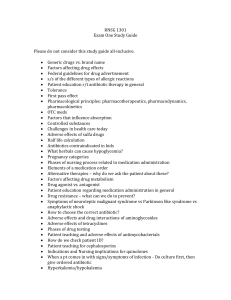
Nursing Process & Drug Therapy: Pharmacology Key Points
advertisement

Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 01: The Nursing Process and Drug Therapy Key Points Overview of the Nursing Process The nursing process is an ongoing, constantly changing, and evolving framework for professional nursing practice. It may be applied to all facets of nursing care, including medication administration. The five phases of the nursing process include assessment; development of nursing diagnoses; planning with outcome identification; implementation, including patient education; and evaluation. Safe, therapeutic, and effective medication administration is a major responsibility of professional nurses as they apply the nursing process to the care of their patients. Critical thinking is a major part of the nursing process and involves the use of the mind and thought processes to gather information and then develop conclusions, make decisions, draw inferences, and reflect on all aspects of patient care. A contemporary trend includes the implementation of Quality and Safety Education for Nurses (QSEN) initiatives in nursing education. The six major initiatives include the following: patient-centered care, teamwork and collaboration, evidence-based practice (EBP), quality improvement (QI), safety, and informatics. Another trend is the development of the Interprofessional Education Collaborative (IPEC), aimed at improving the education of health care professionals and patient care outcomes through collaborative education. Assessment Performing a comprehensive assessment allows you to formulate a nursing diagnosis related to the patient’s needs—specifically, needs related to drug administration. Methods of data collection include interviewing, direct and indirect questioning, observation, medical records review, head-to-toe physical examination, and a nursing assessment. Data are categorized into objective and subjective data. Medication profiles include, but are not limited to, any and all drug use, including home or folk remedies and herbal and/or homeopathic treatments, plant or animal extracts, and dietary supplements; intake of alcohol, tobacco, and caffeine; current or past history of illegal drug use; use of over-the-counter (OTC) medications; use of hormonal drugs; past and present health history and associated drug regimen(s); family history and racial, ethnic, and/or cultural attributes with attention to different responses to medications; Copyright © 2020 Elsevier Inc. All Rights Reserved. 2 growth and developmental stage; and issues related to the patient’s age and medication regimen. Assessment also includes collecting information about a specific drug’s action; signs and symptoms of allergic reactions; adverse effects; dosages and routes of administration; contraindications; drug incompatibilities; drug–drug, drug–food, and drug–laboratory test interactions; and toxicities and available antidotes. Assess whether there are any issues with compliance. o Compliance is the implementation or fulfillment of a prescriber’s or caregiver’s prescribed course of treatment or therapeutic plan by a patient. o Adherence is perceived as implying a more collaborative and active role between patients and their providers. o Noncompliance is an informed decision on the part of the patient not to adhere to or follow a therapeutic plan or suggestion. During assessment, consider the traditional, nontraditional, expanded, and collaborative roles of the nurse and remain current on legal regulations. A prescriber is any health care professional licensed by the appropriate regulatory board to prescribe medications. Planning The major purposes of the planning phase are to prioritize the nursing diagnoses and specify goals and outcome criteria, including the time frame for their achievement. Patient goals reflect objective, realistic, and measurable changes in behavior through nursing care and are developed in collaboration with the patient with an established time period for achievement. Outcome criteria are concrete descriptions of specific patient behaviors or responses that demonstrate meeting of or achievement of goals related to each nursing diagnosis. Outcomes are verifiable, framed in behavioral terms, measurable, and time specific. The ultimate aim of outcome identification, pertinent to drug therapy, is the safe and effective administration of medications. Implementation Implementation is guided by the assessment, nursing diagnoses, and planning. Statements of interventions include frequency, specific instructions, and other information. Nurses are responsible for safe and prudent decision-making in the nursing care of their patients, including the provision of drug therapy. Copyright © 2020 Elsevier Inc. All Rights Reserved. 3 “Nine Rights” of medication administration have been identified as additional standards of care as related to drug therapy, as well as legal and ethical standards related to medication administration and documentation. The registered nurse is responsible for checking all medication orders and/or prescriptions. To ensure that the right drug is given, check the specific medication order against the medication label or profile three times before giving the medication. Always check for the right dose and confirm that it is appropriate for the patient’s age and size, and also check the prescribed dose against the available drug stocks and against the normal dosage range. Medications are to be administered at the right time. Check the health care agency policy regarding routine medication administration times. Give the medications no more than ½ hour before or after the actual time specified in the prescriber’s order. Nursing judgment may lead to some variations in timing, however, any change with the rationale for change must be documented and the prescriber contacted. A complete medication order includes the right route and form of administration. If a medication order does not include the route, never assume the route of administration; ask for clarification. Be certain that you are administering the drug to the right patient by asking the patient to state his or her name, and then checking the patient’s identification band to confirm the patient’s name, identification number, age, and allergies. With newborns and in labor and delivery situations, the mother and baby have identification bracelets with matching numbers, which must be thoroughly and repetitively checked before giving medications. Perform the right documentation. Assess the medical record for the following information: date and time of medication administration, name of medication, dose, route, and site of administration. Documentation of drug action may also be made in the regularly scheduled assessments for changes in symptoms the patient is experiencing, adverse effects, toxicity, and any other drug-related physical and/or psychological symptoms. Right reason or indication refers to the appropriateness in use of the medication to the patient. Right response refers to the drug and its desired response. Continually assess and evaluate the achievement of the desired response as well as any undesired response. The ninth “right” is the right of the patient to refuse. If refusal of a medication occurs, always respect the patient’s right (to refuse), determine the reason, take appropriate action including notifying the prescriber. Document the refusal and a brief, concise description of the reason for refusal. A medication error is defined as any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. Copyright © 2020 Elsevier Inc. All Rights Reserved. 4 Evaluation Evaluation occurs after the nursing care plan has been implemented and is a systematic, ongoing, and dynamic phase of the nursing process as related to drug therapy. It includes monitoring the fulfillment of goals and outcome criteria, as well as monitoring the patient’s therapeutic response to the drug and its adverse effects and toxic effects. Copyright © 2020 Elsevier Inc. All Rights Reserved. 5 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 02: Pharmacologic Principles Key Points Overview The nursing role in drug therapy and the nursing process involve a thorough comprehension of all aspects of pharmaceutics, pharmacokinetics, and pharmacodynamics and the sound application of this drug knowledge to a variety of clinical situations. The nurse’s role in drug therapy and the nursing process as it relates to pharmacologic treatment involve understanding all aspects of pharmaceutics, pharmacokinetics, and pharmacodynamics and application of this drug knowledge to a variety of clinical situations. Nursing considerations vary depending on the drug as well as the route of administration. Pharmacology is defined as the study or science of drugs. Any chemical that affects the physiologic processes of a living organism can broadly be defined as a drug. Throughout the process of its development, a drug will acquire at least three different names. The chemical name describes the chemical composition and molecular structure. The generic name, or nonproprietary name, is shorter and simpler. The trade name, or proprietary name, is the drug’s registered trademark; commercial use is restricted to the owner of the patent. Prototypical drugs are the first drug in a class of drugs. The patent life of a newly discovered drug molecule is normally 17 years, approximately 10 years for research and development and 7 years for sales profit. After the patent expires, generic drugs with the same active ingredient may be produced. The study of the adverse effects of drugs and other chemicals on living systems is known as toxicology. Toxic effects are often an extension of a drug’s therapeutic action. The study of natural drug sources (i.e., plants, animals, minerals) is called pharmacognosy. Pharmacoeconomics focuses on the economic aspects of drug therapy. Pharmaceutics Pharmaceutics is the science of dosage form design. Dosage form determines the rate at which drug dissolution and absorption occur. Copyright © 2020 Elsevier Inc. All Rights Reserved. 6 Dosage forms are designed to achieve a desired therapeutic response with minimal adverse effects; many dosage forms were developed to encourage patient adherence with the medication. Pharmacokinetics Pharmacokinetics is the study of drug distribution among various body compartments after a drug has entered the body, including the phases of absorption, distribution, metabolism, and excretion. A number of dosage formulations are available for delivering medications, but all can be categorized into three basic routes of administration: enteral (GI tract), parenteral, and topical. Pharmacokinetics concerns what happens to a drug from the time it enters the body until the parent drug and all metabolites are excreted. The pharmacokinetic terms absorption, distribution, metabolism, and excretion are used to describe movement of drugs through the body, as well as time to onset of action, time to peak effect, and duration of action. Absorption is the movement of a drug from its site of administration into the bloodstream for distribution to the tissues. Bioavailability is the term used to express the extent of drug absorption. If a large proportion of a drug is chemically changed into inactive metabolites in the liver, then a smaller amount will pass into the circulation; such a drug has a high first-pass effect. First-pass effect reduces the bioavailability of the drug to less than 100%. Many drugs administered by mouth have a bioavailability of less than 100%, whereas drugs administered by the intravenous route are 100% bioavailable. In enteral administration, the drug is absorbed in the mucosa of the stomach or intestines. Drugs administered by the sublingual route are absorbed in the highly vascularized tissue under the tongue—the oral mucosa. The parenteral route is the fastest route for absorption, followed by enteral and topical routes. Parenteral means any route of administration other than the gastrointestinal (GI) tract, usually injection. Drugs can be injected intradermally, subcutaneously, intraarterially, intramuscularly, intrathecally, intraarticularly, or intravenously. Selection of the route of administration is based on patient variables and the specific characteristics of a drug. Intraarterial, intrathecal, or intraarticular injections are usually given by physicians. Medications given by the parenteral route bypass the first-pass effect of the liver, resulting in 100% bioavailability. Copyright © 2020 Elsevier Inc. All Rights Reserved. 7 The topical route of drug administration involves the application of medications to various body surfaces, such as the skin, eyes, ears, nose, lungs, rectum, or vagina. Transdermal drug delivery through adhesive patches is an elaborate topical route of drug administration that is commonly used for systemic drug effects. Inhaled drugs are delivered to the lungs as micrometer-sized drug particles, necessary for the drug to be transported to the small air sacs within the lungs; drug absorption is fairly rapid. Distribution refers to the transport of a drug by the bloodstream to its site of action. Drugs are distributed first to those areas with extensive blood supply. Metabolism is also referred to as biotransformation, involving biochemical alteration into an inactive metabolite, a soluble compound, a potent active metabolite, or less active metabolite. Factors that alter the biotransformation include genetics, diseases, and the concurrent use of other medications. All drugs must eventually be removed from the body by excretion; the primary organ responsible for this elimination is the kidney. Another pharmacokinetic variable is the half-life of the drug, the time required for 50% of a given drug to be removed from the body. Drug effects are the physiologic reactions of the body to the drug. Onset of action is the time required for the drug to elicit a therapeutic response. Peak effect is the time required for a drug to reach its maximum therapeutic response. If the peak blood level is too high, then drug toxicity may occur. Trough level is the lowest blood level of a drug. Duration of action of a drug is the length of time that the drug concentration is sufficient (without more doses) to elicit a therapeutic response. Pharmacodynamics Pharmacodynamics relates to the mechanisms of drug action in living tissues. A positive change in a faulty physiologic system is called a therapeutic effect of a drug. Pharmacotherapeutics Pharmacotherapeutics defines the principles of drug actions—the cellular processes that change in response to the presence of drug molecules. Before drug therapy is initiated, a desired therapeutic outcome, which is patient specific, established in collaboration with the patient and determined with other members of the health care team, is established. Patient therapy assessment is the process by which a practitioner integrates knowledge of medical and drug-related facts with information about a patient’s medical and social history. Copyright © 2020 Elsevier Inc. All Rights Reserved. 8 Considered in the assessment are drugs currently used, pregnancy and breast-feeding status, and concurrent illnesses that could contraindicate initiation of a given medication. A contraindication for a medication is any patient condition, especially a disease state, that makes the use of the given medication dangerous for the patient. Acute therapy often involves intensive drug treatment and is implemented in the acutely ill (those with rapid onset of illness) or even the critically ill to sustain life or treat disease. Maintenance therapy does not eradicate problems the patient may already have but will prevent progression of a disease or chronic condition. Supplemental or replacement therapy supplies the body with a substance needed to maintain normal function, because it cannot be made by the body or is produced in insufficient quantity. Palliative therapy focuses on providing patients with relief from the symptoms, pain, and stress of a serious illness to improve quality of life for both the patient and the family. Supportive therapy maintains integrity of body functions during illness or trauma recovery. Prophylactic therapy is drug therapy provided to prevent illness or other undesirable outcome during planned events. Empiric therapy involves drug administration when a certain pathologic condition has a high likelihood of occurrence based on the patient's initial presenting symptoms. Monitoring Drug actions are related to the pharmacologic, pharmaceutical, pharmacokinetic, and pharmacodynamic properties of a given medication, and each of these has a specific influence on the overall effects produced by the drug in a patient. Evaluating the clinical response requires familiarity with both the drug’s intended therapeutic action (beneficial effects) and unintended possible adverse effects. The ratio of a drug’s toxic level to the level that provides therapeutic benefits is referred to as the drug’s therapeutic index; safety of a particular drug therapy is determined by this index. A low therapeutic index means that the difference between a therapeutically active dose and a toxic dose is small; therefore its use requires closer monitoring. Tolerance is a decreasing response to repeated drug doses. Dependence is a physiologic or psychological need for a drug. Drugs may interact with other drugs, with foods, or with agents administered as part of laboratory tests. Knowledge of drug interactions is vital for the appropriate monitoring. When two drugs with similar actions are given together, they can have additive effects. Copyright © 2020 Elsevier Inc. All Rights Reserved. 9 Synergistic effects occur when two drugs administered together interact in such a way that their combined effects are greater than the sum of the effects for each drug given alone. Antagonistic effects are said to occur when the combination of two drugs results in drug effects that are less than the sum of the effects for each drug given separately. Drug incompatibility occurs when two parenteral drugs or solutions are mixed together and a chemical deterioration of one or both drugs or formation of a physical precipitate occurs. Adverse drug event (ADE) is a broad term for any undesirable occurrence involving medications; a similarly broad term also seen in the literature is drug misadventure. A medication error is a preventable situation involving compromise of the “Six Rights”; they occur during prescribing, dispensing, administering, or monitoring of drug therapy. An adverse drug reaction (ADR) is any reaction to a drug that is unexpected and undesirable and occurs at therapeutic drug dosages; an ADR may or may not be caused by medication errors. An allergic reaction (also known as a hypersensitivity reaction) is an immunologic hypersensitivity reaction resulting from the unusual sensitivity of a patient to a particular medication. An idiosyncratic reaction occurs unexpectedly in a particular patient from a genetically determined abnormal response to normal dosages of a drug. The study of such traits, which are solely revealed by drug administration, is called pharmacogenomics. Drugs that are capable of crossing the placenta can cause drug-induced teratogenesis. Teratogenic effects of drugs or other chemicals result in structural defects in the fetus. Compounds that produce such effects are called teratogens. Copyright © 2020 Elsevier Inc. All Rights Reserved. 10 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 03: Lifespan Considerations Key Points There are many age-related pharmacokinetic effects that lead to dramatic differences in drug absorption, distribution, metabolism, and excretion in the young and the older adult. It is important for the nurse to know that many elements besides the mathematical calculation itself contribute to safe dosage calculations. Safety must remain the first priority and concern with consideration of the Nine Rights of medication administration. From the beginning to the end of life, the human body changes in many ways. These changes have a dramatic effect on the four phases of pharmacokinetics—drug absorption, distribution, metabolism, and excretion. Newborn, pediatric, and older adult patients each have special needs. Drug therapy at the two ends of the spectrum of life is more likely to result in adverse effects and toxicity. Your responsibility is to act as a patient advocate as well as to be informed about growth and developmental principles and the effects of various drugs during the lifespan and in various phases of illness. Drug Therapy During Pregnancy A fetus is exposed to many of the same substances as the mother, including any drugs that she takes—prescription, nonprescription, or street drugs. The first trimester of pregnancy is generally the period of greatest danger of drug-induced developmental defects. Transfer of both drugs and nutrients to the fetus occurs primarily by diffusion across the placenta, although not all drugs cross the placenta. Although exposure of the fetus to drugs is most detrimental during the first trimester, drug transfer to the fetus is more likely during the last trimester. This is the result of enhanced blood flow to the fetus, increased fetal surface area, and increased amount of free drug in the mother’s circulation. The factors that contribute to the safety or potential harm of drug therapy during pregnancy can be broadly broken down into three areas: drug properties, fetal gestational age, and maternal factors. Any change in the mother’s physiology can affect the amount of drug to which the fetus may be exposed. Maternal kidney and liver function affect drug metabolism and excretion. Copyright © 2020 Elsevier Inc. All Rights Reserved. 11 The FDA classifies drugs according to their safety for use during pregnancy based primarily on animal studies and limited human studies, due in part to ethical dilemmas surrounding the study of potential adverse effects on fetuses. The FDA requires new pregnancy labeling to be included in package inserts for all newly approved drugs and allowing currently marketed drugs to be phased in gradually. The new rule requires the use of three subsections in the prescribing information titled “Pregnancy,” “Lactation,” and “Females and Males of Reproductive Potential.” Not all drugs currently on the market have the new information; some inserts will still contain the old categories (A to X). Drug Therapy During Breastfeeding Breastfed infants are at risk for exposure to drugs consumed by the mother. A wide variety of drugs easily cross from the mother’s circulation into the breast milk and subsequently to the breastfeeding infant. Breast milk is not the primary route for maternal drug excretion. Drug levels in breast milk are usually lower than those in the maternal circulation. The actual amount of exposure depends largely on the volume of milk consumed. Whether a breastfeeding mother takes a particular drug depends on the risk/benefit ratio. The risks of drug transfer to the infant in relation to the benefits of continuing breastfeeding and therapeutic benefits to the mother are considered on a case-by-case basis. Considerations for Neonatal and Pediatric Patients Pediatric patients are defined based on age. o A neonate is defined as between birth and 1 month of age. o An infant is between 1 and 12 months of age. o A child is between 1 and 12 years of age. The majority of drug studies have focused on the population between 13 and 65 years of age. It has been estimated that 75% of currently approved drugs lack U.S. Food and Drug Administration (FDA) approval for pediatric use and therefore lack specific dosage guidelines for neonates and children. Pediatric patients metabolize drugs differently than adult patients, based primarily on the immaturity of vital organs. Anatomic structures and physiologic systems and functions of pediatric patients are still developing. Certain drugs may be more toxic, whereas others may be less toxic. The sensitivity of receptor sites may also vary with age; thus, higher or lower dosages may be required depending on the drug. Copyright © 2020 Elsevier Inc. All Rights Reserved. 12 Characteristics of pediatric patients that have a significant effect on dosage include the following: o Skin is thinner and more permeable. o Stomach lacks acid to kill bacteria. o Lungs have weaker mucous barriers. o Body temperature is less well regulated, and dehydration occurs easily. o Liver and kidneys are immature, and, therefore, drug metabolism and excretion are impaired. Formulas involving age, weight, and body surface area (BSA) are most commonly used as the basis for pediatric dosage calculations; BSA-based formulas are the most accurate. To use the BSA method, the nurse needs the following information: o Drug order with drug name, dose, route, time, and frequency o Information regarding available dosage forms o Pediatric patient’s height in centimeters (cm) and weight in kilograms (kg) o BSA nomogram for children o Recommended adult drug dosage Calculating the dosage according to body weight is the most commonly used method today. A common source of medication error and potential toxicity is confusing pounds with kilograms. In calculating pediatric dosages, the factor of organ maturity must always be considered along with body surface area (BSA), age, and weight. Considerations for Older Adult Patients An older adult patient is defined as a person who is 65 years of age or older. The percentage of the population older than 65 years of age continues to grow. Due to the decline in organ function that occurs with advancing age, older adult patients handle drugs physiologically different than adult patients and drug therapy is more likely to result in adverse effects and toxicity. The older adult population consumes a larger proportion of all medications than other population groups, taking 30% of all prescription drugs and over 40% of over-the-counter drugs. At any given time, the average older adult patient takes four or five prescription drugs as well as two over-the-counter medications, which can increase the risk of drug interactions. The simultaneous use of multiple medications is called polypharmacy. Be sure the patient or caregiver understands the dangers of multiple drug use. Copyright © 2020 Elsevier Inc. All Rights Reserved. 13 As the number of medications a person takes increases, so does the risk of drug interaction. Older adult patients are hospitalized frequently due to adverse drug reactions. Many older adults use complementary and alternative medicines such as herbal remedies and dietary supplements, which can interact with prescription drugs. As the body ages, the functioning of several organ systems slowly declines and the collective physiologic changes associated with aging have a major effect on drug disposition and action. More complicated medication regimens predispose older adults to self-medication errors, especially those with reduced visual acuity and manual dexterity. The sensitivity of the older adult patient to many drugs requires careful monitoring and dosage adjustment. In 2012 (and updated in 2015), three categories of medications were identified: (1) potentially inappropriate medications and classes to avoid in older adults, (2) potentially inappropriate medications and classes to avoid in older adults with certain diseases and syndromes, and (3) medications to be used with caution in older adults. Laboratory tests serve as a gauge of organ function for the liver and the kidneys. Advancing age results in reduced absorption of both dietary nutrients and drugs. The concentrations of highly water-soluble (hydrophilic) drugs may be higher in older adult patients because they have less body water in which the drugs can be diluted. Metabolism declines with advancing age. The transformation of active drugs into inactive metabolites is primarily performed by the liver and the liver loses mass with age. Declining renal function, in roughly two thirds of older adult patients, combined with a reduction in cardiac output, can result in delayed drug excretion and therefore drug accumulation. Encourage older adult patients to take medications as directed and not to discontinue them or double up on doses unless recommended or ordered to do so by the provider/prescriber. Drug therapy across the lifespan must be well thought out, with full consideration to the patient’s age, gender, cultural background, ethnicity, medical history, and medication profile. Observation and monitoring for therapeutic effects as well as adverse effects is critical to safe and effective therapy. You must know the patient’s profile and history as well as information about the drug. The drug’s purpose, specific use in the patient, simply stated actions, dose, frequency of dosing, adverse effects, cautions, and contraindications need to be listed and kept available at all times. A current list of all medications and drug allergies must be on their person or with their family/caregiver at all times. Copyright © 2020 Elsevier Inc. All Rights Reserved. 14 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 04: Cultural, Legal, and Ethical Considerations Key Points Cultural Considerations Related to Drug Therapy and Nursing Practice The United States is a very culturally diverse nation as evidenced by its constantly and rapidly changing demographics. The field of ethnopharmacology provides an expanding body of knowledge for understanding the specific impact of cultural factors on patient drug response. Drug therapy and subsequent patient responses may be affected by racial and ethnic variations in levels of specific enzymes and metabolic pathways of drugs. Cultural assessment needs to be part of the assessment phase of the nursing process. A variety of culturally based assessment tools are used in patient care and drug therapy. Acknowledgment and acceptance of the influences of a patient’s cultural beliefs, values, and customs is necessary to promote optimal health and wellness. The concept of polymorphism is critical to an understanding of how the same drug may result in very different responses in different individuals. Factors contributing to drug polymorphism may be categorized into environmental factors (e.g., diet and nutritional status), cultural factors, and genetic (inherited) factors. Medication response depends greatly on the level of compliance; compliance may vary depending on the patient’s cultural beliefs, experiences with medications, personal expectations, family expectations and influence, and level of education. Variations are also reported between ethnic groups in the occurrence of adverse effects. Individuals throughout the world share common views and beliefs regarding health practices and medication use, but specific cultural influences, beliefs, and practices do exist. Attending to each patient’s cultural background helps to ensure safe and quality nursing care, including medication administration. Beliefs vary from patient to patient; therefore, consult with the patient rather than assume that the patient holds certain beliefs because he or she belongs to a certain ethnic group. Barriers to adequate health care for the culturally diverse U.S. patient population include language, poverty, access, pride, and beliefs regarding medical practices. It is important to be knowledgeable about drugs that may elicit varied responses in culturally diverse patients or those from different racial/ethnic groups. Patterns of communication may differ based on a patient’s race or ethnicity. Legal Considerations Related to Drug Therapy and Nursing Practice Copyright © 2020 Elsevier Inc. All Rights Reserved. 15 A balance must be achieved between making new lifesaving therapies available and protecting consumers from potential drug-induced adverse effects. Historically, the Food and Drug Administration (FDA) has had less regulatory authority over vitamin, herbal, and homeopathic preparations because they are designated as dietary supplements rather than drugs. In 1998, Congress established the National Center for Complementary and Alternative Medicine as a new branch of the National Institutes of Health to conduct rigorous scientific studies of alternative medical treatments and to publish the data from such studies. The FDA is responsible for approving drugs for clinical safety and efficacy before they are brought to the market, involving stringent steps, each of which may take years. The FDA has made certain lifesaving investigational drug therapies available sooner than usual by offering an expedited drug approval process, also known as “fast track” approval. The collective goal of these drug-testing phases is to provide information on the safety, toxicity, efficacy, potency, bioavailability, and purity of the new drug. Before any testing on humans begins, the subjects must provide informed consent, and it must be documented. o Informed consent involves careful explanation to the research subject of the purpose of the study, the procedures to be used, the possible benefits, and the risks involved. o Informed consent must be obtained from all patients (or their legal guardians) before they can be enrolled in an investigational new drug (IND) study. o Always obtain informed consent as needed, with complete understanding of your role and responsibilities as patient advocate in obtaining such consent. Phase I studies involve small numbers of healthy subjects rather than those who have the disease or ailment that the new drug is intended to treat. o An exception might be a study involving a very toxic drug used to treat a lifethreatening illness. In this case, the only study subjects might be those who already have the illness and for whom other viable treatment options may not be available. o The purpose of phase I studies is to determine the optimal dosage range and the pharmacokinetics of the drug (i.e., absorption, distribution, metabolism, and excretion) and to ascertain if further testing is needed. Phase II studies involve small numbers of volunteers who have the disease or ailment that the drug is designed to diagnose or treat. o Study participants are closely monitored to determine the drug’s effectiveness and identify any adverse effects. Therapeutic dosage ranges are refined during this phase. Copyright © 2020 Elsevier Inc. All Rights Reserved. 16 Phase III studies involve large numbers of patients who are followed by medical research centers and other types of health care entities. o The purpose of this larger sample size is to provide information about infrequent or rare adverse effects that may not yet have been observed during previous smaller studies. o The three objectives of phase III studies are to establish the drug’s clinical effectiveness, safety, and dosage range. A placebo is an inert substance that is not a drug, given to a portion of the research subjects to separate the real benefits of the investigational drug from the apparent benefits arising out of researcher or subject bias regarding expected or desired results of the drug therapy. Placebo use remains controversial, and if a placebo is ordered, question the prescriber about the specific cause for its use. A study incorporating a placebo is called a placebo-controlled study. If the study subject does not know whether the drug he or she is administered is a placebo or the investigational drug, but the investigator does know, the study is referred to as a blinded investigational drug study. If neither the research staff nor the subjects being tested know which subjects are being given the real drug and which are receiving the placebo, the study is known as a doubleblind investigational drug study. Phase IV studies are postmarketing studies voluntarily conducted by pharmaceutical companies to obtain further proof of the therapeutic and adverse effects of the new drug. o Data from such studies are usually gathered for at least 2 years after the drug’s release. Often the safety and efficacy of the new drug is compared with another drug in the same category. o In rare cases, postmarketing studies are mandated by the FDA. If a pattern of severe reactions to a newly marketed drug begins to emerge, the FDA may request that the manufacturer of the drug issue a black box warning or a voluntary recall. There are three designated classes of drug recall based on FDA response to postmarketing data for a given drug. Various pieces of federal legislation, as well as state law, state practice acts, and institutional policies, have been established to help ensure the safety and efficacy of drug therapy and the nursing process. Federal and state legislation, standards of care, accrediting bodies, and nurse practice acts provide the legal framework for safe nursing practice, including drug administration. Health care facilities must also adhere and/or fulfill specific standards of care and strenuous guidelines to maintain accreditation and from governing bodies such as The Joint Commission (TJC), Healthcare Facilities Accreditation Program (HFAP), Det Norske Veritas (DNV). Copyright © 2020 Elsevier Inc. All Rights Reserved. 17 Health Insurance Portability and Accountability Act (HIPAA) guidelines have increased awareness concerning patient confidentiality and privacy. The Controlled Substances Act of 1970 provides providers with information on drugs that cause little to no dependence versus those with a high level of abuse and dependency. In the IND research process, adhere to the study protocol while also acting as a patient advocate and honoring the patient’s right to safe, quality nursing care. Ethical Considerations as Related to Drug Therapy and Nursing Practice Adhere to legal guidelines, ethical principles, and the American Nurses Association (ANA) Code of Ethics for Nurses so that your actions are based on a solid foundation. The health care team must make a concentrated effort to recognize and understand their own values and be considerate, nonjudgmental, and respectful of the values of others and ethics. The use of drug therapy has evolved from simply administering whatever was prescribed to providing responsible drug therapy for the purpose of achieving defined outcomes that improve a patient’s quality of life. Ethical nursing practice is based on fundamental principles, such as beneficence, autonomy, justice, veracity, and confidentiality. Adherence to these ethical principles and codes of ethics ensures that the nurse is acting on behalf of the patient and with the patient’s best interests at heart. The nurse has the right to refuse to participate in any treatment or aspect of a patient’s care that violates the nurse’s personal ethical principles, without deserting the patient. In instances where refusal of care is not an option, the nurse must always act in the best interest of the patient while remaining an objective patient advocate. Placebos are administered frequently in experimental studies of new drugs to evaluate and measure the pharmacologic effects of a new medicine compared with those of an inert placebo. Except in new drug studies, however, placebo use is often considered unethical and deceitful, possibly creating mistrust among the nurse, the prescriber, and the patient. Nursing Process A thorough cultural assessment is needed for the provision of culturally competent nursing care. There are numerous interventions for implementation of culturally competent nursing care, but one very important requirement is that nurses maintain current knowledge about various cultures and related activities and practices of daily living, health beliefs, and emotional and spiritual health practices and beliefs. Copyright © 2020 Elsevier Inc. All Rights Reserved. 18 Specifically, knowledge about medications that may elicit varied responses due to racial/ethnic variations is most important with application of concepts of culturally competent care and ethnopharmacology to each patient care situation. To ensure a safe, effective, quality, and individualized medication administration process, the nurse must focus the assessment and implementation on all aspects of cultural diversity as well as legal-ethical principles. In the evaluation phase of drug therapy and the nursing process, the nurse must constantly monitor how cultural, legal, and ethical factors lead to the meeting of needs, goals, and outcomes. Copyright © 2020 Elsevier Inc. All Rights Reserved. 19 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 05: Medication Errors: Preventing and Responding Key Points Medication Errors The health care system is very complex and constantly evolving, leading to an increase in the risk for errors. The 1999 Institute of Medicine (IOM) study brought knowledge of medical errors to the public. The number of patient deaths in U.S. hospitals was reported to range from 44,000 to 98,000 annually based on data from two large-scale studies. Similar IOM reports in 2006 and 2010 found no significant change in rates of preventable errors since the original IOM report. One important finding is the notion that most medication errors occur as a breakdown in the medication use system, as opposed to being the fault of the individual. An adverse drug event is a general term that encompasses all types of clinical problems related to medication use. These include medication errors and adverse drug reactions. Adverse drug reactions are reactions that occur with the use of the particular drug. Two types of adverse drug reactions are allergic reaction (often predictable) and idiosyncratic reaction (usually unpredictable). Medication errors are a common cause of adverse health care outcomes and can range from having no significant effect to directly causing patient disability or death. Intangible losses resulting from such adverse outcomes include patient dissatisfaction with, and loss of trust in, the health care system. Medical errors involve all categories of health professionals. In the 2003 IOM Report, “Health Professions Education: A Bridge to Quality”, all educators were challenged to alter the process of professional development so that health care professionals understand the need to continuously improve the quality, safety, and reliability of the health care systems. Competencies related to patient-centered care, interprofessional teamwork and collaboration, evidence-based practice, safety sciences, quality improvement methods, and informatics are essential elements of learning. Many health care institutions have moved from a non-punitive environment to one of “Just Culture.” Just Culture is an environment where, after a systematic review of an error, discipline is applied appropriately. Just Culture recognizes that competent professionals make mistakes but acknowledges that professionals may develop unhealthy habits (i.e., taking shortcuts). Staff members are held accountable for their actions Copyright © 2020 Elsevier Inc. All Rights Reserved. 20 involving such habits. However, when the error is related to a system or process, staff members are held blameless. Issues Contributing to Errors Medication errors can occur at any step in the medication process: procuring, prescribing, transcribing, dispensing, administering, and monitoring. “Near-misses” must also be considered in the process of identifying and addressing medication errors. A near-miss is defined as a situation that is not distinguishable from a preventable adverse event except for the outcome. One study noted that half of all preventable adverse drug events begin with an error at the medication ordering (prescribing) stage. Widely recognized and common causes of errors include misunderstanding of abbreviations, misdiagnosis, patient misidentification, illegibility of prescriber handwriting, miscommunication during verbal or telephone orders, lack of patient monitoring, wrong-site surgery, and confusing drug nomenclature. Errors occurring in homes can be quite harmful as well, as potent drugs once used only in hospitals are now being prescribed for outpatients. The majority of fatal errors at home involve the mixing of prescription drugs with alcohol or other drugs. Medication errors include giving a drug to the wrong patient, administering the wrong drug or wrong dose, giving the drug by the wrong route, and giving the drug at the wrong time. Medication errors also result from the fact that there are large numbers of drugs with similar spelling and/or pronunciation (i.e., look-alike or sound-alike names). Several acronyms have been created to refer to these drugs, including SALAD (sound-alike, lookalike drugs) and LASA (look-alike, sound-alike). Mix-ups between such drugs are most dangerous when two drugs from very different therapeutic classes have similar names. Drugs commonly involved in severe medication errors include central nervous system drugs, anticoagulants, and chemotherapeutic drugs. “High-alert” medications have been identified as those that, because of their potentially toxic nature, require special care when prescribing, dispensing, and/or administering. It is widely recognized that most medication errors result from weaknesses in the systems within health care organizations rather than from individual shortcomings. System weaknesses include failure to create a “just culture” or nonpunitive work atmosphere for reporting errors, excessive workload with minimal time for preventive education, and lack of interdisciplinary communication and collaboration. The Joint Commission began a patient public awareness campaign in 2006 called Speak Up, to encourage patients to take a more active role in their health care by “speaking up” and asking questions whenever they feel the need to do so. Copyright © 2020 Elsevier Inc. All Rights Reserved. 21 Effective use of technologies such as computerized prescriber order entry and bar coding of medication packages has been shown to reduce medication errors. Patient safety begins in the educational process with nursing students and faculty members. Adopting the philosophy that “no question is a stupid question” allows students to begin their careers with greater confidence and with a healthy habit of self-monitoring. Effective communication among all members of the health care team contributes to improved patient care. The most important thing anyone involved in a medication error can do, besides assessing/monitoring the patient, is to report that the error occurred. The Joint Commission requires hospitals to establish procedures for managing disruptive behavior by physicians and others who are granted clinical privileges. Disruptive behavior, as defined by the American Medical Association (AMA), is personal verbal or physical conduct that affects or potentially may affect patient care in a negative fashion. Preventing, Responding to, Reporting, and Documenting Medication Errors: A Nursing Perspective The major categories of medication error are defined by the 2005 National Coordinating Council for Medication Error Reporting and Prevention as (1) no error, although circumstances or events occurred that could have led to an error, (2) medication error that causes no harm, (3) medication error that causes harm, and (4) medication error that results in death. Medication errors may be prevented through a variety of strategies. o To prevent medication errors from misinterpretation of the prescriber’s orders, avoid abbreviations. o Measures to help prevent medication errors include being prepared and knowledgeable and taking time to always triple-check for the right patient, drug, dosage, time, and route. o It is also important for nurses to always be aware of the entire medication administration process and to take a systems analysis approach to medication errors and their prevention. o Use two patient identifiers before giving medications. o The Nine Rights of medication administration should be used consistently, which has been shown to substantially reduce the likelihood of a medication error. o Foster improved communication with other health care team members, including students, and advocate politically for safer conditions for both patients and staff. o Encourage patients to ask questions about their medications and to question any concern about the drug or any component of the medication administration process. Copyright © 2020 Elsevier Inc. All Rights Reserved. 22 o Patients should carry drug allergy information on their persons and keep a current list of medications in their wallets or purses and on their refrigerators, including drug names, reasons for use, usual dosage and dosage prescribed, adverse effects and possible toxicity of the drug, and the prescriber’s name and contact information. o The most common medication errors in pediatrics are dosing errors. Pediatric patients at highest risk of medication errors include: (1) those younger than 2 years of age, (2) those in intensive care units, (3) seriously ill patients in the emergency department between the hours of 4 A.M. and 8 A.M. or on the weekend, (4) those receiving intravenous and/or chemotherapeutic drugs, and (5) those whose weight has not been determined or recorded. Responding to and reporting medication errors are part of the professional responsibilities for which the nurse is accountable. Remember that the nurse’s highest priority at all times during the medication administration process and during a medication error is the patient’s physiologic status and safety. The first priority when an error does occur is to protect the patient from further harm whenever possible. When a medication error has occurred, complete all appropriate forms—including an incident report—as per the facility’s policies and procedures. Report medication errors—include in this documentation assessment of patient status before, during, and after the medication error, as well as specific orders carried out in response to the error. Do not document on the patient’s medical record that an incident report was filled out, and a copy of the incident report should not be kept. All errors should serve as red flags that warrant further reflection, detailed analysis, and future preventive actions on the part of nurses and other health care professionals. Nurses as well as health care facilities may also be involved in external reporting of medication errors. There are nationwide confidential reporting programs that collect and disseminate safety information on a larger scale. Medication reconciliation is a process in which medications are “reconciled” at all points of entry and exit to/from a health care entity. Medication reconciliation requires patients to provide a list of all the medications they are currently taking. Medication reconciliation involves three steps: 1. Verification—Collection of the patient’s medication information with a focus on medications currently used including over-the-counter medications and supplements. 2. Clarification—Professional review of this information to ensure that medications and dosages are appropriate for the patient. 3. Reconciliation—Further investigation of any discrepancies and documentation of relevant communications and changes in medication orders. Copyright © 2020 Elsevier Inc. All Rights Reserved. 23 Other Ethical Issues A 2001 article in the Journal of Clinical Outcomes Management noted the obligation of institutions and providers to provide full disclosure to patients when errors have occurred. Research indicates that such actions help health care organizations to avoid litigation and potentially much larger financial settlements. Medication errors may also affect health care professionals, including nurses and student nurses, in a number of ways. o Nurses may be named as defendants in malpractice litigation. o Disciplinary action, including suspension or termination of employment, may also occur depending on the specific incident. o Nurses who have violated regulations of their state’s nurse practice act may also be counseled or disciplined by their state nursing board, which may suspend or permanently revoke their nursing license. Copyright © 2020 Elsevier Inc. All Rights Reserved. 24 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 06: Patient Education and Drug Therapy Key Points Given the constant change in today’s health care climate and increased consumer awareness, the role of the nurse as an educator continues to increase and remains a significant part of patient care, both in and out of the hospital environment. Professional nurses usually have the most contact with patients and see patients in a variety of settings, and because of this nurses need to be patient advocates and take the initiative to plan, design, create, and present educational materials for teaching about drug therapy. From the time of initial contact with the patient throughout the time you work with the patient, the patient is entitled to all information about medications prescribed as well as other aspects of his or her care. Contributing to the effectiveness of patient education is an understanding of and attention to the three domains of learning: the cognitive, affective, and psychomotor domains; one or a combination of these domains should be addressed in any patient educational session. Teaching and learning principles also must be integrated into patient education plans. You may carefully assess, plan, implement, and evaluate the teaching you provide to help maximize outcome criteria. Evaluation of patient learning is a critical component of safe and effective drug administration. Like the nursing process, the medication administration process and the teaching-learning process provide systematic frameworks for professional nursing practice. Patient education is a qualifier found in professional and accreditation standards including the American Nurses Association document Nursing: Scope and Standards of Practice (2004) and is also one of the grading criteria used by The Joint Commission (2011). An additional accreditation organization, Det Norske Veritas DNV, has also introduced a patient education focused program for the introduction of disease-specific standards and certification programs. Assessment of Learning Needs Related to Drug Therapy As it is related to patient education and drug therapy, the assessment phase includes gathering subjective and objective data about learning needs. Accurate assessment of learning needs and readiness to learn always requires a look at the whole patient, including educational resources, cultural values, health practices, and literacy issues. During the assessment of learning needs, be astutely aware of the patient’s verbal and nonverbal communication. Often patients will not discuss how they truly feel, and a discrepancy in verbal and nonverbal communication warrants investigation. Nursing Diagnoses Related to Learning Needs and Drug Therapy Copyright © 2020 Elsevier Inc. All Rights Reserved. 25 As an example of how nursing diagnoses related to patient education are derived, the nursing diagnosis of deficient knowledge refers to a situation in which the patient, caregiver, or significant other has a limited knowledge base or skills with regard to the medication or medication regimen. Although noncompliance is usually a patient decision, other factors need to be assessed to determine the cause of the noncompliance (e.g., lack of ability of the parent, family, or caregiver to administer the medication; other physical, emotional, or socioeconomic factors). These factors are associated with the nursing diagnosis of ineffective health maintenance and provide a patient-centered approach to the plan of care. Planning: Outcome Identification as Related to Learning Needs and Drug Therapy The planning phase of the teaching-learning process occurs as soon as a learning need has been assessed and then identified in the patient, family, or caregiver. With mutual understanding, the nurse and patient identify goals and outcome criteria that are associated with the identified nursing diagnosis and are able to relate them to the specific medication the patient is taking. Implementation Related to Patient Education and Drug Therapy After you have completed the assessment phase, identified nursing diagnoses, and created a plan of care, the implementation phase of the teaching-learning process begins. This phase includes conveying specific information about the medication to the patient, family, or caregiver. Teaching and learning principles also must be integrated into patient education plans. Evaluation of patient learning is a critical component of safe and effective drug administration. In educational sessions, patients need to receive information through as many senses as possible, such as verbally and visually (e.g., through pamphlets, videotapes, and diagrams), to maximize learning. Information must be presented at the patient’s reading level (in the patient’s native language, if possible) and suitable for the patient’s level of cognitive development. The United States is experiencing increasing diversity and growth in minority populations, with an increase in the percentage of non-English speaking patients. In particular, the increase in the Hispanic population demands that nursing and related health care professions provide patient education materials in both English and Spanish. Be knowledgeable about all available resources for non–English-speaking patients including the use of certified medical interpreters. If you are not able to speak the patient’s native language, a translator needs to be made available to prevent communication problems, minimize errors, and help boost the patient’s level of trust and understanding. Patients who are native English speakers may also have problems learning about their medications and treatment regimens because of learning deficits or difficulties, hearing and speech deficits, lack of education, or minimal previous exposure to treatment Copyright © 2020 Elsevier Inc. All Rights Reserved. 26 regimens and medication use. The teaching of manual skills for specific medication administration is also part of the teaching-learning session. Publications provided for non–English-speaking patients may enable you to convey a sufficient amount of information in the patient's language to help effectively educate the patient while also allowing you to share materials with family members and caregivers for their use. The following strategies may help ensure an effective teaching-learning session: o Begin the teaching-learning process upon patient admission to the health care setting. o Individualize the teaching session to the patient. o Provide positive rewards or reinforcement after accurate return demonstration of a procedure, technique, and/or skill during the teaching session. o Complete a medication calendar that includes the names of the drugs to be taken along with the dosage and frequency. o Allow the patient to see what the medications look like for future reference. o Use audiovisual aids. o Involve family members or significant others in the teaching session, as deemed appropriate. o Keep the teaching on a level that is most meaningful to the patient; research has shown that written materials should be at an eighth-grade reading level. Document the education and include notes about the content provided, strategies used, the patient’s response to the teaching session, and an overall evaluation of learning. Evaluation of Patient Learning Related to Drug Therapy Evaluation of patient learning is a critical component of safe and effective drug administration. To verify the success—or lack of success—of patient education, ask specific questions related to patient outcomes and request that the patient repeat information or give a return demonstration of skills, if appropriate. Evaluation of patient learning and compliance with the medication regimen remains a continuous process and is a critical component of safe and effective drug administration. Be willing to listen to the patient about any aspect of the patient’s drug therapy. Reevaluation of the teaching plan must occur frequently and as needed. Copyright © 2020 Elsevier Inc. All Rights Reserved. 27 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 07: Over-the-Counter Drugs and Herbal and Dietary Supplements Key Points Over-the-Counter Drugs Health care consumers are becoming increasingly involved in the diagnosis and treatment of common ailments. This has led to a great increase in the use of nonprescription or over-the-counter (OTC) drugs. Consumers use herbal products therapeutically for the treatment of diseases and pathologic conditions, prophylactically for long-term prevention of disease, and proactively for the maintenance of health and wellness. More than 80 classes of OTC drugs are marketed to treat a variety of illnesses ranging from acne to cough and cold, pain relief, and weight control. In 1972, the Food and Drug Administration (FDA) initiated an OTC Drug Review to ensure the safety and effectiveness of the OTC products available, as well as to establish appropriate labeling standards. The FDA now requires new stricter “drug facts” labeling for OTC products that includes information on the following: o Purpose and uses of the product o Specific warnings, including when the product should not be used under any circumstances o When it is appropriate to consult a doctor or pharmacist o Side effects that could occur o Substances or activities to avoid o Dosage instructions o Active ingredients, storage information, and inactive ingredients OTC status has many advantages over prescription status. Patients can conveniently and effectively self-treat many minor ailments. A problem associated with OTC drugs is that their use may postpone effective management of chronic disease states and may delay treatment of serious and/or lifethreatening disorders. OTC medication may relieve symptoms without necessarily addressing the cause of the disorder. Toxicity and abuse can be potential hazards with the use of OTC drug products. In 2008, the FDA issued recommendations that OTC cough and cold products not be used in children younger than 2 years of age. Normally, OTC medications are used only for short-term treatment of common minor illnesses. Copyright © 2020 Elsevier Inc. All Rights Reserved. 28 An appropriate medical evaluation is recommended for all chronic health conditions, even if the final decision is to prescribe OTC medications. Health care professionals have an opportunity to prevent common problems associated with the use of OTC drugs, as over 50% of patients consult a health care professional when selecting an OTC product. The importance of patient education cannot be overstated. Provide patients with information about the choice of an appropriate product, correct dosing, common adverse effects, and drug interactions with other medications. Herbal and Dietary Supplements Dietary supplement is a broad term for orally administered alternative medicines and includes the category of herbal supplement. Dietary supplements are products that contain ingredients intended to augment the diet and include vitamins, minerals, herbs or other botanicals, amino acids, and substances such as enzymes, organ tissues, glandular products, metabolites, extracts, and concentrates. Estimates of the prevalence of dietary supplement use differ greatly. Herbs come from nature and include the leaves, bark, berries, roots, gums, seeds, stems, and flowers of plants. Recognition of the increasing use of herbal products and other nontraditional remedies, known as alternative medicine, led to the establishment of the Office of Alternative Medicine by the National Institutes of Health in 1992. This office was later renamed the National Center for Complementary and Alternative Medicine (NCCAM). Complementary medicine refers to the simultaneous use of both traditional and alternative medicine. This practice is also referred to as integrative medicine. NCCAM classifies complementary and alternative medicine into the following five categories: (1) alternative medical systems, (2) mind-body interventions, (3) biologically based therapies, (4) manipulative and body-based methods, and (5) energy therapies. For many years, neither federal legislation nor the FDA provided any safeguards surrounding dietary supplements. Manufacturers were responsible only for ensuring product safety and for not making unproven claims about their efficacy. The 103rd Congress passed the Dietary Supplement and Health Education Act (DSHEA) of 1994. The DSHEA defined dietary supplements and provided a regulatory framework. In 2002, the U.S. Pharmacopeia, an independent organization that is the government’s official standard-setting authority for dietary supplements, began certifying products that it had independently tested as part of its Dietary Supplement Verification Program. A major difference between legend drugs (prescription drugs) and OTC products and dietary supplements is that the DSHEA requires no proof of efficacy and sets no Copyright © 2020 Elsevier Inc. All Rights Reserved. 