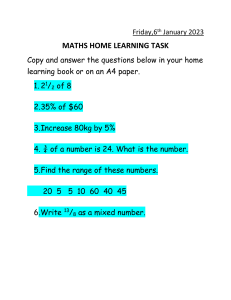
Pre-Simulation Plan of Care COPD Student Name: Naylea Cabral Date: February 6, 2023 Patient Initials: CJ Patient Age: 68 Years Old Admitting Diagnosis: CHF (Congestive Heart Failure) Chief Complaint: Patient is experiencing difficulty breathing Past Medical History: HTN x 10 years, Atrial Fibrillation (AF), CHF x 5 years, hyperlipidemia, and a 20-year history of smoking 1 pack of cigarettes a day. Test & Procedures: CBC - A complete blood count, also known as a full blood count, is a set of medical laboratory tests that provide information about the cells in a person's blood. The CBC indicates the counts of white blood cells, red blood cells and platelets, the concentration of hemoglobin, and the hematocrit. Blood Chemistry Test - A test done on a sample of blood to measure the amount of certain substances in the body. These substances include electrolytes (such as sodium, potassium, and chloride), fats, proteins, glucose (sugar), and enzymes. Blood chemistry tests give important information about how well a person’s kidneys, liver, and other organs are working. An abnormal amount of a substance in the blood can be a sign of disease or side effect of treatment. Blood chemistry tests are used to help diagnose and monitor many conditions before, during, and after treatment. Also called blood chemistry study. Cardiac Enzyme Test - Your heart releases cardiac enzymes when there’s heart damage or stress due to low oxygen. Troponin and creatinine phosphokinase (CPK) levels rise after a heart attack. Elevated heart enzyme levels can also indicate acute coronary syndrome or ischemia. Healthcare providers use enzyme marker tests (blood tests) to measure cardiac enzymes. Echocardiogram - An echocardiogram is an ultrasound and uses sound waves to create pictures of the heart. This common test can show blood flow through the heart and heart valves. Your health care provider can use the pictures from the test to find heart disease and other heart conditions. ECG or EKG - An electrocardiogram records the electrical signals in the heart. It's a common and painless test used to quickly detect heart problems and monitor the heart's health. Chest X-Ray - A chest radiograph, called a chest X-ray is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine. Medications: Medications Indications Significant Side effects Patient’s dose, route and frequency; Normal dose range Nursing responsibilities Generic: Furosemide Indicated to treat CJ for edema related to CHF. Hypotension, headache. Vision problems, hyperglycemia, constipation, fever, and tinnitus. 80mg IV twice a day Assess fluid status. Monitor daily weight, intake and output ratios, amount and location of edema, lung sounds, skin turgor, and mucous membranes. Notify health care professional if thirst, dry mouth, lethargy, weakness, hypotension, or oliguria occurs. Trade: Lasix Classification: Diuretic Normal dose - 20–40 mg, may repeat in 1–2 hours and ↑ by 20 mg every 1–2 hours until response is obtained Patient’s dose is above normal range. Generic: Ramipril Trade: Altace Classification: ACE Inhibitor CJ has a 10x history of HTN. Headache, cough, dizziness, tiredness, nausea, vomiting and stomachache 5mg po daily Normal range is 2.5mg to 20mg per day once Patient is in normal range. Monitor vitals before and administration to detect any changes. during adverse Monitor BP and pulse frequently during initial dose adjustment and periodically during therapy. Notify health care professional of significant changes. Assess patient for signs of angioedema (swelling of face, extremities, eyes, lips, tongue, difficulty in swallowing or breathing); may occur at any time during therapy. Discontinue medication and provide supportive care. Monitor weight and assess patient routinely for resolution of fluid overload (peripheral edema, rales/crackles, dyspnea, weight gain, jugular venous distention). Generic: Carvedilol Trade: Coreg Indicated to CJ to treat heart failure and HTN. Classification: Beta Blocker Fatigue, dizziness, memory loss, pulmonary edema, bradycardia, impaired vision, hypoglycemia, and wheezing. 