow Cardiac Arrest—General Approach Protocol Paramedic Consider and treat possible causes Potential Causes of Asystole Hypoxia Treatment Secure airway and ventilate Dextrose 25 g IV/IO; repeat as needed to achieve blood glucose >70 Sodium bicarbonate 1 mEq/kg IV/IO Calcium Chloride 1 g IV/IO Active re-warming See below Hypoglycemia Hyperkalemia (end stage renal disease) Hypothermia Tablets (drug overdose) Epinephrine 1 mg IV/IO every 3-5 min during arrest Drug overdoses (see specific drug OD/toxicology section) Glucagon 3 mg IV/IO for calcium channel and B-blocker OD Calcium Chloride 1 g IV/IO for calcium channel blocker OD Avoid if patient on Digoxin/Lanoxin Sodium Bicarbonate 1 mEq/kg, IV/IO for Tricyclic antidepressant OD Naloxone (Narcan) 2 mg IV/IO for possible narcotic OD If no response to resuscitative efforts in 20 minutes (at least 2 rounds of drugs) consider discontinuation of efforts (see Termination of Resuscitation Protocol) Contact Medical Control for any additional orders or questions 53 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Signs and Symptoms Pulseless Apneic Electrical activity on ECG No heart tones on auscultation Cardiac Protocol History: Past Medical History Medications Events leading to arrest End stage renal disease Estimated downtime Suspected hypothermia Suspected Overdose DNR Differential Hypovolemia (trauma, AAA, other) Cardiac Tamponade Hypothermia Drug Overdose (Tricyclics, Digitalis, Beta Blockers, Calcium channel blockers) Massive MI Hypoxia Tension pneumothorax Pulmonary embolus Acidosis hyperkalemia Cardiac Arrest Protocol A P Epinephrine 1mg IV/IO every 3‐5 minutes P Do NOT discontinue compressions unless there is a definite pulse P Service MD Approval:______ 2013 AT ANY TIME Return of spontaneous circulation ‐> Go to Post Resuscitation Protocol A IV Protocol Consider Correctable Causes Hypovolemia (most common) – NS 1-2L IV/IO Hypoxia – secure airway and ventilate Hydrogen Ion (acidosis) – Sodium Bicarbonate 1mEq/kg IV/IO Hyperkalemia – Sodium bicarbonate 1mEq/kg IV/IO ‐ Calcium Chloride 1g IV/IO Hypothermia – Active Rewarming Calcium Channel and B-Blocker OD – Glucagon 3mg IV/IO Calcium Channel Blocker OD – Calcium Chloride 1g IV/IO (avoid if patient on Digoxin/Lanoxin) Tricyclic antidepressant OD – Sodium Bicarbonate 1mEq/kg IV/IO Possible Narcotic OD – Naloxone 2mg IV/IO Cardiac Tamponade – NS 1‐2 L IV/IO and expedite transport Tension pneumothorax – Needle thoracostomy Coronary or Pulmonary Thrombosis – Expedite Transport Pearls RECOMMENDED EXAM: Mental Status Consider each cause listed in the differential: survival is based on identifying and correcting the cause. Discussion with Medical Control can be a valuable tool in developing a differential diagnosis and identifying possible treatment options. M Consult Medical Control Termination of Protocol MResuscitation after 20 minutes P M Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 54 Cardiac Arrest: Pulseless Electrical Activity (PEA) All Providers Follow Cardiac Arrest—General Approach Protocol Paramedic Consider and treat possible causes Potential Causes of PEA Treatment Hypovolemia (most common) Normal Saline 1-2 liters IV/IO Hypoxia Secure airway and ventilate Hydrogen Ion (acidosis) Sodium Bicarbonate 1 mEq/kg IV/IO Hyperkalemia (end stage renal disease) Sodium Bicarbonate 1 mEq/kg IV/IO Calcium Chloride 1 g IV/IO Hypothermia Active rewarming Tablets (drug overdose) See below Tamponade, Cardiac Normal Saline 1-2 liters IV/IO Expedite transport Tension pneumothorax Needle thoracostomy Thrombosis, Coronary Expedite transport Thrombosis, Pulmonary Expedite transport Epinephrine 1 mg IV/IO every 3-5 minutes Do not discontinue compressions unless there is a definite pulse Drug overdoses (see specific drug in OD/toxicology section) Glucagon 3 mg IV/IO for calcium channel and B blocker Calcium Chloride 1 g IV/IO for calcium channel blocker or suspected hyperkalemia (dialysis patient) ▪ Avoid if patient on Digoxin/Lanoxin Sodium Bicarbonate 1 mEq/kg, IV/IO for Tricyclic antidepressant OD Naloxone (Narcan) 2 mg IV/IO for possible narcotic OD If no response to resuscitative efforts in 20 minutes (at least 2 rounds of drugs) consider discontinuation of efforts (see Termination of Resuscitation Protocol) 55 A P M Legend EMT A‐EMT Paramedic Medical Control Ventricular Fibrillation Pulseless Vent. Tachycardia A P M History: Estimated down time Past medical history Medications Events leading to arrest Renal failure / dialysis DNR or living will Differential Asystole Artifact / Device failure Cardiac Endocrine / Metabolic Drugs Pulmonary Signs and Symptoms Unresponsive, apneic, pulseless Ventricular fibrillation or ventricular tachycardia on EKG Cardiac Arrest Protocol Cardiac Protocol Defibrillate x1 * AT ANY TIME Rhythm Changes to Nonshockable Rhythm Go to appropriate protocol After defibrillation resume CCR without pulse check Apply non‐rebreather as soon as other care activities will not be interrupted After 2 minutes of CCR Check rhythm – if VF/VT persists Defibrillate – CCR immediatly A AT ANY TIME Return of spontaneous circulation ‐> Go to Post Resuscitation Protocol P Epinephrine 1mg IV/IO every 3‐5 minutes A P Consider Vasopressin 40 units IV/IO with 1st or 2nd epi dose only 2013 P Establish IV/IO P After 2 minutes of CCR Check rhythm – if VF/VT persists Defibrillate – CCR immediatly P P M Amiodarone 300mg IV/IO bolus For persistent VT/VF give Amiodarone 150mg IV/IO bolus on second round P If Polymorphous VT or hypomagnesemic state‐ Magnesium Sulfate 2g IV/IO push over 1‐2 min If suspected hyperkalemia or tricyclic OD Sodium Bicarbonate 1mEq/kg IV/IO If suspected hyperkalemia – Calcium Chloride 1g IV/IO Termination of Resuscitation Protocol M YES Continue cycle of compressions and Drug, rhythm check, compressions shock etc. P Criteria for Discontinuation after 20 minutes NO Pearls RECOMMENDED EXAM: Mental Status *Call first defibrillation time to 911 Center Reassess and document advanced airway placement and EtCO2 frequently, after every move, and at transfer of care. Treatment priorities are: uninterrupted chest compressions, defibrillation, then IV access and airway control. M Consult Medical Control M Service MD Approval:______ Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 56 Cardiac Arrest: Ventricular Fibrillation/ Pulseless Ventricular Tachycardia All Providers Follow Cardiac Arrest—General Approach Protocol Defibrillate for persistent VF/VT use manufacturer recommended energy settings, typically 200J or 360 J ⇒ Continue Chest Compressions immediately after shock (do not stop for pulse or rhythm check) ⇒ Call first defibrillation time to dispatch Analyze rhythm after 2 minutes of good CPR; If VF/VT persists: Defibrillate at 200 J (360 J if available) Continue compressions immediately after shock (do not stop for pulse or rhythm check) Paramedic Epinephrine 1 mg IV/IO every 3-5 min during arrest Vasopressin 40 Units IV/IO with 1st or 2nd Epinephrine doses only Analyze rhythm after 2 minutes of good CPR; If VF/VT persists: Defibrillate at 200 J (360 J if available) Continue Chest Compressions immediately after shock (do not stop for pulse or rhythm check) Amiodarone 300mg IV/IO bolus For persistent VT/VF give Amiodarone 150 mg IV/IO bolus on second round Continue cycle of Compressions & Drug Rhythm Check Compressions Shock Compressions & Drug Rhythm Check Compressions Shock as needed Additional interventions to consider in special circumstances Magnesium Sulfate 2 g IV/IO push over 1-2 minutes only if suspected Polymorphous VT (torsades de pointes) or hypomagnesemic state (chronic alcohol or diuretic use) Sodium Bicarbonate 1 mEq/kg, IV/IO if suspected hyperkalemia (dialysis patient) or tricyclic antidepressant OD Calcium Chloride 1 g IV/IO if suspected hyperkalemia (dialysis patient) Contact Medical Control for any additional orders or questions 57 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Respiratory Arrest Cardiac Arrest Differential Continue to address specific differentials associated with the original dysrhythmia Signs and Symptoms Return of pulse Repeat Primary Assessment P P Consider Induced Hypothermia Protocol Continue Ventilatory Support A P IV Protocol Cardiac Monitor Cardiac Protocol 100% Oxygen ETCO2 goal 40 RR <12 DO NOT HYPERVENTILATE A P Vital Signs (including PulseOx) 12 Lead EKG Hypotension SBP<90mmHg A P Normal Saline bolus 250ml x2 Re Arrest Combative A If not improved by NS bolus ‐Dopamine infusion 5‐20 mcg/kg/min titrated to maintain SBP >90mmHg ‐ Additional 250 ml bolus x2 to 2L max 2013 Continue anti‐arrythmic if ROSC was associated with its use P Lorazepam 1‐2 mg slow IV/IO may repeat x1 (max dose 4mg) or Midazolam 1‐2 mg slow IV/IO may repeat x1 (max dose 4mg) P Follow appropriate arrest protocol P M Consult Medical Control if needed M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Extremities, Neuro Hyperventilation is a significant cause of hypotension and recurrence of cardiac arrest in the post resuscitation phase and must be avoided at all costs. ETCO2 goal is 40mmHg. Most patient’s immediately post resuscitation will require ventilatory assistance The condition of post‐resuscitation patients fluctuates rapidly and continuously, and they require close monitoring. Appropriate post‐ resuscitation management may best be planned in consultation with medical control Common causes of post‐resuscitation hypotension include hyperventilation, hypovolemia, pneumothorax, and medication reaction to ALS drugs Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 58 Cardiac Arrest: Post Resuscitation Care All Providers General Patient Care Protocol—Adult Maintain assisted ventilation as needed Supplemental 100% oxygen ETCO2 if available Paramedic Full ALS Assessment and Treatment Monitor ETCO2, goal is 40mmHg, DO NOT HYPERVENTILATE For hypotension (systolic BP <90 mmHg) not improved by fluid boluses, or when fluid administration is contraindicated: Dopamine infusion at 5-20 mcg/kg/min titrated to maintain systolic BP >90 mmHg If VF/pulseless VT occurred during arrest AND Amiodarone was administered, no additional anti-arrhythmic is required unless arrhythmia recurs. If VF/VT reoccurs after previous conversion with Amiodarone 300 mg: Defibrillate and administer Amiodarone 150 mg IV/IO If patient becomes combative, administer: Lorazepam (Ativan) 1-2 mg slow IV/IO may repeat X 1 (maximum dose 4 mg) or Midazolam (Versed) 1-2 mg slow IV/IO, may repeat X 1 (maximum 4 mg) Consider Therapeutic/Induced Hypothermia Protocol Transport to nearest appropriate facility Contact Medical Control for any additional orders or questions 59 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Non‐traumatic cardiac arrests (drownings and hangings/ asphyxiation are permissible in this protocol) Signs and Symptoms Cardiac Arrest ROSC post‐cardiac arrest Differential Continue to address specific differentials associated with the original dysrhythmia 12 Lead EKG Assessment and document GCS Criteria for Inclusion Transport and continue post resuscitation care Does NOT Meet criteria Witnessed Cardiac Arrest with ROSC Not Pregnant Age = or >18 No evidence of trauma or intracranial hemorrhage Significant altered level of consciousness (not following commands, no purposeful movement, incomprehensible speech) No known surgery within the preceding 2 weeks No history of bleeding disorder (warfarin/coumadin and heparin are NOT contraindications) Patient must have airway secured (BIAD/ETT) 2013 MEETS CRITERIA P Pearls Must have secured airway to undergo cooling Most patients suffering from cardiac arrest with ROSC die with anoxic brain injury. Therapeutic hypothermia serves to improve the chance of a good neuro outcome. Closely monitor ventilation, target ETCO2 to 40 mmHg, do not hyperventilate If at any time there is a loss of spontaneous circulation, discontinue cooling and go to the appropriate protocol. Perform RSA to secure airway (ETT/BIAD) IF: 1) Airway not already in place AND 2) Airway placement will NOT delay transport P Administer Midazolam 1‐2 mg every 3‐5 minutes IV/ IO to a max of 10mg P Administer 30 ml/kg of cool saline (4° C) to a max of 2L Cardiac Protocol Paramedic Only Protocol ROSC P P P Apply Ice Packs to axilla, groin and neck P If Shivering ‐ Rocuronium 1 mg/kg IV/IO P P If Systolic BP<90mmHg Initiate Dopamine infusion at 5‐20mcg/kg/min, titrate to SBP >90mmHg P M Consult Medical Control if needed Service MD Approval:______ Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 60 M Cardiac Arrest: Hypothermia Therapeutic/Induced Most patients suffering from cardiac arrest with return of spontaneous circulation (ROSC) die with anoxic brain injury. Therapeutic hypothermia serves to improve the chance of a good neurologic outcome. Criteria for inclusion: Witnessed cardiac arrest with ROSC Not pregnant Age 18 years No evidence of trauma or intracranial hemorrhage Significant altered level of consciousness Not following commands No purposeful movement Incomprehensible speech No known surgery within the preceding 2 weeks No history of bleeding disorder Warfarin/Coumadin and Heparin are NOT contraindications Patient must have airway secured (BIAD/ETT) Paramedic Full ALS Assessment and Treatment 12-Lead EKG Ensure all inclusion/exclusion criteria are met. If airway not secured and it will not delay transport to the appropriate receiving facility, perform RSA, refer to Rapid Sequence Airway Protocol as needed. Assess neurological status prior to intubation, document each of the three GCS criteria. Once airway secured/sedated, expose patient and apply ice packs to axilla, groin and neck. Administer Midazolam 1-2 mg every 3-5 minutes IV/IO to a max of 10 mg. Administer 30 ml/kg of cool saline (4°C) to a max of 2 liters IV. If shivering, administer Rocuronium 1 mg/kg IV/IO. 61 If systolic blood pressure < 90 mmHg, initiate Dopamine infusion at 5-20 mcg/kg/min, titrate to SBP > 90 mmHg Closely monitor ventilation, target ETCO2 to 40 mmHg, do not hyperventilate. If at any time there is loss of spontaneous circulation, discontinue cooling and go to the appropriate protocol. Contact Medical Control for any additional orders or questions 62 Policy: Unsuccessful cardiopulmonary resuscitation (CPR) and other advanced life support (ALS) interventions may be discontinued prior to transport or arrival at the hospital when this procedure is followed: Note: When asystole is seen on the cardiac monitor, confirmation of the rhythm shall include a PRINTED rhythm strip, as well as documented interpretation of the rhythm strip in more than one lead. Low amplitude V-fib or PEA may be difficult to distinguish from asystole when using only the cardiac monitor display for interpretation. Procedure: 1) Discontinuation of CPR and ALS intervention may be implemented by a Paramedic without Medical Control consultation in a non-hypothermic adult provided all 7 criteria exist: □ Arrest is presumed to be of cardiac origin □ Initial rhythm is asystole, confirmed in two leads on a printed strip □ Terminal rhythm is asystole confirmed in two leads on a printed strip □ Secure airway confirmed by digital capnography (ETT/BIAD) □ At least four doses of Epinephrine have been administered □ Cardiac Arrest refractory to minimum of 20 minutes of ACLS □ Quantitative EtCO2 value is <10mmHg with effective CPR, after 20 minutes of ACLS 2) Field termination if the above 7 criteria aren’t met after 20 minutes of ACLS must be approved by Medical Control. 3) The paramedic has the discretion to continue resuscitation efforts if scene safety, location, patients age, time of arrest, or bystander input compels this decision. DO NOT TERMINATE RESUSCITATION IF PATIENT HAS BEEN MOVED TO THE AMBULANCE OR IF TRANSPORT HAS BEEN INITIATED. Contact Medical Control for any additional orders or questions. Basic and A-EMT need to call Medical Control for Permission to Cease Resuscitation! Service MD Approval:______ Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 63 Policy: Resuscitation can be withheld in Medical Cardiopulmonary Arrest under the following circumstances: □ Adult patient >18 years of age AND □ Pulseless, Apneic and no other signs of life present AND □ Asystole verified in two (2) leads AND □ Not exposed to an environment likely to promote hypothermia AND □ The presence of one or more of the following: *Rigor Mortis *Decomposition of body tissues *Dependent lividity OR *When the patient has a valid State of Wisconsin DNR order/bracelet/ wristband If unknown DNR status or questions regarding validity of DNR status, initiate resuscitation and contact OLMC. Service MD Approval:______ Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 64 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Medications (Aminophylline, diet pills, thyroid supplements, decongestants, Digoxin) Diet (caffeine, chocolate) Drugs (nicotine, cocaine) Past medical history History of palpitations/heart racing Signs and Symptoms Tachycardia QRS <0.12 sec Dizziness, CP, SOB Potential presenting rhythm Sinus tachycardia Atrial fibrillation/flutter Multifocal atrial tachycardia A A IV Protocol HR <150 And no symptoms Monitor and Transport HR >150, Afib on monitor Serious signs and symptoms BP <90mmHg, Altered LOC Sedation if patient condition allows and SBP >90mmHg Fentanyl 25‐50 mcg and Midazolam 1‐2 mg IV/IO/IN Titrate to max total dose of Fentanyl 200 mcg and Midazolam 4mg 12 Lead EKG No History of WPW Diltiazem 0.25 mg/kg IV over 5 minutes (max 20 mg per dose) If unsuccessful afer 10 min and SBP >100mmHg Diltiazem 0.35 mg/kg IV (max 20mg) P P History of WPW P Amiodarone 150mg IV in 100ml D5W over 10 minutes May repeat 1x if SBP >100mmHg P M Synchronized Cardioversion First Energy Level: 100 Joules If no response: 200 J If no response: 200 J (300 J if available) If no response: 200 J (360 J if available) Consult Medical Control P 2013 HR >150, Afib on monitor and SBP >90mmHg and mild symptoms P P Cardiac Protocol General Approach to all Adult Patients Differential Heart Disease (WPW, Valvular) Sick sinus syndrome Myocardial Infarction Electrolyte imbalance Exertion, pain, emotional stress Fever Hypoxia Hypovolemia or Anemia Drug effect / OD (see HX) Hyperthyroidism Pulmonary embolus P M Service MD Approval:______ After rate control/conversion 12 Lead EKG Pearls RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro Monitor for hypotension after administration of Calcium Channel Blocker or Beta Blockers Monitor for respiratory depression and hypotension associated with Midazolam Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention. Repeat Blood Pressure after Diltiazem administration. Do NOT delay treatment if patient is unstable by obtaining 12 Lead EKG unless diagnosis is in question. Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 65 Cardiac Arrhythmias: Atrial Fibrillation or Flutter All Providers General Patient Care Protocol-Adult 12 Lead EKG Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment Do not delay treatment if patient is unstable by obtaining 12-lead ECG unless diagnosis is in question Stable or borderline – Systolic BP >90 mmHg and mild symptoms (chest pain, SOB or lightheadedness) No history of WPW: Diltiazem 0.25 mg/kg IV over 5 min (Max 20 mg per dose) If unsuccessful after 10 min and SBP >100 mmHg Diltiazem 0.35 mg/kg IV (max 20mg) History of WPW Amiodarone 150 mg IV in 100 ml D5W over 10 min If unsuccessful and SBP>100 mmHg, may repeat one time Unstable (serious signs and symptoms-pulmonary edema, BP<90 mmHg systolic, altered consciousness) AND atrial fibrillation at a rate >150 beats/minute Sedation if patient condition and time allows (hold if SBP <90mmHg): Fentanyl 25-50 mcg and Midazolam 1-2 mg IV/IO Titrate to maximum total dose of Fentanyl 200 mcg and Midazolam 4 mg Synchronized Cardioversion 1st energy level: 100 Joules If no response: 200 J If no response: 200 J (300 J if available) If no response: 200 J (360 J if available) Contact Medical Control for any additional orders or questions 66 A P M Legend EMT A‐EMT Paramedic Medical Control A P M General Approach to All Adult Patients 12 Lead EKG A A IV Protocol Monitor NO YES A Transport A IV NS Bolus 250ml 2013 Hypotension ‐ SBP <90mmHg, Altered Mental Status or Chest Pain Cardiac Protocol Differential Acute Myocardial Infarction Hypoxia Pacemaker failure Hypothermia Sinus Bradycardia Athletes Head Injury (elevated ICP) or Stroke Spinal Cord Lesion Sick sinus syndrome AV Blocks (1°, 2°, 3°) Overdose Signs and Symptoms HR <60/minute with hypotension, acute altered mental stufs, chest pain, acute CHF, seizures, syncope, or shock secondary to bradycardia Chest Pain Respiratory distress Hypotension or Shock Altered mental Status Syncope History: Past medical history Medications ‐Beta Blockers ‐Calcium Channel blockers ‐Clonidine ‐Digoxin Pacemaker No Improvement Medication Overdose? P Atropine 0.5mg IVP, repeat every 3 minutes as needed (max 3.0mg/kg P No Improvement Appropriate Overdose Protocol P Dopamine 5‐20mcg/kg/min IV P External Pacing Procedure P No Improvement P Unstable Epi Infusion 2‐10mcg/min titrate to HR>60, SBP <180 (max 10mcg/min) P Unstable Continuous Monitoring Improved Pearls RECOMMENDED EXAM: Mental Status, Neck, Heart, Lungs, Neuro *Start at lowest MA’s, increase until electrical capture with pulses achieved Start rate at 70 or default and increase rate to achieve systolic BP >90mmHg (maximum 100 beats/min) Therapies are only indicated when serious signs and symptoms are present. If symptoms are mild, provide supportive care and expedite transport. In wide complex slow rhythm consider hyperkalemia Be sure to aggressively oxygenate the patient and support respiratory effort Continuous Monitoring P Sedation Protocol Transport P M Consult Medical Control P Fentanyl 25‐50mcg IV/IO (max 200 mcg) P P P Midazolam 1‐2mg IV/IO (max 4mg) M Service MD Approval:______ Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 67 P Cardiac Arrhythmias: Bradycardia All Providers General Patient Care Protocol-Adult 12 Lead EKG Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment Do not delay transport if patient is unstable by obtaining a 12 lead ECG unless diagnosis is in question Note: The following therapies are indicated only when serious signs and symptoms are present. If symptoms are mild, provide supportive care and expedite transport. Symptomatic (SBP<90mmHg, altered mental status or severe chest pain) Atropine 0.5 mg IVP, Repeat every 3 minutes as needed (Maximum dose 3mg) If symptoms persist after Atropine or any delay in establishing IV: Initiate transcutaneous pacing using demand mode Start at lowest MA’s; increase until electrical capture with pulses achieved Start rate at 70 and increase rate to achieve systolic BP >90mmHg (Maximum 100 beats/minute) Sedation if patient condition and time allows (hold if SBP<90 mmHg): Fentanyl 25-50 mcg and Midazolam 1-2 mg IV/IO Titrate to maximum total dose of Fentanyl 200 mcg and Midazolam 4 mg For hypotension (systolic BP <90 mmHg) and/or Bradycardia (HR<60) not improved by above Dopamine infusion at 5-20 mcg/kg/min titrated to maintain HR >60 and SBP >90 mmHg but SBP <180 mmHg. If above unsuccessful: 68 Epinephrine infusion at 2-10 mcg/min titrated to maintain HR>60 and SBP >90 mmHg but SBP <180mmHg. If drug induced, treat for specific drug overdose Calcium Chloride 1g IV/IO for calcium channel blocker OD Contraindicated if patient on Digoxin/Lanoxin Glucagon 3mg IV/IO for calcium channel blocker OD if no response to Calcium Chloride Glucagon 3mg IV/IO for Beta Blocker OD Naloxone (Narcan) can be given in 0.4 mg increments titrated to level of consciousness and respiratory drive If IV access has not been established, Naloxone (Narcan) 2 mg IM or via Mucosal Atomizer Device Sodium Bicarbonate 1 mEq/kg IV/IO for Tricyclic antidepressant OD Contact Medical Control for any additional orders or questions 69 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Signs and Symptoms HR >150 bpm QRS <0.12 sec (if QRS >0.12 sec, go to V‐Tach protocol If history of WPW, go to V‐Tach protocol Dizziness, CP, SOB Potential presenting rhythm Atrial/Sinus tachycardia Atrial fibrillation/flutter Multifocal atrial tachycardia Differential Heart Disease (WPW, Valvular) Sick sinus syndrome Myocardial Infarction Electrolyte imbalance Exertion, pain, emotional stress Fever Hypoxia Hypovolemia or Anemia Drug effect / OD (see HX) Hyperthyroidism Pulmonary embolus Cardiac Protocol History: Medications (Aminophylline, diet pills, thyroid supplements, Decongestants, Digoxin) Diet (caffeine, chocolate) Drugs (nicotine, cocaine) Past medical history History of palpitations/heart racing Syncope / near syncope General Approach to all Adult Patients A Stable Ventricular rate >150 Unstable Ventricular rate >150 12 Lead EKG P Adenosine Phosphate 6 mg rapid IVP over 1‐3 seconds with 20 cc NS flush (repeat with 12mg rapid IVP if no response in 2 min) May repeat x1. P Consult Medical Control M P If NO Response Sedation if patient condition allows and SBP >90mmHg Fentanyl 25‐50 mcg and Midazolam 1‐2 mg IV/IO Titrate to max total dose of Fentanyl 200 mcg and Midazolam 4mg P Diltiazem 0.25mg/kg slow IV over 5 min (max 20mg) (NOT for use with or hx of WPW) Amiodarone 150mg IV over 10 min P 2013 Vagal Maneuvers (Valsalva or Cough) M P Adenosine Phosphate 6mg rapid IVP over 1‐3 seconds with 20 cc NS flush ‐ (repeat with 12mg rapid IVP if no response in 2 min) May repeat x1. P P M A IV Protocol P Synchronized Cardioversion First Energy Level: 50 Joules If no response: 100 J If no response: 200 J If no response: 200 J (300 J if available) If no response: 200 J (360 J if available) P M P P Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro If patient has a history or 12 Lead EKG reveals Wolfe Parkinson White (WPW), NO NOT administer Calcium Channel Blocker (Diltazem) or Beta Blockers Adenosine will not terminate non SVT rhythms such as Afib or Aflutter.. Monitor for hypotension after administration of Calcium Channel Blocker or Beta Blockers Monitor for respiratory depression and hypotension associated with Midazolam Continuous pulse oximetry is required for all SVT patients Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention. Do NOT delay treatment if patient is unstable by obtaining 12 Lead EKG unless diagnosis is in question. Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 70 Cardiac Arrhythmias: Supraventricular Tachycardia All Providers General Patient Care Protocol—Adult 12 Lead EKG Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment Do not delay treatment if patient is unstable by obtaining 12-lead ECG unless diagnosis is in question Stable or borderline (Ventricular rate >150) Vagal maneuvers (Valsalva or Cough) Adenosine Phosphate (Adenocard) 6 mg rapid IVP over 1-3 seconds with 20 ml Normal Saline flush If no response in 2 minutes, Adenosine Phosphate (Adenocard) 12 mg rapid IVP over 1-3 seconds with 20 ml Normal Saline flush. If no response in 2 minutes, may repeat Adenosine Phosphate (Adenocard) 12mg rapid IVP x1. Unstable with serious signs and symptoms (Ventricular rate >150) May give brief trial of Adenosine 6mg rapid IVP over 1-3 seconds with 20 cc Normal Saline flush Sedation if patient condition and time allows (hold if SBP<90mmHg) Fentanyl 25-50 mcg and Midazolam 1-2 mg IV/IO Titrate to maximum total dose of Fentanyl 200 mcg and Midazolam 4 mg Synchronized Cardioversion First energy level: 50 Joules If no response: 100 J If no response: 200 J If no response: 200 J (300 J if available) If no response: 200J (360 J if available) Contact Medical Control for any additional orders or questions Diltiazem 0.25mg/kg slow IV over 5 min (Max 20mg) NOT FOR USE WITH OR HISTORY OF WPW Amiodarone 150mg IV over 10 min 71 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Past Medical History / medications, diet, drugs Syncope / near syncope CHF Palpitations Pacemaker Allergies: lidocaine / novacaine Signs and Symptoms Ventricular tachycardia on ECG (Runs or sustained) Conscious, rapid pulse Chest pain, shortness of breath Dizziness Rate usuaally 150‐180bpm for sustained Vtach QRS >.12 sec Differential Artifact / Device failure Cardiac Endocrine / Metabolic Drugs Pulmonary Cardiac Protocol General Approach to all Adult Patients Vfib/ Pulseless Vtach Protocol NO Palpable pulse? (Paramedics: Wide, regular rhythm with QRS >0.12sec) YES A A IV Protocol 12 Lead EKG Stable and SVT highly likely (Rate >150) P P Adenosine Phosphate 6mg rapid IVP over 1‐3 seconds with 20 cc NS flush (repeat with 12mg rapid IVP if no response in 2 min) May repeat x1. P No Response P Amiodarone 150mg in 100ml D5W IV Piggyback over 10 minutes May repeat every 15 min (Max 450mg total) P P Sedation if patient condition allows and SBP >90mmHg Fentanyl 25‐50 mcg and Midazolam 1‐2 mg IV/IO/IN Titrate to max total dose of Fentanyl 200 mcg and Midazolam 4mg 2013 Stable and unknown Wide complex or Vtach Likely (Rate >150) Unstable With serious signs and symptoms P Synchronized Cardioversion ** First Energy Level: 100 Joules If no response: 200 J If no response: 200 J (300 J if available) If no response: 200 J (360 J if available) P IF wide complex tachy reoccurs Following cardioversion M Contact Medical Control M P If hyperkalemia suspected in any wide complex tachycardia (ie. Renal failure patient) Calcium Chloride 1g IV/IO* Sodium Bicarbonate 1mEq/kg IV/IO Pearls -RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro * Calcium Chloride Contraindicated for patient on Digoxin/Lanoxin Adenosine may not be effective in identifiable atrial flutter/fibrillation, yet is not harmful. Service MD Approval:______ Monitor for hypotension after administration of Calcium Channel Blocker or Beta Blockers Monitor for respiratory depression and hypotension associated with Midazolam Continuous pulse oximetry is required for all SVT patients Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention. Do NOT delay treatment if patient is unstable by obtaining 12 Lead EKG unless diagnosis is in question. ** If delays in synchronization occur and condition is critical, go immediately to unsynchronized shocks Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 72 P Cardiac Arrhythmias: Wide‐Complex Tachycardia All Providers General Patient Care Protocol-Adult 12 Lead EKG Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment Do not delay treatment by obtaining 12-lead ECG unless diagnosis is in question In general, assume unknown wide complex tachycardia, at rates over 150 represent ventricular tachycardia Stable and unknown wide complex or ventricular tachycardia likely (rate >150) Consider Adenosine Phosphate (Adenocard) 6 mg rapid IVP over 1-3 seconds with 20 ml Normal Saline flush For atypical presentation of SVT If no response after first dose and patient still stable move to Amiodarone. Amiodarone 150 mg in 100 ml D5W IV Piggyback over 10 minutes Repeat Amiodarone 150 mg in 100ml D5W IV Piggyback over 10 minutes every 15 minutes (Maximum of 450 mg total) Unstable wide complex tachycardia (rate >150) Sedation if patient condition and time allows (hold for SBP <90 mmHg) Fentanyl 25-50 mcg and Midazolam 1-2 mg IV/IO Titrate to maximum total dose of Fentanyl 200 mcg and Midazolam 4 mg 73 Synchronized Cardioversion: 1st energy level 100 Joules If no response 200 J If no response 200 J (300 J if available) If no response 200 J (360 J if available) If delays in synchronization occur and condition is critical, go immediately to unsynchronized shocks If wide complex tachycardia reoccurs following electrical cardioversion: Amiodarone 150 mg in 100 ml D5W IV Piggyback, over 10 minutes, every 15 minutes (maximum 450 mg cumulative total dose) If hyperkalemia suspected in any wide complex tachycardia (e.g. renal failure patient) administer the following medications: Calcium Chloride 1g IV/IO Contraindicated if patient on Digoxin/Lanoxin Sodium Bicarbonate 1mEq/kg IV/IO Contact Medical Control for any additional orders or questions 74 Signs and Symptoms Ventricular tachycardia on ECG (Runs or sustained) Conscious, rapid pulse Chest pain, shortness of breath Dizziness Rate usuaally 150‐180bpm for sustained Vtach QRS >.12 sec History: Past Medical History / medications, diet, drugs Syncope / near syncope CHF Palpitations Pacemaker Allergies: lidocaine / novacaine Differential Artifact / Device failure Cardiac Endocrine / Metabolic Drugs Pulmonary Vfib/ Pulseless Vtach Protocol Palpable pulse? (Paramedics: Wide, regular rhythm with QRS >0.12sec) NO YES A IV Protocol 12 Lead EKG STABLE P P NO Response P Amiodarone 150mg in 100ml D5W IV Piggyback over 10 minutes May repeat every 15 min (Max 450mg total) A P M A‐EMT Paramedic Medical Control A UNSTABLE Sedation if patient condition allows and SBP >90mmHg Fentanyl 25‐50 mcg and Midazolam 1‐2 mg IV/IO Titrate to max total dose of Fentanyl 200 mcg and Midazolam 4mg 2013 P Magnesium Sulfate 2g slow IV in 10ml NS over 1‐2 min A P M Cardiac Protocol Legend EMT General Approach to all Adult Patients P No Response And UNSTABLE P P Synchronized Cardioversion First Energy Level: 100 Joules If no response: 200 J If no response: 200 J (300 J if available) If no response: 200 J (360 J if available) P If delays in synchronization occur and condition is critical, go immediately to unsynchronized shocks M Contact Medical Control M Pearls -RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro * Calcium Chloride Contraindicated for patient on Digoxin/Lanoxin Adenosine may not be effective in identifiable atrial flutter/fibrillation, yet is not harmful. Service MD Approval:______ Monitor for hypotension after administration of Calcium Channel Blocker or Beta Blockers Monitor for respiratory depression and hypotension associated with Midazolam Continuous pulse oximetry is required for all SVT patients Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention. Do NOT delay treatment if patient is unstable by obtaining 12 Lead EKG unless diagnosis is in question. Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 75 Cardiac Arrhythmias: Polymorphous Ventricular Tachycardia (Torsades de Pointes) All Providers General Patient Care Protocol-Adult 12 Lead EKG Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment Do not delay treatment if patient is unstable by obtaining a 12-lead ECG unless diagnosis is in question Stable Magnesium Sulfate 2 g slow IV in 10 ml NS over 1-2 minutes If no response, Amiodarone 150 mg in 100 ml D5W IV Piggyback over 10 minutes Repeat Amiodarone 150 mg in 100 ml D5W IV Piggyback over 10 minutes every 15 minutes (Maximum of 450 mg total) Unstable-or if no response to the above measures: Sedation if patient condition and time allows (hold if SBP < 90mmHg) Fentanyl 25-50 mcg and Midazolam 1-2 mg IV/IO Titrate to maximum total dose of Fentanyl 200 mcg and Midazolam 4 mg Synchronized Cardioversion: 1st energy level 100 Joules If no response 200 J If no response 200 J (300 J if available) If no response 200 J (360 J if available) If delays in synchronization occur and condition is critical, go immediately to unsynchronized shocks Contact Medical Control for any additional orders or questions 76 Legend EMT A‐EMT Paramedic A P M Medical Control A P M Signs and Symptoms CP (pain, pressure, aching, vice like tightness) Location (substernal, epigastric, arm, jaw, neck, shoulder) Radiation of pain Pale, diaphoresis Shortness of Breath Nausea, vomiting, dizziness Time of Onset Differential Trauma vs. Medical Angina vs. MI Pericarditis Pulmonary embolism Asthma / COPD Pneumothorax Aortic dissection or aneurysm GE reflux or hiatal hernia Esophogeal spasm Chest wall injury or pain Pleural pain OD (Cocaine) or Methamphetamine General Approach to All Adult Patients Obtain and Transmit 12 Lead EKG within 5 minutes of arrival Aspirin 324 mg PO A IV Protocol 250ml if hypotensive M Patient assisted Nitroglycerin 0.4mg SL, repeat every 5 minutes as needed if SBP >90mmHG and not contraindicated* M A Nitroglycerin 0.4mg SL if IV*** established, repeat every 5 minutes as needed if SBP >90mmHG and not contraindicated* A P P P Nausea or Vomiting Ondansetron (Zofran) 4 mg slow IV A STEMI ALERT Transport to PCI (Percutaneous Coronary Intervention) capable hospital University of WI Hospitals and Clinics Meriter Hospital St. Marys Hospital (not Sun Prairie ED) VA Hospital (patient preference should be taken into account) 2013 P For hypotension (<90mmHg) not improved by fluid or if fluid contraindicated – Dopamine infusion at 5‐20 mcg/kg/min titrated to maintain SBP >90mmHg Morphine Sulfate 2‐4mg slow IVP, repeat every 5 minutes as needed (max 15mg) or Fentanyl 25‐50 mcg slow IV, repeat every 5 minutes (max 200mcg)** If Runs of Vtach: Amiodarone 150 mg in 100 ml D5W IV piggyback over 10 minutes (isolated PVCs do not require treatment) IF symptoms for <12 hours, and any of the following: Paramedic interprets ST segment elevation >1mm in two or more contiguous leads Defib interpretation of “**ACUTE MI**” on EKG New Left BBB (confirmed by comparing to prior EKG) Cardiac Protocol History: Age Medications Viagra, Levitra, Cialis Past Medical History (MI, Angina, Diabetes, post menopausal) Allergies (ASA, morphine, lidocaine) Recent physical exertion Palliation/Provocation Quality (crampy, constant, sharp, dull, etc. Region/Radiation/Referred Severity (1‐10) Time (onset/duration/repitition) Notify facility EARLY P P P P Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Neck, Lung, Heart, Abdomen, Back, Extremities, Neuro *Nitro Contraindications: SBP<90, Use of a Phosphodiesterase-5 (PED5) inhibitor within last 24 hours (Viagra [Sildenafil] or Levitra [Vardenafil]) and 48 hours for Cialis (Tadalifil)- Use with caution in Acute Inferior Wall MI, or Right Ventricular infarct (ST elevation in V4R) Patient Assisted Nitro -send EKG and have OLMC determine if Nitro appropriate **Morphine contraindicated if SBP<90mmHg, use with caution in right ventricular or posterior wall MI (ST elevation in posterior leads with marked depression in V1-V4) *** If unable to establish IV, send EKG and contact OLMC for permission to proceed with Nitro Elderly patients, diabetics, and woman are more likely to experience angina (cardiac chest pain) in an atypical fashion – presenting as vague weakness, SOB, arm, back or jaw discomfort, etc. Cardiac Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 77 Chest Pain All Providers General Patient Care Protocol—Adult Obtain and transmit 12-lead ECG within 5 minutes of arrival Aspirin 324 mg PO chewed if patient is able to swallow and Aspirin is not contraindicated or taken within the last hour. Assist patient in self-administration of previously prescribed Nitroglycerin Contact Medical Control for consultation regarding 12 Lead EKG interpretation prior to assisting with patient Nitro. Contraindicated if systolic BP < 90 mmHg Contraindicated if use of a Phosphodiesterase-5 (PED5) inhibitor within last 24 hours (Viagra [Sildenafil] or Levitra [Vardenafil]) This contraindication extends to 48 hours for Cialis (Tadalifil) Repeat patient assisted Nitroglycerin administration every 5 minutes as needed for continued chest pain (provided SBP remains > 90 mmHg) with assessment of patient before and after each NTG dose See STEMI alert information below Advanced EMT IV Protocol For suspected cardiac chest pain: o Aspirin 324 mg PO chewed if patient is able to swallow and Aspirin is not contraindicated or given already o Nitroglycerin 0.4 mg SL, every 5 minutes as needed for chest pain IV access must be secured before Nitroglycerin administration (if unable, contact Medical Control) Contraindicated if systolic BP < 90 mmHg Contraindicated if use of a Phosphodiesterase-5 (PED5) inhibitor within last 24 hours (Viagra [Sildenafil] or Levitra [Vardenafil]) This contraindication extends to 48 hours for Cialis (Tadalifil) o Use with caution in Acute Inferior Wall MI, or Right Ventricular infarct (ST elevation in V4R) o Be prepared to administer IV NS boluses at 250 mL if hypotension develops 78 Paramedic Full ALS Assessment and Treatment Obtain 12-lead ECG within 5 minutes of arrival Identify the presence of ECG changes suggestive of Acute Myocardial Infarct (AMI) See STEMI Alert below Prior to transport notify receiving hospital as per STEMI Alert Criteria For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses, or when fluid boluses are contraindicated Dopamine infusion at 5-20 mcg/kg/min titrated to maintain systolic BP > 90 mmHg For suspected cardiac chest pain: o Aspirin 324 mg PO chewed if patient is able to swallow and Aspirin is not contraindicated or given already o Nitroglycerin 0.4 mg SL, every 5 minutes as needed for chest pain IV access must be secured before Nitroglycerin administration (If unable, contact Medical Control) Contraindicated if systolic BP < 90 mmHg Contraindicated if use of a Phosphodiesterase-5 (PED5) inhibitor within last 24 hours (Viagra [Sildenafil] or Levitra [Vardenafil]) This contraindication extends to 48 hours for Cialis (Tadalifil) IV access must be secured before Nitroglycerin administration (If unable, contact Medical Control) o Use with caution in Acute Inferior Wall MI, or Right Ventricular infarct (ST elevation in V4R) o Be prepared to administer IV NS boluses at 250 mL if hypotension develops o Morphine Sulfate 2-4 mg slow IVP; repeat every 5 minutes as needed (Maximum 15 mg) or Fentanyl 25-50 mcg slow IV; repeat every 5 minutes (Maximum 200 mcg) Contraindicated if systolic BP < 90 mmHg Use with caution in right ventricular or posterior wall MI (ST elevation in posterior leads with marked depression in V1-V4) Runs of Ventricular Tachycardia: Amiodarone 150 mg in 100 ml D5W IV piggyback over 10 minutes Isolated PVCs do not require treatment 79 For patients with severe nausea or vomiting: Ondansetron (Zofran) 4 mg slow IV All Providers STEMI Alert (ST Segment Elevation Myocardial Infarction) A STEMI Alert will be instituted for patients having chest pain or ischemic equivalent symptoms for < 12 hours, and any of the following Computer interpretation of “**ACUTE MI**” on 12-lead ECG (EMT Basic or Advanced) Paramedic Interprets - ST segment elevation 1mm in two or more contiguous leads Paramedic Interprets - New Left Bundle Branch Block (confirmed by comparing to prior ECG) Patients meeting STEMI Alert criteria should be transported to a PCI (Percutaneous Coronary Intervention) capable hospital PCI Capable hospitals in the Madison Area: University of Wisconsin Hospitals and Clinics Meriter Hospital St. Mary’s Hospital Madison VA Hospital Patient preference should be taken into account when determining the transport destination. Early notification/ECG transmission to the receiving facility is imperative. Activation of the STEMI Process must be documented in the Patient Care Run Sheet Contact Medical Control for any additional orders or questions 80 Assure your local Fire Department is dispatched to assist if necessary. Consult Emergency Response Guidebook (ERG) before attempting to handle any toxic chemical exposure patient Upon identifying a possible toxic exposure or overdose: Contact the Regional Poison Control Center (1‐800‐222‐1222) Upon identifying a possible hazmat exposure: Contact City of Madison HIT for chemical information via the 911 Communications Center Chemical Burns and Dermal Exposure Special Response Protocols All Providers General Patient Care Protocol—Adult Refer to the Burn Protocol Stop the burning process Remove all clothing prior to irrigation If a caustic liquid is involved, flush with copious amounts of water For chemical burns with eye involvement, immediately begin flushing the eye with normal saline and continue throughout assessment and transport If a dry chemical is involved, brush it off, then flush with copious amount of water Do not use water to flush the following chemicals: Elemental metals (sodium, potassium, lithium), and phenols Remove obvious metallic fragments from the skin Cover the burn with mineral oil or cooking oil Phenols penetrate the skin more readily when diluted with water If available, dilute with the following (listed in order of efficacy) Polyethylene glycol (PEG) Glycerol Vegetable Oil As a last resort use extremely large amounts of soap and water with continuous irrigation until all phenols are removed Apply a burn sheet or dry sterile dressing to burn areas For inhaled toxin with acute bronchospasm: Albuterol (Proventil) 2.5 mg/3 ml via nebulizer and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer Advanced EMT Consider IV Protocol Paramedic Full ALS assessment and treatment Observe for signs of impending respiratory failure; Refer to the Airway Management Protocol if needed Refer to Pain Management Protocol if needed Other possible #’s for assistance: Chemtrec: 1-800-424-9300 Chemtell: 1-888-255-3924 Infotract: 1-800-535-5053 Contact Medical Control for any additional orders or questions For persistent burning sensation of the airways (after Albuterol/ Atrovent) in the setting of Chlorine/ Chloramine exposure: 4.2 % Sodium Bicarbonate 5ml via nebulizer Mix 2.5 ml of 8.4 % Sodium Bicarbonate with 2.5 ml of 0.9 % Normal Saline for a 5 ml nebulizer 3E: 1-800-451-8346 Special Response Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 81 Hazardous Material Exposures: Basic Approach Assure that local Fire Department is responding with EMS if appropriate. Consult Emergency Response Guidebooks (ERG) before attempting to handle any toxic chemical exposure patient Upon identifying a possible toxic exposure or overdose: Contact the Regional Poison Control Center (1-800-222-1222) Upon identifying a possible hazmat exposure: Contact City of Madison HIT for chemical information via the 911 Communications Center Other possible #’s for assistance: Chemtrec: 1-800-424-9300 Chemtell: 1-888-255-3924 Infotract: 1-800-535-5053 3E: 1-800-451-8346 Chemical Burns and Dermal Exposure All Providers General Patient Care Protocol—Adult Refer to the Burn Protocol Stop the burning process Remove all clothing prior to irrigation If a caustic liquid is involved, flush with copious amounts of water For chemical burns with eye involvement, immediately begin flushing the eye with normal saline and continue throughout assessment and transport If a dry chemical is involved, brush it off, then flush with copious amount of water 82 Do not use water to flush the following chemicals: Elemental metals (sodium, potassium, lithium), and phenols Remove obvious metallic fragments from the skin Cover the burn with mineral oil or cooking oil Phenols penetrate the skin more readily when diluted with water If available, dilute with the following (listed in order of efficacy) Polyethylene glycol (PEG) Glycerol Vegetable Oil As a last resort use extremely large amounts of soap and water with continuous irrigation until all phenols are removed Apply a burn sheet or dry sterile dressing to burn areas For inhaled toxin with acute bronchospasm: Albuterol (Proventil) 2.5 mg/3 ml via nebulizer and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer Advanced EMT Consider IV Protocol Paramedic Full ALS assessment and treatment Observe for signs of impending respiratory failure; Refer to the Airway Management Protocol if needed Refer to Pain Management Protocol if needed Contact Medical Control for any additional orders or questions For persistent burning sensation of the airways (after Albuterol/Atrovent) in the setting of Chlorine/Chloramine exposure: 4.2 % Sodium Bicarbonate 5ml via nebulizer Mix 2.5 ml of 8.4 % Sodium Bicarbonate with 2.5 ml of 0.9 % Normal Saline for a 5 ml nebulizer 83 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Signs Altered mental status Seizures or coma Dyspnea/tachypnea Respiratory distress/apnea Hypertension (early) Hypotension (late) Cardiovascular collapse/Cardiac Arrest Symptoms Headache Confusion Shortness of Breath Chest Pain or tightness Nausea/Vomiting General Approach to All Patients Special Response Protocols Scene Safety – SCBA if toxic inhalation suspected Remove patient from contaminated area Administer 100% Oxygen A IV Protocol A *Administer Cyanokit® 5g IV/IO over 15 minutes P Use NaCl 0.9% as the dilutent for Cyanokit® as per manufacturer instructions P Expedite transport and treat other conditions as per appropriate protocol Service MD Approval:______ Consult Medical Control M If severe symptoms persist (patient in extremis) contact OLMC for consideration of repeat dosing M Pearls *Contraindicated in patients with known anaphylactic reactions to hydroxocobalamin or cyanocobalamin Cyanide poisoning may result form inhalation, ingestion or dermal exposure to cyanide containing compounds, including smoke form closed‐space fires. The presence and extent of the poisoning are often unknown initially. Treatment decisions must be made on the basis of clinical history and signs and symptoms of cyanide intoxication. Not all patients who have suffered smoke inhalation from a closed space fire will have cyanide poisoning. Other conditions such as burns, trauma or other toxic inhalations (ie. Carbon monoxide) may be the cause of symptoms. When smoke inhalation is the suspected source of cyanide exposure assess the patient for the following: ● Exposure to fire or smoke in an enclosed space ● Presence of soot around the mouth, nose or oropharynx ● Altered Mental Status Special Response Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 84 Hazardous Materials Exposure: Cyanide Toxicity and Smoke Inhalation Cyanide poisoning may result from inhalation, ingestion or dermal exposure to cyanide containing compounds, including smoke from closed-space fires. The presence and extent of the poisoning are often unknown initially. Treatment decisions must be made on the basis of clinical history and signs and symptoms of cyanide intoxication. Not all patients who have suffered smoke inhalation from a closed-space fire will have cyanide poisoning. Other conditions such as burns, trauma or other toxic inhalations (e.g. carbon monoxide) may be the cause of symptoms. When smoke inhalation is the suspected source of cyanide exposure assess the patient for the following: Exposure to fire or smoke in an enclosed space Presence of soot around the mouth, nose or oropharynx Altered mental status Common Signs and Symptoms of Cyanide Toxicity Symptoms Signs Headache Confusion Shortness of breath Chest Pain or tightness Nausea/Vomiting Altered mental status Seizures or coma Dyspnea/tachypnea Respiratory distress/apnea Hypertension (early) Hypotension (late) Cardiovascular collapse/cardiac arrest All Providers General Patient Care Protocol—Adult Supplemental 100% Oxygen Advanced EMT Consider IV Protocol Paramedic Perform Full ALS Assessment and Treatment When clinical suspicion of Cyanide poisoning is high Administer Cyanokit 5 g IV/IO over 15 minutes 85 Use NaCl 0.9% as the diluent for Cyanokit as per manufacturer instructions Contraindicated in patients with known anaphylactic reactions to hydroxocobalamin or cyanocobalamin Expedite transport and treat other conditions as per appropriate protocol Contact Medical Control for any additional orders or questions If severe symptoms persist (patient in extremis) contact OLMC for consideration of repeat dosing of Cyanokit 86 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Differential Nerve agent exposure (ie. VX, Sarin, Soman, etc.) Organophosphate exposure (pesticide) Vesicant exposure (ie. Mustard gas) Respiratory irritant exposure (ie. Hydrogen sulfide, ammonia, chlorine, etc.) History: Exposure to chemical, biologic, radiologic or nuclear hazard Potential exposure to unknown substance/hazard M M Alert Medical Control Immediatly Signs and Symptoms Visual Disturbances Headache Nausea/vomiting Salivation Lacrimation Respiratory distress Diaphoresis Seizure activity Respiratory arrest Special Response Protocol Ensure Scene Safety and SCBA if toxic inhalation suspected General Approach to All Patients Obtain history of exposure Observe for specific toxidromes Initiate triage and/or decon as indicated Assess Symptoms MAJOR* Must show symptoms before treatment MINOR* A A IV Protocol Adult P Atropine 2mg IV/IO/IM every 5min until symptoms resolve Pediatric Adult **MARK 1 kit x3 immediately Repeat Atropine 2mg IV/IO/IM every 5 min Until symptoms resolve P Atropine 0.02mg‐0.05mg/kg IV/IO/IM every 5min until symptoms resolve Lorazepam 1‐2mg IV/IO/IM or Diazepam Auto Injector 10mg IM P Monitor and Reassess M Re‐ Contact Medical Control Pediatrics <7 – 1 MARK 1 kit 8‐14 – 2 MARK 1 kits >15 – 3 MARK 1 kits Repeat Atropine 0.02mg‐0.05mg/kg IV/IO/IM every 5 min until symptoms resolve M P Lorazepam 0.1mg IV/IO/IM Service MD Approval:______ Pearls * Minor: salivation, lacrimation, visual disturbances Major: altered mental status, seizure, respiratory distress, respiratory arrest ** MARK 1 and DuoDote kits carried on response vehicles are for Responders ONLY. There use referenced above implies that the WMD stockpile has been released and delivered to the scene. Trained EMT Basic and Advanced may also assist with Mark 1 IM injections Follow local HAZMAT protocols for decon and use of PPE For patients with major symptoms, there is no limit for atropine dosing The main symptom that the atropine addresses is excessive secretions so atropine should be given until salivation improves. Special Response Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 87 Hazardous Materials Exposure: Nerve Agent/WMD SIMULTANEOUSLY ALERT OLMC All Providers General Patient Care Protocol—Adult Ensure Scene safety and proper PPE Obtain history of exposure, observe for toxidromes Initiate triage/Decontamination Consider need for additional resources Mark 1 Kit/DuoDote as below Mark 1 and DuoDote Kits carried on response vehicles are for Responders ONLY. There use referenced below implies that the WMD stockpile has been released and delivered to the scene Paramedic Full ALS Assessment and Treatment Assess symptoms Minor symptoms: salivation, lacrimation, visual disturbances Adults Atropine 2 mg IV/IO/IM every 5 minutes until symptoms resolve Pediatrics Atropine 0.02-0.05 mg/kg every 5 minutes until symptoms resolve Major symptoms: altered mental status, seizures, respiratory distress, respiratory arrest Adults MARK 1 Kit X 3 IM IMMEDIATELY o Repeat Atropine 2 mg IV/IO/IM every 5 minutes until symptoms resolve Lorazepam 1-2 mg IV/IO/IM or Diazepam Auto-injector 10mg IM Pediatrics ≤ 7 years old 1 MARK 1 Kit 8-14 years old, 2 MARK 1 kits ≥ 15 years old 3 MARK 1 Kits o Repeat Atropine 0.02-0.05 mg/kg IV/IO every 5 minutes until symptoms resolve Lorazepam 0.1mg/kg IM/IV/IO Contact Medical Control for any additional orders or questions 88 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Documented Hypertension Related diseases: diabetes, CVA, renal failure, cardiac Medications (compliance ?) Erectile dysfunction medication Pregnancy Signs and Symptoms One of these Systolic BP 200 or greater Diastolic BP 110 or greater And at least one of these Headache Nosebleed Blurred vision Dizziness Differential Hypertensive encephalopathy Primary CNS injury (Cushings response = bradycardia with hypertension) Myocardial Infarction Aortic dissection (aneurysm) Pre‐eclampsia/Eclampsia Medical Protocol General Approach to All Adult Patients Check BP in both arms If Respiratory Distress Consider Adult Dyspnea Protocol 2013 Consider Chest Pain Protocol 12 Lead EKG If Altered Mental Status, Stroke, Pulmonary Edema, Chest Pain or Elevated Blood Pressure Refer to Specific Protocol A M IV Protocol Consult Medical Control if needed A M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs Abdomen, Back, Extremities, Neuro Never treat elevated blood pressure based on one set of vital signs Symptomatic hypertension is typically revealed through end organ damage to the cardiac, CNS, or renal systems All symptomatic patients with hypertension should be transported with their head elevated. Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 89 Hypertensive Emergencies Focus on addressing the manifestations of hypertensive emergencies, such as chest pain or heart failure. Prehospital treatment of isolated hypertension may result in critical reductions in target organ perfusion due to uncontrolled lowering of blood pressure. All Providers General Patient Care Protocol—Adult Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment Symptomatic: Chest Pain present, refer to the specific protocol For patients with altered mental status, signs of stroke or pulmonary edema, who are found to have elevated blood pressure, refer to the specific protocol Asymptomatic: Provide supportive care Contact Medical Control for any additional orders or questions 90 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Age Exposure to increased temperatures and/or humidity Past medical history / medication Extreme exertion Time and length of exposure Poor PO intake Fatigue and/or muscle cramping Differential Fever (Infection) Dehydration Medications Hyperthyroidism (Storm) Delirium tremens (DT’s) Heat cramps Heat Exhaustion Heat stroke CNS lesions or trauma Signs and Symptoms Altered mental status or unconsciousness Hot, dry or sweaty skin Hypotension or shock Seizures Nausea Move patient to cooler enviroment HEAT EXHAUSTION HEAT CRAMPS Dizziness, lightheaded, headache, irritability, normal or decreased LOC, normal or decreased BP, tachycardia, normal or elevated temperature Painful spasms of the extremities or abdominal muscles, normal mental status and vitals) Keep patient supine 100% oxygen Remove clothing Sponge with cool water and fan Oral fluids Sponge with cool water A Overdose Protocol IV PROTOCOL A HEAT STROKE Marked alteration in LOC, extremely high temperature (often >104°F)may be sweating or have red/hot/dry skin Semi‐reclining with head elevated 15‐30° 100% oxygen Rapid cooling (prevent shivering as it increases temperature) Cold packs, sponge with cool water, fan A YES Cocaine or sympathomimetic toxicity suspected? Medical Protocol General Approach to All Adult Patients IV PROTOCOL A Transport NO M Contact Medical Control M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Heart, Lungs, Neuro Extremes of age are more prone to heat emergencies (ie. Young and old) Predisposed by use of: tricyclic antidepressants, phenothiazine, anticholinergic medications, and alcohol. Cocaine, Amphetamines, and Salicylates may elevate body temperatures. Sweating generally disappears as body temperature rises above 104°F (40°C) Intense shivering may occur as patient is cooled. Heat Cramps consists of benign muscle cramping 2° to dehydration and is not associated with an elevated temperature Heat Exhaustion consists of dehydration, salt depletion, dizziness, fever, mental status changes, headache, cramping, nausea, and vomiting. Vital signs usually consist of tachycardia, hypotension, and an elevated temperature Heat Stroke consists of dehydration, tachycardia, hypotension, temperature >104°F (40°C), and an altered mental status Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 91 Hyperthermia All Providers General Patient Care Protocol—Adult Move patient to cooler environment Heat Cramps (Painful spasms of the extremities or abdominal muscles, normal mental status and vital signs) Oral fluids as tolerated Sponge with cool water Heat Exhaustion (Dizziness, light-headedness, headache, irritability, normal or slightly decreased LOC, normal or decreased BP [hypovolemia], tachycardia, normal or slightly elevated temperature) Keep patient supine Supplemental 100% oxygen Remove clothing Sponge with cool water and fan Heat Stroke (Marked alteration in LOC, extremely high temperature [often > 104] may be sweating or have red/hot/dry skin) Semi-reclining with head elevated 15-30 Supplemental 100% oxygen Rapid cooling (prevent shivering as it increases body temperature) Cold packs, sponge with cool water, fan Advanced EMT Consider IV Protocol Paramedic If symptoms are moderate to severe, perform Full ALS Assessment and Treatment Hyperthermia may result from cocaine or sympathomimetic toxicity If cocaine/sympathomimetic toxicity strongly suspected, refer to the Cocaine/Sympathomimetic Protocol Expedite Transport Contact Medical Control for any additional orders or questions 92 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Past medical history Medications Exposure to environment even in normal temperatures Exposure to extreme cold Extremes of age Drug use: alcohol, barbituates Infections / sepsis Length of exposure/ wetness Signs and Symptoms Cold, clammy Shivering Mental status changes Extremity pain or sensory abnormality Bradycardia Hypotension or shock Differential Sepsis Environmental exposure Hypoglycemia CNS dysfunction Stroke Head Injury Spinal Cord Injury Medical Protocol General Approach to All Adult Patients Remove Wet Clothing Measure Temperature <95°F (35°C) Handle Gently Apply Warm blankets/hotpacks A IV PROTOCOL Warm fluid if available max 2L >95°F (35°C) Appropriate Protocol Based on patient symptoms A M Contact Medical Control M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Heart, Lungs, Neuro If cardiac arrest occurs with core temp >88°F: refer to appropriate protocol, prolong interval between drugs to 5 minutes, if defibrillation is necessary, limit to one shock, continue CPR If cardiac arrest occurs with core temp <88°F contact Medical Control NO PATIENT IS DEAD UNTIL WARM AND DEAD Extremes of age are more susceptible (young and old) With temperatures less than 30°C (86°F) ventricular fibrillation is a common cause of death. Handling patients gently may prevent this from occuring. If the temperature is unable to be measured, treat the patient based on the suspected temperature Hypothermia may produce severe bradycardia so take at least 45 seconds to palpate a pulse Hot packs can be activated and placed in the armpit and groin area if available. Care should be taken not to place the packs directly against the patients skin. Consider withholding CPR if patient has organized rhythm or has other signs of life. Discuss with medical control Intubation can cause ventricular fibrillation so it should be done gently by the most experienced person. Do not hyperventilate the patient as this can cause ventricular fibrillation Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 93 Hypothermia All Providers General Patient Care Protocol—Adult Remove wet clothing Measure temperature, If < 95F (35C), handle gently Warm blankets/warm temperature Advanced EMT Consider IV Protocol If available, and no contraindications, administer warmed 0.9% Normal saline (max 2L) Paramedic Full ALS Assessment and Treatment If available, and no contraindications, administer warmed 0.9% Normal saline (max 2L) If Cardiac Arrest occurs with a temp > 88F Refer to appropriate protocol Prolong interval between drugs to 5 minutes If defibrillation is necessary, limit to one shock Continue CPR If cardiac arrest with temp < 88F Contact OLMC Contact Medical Control for any additional orders or questions 94 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Advanced EMT/Paramedic Assess need for IV to administer IV Fluids, Medications in emergent or potentially emergent conditions Place catheter per procedure manual When possible utilize 20g or larger on medical patients and 16 gauge or larger in trauma or hypovolemic shock patients. If peripheral IV attempts are unsuccessful, reconsider need for IV access. If life threatening situation place intraosseous line General Protocols Peripheral IV is the access of choice, lower extremity peripheral IV should rarely be utilized Once access obtained, monitor infusion site, unless administering fluid boluses, either saline lock the catheter or place at TKO rate. Consider intraosseous access for any life-threatening event Paramedic If extremity IV attempts are unsuccessful, reconsider need for IV access. If patient hypotensive, but alert and responsive to pain – consider external jugular vein IV access. ● If patient unstable, go directly to Intraosseous access. General Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 95 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Past medical history Hypertension meds Prenatal care Prior pregnancies / births Gravida / Para Differential Pre‐eclampsia / Eclampsia Placental Previa Placenta abruption Spontaneous abortion Signs and Symptoms Seizures Hypertension Severe headache Visual changes Edema of hands and face Blood Glucose Measurement <70 >70 A IV Protocol Oral Glucose 15g* or Glucagon 1mg IM A IV Protocol A P If Seizure activity or SBP >160mmHg on two readings Magnesium Sulfate 4g in 100ml D5W IV over 10 minutes P if Glucose <70 Dextrose 12.5g‐25g slow IVP or D10W 100mL A 2013 Continued Seizure P Lorazepam 1‐2mg, slow IV/IO Or Midazolam 5mg IV/IO/IM/IN (Max dose Lorazepam 4.0mg, Midazolam 10.0mg) P Seizure not controlled by above OR Seizure reoccurs P Lorazepam 1‐2mg, slow IV/IO Or Midazolam 5mg IV/IO/IM/IN (Max dose Lorazepam 4.0mg, Midazolam 10.0mg) Pediatric and OB Protocols General Approach to all Adult Patients P Pearls RECOMMENDED EXAM(of mother): Mental Status, Heart, Lungs, Abdomen, Neuro * If alert enough to self administer Glutose Pregnancy induced hypertension, pre‐eclampsia and eclampsia are conditions typically encountered in late 2nd or 3rd trimester pregnancy, and less commonly in the postpartum period. Clinical manifestations may include elevated blood pressure (SBP>160mmHg), headache, confusion or agitation.. Service MD Approval:______ OB Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 96 Obstetrics / Gynecology Perinatal Emergencies Pregnancy-induced hypertension, pre-eclampsia and eclampsia are conditions typically encountered in late 2nd or 3rd trimester pregnancy, and less commonly in the postpartum period. Clinical manifestations may include elevated blood pressure (SBP > 160 mmHg), headache, confusion or agitation. All Providers General Patient Care Protocol-Adult Blood Glucose measurement If hypoglycemic (Blood glucose < 70mg/dL) Glucose paste 15 g or other oral glucose agent (e.g. orange juice) if patient alert enough to self-administer If hypoglycemic and unable to take oral glucose: Consider Glucagon 1mg IM Advanced EMT Consider IV Protocol Blood Glucose measurement If < 70 mg/dL administer Dextrose 12.5g-25g slow IVP or D10W 100mL Paramedic Full ALS Assessment and Treatment Blood Glucose measurement If < 70 mg/dL administer Dextrose 12.5g-25g slow IVP or D10W 100mL Administer Magnesium Sulfate 4 g in 100 ml D5W IV over 10 minutes for either of the following: Systolic BP > 160 mm Hg on two readings Seizure activity For active seizures, in addition to Magnesium Sulfate choose one of the following options: Lorazepam (Ativan) 1-2 mg, slow IV/IO -OR Midazolam (Versed) 5 mg IV/IO/IM/IN 97 For seizure not controlled by the above, or if seizure reoccurs after initial control, choose one of the following: Lorazepam (Ativan) 1-2 mg, slow IV/IO -OR Midazolam (Versed) 5 mg IV/IO/IM/IN Max dose of Lorazepam is 4 mg and Max dose of Midazolam is 10 mg Contact Medical Control for any additional orders or questions 98 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Past medical history Hypertension meds Prenatal care Prior pregnancies / births Gravida / Para Differential Pre‐eclampsia / Eclampsia Placental Previa Placenta abruption Spontaneous abortion Signs and Symptoms Vaginal Bleeding Abdominal pain Pediatric and OB Protocols General Approach to all Adult Patients Trimester in Pregnancy? 1st or 2nd Trimester or UNKNOWN 3rd Trimester Position of Comfort Left lateral recumbant position Left lateral recumbant position if hypotensive Blood Pressure Blood Pressure <90mmHg <90mmHg A A >90mmHg Normal Saline Bolus 250 ml until BP >90mmHg A >90mmHg Transport to hospital Complaint of Labor? Does not need to be a OB receiving facility NO 2013 A Normal Saline Bolus 250 ml until BP >90mmHg X4 (max 2L) YES Childbirth Protocol Transport to hospital OB receiving facility* M Contact Medical Control M Service MD Approval:______ Pearls RECOMMENDED EXAM(of mother): Mental Status, Heart, Lungs, Abdomen, Neuro * Imminent deliver or medically unstable mother: Transport to nearest ED (not nearest OB receiving facility) Non‐traumatic abdominal, pelvic or back complaints, vaginal bleeding, spotting or any vaginal fluid leak or discharge: Transport to closest OB receiving facility. Whenever possible, transport to patient’s requested OB receiving facility (ie. High risk pregnancy with pre‐selected OB destination) if patient not having imminent delivery. OB Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 99 Vaginal Bleeding All Providers 1st or 2nd trimester or unknown pregnancy status Position of comfort, consider lateral recumbent position if hypotensive 3rd Trimester Bleeding (>26 weeks) Lateral recumbent position Do not place finger or hand inside birth canal during assessment If gestational age known to be < 20 weeks, transport to closest hospital If gestational age known or possibly ≥ 20 weeks, transport to nearest OB receiving facility Advanced EMT Consider IV Protocol If BP<90 mmHg systolic, administer boluses of 0.9%NaCl at 250 ml until systolic BP>90 mmHg Paramedic If bleeding moderate or heavy, perform Full ALS Assessment and Treatment Contact Medical Control for any additional orders or questions 100 Obstetrical Transport Destination Patient known to be < 20 weeks gestation 1st day of last menstrual period < 20 weeks ago Available information verifying gestational age < 20 weeks (e.g., known due date) Refer to Medical Transport Destination for more information Does not have to be an OB receiving facility Patient known or possibly ≥ 20 weeks gestation Imminent delivery or medically unstable mother: Transport to nearest ED (not nearest OB receiving facility) Non-traumatic abdominal, pelvic or back complaints, vaginal bleeding, spotting or any vaginal fluid leak or discharge: Transport to closest appropriate obstetric receiving facility Contact appropriate obstetric facility ED for radio report and any additional direction/assistance Whenever possible, transport to patient’s requested obstetric receiving facility (e.g. high risk pregnancy with pre-selected obstetrical destination) if patient not having imminent delivery Contact Medical Control for any additional orders or questions 101 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Signs and Symptoms Spasmodic pain Vaginal discharge or bleeding Crowning or urge to push Meconium Differential Abnormal presentation Buttock Foot Hand Prolapsed cord Placenta previa Abruptio placenta Pediatric and OB Protocols History: Due Date Time contractions started /how often Rupture of membranes Time / amount of any vaginal bleeding Sensation of fetal activity Past medical and delivery history Medications Gravida / Para Status High Risk Pregnancy General Approach to all Adult Patients Supplemental Oxygen Inspect perineum (No digital vaginal exam) Presenting part NOT the head Crowning Activate ALS Meconium present Refer to OB Procedures Newborn Resuscitation protocol M Contact Medical Control Double clamp cord 10‐12 inches from abdomen Cut cord between clamps maintain body temperature ** Begin Transport to nearest OB receiving facility M Pearls RECOMMENDED EXAM(of mother): Mental Status, Heart, Lungs, Abdomen, Neuro Document all times (delivery, contraction frequency, and length) If maternal seizures occur, refer to the Obstetrical Emergencies protocol **Allow spontaneous delivery of the placenta; do not apply traction to umbilical cord for placental delivery. If placental delivery occurs, package in biohazardous waste bag and hand over to hospital staff upon arrival Gently massage abdominal wall overlying the uterine fundus until firm. Some perineal bleeding is normal with any childbirth. Large quantities of blood or free bleeding are abnormal. Record APGAR at 1 minute and 5 minutes after birth. Service MD Approval:______ OB Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 102 2013 Delivery: ‐Slow, controlled delivery of head; apply gentle perineal pressure ‐Observe for meconium staining ‐If present, suction oral pharynx and nose as Begin Transport immediately to nearest OB receiving facility Obstetrics / Gynecology: Childbirth All Providers General Patient Care Protocol-Adult Supplemental oxygen Do not place fingers or hand inside the birth canal for assessment If presenting part is not the head (i.e., foot-, arm-, or buttock-first), immediately begin transport to the nearest OB receiving facility while further care continues Delivery Slow, controlled delivery of head; apply gentle perineal pressure Observe for meconium staining If present, suction oral pharynx and nose as soon as head is delivered Following delivery, follow newborn resuscitation protocol Double clamp cord 10-12 inches from abdomen Cut cord between clamps Maintain body temperature Allow spontaneous delivery of placenta; do not apply traction to umbilical cord for placental delivery If placental delivery occurs, package in biohazardous waste bag and hand over to hospital staff upon arrival Postpartum For neonate, see Newborn Resuscitation Protocol Assess for postpartum hemorrhage Gently massage abdominal wall overlying the uterine fundus until firm Transport to nearest OB receiving facility See newborn resuscitation for care of the neonate Contact Medical Control for any additional orders or questions 103 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Ingestion or suspected ingestion of a potentially toxic substance Substance ingested, route, quantity Time of ingestion Reason (suicidal, accidental, criminal) Available medications in home Post medical history, medications Signs and Symptoms Mental Status Changes Hypotension / Hypertension Decreased respiratory rate Tachycardia, dysrhythmias Seizures Nothing by Mouth 12 Lead EKG A IV Protocol A M Consult Medical Control if needed 2013 Refer to specific protocol once agent has been identified or is strongly suspected Medical Protocol General Approach to All Adult Patients Differential Tricyclic antidepressants (TCAs) Acetaminophen (Tylenol) Aspirin Depressants Stimulants Anticholinergic Cardiac medications Solvents, alcohols, cleaning agents Insecticides (organophosphates) M Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Heart, Lungs, Abdomen, Extremities, Neuro * for Intranasal administration A-EMT should administer 0.5mg per nare, total of 1mg and then proceed with additional doses as needed Do not rely on patient history of ingestion, especially in suicide attempts. Make sure patient is still not carrying other medications or any weapons Bring bottles, contents, and emesis to ED Tricyclic : 4 major areas of toxicity: seizures, dysrhythmias, hypotension, decreased mental status or coma; rapid progression from alert to death Acetaminophen: initially normal or nausea/vomiting. If not detected and treated, causes irreversible liver failure Aspirin: Early signs consist of abdominal pain and vomiting. Tachypnea and altered mental status may occur later. Renal dysfunction, liver failure and/or cerebral edema among other things can take place later Depressants: decreased HR, decreased BP, decreased temperature, decreased respirations, non‐specific pupils Stimulants: Increased HR, increased BP, increased temperature, dilated pupils, seizures Anticholinergic: increased HR, increased temperature, dilated pupils, mental status changes Cardiac Medications: dysrhythmias and metal status changes Solvents: nausea, coughing, vomiting, and mental status changes Service MD Approval:______ Insecticides: increased or decreased HR, increased secretions, nausea, vomiting, diarrhea, pinpoint pupils Consider restraints if necessary for patient's and or personnel’s protection per the restraint procedure Consider contacting poison control center for advice 1-800-222-1222 Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 104 Overdose and Poisonings: General Approach For any overdose or poisoning, contact should be made with the Regional Poison Control Center (RPCC) 1-800-222-1222. Whenever possible, determine the agent(s) involved, the time of the ingestion/exposure, and the amount ingested. Bring empty pill bottles, etc. to the receiving facility. All Providers General Patient Care Protocol-Adults Nothing by mouth 12 Lead EKG Advanced EMT Consider IV Protocol Paramedic Refer to the specific protocol when an agent has been identified or is strongly suspected Contact Medical Control for any additional orders or questions 105 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Tricyclic &Tetracyclic Antidepressant Advanced EMT Consider IV Protocol M Category Tricyclic Antidepressants Other Cyclic Antidepressants Selective Serotonin Reuptake Inhibitors (SSRIs) Consult Medical Control if needed M Drugs ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● ● Overdose Effects Amitriptyline (Elavil, Endep, Vanatrip, Levate) Clomipramine (Anafranil) Doxepin (Sinequan, Zonalon, Tridapin) Imipramine (Tofranil, Impril) Nortryptyline (Aventyl, Pamelor, Norventyl) Desipramine (Norpramin) Protriptyline (Vivactil) Trimipraine (Surmontil) Amitriptyline+Chlordiazepoxide (Limbitrol) Maprotiline (Iudiomil) Amoxapine (Asendin) Buproprion (Wellbutrin) Trazadone (Desyrel, Trazorel) Citalopram (Celexa) Fluoxetine (Prozac) Fluvoxamine (Luvox) Paroxetine (paxil) Sertraline (Zoloft) ● Hypotension ● Anti-cholinergic effects(tachycardia, seizures, altered mental status, mydriasis) ● AV conduction blocks (prolonged QT interval, wide QRS) ● VT and VF ● Similar to tricyclics ● Seizures ● Hypertension, tachycardia, agitation, diaphoresis, shivering, ● Malignant Hperthermia Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 106 2013 Full ALS Assessment and Treatment For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses, or when fluid resuscitation is contraindicated: Dopamine infusion at 5-20 mcg/kg/min titrated to maintain systolic BP > 90 mmHg If wide QRS complex (≥ 0.10 sec), hypotension, or any arrhythmias: Sodium Bicarbonate 1 mEq/kg IV/IO Repeat Sodium Bicarbonate 1 mEq/kg IV/IO in 5-10 minutes If any of the following conditions occur, refer to the appropriate protocol: Polymorphous Ventricular Tachycardia Altered Mental Status Seizures Medical Protocol Paramedic A P M Legend EMT A‐EMT Paramedic Medical Control Cholinergic Poisoning / Organophosphates A P M All Providers General Patient Care Protocol-Adult Toxicity to ambulance crew may result from inhalation or topical exposure Supplemental 100% oxygen Decontaminate patient Remove all clothing and contain run-off of toxic chemicals when flushing Advanced EMT Medical Protocol Wear protective clothing including masks, gloves and eye protection Consider IV Protocol 2013 Paramedic Full ALS Assessment and Treatment For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses, or when fluid resuscitation is contraindicated Dopamine infusion at 5-20 mcg/kg/min titrated to maintain systolic BP > 90 mmHg If severe signs of toxicity, (severe respiratory distress, bradycardia, heavy respiratory secretions) do not rely on pupil constriction to diagnose or titrate medications: Atropine 2 mg IVP every 5 minutes, titrate dosing by assessing improvement in respiratory effort/bronchial secretions Consider Mark 1 Kit, see Nerve Agent protocol If any of the following conditions occur, refer to the appropriate protocol: Altered Mental Status Seizures M Consult Medical Control if needed M Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 