29 standards for quality control for supplements. In contrast, the FDA has specific and stringent requirements for manufacturers of legend drugs. In June 2007, the FDA announced that all manufacturers of dietary supplements would be required to comply with the same good manufacturing practices, as prescription manufacturers are required to do. Under these new requirements, manufacturers must provide data that demonstrate product identity, composition, quality, purity, and strength of active ingredients. They must also demonstrate that products are free from contaminants such as microbes, pesticides, and heavy metals (e.g., lead). Manufacturers of supplements may currently claim an effect but cannot promise a specific cure on the product label. Dietary supplements do not need approval from the FDA. Consumers use dietary supplements for the treatment and prevention of diseases and proactively to preserve health and wellness and boost the immune system (e.g., reduce cardiovascular risk factors, increase liver and immune system functions, increase feelings of wellness). Consumers use herbal products therapeutically for the treatment of diseases and pathologic conditions, prophylactically for long-term prevention of disease, and proactively for the maintenance of health and wellness. In addition, herbs may be used as adjunct therapy to support conventional pharmaceutical therapies. Herbal products are not FDA-approved drugs, and therefore their labeling cannot be relied on to provide consumers and patients with adequate instructions for use or even information about warnings. The fact that a drug is an herbal product, dietary supplement, or OTC medication is no guarantee that it can be safely administered to children, infants, pregnant or lactating women, or patients with certain health conditions that may put them at risk. Dietary supplements, and especially herbal medicines, are often perceived as being natural and therefore harmless; however, this is not the case. Many examples exist of allergic reactions, toxic reactions, and adverse effects caused by herbs. Health care providers need to develop a clinical knowledge base regarding these products and know where to find key information as the need arises. The FDA has established the MedWatch program, which has a toll-free number (800332-1088). Consumers can call to report adverse effects of prescription drugs, OTC drugs, herbals, and dietary supplements. Nurses may report adverse events anonymously and without consequence via telephone. Adverse event reporting is also available within medical reference applications such as Epocrates or Medscape. Nursing Process Copyright © 2020 Elsevier Inc. All Rights Reserved. 30 Nursing assessments are always important to perform, but they are especially important in situations in which a patient is self-medicating. Responses to drugs—including over-the-counter (OTC) drugs, herbals, and dietary supplements—may be affected by beliefs, values, and genetics as well as by culture, race, and ethnicity. Reading level, cognitive level, motor abilities, previous use of OTC drugs, successes versus failures with drug therapies and self-medication, and caregiver support are just a few of the variables to be assessed, as deemed appropriate. Assessment of the patient’s (or caregiver’s or family member’s) level of knowledge and experience with OTC self-medication is critical to the patient’s safety, as is assessment of attitudes toward and beliefs about their use, especially a too-casual attitude or a lack of respect for and concern about the use of OTC drugs. Many herbals and dietary supplements may lead to a variety of adverse effects. It is also crucial to patient safety to consider any other contraindications, cautions, and potential drug-drug and drug-food interactions. With OTC drugs, herbals, and dietary supplements, patient education is an important strategy to enhance patient safety. o Patients need to receive as much information as possible about the safe use of these products and to be informed that, even though these are not prescription drugs, they are not completely safe and are not without toxicity. o Include information about safe use, frequency of dosing and dose, specifics of how to take the medication (e.g., with food or at bedtime), as well as strategies to prevent adverse effects, drug interactions, and toxicity in the patient instructions. o Patients taking OTC drugs, herbals, and/or dietary supplements need to carefully monitor themselves for unusual or adverse reactions and therapeutic responses to the medication to prevent overuse and overdosing. The range of therapeutic responses will vary, depending on the specific drug and the indication for which it is used. Copyright © 2020 Elsevier Inc. All Rights Reserved. 31 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 10: Analgesic Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Pain is one of the most common reasons that patients seek health care. To provide quality patient care, as a nurse, you must be well informed about both pharmacologic and nonpharmacologic methods of pain management. Pain is an individual experience and involves sensations and emotions that are unpleasant. It is influenced by age, culture, race, spirituality, and all other aspects of the person. Each culture has its own beliefs, thoughts, and ways of approaching, defining, and managing pain. Attitudes, meanings, and perceptions of pain vary with culture, race, and ethnicity. Pain can be defined as whatever the patient says it is, and it exists whenever the patient says it does. Pain is associated with actual or potential tissue damage and may be exacerbated or alleviated depending on the treatment and type of pain. The cause of the pain, the existence of concurrent medical conditions; the characteristics of the pain; and the psychological and cultural characteristics of the patient need to be considered. The level of stimulus needed to produce a painful sensation is referred to as the pain threshold. The patient’s emotional response to the pain is also molded by the patient’s age, sex, culture, previous pain experience, and anxiety level. Whereas pain threshold is the physiologic element of pain, the psychological element of pain is called pain tolerance. This is the amount of pain a patient can endure without its interfering with normal function. Acute pain is sudden and usually subsides when treated. Chronic pain is persistent or recurring, lasting 3 to 6 months. Changes occur in the nervous system that may require increased dosages, known as tolerance or physical dependence. Somatic pain originates from skeletal muscles, ligaments, and joints. Visceral pain originates from organs and smooth muscles. Superficial pain originates from the skin and mucous membranes. Deep pain occurs in tissues below skin level. Vascular pain is believed to originate from the vascular or perivascular tissues and is thought to account for a large percentage of migraine headaches. Referred pain occurs when visceral nerve fibers synapse at a level in the spinal cord close to fibers that supply specific subcutaneous tissues in the body. Neuropathic pain usually results from damage to peripheral or central nervous system (CNS) nerve fibers by disease or injury but may also be idiopathic (unexplained). Copyright © 2020 Elsevier Inc. All Rights Reserved. 32 Phantom pain occurs in the area of a body part that has been removed—surgically or traumatically—and is often described as burning, itching, tingling, or stabbing. Cancer pain can be acute or chronic or both. It most often results from pressure of the tumor mass against nerves, organs, or tissues. Central pain occurs with tumors, trauma, inflammation, or disease (e.g., cancer, diabetes, stroke, multiple sclerosis) affecting CNS tissues. The body is also equipped with certain endogenous neurotransmitters known as enkephalins and endorphins, which are produced within the body to fight pain. Treatment of Pain in Special Situations It is estimated that one of every three Americans experiences ongoing pain. Effective management of acute pain is often different from management of chronic pain in terms of medications and dosages used. Routes of drug administration may include oral, intravenous (IV), intramuscular (IM), subcutaneous (subcut), transdermal, and rectal. Patient-controlled analgesia (PCA) is an intravenous route commonly used in the hospital setting. Deaths have occurred when family members have administered too much of the opioid drug, called PCA by proxy. The Institute for Safe Medication Practices advises against PCA by proxy. Opioid tolerance is a state of adaptation in which exposure to a drug causes changes in drug receptors that result in reduced drug effects over time. Breakthrough pain often occurs between doses of long-acting opioids for pain. Treatment with prn (as needed) doses of immediate-release dosage forms may be given between doses of extended-release dosage forms to relieve breakthrough pain. Adjuvant drugs (from other chemical categories) assist opioids in relieving pain, allowing the use of smaller dosages of opioids and reducing some adverse effects seen with higher dosages of opioids. It permits drugs with different mechanisms of action to produce synergistic effects. US Food and Drug Administration (FDA) strongly encourages drug manufactures to produce long-acting opioids with built in abuse deterrent properties. The three-step analgesic ladder defined by the World Health Organization (WHO) is often applied as the pain management standard for cancer pain. Step 1 is the use of nonopioids (with or without adjuvant medications) once the pain has been identified and assessed. Step 2 is defined as the use of opioids with or without nonopioids and with or without adjuvants. Step 3 is the use of opioids indicated for moderate to severe pain, administered with or without nonopioids or adjuvant medications. Pharmacology Overview Types of analgesics include the following: o Nonopioids, including acetaminophen, aspirin, and nonsteroidal antiinflammatory drugs (NSAIDs) o Opioids, which are natural or synthetic drugs that either contain or are derived from morphine (opiates) or have opiate-like effects or activities (opioids), and opioid agonist-antagonist drugs Copyright © 2020 Elsevier Inc. All Rights Reserved. 33 An agonist binds to an opioid pain receptor in the brain and causes an analgesic response—the reduction of pain sensation. An agonist-antagonist, also called a partial agonist or a mixed agonist, binds to a pain receptor and causes a weaker pain response than does a full agonist. An antagonist is a competitive antagonist that competes with and reverses effects of agonist and agonist-antagonist drugs at the receptor sites. Opioid analgesics are very strong pain relievers. The amount of pain control or unwanted adverse effects depends on the drug, the receptors to which it binds, and its chemical structure. Contraindications to opioid analgesics include known drug allergy and severe asthma. All opioid drugs have a strong abuse potential. They are common recreational drugs of abuse among the lay public and also among health care professionals, who have easy access. The most serious adverse effect of opioid use is CNS depression, which may lead to respiratory depression. All opioid drugs have a strong abuse potential. They are common recreational drugs of abuse among the lay public and also among health care professionals, who often have relatively easy access. The person taking them to alter his or her mental status will soon become psychologically dependent. The FDA now requires a black box warning on all immediate release and long-acting opioids. Naloxone and naltrexone are opioid antagonists, and they bind to and occupy all receptor sites; these are used in the management of opioid overdose and opioid addiction. Two recently approved drugs, Movantik (naloxegol) and Relistor (methylnaltrexone), are indicated specifically for opioid induced constipation. They are usually used in patients taking opioids chronically. Potential drug interactions with opioids are significant. Nursing Process The challenge for the nurse is that pain is a complex and multifaceted problem that requires astute assessment skills with appropriate interventions based on the individual, the specific type of pain, related diseases, and/or health status. Adequate analgesia requires a holistic, comprehensive, and individualized patient assessment with attention to the type, intensity, and characteristics of the pain and the levels of comfort. Perform a thorough health history, nursing assessment, and medication history as soon as possible or upon the first encounter with the patient, including in your assessment the factors or variables that may have an impact on the individual’s pain experience. Assess and document vital signs, including blood pressure, pulse rate, respirations, temperature, and level of pain (the fifth vital sign). A variety of pain assessment tools are available to gather information about pain. At the initiation of pain therapy, conduct a review of all relevant histories, laboratory test values, nurse-related charting entries, and diagnostic study results in the medical record. Copyright © 2020 Elsevier Inc. All Rights Reserved. 34 Develop goals for pain management in conjunction with the patient, family members, significant others, and/or caregiver. Collaborate with other members of the health care team to select a regimen that will be easy for the patient to follow while in the hospital and, if necessary, at home. Begin pain management immediately and aggressively in conformity with the needs of each individual patient and situation. Be aware that most regimens for acute pain management include treatment with shortacting opioids plus the addition of other medications such as NSAIDs. Be familiar with equianalgesic doses of opioids because lack of knowledge may lead to inadequate analgesia or overdose. When opioid analgesics, or any other CNS depressants, are prescribed, focus assessment on vital signs, allergies, respiratory disorders, respiratory function, presence of head injury, neurologic status, gastrointestinal (GI) tract functioning, and genitourinary functioning. In patients taking opioid agonists-antagonists, such as buprenorphine hydrochloride, assess vital signs with attention to respiratory rate and breath sounds. Opioids or any analgesic must be given before the pain reaches its peak to help maximize the effectiveness of the opioid or other analgesic. Crucial safety measures include keeping bed side rails up, turning bed alarms on (depending on the policies and procedures of the facility), and making sure the call bell is within reach. Remember when giving agonists-antagonists that they react very differently depending on whether they are given by themselves or with other drugs. Opioid antagonists must be given as ordered and be readily available, especially when the patient is receiving PCA with an opioid, is opioid naïve, or is receiving continuous opioids. Use an analgesic appropriate for the situation (e.g., short-acting opioids for severe pain secondary to a myocardial infarction, surgery, or kidney stones). For cancer pain, the regimen usually begins with short-acting opioids with eventual conversion to sustained-release formulations. Use preventative measures to manage adverse effects. Consider the option of analgesic adjuvants, especially in cases of chronic pain or cancer pain; these might include other prescribed drugs, over-the-counter drugs, and herbals. Be alert to patients with special needs, such as patients with breakthrough pain. Identify community resources that can assist the patient, family members, and/or significant others. Because fall prevention is of utmost importance in patient care, monitor the patient frequently. Include review of the effectiveness of multimodal and nonpharmacologic approaches to pain management in your evaluation. Pediatric dosages of morphine must be calculated very cautiously with close attention to the dose and kilograms of body weight. Cautious titration of dosage upward is the standard. Older adult patients may react differently than expected to analgesics, especially opioids and opioid agonists-antagonists. Copyright © 2020 Elsevier Inc. All Rights Reserved. 35 In treating older adults, remember that these patients experience pain the same as does the general population, but they may be reluctant to report pain and may metabolize opiates at a slower rate and thus are at increased risk for adverse effects such as sedation and respiratory depression. The best rule is to start with low dosages, reevaluate often, and go slowly during upward titration. Regardless of the drug(s) used for the pain management regimen, individualization of treatment is one of the most important considerations for effective and quality pain control. Copyright © 2020 Elsevier Inc. All Rights Reserved. 36 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 11: General and Local Anesthetics Key Points Anatomy, Physiology, and Pathophysiology Overview Anesthesia is the loss of the ability to feel pain resulting from the administration of an anesthetic drug. General anesthesia is a drug-induced state in which the nerve impulses of the CNS are altered to reduce pain and other sensations throughout the entire body and normally involves complete loss of consciousness and respiratory drive depression. This loss of normal respiratory function requires mechanical or manual ventilatory support to avoid brain damage and suffocation (death from respiratory arrest). Anesthetics are drugs that reduce or eliminate pain by depressing nerve function in the central nervous system (CNS) and/or the peripheral nervous system (PNS). This state of reduced neurologic function is called anesthesia. Anesthesia is the loss of the ability to feel pain resulting from the administration of an anesthetic drug. Local anesthesia does not involve paralysis of respiratory function but does involve elimination of pain sensation in the tissues innervated by anesthetized nerves. Functions of the autonomic nervous system, which is a branch of the parasympathetic nervous system, may also be affected. Monitored Anesthesia Care (MAC) is a planned procedure in which the patient undergoes local anesthesia along with sedation and analgesia. The fundamental elements of MAC include: safe sedation, control of anxiety, and pain control. Patients are able to answer questions appropriately and protect their airways. MAC allows the patient to be discharged as fast as possible. Pharmacology Overview General Anesthetics General anesthetics are drugs that induce general anesthesia and are most commonly used to induce anesthesia during surgical procedures, including the administration of specific parenteral anesthetics. Inhalational anesthetic drugs are also general anesthetics and include volatile liquids or gases. Adjunct anesthetics are drugs that assist with the induction of general anesthesia and include neuromuscular blocking drugs (NMBDs), sedative-hypnotics, and/or anxiolytics and antiemetics. Nondepolarizing NMBDs are used as an adjunct to general anesthesia to provide skeletal muscle relaxation during surgery and/or mechanical ventilation. The overall effect of general anesthetics is a progressive reduction of sensory and motor CNS functions. The degree and speed of this process varies with the anesthetics and adjuncts used along with their dosages and routes of administration. Copyright © 2020 Elsevier Inc. All Rights Reserved. 37 Adverse effects of general anesthetics are dose dependent and vary with the individual drug. The heart, peripheral circulation, liver, kidneys, and respiratory tract are the sites primarily affected. Malignant hyperthermia is an uncommon, but potentially fatal, genetically linked adverse metabolic reaction to general anesthesia. It is classically associated with the use of volatile inhalational anesthetics as well as neuromuscular blocking drugs. In large doses, anesthetics are potentially life threatening, with cardiac and respiratory arrest as the ultimate causes of death. However, these drugs are almost exclusively administered in a very controlled environment by personnel trained in advanced cardiac life support. Drugs for Moderate Sedation Moderate sedation, conscious sedation, and procedural sedation are synonymous terms for anesthesia that does not cause complete loss of consciousness and respiratory arrest. Moderate sedation allows the patient to relax and have markedly reduced or no anxiety, yet still maintain his or her own open airway and response to verbal commands. The most commonly used drugs for moderate sedation include a benzodiazepine, usually midazolam, with an opioid, usually fentanyl or morphine. Local Anesthetics Local anesthetics are the second major class of anesthetics. Local anesthetics are used to induce a state in which peripheral or spinal nerve impulses are altered to reduce or eliminate pain and other sensations. Spinal anesthesia, or regional anesthesia, is a form of local anesthesia. They are also called regional anesthetics because they render a specific part of the body insensitive to pain. They are commonly used in clinical settings in which loss of consciousness is undesirable or unnecessary, such as childbirth and other situations in which spinal anesthesia is desired, dental procedures, suturing of skin lacerations, and diagnostic procedures. Local anesthesia of specific peripheral nerves is accomplished by nerve block anesthesia or infiltration anesthesia. Nerve block anesthesia involves relatively deep injections of drugs into locations adjacent to major nerve trunks or ganglia. The systemic adverse effects depend on where and how the drug is administered. Local anesthetics have little opportunity to cause toxicity under most circumstances. Systemic reactions are possible if sufficiently large quantities are absorbed into the systemic circulation. To prevent this from occurring, a vasoconstrictor such as epinephrine is often co-administered with the local anesthetic to maintain localized drug activity. Knowing the different classes of local anesthetics is important, as patients who are allergic to an ester-type may not be allergic to an amide type local anesthetic. Moderate or Conscious Sedation Conscious or moderate sedation is a form of general anesthesia resulting in partial or complete loss of consciousness but without reducing normal respiratory drive. The American Academy of Pediatrics recommends that moderate or conscious sedation be used to reduce anxiety, pain, and fear in the pediatric patient. Copyright © 2020 Elsevier Inc. All Rights Reserved. 38 The use of moderate sedation in the pediatric patient allows a procedure to be performed restraint free in most situations, while keeping the patient responsive. Neuromuscular Blocking Drugs Neuromuscular blocking drugs (NMBDs) prevent nerve transmission in skeletal and smooth muscles, leading to paralysis. The main therapeutic use of NMBDs is for maintaining skeletal muscle paralysis to facilitate controlled ventilation during surgical procedures. The muscle paralysis induced by depolarizing NMBDs (e.g., succinylcholine) is sometimes preceded by muscle spasms, which may damage muscles. The primary concern when NMBDs are overdosed is prolonged paralysis requiring prolonged mechanical ventilation. Nursing Process It is important to note that anesthetics are not drugs that are typically given by the registered nurse unless the nurse is a licensed nurse anesthetist. Exceptions to this statement are orders for topical forms, such as oral swish-and-swallow solutions that may be used during chemotherapy and lidocaine patches for pain relief. For any form of anesthesia and during any phase of anesthesia, the major parameters to assess are airway, breathing, and circulation (ABCs). Include in your assessment questions regarding allergies and use of prescription as well as over-the-counter drugs, herbals, supplements, and social and/or illegal drugs. The patient’s use of alcohol and nicotine must be assessed. A history of alcohol abuse may result in the development of withdrawal symptoms during recovery from anesthesia and/or surgery. Neurologic assessment includes a thorough survey of the patient’s mental status. Determine and document level of consciousness, alertness, and orientation to person, place, and time prior to the anesthesia. The therapeutic effects of any general or local anesthesia include the following: loss of consciousness and reflexes during general anesthesia and loss of sensation to a particular area during local anesthesia (e.g., loss of sensation to the eye during corneal transplantation). Nursing assessment is very important to patient safety during and after all forms of anesthesia. With general anesthesia, however, one major problem to be concerned with is that of malignant hyperthermia, which may be fatal if not promptly recognized and aggressively treated. The tendency is inherited, so questions about related signs and symptoms in the family’s and patient’s medical histories are important to document and report. Signs and symptoms include rapid rise in body temperature, increased pulse rate (tachycardia)/respiratory rate (tachypnea), muscle rigidity, and unstable blood pressure. The patient who has undergone general anesthesia should be constantly monitored for the occurrence of adverse effects of the anesthesia. These may include myocardial depression, convulsions, respiratory depression, allergic rhinitis, and decreased renal or hepatic function. Copyright © 2020 Elsevier Inc. All Rights Reserved. 39 For patients about to undergo anesthesia with NMBDs, perform a complete head-to-toe assessment with a thorough medical and medication history. With the use of conscious or moderate sedation, as with any anesthesia technique, assessment for allergies, cautions, contraindications, and drug interactions is important. Moderate sedation provides the therapeutic effect of a decreased sensorium but without the complications of general anesthesia; however, there are CNS depressant effects associated with the drugs used. Use of spinal anesthesia requires thorough assessment with an emphasis on the ABCs, respiratory function, and vital signs, specifically blood pressure. With spinal anesthesia, nursing interventions should include constant monitoring for a return of sensation and motor activity below the anesthetic insertion site. Because of the risk that the anesthetic drug may move upward in the spinal cord and breathing may be affected, continually monitor respiratory and breathing status. The use of epidural anesthesia (also called regional anesthesia in some textbooks) does not pose the same risk of respiratory complications, but monitoring is still needed to confirm overall homeostasis, such as measurement of vital signs and pulse oximetry to determine oxygen saturation levels. For those receiving spinal anesthesia, therapeutic effects include loss of sensation below the area of administration, and adverse effects include hypotension, hypoventilation, urinary retention, the possibility of a prolonged period of decreased sensation or motor ability, and infection at the site. With epidural anesthesia, therapeutic effects are similar to those seen with intrathecal anesthesia; however, adverse effects include possible spinal headache (often severe) and/or loss of motor function or sensation below the area of administration. For local anesthesia, review the patient’s medical history to assess for any preexisting illnesses, such as vascular disease, aneurysms, or hypertension, because these may be contraindications to the use of the vasoconstrictor with the anesthetic. In addition, with these local anesthetics, assess for allergies to the drug as well as baseline vital signs. If an anesthetic ointment or cream is used, the nurse will thoroughly cleanse and dry the area to be anesthetized before applying the drug. If a topical or local anesthetic is being used in the nose or throat, remember that it may cause paralysis and/or numbness of the structures of the upper respiratory tract, which can lead to aspiration. Regardless of the type of anesthesia used, one of the most important nursing considerations during the preanesthesia, intraanesthesia, and postanesthesia periods is close and frequent observation of all body systems. Begin with a focus on the ABCs of nursing care, vital signs, and oxygen saturation levels as measured by pulse oximetry as well as by the clinical presentation of the patient. Should the patient require pain management once the anesthesia has been terminated, remember that the anesthetic and any adjuvant drugs used continue to have an effect on the patient until the period of the drugs’ action has passed. Therefore, administer sedative-hypnotics, opioids, nonopioids, and other CNS depressants for pain relief cautiously and only with close monitoring of vital signs. Copyright © 2020 Elsevier Inc. All Rights Reserved. 40 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 12: Central Nervous System Depressants and Muscle Relaxants Key Points Anatomy, Physiology, and Pathophysiology Overview Sedatives and hypnotics are drugs that have a calming effect or that depress the central nervous system (CNS). A drug is classified as either a sedative or a hypnotic drug depending on the degree to which it inhibits the transmission of nerve impulses to the CNS. Sedatives reduce nervousness, excitability, and irritability without causing sleep, but a sedative can become a hypnotic if it is given in large enough doses. Hypnotics cause sleep and have a much more potent effect on the CNS than do sedatives. Many drugs can act as either a sedative or a hypnotic, depending on dose and patient responsiveness, and for this reason are called sedative-hypnotics. Sedative-hypnotics can be classified chemically into three main groups: barbiturates, benzodiazepines, and miscellaneous drugs. Physiology of Sleep Sleep is defined as a transient, reversible, and periodic state of rest in which there is a decrease in physical activity and consciousness. Normal sleep is cyclic and repetitive, and a person’s responses to sensory stimuli are markedly reduced during sleep. Sleep research involves study of the patterns of sleep, or what is sometimes referred to as sleep architecture, consisting of two basic elements that occur cyclically: rapid eye movement (REM) sleep and non–rapid eye movement (non-REM) sleep. Prolonged sedative-hypnotic use may reduce the cumulative amount of REM sleep; this is known as REM interference. This can result in daytime fatigue because REM sleep provides a certain component of the “restfulness” of sleep. Upon discontinuance of a sedative-hypnotic drug, REM rebound can occur in which the patient has an abnormally large amount of REM sleep, often leading to frequent and vivid dreams. Abuse and misuse of sedative-hypnotic drugs is common. Pharmacology Overview Benzodiazepines and Miscellaneous Hypnotic Drugs Benzodiazepines were once the most commonly prescribed sedative-hypnotic drugs; however, the nonbenzodiazepine drugs are now more frequently prescribed. The sedative and hypnotic action of benzodiazepines is related to their ability to depress activity in the CNS. Benzodiazepines are commonly used for sedation, relief of agitation or anxiety, treatment of anxiety-related depression, sleep induction, skeletal muscle relaxation, and treatment of acute seizure disorders. Copyright © 2020 Elsevier Inc. All Rights Reserved. 41 Contraindications to the use of benzodiazepines include known drug allergy, narrowangle glaucoma, and pregnancy. Benzodiazepines have a relatively favorable adverse effect profile; however, they can be harmful if given in excessive doses or when mixed with alcohol. Adverse effects associated with their use usually involve the CNS. Commonly reported undesirable effects are headache, drowsiness, paradoxical excitement or nervousness, dizziness or vertigo, cognitive impairment, and lethargy. Most sedative-hypnotic drugs suppress REM sleep and should be used only for the recommended period of time. This time frame varies, depending on the specific drug used. An overdose of benzodiazepines may result in one or all of the following symptoms: somnolence, confusion, coma, and diminished reflexes. Benzodiazepines and miscellaneous sedative-hypnotic drugs are prescription-only drugs, and they are designated as Schedule IV controlled substances. Long-acting benzodiazepines include clonazepam, diazepam, and flurazepam. Intermediate-acting benzodiazepines include alprazolam, lorazepam, and temazepam. Short-acting benzodiazepines include eszopiclone, midazolam, ramelteon, triazolam, zaleplon, and zolpidem. The newest drugs for insomnia include suvorexant (Belsomra) and tasimelteon (Hetlioz) became available in 2014. Suvorexant is a selective orexin-receptor antagonist. Tasimelteon is indicated only for disturbances of sleep-wake cycle in totally blind patients. Orexin Receptor Antagonists Orexins, also referred to as hypocretins, are neuropeptides that have been shown to regulate transitions between wakefulness and sleep by promoting cholinergic/monoaminergic neural pathways. Orexin antagonists compete with the physiological effects of orexin. Currently, suvorexant is the only orexin receptor antagonist available. Barbiturates Barbiturates were the standard drugs for treating insomnia and producing sedation. Only a few are in use today due to the favorable safety profile and efficacy of the benzodiazepines. Barbiturates are CNS depressants that act primarily on the brainstem in an area called the reticular formation. Recognize and understand the classification and pharmacokinetic properties of barbiturates. Short-acting barbiturates include pentobarbital and secobarbital. Intermediate-acting barbiturates include butabarbital. Long-acting barbiturates include phenobarbital and mephobarbital. The pharmacokinetics of each group of barbiturates lends specific characteristics to the drugs. Health care providers administering them must understand their life-threatening potential because too rapid an infusion may precipitate respiratory or cardiac arrest. Nursing interventions for barbiturates include careful consideration of parenteral administration. Knowledge about incompatibilities with other drugs in solution as well as dilutional fluid incompatibilities is important for safe administration. Copyright © 2020 Elsevier Inc. All Rights Reserved. 42 Barbiturates can produce many unwanted adverse effects. They are physiologically habit forming and have a low therapeutic index. The sedative and hypnotic effects of barbiturates are dose related, and they act by reducing the nerve impulses traveling to the cerebral cortex. All barbiturates have the same sedative-hypnotic effects but differ in their potency, time to onset of action, and duration of action. They can be used as hypnotics, sedatives, and anticonvulsants and for anesthesia during surgical procedures. It is important to note that the use of barbiturates is no longer recommended for sleep induction. Contraindications to barbiturate use include known drug allergy, pregnancy, significant respiratory difficulties, and severe kidney or liver disease. Barbiturates stimulate the action of enzymes in the liver responsible for the metabolism or breakdown of many drugs. By stimulating the action of these enzymes, they cause many drugs to be metabolized more quickly, which usually shortens their duration of action. Adverse effects of barbiturates relate to the CNS and include drowsiness, lethargy, dizziness, hangover, and paradoxical restlessness or excitement. Phenobarbital is also used to treat status epilepticus (prolonged uncontrolled seizures). In extreme cases, patients may be intentionally overdosed to the extent of causing therapeutic phenobarbital or pentobarbital coma. An overdose of barbiturates produces CNS depression ranging from sleep to profound coma and death. Muscle Relaxants A variety of conditions, such as trauma, inflammation, anxiety, and pain, can be associated with acute muscle spasms; muscle relaxant drugs are capable of providing some relief. The muscle relaxants are a group of compounds that act predominantly within the CNS to relieve pain associated with skeletal muscle spasms. Most muscle relaxants are known as centrally acting skeletal muscle relaxants because their site of action is the CNS. Muscle relaxants are most effective when they are used in conjunction with rest and physical therapy. When taken with alcohol, other CNS depressants, or opioid analgesics, enhanced CNS depressant effects are seen. Muscle relaxants are often used for the treatment of muscle spasms, spasticity, and rigidity. They result in varying levels of decreased sensorium and CNS depression, depending on the drug, dosage, and route of administration. They are not used as sedative-hypnotic drugs. The primary adverse effects of muscle relaxants are an extension of their effects on the CNS and skeletal muscles. Euphoria, lightheadedness, dizziness, drowsiness, fatigue, confusion, and muscle weakness are often experienced early in treatment. The toxicities and consequences of an overdose of muscle relaxants primarily involve the CNS. There is no specific antidote (or reversal drug) for muscle relaxant overdoses. Nursing Process Before administering any CNS depressant drug, perform an assessment focusing on insomnia; vital signs; results of a head-to-toe physical examination for baseline Copyright © 2020 Elsevier Inc. All Rights Reserved. 43 comparisons; neurologic findings; miscellaneous information such as medical history; allergies; use of alcohol and smoking history; caffeine intake; past and current medication profile, including use of any prescription drugs, over-the-counter drugs, herbals; alternative or folk practices; and any changes in health status, weight, nutrition, exercise, life stressors, or lifestyle. For muscle relaxants, always note drug allergies before use, and perform a complete head-to-toe assessment with focus on the neurologic system. In the elderly, there is increased risk of CNS toxicity with possible hallucinations, confusion, and excessive sedation. The miscellaneous drug ramelteon (Rozerem) is a newer medication that is used for insomnia but is not associated with CNS depression, does not carry the potential for abuse or dependence, and does not lead to withdrawal symptoms when treatment stops. Therefore, this drug can be used for patients who are likely to be abusers of CNS depressants. Emphasize that the adverse effects of suvorexant, an orexin receptor antagonist, occur more commonly in female patients. Because of its long half-life, emphasize the importance of safety concerns regarding daytime drowsiness/sleepiness and exacerbation of sedation at night. Patients taking benzodiazepines and other CNS depressants experience sedation and possible ataxia, thus the need for patient safety measures. Before giving any CNS depressant, it is always important to try nonpharmacologic measures to induce sleep. If medication therapy is indicated, preventing respiratory depression and other problems associated with CNS depression is of prime importance, as is maintaining patient safety and preventing injury. Some of the criteria by which to confirm a patient’s therapeutic response to a CNS depressant include the following: an increased ability to sleep at night, fewer awakenings, shorter sleep induction time, few adverse effects such as hangover effects, and an improved sense of well-being because of improved sleep. Therapeutic effects related to muscle relaxants include decreased spasticity, reduction of choreiform movements in Huntington’s chorea, decreased rigidity in parkinsonian syndrome, and relief of pain from trigeminal neuralgia. Copyright © 2020 Elsevier Inc. All Rights Reserved. 44 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 44: Antiinflammatory and Antigout Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Inflammation is defined as a localized protective response stimulated by injury to tissues, which serves to destroy, dilute, or wall off both the injurious agent and the injured tissue. Classic signs and symptoms of inflammation include pain, fever, loss of function, redness, and swelling. The inflammatory response is mediated by a host of endogenous compounds, including proteins of the complement system, histamine, serotonin, bradykinin, leukotrienes, and prostaglandins; the latter two are major contributors to the symptoms of inflammation. Pharmacology Overview Nonsteroidal Antiinflammatory Drugs Antiinflammatory drugs include aspirin, NSAIDs, and COX-2 inhibitors. Nonsteroidal antiinflammatory drugs (NSAIDs) are one of the most commonly prescribed categories of drugs. NSAIDs comprise a large and chemically diverse group of drugs that possess analgesic, antiinflammatory, and antipyretic (antifever) activity. In 1899, acetylsalicylic acid (ASA; aspirin) was marketed and rapidly became the most widely used drug in the world. The first drug in this category to be synthesized was salicylic acid or aspirin. Aspirin is often identified as and included in discussion of antiinflammatory drugs. NSAIDs have analgesic, antiinflammatory, and antipyretic activity; aspirin also has antiplatelet activity. Aspirin is used for its effect in inhibiting platelet aggregation, which has been shown to have protective qualities against certain cardiovascular events such as myocardial infarction and stroke. Corticosteroid drugs are also used for similar purposes. NSAIDs have a generally more favorable adverse effect profile than the corticosteroids. NSAIDs are often used in the treatment of gout, osteoarthritis, juvenile arthritis, rheumatoid arthritis, dysmenorrhea, and musculoskeletal injuries such as strains and sprains. They also have proved beneficial as adjunctive pain relief medications in patients with chronic pain syndromes, such as pain from bone cancer and chronic back pain. NSAIDs relieve pain, headache, and inflammation by blocking the chemical activity of the enzyme called cyclooxygenase (COX). In 1998, the newest class of NSAIDs, the COX-2 inhibitors, was approved. Previous NSAIDs nonspecifically inhibited both COX-1 and COX-2 activity. Enzyme specificity of the COX-2 inhibitors allows for beneficial antiinflammatory effects while reducing adverse effects associated with nonspecific NSAIDs, such as gastrointestinal ulceration. All NSAIDs can be ulcerogenic and induce gastrointestinal bleeding due to their activity against tissue COX-1. Copyright © 2020 Elsevier Inc. All Rights Reserved. 45 One notable effect of aspirin is its inhibition of platelet aggregation, also known as its antiplatelet activity. Aspirin has the unique property among NSAIDs of being an irreversible inhibitor of COX-1 receptors within the platelets themselves. For the relief of pain, NSAIDs are sometimes combined with an opioid. They tend to have an opioid-sparing effect when given together with opioids because the drugs attack pain using two different mechanisms. Contraindications to NSAIDs include known drug allergy and conditions that place the patient at risk for bleeding, such as rhinitis (risk for epistaxis), bleeding disorders, vitamin K deficiency, gastrointestinal tract lesions, and peptic ulcer disease. Over 100,000 hospitalizations occur each year due to NSAID use, with over 16,000 deaths reported annually. Most fatalities associated with NSAID use are related to gastrointestinal bleeding. The three main adverse effects of NSAIDs are gastrointestinal intolerance, bleeding (often gastrointestinal bleeding), and renal impairment. Misoprostol (Cytotec) may be given to prevent gastrointestinal intolerance and ulcers resulting from NSAID use. It is classified as a prostaglandin analog. Many of the adverse effects of NSAIDs are secondary to their inactivation of protective prostaglandins that help maintain the normal integrity of the stomach lining. Misoprostol (Cytotec) may be given to prevent gastrointestinal intolerance and ulcers resulting from NSAID use. It is classified as a prostaglandin analog. There are also many contraindications to the use of NSAIDs, such as gastrointestinal tract lesions, peptic ulcers, and bleeding disorders. Acute renal failure is quite common with NSAID use, especially if the patient is dehydrated. Disruption of prostaglandin function by NSAIDs is sometimes strong enough to precipitate acute or chronic renal failure, depending on the patient’s current level of renal function. Chronic salicylate intoxication is also known as salicylism and results from either shortterm administration of high dosages or prolonged therapy with high or even lower dosages. The most common manifestations of chronic salicylate intoxication in adults are tinnitus and hearing loss. Hyperventilation and central nervous system effects such as dizziness, drowsiness, and behavioral changes occur in children. Metabolic complications such as metabolic acidosis and respiratory alkalosis often occur to varying degrees. The signs and symptoms of acute salicylate toxicity are similar to those of chronic intoxication, but the effects are often more pronounced and occur more quickly. Acute salicylate overdose usually results from the ingestion of a single toxic dose. An acute overdose of nonsalicylate NSAIDs (e.g., ibuprofen) causes effects similar to those of salicylate overdose, but they are generally not as extensive or as dangerous. Most oral NSAIDs are better tolerated if taken with food to minimize gastrointestinal upset. Monitor patients taking NSAIDs for the occurrence of bleeding, such as blood in the stool or vomitus. When NSAIDs are used to decrease joint inflammation in arthritis patients, full therapeutic effects may not be experienced for 1 week or longer. Copyright © 2020 Elsevier Inc. All Rights Reserved. 46 Acetic acid derivatives (e.g., indomethacin), a subclass of the NSAIDs, have analgesic, antiinflammatory, antirheumatic, and antipyretic properties. Ketorolac (Toradol), an acetic acid derivative, is somewhat unique in that, although it does have some antiinflammatory activity, it is used primarily for its powerful analgesic effects. Its analgesic effects are comparable to those of narcotic drugs such as morphine. Ibuprofen is the prototype NSAID in the propionic acid category. It is often used for its analgesic effects in the management of rheumatoid arthritis, osteoarthritis, primary dysmenorrheal, gout, dental pain, and musculoskeletal disorders. Naproxen is the second most commonly used NSAID, with a reportedly somewhat better adverse effect profile than ibuprofen, as well as fewer drug interactions with angiotensinconverting enzyme inhibitors given for hypertension. The COX-2 inhibitors were developed primarily to decrease the gastrointestinal adverse effects characteristic of other NSAIDs because of their COX-2 selectivity. Celecoxib (Celebrex) was the first COX-2 inhibitor and is the only one remaining on the market. It is indicated for the treatment of osteoarthritis, rheumatoid arthritis, acute pain symptoms, ankylosing spondylitis, and primary dysmenorrhea. The enolic acid derivatives include piroxicam, meloxicam, and nabumetone. Piroxicam and meloxicam are very potent drugs that are commonly used in the treatment of mild to moderate osteoarthritis, rheumatoid arthritis, and gouty arthritis. All NSAIDs (except aspirin) share a black box warning regarding an increased risk for adverse cardiovascular thrombotic events, including fatal MI and stroke. NSAIDs may counteract the cardioprotective effects of aspirin. Antigout Drugs Gout is caused by the overproduction of uric acid or decreased uric acid excretion, or both. This overproduction and/or decreased excretion can often result in hyperuricemia. Gouty arthritis is the condition in which one or more joints are inflamed due to the collection of gouty deposits inside the joint anatomy. This is also called articular gout, whereas gout that occurs in tissues outside of the joints is called abarticular gout. Although specific antigout drugs are available, the NSAIDs are considered first-line therapy for most patients with gout. Antigout drugs are indicated for either acute or chronic gout or gout prophylaxis. Diarrhea and abdominal pain are common adverse effects. Antigout drugs are often given to patients to avoid goutlike syndromes and pain during cancer chemotherapy that causes cell death. The specific antigout drugs—allopurinol, febuxostat, colchicine, probenecid, and sulfinpyrazone—are targeted at the underlying defect in uric acid metabolism, which causes either overproduction or underexcretion of uric acid. The new drug febuxostat (Uloric) is a non-purine selective inhibitor of xanthine oxidase. It is the first new drug approved for the treatment of gout since the 1960s. It is more selective for xanthine oxidase than allopurinol. Clinical trials suggest that it may pose a greater risk of cardiovascular events than allopurinol, although the mechanism is still being debated. It is not to be given along with theophylline, azathioprine, or mercaptopurine. Copyright © 2020 Elsevier Inc. All Rights Reserved. 47 Nursing Process Before administering antiinflammatory drugs, perform a nursing assessment including a thorough head-to-toe physical assessment and take vital signs. Perform a thorough medication history noting any drug allergies as well as a listing of prescription, over-thecounter, herbal, and/or supplements that the patient is taking. With aspirin, NSAIDs, other antiinflammatory drugs, and antigout drugs, assess and document the duration, onset, location, and type of inflammation and/or pain the patient is experiencing as well as any precipitating, exacerbating, or relieving factors. Age is important to assess as well, because aspirin and many of the other NSAIDs are not to be used in children and teenagers due to the increased risk for Reye’s syndrome. Develop an individualized patient education plan about all OTC and prescription medications with attention to the patient’s complaints/reporting of any gastrointestinal, cardiovascular, and neurologic symptoms. With aspirin, assess the patient for a history of asthma, wheezing, or other respiratory problems because of the increased incidence of allergic reactions to aspirin in these individuals. Also with aspirin, identify patients who have been diagnosed with what is called the aspirin triad, which includes asthma, nasal polyps, and rhinitis. Most oral NSAIDs are better tolerated if taken with food to minimize gastrointestinal upset. Use of ketorolac requires assessment of the drug order because it is important to be sure the drug has been ordered for a short term (e.g., no more than 5 days) and for patients experiencing moderate to severe acute pain. Assess the patient for underlying signs of infection before the use of any NSAID or other antiinflammatory drug because these drugs may mask symptoms. There are black box warnings issued by the FDA (see www.fda.gov/Drugs/DrugSafety) for NSAIDs. With antigout drugs, perform a thorough assessment of hydration status and baseline serum uric acid levels. If receiving febuxostat (Uloric), assess the patient for a history of cardiovascular disease due to the risk of adverse effects linked to the cardiac system. If the patient is taking allopurinol, assess the integrity of the skin due to potentially lifethreatening skin adverse effects of exfoliative dermatitis, Stevens-Johnson syndrome, and toxic epidermal necrolysis. With colchicine, conduct a thorough assessment for a history of gastrointestinal distress; ulcers; or cardiac, renal, or liver disease. When assessing the prescriber’s order, remember that there is only one colchicine product available, Colcrys, because the Food and Drug Administration required the withdrawal of all “unapproved” colchicine products from the market. If aspirin is used, the oral dosage forms are given with food, milk, or meals. Advise the patient that sustained-release or enteric-coated tablets are not to be crushed or broken. Aspirin therapy is not generally recommended or commonly used because of its toxicity. Copyright © 2020 Elsevier Inc. All Rights Reserved. 48 Advise the patient to avoid other ulcerogenic substances (e.g., alcohol, prednisone, aspirin-containing products, other NSAIDs) to help minimize the risk of gastrointestinal mucosal breakdown. Celecoxib may be taken without regard to meals; however, taking the drug with food and fluids may decrease any gastrointestinal upset. Instruct the patient to report immediately to the prescriber any stomach or abdominal pain, gastrointestinal problems, unusual bleeding, blood in the stool or vomitus, chest pain, edema, and/or palpitations. Educate the patient with gout on the importance of increasing fluid intake of up to 3 L/day unless contraindicated. Therapeutic responses to NSAIDs include the following: decrease in acute pain; decrease in swelling, pain, stiffness, and tenderness of a joint or muscle area; improved ability to perform activities of daily living (ADLs); improved muscle grip and strength; reduction in fever; return to normal laboratory values for complete blood cell count, red blood cell count, hemoglobin level, hematocrit, and sedimentation rate; and return to a less inflamed state. Use of COX-II inhibitors is expected to result in improved joint function and fewer inflammation-based signs and symptoms. Patients are expected to begin to show improvement in mobility and the ability to perform ADLs. Therapeutic responses to the antigout drug colchicine include decreased pain in the affected joints and increased sense of well-being. A therapeutic response to allopurinol, another antigout drug, includes a decrease in pain in the joints, a decrease in uric acid levels, and a decrease in stone formation in the kidneys. Copyright © 2020 Elsevier Inc. All Rights Reserved. 49 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 13: Central Nervous System Stimulants and Related Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview The central nervous system (CNS) is a very complex system in the human body. Many therapeutic drugs either work in the CNS or cause adverse effects in the CNS. CNS stimulants are a broad class of drugs that stimulate specific areas of the brain or spinal cord. Most CNS stimulant drugs act by stimulating the excitatory neurons in the brain. The actions of these stimulants mimic those of the neurotransmitters of the sympathetic nervous system (e.g., norepinephrine, dopamine, and serotonin). Adrenergic drugs are also called sympathomimetic drugs. CNS stimulant drugs are classified into three ways. The first is on the basis of chemical structural similarities. Major chemical classes of CNS stimulants include amphetamines, serotonin agonists, sympathomimetics, and xanthines. Second, these drugs can be classified according to their site of therapeutic action in the CNS. Third, they can be categorized according to five major therapeutic usage categories for CNS stimulant drugs. These include anti–attention deficit, antinarcoleptic, anorexiant, antimigraine, and analeptic drugs. Attention deficit hyperactivity disorder (ADHD), formerly known as attention deficit disorder (ADD), is the most common psychiatric disorder in children, affecting 4% to 10% of school-age children, with 6.1% children being treated with medication. Primary symptoms of ADHD are a developmentally inappropriate ability to maintain attention span and/or the presence of hyperactivity and impulsivity. Narcolepsy is an incurable neurologic condition in which patients unexpectedly fall asleep in the middle of normal daily activities. These “sleep attacks” are reported to cause car accidents or near-misses in 70% or more of patients. Another major symptom of the disease is dysfunctional rapid eye movement sleep. Overweight is defined as a BMI of 25 to 29.9, whereas obesity is defined as a BMI of 30 or higher. According to the National Institutes of Health and the Centers for Disease Control and Prevention, approximately 35% of Americans are obese and nearly two thirds (64.5%) are overweight. A migraine is a common type of recurring headache, usually lasting from 4 to 72 hours. Typical features include a pulsatile quality with pain that worsens with each pulse. The pain is most commonly unilateral but may occur on both sides of the head. Associated symptoms include nausea, vomiting, photophobia, and phonophobia. Migraines affect about 37 million people in the United States, with a reported incidence in females roughly three times that in males. Neonatal apnea, or periodic cessation of breathing in newborn babies, is a common condition seen in neonatal intensive care units. It occurs in about 25% of premature infants whose pulmonary and CNS structures, including the medullary centers that control breathing, have not completed their gestational development due to preterm birth. Copyright © 2020 Elsevier Inc. All Rights Reserved. 50 Pharmacology Overview Drugs for Attention Deficit Hyperactivity Disorder and Narcolepsy CNS stimulants are the first-line drugs of choice for both ADHD and narcolepsy. They are potent drugs with a strong potential for tolerance and psychological dependence classified as Schedule II drugs under the Controlled Substances Act. CNS stimulants are drugs that stimulate the brain or spinal cord. The actions of these stimulants mimic those of the neurotransmitters of the sympathetic nervous system. Included in the family of CNS stimulants are amphetamines, analeptics, and anorexiants with therapeutic uses for ADHD, narcolepsy, and appetite control. One of the newest drugs in the ADHD arsenal is lisdexamfetamine (Vyvanse). It is a prodrug for dextroamphetamine, meaning it is converted in the body to dextroamphetamine. Amphetamines stimulate areas of the brain associated with mental alertness, such as the cerebral cortex and the thalamus. Pharmacologic actions of CNS stimulants are similar to the actions of the sympathetic nervous system in that the CNS and respiratory systems are the primary systems affected. CNS effects include mood elevation or euphoria, increased mental alertness and capacity for work, decreased fatigue and drowsiness, and prolonged wakefulness. Adverse effects associated with CNS stimulants include changes in mental status or sensorium, changes in mood or affect, tachycardia, loss of appetite, nausea, altered sleep patterns (e.g., insomnia), physical dependency, irritability, and seizures. Contraindications to the use of amphetamine and nonamphetamine stimulants include known drug allergy or cardiac structural abnormalities. These drugs can also exacerbate the following conditions: marked anxiety or agitation, Tourette’s syndrome and other tic disorders (hyperstimulation), hypertension, and glaucoma. Both amphetamine and nonamphetamine stimulants have a wide range of adverse effects that most often arise when these drugs are administered at high doses. Effects on the cardiovascular system include increased heart rate and blood pressure. Other adverse effects include angina, anxiety, insomnia, headache, tremor, blurred vision, increased metabolic rate, gastrointestinal distress, dry mouth, and worsening of or new onset of psychiatric disorders, including mania, psychoses, or aggression. Common adverse effects associated with atomoxetine include headache, abdominal pain, vomiting, anorexia, and cough. Anorexiants Anorexiants are CNS stimulants that are believed to work by suppressing appetite control centers in the brain. Some evidence suggests that they also increase the body’s basal metabolic rate, including mobilization of adipose tissue stores and enhanced cellular glucose uptake, as well as reduce dietary fat absorption. Current evidence-based guidelines for the treatment of obesity do not support the use of anorexiants as monotherapy. Their effects are often minimal without accompanying behavioral modifications involving diet and exercise. Copyright © 2020 Elsevier Inc. All Rights Reserved. 51 Orlistat differs from other antiobesity drugs in that it is not a CNS stimulant. It works by inhibiting the enzyme lipase to reduce absorption of dietary fat from the intestinal tract and increase fat elimination in the feces. Lorcaserin (Belviq) is a serotonin 2C receptor agonist. Other drugs used for obesity include the combination of phentermine and topiramate (Qsymia); naltrexone (Contrave) and liraglutide (Saxenda). Naltrexone is an opioid antagonist and liraglutide is used to treat diabetes and topiramate is an antiepileptic used to treat seizures. Contraindications to anorexiants include drug allergy, any severe cardiovascular disease, uncontrolled hypertension, hyperthyroidism, glaucoma, mental agitation, history of drug abuse, eating disorders (e.g., anorexia, bulimia), and use of monoamine oxidase inhibitors. Other contraindications to the use of anorexiants, as well as other CNS stimulants, include hypersensitivity, seizure activity, convulsive disorders, and liver dysfunction. With the exception of diethylpropion, anorexiants may raise blood pressure and cause heart palpitations and even dysrhythmias at higher dosages. Ironically, at therapeutic dosages, they may actually reflexively slow the heart rate. Antimigraine Drugs The triptan antimigraine drugs, also referred to as selective serotonin receptor agonists (SSRAs), are indicated for abortive therapy of an acute migraine headache. The SSRAs are a newer class of CNS stimulants and are not to be given to patients with coronary heart disease. SSRAs may be taken during aura symptoms, but are not indicated for preventive therapy. Preventive therapy is indicated if migraines occur one or more days per week. Serotonin agonists may be administered as a subcutaneous injection, as a nasal spray, and as oral tablets. Any chest pain or tightness, tremors, vomiting, or worsening symptoms need to be reported to the prescriber immediately. Contraindications to triptans include drug allergy and the presence of serious cardiovascular disease, because of the vasoconstrictive potential of these medications. Contraindications to the use of ergot alkaloids include uncontrolled hypertension; cerebral, cardiac, or peripheral vascular disease; dysrhythmias; glaucoma; and coronary or ischemic heart disease. Triptans have potential vasoconstrictor effects, including effects on the coronary circulation. Injectable dosage forms may cause local irritation at the site of injection. Other adverse effects include tingling, flushing, and a congested feeling in the head or chest. Ergot alkaloids are associated with the adverse effects of nausea, vomiting, cold or clammy hands and feet, muscle pain, dizziness, numbness, a vague feeling of anxiety, a bitter or foul taste in the mouth or throat, and irritation of the nose. Analeptics Analeptics include doxapram (Dopram) and the methylxanthines aminophylline, theophylline, and caffeine. These drugs are sometimes used to treat neonatal and postoperative respiratory depression. Analeptics work by stimulating areas of the CNS that control respiration, mainly the medulla and spinal cord. At higher dosages, analeptics stimulate the vagal, vasomotor, Copyright © 2020 Elsevier Inc. All Rights Reserved. 52 and respiratory centers of the medulla in the brainstem, as well as increasing blood flow to skeletal muscles. Indications for analeptics include neonatal apnea, bronchopulmonary dysplasia, hypercapnia with chronic obstructive pulmonary disease (COPD), and respiratory depression related to anesthesia and secondary to drugs of abuse. At higher dosages, analeptics stimulate the vagal, vasomotor, and respiratory centers of the medulla and the brainstem, as well as increase blood flow to skeletal muscles. In newborns, administration of caffeine is associated with less tachycardia, CNS stimulation, and feeding intolerance than administration of theophylline or aminophylline. Contraindications to the use of analeptics include drug allergy, peptic ulcer disease (especially for caffeine), and serious cardiovascular conditions. Nursing Process CNS stimulants have addictive potential, and so assessment data need to be collected before their use, regardless of indication: (1) a thorough medical history with attention to preexisting diseases or conditions, especially those of the cardiovascular, cerebrovascular, neurologic, renal, and liver systems; (2) past and current history of addictive or substance abuse behaviors; (3) complete medication profile with a listing of prescription, over-the-counter (OTC), and herbal drugs and any use of alcohol, nicotine, and/or social or illegal drugs; and (4) a complete nutritional and dietary history. Assessment of all these parameters is important due to the specific mechanism of action of CNS stimulants leading to increases in pulse rate and blood pressure, seizure activity and/or intracerebral bleeding. Stimulation of the respiratory system is actually desirable and especially beneficial in those suffering from CNS depression, such as patients who are postoperative. Because anorexiants are generally used for a short period of time, emphasize to the patient and all members of the patient’s support system that a suitable diet, appropriate independent and/or supervised exercise program, and behavioral modifications are necessary to support a favorable result and to help the patient cease overeating and experience healthy weight loss. With drugs used for the treatment of ADHD, some pediatric patients may respond better to certain dosage forms such as immediate release. Well-planned scheduling of these medications and close communication among the school, teachers, school nurse, and the family and patient are very important to successful treatment. Therapeutic responses to drugs for ADHD include decreased hyperactivity, increased attention span and concentration, improved behavior, and, for adults, increased effectiveness at work. For drugs used to treat narcolepsy, therapeutic responses include a decrease in daytime sleepiness. Adverse effects for which to monitor include headache, nausea, nervousness, insomnia, and anxiety. Therapeutic effects of anorexiants include appetite control and weight loss for the treatment of obesity. Adverse effects of these drugs include dry mouth, headache, insomnia, constipation, tachycardia, cardiac irregularities, hypertension, changes in Copyright © 2020 Elsevier Inc. All Rights Reserved. 53 mental status or sensorium, changes in mood or affect, alteration of sleep patterns, and seizures. Evaluating for any increased irritability and withdrawal symptoms (e.g., headache, nausea and vomiting) is also important. If the anorexiant affects fat metabolism, then there may be adverse effects such as flatulence with an oily discharge, spotting, and fecal urgency. Fat-soluble vitamins (A, D, E, and K) need to be monitored because levels may be affected by the decreased absorption of fats. Serotonin agonists may be administered as a subcutaneous injection, as a nasal spray, and as oral tablets. Therapeutic responses to the serotonin agonists include aborting migraine headaches with improved daily functioning and performance. Adverse effects to monitor include pain at the injection site, flushing, chest tightness or pressure, weakness, sedation, dizziness, sweating, increase in blood pressure and pulse rate, and bad taste with the nasal spray formulation, which may precipitate nausea. Any chest pain or tightness, tremors, vomiting, or worsening symptoms needs to be reported to the prescriber immediately. Journaling is helpful in evaluating the effects of all drugs used to treat ADHD, obesity, migraines, and narcolepsy. Copyright © 2020 Elsevier Inc. All Rights Reserved. 