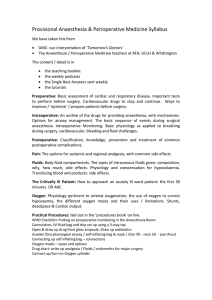
OCULAR ANAESTHESIA Chairperson: DR. RUBINA YASMIN ASSOCIATE PROFESSOR DEPT. OF ANAESTHESIOLOGY NIO&H Moderator: DR. KANIJUN NAHAR QUADIR ASSISTANT PROFESSOR DEPT. OF ANAESTHESIOLOGY NIO&H Presenter: DR. NAFIZ MAHMOOD DO STUDENT NIO&H ANAESTHESIA: Reversible loss of feeling or sensation, specially the loss of pain sensation induced to permit to performance of surgery or other painful procedures. From the page of History Karl Koller Born: Died: December 3, 1857 March 21, 1944 Nationality: Austria Fields: Ophthalmology Cocaine Known for: (a south american bush ERYTROXYLUM COCA.) as a local anaesthetic in 1884 Ophthalmic surgeon work in Vienna From the page of History Hermann Jakob Knapp Born: Died: March 17, 1832 April 30, 1911 In 1884 used cocaine for retrobulbar block. van Lint achieved orbicularis akinesia by local injection From the page of History General anaesthesia: First used by W.T.G Morton of Boston, US Used – ETHER at Massachusetts General Hospital on 16th October 1846 to Gilbert Abbott Types of ocular anaesthesia : General anaesthesia Local anaesthesia Topical Regional Peribulbar block Retrofbulbar block Parabulbar or sub-tenon block Intracameral block Facial block Frontal block PREFERRED ANAESHETIC TECHNIQUE LOCAL ANAESTHESIA: • • • • • • • • • Pterygium Cataract Surgery for glaucoma Minor extra-ocular plastic surgery Keratoplasty Dacryocystorhinostomy Minor anterior segment procedures Refractive surgey Vitreo-retinal surgery etc GENERAL ANAESTHESIA: • • • • • • Paediatric surgery Sqint surgery Major oculoplastic surgery Orbital trauma repair Dacryocystorhinostomy Vitreo-retinal surgery GENERAL ANAESTHESIA FOR OCULAR SURGERY INDICATION: 1. 2. 3. 4. In children and infant Anxious & uncooperative patient Mentally retarded adult Patient’s preference OBJECTIVE: 1. 2. 3. 4. Analgesia Amnesia Loss of consciousness Adequate skeletal muscle relaxation Advantages: I. safe operative environment II. Complete akinesia III. Controlled intra-ocular pressure IV. For bi-lateral surgery V. Avoiding complications of L/A PRE- ANAESTHETIC CHECKUP GENERAL: • Nutritional status • Retarded growth • Anaemia • Jaundice • Cough • Temperature • Oedema • History of convulsion RESPIRATORY SYSTEM : • Cyanosis • Dyspnoea • Auscultation of lung field AIRWAY: • Mouth opening • Neck movement • Dentition CARDIOVASCULAR SYSTEM : • Pulse • Blood pressure • Heart sound (auscultation) • Dependent oedema INVESTIGATIONS Full blood count Urine analysis Stool R/E Chest X-ray Over 40 years Blood glucose ECG Blood urea S.Creatinine Echocardiogram – specially for congenital heart disease (valvular disease) also for adult – if indicated OTHER INVESTIGATIONS: S. electrolytes Liver function test Coagulation screening Procedure of General Anaesthesia 1) Pre-medication for anaesthesia 2) Induction & intubation 3) Maintenance & Monitoring 4) Extubation and Recovery Drugs used in G/A 1. Pre-medication for anaesthesia with • Benzodiazepines (diazepam) –for sedation and reduce anxiety • Anti-emetics – metaclorpramide , ondansetron • Atropine - prevent bradycardia reduce bronchial and salivary secretion • Medication for selective patients - hypertensive , diabetic , coronary artery disease 2.Induction Thiopentone ( thiopental sodium) – 5 mg/kg Propofol – 2.5 mg/kg 3. Maintenance • Muscle relaxants – suxamethonium, vecuronium etc • anaesthetic gas – nitrous oxide (N2O) with O2 and Halothene , isoflurane etc. • Intravenous agent – pethidine , Fentanyl , NSAID (for pain reduction) 4. Recovery • Neostigmine • Atropine COMPLICATION of G/A • Hypoxia • Laryngospasm • Respiratory depression • Aspiration pneumonitis • Cardiac arrythmia • Hypotension / Hypertension • Convulsion • Restlessness EFFECTS OF ANAESTHETIC AGENTS ON IOP DRUGS INHALED ANAESTHETICS Volatile agents Nitrous oxide Intravenous agents Barbiturates Benzodiazepines Ketamine Opioids MUSCLE RELAXENT Depolarizers (succinylcholine) Non- depolarizers EFFECT ON IOP LOCAL ANAESTHESIA acts by producing reversible block to the