107 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Antipsychotics / Acute Dystonic Reaction Medical Protocol Haloperidol Prolixin Thorazine Prochlorperazine (Compazine) Promethazine (Phenergan) Advanced EMT Consider IV protocol 2013 Paramedic Full ALS Assessment and Treatment For Dystonic reactions, administer Diphenhydramine (Benadryl) 25 mg IV Repeat Diphenhydramine 25 mg IV if inadequate response in 10 minutes M Consult Medical Control if needed M Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 108 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Beta Blocker Toxicity ● ● ● ● ● ● ● Single Agent Medication Proprandolol (Inderal) Atenolol (Tenormin) Metroprolol (Lopressor, Toprol) Nadolol (Corgard) Timolol (Blocadren) Labetolol (Trandate) Esmolol (Brevibloc) ● ● ● ● ● ● Medical Protocol Examples of commonly used Beta Blocker medications: Combination Medication Corzide (Nadolol/bendroflumethlazide) Inderide (Propranolol/HCTZ) Lopressor HCT (Metoprolol/HCTZ) Tenoretic (Atenolol/Chlorthalidone) Timolide (Timolo/HCTZ) Ziac (Bisoprolol/HCTZ) 2013 Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment For all patients with cardiovascular toxicity, defined by: Chest Pain, SBP < 90 mmHg or altered mental status, AND Heart Rate < 60 or 2nd or 3rd degree heart blocks Administer the following agents: Atropine 0.5 mg IV/IO, may repeat X 2 use with caution in the setting of 2º or 3º heart block If no response, Glucagon 3 mg IV/IO If vomiting after Glucagon, administer Ondansetron (Zofran) 4 mg IV If no response, begin Transcutaneous Pacing M Consult Medical Control if needed M Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 109 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Calcium Channel Blockers Examples of commonly used Calcium Channel Blocker medication: Medical Protocol Amlodipine (Norvasc) Felodipine (Plendil, Renedil) Isradipine (DynaCirc) Nicardipine (Cardene) Nifedipine (Procardia, Adalat) Verapamil (Calan) Diltiazem (Cardizem) Advanced EMT Consider IV Protocol 2013 Paramedic Full ALS Assessment and Treatment For all patients with cardiovascular toxicity, defined by: Chest Pain, SBP < 90 mmHg or altered mental status, AND Heart Rate < 60 or 2nd or 3rd degree heart blocks Administer the following agents Atropine 0.5 mg IV/IO, may repeat X 2 use with caution in the setting of 2º or 3º heart block If no response, administer Calcium Chloride 1 g IV/IO Contraindicated if patient taking Digoxin (Lanoxin) If no response, may repeat Calcium Chloride 1 g IV/IO no response, begin Transcutaneous Pacing M Consult Medical Control if needed M Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 110 History: Known or suspected CO exposure Suspected source/duration exposure Age Known or possible pregnancy Reason (accidental, suicidal) Measured atmospheric levels Past medical history, medications Signs and Symptoms Altered mental status / dizziness Headache, Nausea/Vomiting Chest Pain/Respiratory distress Neurological impairments Vision problems/reddened eyes Tachycardia/tachypnea Arrhythmias, seizures, coma Differential Effects of other toxic fire by product Acute cardiac event Acute neurological event Flu/GI illness Acute intoxication Diabetic Ketoacidosis Headache or non‐toxic origin General Approach to All Adult Patients Scene Safety – SCBA if toxic inhalation suspected A P M Remove patient from contaminated area Administer 100% Oxygen COHb% (SpCO) Measurement Available? SpCO<5% Paramedic Medical Control A P M Appropriate Protocol based on symptoms Not available SpCO>5% No treatment for CO required Appropriate Protocol based on symptoms A‐EMT SpCO >5% SpCO <15% SpO2 >90% Symptoms of CO and/or hypoxia? Special Response Protocols Legend EMT SpCO >15% SpO2 <90% 100% Oxygen via NRB Transport to ED YES NO Service MD Approval:______ If cardiac/ respiratory/ neurological symptoms are also present, go to appropriate protocol No treatment for CO required* Recommend evaluation of home/ work environment for presence of CO M Consult Medical Control M Pearls *Fetal hemoglobin has a greater attraction for CO than maternal hemoglobin. Females who are known to be pregnant or who could be pregnant should be advised that EMS-measured SpCO levels reflect the adults level and that fetal COHb levels may be higher. Recommend Hospital evaluation for any CO exposed pregnant person. The absence (or low detected levels of) COHb in not a reliable predictor of firefighter or victim exposure to other toxic byproducts of fire – also consider Cyanide Poisoning Protocol Attempt to evaluate other correctable causes when possible Special Response Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 111 Overdose and Poisonings: Carbon Monoxide All Providers General Patient Care Protocol—Adult Wear appropriate PPE (SCBA) as indicated Remove the patient from the contaminated source Supplemental 100% oxygen, document time oxygen started If CO monitoring available Document initial CO level Follow Carboxyhemoglobin SpCo Monitoring Procedure Paramedic Full ALS Assessment and Treatment For smoke inhalation patients also consider Cyanide poisoning (See Hazardous Materials—Basic Approach Protocol) Contact Medical Control for any additional orders or questions 112 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Cocaine and Sympathomimetic All Providers Medical Protocol General Patient Care Protocol—Adult Advanced EMT Consider IV Protocol Paramedic M Consult Medical Control if needed 2013 Full ALS Assessment and Treatment For patients with Sympathomimetic toxidrome (e.g. hypertension, tachycardia, agitation): Lorazepam (Ativan) 1-2 mg, slow IV If no IV access, Midazolam (Versed) 5 mg IM/IN if < 60 years old 2.5 mg IM/IN if > 60 years old Repeat either medication once in 5-10 minutes if signs and symptoms continue If seizures occur, refer to Seizure Protocol Refer to Behavioral Emergency Protocol M Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 113 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Opiates All Providers Advanced EMT M Consult Medical Control if needed 2013 ● Consider IV Protocol For patients with opiate toxidrome (ie. Coma, pinpoint pupils, respiratory depression) □ Naloxone (Narcan) 2 mg IV/IO every 3 minutes Naloxone (Narcan) can be administered in 0.4 mg increments titrated to respiratory drive and level of consciousness If IV access has not been established, Naloxone (Narcan) 2 mg IM or Advanced EMT ‐ 0.5 mg per nare IN (total 1.0mg per administration), Paramedics - 1.0 mg per nare (total 2.0mg per administration) □ Repeat every 3 minutes if signs and symptoms continue (max 8.0mg) If respiratory depression not improved, refer to Airway protocol Medical Protocol General Patient Care Protocol—Adult Airway Protocol for respiratory depression M Overdose and Poisoning: Opiates Single Agent Medication ● Oxycodone ● Hydrocodone ● Morphien ● Heroin ● Dilaudid ● Fentanyl ● Codeine Combination Medication ● Vicodin ● Norcodin ● Percocet ● Darvocet ● Vicoprofen Long Acting* ● Oxycontin ● MS Contin ● Methadone * May Need Repeat Dosing Service MD Approval:______ Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 114 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Age Location Duration Severity (1‐10) Past medical history Medications Drug Allergies Differential Per the specific protocol Musculoskeletal Visceral (abdominal) Cardiac Pleural / Respiratory Neurogenic Renal (colic) Signs and Symptoms Severity (pain scale) Quality (sharp, dull, etc) Radiation Relation to movement, respiration Increased with palpation Medical Protocol General Approach to All Adult Patients Patient care according to PROTOCOL Based on specific complaint Pain Severity >6 out of 10 A P A IV Protocol Morphine Sulfate 2‐5mg slow IVP every 5 min until relief achieved (max 15mg)* OR Fentanyl 50‐75mcg slow IVP every 5 min until relief achieved (max 200mcg)* If available consider Intranasal administration, same dose as above divided between nares Continuous Respiratory monitoring SPO₂ and End Tidal CO₂ P After each dose: Reassess pain level Ondansetron 4mg slow IV for severe nausea or vomiting M Contact Medical Control for additional orders or questions OLMC must authorize a change in Opiate once administration has begun. M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Area of pain, Neuro * Contraindicated if SBP <90mmHg Analgesic agents may be administered under standing orders for patients experiencing moderate / severe pain (typically >6/10) Common Complaints: trauma/isolated extremity injury, Burns (without airway, breathing or circulation compromise), sickle crisis, Acute chest pain (follow protocol), Kidney stone highly suspected (follow abdominal pain protocol) Vitals and pain scale should be documented before and after every medication dose. Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 115 2013 Pulse Oximetry Pain Management—Adult All Providers General Patient Care Protocol Assess baseline pain level (0-10 scale: 0=no pain, 10=worst pain) Advanced EMT Consider IV Protocol Paramedic Analgesic agents may be administered under standing orders for patients experiencing moderate/severe pain (typically ≥ 6/10) Common complaints: Trauma/isolated extremity injury Burns (without airway, breathing or circulation compromise) Sickle crisis Acute Chest Pain, in accordance with the Chest Pain protocol Kidney stone highly suspected, in accordance with the Abdominal Pain protocol Agents for pain control Morphine Sulfate 2-5 mg slow IVP every 5 minutes until pain relief achieved (Maximum 15 mg) -OR Fentanyl 50-75 mcg slow IVP every 5 minutes until pain relief achieved (Maximum 200 mcg) Both are contraindicated if SBP 90 mmHg If available consider Intranasal administration, same dose as above divided between nares. After each drug dosage administration Reassess and document the patient’s pain level (0-10 scale) Note adequacy or ventilation and perfusion Assess and document vital signs Continuously monitor oxygen saturation and end tidal CO2 For severe nausea or vomiting, Ondansetron (Zofran) 4 mg slow IV 116 Contact Medical Control for any additional orders or questions Medical Control must authorize a change in Opiate once administration has begun. Listed maximum dosages pertain unless other orders given by medical control 117 A P M Legend EMT A‐EMT Paramedic Medical Control A P M After assessing the patient and treating any obvious conditions, transport to the ED should be offered in a manner consistent with the Dane County EMS System General Guidelines. If the detained patient refuses transport, execute a standard refusal process as detailed in protocol. Advise the Law Enforcement Officer (LEO) of the patient’s decision, and if all criteria are met, release the patient to the LEO. If the patient does not meet refusal criteria, advise the LEO that transport is indicated and coordinate a safe transport of the detained patient in accordance with Agency SOPs. If the LEO requires EMS transport in a scenario where the patient has refused, comply with the LEO’s request and transport the patient to the nearest appropriate ED. 2013 In scenarios where a LEO is unwilling to allow transport of a detained patient after EMS personnel have determined transport is indicated (i.e. requested transport, is not a candidate for refusal, or obvious medical necessity) adhere to the following: Assure that the LEO understands transport is indicated and that medical clearance prior to incarceration is not a procedure performed by EMS. Contact On-Line Medical Control for further input and assistance as needed. If these actions fail to resolve the issue, defer to the officer’s legal authority to retain custody of the patient. Document the interaction well, including the law enforcement agency and officer involved. Special Response Protocol When called to a scene to assess a person in police custody, perform all assessment and treatment consistent with the standards set for the typical, non-detained patient. EMS personnel are not equipped to perform formal medical clearance for patients in police custody prior to jail transport. Contact Medical Control for any additional orders or questions Service MD Approval:______ Special Response Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 118 A P M Legend EMT A‐EMT Paramedic Medical Control A P M All Providers Confirm scene safety with law enforcement Turn patient supine if found in a prone position Secure the taser prongs in place if not removed by law enforcement Do not remove the prongs if lodged in the patient and left in place by law enforcement unless there is interference with important patient care measures Paramedic 2013 If the patient requires Chemical or Physical restraints, perform Full ALS Assessment and Treatment For patients with severe agitation resulting in interference with patient care or patient/crew safety, or for patients who continue to struggle against restraints refer to Behavioral Emergencies Protocol Transport patient supine or lateral recumbent position only Special Response Protocol For patients who have been controlled by law enforcement via a Taser device, follow this protocol in conjunction with any protocol that applies to underlying conditions (e.g. behavioral emergencies, cocaine/sympathomimetic toxicity, agitated delirium) Patient transport in the prone position is not authorized! Contact Medical Control for any additional orders or questions Service MD Approval:______ Special Response Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 119 General guidelines for patient refusal of treatment and/or transport: A patient is any person who is requesting and/or is in need of medical attention or medical assistance of any kind. All patients shall be assessed and offered transport by ambulance to the nearest appropriate emergency department, regardless of the nature of the complaint. In the event a patient, or his/her guardian, refuses transport to the hospital, a properly executed refusal process must be completed. Three-Step Process for EMS personnel when accepting a refusal of care: Step 1: Determine if the patient is legally recognized as an informed decision maker. Step 2: Determine if the patient’s decision making capacity appears to be intact. Step 3: Document the interaction well. Step 1 To undergo the informed refusal of medical care process, the patient should be one of the following: A person 18 years of age A court-emancipated minor A legally married person of any age An unwed pregnant female < 18 years of age only when the medical concern relates to her pregnancy A parent (of any age)/ or legal guardian on behalf of their child when the refusal of care does not place the child at risk Involve OLMC for any refusal involving a minor when the parent/legal guardian cannot be contacted Step 2 To undergo the informed refusal of medical care process, the patient or his/her guardian’s decisionmaking process cannot be impaired by medical or psychiatric conditions: All of the following must be present: Awake, alert and oriented to person, place, time and situation (A+OX4) Is not experiencing a medical condition which may interfere with informed decision making capacity (e.g. hypoxia, hypoglycemia, head injury, sepsis etc.) Does not appear clinically intoxicated or under the influence of substances which may impair decision making and judgment Does not express suicidal or homicidal ideations, and does not otherwise pose an obvious threat to themselves or others Is not experiencing hallucination or other apparent thought disorder continued 120 Refusal of Medical Care ‐ continued Step 3 The following items should be documented for every refusal: A mental status examination as detailed in Step 2 above A physical examination (including vital signs) Perform blood glucose level and oxygen saturation when appropriate Pediatric Refusals The following scenarios require OLMC contact prior to completing the refusal process: Refusals involving patients less than 1 year old Pediatric refusals where significant vital sign/ or physical exam abnormalities are present In the event a parent or guardian refuses medical care for a minor when there is reasonable concern that this decision poses a threat to the well-being of the minor: Contact the OLMC Physician for input Enlist the aid of law enforcement personnel for patient and crew safety If an immediately life threatening condition exists, transport the patient to the nearest appropriate emergency department. Refusal of Transport After ALS Initiated: Contact OLMC for refusal situations that arise after advanced life support measures have been initiated Exceptions to this requirement are: Bronchospasm, resolved after nebulizer treatment (see protocol) Insulin-induced hypoglycemia, resolved after glucose administration (see protocol) M Consult Medical Control if needed 121 M Refusal of Transport After Treatment Given Bronchospasm Resolved After Nebulizer Treatment After treatment of bronchospasm, and return to an asymptomatic state, some patients will refuse transport to the hospital. The following items should be accounted for and included in the assessment and documentation: The presentation is consistent with a mild exacerbation of asthma No severe dyspnea at onset No pain, sputum, fever or hemoptysis Not clinically hypoxic (oxygen saturation > 92%) Significant improvement after a single nebulizer treatment Complete resolution of symptoms Vital signs within normal limits after treatment (BP, pulse, respiratory rate and oxygenation) Additional patient safety measures that should be considered: A family member or caregiver should be available to stay with the patient and assist if a relapse occurs Assure the patient understands transport has been offered and subsequently refused Inform the patient to follow-up with their physician as soon as possible and/or to re-contact 911 if symptoms reoccur If the above are accounted for, a properly executed refusal of medical care can be accepted from the patient or custodian without contacting Medical Control. M Consult Medical Control if needed 122 M Refusal of Transport After Treatment Given Insulin-Induced Hypoglycemia—Resolved This protocol applies only to insulin dependent diabetic patients refusing transport after the resolution of insulin-induced hypoglycemia by the administration of intravenous glucose. This protocol cannot be used if the patient takes any oral diabetes medications. After treatment of insulin-induced hypoglycemia and return to an asymptomatic state, some patients will refuse transport to the hospital. The following items should be accounted for and included in the assessment and documentation. The patient is on Insulin only (does not take any oral diabetes medications) The presentation is consistent with hypoglycemia Rapid improvement, and complete resolution of symptoms after glucose Vital signs within normal limits after glucose given (BP, pulse, respiratory rate, oxygenation and blood sugar > 70) There is no indication of an intentional overdose or dosing error Additional patient safety measures that should be considered: A family member or caregiver should be available to stay with the patient and assist if a relapse occurs Assure the patient understands transport has been offered and subsequently refused Inform the patient to follow-up with their physician as soon as possible and/or to re-contact 911 if symptoms reoccur If the above are accounted for, a properly executed refusal of medical care can be accepted from the patient or custodian without contacting Medical Control. M Consult Medical Control if needed 123 M Sedation/Sedative Agent Use Because sedation is a continuum, it is not always possible to predict how an individual patient receiving an agent with sedative properties will respond. This protocol is to be used in conjunction with any protocol that involves the use of medication given by any route, which may result in sedation. Examples of medications that may result in sedation are narcotics, benzodiazepines, haloperidol, diphenhydramine, and ketamine. Minimal Sedation (anxiolysis): A drug induced state in which patients respond normally to verbal commands. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected. Moderate sedation (“conscious sedation”): A drug-induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. Airway patency, spontaneous ventilations, gag reflex, and cardiovascular function are maintained. Deep Sedation: Only to be used in patients with a secured airway. A drug induced depression of consciousness, during which patients cannot be easily aroused but respond purposefully after repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. Patients will require assistance in maintaining a patent airway and spontaneous ventilations may be inadequate. The goal of sedative agent use is to produce the minimal degree of sedation that achieves the desired clinical effect. Sedative agent use should ideally result in minimal or moderate sedation only. Paramedic Full ALS Assessment and Treatment Continuously monitor the following: Patency of airway Vital signs Oxygen saturation and capnography Cardiac rhythm Level of consciousness and ability to follow commands Assure that appropriate equipment and personnel are immediately available for care and resuscitation if problems arise Document the indications for sedation M Consult Medical Control if needed 124 M A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Reported/witnessed seizure activity Previous seizure history Medical alert tag information Seizure medications History of Trauma History of Diabetes History of Pregnancy Signs and Symptoms Decreased Mental Status Sleepiness Incontinence Observed seizure activity Evidence of trauma Unconscious Supplemental O2 – Protect Patient from Injury Blood Glucose – treat if appropriate A A IV Protocol Assess Patient Active Seizure Not seizing P P P Diazepam rectal gel if available* P Seizure Re-occurs P YES Lorazepam 1‐2mg IV/IO (max dose 4mg) Or Midazolam 5mg IV/IO/IM/IN if <60 years old 2.5 mg IV/IO/IM/IN if >60 years old (max dose 10mg) P Service MD Approval:______ Still Seizing? NO Monitor vitals and transport 2013 Monitor vitals and transport Lorazepam 1‐2mg IV/IO (max dose 4mg) Or Midazolam 5mg IV/IO/IM/IN if <60 years old 2.5 mg IV/IO/IM/IN if >60 years old (max dose 10mg) Medical Protocol General Approach to all Adult Patients Differential CNS (Head) Trauma Tumor Metabolic, Hepatic, or Renal Failure Hypoxia Electrolyte abnormality (Na, Ca, Mg) Drugs, Medications, Non‐compliance Infection/Fever Alcohol withdrawal Eclampsia Stroke Hyperthermia Hypoglycemia P M Consult Medical Control for additional Benzodiazepines M P Pearls RECOMMENDED EXAM: Mental Status, HEENT, Heart, Lungs, Extremities, Neuro Status epilepticus is defined as two or more successive seizures without a period of consciousness or recovery. This is a true emergency requiring rapid airway control, treatment and transport Grand mal seizures (generalized) are associated with loss of consciousness, incontinence, and tongue trauma * Diazepam Focal seizures (petit mal) effect only a part of the body and are not usually associated with a loss of consciousness 12+ Years (0.2mg/kg) Jacksonian seizures are seizures which start as a focal seizure and become generalized Dose Weight Be prepared for airway problems and continued seizures (kg) (lb) (mg) Assess possibility of occult trauma and substance abuse 14-27 30-60 5 Be prepared to assist ventilations especially if diazepam or midazolam is used 28-50 61-111 10 For any seizure in a pregnant patient, follow the OB emergencies protocol 51-75 112-166 15 Diazepam is not effective when administered IM. It should only be given rectally. 76-111 167-244 20 Midazolam is well absorbed when administered IM. Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 125 Seizure All Providers General Patient Care Protocol—Adult Supplemental 100% oxygen Nasal cannula is sufficient if no active seizures and no respiratory signs or symptoms Protect patient from injury Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment If Blood Glucose < 70 mg/dL, treat per Altered Mental Status/Hypoglycemia Protocol For active seizures choose one of the following options: Lorazepam (Ativan) 1-2 mg IV/IO - OR Midazolam (Versed) 5 mg IV/IO/IM/IN if < 60 years old 2.5 mg IM/IN/IO/IV if > 60 years old - OR Diazepam rectal gel (Diastat) if available 12 + Years (0.2mg/kg) Weight Dose (Kg) (Lb) (mg) 14-27 30-60 5 28-50 61-111 10 51-75 112-166 15 76-111 167-244 20 126 For seizure not controlled by the above, or if the seizure re-occurs after initial control, choose one of the following: Lorazepam (Ativan) 1-2 mg IV/IO - OR - Midazolam (Versed) 5 mg IV/O/IM/IN if < 60 years old 2.5 mg IM/IN if > 60 years old Maximum dose of Lorazepam is 4 mg Maximum dose of Midazolam is 10 mg If hypoxic seizures, drug induced seizures, seizures from head trauma, stroke or eclampsia suspected Treat as above and refer to appropriate protocol for further care Contact Medical Control for any additional orders or questions Additional Benzodiazepines 127 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Blood Loss – vaginal or GI bleeding, AAA, ectopic Fluid loss – vomiting, diarrhea, fever Infection Cardiac Ischemia (MI, CHF) Medications Allergic reaction Pregnancy History of poor oral intake General Approach to All Adult Patients A A IV Protocol Trauma Cardiac Medical Protocol Differential Shock Hypovolemic Cardiogenic Septic Neurogenic Anaphylactic Ectopic Pregnancy Dysrhythmias Pulmonary Embolus Tension pneumothorax Medication effect / OD Vasovagal Physiologic (pregnancy) Signs and Symptoms Restlessness, confusion Weakness, dizziness Weak, rapid pulse Pale, cool, clammy skin Delayed capillary refill Hypotension Coffee‐ground emesis Tarry stools Non Cardiac Non Trauma A Normal Saline fluid bolus‐250mL May repeat until SBP>90mmHg or max 2L P A If no improvement after 4th fluid bolus ‐ Consider Dopamine 5‐20 mcg/kg/min IV titrated to SBP >90mmHg M Consult Medical Control if needed M Treament per appropriate Cardiac Protocol P Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro Hypotension can be defined as a systolic blood pressure of less than 90 Consider performing orthostatic vital signs on patients in non-trauma situation if suspected blood or fluid loss Consider all possible causes of shock and treat per appropriate protocol Reassess for pulmonary edema after each fluid bolus (lung sounds, respiratory distress, EKG) For non-cardiac, non-trauma hypotension, Dopamine should only be started after 1 liter of NS have been given. Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 128 2013 Treatment per appropriate Trauma Protocol Shock (Non‐Trauma) Shock is defined as a state of inadequate organ perfusion and tissue oxygenation. It is evidenced by the presence of any of the following signs and symptoms: Hypotension Narrow pulse pressure Tachypnea Tachycardia Delayed capillary refill Mottled skin appearance Diaphoresis Cool clammy skin Pallor Altered mental status Signs and symptoms vary depending upon the stage of shock, which may be compensated (normal perfusion maintained) or decompensated (unable to maintain normal perfusion). Categories of shock Obstructive shock: Caused by an obstruction that interferes with return of blood to the heart (e.g. tension pneumothorax, cardiac tamponade, massive pulmonary embolus) Hypovolemic shock: Caused by decreased blood or water volume. Hypovolemic shock may be hemorrhagic or non-hemorrhagic Distributive shock: Caused by abnormal distribution of blood resulting from vasodilaton, vasopermeability or both. Distributive shock may result from anaphylactic reactions, sepsis, or spinal cord injury Cardiogenic shock: Caused as a result of cardiac pump failure, usually secondary to severe Left Ventricular failure. May result from massive MI Perform the following in conjunction with protocols that apply to the specific etiology of the shock state (e.g. allergic reactions, STEMI, etc.): Advanced EMT Consider IV Protocol Do not delay transport for IV insertion IV 0.9% NaCl en route (if not contraindicated): Administer 250 ml boluses until systolic BP > 90 mmHg Total amount of IVF should not exceed 2 L Boluses may be given in rapid succession if systolic remains < 90 mmHg Paramedic Full ALS Assessment and Treatment Do not delay transport for IV insertion IV 0.9% NaCl en route (if not contraindicated): 129 Administer 250 ml boluses until systolic BP > 90 mmHg Total amount of IVF should not exceed 2 L Boluses may be given in rapid succession if systolic remains < 90 mmHg If systolic BP remains < 90 mmHg after 4th bolus (1000ml): Consider Dopamine infusion at 5-20 mcg/kg/min, titrated to maintain SBP > 90 mmHg Contact Medical Control for any additional orders or questions 130 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Previous CVA, TIA’s Previous cardiac,/vascular surgery Associated diseases: diabetes, hypertension, CAD Atrial Fibrillation Medications (blood thinners) History of Trauma Differential See Altered Mental Status TIA (Transient Ischemic Attack) Seizure Hypoglycemia Stroke Thrombotic Embolic (~85%) Hemorrhagic (~15%) Tumor Trauma General Approach to all Adult Patients Blood Glucose Glucose <70 Glucose >70 Altered Mental Status Protocol* Cincinnati Stroke Scale Positive If Positive and Symptoms <24 hour, early notification of Stroke Alert and rapid transport to stroke center Medical Protocol Signs and Symptoms Altered mental status Weakness / Paralysis Blindness or other sensory loss Aphasia / Dysarthria Syncope Vertigo / Dizziness Vomiting Headache Seizures Respiratory pattern change Hypertension / Hypotension 2013 Negative 12 Lead EKG Consider other protocols as indicated: Altered Mental Status Hypertension Hypotension Seizure Overdose / Toxic Ingestion Service MD Approval:______ M Consult Medical Control M Pearls RECOMMENDED EXAM: Mental Status, HEENT, Heart, Lungs, Abdomen, Extremities, Neuro * Reassess for Stroke if no improvement with Altered Mental Status Protocol Remember FAST in radio report: Facial Droop, Arm Strength, Speech, Time last normal Cincinnati Stroke scale in procedure section Supplemental oxygen via nasal only if O2 saturation <93% Keep head of stretcher at 30-45° elevation (unless clinical condition will not allow) Spinal immobilization if indicated; elevate head of backboard 15-30° Do NOT delay transport to start IV Onset of symptoms is defined as the last witnessed time the patient was symptom free (ie awakening in the morning with stroke symptoms would be defined as an onset time of the previous night when patient was symptom free) Be alert for airway problems (swallowing difficulty, vomiting/aspiration) Hypoglycemia can present as a localized neurologic deficit, especially in the elderly Document the stroke scale (including the EMD stroke scale results if available) Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 131 Stroke—Suspected Early recognition and transport of stroke is essential to good patient outcomes. Any patient presenting with a normal blood glucose (> 70 mg/dL), a positive Cincinnati Pre-Hospital Stroke Screen and onset of symptoms (when last seen normal) less than 24 hours should have early notification of the stroke center (STROKE ALERT) and rapid transport. All Providers General Patient Care Protocol-Adult Supplemental oxygen via nasal cannula only if O2 saturation < 93% Keep head of stretcher at 30-45 elevation (unless clinical condition will not allow) Spinal Immobilization if indicated; elevate head of backboard 15-30 Check Blood Glucose Give nothing by mouth (oral glucose is permitted if patient is able to self administer) Cincinnati Pre-Hospital Stroke Screen If patient blood glucose is ≥ 70 mg/dl, Cincinnati Pre-Hospital Stroke Screen is positive and onset of symptoms (when last seen normal) is < 24 hours, immediately notify ED (STROKE ALERT) and commence rapid transport. Advanced EMT Consider IV Protocol If hypoglycemic (<70 mg/dL) with IV access Dextrose 12.5g-25g slow IV push or D10W 100mL May repeat as needed every 5-10 minutes to blood glucose > 70 mg/dL If hypoglycemic (< 70 mg/dL) without IV access Glucose paste 15 g or other oral glucose agent (e.g., orange juice) if patient alert enough to self administer oral agent - OR Glucagon 1 mg IM DO NOT DELAY TRANSPORT TO OBTAIN IV ACCESS Paramedic Full ALS Assessment and Treatment Check blood glucose 132 For hypotension (systolic BP < 90 mmHg) not improved by fluid boluses or when fluid resuscitation is contraindicated Dopamine infusion 5-20 mcg/kg/min titrated to maintain systolic BP > 90 mmHg Contact Medical Control for any additional orders or questions 133 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Cardiac history, stroke, seizure Occult blood loss (GI, ectopic) Females: LMP, vaginal bleeding Fluid loss: nausea, vomiting, diarrhea Past Medical History Medications Signs and Symptoms Loss of consciousness with recovery Lightheadedness, dizziness Palpitations, slow or rapid pulse Pulse irregularity Decreased blood pressure General Approach to all Adult Patients Blood Glucose Glucose <70 Altered Mental Status Protocol >70 IV Protocol ‐ NS bolus 250ml to maintain SBP >90mmHg (max 2L) A 2013 A 12 Lead EKG P If SBP <90mmHg not improved by fluid Dopamine infusion 5‐20 mcg/kg/min titrated to maintain SBP >90mmHg Medical Protocol Differential Vasovagal Orthostatic hypotension Cardiac syncope Micturation / Defecation syncope Psychiatric Stroke Hypoglycemia Seizure Shock (see shock protocol) Toxicologic (alcohol) Medication effect (Hypertension) P AT ANY TIME If relevant signs / symptoms found Go to appropriate protocol: DYSRHYTHMIA ALTERED MENTAL STATUS M Consult Medical Control M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Heart, Lungs, Abdomen, Back, Extremities, Neuro Assess for signs and symptoms of trauma if associated or questionable fall with syncope Consider dysrhythmias, GI bleed, ectopic pregnancy, and seizure as possible causes of syncope. Spinal Immobilization Protocol if appropriate . Medical Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 134 Syncope All Providers General Patient Care Protocol-Adult 12 Lead EKG Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment For hypotension (systolic BP < 90 mmHg) not improved by NS fluid boluses or when fluid resuscitation is contraindicated Dopamine infusion 5-20 mcg/kg/min titrated to maintain systolic BP > 90 mmHg If hypoglycemic (< 70mg/dL), treat per Altered Mental Status/Hypoglycemia Protocol If ECG rhythm is bradycardia, heart block or dysrhythmia see specific protocol If Altered Mental Status persists, or if Acute Stroke suspected, refer to appropriate protocol. Contact Medical Control for any additional orders or questions 135 136 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Time and mechanism of injury Damage to structure or vehicle Location in structure or vehicle Others injured or dead Speed and details of MVC Restraints/ protective equipment Past medical history medications Signs and Symptoms Pain, swelling Deformity, lesions, bleeding Altered Mental Status or unconscious Hypotension or shock Arrest General Approach to All Adult Patients Differential Chest Tension Pneumothorax, flail chest, pericardial tamponade, open chest wound, hemothorax Intra‐abdominal bleeding Pelvis/femur fracture Spine fracture / Cord injury Head injury (see head trauma) Extremity fracture/dislocation HEENT (Airway Obstruction) Hypothermia Trauma Protocol Presentation or Mechanism Consistent with Trauma YES NO Appropriate Medical Protocol Assess ABC’s INADEQUATE Airway, Adult Protocol ADEQUATE Spinal Immobilization Protocol Obvious Bleeding? YES NO Disability and GCS Direct Pressure Service MD Approval:______ Complete Head to Toe Survey Pressure Point Tourniquet for uncontrolled extremity hemorrhage Vital Signs Abnormal** Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Heart, Lungs, Abdomen, Extremity, Back, Neuro * Pleural Decompression should only be preformed when all 3 criteria are present: 1-severe respiratory distress with hypoxia 2-unilateral decreased or absent lung sounds (may see tracheal deviation away from collapsed lung) 3-evidence of hemodynamic compromise (ie. Shock, hypotension, tachycardia, altered mental status) ** Abnormal: hypotension, Tachycardia, Hypoxia If indicated perform pleural decompression at the 2nd intercostal space, mid-clavicular line Assess all patients for major trauma criteria. Major trauma patients should have transport initiated within 10 minutes of arrival on scene whenever possible. In the setting of major trauma, DO NOT prolong scene time to perform procedures unless immediately necessary to stabilize patient (ie. Hemorrhage control). Initiate all other procedures while enroute to the trauma center. Disability – assessment neurological deficits: paralysis, weakness, abnormal sensation, etc. A IV Protocol 250ml bolus NS x2 YES P Notify receiving hospital A Tension Pneumothorax? NO P Pain Control Protocol Decompress* M Contact Medical Control Normal M High suspicion severe injury Facility/Provider discretion Rapid Transport to Trauma Receiving Facility <10 minutes Trauma Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 137 Trauma: General Approach to All Trauma Patients Assess all patients for major trauma criteria. Major trauma patients should have transport initiated within 10 minutes of arrival on scene whenever possible. In the setting of major trauma, DO NOT prolong scene time to perform procedures unless immediately necessary to stabilize patient (e.g. hemorrhage control). Initiate all other procedures en-route to the trauma center. All Providers General Patient Care Protocol—Adult Secure airway/spinal immobilization if indicated Supplemental 100% oxygen if any respiratory symptoms Examine patient for obvious bleeding Control active bleeding with direct pressure Assess disability-neurologic status/record Glasgow coma score Head to toe examination to assess for injuries Restrain as needed Paramedic When conditions warrant (specified as “Full ALS Assessment and Treatment” in individual protocol) Advanced airway/ventilatory management as needed Perform cardiac monitoring Record and monitor O2 saturation Microstream capnography if any acute respiratory symptoms IV 0.9% NaCl TKO/KVO or IV lock If SBP < 90 mmHg, administer boluses of 0.9%NaCl at 250 ml until SBP > 90 mmHg Assess for Tension Pneumothorax Tension pneumothorax should be suspected in patients who exhibit Severe respiratory distress with hypoxia Unilateral decreased or absent lung sounds (may see tracheal deviation away from collapsed lung field) Evidence of hemodynamic compromise (e.g. shock, hypotension, tachycardia, altered mental status) 138 Pleural decompression for tension pneumothorax should only be preformed when all 3 of the above criteria are present; If indicated perform pleural decompression at the 2nd intercostal space, mid-clavicular line Refer to Pain Management Protocol as needed Contact Medical Control for any additional orders or questions 139 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Type of exposure (heat, gas, chemical) Inhalation injury Time of injury Past medical history and medications Other trauma Loss of consciousness Tetanus/immunization status Signs and Symptoms Burns, pain, swelling Dizziness Loss of consciousness Hypotension/shock Airway compromise/distress Singed facial or nasal hair Hoarseness/wheezing Differential Superficial (1st degree) red and painful Partial thickness (2nd degree) blistering Full thickness (3rd degree) painless/charred or leathery skin Thermal Chemical Electrical Radiation General Approach to All Adult Patients Transport to Burn Center Trauma Protocol 2nd degree burns