54 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 14: Antiepileptic Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Epilepsy is a disorder of the brain manifested as a chronic, recurrent pattern of seizures. It is the most common chronic neurologic illness, affecting 3 million people in the United States and 50 million people worldwide. A seizure is a brief episode of abnormal electrical activity in the nerve cells of the brain. A convulsion is a more severe seizure characterized by involuntary spasmodic contractions of any or all voluntary muscles throughout the body, including skeletal, facial, and ocular muscles. Commonly reported symptoms include abnormal motor function, loss of consciousness, altered sensory awareness, and psychic changes. Seizures are classified as follows: partial-onset seizures or those originating in a more localized region of the brain; status epilepticus, characterized by generalized tonic-clonic convulsions that occur repeatedly in succession; and tonic-clonic seizures involving initial muscular contraction throughout the body (tonic) and progressing to alternating contraction and relaxation (clonic phase). Generalized onset seizures, formerly called grand mal seizures, are characterized by neuronal activity that originates simultaneously in the gray matter of both hemispheres. Tonic-clonic seizures begin with muscular contraction throughout the body (tonic phase) and progress to alternating contraction and relaxation (clonic phase). Partial onset seizures originate in a localized or focal region (e.g., one lobe) of the brain. In status epilepticus, multiple seizures occur with no recovery between them. If appropriate therapy is not prompt, hypotension, hypoxia, brain damage, and death can quickly ensue. Excessive electrical discharges can often be detected by an electroencephalogram. Fluctuations in the brain’s electrical potential are seen in the form of waves. These waves correlate well with different neurologic conditions and are used as diagnostic indicators. Epilepsy without an identifiable cause is known as primary epilepsy or idiopathic epilepsy. Primary epilepsy accounts for roughly 50% of cases. In other cases, epilepsy has a distinct cause, such as trauma, infection, cerebrovascular disorder, or other illness; this is known as secondary or symptomatic epilepsy. The chief causes of secondary epilepsy in children and infants are developmental defects, metabolic disease, and injury at birth. Febrile seizures occur in children 6 months to 5 years of age and are caused by fever. Children usually outgrow the tendency to have such seizures, and thus these seizures do not constitute a chronic illness. In adults, acquired brain disorder is the major cause of secondary epilepsy; including head injury, disease or infection of brain/spinal cord, stroke, metabolic disorders, and drug reactions. Copyright © 2020 Elsevier Inc. All Rights Reserved. 55 Pharmacology Overview Antiepileptic drugs are also called anticonvulsants. Antiepileptic drugs are a more appropriate term because many of these medications are indicated for the management of all types of epilepsy, and not necessarily just convulsions. Anticonvulsants, on the other hand, are medications that are used to prevent the convulsive seizures typically associated with epilepsy. The goal of antiepileptic drug therapy is to control or prevent seizures while maintaining a reasonable quality of life. Approximately 70% of patients can expect to become seizure-free while taking only one drug. Single-drug therapy must fail before multidrug therapy is attempted. The dosage of the medication is slowly increased until the seizures are controlled or until clinical toxicity occurs. Therapeutic drug monitoring of serum drug concentrations provides a useful guideline in assessing the effectiveness of and adherence to therapy. The antiepileptic drugs traditionally used to manage seizure disorders include barbiturates, hydantoins, and iminostilbenes, plus valproic acid. Second- and third-generation antiepileptics are also available. Newer approved drugs include perampanel (Fycompa,) ezogabine (Potiga), vigabatrin (Sabril), eslicarbazepine (Aptiom), clobazam (Onfi), and brivaracetam (Briviact). These drugs fall into the miscellaneous category of antiepileptics and have greatly expanded the options currently available to treat patients with seizure disorders. o o o o Ezogabine (Potiga) is indicated for adjunctive therapy for partial onset seizures and can cause potential vision loss and skin discoloration both which may be permanent. The FDA recommends it be used only in patients who have not responded to other drugs. Perampanel (Fycompa) is also indicated as adjunctive therapy for partial onset seizures. It is associated with a high incidence of dizziness. Vigabatrin (Sabril) is indicated for refractory complex partial seizures. It carries the risk of visual impairment and as such is only available through a restricted distribution program. Eslicarbazepine (Aptiom) is indicated as adjunctive therapy for partial onset seizures. o Clobazam (Onfi) is a benzodiazepine indicated as adjunctive therapy for LennoxGastault syndrome. o Brivaracetam (Briviact) is indicated for partial-onset seizures in patients 16 years and older. The major pharmacologic effects of antiepileptics are threefold. First, they increase the threshold of activity in the area of the brain called the motor cortex. Second, they act to limit the spread of a seizure discharge from its origin by suppressing the transmission of impulses from one nerve to the next. Third, they can decrease the speed of nerve impulse conduction within a given neuron. Antiepileptics are used for the long-term maintenance treatment of epilepsy. However, they are also useful for the acute treatment of status epilepticus. Copyright © 2020 Elsevier Inc. All Rights Reserved. 56 The only usual contraindication to antiepileptics is known drug allergy. Pregnancy is also a common contraindication; however, the prescriber must consider the risks to mother and infant of untreated maternal epilepsy and the increased risk for seizure activity. Many women take antiepileptics throughout their pregnancy. The newer-generation antiepileptic drugs appear to be safer in pregnancy than the traditional drugs. Antiepileptic drugs have many adverse effects, which often limit their usefulness. Many patients cannot tolerate the adverse effects, and therapy must be withdrawn. Birth defects in infants of epileptic mothers are higher than normal, regardless of whether the mother was receiving drug therapy. In December 2008, the U.S. Food and Drug Administration (FDA) required black box warnings on all antiepileptic drugs regarding the risk of suicidal thoughts and behavior. Patients being treated with antiepileptic drugs for any indication need to be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, or any unusual changes in mood or behavior. For certain antiepileptic drugs, the safe and toxic levels are very close together; that is, they have a narrow therapeutic range. Nursing Process With use of any of the antiepileptic drugs, perform a thorough physical assessment and obtain a comprehensive health and medication history so that any possible allergies, drug interactions, adverse reactions, cautions, and contraindications can be identified. You must be able to distinguish between the different types of seizure, and assess/document all symptoms, events, and problems that occur before, during, and after any seizure activity. This information may aid in the diagnosis of the type of seizure the patient is experiencing. Thoroughly review the patient’s medical history and note any type of seizure disorder, precipitating events, and the duration, frequency, and intensity of the seizure activity. Before giving these drugs, review the laboratory test results, which may include the results of red blood cell and white blood cell counts, clotting studies, and renal and/or liver function studies. If barbiturates have been ordered, carefully assess not only the neurologic system but also vital signs because of the central nervous system depression associated with this class of drugs. In addition, identify patients at high risk for excessive sedation for safety purposes. Interventions for patients taking antiepileptic drugs are aimed at monitoring the patient while providing safety measures and securing the airway, breathing, and circulation. Airway maintenance is of critical importance for epileptic patients because the tongue relaxes during seizure activity, falling backward and subsequently blocking the airway. Maintain the patient’s airway in the same way as during cardiopulmonary resuscitation, using the chin lift or jaw thrust method. Distinguish between the different types of seizure and assess and document all symptoms, events, and problems that occur before, during, and after any seizure activity. With antiepileptic drug administration, adhere closely to the drug dose and frequency of dosing, as ordered. Close monitoring of dosing is important to attain therapeutic blood Copyright © 2020 Elsevier Inc. All Rights Reserved. 57 levels. Administering the antiepileptic drug at the same time every day is also important to maintain blood levels. Grapefruit or related citrus fruits or pomegranate juice needs to be avoided with carbamazepine (Tegretol). The occurrence of a therapeutic response to antiepileptic drugs does not mean that the patient has been cured of the seizures but only that seizure activity is decreased or absent. Thoroughly document any response to the medication in the medical record. Noncompliance with the drug regimen is the most important factor leading to treatment failure. Monitor therapeutic blood levels at all times, and avoid abrupt withdrawal of the antiepileptic drug to prevent rebound seizure activity. Intravenous infusions of antiepileptic drugs are very dangerous and must be managed cautiously, with adherence to hospital or facility policy and manufacturer’s guidelines. Avoid rapid infusions because of the risk for cardiac and/or respiratory arrest. Older adult patients may experience paradoxical reactions to antiepileptic drugs, resulting in hyperactivity and irritability versus sedation. Copyright © 2020 Elsevier Inc. All Rights Reserved. 58 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 15: Antiparkinson Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Parkinson’s disease is a chronic, progressive, neurodegenerative disorder causing the degeneration of dopamine-producing neurons in the brain. Patients with this disease also have elevated acetylcholine levels and lowered dopamine levels. Dopamine is an inhibitory neurotransmitter and acetylcholine is an excitatory neurotransmitter in this area of the brain. Parkinson’s disease results from an imbalance in these two neurotransmitters in the basal ganglia. Parkinson’s disease affects at least 1 million Americans and 4 million people worldwide. Over 60,000 patients are diagnosed each year in the United States. It is the second most common neurodegenerative disease after Alzheimer’s disease. There are no readily available laboratory tests that can detect or confirm Parkinson’s disease. The diagnosis is usually made on the basis of the classic symptoms and physical findings. The classic symptoms of Parkinson’s disease include bradykinesia, postural instability, rigidity, and tremors (TRAP [tremor, rigidity, akinesia, postural instability] with akinesia really manifesting as bradykinesia). Symptoms of Parkinson’s disease do not appear until approximately 80% of the dopamine store in the substantia nigra has been deleted; thus, by the time the disease is diagnosed, only approximately 20% of the patient’s original dopaminergic terminals are functioning normally. Rapid swings in the response to levodopa, called the on-off phenomenon, result in worsening of the disease with too little dopamine or dyskinesias with too much. In contrast, the wearing-off phenomenon occurs when anti–Parkinson’s disease medications begin to lose their effectiveness, despite maximal dosing, as the disease progresses. Dyskinesia is the difficulty in performing voluntary movements and is commonly seen in the disease. Most frequent are chorea (irregular, spasmodic, involuntary movements of the limbs or facial muscles) and dystonia (abnormal muscle tone leading to impaired or abnormal movements). Dystonia commonly involves the head, neck, or feet and is a symptom common to patients with Parkinson’s disease. Dyskinesias also occur as adverse effects of some of the antiparkinson drugs. These motor complications make Parkinson’s disease a prominent cause of disability. Dementia may also result and is referred to as Parkinson’s disease–associated dementia. Up to 40% of patients with Parkinson’s disease will experience psychosis and hallucinations. In 2016, a new drug, pimavanserin (Nuplazid), was approved for the treatment of hallucinations and delusions associated with Parkinson’s disease psychosis. Copyright © 2020 Elsevier Inc. All Rights Reserved. 59 Pimavanserin is a selective serotonin 5-HT2A inverse agonist and has no effect on dopaminergic receptors. Treatment of the disease centers around drug therapy, but many experts believe that physical activity is as important as any drug therapy, and together these greatly improve mobility. For severe cases, the surgical technique of deep brain stimulation may be used. Drug therapy is aimed at increasing the levels of dopamine and/or antagonizing the effects of acetylcholine. Drug therapy is used to slow the progression of symptoms. Drugs used in the treatment of Parkinson’s disease include amantadine, benztropine, bromocriptine, carbidopa-levodopa, entacapone, ropinirole, and selegiline. They have a variety of mechanisms of action and many adverse effects, drug interactions, and dosing concerns. As long as there are functioning nerve terminals that can take up dopamine, the symptoms of Parkinson’s disease can be at least partially controlled. Pharmacology Overview Indirect-Acting Dopaminergic Drugs Monoamine Oxidase Inhibitors The primary role of monoamine oxidase (MAO) enzymes is the breakdown of catecholamines, such as dopamine, norepinephrine, and epinephrine, as well as serotonin. Giving an MAO-B inhibitor such as selegiline or rasagiline causes an increase in the levels of dopaminergic stimulation in the central nervous system (CNS), helping to counter the dopaminergic deficiency. Selegiline and rasagiline are adjunctive drugs currently approved for use in combination with carbidopa-levodopa when response to levodopa is fluctuating; they may also be beneficial as prophylactic drugs to delay reduction in a patient’s response to levodopa. As Parkinson’s disease progresses, it becomes more difficult to manage it with levodopa and ultimately the patient is seriously debilitated, generally 5 to 10 years after the start of therapy. Dopamine Modulator Only one drug—amantadine (Symmetrel)—is currently known to function as a dopamine modulator for management of Parkinson’s disease. Amantadine appears to work by causing the release of dopamine and other catecholamines from their storage sites and also blocks the reuptake of dopamine into the nerve fibers. Because amantadine does not directly stimulate dopaminergic receptors, it is considered to be indirect acting. Amantadine also has some anticholinergic properties. Amantadine is generally indicated in the early stages of Parkinson’s disease while there are still some intact neurons. It can be used in the moderate to advanced stages to help control symptoms of tremor but is usually effective for only 6 to 12 months. Common adverse effects include dizziness, insomnia, and nausea. Amantadine causes increased anticholinergic adverse effects when given with anticholinergic drugs. Catechol Ortho-Methyltransferase Inhibitors There are currently two drugs in this category: tolcapone and entacapone. Copyright © 2020 Elsevier Inc. All Rights Reserved. 60 Tolcapone acts both centrally and peripherally, whereas entacapone cannot cross the blood-brain barrier and therefore can act only peripherally. They prolong the duration of action of levodopa, especially when levodopa is given with carbidopa, resulting in reduction of the wearing-off phenomenon. Both catechol ortho-methyltransferase (COMT) inhibitors (tolcapone and entacapone) are contraindicated in cases of known drug allergy. Tolcapone is also contraindicated in cases of liver failure. Tolcapone has been associated with severe liver failure and carries a black box warning related to hepatotoxicity. Commonly reported adverse effects with both COMT inhibitors include gastrointestinal (GI) upset and urine discoloration. In addition, they also can worsen dyskinesia. Neither tolcapone nor entacapone are to be taken with nonselective MAO inhibitors because of cardiovascular risk due to reduced catecholamine metabolism. However, the selective MAO-B inhibitor selegiline may be safely taken concurrently with COMT inhibitors. Direct-Acting Dopamine Receptor Agonists Direct-acting dopamine receptor agonists are drugs used to treat Parkinson’s disease, often as first-line agents used on diagnosis. These drugs include two subclasses: nondopamine dopamine receptor agonists (NDDRAs) and dopamine replacement drugs. All NDDRAs work by direct stimulation of presynaptic and/or postsynaptic dopamine receptors in the brain. They may be used in early or late stages of the disease. The traditional role of the NDDRAs bromocriptine, pramipexole, ropinirole, and rotigotine has been as adjuncts to levodopa for management of motor fluctuations; however, they are now often used as first-line therapy. Known allergy is a contraindication to dopaminergic drug therapy. These drugs are not to be used concurrently with catecholamines due to the cardiovascular risks. The traditional cornerstone of therapy for Parkinson’s disease has been the drug levodopa, the biologic precursor of dopamine. Dopamine must be administered orally as levodopa because exogenously administered dopamine cannot pass through the bloodbrain barrier. Levodopa cannot be used by itself in the brain and must be combined with another substance, carbidopa. The combination product carbidopa-levodopa provides exogenous sources of dopamine and is the drug of choice in the later stages of Parkinson’s disease. Large doses result in high peripheral levels of dopamine and lead to many unwanted adverse effects, including confusion, involuntary movements, GI distress, hypotension, and even cardiac dysrhythmias. These problems are avoided when levodopa is given with carbidopa. Levodopa and carbidopa are both contraindicated in cases of angle-closure glaucoma because they can raise intraocular pressure, but they may be used cautiously in openangle glaucoma. Neither drug is to be used in patients with any undiagnosed skin condition, because both drugs can activate malignant melanoma. Adverse effects of dopamine replacement drugs include cardiac dysrhythmias, hypotension, chorea, muscle cramps, and GI distress. Anticholinergic Drugs Copyright © 2020 Elsevier Inc. All Rights Reserved. 61 Anticholinergic drugs block the effects of the neurotransmitter acetylcholine at cholinergic receptors in the brain as well as in the rest of the body. They are used as adjunct drug therapy in Parkinson’s disease due to their anti-tremor properties. Anticholinergic drugs can cause dry mouth or decreased salivation, urinary retention, decreased GI motility (constipation), dilated pupils (mydriasis), and smooth muscle relaxation. Anticholinergics must be used cautiously in older adults because of significant potential adverse effects, such as confusion, urinary retention, visual blurring, palpitations, and increased intraocular pressure. Nursing Process After patients are confronted with the diagnosis of Parkinson’s disease, they will soon learn that their quality of life depends on drug therapy and nondrug measures. Before medications for Parkinson’s disease are given, assess and document vital signs and ABCs (airway, breathing, and circulation). Obtain a complete nursing history with a thorough physical assessment, including compiling a comprehensive medication profile. With indirect-acting dopamine receptor agonists, such as amantadine, and direct-acting dopamine receptor agonists, such as carbidopa-levodopa, include supine and standing blood pressures (because of drug-related postural hypotension), height, weight, medication and medical history, and nursing history. Include family, significant others, and caregiver in the assessment and data collection process. Assess motor skills, including abilities and deficiencies, and for the presence of akinesia, bradykinesia, postural instability, rigidity, tremors, staggering gait, or drooling. It is important to understand the gynecologic history of the patient and to know if the patient is pregnant and/or lactating. Some dopamine replacement drugs cross into the placenta and into breast milk and have unknown actions in the pediatric patient. When anticholinergic drugs are prescribed, assess the patient carefully to determine gross level of organ functioning—especially in those systems most affected by Parkinson’s disease, including the GI, genitourinary, visual, cardiac, and neurologic systems. Pay close attention to any present or past changes in mental status as well as the presence of confusion, disorientation, or psychotic-like behavior. This is important to consider in elderly patients because of a decline in liver function and a subsequent higher risk for adverse effects and possible toxicity and an overall increased sensitivity to drugs. With indirect-acting dopamine receptor agonists, cardiac status is important to assess and document because of the adverse effects of hypotension/hypertension and chest pain. Encourage patients, family, or caregivers to begin keeping a daily drug calendar or journal including the drugs prescribed, dosage, frequency/timing, and therapeutic and adverse changes. During the start of dopaminergic drug therapy, the patient will most likely need assistance when walking because of the dizziness and possibly syncope caused by these drugs. With anticholinergic drugs, patients need to take the medication as prescribed, after meals or at bedtime, and not at the same time as with other medications. Copyright © 2020 Elsevier Inc. All Rights Reserved. 62 Be cautious with the sound-alike drugs: selegiline is a MAOI, whereas salagen is an oral form of pilocarpine used to manage dry mouth in patients with Sjögren’s syndrome or in those receiving radiation therapy. Nutritional concerns include making sure the patient is taking adequate fiber, vegetable and fruit, as well as increase in fluid intake, if not contraindicated. Additional concerns include distribution of protein intake over the course of the day if taking levodopa/carbidopa. The drug is to be taken one-half hour before eating a proteincontaining meal or one hour after. Be aware of all other forms of therapies that may be beneficial, such as support groups, water aerobics, and occupational and physical therapy. Aerobic exercise may have a positive effect on the patient while improving quality of life and socialization. Although it has not been proven that exercise can slow the progression of this disease, it can help patients feel better mentally and physically. Tai Chi may be one option of exercise that has been shown to improve balance, flexibility, and strength in a variety of individuals. Simple stretching and strengthening exercises are important to consider in those with Parkinson’s disease. All exercises must be approved by the patient’s health care provider. Prevention of falls is important—reduce risk by installing shower or tub grab-bars, adequate lighting in the house especially at night and removing/securing loose rugs that may increase the risk of tripping. Therapeutic responses to the antiparkinson drugs include an improved sense of wellbeing, improved mental status, increased appetite, ability to perform activities of daily living, improved concentration and ability to think more clearly, and a decrease in the intensity of parkinsonian symptoms. Monitor for adverse effects such as dizziness; nausea; syncope; insomnia; GI upset (associated with indirect-acting dopamine receptor agonists such as selegiline, amantadine, entacapone, and tolcapone); ataxia; depression (associated with direct-acting dopamine receptor agonists such as bromocriptine); palpitations; hypotension; urinary retention; and depression (associated with dopamine replacement drugs such as levodopa and carbidopa). Patient considerations include providing individual and family support along with options for care of the family member with Parkinson’s disease. The disease is long term and lifelong, as well as debilitating. A holistic approach in which all aspects of the patient and family are considered and respected is the key to quality nursing care. Copyright © 2020 Elsevier Inc. All Rights Reserved. 63 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 16: Psychotherapeutic Drugs Key points Anatomy, Physiology, and Pathophysiology Overview The treatment of mental disorders is called psychotherapeutics. Long-term pharmacotherapy in conjunction with psychotherapy is recommended when emotions or behaviors compromise quality of life, ability to carry out normal activities of daily living, social functioning, or occupational functioning over a prolonged period. In the biochemical imbalance theory, mental disorders are thought to arise as the result of abnormal levels of endogenous chemicals in the brain known as neurotransmitters. Drugs used to treat mental illnesses, including anxiety, affective disorders, and psychoses, work by blocking or stimulating the release of various endogenous neurotransmitters. Patients with mental illness are at greater risk for physical illnesses associated with obesity, including diabetes, hypertension, and heart disease. Economic, educational, and psychosocial issues may preclude a mentally ill person from seeking psychiatric health care, resulting in self-medication with substances of abuse, including alcohol, tobacco, and illegal or unauthorized prescription drugs. Ideal mental health care involves many components, including a carefully detailed patient interview and carefully chosen and regularly monitored drug therapy. Nonpharmacologic treatments include psychotherapy, support groups, social and family support systems, and often spiritual support systems. There are three common types of mental illness: anxiety, affective, and psychotic disorders. The drugs used to treat anxiety are anxiolytics. Mood stabilizers and antidepressants are used to treat affective disorders, while antipsychotics are used to treat psychotic disorders. Psychosis is a major emotional disorder that impairs mental function. A person experiencing psychosis cannot participate in everyday life and shows loss of contact with reality. Affective disorders are emotional disorders characterized by changes in mood. They range from mania to depression and include anxiety, a normal emotion that may be a healthy reaction but becomes pathologic when it is life-altering. Anxiety disorders occur in approximately 18% of the adult population in the U.S. Obsessive-compulsive disorder is twice as common as schizophrenia or panic disorders in the general population. Situational anxiety arises in response to specific life events, and nursing assessment is key to identifying patients at risk. Pharmacology Overview Psychotropic drugs are among the most commonly prescribed drugs in the United States. Copyright © 2020 Elsevier Inc. All Rights Reserved. 64 The effectiveness of drug therapy is often measured by verbal reports from patients regarding the level of improvement (if any) in their social and occupational functioning. Nonadherence to the prescribed regimen is common as patients may remain in denial about the reality of their mental illness, including the need to take psychotropic medications. Anxiolytic Drugs Primary anxiolytic drugs include the benzodiazepine drug class and the miscellaneous drug buspirone. The benzodiazepines are commonly used as first-line drug therapy for both acute and chronic anxiety disorders. Other drugs that are effective as anxiolytics include selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs), antipsychotics, and the antihistamine hydroxyzine. All anxiolytic drugs decrease anxiety by reducing overactivity in the central nervous system (CNS). Benzodiazepines are the largest and most commonly prescribed anxiolytic drug class because they offer several advantages over other drugs used to treat anxiety. Benzodiazepines exert their effect by depressing activity in areas of the brain when it increases the action of gamma-aminobutyric acid (GABA), which is an inhibitory neurotransmitter in the brain that blocks nerve transmission in the CNS. The most common undesirable effect is an overexpression of their therapeutic effects, in particular CNS depression. Benzodiazepines can also cause hypotension. Elderly patients tend to be more sensitive to the sedating effects of benzodiazepines, which can increase their risk for falls; lower doses are usually needed. When benzodiazepines are taken alone, an overdose is generally not life threatening. When they are combined with alcohol or other CNS depressants, the outcome is much more severe. Buspirone (BuSpar) is an anxiolytic drug that is different from the benzodiazepines; it appears to have agonist activity at both serotonin and dopamine receptors. Affective Disorders Mood-Stabilizing Drugs Mood stabilizers are drugs used to treat bipolar illness. Catecholamines play an important role in the development of mania; serotonin also appears to be involved. Lithium has been in use for many years and is still used to effectively alleviate the symptoms of acute mania in bipolar disorder as well as for maintenance therapy to prevent episodes. A new antipsychotic, cariprazine (Vraylar), was approved in 2016 for the treatment of bipolar disorder. A variety of medications may be used in conjunction with lithium to regulate mood or achieve stability, including benzodiazepines, antipsychotic drugs, antiepileptic drugs, and dopamine receptor agonists. Antidepressant Drugs Copyright © 2020 Elsevier Inc. All Rights Reserved. 65 Antidepressants are the pharmacologic treatment of choice for major depressive disorders. They are also useful in treating other disorders, such as dysthymia, schizophrenia, eating disorders, and personality disorders. Some of the antidepressants are also used in the treatment of various medical conditions, including migraine headaches, chronic pain syndromes, sleep disorders, premenstrual syndrome, and hot flashes associated with menopause. Many drugs used to treat affective disorders increase the levels of neurotransmitter concentrations in the CNS, including serotonin, dopamine, and norepinephrine. The permissive hypothesis led to the creation of the selective SSRI drug class. The permissive theory postulates that reduced concentrations of serotonin are the predisposing factor in patients with affective disorders. Depression results from decreases in both the serotonin and catecholamine levels, whereas mania results from increased dopamine and norepinephrine levels but decreased serotonin. Anxiety and depression commonly occur together, so there is much crossover in symptom control between antidepressant and anxiolytic drugs. A nonresponse to antidepressant drug therapy is defined as failure to respond to at least 6 weeks of therapy with adequate drug dosages. Twenty percent to 30% of patients who do not respond to the usual dosage of an antidepressant will respond to higher dosages. In 2005, the Food and Drug Administration (FDA) issued special black box warnings for all classes of antidepressants in both adult and pediatric patient populations; data indicated a higher risk for suicide in patients receiving these medications. Current recommendations for all patients receiving antidepressants include regular monitoring for signs of worsening depressive symptoms, especially when the medication is started or the dosage is changed. Tricyclic Antidepressants TCAs were the original first-generation antidepressants; their use has largely been replaced with the SSRIs and serotonin-norepinephrine reuptake inhibitors. The TCAs are considered second-line drug therapy in patients for whom the SSRIs are ineffective or as adjunct therapy with newer drugs. Originally used to treat depression, currently TCAs are most commonly used to treat neuropathic pain syndromes and insomnia. Undesirable effects of TCAs are a result of their effects on various receptors. Blockade of cholinergic receptors results in undesirable anticholinergic adverse effects, the most common being constipation and urinary retention. TCA overdoses are notoriously lethal. It is estimated that 70% to 80% of patients who die of TCA overdose do so before reaching the hospital, especially if the drugs are taken with alcohol. The systems affected are the CNS and cardiovascular system. Most TCAs are rated as pregnancy category D drugs, which makes their use by pregnant women relatively more hazardous than that of most of the newer drugs. Monoamine Oxidase Inhibitors MAOIs, along with TCAs, represent the first generation of antidepressant drug therapy; they are rarely used as antidepressants but are used to treat Parkinson’s disease. Copyright © 2020 Elsevier Inc. All Rights Reserved. 66 MAOI use may cause a hypertensive crisis when taken with stimulant medications or with a substance containing tyramine, which is found in many common foods and beverages. Clinical symptoms of MAOI overdose generally do not appear until about 12 hours after ingestion. The primary signs and symptoms are cardiovascular and neurologic. Second-Generation Antidepressants The second-generation antidepressants include trazodone, bupropion, the SSRIs (e.g., fluoxetine, sertraline, paroxetine), the serotonin-norepinephrine reuptake inhibitors (e.g., venlafaxine), and miscellaneous drugs, nefazodone and mirtazapine. The inhibition of serotonin reuptake is the primary mechanism of action of the selective serotonin reuptake inhibitor (SSRIs). SSRIs and SNRIs are often prescribed because of their superiority to older antidepressants. The adverse effect profiles of the second-generation antidepressants are associated with significantly fewer and less severe effects than TCAs and MAOIs. Second-generation antidepressants take the same amount of time to reach maximum clinical effectiveness as do the TCAs and MAOIs—typically 4 to 6 weeks. Although depression is the primary indication, the drugs have shown benefit in treating other mental and physical disorders, such as bipolar disorder, obesity, eating disorders, obsessive-compulsive disorder, panic attacks or disorders, social anxiety disorder, posttraumatic stress disorder, premenstrual dysphoric disorder, the neurologic disorder myoclonus, and various substance abuse problems such as alcoholism. Some of the most common adverse effects are insomnia, weight gain, and sexual dysfunction, primarily related to inability to achieve orgasm. One potentially hazardous adverse effect of any drug or combination of drugs that have serotoninergic activity is known as serotonin syndrome. SSRIs are associated with a discontinuation syndrome or withdrawal syndrome, and the drugs must be very slowly tapered. SSRIs with the shortest half-lives (citalopram, escitalopram, sertraline, paroxetine) are most commonly associated with the discontinuation syndrome. Symptoms include flulike feeling, difficulty concentrating, faintness, and GI symptoms. While most commonly associated with SSRIs, it can occur with the SNRIs: venlafaxine, desvenlafaxine, duloxetine, milnacipran, levomilnacipran. To prevent potentially fatal pharmacodynamic interactions with the MAOIs, a 2- to 5week washout period is recommended between use of SSRIs and MAOIs. Antipsychotic Drugs Antipsychotic drugs are used to treat serious mental illnesses such as drug-induced psychoses, schizophrenia, and autism and to treat extreme mania (as an adjunct to lithium), bipolar disorder, depression that is resistant to other therapy, certain movement disorders (e.g., Tourette’s syndrome), and certain other medical conditions (e.g., nausea, intractable hiccups). Copyright © 2020 Elsevier Inc. All Rights Reserved. 67 The phenothiazines are the largest chemical class of antipsychotic drugs, constituting about two thirds of all antipsychotics; they were the original drugs in this category. More recently, a new generation of antipsychotic medications has evolved referred to as atypical antipsychotics. Atypical antipsychotics differ from conventional drugs in that they tend to have better adverse effect profiles. The atypical antipsychotics tend to cause weight gain, although the amount varies with the individual drugs. Antipsychotic drugs are indicated for psychotic illness, most commonly schizophrenia. Their indications have expanded to include anxiety and mood disorders as well. Common adverse effects are caused by blockade of the alpha-adrenergic, dopamine, endocrine, histamine, and cholinergic receptors. Possible severe hematologic effects include agranulocytosis and hemolytic anemia. CNS effects include drowsiness, neuroleptic malignant syndrome, extrapyramidal symptoms, and tardive dyskinesia. In 2011, the FDA required manufacturers to change a product’s labeling to include stronger wording regarding the use of antipsychotics in pregnant women, including consistent information about the potential risk for abnormal muscle movements (extrapyramidal symptoms) and withdrawal symptoms in newborns whose mothers were treated with these drugs during the third trimester of pregnancy. In April 2005, the FDA issued a special public health advisory concerning the use of atypical antipsychotic drugs in elderly patients for all-label uses. These drugs are commonly used to control behavioral symptoms of agitation in elderly patients with dementia. The FDA data found that elderly patients given atypical antipsychotics for this reason were up to 1.7 times more likely to die during treatment. Antihypertensives may have additive hypotensive effects and CNS depressants may have additive CNS depressant effects when taken with antipsychotics. Atypical antipsychotics can be used in bipolar disorder or depression including drugs such as aripiprazole (Abilify) and lurasidone (Latuda). In 2017, valbenazine (Ingrezza) was approved as the first drug indicated to treat adults with tardive dyskinesia. Antipsychotics are associated with development of metabolic syndrome, which can cause serious long-term health problems; this is seen most commonly with the atypical antipsychotics. All antipsychotics require a medication guide to be included in the dispensing. Antipsychotics should not be stopped abruptly due to risk of withdrawal psychosis. Nursing Process Nursing considerations related to psychotherapeutic drugs include the need for skillful patient assessment with an emphasis on past and present medical history, physical examination, and a thorough medication history and profile as a comparative baseline for the patient during and after initiation of therapy. Thoroughly assess the patient’s neurologic functioning, including level of consciousness, mental alertness, and level of motor and cognitive functioning. Copyright © 2020 Elsevier Inc. All Rights Reserved. 68 The Mini-Mental State Examination (MMSE) is one tool that you may use to assess cognitive status and help identify impairments often found in mental illnesses. Constantly assess the patient for any suicidal ideations or tendencies because of the potential for suicide, with or without the concurrent use of other medications or alcohol. It is important to assess sleep habits and nutritional intake and to perform a head-to-toe physical examination for baseline and comparative purposes. Note any drug allergies as well as any contraindications, cautions, and potential drug interactions. With psychotherapeutic drug therapy, assess the patient’s mouth and oral cavity to make sure the patient has swallowed the entire oral dosage. This helps to prevent hoarding or “cheeking” of medications, noncompliance that may lead to drug toxicity or overdose. All psychotherapeutic drugs are to be taken exactly as prescribed and at the same time every day and without failure. If omission occurs, contact the prescriber immediately. Abrupt withdrawal may have negative effects on the patient’s physical and mental status. Always provide a medication guide and instructions upon dispensing of all psychotherapeutic medications. Monitor the therapeutic effects of psychotherapeutic medications and the patient’s progress before and during drug therapy. Mental alertness, cognition, affect, mood, ability to carry out activities of daily living, appetite, and sleep patterns are all areas that need to be closely monitored and documented Copyright © 2020 Elsevier Inc. All Rights Reserved. 69 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 18: Adrenergic Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview The body’s nervous system is divided into two major branches: the central nervous system (CNS) and the peripheral nervous system. The central nervous system contains the brain and the spinal cord. The peripheral nervous system is subdivided into somatic and autonomic nervous systems, and the autonomic nervous system is further subdivided into the parasympathetic (cholinergic) and the sympathetic (adrenergic) nervous systems. Adrenergic compounds include several exogenous (synthetic) and endogenous (produced in the body naturally) substances. They have a wide variety of therapeutic uses depending on their site of action and their effect on different types of adrenergic receptors. Catecholamines are substances that produce a sympathomimetic response (stimulate the SNS). The naturally occurring or endogenous catecholamines include epinephrine, norepinephrine, and dopamine. An example of an exogenous catecholamine is dobutamine. There are receptor sites for the catecholamines norepinephrine and epinephrine throughout the body referred to as adrenergic receptors. At these receptors, adrenergic drugs bind and produce effects. The beta-adrenergic receptors are all located on postsynaptic effector cells. The beta1adrenergic receptors are primarily located in the heart, whereas the beta2-adrenergic receptors are located in the smooth muscle fibers of the bronchioles, arterioles, and visceral organs. Another type of adrenergic receptor is the dopaminergic receptor. When stimulated by dopamine (only), these receptors cause the vessels of the renal, mesenteric, coronary, and cerebral arteries to dilate, which increases blood flow to these tissues. Pharmacology Overview Adrenergic Drugs Adrenergics are drugs with effects that are similar to or mimic the effects of the SNS neurotransmitters norepinephrine, epinephrine, and dopamine. They are either endogenous substances such as epinephrine, norepinephrine, and dopamine, or synthetic substances such as dobutamine and phenylephrine. The three endogenous catecholamines are also available in synthetic drug form. Non-catecholamine adrenergic drugs, such as phenylephrine, metaproterenol, and albuterol, are structurally dissimilar to the endogenous catecholamines and have a longer duration of action than either the endogenous or synthetic catecholamines. Epinephrine is available in two strengths for IV use, and was historically labeled as a ratio, which led to many medication errors. It is available as 1 : 1000 (1 mg/mL) and also Copyright © 2020 Elsevier Inc. All Rights Reserved. 70 as 1 : 10,000 (0.1 mg/mL). Starting May 2016, epinephrine injections will no longer be labeled with the ratios, instead will be labeled like all other injectable drugs in a mg/ml concentration, as 1 mg/mL or 0.1 mg/mL. Mechanism of Action and Drug Effects A direct-acting sympathomimetic, such as epinephrine, binds directly to the receptor and causes a physiologic response. An indirect-acting sympathomimetic causes the release of the catecholamine from the storage sites (vesicles) in the nerve endings; it then binds to the receptors and causes a physiologic response. Adrenergic agents can also be classified as either selective or nonselective in their actions, meaning they affect only one receptor subtype. Although adrenergics work primarily at postganglionic receptors peripherally, they may also work more centrally in the nervous system at the preganglionic sympathetic nerve trunks. When beta1-adrenergic receptors, located on the myocardium and in the conduction system of the heart, are stimulated by an adrenergic drug, three things result: 1. An increase in the force of contraction (positive inotropic effect) 2. An increase in heart rate (positive chronotropic effect) and 3. An increase in the conduction of cardiac electrical nerve impulses through the atrioventricular node (positive dromotropic effect) In addition, stimulation of beta1 receptors in the kidney causes an increase in renin secretion. Activation of beta2-adrenergic receptors produces relaxation of the bronchi (bronchodilation) and uterus and also causes increased glycogenolysis (glucose release) from the liver. Epinephrine is available in two strengths for IV use and was historically labeled as a ratio, which led to many medication errors. Starting in May 2016, epinephrine injections are labeled like all other injectable drugs in a mg/ml concentration, as 1 mg/mL or 0.1 mg/mL. Indications Adrenergics, or sympathomimetics, are used in the treatment of a wide variety of illnesses and conditions. Bronchodilators are drugs that have an affinity for the adrenergic receptors in the respiratory system, preferentially stimulating the beta2-adrenergic receptors and causing bronchodilation. The intranasal application of certain adrenergics can cause the constriction of dilated arterioles and a reduction in nasal blood flow, which thus decreases congestion. Some adrenergics, called ophthalmics, are applied to the surface of the eye. They work in much the same way as nasal decongestants except that they affect the vasculature of the eye. Adrenergics can also be used to reduce intraocular pressure, which makes them useful in the treatment of open-angle glaucoma. They can also dilate the pupils (mydriasis), which makes them useful for diagnostic eye examinations. They produce these effects by stimulating alpha- or beta2-adrenergic receptors, or both. Copyright © 2020 Elsevier Inc. All Rights Reserved. 71 Adrenergic agents are also used to support the cardiovascular system during cardiac failure or shock and are referred to as vasoactive sympathomimetics, vasoconstrictive drugs (known as vasopressive drugs, pressor drugs, or pressors), inotropes, or cardioselective sympathomimetics. Adrenergics that have primarily cardioselective effects are referred to as vasoactive adrenergics and are used to support a failing heart or treat shock or orthostatic hypotension. The beta3 agonist, mirabegron (Myrbetriq), relaxes the detrusor muscle during the storage phase of the bladder fill cycle which leads to an increase in bladder storage capacity. This new mechanism of action is an improvement over other drugs for overactive bladder. Mirabegron should not be used with silodosin, thioridazine, and certain chemotherapeutic agents. It can increase the effects of desipramine, digoxin, aripiprazole, colchicine, and others. It may decrease the effects of metoprolol, tamoxifen, tramadol, and codeine. In 2014, a new oral drug called droxidopa (Northera) was approved for the treatment of neurogenic orthostatic hypotension. Droxidopa is converted to norepinephrine in the body. The most common adverse events are headache, dizziness, nausea, hypertension, and fatigue. Adverse Effects Unwanted CNS effects of the alpha-adrenergic drugs include headache, restlessness, excitement, insomnia, and euphoria. Possible cardiovascular adverse effects of the alphaadrenergic drugs include chest pain, vasoconstriction, hypertension, tachycardia, and palpitations or dysrhythmias. Effects on other body systems include anorexia (loss of appetite), dry mouth, nausea, vomiting, and, rarely, taste changes. The beta-adrenergic drugs can adversely stimulate the CNS, causing mild tremors, headache, nervousness, and dizziness, or the cardiovascular system, including increased heart rate (positive chronotropy), palpitations (dysrhythmias), and fluctuations in blood pressure. The toxic effects of adrenergic drugs are an extension of their common adverse effects, such as seizures from excessive CNS stimulation, hypotension or hypertension, dysrhythmias, palpitations, nervousness, dizziness, fatigue, malaise, insomnia, headache, tremor, dry mouth, and nausea. The two most life-threatening effects involve the CNS and cardiovascular system. Interactions Numerous drug interactions can occur and although many of the interactions result only in a diminished effect because of direct antagonism at and competition for receptor sites, some reactions can be life threatening. Nursing Process Use of adrenergic agonists requires careful patient assessment and monitoring to maximize therapeutic effects and minimize possible adverse effects. Focus assessment on a comprehensive health history with past and present medical history, and obtain a past/present medication history. Also include specific system-based questions and identify cautions, contraindications, and drug interactions. Copyright © 2020 Elsevier Inc. All Rights Reserved. 72 Perform a thorough head-to-toe physical assessment and thoroughly assess baseline vital signs, including breath sounds, heart sounds, peripheral pulses, skin color, and capillary refill. There are several nursing interventions that may maximize the therapeutic effects of adrenergic drugs and minimize their adverse effects, such as checking package inserts for the types and amounts of dilutional solutions to use with parenteral dosage forms. When these drugs are given via an inhaler or nebulizer, provide the patient with complete, thorough, and age-appropriate instructions about correct use, storage, and care of equipment. Patients with chronic lung disease who are receiving adrenergic drugs need to avoid anything that may exacerbate their respiratory condition (e.g., food or other allergens, cigarette smoking). If the patient has a chronic respiratory disease, such as emphysema or chronic asthma or bronchitis, it is important for the patient to avoid contact with individuals who may have infections to help minimize situations that would exacerbate the original problem. Respiratory irritants must be avoided. With nasal preparations, rebound nasal congestion or ulcerations of the nasal mucosa may occur if drugs are overused; therefore, educate patients to use these products only as directed. Midodrine use requires careful blood pressure monitoring, so patient education about supine blood pressure measurement and journaling of measured blood pressure values is very important to the effective use of the drug. Myrbetriq, a newer drug for overactive bladder, is associated with dizziness and so encourage the patient to avoid hazardous activities if this occurs. As with any patient with overactive bladder, avoid liquids before bedtime. Inhaled forms of beta2 agonists are used for their bronchodilating action and must be taken only as prescribed, with caution to avoid any overuse of the drug. Overdosage of these drugs may lead to severe cardiovascular, CNS, and cerebrovascular adverse effects and stimulation. Monitor for therapeutic effects of the adrenergic drugs. To evaluate for the occurrence of adverse effects with adrenergic drugs, monitor for stimulation of the systems that are affected, such as the cardiac system and the CNS. Copyright © 2020 Elsevier Inc. All Rights Reserved. 73 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 19: Adrenergic-Blocking Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview The autonomic nervous system consists of the parasympathetic and sympathetic nervous systems (SNS). Adrenergic agonist drugs stimulate the SNS. Those drugs are called agonists because they bind to receptors and cause a response. Adrenergic blockers have the opposite effect and are therefore referred to as antagonists. They bind to adrenergic receptors, but in doing so inhibit or block stimulation by the SNS. Adrenergic blockers are also referred to as sympatholytics because they “lyse,” or inhibit, SNS stimulation. There are receptor sites for the endogenous sympathetic neurotransmitters norepinephrine and epinephrine known as adrenergic receptors. Two basic types are alpha and beta; subtypes of the alpha- and beta-adrenergic receptors are designated 1 and 2. Adrenergic blockers are classified by the type of adrenergic receptor they block—alpha, beta, or both; therefore, they are called alpha blockers, beta blockers, or alpha/beta blockers. Adrenergic-blocking drugs block the stimulation of the alpha-, beta1-, and/or beta2adrenergic receptors, with the net result of blocking the effects of either norepinephrine or epinephrine on the receptors. This blocking action leads to a variety of physiologic responses depending on which receptors are blocked. Knowing how these receptors work allows the nurse to understand and predict the expected therapeutic effects of the drugs as well as the expected adverse effects. With alpha blockers, the predominant response is vasodilation due to blocking of the alpha-adrenergic effect of vasoconstriction, which results in blood vessel relaxation. Vasodilation of blood vessels with the alpha blockers results in a drop in blood pressure and a reduction in urinary obstruction, which may lead to increased urinary flow rates. For this reason, alpha blockers are given to patients with benign prostatic hyperplasia to decrease resistance to urinary outflow. Beta blockers inhibit the stimulation of beta-adrenergic receptors by blocking the effects of the SNS neurotransmitters norepinephrine, epinephrine, and dopamine. o Stimulation of beta1 receptors leads to an increase in heart rate, conduction, and contractility. o Stimulation of beta2 receptors results in bronchial smooth muscle relaxation or bronchodilation. o Blocking of beta1 receptors results in a decrease in heart rate, conduction, and contractility. o Blocking of beta2 receptors leads to a decrease in bronchial smooth muscle relaxation or bronchoconstriction. Copyright © 2020 Elsevier Inc. All Rights Reserved. 74 Beta blockers are classified as either selective or nonselective. Selective beta blockers are also called cardioselective beta blockers and block only the beta-adrenergic receptors in the heart that are located on the postsynaptic effector cells (i.e., the cells that nerves stimulate). Beneficial effects of the cardioselective beta blockers include decreased heart rate, reduced cardiac conduction, and decreased myocardial contractility with no bronchoconstriction. These drugs are a good choice for patients with hypertension who also have bronchospastic airway disease or other pulmonary disease. Nonselective beta blockers block both beta1- and beta2-adrenergic receptors and affect the heart and bronchial smooth muscle. These drugs are used to treat patients with hypertension who do not have a problem with bronchospasm or pulmonary airway disease. Pharmacology Overview Alpha Blockers The alpha-adrenergic–blocking drugs, or alpha blockers, interrupt stimulation of the SNS at the alpha1-adrenergic receptors, either by direct competition with norepinephrine or by a noncompetitive process. Alpha blockers have a greater affinity for the alpha-adrenergic receptor than norepinephrine does and therefore can chemically displace norepinephrine molecules from the receptor. With alpha blockers, the predominant response is vasodilation. This is due to blocking of the alpha-adrenergic effect of vasoconstriction, which results in blood vessel relaxation. Vasodilation of blood vessels with the alpha blockers results in a drop in blood pressure and a reduction in urinary obstruction, which may lead to increased urinary flow rates. Monitor for these effects in patients taking alpha blockers. The alpha blockers such as doxazosin, prazosin, and terazosin cause both arterial and venous dilation, which reduces peripheral vascular resistance and blood pressure. These drugs are used to treat hypertension. Other alpha blockers can inhibit responses to adrenergic stimulation and will noncompetitively block alpha-adrenergic receptors on smooth muscle and various exocrine glands. Because of this action, they are very useful in controlling or preventing hypertension in patients who have a pheochromocytoma, a tumor that forms on the adrenal gland on top of the kidney and secretes norepinephrine, thus causing SNS stimulation. The alpha blockers are also useful in the treatment of patients who have increased endogenous alpha-adrenergic agonist activity, which results in vasoconstriction. Three conditions in which this occurs are Raynaud’s disease, acrocyanosis, and frostbite. Other alpha blockers, such as phentolamine, are effective at counteracting the effects of injected epinephrine and norepinephrine by causing peripheral vasodilation and reducing peripheral resistance by blocking catecholamine-stimulated vasoconstriction. Because of their potent vasodilating properties and their fast onset of action, they are used to prevent skin necrosis and sloughing after the extravasation of vasopressors. Copyright © 2020 Elsevier Inc. All Rights Reserved. 75 The primary adverse effects of alpha blockers are those related to effects on the vasculature. First-dose phenomenon, which is a severe and sudden drop in blood pressure after the administration of the first dose of an alpha-adrenergic blocker, can cause patients to fall or faint. All patients must be warned about this adverse effect before they take their first dose of an alpha blocker. Orthostatic hypotension can occur with any dose of an alpha blocker, and patients must be warned to get up slowly from a supine position. In an acute oral overdose, activated charcoal is administered to bind the drug and remove it from the stomach and the circulation. The most severe drug interactions with alpha blockers are the ones that potentiate the effects of the alpha blockers. Beta Blockers Beta blockers are classified as either selective or nonselective. Selective beta blockers are also called cardioselective beta blockers and block only the beta-adrenergic receptors in the heart that are located on the postsynaptic effector cells (i.e., the cells that nerves stimulate). The beneficial effects of the cardioselective beta blockers include decreased heart rate, reduced cardiac conduction, and decreased myocardial contractility with no bronchoconstriction. These drugs are a good choice for patients with hypertension who also have bronchospastic airway disease or other pulmonary disease. Nonselective beta blockers block both beta1- and beta2-adrenergic receptors and affect the heart and bronchial smooth muscle. These drugs are used to treat patients with hypertension who do not have a problem with bronchospasm or pulmonary airway disease. The beta-adrenergic–blocking drugs block SNS stimulation of the beta-adrenergic receptors by competing with norepinephrine and epinephrine. The beta blockers can be either selective or nonselective, depending on the type of beta-adrenergic receptors they antagonize. Beta1-adrenergic receptors are located primarily in the heart; beta blockers that are selective for these receptors are called cardioselective beta blockers or beta1-blocking drugs. Other beta blockers block both beta1- and beta2-adrenergic receptors and are referred to as nonselective beta blockers. Beta2 receptors are located primarily on the smooth muscles of the bronchioles and blood vessels. Stimulation of beta1 receptors leads to an increase in heart rate, conduction, and contractility. Stimulation of beta2 receptors results in bronchial smooth muscle relaxation or bronchodilation. Blocking of beta1 receptors results in a decrease in heart rate, conduction, and contractility. Blocking of beta2 receptors leads to a decrease in bronchial smooth muscle relaxation or bronchoconstriction. When the beta2 receptors in the bronchioles are blocked, the smooth muscle surrounding the airway contracts, causing these airways to narrow; this may lead to shortness of breath. When this beta2 stimulation is blocked, the muscles are then stimulated by unopposed sympathetic activity at the beta1 receptors, which causes them to contract. This causes increased peripheral vascular resistance. Copyright © 2020 Elsevier Inc. All Rights Reserved. 76 Catecholamines also promote glycogenolysis and mobilize glucose in response to hypoglycemia. Nonselective beta blockers impair this process and also impede the secretion of insulin from the pancreas, which causes elevation of blood glucose level. Beta blockers can cause the release of free fatty acids from adipose tissue, which may result in moderately elevated blood levels of triglycerides and reduced levels of the “good cholesterol” known as high-density lipoprotein (HDL). Indications for beta blockers include angina, myocardial infarction (MI), cardiac dysrhythmias, hypertension, and heart failure. Beta blockers are also considered cardioprotective because they inhibit stimulation of the myocardium by circulating catecholamines. MI causes catecholamines to be released. Unopposed stimulation by catecholamines would further increase the heart rate and the contractile force and thereby increase myocardial oxygen demand. Because of this characteristic, beta blockers are commonly given to patients to protect the heart after they have experienced an MI. Conduction in the sinoatrial (SA) node is slowed by beta blockers, which results in a decreased heart rate and slowing of conduction through the atrioventricular (AV) node. This is useful in the treatment of various types of irregular heart rhythms called dysrhythmias. Beta blockers are useful in treating hypertension because of their ability to reduce SNS stimulation of the heart, thereby reducing the heart rate and the force of myocardial contraction. Because of their lipophilicity (attraction to lipid or fat), some beta blockers can easily gain entry into the central nervous system and are used to treat migraine headaches. The topical application of timolol to the eye has been very effective in treating ocular disorders such as glaucoma. Contraindications to the use of beta blockers include known drug allergies and may include uncompensated heart failure, cardiogenic shock, heart block or bradycardia, pregnancy, severe pulmonary disease, and Raynaud’s disease. The adverse effects of beta blockers, most of which are mild and diminish with time, are primarily extensions of their pharmacologic activity. For overdoses of both oral and injectable dosage forms, treatment consists primarily of symptomatic and supportive care. Nursing Process Because of the impact of these drugs, primarily on the cardiac and respiratory systems, their use requires careful assessment to help minimize the adverse effects and maximize the therapeutic effects. Understanding the basic anatomy and physiology of adrenergic receptors and their subsequent actions if stimulated or blocked is also critical in carrying out assessment and other aspects of the nursing process and drug therapy. Begin a thorough assessment by gathering information about the patient’s allergies and past and present medical conditions and conducting a system overview and medication history. Several nursing interventions may help maximize therapeutic effects of adrenergicblocking drugs and minimize their adverse effects. Copyright © 2020 Elsevier Inc. All Rights Reserved. 77 Count the apical pulse for 1 full minute, and measure and document both supine and standing blood pressures. To help minimize dry mouth, encourage intake of water within any restrictions and frequent rinsing/spraying of mouth with over-the-counter dental products indicated for dry mouth. If drugs are given intravenously, electrocardiographic (ECG) monitoring/cardiac monitoring is usually recommended. Encourage patients taking alpha blockers to change positions slowly and with purpose to prevent or minimize postural hypotension with subsequent dizziness and/or syncope. Use of the newer alpha blocker tamsulosin in patients with BPH is quite common, and it is not uncommon to see it prescribed for females with kidney stones. Patients taking this drug need to inform all health care providers—including dentists—that this is part of their medical regimen, especially before any type of surgery. Anything leading to vasodilation should be avoided to prevent postural hypotension with resultant dizziness, lightheadedness, and syncope, including alcohol intake, excessive exercise, exposure to hot climates, and use of saunas, hot tubs, and heated showers or baths. Contact the prescriber immediately if (1) the patient has any problems with dizziness, fainting, or lightheadedness, (2) the systolic blood pressure is lower than 100 mm Hg or the diastolic is less than 80 mm Hg diastolic, or (3) the pulse rate is lower than 60 beats/min. The patient should also report muscle weakness, shortness of breath, weight gain, and collection of fluid in the lower extremities. Nursing considerations for patients taking alpha and beta blockers include teaching patients that they must weigh themselves daily, avoid sudden changes in position, and increase intake of fluids and fiber. Weight gain, dizziness, fainting, and/or a decrease in heart rate below 60 beats/min or a blood pressure of less than 100 mm Hg systolic or less than 80 mm Hg diastolic need to be reported immediately. Therapeutic effects to monitor in patients include, but are not limited to, a decrease in blood pressure, pulse rate, and palpitations; alleviation of the symptoms of the disorder for which the drug was indicated; a return to normal blood pressure and pulse; and a decrease in chest pain in patients with angina. Monitor patients for adverse effects associated with these medications, including bradycardia, depression, fatigue, and hypotension. Keeping a journal documenting daily weights, blood pressure readings, pulse rates, adverse effects, and overall feelings of wellness or lack thereof will be important to the monitoring of the therapeutic regimen. Copyright © 2020 Elsevier Inc. All Rights Reserved. 