3.125mg po daily Normal dose range is 6.25mg twice daily or 3.125mg twice daily CJ’d dose is in limits. Generic: Amiodarone CJ has 5x history of atrial fibrillation. Trade: Nexterone Pacerone Classification: Antiarrhythmics Generic: Potassium Chloride Trade: Klor-Con Classification: Electrolytes Indicated to CJ to prevent hypokalemia a common complication of CHF. Cough, fever, dizziness, faint, numbness in fingers, painful breathing, trembling, constipation, headache, nausea. 200mg po daily Nausea, vomiting, diarrhea, and stomachache 40 meq po daily. Normal dose range is 800mg-1600mg po per day Patient’s dose is below normal limits. Normal dose range is 40100 meq per day Patient is in normal range. Monitor the patient’s vital signs frequently and any changes in heart rate and BP. In addition, assess the chest and lungs for any symptoms of pulmonary edema. Monitor intake and output ratios and daily weight. Assess patient routinely for evidence of fluid overload (peripheral edema, dyspnea, rales/crackles, fatigue, weight gain, jugular venous distention). Patients may experience worsening of symptoms during initiation of therapy for heart failure. Monitor patient’s vital signs and ECG for changes in HR and any arrythmias that occurs. Auscultate chest for any abnormalities. Report bradycardia arrhythmias promptly or increase in Observe patient carefully for evidence of electrolyte excess or insufficiency. Monitor lab values before and periodically throughout therapy. Generic: Spironolactone Trade: Aldactone Classification: Diuretics Indicated to CJ to counteract potassium loss caused by other diuretics. Used with other agents to treat edema or hypertension. Drowsiness, dizziness, headache, lightheadedness, and electrolyte disturbance. 12.5mg po daily Normal range is 25200mg daily Patient is below normal range. Monitor patient’s vital signs are within normal range. Must monitor potassium levels and BP. Monitor intake and output ratios and daily weight during therapy. Assess patient frequently for development of hyperkalemia (fatigue, muscle weakness, paresthesia, confusion, dyspnea, ECG changes, cardiac arrhythmias) Generic: Warfarin Trade: Coumadin Jantoven Classification: Anticoagulant Indicated to CJ as prophylaxis treatment to prevent blood clots, DVT and pulmonary embolism as well as management of atrial fibrillation Nausea, dermal necrosis, increased risk of bleeding, fever, and cramps. 2.5mg po daily Normal dose range is 2mg -5mg daily for about 2-4 days. Monitor for clotting factors and any sign of hemorrhaging. Assess for bruises, bleeding gums, distended abdomen, bloody stools. Patient is in normal range. Focused Assessments: Cardiovascular: Patient has history of congestive heart failure for 5 years, high blood pressure for 10 years, and atrial fibrillation. Psychosocial/ Emotional: Not Assessed Respiratory: Safety: CJ is having difficulty breathing. CJ is having difficulty breathing making him a fall risk when ambulating. GU: Not Applicable Patient/Family educational needs: Patient and family must be educated on smoking cessation and provided with outpatient resources to aid in lifestyle change. GI: Not Applicable Musculoskeletal: Not Applicable Endocrine: Not Applicable Medical Plan of Care: Problem 1: CHF (Congestive Heart Failure) Assessment: Patient having difficulty breathing Chest X-Ray, CBC, Blood Chemistry, Echocardiogram, EKG, and Cardiac Enzymes tests ordered by physician – pending results Treatment/Outcomes/Medications: Patient receiving: Lasix 80 mg IV twice daily. Altace 5 mg po daily Coreg 3.125mg po twice daily Amiodarone 200mg po daily K-dur 40 meq po daily Spironolactone 12.5mg po daily Coumadin 2.5 mg po daily Nursing Plan of Care: Assessment: Problem: Include your patient’s defining characteristics, risk factors, Signs, and symptoms (List 3 Diagnoses) NANDA 2-part statement (Diagnostic label related to...) CJ is having difficulty breathing. CJ has 5-year history of CHF. CJ has 5-year history of atrial fibrillation. . Decreased cardiac output related to alterations in rate, rhythm, electrical conduction as evidenced by atrial fibrillation. Patient safety Issues Identify potential complications and explain how it is related to the identified nursing diagnosis Decreased cardiac output may result in insufficient blood