greater than 10% total body surface area or those on hands, feet, face or groin 3rd degree burns Electrical burns (spinal immobilization if high voltage, monitor for cardiac arrhythmias, initiate fluid resuscitation immediately Chemical burns (remove clothing, brush away dry powder before irrigating, flush with copious warm water on scene and continue irrigation enroute, eyes: remove contacts and irrigate continuously with NS for at least 30 minutes, avoid hypothermia ABC’s *Airway Protocol Remove or cool heat source if present Remove all clothing, contact lenses, and jewelry (especially rings) If inhalation injury – place patient on 100% O2, monitor ETCO2 continuously Maintain core temperature Cover burn with plastic wrap, plastic chucks, or clean dry dressings IV Protocol A Large bore in unburned skin if possible If burn is >20%TBSA 2nd/3rd degree burns – NS at 500ml/hr If burn is >30%, place 2 large bore IVs Pearls RECOMMENDED EXAM: Mental Status, HEENT, Skin, Neck, Lung, Heart, Abdomen, Extremities, Back, and Neuro Burn patients are trauma patients, evaluate for multisystem trauma Assure whatever has caused the burn, is no longer contacting the injury (stop the burning process) Early intubation is required when the patient experiences significant inhalation injuries Potential CO exposure should be treated with 100% oxygen. Circumferential burns to extremities are dangerous due to potential vascular compromise secondary to soft tissue swelling Burn patients are prone to hypothermia – never apply ice or cool burns, must maintain normal body temperature Evaluate the possibility of child abuse with children and burn injuries *Signs and symptoms of inhalation injury: carbonaceous sputum, facial burns or edema, hoarseness, singed nasal hairs, agitation, anxiety, cyanosis, stupor or other signs of hypoxia A Consider Pain Management Protocol M Contact Medical Control M Service MD Approval:______ Trauma Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 140 Trauma: Burns—Thermal All Providers General Patient Care Protocol – Adult o Stay focused on ABC’s, don’t get side tracked by burn! o DON’T BECOME A SECOND VICTIM! Remove or cool heat source if present (e.g. clothing, tar) o Cool burns with room temperature water for 3-5 minutes only except for tar burns which will take an extended time to cool. o NEVER COOL WITH ICE! The goal is to bring burns to room temperature, not cold. Remove all clothing, contact lenses, and jewelry, especially rings Maintain core temperature. Keep patient warm and dry with sheets and blankets. Cover burns with plastic wrap, plastic chucks, or clean, dry dressings. If inhalation injury is suspected o Place patient on 100% oxygen – DO NOT DECREASE o Monitor ETCO2 continuously (if available) Estimate Total Body Surface Area (TBSA) o Rule of Nines o For scattered burns, use the size of patient’s hand, including fingers, to equal 1% burn. INDICATIONS FOR TRANSFER TO A BURN CENTER 2nd Degree burns greater than 10% total body surface area or those on hands, feet, face, or groin 3rd degree burns Electrical burns - Spinal immobilization if high voltage electrical injury - Monitor for cardiac arrhythmias - Initiate fluid resuscitation immediately Chemical burns - Remove clothing - If dry powder is present, brush away before irrigating - Flush with copious warm water on scene and continue irrigation enroute to UW Hospital - Chemical injuries to eyes are an EMERGENCY. Remove contacts and irrigate continuously with normal saline for at least 30 minutes. - Avoid hypothermia 141 Advanced EMT Consider IV Protocol Place large bore peripheral IV’s in unburned skin if possible If TBSA % greater than 20% of 2nd and 3rd degree burns, initiate fluid resuscitation with 0.9% Normal Saline at 500ml/hour If TBSA greater then 30%, place 2 large bore peripheral IV’s Paramedic Observe for signs of impending loss of airway; Refer to the Airway Management Protocol as needed: Hypoxia Poor ventilatory effort Altered Mental status/decreased level of consciousness Inability to maintain patent airway Signs or Symptoms of Inhalation injury Carbonaceous sputum Extensive facial burns or facial edema Hoarseness Singed nasal hairs Agitation, anxiety, cyanosis, stupor or other signs of hypoxia ● If inhalation injury is suspected Place patient on 100% oxygen-DO NOT DECREASE Monitor ETCO2 continuously Consider Airway Management Protocol If moderate to severe pain, see Pain Management Protocol Contact Medical Control for any additional orders or questions 142 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Trauma: Chest Injuries General Patient Care Protocol—Adult Assess breath sounds frequently Assess for ventilatory compromise and assist with BVM as needed For open/sucking chest wounds, apply occlusive dressing sealed on three (3) sides or commercially available chest seal Remove temporarily to vent air if respiratory status worsens Paramedic Full ALS Assessment and Treatment Assess for flail segment Observe for signs of impending respiratory failure; Refer to the Airway Management Protocol as needed: Hypoxia Poor ventilatory effort Altered mental status/decreased level of consciousness Inability to maintain patent airway Contact Medical Control for any additional orders or questions Service MD Approval:______ Trauma Protocol Any local EMS Agency changes to this document must follow the 76 DCEMS Protocol Change Policy and be approved by WI EMS 143 Trauma Protocol All Providers A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Type of injury Mechanism (blunt vs. penetrating) Loss of consciousness Bleeding Past medical history Medications Evidence of multi‐trauma Signs and Symptoms Pain, swelling, bleeding Altered mental status Unconscious Respiratory distress / failure Vomiting Major traumatic mechanism of injury seizure Differential Skull fracture Brain injury (concussion, contusion, hemorrhage, or laceration) Epidural hematoma Subdural hematoma Subarachnoid hemorrhage Spinal injury Abuse General Approach to All Adult Patients Trauma Protocol Restrain as needed Spinal Immobilization Protocol elevate head of backboard to 15°‐30° (if normotensive or hypertensive) Obtain and Record GCS A A IV Protocol Airway Protocol Maintain Pulse Ox >93% EtCO2 target 40 Seizure Protocol YES Seizure? Service MD Approval:______ NO P Lorazepam 1‐2mg IV/IO (max 4mg) Or Midazolam 1‐2mg IV/IO (max 4mg) P Severe Agitation/Combative? YES NO Monitor and Reassess M Contact Medical Control M Pearls RECOMMENDED EXAM: Mental Status, HEENT, Heart, Lungs, Abdomen, Extremity, Back, Neuro If GCS <12 consider Air transport or Rapid Transport Airway interventions can be detrimental to patients with head injury by raising intracranial pressure, worsening hypoxia (and secondary brain injury) and increasing risk of aspiration. Whenever possible these patients should be managed in the least invasive manner to maintain O2 saturation >90% (ie. NRB, BVM with 100% O2) Acute herniation should be suspected when the following signs are present: acute unilateral dilated and non‐reactive pupil, abrupt deterioration in mental status, abrupt onset of motor posturing, abrupt increase in blood pressure, abrupt decrease in heart rate. Only in suspected acute herniation – hyperventilate (rate 20/minute) and target EtCO2 30‐35mmHg Increased intracranial pressure (ICP) may cause hypertension and bradycardia (Cushings response) Hypotension usually indicates injury or shock unrelated to the head injury and should be treated aggressively Most important vital sign to monitor and document is level of consciousness (GCS) Concussions are periods of confusion or LOC associated with trauma which may have resolved by the time EMS arrives. Any prolonged confusion or mental status abnormality which does not return to normal within 15 minutes or any documented loss of consciousness should be evaluated ASAP by a physician. Trauma Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 144 Trauma: Head Injuries All Providers General Patient Care Protocol-Adult Supplemental oxygen Restrain as needed Spinal Immobilization If normotensive or hypertensive Elevate head of backboard 15 - 30 Paramedic Full ALS Assessment and Treatment Advanced airway/ventilatory management as needed Note: Airway interventions can be detrimental to patients with head injury by raising intracranial pressure, worsening hypoxia (and secondary brain injury) and increasing risk of aspiration. Whenever possible these patients should be managed in the least invasive manner to maintain O2 saturation > 93% (i.e. NRB, BVM with 100% O2) Observe for signs of impending respiratory failure; Refer to the Airway Management Protocol if needed: Hypoxia Poor ventilatory effort Altered mental status/decreased level of consciousness Inability to maintain patent airway For patients with assisted ventilation Administer eucapneic (normal rate 12-15/min) ventilations Titrate to target an ETCO2 of 40 mmHg Acute herniation should be suspected when the following signs are present: Acute unilateral dilated and non-reactive pupil Abrupt deterioration in mental status Abrupt onset of motor posturing Abrupt increase in blood pressure Abrupt decrease in heart rate Hyperventilation (ventilatory rate of 20) is a temporizing measure which is only indicated in the event of acute herniation If signs of herniation develop, increase ventilatory rate to 20/minute and target an ETCO2 of 30-35 mmHg 145 If severely agitated/combative and unable to de-escalate by any other means, consider: Lorazepam 1-2 mg IV/IO, max 4 mg OR Midazolam 1-2 mg IV/IO, max 4 mg Contact Medical Control for any additional orders or questions Additional sedation for combative patients 146 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Trauma: Eye Injuries General Patient Care Protocol—Adult Measure visual acuity If injury is secondary to a chemical exposure: Remove patient from source if safe to do so Remove contact lenses if appropriate; transport with patient Irrigate the eyes with 0.9 % Normal Saline for a minimum of 20 minutes Determine chemical involved, bring MSDS sheet if available If eye injury is due to trauma: Stabilize any penetrating objects Do not remove any impaled object Protective metal shield unless impaled object precludes Prevent patient bending or standing If blood observed in anterior chamber, transport with head elevated 60 Contact Medical Control for any additional orders or questions Service MD Approval:______ Trauma Protocol Any local EMS Agency changes to this document must follow the 76 DCEMS Protocol Change Policy and be approved by WI EMS 147 Trauma Protocol All Providers A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Type of injury Mechanism: crush/penetrating/amputation Time of injury Open vs. closed wound / fracture Wound contamination Medical history medications Signs and Symptoms Pain, swelling Deformity Altered sensation/motor function Diminished pulse/capillary refill Decreased extremity temperature Differential Abrasion Contusion Laceration Sprain Dislocation Fracture Amputation General Approach to All Adult Patients Trauma Protocol Wound care Control Hemorrhage with Pressure Splinting as required** If hemorrhage can not be controlled by direct pressure and is life threatening then consider Tourniquet procedure* A IV Protocol If life or limb threatening event or if pain medication needed A 250 ml NS bolus to maintain SBP >90mmHg (max 2L) Pain Control Protocol If amputation: clean amputated part and wrap part in sterile dressing soaked in NS and place in an air tight container, place container on ice if available M Contact Medical Control Service MD Approval:______ M Pearls RECOMMENDED EXAM: Mental Status, Extremity, Neuro *Apply commercially available tourniquet device as proximal on extremity as possible, commercial must be at least 1.5 inches wide, non-commercial must be at least 2 inches wide. Tighten tourniquet until bright red bleeding has stopped. Secure in place and expedite transport to Level 1 trauma center. Document time of placement in patient care report and on device (if possible). Notify medical control of tourniquet use. **Check distal pulses, capillary refill, sensation/movement prior to splinting: If pulse present, splint in position found if possible; If pulse absent, attempt to place the injury into anatomical position Open wounds/fractures should be covered with sterile dressings and immobilized in the presenting position Dislocations should be immobilized to prevent any further movement of the joint Check distal pulses, capillary refill and sensation after splinting Peripheral neurovascular status is important (CMS) In amputations, time is critical. Transport and notify medical control immediately. Hip dislocations and knee and elbow fracture/dislocations have a high incidence of vascular compromise. Urgently transport any injury with vascular compromise Blood loss may be concealed or not apparent with extremity injuries Lacerations must be evaluated for repair within six hours from the time of injury Trauma Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 148 Trauma: Extremity All Providers General Patient Care Protocol—Adult Remove or cut away clothing to expose area of injury Control active bleeding For uncontrollable hemorrhage (heavy bleeding despite aggressive direct pressure): Apply commercially available tourniquet device as proximal on extremity as possible, minimum 2” proximal to the hemorrhage site. Do not place over a joint Commercial Tourniquets must be at least 1.5 inches wide Non-Commercial Tourniquets must be at least 2 inches wide Tighten tourniquet until bleeding has stopped Secure in place and expedite transport to Level 1 Trauma Center Document time placed on chart and on device (if possible) Notify receiving center of presence, time placed, and location of tourniquet Check distal pulses, capillary refill, sensation/movement prior to splinting If pulse present, splint in position found if possible If pulse absent, attempt to place the injury into anatomical position Open wounds/fractures should be covered with sterile dressings and immobilized in the presenting position Dislocations should be immobilized to prevent any further movement of the joint Check distal pulses, capillary refill and sensation after splinting Advanced EMT Consider IV Protocol Paramedic Full ALS Assessment and Treatment For isolated extremity trauma: Stabilize BP (SBP 90 mmHg) Refer to the Pain Management protocol as needed Contact Medical Control for any additional orders or questions 149 Trauma: Traumatic Amputations All Providers General Patient Care Protocol—Adult For uncontrollable hemorrhage (heavy bleeding despite aggressive direct pressure): Apply tourniquet device as proximal on extremity as possible, a minimum of 2” proximal to the hemorrhage site. ▪ Do not place over a joint ▪ Commercial Tourniquet must be at least 1.5 inches wide ▪ Non-Commercial Tourniquet must be 2 inches wide Tighten tourniquet until bleeding has stopped Secure in place and expedite transport to Level 1 Trauma Center Document time placed on chart and on device (if possible) Notify receiving center of presence, time placed, and location of tourniquet If amputation incomplete: Attempt to stabilize with bulky pressure dressing Splint inline If amputation complete: Cleanse amputated part with sterile saline Wrap in sterile dressing moistened in sterile saline Place in plastic bag if possible Attempt to cool with cool pack during transport Advanced EMT Consider IV Protocol Paramedic For isolated extremity trauma: Stabilize BP (SBP 90 mmHg) Refer to Pain Management protocol as needed Contact Medical Control for any additional orders or questions 150 A P M Legend EMT A‐EMT Paramedic Medical Control A P M History: Patient who has suffered traumatic injury and is now pulseless Signs and Symptoms Evidence of penetrating trauma Evidence of blunt trauma General Approach to All Adult Patients PNB and: (one or more of the following) Trauma Protocol Injuries Incompatible with life? (Incineration, decapitation, hemicorporectomy) OR Rigor Mortis OR Decomposition of body tissue OR Dependent Lividity OR Evidence of significant time lapse Differential Medical condition preceding traumatic event as cause of arrest. Tension Pneumothorax Hypovolemic Shock External hemorrhage Unstable pelvic fracture Displaced long bone fracture(s) Hemothorax Intra‐abdominal hemorrhage Retroperitoneal hemorrhage Criteria does not apply for: PNB after blunt or penetrating trauma and: pulseless and apneic lack of pupillary reflexes and spontaneous movement Asystole or agonal rhythm <20 on monitor Lightening or other high voltage injury, Drowning, Suspected Hypothermia, Cardiac Arrest Inconsistent with arrest due to trauma, or Transport has been initiated PNB after traumatic injury when transport to nearest ED is >15 minutes and: pulseless and apneic lack of pupillary reflexes and spontaneous movement Asystole or agonal rhythm <20 on monitor YES Withhold Resuscitative Efforts NO Appropriate Cardiac Arrest Protocol Contact Law Enforcement and/or Medical Examiner M Contact Medical Control Service MD Approval:______ M Pearls Injuries obviously incompatible with life include decapitation, massively deforming head or chest injuries, or other features of a particular patient encounter that would make resuscitation futile, when in doubt, place patient on the monitor. Consider using medical cardiac arrest protocols if uncertainty exists regarding medical or traumatic cause of arrest. As with all major trauma patients, transport should generally not be delayed for these patients Where the use of spinal immobilization interferes with performance of quality CPR, make reasonable efforts to manually limit patient movement Trauma Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 151 Trauma: Indications for Withholding Resuscitation in Traumatic Cardiopulmonary Arrest CPR can be withheld in Traumatic Cardiopulmonary Arrest under the following circumstances: Pulseless, apenic, and no other signs of life present AND The presence of one or more of the following: Rigor Mortis Decomposition of body tissues Dependant Lividity Injuries incompatible with life (e.g. incineration, decapitation, hemicorporectomy) Evidence of significant time lapse since pulselessness - OR - Patients who present pulseless after blunt trauma or penetrating trauma provided that all other signs of life are absent: Pulseless and Apenic Lack of pupillary reflexes and spontaneous movement Asystole or agonal rhythm < 20 on cardiac monitor - OR - Patients who become pulseless after severe traumatic injury when transport to the NEAREST ED cannot be accomplished within 15 minutes (i.e., prolonged extrications), provided that all other signs of life are absent and transport has not been initiated: Pulseless and apenic Lack of pupillary reflexes and spontaneous movement Asystole or agonal rhythm < 20 on cardiac monitor This criteria does not apply in the following scenarios: When the Cardiac Arrest is inconsistent with Cardiac Arrest due to trauma Lightning or other high voltage injuries Drowning Suspected hypothermia Transport has been initiated Contact Medical Control for any additional orders or questions 152 A P M Legend EMT A‐EMT Paramedic Medical Control A P M General Patient Care Protocol For victims of sexual assault who meet major trauma criteria, transport to Level 1 Trauma Center For all other cases, transport to nearest appropriate Emergency Department □ If medically stable and appropriate consider transport to SANE (Sexual Assault Nurse Examiner) capable facility. Provide supportive care as indicated by patient’s condition Preserve evidence □ Paper bags are preferred to plastic in evidence preservation. □ If present, defer to law enforcement for proper chain of custody. Contact Medical Control for any additional orders or questions Service MD Approval:______ Trauma Protocol Any local EMS Agency changes to this document must follow81the 76 DCEMS Protocol Change Policy and be approved by WI EMS 153 Trauma Protocol Trauma: Sexual Assault Legend EMT A‐EMT Paramedic A A P P Medical Control M M Determining the need for spinal immobilization requires a careful assessment of the injury, the patient’s complaints and overall condition, and the patient’s ability to recognize and convey the presence of spinal injury symptoms. It is not feasible to “clear” the spine in the prehospital setting. Spinal immobilization should always be applied when any doubt exists as to the possibility of spinal trauma. The following algorithms (Blunt and Penetrating Trauma) can be used to assist EMS in making the most appropriate decision about the need for spinal immobilization. Blunt Trauma Altered Level of Consciousness? GCS <15 Presence of neurologic deficit or complaints₂ ? Test Motor functioning both upper and lower extremities (entire extremity) Test sensation in both upper and lower extremities (start proximal and work towards hands and feet) Ask about numbness and tingling in extremities. NO Any of the following: YES YES YES ▪ spinal pain or tenderness ₁ ▪neurologic deficit or complaint₂ ▪anatomical deformity of the spine YES NO Trauma Protocol YES Immobilize Penetrating Trauma If in Doubt - Immobilize NO Concerning Mechanism of Injury*? NO Any of the following: ▪ Evidence of (significant) clinical intoxication ▪ Distracting Injury₃ ▪ Inability to communicate₄ Immobilize Immobilization not indicated NO Immobilization not indicated M Medical Control If Needed M Service MD Approval:______ Pearls ₁ Tenderness to the midline posterior neck and back, including the paraspinal musculature ₂ Examples are numbness, focal weakness, focal sensory deficit, parasthesias ₃ Examples are long bone fractures, dislocations, large lacerations, degloving injuries, serious burns or any other injury causing functional impairment. ₄ Examples include language barrier, hearing or speech impairment, dementia and age (young children) * Concerning MOI: ‐Any mechanism that produces a violent impact on the head, neck, torso or pelvis ‐Incidents that produce sudden acceleration or deceleration, including lateral bending forces ‐ Any fall, especially in the elderly ‐ Ejection or fall from a moving mode of transportation ‐ Shallow‐water drowning or diving injuries – must immobilize ‐ High voltage electrical injuries – must immobilize If spinal immobilization is indicated but refused by the patient: Advise the patient of the indication for immobilization and the risks of refusing the intervention. If the patient allows, apply the cervical collar even if backboard is refused. Maintain spinal alignment as best as can be achieved during transport. Clearly document refusal of immobilization For patients who cannot tolerate supine position due to clinical condition: apply all elements the patient can tolerate, maintain spinal alignment as best as can be achieved during transport, clearly document clinical condition that interfered with full immobilization. Determining the presence of neurological signs and symptoms requires careful assessment and history taking. Trauma Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 154 Spinal Immobilization: Indications Determining the need for spinal immobilization requires a careful assessment of the injury, the patient’s complaints and overall condition, and the patient’s ability to recognize and convey the presence of spinal injury symptoms. It is not feasible to “clear” the spine in the prehospital setting. Spinal immobilization should always be applied when any doubt exists as to the possibility of spinal trauma. The following algorithms (Blunt and Penetrating Trauma) can be used to assist EMS in making the most appropriate decision about the need for spinal immobilization. Blunt Trauma Assess for concerning mechanism of injury: Any mechanism the produces a violent impact on the head, neck, torso or pelvis Incidents that produce sudden acceleration or deceleration, including lateral bending forces Any fall with neck pain, back pain, altered mental status and/or neurologic deficit, especially in the elderly Ejection or fall from a moving mode of transportation Shallow-water drowning or diving injuries High-voltage electrical injuries Assess patient’s ability to clearly communicate and/or comprehend the nature of their injuries: Altered level of consciousness GCS < 15 Evidence of significant intoxication Dementia Speech or hearing impairment Age (young children) Language barrier Assess for physical signs or symptoms of spinal trauma: Spinal pain or tenderness, including paraspinal muscles Neurologic deficit or complaint, including parasthesia, paralysis, or weakness Anatomical deformity of the spine 155 Assess for presence of distracting injuries, including but not limited to: Long bone fractures Joint dislocations Abdominal or thoracic pain, or obvious visceral injury Large lacerations, degloving injuries or crush injuries Any injury producing acute functional impairment Craniofacial injuries IF ANY OF THE ABOVE MENTIONED FEATURES ARE PRESENT, OR IF ANY QUESTION, IMMOBILIZE! Contact Medical Control for any additional orders or questions 156 Immobilize all patients with the following conditions: High voltage electrical injuries (does not include Taser use) Shallow water drowning or diving injuries If spinal immobilization is indicated but refused by the patient: Advise the patient of the indication for immobilization and the risks of refusing the intervention. If the patient allows, apply the cervical collar even if backboard is refused. Maintain spinal alignment as best as can be achieved during transport. Clearly document refusal of immobilization. For patients who cannot tolerate supine position due to clinical condition: Apply all elements of spinal immobilization that the patient will tolerate. Maintain spinal alignment as best as can be achieved during transport. Clearly document the clinical condition that interfered with full immobilization. Contact Medical Control for any additional orders or questions 157 158 The following measures will apply to the management of all pediatric patients: A Child shall be defined as: Age <12 years of age or weight <40 kg (if age unknown) No signs of puberty if age/weight not able to be determined For PALS resuscitation <8 years For Major Trauma <18 years All Providers Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 159 2013 Contact Medical Control for any additional orders or questions Pediatric Protocol Ensure scene safety Scene survey to determine environmental conditions, mechanism of injury or illness and potential for hazardous conditions Form general impression of patient’s condition Establish patient responsiveness Immobilize spine if cervical or other spine injury suspected Assess airway and breathing, manage as appropriate Supplemental 100% Oxygen if any respiratory signs or symptoms Assess circulation and perfusion by measuring heart rate, and observing skin color, temperature, capillary refill and the quality of central/peripheral pulses. □ For children with absent pulses, initial cardiopulmonary resuscitation Control hemorrhage using direct pressure or a pressure dressing Measure Blood Pressure in children older than 3 Evaluate mental status including pupil reaction, motor function and sensation Vital Signs for Children □ For mental status, use the AVPU scale: • A‐ The patient is alert and oriented (age appropriate) Respiratory Systolic Blood Age Group Rate Heart Rate Pressure • V – The patient is responsive to verbal stimulus Newborn 30-60 120-180 >60 • P – The patient is responsive to painful stimulus Infant (1-12 Months) 20-40 100-140 >70 • U – The patient is unresponsive to any stimulus Toddler (1-3 years) 20-34 90-130 >75 Expose the child only as necessary to perform further assessments Preschooler Maintain the child’s body temperature throughout assessment (3-5 Years) 20-30 80-120 >80 School Age Utilize the Broslow‐Luten® system for estimating patient weight (6-12 Years) 18-30 70-110 >80 Advanced EMT Adolescent (13+ Years) 12-20 60-100 >90 ● Consider IV Protocol Paramedic ● When condition warrants (specified as “Full Pediatric ALS Assessment and Treatment” in individual protocols): □ Airway/ventilatory management as needed □ Perform cardiac monitoring □ Record and monitor O2 saturation □ Record and monitor End‐tidal CO2 □ If symptoms severe or for medication access IV 0.9% NaCl TKO/KVO or IV Lock ● If signs of shock administer boluses of 0.9% NaCl at 20 ml/kg until signs of shock resolve or 60 ml/kg total ● If signs of severe cardiopulmonary compromise (poor systemic perfusion, hypotension, altered consciousness and/or respiratory distress/failure) and IV attempts unsuccessful (max 2 attempts) in a child consider intraosseous access □ If a child’s condition is critical or unstable, initiate transport without delay ● Perform procedures, history and detailed physical exam en route to the hospital ● Unless specified in protocol, all medication dosages and equipment sizes should be calculated using the Broselow‐ Luten system □ Reassess the patient frequently Legend EMT A‐EMT Paramedic A A P P Medical Control M M History: Time of arrest Possibility of foreign body Medical history Medications Fever or respiratory infection Other sick siblings History of trauma Signs and Symptoms Wheezing or stridor Respiratory retractions Increased heart rate Altered level of consciousness Anxious appearance General Approach to all Pediatric Patients Ventilatory Insufficiency Respiratory Failure Assess ABC’s Stridor? YES NO Airway, Pediatric Protocol Drooling, Dysphonia, Fever, “Toxic Appearing” Pulse Ox and Lung Sounds NO Wheezing? YES Allergic Reaction Suspected? NO Supplemental O₂ Keep SpO₂ >93% Supplemental O₂ Keep SpO₂ >93% YES Albuterol 2.5mg/3ml Ipratropium 0.5mg/2.5ml May repeat Albuterol (total 3 doses)*** IMPROVED Comfort and transport As appropriate WORSENING A UNCHANGED P M P Consider Inhaled Epi 3ml of 1:1,000 mixed in 3ml NS M IV Protocol Position of Comfort Supplemental O₂ As tolerated Transport Rapidly A 2013 Epi IM** 0.01mg/kg (0.3max) NO YES Pediatric and OB Protocols Differential (Life Threatening) Allergic reaction Asthma Aspiration Foreign body Infection Pneumonia, croup, epiglotits Congenital heart disease Medication or toxin Trauma Methylprednisolone 2mg/kg IV or IM (max dose 125mg) Magnesium Sulfate 50mg/kg IV (max 2g) in 100ml D5W over 5‐10min* P P M Contact Medical Control M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, HEENT, Skin, Neck, Heart, Lungs, Abdomen, Extremities, Neuro *Magnesium sulfate contraindicated if history of renal failure ** Epi Pen Jr. .15mg <60pounds, Epi Pen .30mg >60pounds. *** If Basic or A-EMT is needing to provide additional Albuterol, Medical Control or Paramedics should be consulted. Whenever available utilize capnography Pulse oximetry should be monitored continuously if initial saturation is <96%, or there is a decline in patient status despite normal pulse oximetry readings. Do not force a child into a position. They will protect their airway by their body position The most important component of respiratory distress is airway control Bronchiolitis is a viral infection typically affecting infants which results in wheezing which may not respond to beta‐agonists. Consider Epinephrine if patient <18 months and not responding to initial beta‐agonist treatment Croup typically affects children <2years of age. It is viral, possible fever, gradual onset, no drooling is noted. Epiglotitis typically affects children >2 years of age. It is bacterial, with fever, rapid onset, possible stridor, patient wants to sit up to keep airway open, drooling is common. Airway manipulation may worsen the condition. Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 160 Airway Emergencies: Pediatric Dyspnea All Providers General Patient Care Protocol—Pediatric Supplemental 100% oxygen For Bronchospasm: Albuterol (Proventil) 2.5 mg/3 ml via nebulizer and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer (if additional Albuterol needed, contact Medical Control or Paramedic Intercept) If severe: Hypoxia: < 93%, severe respiratory distress, anaphylactic shock, stridor Assist with patient-prescribed Epinephrine auto-injector (e.g. Epi-Pen or Epi-Pen Jr.) If foreign body obstruction is suspected refer to foreign body protocol If partial upper airway obstruction or stridor without severe respiratory distress Do nothing to upset the child Perform critical assessments only Have parent administer blow by supplemental oxygen Place patient in position of comfort Do not attempt vascular access Expedite transport If complete airway obstruction or severe respiratory distress, failure or arrest Airway/ventilatory management as needed Advanced EMT Consider IV Protocol For Bronchospasm: Albuterol (Proventil) 2.5 mg/3 ml via nebulizer and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer (if additional Albuterol needed, contact Medical Control or Paramedic Intercept) If patient shows signs of worsening respiratory distress, inadequate ventilations or respiratory failure in the setting of bronchospasm or a history of asthma Epinephrine 1:1000 at 0.01 mg/kg (max 0.3 mg) IM 161 Paramedic Full Pediatric ALS Assessment and Treatment For Bronchospasm: Albuterol (Proventil) 2.5mg/3ml via nebulizer every 15 minutes (max 3 treatments) If patient shows signs of worsening respiratory distress, inadequate ventilations or respiratory failure in the setting of bronchospasm or a history of asthma Epinephrine 1:1000 at 0.01 mg/kg (max 0.3 mg) IM May repeat epinephrine every 15 minutes X 2 additional doses (3 total) if severe symptoms present May administer at same time nebulizer is being administered Methylprednisolone (Solu-Medrol) 2 mg/kg IV or IM (Maximum individual dose 125 mg) Magnesium Sulfate 50mg/kg IV (max individual dose 2g) in 100 ml D5W over 20 minutes; contraindicated if history if renal failure Drowning/Near Drowning Ventilatory management as indicated/100% O2 as indicated Spinal Immobilization if indicated Protect from heat loss Patients may develop delayed onset respiratory symptoms Refer to appropriate protocol if cardiac arrest present Paramedic - Contact Medical Control for any additional orders or questions Nebulized Epinephrine 162 Legend EMT A‐EMT Paramedic A A P P MMedical Control M Supplemental Oxygen ADEQUATE Maintain SPO2 >93% Assess ABC’s -Respiratory Rate ‐Effort ‐Adequacy Pulse Oximetry INADEQUATE UNSUCCESSFUL If > 4 feet, Blind insertion airway device(Paramedic‐ if <4feet LMA) Only one attempt P Or Endotracheal Intubation Only one attempt LONG TRANSPORT OR NEED TO PROTECT AIRWAY OBSTRUCTION SUCCESSFUL Continue BVM SUCCESSFUL Airway Obstruction Procedure (per AHA standards) UNSUCCESSFUL P UNSUCCESSFUL Resume BVM Attempt LMA or BIAD Confirm with ETCO2 and exam UNSUCCESSFUL M P If available, consider gastric decompression Perform needle cricothyrotomy and jet insufflation M Consult Medical Control P M 2013 SUCCESSFUL Laryngoscope and Magill forceps Pediatric and OB Protocol Basic Maneuvers First ‐open airway ‐suction ‐nasal or oral airway ‐BVM M Service MD Approval:______ Pearls If Capnography is available it is expected to be used with all methods of airway placement. Document results If an effective airway is being maintained by BVM with continuous pulse oximetry values of >93, it is acceptable to continue with basic airway measures instead of using a Blind insertion device or intubation. For the purposes of this protocol a secure airway is when the patient is receiving appropriate oxygenation and ventilation An intubation attempt is defined as passing the laryngoscope blade or endotracheal tube past the teeth or inserted into the nasal passage Ventilatory rate should be 30 for neonates, 25 for toddlers, 20 for school age children, and 12 for adolescents. Maintain an ETCO2 of 30‐35. Avoid hyperventilation Quality assurance should always be completed after the use of blind insertion device or intubation Maintain C‐spine immobilization for patients with suspected spinal injury Do not assume hyperventilation is psychogenic – use oxygen, not a paper bag. Sellick’s and or BURP maneuver should be used to assist with difficult intubations Hyperventilation in deteriorating head trauma should only be done to maintain an ETCO2 of 30‐35 Gastric tube placement should be considered in all intubated patients if available It is important to secure the endotracheal tube well and consider c‐collar to better maintain ETT placement Suction all debris, secretions from the airway if necessary Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 163 Airway Emergencies: Pediatric Airway Management All Providers General Pediatric Patient Care Protocol If suspicion of trauma, maintain c-spine immobilization Suction all debris, secretions from airway Bag valve mask ventilate as needed Ventilate at a rate of 20 breaths/minute for all ages Supplemental 100% O2 Have assistant apply cardiac monitor as soon as possible Monitor end-tidal CO2 and oxygen saturation continuously Advanced EMT Consider IV Protocol Paramedic Have assistant apply cardiac monitor as soon as possible Address cardiac rhythm abnormalities per appropriate protocol Monitor end-tidal CO2 and oxygen saturation continuously Follow sequence listed below (use Broselow-Luten® tape to select appropriate equipment) 164 Following placement of ETT or LMA confirm proper placement Assess epigastric sounds, breath sounds and chest rise and fall Observe for presence of alveolar waveform on capnography Record tube depth and secure in place using a commercial tube holder (if available) Utilize head restraint device (i.e. “head blocks”) or rigid cervical collar and long spine board as needed to help secure airway in place Capnography/ETCO2 Monitoring Digital capnography (waveform) is the system standard for ETCO2 monitoring. Only in the event digital capnography is not available due to on-scene equipment failure, is continuous colorimetric monitoring of ETCO2 an acceptable alternative. Continuous ETCO2 monitoring is a MANDATORY component of invasive airway management. If ETCO2 monitoring cannot be accomplished by either of the above methods, the invasive device MUST be REMOVED, and the airway managed non-invasively. If an alveolar waveform is not present with capnography (i.e. flat line), briefly check the filter line coupling to assure it is securely in place then remove the ETT/LMA or LTA and proceed to the next step in the algorithm. Foreign Body Airway Obstruction Immediate transport is indicated If unresponsive open airway using a head tilt/chin lift (if no trauma) If < 1 year old, administer up to 5 back blows and 5 chest thrusts If 1 to 8 years, administer compressions and attempts at ventilation until the foreign body is dislodged If ventilation is unsuccessful (O2 saturations cannot be kept > 93 %) perform in the following order: Reposition airway and attempt bag valve mask assisted ventilation again If unsuccessful, establish direct view of object with laryngoscope and attempt to remove it with Magill forceps If unsuccessful, re-attempt BVM ventilation; If oxygen saturation > 93% with BVM proceed no further and expedite transport If patient cannot be ventilated/oxygenated with the above measures, Paramedics- simultaneously contact medical control and perform needle cricothyrotomy and needle jet insufflation as a last resort. Expedite transport to nearest emergency department Contact Medical Control for any additional orders or questions 165 Legend EMT A‐EMT Paramedic A A P P MMedical Control M History: Onset and location Insect sting or bite Food allergy / exposure Medication allergy / exposure New clothing, soap, detergent Past history of reactions Past medical history Medication history Differential Urticaria (rash only) Anaphylaxis (systemic effect) Shock (Vascular effect) Angioedema (drug induced) Aspiration / Airway obstruction Vasovagal event Asthma or COPD CHF Signs and Symptoms Itching or hives Coughing / wheezing Or respiratory distress Chest or throat constriction Difficulty swallowing Hypotension or shock Edema Pediatric Protocol General Approach to All Pediatric Patients Allergic Reaction suspected – history/exposure to allergen Severe Reaction Anaphylactic shock, Stridor, lip swelling Severe respiratory distress Mild Reaction Hives / Rash Only No respiratory component Moderate Reaction Dyspnea, Wheezing, Chest Tightness Epinephrine 1:1000 Auto‐Injector * 0.3mg >60lb 0.15mg <60lb A Consider IV Protocol Diphenhydramine 1mg/kg IV/IM (max 50mg) A P Worsening Consider IV Protocol A P P 0.3mg >60lb 0.15mg <60lb .01mg/kg (max 0.3mg) Pearls RECOMMENDED EXAM: Mental Status, Skin, Heart, Lungs A A Diphenhydramine 1mg/kg IV/IM (max 50mg) P Methylprednisolone 2 mg/kg IV/IM (max 125mg) P M No Improvement Repeat Epinephrine M Severe Reactions Improvement * Online Medical Control if HR >150 or History of Coronary Artery Disease **May repeat Albuterol PRN for continued wheezing – max 3 doses The shorter the onset from symptoms to contact, generally the more severe the reaction NS Bolus 20ml/kg if hypotensive P Epinephrine 1:1000 Auto‐Injector * Epinephrine 1:1000 IM* IV Protocol A Worsening A A Albuterol 2.5mg/3ml** & Ipratropium 0.5mg/2.5ml Diphenhydramine 1mg/kg IV/IM (max 50mg) P .01mg/kg (max 0.3mg) 2013 Albuterol 2.5mg/3ml** & Ipratropium 0.5mg/2.5ml P Epinephrine 1:1000 IM* A A For severe reactions: M Contact Medical Control M MP Famotidine 0.5mg/kg in 100ml D5W IV Piggyback (max dose 20mg) over 15 minutes *** Severe bradycardia, unresponsive, no obtainable blood pressure or radial pulse Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 166 P M Allergic Reactions: Pediatric All Providers General Patient Care Protocol-Pediatrics Nothing by mouth Moderate Reaction (Dyspnea, Wheezing, Chest Tightness) As above plus: Albuterol (Proventil) 2.5 mg/3 ml via nebulizer and Ipratropium Bromide 0.02% (Atrovent) 0.5 mg/2.5 ml via nebulizer May repeat Albuterol in 15 minutes for continued wheezing Severe Systemic Reaction (Anaphylactic shock, Stridor, Severe respiratory distress) As above plus: Epinephrine 1:1000 solution, 0.01 mg/kg IM (Max dose 0.3 mg) Massage injection site vigorously for 30-60 seconds Advanced EMT Consider IV Protocol Paramedic If moderate or severe symptoms, perform Full Pediatric ALS Assessment and Treatment Mild Reaction (hives) As above plus: Diphenhydramine (Benadryl) 1 mg/kg IV (maximum 50 mg) May be administered IM if no IV access available Severe Systemic Reaction (Anaphylactic shock, Stridor, Severe respiratory distress) As above plus: Methylprednisolone (Solumedrol) 2 mg/kg IV or IM (Maximum individual dose 125 mg) Contact Medical Control for any additional orders or questions All Providers –Repeat epinephrine if signs of severe reaction or shock persist after initial dose Paramedics - For severe reactions, Famotidine 0.5mg/kg in 100 ml D5W IV Piggyback (max dose 20mg) over 15 minutes. 