78 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 20: Cholinergic Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Cholinergics, cholinergic agonists, and parasympathomimetics are all appropriate terms for the class of drugs that stimulate the parasympathetic nervous system, which is the branch of the autonomic nervous system that opposes the sympathetic nervous system. The primary neurotransmitter responsible for the transmission of nerve impulses to effector cells of the parasympathetic nervous system is acetylcholine. There are two types of cholinergic receptors: nicotinic and muscarinic, as determined by their location and their action. A cholinergic receptor is a receptor that binds acetylcholine and mediates its actions. Nicotinic receptors are located in the ganglia of both the parasympathetic nervous system and sympathetic nervous system. They are called nicotinic because they can also be stimulated by nicotine. The other type of cholinergic receptor is the muscarinic receptor. Muscarinic receptors are located postsynaptically in the effector organs (i.e., smooth muscle, cardiac muscle, and glands) supplied by the parasympathetic fibers. They are called muscarinic because they are stimulated by the alkaloid muscarine, a substance isolated from mushrooms. Pharmacology Overview Cholinergic drugs, also known as cholinergic agonists or parasympathomimetics, mimic the effects of acetylcholine, stimulating cholinergic receptors either directly or indirectly. Direct-acting cholinergic agonists bind directly to cholinergic receptors and activate them. Indirect-acting cholinergic agonists stimulate the postsynaptic release of acetylcholine at the receptor site. This then allows acetylcholine to bind to and stimulate the receptor. Indirect-acting cholinergic drugs (also known as cholinesterase inhibitors) work by inhibiting the action of acetylcholinesterase, the enzyme responsible for breaking down acetylcholine. Acetylcholinesterase is also referred to as cholinesterase. There are two categories of cholinesterase inhibitors: reversible inhibitors and irreversible inhibitors. Reversible cholinesterase inhibitors bind to cholinesterase for a short period of time, whereas irreversible cholinesterase inhibitors have a long duration of activity, and the body must generate new cholinesterase enzymes to override the effects of the irreversible drugs. The effects of direct- and indirect-acting cholinergic drugs are seen when the parasympathetic nervous system is stimulated. Mnemonics aid in remembering these effects. One is to think of the parasympathetic nervous system as the “rest and digest” system, in contrast to the “flight or fight” sympathetic nervous system. Cholinergic drugs are used primarily to stimulate the intestine and bladder, which results in increased gastric secretions, gastrointestinal (GI) motility, and urinary frequency. They Copyright © 2020 Elsevier Inc. All Rights Reserved. 79 also stimulate constriction of the pupil, termed miosis. This helps decrease intraocular pressure. In addition, cholinergic drugs cause increased salivation and sweating. Cardiovascular effects include reduced heart rate and vasodilation. Pulmonary effects include causing the bronchi of the lungs to constrict and the airways to narrow. At recommended dosages, cholinergic drugs primarily affect the muscarinic receptors, but at high dosages the nicotinic receptors can also be stimulated. The desired effects come from muscarinic receptor stimulation; many of the undesirable adverse effects are due to nicotinic receptor stimulation. Direct-acting drugs, such as carbachol, pilocarpine, and echothiophate, are used topically to reduce intraocular pressure in patients with glaucoma or in those undergoing ocular surgery. The direct-acting drug bethanechol affects the detrusor muscle of the urinary bladder and also the smooth muscle of the GI tract. It causes increased bladder and GI tract tone and motility. Indirect-acting drugs work by increasing acetylcholine concentrations at the receptor sites, which leads to stimulation of the effector cells. Indirect-acting drugs cause skeletal muscle contraction and are used for the diagnosis and treatment of myasthenia gravis. The ability of indirect-acting drugs to inhibit acetylcholinesterase also makes them useful for the reversal of neuromuscular blockade produced either by neuromuscular blocking drugs or by anticholinergic poisoning. Indirect-acting drugs are also used to treat Alzheimer’s disease, which is a neurologic disorder in which patients have decreased levels of acetylcholine. Contraindications to the use of cholinergic drugs include known drug allergy, GI or genitourinary (GU) tract obstruction, bradycardia, defects in cardiac impulse conduction, hyperthyroidism, epilepsy, hypotension, or chronic obstructive pulmonary disease. The primary adverse effects of cholinergic drugs are the consequence of overstimulation of the parasympathetic nervous system. They are extensions of the cholinergic reactions that affect many body functions. There is little systemic absorption of the topically administered drugs and therefore little systemic toxicity. o When administered locally in the eye, cholinergic drugs can cause temporary ocular changes such as transient blurring and dimming of vision. o Systemic toxicity with topically applied cholinergics is seen most commonly when longer-acting drugs are given repeatedly over a long period, resulting in overstimulation of the parasympathetic nervous system. The most severe consequence of an overdose of a cholinergic drug is a cholinergic crisis resulting in circulatory collapse, hypotension, bloody diarrhea, shock, and cardiac arrest. Nursing Process Before cholinergic drugs are given, perform a thorough head-to-toe physical examination, and obtain a nursing history and medication history. Document drug allergies and past and present medical conditions as well. Identify cautions, contraindications, and drug interactions, and document if a cholinergic drug is given. Copyright © 2020 Elsevier Inc. All Rights Reserved. 80 Assess vital signs and document, with special attention to baseline blood pressure readings because of the potential for orthostatic hypotension. Patients taking cholinergics need to change positions slowly to avoid dizziness and fainting that may result from the adverse effect of postural hypotension. Several nursing interventions may help to maximize the therapeutic effects of cholinergic drugs and minimize their adverse effects. If the patient has undergone surgery and cholinergic drugs are indicated, encourage ambulation and increased intake of fluids and fiber, unless contraindicated. Early ambulation helps to increase GI peristalsis and possibly prevent the need for drugs such as bethanechol, which is used to treat decreased or absent peristalsis related to the surgery and/or anesthesia. Cholinergic drugs must not be administered in any patient with a suspected/confirmed mechanical obstruction within the GI tract. An obstruction would be confirmed with presenting signs and symptoms along with the confirmation of obstruction through a variety of diagnostic procedures. Nursing considerations for the administration of cholinergic drugs include giving the drug as directed and monitoring the patient carefully for the occurrence of bradycardia, hypotension, headache, dizziness, respiratory depression, and bronchospasm. If these occur in a patient taking cholinergics, the prescriber must be contacted immediately. It may take up to 6 weeks for a therapeutic response to occur with some of the medications used with Alzheimer’s disease. Patients taking cholinergics should always change positions slowly to avoid dizziness and fainting that may result from the adverse effect of postural hypotension. For drugs used to treat myasthenia gravis, give the oral medication about 30 minutes before meals to allow for onset of action and therapeutic effects (e.g., decreased dysphagia or decreased difficulty swallowing). Atropine is the antidote to a cholinergic overdose; therefore, this medication needs to be readily available and given per the prescriber’s order. Most cholinergic agonists have dose-limiting adverse effects that include severe GI disturbances such as nausea and vomiting. Blood pressure readings and pulse rates need to be taken and recorded before, during, and after initiation of drug therapy. Dizziness may occur with therapy, resulting in the need for assistance with ambulation and other activities of daily living (ADLs). For patient safety, blood pressure, pulse rate, and electrocardiogram need to be carefully monitored throughout therapy. Instruct the patient, family, or caregiver to report any cardiac problems such as a decrease in pulse rate (<60 beats/min) and/or a drop in blood pressure. An overdose of cholinergic drugs may result in a cholinergic crisis with early manifestations of abdominal cramping, flushing of the skin, nausea, vomiting, and salivation. If left untreated, symptoms may progress to circulatory collapse, hypotension, and cardiac arrest. For patient safety, blood pressure, pulse rate, and electrocardiogram need to be carefully monitored throughout therapy. Dissolving forms of the medication donepezil are to be placed on the tongue and allowed to dissolve before the patient drinks fluids or swallows. Copyright © 2020 Elsevier Inc. All Rights Reserved. 81 Because most cholinergic drugs are used to treat patients diagnosed with Alzheimer’s disease, monitor the patient’s family and other support personnel closely, and be sure that their questions are answered fully and completely and their needs met. Monitor patients for the following therapeutic effects: o In patients with myasthenia gravis, a decrease in the signs and symptoms of the disease; o In patients experiencing a decrease in GI peristalsis postoperatively, an increase in bowel sounds, the passage of flatus, and the occurrence of bowel movements; o In patients who have a hypotonic bladder with urinary retention, micturition (voiding) within about 60 minutes of the administration of bethanechol. Monitor for adverse effects of these medications, including increased respiratory secretions, bronchospasm, nausea, vomiting, diarrhea, hypotension, bradycardia, and conduction abnormalities. Copyright © 2020 Elsevier Inc. All Rights Reserved. 82 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 21: Cholinergic-Blocking Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Cholinergic blockers, parasympatholytics, anticholinergics, and antimuscarinics are all terms that refer to drugs that block or inhibit the actions of acetylcholine in the parasympathetic nervous system. Acetylcholine is the neurotransmitter responsible for the transmission of nerve impulses to effector cells in the parasympathetic nervous system. A cholinergic receptor is one that binds acetylcholine and mediates its actions. Cholinergic-blocking drugs inhibit the effects of the parasympathetic nervous system, allowing the sympathetic nervous system to dominate. Cholinergic blockers have many of the same effects as the adrenergics. The use of these cholinergic blockers allows the sympathetic nervous system to dominate. These drugs are classified chemically as natural, semisynthetic, and synthetic cholinergic blockers. These drugs may be competitive antagonists (blockers) and compete with acetylcholine at the muscarinic receptors. In high dosages, they result in partial blocking actions at the nicotinic receptors. Some of the indications for the use of cholinergic blockers include bradycardia, irritable bowel syndrome, neurogenic bladder, overactive bladder, prevention of motion sickness and to control secretions preoperatively. Pharmacology Overview Cholinergic blockers have many therapeutic uses and are one of the oldest groups of therapeutic drugs. They were originally derived from various plant sources, but today they are part of a larger group of cholinergic blockers including synthetic and semisynthetic drugs. Cholinergic-blocking drugs block the action of the neurotransmitter acetylcholine at the muscarinic receptors in the parasympathetic nervous system (PNS). In high dosages, they result in partial blocking actions at the nicotinic receptors. Acetylcholine that is released from a stimulated nerve fiber is then unable to bind to the receptor site and fails to produce a cholinergic effect, which is why the cholinergic blockers are also referred to as anticholinergics. Cholinergic blockers are competitive antagonists. They compete with acetylcholine for binding at the muscarinic receptors of the PNS. Anticholinergics have the opposite effects of the cholinergics. The major sites of action of the anticholinergics are the heart, respiratory tract, gastrointestinal (GI) tract, urinary bladder, eye, and exocrine glands (sweat gland, salivary gland). Anticholinergic effects on the cardiovascular system manifest as an increase in heart rate. Copyright © 2020 Elsevier Inc. All Rights Reserved. 83 Respiratory system effects are dry mucous membranes and bronchial dilation. In the GI tract, cholinergic blockers cause a decrease in GI motility, GI secretions, and salivation. In the genitourinary (GU) system, they lead to decreased bladder contraction, which can result in urinary retention. In the skin, they reduce sweating, and finally, anticholinergics cause the pupils to dilate and increase intraocular pressure. In the central nervous system, cholinergic blockers have the therapeutic effect of decreasing muscle rigidity and diminishing tremors; this is of benefit in the treatment of both Parkinson’s disease and drug-induced extrapyramidal reactions such as those associated with antipsychotic drugs. These conditions involve dysfunction of the extrapyramidal parts of the brain and include motor dysfunctions, such as chorea, dystonia, and dyskinesia. Cardiovascular effects of anticholinergics are related to their cholinergic-blocking actions on the heart’s conduction system. At low dosages, the anticholinergics may actually slow the heart rate through their effects on the cardiac center in the portion of the brain called the medulla. At high dosages, cholinergic blockers block the inhibitory vagal (i.e., parasympathetic or cholinergic) effects on the pacemaker cells of the sinoatrial and atrioventricular nodes, which leads to acceleration of the heart rate due to unopposed sympathetic activity. Atropine is used primarily in the management of cardiovascular disorders, such as in the diagnosis of sinus node dysfunction, the treatment of patients with symptomatic seconddegree atrioventricular block, and provision of advanced life support in the treatment of sinus bradycardia that is accompanied by hemodynamic compromise. It also has ophthalmic uses. In the respiratory tract, this results in decreased secretions from the nose, mouth, pharynx, and bronchi. It also causes relaxation of the smooth muscles in the bronchi and bronchioles, which results in decreased airway resistance and bronchodilation. o Therefore, cholinergic blockers have proved beneficial in treating exerciseinduced bronchospasm, chronic bronchitis, asthma, and chronic obstructive pulmonary disease. o They are also used preoperatively to reduce salivary secretions, which aids in intubation and other procedures. Gastric secretions and the smooth muscles responsible for producing gastric motility are both controlled by the PNS, which is primarily under the control of muscarinic receptors. Cholinergic blockers antagonize these receptors, causing reduced secretions, relaxation of smooth muscle, and reduced GI motility and peristalsis. For these reasons, cholinergic blockers are commonly used in the treatment of irritable bowel disease and GI hypersecretory states. Anticholinergics are useful in the treatment of such GU tract disorders as reflex neurogenic bladder and incontinence. They relax the detrusor muscles of the bladder and increase constriction of the internal sphincter. Overactive bladder (OAB) is not a disease; it is the name of a group of urinary symptoms. The most common symptoms include a sudden urge to urinate that the patient cannot control. Leaking of urine with feeling the urge may also occur as well as having to go to the bathroom many times during the day and night. Copyright © 2020 Elsevier Inc. All Rights Reserved. 84 In the U.S., an estimated 46 million adults aged 40 and older—or 1 in 3—report symptoms and/or live with the symptoms of overactive bladder. Approximately 30% of all men and 40% of all women in the U.S. live with OAB symptoms. Newer drugs for this purpose include solifenacin (Vesicare), darifenacin (Enablex), trospium (Sanctura), and fesoterodine (Toviaz). The newer drugs are associated with a much lower incidence of dry mouth, in part because of their pharmacologic specificity for the bladder as opposed to the salivary glands. The newest drug, mirabegron (Myrbetriq), was approved for overactive bladder. It is a beta3 agonist and represents a new class of therapy for this condition. Mirabegron does not have same side effects as other drugs to treat OAB since it is a beta3 agonist, as opposed to being a muscarinic blocker. The ability of cholinergic blockers to decrease glandular secretions makes them potentially useful drugs for reducing gastric and pancreatic secretions in patients with acute pancreatitis. Anticholinergic drugs cause widely varied adverse effects covering many body systems. Certain patient populations are more susceptible to the effects of the anticholinergics, including infants, children with Down syndrome, those with spastic paralysis or brain damage, and the elderly. The elderly are extremely sensitive to the CNS effects of anticholinergics, and it is not uncommon for elderly patients to develop delirium due to anticholinergic effects. The dosage of cholinergic blockers is important, because there is a very small difference between therapeutic and toxic dosages, referred to as having a low therapeutic index. The treatment of cholinergic blocker overdose consists of symptomatic and supportive therapy. The patient should be hospitalized with continuous monitoring, including continuous electrocardiographic monitoring. Activated charcoal has proven very effective in removing any drug that has not yet been absorbed from the GI tract. Among the oldest and best known naturally occurring cholinergic blockers are the belladonna alkaloids; atropine is the prototypical drug. It has been used for hundreds of years and continues to be widely administered because of its effectiveness. In addition to atropine, scopolamine and hyoscyamine are the other major cholinergic blocking drugs that occur naturally. Nursing Process A thorough medical history; complete medication history with a listing of prescription drugs, over-the counter drugs, and herbals; as well as a thorough head-to-toe examination will help you identify the presence of any contraindications, cautions, and/or potential drug interactions associated with the cholinergic-blocking drugs. Lifespan considerations for the very young or pediatric patient and the elderly include a need for close assessment and monitoring because of the increased susceptibility of these groups to the adverse effects of restlessness, irritability, disorientation, constipation, urinary retention, blurred vision (from pupil dilation), and tachycardia. In assessing patients receiving atropine and other cholinergic blockers, check for allergies, glaucoma, certain eye conditions (e.g., adhesions in the iris and lens of the eye), gastroesophageal reflux disease, poor intestinal motility, obstructions of the GI and GU systems, and severe ulcerative colitis as these conditions may be exacerbated. Copyright © 2020 Elsevier Inc. All Rights Reserved. 85 A preventative focus for nursing care is important to the effective use of cholinergicblocking drugs, especially with regard to patient teaching about how to decrease the need for these medications. Some important nursing interventions include giving the drug at the same time each day and per the prescriber’s orders, and giving the medication with adequate fluid intake (6 to 8 glasses of water daily). Because drugs such as atropine and glycopyrrolate are compatible with some of the commonly used opioids (e.g., meperidine and morphine), they may be used in combination with these drugs and mixed in the same syringe for parenteral dosing. Always double-check compatibility for patient safety. If a cholinergic-blocking drug is given via the ophthalmic route, always check the concentration of the drug and, once it is given, apply light pressure with a tissue to the inner canthus of the eye for approximately 30 to 60 seconds. This helps to minimize the possibility of systemic absorption of the drug. Adverse effects of constipation and the patient’s inability to sweat or perspire are associated with the cholinergic-blocking drugs. Include patient education on how to minimize these effects. Monitoring of goals and outcome criteria is a starting place for effective evaluation of therapy with these medications. In particular, therapeutic effects of cholinergic-blocking drugs include the following: o Improved ability to perform activities of daily living and fewer problems with tremors, salivation, and drooling in patients with Parkinson’s disease. o Decreased GI symptoms, such as hyperacidity, abdominal pain, and nausea and vomiting, with improved comfort. o Decreased GU hypermotility, with increased comfort and improved patterns of voiding with an increase in time between voidings. o Fewer bronchospasms with induction of anesthesia and fewer problems with thickened, viscous secretions in patients before, during, and after surgery. Monitor the patient for the occurrence of adverse effects such as constipation, tachycardia, palpitations, confusion, sedation, drowsiness, hallucinations, urinary retention, and decreased sweating leading to hot, dry skin. Toxic effects of anticholinergics include delirium, hallucinations, and cardiac dysrhythmias. Copyright © 2020 Elsevier Inc. All Rights Reserved. 86 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 22: Antihypertensive Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Hypertension, defined as a persistent systolic blood pressure (SBP) of greater than 150 mm Hg and/or a diastolic blood pressure (DBP) greater than 90 mm Hg for patients 60 years or older and SBP greater than 140 and DBP greater than 90 for patients younger than 60 and those who have chronic kidney disease or diabetes. Hypertension affects approximately 70 million people in the United States and approximately 1 billion people worldwide, designating it as the most common disease state. Hypertension is a major risk factor for coronary artery disease, cardiovascular disease, and death resulting from cardiovascular causes. It is the most important risk factor for stroke and heart failure, and it is also a major risk factor for renal failure and peripheral vascular disease. Blood pressure is determined by the product of cardiac output and systemic vascular resistance (SVR). All antihypertensives in some way affect cardiac output. Cardiac output is the amount of blood that is ejected from the left ventricle. SVR is the resistance to blood flow that is determined by the diameter of the blood vessel and the vasculature musculature. If the cause of hypertension is unknown, it may be called essential, idiopathic, or primary hypertension, comprising 90% of cases. Secondary hypertension is most commonly the result of another disease such as pheochromocytoma, preeclampsia of pregnancy, renal artery disease, sleep apnea, thyroid disease, or parathyroid disease or the use of certain medications. If the cause of secondary hypertension can be eliminated, blood pressure usually returns to normal. If untreated, hypertension can cause damage to end organs such as the heart, brain, kidneys, and eyes. The Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 8—December 2013) provides treatment guidelines for hypertension assembled by two large expert panels based on a review of the latest clinical research publications on the disease. The classification scheme used to categorize individual cases of hypertension has been simplified to the following four stages based on blood pressure measurements: normal, prehypertension, stage 1 hypertension, and stage 2 hypertension. According to the JNC 8, therapy should be started if blood pressure is at or greater than 150/90 for patients over 60 years and 140/90 for patients younger than 60 and those who have chronic kidney disease or diabetes. Pharmacology Overview Copyright © 2020 Elsevier Inc. All Rights Reserved. 87 Drug therapy for hypertension needs to be individualized. Demographic factors, cultural implications, the ease of medication administration, and cost are important considerations. The main categories of pharmacologic drugs used to treat hypertension include diuretics, adrenergic drugs, vasodilators, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), calcium channel blockers (CCBs), and direct renin inhibitors. All of these antihypertensive drugs (with the exception of diuretics) have some vasodilatory action. Those drugs in the vasodilator category are also called direct vasodilators. Drugs in any of these classes may be used either alone or in combination. Adrenergic Drugs Five specific drug subcategories are included in the adrenergic antihypertensive drugs, which have central action (in the brain) or peripheral action (at the heart and blood vessels). These drugs include the adrenergic neuron blockers (central and peripheral), the alpha2receptor agonists (central), the alpha1-receptor blockers (peripheral), the beta-receptor blockers (peripheral), and the combination alpha1- and beta-receptor blockers (peripheral). The centrally acting adrenergic drugs work by stimulating the alpha2-adrenergic receptors in the brain. This results in a lack of norepinephrine production, which reduces blood pressure. Stimulation of the alpha2-adrenergic receptors also affects the kidneys, reducing the activity of renin. Renin is the hormone and enzyme that converts the protein precursor angiotensinogen to the protein angiotensin I, the precursor of angiotensin II (AII), a potent vasoconstrictor that raises blood pressure. In the periphery, the alpha1 blockers doxazosin, prazosin, and terazosin also modify the function of the sympathetic nervous system (SNS). They do so by blocking the alpha1adrenergic receptors. When these receptors are blocked, blood pressure is decreased. The beta blockers also act in the periphery and include propranolol, metoprolol, and atenolol as well as several other drugs. Their antihypertensive effects are related to their reduction of the heart rate through beta1-receptor blockade. Beta blockers also cause a reduction in the secretion of the hormone renin, which in turn reduces both AII-mediated vasoconstriction and aldosterone-mediated volume expansion. Long-term use of beta blockers also reduces peripheral vascular resistance. Two dual-action alpha1- and beta-receptor blockers, labetalol and carvedilol, have the dual antihypertensive effects of reduction in heart rate (beta1-receptor blockade) and vasodilation. Nebivolol (Bystolic) is the newest beta blocker, released in 2008. It is a beta1-selective beta blocker approved for use in hypertension. It is also used for the treatment of heart failure. The most common adverse effects of adrenergic drugs are bradycardia with reflex tachycardia, postural and post-exercise hypotension, dry mouth, drowsiness, dizziness, depression, edema, constipation, and sexual dysfunction. Other effects include headaches, sleep disturbances, nausea, rash, and palpitations. Copyright © 2020 Elsevier Inc. All Rights Reserved. 88 There is a high incidence of orthostatic hypotension in patients taking alpha blockers. When the patient changes positions, a situation known as first-dose syncope, in which the hypotensive effect is severe enough to cause the patient to lose consciousness with even the first dose of medication, can occur. Educate the patient to change positions slowly. The abrupt discontinuation of the centrally acting alpha2-receptor agonists can result in rebound hypertension, characterized by a sudden and very high elevation of blood pressure. Nonselective blocking drugs are also commonly associated with bronchoconstriction as well as metabolic inhibition of glycogenolysis in the liver, which can lead to hypoglycemia. Any change in the dosing regimen for cardiovascular medications should be undertaken gradually and with appropriate patient monitoring and follow-up. Angiotensin-Converting Enzyme (ACE) Inhibitors ACE inhibitors work by blocking a critical enzyme system responsible for the production of AII (angiotensin II; a potent vasoconstrictor). They (1) prevent vasoconstriction caused by AII, (2) prevent aldosterone secretion and therefore sodium and water resorption, and (3) prevent the breakdown of bradykinin (a potent vasodilator) by AII. Currently, there are 10 ACE inhibitors available for clinical use, including captopril (Capoten), benazepril (Lotensin), enalapril (Vasotec), fosinopril (Monopril), lisinopril (Prinivil), moexipril (Univasc), perindopril (Aceon), quinapril (Accupril), ramipril (Altace), and trandolapril (Mavik). These drugs are very safe and efficacious and are often used as first-line drugs in the treatment of both heart failure and hypertension. The therapeutic effects of the ACE inhibitors are related to their potent cardiovascular effects. They may be used alone or in combination with other drugs such as diuretics in the treatment of hypertension or heart failure. Because of their ability to decrease SVR and preload, ACE inhibitors can stop the progression of left ventricular hypertrophy (sometimes seen after a myocardial infarction [MI]), a pathologic process known as ventricular remodeling. The ability of ACE inhibitors to prevent this is termed a cardioprotective effect. ACE inhibitors have been shown to have a protective effect on the kidneys, because they reduce glomerular filtration pressure. This is one of the reasons that they are among the cardiovascular drugs of choice for diabetic patients. CNS effects of the ACE inhibitors include fatigue, dizziness, mood changes, headaches, and a characteristic dry, nonproductive cough reversible with discontinuation of the therapy. The most pronounced symptom of an overdose is hypotension. Treatment is symptomatic and supportive and includes the administration of intravenous fluids to expand volume. All ACE inhibitors are contraindicated in lactating women, children, and in patients with bilateral renal artery stenosis. All ACE inhibitors carry a black box warning regarding fetal toxicity and should be avoided in pregnancy. Angiotensin II Receptor Blockers Angiotensin II receptor blockers (ARBs) are similar to the ACE inhibitors. The class includes losartan (Cozaar), eprosartan (Teveten), valsartan (Diovan), irbesartan (Avapro), Copyright © 2020 Elsevier Inc. All Rights Reserved. 89 candesartan (Atacand), olmesartan (Benicar), telmisartan (Micardis), and azilsartan (Edarbi). In contrast to ACE inhibitors, the ARBs affect primarily vascular smooth muscle and the adrenal gland. By selectively blocking the binding of AII to the type 1 AII receptors in these tissues, ARBs block vasoconstriction and the secretion of aldosterone. The end result is a decrease in blood pressure. Clinically, ACE inhibitors and ARBs appear to be equally effective for the treatment of hypertension, but ARBs do not cause cough. ARBs are better tolerated and are associated with lower mortality after MI than ACE inhibitors. It is not yet clear whether ARBs are as effective as ACE inhibitors in treating heart failure (cardioprotective effects) or in protecting the kidneys, as in diabetes. Both types of drugs are contraindicated for use in the second or third trimester of pregnancy. The therapeutic effects of ARBs are related to their potent vasodilating properties. The beneficial hemodynamic effect of ARBs is their ability to decrease SVR. The most common adverse effects of ARBs are upper respiratory tract infections and headache. Occasionally dizziness, inability to sleep, diarrhea, dyspnea, heartburn, nasal congestion, back pain, and fatigue can occur. Hyperkalemia is less likely than with the ACE inhibitors. All ARBs carry a black box warning regarding fetal toxicity and should not be used in pregnancy. Overdose may manifest as hypotension and tachycardia; bradycardia occurs less often. Treatment is symptomatic and supportive. Calcium Channel Blockers Calcium channel blockers may be used to treat angina, dysrhythmias, and hypertension and help to reduce blood pressure by causing smooth muscle relaxation and dilatation of blood vessels. If calcium is not present, then the smooth muscle of the blood vessels cannot contract. CCBs are also effective antidysrhythmics. Amlodipine (Norvasc) is the CCB most commonly used for hypertension. Nimodipine can prevent the cerebral artery spasms that can occur after a subarachnoid hemorrhage. CCBs are also sometimes used in the treatment of Raynaud’s disease and migraine headache. CCBs are used in combination with other drugs, such as amlodipine/atorvastatin (Caduet), which is both an antihypertensive and a cholesterol-lowering drug, and amlodipine/benazepril (Lotrel), amlodipine/olmesartan (Azar), and amlodipine/valsartan (Exforge), which each combine a CCB with an ARB to treat hypertension. Diuretics Diuretics are a highly effective class of antihypertensive drugs. They are listed as the current first-line antihypertensives in the JNC 8 guidelines for the treatment of hypertension. Their primary therapeutic effect is decreasing the plasma and extracellular fluid volumes, which results in decreased preload, cardiac output, and total peripheral resistance, thereby decreasing the workload of the heart. Copyright © 2020 Elsevier Inc. All Rights Reserved. 90 The thiazide diuretics are the most commonly used diuretics for treatment of hypertension. Vasodilators Vasodilators act directly to relax arteriolar and/or venous smooth muscle; they include minoxidil, hydralazine (Apresoline), diazoxide (Hyperstat), and nitroprusside (Nitropress). Direct-acting vasodilators are useful because of their ability to directly cause peripheral vasodilation, resulting in a reduction in SVR. Sodium nitroprusside and intravenous diazoxide are reserved for the management of pertensive emergencies, in which blood pressure is severely elevated. Diazoxide has many undesirable adverse effects, including dizziness, headache, orthostatic hypotension, dysrhythmias, sodium and water retention, nausea, vomiting, and hyperglycemia in diabetic patients. A new combination drug product is a tablet that contains both 37.5 mg of hydralazine and 20 mg of the antianginal drug isosorbide dinitrate. This drug, known as BiDil, has demonstrated improved patient survival and prolonged time to hospitalization for heart failure in African-American patient populations. Adverse effects of hydralazine include dizziness, headache, anxiety, tachycardia, edema, dyspnea, nausea, vomiting, diarrhea, hepatitis, systemic lupus erythematosus, and rash. Adverse effects of minoxidil include T-wave electrocardiographic changes, pericardial effusion or tamponade, angina, breast tenderness, rash, and thrombocytopenia. Adverse effects of sodium nitroprusside include bradycardia, decreased platelet aggregation, rash, hypothyroidism, hypotension, methemoglobinemia, and, rarely, cyanide toxicity. The main symptom of diazoxide overdose or toxicity is hypotension; treatment is supportive and symptomatic. If necessary, pressor drugs can be infused to quickly raise blood pressure. Three newer medications exemplify some of the antihypertensive drugs most recently made available, including eplerenone (Inspra), bosentan (Tracleer), and treprostinil (Remodulin); all are for adult use only. Epleronone (Inspra) is currently the only drug in a new class of drugs called selective aldosterone blockers. It reduces blood pressure by blocking the actions of aldosterone at its corresponding receptors in the kidney, heart, blood vessels, and brain. Nursing Process Assessment Obtain a thorough health history and perform a head-to-toe physical assessment. Measure and document blood pressure, pulse rate, respirations, pulse oximetry readings, and monitor laboratory tests. A thorough nursing assessment includes determining whether the patient has any underlying causes of hypertension, such as renal or liver dysfunction, a stressful lifestyle, Cushing’s disease, Addison's disease, renal artery stenosis, peripheral vascular disease, or pheochromocytoma. Always assess for the presence of contraindications, cautions, and potential drug Copyright © 2020 Elsevier Inc. All Rights Reserved. 91 interactions before administering any of the antihypertensive drugs. Contraindications include a history of MI or chronic renal disease. Cautious use is recommended in patients with renal insufficiency or glaucoma. Drugs that interact with antihypertensive drugs include other antihypertensive drugs, anesthetics, and diuretics. Exercise caution with the use of these drugs in the elderly and those with chronic illnesses because of further compromise of the physical condition of these patients due to uncontrolled or untreated hypertension or the adverse effects of antihypertensives. Use of alpha-adrenergic agonists demands close assessment of the patient’s blood pressure, pulse rate, and weight before and during treatment. If the drug is a nonselective beta blocker, it blocks both beta1 and beta2 receptors and will have both cardiac and respiratory effects, whereas if a drug is only a beta1-blocking drug, the cardiac system will be affected but there will be no beta2 effects, which limits any concern regarding respiratory problems, such as bronchoconstriction. With the use of beta blockers, assess blood pressure and apical pulse rate immediately before each dose. If the systolic blood pressure is less than 90 mm Hg or the pulse rate is less than 60 beats/min, notify the prescriber because of the risk of adverse effects. In addition, for patients with heart failure, understand that beta blockers also have a negative inotropic effect on the heart (decreased contractility); their use would lead to worsening of heart failure. With ACE inhibitors, assess blood pressure, apical pulse rate, and respiratory status. Perform a baseline neurologic assessment with the use of vasodilators, with attention to level of consciousness and cognitive ability. Use these drugs with extreme caution with the elderly because they are more sensitive to the drugs’ effects and experience more problems with hypotension, dizziness, and syncope. Other factors to be assessed in any patient receiving these drugs, as well as most other drugs, include the patient’s cultural background, racial or ethnic group, reading level, learning needs, developmental and cognitive status, financial status, mental health status, available support systems, and overall physical health. Consideration of the patient’s cultural and ethnic group is particularly important with antihypertensives, because research studies have documented differences in responses to antihypertensives among different racial and ethnic groups. Implementation Goals should include making sure the patient understands the nature of the disease, its symptoms and treatment, and the importance of adhering to the treatment regimen. Hypertension is managed by both pharmacologic and nonpharmacologic measures. Patients need to consume a diet low in fat, make any other necessary modifications in their diet, engage in regular supervised exercise, and reduce the amount of stress in their lives. Many patients have problems complying with treatment because the disease itself is silent or without symptoms. Inform patients that any abrupt withdrawal is a serious concern because of the risk of developing rebound hypertension, a sudden and very high elevation of blood pressure. Copyright © 2020 Elsevier Inc. All Rights Reserved. 92 Patients taking alpha-adrenergic agonists will need to monitor their blood pressure and pulse rate at home or have these parameters measured by a family member who has received instructions or by other professionals. Provide clear and concise instructions about reporting adverse effects and instructions for taking blood pressure and pulse rates. There are various free tools and applications (apps) available through a smart phone for a patient to use in monitoring blood pressure, pulse, etc., such as a printable blood pressure tracker and medication chart available at heart.org sponsored by the American Heart Association and a Blood Pressure Companion application (app). Monitor the patient's progress in the use of proper blood pressure/pulse-taking techniques. If a beta1 blocker causes shortness of breath, it is most likely due to edema and/or exacerbation of heart failure. Report any dizziness, postural hypotension, edema, constipation, or sexual dysfunction to the prescriber immediately. If angioedema occurs with ACE inhibitors, contact the prescriber immediately. If any drug must be discontinued, weaning is recommended to avoid rebound hypertension. If hypovolemia or hepatic dysfunction occurs with ARBs, the dose may need to be reduced. Nursing considerations for vasodilator are similar to those for other antihypertensives; however, the impact of the vasodilators on blood pressure may be more drastic. Emphasize the importance of safety and the need to avoid smoking and excessive alcohol intake as well as excessive exercise, hot climates, saunas, hot tubs, and hot environments. Heat may precipitate vasodilation and lead to worsening of hypotension with the risk for lightheadedness, dizziness, fainting, and possible injury to self. Evaluation The most important aspect of the evaluation process is collecting data and monitoring patients for evidence of controlled blood pressure. Blood pressure must be maintained at values lower than the parameters established by the Joint National Committee or below the levels set by the Joint National Committee for “prehypertension,” namely, a systolic blood pressure of 120 to 139 mm Hg and/or a diastolic blood pressure of 80 to 89 mm Hg. If compelling indications are present, such as diabetes mellitus or kidney disease, the blood pressure goal is often lower. Monitoring patients for the adverse effects and toxic effects of the various types of antihypertensive drugs helps to identify potentially life-threatening complications. Assess for contraindications associated with epleronone (Inspra), such as elevated serum potassium levels (greater than 5.5 mEq/L) or severe renal impairment. Assess for contraindications associated with epleronone (Inspra), a drug from a new class of drugs (selective aldosterone blockers), such as elevated serum potassium levels or severe renal impairment. This drug needs to be avoided in concurrent use of drugs that inhibit the action of cytochrome P-450 enzyme 3A4 such as antifungals, antivirals, and some antibiotic drugs. Bosentan (Tracleer) is only available through a limited distribution program, and is associated with contraindications of liver dysfunction and not to be given concurrently with cyclosporine or glyburide. Assess baseline blood pressure readings. Copyright © 2020 Elsevier Inc. All Rights Reserved. 93 The most important aspect of the evaluation process is collecting data and monitoring patients for evidence of controlled blood pressure. Changes in the fundus have been found to be a more reliable indicator of the long-term effectiveness of treatment than blood pressure readings because of the changes in the vasculature of the eye caused by high blood pressure. Therapeutic effects of antihypertensives in general include an improvement in blood pressure and in the disease process, with improved energy levels and decreased signs and symptoms of hypertension, such as less edema, improved breath sounds, no abnormal heart sounds, capillary refill in less than 5 seconds, and less shortness of breath (dyspnea). Copyright © 2020 Elsevier Inc. All Rights Reserved. 94 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 23: Antianginal Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview The heart’s oxygen supply is delivered to the heart muscle by means of the coronary arteries. The heart is a very aerobic (oxygen-requiring) muscle, and when it does not receive enough oxygen, pain (angina) occurs. Under ischemic conditions when the myocardium is deprived of oxygen, the heart shifts to anaerobic metabolism to meet its energy needs. One of the by-products of anaerobic metabolism is lactic acid. Accumulation of lactic acid and other metabolic by-products causes the pain receptors surrounding the heart to be stimulated, which produces the heart pain known as angina. Angina pectoris (chest pain) occurs because of a mismatch between the oxygen supply and oxygen demand, with either too high a demand for oxygen or too little oxygen delivery. Coronary artery disease is an abnormal condition of the arteries that delivers oxygen to the heart muscle. These arteries may become narrowed, which results in reduced flow of oxygen and nutrients to the myocardium. Poor blood supply to an organ is referred to as ischemia. The condition is called ischemic heart disease. When the coronary arteries that deliver oxygen to the heart muscle become blocked, a heart attack or myocardial infarction (MI) occurs. Many substances and situations can increase heart rate and contractility and oxygen demand, including caffeine, exercise, and stress, and result in stimulation of the sympathetic nervous system, leading to increased heart rate and contractility. Some of the drugs used to treat angina are aimed at correcting the imbalance between myocardial oxygen supply and demand by decreasing heart rate and contractility. There are three classic types of chest pain, or angina pectoris. o Chronic stable angina has atherosclerosis as its primary cause. Chronic stable angina can be triggered by exertion or other stress, as well as nicotine in tobacco, alcohol, coffee, and other drugs that stimulate the sympathetic nervous system. The pain of chronic stable angina is commonly intense but subsides within 15 minutes of either rest or appropriate antianginal drug therapy. o Unstable (preinfarction) angina is usually the early stage of progressive coronary artery disease, often ending in an MI in subsequent years. Another term for this type of angina is crescendo angina, because the pain increases in severity, as does the frequency of attacks. Later, pain may even occur while the patient is at rest. o Vasospastic angina results from spasms in the layer of smooth muscle that surrounds atherosclerotic coronary arteries, often occurring at rest and without any precipitating cause, but following a regular pattern, such as the same time of day. This type of angina is also called Prinzmetal angina or variant angina. Copyright © 2020 Elsevier Inc. All Rights Reserved. 95 o Dysrhythmias and electrocardiogram (ECG) changes often accompany these different types of anginal attacks. Pharmacology Overview The three main classes of drugs used to treat angina pectoris are the nitrates and nitrites, the beta blockers, and the calcium channel blockers (CCBs). Ranolazine (Ranexa) is the newest antianginal drug, approved by the FDA in 2006 for chronic angina. Its mechanism of action is unknown. Unlike other antianginal drugs, its antianginal and antiischemic effects do not involve reductions in heart rate or blood pressure. Ranolazine is known to prolong the QT interval on the ECG, so is reserved for patients who have failed to benefit from other antianginal drug therapy. There are three main therapeutic objectives of antianginal drug therapy: (1) minimizing the frequency of attacks and decrease the duration and intensity of the anginal pain; (2) improving the patient’s functional capacity with as few adverse effects as possible; and (3) preventing or delaying the worst possible outcome, MI. The overall goal of antianginal drug therapy is to increase blood flow to ischemic myocardium, decrease myocardial oxygen demand, or both. Nitrates or Nitrites Nitrates have long been the mainstay for both the prophylaxis and treatment for angina. Quick-onset nitrates are used to treat acute anginal attacks, while longer-onset nitrates are used for prophylaxis. The rapid- and long-acting nitrates available for clinical use include amyl nitrite (rapid acting), nitroglycerin (both rapid and long-acting), isosorbide dinitrate (both rapid and long-acting), and isosorbide mononitrate (primarily long-acting). Nitrates dilate constricted coronary arteries, helping to increase the supply of oxygen and nutrients to the heart muscle, but they also dilate all blood vessels, predominantly affecting venous vascular beds. The venous dilation results in a decrease in blood return to the heart (decreased preload), whereas the arterial dilation results in a decrease of peripheral resistance (decreased afterload—that is, the pressure or force against which the left ventricle must pump). However, they also have a dose-dependent arterial vasodilator effect. Nitroglycerin is the prototypical nitrate. Isosorbide dinitrates were the first group of oral drugs used to treat angina; isosorbide mononitrates are new and improved nitrates used for angina therapy. Exercise-induced spasms in atherosclerotic coronary arteries can also be reversed or prevented by administration of nitrates, encouraging healthy physical activity in patients. The nitrates are used to treat stable, unstable, and vasospastic (Prinzmetal) angina. Dosage forms include conventional tablets, translingual spray, controlled-release and sustained-release capsules, transdermal patch, topical ointment, and intravenous injection. If the goal of treatment is to abort or treat a sudden attack of angina, then rapid onset of action is needed, such as with intravenous infusion, sublingual tablet, and/or translingual spray, with pharmacokinetics that allow quick entry of the drug into the bloodstream. Nitrates are well tolerated, and most adverse effects are usually transient and involve the cardiovascular system. The most common undesirable effect is headache, which Copyright © 2020 Elsevier Inc. All Rights Reserved. 96 generally diminishes soon after the start of therapy. Other cardiovascular effects include tachycardia and postural hypotension. If nitrate-induced vasodilation occurs too rapidly, the cardiovascular system overcompensates and increases the heart rate, a condition referred to as reflex tachycardia. Topical nitrate dosage forms can produce various types of contact dermatitis (skin inflammation), but these are actually reactions to the dosage delivery system. Tolerance to the antianginal effects of nitrates can occur surprisingly quickly in some patients, especially those taking long-acting formulations or taking nitrates around the clock. Cross-tolerance arises when patients receive more than one nitrate dosage form. To prevent this, nitrate-free periods allow certain enzymatic pathways to replenish themselves. Beta Blockers Beta blockers are also used to relieve angina and do so by decreasing the heart rate, reducing workload on the heart, and decreasing oxygen demands. Most available beta blockers demonstrate antianginal efficacy, although not all have been approved for this use. Those approved are atenolol, metoprolol, nadolol, and propranolol. When beta receptors are blocked by beta blockers, the rate at which the pacemaker (sinoatrial [SA] node) fires decreases, and the time it takes for the node to recover increases. The beta blockers also slow conduction through the atrioventricular node and reduce myocardial contractility. Both effects serve to slow the heart rate and reduce myocardial oxygen demand, which aids in the treatment of angina by reducing the workload of the heart. Following an MI, there is a high level of circulating catecholamines that will produce harmful consequences if their actions go unopposed. They cause the heart rate to increase, which leads to a further imbalance in the supply-and-demand ratio, and irritate the conduction system of the heart, which can result in potentially fatal dysrhythmias. The beta blockers block all of these harmful effects, and their use has been shown to improve the chances for survival in patients after MI. The beta blockers are most effective in the treatment of exertional angina because the usual physiologic effects of an increase in the heart rate and systolic blood pressure that occurs during exercise or stress is blunted by the beta blockers, thereby decreasing the myocardial oxygen demand. For an elderly patient with significant angina, “exercise” may simply be carrying out the activities of daily living, such as bathing, dressing, or cooking. Systolic heart failure and serious conduction disturbances are contraindications to beta blockers. The adverse effects of the beta blockers result from their ability to block beta-adrenergic receptors in various areas of the body, resulting in a decrease in heart rate, cardiac output, and cardiac contractility, bronchoconstriction, and increased airway resistance. All beta blockers carry a black box warning regarding abrupt discontinuation emphasizing the critical importance of tapering when a beta blocker has been discontinued. Calcium Channel Blockers Copyright © 2020 Elsevier Inc. All Rights Reserved. 97 There are three chemical classes of CCBs: phenylalkylamines, benzothiazepines, and dihydropyridines, commonly represented by verapamil, diltiazem, and amlodipine, respectively. Relaxation of the smooth muscles that surround the coronary arteries causes them to dilate, increasing blood flow to the ischemic heart, which in turn increases the oxygen supply and helps shift the supply/demand ratio back to normal. Because of the CCB’s very acceptable adverse effect and safety profiles, they are considered first-line drugs for the treatment of such conditions as angina, hypertension, and supraventricular tachycardia and are often effective for the treatment of coronary artery spasms (vasospastic or Prinzmetal angina). The adverse effects of the CCBs are limited and primarily relate to overexpression of their therapeutic effects. In review, antianginal drugs such as nitrates, nitrites, beta blockers, and CCBs are used to reduce ischemia by increasing the delivery of oxygen-rich blood to cardiac tissues or by reducing oxygen consumption by the coronary vessels. Either of these mechanisms can reduce ischemia and lead to a decrease in anginal pain. Nursing Process Before antianginal drugs are administered, obtain a thorough past and present medical health history and medication history, and document the findings. Also measure weight, height, and vital signs, with attention to supine, sitting, and standing blood pressures. If the patient is experiencing pain, include description of onset, character, intensity, location, duration, precipitating factors, alleviating factors, and presence of nausea or vomiting. Significant interactions include alcohol, beta blockers, CCBs, phenothiazines, and erectile dysfunction drugs, such as sildenafil, tadalafil, and vardenafil. Taking these drugs with nitrates will result in worsening of hypotensive responses, paradoxical bradycardia, and a resultant increase in angina with subsequent significant risk of cardiac or cerebrovascular complications due to the decreased perfusion. Older adult patients often have difficulty with blood pressure control because of the occurrence of normal age-related periods of hypotension, and the use of antianginals may lead to worsening of hypotensive responses. Concerns arise with the use of nonselective beta blockers and beta2 blockers in patients with bronchospastic disease because of the drug-related effects of bronchoconstriction and increased airway resistance, which results in wheezing and dyspnea as adverse effects. In patients taking CCBs, assess for possible drug-food interactions and toxicity, including grapefruit juice, which reduces the metabolism of nifedipine. Assess patients taking ranolazine (Ranexa), one of the newest antianginal drugs, for liver dysfunction through specific liver function testing before taking the medication. Always review and/or record the patient’s vital signs and description of chest pain for the duration of therapy. Include in your evaluation a review for accomplishment of goals and outcomes, such as appropriate decrease in blood pressure, increase in cardiac output and tissue perfusion Copyright © 2020 Elsevier Inc. All Rights Reserved. 98 with decrease in angina, and a gradual increase in activity and performance of activities of daily living without exacerbation of anginal episodes. CCBs and beta blockers may be associated with the adverse effects of postural hypotension, dizziness, headache, and edema. The nonselective beta blockers may exacerbate congestive heart failure, problems related to respiratory bronchospasm, and hypoglycemia. Check the patient’s pulse rate before drug administration, and if it is 60 beats/min or lower, contact the prescriber for further instructions. Instruct patients to always keep a fresh supply of sublingual nitroglycerin on their person and in their home because the drug is stable for only 3 to 6 months. The use of smart pump technology has reduced the incidence of errors, but the nurse must still understand the difference between ‘mL/hr” and “mcg/min” when programming the infusion rates. Infusion rates are not interchangeable with ordered doses! Some health care institutions also require two nurses to double-check infusion pump settings before intravenous medication therapy is begun. Patches are worn for 12 to 14 hours per day to decrease tolerance to its effect. Before a new patch is applied, locate and remove the old patch and clean the skin of any residual drug. Carefully dispose of used, unneeded, or defective transdermal patches of any medication. Follow drug insert instructions for disposal to avoid the possible contact with residual drug by babies, children, pets, and adults. Instruct the patient on how to self-monitor and record blood pressure, pulse rate, and daily weights. Maintaining a journal with this information as well as responses and/or adverse effects related to the medication regimen is important to safe and effective therapy. Copyright © 2020 Elsevier Inc. All Rights Reserved. 99 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 24: Heart Failure Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Heart failure is a clinical syndrome caused by numerous cardiac disorders. It is a pathologic state in which the heart is unable to pump blood in sufficient amounts from the ventricles to meet the body’s metabolic needs, or can do so only at elevated filling pressures. The signs and symptoms typically associated with this insufficiency make up the syndrome of heart failure. Heart failure occurs due to a reduced ratio of ejection fraction to left ventricular enddiastolic volume. The physical defects causing heart failure are of two types: (1) a myocardial defect such as myocardial infarction (MI) or valve insufficiency, which leads to inadequate cardiac contractility and ventricular filling; and (2) a defect outside the myocardium (e.g., coronary artery disease, pulmonary hypertension, or diabetes), which results in an overload on an otherwise normal heart. Heart failure can be stratified into classes using the older New York Heart Association’s (NHYA) functional classification or the more recent American College of Cardiology Foundation/American Heart Association (ACCF/AHA) stages of heart failure. The best way to prevent heart failure is to control risk factors associated with heart failure including hypertension, coronary artery disease, obesity, and diabetes. Drug therapy is individualized based on the patient’s class of heart failure. Pharmacology Overview Inotropic drugs affect the force of myocardial contraction; positive inotropics (e.g., digoxin) increase the force of contractions, and negative inotropics (e.g., beta blockers, calcium channel blockers) decrease myocardial contractility. Chronotropics affect heart rate per minute, with positive chronotropics increasing heart rate and negative chronotropics decreasing the heart rate. Dromotropic drugs affect the conduction of electrical impulses through the heart; positive dromotropic drugs increase the speed of electrical impulses through the heart, whereas negative dromotropic drugs have the opposite effect. Be aware of the important physiologic concepts such as ejection fraction. A patient’s ejection fraction reflects the contractility of the heart and is about 65% (0.65) in a normal heart. This value decreases as heart failure progresses; therefore, patients with heart failure have low ejection fractions because their hearts are failing to pump effectively. American Heart Association and American College of Cardiology Guidelines for the Diagnosis and Management of Heart Failure in Adults (updated in 2013) approach to the treatment of chronic heart failure revolves around reducing the effects of the reninangiotensin-aldosterone system and the sympathetic nervous system. Copyright © 2020 Elsevier Inc. All Rights Reserved. 100 o Drugs used for the initiation of therapy for heart failure include ACE inhibitors (lisinopril, enalapril, captopril, and others) or ARBs (valsartan, candesartan, losartan, and others) and certain beta blockers (metoprolol, a cardioselective beta blocker; carvedilol, a nonspecific beta blocker). o Loop diuretics (furosemide) are used to reduce the symptoms of heart failure secondary to fluid overload, and the aldosterone inhibitors (spironolactone, eplerenone) are added as the heart failure progresses. o Only after these drugs are used digoxin is added. o Hydralazine/isosorbide dinitrate became the first drug approved specifically for use in the African-American population. o Two new classes of drugs were approved in 2015; the sinoatrial modulators and the angiotensin receptor-neprilysin inhibitors. Angiotensin-Converting Enzyme Inhibitors The ACE inhibitors are a class of drugs that inhibit angiotensin-converting enzyme, which is responsible for converting angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor and induces aldosterone secretion by the adrenal glands. Aldosterone stimulates sodium and water resorption, which can raise blood pressure. Together, these processes are referred to as the renin-angiotensin-aldosterone system. The ACE inhibitors are beneficial in the treatment of heart failure because they prevent sodium and water resorption by inhibiting aldosterone secretion. This causes diuresis, which decreases blood volume and blood return to the heart. This in turn decreases preload, or the left ventricular end-diastolic volume, and the work required of the heart. A dry cough is common with ACE inhibitors. Angiotensin II Receptor Blockers The therapeutic effects of ARBs in heart failure are related to their potent vasodilating properties. They may be used alone or in combination with other drugs such as diuretics in the treatment of hypertension or heart failure. The beneficial hemodynamic effect of ARBs is their ability to decrease systemic vascular resistance. The ARBs are not as likely to cause the cough associated with the ACE inhibitors. Valsartan and all ARBs share the same pregnancy concerns and potential for decreased renal function as the ACE inhibitors. Angiotensin Receptor-Neprilysin Inhibitors A new class of drugs, called the angiotensin receptor-neprilysin inhibitors (ARNI), was approved in 2015. The only drug in its class at the time of publication is valsartan/sacubitril (Entresto). Sacubitril is a neprilysin inhibitor that blocks the degradation of vasoactive peptides by inhibiting the neprilysin enzyme. Sacubitril is combined with valsartan, an ARB. The American College of Cardiology and American Heart Association give valsartan/sacubitril a Class I recommendation (strongest level) for the management of patients with heart failure with a reduced ejection fraction. Beta Blockers Copyright © 2020 Elsevier Inc. All Rights Reserved. 