Tepmetko (Tepotinib) Drug Information: Clinical Pharmacy Assignment
advertisement

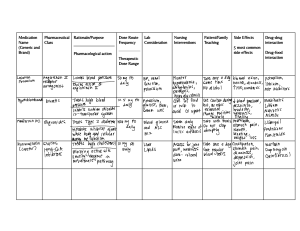
DECCAN SCHOOL OF PHARMACY DAR-US-SALAM, AGHAPURA. HYDERABAD -500 001, TELANGANA. CLINICAL PHARMACY ASSIGNMENT-01 TOPIC: -DRUG INFORMATION QUERY ON TEPMETKO Submitted to: -Ms. Sara Shireen (DEPARTMENT OF PHARMACY PRACTICE) PREPARED BY: HALEEMA SADIA SIDDIQUI REGISTRATION NO: 170722883002 PHARM.D (PB) 1st YEAR TABLE OF CONTENTS S.No List of Contents Page no 1. Drug name information 1 2. Drug class 1 3. Regulatory status 1 4. FDA approval Date 1 5. Manufactured by 1 6. Indication 1 7. Dosage form 1 8. Strength 1 9. Administration 1 10. Dosing 1 11. Contraindications 2 12. Precautions 2 13. Adverse effects 2 14. Pharmacological Properties 3 15. Drug interactions 3 16. Safety studies 4 17. Efficacy studies 4 18. Toxicology studies 5 19. Storage and handling 6 20. Patient counselling information 7 21. Reference 8 TEPMETKO (TEPOTINIB) BRAND NAME: Tepmetko GENERIC NAME: Tepotinib DRUG CLASS: Antineoplastic, Tyrosine Kinase inhibitor REGULATORY STATUS: Rx FDA APPROVAL DATE: February 3rd, 2021 MANUFACTURED BY: Merck KGaA, "EMD Serono Inc”. INDICATION: Treatment of adult patients with metastatic non-small cell lung cancer (NSCLC), Metastatic harbouring mesenchymal-epithelial transition (MET) exon 14 skipping alterations. DOSAGE FORM: Tablet STRENGTH: 225mg ADMINISTRATION: Orally, to swallow tablets whole. Do not chew, crush or split tablets DOSING: Adult Dose: 450 mg (2 tablets) orally once daily with food. If a daily dose is missed, it can be taken as soon as remembered on the same day, unless the next dose is due within 8 hours. Pediatric Dose: The safety and efficacy of Tepotinib in Pediatric patients have not been established. Dose modification for adverse reactions: The recommended dose reduction level for the management of adverse reactions is 225 mg (1 tablet) daily. Detailed recommendations for dose modification are provided in the table CONTRAINDICATIONS: None PRECAUTIONS: Hepatic: Hepatotoxicity: Monitor liver function tests. Withhold, dose reduce, or permanently discontinue TEPMETKO based on the severity. Respiratory: Interstitial Lung Disease (ILD)/Pneumonitis: Immediately withhold TEPMETKO in suspected ILD/pneumonitis patients. Permanently discontinue TEPMETKO in patients diagnosed with ILD/pneumonitis of any severity. Reproductive: Embryo-foetal toxicity: TEPMETKO can cause fetal harm. Advise females of the reproductive potential risk to use of effective contraception during treatment and for 1 week after the final dose. ADVERSE EFFECTS: COMMON: • Cardiovascular: Edema(70%) • Gastrointestinal: Diarrhea (26%) • Nausea (27%) • Musculoskeletal pain (24%) • Respiratory: Dyspnea (20%) • Other: Fatigue (27%) SERIOUS: Hepatic: ALT/SGPT level raised, Hepatotoxicity, increased aspartate transaminase level, liver failure. Respiratory: Interstitial lung disease, pneumonitis, pulmonary embolism. PHARMACOLOGICAL PROPERTIES: Mechanism of action Tepotinib is a reversible Type I adenosine triphosphate (ATP)-competitive small molecule inhibitor of MET. Tepotinib blocks independent MET phosphorylation and MET-dependent downstream signalling such as the phosphatidylinositol 3-kinase/protein kinase B (PI3K/Akt) and mitogenactivated protein kinase/extracellular-signal-regulated kinase (MAPK/ERK) pathways in a dose-dependent manner. Pharmacokinetics: Absorption: • Bioavailability, oral 71.6% • Effects of food: AUC increased 1.6-fold, Cmax increased 2-fold and Tmax shifted from 12 to 8 hours (High-fat, high-calorie meal). • Tmax, oral: 8 hours Distribution: • Protein binding: 98% concentration independent • Volume of distribution (Vd): 1038L Metabolism: • Hepatic, via CYP3A4 and CYP2C8 • Inhibitor of P-gp and BCRP • Substrate of CYP3A4, CYP2C8 and P-gp • Only one major circulating plasma metabolite has been identified, (M506). Excretion: • Total body clearance: 23.8 L/hr • Elimination half-life: 32 hours (oral) Upon giving a radiolabeled dose of 450 mg tepotinib, approximately 85% of the dose was recovered in feces (45% unchanged) and 