167 Legend EMT A‐EMT Paramedic A A P P MMedical Control M General Approach to All Pediatric Patients Glucose Level 2months‐12years <70 <2months <40 Glucose Level 2months‐12years >70 <2months >40 Blood Glucose A Consider IV Protocol A A Dextrose 10% at 4ml/kg (max 250mL) IV Naloxone 0.1 mg/kg IV/IO/IN* (max dose 2.0mg) A Consider other causes: Head injury, OD/toxic ingestion, stroke, hypoxia, hypothermia A P Assess Cardiac Rhythm P NO Return to baseline? YES Refusal of transport after treatment given protocol M Consult Medical Control M Pearls RECOMMENDED EXAM: Mental Status, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro. Pay special attention to the head exam for signs of bruising or other injury. * for Intranasal administration A-EMT should administer 0.5mg per nare, total of 1mg and then proceed with additional doses as needed Be aware of AMS as presenting sign of an environmental toxin or Hazmat exposure and protect personal safety It is safer to assume hypoglycemia than hyperglycemia if doubt exists. Recheck blood glucose after Dextrose or glucagon Consider restraints if necessary for patients and/or personnel's protection per the restraint protocol Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 168 2013 Glucagon <1 year old – 0.5 mg IM >1 year old – 1.0 mg IM A Differential Head Trauma CNS (stroke, tumor, seizure, infection) Cardiac (MI, CHF) Hypothermia Infection (CNS or other) Thyroid (hyper/hypo) Shock (septic, metabolic, traumatic) Diabetes (hyper/hypo) Toxicologic or Ingestion Acidosis/Alkalosis Environmental exposure Pulmonary (hypoxia) Electrolyte abnormality Psychiatric disorder Pediatric Protocol Signs and Symptoms Decreased mental status or Lethargy Change in baseline mental status Bizarre behavior Hypoglycemia (cool/ Diaphoretic skin) Hyperglycemia (warm, dry Skin, fruity breath, kussmaul respirations, signs of dehydration Irritability History: Known Diabetic Drugs, Drug Paraphernalia Report of illicit drug use or toxic ingestion Past medical history Medications History of trauma Change in condition Changes in feeding or sleep habits Altered Mental Status: Pediatric This protocol is intended for pediatric patients with new altered mental status of unknown etiology. All Providers General Pediatric Patient Care Protocol If trauma suspected, stabilize spine Supplemental 100% oxygen Blood glucose check Neonates ( 2 months) < 40 mg/dL Child (2 months-12 years) <70 mg/dL Glucagon - <1 year old – 0.5mg or >1 year old – 1.0mg IM Advanced EMT Consider IV Protocol Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Dextrose 10% at 4 ml/kg Child (2 months-12 years) <70 mg/dL Dextrose 10% at 4ml/kg to max of 250 mL - OR - Glucagon <1 year old = 0.5mg or >1 year old = 1.0mg if IV or IO access unavailable Repeat Dextrose X1 if blood glucose remains < 70 mg/dL (<40 in a neonate) after treatment or unable to determine blood glucose and no change in mental status. If patient has continued altered mental status: Naloxone at 0.1 mg/kg (maximum individual dose 2 mg) via IV/IO If no IV access, administer IN via mucosal atomizer device (MAD), with one-half of dose administered to each nostril. Paramedic Full Pediatric ALS Assessment and Treatment Contact Medical Control for any additional orders or questions 169 A P M Legend EMT A‐EMT Paramedic Medical Control A P M (ALTE) Apparent Life-Threatening Event (ALTE) All Providers Assume the history given is accurate and reliable Determine the severity, nature and duration of the episode Obtain a medical history: Known chronic diseases History of preterm delivery Evidence of seizure activity Current or recent infections Gastroesophageal reflux Inappropriate mixture of formula Recent trauma Perform a thorough physical assessment that includes the general appearance, skin color, level of interaction with environment and evidence of trauma and blood glucose check Transport to the nearest appropriate receiving facility For patients < 1 year of age If the parent/guardian is refusing medical care and/or EMS transport, OLMC must be contacted prior to accepting a refusal. Contact Medical Control for any additional orders or questions Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow81the 76 DCEMS Protocol Change Policy and be approved by WI EMS 170 Pediatric Protocol An Apparent Life Threatening Event (ALTE), often referred to as a “near miss SIDS”, is an episode that is frightening to the observer/caregiver, and involves some combination of the following: Apnea (central or obstructive) Color change (cyanosis, pallor, erythema, plethora) Marked change in muscle tone (e.g. limpness/rigid) Choking or gagging Legend EMT A‐EMT Paramedic A A P P Medical Control M M History: Time of arrest Medical history Medications Possibility of foreign body Hypothermia Signs and Symptoms Unresponsive Cardiac Arrest CPR Pediatric and OB Protocols General Approach to all Patients Differential (Life Threatening) Respiratory failure Foreign body, secretions, infection (croup, epiglotitis) Hypovolemia (dehydration) Congenital heart disease Trauma Tension pneumothorax, cardiac tamponade, pulmonary embolism Hypothermia Toxin or medication Electrolyte abnormalities (glucose, K) acidosis Cardiac Monitor Asystole/PEA Ventricular Fibrillation/Tachycardia Give 1 shock Manual: 2J/kg May use AED if >1year of age (use pediatric AED if possible for 1‐8 years old) AED per manufacturer recommendation if <1 Immediately start CPR, do not check for pulse *Airway Protocol Check Blood Glucose and treat if appropriate A A IV Protocol AT ANY TIME Return of spontaneous circulation ‐> Treat per appropriate dysrhythmia protocol Expedite Transport A Give 5 cycles CPR Check rhythm, check pulse Shockable rhythm? P A Epinephrine IV/IO 1:10,000 at 0.01mg/kg (max1mg) Repeat every 3‐5 minutes (flush with 10‐20 ml NS) P Continue CPR 5 cycles at time Check rhythm, between cycles 2013 *Airway Protocol Check Blood Glucose and treat if appropriate IV Protocol Only check pulse between cycles of CPR and if there is a perfusing rhythm YES P Give 1 shock 4J/kg or use AED as described above Resume CPR immediately after shock Epinephrine IV/IO 1:10,000 at 0.01mg/kg Repeat every 3‐5 minutes (flush with 10‐20 ml NS) Try to Identify and Treat the Cause: P Check rhythm, check pulse Shockable rhythm? YES P Hypoxemia – assist ventilation Acidosis ‐ Volume depletion – 0.9%NaCl at 20ml/kg may repeat (max 60ml/kg) Tension pneumothorax ** Hypothermia ‐ rewarm Hypoglycemia – Dextrose 10% 4ml/kg Hypo or Hyperkalemia‐ Give 1 shock 4J/kg or use AED as described above Resume CPR immediately after shock Consider Amiodarone 5mg/kg IV/IO bolus(max dose 300mg) – Give during CPR Magnesium 50mg/kg IV/IO for suspected torsades de pointes(max 2g) P M Contact Medical Control Pearls RECOMMENDED EXAM: Mental Status In order to be successful in pediatric arrests, a cause must be identified and corrected Airway is the most important intervention. This should be accomplished immediately. Patient survival is often dependent on airway management success. *Airway Management by BVM is sufficient in the pediatric arrest patient. A single attempt at intubation can be made only if time allows. Do not prolong transport or scene time to attempt intubation. **If unilateral decreased or absent lung sounds (may see tracheal deviation away from collapsed lung) and/or evidence of hemodynamic compromise – perform pleural decompression at 2nd intercostal space, midclavicular line M Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 171 Cardiac Arrest, General: Pediatric Airway management by BVM is sufficient in the pediatric arrest patient. A single attempt at intubation can be made only if time allows. Do not prolong transport or scene time to attempt intubation. All Providers General Pediatric Patient Care Protocol Establish responsiveness If trauma suspected, stabilize spine Confirm apnea and pulselessness and administer CPR Apply AED as soon as available for 8 years old For children 1-8 years old use pediatric AED cables/electrodes if available As a last resort in a child 1-8 years old, apply AED with available cables/electrodes If utilizing Defibrillator in Manual Mode and shockable rhythm - Defibrillate at 2 J/kg (maximum of 200J) AED per manufacturer instructions for children < 1 year old Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Child (2 months-12 years) <70 mg/dL Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg Advanced EMT Consider IV Protocol Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Dextrose 10% at 4 ml/kg Child (2 months-12 years) <70 mg/dL Dextrose 10% at 4 ml/kg , maximum 250 mL - OR – Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg if IV or IO access unavailable Repeat Dextrose X1 if blood glucose remains < 70 mg/dL (<40 in a neonate) after treatment or unable to determine blood glucose and no change in mental status. 172 Paramedic Full Pediatric ALS Assessment and Treatment Determine cardiac rhythm and refer to appropriate protocol for further management actions Due to the child’s critical condition, initiate transport without delay Contact Medical Control for any additional orders or questions 173 Cardiac Asystole and PEA: Pediatric Asystole and Pulseless Electrical Activity Paramedic Follow Cardiac Arrest, General—Pediatric Protocol Confirm the presence of asystole in 2 leads Minimize any interruptions in compressions Using the most readily available route, administer (during CPR) Epinephrine 1:10,000 at 0.01 mg/kg IV/IO (max dose 1mg) Repeat Epinephrine as above every 3-5 minutes Flush medication with 10-20 ml of normal saline after each dose Treat any suspected contributing factors: If hypovolemic, administer 0.9% NaCl at 20 ml/kg IV/IO bolus, may repeat twice (to a maximum of 60 ml/kg) If hypoxic, secure airway and assist ventilation If hypothermic, rewarm If hyperkalemia suspected (history of renal failure/dialysis) Calcium Chloride (10%), 20 mg/kg IV/IO (max 1 g) Sodium Bicarbonate 1 mEq/kg IV/IO (max dose 50 mEq) If narcotic suspected, Naloxone 0.1 mg/kg (max dose 2 mg) IM/IV/IO/IN If toxic ingestion, see specific toxin Assess for tension pneumothorax Unilateral decreased or absent lung sounds (may see tracheal deviation away from collapsed lung) Evidence of hemodynamic compromise If tension pneumothorax suspected due to history or condition, perform pleural decompression at 2nd intercostal space, mid-clavicular line Contact Medical Control for any additional orders or questions 174 Cardiac Arrest: VF/VT: Pediatric Ventricular Fibrillation or Pulseless Ventricular Tachycardia Paramedic Follow Cardiac Arrest, General -Pediatric Protocol Confirm the presence of ventricular fibrillation/pulseless ventricular tachycardia Defibrillate at 2 J/kg (maximum of 200J) Continue compressions while defibrillator charges Immediately resume CPR after shock Check rhythm after 2 minutes of CPR Using the most readily available route (give drug during CPR) Epinephrine 1:10,000 at 0.01 mg/kg IV/IO Repeat Epinephrine as above every 3-5 minutes Flush medication with 10-20 ml of normal saline after each dose If shockable rhythm persists, Defibrillate at 4 J/kg Continue compressions while defibrillator charges Immediately resume CPR after shock Check rhythm after 2 minutes of CPR Amiodarone 5 mg/kg IV/IO bolus (give during CPR) (max dose 300mg) Magnesium 50 mg/kg IV/IO bolus for suspected torsades de pointes (max dose 2g ) If shockable rhythm persists, Defibrillate at 4 J/kg Continue compressions while defibrillator charges Immediately resume CPR after shock Check rhythm after 2 minutes of CPR Continue cycle Contact Medical Control for any additional orders or questions 175 Legend EMT A‐EMT Paramedic A A P P Medical Control M M Signs and Symptoms Decreased heart rate Delayed capillary refill or cyanosis Mottled, cool skin Hypotension or arrest Altered level of consciousness General Approach to all Patients Heart rate in infant <60? Pediatric Airway Protocol Poor perfusion Decreased blood pressure Respiratory insufficiency CPR YES A NO Differential Respiratory failure Foreign body Secretions Infection (croup, epiglotits) Hypovolemia (dehydration) Congenital heart disease Trauma Tension pneumothorax Hypothermia Toxin or medication Hypoglycemia Acidosis IV Protocol* A Monitor and reassess P Epinephrine 0.01mg/kg of a 1:10,000 solution IV/IO (max 1mg) repeat every 3‐5min IF no IV, Glucagon <1 year old = 0.5mg >1 year old = 1.0mg A IV Protocol D10 IV/IO Dextrose 10% at 4ml/kg (max 250 ml) May repeat x1 P 2013 If Blood glucose <40mg/dL if less than 2 months Or if Blood glucose <70mg/dL 2 months‐12 years P Atropine 0.02mg/kg IV/IO (max individual dose 0.5mg) Repeat every 3‐5 min Reassess A P Pulseless Arrest Protocol NO PULSE Continue Compromise Improved Pediatric and OB Protocols History: Past medical history Foreign body exposure Respiratory distress or arrest Apnea Possible toxic or poison exposing Congenital disease Medication (maternal or infant) If signs of severe compromise despite Epi/Atropine Consider External Cardiac Pacing** M Contact Medical Control M P Lowest setting that provides ventricular capture 100bpm Sedation if time allows and BP >90mmHg Fentanyl 1.0mcg/kg and Midazolam 0.1 mg/kg IV/IO (max Fentanyl 200mcg and Midazolam 4mg) P Pearls RECOMMENDED EXAM: Mental Status, HEENT, Skin, Heart, Lungs, Abdomen, Back, Extremities, Neuro For all drug doses not specified in protocols, please refer to Broselow-Luten tape. * If unable to secure IV in three attempts or 90 seconds, acquire IO access Infant =<1 year of age The majority of pediatric arrests are due to airway problems Most maternal medications pass through breast milk to the infant Hypoglycemia, severe dehydration and narcotic effects may produce bradycardia Pediatric patients requiring external transcutaneous pacing require the use of pads appropriate for pediatric patients per the manufacturers guidelines. Minimum Atropine dose is 0.1mg IV ** If weight >15kg, apply adult transcutaneous pacemaker, if weight <15kg use pediatric pads. P If severe cardiopulmonary compromise persists despite pacing: Dopamine infusion 5‐20mcg/kg/min IV/IO Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 176 P Cardiac Arrhythmia: Pediatric Bradycardia All Providers General Pediatric Patient Care Protocol Supplemental 100% oxygen Assist ventilation as needed with bag valve mask Look for signs of obstruction Absent breath sounds, tachypnea, intercostal retractions, stridor or drooling, choking, bradycardia or cyanosis If foreign body obstruction is suspected refer to foreign body protocol Open airway using head tilt/chin lift if no spinal trauma is suspected and modified jaw thrust if spinal trauma suspected If signs of severe cardiopulmonary compromise are present in an infant (< I year) and the heart rate remains slower than 60 beats per minute despite oxygenation and ventilation: Initiate chest compressions Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Child (2 months-12 years) <70 mg/dL Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg IM Advanced EMT Consider IV Protocol Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Dextrose 10% at 4 ml/kg Child (2 months-12 years) <70 mg/dL Dextrose 10% at 4 ml/kg , maximum of 250 mL - OR – Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg if IV or IO access unavailable Repeat Dextrose X1 if blood glucose remains < 70 mg/dL (<40 in a neonate) after treatment or unable to determine blood glucose and no change in mental status 177 Paramedic Full Pediatric ALS Assessment and Treatment If signs of severe cardiopulmonary compromise persist (use first available route) Epinephrine 0.01 mg/kg of a 1:10,000 solution IV/IO (max 1 mg) Repeat dose every 3-5 minutes until either the bradycardia or severe cardiopulmonary compromise resolves. Identify and treat possible causes of bradycardia: If hypoxia, open airway/assist breathing If hypothermic, rewarm If acutely deteriorating head injury, hyperventilate If heart bock or post heart transplant, apply transcutaneous pacer (see below) If toxin ingestion, see specific toxin If signs of severe cardiopulmonary compromise persist despite Epinephrine and above measures Atropine at 0.02 mg/kg IV/IO Minimum dose is 0.1 mg Maximum individual dose is 0.5 mg May repeat once after 3-5 minutes If signs of severe cardiopulmonary compromise persist despite Epinephrine/Atropine apply transcutaneous pacemaker If weight 15 kg, apply adult transcutaneous pacemaker pads If < 15 kg use pediatric pads (small/medium electrodes) in the standard configuration for adult size pacer pads Use the lowest setting that provides ventricular capture (pulse) Set rate to 100 beats per minute Sedation if patient condition and time allows (hold if SBP<90mmHg): Fentanyl 1.0mcg/kg and Midazolam 0.1mg/kg IV/IO Titrate to Max dose Fentanyl 200mcg and Midazolam 4mg. If severe cardiopulmonary compromise persists despite pacing: Dopamine infusion at 5-20 mcg/kg/min IV/IO Contact Medical Control for any additional orders or questions 178 Legend EMT A‐EMT Paramedic Wide Complex Tachycardia with Pulse - Pediatric A A P P MMedical Control M General Approach to all Patients Pediatric and OB Protocols Differential (Life Threatening) Heart Disease (congenital) Hypo/hyper thermia Hypovolemia or anemia Electrolyte imbalance Anxiety / pain/ emotional stress Fever / infection / sepsis Hypoxia Hypoglycemia Mediation/toxin/drugs Pulmonary embolus Trauma Tension pneumothorax Signs and Symptoms Heart Rate Child >180bpm Infant >220bpm Pale or Cyanosis Diaphoresis Tachypnea Vomiting Hypotension Altered LOC Pulmonary congestion syncope History: Past medical history Medications or Toxic Ingestion (Aminophyline, diet pills, thyroid supplements, decongestants, digoxin) Drugs (nicotine, cocaine) Congenital heart disease Respiratory distress Syncope or near syncope Blood Glucose Measurement and Treat if appropriate Continuous Cardiac Monitor P P Attempt to identify cause – narrow QRS duration <0.08 sec STABLE A IV Protocol A I P Amiodarone 5mg/kg IV over 10 minutes UNSTABLE Or No IV access P Synchronized cardioversion at 0.5‐1.0 J/kg (max individual dose 150mg) P P May repeat Synchronized cardioversion at 1.0‐2.0 J/kg ** If rhythm changes go to appropriate protocol M Contact Medical Control 2013 If time allows: Consider sedation – Midazolam 0.1mg/kg IV/IO (max dose 2mg) If Torsade de Pointes is suspected:: P Magnesium Sulfate 50mg/kg in 100ml D5W IV/IO over 10 minutes (max individual dose 2mg) M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro **Max dose 360J Carefully evaluate the rhythm to distinguish sinus tachycardia, supraventricular tachycardia, and ventricular tachycardia Separating the child from the caregiver may worsen the child's clinical condition Monitor for respiratory depression and hypotension associated if diazepam or midazolam is used. Continuous pulse oximety is required for all SVT patients if available Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention As a rule of thumb, the max sinus tachycardia rate is 220 minus the patients age in years. Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 179 P Narrow Complex Tachycardia with Pulse (SVT)- Pediatric Legend EMT A‐EMT Paramedic A A P P MMedical Control M General Approach to all Patients Pediatric and OB Protocols Differential (Life Threatening) Heart Disease (congenital) Hypo/hyper thermia Hypovolemia or anemia Electrolyte imbalance Anxiety / pain/ emotional stress Fever / infection / sepsis Hypoxia Hypoglycemia Mediation/toxin/drugs Pulmonary embolus Trauma Tension pneumothorax Signs and Symptoms Heart Rate Child >180bpm Infant >220bpm Pale or Cyanosis Diaphoresis Tachypnea Vomiting Hypotension Altered LOC Pulmonary congestion syncope History: Past medical history Medications or Toxic Ingestion (Aminophyline, diet pills, thyroid supplements, decongestants, digoxin) Drugs (nicotine, cocaine) Congenital heart disease Respiratory distress Syncope or near syncope Continuous Cardiac Monitor Paramedics: Attempt to identify cause – narrow QRS duration <0.08 sec A IV Protocol A UNSTABLE – Severe Cardiopulmonary Compromise STABLE If time and condition allows attempt vagal maneuvers Expedite Transport If vascular access ready: P Adenosine 0.1mg/kg IV/IO (max individual dose P 2013 6mg) May repeat twice at 0.2mg/kg if needed (max individual dose 12mg) UNSUCCESSFUL and Severe Cardiopulmonary Compromise Synchronized cardioversion at 0.5‐1.0 J/kg P P sedation if time permits Midazolam 0.1mg/kg IV/IO (max 2.0mg) May repeat Synchronized cardioversion at 1.0‐2.0 J/kg ** If rhythm changes go to appropriate protocol M Contact Medical Control M Service MD Approval:______ Pearls RECOMMENDED EXAM: Mental Status, Skin, Neck, Heart, Lungs, Abdomen, Back, Extremities, Neuro **Max dose 360J Carefully evaluate the rhythm to distinguish sinus tachycardia, supraventricular tachycardia, and ventricular tachycardia Separating the child from the caregiver may worsen the child's clinical condition Monitor for respiratory depression and hypotension associated if diazepam or midazolam is used. Continuous pulse oximety is required for all SVT patients if available Document all rhythm changes with monitor strips and obtain monitor strips with each therapeutic intervention As a rule of thumb, the max sinus tachycardia rate is 220‐the patients age in years. Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 180 Cardiac Arrhythmia: Pediatric Tachycardia Note: Infants with heart rates < 220 and children with heart rates < 180 typically will respond when the precipitating cause is treated (e.g. fever, dehydration) All Providers General Pediatric Patient Care Protocol If trauma suspected, stabilize spine Supplemental 100% oxygen Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Child (2 months-12 years) <70 mg/dL Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg IM Advanced EMT Consider IV Protocol Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Dextrose 10% at 4 ml/kg Child (2 months-12 years) <70 mg/dL Dextrose 10% at 4 ml/kg , maximum of 250 mL - OR - Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg if IV or IO access unavailable Repeat Dextrose X1 if blood glucose remains < 70 mg/dL (< 40 in a neonate) after treatment or unable to determine blood glucose and no change in mental status Paramedic Full Pediatric ALS Assessment and Treatment Sinus Tachycardia Identify and treat possible causes 181 Supraventricular tachycardia with severe cardiopulmonary compromise If time and patient condition permits, attempt vagal maneuvers If vascular access is available, Adenosine (Adenocard) 0.1 mg/kg (Maximum individual dose is 6 mg) via rapid IV/IO bolus (IV access in the antecubital space is preferred) Repeat Adenosine (Adenocard) twice at 0.2 mg/kg if needed (maximum individual dose is 12mg) If Adenosine is unsuccessful and patient still has severe cardiopulmonary compromise: Synchronized Cardioversion at 0.5-1 J/kg Consider sedation if time permits Midazolam 0.1 mg/kg IV/IO (max dose 2 mg) May repeat synchronized cardioversion at double the initial energy (maximal individual dose 360 J) Ventricular Tachycardia with a pulse If vascular access is readily available OR the patient is stable: Amiodarone 5 mg/kg/IV over 10 minutes, (Max individual dose is 150 mg) If vascular access is not readily available AND the patient is unstable: Synchronized Cardioversion at 0.5-1.0 J/kg Consider sedation if time permits: Midazolam 0.1 mg/kg IV/IO (max dose 2 mg) May repeat at double the initial energy (maximal individual dose 360 J) If Torsade de Pointes is suspected: Magnesium Sulfate 50mg/kg in 100 ml D5W IV/IO over 10 minutes (max dose 2 g) Contact Medical Control for any additional orders or questions Paramedic - Failed response to 2 attempts at cardioversion 182 Legend EMT A‐EMT Paramedic A A P P MMedical Control M General Approach to all patients Assign Provider to care for mother Twin Gestation? Call for additional help YES NO Suction mouth then nose – activate ALS YES NO Dry infant/keep warm/stimulate Bulb syringe suction mouth/nose P Childbirth Procedure if appropriate Note APGAR score Respirations 60-100bpm ------------------ <60 bpm Assess Respiratory Drive Crying Good Tone Immediate CPR per AHA Labored Breathing Persistent Cyanosis Improved Monitor Reassess 5 Minute APGAR Support with BVM At 40‐60 breaths/min with 100% oxygen Peds Airway Protocol A Consider IV Protocol Clear airway SpO₂, supplemental O₂ 2013 Give report to receiving hospital P Repeat until free of meconium Heart Rate >100bpm Visualize hypopharynx and perform deep suction Pediatric and OB Protocols Thick meconium in amniotic fluid? Treat per appropriate medical protocol Support with BVM At 40‐60 breaths/ min with 100% oxygen Improved A No Change Reassess Heart Rate A Consider IV Protocol Glucose Check and treat if appropriate A A P Consider Peds Airway Naloxone** 0.01mg/kg Dextrose 10% at 4ml/kg**** Epinephrine 0.01mg/kg of a 1:10,000 solution*** A P M Contact Medical Control Rapid Transport‐ OB receiving facility M Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Neck, Chest, Heart, Abdomen, Extremities, Neuro CPR in infants is 120 compressions/minute with a 3:1 compressions to ventilation ratio Service MD Approval:______ It is extremely important to keep infant warm * if no IV access after 3 attempts, or within 90 seconds – obtain IO access **if respiratory depression in a newborn of a mother who received narcotics within 4 hours of delivery, use caution in infants born to opiate addicted mothers.(Naloxone effective but may precipitate seizures) ***May repeat same dose of Epinephrine every 3‐5 minutes if no response. ****Consider hypoglycemia in infant and treat if glucose <40mg/dL ‐ D10=D50 diluted (1ml of D50 with 4ml NS). Document 1 and 5 minute APGARS in PCR Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 183 Newborn Resuscitation All Providers Note gestational age, and if twin gestation is known Assess for presence of meconium Assess breathing or presence of crying Assess muscle tone Assess color Provide warmth Open airway and suction with bulb syringe as soon as infant is delivered. Suction mouth first then nasopharynx Dry, stimulate and reposition Administer supplemental blow-by oxygen Evaluate respirations, heart rate and color If apnea or HR < 100, provide positive pressure ventilation using BVM and 100% oxygen If HR remain < 60, begin chest compressions Note APGAR scores at 1 and 5 minutes after birth and then sequentially every 5 minutes until VS have stabilized Paramedic If the fluid contains meconium and the newborn has absent or depressed respirations, decreased muscle tone or heart rate < 100 bpm Suction any visible meconium from the airway – refer to Childbirth Complication Procedure as appropriate. After suctioning, apply positive pressure ventilation using a BVM and 100% oxygen If apnea, or HR < 100, provide positive pressure ventilations with 100% oxygen If HR 60-100, and no increase with positive pressure ventilations with 100% oxygen Continue assisted ventilations Begin chest compressions Naloxone (Narcan) 0.01 mg/kg, IV/IO if respiratory depression in a newborn of a mother who received narcotics within 4 hours of delivery, use caution in infants born to opiate addicted mothers May Repeat Naloxone (Narcan) dose as needed to a max of 0.03 mg/kg 184 Check blood glucose and treat glucose < 40 mg/dL Dextrose 10% at 4 ml/kg If HR < 60 begin chest compressions IV 0.9% NaCl KVO or lock If no IV access obtained after 3 attempts, or within 90 seconds, obtain IO access Naloxone (Narcan) 0.01 mg/kg, IV/IO if respiratory depression in a newborn of a mother who received narcotics within 4 hours of delivery, use caution in infants born to opiate addicted mothers May Repeat Naloxone (Narcan) dose as needed to a max of 0.03 mg/kg Epinephrine 0.01 mg/kg of a 1:10,000 solution Repeat Epinephrine (same dose) every 3 to 5 minutes if no response Check blood glucose and treat glucose < 40 mg/dL Dextrose 10% at 4 ml/kg Rapid transport Contact Medical Control for any additional orders or questions 185 A P M Legend EMT A‐EMT Paramedic Medical Control A P M For any overdose or poisoning, contact should be made with the Regional Poison Control Center (RPCC), 1-800-222-1222. Whenever possible, determine the agent(s) involved, the time of the ingestion/exposure and the amount ingested. Bring empty pill bottles, etc., to the receiving facility. General Patient Care Protocol-Pediatric Nothing by mouth Advanced EMT Consider IV Protocol If respiratory depression is present and a narcotic overdose is suspected: o Naloxone (Narcan) 0.1 mg/kg IV/IO/IM or IN via MAD (max. dose is 2 mg) Pediatric Protocol All Providers Paramedic If any symptoms present, perform Full Pediatric ALS Assessment and Treatment Treatment for specific toxic exposures is indicated only when patients are clearly symptomatic. In the absence of significant symptoms, monitor closely and expedite transport. Organophosphates: Dyspnea, bronchorrhea, lacrimation, vomiting/diarrhea, weakness, paralysis, seizures: Atropine 0.02 mg/kg IV/IO (minimum dose 0.1 mg), repeat every 2 minutes if needed X 3 doses If seizures present, see Pediatric Seizure Protocol Tri-cyclic Antidepressant: Hypotension, arrhythmias, wide QRS complex (0.12 sec): Sodium Bicarbonate 1 mEq/kg IV/IO May be repeated in 10 minutes Beta Blocker overdose: Bradycardia, hypotension, heart blocks: Atropine 0.02 mg/kg IV/IO (minimum dose 0.1 mg, maximum individual dose 0.5 mg) for bradycardia If the symptoms persist, Glucagon 0.1 mg/kg IV/IO (Maximum dose 1 mg) Pediatric Protocol Service MD Approval:______ Any local EMS Agency changes to this document must follow81the 76 DCEMS Protocol Change Policy and be approved by WI EMS 186 A P M Legend EMT A‐EMT Paramedic Medical Control A P M Calcium Channel Blocker overdose: Calcium Chloride 20 mg/kg slow IV/IO (maximum dose 1g) Pediatric Protocol Dystonic Reactions: Acute uncontrollable muscle contractions Diphenhydramine (Benadryl) 1 mg/kg IV or IM (maximum dose 25 mg) Insulin Overdose: Hypoglycemia or unknown blood glucose and altered mental status: Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Dextrose 10% at 4 ml/kg Child (2 months-12 years) <70 mg/dL Dextrose 10% at 4 ml/kg , maximum of 250 mL - OR – Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg IM if IV or IO access unavailable Repeat Dextrose X1 if blood glucose remains < 70 mg/dL (<40 in a neonate) after treatment or unable to determine blood glucose and no change in mental status Contact Medical Control for any additional orders or questions Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow81the 76 DCEMS Protocol Change Policy and be approved by WI EMS 187 Legend EMT A‐EMT Paramedic A A P P MMedical Control M History: Age Location Duration Severity (1‐10) If child use Wong‐Baker faces scale Past medical history Medications Drug allergies Differential Per the specific protocol Musculoskeletal Visceral (abdominal) Cardiac Pleural / Respiratory Neurogenic Renal (colic) Signs and Symptoms Severity (pain scale) Quality (sharp, dull, etc) Radiation Relation to movement, respiration Increased with palpation Pediatric Protocol General Approach to All Pediatric Patients Patient care according to PROTOCOL Based on specific complaint Pain Severity >6 out of 10 Or Indication for IV/IM Medication A P Consider IV Protocol 2013 Pulse Oximetry and EndTidal CO₂ A Morphine Sulfate 0.1mg/kg slow IV/IO, may repeat in 10 min x1 OR Fentanyl 1.5mcg/kg IN half volume per nare (max 100mcg) may repeat one half (½) the original dose after 10 min. if needed P After each dose: Reassess pain level Respiratory adequacy Vital signs (SPO2, EndTidal) Service MD Approval:______ M Contact Medical Control for additional orders or questions Pearls RECOMMENDED EXAM: Mental Status, Area of pain, Neuro Analgesic agents may be administered under standing orders for patients experiencing moderate / severe pain (typically >6/10) Common Complaints: trauma/isolated extremity injury, Burns (without airway, breathing or circulation compromise), sickle crisis Vitals and pain scale should be documented before and after every medication dose. M Fentanyl Concentration (50mcg/mL), 0.1ml=5mcg Weight Dose Volume of 50 mcg/mL (kg) (mcg) add 0.1 ml for dead space 3‐5 10 0.2+0.1=0.3mL 6‐10 20 0.4+0.1=0.5mL 11‐15 30 0.6+0.1=0.7mL 16‐20 40 0.8+0.1=0.9mL 21‐25 50 1.0+0.1=1.1mL 26‐30 60 1.2+0.1=1.3mL 31‐35 70 1.4+0.1=1.5mL 36‐40 80 1.6+0.1=1.7mL 41‐45 90 1.8+0.1=1.9mL 2.0*mL (admin dose in two separate administrations 10 min apart) 46‐50 100 Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 188 Pain Management: Pediatric All Providers General Pediatric Patient Care Protocol Assess baseline pain level (0-10 scale: 0=no pain; 10=worst pain) Advanced EMT Consider IV Protocol Paramedic Full ALS Pediatric Assessment and Treatment if administering narcotics Analgesic agents may be administered under standing orders for patients experiencing moderate/severe pain (≥ 6/10) Common complaints: Isolated extremity injury Burns (without airway, breathing, or circulation compromise) Sickle crisis Agents for pain control: Both are contraindicated if hypotensive: Morphine Sulfate 0.1 mg/kg IV/IO May repeat every 10 min x 1 OR Fentanyl 1.5 mcg/kg IN via MAD with one-half of the volume administered to each nare (max. individual dose 100 mcg) May repeat one-half (½) the original dose after 10 minutes if needed. 