101 Beta blockers work by reducing or blocking sympathetic nervous system stimulation to the heart and the heart’s conduction system. By doing this, beta blockers prevent catecholamine-mediated actions on the heart. This is known as a cardioprotective quality of beta blockers. The resulting cardiovascular effects include reduced heart rate, delayed atrioventricular (AV) node conduction, reduced myocardial contractility, and decreased myocardial automaticity. Metoprolol is the beta blocker most commonly used to treat heart failure. Carvedilol (Coreg) has many effects, including acting as a nonselective beta blocker, an alpha1 blocker, and possibly a calcium channel blocker and antioxidant. It is used primarily in the treatment of heart failure but is also beneficial for hypertension and angina. It has been shown to slow the progression of heart failure and to decrease the frequency of hospitalization in patients with mild to moderate (class II or III) heart failure. Aldosterone Antagonists Aldosterone antagonists spironolactone and eplerenone are useful in severe stages of heart failure. Activation of the renin-angiotensin-aldosterone system causes increased levels of aldosterone, which causes retention of sodium and water, leading to edema that can worsen heart failure. Spironolactone (Aldactone) is a potassium-sparing diuretic that also acts as an aldosterone antagonist, which has been shown to reduce the symptoms of heart failure. Eplerenone (Inspra) is a selective aldosterone blocker, blocking aldosterone at its receptors in the kidney, heart, blood vessels, and brain. Miscellaneous Heart Failure Drugs Hydralazine/isosorbide dinitrate (BiDil) was the first drug approved for a specific ethnic group, namely African Americans. Dobutamine is a beta1-selective vasoactive adrenergic drug that is structurally similar to the naturally occurring catecholamine dopamine. Dobutamine increases cardiac output by increasing contractility (positive inotropy), which increases the stroke volume, especially in patients with heart failure. Ivabradine (Corlanor) is the first drug in a new class of drugs called sinoatrial node modulators. It inhibits f-channels within the sinoatrial node which ultimately results in reduced heart rate. Ivabradine is indicated to reduce the risk of hospitalization in patients with stable, symptomatic heart failure with an ejection fraction of less than or equal to 35%. B-Type Natriuretic Peptide The newest class of medications for heart failure, the B-type natriuretic peptides, currently includes only one drug, nesiritide. Nesiritide is a synthetic B-type natriuretic hormone that has vasodilating effects on both arteries and veins. This vasodilation takes place in the heart itself and throughout the body. The effects of nesiritide have been shown to include diuresis, natriuresis, and vasodilation. These properties lead to an indirect increase in cardiac output and suppression of neurohormonal systems such as the renin-angiotensin system. Copyright © 2020 Elsevier Inc. All Rights Reserved. 102 Nesiritide is used in the intensive care setting as a final effort to treat severe, lifethreatening heart failure, often in combination with several other cardiostimulatory medications. Its use is no longer recommended as a first-line drug for heart failure. Phosphodiesterase Inhibitors Phosphodiesterase inhibitors (PDIs) are a group of inotropic drugs that work by inhibiting the action of an enzyme called phosphodiesterase. Presently only one drug in this category is available in the United States: milrinone (Primacor). Milrinone causes an intracellular increase in cyclic adenosine monophosphate (cAMP), which results in two beneficial effects in a patient with heart failure: a positive inotropic response and vasodilation. For this reason, this class of drugs may also be referred to as inodilators (inotropics and dilators). Recognize that hypotension, dysrhythmias, and thrombocytopenia are major adverse effects of milrinone. PDIs are primarily used in the intensive care setting for the short-term management of acute heart failure. The primary adverse effect seen with milrinone therapy is ventricular dysrhythmia. Concurrent administration of diuretics may cause significant hypovolemia and reduced cardiac filling pressure. Appropriately monitor the patient in an intensive care setting to detect and respond to these problems. Cardiac Glycosides Digoxin is primarily used in the treatment of systolic heart failure and atrial fibrillation. The latest heart failure treatment guidelines recommend that digoxin be used as an adjunct to drugs of other classes, including beta blockers, diuretics, ACE inhibitors, and ARBs. Digoxin is the only cardiac glycoside currently available in the United States. Although a powerful positive inotropic drug, it has not been shown to reduce mortality. The beneficial effect of digoxin is thought to be an increase in myocardial contractility— known as a positive inotropic effect. Digoxin decreases the velocity (rate) of electrical conduction and prolongs the refractory period in the conduction system. The common undesirable effects associated with digoxin use are cardiovascular, central nervous system, ocular, and gastrointestinal effects. Digoxin has a low therapeutic index, so levels are monitored when the patient first starts taking the drug. Low potassium or magnesium levels may increase the potential for digoxin toxicity. Estimates are that as many as 20% of patients taking digoxin exhibit symptoms of toxicity. A decrease in renal function is also a common cause of digoxin toxicity, because digoxin is excreted almost exclusively via the kidneys. Signs and symptoms of digoxin toxicity include bradycardia, headache, dizziness, confusion, nausea, and visual disturbances (blurred vision or yellow vision). With toxicity, electrocardiographic (ECG) findings may include heart block, atrial tachycardia with block, or ventricular dysrhythmias. When significant toxicity develops as a result of digoxin therapy, digoxin immune Fab may be indicated. Digoxin immune Fab is an antibody that recognizes digoxin as an antigen and forms an antigen-antibody complex with the drug, thus inactivating the free digoxin. Copyright © 2020 Elsevier Inc. All Rights Reserved. 103 Incorrect decimal placement can be lethal when calculating digoxin dosages. According to the Institute for Safe Medication Practices (ISMP), trailing zeros are not to be used after decimal points. The ISMP also recommends that leading zeros be used if a dose is less than a whole number. Keep informed of the contraindications to the use of digoxin, which include a history of allergy to the digitalis medications, ventricular tachycardia and fibrillations, and AV block. Nursing Process Perform a thorough assessment, including assessment of the patient’s past and present medical history, drug allergies, and family medical history with emphasis on any history of cardiac, hypertensive, or renal diseases. Hyperkalemia is an adverse effect; therefore, perform an assessment of serum potassium before giving these drugs and administer potassium supplementation and/or potassiumsparing diuretics with caution. Assess respiratory history, specifically any previous problems of cough. ACE inhibitors may cause a dry cough, which is not harmful but may be annoying. Aldosterone antagonists, such as spironolactone and eplerenone, require close assessment of heart and breath sounds as well as for the occurrence of edema, a known adverse effect. It is always important to assess support systems at home, because safe and effective therapy depends on close observation, monitoring of appropriate parameters (e.g., daily weight), attention to patient complaints, and evaluation of how the patient is feeling and functioning. Before giving digoxin, closely monitor the apical pulse rate and serum electrolytes, especially potassium levels because low levels or hypokalemia may precipitate toxicity. Nesiritide is strictly used in an intensive care setting in very ill patients who are experiencing acute decompensated heart failure and receiving continuous cardiac monitoring. While the drug is being administered intravenously, monitor the patient for all of its severe adverse effects, such as hypotension, dysrhythmias, headache, and abdominal pain. Avoid co-administration of drugs that decrease the patient’s blood pressure, such as ACE inhibitors and diuretics, if at all possible. Always check for compatibility of solutions when giving the PDI milrinone. Recognize that hypotension, dysrhythmias, and thrombocytopenia are major adverse effects of milrinone. The drug, ivabradine (Corlanor), is a newer drug in the class of sinoatrial node modulators. Assess baseline cardiac status because of the increased risk of atrial fibrillation, bradycardia, and other conduction disturbances. If ARNIs are used, educate about the common side effects of hypotension, hyperkalemia, and increased serum creatinine. Because of these side effects, periodic monitoring of serum potassium, renal functioning, and blood pressure are needed. Record intake and output, heart rate, blood pressure, daily weight, respiration rate, and heart and breath sounds. Report any evidence of hypokalemia to the prescriber immediately, and monitor the patient closely. Copyright © 2020 Elsevier Inc. All Rights Reserved. 104 When heart failure drugs, such as digoxin, milrinone, and digoxin immune Fab, are administered parenterally, use an infusion pump unless the order is to administer them as an intravenous push. Monitoring patients after the administration of drugs to improve heart contractility, or positive inotropic drugs, is critical for identifying therapeutic effects and adverse effects. The therapeutic effects of these drugs include increased urinary output, decreased edema, decreased dyspnea and crackles, decreased fatigue, resolution of paroxysmal nocturnal dyspnea, and improved peripheral pulses, skin color, and temperature. Copyright © 2020 Elsevier Inc. All Rights Reserved. 105 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 25: Antidysrhythmic Drugs Key Points Anatomy, Physiology, and Pathophysiology Overview Dysrhythmias and Normal Cardiac Electrophysiology Any disturbance or abnormality in the normal pattern of the heartbeat and pulse rate is termed a dysrhythmia. The term arrhythmia (literally “no rhythm”) implies asystole or no heartbeat at all. Dysrhythmias are usually serious and may require treatment with an antidysrhythmic drug or nonpharmacologic therapies; however, not all dysrhythmias require medical treatment. Disturbances in cardiac rhythm are the result of abnormally functioning cardiac cells. Antidysrhythmic drugs are used to correct dysrhythmias; however, they may also cause dysrhythmias, and for this reason are said to be prodysrhythmic. Cardiac cells become excited when there is a change in the baseline distribution of ions across their membranes that leads to the propagation of an electrical impulse. Action potentials occur in a continuous and regular manner in the cells of the cardiac conduction system, such as the sinoatrial node (SA), atrioventricular node (AV), and HisPurkinje system. All of these tissues have the property of spontaneous electrical excitability known as automaticity. This excited state creates action potentials, which in turn generate electrical impulses that travel through the myocardium ultimately to create the heartbeat via contraction of cardiac muscle fibers. The SA node is the pacemaker because it can spontaneously depolarize easier and faster than the other areas. The level of the resting membrane potential (RMP) for a given type of cell is an important determinant of the rate of its impulse conduction to other cells. In Purkinje cells, electrical conduction is relatively fast, and therefore electrical impulses are conducted quickly. These cells are referred to as fast-response cells, or fast-channel cells. Many antidysrhythmic drugs affect the RMP and sodium channels, which in turn influence the rate of impulse conduction. The SA node, AV node, and His-Purkinje system are all areas in which there is automaticity (cells can depolarize spontaneously). The SA node is the pacemaker because it can spontaneously depolarize easier and faster than the other areas. The cells of the SA node have a slower upstroke velocity. Any abnormality in cardiac automaticity or impulse conduction often results in some type of dysrhythmia. Electrocardiography Electrophysiological cardiac events correspond to the tracings of an electrocardiogram. The P wave corresponds to spontaneous impulse generation in the SA node followed immediately by depolarization of atrial myocardial fibers and their muscular contraction. Copyright © 2020 Elsevier Inc. All Rights Reserved. 106 This normally determines the heart rate. The QRS complex (or QRS interval) corresponds to depolarization and contraction of ventricular fibers. The J point marks the start of the ST segment, which corresponds to the beginning of ventricular repolarization. The T wave corresponds to completion of the repolarization of these ventricular fibers. Common Dysrhythmias Dysrhythmias are subdivided into several broad categories depending on their anatomic site of origin in the heart. o Supraventricular dysrhythmias originate above the ventricles in the SA or AV node or atrial myocardium. o Ventricular dysrhythmias originate below the AV node in the His-Purkinje system or ventricular myocardium. o Dysrhythmias that originate outside the conduction system (i.e., in atrial or ventricular cells) are called ectopic and their points of origin are called ectopic foci. Conduction blocks are dysrhythmias that involve disruption of impulse conduction between the atria and ventricles through the AV node, directly affecting ventricular function. They may also originate in the His-Purkinje system. Less commonly, impulse conduction between the SA and AV node is affected. Among the supraventricular dysrhythmias, atrial fibrillation is a very common condition characterized by rapid atrial contractions that incompletely pump blood into the ventricles. Atrial fibrillation is notable in that it predisposes the patient to stroke. AV nodal reentrant tachycardia (AVNRT) is a conduction disorder that often gives rise to a dysrhythmia known as paroxysmal supraventricular tachycardia (PSVT). Varying degrees of AV block (often called heart block) involve different levels of disrupted conduction of impulses from the AV node and His-Purkinje system to the ventricles. Premature ventricular contractions (PVCs) occur when impulses originate from ectopic foci within the ventricles (His-Purkinje system). They become problematic when they occur frequently enough to compromise systolic blood volume. Ventricular tachycardia refers to a rapid heartbeat from impulses originating in the ventricles. It can be nonsustained (brief) or sustained, requiring definitive treatment. Worsening ventricular tachycardia can deteriorate into torsades de pointes, an intermediate dysrhythmia that often deteriorates into ventricular fibrillation. Ventricular fibrillation is fatal if not reversed, which most often requires defibrillation. Pharmacology Overview Antidysrhythmic Drugs Antidysrhythmic drugs are used to correct dysrhythmias; however, they may also cause dysrhythmias, and for this reason are said to be prodysrhythmic. The Vaughan Williams classification is the system most commonly used to categorize antidysrhythmic drugs. It classifies drugs into the following groups according to where and how they affect cardiac cells and what their mechanisms of action is: Copyright © 2020 Elsevier Inc. All Rights Reserved. 107 o Class I: membrane-stabilizing drugs (e.g., class Ia, quinidine; class Ib, lidocaine; class Ic, flecainide); these drugs exert their actions on the sodium (fast) channels. o Class II: beta-adrenergic blockers that depress phase 4 depolarization (e.g., atenolol); these drugs are commonly used as antihypertensives, working by blocking sympathetic nervous system stimulation to the heart and, as a result, the transmission of impulses in the heart’s conduction system. These drugs mostly affect slower-conducting cardiac tissues. o Class III: drugs that prolong repolarization in phase 3 (e.g., amiodarone and dofetilide); these drugs affect fast tissue and are most commonly used to manage dysrhythmias that are difficult to treat. o Class IV: calcium channel blockers that depress phase 4 depolarization (e.g., verapamil); these drugs work specifically by inhibiting the calcium channels, which reduces the influx of calcium ions during action potentials. Diltiazem and verapamil are the calcium channel blockers most commonly used to treat cardiac dysrhythmias. Flecainide has a black box warning regarding increased mortality and proarrhythmic effects. Propafenone has a black box warning regarding proarrhythmic effects. The role of class II drugs (beta blockers) continues to grow in the field of cardiology, including in dysrhythmia management. Class III drugs have emerged as among the most widely used antidysrhythmics at this time. Dronedarone (Multaq) is the newest drug. It is very similar to amiodarone and is thought to have less potential for causing the classic amiodarone adverse effects and less potential for drug interactions. Dronedarone has a black box warning regarding risk of death, stroke, and heart failure. In 2011, the FDA issued an advisory regarding the potential for hepatotoxicity related to dronedarone. Dofetilide (Tikosyn) is one of the newer antidysrhythmic drugs. Because dofetilide can cause serious toxicity, specifically torsades de pointes, only physicians who have received special training are allowed to prescribe it. Dofetilide therapy must be initiated in the hospital. The class IV drugs (calcium channel blockers) have limited usefulness in treating tachydysrhythmias (dysrhythmias involving tachycardia). Digoxin still has a place in dysrhythmia management, especially in the prevention of dangerous ventricular tachydysrhythmias secondary to atrial fibrillation. Adverse effects common to most antidysrhythmics include hypersensitivity reactions, nausea, vomiting, and diarrhea. Other common effects include dizziness, headache, and blurred vision. In addition, many antidysrhythmics are themselves capable of producing new dysrhythmias (prodysrhythmic effect). The main toxic effects of the antidysrhythmics involve the heart, circulation, and central nervous system (CNS). Specific antidotes are not available, and the management of an overdose involves maintaining adequate circulation and respiration. Significant interactions are those that can result in dysrhythmias, hypotension or hypertension, respiratory distress, or excessive therapeutic or toxic drug effects. One particular interaction common to many antidysrhythmics is the potentiation of Copyright © 2020 Elsevier Inc. All Rights Reserved. 108 anticoagulant activity with warfarin (Coumadin). Because many patients receiving antidysrhythmic therapy also need warfarin, the international normalized ratio (INR) must be closely monitored and necessary adjustments made to the warfarin dosage. This is especially true with amiodarone. Amiodarone also has a black box warning regarding hepatotoxicity, pulmonary toxicity, and proarhythmic effects. Sotalol has a black box warning regarding proarrhythmic effects. Nursing Process Before administering any antidysrhythmic to a patient, conduct a thorough nursing assessment and head-to-toe physical assessment, and complete a medical history and medication profile. Assess baseline levels of alertness and any increase in anxiety levels, and/or restlessness, which may indicate hypoxia. Nursing actions for the various antidysrhythmics include skillful nursing assessment and close monitoring of heart rate, blood pressure, heart rhythms, general well-being, skin color, temperature, and heart and breath sounds. Gender-based differences in the pattern and outcomes of the presentation of CVD remain complex with anatomical, physiological, and genetic factors to health behavior differences, delays in the response to symptoms, and under use of gold-standard testing and treatments. Review any baseline ECGs and interpret the results; measure the patient’s vital signs with attention to blood pressure, postural blood pressure, heart sounds, and heart rate, rhythm, and quality. Other signs and symptoms to assess for related to decreased cardiac functioning (as a result of dysrhythmia and decrease in cardiac output) include apical-radial pulse deficits, jugular vein distension, edema, prolonged capillary refill (longer than 5 seconds), decreased urinary output, activity intolerance, chest pain or pressure, dyspnea, and fatigue. Document any changes in level of alertness, increase in anxiety levels, syncope, or dizziness. With the use of lidocaine, assess the cardiovascular system, with attention to heart rate and blood pressure. With amiodarone, assess respiratory, thyroid, hepatic, dermatologic, and/or hypertensive conditions due to possible drug-related pulmonary toxicity, exacerbation of thyroid disorders, abnormal liver function tests, and rash. Amiodarone may lead to gastrointestinal upset, which may be prevented or decreased by taking the drug with food or a snack. Photosensitivity and photophobia are other concerns with this drug. When antidysrhythmics are administered, monitor vital signs, especially pulse rate and blood pressure; if pulse rate is lower than 60 beats/min, notify the prescriber. During the initiation of therapy, closely monitor the electrocardiogram and vital signs because of possible prolongation of the QT interval by more than 50%. The end result may be the occurrence of a variety of conduction disturbances. Advise patients that oral dosage forms are generally better tolerated if taken with food and fluids to help minimize gastrointestinal upset, unless otherwise ordered. Copyright © 2020 Elsevier Inc. All Rights Reserved. 109 With lidocaine, vials of clear solution are labeled as either for cardiac or not for cardiac use. This is important to remember when reading the vial’s label so that the wrong drug is not given. Beta blockers, diltiazem, and verapamil may all be used to manage abnormal rhythms and are to be given only after checking and documenting pulse rates and blood pressures. Contact the prescriber and withhold the drug—if supported by facility policy and the prescriber’s guidelines—if the pulse rate is 60 beats/min or lower or 100 beats/min or higher and/or the systolic blood pressure is 90 mm Hg or lower. With the use of dofetilide, continually monitor the patient for any changes in the ECG, especially over the first few days of treatment. This drug requires specialized monitoring once ordered by the prescriber, who must have received special prescription training. Encourage the patient to report any difficulty, such as chest pain, nausea, or diarrhea, to the prescriber immediately. Class I through class IV drugs have many overlapping therapeutic effects, adverse effects, and toxicities. Therapeutic effects, in general, include improved cardiac output; decreased chest discomfort; decreased fatigue; improved vital signs, skin color, and urinary output; and conversion of irregularities to normal rhythm. Adverse effects for the class I antidysrhythmics include hypotension, rash, diarrhea, systemic lupus erythematosus–like syndrome (procainamide); ECG changes, bitter taste, anorexia, blurred vision, and tinnitus (quinidine); and gingival hyperplasia and decrease in blood pressure and pulse rate (phenytoin). Class II beta blockers may cause bradycardia, AV block, heart failure, bronchospasm, and changes in blood glucose levels. Amiodarone, a class III drug, may lead to pulmonary toxicity, thyroid disorders, decrease in blood pressure and pulse rate, photosensitivity, and abnormal liver function. Calcium channel blockers or class IV drugs are associated with heart block, hypotension, constipation, dizziness, and dyspnea. The therapeutic responses to antidysrhythmics include a decrease in blood pressure in hypertensive patients, a decrease in edema, and restoration of a regular pulse rate or a pulse rate without major irregularities or with improved regularity compared with the irregularity that existed before therapy. Copyright © 2020 Elsevier Inc. All Rights Reserved. 110 Week 11- Assignment for preparation for the lecture/discussion to come this Thursday 4.7.2022 & 4.9.2022 Instructions: 1. Please create drug cards for the drugs in chapters, 26, 27, 28, 29, 31, 32, & 36 2. Review the key points from each chapter. 3. Go to the end of the chapters and complete the questions there and submit it to me via email for review. Chapter 26-Coagulation Modifier Drugs Copyright © 2020 Elsevier Inc. All Rights Reserved. 111 Chapter 27-Antilipemic Drugs Chapter 28-Diuretic Drugs Chapter 29- Fluids & Electrolytes Chapter 31 Thyroid and Anti-Thyroid Drugs Copyright © 2020 Elsevier Inc. All Rights Reserved. 112 Chapter 32- Diabetes Drugs Chapter 36- Drugs Affecting the Respiratory System Copyright © 2020 Elsevier Inc. All Rights Reserved. 113 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 26: Coagulation Modifier Drugs Chapter 26 1. d; 2. a, c, d; 3. b; 4. c; 5. b; 6. b, c, d; 7. 110 mg; 0.73 mL; 8. a, b, e. Key Points Anatomy, Physiology, and Pathophysiology Overview Hemostasis is a general term for any process that stops bleeding. This can be accomplished by either mechanical or surgical means. When hemostasis occurs as a result physiologic clotting of blood, it is called coagulation, which is the process of blood clot formation. The technical term for a blood clot is a thrombus. A thrombus that is not stationary but moves through blood vessels is called an embolus. Normal hemostasis involves the complex interaction of substances that promote clot formation and substances that either inhibit coagulation or dissolve the formed clot. Substances that promote coagulation include platelets, von Willebrand factor, activated clotting factors, and tissue thromboplastin. Substances that inhibit coagulation include prostacyclin, antithrombin III, and proteins C and S. In addition, tissue plasminogen activator is a natural substance that dissolves clots that are already formed. The coagulation system is called a cascade (or coagulation cascade) because each activated clotting factor serves as a catalyst that amplifies the next reaction. The result is a large concentration of a clot-forming substance called fibrin. Once a clot is formed and fibrin is present, the fibrinolytic system is activated. This system initiates the breakdown of clots and serves to balance the clotting process. Hemophilia is a rare genetic disorder in which the previously mentioned natural coagulation and hemostasis factors are limited or absent. Hemophilia is categorized into two main types depending on which of the coagulation factors is absent (factor VII, factor VIII, and/or factor IX). Patients with hemophilia can bleed to death if coagulation factors are not given. Pharmacology Overview Drugs that affect coagulation are commonly associated with adverse drug reactions. Coagulation modifiers work by preventing/promoting clot formation, lysing a preformed clot, and/or reversing the action of anticoagulants. Coagulation modifiers include anticoagulants, antiplatelets, thrombolytics, antifibrinolytics, and reversal drugs. Anticoagulants inhibit the action or formation of clotting factors and therefore prevent clots from forming. Antiplatelet drugs prevent platelet plugs from forming by inhibiting platelet aggregation, which can be beneficial in preventing heart attacks and strokes. Hemorheologic drugs alter platelet function without preventing the platelets from working. Copyright © 2020 Elsevier Inc. All Rights Reserved. 114 Sometimes clots form and totally block a blood vessel. When this happens in one of the coronary arteries, a heart attack occurs, and the clot must be lysed to prevent or minimize damage to the myocardial muscle. Thrombolytic drugs lyse (break down) clots, or thrombi, that have already formed. Antifibrinolytic drugs, also known as hemostatic drugs, have the opposite effect of these other classes of drugs; they actually promote blood coagulation and are helpful in the management of conditions in which excessive bleeding would be harmful. There are also several newer drug classes, including low–molecular-weight heparins (LMWHs), direct thrombin inhibitors, and selective factor Xa inhibitors. Anticoagulants Drugs that prevent the formation of a clot by inhibiting certain clotting factors are called anticoagulants. Once a clot forms on the wall of a blood vessel, it may dislodge and travel through the bloodstream as an embolus. If it lodges in a coronary artery, it causes a myocardial infarction (MI); if it obstructs a brain vessel, it causes a stroke; if it goes to the lungs, it is a pulmonary embolism; and if it goes to a vein in the leg, it is a deep vein thrombosis (DVT). Collectively, these complications are called thromboembolic events. Anticoagulants are also called antithrombotic drugs because they work to prevent the formation of a clot or thrombus, a condition known as thrombosis. All anticoagulants work in the clotting cascade but do so at different points. Heparin works by binding to a substance called antithrombin III, which turns off three main activating factors: activated factor II (thrombin), activated factor X, and activated factor IX. The drug name heparin usually refers to unfractionated heparin, which is a relatively large molecule derived from various animal sources. Low–molecular-weight heparins (LMWHs) are synthetic and have a smaller molecular structure; they include enoxaparin (Lovenox) and dalteparin (Fragmin). The LMWHs differ from heparin in that they are much more specific for activated factor X (Xa) than for activated factor II (IIa, or thrombin). Warfarin (Coumadin) works by inhibiting vitamin K synthesis by bacteria in the gastrointestinal tract. This, in turn, inhibits production of clotting factors II, VII, IX, and X, which are known as vitamin K–dependent clotting factors. It is used prophylactically to prevent clots from forming; it cannot lyse preformed clots. Fondaparinux (Arixtra) inhibits thrombosis by its specific action against factor Xa alone. Rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Savaysa), and betrixaban (Bevyxxa) are new oral-acting factor Xa inhibitors. There are also currently five antithrombin drugs that inhibit the thrombin molecules directly, one natural and four synthetic. The natural drug is human antithrombin III (Thrombate), which is isolated from the plasma of human donors. The synthetic drugs are lepirudin (Refludan), argatroban (Argatroban), bivalirudin (Angiomax), and dabigatran (Pradaxa). Dabigatran is a new oral direct thrombin inhibitor that was approved in 2010. All of these drugs work similarly to inhibit thrombus formation by inhibiting thrombin. Copyright © 2020 Elsevier Inc. All Rights Reserved. 115 The ability of anticoagulants to prevent clot formation is of benefit in certain settings in which there is likelihood of clot formation, including MI, unstable angina, atrial fibrillation, use of indwelling devices such as mechanical heart valves, and conditions in which blood flow may be slowed and blood may pool, such as major orthopedic surgery or prolonged periods of immobilization, for example, hospitalization or even long plane rides. Warfarin is indicated for prevention of any of these events, whereas unfractionated heparins, LMWHs, direct thrombin inhibitors, and factor Xa inhibitors are used for both prevention and treatment. Patients at risk for clots are given medications for DVT prophylaxis while in the hospital and after major surgery. All of the drugs in this class can be used for prophylaxis or treatment of a DVT or PE except betrixaban, which is only approved for prophylaxis, at the time of this publication. LMWHs, especially enoxaparin, are also routinely used as anticoagulant bridge therapy in situations in which a patient must stop warfarin for surgery or other invasive medical procedures. Enoxaparin acts as a bridge to provide anticoagulation while the patient must be without warfarin therapy. Bleeding is the main complication of anticoagulation therapy, and the risk increases with increasing dosages. Such bleeding may be localized or systemic. One particularly notable adverse effect of heparin is heparin-induced thrombocytopenia (HIT), which is also called heparin-associated thrombocytopenia. All of the novel oral anticoagulants, rivaroxaban, apixaban, edoxaban, and dabigatran have black box warnings related to premature discontinuation which can lead to increased clots. Warfarin has a black box warning regarding bleeding risk, although all anticoagulants share the risk of bleeding. Enoxaparin and the oral factor Xa inhibitors have a black box warning regarding potential spinal hematomas if the patient has an epidural catheter. Although the toxic effects of heparin, LMWH, and warfarin are hemorrhagic in nature, the management is different for each drug. Symptoms that may be attributed to toxicity or an overdose of anticoagulants are hematuria, melena (blood in the stool), petechiae, ecchymoses, and gum or mucous membrane bleeding. In the event of heparin or warfarin toxicity, the drug is to be stopped immediately. Stopping heparin alone may be enough to reverse the toxic effects because of the drug’s short half-life (1 to 2 hours). In severe cases, intravenous (IV) injection of protamine sulfate is indicated. In warfarin toxicity or overdose, the first step is to discontinue the warfarin. Because warfarin inactivates the vitamin K–dependent clotting factors and because these clotting factors are synthesized in the liver, it may take 36 to 42 hours before the liver can resynthesize enough clotting factors to reverse the warfarin effects. Giving vitamin K1 (phytonadione) can hasten the return to normal coagulation. Idarucizumab (Praxbind) is a specific dabigatran antidote which was recently approved. Idarucizumab reverses the anticoagulant effects of dabigatran for emergency surgery or in life-threatening or uncontrolled bleeding. Antidotes for the oral Xa inhibitors are in the phase III trials at the time of this writing. Copyright © 2020 Elsevier Inc. All Rights Reserved. 116 Drug interactions involving the oral anticoagulants are profound and complicated. The main interaction mechanisms responsible for increasing anticoagulant activity include enzyme inhibition of metabolism, displacement of the drug from inactive protein-binding sites, decrease in vitamin K absorption or synthesis by the bacterial flora of the large intestines, and alteration in the platelet count or activity. Antiplatelet Drugs Antiplatelet drugs work to prevent platelet adhesion at the site of blood vessel injury, which actually occurs before the clotting cascade. A platelet plug that has formed at a site of vessel injury is not stable and can be dislodged. The clotting cascade is then stimulated to form a more permanent fibrin plug (blood clot). Aspirin is widely used for its analgesic, antiinflammatory, and antipyretic (antifever) properties, but it also has antiplatelet effects. Dipyridamole, another antiplatelet drug, also works to inhibit platelet aggregation by preventing the release of adenosine diphosphate (ADP), platelet factor IV, and thromboxane A2 (TXA2), all substances that stimulate platelets to aggregate or form a clot. Clopidogrel is a drug that belongs to the class of antiplatelet drugs called ADP inhibitors. It inhibits platelet aggregation by altering the platelet membrane so that it can no longer receive the signal to aggregate and form a clot. Prasugrel (Effient) is an antiplatelet drug, similar to clopidogrel, that is used primarily after interventional cardiac procedures and for patients who do not respond to clopidogrel. Vorapaxar (Zontivity), a novel antiplatelet drug and the first in its class. Vorapaxar is an antagonist of protease-activated receptor-1 (PAR-1), which inhibits the action of thrombin on the platelet. It is contraindicated in those with a history of stroke, transient ischemic attacks (TIAs), intracranial hemorrhage, and active bleeding. Glycoprotein (GP) IIb/IIIa inhibitors work by blocking the receptor protein by the same name that occurs in the platelet wall membranes. Aspirin has many therapeutic effects, but many of them vary depending on the dosage. Aspirin is officially recommended for stroke prevention by the American Stroke Society. Clopidogrel is given to reduce the risk for thrombotic stroke and is used for prophylaxis against transient ischemic attacks as well as for post-MI prevention of thrombosis. Dipyridamole is used as an adjunct to warfarin in the prevention of postoperative thromboembolic complications and to decrease platelet aggregation in various other thromboembolic disorders. The GP IIb/IIIa inhibitors are used to treat acute unstable angina and MI and are given during percutaneous coronary intervention procedures, such as angioplasty. Pentoxifylline is indicated for peripheral vascular disease, whereas cilostazol is indicated specifically for intermittent claudication. Cilostazol has been shown to be superior to pentoxifylline in improving exercise tolerance in elderly patients. The potential adverse effects of the various antiplatelet drugs can be serious, and they all pose a risk for inducing a serious bleeding episode. Copyright © 2020 Elsevier Inc. All Rights Reserved. 117 The use of dipyridamole with clopidogrel, aspirin, and other nonsteroidal antiinflammatory drugs (NSAIDs) produces additive antiplatelet activity and increased bleeding potential. The combined use of steroids or nonaspirin NSAIDs with aspirin can increase the ulcerogenic effects of aspirin. Thrombolytic Drugs Thrombolytics are able to break down or lyse preformed clots in blood vessels such as those that supply the heart with blood. Therapeutic effects for which to monitor include improved tissue perfusion, decreased chest pain, and prevention of further myocardial damage. The therapeutic effects of most coagulation modifier drugs include improved circulation, improved tissue perfusion, decreased pain, and prevention of further tissue damage. Before giving these drugs, a thorough physical assessment should be performed as well as checking of pertinent laboratory values (e.g., INR, aPTT, PT). Thrombolytics are coagulation modifiers that lyse thrombi in the coronary arteries. If the blood flow is reestablished early, the heart muscle and left ventricular function can be saved. Tissue plasminogen activator (t-PA) and anisoylated plasminogen streptokinase activator complex (APSAC) are two of these drugs. The use of thrombolytics has largely been replaced by interventional cardiologic procedures, such as percutaneous coronary intervention, but is still a viable option in hospitals that do not offer percutaneous coronary intervention. The newer thrombolytics have chemical specificity for fibrin threads and work primarily at the site of a clot. They still carry some bleeding risk. The indications for thrombolytic therapy include acute MI, arterial thrombosis, DVT, occlusion of shunts or catheters, pulmonary embolism, and acute ischemic stroke. The most common undesirable effect of thrombolytic therapy is internal, intracranial, and superficial bleeding. Other problems include hypersensitivity, anaphylactoid reactions, nausea, vomiting, and hypotension. These drugs can also induce cardiac dysrhythmias. Treatment for toxicity is symptomatic and supportive because thrombolytic drugs have a relatively short half-life and no specific antidotes. Antifibrinolytic Drugs These drugs prevent the lysis of fibrin; in doing so, they actually promote clot formation. For this reason, they are also called hemostatic drugs. Three synthetic antifibrinolytics are available—aminocaproic acid, tranexamic acid, and desmopressin. There are three drugs used for the treatment of hemophilia produced by recombinant DNA technology, which eliminates the risk associated with obtaining them from human blood. Products currently available include rVII, rVIII, and rIX. Antifibrinolytics are useful in both the prevention and treatment of excessive bleeding resulting from systemic hyperfibrinolysis or surgical complications. They have also proved successful in arresting excessive oozing from surgical sites such as chest tubes as well as in reducing the total blood loss and the duration of bleeding in the postoperative period. Desmopressin may also be used in patients who have hemophilia A or type I von Willebrand disease. Copyright © 2020 Elsevier Inc. All Rights Reserved. 118 Recombinant factors VII, VIII, and IX are used to treat hemophilia or to stop the bleeding from excessive warfarin therapy. When drugs such as estrogens or oral contraceptives are used concurrently with aminocaproic acid or tranexamic acid, increased coagulation may occur. Nursing Process Coagulation modifiers have a variety of uses, including the following: (1) prevention or elimination of clotting in a peripherally inserted catheter, (2) maintenance of patency (without clotting) of central venous catheters, (3) clot prevention in coronary artery bypass grafting, (4) prevention of clotting after major vessel injury, (5) treatment of thrombophlebitis to prevent venous and/or arterial thromboembolism, and (6) prevention of clotting with use of prosthetics (e.g., heart valve replacements) and in atrial fibrillation. Perform a thorough patient assessment to identify the presence of risk factors. The use of Homan's sign is not recommended for assessment/evaluation of DVT of the leg due to its lack of reliability. It is also important to assess the skin, oral mucous membranes, gums, urine, and stool for any evidence of bleeding. Assess patients for any blood in the urine or stool, easy bruising, excessive bleeding from toothbrushing or shaving, or unexplained nosebleeds while receiving these medications, and report any such findings. It is crucial to patient safety to remember that heparin is not interchangeable unit for unit with drugs in another class of anticoagulants, the LMWHs. Heparin sodium contains benzyl alcohol; therefore, assess for allergy to this additional component. Heparin, given IV or subcutaneously, prevents clot formation by binding to antithrombin III, which turns off certain activating factors. The overall effect is to inactivate the coagulation pathway and prevent clots from forming. Heparin does not lyse (break down) a clot. Antiplatelet drugs prevent clot formation by preventing platelet involvement in clot formation. With antiplatelet drugs, obtain a thorough nursing history and medication history, and perform a physical assessment before beginning drug therapy. Aspirin is not to be used in children and teenagers, in patients with any bleeding disorder, in pregnant or lactating women, or in patients with vitamin K deficiency or peptic ulcer disease. Before use of thrombolytics, assess for a history of hypotension and cardiac dysrhythmias. Thrombolytics are able to break down or lyse preformed clots in blood vessels such as those that supply the heart with blood. Therapeutic effects for which to monitor include improved tissue perfusion, decreased chest pain, and prevention of further myocardial damage. The therapeutic effects of most coagulation modifier drugs include improved circulation, improved tissue perfusion, decreased pain, and prevention of further tissue damage. Before giving these drugs, a thorough physical assessment must be performed as well as checking of pertinent laboratory values (e.g., INR, aPTT, PT). Antifibrinolytics prevent the lysis of fibrin, thus promoting clot formation, and have an effect opposite to that of the anticoagulants. Nursing care is very individualized and is Copyright © 2020 Elsevier Inc. All Rights Reserved. 119 based on the characteristics of the patient, thorough assessment data, existing medical conditions, and the specific drug. There are additional concerns for patients with dysrhythmias, hypotension, bradycardia, convulsive disorders, nausea, vomiting, and abdominal pain or diarrhea. Tranexamic acid, saved for use intravenously prior to surgery, is not to be given in patients with a history of active thromboembolic disease or with hormonal contraceptives. Baseline vital signs are important to assess and document. Routinely monitor vital signs, heart sounds, peripheral pulses, and neurologic status in all patients during and immediately after anticoagulant therapy. The degree of anticoagulation (for any of these medications) is monitored by the PT. The antidote to hemorrhage or uncontrolled bleeding resulting from heparin or LMWH therapy is protamine sulfate. Therapeutic levels of anticoagulants and other clotting-altering drugs or coagulation modifier drugs are also monitored by laboratory studies such as activated partial thromboplastin time (aPTT), prothrombin time (PT), and international normalized ratio (INR.) Some of the therapeutic effects include decreased chest pain and a decrease in dizziness as well as in other neurologic symptoms. Adverse effects of anticoagulants include bleeding and hematoma formation (heparin); thrombocytopenia (heparin and LWMHs); bleeding, dizziness, shortness of breath, and fever (direct thrombin inhibitors); bleeding, hematoma, dizziness, and gastrointestinal distress (selective factor Xa inhibitors); and bleeding, lethargy, and muscle pain (warfarin). Early signs of drug overdose for any of the clotting-altering drugs (i.e., anticoagulants) include bleeding of the gums during toothbrushing, unexplained nosebleeds or bruising, and heavier-than-usual menstrual bleeding. With the oral anticoagulants, rivaroxaban, apixaban, edoxaban, betrixaban, and dabigatran, it is important—to patient safety—to be aware of their black box warnings related to the concern for increased clotting with premature discontinuation. REVIEW QUESTIONS1. The nurse is monitoring a patient who is receiving antithrombolytic therapy in the emergency department because of a possible MI. Which adverse effect would be of the greatest concern at this time? a. Dizziness b. Blood pressure of 130/98 mm Hg c. Slight bloody oozing from the IV insertion site d. Irregular heart rhythm2. A patient is receiving instructions regarding warfarin therapy and asks the nurse about what medications she can take for headaches. The nurse will tell her to avoid which type of medication? Select all that apply. a. aspirin b. acetaminophen c. NSAIDs d. The herbal product gingko e. Caffeine3. The nurse is teaching a patient about the self-administration of enoxaparin (Lovenox). Which statement will be included in this teaching session? a. “We will need to teach a family member how to give this drug in your arm.”b. “This drug is given in the folds of your abdomen, but at least 2 inches away from your navel.”c. “This drug Copyright © 2020 Elsevier Inc. All Rights Reserved. 120 needs to be taken at the same time every day with a full glass of water.”d. “Be sure to massage the injection site thoroughly after administering the drug.”4. A patient is receiving dabigatran (Pradaxa) 150 mg twice daily as part of treatment for atrial fibrillation. Which condition, if present, would be a concern if the patient were to receive this dose? a. Asthma b. Elevated liver enzymes c. Renal impairment d. History of myocardial infarction5. A patient received a double dose of heparin during surgery and is bleeding through the incision site. While the surgeons are working to stop the bleeding at the incision site, the nurse will prepare to take what action? a. Give IV vitamin K as an antidote. b. Give IV protamine sulfate as an antidote. c. Call the blood bank for an immediate platelet transfusion. d. Obtain an order for packed red blood cells.6. A patient is starting warfarin (Coumadin) therapy as part of treatment for atrial fibrillation. The nurse will follow whichprinciples of warfarin therapy? (Select all that apply.) a. Teach proper subcutaneous administration. b. Administer the oral dose at the same time every day. c. Assess carefully for excessive bruising or unusual bleeding. d. Monitor laboratory results for a target INR of 2 to 3. e. Monitor laboratory results for a therapeutic aPTT value of 1.5 to 2.5 times the control value.7. The order for enoxaparin (Lovenox) reads as follows: Give 1 mg/kg subQ every 12 hours. The patient weighs 242 lb, and the medication is available in an injection form of 120 mg/0.8 mL. How many milligrams will this patient receive? How many milliliters will the nurse draw up for the injection? (Round to hundredths.) 8. The nurse is assessing a patient who has a new prescription for vorapaxar (Zontivity). Which of these conditions are considered contraindications to the use of vorapaxar? (Select all that apply.) a. Impaired renal function b. Impaired liver function c. History of myocardial infarction d. Peripheral artery disease e. History of intracranial hemorrhage Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 27: Antilipemic Drugs Chapter 27 1. b; 2. a, c, f; 3. c; 4. c; 5. b; 6. b, d, e, f; 7. 2 tablets; 8. b, c, d, f. Key Points Anatomy, Physiology, and Pathophysiology Overview Copyright © 2020 Elsevier Inc. All Rights Reserved. 121 Lipids and Lipid Abnormalities Triglycerides and cholesterol are the two primary forms of lipids in the blood. Fats are taken into the body in food and are broken down in the small intestine to form triglycerides. Triglycerides function as an energy source and are stored in adipose tissue. Cholesterol is primarily used to make steroid hormones, cell membranes, and bile acids. Triglycerides and cholesterol are both water-insoluble fats that must be bound to specialized lipid-carrying proteins called apolipoproteins. The combination of triglycerides and cholesterol with an apolipoprotein is referred to as a lipoprotein. Lipoproteins transport lipids via the blood. The liver is the major organ where lipid metabolism occurs. The liver produces very-lowdensity lipoprotein from both endogenous and exogenous sources. High-density lipoprotein (HDL) is produced in the liver and intestines and is also formed when chylomicrons are broken down. If the liver has an excess amount of cholesterol, the number of low-density lipoprotein (LDL) receptors on the liver decreases, which results in an accumulation of LDL in the blood. A major function of the liver is to manufacture cholesterol, a process that requires acetyl coenzyme A (CoA) reductase. It is important to understand the pathology of this disease process so that appropriate patient education may be delivered. Antilipemic drugs are used to lower the high levels of lipids in the blood (triglycerides and cholesterol). Atherosclerotic Plaque Formation Lipids and lipoproteins participate in the formation of atherosclerotic plaque, which subsequently leads to the development of coronary heart disease (CHD). When serum cholesterol levels are elevated, circulating monocytes burrow into the next layer of the blood vessel and change into macrophage cells and take up cholesterol from circulating lipoproteins until filled with fat. They become foam cells, the characteristic precursor lesion of atherosclerosis, also known as a fatty streak. Once established, it is present throughout the coronary and systemic circulation. When plaque forms in the blood vessels that supply the heart with needed oxygen and nutrients, the lumens of these blood vessels eventually decrease in size and the amount of oxygen and nutrients that can reach the heart is reduced. Cholesterol and Coronary Heart Disease As blood cholesterol increases, the incidence of death and disability from CHD increases. Statistics show that half of all Americans, both male and female, will die of a heart attack. The goals of treatment are two-pronged: primary prevention of cardiac events in patients with risk factors and secondary prevention of subsequent cardiac events in individuals who have previously experienced a cardiac event (e.g., myocardial infarction). Copyright © 2020 Elsevier Inc. All Rights Reserved. 122 Measures taken early in life to reduce and maintain cholesterol levels in a desirable range can have a dramatic effect in terms of preventing CHD. These include lifestyle modifications related to diet, weight, and activity level. Results of some of the larger investigations support the view that, in patients with known risk factors for CHD, therapy with an antilipemic drug can reduce the occurrence of CHD. Drug therapy can also reduce first-time heart attack and death caused by heart disease. The consumption of fatty fish or dietary supplements containing omega-3 fatty acids appears to have beneficial effects on triglyceride and HDL levels. Hyperlipidemias and Treatment Guidelines The decision to prescribe antilipemic drugs as an adjunct to dietary therapy in patients with elevated cholesterol levels is based on the patient’s clinical profile. This includes the patient’s age, sex, menopausal status for women, family history, and response to dietary treatment, as well as the presence of risk factors for premature CHD and the cause, duration, and phenotypic pattern of the patient’s hyperlipidemia. The selection of dietary and drug therapy options is determined by the presence of certain risk factors. The major source of guidance for antilipemic treatment in the United States is the ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. These guidelines are updated in 2013. When the decision to institute drug therapy has been made, the choice of drug is determined by the specific lipid profile of the patient. Five patterns or phenotypes of hyperlipidemia have been identified, and these are defined by the plasma (serum) concentrations of total cholesterol, triglycerides, and lipoprotein fractions. One of the basic tenets of the National Cholesterol Education Panel (NCEP) guidelines is that all reasonable nonpharmaceutical means of controlling the blood cholesterol level (e.g., diet, exercise) are to be tried for at least 6 months and found to fail before drug therapy is considered. Factors to be considered before the initiation of therapy are the type and magnitude of dyslipidemia, the age and lifestyle of the patient, and relative indications and contraindications of different drugs, potential drug interactions, adverse effects, and the overall cost of therapy. Antilipemic drugs are used to lower the high levels of lipids in the blood (triglycerides and cholesterol). There are currently four established classes of drugs used to treat dyslipidemia: (1) hydroxymethylglutaryl–coenzyme A (HMG–CoA) reductase inhibitors (statins), (2) bile acid sequestrants, (3) the B vitamin niacin (vitamin B3, nicotinic acid), and (4) the fibric acid derivatives (fibrates). A cholesterol absorption inhibitor, ezetimibe (Zetia), is also available. Vytorin is an example of a combination tablet that contains both the statin drug simvastatin and ezetimibe. Mipomersen is a once-weekly subcutaneous injection, as an adjunct to maximally tolerated lipid-lowering medications and diet for the treatment of patients with homozygous familial hypercholesterolemia. Copyright © 2020 Elsevier Inc. All Rights Reserved. 123 Lomitapide (Juxtapid) is a microsomal triglyceride transfer protein inhibitor. Alirocumab (Praluent) and evolocumab (Repatha) belong to a new class of lipid-lowering drugs called proprotein convertase subtilisn kexin 9 (PCSK9) inhibitors. Pharmacology Overview Hydroxymethylglutaryl–Coenzyme A Reductase Inhibitors The rate-limiting enzyme in cholesterol synthesis is known as HMG–CoA reductase. The class of medications that competitively inhibit this enzyme, called the hydroxymethylglutaryl–coenzyme A (HMG–CoA) reductase inhibitors, are potent drugs for reducing plasma concentrations of LDL cholesterol. Lovastatin was the first drug in this class to be approved for use, which occurred in 1987. Since that time, six other HMG–CoA reductase inhibitors have become available on the U.S. market: (1) pravastatin, (2) simvastatin, (3) atorvastatin, (4) fluvastatin, (5) rosuvastatin, and (6) pitavastatin. The liver requires HMG–CoA reductase to produce cholesterol. The statins inhibit this enzyme, thereby decreasing cholesterol production. The statins are recommended as first-line drug therapy for hypercholesterolemia (especially elevated levels of LDL cholesterol), the most common and dangerous form of dyslipidemia. The HMG–CoA reductase inhibitors are generally well tolerated, and significant adverse effects are fairly uncommon. Mild, transient gastrointestinal disturbances, rash, and headache are the most common problems and tend to be underreported in clinical trials. A clinically important adverse effect is myopathy (muscle pain), which may progress to a serious condition known as rhabdomyolysis. Some patients experience irreversible renal damage and severe pain and may have to alter dosages or change drugs as ordered by the prescriber. Bile Acid Sequestrants Bile acid sequestrants bind bile and prevent the resorption of the bile acids from the small intestine. An insoluble bile acid and resin (drug) complex is formed and then excreted in the bowel movement. Bile acids are necessary for the absorption of cholesterol from the small intestine and are also synthesized from cholesterol by the liver. The more that bile acids are excreted in the feces, the more the liver converts cholesterol to bile acids. This reduces the level of cholesterol in the liver and thus in the circulation as well. Bile acid sequestrants may be used as primary or adjunct drug therapy in the management of type II hyperlipoproteinemia. A common strategy is to use them along with statins for an additive drug effect in reducing LDL cholesterol levels. The adverse effects of colestipol, cholestyramine, and colesevelam are similar; however, colesevelam is reported to have fewer gastrointestinal adverse effects and drug interactions. Constipation is a common problem and may be accompanied by heartburn, nausea, belching, and bloating. These adverse effects tend to disappear over time. Niacin Copyright © 2020 Elsevier Inc. All Rights Reserved. 124 Niacin, or nicotinic acid, is not only a very unique lipid-lowering drug, it is also a vitamin. The beneficial effects are believed to be related to its ability to inhibit lipolysis in adipose tissue, decrease esterification of triglycerides in the liver, and increase the activity of lipoprotein lipase. Niacin has been shown to be effective in lowering lipid levels, including triglyceride, total serum cholesterol, and LDL cholesterol levels. It also increases HDL cholesterol levels. Niacin can cause flushing, pruritus, and gastrointestinal distress. Small doses of aspirin or nonsteroidal antiinflammatory drugs (NSAIDs) may be taken 30 minutes before the niacin dose to minimize the cutaneous flushing. Fibric Acid Derivatives Current fibric acid derivatives include gemfibrozil and fenofibrate. These drugs primarily affect the triglyceride levels but may also lower the total cholesterol and LDL cholesterol levels and raise the HDL cholesterol level. They are often collectively referred to as fibrates. Fibric acid drugs are believed to work by activating lipoprotein lipase, an enzyme responsible for the breakdown of cholesterol. They are indicated for the treatment of type III, IV, and V hyperlipidemia, and in some cases the type IIb form, although other classes of antilipemics are usually tried first. The most common adverse effects of the fibric acid derivatives are abdominal discomfort, diarrhea, nausea, headache, blurred vision, increased risk for gallstones, and prolonged prothrombin time. Liver function tests may also show increased enzyme levels. Gemfibrozil can enhance the action of oral anticoagulants; thus careful adjustment of the dosage of warfarin is required. The risk for myositis, myalgias, and rhabdomyolysis is increased when either gemfibrozil or fenofibrate is given with a statin. Cholesterol Absorption Inhibitor Ezetimibe (Zetia) is currently the only cholesterol absorption inhibitor available. Ezetimibe has a novel mechanism of action in that it selectively inhibits absorption of cholesterol and related sterols in the small intestine. The result is a reduction in several blood lipid parameters: total cholesterol level, LDL cholesterol level, apolipoprotein B level, and triglyceride level. Serum levels of HDL cholesterol, the so-called good cholesterol, have been shown to increase with the use of ezetimibe. PSCK-9 Inhibitors PCSK9 inhibitors have been shown to significantly lower LDL-C levels. Alirocumab (Praluent) was the first PCSK9 inhibitor approved by the FDA in 2015 and evolocumab (Repatha) was approved soon after. Both drugs are approved for hyperlipidemia and are given subcutaneously, every 2 to 4 weeks. Nursing Process Copyright © 2020 Elsevier Inc. All Rights Reserved. 125 Obtain a thorough health and medication history with a listing of allergies and any prescription drugs, over-the-counter drugs, herbals, or supplements the patient is taking. Assess the patient’s dietary patterns, exercise program and frequency, weight, height, and vital signs, and document these parameters—especially food intake—over time, such as for several weeks. Also, document the patient’s use of tobacco, alcohol, and/or social drugs, along with information about frequency, amount, and duration of use. Some lipid disorders are hereditary; therefore, perform a thorough assessment of family history, including positive risk factors for CHD. Perform an assessment to identify any cautions, contraindications, and potential drug interactions before initiating use of any of the antilipemics. Assess serum lipid values and lipoprotein levels. HMG–CoA reductase inhibitors (the statins) are not to be used in patients with liver disease or those who have increased liver enzyme levels. Use of bile acid sequestrants requires careful assessment of possible contraindications such as a patient history of biliary or bowel obstructions and phenylketonuria (PKU). Cholestyramine contains aspartame and would be contraindicated with a history of phenylketonuria (PKU). Patients who are taking antilipemics for a long period may have altered levels of the fatsoluble vitamins and may then require supplementation of vitamins A, D, and K. Appropriate actions need to be taken to avoid or minimize constipation, such as increasing intake of fiber and fluids. Because severe cardiovascular diseases and cerebral vascular accidents are associated with very high cholesterol levels, it is critical that the patient continue with any prescribed nonpharmacologic and/or pharmacologic therapies, regardless of the antilipemic used. Bile acid sequestrants often come in powder form and must be mixed thoroughly with food or fluids (at least 4 to 6 oz of fluid). Powder and/or granule dosage forms are never to be taken in dry form. It is important that any of these drugs be taken 1 hour before or 4 to 6 hours after any other oral medication or meals because of the high risk for drug-drug and drug-food interactions. With niacin, flushing of the face may occur; educate the patient on this adverse effect. To minimize gastrointestinal upset, advise the patient to take this medication with meals. Cholesterol and triglyceride levels are used to monitor the patient’s response to the medication regimen. The therapeutic effects of both nonpharmacologic and pharmacologic measures are evidenced by a decrease in cholesterol and triglyceride levels to within normal ranges. Nonpharmacologic measures include a low-fat, low-cholesterol diet; supervised, moderate exercise; weight loss; cessation of smoking and drinking; and relaxation therapy. Adverse effects for which to monitor include gastrointestinal upset, increased liver enzyme levels, hepatomegaly, myalgias, and other effects mentioned in the textbook chapter. Copyright © 2020 Elsevier Inc. All Rights Reserved. 126 Fat-soluble vitamins may need to be prescribed for patients taking these medications for long periods because the antilipemics have long-term effects on the liver’s production of these vitamins. Monitoring for adverse effects of the antilipemics includes periodic liver and renal function studies. The statins have gained much attention for their adverse effects of muscle aches and pain due to the breakdown of muscle tissue. Some patients experience irreversible renal damage and severe pain and may have to alter dosages or change drugs as ordered by the prescriber. Notify the prescriber if there are any new or troublesome symptoms or if there is persistent gastrointestinal upset, constipation, gas, bloating, heartburn, nausea, vomiting, abnormal or unusual bleeding, or yellow discoloration of the skin. Another symptom to report is muscle aches and pain. Educate patients about desired laboratory levels. REVIEW QUESTIONS1. A nurse administering niacin would implement which action to help to reduce adverse effects? a. Give the medication with grapefruit juice. b. Administer a small dose of aspirin or an NSAID 30 minutes before the niacin dose.c. Administer the medication on an empty stomach. d. Have the patient increase dietary fiber intake.2. In administering niacin, the nurse must monitor for which adverse effects? (Select all that apply.) a. Flushing of the skin b. Muscle pain c. Pruritus d. Headache e. Constipation f. GI upset3. Which point will the nurse emphasize to a patient who is taking an antilipemic medication in the statin class? a. The drug must be taken on an empty stomach before meals.b. A low-fat diet is not necessary while taking these medications.c. It is important to report muscle pain immediately. d. Improved cholesterol levels will be evident within 2 weeks.4. A patient is being assessed before a newly ordered antilipemic medication is started. Which condition would be a potential contraindication? a. Diabetes insipidus b. Pulmonary fibrosis c. Liver cirrhosis d. Myocardial infarction5. A patient is currently taking a statin. The nurse considers that the patient may have a higher risk for developing rhab-domyolysis when also taking which product? a. NSAIDs b. A fibric acid derivative c. Orange juice d. Fat-soluble vitamins6. The nurse is administering cholestyramine (Questran), a bile acid sequestrant. Which nursing intervention(s) is(are) appropriate? (Select all that apply.) a. Administering the drug on an empty stomach b. Administering the drug with meals c. Instructing the patient to follow a low-fiber diet while taking this drugd. Instructing the patient to take a fiber supplement while taking this druge. Increasing fluid intake f. Not administering this drug at the same time as other drugs7. The medication order reads, “niacin, 500 mg PO, every evening.” The medication is available in 250-mg tablets. How many tablets will the patient receive per dose?8. A patient has been taking simvastatin (Zocor) for 6 months. Copyright © 2020 Elsevier Inc. All Rights Reserved. 127 Today he received a call that he needs to come to the office for a “laboratory check.” The nurse expects which laboratory studies to be ordered at this time? (Select all that apply.) a. PT/INR b. Total cholesterol c. Triglycerides d. Liver function studies e. Complete blood count f. HDL and LDL levels_________________________________________________________________________ ___________ Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 28: Diuretic Drugs Chapter 28 1. b, e, f; 2. a; 3. c; 4. b; 5. d; 6. a, c, f; 7. 