13.6% in urine (7% unchanged). The major circulating metabolite M506 accounted for about 40.4% of the total radioactivity in plasma. DRUG INTERACTIONS: Dual Strong CYP3A Inhibitors and P-gp Inhibitors: Avoid concomitant use of TEPMETKO with dual strong CYP3A inhibitors and P-gp inhibitorss (e.g. itraconazole, ketoconazole, ritonavir,saquinavir, nelfinavir) Metabolism and in vitro data suggest concomitant use of drugs that are strong CYP3A inhibitors and P-gp inhibitors may increase tepotinib exposure, which may increase the incidence and severity of adverse reactions of TEPMETKO. Strong CYP3A and P-gp Inducers Avoid concomitant use of TEPMETKO with strong CYP3A and P-gp inducers (e.g., carbamazepine, phenytoin, rifampicin, St.John's wort) In vitro data suggest concomitant use may decrease tepotinib exposure which may reduce TEPMETKO efficacy. P-gp substrates Concomitant use of TEPMETKO increases the concentration of P-gp substrates which may increase the incidence and severity of adverse reactions of these substrates. Caution and monitoring for adverse reactions of other P-gp-dependent substances with a narrow therapeutic index (e.g. digoxin, aliskiren, everolimus, sirolimus) is recommended during coadministration with TEPMETKO. BCRP substrates: Tepotinib can inhibit the transport of substrates of the breast cancer resistance protein (BCRP) in vitro. Monitoring for adverse reactions of sensitive BCRP substrates (e.g. rosuvastatin, methotrexate, topotecan) is recommended during co-administration with TEPMETKO. Substrates of OCT and MATE: Based on in vitro data, tepotinib or its metabolite may have the potential to alter the exposure of substrates of the transporters OCT1 and 2 and MATE1 and 2 Example is metformin. Monitoring of the clinical effects of metformin is recommended during co-administration with TEPMETKO. SAFETY STUDIES: In Phase 1 open label trial was conducted to investigate the safety, absolute bioavailability of tepotinib in two groups of healthy male volunteers where one group received single oral dose of tepotinib 500mg and an IV tracer dose of 11.7 ug/ml. The volume of distribution at steady state for oral tepotinib was slightly greater than IV upon studying the PK parameters and the bioavailability for oral administration was found to be 72%. The single oral dose of 500mg of tepotinib was well tolerated. 9 OF 12 Patients experienced 19 TEAEs, 17 of which were of grade 1 severity. No withdrawals, deaths, serious adverse events were reported. This study has demonstrated that a tablet formulation of 500mg once daily has high oral bioavailability supporting its use in phase 2 studies. Low to moderate clearance and high volume of distribution, resulting in long plasma t1/2 . Hepatic elimination is major pathway in humans primarily excreted via faeces only to a minor extent via urine. The results also indicate that the potential for drug-drug interaction affecting PK of tepotinib is low. EFFICACY STUDIES: The efficacy of TEPMETKO was evaluated in a single-arm, open-label, multicenter, nonrandomized, multicohort study (VISION, NCT02864992). Eligible patients were required to have advanced or metastatic NSCLC harboring METex14 skipping alterations, epidermal growth factor receptor (EGFR) wild-type and anaplastic lymphoma kinase (ALK) negative status. Patients with symptomatic CNS metastases, clinically significant uncontrolled cardiac disease, or who received treatment with any MET or hepatocyte growth factor (HGF) inhibitor were not eligible for the study. Patients who received tepotinib for second- or later line therapy (n = 138) had a median age of 71 years (range 41 to 89), 51% were female and 49% male. The majority of patients were white (55%), followed by Asian patients (38%) and were never (54%) or former smokers (29%). Most patients were ≥ 65 years of age (75%) and 36% of patients were ≥ 75 years of age. The majority of patients (96%) had stage IV disease, 80% had adenocarcinoma histology. Thirteen percent of the patients had stable brain metastases. Eighty-six percent of patients had received prior platinum-based