189 DOSING: Fentanyl Concentration (50 mcg/mL), 0.1 ml=5 mcg Weight (kg) 3-5 6-10 11-15 16-20 21-25 26-30 31-35 36-40 41-45 46-50 Dose (mcg) 10 20 30 40 50 60 70 80 90 100 Volume of 50 mcg/mL + 0.1 ml for dead space 0.2+0.1=0.3 mL 0.4+0.1=0.5 mL 0.6+0.1=0.7 mL 0.8+0.1=0.9 mL 1.0+0.1=1.1 mL 1.2+0.1=1.3 mL 1.4+0.1=1.5 mL 1.6+0.1=1.7 mL 1.8+0.1=1.9 mL 2.0* mL * administer dose in two (2) separate administrations 10 minutes apart After each drug dosage administration: Reassess the patient’s pain level Note adequacy of ventilation and perfusion Assess vital signs Continuously monitor oxygen saturation and end tidal CO2 Contact Medical Control for any additional orders or questions 190 Legend EMT A‐EMT Paramedic A A P P MMedical Control M History: Fever Prior history of seizures Seizure medications Reported seizure activity History of recent head trauma Congenital abnormality Signs and Symptoms Observed Seizure activity Altered mental status Hot, dry skin or elevated body temperature General Approach to all Patients Pediatric Airway Protocol If <40 (<2 months of age) or <70 (2 months to 12 years of age) Blood Glucose Altered Level of Consciousness A P IV Protocol ACTIVELY SEIZING A Assess Patient If no IV, Glucagon <1 year old.1mg/kg – 0.5 mg IM Glucagon IM Evidence of Trauma? P >1 year old – 1.0 mg IM Pediatric Head Injury Protocol A Obtain Temperature IV Protocol – D10 4ml/kg (max 250ml) A FEBRILE I Seizure recurs Blood Glucose Cooling measures If <40 (<2 months of age) or <70 (2 months to 12 years of age) Glucose Level 2months‐12years >70 <2months >40 If no IV, Glucagon Service MD Approval:______ <1 year old – 0.5 mg IM >1 year old – 1.0 mg IM A D10 4ml/kg (max 250ml) A M Contact Medical Control Pearls RECOMMENDED EXAM: Mental Status, HEENT, Skin, Neck, Heart, Lungs, Extremities, Neuro Addressing the ABCs and verifying blood glucose is more important than stopping the seizure Avoiding hypoxemia is extremely important Status Epilepticus is defined as two or more successive seizures without a period of consciousness or recovery. This is a true emergency requiring rapid airway control, treatment, and transport Grand mal seizures (generalized) are associated with loss of consciousness, incontinences, and tongue trauma Focal seizures (petit mal) effect only a part of the body and do not usually result in a loss of consciousness Jacksonian seizures are seizures which start as a focal seizure and become generalized Be prepared to assist ventilations especially if a benzodiazepine is used. If evidence or suspicion of trauma, spine should be immobilized IN an infant, a seizure may be the only evidence of a closed head injury M Patient Prescribed Rectal Diazepam (Diastat) if available: DIASTAT 2-5 Years (0.5 mg/kg) Dose Weight (kg) (lb) (mg) 6‐11 13‐25 5 12‐22 26‐49 10 23‐33 50‐74 15 34‐44 75‐98 20 DIASTAT 6-11 + Years (0.3 mg/kg) Dose Weight (kg) (lb) (mg) 10‐18 22‐41 5 19‐37 42‐82 10 38‐55 83‐122 15 56‐74 123‐164 20 Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 191 2013 Lorazepam 0.05mg/kg slow IV/IO (max 2mg) Or Midazolam 0.2mg/kg IV/IO/IN (max 2mg) May repeat if seizure not controlled or recurs Or Patient prescribed Diazepam Pediatric and OB Protocols Differential (Life Threatening) Fever Infection Head trauma Medication or Toxin Hypoxia or respiratory failure Hypoglycemia Metabolic abnormality / acidosis Tumor Seizure: Pediatric All Providers Pediatric General Patient Care Protocol Supplemental 100% oxygen Nasal cannula is sufficient if no active seizures and no respiratory signs of symptoms Protect patient from injury Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Child (2 months-12 years) <70 mg/dL Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg IM Advanced EMT Consider IV Protocol Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Dextrose 10% at 4 ml/kg Child (2 months-12 years) <70 mg/dL Dextrose 10% at 4 ml/kg , maximum of 250 mL OR Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg IM if IV or IO access unavailable Repeat Dextrose X1 if blood glucose remains < 70 mg/dL (<40 in a neonate) after treatment or unable to determine blood glucose and no change in mental status. Paramedic Full Pediatric ALS Assessment and Treatment Determine blood glucose and treat: Neonates ( 2 months) < 40 mg/dL Dextrose 10% at 4 ml/kg Child (2 months-12 years) <70 mg/dL Dextrose 10% at 4 ml/kg , maximum of 250 mL OR 192 Glucagon - <1 year old = 0.5mg or >1 year old = 1.0mg IM if IV or IO access unavailable Repeat Dextrose X1 if blood glucose remains < 70 mg/dL (<40 in a neonate) after treatment or unable to determine blood glucose and no change in mental status. For active seizures choose one of the following options: Lorazepam (Ativan) 0.05 mg/kg slow IV/IO via (max. individual dose 2 mg) OR Midazolam (Versed) 0.2 mg/kg IV/IO/IN via MAD (Max individual dose 2 mg) OR Patient-prescribed Diazepam rectal gel (Diastat) if available 2-5 Years (0.5 mg/kg) Weight Dose (kg) (lb) (mg) 6-11 13-25 5 12-22 26-49 10 23-33 50-74 15 34-44 75-98 20 6-11 + Years (0.3 mg/kg) Weight Dose (kg) (lb) (mg) 10-18 22-41 5 19-37 42-82 10 38-55 83-122 15 56-74 123-164 20 For seizure not controlled by the above, or if the seizure recurs after initial control, choose one of the following: Lorazepam (Ativan) 0.05 mg/kg slow IV (max individual dose 2 mg) OR Midazolam (Versed) 0.2 mg/kg IV/IO/IN via MAD (max individual dose 2mg) Contact Medical Control for any additional orders or questions 193 Legend EMT A‐EMT Paramedic A A P P Medical Control M M Signs and Symptoms Pain, swelling Deformity, lesions, bleeding Altered mental status Unconscious Hypotension or shock Arrest General Approach to all Pediatric Patients Pediatric = Anyone <18 years of age Differential (Life Threatening) Chest Tension pneumo, flail chest, pericardial tamponade, open chest wound, hemothorax Intra‐abdominal bleeding Pelvis / femur fracture Spine fracture / cord injury Head injury (see head trauma) Extremity fracture / dislocation HEENT (airway obstruction) Hypothermia Presentation or Mechanism consistent with trauma? Assess ABC’s INADEQUATE YES Go to appropriate medical protocol ADEQUATE Pediatric Airway Protocol Spinal Immobilization Protocol Obvious Bleeding? YES Disability and GCS (document) Pressure Point Complete head to toe exam Vital Signs Hypotension, Tachy Hypoxia IV Protocol NS Bolus 20ml/kg NO 2013 Direct Pressure A NO A Pediatric and OB Protocols History: Time and Mechanism of injury Height of any fall Damage to structure or vehicle Location in structure or vehicle Others injured or dead Speed and details of MVS Restraints/protective equipment Car Seat, Helmet, Pads Ejection Past medication history Medications Normal for Age Notify receiving hospital Tension Pneumothorax?* High suspicion severe injury Facility/provider discretion NO Pain Management Protocol YES P Decompression P M Contact Medical Control M Rapid Transport to appropriate destination Limit scene time to 10 minutes Pearls RECOMMENDED EXAM: Mental Status, Skin, HEENT, Heart, Lungs, Abdomen, Extremities, Back, Neuro *Pleural Decompression for tension pneumo ONLY if all 3 criteria present: 1) Severe respiratory distress with hypoxia 2) Unilateral decreased or absent lung sounds (may see tracheal deviation away from collapsed lung field) 3) Evidence of hemodynamic compromise (shock, hypotension, altered mental status) If indicated, pleural decompression at 2nd intercostal space, midclavicular line Mechanism is the most reliable indicator of serious injury. Examine all restraints/protective equipment for damage. In prolonged extrications or serious trauma consider air transport Do not overlook the possibility of child abuse Scene times should not be delayed for procedures. These should be performed enroute when possible Bag valve mask is an acceptable method of managing the airway if pulse oximetry can be maintained about 93% Disability – assessment of paralysis, weakness, abnormal sensation, etc. Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 194 Trauma: Pediatric For major trauma criteria, a pediatric patient is anyone < 18 years of age All Providers Pediatric Patient Care Protocol Stabilize spine Use modified jaw thrust if airway obstructed Supplemental 100% oxygen Control hemorrhage using direct pressure or pressure dressing Perform head-to-toe survey to identify injuries Splint obvious fractures of long bones Attempt to preserve body temperature Advanced EMT Consider IV Protocol Paramedic If moderate or severe injuries present, perform Full Pediatric ALS Assessment and Treatment Assess for Pediatric Trauma Triage Criteria and initiate transport to Pediatric Trauma Center Assess for Tension Pneumothorax Severe respiratory distress with hypoxia Unilateral decreased or absent lung sounds (may see tracheal deviation away from collapsed lung field) Evidence of hemodynamic compromise (shock, hypotension, altered mental status) Pleural decompression for tension pneumothorax should only be performed when all 3 of the above criteria are present! If indicated, perform pleural decompression at 2nd intercostal space, midclavicular line Initiate transport to an appropriate trauma facility within 10 minutes of arrival on the scene, unless extenuating circumstances (extrication) Perform procedures, history and detailed physical examination en route to the hospital If moderate to severe pain, treat per Pediatric Pain Management Protocol Reassess frequently Contact Medical Control for any additional orders or questions 195 Legend EMT A‐EMT Paramedic A A P P MMedical Control M History: Type of exposure (heat, gas, chemical) Inhalation injury Time of injury Past medical history and medications Other trauma Loss of consciousness Tetanus/immunization status Signs and Symptoms Burns, pain, swelling Dizziness Loss of consciousness Hypotension/shock Airway compromise/distress Singed facial or nasal hair Hoarseness/wheezing Differential Superficial (1st degree) red and painful Partial thickness (2nd degree) blistering Full thickness (3rd degree) painless/charred or leathery skin Thermal Chemical Electrical Radiation General Approach to All Pediatric Patients Pediatric and OB Protocols Transport to Burn Center 2nd degree burns greater than 10% total body surface area or those on hands, feet, face or groin 3rd degree burns Electrical burns (spinal immobilization if high voltage, monitor for cardiac arrhythmias, initiate fluid resuscitation immediately Chemical burns (remove clothing, brush away dry powder before irrigating, flush with copious warm water on scene and continue irrigation enroute, eyes: remove contacts and irrigate continuously with NS for at least 30 minutes, avoid hypothermia ABC’s *Airway Protocol If inhalation injury – place patient on 100% O2, monitor ETCO2 continuously Remove or cool heat source if present IV Protocol Remove all clothing, contact lenses, and jewelry (especially rings) Maintain core temperature Cover burn with plastic wrap, plastic chucks, or clean dry dressings A Large bore in unburned skin if possible If burn is >20%TBSA 2nd/3rd degree burns – Less than 5 years old, start 0.9 %Normal Saline at 125ml/hr 6‐13 years old, start 0.9% Normal Saline at 250ml/hr 14 years and older, start 0.9% Normal Saline at 500ml/hr Specific fluid resuscitation based on TBSA and weight will occur at initial hospital or Burn Center Pearls RECOMMENDED EXAM: Mental Status, HEENT, Skin, Neck, Lung, Heart, Abdomen, Extremities, Back, and Neuro Burn patients are trauma patients, evaluate for multisystem trauma Assure whatever has caused the burn, is no longer contacting the injury (stop the burning process) Early intubation is required when the patient experiences significant inhalation injuries Potential CO exposure should be treated with 100% oxygen. Circumferential burns to extremities are dangerous due to potential vascular compromise secondary to soft tissue swelling Burn patients are prone to hypothermia – never apply ice or cool burns, must maintain normal body temperature Evaluate the possibility of child abuse with children and burn injuries *Signs and symptoms of inhalation injury: carbonaceous sputum, facial burns or edema, hoarseness, singed nasal hairs, agitation, anxiety, cyanosis, stupor or other signs of hypoxia A Consider Pain Management Protocol M Contact Medical Control M Service MD Approval:______ Pediatric Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 196 Trauma: Pediatric Burns All Providers General Pediatric Patient Care Protocol o Stay focused on ABC’s, don’t get side tracked by burn. o DON’T BE A SECOND VICTIM! Remove or cool heat source if present (e.g. clothing, tar) o Cool burns with room temperature water for 3-5 minutes only except for tar burns which will take an extended time to cool. o NEVER COOL WITH ICE! The goal is to bring burns to room temperature, not cold. Remove all clothing, contacts, and jewelry, especially rings Keep patient warm and dry with sheets and blankets. Cover burns with plastic wrap, plastic chucks, clean, dry dressings, or aluminum foil. 2nd Degree burns – greater than 10% of total body surface area or those on hands, feet, face, or groin 3rd Degree burns Electrical burns - Spinal immobilization if high voltage electrical injury - Monitor for cardiac arrhythmias - Initiate fluid resuscitation immediately Chemical burns - Remove clothing - If dry powder is present, brush away before irrigating - Flush with copious warm water on scene and continue irrigation enroute to UW Hospital - Chemical injuries to eyes are an EMERGENCY. Remove contacts and irrigate continuously with normal saline – DO NOT STOP. Assess for Pediatric Trauma Triage Criteria and initiate transport to Pediatric Trauma Center if appropriate Advanced EMT Consider IV Protocol o Place a large bore peripheral IV in unburned skin if possible. o If TBSA % greater than 30%, place 2 large bore peripheral IV’s. o If greater than 20% TBSA of 2nd and 3rd degree burns, initiate volume resuscitation with 0.9% Normal Saline Less than 5 years old, start 0.9 %Normal Saline at 125ml/hr 6-13 years old, start 0.9% Normal Saline at 250ml/hr 14 years and older, start 0.9% Normal Saline at 500ml/hr Specific fluid resuscitation based on TBSA and weight will occur at initial hospital or Burn Center 197 Paramedic Perform Full Pediatric ALS Assessment and Treatment If not already done, consider IV Protocol o Place a large bore peripheral IV in unburned skin if possible. If TBSA % greater than 30%, place 2 large bore peripheral IV’s. Observe for signs of impending loss of airway; refer to the Airway Management Protocol as needed - Hypoxia - Poor ventilatory effort - Altered mental status or decreased level of consciousness - Inability to maintain patent airway - Signs or symptoms of inhalation injury Carbonaceous sputum Extensive facial burns Hoarseness Singed nasal hairs Agitation, anxiety, cyanosis, stupor, or other signs of hypoxia If moderate to severe pain, see Pain Management Protocol Estimate Total Body Surface Area (TBSA) - Rule of Nines Age Body Part A = whole head B = thigh C = lower leg 0 yr 19 5½ 5 1 yr 17 6½ 5 5 yr 13 8 5½ 10 yr 11 8½ 6 15 yr 9 9 6½ - If greater than 20% TBSA of 2nd and 3rd degree burns, initiate volume resuscitation with 0.9% Normal Saline Less than 5 years old, start 0.9 %Normal Saline at 125ml/hr 198 6-13 years old, start 0.9% Normal Saline at 250ml/hr 14 years and older, start 0.9% Normal Saline at 500ml/hr Specific fluid resuscitation based on TBSA and weight will occur at initial hospital or Burn Center Contact Medical Control for any additional orders or questions 199 Legend EMT A‐EMT Paramedic A A P P MMedical Control M Signs and Symptoms Pain, swelling, bleeding Altered mental status Unconscious Respiratory distress / failure Vomiting Major traumatic mechanism of injury seizure Differential Skull fracture Brain injury (concussion, contusion, hemorrhage or laceration) Epidural hematoma Subdural hematoma Subarachnoid hemorrhage Spinal injury Abuse General Approach to all Pediatric Patients Pediatric Trauma Protocol Isolated Head Trauma? Other injuries suspected YES Spinal Immobilization Protocol if normotensive or hypertensive elevate backboard 15‐30° A A IV Protocol Check Blood Glucose and treat if appropriate Assess and Record GCS Able to manage airway with basic maneuvers Basic Airway maneuvers (O₂, NRB, BVM) As needed to maintain O₂ sat >93% Unable to manage airway With basic maneuvers Secure Airway per Pediatric Airway Protocol No signs of herniation Continuous EtCO₂ If severely agitated/combative* consider Lorazepam 0.05mg/kg IV/IO (max 2.0mg) P Monitor for signs of herniation: ‐Abrupt increase in BP ‐Abrupt decrease in HR ‐Acute unilateral dilated and non‐reactive pupil ‐Abrupt deterioration in mental status ‐Abrupt onset of motor posturing P P Pearls RECOMMENDED EXAM: Mental Status, HEENT, Heart, Lungs, Abdomen, Back, Extremities, Neuro * unable to deescalate by any other means, then consider Lorazepam If GCS <12, consider air/rapid transport and if GCS <8 airway control should be anticipated Increased intracranial pressure (ICP) may cause hypertension and bradycardia (Cushing’s Response) Hypotension usually indicates injury or shock unrelated to the head injury The most important item to monitor and document is a change in level of consciousness. Concussions are periods of confusion or LOC associated with trauma which may have resolved by the time EMS arrives. Any prolonged confusion or mental status abnormality which does not return to normal within 15 minutes or any document loss of consciousness should be evaluated by a physician ASAP. 2013 Transport to appropriate emergency department Pediatric and OB Protocols History: Time of injury Mechanism (blunt vs. penetrating) Loss of consciousness Bleeding Past medical history Medications Evidence of multi‐trauma P Signs of herniation Hyperventilate: P <1 year – 35/min, >1 year – 25/min Target EtCO₂ 30‐35 P Contact Medical Control simultaneously M Contact Medical Control for additional orders M Service MD Approval:______ Protocol Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 200 Trauma: Pediatric Head Injuries All Providers Supplemental oxygen Stabilize spine Check blood glucose Apply physical restraints if needed to ensure patient/crew safety. Adhere to procedure on Physical Restraint of Agitated Patients when this process is deemed necessary If normotensive or hypertensive Elevate head of backboard 15-30 Paramedic Full Pediatric ALS Assessment and Treatment Advanced airway/ventilatory management as needed Note: Airway interventions can be detrimental to patients with head injury by raising intercranial pressure, worsening hypoxia (and secondary brain injury) and increasing risk of aspiration. Whenever possible these patients should be managed in the least invasive manner to maintain O2 saturation > 93% (i.e., NRB, BVM with 100% O2) Observe for signs of impending respiratory failure; Refer to the Airway Management Protocol if needed: Hypoxia Poor ventilatory effort Altered mental status/decreases level of consciousness Inability to maintain patent airway For patients with assisted ventilation: Administer ventilations at normal rate for age range Acute herniation should be suspected when the following signs are present: Abrupt increase in blood pressure Abrupt decrease in heart rate Acute unilateral dilated and non-reactive pupil Abrupt deterioration in mental status Abrupt onset of motor posturing Hyperventilation is a temporizing measure which is only indicated in the event of acute herniation 201 If signs of herniation develop, begin hyperventilation If < 1 year old, 35/minute If > 1 year old, 25/minute Target an ETCO2 of 30-35 mmHg If severely agitated/combative and unable to deescalate by any other means, consider: Lorazepam 0.05 mg/kg IV/IO (max 2.0 mg) Contact Medical Control for any additional orders or questions Paramedic - Any additional sedation 202 Table of Contents Legend EMT A‐EMT Paramedic A A P P Medical Control M M 12‐Lead EKG Airway Obstruction Airway Orotracheal Intubation Airway Video Laryngoscopy Airway Suctioning ‐ Basic Airway Suctioning ‐ Advanced Blood Glucose Analysis Carboxyhemoglobin SpCO Monitoring Cardioversion CCR ‐ Cardiocerebral Resuscitation Chest Decompression Childbirth Procedure Childbirth Complications CPAP CPR ‐ Cardiopulmonary Resuscitation Cricothyrotomy Decontamination Defibrillation ‐ Automated Defibrillation ‐ Manual Endotracheal Tube Introducer External Cardiac Pacing LMA ‐ Laryngeal Mask Airway MCI ‐ Mass Casualty Incident MAD ‐ Mucosal Atomizer Device Orogastric Tube Insertion King LTS‐D Pulse Oximetry RSA ‐ Rapid Sequence Airway Restraints Spinal Immobilization Spinal Immobilization ‐ Football Players Splinting Stroke Screen Temperature Measurement Tourniquet Trauma Guidelines Venous Access ‐ Existing Venous Access ‐ Extremity Venous Access ‐ Intraosseous Wound Care 204 205 206 208 210 211 212 213 214 215 220 221 222 223 224 225 226 227 228 229 230 231 234 235 236 237 241 242 243 244 245 247 248 249 250 252 253 254 256 257 Service MD Approval:______ Procedure Section Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 203 Procedure EMT Clinical Indications: A P Suspected cardiac patient Suspected tricyclic overdose Electrical injuries Syncope CHF Abdominal pain above the umbilicus Undifferentiated respiratory complaints A‐EMT Paramedic A P Procedure: 1) 2) Assess patient and monitor cardiac status If patient is unstable, definitive treatment is the priority. If patient is stable or stabilized after treatment, perform a 12-Lead EKG 3) Prepare EKG monitor and connect patient cable to electrodes 4) Expose chest and prep as necessary. Modesty of the patient should be respected. 5) Apply chest leads and extremity leads using the following landmarks: -RA: Right arm or as directed by manufacturer -LA: Left arm or as directed by manufacturer -RL: Right leg -LL: Left leg -V1: 4th intercostal space at right sternal border -V2: 4th intercostal space at left sternal border -V3: Directly between V2 and V4 -V4: 5th intercostal space at midclavicular line -V5: Level with V4 at left anterior axillary line -V6: Level with V5 at left midaxillary line 6) Instruct patient to remain still 7) Press the appropriate button to acquire the 12-Lead EKG (complete age and gender questions correctly) 8) Print data as per guidelines and attach a copy of the 12-Lead to the PCR. Place the name and age of the patient on the paper copy of the EKG Paramedic: If STEMI identified, notify STEMI Hospital immediately. Report STEMI alert and a detailed report to follow. If able transmit the EKG as soon as possible. Non-Paramedic: transmit the 12-Lead EKG as soon as obtained. If transmission does not work, read the defibrillator interpretation that prints on the EKG to Medical Control. 11) Document the procedure, time and results on/with the PCR. 12) An EMT-Basic may perform a 12-Lead EKG; a Paramedic, however should review it before implementing any treatment modalities. Service MD Approval:______ Procedure 1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 204 Procedure A P Clinical Indications: EMT A‐EMT Paramedic Complete or partial obstruction of the airway due to a foreign body. Patient with unknown illness or injury who cannot be ventilated after proper opening of the airway. A P Procedure: Foreign Body Airway Obstruction - >1 year old, conscious □ If coughing, wheezing and exchanging air, do not interfere with the victims efforts to expel the foreign body. □ If unable to speak, weak or absent cough or no air exchange → Use abdominal thrusts (Heimlich Maneuver) if victim > 1 year ▪make a fist with one hand ▪place the thumb side of your fist against the victims abdomen in midline, above the navel but below the breastbone. ▪grasp your fist with your other hand and press your fist into the victims abdomen with a quick, upward thrust. ▪ repeat steps above until the object is expelled or the victim becomes unresponsive. Foreign Body Airway Obstruction - < 1 year old, conscious □ If coughing, wheezing and exchanging air, do not interfere with the victims efforts to expel the foreign body. □ If unable to cry or speak, weak or absent cough or no air exchange → Support the victim in the head down position with your non-dominant hand and forearm. → Perform back blows with the heel of your dominant hand between the shoulder blades → Repeat the steps above until the object is expelled or the victim becomes unresponsive. Foreign Body Airway Obstruction - unconscious □ If patient was responsive and then became unresponsive → lower the victim to the ground and begin CPR, starting with compressions (do not check for a pulse) → Every time you open the airway to give breaths, open the mouth wide and look for the object → If you see an object that can easily be removed, remove it with your finger → If you do not see an object, continue CPR → If a foreign object is visualized but cannot be removed with finger, attempt to remove it with the Magill forceps ___________________________________________________________________________________ PARAMEDICS: ▪ If the foreign body is not visualized or it cannot be retrieved, attempt endotracheal intubation with appropriate size ET Tube or 0.5 smaller ▪ If ETT cannot pass and patient is > 1 year old but <12 years old perform needle jet insufflation ▪If ETT cannot pass and patient is >12 years old perform cricothyrotomy with pertrach per procedure section Transport rapidly to the closest facility! Service MD Approval:______ Procedure 2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 205 Procedure Clinical Indications: P Paramedic Respiratory or Cardiac Arrest Inadequate ventilation with Bag Valve Mask Impending respiratory failure: □ Decreased level of consciousness with hypoxia unimproved by 100% oxygen, apnea, and/or respiratory rate <8 □ OR poor ventilatory effort (with hypoxia unresponsive to 100% Oxygen) □ OR unable to maintain patent airway Airway obstruction P Equipment: Laryngoscope handle with appropriate size blade. Proper size endotracheal tube (ETT) plus back up ETT 0.5-1.0 mm smaller Water-soluble lubrication gel, (lubricate distal end of tube at cuff) 10cc syringe (larger syringe if low pressure cuff) Stylet, (insert into ET tube and do not let stylet extend beyond tip of ET tube) Tape or ETT securing device Proper size oral pharyngeal airway BVM Oxygen source Suction device Stethoscope Capnography Oxygen saturation monitor Procedure: Patient/equipment preparation: □ Maintain cervical alignment and immobilization, as necessary □ Attach proper blade to laryngoscope handle and check light □ Check endotracheal tube cuff □ Raise gurney so that patient's nose is at intubator’s xiphoid (if possible) □ Confirm patient attached to cardiac monitor and oxygen saturation monitor □ Ready ETCO2 detection device □ Specify personnel to: ~apply cricoid pressure ~ maintain cervical alignment and immobilization during procedure ~watch cardiac and oxygen saturation monitors Continued on page 2 Service MD Approval:______ Procedure 3.1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 206 Procedure P Paramedic P Intubation: □ preoxygenate patient with 100% Oxygen (BVM or NRB) before intubation attempt to achieve O2 saturation >93% for 5 minutes or 8 vital capacity breaths. Have assistant apply cricoid pressure (Sellicks’s maneuver) during entire procedure. □ Remove all foreign objects, such as dentures, oral pharyngeal airways, etc. and suction the patient’s airway if needed. (Do not remove an esophageal located ETT if in place from prior attempt) □ Grasp laryngoscope handle in left hand. □ Grasp ET tube in right hand □ Insert the blade into the right side of the patient’s mouth sweeping the tongue to the left side □ Visualize the vocal cords while avoiding any pressure on the teeth □ Insert the endotracheal tube until the cuff passes the vocal cords. (Insert far enough so that at balloon port tubing is even with lips) □ Typical depth = tube size (ID) x3 (example would be tube depth of 24 for a 8.0mm tube) □ Remove the laryngoscope blade □ Inflate the endotracheal cuff with the syringe with 5-10cc of air (low pressure cuff may require larger volume) and remove the syringe from inflation valve □ Confirm tube placement □ Ventilate with BVM and: ~observe immediate (within 6 breaths) ETCO2 waveform and number with capnography ~watch for chest rise AND ~listen to abdomen to ensure tube is not esophageal □ Then, listen for bilateral breath sounds □ Observe oxygen saturation Note: regardless of the apparent presence of lung sounds, tube misting and chest rise, or lack of gastric sounds, if ETCO2 does not indicate proper tube location (alveolar waveform), ETT must be removed. If unilateral right sided breath sounds are heard consider: □ Right mainstem intubation □ If present, deflate the cuff and withdraw tube 1-2cm □ Repeat auscultation procedure as above for breath sounds If bowel sounds heard with bagging or ETCO2 device does not indicate proper ETT placement, deflate cuff, remove tube and ventilate with BVM for two minutes If intubation attempt unsuccessful, refer to the next step in the Airway, Adult Protocol If successful tube placement: □ Secure tube using an endotracheal securing device □ Document depth of tube □ Reassess lung sounds and patient clinical status □ Insert oral pharyngeal airway, or use ET tube holder with built in bite block (if available) □ Ensure c-spine is immobilized □ Continue ventilations □ Document ETCO2 waveform and reading continuously at time of EACH patient movement, including waveform and reading at time of transfer of care at the emergency department. Procedure 3.2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 207 Procedure Clinical Indications: P Paramedic Respiratory or Cardiac Arrest Inadequate ventilation with Bag Valve Mask Impending respiratory failure: □ Decreased level of consciousness with hypoxia unimproved by 100% oxygen, apnea, and/or respiratory rate <8 □ OR poor ventilatory effort (with hypoxia unresponsive to 100% Oxygen) □ OR unable to maintain patent airway Airway obstruction P Equipment: Video Assisted Laryngoscope (VAL) with appropriate size blade. Proper size endotracheal tube (ETT) and back up ETT 0.5-1.0 mm smaller Water-soluble lubrication gel, (lubricate distal end of tube at cuff) 10cc syringe (larger syringe if low pressure cuff) Stylet if compatible with VAL device (insert into ET tube and do not let stylet extend beyond tip of ET tube) Tape or ETT securing device Proper size oral pharyngeal airway BVM Oxygen source Suction device Stethoscope Capnography Oxygen saturation monitor Procedure: Patient/equipment preparation: □ Maintain cervical alignment and immobilization, as necessary □ Attach proper blade to VAL device and ensure function of video screen □ Check endotracheal tube cuff □ Raise gurney so that patient's nose is at intubator’s xiphoid (if possible) □ Confirm patient attached to cardiac monitor and oxygen saturation monitor □ Ready ETCO2 detection device □ Specify personnel to: ~apply cricoid pressure ~maintain cervical alignment and immobilization during procedure ~watch cardiac and oxygen saturation monitors Continued on page 2 Service MD Approval:______ Procedure 4.1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 208 Procedure P Paramedic P Intubation: □ Preoxygenate patient with 100% Oxygen (BVM or NRB) before intubation attempt to achieve O2 saturation >93% for 5 minutes or 8 vital capacity breaths. Have assistant apply cricoid pressure (Sellicks’s maneuver) during entire procedure. □ Remove all foreign objects, such as dentures, oral pharyngeal airways, etc. and suction the patient’s airway if needed. (Do not remove an esophageal located ETT if in place from prior attempt) □ Load ET tube into VAL device as per manufacturer recommendations □ Grasp VAL device in left hand. □ Insert the VAL device midline in the patient’s mouth □ Visualize the vocal cords while avoiding any pressure on the teeth □ Visualize the endotracheal tube passing the vocal cords until cuff is beyond the cords. □ Typical depth = tube size (ID) x3 (example would be tube depth of 24 for a 8.0mm tube) □ Remove the VAL device □ Inflate the endotracheal cuff with the syringe with 5-10cc of air (low pressure cuff may require larger volume) and remove the syringe from inflation valve □ Confirm tube placement □ Ventilate with BVM and: ~observe immediate (within 6 breaths) ETCO2 waveform and number with capnography ~watch for chest rise AND ~listen to abdomen to ensure tube is not esophageal □ Then, listen for bilateral breath sounds □ Observe oxygen saturation Note: regardless of the apparent presence of lung sounds, tube misting and chest rise, or lack of gastric sounds, if ETCO2 does not indicate proper tube location (alveolar waveform), ETT must be removed. If unilateral right sided breath sounds are heard, then consider: □ Right mainstem intubation □ If present, deflate the cuff and withdraw tube 1-2cm □ Repeat auscultation procedure as above for breath sounds If bowel sounds heard with bagging or ETCO2 device does not indicate proper ETT placement, deflate cuff, remove tube and ventilate with BVM for two minutes If intubation attempt unsuccessful, refer to the next step in the Airway, Adult Protocol If successful tube placement: □ Secure tube using an endotracheal securing device □ Document depth of tube □ Reassess lung sounds and patient clinical status □ Insert oral pharyngeal airway, or use ET tube holder with built in bite block (if available) □ Ensure c-spine is immobilized □ Continue ventilations □ Document ETCO2 waveform and reading continuously at time of EACH patient movement, including waveform and reading at time of transfer of care at the emergency department. Procedure 4.2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 209 Procedure Clinical Indications: Obstruction of the airway (secondary to secretions, blood, or any other substance) in a patient who cannot maintain or keep the airway clear. EMT Procedure: A P A‐EMT A P 1) Ensure suction device is in proper working order with suction tip in place 2) Preoxygenate the patient. 3) Explain the procedure to the patient if they are coherent. 4) Examine the oropharynx and remove any potential foreign bodies or material that may occlude the airway if dislodged by the suction device. 5) If applicable, remove ventilation devices (ie. BVM) from the airway. 6) Use the suction device to remove any secretions, blood, or other substances The alert patient may assist with this procedure. 7) Reattach ventilation device (ie. BVM) and ventilate or assist the patient. 8) Record the time and result of the suctioning procedure in the patient care report (PCR) Paramedic Service MD Approval:______ Procedure 5 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 210 Procedure Clinical Indications: Obstruction of the airway (secondary to secretions, blood, or any other substance) in a patient currently being assisted with an airway adjunct such as a LTA/LMA, endotracheal tube, tracheostomy tube, or a cricothyrotomy tube. Procedure: 1) Ensure suction device is in proper working order with suction tip in place 2) Preoxygenate the patient. 3) Attach suction catheter to suction device, keeping sterile plastic covering over catheter. 4) For all devices, use the suprasternal notch as the end of the airway. Measure the depth desired for the catheter (judgment must be used regarding the depth of suctioning with cricothyrotomy and tracheostomy tubes). 5) If applicable, remove ventilation devices(ie. BVM) from the airway. 6) With the thumb port of the catheter uncovered, insert the catheter through the airway device. 7) Once the desired depth (measured in #4 above) has been reached, occlude the thumb port and remove the suction catheter slowly. 8) Small volume (<10ml) of normal saline lavage may be used as needed. 9) Reattach ventilation device (ie. BVM) and ventilate or assist the patient. 10) Record the time and result of the suctioning procedure in the patient care report (PCR) P Paramedic P Service MD Approval:______ Procedure 6 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 211 Procedure Clinical Indications: Patients with suspected hypoglycemia (diabetic emergencies, altered/change in mental status, bizarre behavior, etc.). EMT A P Procedure: A‐EMT 1) Gather and prepare equipment 2) Blood samples for performing glucose analysis should be obtained simultaneously with intravenous access when possible 3) Place correct amount of blood on reagent strip or site on glucometer per the manufacturer’s instructions. 4) Time the analysis as instructed by the manufacturer. 5) Document the glucometer reading and treat the patient as indicated by the appropriate protocol 6) If reading appears incorrect, redraw and repeat analysis. 7) Repeat glucose analysis as indicated for reassessment after treatment and as per protocol. Paramedic A P Service MD Approval:______ Procedure 7 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 212 Procedure EMT Clinical Indications: Persons with suspected or known exposure to carbon monoxide Procedure: A P A‐EMT Paramedic A P 1) Apply probe to patient’s middle finger or any other digit as recommended by the manufacturer. If near strobe lights, cover the finger to avoid interference and/or move away from lights if possible. Where the manufacturer provides a light shield it should be used. 2) Allow machine to register percent circulating carboxyhemoglobin values 3) Verify pulse rate on machine with actual palpable pulse of the patient. 4) Record levels in patient care report or on the scene rehabilitation form. ▪ If CO <5%, assess for other possible illness or injury ▪ If CO >5% to <15% and symptomatic from Carbon Monoxide – treat per Carbon Monoxide Exposure Protocol Signs and Symptoms ‐ Altered mental status / dizziness, headache, nausea/vomiting, chest pain/respiratory distress, neurological impairments, vision problems/reddened eyes, tachycardia/tachypnea, arrhythmias, seizures, coma ▪ If CO >15% = Treat per Overdose and Poisoning: Carbon Monoxide Protocol and Transport. 5) Monitor critical patients continuously with pulseox and SpCO until arrival at the hospital. 6) Document percent of carboxyhemoglobin values every time vital signs are recorded during therapy for exposed patients. 7) Use the pulse oximetry feature of the device as an added tool for patient evaluation. Treat the patient, not the data provided by the device. Utilize the relevant protocol for guidance. 8) The pulse oximeter reading should never be used to withhold Oxygen from a patient in respiratory distress 9) Factors which may reduce the reliability of the reading include: □ Poor peripheral circulation (blood volume, hypotension, hypothermia) □ Excessive external lighting, particularly strobe/flashing lights □ Excessive sensor motion □ Fingernail polish (may be removed with acetone pad) □ Irregular heart rhythms (atrial fibrillation, SVT, etc.) □ Jaundice □ Placement of BP cuff on same extremity as pulse ox probe Service MD Approval:______ Procedure 8 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 213 Procedure P Clinical Indications: Paramedic P Unstable patient with tachydysrhythmia (rapid atrial fibrillation, supraventricular tachycardia, ventricular tachycardia) Patient is not pulseless (pulseless patient requires unsynchronized cardioversion, ie. defibrillation). Procedure: 1) Ensure the patient is attached properly to a monitor/defibrillator capable of synchronized cardioversion. 2) Have all equipment prepared for unsynchronized cardioversion/defibrillation, if the patient fails synchronized cardioversion and the condition worsens. 3) Consider the use of pain medication or sedatives per protocol. 4) Set energy selection to the appropriate setting 5) Set monitor/defibrillator to synchronized cardioversion mode 6) Make certain all personnel are clear of patient. 7) Press and hold the shock button to cardiovert. Stay clear of the patient until you are certain the energy has been delivered. NOTE: It may take the monitor/defibrillator several cardiac cycles to “synchronize”, so there may be a delay between activating the cardioversion and the actual delivery of energy. 8) Note patient response and perform immediate unsynchronized cardioversion/defibrillation if the patient's rhythm has deteriorated into pulseless ventricular tachycardia/ventricular fibrillation. Follow the procedure for Defibrillation-Manual 9) If the patient’s condition is unchanged, repeat steps 2-8 above, using escalating energy settings per protocol. 10) Repeat per protocol until maximum setting or until efforts succeed. 