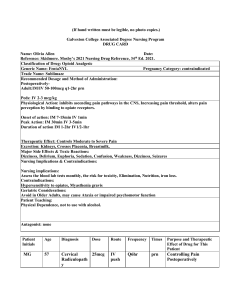
Cardiac Meds Hypertension 1. ACE inhibitors – blocks production of angiotensin II vasodilation, sodium and urine excretion, potassium retention a. “pril” – captopril, enalapril, lisinopril b. Adverse reactions hypotension, rash, dry cough c. Nursing interventions monitor for hyperkalemia d/t potassium retention, poss stop diuretics temporarily, monitor for angioedema d. Administration oral 2-3 times daily, given before meal to increase absorption e. Contraindications not for use on patients w/ decreased renal function f. Interactions potassium sparing diuretics/potassium supplements, nitroglycerin d/t extreme vasodilation (hypotension) 2. Angiotensin II receptor blockers (ARBs) – blocks receptors for angiotensin II vasodilation, sodium and urine excretion, potassium retention a. Similar to ACE inhibitors, but less effective for preventing acute cardiovascular events (MI). b. “artan” – losartan, valsartan, candesartan c. Adverse reactions angioedema, dizziness, hypotension, insomnia d. Nursing interventions monitor BP before administration, monitor for angioedema (treat w/ epinephrine) e. Administration oral only, take with or without food f. Contraindications caution w/ diuretic use, hyperkalemia, and renal issues g. Interactions if given w/ other antihypertensives monitor for hypotension Cardiac Meds 3. Calcium channel blockers – also used for dysrhythmias and angina – blocks calcium channels in vascular smooth muscle vasodilation and lowered blood pressure a. Nifedipine, verapamil b. Adverse reactions reflex tachy and angina, headache, lightheadedness and dizziness d/t vasodilatory effect c. Nursing interventions monitor heart rate, monitor for lightheaded and dizziness, monitor BP and hold if systolic below 90, have regular dental checkups and good oral hygiene d. Administration nifedipine oral, some others can be IV use, do not crush or chew sustained-release forms, may also be administered with a beta blocker to prevent reflex tachycardia e. Contraindications/precautions no grapefruit juice, st johns wort, or use in people who have renal impairment f. Interactions st johns wort decreases affects, grapefruit juice may increase blood levels and antihypertensive effects 4. Alpha 1 blockers – also used for BPH – blocks alpha 1 receptors dilation of target organ a. Doxazosin, prazosin b. Adverse reactions orthostatic hypotension, reflex tachycardia (natural response to sudden drop in BP) c. Nursing interventions monitor headaches and for reflex tachycardia d. Administration take at bedtime and rise slowly from lying e. Contraindications/precautions caution w/ hepatic disease and geriatric clients f. Interactions use w/ Viagra increases hypotension 5. Beta blockers – also used for angina, dysrhythmias, MI, and heart failure – blocks beta receptors in heart and kidneys decreased release of renin from kidneys and decreased HR and contractility a. “olol” – atenolol, metoprolol, propranolol b. Adverse reactions bradycardia, SOB, coughing especially when laying flat c. Nursing interventions monitor HR (less than 60 report), monitor for SOB, do not stop med suddenly d. Administration oral and IV use, may be enhanced with food, take at same time everyday (before meals or bedtime) e. Contraindications/precautions do not use for bradycardia, or greater than 1st degree heart block, heart failure. Caution with Reynaud’s disease, liver disorders, renal disorders. f. Interactions use with other antihypertensive drugs may increase effects, use with digoxin may increase bradycardia, anticholinergic drugs may decreased beta blocker effects Cardiac Meds 6. Alpha 2 agonists – also used epidural injection and ADHD management – selectively activates alpha 2 receptors in brain reduces BP by reducing sympathetic stimulation a. Clonidine b. Adverse reactions CNS effects like drowsiness and dizziness, as well as dry mouth, rebound hypertension may occur if stopped abruptly c. Nursing interventions monitor for CNS effects, dry mouth will resolve after few weeks, taper slowly d. Administration oral, transdermal patch, give oral at bedtime to reduce drowsiness, apply patch to dry upper outer arm or anterior chest once every 7 days (rotate locations). e. Contraindications/precautions do not use w/ anticoag therapy f. Interactions increased sedation effects of CNS depressants (alcohol, opioids), decreased effects when used with MAO inhibitors, tricyclic antidepressants, and amphetamines 7. Alpha/Beta blockers – also used for heart failure in conjunction with digoxin/ace inhibitors/diuretics – blocks alpha and beta receptors dilation of arterioles, decreased heart rate and contractility, and decreased release of renin decreased resistance of blood vessels, decreased cardiac output, and increased excretion of water and sodium a. “lol – carvedilol, labetalol b. Adverse reactions dizziness, hypotension, bradycardia, postural hypotension c. Interventions monitor BP and report hypotension, report HR below 60 and hold drug d. Administration oral, give with food to minimize hypotension e. Contraindications/precautions do not use with severe unstable HF, asthma, severe bradycardia, or cardiogenic shock f. Interactions use with insulin will alter effectiveness of hypoglycemic meds 8. Vasodilators – also used for HF, angina – dilates arterioles which decreases resistance and blood pressure a. Hydralazine b. Adverse reactions reflex tachycardia, dizziness, weakness, fluid retention and edema, taper when stopping, facial rash, joint pain c. Nursing interventions monitor for tachycardia, monitor for systemic lupus effects, monitor for crackles in lungs (fluid retention) d. Administration oral, IM, IV, oral with food to enhance absorption,, IV undiluted (only use to stop hypertensive crisis so need to monitor BP) e. Interactions severe hypotension with MAOI antidepressants and other hypertensives, NSAIDS may decrease effectiveness