37.5 g, 187.5 mL; 8. b. Key Points Anatomy, Physiology, and Pathophysiology Overview Diuretics are drugs that accelerate the rate of urine formation via a variety of mechanisms, resulting in the removal of sodium and water from the body. The five main types of diuretics are carbonic anhydrase inhibitors, loop diuretics, osmotic diuretics, potassium-sparing diuretics, and thiazide and thiazide-like diuretics. The loop, potassium-sparing, and thiazide diuretics are the most commonly used. Remember that the loop diuretics are more potent than the thiazides, combination diuretics, and potassium-sparing diuretics. Copyright © 2020 Elsevier Inc. All Rights Reserved. 128 The Seventh Joint National Committee on the Detection, Evaluation, and Treatment of Hypertension reaffirmed the role of diuretics, especially the thiazides, as first-line drugs in the treatment of hypertension. All diuretics work primarily in the kidney. The kidney filters out toxic waste products from the blood while simultaneously conserving essential substances. This delicate balance between elimination of toxins and retention of essential chemicals is maintained by the nephron. The nephron is the main structural unit of the kidney, and each kidney contains approximately 1 million nephrons. The initial filtering of the blood takes place in the glomerulus, a cluster of capillaries surrounded by the glomerular capsule. The rate at which this filtering occurs is referred to as the glomerular filtration rate and it is used as a gauge of how well the kidneys are functioning as filters. It is important to have a thorough knowledge of renal anatomy and physiology and how it relates to the action of the various diuretics; for example, if a loop diuretic is given, its site of action is the loop of Henle and it causes the excretion of sodium, potassium, and chloride into the urine. Pharmacology Overview The various diuretics are classified according to their sites of action within the nephron, their chemical structure, and their diuretic potency. The most potent diuretics are the loop diuretics, followed by mannitol, metolazone (a thiazide-like diuretic), the thiazides, and the potassium-sparing diuretics. The potency of these diuretics is a function of where they work in the nephron to inhibit sodium and water resorption. The more sodium and water they inhibit from resorption, the greater the amount of diuresis and therefore the greater the potency. Carbonic Anhydrase Inhibitors Carbonic anhydrase inhibitors (CAIs) are chemical derivatives of sulfonamide antibiotics. They inhibit the activity of the enzyme carbonic anhydrase, which is found in the kidneys, eyes, and other parts of the body. The carbonic anhydrase system in the kidney is located just distal to the glomerulus in the proximal tubules, where roughly two thirds of all sodium and water is resorbed into the blood. For sodium and water to be resorbed back into the blood, hydrogen must be exchanged for it. The CAIs reduce the formation of hydrogen (H+) and bicarbonate (HCO3–) ions from carbon dioxide and water through the noncompetitive, reversible inhibition of carbonic anhydrase activity, resulting in a reduction in the availability of the ions, mainly hydrogen. An undesirable effect of CAIs is elevation of the blood glucose level and glycosuria in diabetic patients. This may be due in part to CAI-enhanced potassium loss through the urine. Therapeutic use of CAIs is in treatment of glaucoma, edema, and high-altitude sickness. Copyright © 2020 Elsevier Inc. All Rights Reserved. 129 Undesirable effects are metabolic abnormalities such as acidosis and hypokalemia, as well as drowsiness, anorexia, paresthesias, hematuria, urticaria, photosensitivity, and melena. Because CAIs can cause hypokalemia, an increase in digoxin toxicity may occur when they are combined with digoxin. Use with corticosteroids may also cause hypokalemia. Loop Diuretics Loop diuretics (bumetanide, ethacrynic acid, furosemide, and torsemide) are very potent diuretics. Loop diuretics have renal, cardiovascular, and metabolic effects. These drugs act primarily along the thick ascending limb of the loop of Henle, blocking chloride and, secondarily, sodium resorption. They are also thought to activate renal prostaglandins, which results in dilatation of the blood vessels of the kidneys, the lungs, and the rest of the body. Loop diuretics are used for edema associated with heart failure and hepatic or renal disease, hypertension, and to increase the renal excretion of calcium in patients with hypercalcemia. They may also be indicated for heart failure resulting from diastolic dysfunction. Loop diuretics produce a potent diuresis and subsequent loss of fluid. The resulting decreased fluid volume leads to a decreased return of blood to the heart, or decreased filling pressures resulting in reduced blood pressure, pulmonary vascular resistance, systemic vascular resistance, central venous pressure, and left ventricular end-diastolic pressure. Loop diuretics are particularly useful when rapid diuresis is needed because of their rapid onset of action. The diuretic effect lasts at least 2 hours. Loop diuretics have a distinct advantage over thiazide diuretics in that their diuretic action continues even when creatinine clearance decreases below 25 mL/min. The major adverse effect of loop diuretics is electrolyte disturbances. Prolonged administration of high dosages can also result in hearing loss stemming from ototoxicity. Hypokalemia is of serious clinical importance. To prevent hypokalemia, patients often receive potassium supplements along with furosemide. Electrolyte loss and dehydration, which can result in circulatory failure, are the main toxic effects of loop diuretics that require attention. Treatment involves electrolyte and fluid replacement. Furosemide can produce erythema multiforme, exfoliative dermatitis, photosensitivity, and in rare cases, aplastic anemia. Furosemide has a black box warning regarding fluid and electrolyte loss. Torsemide may rarely cause blood disorders, including thrombocytopenia, agranulocytosis, leukopenia, neutropenia, and Stevens-Johnson syndrome. Loop diuretics exhibit both neurotoxic and nephrotoxic properties, and they produce additive effects when given in combination with drugs that have similar toxicities. Loop diuretics also affect certain laboratory results, increasing serum levels of uric acid, glucose, alanine aminotransferase, and aspartate aminotransferase. Osmotic Diuretics Copyright © 2020 Elsevier Inc. All Rights Reserved. 130 The osmotic diuretics include mannitol, urea, organic acids, and glucose. Mannitol is the most commonly used of these drugs. Mannitol works along the entire nephron, but primarily in the proximal tubule and descending limb of the loop of Henle. Because it is not absorbed, it increases osmotic pressure in the glomerular filtrate, which in turn pulls fluid into the renal tubules from the surrounding tissues. This process also inhibits the tubular resorption of water and solutes, which produces a rapid diuresis. Mannitol may induce vasodilation and in doing so increases both glomerular filtration and renal plasma flow, making it an excellent drug for preventing kidney damage during acute renal failure. It is commonly used in the treatment of patients in the early, oliguric phase of acute renal failure. Mannitol is also often used to reduce intracranial pressure and cerebral edema resulting from head trauma. In addition, mannitol treatment may be tried when elevated intraocular pressure is unresponsive to other drug therapies. Significant undesirable effects of mannitol include convulsions, thrombophlebitis, and pulmonary congestion. Other less significant effects are headaches, chest pains, tachycardia, blurred vision, chills, and fever. Potassium-Sparing Diuretics The currently available potassium-sparing diuretics are amiloride, spironolactone, and triamterene. These diuretics are also referred to as aldosterone-inhibiting diuretics because they block the aldosterone receptors. Spironolactone is a competitive antagonist of aldosterone, and for this reason it causes sodium and water to be excreted while potassium is retained. It is the most commonly used of the three drugs. Potassium-sparing diuretics work in the collecting ducts and distal convoluted tubules, where they interfere with sodium-potassium exchange. Spironolactone competitively binds to aldosterone receptors and therefore blocks the resorption of sodium and water that is induced by aldosterone secretion. The potassium-sparing diuretics are relatively weak compared with the thiazide and loop diuretics. When diuresis is needed, they are generally used as adjuncts to thiazide treatment. This combination is beneficial in two respects. First, the drugs have synergistic diuretic effects; second, the two drugs counteract the adverse metabolic effects of one another. The thiazide diuretics cause potassium, magnesium, and chloride to be lost in the urine, and the potassium-sparing diuretics counteract this by elevating the potassium and chloride levels. Spironolactone and triamterene are used to treat hyperaldosteronism and hypertension and to reverse the potassium loss caused by the potassium-wasting (e.g., loop, thiazide) diuretics. Permanent ventricular myocardial wall damage, known as remodeling, may follow myocardial infarction. Various clinical trials have demonstrated a cardioprotective benefit of spironolactone in preventing this remodeling process due to aldosterone-inhibiting activity. Spironolactone can cause gynecomastia, amenorrhea, irregular menses, and postmenopausal bleeding. Copyright © 2020 Elsevier Inc. All Rights Reserved. 131 Triamterene may reduce folic acid levels and cause the formation of kidney stones and urinary casts. It may also precipitate megaloblastic anemia. Hyperkalemia may occur when potassium-sparing diuretics are used in combination with each other and/or with other potassium-sparing drugs such as angiotensin-converting enzyme (ACE) inhibitors. Thiazide Diuretics Thiazide diuretics are benzothiadiazines, chemical derivatives of sulfonamide antibiotics. The thiazide diuretics include chlorothiazide and hydrochlorothiazide. Hydrochlorothiazide is the most commonly prescribed and the least expensive of the thiazide diuretics. The thiazide-like diuretics are very similar to the thiazides and include chlorthalidone, indapamide, and metolazone. The primary site of action of thiazides and thiazide-like diuretics is the distal convoluted tubule, where they inhibit the resorption of sodium, potassium, and chloride, resulting in osmotic water loss. As renal function decreases, the efficacy of thiazides diminishes because delivery of the drug to the site of activity is impaired. The thiazide and thiazide-like diuretics are used in the treatment of edema of various origins, idiopathic hypercalciuria, and diabetes insipidus, in addition to hypertension. They are also used as adjunct drugs in the management of heart failure and hepatic cirrhosis. Major adverse effects of the thiazide and thiazide-like diuretics relate to electrolyte and metabolic disturbances—mainly reduced potassium levels and elevated levels of calcium, lipids, glucose, and uric acid. Other effects, such as gastrointestinal disturbances, skin rashes, photosensitivity, thrombocytopenia, pancreatitis, and cholecystitis, are less common. Dizziness and vertigo are common adverse effects of metolazone therapy and are attributed to sudden shifts in the plasma volume brought about by the drug. Headache, impotence, and decreased libido are other important adverse effects of these drugs. Nursing Process Perform a physical assessment and document all findings, with emphasis on the body systems affected by the disease process or indication for the diuretic and by potential drug-related adverse effects. Baseline assessment needs to include auscultation of breath sounds and heart sounds, determining neurologic status and checking skin turgor (for edema or dehydration), moisture levels of mucus membranes, and capillary refill. Assess and document the patient’s baseline fluid volume status and postural blood pressures before and during drug therapy because of diuretic-induced fluid volume loss. Methods for monitoring excess and deficit fluid volume states include assessment of skin and mucous membranes, blood pressure, pulse rate, intake and output, and daily weights. With diuretics, always be concerned about the more vulnerable patient populations, such as the older adult patient, those with chronic illnesses, and patients with altered renal or liver function. Copyright © 2020 Elsevier Inc. All Rights Reserved. 132 Carbonic anhydrase inhibitors require close assessment of sodium and potassium levels. These drugs are not to be used in patients with a history of renal or liver dysfunction. There is increased risk for digoxin toxicity with diuretics that result in loss of potassium. Loop diuretics are more potent than thiazide diuretics, combination products, and potassium-sparing diuretics, so these drugs may pose more problems for the elderly or those with severe electrolyte loss and liver failure. Use caution in administering loop diuretics with other medications that are neurotoxic or ototoxic. With potassium-sparing diuretics, hyperkalemia may be an adverse effect; therefore, assess the patient’s serum levels of potassium. Potassium supplements, ACE inhibitors, and severe renal failure are contraindications. Emphasize the importance of taking diuretics at the same time every day. These drugs are generally ordered to be taken in the morning to help prevent nocturia, which may result in lack of sleep. Measure and record blood pressure, pulse rate, intake and output, and daily weights during diuretic therapy. Monitor for the presence of dizziness, fainting, lightheadedness on standing or changing positions, weakness, fatigue, tremor, muscle cramping, changes in mental status, or cold clammy skin. Diuretic therapy may also precipitate cardiac irregularities or palpitations; therefore, continue to monitor heart rate and rhythm. Fluid loss from the action of the diuretic may lead to the adverse effect of constipation so that preventative measures are required, such as increased intake of fluids and fiber (unless contraindicated) and/or the use of natural bulk-forming products. The therapeutic effects of diuretics include the resolution of or reduction in edema, fluid volume overload, heart failure, or hypertension, or a return to normal intraocular pressures. Monitor the patient for the occurrence of adverse reactions to the diuretics, such as hypotension, electrolyte imbalances, metabolic acidosis, drowsiness (with CAIs), hypokalemia, tachycardia, and hyperkalemia (potassium). REVIEW QUESTIONS1. The nurse is reviewing the medications that have been ordered for a patient for whom a loop diuretic has just been prescribed. The loop diuretic may have a possible interaction with which of the following? (Select all that apply.) a. Vitamin D b. Antidiabetic drugs c. Penicillins d. NSAIDs e. Corticosteroids f. warfarin2. In monitoring laboratory test results for patients receiving loop and thiazide diuretics, the nurse knows to look for which of these results? a. Decreased serum levels of potassium b. Increased serum levels of calciumc. Decreased serum levels of glucose d. Increased serum levels of sodium3. When the nurse is checking the laboratory data for a patient taking spironolactone (Aldactone), which result would be a potential concern? a. Serum sodium level of 140 mEq/L b. Serum calcium level of 10.2 mg/dL Copyright © 2020 Elsevier Inc. All Rights Reserved. 133 c. Serum potassium level of 5.8 mEq/L d. Serum magnesium level of 2.0 mg/dL4. Which statement must be included when the nurse provides education for a patient with heart failure who is taking daily doses of spironolactone (Aldactone)? a. “Be sure to eat foods that are high in potassium.” b. “Avoid foods that are high in potassium.” c. “Avoid grapefruit juice while taking this medication.” d. “A low-fiber diet will help prevent adverse effects of this medication.”5. A patient with diabetes has a new prescription for a thiazide diuretic. Which statement will the nurse include in teaching the patient about the thiazide drug? a. “There is nothing for you to be concerned about when you are taking the thiazide diuretic.”b. “Be sure to avoid foods that are high in potassium.” c. “You need to take the thiazide at night to avoid interactions with the diabetes medicine.”d. “Monitor your blood glucose level closely because the thiazide diuretic may cause the levels to increase.”6. An older adult patient has been discharged following treatment for heart failure, and he will be taking a loop diuretic. Which instruction(s) from the nurse are appropriate? (Select all that apply.) a. “Take the diuretic at the same time each morning.” b. “Take the diuretic only if you notice swelling in your feet.” c. “Be sure to stand up slowly because the medicine may make you feel dizzy if you stand up quickly.”455d. “Drink at least 8 glasses of water each day.” e. “Here is a list of foods that are high in potassium; you need to avoid these.”f. “Please call your doctor immediately if you notice muscle weakness or increased dizziness”7. The order reads: Give mannitol 0.5 g/kg IV now, over 2 hours. The patient weighs 165 lb and you have a 100-mL vial of 20% mannitol. How many grams will the patient receive? How many milliliters of mannitol will you prepare for this infusion?8. A patient is taking an aminoglycoside antibiotic for pneumonia and will also be taking the loop diuretic furosemide (Lasix) due to fluid overload. The nurse will monitor carefully for which potential effect from the interaction of these two drugs? a. Nephrotoxicity b. Ototoxicity c. Pulmonary fibrosis d. Hepatotoxicity__________________________________________________________________ ___________________ Copyright © 2020 Elsevier Inc. All Rights Reserved. 134 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 29: Fluids and Electrolytes Chapter 29 1. a; 2. c; 3. b, d; 4. d; 5. d; 6. b, c, d; 7. 125 mL/hr; 31 gtt/min; 8. b. Key Points Anatomy, Physiology, and Pathophysiology Overview Understanding fluid and electrolyte management requires knowledge of the extent and composition of the various body fluid compartments. Approximately 60% of the adult human body is water, distributed in the following proportions: intracellular fluid 67%; interstitial fluid 25%; and plasma volume 8%. Total body water (TBW) is divided into intracellular and extracellular compartments. Fluid volume outside the cells is either in the plasma or between the tissues, cells, or organs. Intravascular fluid describes the fluid inside the blood vessels, and extravascular fluid refers to the fluid outside the blood vessels. Plasma or serum is the fluid that flows through the blood vessels (intravascular fluid). The interstitial fluid (ISF) is the fluid that is in the space between cells, tissues, and organs. There is one big difference between the plasma and the ISF. Plasma has a protein concentration (primarily albumin) four times greater than that of the ISF. Protein solutes have a large molecular weight, making them too large to pass through the walls of blood vessels. Copyright © 2020 Elsevier Inc. All Rights Reserved. 135 Protein in the vessels exerts a constant osmotic pressure that prevents the leakage of too much plasma through the capillaries into the tissues. This is called colloid oncotic pressure and normally it is 24 mm Hg. The opposing pressure exerted by the interstitial fluid is called hydrostatic pressure and normally it is 17 mm Hg—less than the colloid oncotic pressure. Dehydration leads to a disturbance in the balance between the amount of fluid in the extracellular compartment and that in the intracellular compartment. Dehydration may be hypotonic, resulting from the loss of salt; hypertonic, resulting from fever with perspiration; or isotonic, resulting from diarrhea or vomiting. Each form of dehydration is treated differently. Carefully assess intake and output as well as skin turgor, urine specific gravity, and blood levels of potassium, sodium, and chloride. Death often occurs when 20% to 25% of TBW is lost. Acid-base balance is also important to normal bodily functions and is regulated by the respiratory system and the kidney. Pharmacology Overview Crystalloids The choice of whether to use a crystalloid or a colloid depends on the patient’s condition. Crystalloids are fluids given by intravenous (IV) injection that supply water and sodium to maintain the osmotic gradient between the extravascular and intravascular compartments. Crystalloid solutions contain fluids and electrolytes that are normally found in the body, but do not contain proteins. The administration of large quantities of crystalloid solutions for fluid resuscitation decreases the colloid oncotic pressure via a dilutional effect. They can leak from the plasma into the tissues and cells, resulting in edema anywhere in the body. Crystalloids are distributed faster into the interstitial and intracellular compartments than colloids, making them better for treating dehydration than for expanding the plasma volume. Crystalloid solutions are most commonly used as maintenance fluids to compensate for insensible fluid losses, replace fluids, and manage specific fluid and electrolyte disturbances. Crystalloids also promote urinary flow and are less expensive. Hypertonic solutions must be used very cautiously and given slowly because of the risk for hypervolemia from overzealous replacement. Colloids Colloids are large protein particles that increase the colloid oncotic pressure and cannot leak from the blood vessels. They are naturally occurring and consist of proteins (albumin), carbohydrates (dextrans or starches), fats (lipid emulsion), and animal collagen (gelatin). The total protein level must be in the range of 7.4 g/dL. If this level falls below 5.3 g/dL, fluid shifts from blood vessels into the tissues. Colloid oncotic pressure decreases with age and with hypotension and malnutrition. Copyright © 2020 Elsevier Inc. All Rights Reserved. 136 The mechanism of action of colloids is related to their ability to increase the colloid oncotic pressure. Colloids increase the blood volume and are sometimes called plasma expanders. Clinically, colloids are superior to crystalloids because of their ability to maintain the plasma volume for a longer time. They can maintain the colloid oncotic pressure for several hours. Colloids are relatively safe agents, although they have no oxygen-carrying ability and contain no clotting factors, unlike blood products. Because of this, they can alter the coagulation system through a dilutional effect, which results in impaired coagulation and possibly bleeding. They may also dilute the plasma protein concentration, which in turn may impair platelet function. Rarely, dextran therapy causes anaphylaxis or renal failure. The three most commonly used colloids are 5% albumin, dextran 40, and hetastarch. They all have a very rapid onset of action as well as a long duration of action. Blood Products The mechanism of action of blood products is related to their ability to increase the colloid oncotic pressure, and hence the plasma volume. Blood products are the only fluids that are able to carry oxygen because they are the only fluids that contain hemoglobin. Patients will hopefully begin to show improved energy and increasing tolerance for activities of daily living as a result of the treatments with blood products. Pulse oximeter readings will also show improved readings. Blood products are used to treat a wide variety of clinical conditions; the blood product used depends on the specific indication. Because there is a risk for transfer of infectious disease, although remote, their use needs to be based on careful clinical evaluation of the patient’s condition. Because these products come from other humans, they can be incompatible with the recipient’s immune system. They can also transmit pathogens from the donor to the recipient. It is imperative that blood is not administered with any solution other than normal saline. Physiology of Electrolyte Balance The principal electrolytes in the extracellular fluid are sodium cations (Na+) and chloride anions (Cl–). The major electrolyte in the intracellular fluid (ICF) is the potassium cation (K+). Other important electrolytes are calcium, magnesium, and phosphorus. Electrolytes are controlled by the renin-angiotensin-aldosterone system, antidiuretic hormone system, and sympathetic nervous system. When these neuroendocrine systems are out of balance, adverse electrolyte imbalances commonly result. Patients who receive diuretics are at risk of electrolyte abnormalities. Potassium Hyperkalemia is defined as a serum potassium level exceeding 5.5 mEq/L. Symptoms include muscle weakness, paresthesia, paralysis, cardiac rhythm irregularities that can result in ventricular fibrillation, and cardiac arrest. Hypokalemia is defined as a serum potassium level of less than 3.5 mEq/L. Copyright © 2020 Elsevier Inc. All Rights Reserved. 137 Early symptoms of hypokalemia include hypotension, lethargy, mental confusion, nausea, and muscle weakness. Late symptoms include cardiac dysrhythmias (the patient may feel palpitations or shortness of breath), neuropathies, and paralytic ileus. A number of life-sustaining physiologic functions require potassium. Muscle contraction, the transmission of nerve impulses, and the regulation of heartbeats are a few. Potassium is also essential for the maintenance of acid-base balance, isotonicity, and the electrodynamic characteristics of the cell. It plays a role in many enzymatic reactions and is essential in gastric secretion, renal function, tissue synthesis, and carbohydrate metabolism. Potassium replacement therapy is indicated in the treatment or prevention of potassium depletion in patients whenever dietary measures prove inadequate. Potassium salts used for this purpose include potassium chloride, potassium phosphate, and potassium acetate. The adverse effects of oral potassium are primarily limited to the gastrointestinal (GI) tract, including diarrhea, nausea, and vomiting. GI bleeding and ulceration are more significant. The parenteral administration of potassium usually produces pain at the injection site. Intravenous potassium is identified as a high alert drug because of the serious toxicity which can occur when potassium is given intravenously. Patiromer (Veltassa) is a new oral drug indicated for hyperkalemia. It is a non-absorbed cation exchange polymer which increases fecal potassium excretion and ultimately reduces serum potassium levels. Patiromer has a black box warning regarding the decreased absorption of many orally medications. Sodium Sodium is the major cation in extracellular fluid and is involved in the control of water distribution, fluid and electrolyte balance, and osmotic pressure of body fluids. Sodium also participates along with both chloride and bicarbonate in the regulation of acid-base balance. Hyponatremia is a condition of sodium loss or deficiency and occurs when the serum levels decrease less than 135 mEq/L. Hyponatremia is manifested by lethargy, hypotension, stomach cramps, vomiting, diarrhea, and seizures. Osmotic demyelination syndrome (previously called central pontine myelinolysis) may occur when there is rapid correction of chronic hyponatremia. Hypernatremia is the condition of sodium excess and occurs when the serum levels of sodium exceed 145 mEq/L. Hypernatremia is associated with symptoms of water retention but can be associated with normal fluid or even low fluid volume. Hypernatremia symptoms include edema, hypertension, red, flushed skin; dry, sticky mucous membranes; increased thirst; temperature elevation; and decreased or absent urination. Sodium is primarily administered for the treatment or prevention of sodium depletion when dietary measures have proved inadequate. Sodium chloride is used for this purpose. Hypertonic saline (3% NaCl), sometimes used for severe hyponatremia, is a high-risk treatment because if it is given rapidly or at too high a dose it can cause central pontine myelinolysis (osmotic demyelination syndrome) that can lead to irreversible brainstem damage. Copyright © 2020 Elsevier Inc. All Rights Reserved. 138 The oral administration of sodium chloride can cause gastric upset consisting of nausea, vomiting, and cramps. Drugs for the treatment of euvolemic (normal fluid volume) hyponatremia include the dual arginine vasopressin (AVP) V1A and V2 receptor antagonists. These drugs are conivaptan (Vaprisol) and tolvaptan (Samsca) (vaptans). Conivaptan (Vaprisol) is a nonpeptide dual arginine vasopressin (AVP) V1A and V2 receptor antagonist that inhibits the effects of AVP, also known as antidiuretic hormone, on receptors in the kidneys. It is indicated for the treatment of hospitalized patients with euvolemic hyponatremia, or low serum sodium levels at normal water volumes. Tolvaptan has a black box warning stating that the patient must in a hospital where sodium levels can be closely monitored when starting therapy. Nursing Process Assess the patient’s medical history, including diseases of the GI, renal, cardiac, and/or hepatic systems. Assess fluid volume and electrolyte status (through laboratory testing and measurement of urinary specific gravity, vital signs, and intake and output) and document the findings. Confirm orders with authoritative resources or by speaking with a pharmacist. After verifying all prescriber orders, assess the solution or product, the patient, and the IV site. Assess the following for IV infusions of fluids and/or electrolytes: the solution to be infused, infusion equipment, infusion rate of the solution, concentration of the parenteral solution, related mathematical calculations, laboratory values (e.g., sodium, chloride, potassium), and parenteral compatibilities. Remember that you are responsible for making sure that the drug therapy administration process—beginning with the assessment phase of the nursing process and through to evaluation—is accurate and safe and meets professional standards of care. Each form of dehydration is treated differently. Carefully assess intake and output as well as skin turgor, urine specific gravity, and blood levels of potassium, sodium, and chloride. Hydrating and hypotonic solutions include 0.25% NaCl and 0.45% NaCl/D5W. Isotonic solutions (e.g., 0.9% NaCl [normal saline] and lactated Ringer’s solution) are used to augment extracellular volume in patients experiencing blood loss and/or severe vomiting. Hypertonic solutions (e.g., 3% or 5% sodium chloride) are used for replacement of fluids and electrolytes in specific situations. The skin and mucous membranes also reflect a patient’s hydration status; assess skin turgor and/or rebound elasticity of skin over the top of the hand and other areas over the body. Document the findings as “immediate” rebound or “delayed” rebound. Count the number of seconds that the patient’s skin stays in the pinched-up position, with normal return being immediately or within 3 to 5 seconds. Administer albumin with caution because of the high risk for hypervolemia and possible heart failure. Monitor intake and output, weights, heart and breath sounds, and lab values. Copyright © 2020 Elsevier Inc. All Rights Reserved. 139 Venous access is an issue with parenteral potassium supplementation because the vein can be irritated if infiltration occurs or if the solution has not been mixed thoroughly. During the infusion of blood components, constantly assess for the occurrence of fever and blood in the urine, both being indicative of a reaction requiring immediate attention. During replacement therapy, serum electrolyte levels need to remain within normal ranges and not exceed these ranges. With parenteral dosing, monitor infusion rates as well as the appearance of the fluid or solution; potassium and saline solutions are clear and albumin is brown, clear, and viscous. Frequently monitor the IV site for evidence of infiltration. Remember that elderly and/or pediatric patients have an increased sensitivity to these solutions and fluids. For the patient who is at risk for hypokalemia, provide educational materials and patient teaching to encourage consumption of certain foods high in potassium. Early symptoms of hypokalemia include hypotension, lethargy, mental confusion, nausea, and muscle weakness. Late symptoms include cardiac dysrhythmias (the patient may feel palpitations or shortness of breath), neuropathies, and paralytic ileus. Symptoms of hyperkalemia include muscle weakness, paresthesia, paralysis, and cardiac rhythm abnormalities. Hyperkalemia is treated with sodium polystyrene sulfonate (Kayexalate). It is used only under very specific situations and under very close monitoring of the patient and his or her serum potassium, sodium, calcium, and magnesium levels. Patiromer (Veltassa), a new drug, is indicated for treatment of hyperkalemia. Because of altering the absorption of other oral medications, patiromer is not to be given six hours before or after other oral medications. Patiromer needs to be diluted and given with food. Potassium is never given by IV push or IV bolus or in an undiluted form. Potassium administered in this manner is associated with cardiac arrest. Always carry out IV infusion of albumin and other colloids slowly and cautiously, and carefully monitor the patient to prevent fluid overload and potential heart failure. With administration of blood products, measurement of vital signs and frequent monitoring of the patient before, during, and after infusions are critical to patient safety. Blood products must be given only with normal saline (0.9% sodium chloride). The solution of D5W results in hemolysis of red blood cells if infused together. A transfusion reaction may include apprehension, restlessness, flushed skin, increased pulse and respirations, dyspnea, rash, joint or lower back pain, swelling, fever and chills (a febrile reaction beginning 1 hour after the start of administration and possibly lasting up to 10 hours), nausea, weakness, and jaundice. Encourage patients receiving any type of fluid or electrolyte substance, colloid, or blood component to immediately report unusual adverse effects to their prescriber, including chest pain, dizziness, weakness, and shortness of breath. The therapeutic response to fluid, electrolyte, and blood or blood component therapy includes normalization of fluid volume and laboratory values, including RBC and WBC counts, hemoglobin level, hematocrit, and sodium and potassium levels. Copyright © 2020 Elsevier Inc. All Rights Reserved. 140 Frequently monitor for adverse effects of any of these drugs and/or solutions, and check for distended neck veins; shortness of breath; anxiety; insomnia; expiratory crackles; frothy, blood-tinged sputum; and cyanosis (indicative of fluid volume overload). REVIEW QUESTIONS1. Which action by the nurse is most appropriate for the patient receiving an infusion of packed red blood cells? a. Flush the IV line with normal saline (NS) before the blood is added to the infusion.b. Flush the IV line with dextrose before the blood is added to the infusion.c. Check the patient’s vital signs after the infusion is completed.d. Anticipate that flushed skin and fever are expected reactions to a blood transfusion.2. When preparing an IV solution that contains potassium, which of these conditions must a nurse recognize as a contraindica-tion to the potassium infusion? a. Diarrhea b. Serum sodium level of 145 mEq/L c. Serum potassium level of 5.6 mEq/L d. Dehydration3. When assessing a patient who is about to receive an albumin infusion, which of these conditions must a nurse recognize as a possible contraindication to albumin infusion? (Select all that apply.) a. Pancreatitis b. Heart failure c. Severe burnsd. Renal insufficiency e. Fluid-volume deficit4. The nurse is preparing an infusion for a patient who has a deficiency in clotting factors. Which type of infusion is most appropriate? a. Albumin 5% b. Packed RBCs c. Whole blood d. Fresh frozen plasma5. While monitoring a patient who is receiving an infusion of a crystalloid solution, the nurse will monitor for which potential problem? a. Bradycardia b. Hypotension c. Decreased skin turgor d. Fluid overload6. The nurse is administering an IV solution that contains potassium chloride to a patient in the critical care unit who has a severely decreased serum potassium level. Which action(s) by the nurse are appropriate? (Select all that apply.) a. Administer the potassium by slow IV bolus. b. Administer the potassium at a rate no faster than 20 mEq/hr with a heart monitor. d. Use an infusion pump for the administration of IV potassium chloride.e. Administer the potassium via IV push.7. The order reads: “Infuse 1000 mL of NS over the next 8 hours.” The IV tubing has a drop factor of 15 gtt/mL. Calculate the mL/hour rate, and calculate the drops/minute setting for the IV tubing with this gravity infusion.8. A patient is about to receive a dose of the nonprotein plasma expander, dextran. The nurse knows that this product is indicated for which type of blood loss? a. Slow loss of 20% or less b. Slow loss of 20% to 50% c. Slow loss of over 50% or acute loss of 20% d. Loss of 80% or more_________________________________________________________________________ __________ Copyright © 2020 Elsevier Inc. All Rights Reserved. 141 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 31: Thyroid and Antithyroid Drugs Chapter 31 1. a, c; 2. d; 3. a; 4. c; 5. b; 6. a, c; 7. 100 mcg; 8. a, d. Key Points Anatomy, Physiology, and Pathophysiology Overview The thyroid gland lies across the larynx in front of the thyroid cartilage. Its lobes extend laterally on both sides of the front of the neck. The thyroid gland is responsible for the secretion of three hormones essential for the proper regulation of metabolism: thyroxine (T4), triiodothyronine (T3), and calcitonin. Thyroxine (T4) and triiodothyronine (T3) are produced in the thyroid gland; thyroid hormones are made by iodination and coupling with the amino acid tyrosine. The iodide needed for this process is acquired from the diet. When the thyroid gland is signaled to do so, the thyroglobulin–thyroid hormone complex is enzymatically broken down to release T3 and T4 into the circulation. This entire process is triggered by thyroid-stimulating hormone (TSH), also called thyrotropin. Its release from the anterior pituitary gland is stimulated when blood levels of T3 and T4 are low. The thyroid hormones (1) regulate the basal metabolic rate and lipid and carbohydrate metabolism, (2) are essential for normal growth and development, (3) control the heatregulating system (thermoregulatory center in the brain), and (4) have various effects on the cardiovascular, endocrine, and neuromuscular systems. Pathophysiology of Hypothyroidism Primary hypothyroidism occurs when the thyroid gland is not able to perform one of its many functions, such as releasing the thyroid hormones from their storage sites, coupling iodine with tyrosine, trapping iodide, converting iodide to iodine, or any combination of these defects. Primary hypothyroidism is the most common of the three types of hypothyroidism. Copyright © 2020 Elsevier Inc. All Rights Reserved. 142 Secondary hypothyroidism begins at the level of the pituitary gland and results from reduced secretion of TSH. TSH is needed to trigger the release of the T3 and T4 stored in the thyroid gland. Tertiary hypothyroidism is caused by a reduced level of the thyrotropin-releasing hormone from the hypothalamus. This reduced level, in turn, reduces TSH and thyroid hormone levels. Symptoms of hypothyroidism include cold intolerance, unintentional weight gain, depression, dry brittle hair and nails, and fatigue. Hyposecretion of thyroid hormone during youth may lead to cretinism, which is characterized by low metabolic rate, retarded growth and sexual development, and possible mental retardation. Hyposecretion of thyroid hormone as an adult may lead to myxedema, which is manifested by decreased metabolic rate but also involves loss of mental and physical stamina, weight gain, hair loss, firm edema, and yellow dullness of the skin. Some forms of hypothyroidism may result in the formation of a goiter, which is an enlargement of the thyroid gland resulting from its overstimulation by elevated levels of TSH. Pathophysiology of Hyperthyroidism Hyperthyroidism is caused by excessive secretion of thyroid hormone by the thyroid gland and may be caused by different diseases. Always assess and document important information about the patient’s medical history appropriately. Diseases known to cause hyperthyroidism include Graves’ disease, which is the most common cause; Plummer disease, also known as toxic nodular disease, which is the least common cause; multinodular disease; and thyroid storm, which is a severe and potentially life-threatening exacerbation of the symptoms of hyperthyroidism that is usually induced by stress or infection. Hyperthyroidism can affect multiple body systems, resulting in an overall increase in metabolism. Commonly reported symptoms are diarrhea, flushing, increased appetite, muscle weakness, fatigue, palpitations, irritability, nervousness, sleep disorders, heat intolerance, and altered menstrual flow. Pharmacology Overview Thyroid Replacement Drugs Thyroid hormone replacement is generally carried out carefully by the prescriber with frequent monitoring of serum levels until stabilization appears to have occurred. Monitor and review laboratory values to be sure that serum levels are within normal limits to avoid possible toxicity. Thyroid hormone replacement drugs can be either natural or synthetic in origin. The natural thyroid preparations are derived from the thyroid glands of animals such as cattle and hogs. Currently only one natural thyroid replacement preparation is available in the United States, and it is called simply thyroid or thyroid, desiccated. Monitoring of serum TSH and free thyroid hormone levels is required to determine the appropriate dose of thyroid replacement drugs. Copyright © 2020 Elsevier Inc. All Rights Reserved. 143 At the cellular level, thyroid drugs work to induce changes in the metabolic rate, including the rate of protein, carbohydrate, and lipid metabolism, and to increase oxygen consumption, body temperature, blood volume, and overall cellular growth and differentiation. They also stimulate the cardiovascular system by increasing the number of myocardial beta-adrenergic receptors. This, in turn, increases the sensitivity of the heart to catecholamines and ultimately increases cardiac output. In addition, thyroid hormones increase renal blood flow and the glomerular filtration rate, which results in a diuretic effect. Thyroid drugs can also be used for the diagnosis of suspected hyperthyroidism (as in a TSH-suppression test) and in the prevention or treatment of various types of goiters. They are also used for replacement hormonal therapy in patients whose thyroid glands have been surgically removed or destroyed by radioactive iodine in the treatment of thyroid cancer or hyperthyroidism. Hypothyroidism during pregnancy is treated with dosage adjustments every 4 weeks to maintain the TSH level at the lower end of the normal range. Thyroid drugs may enhance the activity of oral anticoagulants, the dosages of which may need to be reduced. Taking thyroid preparations concurrently with digitalis glycosides may decrease serum digitalis levels. Cholestyramine binds to thyroid hormone in the gastrointestinal tract, which possibly reduces the absorption of both drugs. Diabetic patients taking a thyroid drug may require increased dosages of their hypoglycemic drugs. The most commonly used thyroid replacement drugs are the synthetic drugs levothyroxine and liotrix. Levothyroxine is preferred because its hormonal content is standardized and its effect is predictable. Some patients experience better results with the animal-derived products. Although the thyroid drugs differ chemically, therapeutic actions are all the same. Care must be taken when preparing IV doses of levothyroxine for infusions. It is essential to remember that the vial must be diluted FIRST, and then the dose is calculated based on the concentration of the reconstituted medication, not the size of the vial. For levothyroxine (Synthroid, Levothroid, Levoxyl), the pharmacokinetic characteristics include an onset of action of 3 to 5 days, peak plasma concentrations within 24 hours, elimination half-life of 6 to 10 days, and a duration of action of 24 hours. Due to the prolonged half-life of this drug, there is an increased risk of toxicity. The adverse effects of thyroid medications are usually the result of overdose. The most significant adverse effect is cardiac dysrhythmia with the risk for life-threatening or fatal irregularities. Adverse effects associated with thyroid drugs include tachycardia, palpitations, angina, dysrhythmias, hypertension, insomnia, tremors, headache, anxiety, nausea, diarrhea, cramps, menstrual irregularities, weight loss, sweating, fever, and heat intolerance. Toxicity is manifested by the following: weight loss, tachycardia, nervousness, tremors, hypertension, headache, insomnia, menstrual irregularities, and cardiac irregularities or palpitations. Another important pharmacokinetic property is that the drug is protein bound. A highly protein-bound drug acts like a biologic sustained-release drug and remains in the body longer, with increased risk of more interactions with other highly protein-bound drugs as well as greater potential for toxicity. Copyright © 2020 Elsevier Inc. All Rights Reserved. 144 Patients receiving levothyroxine need to report the occurrence of excitability, irritability, or palpitations to the prescriber because these symptoms may indicate toxicity. Antithyroid Drugs Treatment of hyperthyroidism is aimed at treating either the primary cause or the symptoms of the disease. Antithyroid drugs, iodides, ionic inhibitors, surgery, and radioactive isotopes of iodine are used to treat the underlying cause, and drugs such as beta blockers are used to treat the symptoms. Antithyroid drugs include thioamide derivatives, namely methimazole and propylthiouracil. In addition to the thioamides, radioactive iodine (iodine 131) and potassium iodide may be used to treat hyperthyroidism. Radioactive iodine works by destroying the thyroid gland, in a process known as ablation, emitting destructive beta rays once it is taken up into the follicles of the thyroid gland. It is a commonly used treatment for both hyperthyroidism and thyroid cancer. Potassium iodide is also used as prophylaxis for radiation exposure. Methimazole and propylthiouracil act by inhibiting the incorporation of iodine molecules into the amino acid tyrosine, a process required to make the precursors of T3 and T4. By doing so, these drugs impede the formation of thyroid hormone. Antithyroid drugs are used to treat hyperthyroidism and to prevent the surge in thyroid hormones that occurs after the surgical treatment of or during radioactive iodine therapy for hyperthyroidism or thyroid cancer. In some types of hyperthyroidism, such as that seen in Graves’ disease, the long-term administration of these drugs (for several years) may induce a spontaneous remission. Surgical resection of the thyroid gland (thyroidectomy) involves removal of part or all of the thyroid gland. It is usually a very effective way to treat hyperthyroidism, but lifelong hormone replacement therapy is normally required after thyroid surgery. It is often used both in patients who are intolerant of antithyroid drug therapy and in pregnant women. The most damaging or serious adverse effects of the antithyroid medications are liver and bone marrow toxicity. Adverse effects associated with antithyroid drugs include drowsiness, headache, vertigo, nausea, vomiting, diarrhea, loss of taste, bleeding, leukopenia, rash, myalgia, and arthralgia. Drug interactions that occur with antithyroid drugs include additive leukopenic effects when they are taken in conjunction with other bone marrow depressants and an increase in the activity of oral anticoagulants. Nursing Process Assess levels of T3, T4, and TSH before and during drug therapy, as ordered. Review baseline vital signs with increased attention to a history of cardiac dysrhythmias because of the possible adverse effects of cardiac irregularities that may be life threatening. For the female patient, perform a thorough assessment of the reproductive system due to the impact of thyroid hormones on this system. Lifespan considerations include increased sensitivity to the effects of thyroid medications in elderly patients. Copyright © 2020 Elsevier Inc. All Rights Reserved. 145 For antithyroid drugs, such as propylthiouracil and methimazole, first measure vital signs and assess for signs and symptoms of thyroid crisis or thyroid storm. Assess for potential causes of thyroid storm such as stress or infection. When thyroid drugs are administered, it is important that the drug be given at the same time every day to help maintain consistent blood levels of the drug. Emphasize to the patient that it is best to administer thyroid drugs once daily in the morning, if possible, to decrease the likelihood of insomnia, which may result from evening dosing and the subsequent increase in energy level. Educate the patient taking the antithyroid drug propylthiouracil about taking the medication with meals to help decrease stomach upset. Any fever, sore throat, mouth ulcers or sores, or skin eruptions, as well as any unusual bleeding or bruising, needs to be reported to the prescriber immediately. These symptoms may indicate problems of liver and bone marrow toxicity and possible leukopenia. Further educate patients to avoid the use of iodized salt or eating shellfish because of their potential for altering the drug’s effectiveness. Advise patients to be aware of the signs and symptoms of hypothyroidism, including unexplained weight gain, loss of mental and physical stamina, hair loss, firm edema, and yellow dullness of the skin (indicative of myxedema or a decrease in metabolic rate). If these occur, patients must report them immediately to the prescriber. Frequently monitor complete blood counts to watch for potential problems with leukopenia. It is also important to monitor the results of liver function studies. A therapeutic response to thyroid drugs is manifested by the disappearance of the symptoms of hypothyroidism; the patient would demonstrate improved energy levels as well as improved mental and physical stamina. Adverse effects to monitor for include cardiac dysrhythmia. A therapeutic response to antithyroid medications includes a return to normal status with little to no evidence of hyperthyroid. Adverse effects include the possibility of leukopenia, which may be manifested by fever, sore throat, lesions, or other signs of infection. REVIEW QUESTIONS1. When monitoring the laboratory values for a patient who is taking antithyroid drugs, the nurse knows to watch for which of these? (Select all that apply.) a. Decreased platelet counts b. Increased white blood cell counts c. Increased blood urea nitrogen level d. Increased blood glucose levels e. Decreased creatinine levels2. The pharmacy has called a patient to notify her that the current brand of thyroid replacement hormone is on back order. The patient calls the clinic to ask what to do. Which is the best response by the nurse? a. “Go ahead and take the other brand that the pharmacy has available for now.”b. “You can stop the medication until your current brand is available.”c. “You can split the thyroid pills that you have left so that they will last longer.”d. “Let me ask your prescriber what needs to be done; we will need to watch how you do if you switch brands.”3. The nurse is assessing a 72-yearCopyright © 2020 Elsevier Inc. All Rights Reserved. 146 old patient who will be start-ing thyroid replacement therapy. Which statement is true regarding the dosage of thyroid replacement hormones for the older adult? a. Thyroid hormone replacement requirements are approxi-mately 25% lower for this age group.b. Older adults require higher dosages of thyroid replacement hormone for therapeutic effects.c. There is no difference in the dosage of thyroid replacement hormone in older adults versus younger adults.d. The dosage of thyroid hormone will depend upon the amount of iodine in the patient’s diet.4. To help with the insomnia associated with thyroid hormone replacement therapy, the nurse will include which statement in the teaching session? a. “Take half the dose at lunchtime and the other half 2 hours later.”b. “You will need to use a sedative to help you fall asleep.” c. “Take the dose upon awakening in the morning.” d. “The dose may need to be reduced if you can’t sleep.”5. The nurse is teaching a patient who has a new prescription for the antithyroid drug propylthiouracil (PTU). Which statement by the nurse is correct? a. “There are no food restrictions while on this drug.” b. “You need to avoid foods high in iodine, such as iodized salt, seafood, and soy products.”c. “This drug is given to raise the thyroid hormone levels in your blood.”d. “Take this drug in the morning on an empty stomach.”6. When teaching a patient who has a new prescription for thyroid hormone, the nurse will instruct the patient to notify the prescriber if which adverse effects are noted? (Select all that apply.) a. Palpitations b. Weight gain c. Angina d. Fatigue e. Cold intolerance7. The nurse is giving an intravenous dose of levothyroxine (Synthroid). The order reads: “Give 0.1 mg IV push now.” What is the ordered dose in micrograms? 8. Which laboratory tests does the nurse know are used to monitor thyroid hormone replacement therapy? (Select all that apply.) a. Serum TSH b. BUN c. CBC d. Free thyroid hormone levels e. Serum iodine levels Lilley: Pharmacology and the Nursing Process, 9th Edition Copyright © 2020 Elsevier Inc. All Rights Reserved. 147 Chapter 32: Antidiabetic Drugs Chapter 32 1. a; 2. c; 3. c; 4. c; 5. a; 6. b; 7. a, b, c, f; 8. b, c. Key Points Anatomy, Physiology, and Pathophysiology Overview Pancreas The pancreas is both an exocrine gland (secreting digestive enzymes through the pancreatic duct) and an endocrine gland (secreting hormones directly into the bloodstream and not through a duct). Two main hormones that are produced by the pancreas are insulin and glucagon. Both hormones play an important role in the regulation of glucose homeostasis, specifically the use, mobilization, and storage of glucose by the body. Glucose is one of the primary sources of energy for the cells of the body. It is also the simplest form of carbohydrate (sugar) found in the body and is often referred to as dextrose. When the quantity of glucose in the blood is sufficient, the excess is stored as glycogen in the liver and, to a lesser extent, in skeletal muscle tissue, where it remains until needed. Glucose is also stored in adipose tissue as triglyceride, body fat. When more circulating glucose is needed, glycogen—primarily that stored in the liver— is converted back to glucose through a process called glycogenolysis. The hormone responsible for initiating this process is glucagon. Glucagon has only minimal effects on muscle glycogen and adipose tissue triglyceride stores. Because of the critical role of the pancreas in producing and maintaining these two hormones, pancreatic or islet cell transplant are sometimes undertaken to treat type 1 diabetes that has not been successfully controlled by other means. Insulin normally facilitates removal of glucose from the blood and its storage as glycogen in the liver. Insulin also has a direct effect on fat metabolism. It stimulates lipogenesis and inhibits lipolysis and the release of fatty acids from adipose cells. Pathophysiology of Diabetes Mellitus Diabetes mellitus, more commonly referred to simply as diabetes, is primarily a disorder of carbohydrate metabolism that involves either a deficiency of insulin, a resistance of tissue (e.g., muscle, liver) to insulin, or both. Two major types of diabetes mellitus are type 1 and type 2. Type 1 diabetes was previously called insulin-dependent diabetes mellitus (IDDM) or juvenile-onset diabetes. Little or no endogenous insulin is produced by individuals with type 1 diabetes, which affects only about 10% of all diabetic patients. Patients with type 1 diabetes usually are not obese. The primary treatment for type 1 diabetes mellitus is insulin therapy. Patients with the cognitive and financial ability are encouraged to consider insulin pumps with continuous glucose monitoring. Type 2 diabetes was previously called non–insulin-dependent diabetes mellitus (NIDDM) or adult-onset diabetes. Copyright © 2020 Elsevier Inc. All Rights Reserved. 148 Type 2 diabetes mellitus accounts for at least 90% of all cases of diabetes mellitus. Type 2 diabetes mellitus is caused by both insulin resistance and insulin deficiency, but there is no absolute lack of insulin as in type 1 diabetes. Type 2 diabetes is a multifaceted disorder. Although loss of blood glucose control is its primary hallmark, other conditions associated with it are obesity, coronary heart disease, dyslipidemia, hypertension, microalbuminuria, and an increased risk for thrombotic events. Patients with type 2 diabetes are managed with lifestyle changes (dietary changes, exercise, smoking cessation) and oral drug therapy (one or more drugs). If normal blood glucose levels are not achieved after 2 to 3 months of lifestyle changes, treatment with oral diabetes drugs is often added to the regimen. The current key diagnostic criterion for diabetes mellitus is hyperglycemia with a fasting plasma glucose (FPG) level of higher than 126 mg/dL or a hemoglobin A1C (A1C) level greater than or equal to 6.5%. The most common signs and symptoms of diabetes are elevated blood glucose level (fasting glucose level higher than 126 mg/dL) and polyuria, polydipsia, polyphagia, glucosuria, weight loss, blurred vision, and fatigue. A new term, estimated average glucose (eAG), is a mathematical conversion of the A1C into an average blood glucose level in the units of measure seen by patients on glucose meters for self-monitoring (mg/dl). Similar to A1C, eAG evaluates a patient’s overall success at controlling glucose levels and helps patients understand the monitoring of their long-term treatment. Type 1 diabetes mellitus is characterized by a lack of insulin production or by the production of defective insulin, which results in acute hyperglycemia. Affected patients require exogenous insulin to lower the blood glucose level and prevent diabetic complications. When blood glucose levels are high but no insulin is present to allow glucose to be used for energy production, the body may break down fatty acids for fuel, producing ketones as a metabolic by-product and resulting in diabetic ketoacidosis (DKA). DKA is a complex multisystem complication of uncontrolled diabetes. Another complication that is also triggered by extreme hyperglycemia is hyperosmolar nonketotic syndrome (HNKS). The most common precipitator of DKA and HNKS is some type of physical or emotional stress. Both disorders can occur with diabetes of either type. The goal for patients with diabetes is a blood pressure less than 130/80 mm Hg and lowdensity lipid less than 100 mg/dL. Gestational diabetes is a type of hyperglycemia that occurs in about 2% to 10% of pregnancies. Many patients are well controlled with diet, but the use of insulin may be necessary to decrease the risk of birth defects, hypoglycemia in the newborn, and high birth weight. As many as 30% of patients who experience gestational diabetes are estimated to develop type 2 diabetes within 10 to 15 years. Adults 45 years of age and older should be screened for elevated FPG levels every 3 years. Patients diagnosed with type 1 diabetes always require insulin therapy. For patients with new-onset type 2 diabetes, lifestyle changes should be initiated as a first step in treatment. Weight loss, improved dietary habits, smoking cessation, reduced alcohol consumption, and regular physical exercise are just a few examples of lifestyle changes. Copyright © 2020 Elsevier Inc. All Rights Reserved. 149 The glycemic goal recommended by the American Diabetes Association (ADA) for diabetic patients is an A1C level of less than 7%. The A1C can be used as diagnostic criteria as follows: A1C less than 5.7 is considered normal; A1C between 5.7 and 6.4 is considered prediabetes; A1C above 6.5 is considered type 2 diabetes. Pharmacology Overview The major classes of drugs used to treat diabetes mellitus are the insulins and the oral antidiabetic drugs. Several new classes of injectable drugs with unique mechanisms of action have been developed that may be used in addition to insulins or oral antidiabetic drugs to treat resistant diabetes. All of these drugs are referred to as antidiabetic drugs and are aimed at producing a normoglycemic or euglycemic (normal blood glucose) state. Insulins Currently insulin is synthesized in laboratories using recombinant deoxyribonucleic acid (DNA) technology and is referred to as human insulin. Insulin was originally isolated from cattle and pigs, but bovine and porcine insulins are associated with a higher incidence of allergic reactions and insulin resistance and are no longer available in the U.S. market. Exogenous insulin functions as a substitute for the endogenous hormone. When an insulin pump is used, insulin is administered constantly over a 24-hour period and the patient is then allowed to give bolus injections based on the amount of food ingested. All insulin preparations can be used to treat both type 1 and type 2 diabetes, but each patient requires careful customization of the dosing regimen for optimal glycemic control. Additional therapeutic approaches such as lifestyle modifications (e.g., dietary and exercise habits) are also indicated and, for type 2 diabetes, oral drug therapy as well. Hypoglycemia resulting from excessive insulin dosing can result in brain damage, shock, and possible death. This is the most immediate and serious adverse effect of insulin. Two special patient populations for whom careful attention is required during insulin therapy are pediatric patients and pregnant women. The combination lispro product Humalog 75/25 is not currently approved for use in children younger than 18 years of age. Children need age-appropriate education and supervision by health care professionals and parents, which includes a gradual transfer of responsibility for self-management. Oral medications are generally not recommended for pregnant patients because of a lack of firm safety data. Insulin therapy is the only currently recommended drug therapy. There are currently four major classes of insulin, as determined by their pharmacokinetic properties: rapid-acting, short-acting, intermediate-acting, and long-acting. The duration of action ranges from several hours to over 24 hours depending on the insulin class. The rapid-acting insulins are considered human insulin analogues. This means that they are insulin molecules with synthetic alterations to their chemical structures that alter their onset or duration of action. They have a faster onset of action and a shorter time to peak plasma level, but they also have a shorter duration of action than does regular insulin. Copyright © 2020 Elsevier Inc. All Rights Reserved. 150 Four long-acting insulin products are available: insulin glargine (Lantus), insulin detemir (Levemir); insulin degludec (Tresiba), and the first biosimilar insulin, Basaglar (insulin glargine). New combination products combining long-acting insulin glargine and one of the GLP-1 agonists are available. Soliqua (insulin glargine and lixisenatide) and Xultophy (insulin degludec and liraglutide) are the two combination products available at this time. When an individual is on a sliding-scale insulin regimen, blood glucose concentrations are determined several times a day (e.g., before meals and at bedtime) for patients on normal meal schedules, or every 4 to 6 hours around the clock for patients receiving total parenteral nutrition (TPN) or enteral tube feedings. Current research does not support the use of sliding scales or insulin without basal insulin, and many institutions are moving away from sliding-scale coverage. Basal-bolus insulin dosing is now the preferred method of treatment for hospitalized diabetic patients. A long-acting insulin (insulin glargine) is used to mimic the basal secretion of a healthy pancreas and constant delivery of insulin, keeping the blood glucose level from fluctuating and then the bolus is used (insulin lispro or insulin apart) to mimic the burst secretions of the pancreas in response to increases in blood glucose levels, broken up into meal and correction boluses. In 2014, the FDA approved a new inhaled method of insulin delivery. Afrezza is an inhaled rapid-acting insulin with a rapid onset of action, peak of 12 to 15 minutes and short duration of action of 2 to 3 hours. Administered within 20 minutes before each meal, it is given in conjunction with long-acting insulins or oral diabetic agents (in type 2 diabetes). The most common side effects include hypoglycemia, cough, and throat pain. Afrezza has a black box warning regarding the risk of acute bronchospasms and is contraindicated in smokers or those with chronic lung diseases. Regular insulin is available as a U-500, which is a high-alert medication. Many hospitals do not allow U-500 insulin because of the potential for errors. However, due to patient safety concerns, U-500 is now available in a pen which is designed to alleviate dosing errors. More concentrated insulins are being developed in pens to provide required insulin doses with less volume. Oral Antidiabetic Drugs The 2013 ADA Guidelines recommend that new-onset type 2 diabetes be treated with both lifestyle interventions and the oral biguanide drug metformin, if there are no contraindications to the drug. If lifestyle modifications and the maximum tolerated metformin dose do not achieve the recommended A1C goals after 3 to 6 months, additional treatment with a second oral agent, GLP-1 agonist (liraglutide, exenatide, abliglutide) or insulin is recommended. Metformin is currently the only drug classified as a biguanide. It is considered a first-line drug, especially for patients with a body mass index over 25, and is the most commonly used oral drug for the treatment of type 2 diabetes. Metformin is contraindicated in patients with renal disease or renal dysfunction (serum creatinine level higher than 1.5 mg/dL in males or higher than 1.4 mg/dL in females). Copyright © 2020 Elsevier Inc. All Rights Reserved. 