11) Note procedure, response, and times in the PCR. Service MD Approval:______ Procedure 9 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 214 Procedure Clinical Indications: Age > 18 years of age ( CCR causes worse outcomes in the pediatric population) Suspected cardiac cause of arrest (not respiratory-OD, drowning, etc.) EMT A P A‐EMT Paramedic A P It occurs with Ventricular Fibrillation or Pulseless Ventricular Tachycardia, with PEA and with Asystole. You must assume there is no blood perfusing the brain and heart….which is bad for survival. Your patient needs both a pump (chest compressions) and diastolic pressure support (to perfuse the coronary arteries). Time spend doing other things (such as prolonged airway management) at the expense of not delivering pump support is not good for the patient. Determine as close as possible when the patient collapsed, and document this. Also look for any signs of patient gasping prior to and/or during resuscitation, and document this. If gasping is present, note pupil reaction and document also. It is also important to remember that not all Pulseless patients are the result of cardiac related events. Other mechanisms such as trauma, drowning, hypothermia, choking and other respiratory problems, etc. must be considered as a possible cause for the arrest and should be addressed with immediate, appropriate airway intervention. Key points in the Cardio Cerebral Resuscitation (CCR) approach: Survival is determined by a functional recovery of two organs: the heart and the brain □ without adequate blood flow neither organ will survive □ that makes properly performed chest compressions (CC) the single most important determinant of survival. □ Anything that interrupts or otherwise decreases the quality of CC contributes to the death of your patient. □ This concept – continuous maximal quality CC – must become the foundation of all you think and do during resuscitation. All patients are treated the same during the first two minutes of the code. □ They get uninterrupted continuous CC (CCC) while other interventions are performed. □ The cardiac rhythm is irrelevant during this period. The cardiac rhythm determines subsequent management. □ It is analyzed (using manual interpretation) briefly AFTER each set of 200 CCC □ It is either shockable or non-shockable - don’t make it more complicated than that. CCCs are to be resumed immediately following a rhythm assessment + shock. □ The rhythm observed after a shock is not – meaning NOT – to be treated. □ Otherwise deadly pauses in CCC will be introduced in an attempt to gather information that is irrelevant to survival! The initial rhythm (after 200 CCC) determines subsequent treatments: □ When to initiate invasive airway insertion and positive pressure ventilation. □ Need for anti-arrhythmic medications □ How long to remain on scene. Success depends on: □ Leadership □ Delegation of a limited set of specific tasks □ Timely focused completion of these specific tasks by rescuers Service MD Approval:______ Procedure 10-1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 215 Procedure Interventions that are critical to survival MUST whenever possible be performed by two persons solely dedicated to that task. □ One to perform it and a second person to assure quality performance. □ This applies especially to chest compressions and it is also important in the management of an invasive airway + ventilations. Code Commander: Someone must assume the role of code commander. This person is responsible for delegating tasks, is the only person interpreting the rhythm, and is responsible for monitoring/critiquing the overall performance of the team. Other members must work as a team and take direction from the code commander. They must focus on their assigned tasks and let the code commander manage the overall response (in other words, keep their noses out of other rescuers business) Critical First Tasks: (delegated and performed in first two minutes if at all possible) MCMAID – a prioritized sequence consisting of: □ M = Metronome (100/min) □ C = Chest compressions (focus on rate, recoil and depth) □ M = Monitor (turn on in defib mode, pads on, joules set at maximum) □ A = Airway (OPA, ensure patency, NRB @ 15/lpm) □ I = Intravenous or Intraosseous access □ D = Drugs (Epi, Vasopressin, Amiodarone) (be ready to administer when needed and monitor timing for repeat doses) Chest Compressions: MCMAID Metronome should be turned on to assure a rate of 100/minute. CCC should be started ASAP after arrival. A two-person task if at all possible □ Switch compressors rapidly/frequently (every 1-2 minutes) □ The non-compressor continuously monitors the quality of CCC: rate, depth and recoil CCC should be continuous = not interrupted □ The only valid reasons for interrupting compressions are for analyzing the rhythm and shocking. □ All other requests to pause CCC must be cleared by the code commander, and the reason and duration documented in the run report. Monitor/Defibrillator: MCMAID Initial: □ Turn unit on when compressions are started and set mode to defib. □ Ensure joules are set to maximum allowed ▪ Place pads in sternum/apex position without interruption of chest compressions. Service MD Approval:______ Procedure 10-2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 216 Procedure Defibrillation Process: □ Charge defibrillator during the last 10 seconds of 200 CCC. □ Ensure all rescuers will be clear if a shock is needed. □ Pause a few seconds only for analysis – determine if it is shockable or not. ▪ If indicated, immediately deliver a single (not stacked) shock at maximum joules. ▪ If no shock is indicated, dump the charge by either decreasing the energy level and immediately returning back to maximum energy setting (200J or 360J), OR switching the mode to monitor and then quickly back to defib mode. □ Immediately resume CCC after analysis + shock. ▪The pause from stopping CCC to resumption of CCC should be less than 5 seconds. Airway: MCMAID Initially: □ Insert OPA, apply NRB @15 lpm (look for misting), ensure patency (listen for exhausted air with compressions. If unsure, give one single breath with BVM, looking for chest rise and fall for compliance). When to insert invasive airway depends on the initial rhythm: □ If non-shockable, initiate immediately after first rhythm analysis. □ If shockable – ONLY after three cycles (2 min. of CCC + analysis + shock). NOT earlier, even if second rhythm is non-shockable. Once the invasive airway is in place, the airway persons sole task is to perform/monitor that task and no other. Invasive airway monitoring includes attention to: □ Proper placement □ Apply Capnography and verify waveform/presence of ETCO2. □ Avoidance of any interruption of CCC □ Ventilation rate of 6 per minute. Each breath must be timed – aim for 10 seconds between each breath. Excessive ventilation rates are deadly! □ Volume should be ~500cc. □ Delivery of breath should be over one second. Use an LTA if placing an endotracheal tube is met with any problems or delays. If the initial rhythm is shockable, seriously consider using the LTA instead of an ETT because these patient’s cannot tolerate even brief periods of less than optimal CCC. Assure that oxygen is attached. Intravenous/Intraosseous access: MCMAID Consider intraosseous route whenever there are any delays in IV insertion. Consider spiking a bag en route and having it ready on arrival. Service MD Approval:______ Procedure 10-3 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 217 Procedure Drugs: MCMAID The individual assigned to the Drug “Task”: □ Initially ensures medications are available and ready to administer. □ Is responsible for: ▪ The rapid administration when indicated. ▪ Re-dosing at appropriate intervals. ▪ Detecting when V-Fib is persistent or recurrent, and therefore indicating the use of Amiodarone. ▪ Accurate timing of when meds are to be given (to the second – using elapsed time since defibrillator was turned on.) Vasopressors should be given ASAP after analysis + shock, so their effect will be seen after the next 200 chest compressions. Epinephrine first! □ **The one exception is the patient who you suspect may get return of spontaneous circulation with the first shock. Such patients may include those with short down times or those who have had excellent chest compression generated perfusion. A clue to this is the presence of regular agonal respirations (gasping). In these patients consider giving Vasopressin initially, and reserving Epinephrine until the Code Commander observes persistent pulseless V-fib/Tach after the first shock – or until another 200 CCC cycle has been completed. □ Epi dose is 1mg IV/IO. Endotracheal administration is not to be utilized – start an IO instead □ If repeating doses, administer every other cycle of 200 compressions. (equivalent to every 4 min) Vasopressin: administer with first or second Epi dose as per protocol □ Dose is 40 units (two vials of 20 U each) □ Same dose is used for IV or intraosseous (IO) routes. Amiodarone is administered for persistent or recurrent pulseless V-fib/Tach. This should be administered immediately during the next 200 chest compression cycle if a second shock was indicated and delivered at the time of analysis. The Code Commander may visualize return of fibrillation during the 200 CCC and as such may order Amiodarone earlier since it has recurred. □ Dose is 300mg IV/IO □ Repeat doses are 150mg IV/IO Additional Treatments to consider: Consider possible renal failure (hyperkalemia) or suspected Tricyclic antidepressant overdose. If suspected, administer Sodium Bicarbonate 1mEq/Kg. If renal failure is suspected, also administer Calcium Chloride 1g IVP. If rhythm is persistent shockable V-fib or Pulseless V-Tach, consider the possible use of Magnesium Sulfate 2g IVP. Service MD Approval:______ Procedure 10-4 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 218 Procedure Additional Treatments to consider (continued): If the patient is successfully converted from V-Fib/Pulseless V-tach to a perfusing sustainable rhythm, consider post resuscitation Amiodarone boluses. □ Amiodarone bolus: 150mg If rhythm is a non-shockable Asystole or PEA, seek out and treat any possible contributing factors. Also consider external pacing: for PEA. Apply the pads in (or move them to) the anterior/posterior position, attach the 4-Lead cable, and set the pacer at the maximum milliamps at a rate of 80/min. Do NOT interrupt compressions while attempting pacing. When to stop CCC: If the patient shows signs of cerebral activity and the rhythm is non-shockable. Use end-tidal CO2 as a marker for possible ROSC. Look for a dramatic increase. Pulse checks are ONLY performed during brief rhythm analysis with location of carotid pulse ascertained during chest compressions. □ This may be modified by the Code Commander if cerebral function signs of life appear □ The Code Commander is the only individual who can order a pulse check other than that done during rhythm analysis. □ The Code Commander must ensure the pulse checker is clear if a shock is indicated. When to move the patient: Remember that moving the patient inevitably results in compromised quality of compressions. If crew safety is compromised or inadequate resuscitation space is available, patient should be quickly moved to a safe or larger area. This should be done initially and not after resuscitation efforts have begun. Initially shockable patients will live or die in the field! □ Move is allowed after 3 cycles are completed and a non-shockable rhythm is identified at the 3rd analysis ▪ If 3rd analysis is still shockable, continue resuscitation at the scene until a non-shockable rhythm is encountered. Initially non-shockable rhythms □ Medical Control must make this determination, but these patients may deserve at least 3 cycles of treatment with optimal quality compressions. Avoid Excessive Pauses: Rhythm analysis – ONLY the Code Commander pays attention to the rhythm (not everyone) Resume CCC immediately after analysis + shock. The Code Commander must assure this happens Charging – perform during last 10 seconds of 200 chest compressions During Intubation – It is responsibility of both the Code Commander and the second airway person to avoid pauses in CCC. This MUST be able to be performed without any interruption of compressions! Consider using the LTA if unable to intubate effectively. Pulse Checks – only performed during the rhythm analysis pause; must be correlated with rhythm Service MD Approval:______ Procedure 10-5 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 219 Procedure P Clinical Indications: Paramedic P Tension pneumothorax should be suspected in patients who exhibit: □ Severe respiratory distress with hypoxia □ Unilateral decreased or absent lung sounds □ Evidence of hemodynamic compromise (Shock, Hypotension, Tachycardia, Altered Mental Status) □ Tracheal deviation away from the collapsed lung field (less reliable than the above) Pleural decompression for tension pneumothorax should only be preformed when at least 3 of the above criteria are present. Equipment: 14 gauge 2 inch – 2.5 inch over the needle catheter Tape Sterile gauze pads Antiseptic swabs Occlusive dressing Procedure: Locate decompression site □ Identify the 2nd intercostal space in the mid-clavicular line on the same side as the pneumothorax Prepare the site with an antiseptic swab: □ Firmly introduce catheter immediately above distal rib of selected site. Insert the catheter into the thorax until air exits Advance catheter and remove needle. Secure the catheter taking care not to allow it to kink Reassess lung sounds and patient condition Dress area with occlusive dressing then cover with sterile gauze pad Assess breath sounds and respiratory status. Service MD Approval:______ Procedure 11 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 220 Procedure EMT Clinical Indications: A P A‐EMT Paramedic Active labor with perineal crowning Apply personal protective equipment and prepare for childbirth Allow head to deliver passively and control delivery by placing palm of hand over occiput. Protect perineum with pressure from other hand If amniotic sac is still intact, gently pinch and twist to manually rupture. Note presence or absence of meconium. If meconium is present, see Complication of Childbirth Once the head is delivered and passively turns to one side, suction mouth and nose If nuchal cord present, gently lift cord from around infant’s neck Gently apply downward pressure to infant to facilitate delivery of upper shoulder Once upper shoulder has delivered, apply gentle upward pressure to deliver lower shoulder Grasp the infant as it emerges from birth canal Keep infant at level of perineum until cord stops pulsating and cord is clamped. A P Care of the Newborn: Double clamp cord 10-12 inches from abdomen, once it stops pulsating cut cord. Suction mouth and nose Dry and warm the neonate. Wrap in blankets Stimulate infant by rubbing back or soles of feet Refer to Neonatal Resuscitation Protocol if infant is hypoxic, not breathing properly or heart rate <100. 0 1 2 Obtain APGAR Score Appearance Pulse Grimace Activity Respiratory Effort Blue Absent No response Limp Absent Peripheral Cyanosis Pink <100/minute >100/minute Grimace Cough/Sneeze Minimal Movement Active Motion Weak Cry Strong Cry Post Partum Care: Allow placenta to deliver spontaneously while transporting patient to hospital. Do not pull on cord. Apply direct pressure to any actively bleeding areas on the perineum If blood loss significant or vaginal bleeding continues □ Fluid bolus as needed □ Massage top of uterus □ Allow newborn to nurse / breast feed if stable Service MD Approval:______ Procedure 13 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 221 Procedure Shoulder Dystocia: Place mother in knee-chest position and reattempt delivery If delivery fails, support child’s airway, provide supplemental oxygen. EMT A P A‐EMT A P Breech Birth: Paramedic Do not attempt to pull infant by trunk or legs. Place mother in knee-chest position If head does not deliver, push baby’s mouth and nose away from vaginal wall with two gloved fingers. Provide supplemental oxygen to infant. Prolapsed Cord: Place mother in knee-chest position Do not push cord back into birth canal Insert gloved fingers into birth canal and keep pressure off prolapsed cord Cover exposed cord with warm moist dressing Meconium-Stained Amniotic Fluid: Suction mouth and nose after delivery If baby is vigorous (normal respiratory effort, muscle tone, and heart rate >100), provide supportive care If baby is not vigorous (depressed respirations, poor muscle tone, or heart rate <100) – REQUEST ALS Meconium-Stained Amniotic Fluid: P Paramedic P Suction mouth and nose after delivery If baby is vigorous (normal respiratory effort, muscle tone, and heart rate >100), provide supportive care If baby is not vigorous (depressed respirations, poor muscle tone, or heart rate <100), perform endotracheal intubation and suction trachea while removing ET tube, may repeat one additional time. Support ventilation and re-intubate with a clean tube Service MD Approval:______ Procedure 12 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 222 Procedure Clinical Indications: For patients with Acute Bronchospastic Disorders (acute or chronic bronchitis, emphysema, or asthma) or Acute Pulmonary Edema, who have hypoxemia and/or respiratory distress that does not quickly improve with pharmaceutical treatment. Consider CPAP protocol if 2 or more are present: Retraction of intercostals or accessory muscles Bronchospasm Rales Respiratory Rate >25 per minute Oxygen saturation <93% on high flow Oxygen EMT A P A‐EMT Paramedic A P Contraindications: Respiratory arrest Agonal respirations Unconsciousness or obtundation Shock associated with cardiac insufficiency Trauma Persistent nausea and vomiting Facial anomalies Inability to cooperate with the procedure Current tracheostomy Equipment: Medical Director approved Continuous Positive Airway Pressure (CPAP) device Procedure: Perform primary and secondary survey Attach cardiac monitor, capnography if available, and pulse oximetry Service MD Approval:______ Verbally instruct patient (this is a critical item) □ Patient requires verbal sedation to use this device effectively □ Setup CPAP device as per manufacturer’s instructions □ Instruct patient to slowly breathe in through the nose and exhale through the mouth (exhalation phase should be about 4 seconds) Continue treatment throughout transport to ED - document CPAP level used and FiO2 level used Record and monitor vital signs, ETCO2, and O2 saturation as needed/available In the event of progressive respiratory failure: □ Offer reassurance □ Stop treatment if necessary □ Institute BLS and ALS care per appropriate protocol □ Document adverse reactions, and reasons why CPAP was discontinued, in PCR Procedure 15 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 223 Procedure Clinical Indications: Pediatric Arrest Suspected non-cardiac arrest/respiratory arrest in adult patients (ie. overdose, drowning) EMT A P A‐EMT Paramedic A P Procedure: 1) Assess the patient’s level of responsiveness (signs of life) 2) If no response, open the patient’s airway with the head-tilt, chin-lift. Look, listen and feel for respiratory effort. If the patient may have sustained c-spine trauma, use the modified jaw thrust while maintaining immobilization of the c-spine. For infants, positioning the head in the sniffing position is the most effective method for opening the airway. 3) If patient is an adult, go to step 4. If no respiratory effort in the pediatric patient, give two ventilations. If air moves successfully, go to step 4. If air movement fails, proceed per AHA obstructed airway guidelines. 4) Check for pulse (carotid for adults and older children, brachial or femoral for infants) for at least 10 seconds. If no pulse, begin chest compressions as directed below. Age Infant Child Adult Location Over sternum, between nipples (inter‐mammary line), 2‐3 fingers Depth Rate 1.5 inches (1/3 the anterior‐posterior chest dimension At least 100/minute 2 inches (1/3 the anterior‐ Over sternum, between posterior chest nipples, heel of one hand dimension At least 100/minute Over sternum, just above the xyphoid process, At least 2 inches (1/3 the hadns with interlocked anterior‐posterior chest fingers dimension At least 100/minute 5) Go to Cardiac Arrest protocol 6) Chest compressions should be provided in an uninterrupted manner. Only brief interruptions are allowed for rhythm analysis and defibrillation 7) Document the time and procedure in the PCR. Service MD Approval:______ Procedure 16 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 224 Procedure If Possible Contact Medical Control Before Proceeding! P Paramedic P Clinical Indications: When all airway management measures have failed and the patient needs an advanced airway immediately, consider performing cricothyrotomy. The percutaneous approach is preferred. If, in the paramedics judgment, the time necessary to contact medial control will compromise the patient's chance of survival AND it is not possible to ventilate the patient with a bag-valve-mask during transport, cricothyrotomy may be performed without Medical Control. Relative Contraindications: Ability to ventilate patient with an oral-pharyngeal/nasal-pharyngeal airway, BVM, LTA/LMA, or endotracheal tube. Procedure: 1) Cleanse anterior neck. 2) Identify and mark cricothyroid membrane 3) Fill a 10cc syringe with 5cc’s of 0.9% normal saline 4) Remove dilator from the package and sheath and advance into the tracheostomy tube 5) Penetrate the skin and cricothyroid membrane with the splitting needle perpendicular to the skin while gently aspirating with the syringe. Air aspiration as evidenced by bubbles into syringe should flow easily confirming tracheal airspace. Incline needle more than 45 degrees toward carina and complete insertion of needle aspirating to ensure continued proper placement 6) Disconnect needle from syringe and advance tip of dilator into the hub of the splitting needle until resistance is met. 7) Squeeze wings of needle together then, open them out completely to split the needle. Remove needle, continuing to pull it apart in opposite directions, while leaving the dilator in the trachea. 8) Place thumb on dilator knob while first and second fingers are curved under flange of trachea tube. By exerting pressure, advanced dilator and tracheostomy tube into position until flange is against skin. 9) Remove dilator and inflate cuff until you have control of the airway (max 5cc’s). Attach ETCO2 and BVM. Secure tube around patient’s neck with twill tape. 10) Confirm placement with gentle ventilation via BVM, continuous capnography and physical means. Be sure air movement is fluid with bilateral symmetric chest rise and that no visible neck softtissue distortion is noted. 11) If tracheal placement is unclear, remove and transport immediately to the closest ER 12) Secure tube and consider sedation protocol 13) If not previously done, immediately notify Medical Control. Service MD Approval:______ Procedure 17 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 225 Procedure EMT A P A‐EMT Paramedic A P Clinical Indications: Any patient who may have been exposed to significant hazardous materials, including chemical, biological, or radiological weapons. Procedure: In coordination with HazMat and other Emergency Management personnel, establish hot, warm, and cold zones of operation. Ensure that personnel assigned to operate within each zone have proper personal protective equipment. In coordination with other public safety personnel, assure each patient from the hot zone undergoes appropriate initial decontamination. This is specific to each incident; such decontamination may include: □ Removal of patient from hot zone □ Simple removal of clothes □ Irrigation of eyes □ Passage through high-volume water bath (ie. Between two fire apparatus) for patients contaminated with liquids or certain solids. Patients exposed to gases, vapors, and powders often will not require this stop as it may unnecessarily delay treatment and/or increase dermal absorption of the agent(s). Initial triage of patients should occur after step #3. Immediate life threats should be addressed prior to technical decontamination. Assist patients with technical decontamination (unless contraindicated based on #3 above). This may include removal of all clothing and gentle cleaning with soap and water. All body areas should be thoroughly cleansed, although overly harsh scrubbing which could break the skin should be avoided. Place triage identification on each patient Match triage information with each patient’s personal belongings, which were removed during technical decontamination. Preserve these personnel affects for law enforcement. Service MD Approval:______ Monitor all patients for environmental illness. Transport patients per local protocol. Procedure 18 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 226 Procedure EMT Clinical Indications: Patients in cardiac arrest (pulseless, non-breathing) Age <8 years, use pediatric pads if available A P A‐EMT Paramedic A P Contraindications: Pediatric patients whose body size is such that the pads cannot be placed without touching one another. Procedure: 1) If multiple rescuers available, one rescuer should provide uninterrupted chest compression while the AED is being prepared for use. 2) Apply defibrillator pads per manufacturer recommendations. Use alternate placement when implanted devices (pacemakers, AICD’s) occupy preferred pad positions. 3) Remove any medication patches on the chest and wipe off any residue 4) If necessary, connect defibrillator leads: per manufacturer recommendations. 5) Activate AED for analysis of rhythm 6) Stop chest compressions and clear the patient for rhythm analysis. Keep interruption in chest compressions as brief as possible 7) Defibrillate if appropriate by depressing the “shock” button. Assertively state “CLEAR” and visualize that no one, including yourself, is in contact with the patient prior to defibrillation. The sequence of defibrillation charges is preprogrammed for monophasic defibrillators. Biphasic defibrillators will determine the correct joules accordingly. 8) Begin CPR/CCR immediately after the delivery of the shock beginning with chest compressions. 9) After 2 minutes of CPR/CCR, analyze rhythm and defibrillate if indicated. Repeat this step every 2 minutes. 10) If “no shock advised” appears, perform CPR/CCR for two minutes and then reanalyze. 11) Transport and continue treatment as indicated. 12) Keep interruption of compressions as brief as possible. Adequate CPR/CCR is a key to successful resuscitation. Service MD Approval:______ If pulse returns: See Post-Resuscitation Protocol Procedure 19 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 227 Procedure EMT Clinical Indications: Cardiac arrest with ventricular fibrillation or pulseless ventricular tachycardia A P A‐EMT Paramedic A P Procedure: 1) Ensure chest compressions are adequate and interrupted only when necessary 2) Clinically confirm the diagnosis of cardiac arrest and identify the need for defibrillation 3) Apply hands-free pads to the patient’s chest in the proper position 4) Charge the defibrillator to the maximum energy level. Continue chest compressions while the defibrillator is charging. 5) Pause compressions, assertively state, “CLEAR” and visualize that no one, including yourself, is in contact with the patient. 6) Deliver the shock by depressing the shock button for hands-free operation. 7) Immediately resume chest compressions and ventilations for 2 minutes. After 2 minutes of CPR/ CCR, analyze rhythm and check for pulse only if organized rhythm. 8) Repeat the procedure every two minutes as indicated by patient response and EKG rhythm. 9) Keep interruption of compressions as brief as possible. Adequate compressions are the key to successful resuscitation. If pulse returns: See Post-Resuscitation Protocol Service MD Approval:______ Procedure 20 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 228 Procedure Clinical Indications: Patients meet clinical indications for oral intubation Initial intubation attempt for medical indication unsuccessful Predicted difficult intubation P Paramedic P Contraindications: ETT size less than 6.5mm. Already failed twice on medical indicated intubation attempts or failed on one trauma intubation attempt DO NOT UTILIZE BOUGIE. Procedure: 1) Prepare, position, and oxygenate the patient with 100% Oxygen 2) Select proper ET tube without stylette, test cuff and prepare suction 3) Lubricate the distal end and cuff of the endotracheal tube (ETT) and the distal ½ of the endotracheal tube introducer (Bougie) (note: failure to lubricate the Bougie and the ETT may result in being unable to pass the ETT) 4) Using laryngoscopic techniques, visualize the vocal cords if possible using Sellick’s/BURP as needed. 5) Introduce the Bougie with curved tip anteriorly and visualize the tip passing the vocal cords or above the arytenoids if the cords cannot be visualized 6) Once inserted, gently advance the Bougie until you meet resistance or “hold-up” (if you do not meet resistance you have a probable esophageal intubation and insertion should be re-attempted or the failed airway protocol implemented as indicated. 7) Withdraw the Bougie ONLY to a depth sufficient to allow loading of the ETT while maintaining proximal control of the Bougie 8) Gently advance the Bougie and loaded ET tube until you have hold-up again, thereby assuring tracheal placement and minimizing the risk of accidental displacement of the Bougie. 9) While maintaining a firm grasp on the proximal Bougie, introduce the ET tube over the Bougie passing the tube to its appropriate depth 10) If you are unable to advance the ETT into the trachea and the Bougie and ETT are adequately lubricated, withdraw the ETT slightly and rotate the ETT 90 degrees COUNTER clockwise to turn the bevel of the ETT posteriorly. If this technique fails, to facilitate passing of the ETT you may attempt direct laryngoscopy while advancing the ETT (this will require an assistant to maintain the position of the Bougie and , if so desired, advance the ETT) 11) Once the ETT is correctly placed, hold the ET tube securely and remove the Bougie 12) Confirm tracheal placement with capnography according to the intubation protocol. Inflate the cuff, auscultate for equal breath sounds and reposition accordingly. 13) When final position is determined secure the ET tube, continuously record and monitor capnography, reassess breath sounds and monitor patient to assure continued tracheal intubation. 14) If there is any question regarding placement of ETT (Esophageal vs. Tracheal) remove immediately and ventilate with BVM. Service MD Approval:______ Procedure 21 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 229 Procedure Clinical Indications: Monitored heart rate less than 60 per minute with signs and symptoms of inadequate cerebral or cardiac perfusion such as: □ Severe chest pain P Paramedic □ Hypotension □ Pulmonary edema □ ALOC, disorientation, confusion, etc PEA, where the underlying rhythm is bradycardic and reversible causes have been treated P Procedure: 1) Attach standard four-lead monitor 2) Apply defibrillation/pacing pads to chest and back: □ One pad to left mid chest next to sternum, one pad to left mid posterior back next to spine 3) Choose pacing option 4) Adjust heart rate to 70 BPM for an adult, 100 BPM for pediatric patients 5) Note pacer spikes on EKG screen 6) Slowly increase output until capture of electrical rhythm on the monitor 7) If unable to capture while at maximum current output, stop pacing immediately 8) If capture observed on monitor, check for corresponding pulse and assess vital signs 9) Mechanical capture occurs when paced electrical spikes on the monitor correspond with palpable pulse 10) Consider the use of sedation or analgesia if patient is uncomfortable, per protocol 11) Document the dysrhythmia and the response to external pacing with EKG strips in the PCR. Service MD Approval:______ Procedure 22 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 230 Procedure Clinical Indications: Inability to BVM ventilate When an alternative airway device is needed in the management of respiratory failure P Contraindications: Pharyngeal pathology (abscess or hematoma) Obstructive lesions below the glottis Limited mouth opening Intact gag reflex Paramedic P Equipment: Correctly sized laryngeal mask airway (see chart below) Bag valve mask or automatic ventilator Oxygen reservoir Suction device Bite block and/or endotracheal tube holder (if available) 25 and/or 35ml syringes for expanding cuff End Tidal CO2 and oxygen saturation monitoring devices Laryngeal Mask Airway Sizes Mask Size 1 1.5 2 2.5 3 4 5 Patient weight (kg) <5kg 5‐10 10‐20 20‐30 30‐60 60‐80 >80 Age (years) <0.5yrs Length (cm) 10cm 10 11.5 12.5 19 19 19 .5‐5 5‐10 10‐15 >15 >15 Cuff volume (ml) 4 5‐7 7‐10 14 15‐20 25‐30 30‐40 Largest ETT* 3.5mm 4.5 5 6 6.5 7 *Appropriately sized endotracheal tube (internal diameter) that can be passed through LMA for blind intubation if intubating LMA is inserted. Service MD Approval:______ Procedure 23-1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 231 Procedure Procedure – Laryngeal Mask Airway Placement: Pre-oxygenate patient with 100% Oxygen via bag valve mask to achieve O2 saturation of >93% if possible Remove the red tag from the balloon port P Paramedic P Check the integrity of the cuff and pilot balloon Tightly deflate the cuff with the syringe □ The deflated cuff should appear BOAT shaped Lubricate the posterior surface Place patient in neutral sniffing position (if no c-spine/spinal injury suspected) □ For patients with suspected c-spine injury, perform two person insertion technique: •One person maintains manual in-line cervical spine stabilization while the other person proceeds with procedure as below: Pull mandible down to open mouth Insert uninflated LMA into oral cavity with cuff facing away from hard palate Guide LMA around curvature of the posterior pharynx into the hypopharynx until resistance is felt. Resistance is due to the tip of the LMA stopping at the upper esophageal sphincter If uninflated LMA insertion is difficult: □ If the curvature of the posterior/hypopharynx is too acute, perform a jaw thrust, pulling the tongue forward. Alternately, a laryngoscope may be used to lift the jaw/mandible to facilitate insertion. □ A slight inflation of the cuff to 1/3 – ½ of typical inflation volume may also increase ease of insertion □ Insert LMA with cuff facing hard palate, then rotate 180 degrees into the proper position after the angel around the posterior aspect of the tongue has been cleared. Inflate cuff without holding the tube Ensure that the black line running the length of the LMA shaft is in the midline of the upper lip and between the two central incisors (this will help maintain a seal) Administer gentle positive pressure ventilation Obtain end-tidal CO2 (waveform), listen for breath sounds bilaterally, look for chest excursion, and check oxygen saturation. Secure in the midline to help maintain a good seal over the Larynx Place bite block, gauze or endotracheal tube holder (if available) between teeth to prevent biting tube. Ensure c-spine is still immobilized If repeated attempts are made, oxygenate with 100% O2 for 2 minutes between attempts Endotracheal intubation using Intubating Laryngeal Mask Airway (ILMA): Select correct size ILMA Insert endotracheal tube into oropharynx at 90 degree angle (from corner of mouth) During insertion and passage through the ILMA rotate ET tube 90 degrees so that the tip of the ET tube will pass through the bars that traverse the distal opening of the ILMA. Confirm placement as per endotracheal intubation procedure. Service MD Approval:______ Procedure 23-2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 232 Procedure P Paramedic P Service MD Approval:______ Procedure 23-3 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 233 Procedure History: Number of patients Cause of Incident Chemical, Biological, Radiological contamination Secondary Devices Signs and Symptoms: SLUDGE for chemical exposure Respiratory Distress for Narcotic Exposure Nausea Vomiting for radiation Differential: Blast Response MCI penetrating trauma MCI blunt trauma/MVC Scene Safety – If blast, wear N95 mask and full turnout gear until advised to remove Provide scene size‐up on radio; activate MCI plan if more than 5 patients EMT A P A‐EMT Paramedic A P If not already accomplished, establish Incident Command, Staging and Triage Move all ambulatory patients to safe area in cold zone Move non‐ambulatory patients to transportation as rapidly as possible. Establish treatment areas only if there are insufficient transport resources available for rapid transport. Consider public transportation to alternative receiving facility for ambulatory patients Service MD Approval:______ Pearls Task cards and job vest should be utilized by all personnel involved in a MCI If blast injury with more than 5 patients, patient with SBP<90 and/or obvious external trauma to 4 or more body surface areas should go to the Level 1 Trauma Center. Other may be considered for transport to the other area hospitals. Multiple patients may be transported in the same EMS unit if needed. When possible, patients of similar acuity should be transported in the same unit to assist with appropriate transport destination. Utilize state/local approved triage system. Procedure 24 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 234 Procedure Purpose: Administration of medication via a non-invasive route Clinical Indications: Altered mental status, presumed or possible opiate overdose Seizures Pain management EMT A P A‐EMT Paramedic A P Contraindications: DO NOT USE on patient if: Severe nasal/facial trauma Active nasal bleeding or discharge Procedure for medication administration via the MAD®: 1) 2) 3) 4) 5) 6) 7) 8) Determine appropriate dose of medication per protocol Draw medication into syringe and dispose of the sharps (add an additional 0.1 ml of medication due to dead space), do not administer more than 1 ml per nostril. Attach Mucosal Atomizer Device (MAD) to syringe With one hand, control the patient’s head Gently introduce MAD into nare, stop when resistance is met. Aim slightly upwards and toward the ear on the same side. Briskly compress the syringe to administer one-half of the medication, repeat the procedure with the remaining medication on the other nare. Document the results in the PCR. Service MD Approval:______ Procedure 25 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 235 Procedure Clinical Indications: Gastric decompression in adult intubated patients After successful placement of an LTA or BIAD Contraindications: History of alkali ingestion, or esophageal disease (ie. stricture or cancer) Comatose state with unprotected airway (as procedure will induce vomiting) Penetrating cervical injuries in the awake trauma patient. EMT A P A‐EMT Paramedic A P Procedure: 1) 2) 3) 4) 5) 6) 7) 8) Measure the length of the tube from the umbilicus to ear lobe to corner of the mouth. Lubricate the tube with a water based lubricant prior to insertion Insert lubricated tube through the gastric port of the LTA or lift tongue/jaw anteriorly while passing tip lateral to endotracheal tube. Continue to advance the tube gently until the appropriate distance is reached. Confirm placement by injecting 20cc of air and auscultate for the whoosh or bubbling of the air over the stomach. If any doubt about placement, remove and repeat the insertion. Secure the tube. Decompress the stomach of air and food by connecting the tube to low continuous suction (green). Document the procedure, time, and result (success) on/with the PCR. EMT-B and EMT-A must have State approval to perform this skill Service MD Approval:______ Procedure 26 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 236 Standards Procedure Purpose: To establish control of the patient's airway and to facilitate ventilation for the listed indications. EMT A P A‐EMT Paramedic Indications: When an alternative airway device is needed in the management of respiratory failure in patients 4 feet tall or greater Contraindications: Intact gag reflex Patients with known esophageal disease Patients who have ingested caustic substances Patient with known tracheal obstruction Patient with a tracheostomy or laryngectomy Patients less than 4 feet tall. Equipment: Correctly sized LTA (see chart below) Bag valve mask Oxygen reservoir Suction device Bite block and/or endotracheal tube holder (if available) Appropriately sized syringes for expanding cuff End Tidal CO2 and oxygen saturation monitoring devices Airway Size Connector Color 3 Yellow 4 Red 5 Purple King LTS-D Airway Sizes Patient Height OD/ID (mm) 4‐5 feet 18/10mm 5‐6 feet 18/10 >6 feet 18/10 Cuff Volume (ml) 45‐60 ml 60‐90 70‐90 Gastric Tube (Fr.) Up to 18 Up to 18 Up to 18 Procedure: 1) Pre-oxygenate patient with 100% Oxygen via Bag Valve Mask or spontaneous ventilation to achieve O2 saturation of >93% if possible 2) Check the integrity of the cuff inflation system and pilot balloon 3) Tightly deflate the cuff with the syringe 4) Lubricate the posterior distal tip of the LTA with a water soluble lubricant 5) Place patient in neutral sniffing position (if no c-spine/spinal injury suspected) □ For patients with suspected c-spine injury, perform two-person insertion technique • One person maintains manual in-line cervical spine stabilization while the other person proceeds with procedure Service MD Approval:______ Procedure 27-1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 237 A P Procedure EMT Procedure (Continued): A‐EMT A A 6) Pull mandible down to open mouth P 7) Insert uninflated LTA into oral cavity with midline or a lateral technique P Paramedic 8) Advance the tip behind the base of the tongue while rotating tube back to midline so that the blue orientation line faces the chin of the patient. 