supply and compromise vital reactions leading to organ damage. Planned outcomes Implementation Rationale for Interventions Position the patient upright (fowlers or semi-fowlers) if tolerated. Regularly check the patient’s position to prevent sliding down in bed. Elevating the head of the bed will allow the patient better positioning for breathing and be able to maintain an appropriate oxygenation level. Give medications as prescribed, such as beta blockers and ACE inhibitors noting effectiveness and side effects. Medications are prepared to manage specific problems. For CJ his prescriptions will help to improve heart function and decrease patient’s symptoms and cardiac workload. Educate patient about smoking cessation and provide outpatient resources Smoking causes damage to body’s organs and impairs proper function. Long term AND short term goals. Must be measurable including a time frame Patient will demonstrate adequate cardiac output as evidenced by vital signs within acceptable limits, dysrhythmias controlled, and no symptoms of failure by end of shift. Patient will report decreased episodes of dyspnea and angina by end of shift. Long Term – Patient will be able to verbalize future selfcare activities to improve cardiac health such as smoking cessation CJ is having difficulty breathing. Impaired gas exchange related to pulmonary congestion secondary to CHF as evidenced by dyspnea. Potential complications from this nursing diagnosis include inadequate oxygenation, hypoxemia, or hypercapnia Patient will maintain SpO2 above 90% by end of shift Patient’s respiratory pattern will be effective without causing fatigue by end of shift Long Term – Patient will stop smoking and continue respiratory rehabilitation CJ is having difficulty breathing. CJ has 5-year history of CHF. Acute pain related to decreased myocardial blood flow as evidenced by difficulty breathing Potential complications from acute pain are worsening of existing chronic diseases, alterations in HR, BP, and RR. Acute pain will also increase the patient’s risk for falls. Patient’s pain will be decreased by end of shift. The client will report reduced episodes of dyspnea. Administer oxygen as ordered to maintain oxygen saturation above 90%. Position the patient upright (fowlers or semi-fowlers) if tolerated. Regularly check the patient’s position to prevent sliding down in bed. Educate patient about smoking cessation and provide outpatient resources Administer prescribed medications such as vasodilators and pain medication as ordered. Provide comfort measures. Long Term: Patient will be able to ambulate and perform ADLs without pain. Supplemental oxygen improves gas exchange and oxygen saturation. The patient may need a nasal cannula or other devices such as a venturi mask This position promotes better lung expansion and improved air exchange. Smoking causes damage to body’s organs and impairs proper function. The vasodilator nitroglycerin enhances blood flow to the myocardium. It reduces the amount of blood returning to the heart, decreasing preload, decreasing its workload. To provide nonpharmacological pain management options and relieve outside stress factors. Pathophysiology, Medical Treatment, Nursing Management: Heart failure (HF) or Congestive Heart Failure (CHF) is a biological state in which the heart cannot pump enough blood to meet the body’s metabolic due to any structural or functional damage of ventricular filling or ejection of blood. Heart failure results from changes in the systolic or diastolic function of the left ventricle. The heart fails when, because of disease or structural issue it cannot handle a normal blood volume or tolerate a sudden expansion in blood volume. Heart failure is caused by conditions such as chronic hypertension, coronary artery disease, and valvular disease. Heart failure is a progressive and chronic condition managed by lifestyle changes and medical therapy to improve quality of life. Some common medications can include: ACE Inhibitors / Angiotensin II Receptor Blockers – relax blood vessels to lower blood pressure and decrease strain on the heart Beta Blockers – Slow heart rate and reduce blood pressure and can reduce signs and symptoms of heart failure Diuretics – Decrease fluid in the body Aldosterone antagonists - Potassium-sparing diuretics that have additional properties that may help people with severe systolic heart failure live longer. Positive inotropes - Can help the heart pump blood more effectively and maintain blood pressure. Usually given via IV to hospitalized patients. Digoxin – Increases the strength of your heart muscle contractions. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in systolic heart failure. Nursing management for CHF patients would consist of frequent observation and cardiac assessments as well as monitoring of vitals and telemetry. Nurses must administer ordered medications on time and make sure to observe patient for any changes. Pre-Simulation Plan of Care CAD Student Name: Naylea Cabral Date: February 6, 2023 Patient Initials: CS Patient Age: 54 Years Old Admitting Diagnosis: CAD (Coronary Artery Disease) CAD Pathophysiology: Coronary artery disease is a common heart condition. The major blood vessels that supply the heart struggle to send enough blood, oxygen and nutrients to the heart muscle. Cholesterol deposits, called plaques, in the heart arteries and inflammation are usually the cause of coronary artery disease. Medications: Medications Indications Significant Side effects Patient’s dose, route and frequency; Normal dose range Nursing responsibilities 1. Treats severe pain. Nausea, vomiting, constipation, lightheadedness, dizziness or drowsiness may occur. 2.0 mg IV Push Observe for any changes in respiratory rate for respiratory depression. Normal Dosage for adults: Assess lung sounds, pulse, RR and BP before and after administration medication. GenericMorphine Sulfate Morphine will act as an analgesic to reduce pain. Trade MS Contin Morphabond Respiratory depression 2-10mg every 3-4 hours as needed. Patient is in dose range. ClassificationOpioid Analgesic Assess pain level before medication administration. and after 2. Generic – Aspirin / acetylsalicylic acid Trade – Bayer Plus Aspir-Low to treat pain and reduce fever or inflammation. It is sometimes used to treat or prevent heart attacks, strokes, and chest pain (angina). Heartburn, stomachache, nausea, vomiting and irritation. Generic: Nitroglycerin SL Trade: Nitrostat Classification: Vasodilators Normal Dosage for adults: Patient’s dose normal range. To treat angina. Assess pain and limitation of movement; note type, location, and intensity prior to and at the peak following administration of medication 325mg-650mg orally once q4-6h. Classification – NSAID 3. 325mg Chewable Tablet Dizziness, headaches, nausea, burning in tongue, and lightheadedness. is in 1 tablet (1/150gr) sublingual route. Normal Dosage for adults: 2.5 to 6.5 mg 3 to 4 times a day. Patient’s dose is below normal range. Assess patient for chest pain and monitor heart. References: Chronic obstructive pulmonary disease - statpearls - NCBI bookshelf. (n.d.). Retrieved February 7, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK559281/ Mayo Foundation for Medical Education and Research. (2021, December 10). Heart failure. Mayo Clinic. Retrieved February 7, 2023, from https://www.mayoclinic.org/diseases-conditions/heart-failure/diagnosis-treatment/drc-20373148 Mayo Foundation for Medical Education and Research. (2023, January 31). Echocardiogram. Mayo Clinic. Retrieved February 7, 2023, from https://www.mayoclinic.org/tests-procedures/echocardiogram/about/pac-20393856 Mayo Foundation for Medical Education and Research. (2021, May 21). Pneumothorax. Mayo Clinic. Retrieved February 7, 2023, from https://www.mayoclinic.org/diseases-conditions/pneumothorax/symptoms-causes/syc-20350367 Reference ID: 3043802 - food and drug administration. (n.d.). Retrieved February 7, 2023, from https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/202515s000lbl.pdf Vallerand, A. H., & Sanoski, C. A. (2023). Davis's drug guide for Nurses. F.A. Davis. Wikimedia Foundation. (2023, January 29). Complete blood count. Wikipedia. Retrieved February 6, 2023, from https://en.wikipedia.org/wiki/Complete_blood_count Wikimedia Foundation. (2023, February https://en.wikipedia.org/wiki/Chest_radiograph 5). Chest radiograph. Wikipedia. Retrieved February 6, 2023, from