151 The most common adverse effects of metformin are gastrointestinal. Metformin can cause abdominal bloating, nausea, cramping, a feeling of fullness, and diarrhea, especially at the start of therapy. These effects are all usually self-limiting. Exenatide (Byetta; pregnancy category C) was approved in 2005 as the first incretin mimetic drug. Exenatide is a long-acting analogue of GLP-1 that was initially derived from the salivary gland of the Gila monster. This drug is available only as a subcutaneous injection and is indicated only for patients with type 2 diabetes who have been unable to achieve blood glucose control with metformin, a sulfonylurea, and/or a glitazone. It cannot be used with insulin. It is best given 60 minutes before a meal. Liraglutide (Victoza) is similar to exenatide. Albiglutide (Tanzeum) is the newest GLP-1 agonist and was released in 2014. The sulfonylureas second-generation drugs include glipizide (Glucotrol), glyburide (Diabeta), and glimepiride (Amaryl). Sulfonylureas bind to specific receptors on beta cells in the pancreas to stimulate the release of insulin and secondarily decrease the secretion of glucagon. The patient must still have functioning beta cells in the pancreas. Sulfonylureas are recommended as second-step drugs for patients with type 2 diabetes whose A1C levels remain elevated after metformin is initiated. The most common adverse effect of the sulfonylureas is hypoglycemia, depending on the dose, eating habits, and presence of hepatic or renal disease, and weight gain. Repaglinide (Prandin) and nateglinide (Starlix) are currently the only two drugs in the glinide class, different from the sulfonylureas but with a similar mechanism of action. They have a much shorter duration of action and must be given with each meal. The glinides are indicated for treatment of type 2 diabetes and are useful for diabetic patients with high postprandial glucose levels who have low levels of circulating insulin. Qtern is a new combination of saxagliptin and dapaglifiozin. The most commonly reported adverse effect of the glinides is hypoglycemia, which can occur particularly if food is not eaten after a dose. Weight gain is also commonly reported. The thiazolidinediones, most commonly referred to as glitazones, act by regulating genes involved in glucose and lipid metabolism. Pioglitazone (Actos) is the only glitazone currently available and is widely used. Rosiglitazone (Avandia) is not available in retail pharmacies and it can be purchased only through specially certified pharmacies participating in the Avandia-Rosiglitazone Medicines Access Programs. Thiazolidinediones are contraindicated for use in patients with New York Heart Association class III or IV heart failure and are to be used with caution in patients with liver or kidney disease. The glitazones increase the risk of heart failure (commonly cause peripheral edema and weight gain) and are not recommended for use in patients with symptoms of heart failure. Less commonly used oral drugs are the alpha-glucosidase inhibitors, acarbose (Precose) and miglitol (Glyset), which work by reversibly inhibiting the enzyme alpha-glucosidase that is found in small intestine. When this enzyme is blocked, glucose absorption is delayed. The alpha-glucosidase inhibitors are used to treat type 2 diabetes, usually in combination with another oral hypoglycemic drug and especially for high postprandial glucose levels. Copyright © 2020 Elsevier Inc. All Rights Reserved. 152 The timing of administration of the alpha-glucosidase inhibitor is important, and they must be taken with food. When an alpha-glucosidase inhibitor is taken with a meal, excessive postprandial blood glucose elevation can be prevented or reduced. These drugs can cause a high incidence of flatulence, diarrhea, and abdominal pain. At high dosages, they may also elevate levels of hepatic enzymes (transaminases). Dipeptidyl peptidase-IV (DPP-IV) inhibitors work by delaying the breakdown of incretin hormones by inhibiting the enzyme DPP-IV. Currently there are three DPP-IV inhibitors: sitagliptin (Januvia), saxagliptin (Onglyza), and linagliptin (Tradjenta). The most common effects are upper respiratory tract infection, headache, and diarrhea. Hypoglycemia can occur and is more common if used in conjunction with a sulfonylurea. SGLT2 inhibitors are a new class of oral drugs for the treatment of type 2 diabetes mellitus which inhibit glucose re-absorption in the proximal renal tubules resulting in glycosuria. They may also increase insulin sensitivity and glucose uptake in the muscle cells and decrease gluconeogenesis. Their use in clinical practice is associated with improved glycemic control, weight loss, and a low risk of hypoglycemia. SGLT2 inhibitors currently under development including ipragliflozin and tofogliflozin. Canagliflozin (Invokana), dapagliflozin (Farxiga), and empagliflozin (Jardiance) are the three that are currently FDA approved. They are all pregnancy category C. The drugs may be used solo or in combination with other drugs. Assess for contraindications such as impaired kidney function and diabetic ketoacidosis. Glucose-Elevating Drugs Hypoglycemia is an abnormally low blood glucose level (generally below 50 mg/dL). When the cause is organic and the effects are mild, treatment usually consists of dietary modifications to prevent a rebound postprandial hypoglycemic effect. Oral forms of concentrated glucose are available for patients to use in the event of a hypoglycemic crisis. Glucagon is available as a subcutaneous injection to be given when a quick response to severe hypoglycemia is needed. This may induce vomiting. Use of an insulin pump (continuous subcutaneous insulin infusion) leads to a more rapid, consistent absorption of the drug and a reduction in the occurrence of hypoglycemia. Nursing Process Assess the patient’s knowledge about the disease and recommended treatment. Complete a head-to-toe physical assessment, medication history taking, and nursing assessment. Review the appropriate laboratory test results (e.g., FPG level, A1C level) for any abnormalities compared with baseline levels. Assess the prescriber’s order for insulin, so that the correct drug, route, type of insulin (i.e., rapid-acting, short-acting, intermediateacting, short- and intermediate-acting mixtures, long-acting), and dosage are implemented correctly. Assess the specific insulin, paying additional attention to the specific pharmacokinetics such as onset of action, peak, and duration of action. Make sure to know the patient’s history because type 2 diabetes can be treated with oral antidiabetic drugs, most of which require functioning beta cells in the pancreas. With sulfonylureas, it is important to know baseline glucose levels as well as conditions that may predispose the patient to hypoglycemia, such as a drop in caloric intake, alcohol Copyright © 2020 Elsevier Inc. All Rights Reserved. 153 use, or advanced age. Assessment of allergic reaction to sulfonamide antibiotics is important. Assess the patient for any signs and symptoms of hypoglycemia (e.g., acute onset of confusion, irritability, tremor, and sweating, with progression to possible hypothermia and seizures, and blood glucose level of less than 50 mg/dL) or of hyperglycemia (e.g., polyuria, polydipsia, polyphagia, glucosuria, weight loss, and fatigue, with a fasting blood glucose level of 126 mg/dL or higher or a nonfasting blood glucose level of 200 mg/dL or higher). Assessment is even more critical for a diabetic patient who is also under stress, has an infection or is ill, is pregnant or lactating, or is experiencing trauma or any serious change in health status. Always carefully check the exact timing of the dose of insulin or oral diabetes drug against the prescriber's order. Take into consideration the drug's pharmacokinetics, including onset, peak, and duration of action. All rapid-acting, short-acting, and long-acting insulin preparations are clear solutions. Intermediate-acting insulins are cloudy solutions. Mixtures of short- and intermediateacting insulins still look uniformly cloudy. Vials of insulin should be rolled in the hands instead of shaken when used. Administer insulins at room temperature. Insulin may be stored at room temperature if used within 1 month; otherwise, refrigeration is needed. Administer insulin subcutaneously at a 90-degree angle unless the patient is emaciated, in which case you may give the insulin at a 45-degree angle. Only regular insulin may be administered intravenously and is often used in intensive care settings. Only use insulin syringes for subcutaneous injections or when drawing up insulin dosage amounts. Oral antidiabetic drugs are usually given at least 30 minutes before meals, as ordered. Because the glitazones (e.g., rosiglitazone and pioglitazone) may both cause moderate weight gain and edema, weigh the patient daily at the same time every day and in the same clothing. When the patient is on nothing by mouth (NPO) status and is taking either an oral antidiabetic drug or insulin, it is crucial to follow the prescriber’s orders regarding drug administration. Complications associated with diabetes include retinopathy, neuropathy, nephropathy, hypertension, cardiovascular disease, and coronary artery disease. Annual screening with an ophthalmologist specializing in retinopathies is needed in the care of diabetic patients for screening purposes. Because of the renal complications (e.g., nephropathies), annual urinalysis screening is also recommended for diabetic patients. Nursing care must be individualized with patient education focused on the patient’s needs and learning abilities. Present information on all aspects of the disease process, drug therapy, and lifestyle modifications. Understanding new and different drugs and their pharmacokinetic properties allows you to help patients achieve better quality of life, minimize risks, and maximize wellness. Nursing care must be individualized with patient education focused on the patient's needs and learning abilities. Include pertinent and age-appropriate information on the disease process, drug therapy, and lifestyle modifications. Copyright © 2020 Elsevier Inc. All Rights Reserved. 154 REVIEW QUESTIONS1. Which is the most appropriate timing regarding the nurse’s administration of a rapid-acting insulin to a hospitalized patient? a. Give it 15 minutes before the patient begins a meal. b. Give it 12 hour before a meal.c. Give it 1 hour after a meal. d. The timing of the insulin injection does not matter with insulin lispro.2. Which statement is appropriate for the nurse to include in patient teaching regarding type 2 diabetes? a. “Insulin injections are never used with type 2 diabetes.” b. “You don’t need to measure your blood glucose levels because you are not taking insulin injections.”c. “A person with type 2 diabetes still has some functioning beta cells in his or her pancreas.”d. “Patients with type 2 diabetes usually have better control over their diabetes than those with type 1 diabetes.”3. The nurse monitoring a patient for a therapeutic response to oral diabetes drugs will look for which of these? a. Fewer episodes of diabetic ketoacidosis (DKA) b. Weight loss of 5 pounds c. Hemoglobin A1C levels of less than 7% d. Glucose levels of 150 mg/dL4. A patient with type 2 diabetes is scheduled for magnetic resonance imaging (MRI) with contrast dye. The nurse reviews the orders and notices that the patient is receiving metformin (Glucophage). Which action by the nurse is appropriate? a. Proceed with the MRI as scheduled. b. Notify the radiology department that the patient is receiving metformin.c. Expect to hold the metformin the day of the test and for 48 hours after the test is performed.d. Call the prescriber regarding holding the metformin for 2 days before the MRI is performed.5. A patient with type 2 diabetes has a new prescription for repa-glinide (Prandin). After 1 week, she calls the office to ask what to do, because she keeps missing meals. “I work right through lunch sometimes, and I’m not sure whether I need to take it. What do I need to do?” What is the nurse’s best response?a. “You need to try not to skip meals, but if that happens, you will need to skip that dose of Prandin.”b. “We will probably need to change your prescription to insulin injections because you can’t eat meals on a regular basis.”c. “Go ahead and take the pill when you first remember that you missed it.”d. “Take both pills with the next meal, and try to eat a little extra to make up for what you missed at lunchtime.”6. When checking a patient’s fingerstick blood glucose level, the nurse obtains a reading of 42 mg/dL. The patient is awake but states he feels a bit “cloudyheaded.” After double-checking the patient’s glucose level and getting the same reading, which action by the nurse is most appropriate? a. Administer two packets of table sugar. b. Administer oral glucose in the form of a semisolid gel. c. Administer 50% dextrose IV push. d. Administer the morning dose of lispro insulin.7. A patient is taking metformin for Copyright © 2020 Elsevier Inc. All Rights Reserved. 155 new-onset type 2 diabetes mellitus. When reviewing potential adverse effects, the nurse will include information about: (Select all that apply.) a. Abdominal bloating b. Nausea c. Diarrhea d. Headache e. Weight gain f. Metallic taste8. A patient who has a new diagnosis of type 2 diabetes asks the nurse about a new insulin that can be inhaled. “Is there a reason I can’t take that drug?” Which conditions, if present in the patient, would be a concern? (Select all that apply.) a. Atrial fibrillation b. History of smoking c. Chronic lung disease d. Hypothyroidism e. Rheumatoid arthritis___________________________________________________________ _______ Chapter 36 KEY POINTSChapter 36 1. a, c; 2. c; 3. b; 4. c; 5. d; 6. b, c, d, f; 7. 15 mL; 8. a. • Otic drugs may include the following ingredients, either by themselves or mixed together (depending on the prescriber’s order): steroids, antibacterials, antifungals, antiinflammatories, and wax-emulsifying compounds. Many of the antiinfective drugs are combined with steroids (in solution) to take advantage of the additional antiinflammatory, antipruritic, and antiallergic drug effects of the steroids.• Some ear infections require additional drug therapy with systemic dosage forms of corticosteroids, antibiotics, anti-fungals, and antiinflammatory drugs, so remind the patient of oral and other dosage forms.• Some disorders of the ear are self-limiting to a degree, but appropriate treatment is important to prevent complications__________________________________________________________________ ___________________ Copyright © 2020 Elsevier Inc. All Rights Reserved. 156 REVIEW QUESTIONS 1. While teaching a patient about treatment of otitis media, the nurse should mention that untreated otitis media may lead to which condition? a. Mastoiditis b. Throat infections c. Fungal ear infection d. Decreased cerumen production 2. During a teaching session about eardrops, the patient tells the nurse, “I know why an antibiotic is in this medicine, but why is hydrocortisone in these eardrops?” What is the nurse’s best response? a. “The hydrocortisone will help to soften the cerumen.” b. “The hydrocortisone reduces itching and inflammation.” c. “The hydrocortisone also has antifungal effects.” d. “This medication helps to anesthetize the area to decrease pain.” 3. The nurse is assisting a nursing student who is about to administer eardrops. Which technique by the nursing student indicates a need for further instruction? (Select all that apply.) a. Warm the solution to 100°F (37.7°C) before using. b. Position the patient so that the affected ear is accessible. c. Massage the tragus before administering the eardrops. d. Gently insert a cotton ball into the outer ear canal after the drops are given.e. Have the patient lie in the same position for 5 minutes after the drops are given. 4. The nurse is discussing treatment of earwax buildup with a patient. Which statement about earwax emulsifiers is correct? a. These drugs are useful for treatment of ear infections. b. They loosen impacted cerumen so that it may be removed by irrigation. c. They are used to rinse out excessive earwax. d. They enhance the secretion of earwax. 5. During an examination, the nurse notes that a patient has a perforated tympanic membrane. There is an order for ciprofloxacin eardrops. Which is the nurse’s most appropriate action at this time? a. Give the medication as ordered. b. Check the patient’s hearing, and then give the drops. c. Hold the medication, and check with the prescriber. d. Administer the drops with a cotton wick. 6. The nurse is preparing to administer eardrops and finds that the bottle has been stored in the medication room refrigerator. Which is the nurse’s best action at this time? a. Remove the bottle from the refrigerator, and administer the drops.b. Heat the bottle for 5 seconds in the microwave oven before administering the drops.c. Let the bottle sit in a cup of hot water for 15 minutes before administering the drops.d. Remove the bottle from the refrigerator 1 hour before the drops are due to be given. 7. The nurse is preparing to administer carbamide peroxide (Debrox) to an adult patient with impacted cerumen. Which actions by the nurse are correct? (Select all that apply.) a. Have the patient lie on his or her side with the affected ear up.b. Chill the medication before administering it. Copyright © 2020 Elsevier Inc. All Rights Reserved. 157 c. Pull the pinna of the ear down and back. d. Pull the pinna of the ear up and back. e. Gently irrigate the ear with warm water to remove the softened earwax. 8. A child is in the clinic with a severe case of otitis media. Theprescriber has decided to treat it with an antibiotic, and the nurse anticipates that which antibiotic will be prescribed as a first-line drug for this condition? a. tetracycline b. penicillin c. amoxicillin d. ciprofloxacin Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 37: Respiratory Drugs Chapter 37 1. a; 2. a; 3. b, d, e; 4. c; 5. b; 6. a, c, e; 7. c; 8. 45 mL. Key Points Anatomy, Physiology, and Pathophysiology Overview The main function of the respiratory system is to deliver oxygen to, and remove carbon dioxide from, the cells of the body. The respiratory system consists of two divisions or tracts: the upper and lower respiratory tracts. The upper respiratory tract is composed of the structures that are located outside the chest cavity or thorax, including the nose, nasopharynx, oropharynx, laryngopharynx, and larynx. Copyright © 2020 Elsevier Inc. All Rights Reserved. 158 The lower respiratory tract is located almost entirely within the thorax and is composed of the trachea, all segments of the bronchial tree, and the lungs. The beta agonists stimulate beta1 and beta2 receptors. The beta2 agonists are specific for the lungs. Pathophysiology of Diseases of the Respiratory System Diseases that affect the upper respiratory tract (URT) include colds, rhinitis, and hay fever. The major diseases that impair the function of the LRT include asthma and chronic obstructive pulmonary disease (COPD), which used to be referred to as emphysema, and chronic bronchitis. All of these diseases have one feature in common: They all involve the obstruction of airflow through the airways. Bronchial asthma is defined as a recurrent and reversible shortness of breath and occurs when the airways of the lung become narrow as a result of bronchospasm, inflammation and edema of the bronchial mucosa, and the production of viscous mucus. Allergic asthma, or extrinsic asthma, is caused by a hypersensitivity to an allergen or allergens in the environment. Intrinsic, or idiopathic, asthma does not have a specific cause but certain factors have been noted to precipitate asthma attacks including respiratory infections, stress, and cold weather. An asthma attack may be prolonged and may not respond to typical drug therapy. This is a condition known as status asthmaticus and is considered a medical emergency. Chronic bronchitis is a continuous inflammation and low-grade infection of the bronchi. The inflammation in the bronchioles is responsible for most of the airflow obstruction. Chronic bronchitis is no longer used as a term, but is included into COPD. Emphysema is a condition in which the air spaces enlarge as a result of the destruction of the alveolar walls, caused by the effect of proteolytic enzymes released from leukocytes in response to alveolar inflammation. Emphysema is no longer used as a term, but is included into COPD. In the past, the treatment of asthma and other chronic obstructive pulmonary diseases (COPDs) was focused primarily on the use of drugs that cause the airways to dilate; now the focus has shifted from the bronchoconstriction component of the disease to the inflammatory component. Pharmacology Overview Bronchodilators Bronchodilators relax bronchial smooth muscle, which causes dilation of the bronchi and bronchioles that are narrowed as a result of the disease process. There are three classes of such drugs: beta-adrenergic agonists, anticholinergics, and xanthine derivatives. Beta-Adrenergic Agonists The beta-adrenergic agonists are commonly used during the acute phase of an asthmatic attack to quickly reduce airway constriction and restore airflow to normal. They are agonists, or stimulators, of the adrenergic receptors in the sympathetic nervous system. Short-acting beta agonist (SABA) inhalers include albuterol (e.g., Ventolin), levalbuterol (Xopenex), pirbuterol (Maxair), terbutaline (Brethine), and metaproterenol (Alupent). Copyright © 2020 Elsevier Inc. All Rights Reserved. 159 Long-acting beta agonist (LABA) inhalers include arformoterol (Brovana), formoterol (Foradil, Perforomist), and salmeterol (Serevent). The newest long-acting beta agonists are indacaterol (Arcapta Neohaler); vilanterol in conjunction with fluticasone (Breo Ellipta), olodaterol (Striverdi), and vilanterol in conjuction with the anticholingeric, umeclidinium (Anoro Ellipta). The term Ellipta refers to a new delivery system. Because the long-acting beta agonists (LABA) have a longer onset of action, they must never be used for acute treatment. Patients must be taught to use the short-acting beta agonist (SABA) as rescue treatment. Nonselective adrenergic drugs, such as epinephrine, stimulate the beta, beta1 (cardiac), and beta2 (respiratory) receptors. Nonselective beta-adrenergic drugs, such as metaproterenol, stimulate both beta1 and beta2 receptors. Selective beta2 drugs, such as albuterol, primarily stimulate the beta2 receptors. The primary therapeutic effect of the beta agonists is the prevention or relief of bronchospasm related to bronchial asthma, bronchitis, and other pulmonary diseases. However, they are also used for effects outside the respiratory system. Contraindications include known drug allergy, uncontrolled hypertension or cardiac dysrhythmias, and high risk of stroke. Mixed alpha/beta agonists produce the most adverse effects, including insomnia, restlessness, anorexia, cardiac stimulation, hyperglycemia, tremor, and vascular headache. The adverse effects of the nonselective beta agonists are limited to beta-adrenergic effects, including cardiac stimulation, tremor, anginal pain, and vascular headache. The beta2 drugs can cause hypertension and hypotension, vascular headaches, and tremor. Anticholinergics Anticholinergic drugs are used for maintenance and not for relief of acute bronchospasm and work by blocking the bronchoconstrictive effects of ACh. Two anticholinergic drugs are used in the treatment of COPD: ipratropium (Atrovent) and tiotropium (Spiriva). Anticholinergic drugs are used for maintenance and not for relief of acute bronchospasm and work by blocking the bronchoconstrictive effects of ACh. On the surface of the bronchial tree are receptors for acetylcholine (Ach), the neurotransmitter for the parasympathetic nervous system (PSNS). ACh binds to the ACh receptors on the surface of the bronchial tree, which results in bronchial constriction and narrowing of the airways. Anticholinergic drugs block these ACh receptors to prevent bronchoconstriction. This indirectly causes airway dilation. Anticholinergic agents also help reduce secretions in patients with COPD. Because their actions are slow and prolonged, anticholinergics are used for prevention of the bronchospasm associated with chronic bronchitis or emphysema. The only usual contraindication to the use of bronchial anticholinergic drugs is drug allergy, including allergy to atropine. In the past, an allergy to peanuts or soy was listed as a contraindication to ipratropium inhalers. This was related to the propellant used and the new HFA inhalers have eliminated the concern. Thus, there is no contraindication Copyright © 2020 Elsevier Inc. All Rights Reserved. 160 using ipratropium in patients with peanut or soy allergies. Caution is necessary in patients with acute narrow-angle glaucoma and prostate enlargement. The most commonly reported adverse effects of ipratropium and tiotropium therapy are related to the drugs’ anticholinergic effects and include dry mouth or throat, nasal congestion, heart palpitations, gastrointestinal (GI) distress, urinary retention, increased intraocular pressure, headache, coughing, and anxiety. Xanthine Derivatives Natural xanthines consist of the plant alkaloids caffeine, theobromine, and theophylline; theophylline and caffeine are used. Synthetic xanthines include aminophylline and dyphylline. Xanthines, such as theophylline, help to relax the smooth muscles of the bronchioles by inhibiting phosphodiesterase. Phosphodiesterase breaks down cAMP, which is needed to relax smooth muscles. Theophylline is metabolized to caffeine in the body, whereas aminophylline is metabolized to theophylline. Theophylline and other xanthines also stimulate the CNS but to a lesser degree than caffeine. This stimulation of the CNS has the beneficial effect of acting directly on the medullary respiratory center to enhance respiratory drive. Xanthines are used to dilate the airways in patients with asthma, chronic bronchitis, or emphysema. They may be used in mild to moderate cases of acute asthma and as an adjunct drug in the management of COPD. Xanthines are now deemphasized as treatment for milder asthma because of their greater potential for drug interactions and the greater interpatient variability in drug levels. Caffeine is used without prescription as a CNS stimulant or to promote alertness. The common adverse effects of the xanthine derivatives include nausea, vomiting, anorexia, and gastroesophageal reflux during sleep. Cardiac adverse effects include sinus tachycardia, extrasystole, palpitations, and ventricular dysrhythmias. Transient increased urination and hyperglycemia are other possible adverse effects. Nonbronchodilating Respiratory Drugs Other drugs are effective in suppressing the various underlying causes of some of the respiratory illnesses, including leukotriene receptor antagonists (montelukast, zafirlukast, and zileuton) and corticosteroids (beclomethasone, budesonide, dexamethasone, flunisolide, fluticasone, ciclesonide, and triamcinolone). Leukotriene Receptor Antagonists (LTRAs) In people with asthma, leukotrienes cause inflammation, bronchoconstriction, and mucus production. This in turn leads to coughing, wheezing, and shortness of breath. LTRAs prevent leukotrienes from attaching to receptors located on circulating immune cells as well as local immune cells within the lungs. This reduces inflammation in the lungs. The LTRAs montelukast, zafirlukast, and zileuton are used for the prophylaxis and longterm treatment and prevention of asthma in adults and children 12 years of age and older. Copyright © 2020 Elsevier Inc. All Rights Reserved. 161 These drugs are not meant for the management of acute asthmatic attacks. The LTRAs, such as zileuton and zafirlukast, are given orally. Adverse effects include headache, dizziness, insomnia, and dyspepsia. The most common adverse effects of zafirlukast include headache, nausea, and diarrhea. Both drugs may also lead to liver dysfunction. Corticosteroids Corticosteroids, also known as glucocorticoids, are either naturally occurring or synthetic drugs used in the treatment of pulmonary diseases for their antiinflammatory effects. Corticosteroids (e.g., beclomethasone, dexamethasone, flunisolide, triamcinolone) have many indications and work by stabilizing the membranes of cells that release harmful bronchoconstricting substances. The systemic corticosteroids most commonly used for respiratory illness include prednisone (oral) and methylprednisolone (intravenous or oral). They have the dual effects of reducing inflammation and enhancing the activity of beta agonists. Corticosteroids have also been shown to restore or increase the responsiveness of bronchial smooth muscle to beta-adrenergic receptor stimulation, which results in more pronounced stimulation of the beta2 receptors by beta agonist drugs such as albuterol. Symbicort, a newer inhaler consisting of the corticosteroid budesonide and the bronchodilator formoterol, is similar to Advair as is Dulera, which is a combination of formoterol and mometasone. The main undesirable effects of inhaled corticosteroids include pharyngeal irritation, coughing, dry mouth, and oral fungal infections. Instruct patients to rinse their mouths after use of an inhaled corticosteroid. With significant systemic absorption, which is most likely with high-dose intravenous or oral administration, corticosteroids can affect any of the organ systems in the body. When patients are switched to inhaled corticosteroids after receiving systemic corticosteroids, especially at high dosages for an extended period, adrenal suppression (Addisonian crisis) may occur when the systemically administered corticosteroid is not tapered slowly. Patient deaths have been reported due to adrenal gland failure in such cases when the switch is made quickly and the dosage of corticosteroids is not reduced gradually. There is evidence that bone growth is suppressed in children and adolescents taking corticosteroids. Phosphodiesterase-4 Inhibitor In 2011, the Food and Drug Administration (FDA) approved roflumilast (Daliresp), a selective inhibitor of the enzyme called phosphodiesterase type 4 (PDE4), indicated to prevent coughing and excess mucus from worsening and to decrease the frequency of life-threatening COPD exacerbations. It is not intended to treat acute bronchospasm. Commonly reported adverse effects include nausea, diarrhea, headache, insomnia, dizziness, weight loss, and psychiatric symptoms. The FDA requires a medication guide that informs patients of the potential risk of psychiatric adverse effects. Copyright © 2020 Elsevier Inc. All Rights Reserved. 162 Monoclonal Antibody Antiasthmatic Omalizumab (Xolair), mepolizumab (Nucala), and reslizumab (Cinqair) are the newest antiasthmatic medications. Omalizumab is a monoclonal antibody that selectively binds to the immunoglobulin IgE, which in turn limits the release of mediators of the allergic response. Mepolizumab and reslizumab are also monoclonal antibodies that are interleukin-5 receptor antagonists. Omalizumab is given by injection and has the potential for producing anaphylaxis. Patients receiving omalizumab must be monitored closely for hypersensitivity reactions. These drugs are indicated as an add-on therapy for the treatment of asthma. Patients receiving these monoclonal antibodies must be monitored closely for hypersensitivity reactions. Nursing Process The net drug effect of beta agonists, xanthine derivatives, anticholinergics, LTRAs, and corticosteroids is improved airflow in airway passages and increased oxygen supply. Assess for cautions, contraindications, and drug interactions before administering these drugs, including assessing the patient’s skin color, temperature, respiration rate, respiration depth and rhythm, breath sounds, blood pressure, and pulse rate. Determine if the patient is having problems with cough, dyspnea, orthopnea, or hypoxia, or has other signs or symptoms of respiratory distress. If a cough is present, assess its character, frequency, presence or absence of sputum, as well as the color of the sputum. Assess the patient for the presence of any of the following: sternal retractions, cyanosis, restlessness, activity intolerance, cardiac irregularities, palpations, hypertension, tachycardia, and use of accessory muscles to breathe, indicating significant respiratory compromise. Collect information about environmental allergies, such as to dust, mold, pollen, mildew, and seasonal allergies, as well as food allergies. Note the characteristics of any respiratory symptoms and any family history of respiratory diseases. Assess the patient’s intake of caffeine and use of over-the-counter (OTC) medications containing caffeine. The intake of caffeine is important because of its sympathomimetic effects and possible potentiation of adverse effects associated with albuterol and other beta agonists. With use of the nonselective adrenergic agonist drug EpiPen or EpiPen Jr AutoInjectors, assess for the main indication, which is emergency use with severe allergic reactions caused by allergens, exercise, and unknown triggers and for those who are at increased risk. For patients taking anticholinergics, include any history of heart palpitations, GI distress, benign prostatic hyperplasia and/or urinary retention, and glaucoma due to the adverse effects of the drugs, leading to potentiation of these conditions or symptoms. In patients taking xanthine derivatives, perform a careful cardiovascular assessment, noting heart rate, blood pressure, and history of cardiac disease, because of the adverse effects of sinus tachycardia and palpitations. GI reflux may also occur with these drugs, so perform an assessment for bowel patterns and pre-existing disease. Copyright © 2020 Elsevier Inc. All Rights Reserved. 163 With corticosteroids, perform a baseline assessment of vital signs, breath sounds, and heart sounds. Assessment for underlying adrenal disorders is important because of the adrenal suppression that occurs with the use of these medications. Some inhalation products use capsules and a device that pierces the capsules to allow the powdered medication to be inhaled with a special inhaler. Even though these capsules are packaged with inhaler devices, they closely resemble oral capsules. The FDA has received reports that the capsules have been taken orally by patients, resulting in adverse effects. The use of metered-dose inhalers (MDIs) requires coordination to inhale the medication correctly and to obtain approximately 10% of drug delivery to the lungs. If a second puff of the same drug is ordered, instruct the patient to wait 1 to 2 minutes between puffs. If a second inhaled drug is ordered, instruct the patient wait 2 to 5 minutes between the medications or as prescribed. Beta agonists must be taken exactly as prescribed because overdosage may be life threatening. Educate patients not to crush or chew oral sustained-release tablets and to take them with food to decrease GI upset. Encourage journaling to record peak flow levels, signs, and symptoms of the disease, any improvement, and the occurrence of adverse effects associated with therapy. For pediatric patients, use of systemic forms of corticosteroids is a concern, possibly leading to suppression of the hypothalamic-pituitary-adrenal axis and subsequent growth stunting. The therapeutic effects of any of the drugs used to improve the control of acute or chronic respiratory diseases and to treat or help prevent respiratory symptoms include the following: decreased dyspnea, wheezing, restlessness, and anxiety; improved respiratory patterns with return to normal rate and quality; improved oxygen saturation levels; improved activity tolerance and arterial blood gas levels; improved quality of life; and decreased severity and incidence of respiratory symptoms. REVIEW QUESTIONS- Chapter 371. A patient who has a history of asthma is experiencing an acute episode of shortness of breath and needs to take a medication for immediate relief. The nurse will choose which medication that is appropriate for this situation? a. A beta agonist, such as albuterol b. A leukotriene receptor antagonist, such as montelukast c. A corticosteroid, such as fluticasone d. An anticholinergic, such as ipratropium 2. After a nebulizer treatment with the beta agonist albuterol, the patient complains of feeling a little “shaky,” with slight tremors of the hands. The patient’s heart rate is 98 beats/min, increased from the pretreatment rate of 88 beats/min. The nurse knows that this reaction is which of these? a. An expected adverse effect of the medication. b. An allergic reaction to the medication. c. An indication that he has received an overdose of the medication.d. An idiosyncratic reaction to the medication. 3. A patient is receiving ipratropium via an inhaler. The nurse will assess the patient for which of these adverse effects? (Select all that apply.) a. CNS depression b. Dry mouth or throat Copyright © 2020 Elsevier Inc. All Rights Reserved. 164 c. Increased appetite d. Nasal congestion e. Headache 4. During a teaching session for a patient who will be receiving a new prescription for the LTRA montelukast (Singulair), the nurse will tell the patient that the drug has which therapeutic effect? a. Improves the respiratory drive b. Loosens and removes thickened secretions c. Reduces inflammation in the airway d. Stimulates immediate bronchodilation 5. After the patient takes a dose of an inhaled corticosteroid, such as fluticasone (Flovent), what is the most important action the patient needs to do next? a. Hold the breath for 60 seconds. b. Rinse out the mouth with water. c. Follow the corticosteroid with a bronchodilator inhaler, if ordered.d. Repeat the dose in 15 minutes if the patient feels short of breath. 6. The nurse is teaching a patient about the inhaler Advair (fluticasone/salmeterol). Which statements by the patient indicate a correct understanding of this medication? (Select all that apply.) a. “I will rinse my mouth with water after each dose.” b. “I need to use this inhaler whenever I feel short of breath, but not less than 4 hours between doses.”c. “This medication is taken twice a day, every 12 hours.” d. “I can take this inhaler if I get short of breath while exercising.”e. “I will call my doctor if I notice white patches inside my mouth. Copyright © 2020 Elsevier Inc. All Rights Reserved. 165 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 41: Antitubercular Drugs Chapter 41 1. b, c, f; 2. b; 3. a; 4. d; 5. d; 6. b, d, f; 7. 625 mg/dose, No, the maximum dose is 300 mg; 8. a. Key Points Anatomy, Physiology, and Pathophysiology Overview Pathophysiology of Tuberculosis Tuberculosis (TB) is the medical diagnosis for any infection caused by a bacterial species known as Mycobacterium. TB is most commonly characterized by granulomas in the lungs, nodular accumulations of inflammatory cells that are delimited (“walled off” with clear boundaries). There are two mycobacterial species that can cause TB: Mycobacterium tuberculosis (MTB) and Mycobacterium bovis. Infections caused by M. tuberculosis are the most common. MTB is an aerobic bacillus, a rod-shaped microorganism that requires a large supply of oxygen to grow and flourish (aerobic). This is why Mycobacterium infections most Copyright © 2020 Elsevier Inc. All Rights Reserved. 166 commonly affect the lungs. Other common sites of infection are the growing ends of bones and the brain. Tubercle bacilli (a common synonym for MTB) are transmitted from one of three sources: humans, cattle, or birds; bovine and avian transmission are much less common than human. Tubercle bacilli are conveyed in droplets expelled by infected people or animals during coughing or sneezing and then inhaled by the new host. MTB is a very slow-growing organism. Many of the antibiotics used to treat TB work by inhibiting growth rather than by directly killing the organism. Microorganisms that grow slowly are more difficult to kill because their cells are not as metabolically active as those of faster-growing organisms. Most bactericidal drugs work by disrupting critical cellular metabolic processes in the organism; therefore, the most drug-susceptible organisms are those with faster (not slower) metabolic activity. The first infectious episode is considered the primary TB infection; reinfection represents the more chronic form of the disease. TB does not develop in all exposed people. In 1992, there was a resurgence peak in the United States, but it has decreased every year since that time. The decline is attributed to intensified public health efforts aimed at preventing, diagnosing, and treating TB as well as HIV infection. However, the concern now focuses on the increasing number of multidrug-resistant tuberculosis (MDR-TB) cases. Members of racial and ethnic minority groups are at greater risk than white populations and account for two thirds of new cases. Asian and Hispanic immigrants are at particularly high risk, accounting for more than half of all U.S. cases of foreign-acquired TB. The prevalence and growth of TB continues to be greater in the larger global community; TB infects one third of the world’s population. It is currently second only to HIV infection in the number of deaths caused by a single infectious disease. MDR-TB is defined as TB that is resistant to both isoniazid and rifampin, according to the World Health Organization. Close contacts of patients need to be treated as well. Pharmacology Overview Antitubercular Drugs The drugs used to treat infections caused by all forms of Mycobacterium are called antitubercular drugs. They are categorized as primary or first-line drugs and secondary or second-line drugs. INH is a primary antitubercular drug and is the most widely used. It can be administered either as the sole drug in the prophylaxis of TB or in combination with other drugs. The 2016 American Thoracic Society/CDC treatment guidelines recommend the use of multiple medications because of the increasing presence of resistance. Key elements in the planning and implementation of effective therapy: o Drug-susceptibility tests are performed on the first Mycobacterium species that is isolated from a patient specimen (to prevent the development of MDR-TB). o Before the results of the susceptibility tests are known, the patient is started on a four-drug regimen consisting of isoniazid, rifampin, pyrazinamide (PZA), and Copyright © 2020 Elsevier Inc. All Rights Reserved. 167 ethambutol or streptomycin, which together are 95% effective in combating the infection. The use of multiple medications reduces drug resistance. o Once drug susceptibility results are available, the regimen is adjusted accordingly. Patient adherence to the prescribed drug regimen and any adverse effects of therapy need to be monitored closely; the incidence of both patient noncompliance and adverse effects is high. Treatment has been made difficult by two problems: patient nonadherence with therapy and the growing incidence of drug-resistant organisms. Bedaquiline (Sirturo) is the first drug approved in over 40 years with a new mechanism of action and is indicated for the treatment of multidrug-resistant TB. It inhibits mycobacterial ATP synthase. Side effects include headache, chest pain, nausea, and QT prolongation. It is classified as a pregnancy category B drug. Antitubercular drugs act on MTB by inhibiting protein synthesis, inhibiting cell wall synthesis, or various other mechanisms. The major effects of drug therapy include reduction of cough and, therefore, reduction of the infectiousness of the patient. This normally occurs within 2 weeks of the initiation of drug therapy, assuming that the patient’s TB strain is drug sensitive. In addition to their use as the initial treatment of TB, antitubercular drugs have also proved effective in the management of treatment failures and relapses. INH, one of the mainstays of treatment, is noted for causing pyridoxine deficiency and liver toxicity. It has a black box warning regarding possible hepatitis. Nursing Process Note any specific history of diagnoses or symptoms of TB, as well as the results of the patient’s last purified protein derivative or tuberculin skin test and the reaction at the site of the intradermal injection. Also review the most recent chest radiograph and results. Assess the results of liver function and kidney function studies because major liver and/or renal dysfunction are contraindications for antitubercular drugs. Because some drugs may lead to peripheral neuropathies, note baseline neurologic functioning before therapy. Assess hearing status, especially when streptomycin is to be used, because of its drugrelated ototoxicity. A gross eye examination is important due to the drug-induced adverse effect of visual disturbances and optic neuritis with isoniazid, levofloxacin, and ofloxacin and blindness with ethambutol. The likelihood of adverse reactions and toxicity is increased in elderly patients due to agerelated liver and kidney dysfunction. The safety of these drugs in children 13 years of age and younger has not been established. All antitubercular drugs are to be taken exactly as prescribed. Emphasize adherence to the therapeutic regimen and long-term dosing combined with healthy living practices. Emphasize that the entire prescription must be finished over the prescribed time and as ordered by a prescriber, even if the patient is feeling better. Antitubercular drugs may need to be taken with food to minimize gastrointestinal upset. Copyright © 2020 Elsevier Inc. All Rights Reserved. 168 Constantly monitor for any signs and symptoms of liver dysfunction such as fatigue, jaundice, nausea, vomiting, dark urine, and anorexia. Monitor uric acid levels during therapy, and advise the patient to report any symptoms of gout, such as hot, painful, or swollen joints of the big toe, knee, or ankle. Because many of the patients affected by tuberculosis may be from other countries and cultures, it is important to have a translator available. Cultural considerations associated with these drugs include the fact that when patients have active TB, thorough patient teaching of all family members is required, and some family members may need prophylactic therapy for up to 1 full year. Because some cultural practices include living in close-knit communities or close living quarters, this teaching is critical to ensure adequate prevention of the spread of this highly communicable disease. A therapeutic response to antitubercular therapy is manifested by a decrease in the symptoms of TB, such as cough and fever, and by weight gain. Therapeutic effects include resolution of pulmonary and extrapulmonary MTB infections. Monitor patients for the occurrence of adverse reactions to antitubercular drugs, such as hearing loss (ototoxicity); nephrotoxicity; seizure activity; altered vision; blindness; extreme gastrointestinal upset; fatigue; nausea; vomiting; fever; jaundice; numbness, tingling, or burning of the extremities; abdominal pain; and easy bruising. Vitamin B6 is needed to combat the peripheral neuropathy associated with isoniazid. Bedaquiline should be given with food since administration with food significantly increases absorption. Adverse effects of bedaquiline (Sirturo) include headache, chest pain, nausea, and prolongation of the QT interval. Because of the need for long-term therapy and possible treatment of family or those in close contact, further evaluation of these individuals is important during and after completion of therapy. Counsel women taking oral contraceptive therapy who are prescribed rifampin about switching to other forms of birth control, because of the ineffectiveness of oral contraception when rifampin is taken. Educate the patient about the importance of strict adherence to the drug regimen for improvement or cure of the condition. Provide instructions in written and oral formats about drug interactions and the need to avoid alcohol while taking any of these medications. REVIEW QUESTIONS- Chapter 41 1. The nurse is teaching a patient who is starting antitubercular therapy with rifabutin. Which adverse effects would the nurse expect to see? (Select all that apply.) a. Headache and neck pain b. GI tract disturbances c. Reddish brown urine d. Numbness or tingling of extremities e. Gynecomastia f. Neutropenia 2. During antitubercular therapy with isoniazid, a patient received another prescription for pyridoxine. Which statement by the nurse best explains the rationale for this second medication? a. “This vitamin will help to improve your energy levels.” Copyright © 2020 Elsevier Inc. All Rights Reserved. 169 b. “This vitamin helps to prevent neurologic adverse effects.” c. “This vitamin works to protect your heart from toxic effects.”d. “This vitamin helps to reduce gastrointestinal adverse effects.” 3. The nurse is counseling a woman who is beginning antitu-bercular therapy with rifampin. The patient also takes an oral contraceptive. Which statement by the nurse is most accurate regarding potential drug interactions? a. “You will need to switch to another form of birth control while you are taking the rifampin.”b. “Your birth control pills will remain effective while you are taking the rifampin.”c. “You will need to take a stronger dose of birth control pills while you are on the rifampin.”d. “You will need to abstain from sexual intercourse while on the rifampin to avoid pregnancy.” 4. When counseling a patient who has been newly diagnosed with TB, the nurse will make sure that the patient realizes that he or she is contagious during which time? a. During all phases of the illness. b. Any time up to 18 months after therapy begins.c. During the postictal phase of TB. d. During the initial period of the illness and its diagnosis. 5. While monitoring a patient, the nurse knows that a thera-peutic response to antitubercular drugs would be which of these? a. The patient states that he or she is feeling much better. b. The patient’s laboratory test results show a lower white blood cell count.c. The patient reports a decrease in cough and night sweats. d. There is a decrease in symptoms, along with improved chest x-ray and sputum culture results. 6. The nurse is monitoring for liver toxicity in a patient who has been receiving long-term isoniazid therapy. Manifestations of liver toxicity which of these? (Select all that apply.) a. Orange discoloration of sweat and tears. b. Darkened urine. c. Dizziness. d. Fatigue. e. Visual disturbances. f. Jaundice. 7. The order for isoniazid (INH) reads: “Give 5 mg/kg PO daily.” The patient weighs 275 pounds. What is the amount per dose? Is this a safe dose? 8. Bedaquiline (Sirturo) is prescribed for a patient, and the nurse is providing instructions to the patient about the medication. Which statement by the patient indicates a correct understand-ing of the instructions? a. “I will take this with food.” b. “I need to take this 1 hour before breakfast.” c. “I can stop this drug if the side effects bother me.” d. “It’s okay to have a glass of wine while taking this drug.” Copyright © 2020 Elsevier Inc. All Rights Reserved. 170 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 50: Acid-Controlling Drugs Chapter 50 1. d; 2. c; 3. b, e; 4. b; 5. a; 6. a, c; 7. 200 mL/hr; 8. c. Key Points One stomach condition requiring drug therapy is hyperacidity, or excessive acid production. Left untreated, hyperacidity can lead to serious conditions such as acid reflux, ulcer disease, esophageal damage, and even esophageal cancer. Anatomy, Physiology, and Disease Overview The stomach secretes many substances (hydrochloric acid, pepsinogen, mucus, bicarbonate, intrinsic factor, and prostaglandins). The gastric glands are highly specialized secretory glands composed of several different types of cells: parietal, chief, mucous, endocrine, and enterochromaffin. Parietal cells produce and secrete hydrochloric acid (HCl). They are the primary site of action for many of the drugs used to treat acid-related disorders. Chief cells secrete pepsinogen. Pepsinogen is a proenzyme (enzyme precursor) that becomes pepsin when activated by exposure to acid. Pepsin breaks down proteins and is therefore referred to as a proteolytic enzyme. Mucous cells are mucus-secreting cells that are also called surface epithelial cells. The secreted mucus serves as a protective coating against the digestive action of HCl and digestive enzymes. Copyright © 2020 Elsevier Inc. All Rights Reserved. 171 In acid-related disorders, there is an impairment of the balance among the substances secreted by the stomach. The most harmful of the acid-related diseases involve hypersecretion of acid and include peptic ulcer disease and esophageal cancer. The most common condition is mild to moderate hyperacidity. Hyperacidity is often associated with gastroesophageal reflux disease (GERD). This is the tendency of excessive and acidic stomach contents to back up, or reflux, into the lower (and even upper) esophagus. Over time, this condition can lead to more serious disorders such as erosive esophagitis and Barrett esophagus, a precancerous condition. HCl maintains the environment of the stomach at a pH of 1 to 4. This acidity aids in digestion and also serves as one of the body’s defenses against microbial infection via the gastrointestinal (GI) tract. Several substances stimulate HCl secretion by the parietal cells, such as food, caffeine, chocolate, and alcohol. In moderation, any of these is usually not problematic. Excessive consumption of large, fatty meals or alcohol, as well as emotional stress, may result in hyperproduction of HCl and lead to hypersecretory disorders such as peptic ulcer disease. Peptic ulcer disease is a general term for gastric or duodenal ulcers that involve digestion of the GI mucosa by the enzyme pepsin. Because the process of ulceration is driven by the proteolytic (protein breakdown) actions of pepsin together with the caustic effects of HCl, peptic ulcer disease and related problems are also referred to by the more general term acid-peptic disorders. Helicobacter pylori (H. pylori) is implicated in the pathophysiology of peptic ulcer disease. The prevalence of H. pylori as measured by serum antibody tests is approximately 40% to 60% for patients older than 60 but only 10% for those younger than 30 years of age. H. pylori is found in the GI tracts of roughly 90% of patients with duodenal ulcers and 70% of those with gastric ulcers. First-line therapy includes a 10- to 14-day course of a proton pump inhibitor and the antibiotics clarithromycin and either amoxicillin or metronidazole. Stress-related mucosal damage is an important issue for critically ill patients. Stress ulcer prophylaxis is used in almost all patients in intensive care units (ICUs) and some on general medical surgical units. GI lesions are common in ICU patients, especially in the 24 hours after admission. Factors include decreased blood flow, mucosal ischemia, hypoperfusion, and reperfusion injury. Guidelines suggest that all such patients receive either a histamine receptor–blocking drug or a proton pump inhibitor. Pharmacology Overview Antacids Antacids are basic compounds used to neutralize stomach acid. Most commonly they are nonprescription salts of aluminum, magnesium, calcium, and/or sodium. Many antacid preparations contain the antiflatulent drug simethicone, which reduces gas and bloating. Copyright © 2020 Elsevier Inc. All Rights Reserved. 172 Many aluminum- and calcium-based formulations also include magnesium, which not only contributes to the acid-neutralizing capacity but also counteracts the constipating effects of aluminum and calcium. Antacids work primarily by neutralizing gastric acidity. They do not prevent the overproduction of acid but instead help to neutralize acid secretions. It is also believed that antacids promote gastric mucosal defensive mechanisms, especially at lower dosages. The primary drug effect of antacids is the reduction of the symptoms associated with various acid-related disorders, such as pain and reflux. Antacids are indicated for the acute relief of symptoms associated with peptic ulcer, gastritis, gastric hyperacidity, and heartburn. Adverse effects of antacids are limited. Magnesium preparations, such as milk of magnesia, can cause diarrhea. Aluminum- and calcium-containing formulations can cause constipation. Magnesium-aluminum combination antacids are used to prevent the adverse effects of constipation and diarrhea. Some of the more serious concerns with antacids include acid rebound, hypercalcemia, milk-alkali syndrome, and metabolic alkalosis. Combination products containing both magnesium and aluminum may have fewer adverse effects than either type of antacid by itself. The net effect is a balancing of both adverse effects and fewer problems with altered bowel patterns. An adverse effect more common with the calcium-containing products is rebound hyperacidity, in which the patient has hyperacidity when antacid use is discontinued. Cautious use of antacids high in sodium is recommended in patients who have heart failure, hypertension, or other cardiac diseases or who require sodium restriction. Many drug interactions occur with the acid-controlling drugs due to alteration of oral dosage forms, and so other medications are to be avoided within 1 to 2 hours of taking an antacid. Antacids are sometimes to be avoided when other acid-controlling drugs are taken. Four basic mechanisms by which antacids cause interactions include adsorption of other drugs to antacids, which reduces the ability of the other drug to be absorbed into the body; chelation, which is the chemical inactivation of other drugs that produces insoluble complexes; increased stomach pH, which increases the absorption of basic drugs and decreases the absorption of acidic drugs; and increased urinary pH, which increases the excretion of acidic drugs and decreases the excretion of basic drugs. Significant patient harm may ensue when the quinolone antibiotics (ciprofloxacin, levofloxacin, moxifloxacin) are given with antacids. Some of the more serious concerns with antacids include acid rebound, hypercalcemia, milk-alkali syndrome, and metabolic alkalosis. H2 Receptor Antagonists H2 receptor antagonists, also known as H2RAs and H2 receptor blockers, are the prototypical acid-secretion antagonists. They are H2 blockers that bind to and block histamine receptors located on parietal cells. This blockade renders these cells less responsive to stimuli and thus decreases their acid secretion. Up to 90% inhibition of acid secretion can be achieved. Copyright © 2020 Elsevier Inc. All Rights Reserved. 173 The effect of reduced hydrogen ion secretion from the parietal cells results in an increase in the stomach pH and relief of symptoms associated with hyperacidity-related conditions. H2 receptor antagonists are used for GERD, peptic ulcer disease, and erosive esophagitis; adjunct therapy in the control of upper GI tract bleeding; and treatment of pathologic gastric hypersecretory conditions such as Zollinger-Ellison syndrome. The H2 receptor antagonists include the drugs cimetidine, ranitidine, famotidine, and nizatidine. Ranitidine (Zantac) has many fewer drug interactions compared to cimetidine and has become the most widely used H2 receptor antagonist. Cimetidine carries a higher risk of drug interactions than ranitidine, famotidine, and nizatidine, especially in elderly. Cimetidine binds enzymes of the hepatic cytochrome P450 microsomal oxidase system, liver enzymes that metabolize many different drugs. By inhibiting the metabolism of drugs metabolized via this pathway, it may raise the blood concentrations of certain drugs. All drugs in this class are available over the counter. Proton Pump Inhibitors Drugs used for the treatment of acid-related disorders are the proton pump inhibitors (PPIs). These include lansoprazole (Prevacid), omeprazole (Prilosec), rabeprazole (AcipHex), pantoprazole (Protonix), esomeprazole (Nexium), and dexlansoprazole (Dexilant). Zegerid is a combination of omeprazole and sodium bicarbonate. The PPIs bind directly to the hydrogen-potassium-ATPase pump mechanism and irreversibly inhibit the action of this enzyme, resulting in total blockage of hydrogen ion secretion. PPIs block the final step in the acid production pathway, the hydrogenpotassium-ATPase pump, and they block all acid secretion. PPIs are currently indicated as first-line therapy for erosive esophagitis, symptomatic GERD that is poorly responsive to other medical treatment such as therapy with H2 receptor antagonists, short-term treatment of active duodenal ulcers and active benign gastric ulcers, gastric hypersecretory conditions (e.g., Zollinger-Ellison syndrome), nonsteroidal antiinflammatory drug (NSAID)–induced ulcers, and for stress ulcer prophylaxis. All PPIs can be used in combination with antibiotics to treat H. pylori infections. When omeprazole is given with clopidogrel, there is some concern of a decrease in clopidogrel’s effectiveness due to the fact that clopidogrel is dependent on its conversion to an active metabolite by the CYP-450 enzyme system, specifically CYP2C19. PPIs are generally well tolerated. The U.S. Food and Drug Administration issued a warning in 2010 regarding long-term use of high-dose PPIs, which has been associated with Clostridium difficile infections; risk of wrist, hip, and spine fractures; and pneumonia. In 2011, depletion of magnesium was added to the warning. PPIs may increase serum levels of diazepam and phenytoin and there may be an increased chance of bleeding in patients who are taking both a PPI and warfarin. Miscellaneous Acid-Controlling Drugs Copyright © 2020 Elsevier Inc. All Rights Reserved. 174 There are a few other acid-controlling drugs that are unique in terms of their mechanisms and other features, including sucralfate, misoprostol, and simethicone. Sucralfate is used for the treatment of peptic ulcer disease and stress-related ulcers. It binds to tissue proteins in the eroded area and prevents exposure of the ulcerated area to stomach acid. Misoprostol (Cytotec) is a synthetic prostaglandin analog that inhibits gastric acid secretion and is used to prevent NSAID-related ulcers. Simethicone (Mylicon) is used to reduce the discomforts of gastric or intestinal gas (flatulence) and aid in its release via the mouth or rectum. Nursing Process Before an acid-controlling drug is given, perform a thorough patient assessment with attention to past and present medical history and with special focus on GI tract–related disorders and signs and symptoms of ulcer disease and GERD. Since acid-controlling drugs have many interactions, underscore the importance of obtaining a medication history about prescription drugs, over-the-counter drugs, and herbals. The high sodium content of various antacids may lead to exacerbation of cardiac problems, renal dysfunction, and fluid-electrolyte problems. With quinolone antibiotics, there may be serious harm if given with antacids because of a 50% reduction in antibiotic absorption. For patients using H2 receptor antagonist drugs, assess renal and liver function and level of consciousness. Elderly patients react to these drugs with more disorientation and confusion. Do not administer drugs such as cimetidine and famotidine simultaneously with antacids. Since there are documented concerns about the use of PPIs and development of osteoporosis, thoroughly assess patients for any history of this disorder. The use of simethicone and sucralfate requires assessment of the patient’s bowel patterns and bowel sounds and evaluation for abdominal distention and rigidity. When giving acid-controlling drugs, instruct the patient to thoroughly chew the chewable tablets and to thoroughly shake liquid forms. Antacids need to be given with at least 8 oz of water to enhance absorption, except for newer forms that are rapidly dissolving drugs. For all of these H2 receptor antagonists, monitor blood pressure readings as needed during intravenous infusion because of the risk of hypotension. Continue to monitor the patient for GI tract bleeding with the diagnosis of ulcers or GI irritation. Report any blood in the stools or the occurrence of black, tarry stools or hematemesis. With PPIs, give lansoprazole oral dosage forms as ordered and with fluids. Monitor for abdominal pain, distention, and abnormal bowel sounds. Always double-check the names and dosages of these drugs to ensure that they are not confused with similarly named drugs. Therapeutic response to the administration of antacids, H2 receptor antagonists, PPIs, and other related drugs includes the relief of symptoms associated with peptic ulcer, gastritis, esophagitis, gastric hyperacidity, or hiatal hernia (i.e., decrease in epigastric pain, fullness, and abdominal swelling). Copyright © 2020 Elsevier Inc. All Rights Reserved. 