9) Without exerting excessive force, advance tube until base of the colored connector is aligned with teeth or gums 10) Inflate the King with the appropriate volume: □ If uninflated King Airway insertion is difficult, perform a jaw thrust, pulling the tongue forward. Alternately, a laryngoscope may be used to lift the jaw/mandible to facilitate insertion. 11) Attach the BVM to the King LTSD 12) While bagging the patient, gently withdraw the tube until ventilation becomes easy and free flowing (large tidal volume with minimal airway pressure) 13) Adjust cuff inflation if necessary to obtain a seal of the airway at the peak ventilatory pressure employed. 14) Obtain end-tidal CO2 (waveform), listen for breath sounds bilaterally, look for chest excursion, and check oxygen saturation 15) Secure in the midline to help maintain a good seal over the Larynx 16) Place bite block, oral airway or endotracheal tube holder (if available) between teeth to prevent biting tube. 17) Place orogastric tube and attach to low continuous suction as directed in the applicable procedure to assist in gastric decompression. 18) Ensure c-spine is still immobilized 19) If repeated attempts are made, oxygenate with 100% O2 for 2 minutes between attempts 20) **Follow manufacturers suggested guidelines at all times** Service MD Approval:______ Procedure 27-2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 238 Procedure EMT A P A‐EMT Paramedic A P Service MD Approval:______ Procedure 27-3 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 239 Procedure EMT A P A‐EMT Paramedic A P Service MD Approval:______ Procedure 27-4 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 240 Procedure Indications: Patients with suspected hypoxemia, altered level of consciousness respiratory issues, or as specified in protocol. EMT A P A‐EMT Paramedic A P Procedure: 1) Apply probe to patient’s finger or any other digit as recommended by the device manufacturer. 2) Allow machine to register saturation level. 3) Record time and initial saturation percent on room air if possible on/with the PCR 4) Verify pulse rate on machine or with actual manual pulse check of the patient 5) Monitor critical patients continuously until arrival at the hospital. If recording a one-time reading, monitor patients for a few minutes as oxygen saturation can vary. 6) Document percent of oxygen saturation every time vial signs are recorded and in response to therapy to correct hypoxemia 7) In general, normal saturation is 97-99%. Below 93% suspect a respiratory compromise 8) Use the pulse oximetry as an added tool for patient evaluation. Treat the patient, not the data provided by the device 9) The pulse oximeter reading should never be used to withhold oxygen from a patient in respiratory distress or when it is the standard of care to apply oxygen despite good pulse oximetry readings, such as chest pain. 10) Factors which may reduce the reliability of the pulse oximetry reading include: □ Poor peripheral circulation (blood volume, hypotension, hypothermia) □ Excessive pulse oximeter sensor motion □ Fingernail polish (may be removed with acetone pad) □ Carbon monoxide bound to hemoglobin □ Irregular heart rhythms (atrial fibrillation, SVT, etc.) □ Jaundice □ Placement of BP cuff on same extremity as pulse ox probe Service MD Approval:______ Procedure 29 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 241 Procedure Indications: Age >18 unless specific permission given prior to procedure by Medical Control Need for invasive airway management in the setting of an intact gag reflex or inadequate sedation to perform non‐pharmacologically assisted airway management □ Apnea □ Decreased LOC with respiratory failure (ie. Hypoxia [O2 sat <90%] not improved by 100% Oxygen, and/or respiratory rate <8) □ Poor ventilatory effort (with hypoxia not improved by 100% Oxygen) □ Unable to maintain patent airway by other means □ Burns with suspected significant inhalation injury Contraindications: Sensitivity to Succinylcholine or other RSA drugs Inability to ventilate via BVM Suspected Hyperkalemia Myopathy or neuromuscular disease History of Malignant Hyperthermia Recent crush injury or major burn (>48 hours after injury) End Stage Renal Disease Recent Spinal Cord Injury (72 hours – 6 months) TWO PARAMEDICS REQUIRED FOR THIS PROCEDURE PREPERATION (T-8 minutes) Monitoring (continuous EKG, SPO2, Blood Pressure) Double P Paramedic 2 patent IV’s Functioning Laryngoscope and BVM with highflow O2 Endotracheal tube(s), stylet, syringe(s) LTA(s) and appropriate syringe(s) Alternative/Rescue Airway (LMA and surgical airway kit) immediately available All medications drawn up and labeled (including post-procedure sedation) Suction – turned on and functioning End Tidal CO2 device on and operational (colometric immediately available as backup only) Assess for difficult airway – LEMON PREOXYGENATE 100% O2 x5 minutes (NRB) or 8 vital capacity breaths with 100% O2 (BVM/NRB) PRETREATMENT (T-3 minutes) Evidence of head injury or stroke Lidocaine 1.5mg/kg IV/IO (max 150mg) Begin cricoid pressure / Sellick’s maneuver PARALYSIS and INDUCTION (T=0) Etomidate 0.3mg/kg (max 20mg) Succinylcholine 2 mg/kg (max 200mg) PLACEMENT with PROOF (T+30 seconds) Place LTA/ETT Confirm with: □ End Tidal CO2 Waveform □ Auscultation □ Physical findings Secure device, note position POST-PLACEMENT MANAGEMENT (T+1 minute) Sedation: Morphine 3mg IV/IO AND Midazolam 3mg IV/IO, repeat x2 as needed If additional needed and transport time >10 minutes: Rocuronium 1mg/kg IV/IO Service MD Approval:______ Procedure 30 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 242 P Procedure Clinical Indications: Any patient who may harm himself, herself, or others may be gently restrained to prevent injury to the patient or crew. This restrain must be in a humane manner and used only as a last resort. Other means to prevent injury to the patient or crew must be attempted first. These efforts could include reality orientation, distraction techniques, or other less restrictive therapeutic means. Physical or chemical restraint should be a last resort technique. EMT A P A‐EMT Paramedic Procedure: 1) Attempt less restrictive means of managing the patient. 2) Ensure that there are sufficient personnel available to physically restrain the patient safely 3) A P Restrain the patient in a lateral or supine position. No devices such as backboards, splints, or other devices will be on top of the patient. The patient will never be restrained in the prone position 4) 5) 9) The patient must be under constant observation by the EMS crew at all times. This includes direct visualization of the patient as well as cardiac, pulse oximetry and capnography monitoring as indicated. The extremities that are restrained will have a circulation check at least every 15 minutes. The first of these checks should occur as soon after placement of the restraints as possible. This MUST be documented on the PCR. If the above actions are unsuccessful, or if the patient is resisting the restraints, consider chemical restraint per protocol. If a patient is restrained by law enforcement personnel with handcuffs or other devices EMS personnel cannot remove, a law enforcement officer must accompany the patient to the hospital in the transporting EMS vehicle. Consider Behavioral protocol. 10) Restraining a patient in the prone position is never authorized. 6) 7) 8) Service MD Approval:______ Procedure 31 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 243 Procedure EMT Clinical Indications: Need for spinal immobilization as determined by protocol Procedure: A P A‐EMT Paramedic A P 1) Gather a backboard, straps, c-collar appropriate for patient’s size, tape, and head rolls or similar device to secure the head. 2) Explain the procedure to the patient. 3) Apply an appropriately sized c-collar while maintaining in-line stabilization of the c-spine. This stabilization, to be provided by a second rescuer, should not involve traction or tension but rather simply maintaining the head in a neutral, midline position while the first rescuer applies the collar. This may be performed by any credentialed responder if indicated by protocol. 4) Once the collar is secure, the second rescuer should still maintain their position to ensure stabilization (the collar is helpful, but will not do the job by itself). 5) If the patient is supine or prone, consider the log roll technique. For the patient in a vehicle or otherwise unable to be placed prone or supine, place them on a backboard by the safest method available that maximizes maintenance of in-line spinal stability. 6) Stabilize the patient with straps and head rolls/tape or other similar device. Once the head is secured to the backboard, the second rescuer may release manual in-line stabilization. 7) NOTE: Some patients, due to size or age, will not be able to be immobilized through in-line stabilization with standard backboards and C-collars. Never force a patient into a non-neutral position to immobilize them. Such situation may require a second rescuer to maintain manual stabilization throughout the transport to the hospital. 8) Document the time of the procedure in the PCR. Service MD Approval:______ Procedure 32 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 244 Procedure EMS providers must use extreme caution when evaluating and treating an injured football player, especially when the extent of the injury remains unknown. Suspect any unconscious football player to have an accompanying spinal injury until proven otherwise. If the football player isn’t breathing or the possibility of respiratory arrest exists, its essential that certified athletic trainers and EMS providers work quickly and effectively to remove the face mask and administer care. In most situations, the helmet should not be removed in the field. Proper management of head and neck injuries includes leaving the helmet and shoulder pads in place whenever possible, removing only the face mask from the helmet and developing a plan to manage head-and-neck injured football players using well-trained sports medicine and EMS providers. EMT Guidelines and Recommendations: The following guidelines and recommendations were developed by the Inter-Association Task Force for the Appropriate Care of the Spine-Injured Athlete: A P A‐EMT Paramedic A P General Guidelines for Care Prior to Arrival of EMS □ The Emergency Medical Services system should be activated. □ Any athlete suspected of having a spinal injury should not be moved and should be managed as though a spinal injury exists. □ The athlete’s airway, breathing and circulation, neurological status and level of consciousness should be assessed. □ The athlete should NOT be moved unless absolutely essential to maintain airway, breathing and circulation □ If the athlete must be moved to maintain airway, breathing and circulation, the athlete should be placed in a supine position while maintaining spinal immobilization □ When moving a suspected spine injured athlete, the head and trunk should be moved as a unit. one accepted technique is to manually splint the head to the trunk. Face Mask Removal □ The face mask should be removed prior to transpiration, regardless of current respiratory status (see figure 1) □ Those involved in the pre-hospital care of injured football players must have the tools for face mask removal readily available. Indications for Football Helmet Removal: The athletic helmet and chin straps should only be removed if: □ The helmet and chin strap do not hold the head securely, such that immobilization of the helmet does not also immobilize the head □ The design of the helmet and chin strap is such that even after removal of the face mask the airway cannot be controlled, or ventilation be provided. □ The face mask cannot be removed after a reasonable period of time □ The helmet prevents immobilization fro transportation in an appropriate position. Service MD Approval:______ Procedure 33-1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 245 Procedure EMT A P A‐EMT A P Paramedic Helmet Removal: If it becomes absolutely necessary, spinal immobilization must be maintained while removing the helmet. □ Helmet removal should be frequently practiced under proper supervision by an EMS supervisor or Training Division. □ Due to the varying types of helmets encountered, the helmet should be removed with close oversight by the team athletic trainers and/or sports medicine staff □ In most circumstances, it may be helpful to remove cheek padding and/or deflate air padding prior to helmet removal. Spinal Alignment: Appropriate spinal alignment must be maintained during care and transport using backboard, straps, tape, head blocks or other necessary equipment. □ Be aware that the helmet and shoulder pads elevate an athlete’s trunk when in the supine position □ Should either be removed, or if only one is present, appropriate spinal alignment must be maintained. □ The front of the shoulder pads can be opened to allow access for CPR and defibrillation. Service MD Approval:______ Procedure 33-2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 246 Procedure EMT A P A‐EMT Paramedic A P Clinical Indications: Immobilization of an extremity for transport, either due to suspected fracture, sprain or injury. Immobilization of an extremity for transport to secure medically necessary devices such as intravenous catheters. Procedure: 1) Assess and document pulses, sensation, and motor function prior to placement of the splint. If no pulses are present and a fracture is suspected, consider reduction of the fracture prior to placement of the splint. 2) Remove all clothing from the extremity 3) Select a site to secure the splint both proximal and distal to the area of suspected injury, or the area where the medical device will be placed. 4) Do not secure the splint directly over the injury or device 5) Place the splint and secure with Velcro, straps or bandage material (ie. Kling, kerlex, cloth bandage, etc.) depending on the splint manufacturer and design 6) Document pulses, sensation and motor function after placement of the splint. If there has been a deterioration in any of these 3 parameters, reposition the splint and reassess. If no improvement, remove splint. 7) If a femur fracture is suspected and there is no evidence of pelvic fracture or instability, place a traction splint 8) Consider pain management per protocol 9) Document the time, type of splint, and the pre and post assessment of pulse, sensation and motor function in the PCR. Service MD Approval:______ Procedure 34 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 247 Procedure Clinical Indications: EMT Suspected stroke patient. A P Procedure: A‐EMT Paramedic A P 1) Assess and treat suspected stroke patients as per protocol 2) The Cincinnati Stroke Screen should be completed for all suspected stroke patients 3) Establish the “time last normal” for the patient. This will be the presumed time of onset. 4) Perform the screen through physical exam: □ Look for facial droop by asking the patient to smile □ Have patient, while sitting upright or standing, extend both arms parallel to floor, close eyes, and turn their palms upward. Assess for unilateral drift of an arm. □ Have the person say, "You can't teach an old dog new tricks," or some other simple, familiar saying. Assess for the person to slur the words, get some words wrong, or inability to speak. 5) One of these exam components must be positive to answer “yes” 6) Evaluate Blood Glucose level results 7) If the “time last normal” is less than 24 hours, blood glucose is between 60 and 400, and at least one of the physical exam elements is positive, follow the Suspected Stroke Protocol, alerting the receiving hospital of a possible stroke patient as early as possible. 8) All sections of the Cincinnati screen must be completed. 9) The complete screening should be documented in the PCR. Service MD Approval:______ Procedure 35 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 248 Procedure EMT A P A‐EMT Paramedic Clinical Indications: Monitoring body temperature in a patient with suspected infection, hypothermia, hyperthermia, or to assist in evaluating resuscitation. Procedure: 1) If clinically appropriate, allow the patient to reach equilibrium with the surrounding environment. 2) Leave the device in place until there is indication of an accurate temperature acquisition (per the “beep” or other indicator specific to the device) 3) Record time, temperature, method (tympanic, rectal or oral), and scale (C° or F°) in PCR Service MD Approval:______ Procedure 36 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 249 A P Procedure (CAT‐Combat Application Tourniquet) EMT A P A‐EMT Paramedic A P Clinical Indications: Extremity injury/amputation with uncontrollable hemorrhage despite aggressive direct pressure. Procedure: Apply tourniquet device as proximal on extremity as possible, minimum of 2" proximal to hemorrhage site. (see procedure below) Secure in place and expedite transport to Level 1 Trauma Center Document time placed in patient care report and on device (if possible) Notify receiving center of presence, time placed, and location of tourniquet 1) Route the Self-Adhering Band around the extremity and pass the free-running end of the band through the inside slit of the friction adaptor buckle 2) Pass the band through the outside slit of the buckle, utilizing the friction adaptor buckle which will lock the band in place. Service MD Approval:______ Procedure 14-1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 250 Procedure (CAT‐Combat Application Tourniquet) 3) Pull the Self-Adhering Band tight and securely fasten the band back on itself. EMT A P A‐EMT Paramedic A P 4) Twist the rod until bright red bleeding has stopped. 5) Lock the rod in place with the Windlass Clip™ 6) Hemorrhaging is now controlled. Secure the rod with the strap: Grasp the Windlass Strap™, pull it tight and adhere it to the opposite hook on the Windlass Clip™ **IF needed a second tourniquet can be added more proximal Service MD Approval:______ Procedure 14-2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 251 Procedure EMT A P A‐EMT Paramedic A P Patients with major trauma (one or more of the following) should be transported to UW Hospital: Patient unresponsive to voice and/or GCS <12 Adult unstable vital signs (BP<90mmHg, HR >120 or <60, Respirations <10 or >30) Pediatric unstable vital signs Heart Rate Less than 1 year <90 or >205 1 to 5 years <70 or >140 5 to 12 years <60 or >140 Systolic BP <60 <70 <80 Respirations <20 or >80 <16 or >30 <12 or >30 Clinical signs of shock Penetrating injuries to head, neck, torso, groin or extremity with signs of distal vascular compromise Flail chest or pelvic fracture Burns >15% TBSA and/or airway involvement Two or more proximal long bone fractures (humerus, femur) Signs of spinal cord injury Amputation injuries proximal to the wrist or ankle Significant mechanism of injury in a pregnant patient Consider transport to UW ED for patients with the following mechanisms of injury and medical conditions: Ejection from an automobile during a motor vehicle crash Death of another patient in the same auto Extrication time of greater than 20 minutes Falls: □ Children >10 feet (2-3x’s patient height) □ Adults >20 feet Victim of a high speed auto crash (impact speed of greater than 40 mph, major auto deformity, intrusion of auto damage into the passenger compartment) Auto-pedestrian or auto-bicycle injury with significant (>20mph) speed Pedestrian thrown or run over Motorcycle crash of greater than 20 mph, or separation of rider from bike Age of less than 5 or greater than 55 years old Patient with cardiac or respiratory disease Major trauma patient with immune system problems Major trauma patient with bleeding disorder, or currently taking an anticoagulant medication. Note: Above reference is from the Wisconsin Trauma Field Triage Protocol Service MD Approval:______ Procedure 37 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 252 Procedure P Paramedic P Clinical Indications: Access of an existing venous catheter for medication or fluid administration in a life threatening situation when no other access is available Central venous access in a patient in cardiac arrest Contraindications: Non-externalized ports (subcutaneous or tunneled ports) Procedure: 1) Clean the port of the catheter with alcohol wipe 2) Using sterile technique, withdraw 5-10cc of blood and place syringe in sharps box 3) Using 5cc normal saline, access the port with sterile technique and gently attempt to flush the saline 4) If there is no resistance, no evidence of infiltration (ie. no subcutaneous, collection of fluid), and no pain experienced by the patient, then proceed to step 5. If there is resistance, evidence of infiltration, pain experienced by the patient, or any concern that the catheter may be clotted or dislodged, do not use the catheter. 5) Begin administration of medications or IV fluids slowly. Observe for any signs of infiltration. If difficulties are encountered, stop the infusion and reassess. 6) Record procedure, any complications, and fluids/medications administered in the PCR. Service MD Approval:______ Procedure 38 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 253 Procedure A A‐EMT Clinical Indications: P Paramedic Patients requiring IV medications or fluids Patients with any potential for deterioration (ie. seizures, altered mentation, trauma, chest pain, difficulty) A P Contraindications: Child with partial airway obstruction (ie. Suspected epiglotitis) – when agitation from performing procedure may worsen respiratory difficulty. Equipment: Appropriate tubing or IV lock #14-#24 catheter over the needle, or butterfly needle Venous tourniquet Antiseptic swab Gauze pad or adhesive bandage Tape or other securing device Procedure: 1) Saline locks may be used as an alternative to IV tubing and fluid at the discretion of the paramedic 2) Paramedics and A-EMT can use intraosseous access where threat to life exists as provided for in the Venous Access – Intraosseous procedure. 3) Use the largest catheter bore necessary based upon the patient’s condition and size of veins 4) Fluid and setup choice is preferably: □ Normal Saline with a macro drip (10-gtt/cc) for medical/trauma conditions. □ Normal Saline with a micro drip (60gtt/cc) for medication infusions or for patients where fluid overload is of concern. 5) Assemble IV solution and tubing: □ Open IV bag and check for clarity, expiration date, etc. □ Verify correct solution □ Open IV tubing □ Assemble IV tubing according to manufacturer's guidelines 6) Insertion □ Explain to the patient that an IV is going to be started. □ Place the tourniquet around the patient's arm proximal to the IV site, if appropriate □ Palpate veins for resilience □ Clean the skin with the antiseptic swab in an increasing sized concentric circle and follow it with an alcohol swab □ Stabilize the vein distally with the thumb/fingers □ Enter the skin with the bevel of the needle facing upward □ Enter the vein, obtain a flash, and advance the catheter into the vein while stabilizing the needle. □ Remove the needle while compressing the proximal tip of the catheter to minimize blood loss Continued on next pageService MD Approval:______ Procedure 39-1 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 254 Procedure 6) 7) A A A‐EMT Insertion (continued) P Paramedic P □ Remove the tourniquet □ Connect IV tubing to the catheter, or secure the IV lock to the catheter and flush with appropriate solution (normal saline) □ Open the IV clamp to assure free flow □ Set IV infusion rate. Secure the IV: □ Secure the IV catheter and tubing □ Recheck IV drip rate to make sure it is flowing at appropriate rate. □ Troubleshooting the IV, (if the IV is not working well): • Make sure the tourniquet is off • Check the IV insertion site for swelling • Check the IV tubing clamp to make sure it is open • Check the drip chamber to make sure it is half full • Lower the IV bag below IV site and watch for blood to return into the tubing External Jugular IV Access: Contraindications: ● Anterior neck hematoma ● Anterior neck mass ● Medical appliance in place covering anterior neck ● Previous Surgical Procedure of anterior neck P Paramedic P □ If extremity IV attempts are unsuccessful, reconsider need for IV access. □ If patient hypotensive, but alert and responsive to pain – consider external jugular vein IV access. If patient unstable, go directly to Intraosseous access. □ Monitor for complications ▪ Expanding hematoma ▪ Tracheal shift ▪ Difficulty breathing ▪ Increase in pain Service MD Approval:______ Procedure 39-2 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 255 Procedure Clinical Indications: Patients where rapid, regular IV access if unavailable with any of the following: Cardiac Arrest CCR – IO is preferable Multisystem trauma with severe hypovolemia Severe dehydration with vascular collapse and/or loss of consciousness Respiratory failure/respiratory arrest A P A‐EMT Paramedic A P Contraindications: Fracture proximal to proposed intraosseous site. History of Osteogenesis Imperfecta Current or prior infection at proposed intraosseous site Previous intraosseous insertion or joint replacement at the selected site. Procedure: 1) Identify anteromedial aspect of the proximal tibia (bony prominence below the knee cap). The insertion location will be 1-2 cm (2 finger widths) below this. 2) Cleanse the site 3) For manual pediatric devices, hold the intraosseous needle at a 60-90° angle, aimed away form the nearby joint and epiphyseal plate, twist the needle handle with a rotating grinding motion applying controlled downward force until a “pop” or “give” is felt indicating loss of resistance. Do not advance the needle any further 4) For the EZ-IO intraosseous device, hold the intraosseous needle at a 60-90° angle, aimed away from the nearby joint and epiphyseal plate, power the driver until a “pop” or “give” is felt indicating loss of resistance. Do not advance the needle any further. 5) Remove the stylette and place in an approved sharps container 6) Attach a 12cc syringe filled with 5cc NS; aspirate bone marrow to verify correct placement, then inject 5cc of NS to clear the lumen of the needle. 7) Attach the IV line. Use a pressure bag 8) Stabilize and secure the needle with dressings and tape 9) Paramedics may administer 10-20mg (1-2cc) of 2% Lidocaine in adult patients who experience infusion related pain. 10) Following the administration of IO medications, flush the IO line with 10cc of IV fluid to expedite medication absorption. 11) Document the procedure, time, and result (success) on/with the PCR. Service MD Approval:______ Procedure 40 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 256 Procedure Clinical Indications: Protection of open wounds prior to and during transport EMT A P A‐EMT Paramedic A P Procedure: 1) If active bleeding, elevate the affected area if possible and hold direct pressure. Do not rely on compression bandage to control bleeding. Direct pressure is much more effective. 2) Once bleeding is controlled, irrigate contaminated wounds with saline as appropriate (this may have to be avoided if bleeding was difficult to control). 3) Cover wounds with sterile gauze/dressings. Check distal pulses, sensation, and motor function to ensure the bandage is not too tight. 4) Monitor wounds and/or dressing throughout transport for bleeding 5) Consider tourniquet use as indicated in protocol/procedure 6) Document the wound assessment and care in the PCR Service MD Approval:______ Procedure 41 Any local EMS Agency changes to this document must follow the DCEMS Protocol Change Policy and be approved by WI EMS 257 258 259 Table of Contents: Authorized Pharmaceuticals Overview...................................................................................................... D-3 Adenosine (Adenocard®) ............................................................................. D-4 Albuterol Sulfate (Proventil, Ventolin ) ........................................................ D-5 Amiodarone (Cordarone®) ........................................................................... D-6 Acetylsalicylic Acid (Aspirin®)....................................................................... D-8 Atropine Sulfate (As a Cardiac Agent) ......................................................... D-9 Atropine Sulfate (As an Antidote for Poisonings) ......................................... D-11 Calcium Chloride.......................................................................................... D-13 Dextrose ...................................................................................................... D-14 Diazepam..................................................................................................... D-15 Diltiazem (Cardizem®).................................................................................. D-16 Diphenhydramine Hydrochloride (Benadryl®) .............................................. D-18 Dopamine Hydrochloride (Intropin ®)............................................................ D-20 DuoDote Kit (see Mark 1 Kit) ....................................................................... D-43 Epinephrine Hydrochloride (1:1,000) ........................................................... D-23 Epinephrine Hydrochloride (1:10,000) ....................................................... D-25 Adult Epinephrine Dosing Summary ............................................................ D-27 Pediatric Epinephrine Dosing Summary ...................................................... D-27 Etomidate..................................................................................................... D-28 Famotidine (Pepcid®) ................................................................................... D-29 Fentanyl ....................................................................................................... D-30 Glucagon ..................................................................................................... D-32 Glucose (Oral).............................................................................................. D-33 Haloperidol (Haldol ®)................................................................................... D-34 Hydroxocobalamin (Cyanokit®) ................................................................... D-36 Ipratropium bromide (Atrovent®) .................................................................. D-37 Ketamine...................................................................................................... D-38 Lidocaine Hydrochloride (Xylocaine®).......................................................... D-39 Lorazepam (Ativan ®) ................................................................................... D-40 Magnesium Sulfate ...................................................................................... D-41 Mark 1 Kit..................................................................................................... D-43 Methylprednisolone (Solumedrol®)............................................................... D-44 Midazolam (Versed®) ................................................................................... D-45 Morphine Sulfate.......................................................................................... D-47 Naloxone (Narcan ®) .................................................................................... D-49 Nitroglycerin (Nitrostat ®).............................................................................. D-51 Ondansetron Hydrochloride (Zofran®).......................................................... D-53 Rocuronium ................................................................................................. D-54 Sodium Bicarbonate..................................................................................... D-55 Succinylcholine ............................................................................................ D-56 Vasopressin ................................................................................................. D-59 260 Overview The purpose of this document is to serve as a drug information supplement and to provide a brief description of the prehospital drugs used. This document in no way represents the comprehensive drug knowledge required for use of these medications by paramedic practitioners. The comprehensive information about use of these medications by practicing paramedics, requires reference to other sources, including, but not limited to, pharmacological textbooks, the DOT curriculum, the Physician’s Desk Reference, paramedic text book (e.g. Prehospital Emergency Care, Paramedic Care: Principles and Practice, BTLS, PHTLS), American Heart Association publications (e.g., ACLS, PALS, NALS), etc. Drugs are listed alphabetically, based on their generic names (brand names are shown in parenthesis). Michael T. Lohmeier, MD, FACEP Medical Director Dane County EMS 261 262 263 264 265 266 267 268 269 270 271 272 273 274 275 276 277 278 279 280 281 282 283 284 285 286 287 288 289 290 291 292 293 294 295 296 297 298 299 300 301 302 303 304 305 306 307 308 309 310 311 312 313 314 315 A&Ox3 A&Ox4 A‐FIB AAA ABC ABD ACLS AKA ALS AMA AMS AMT APPROX ASA ASSOC Alert and Oriented to Person, Place and Time Alert and Oriented to Person, Place, Time and Event Atrial Fibrillation Abdominal Aortic Aneurysm Airway, Breathing, Circulation Abdomen Advanced Cardiac Life Support Above the Knee Amputation Advanced Life Support Against Medical Advice Altereed Mental Status Amount Approximately Aspirin Associated BG BILAT BKA BLS BM BP BS BVM Blood Glucose Bilateral Below the Knee Amputation Basic Life Support Bowel Movement Blood Pressure Breath Sounds Bag‐Valve‐Mask C‐SECTION C‐SPINE C/O CA CABG CAD CATH CC CEPH CHF CNS COPD CP CPR CSF CT CVA Caesarean Section Cervical Spine Complains Of Cancer Coronary Artery Bypass Graft Coronary Artery Disease Catheter Chief Complaint Cephalic Congestive Heart Failure Central Nervous System Chronic Obstructive Pulmonary Disease Chest Pain Cardiopulmonary Resuscitation Cerebrospinal Fluid Cat Scan Cerebrovascular Accident (stroke) 316 D5W DKA DNR DOA DT Dx 5% Dextrose in Water Diabetic Ketoacidosis Do Not Resuscitate Dead on Arrival Delirium Tremens Diagnosis EKG EEG ET ETOH ETT EXT Electrocardiogram Electroencephelogram Endotracheal Ethanol (alcohol) Endotracheal Tube External (extension) FB FLEX Fx Foreign Body Flexion Fracture g GI GSW gtts GU GYN gram(s) Gastrointestinal Gunshot Wound drops Gastrourinary gynecology (gynecological) H/A HEENT HR HTN Hx Headache Head, Eyes, Ears, Nose, Throat Heart Rate (hour) Hypertension History ICP ICU IM IV JVD kg KVO Intracranial Pressure Intensive Care Unit Intramuscular Intraveneous Jugular Vein Distension kilogram Keep Vein Open L‐SPINE L/S‐SPINE L&D LAT lb LLQ LMP LOC LR LUQ MAST mcg MED mg MI min MS MVC MVA Lumbar Spine Lumbarsacral spine Labor and Delivery Lateral pound Left Lower Quadrant Last Menstrual Period Level of Consciousness (loss of consciousness) Lactated Ringers Left Upper Quadrant Military anti‐shock trousers microgram(s) Medicine miligram(s) Myocardial Infarction (heart attack) minimum/minute Mental Status Motor Vehicle Crash Motor Vehicle Accident N/V N/V/D NAD NC NEB NKDA NRB NS NSR OB/GYN PALP PAC PE PERRL PMHx PO PRN PT PVC Nausea/Vomiting Nausea/Vomiting/Diarrhea No Apparent Distress Nasal Cannula Nebulizer No Known Drug Allergies Non‐Rebreather Normal Saline Normal Sinus Rhythm Obstetrics/Gynecology Palpation Premature Atrial Contraction Pulmonary Embolus Pupils Equal. Round, Reactive to Light Past Medical History Orally as needed Patient Premature Ventricular Contraction 317 RLQ RUQ Rx Right Lower Quadrant Right Upper Quadrant Medicine S/P SOB SQ ST SVT Sx SZ Status Post Shortness of Breath Subcutaneous Sinus Tachycardia Supraventricular Tachycardia Symptom Seizure T‐SPINE Temp TIA TKO Tx Thoracic Spine Temperature Transient Ischemic Attack To keep Open Treatment UOA URI UTI Upon our Arrival Upper Respiratory Infection Urinatry Tract Infection VF VS VT Ventricular Fibrillation Vital Signs Ventricular Tachycardia WAP WNL Wandering Atrial Pacemaker Within Normal Limits YO (YOA) Years Old (Years of Age) + ‐ ? ~ > < = Positive Negative Questionable Approximately Greater Than Less Than Equal 318 319 12‐Lead EKG 204 Abdominal Pain 23 Acute Dystonic 108 Decontamination 226 Defibrillation ‐ Automated 227 Defibrillation ‐ Manual 228 Adult ‐ Airway Management 30 Destination 11 Adult ‐ Dyspnea 25 DNR 18 Airway Obstruction 205 Endotracheal Tube Indroducer 229 Airway Orotracheal Intubation 206 Envenomations 48 Airway Suctioning ‐ Advanced 211 Excited Delirium 46 Airway Suctioning ‐ Basic 210 External Cardiac Pacing 230 Airway Video Laryngoscopy 208 Extremity Trauma 148 Allergic Reaction 40 Eye Trauma 147 Altered Mental Status 43 GI Bleeding 23 81 Antidepressants 106 Hazardous Material Antipsychotics 108 Head Trauma 144 Asystole 52 Hypertensive 89 Atrial Fibrillation 65 Hyperthermia 91 Atrial Flutter 65 Hypothermia 93 Behavioral 46 Induced Hypothermia 60 Beta Blocker Bites Blood Glucose Analysis Bradycardia 109 48 212 67 Intercept 10 Interfacility 14 Intravenous Access 95, 253, 254, 256 King LTS‐D 237 Burns 140 Labor 102 Calcium Channel Blockers 110 LMA ‐ Laryngeal Mask Airway 231 Carbon Monoxide 111 MAD ‐ Mucosal Atomizer Device 235 Carboxyhemoglobin SpCO Monitoring 213 MCI ‐ Mass Casualty Incident 234 Cardiac Arrest Nerve Agent 87 Cardiac Arrest ‐ Traumatic 151 50 Obstetrics 96 Cardioversion 214 Opiate 114 CCR ‐ Cardiocerebral Resuscitation 215 Organophosphates 107 Chest Decompression 220 Orogastric Tube Insertion 236 Chest Trauma 143 Overdose 104 Pain 115 Chest Pain 77 Childbirth 102 Paramedic Childbirth Complications 222 Pediatric ‐ Burns 196 Childbirth Procedure 221 Pediatric ‐ Airway Management 163 Cholinergic 107 Pediatric ‐ Allergic Reactions 166 Cocaine 113 Pediatric ‐ Altered Mental Status 168 10 CPAP 223 Pediatric ‐ ALTE 170 CPR ‐ Cardiopulmonary Resuscitation 224 Pediatric ‐ Bradycardia 176 Cricothyrotomoy 225 Pediatric ‐ Cardiac Arrest 171 Pediatric ‐ Dyspnea 160 Cyanide 84 Pediatric‐ General 159 Pediatric ‐ Head Injuries 200 Tricyclic 106 Pediatric ‐ Narrow Complex Tachycardia (SV 180 Venous Access ‐ Existing 253 Pediatric ‐ Newborn Resuscitation 183 Venous Access ‐ Extremity 254 Pediatric ‐ Overdose, Poisoning, Or Ingestion 186 Venous Access ‐ Intraosseous 256 Pediatric ‐ Pain Management 188 Ventricular Fibrillation 56 Pediatric ‐ Seizure 191 Wide‐Complex Tachycardia 72 Pediatric ‐ Trauma 194 WMD 87 Pediatric ‐ Wide Complex Tachycardia 179 Wound Care Perinatal Emergencies Pharmaceuticals 96 259 Physician 12 Poisonings 104 Policy Custody 118 Polymorphous Ventricular Tachycardia 75 Post‐Resuscitation 58 Pulse Oximetry Pulseless Electrical Activity (PEA) Radio Report Rapid Sequence Airway Refusal 241 54 15 33, 242 120, 122, 123 Restraints 243 Sedation 124 Seizure 125 Sexual Assault 153 Shock (Non‐Trauma) 128 Spinal Immobilization ‐ Protocol 154, 244 Spinal Immobilization ‐ Football Players 245 Splinting 247 Stroke Supraventricular Tachycardia 131, 248 70 Sympathomimetic 113 Syncope 134 Taser 119 Temperature Measurement 249 Termination of Resuscitation 63 Tetracyclic 106 Tourniquet 250 Trauma 137 Trauma Guidelines 252 257