cancer therapy and 53% of patients had received immune-based cancer therapy, including 37% of patients who had received immunotherapy as monotherapy. METex14 skipping was prospectively detected by testing from tumour tissue in 43% of patients and by testing from plasma in 36% of patients; 21% of patients tested positive with both methods. Patients received 450 mg tepotinib once daily until disease progression or unacceptable toxicity. Median treatment duration was 6.67 months The major efficacy outcome measure was confirmed overall response rate (ORR) according to Response Evaluation Criteria in Solid Tumors (RECIST) as evaluated by a Blinded Independent Review Committee (BIRC). In conclusion, the findings indicate that the selective MET inhibitor tepotinib demonstrated durable clinical benefit with advanced NSCLC harboring MET exon 14 skipping. TOXICOLOGY STUDIES: The data described below reflect exposure to TEPMETKO 450 mg once daily in 255 patients with metastatic non-small cell lung cancer (NSCLC) with METex14 skipping alterations. Serious adverse reactions occurred in 45% of patients who received TEPMETKO. Adverse Reactions in ≥ 10% of Patients with NSCLC with METex14 Skipping Alterations Who Received TEPMETKO. Select Laboratory Abnormalities (≥ 20%) That Worsened from Baseline in Patients Who Received TEPMETKO Patients with chronic kidney disease should not be given tepotinib decreases albumin and increase creatinine levels which can lead to renal failure. Patients with liver diseases like hepatitis, cirrhosis and other liver disorders should avoid tepotinib as it increases alanine aminotransferase, aspartate aminotransferase, gammaglutamyl transferase. . Pancreatitis patients should not take tepotinib as it increases amylase levels. STORAGE AND HANDLING TEPMETKO (tepotinib) tablets: 225 mg tepotinib, white-pink, oval, biconvex film-coated tablet with embossment “M” on one side and plain on the other side. PATIENT COUNSELING INFORMATION Advise the patient to read the FDA-approved patient labeling (Patient Information). Interstitial Lung Disease (ILD)/Pneumonitis Inform patients of the risk of severe or fatal ILD/pneumonitis. Advise patients to contact their healthcare provider immediately to report new or worsening respiratory symptoms Hepatotoxicity Inform patients that they will need to undergo lab tests to monitor liver function. Advise patients to immediately contact their healthcare provider for signs and symptoms of liver dysfunction Embryo-Fetal Toxicity Advise males and females of reproductive potential that TEPMETKO can cause fetal harm. Advise females of reproductive potential to use effective contraception during and for one week after the final dose of TEPMETKO Advise male patients with female partners of reproductive potential to use effective contraception during treatment with TEPMETKO and for one week after the final dose of TEPMETKO Lactation Advise women not to breastfeed during treatment with TEPMETKO and for one week after the final dose Drug Interactions Advise patients to inform their healthcare provider of all concomitant medications, including prescription medicines, over-the-counter drugs and herbal products Dosing and Administration Instruct patients to take 450 mg TEPMETKO once daily with food Missed Dose Advise patients that a missed dose of TEPMETKO can be taken as soon as remembered on the same day unless the next dose is due within 8 hours. If vomiting occurs after taking a dose of TEPMETKO, advise patients to take the next dose at the scheduled time REFERENCE: IBM Micromedex Drug Reference Kohei Shitara, Kentaro Yamazaki, et al. “Phase I trial of the MET inhibitor Tepotinib in Japanese patients with solid tumors” Japanese Journal of Clinical Oncology, 2020, 1–9. Hiroshi Sakai, Masahiro Morise “Tepotinib in patients with NSCLC harbouring MET exon 14 skipping: Japanese subset analysis from the Phase II VISION study”, Japanese Journal of Clinical Oncology, 2021, 1-9. https://www.fdaaccessdata.gov.in https://www.clinicaltrials.gov.in https://medinfo.emdserono.ca/en/home/oncology/tepmetko.html