175 Adverse effects range from constipation or diarrhea to nausea, vomiting, abdominal pain, and hypotension. Milk-alkali syndrome, acid rebound, hypercalcemia, and metabolic alkalosis are known complications associated with the various antacids. Revies Questions- Chapter 50 A patient is taking simethicone for excessive flatus associated with diverticulitis. The nurse is teaching about the mechanism of action of simethicone. Which statement is correct? a. “It neutralizes gastric pH, thereby preventing gas.” b. “It buffers the effects of pepsin on the gastric wall.” c. “It decreases gastric acid secretion and thereby minimizes flatus.”d. “It causes mucus-coated gas bubbles to break into smaller ones.” 2. The nurse is evaluating the medication list of a patient who will be starting therapy with an H2of these drugs may cause an interaction? a. codeine b. penicillin c. phenytoin d. acetaminophen 3. Which is the correct action when the nurse is administering sucralfate? (Select all that apply.) a. Giving the drug with meals b. Giving the drug on an empty stomach c. Instructing the patient to restrict fluids d. Waiting 30 minutes before administering other drugs e. Giving other drugs 2 hours before giving the sulcrafate 4. A patient with a history of renal problems is asking for advice about which antacid he should use. The nurse will make which recommendation? a. “Patients with renal problems cannot use antacids.” b. “Aluminum-based antacids are the best choice for you.” c. “Calcium-based antacids are the best choice for you.” d. “Magnesium-based antacids are the best choice for you.” 5. A patient who is taking oral tetracycline complains of heartburn and requests an antacid. Which action by the nurse is correct?receptor antagonist. Whicha. Give the tetracycline, but delay the antacid for 1 to 2 hours.b. Give the antacid, but delay the tetracycline for at least 4 hours.c. Administer both medications together. d. Explain that the antacid cannot be given while the patient is taking the tetracycline. 6. When the nurse is administering a proton pump inhibitor (PPI), which actions by the nurse are correct? (Select all that apply.) a. Giving the PPI on an empty stomach b. Giving the PPI with meals Copyright © 2020 Elsevier Inc. All Rights Reserved. 176 c. Making sure the patient does not crush or chew the capsulesd. Instructing the patient to open the capsule and chew the contents for best absorptione. Administering the PPI only when the patient complains of heartburn 7. The order reads: “Give pantoprazole (Protonix) 40 mg in 100 mL normal saline IVPB once daily. Infuse over 30 minutes.” The infusion pump can only be programmed to deliver over 1 hour (mL per hour). The nurse will set the pump to deliver how many mL per hour for each IVPB dose? 8. The nurse is preparing to administer the first dose of miso-prostol (Cytotec) for a patient who has been diagnosed with a gastric ulcer. What condition would be a contraindication to this medication? a. Hypothyroidism b. Type 2 diabetes mellitus c. Pregnancy d. Hypertension Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 51: Bowel Disorder Drugs Copyright © 2020 Elsevier Inc. All Rights Reserved. 177 Chapter 51 1. c; 2. d; 3. b; 4. a; 5. b; 6. d; 7. a, c; 8. b. Key Points Anatomy, Physiology, and Pathophysiology Overview The key symptoms of gastrointestinal (GI) disease are abdominal pain, nausea and/or vomiting, and diarrhea. Diarrhea is a leading cause of morbidity and mortality in underdeveloped countries. Diarrhea is defined as the passage of stools with abnormally increased frequency, fluidity, and weight, or increased stool water excretion. Acute diarrhea refers to diarrhea of sudden onset in a previously healthy individual. It lasts from 3 days to 2 weeks and is self-limiting, resolving without sequelae. Causes of acute diarrhea include drugs, bacteria, viruses, nutritional factors, and protozoa. Chronic diarrhea lasts for longer than 3 to 4 weeks and is associated with recurrent passage of diarrheal stools, possible fever, nausea, vomiting, weight reduction, and chronic weakness. Causes of chronic diarrhea include tumors, acquired immunodeficiency syndrome, diabetes mellitus, hyperthyroidism, Addison’s disease, and irritable bowel syndrome. Treatment is aimed at stopping stool frequency, alleviating abdominal cramps, replenishing fluids and electrolytes, and ending weight loss and nutritional deficits from malabsorption. Fluid and electrolyte replacement is vital while a patient is experiencing diarrhea. Pharmacology Overview Antidiarrheals Copyright © 2020 Elsevier Inc. All Rights Reserved. 178 Drugs used to treat diarrhea are called antidiarrheal drugs. Based on the specific mechanism of action, they are divided into different groups: adsorbents, antimotility drugs, and probiotics (also known as intestinal flora modifiers and bacterial replacement drugs). Adsorbents work by coating the walls of the GI tract. They bind the causative bacteria or toxin to the adsorbent surface in the intestine to be eliminated from the body through stool. They may increase bleeding and cause constipation, dark stools, and black tongue. The adsorbent bismuth subsalicylate is a form of aspirin, or acetylsalicylic acid, and therefore it also has many of the same drug effects as aspirin. Activated charcoal not only is helpful in coating the walls of the GI tract and adsorbing bacteria but also is useful in cases of overdose because of its drug-binding properties. The antilipemic drugs colestipol and cholestyramine are anion exchange resins prescribed as antidiarrheal adsorbents and lipid-lowering drugs. Opiates are also used as antidiarrheals and help to decrease bowel motility and thus permit longer contact of intestinal contents with the absorptive surface of the bowel. A secondary effect that makes opiates beneficial in the treatment of diarrhea is reduction of the pain associated with diarrhea by relief of rectal spasms. Anticholinergic drugs work to slow peristalsis by reducing the rhythmic contractions and smooth muscle tone of the GI tract; they also have a drying effect and reduce gastric secretions. They are used in combination with adsorbents and opiates. Adverse effects include urinary retention, headache, confusion, dry skin, rash, and blurred vision. Probiotics are also used to manage diarrhea and consist of bacterial cultures of Lactobacillus. They reestablish normal intestinal flora destroyed by infection or antibiotics and suppress the growth of diarrhea-causing bacteria. Many drugs are absorbed from the intestines into the bloodstream, where they are delivered to their respective sites of action. A number of the antidiarrheals have the potential to alter this normal process by either increasing or decreasing the absorption of these other drugs. The therapeutic effects of the anticholinergic antidiarrheals can be decreased by coadministration with antacids. Amantadine, tricyclic antidepressants, monoamine oxidase inhibitors, opiates, and antihistamines, when given with anticholinergics, can result in increased anticholinergic effects. Anticholinergics work by decreasing GI peristalsis through their parasympathetic blocking effects. Adverse effects include urinary retention, headache, confusion, dry skin, rash, and blurred vision. The opiate antidiarrheals have additive central nervous system (CNS) depressant effects if they are given with CNS depressants, alcohol, opioids, sedative-hypnotics, antipsychotics, or skeletal muscle relaxants. Laxatives Laxatives are used for the treatment of constipation, which is defined as abnormally infrequent and difficult passage of feces through the lower GI tract. Drugs used to treat diarrhea include adsorbents, anticholinergics, opiates, and probiotics. Constipation is a symptom, not a disease; it is a disorder of movement through the colon and/or rectum that can be caused by a variety of diseases or drugs. Copyright © 2020 Elsevier Inc. All Rights Reserved. 179 Treatment of constipation is individualized, with consideration of the patient’s age, concerns, and expectations; duration and severity of constipation; and potential contributing factors. Treatment can be either surgical (in extreme cases) or nonsurgical. Nonsurgical treatments can be separated into three broad approaches: dietary (e.g., fiber supplementation), behavioral (e.g., increased physical activity), and pharmacologic. Laxatives are among the most misused over-the-counter (OTC) medications. Long-term and often inappropriate use of laxatives may result in laxative dependence, produce damage to the bowel, or lead to previously nonexistent intestinal problems. With the exception of the bulk-forming type, laxatives are not to be used for long periods. Laxatives may act by (1) affecting fecal consistency, (2) increasing fecal movement through the colon, and/or (3) facilitating defecation through the rectum. Bulk-forming laxatives are composed of water-retaining (hydrophilic) natural and synthetic cellulose derivatives. They act in a manner similar to that of the fiber naturally contained in the diet. They absorb water into the intestine, which increases bulk and distends the bowel to initiate reflex bowel activity, thus promoting a bowel movement. Emollient laxatives either directly lubricate the stool and the intestines, as with mineral oil, or act as fecal softeners. By lubricating the fecal material and the intestinal walls, lubricant emollient laxatives prevent water from moving out of the intestines, which softens and expands the stool. Stool softeners and bulk-forming drugs are often preferred to other drugs in the treatment of constipation because they are not as problematic with regard to fluid and electrolyte loss. Hyperosmotic laxatives (e.g., glycerin, lactulose, sorbitol, and polyethylene glycol) work by increasing fecal water content, which results in distention, increased peristalsis, and evacuation. Their site of action is limited to the large intestine. Saline laxatives consist of various magnesium or sodium salts that increase osmotic pressure and draw water into the colon, producing a watery stool, usually within 3 to 6 hours of ingestion. Stimulant laxatives stimulate nerves that innervate the intestines, resulting in increased peristalsis. Laxatives, especially osmotic medications, may cause fluid and electrolyte loss. Methylnatrexone (Relistor), alvimopan (Entereg), and naloxagol (Movantik) are a newer group of drugs that actually allow the bowels to function normally even with the continued use of opioids. Naloxegol is available orally and is indicated for opioidinduced constipation. It is generally reserved for those patients taking chronic opioid therapy. Some of the common uses of laxatives include facilitation of bowel movements in patients with inactive colon or anorectal disorders, reduction of ammonia absorption in hepatic encephalopathy (lactulose only), treatment of drug-induced constipation, treatment of constipation associated with pregnancy and/or the postobstetric period, treatment of constipation caused by reduced physical activity or poor dietary habits, removal of toxic substances from the body, facilitation of defecation in megacolon, and preparation for colonic diagnostic procedures or surgery. Copyright © 2020 Elsevier Inc. All Rights Reserved. 180 Use caution with laxatives in the presence of the following: acute surgical abdomen; appendicitis symptoms such as abdominal pain, nausea, and vomiting; fecal impaction (mineral oil enemas excepted); intestinal obstruction; and undiagnosed abdominal pain. Laxatives alter intestinal function; therefore, they can interact with other drugs because many drugs are absorbed in the intestines. Drugs for Irritable Bowel Syndrome Irritable bowel syndrome (IBS) is a condition of chronic intestinal discomfort characterized by cramps, diarrhea, and/or constipation. Patients usually cope with the symptoms by avoiding irritating foods and/or taking OTC laxatives and antidiarrheal drugs. Drugs used to treat IBS are divided into those used to treat IBS with diarrhea (IBS-D) and those used to treat IBS with constipation (IBS-C). There are three drugs specifically indicated for IBS-D; alosetron (Lotronex), rifaximin (Xifaxan), and eluxadoline (Viberzi). There are two drugs specifically indicated for the treatment of IBS-C; lubiprostone (Amitiza) and linacotide (Linzess). Psyllium is moderately effective in IBS. The antidiarrheal loperamide (Imodium A-D) is not more effective than placebo at reducing pain or bloating, but it is an effective agent for the treatment of diarrhea, reducing stool frequency, and improving stool consistency. The 5-hydroxytryptamine-3 receptor antagonist alosetron (Lotronex) is indicated for the treatment of severe, chronic, diarrhea-predominant IBS in women who have failed conventional therapy. The FDA has issued a black box warning regarding infrequent but serious GI adverse reactions including ischemic colitis. Rifaximin is an antibiotic that works by reducing or altering bacteria in the gut. It is only slightly absorbed and generally well tolerated. Eluxadoline is the newest drug for IBS-D. It is a mixed opioid receptor agonist which activates receptors in the nervous system that lessen bowel contractions, thus reducing abdominal pain and diarrhea. The 5-hydroxytryptamine-4 receptor agonist tegaserod (Zelnorm) and the chloride channel activator lubiprostone (Amitiza) are more effective than placebo. Tricyclic antidepressants and selective serotonin reuptake inhibitors are more effective than placebo at relieving IBS symptoms and appear to reduce abdominal pain. Drugs used for treatment of IBS are to be given with extreme caution due to the side effects. Nursing Process In the abdominal assessment, include auscultation of bowel sounds in all four quadrants after inspection of the entire abdomen but before percussion and palpation. When the frequency of bowel sounds ranges from 6 to 32 per minute, it is important to describe exactly what is heard and the amount of activity in each of the four quadrants. Terms such as high-pitched, low-pitched, gurgling, or tinkling may be used to describe the character of the sounds, whereas activity may be described as hypoactive (fewer than 6 sounds per minute), normoactive (between 6 and 32 sounds per minute), or hyperactive (more than the normal range). Copyright © 2020 Elsevier Inc. All Rights Reserved. 181 Older adult patients are more susceptible to fluid and electrolyte depletion associated with diarrhea; therefore, closely assess hydration status and age. In pediatric or adolescent patients, assess for eating disorders with use of laxatives. With hyperosmotic laxatives (e.g., polyethylene glycol, lactulose, sorbitol, glycerin), assess baseline fluid and electrolyte levels to identify any deficits prior to use. Patients taking drugs for IBS need additional assessment of liver functioning as well as assessment for any underlying cardiac disease. Do not use lubiprostone in patients with a known or suspected bowel obstruction. Document any changes in bowel patterns, weight, fluid volume, intake and output, as well as in the mucous membranes during and after treatment—whether for constipation or diarrhea. Bismuth subsalicylate is a salicylate-based product and is not to be taken with other salicylates to avoid the risk of toxicity. It is also to be avoided in pediatric patients, including teenagers, who are at risk for Reye’s syndrome. Bulk-forming laxatives such as methylcellulose must be taken with at least 8 oz or 1 full glass of liquid after the powder form has been thoroughly stirred into it. The fluid must be taken immediately because of a congealing effect that continues to harden with time. To avoid choking or swelling of the product in the throat or esophagus, the patient must swallow or receive the drug immediately upon stirring. The medication is never taken or administered in its dry form. Encourage the patient to try and keep a suppository in place by lying still on the left side for at least 15 to 30 minutes to allow the drug to dissolve for maximal effectiveness. Tegaserod, available under restricted guidelines, must be taken only for up to 4 to 6 weeks. Monitor for the serious cardio-cerebrovascular adverse effects with continual observation of complaints of chest pain, lightheadedness, and dizziness as well as frequent monitoring of vital signs and neurologic checks (e.g., level of consciousness, reflexes, pupils for reactivity and size, speech). Therapeutic responses to any of these medications include an improvement in the GIrelated signs and symptoms reported by the patient (e.g., decrease in diarrhea or constipation), return to normal bowel patterns with normal bowel sounds, and absence of abnormal findings on assessment of the abdomen and bowel patterns. Encourage patients to check and recheck dosage instructions before taking medication and to note any drug-food and drug-drug interactions. Alert patients to the abuse potential of laxatives and the problems associated with their misuse as well as laxative dependency issues. REVIEW QUESTIONS- Chapter 511. A patient is being prepared for a colonoscopy. The nurse expects which laxative to be used as preparation for this procedure? a. Methylcellulose b. Docusate sodium c. PEG-3350 d. Glycerin 2. The nurse is administering oral methylcellulose (Citrucel), keeping in mind that a major potential concern with this drug is which of these? a. Dehydration b. Tarry stools c. Renal calculi Copyright © 2020 Elsevier Inc. All Rights Reserved. 182 d. Esophageal obstruction 3. A 45-year-old woman has been diagnosed with irritable bowel syndrome (IBS) and will be taking linaclotide (Linzess). Which of these conditions that may be a contraindication to this drug will the nurse look for during the assessment? a. Constipation b. Bowel obstruction c. Renal calculi d. Anemia 4. When the nurse teaches a patient about taking bisacodyl tablets, which instruction is correct? a. “Take this medication on an empty stomach.” b. “Chew the tablet for quicker onset of action.” c. “Take this medication with juice or milk.” d. “If it upsets your stomach, take this medication with an antacid.” 5. A patient has been receiving long-term antibiotic therapy as part of treatment for an infected leg wound. He tells the nurse that he has had “spells of diarrhea” for the last week. Which medication is most appropriate for him at this time? a. bismuth subsalicylate b. L. acidophilusc. diphenoxylate with atropine d. codeine 6. A parent calls to ask about giving a medication for diarrhea to his child, 15 years of age, who is recovering from the flu. The nurse expects the prescriber to recommend which medication? a. bismuth subsalicylate (Pepto-Bismol) b. Lactobacillus GG (Culturelle) c. belladonna alkaloid/phenobarbital combination (Donnatal Elixir)d. loperamide (Imodium AD) 7. A patient has been instructed to use an over-the-counter (OTC) form of the bulk-forming laxative methylcellulose (Citrucel) to prevent constipation. The nurse will advise the patient of potential adverse effects, including which of these? (Select all that apply) a. Electrolyte imbalances b. Decreased absorption of vitamins c. Gas formation d. Darkened stools e. Discolored urine 8. A patient has been given a new prescription for alosetron (Lotronex), and the nurse is providing education about this medication. Which statement by the patient indicates a need for further education? a. “I will not take a double dose in the afternoon if I forget my morning dose.”b. “I should be seeing improvement within a few days.” c. “I will call my doctor if I experience severe constipation or bloody diarrhea.”d. “This drug will improve symptoms but won’t cure my IBS.” Copyright © 2020 Elsevier Inc. All Rights Reserved. 183 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 52: Antiemetic and Antinausea Drugs Chapter 52 1. b; 2. a; 3. b; 4. c, d; 5. d; 6. a, c, e; 7. 0.5 mL; 8. b, c, e. Copyright © 2020 Elsevier Inc. All Rights Reserved. 184 Key Points Anatomy, Physiology, and Pathophysiology Overview Nausea and vomiting are two gastrointestinal (GI) disorders that can be extremely unpleasant but also can lead to more serious complications if not treated promptly. Nausea is an unpleasant feeling that often precedes vomiting. If it does not subside spontaneously or is not relieved by medication, it can lead to vomiting. Vomiting, which is also called emesis, is the forcible emptying or expulsion of gastric and, occasionally, intestinal contents through the mouth. A variety of stimuli can induce nausea and vomiting, including foul odors or tastes, unpleasant sights, irritation of the stomach or intestines, and certain drugs (ipecac or antineoplastic drugs). Two specific types of nausea and vomiting, chemotherapy-induced and postoperative, produce much more intense symptoms and are treated much more aggressively than general nausea and vomiting. Pharmacology Overview Drugs used to relieve nausea and vomiting are called antiemetic drugs. Antiemetics help to control vomiting, or emesis, and are also useful in relieving or preventing nausea. Antiemetics are used to prevent motion sickness, reduce secretions before surgery, treat delayed gastric emptying, and prevent postoperative nausea and vomiting. Most of these drugs can cause drowsiness. All antiemetic drugs work at some site in the vomiting pathways. Copyright © 2020 Elsevier Inc. All Rights Reserved. 185 Anticholinergics work by blocking acetylcholinesterase (Ach) receptors in the vestibular nuclei and reticular formation, preventing areas in the brain from being activated by nauseous stimuli. Anticholinergics also tend to dry GI secretions and reduce smooth muscle spasms, effects that are often helpful in reducing acute GI symptoms, including nausea and vomiting. Antihistamines prevent cholinergic stimulation in both the vestibular and reticular systems. Nausea and vomiting occur when these systems are stimulated. Antihistamines work by blocking H1 receptors, which produces the same effect as the anticholinergics. Antidopaminergic drugs, although traditionally used for antipsychotic effects, also prevent nausea and vomiting by blocking dopamine receptors in the chemoreceptor trigger zone (CTZ). Many also have actions similar to those of anticholinergic drugs. They also calm the central nervous system. Aprepitant (Emend) is an antagonist of substance P–neurokinin 1 receptors in the brain. Studies show that aprepitant augments the antiemetic actions of both ondansetron and dexamethasone. This drug is specifically indicated for the prevention of nausea and vomiting associated with highly emetogenic cancer chemotherapy regimens. Rolapitant (Varubi) is the newest drug in this class. Prokinetic drugs, in particular metoclopramide, act as antiemetics by blocking dopamine receptors in the CTZ, which desensitizes the CTZ to impulses it receives from the GI tract. The primary action is to stimulate peristalsis in the GI tract. This enhances the emptying of stomach contents into the duodenum, as well as intestinal movements. The serotonin-blocking drugs (granisetron and ondansetron) work by blocking serotonin receptors located in the GI tract, CTZ, and vomiting center. They are most commonly used for the prevention of chemotherapy-induced nausea and vomiting. Dronabinol therapy is used to prevent chemotherapy-induced nausea and vomiting and is associated with postural hypotension. Tetrahydrocannabinol (THC), in a drug class by itself, is the major psychoactive substance in marijuana. Non-intoxicating doses in the form of the drug dronabinol (Marinol) are occasionally used as an antiemetic because of the drug’s inhibitory effects on the reticular formation, thalamus, and cerebral cortex. Dronabinol therapy is used to prevent chemotherapy-induced nausea and vomiting and is associated with postural hypotension. Most of the adverse effects of the antiemetics stem from their nonselective blockade of various receptors. The ultimate goals of antiemetic therapy are minimizing or preventing fluid and electrolyte disturbances and minimizing deterioration of the patient’s nutritional status. Two commonly used antiemetic drugs may have serious consequences for the patient if they are given via the wrong route. o Hydroxyzine (Vistaril) is an antihistamine-class antiemetic that is only to be given either by oral or intramuscular routes. o The oral and intramuscular routes are the preferred routes of administration for promethazine (Phenergan). The intravenous route is not the preferred route. If given intraarterially, severe tissue damage, possibly leading to amputation, may occur. Sedation is the most adverse common effect. Nursing Process Copyright © 2020 Elsevier Inc. All Rights Reserved. 186 Identify any factors precipitating nausea or vomiting; note any weight loss; measure baseline vital signs; assess intake and output; examine the skin and mucous membranes, noting turgor and color; and assess and document capillary refill (normal is less than 5 seconds). One very important concern to reemphasize with scopolamine, which is commonly administered in patch form to prevent motion sickness, is the contraindication to its use in patients with narrow-angle glaucoma. Use antihistamines cautiously in pediatric patients, who may have severe paradoxical reactions, and in older adult patients, who often develop agitation, mental confusion, hypotension, and even psychotic-type reactions in response to these drugs. Antidopaminergic drugs, such as promethazine, should be used only after cautious assessment for signs and symptoms of dehydration and electrolyte imbalance by evaluating skin turgor and examining the tongue for the presence of longitudinal furrows. The prokinetic drug (e.g., metoclopramide) is often reserved for the treatment of nausea and vomiting associated with antineoplastic drug therapy or radiation therapy and for the treatment of GI motility disturbances. Keep suppository dosage forms in their foil covering until use and, once the wrap is removed, you may moisten them with water or water-soluble lubricating gel before being inserted well into the rectum. Frequently monitor blood pressure in patients taking meclizine, especially if they are elderly. Do not give metoclopramide in combination with any other medications, such as phenothiazines, that would lead to exacerbation of extrapyramidal reactions. Report extrapyramidal reactions to the prescriber immediately. The development of tardive dyskinesia, an involuntary neurologic movement, has been associated with the long-term use of metoclopramide. Antiemetics are often given 30 to 60 minutes before a chemotherapy drug is administered (time may vary depending on the specific drug) and may also be given during the chemotherapeutic treatment. Caution patients taking antiemetic or antinausea drugs that drowsiness and hypotension may occur and to avoid driving and using heavy machinery while taking these medications. The therapeutic effects of antiemetic and antinausea drugs include a decrease in or elimination of nausea and vomiting, and avoidance or elimination of complications such as fluid and electrolyte imbalances and weight loss. Monitor the patient for adverse effects such as GI upset, drowsiness, lethargy, weakness, extrapyramidal reactions, and orthostatic hypotension during antiemetic therapy. Review Questions- Chapter 52 A nurse is providing patient teaching regarding scopol-amine transdermal patches (TransdermScōp) to a patient who is planning an ocean cruise. Which instruction is most appropriate? a. “Apply the patch the day before traveling.” b. “Apply the patch at least 4 hours before traveling.” c. “Apply the patch to the shoulder area.” Copyright © 2020 Elsevier Inc. All Rights Reserved. 187 d. “Apply the patch to the temple just above the ear.” 2. A middle-aged woman is experiencing severe vertigo associated with motion sickness. The nurse expects that this patient will receive which drug? a. meclizine (Antivert) b. prochlorperazine (Compazine) c. metoclopramide (Reglan) d. dronabinol (Marinol) 3. A patient is in the outpatient cancer center for his first round of chemotherapy. Which schedule does the nurse consider most appropriate in terms of timing for the intravenous antiemetic drug? a. Four hours before the chemotherapy begins b. Thirty to sixty minutes before the chemotherapy begins c. At the same time as the chemotherapy drugs are given d. At the first sign of nausea 4. In reviewing the various types of antinausea medications, the nurse recognizes that prokinetic drugs are also used for which condition(s)? (Select all that apply.) a. Motion sickness b. Vertigo c. Gastroesophageal reflux d. Delayed gastric emptying e. GI obstruction5. A patient who has been receiving chemotherapy tells the nurse that he has been searching the Internet for antinausea remedies and that he found a reference to a product called Emetrol (phosphorated carbohydrate solution). He wants to know if this drug would help him. What is the nurse’s best answer? a. “This may be a good remedy for you. Let’s talk to your prescriber.”b. “This drug is used only after other drugs have not worked.”c. “This drug is used only to treat severe nausea and vomiting caused by chemotherapy.”d. “This drug may not help the more severe nausea symptoms associated with chemotherapy.” 6. The nurse is preparing to administer dronabinol (Marinol) to a patient. Which statements about dronabinol therapy are true? (Select all that apply.) a. It is approved for nausea and vomiting related to cancer chemotherapy.b. It is approved for use with hyperemesis gravidarum (nausea and vomiting associated with pregnancy).c. It is approved to help stimulate the appetite in patients with nutritional wasting due to cancer or AIDS.d. It may cause extrapyramidal symptoms. e. It may cause drowsiness or euphoria. 7. The order reads: “Give promethazine (Phenergan) 12.5 mg IM q4hr prn nausea/vomiting.” The medication is available in 25-mg/mL vials. How many milliliters will the nurse draw up for this dose? 8. The nurse is reviewing the current medications for a patient who has a new prescription for aprepitant (Emend). Which of these medications may have an interaction with aprepitant? (Select all that apply.)a. digoxin b. warfarin c. Oral contraceptives d. Nonsteroidal antiinflammatory drugs e. Corticosteroids Copyright © 2020 Elsevier Inc. All Rights Reserved. 188 Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 57: Ophthalmic Drugs Chapter 57 1. d; 2. b; 3. c; 4. b, c; 5. a; 6. d; 7. a, c, e; 8. b Copyright © 2020 Elsevier Inc. All Rights Reserved. 189 Key Points Anatomy, Physiology, and Pathophysiology Overview The eye is the organ responsible for the sense of sight. The exposed anterior portion of the eye is covered by three layers: the protective external layer (cornea and sclera), a vascular middle layer known as the uvea (includes the choroid, iris, and ciliary body), and the internal layer, known as the retina. All of these layers are protected by the eyelid, which serves as an external protective tissue. Each eye is held in place and moved by six muscles that are controlled by cranial nerves. These muscles include the rectus and oblique muscles. There are four types of rectus muscles: inferior, superior, medial, and lateral. There are two types of oblique muscles: inferior and superior. Copyright © 2020 Elsevier Inc. All Rights Reserved. 190 Lacrimal Glands The lacrimal glands produce tears that bathe and cleanse the exposed anterior portion of the eye. Tears are composed of an isotonic, aqueous solution that contains an enzyme called lysozyme, which acts as an antibacterial to help prevent eye infections. Tears drain into the nasal cavity through the lacrimal ducts. Layers of the Eye The fibrous outer layer of the eye has two parts that are continuous with each other: the sclera and the cornea. The sclera is a tough, fibrous layer that protects and maintains the shape of the eye. The cornea is a nonvascular transparent portion of the outer layer that allows light to enter the eye. It obtains nutrition from the aqueous humor, the clear watery fluid that circulates in the anterior and posterior chambers of the eye. The vascular middle layer of the eye is composed of the iris (to the anterior), ciliary body, and choroid (to the posterior), collectively called the uvea. The iris gives color to the eye and has an adjustable opening in the center called the pupil. The main function of the iris is to regulate the amount of light that enters the eye by causing the size of the pupil to vary. Pupil size is controlled by the sphincter pupillae muscle and by a radial smooth muscle called the dilator muscle. Aqueous humor contributes, along with vitreous humor, to the intraocular pressure of the eye. The lens is the transparent crystalline structure of the eye, located behind the iris and the pupil. It has a biconvex shape and is held in place by ligaments attached to the ciliary muscle. The larger chamber behind the lens is filled with a jellylike fluid called the vitreous body. The lens is transparent to allow light to pass through easily. A loss of lens transparency results in a visual condition called a cataract. The elasticity of the lens enables it to change its shape and focusing power (accommodation), facilitated by the ciliary body. Paralysis of accommodation is called cycloplegia. Mydriatics are drugs that dilate the pupil (e.g., apraclonidine). Drugs that constrict the pupil are called miotics (e.g., acetylcholine, pilocarpine). Drugs that paralyze the ciliary body are called cycloplegics, but they also have mydriatic properties (e.g., atropine, cyclopentolate). The third and inner layer of the eye is a thin delicate layer known as the retina. It contains light-sensitive photoreceptors called rods and cones. The basic function of the retina is to receive the light image formed by the lens and to convert it into the neural signals that support vision. Pathophysiology of Glaucoma Glaucoma is a disorder of the eye caused by inhibition of the normal flow and drainage of aqueous humor, and treatment helps to reduce intraocular pressure either by increasing the drainage of aqueous humor or decreasing its production. Drugs that increase aqueous humor drainage are direct cholinergics, indirect cholinergics, sympathomimetics, and beta blockers. Two major types of glaucoma are angle-closure glaucoma and open-angle glaucoma. Copyright © 2020 Elsevier Inc. All Rights Reserved. 191 Glaucoma can be a primary illness or it can be secondary to another eye condition or injury (e.g., posttraumatic glaucoma). Congenital glaucoma can also occur in infants. Pharmacology Overview Medications used to treat disorders of the eye can be divided into several major drug groups: antiglaucoma drugs, antimicrobials, antiinflammatory drugs, topical anesthetics, diagnostic drugs, antiallergic drugs, and lubricants and moisturizers. Antiglaucoma Drugs Treatment of glaucoma involves reducing intraocular pressure by either increasing the drainage of aqueous humor or decreasing its production. Some drugs may do both. Drug classes used to reduce intraocular pressure include direct-acting cholinergics (also called miotics and parasympathomimetic drugs), indirect-acting cholinergics (also called miotics, cholinesterase inhibitors, and parasympathomimetic drugs), adrenergics (also called mydriatics and sympathomimetic drugs), antiadrenergics (beta blockers; also called sympatholytic drugs), carbonic anhydrase inhibitors, osmotic diuretics, and prostaglandin agonists. The newest class of drugs used to treat glaucoma is the prostaglandin agonists. The most commonly used drugs in this class include latanoprost (Xalatan), travoprost (Travatan-Z), bimatoprost (Lumigan), and tafluprost (Zioptan). Cholinergic Drugs (Miotics) Direct-acting cholinergics include acetylcholine, carbachol, and pilocarpine. Indirect-acting drugs, which are also called cholinesterase inhibitors, include echothiophate, the only available drug. Since the primary effect is pupillary constriction, or miosis, they are also commonly called miotics. Acetylcholine is the neurochemical mediator of nerve impulses in the parasympathetic nervous system, stimulating parasympathetic or cholinergic receptors resulting in several effects on the eye: miosis, vasodilation of blood vessels in and around the eye, contraction of ciliary muscles, drainage of aqueous humor, and reduced intraocular pressure. Ciliary muscle contraction promotes aqueous humor drainage by widening the space where the drainage occurs. Miosis promotes aqueous humor drainage by causing the iris to stretch, which also serves to widen this space. Direct- and indirect-acting miotics have effects similar to those of acetylcholine, but their actions are more prolonged. The direct- and indirect-acting miotics are used for treatment of open-angle glaucoma, angle-closure glaucoma, and convergent strabismus (“cross-eye”) and in ocular surgery. Most adverse effects from the use of cholinergics and cholinergic inhibitors are local and limited. Adverse effects are more likely with indirect-acting miotics because they are longer-lasting. Effects include blurred vision, drug-induced myopia (nearsightedness), and accommodative spasms. Sympathomimetics (Mydriatics) Copyright © 2020 Elsevier Inc. All Rights Reserved. 192 Sympathomimetic drugs are used for the treatment of glaucoma and ocular hypertension. These drugs include alpha receptor agonists brimonidine (Alphagan P) and apraclonidine (Iopidine), and alpha and beta receptor agonists epinephryl (Epinal) and dipivefrin (Propine). Sympathomimetic drugs mimic the neurotransmitters norepinephrine and epinephrine, stimulating dilator muscle contraction by alpha and/or beta receptor interaction resulting in mydriasis. Both epinephrine and dipivefrin are used to reduce elevated intraocular pressure in the treatment of chronic open-angle glaucoma, either as initial therapy or as long-term therapy. Increases in intraocular pressure during surgery are usually mediated via increased catecholamine stimulation. Adverse effects of the sympathomimetic mydriatics are primarily limited to temporary ocular effects and include burning, eye pain, and lacrimation. Beta-Adrenergic Blockers The antiglaucoma beta-adrenergic blockers that reduce intraocular pressure include the beta1-selective drugs betaxolol and levobetaxolol. The ophthalmic beta blockers reduce both elevated and normal intraocular pressure. They reduce intraocular pressure by reducing aqueous humor formation. Ophthalmic beta blockers are used to reduce elevated intraocular pressure in chronic open-angle glaucoma and ocular hypertension. They may also be used alone or in combination with a topical miotic, which may have an additive intraocular pressurelowering effect. Adverse effects of beta blockers include transient burning and discomfort, blurred vision, pain, photophobia, lacrimation, blepharitis, keratitis, and decreased corneal sensitivity. Carbonic Anhydrase Inhibitors Ophthalmic carbonic anhydrase inhibitors include brinzolamide (Azopt) and dorzolamide (Trusopt). These two drugs are available only in topical ophthalmic form. Both drugs are also sulfonamides and are chemically related to the sulfonamide antibiotics. They should be used with caution in patients who are allergic to sulfa antibiotics. Carbonic anhydrase inhibitors work by inhibiting the enzyme carbonic anhydrase, which results in decreased intraocular pressure by reduction of aqueous humor formation. Ocular carbonic anhydrase inhibitors are used primarily for management of glaucoma, both open-angle and angle-closure types, and may be used preoperatively to control intraocular pressure. Patients with sulfa allergies may develop cross-sensitivities to carbonic anhydrase inhibitors. Osmotic Diuretics Osmotic drugs may be administered either intravenously, orally, or topically to reduce intraocular pressure; glycerin and mannitol are most commonly used. Osmotic diuretics reduce ocular hypertension by causing the blood to become hypertonic, creating an osmotic gradient that pulls water from the aqueous and vitreous humors into the bloodstream, causing reduced volume of intraocular fluid and decreased intraocular pressure. Copyright © 2020 Elsevier Inc. All Rights Reserved. 193 Osmotic diuretics are used for acute glaucoma episodes and reduction of intraocular pressure before or after ocular surgery. Glycerin is used first; if unsuccessful, mannitol is tried. Osmotic diuretics are contraindicated with allergy, anuria, acute pulmonary edema, cardiac decompensation, and severe dehydration because they can worsen all of these conditions. The most frequent reactions to osmotic diuretics are nausea, vomiting, and headache. The most significant adverse effects are fluid and electrolyte imbalances. Prostaglandin Agonists The newest class of drugs used to treat glaucoma is the prostaglandin agonists, including latanoprost (Xalatan), travoprost (Travatan Z), and bimatoprost (Lumigan). Prostaglandins reduce intraocular pressure in glaucoma by increasing the outflow of aqueous humor between the uvea and sclera as well as through the trabecular meshwork. Prostaglandin agonists are well tolerated. Adverse effects include foreign body sensation, punctate epithelial keratopathy (dotted appearance of the cornea), stinging, conjunctival hyperemia, blurred vision, itching, and burning. Systemic effects occur infrequently. In some people with hazel, green, or bluish-brown eye color, eye color will turn permanently brown, even after the medication is discontinued. Concurrent administration of prostaglandin agonists with any other eye drops containing the preservative thimerosal may result in precipitation. Antimicrobials A variety of infections can occur in the eye; many are self-limiting. Topical antimicrobials used to treat ocular infections include antibacterial, antifungal, and antiviral drugs. Topical antimicrobials used to treat infections of the eye work to destroy the invading organism; actions are similar to those described for systemically administered drugs. Ocular antimicrobials are used for known or suspected infection with one or more specific microorganisms. Empirical treatment is based on clinical evaluation of presenting symptoms. The most common adverse effects of ocular antibiotics are local and transient inflammation, burning, stinging, urticaria, dermatitis, angioedema, and drug hypersensitivity. Concurrent use of antibiotics and corticosteroids may interact. Corticosteroids have immunosuppressive effects that may impede the therapeutic effects of ocular antimicrobials. A large proportion of the inflammatory diseases of the eye are caused by viruses, and many ocular antimicrobials are available to treat bacterial, viral, and fungal infections of the eye. Common infections include conjunctivitis, hordeolum, keratitis, uveitis, and endophthalmitis. Antiinflammatory Drugs A large proportion of the inflammatory diseases of the eye are caused by viruses, and many ocular antimicrobials are available to treat bacterial, viral, and fungal infections of Copyright © 2020 Elsevier Inc. All Rights Reserved. 194 the eye. Common ocular infections include conjunctivitis, hordeolum (sty), keratitis, uveitis, and endophthalmitis. Antiinflammatory ophthalmic drugs include corticosteroids and are used to inhibit inflammatory responses to mechanical forces, chemicals, and immunologic reactions. Antiinflammatory drugs used systemically may also be used ophthalmically to treat various ocular inflammatory disorders and ocular surgery-related pain and inflammation. These drugs include both nonsteroidal antiinflammatory drugs (NSAIDs) and corticosteroids. There are several NSAID eye drops, including bromfenac, ketorolac, flurbiprofen, and diclofenac, which can be used to decrease ocular inflammation following eye surgery or for seasonal conjunctivitis. Corticosteroids and NSAIDs are applied topically for symptomatic relief of many ophthalmic inflammatory conditions and may be used to treat corneal, conjunctival, and scleral injuries from chemical, radiation, or thermal burns or from penetration of foreign bodies during acute phases of the injury to prevent fibrosis and scarring, which result in visual impairment. The most common adverse effect of corticosteroids is transient burning or stinging. Extended use may result in cataracts, increased intraocular pressure, and optic nerve damage. Topical Anesthetics Topical anesthetics are used to prevent pain to the eye and are beneficial during surgery, ophthalmic examinations, and removal of foreign bodies. The two currently available topical anesthetics used for ophthalmic purposes are proparacaine and tetracaine. Application of topical anesthetic drugs results in local anesthesia in less than 30 seconds; they are used to produce ocular anesthesia for short corneal and conjunctival procedures. Adverse effects are rare with ophthalmic anesthetic drugs and are limited to local effects such as stinging, burning, redness, lacrimation, and blurred vision. Diagnostic Drugs Atropine sulfate solution and ointment are used as mydriatic and cycloplegic drugs. It is used to assist in eye examination or to treat uveal tract inflammatory states. Cyclopentolate solution (Cyclogyl) is used as a diagnostic mydriatic and cycloplegic drug. Fluorescein is a diagnostic dye used to identify corneal defects and foreign objects. Antiallergic Drugs Olopatadine (Patanol) is an ocular antihistamine used for allergic conjunctivitis (hay fever), which can be seasonal or nonseasonal. It works by competing at receptor sites for histamine, which produces ocular symptoms such as itching and tearing. Ocular antihistamines include azelastine (Optivar), emedastine (Emadine), ketotifen (Zaditor), and epinastine (Elestat). Cromolyn sodium (Crolom), an antiallergic drug that inhibits release of inflammationproducing mediators from sensitized inflammatory cells, is used to treat vernal keratoconjunctivitis. Copyright © 2020 Elsevier Inc. All Rights Reserved. 195 Tetrahydrozoline is an ocular decongestant, promoting vasoconstriction of blood vessels in and around the eye to reduce the edema associated with allergic and inflammatory processes. It is specifically indicated to control redness, burning, and other minor irritations. An array of products is available over the counter to provide lubrication or moisture for the eyes. This is helpful to patients with dry or otherwise irritated eyes. The newest drug approved for dry eyes is lifitegrast (Xiidra). Lifitegrast is the first in a new class called lymphocyte function-associated antigen 1 (LFA-1) antagonist. Nursing Process Document any redness, swelling, pain, excessive tearing, eye drainage or discharge, decrease in visual acuity, or other unusual symptoms. Focus the nursing history on past or present systemic disease processes and exposure to any chemicals that could be topical irritants to the eye, skin, or mucous membranes, including past or present occupational and environmental exposures. Always inspect the solution, and administer only clear, unexpired products (e.g., drops, ointments, solutions) to the eye. Administer all ophthalmic preparations exactly as ordered. Always apply into the conjunctival sac. Safe and accurate application or instillation technique also includes avoiding contact of the eyedropper or tube to the eye to prevent contamination of the drug. Applying pressure to the inner canthus after instillation of medication is needed to prevent or decrease systemic absorption and subsequent systemic adverse effects. With abrasion or injury to the eye and appropriate medications, patching the affected eye is used to prevent further injury resulting from loss of blink reflex due to topical anesthetic. Advise patients to report to the prescriber immediately any increase in symptoms, such as eye pain or drainage and fever. Therapeutic responses to miotics include decreased aqueous humor of the eye with resultant decreased intraocular pressure and signs, symptoms, and long-term effects of glaucoma. Beta-adrenergic blockers are therapeutic if intraocular pressure decreases. Adverse effects include weakness, eye irritation, rash, bradycardia, hypotension, and dysrhythmias. Therapeutic responses to antibiotic, antifungal, and antiviral ophthalmic drugs include elimination of infection or condition and complications and resolution of symptoms. Therapeutic responses to ophthalmic anesthetics include prevention/relief of pain. Adverse effects may include central nervous system (CNS) excitation (e.g., dizziness, tremors, restlessness, nervousness) if the drug is systemically absorbed. Antiinflammatory ophthalmic solutions result in a decrease in allergic reactions with a decrease in itching, tearing, redness, and eye discharge. Potential complications of these solutions include swelling of the conjunctiva (chemosis). Copyright © 2020 Elsevier Inc. All Rights Reserved. 196 Review QUESTIONS- Chapter 57 1. The nurse is providing patient teaching regarding scopol-amine transdermal patches (Transderm-Scōp) to a patient who is planning an ocean cruise. Which instruction is most appropriate? a. “Apply the patch the day before traveling.” b. “Apply the patch at least 4 hours before traveling.” c. “Apply the patch to the shoulder area.” d. “Apply the patch to the temple just above the ear.” 2. A middle-aged woman is experiencing severe vertigo associated with motion sickness. The nurse expects that this patient will receive which drug? a. meclizine (Antivert) b. prochlorperazine (Compazine) c. metoclopramide (Reglan) d. dronabinol (Marinol) 3. A patient is in the outpatient cancer center for his first round of chemotherapy. Which schedule does the nurse consider most appropriate in terms of timing for the intravenous antiemetic drug? a. Four hours before the chemotherapy begins b. Thirty to sixty minutes before the chemotherapy begins c. At the same time as the chemotherapy drugs are given d. At the first sign of nausea 4. In reviewing the various types of antinausea medications, the nurse recognizes that prokinetic drugs are also used for which condition(s)? (Select all that apply.) a. Motion sickness b. Vertigo c. Gastroesophageal reflux d. Delayed gastric emptying e. GI obstruction 5. A patient who has been receiving chemotherapy tells the nurse that he has been searching the Internet for antinausea remedies and that he found a reference to a product called Emetrol (phosphorated carbohydrate solution). He wants to know if this drug would help him. What is the nurse’s best answer? a. “This may be a good remedy for you. Let’s talk to your prescriber.”b. “This drug is used only after other drugs have not worked.”c. “This drug is used only to treat severe nausea and vomiting caused by chemotherapy.”d. “This drug may not help the more severe nausea symptoms associated with chemotherapy.” 6. The nurse is preparing to administer dronabinol (Marinol) to a patient. Which statements about dronabinol therapy are true? (Select all that apply.) a. It is approved for nausea and vomiting related to cancer chemotherapy.b. It is approved for use with hyperemesis gravidarum (nausea and vomiting associated with pregnancy).c. It is approved to help stimulate the appetite in patients with nutritional wasting due to cancer or AIDS.d. It may cause extrapyramidal symptoms. e. It may cause drowsiness or euphoria. 7. The order reads: “Give promethazine (Phenergan) 12.5 mg IM q4hr prn nausea/vomiting.” The medication is available in 25-mg/mL vials. How many milliliters will the nurse draw up for this dose? Copyright © 2020 Elsevier Inc. All Rights Reserved. 197 REVIEW QUESTIONS1. The ophthalmologist has given a patient a dose of ocular atropine drops before an eye examination. Which statement by the nurse accurately explains to the patient the reason for these drops? a. “These drops will cause the surface of your eye to become numb so that the doctor can do the examination.”b. “These drops are used to check for any possible foreign bodies or corneal defects that may be in your eye.”c. “These drops will reduce your tear production for the eye examination.”d. “These drops will cause your pupils to dilate, which makes the eye examination easier.” 2. When assessing a patient who is receiving a direct-acting cholinergic eyedrop as part of treatment for glaucoma, the nurse anticipates that the drug affects the pupil in which way? a. It causes mydriasis, or pupil dilation. b. It causes miosis, or pupil constriction. c. It changes the color of the pupil. d. It causes no change in pupil size. 3. During patient teaching regarding self-administration of ophthalmic drops, which statement by the nurse is correct? a. “Hold the eyedrops over the cornea, and squeeze out the drop.”b. “Apply pressure to the lacrimal duct area for 5 minutes after administration.”c. “Be sure to place the drop in the conjunctival sac of the lower eyelid.”d. “Squeeze your eyelid closed tightly after placing the drop into your eye.” 4. When the nurse is providing teaching about eye medications for glaucoma, the nurse tells the patient that miotics help glaucoma by which mechanism of action? (Select all that apply.) a. Decreasing intracranial pressure b. Decreasing intraocular pressure c. Enhancing aqueous humor drainage d. Increasing tear production e. Causing pupillary dilation 5. During the assessment of a glaucoma patient who has newly prescribed carbonic anhydrase inhibitor eyedrops, the nurse would report a history of which condition? a. Allergy to sulfa drugs b. Decreased renal function c. Diabetes mellitus d. Hypertension 6. The nurse is preparing to administer ketorolac (Acular) eyedrops. The patient asks, “Why am I getting these eyedrops?” What is the nurse’s correct response? a. “These drops will reduce the pressure inside your eye as part of treatment for glaucoma.”b. “These drops are for a bacterial eye infection.” c. “These drops will relieve your dry eyes.” d. “These drops work to reduce the inflammation in your eyes.” 7. A patient has undergone an eye procedure during which ophthalmic mydriatics and anesthetic drops were used. The nurse gives which instructions to the patient prior to discharge? (Select all that apply.) a. “Do not rub or touch the numb eye.” b. “You may reinsert your contact lenses before you leave.” c. “Be sure to wear sunglasses when you go outside.” d. “Your pupils will appear very tiny until the medication wears off.”e. “Report any increase in eye pain or drainage to the oph-thalmologist immediately.” Copyright © 2020 Elsevier Inc. All Rights Reserved. 198 8. The nurse is administering sympathomimetic ophthalmic drops. Which therapeutic drug effect will these drops have on the patient’s eyes? a. Miosis b. Reduced intraocular pressure c. Reduced inflammation d. Increased lubrication Lilley: Pharmacology and the Nursing Process, 9th Edition Chapter 58: Otic Drugs Chapter 58 1. a; 2. b; 3. a, c; 4. b; 5. a; 6. d; 7. a, d, e; 8. c. Copyright © 2020 Elsevier Inc. All Rights Reserved. 199 Key Points Anatomy, Physiology, and Pathophysiology Overview The ear is made up of four parts: the external, outer, middle, and inner ears. The external ear is composed of the pinna and the external auditory meatus or opening of the ear canal. The term outer ear refers primarily to the external auditory canal, the space between the external auditory meatus and the tympanic membrane. The middle ear is composed of the tympanic cavity, the space that begins with the tympanic membrane and ends with the oval window. The middle ear has three bony structures of the mastoid bone—the malleus (“hammer”), incus (“anvil”), and stapes (“stirrup”)—as well as the auditory or Eustachian tube. The inner ear includes the cochlea and semicircular canals. External ear disorders are generally the result of physical trauma to the ear and consist of lacerations or scrapes to the skin and localized infection of the hair follicles, which often causes the development of a boil. These tend to be self-limiting and heal with time. Copyright © 2020 Elsevier Inc. All Rights Reserved. 200 Other examples of external ear disorders are contact dermatitis, seborrhea, and psoriasis, as evidenced by itching, local redness, inflammation, weeping, or drainage. These conditions usually respond to the same topical medications used for any other local skin disorders. Symptoms such as drainage, pain, and dizziness are sometimes also the first signs of a more serious underlying condition (e.g., head trauma, meningitis) and warrant prompt medical evaluation. The most common disorders affecting the outer and middle ear are bacterial and fungal infections, inflammation, and earwax accumulation. Such disorders of the ear are selflimiting to a degree, but appropriate treatment is important to prevent complications to the ear and/or systemic complications, such as a decrease in or loss of hearing. If problems persist or are untreated, more serious problems such as hearing loss may result. Infections in the ear canal are otitis externa; those in the middle ear are otitis media (OM). OM is common in infancy/early childhood, often preceded by upper respiratory tract infection. In adults, otitis externa is more likely, involving the ear canal and/or external tympanic membrane. If the condition is left untreated, tinnitus (ringing in the ears), nausea, vertigo, mastoiditis, and even temporary or permanent hearing deficits may occur. In 2013, the American Academy of Pediatrics updated their clinical practice guidelines on acute OM, with more stringent diagnostic criteria. The guidelines recommend antibiotics for severe symptoms with unilateral or bilateral OM and for bilateral nonsevere OM. Patients with non-severe unilateral OM are either observed or can be placed on antibiotics. They also recommend that a pain assessment and pneumococcal and influenza vaccines be given. The guidelines no longer recommend prophylactic antibiotics. Pharmacology Overview Treatment of Ear Disorders Drugs that treat ear conditions are known as otic drugs, and most are used topically in the ear canal. There are usually no drug interactions. Adverse effects are rare; localized irritation may occur. Otic drugs may include the following ingredients, either by themselves or mixed together (depending on the prescriber’s order): steroids, antibacterials, antifungals, antiinflammatories, and wax-emulsifying compounds. Many of the antiinfective drugs are combined with steroids (in solution) to take advantage of the additional antiinflammatory, antipruritic, and antiallergic drug effects of the steroids. Some ear infections require additional drug therapy with systemic dosage forms of corticosteroids, antibiotics, antifungals, and antiinflammatory drugs, so remind the patient of oral and other dosage forms. Copyright © 2020 Elsevier Inc. All Rights Reserved. 201 Some disorders of the ear are self-limiting to a degree, but appropriate treatment is important to prevent complications to the ear and/or systemic complications. If left untreated, ear infections or disorders may lead to a decrease in or loss of hearing. Antibacterial and Antifungal Otic Drugs Cortisporin (and other brands) is a three-drug combination that includes hydrocortisone and two antimicrobials, neomycin (an aminoglycoside), and polymyxin B. Hydrocortisone is the corticosteroid most commonly used in otic drugs, although there is one preparation (Ciprodex) that contains ciprofloxacin and dexamethasone. The steroid component is for reduction of inflammation and itching associated with ear infections. All of these products are used for the treatment of bacterial otitis externa or OM caused by susceptible bacteria such as Staphylococcus aureus, Escherichia coli, Klebsiella species, and others. With some otic drugs, it is recommended to saturate a retrievable cotton or tissue wick and let this wick soak inside the ear canal, as a means of dosing the drug. Antifungal otic drugs are used primarily for otitis externa and may also have antibacterial and antiviral properties. Two commonly used preparations are Cortic and Acetasol HC. Cortic, also available as Otomar, Aero Otic HC, and Mediotic HC, is composed of hydrocortisone (a steroid), pramoxine (a local anesthetic), chloroxylenol (an antiseptic antifungal), propylene glycol diacetate (an emulsifying drug), and benzalkonium chloride (antiseptic preservative). Earwax Emulsifiers Wax, or cerumen, is a natural product of the ear and is normally produced by modified sweat glands in the auditory canal. It can build up and become impacted, which results in pain and partial temporary deafness. Emulsifying otic drugs (such as carbamide peroxide) loosen and help remove this wax. Earwax emulsifiers loosen impacted cerumen, which allows it to be flushed out of the ear canal through irrigation (with water). Nursing Process Before administering any of the otic preparations, assess baseline hearing or auditory status, if deemed appropriate, and document the findings. Single drugs and combination drug products are used to treat many ear conditions, and it is important to know the indications for and specific information about these drugs to ensure their safe use. Perforated eardrums are usually a contraindication to the use of otic drugs. Neomycin, polymyxin B, and hydrocortisone otic preparations are contraindicated in patients with a perforated eardrum. Ciprofloxacin and ofloxacin can be used with perforated eardrums. Instill eardrops only after the ear has been thoroughly cleansed, all cerumen (earwax) has been removed (by irrigation if necessary, or as ordered), and the dropper has been cleansed. Store eardrops, solutions, and ointments at room temperature before instillation. Administration of solutions that are too cold may cause a vestibular-type reaction with vomiting and dizziness. Copyright © 2020 Elsevier Inc. All Rights Reserved. 202 Gentle massage to the tragus area of the ear may also help to increase coverage of the medication after the solution is given. Therapeutic effects of otic drugs include less pain, redness, and swelling in the ear; a reduction in fever; and resolution of any other signs and symptoms associated with the ear disorder. Improvement in hearing may also be an anticipated therapeutic effect. Monitor the ear canal for the occurrence of rash and/or any signs of local irritation, such as redness and heat at the site. Evaluate the patient for adverse effects with each application or instillation, and report unusual appearance of the outer ear and ear canal immediately. The Institute for Safe Medication Practices has reported several instances of eardrops being used in the eyes, which may be related to the similarities between the words “otic” (meaning ear) and “optic” (meaning eye). Patients who receive eardrops in the eyes will immediately complain of burning and stinging; redness and swelling may develop later. REVIEW QUESTIONS Chapter 58 1. While teaching a patient about treatment of otitis media, the nurse should mention that untreated otitis media may lead to which condition? a. Mastoiditis b. Throat infections c. Fungal ear infection d. Decreased cerumen production 2. During a teaching session about eardrops, the patient tells the nurse, “I know why an antibiotic is in this medicine, but why is hydrocortisone in these eardrops?” What is the nurse’s best response? a. “The hydrocortisone will help to soften the cerumen.” b. “The hydrocortisone reduces itching and inflammation.” c. “The hydrocortisone also has antifungal effects.” d. “This medication helps to anesthetize the area to decrease pain.” 3. The nurse is assisting a nursing student who is about to administer eardrops. Which technique by the nursing student indicates a need for further instruction? (Select all that apply.) a. Warm the solution to 100°F (37.7°C) before using. b. Position the patient so that the affected ear is accessible. c. Massage the tragus before administering the eardrops. d. Gently insert a cotton ball into the outer ear canal after the drops are given.e. Have the patient lie in the same position for 5 minutes after the drops are given. 4. The nurse is discussing treatment of earwax buildup with a patient. Which statement about earwax emulsifiers is correct? a. These drugs are useful for treatment of ear infections. b. They loosen impacted cerumen so that it may be removed by irrigation hey are used to rinse out excessive earwax. c. They are used to rinse out excessive earwax. d. They enhance the secretion of earwax. 5. During an examination, the nurse notes that a patient has a perforated tympanic membrane. There is an order for cip-rofloxacin eardrops. Which is the nurse’s most appropriate action at this time? Copyright © 2020 Elsevier Inc. All Rights Reserved. 203 a. Give the medication as ordered. b. Check the patient’s hearing, and then give the drops. c. Hold the medication, and check with the prescriber. d. Administer the drops with a cotton wick. 6. The nurse is preparing to administer eardrops and finds that the bottle has been stored in the medication room refrigerator. Which is the nurse’s best action at this time? a. Remove the bottle from the refrigerator, and administer the drops.b. Heat the bottle for 5 seconds in the microwave oven before administering the drops.c. Let the bottle sit in a cup of hot water for 15 minutes before administering the drops.d. Remove the bottle from the refrigerator 1 hour before the drops are due to be given. 7. The nurse is preparing to administer carbamide peroxide (Debrox) to an adult patient with impacted cerumen. Which actions by the nurse are correct? (Select all that apply.) a. Have the patient lie on his or her side with the affected ear up.b. Chill the medication before administering it. c. Pull the pinna of the ear down and back. d. Pull the pinna of the ear up and back. e. Gently irrigate the ear with warm water to remove the softened earwax. 8. A child is in the clinic with a severe case of otitis media. Theprescriber has decided to treat it with an antibiotic, and the nurse anticipates that which antibiotic will be prescribed as a first-line drug for this condition? a. tetracycline b. penicillin c. amoxicillin d. ciprofloxacin https://eagleonline.hccs.edu/courses/185657/files/38637668/download Copyright © 2020 Elsevier Inc. All Rights Reserved. 204 Kelly & Kelly (n.d.) Retrieved from https://kellykellylaw.com/michigan-criminal-law/drugcharges/ Copyright © 2020 Elsevier Inc. All Rights Reserved.