transmission of peripheral nerve impulses ADVANTAGES: Patient is conscious and alert Drugs used in G/A can be avoided Systemic complication is less – Post-operative confusion Nausea , Vomiting Urinary retention Stress response to cardiac patient DISADVANTAGES: • Painful • Difficult in uncooperative patients NOT SUITABLE FOR: • Young patient • Mentally unstable patient • Patient with physical disabilities that prevent lying DESIRED PROPERTIES OF L/A 1. Non-irritating , safe and painless 2. Must be water soluable 3. Rapid onset of action 4. Duration of action appropriate to the operation to be performed 5. Non-toxic 6. No local after effects ( nerve damage , necrosis) 7. Must be effective regardless its application to tissue or mucous membrane 8. Quickly block motor and sensory nerves ACTION OF LA NERVE AXON MEMBRANE LOCAL ANAESTHESIA LAH+ (ionised drug) LA (free base) LA (free base) Na channel LAH+ (ionised drug) MECHANISM OF ACTION OF L/A Binds with protein of Na+ channels (at interior side) Block voltage dependent Na+ conductance ( prevent Na+ influx) Block depolarization Initiation and propagation of action potential fails Afferent impulses can not go to higher center No pain sensation Patient preparation for LA As for GA Optimal health condition Friendly rapport A suitable vein should always be cannulated in all patient Full cardio-pulmonary resuscitation equipment Appropriate monitoring Toxicity of LA: • Light headedness • Numbness or tingling of circumoral area • Anxious • Drowsy • Tinnitus • Convulsion ( To prevent- Diazepam or TPS) • Coma & apnoea develop subsequently (O2) • Cardiovascular collapse may result due to myocardial depression & vasodilatation HYPOXAEMIA APNOEA Types of LA According to chemical structure Ester group Amide group Procaine Cocaine Tetracaine benzocaine Lidocaine Bupivacaine Ropivacaine mepivacaine Esters may cause more allergies COMMONLY USED L/A L/A Oxybuprocaine Onset of action 6-20 sec Duration of action 15 min Use Topical (0.4%) 5-10 min 30-60 min Infiltration (concentration) (1%,2%,4%) Lignocaine Bupivacaine 10- 35 sec 15-20 min Topical (4%) Moderate 75-90 min Infiltration (0.25- 0.75%) OTHERS L/A Onset of action Duration of action Use (concentration) Proparacaine 15-30 sec 15-20 min Topical (0.5%) Amethocaine 10-25 sec 10-20 min Topical (0.5-1%) Ropivacaine Moderate 1.5-6hrs Infiltration (1%) TOPICAL ANAESTHESIA ADVANTAGES: Cost effective Immediate visual recovery Avoidance of complication - globe rupture , nerve damage DISADVANTAGES: No akinesia Not suitable for extended surgery Well informed and motivated patient is required ADVERSE EFFECT OF TOPICAL ANAESTHESIA • Epithelial and Endothelial toxicity • Allergy to drug • Alteration of lacrimation • Surface keratopathy USES OF TOPICAL ANAESTHESIA • Manipulation of superficial cornea and conjunctiva • Phacoemulsification in cooperative patient • Prior to regional blocks PERIBULBAR BLOCK Most popular now a days AIM: Injected into peribulbar space Spreads to lid and other spaces Produces globe and orbicularis akinesia and anaesthesia. L/A agent : o Lignocaine 2% o Bupivacaine 0.75% Along with o Hyaluronidase 5-7.5 IU/ml o Adranaline 1: 200,000 VOLUME : 8-10 ml (approximately) INSERTION POINT: • 1st - Junction of medial 2/3rd and lateral 1/3rd of lower lid adjacent & Parallel to orbital floor • 2nd - Just infero-medial to supra orbital notch or just medial to medial canthus POSITION OF PATIENT: Supine and in primary gaze USE OF PERIBULBAR BLOCK 1. Cataract 2. Glaucoma 3. Keratoplasty 4. Vitreoretinal surgery 5. Strabismus surgery ADVANTAGES: • Less chance of globe injury • Less chance of optic nerve damage DISADVANTAGES: • Pain • Conjunctival chemosis • Less akinesia than retrobulbar block RETROBULBAR BLOCK AIM: Injected in muscle cone to block • Cilliar nerve and ganglion • 3rd , 4th & 6th cranial nerves • provides - akinesia and anaesthesia of the globe. POSITION OF PATIENT : Supine and in primary gaze SITE OF INJECTION : In the lower lid margin just above a point between medial 2/3rd & lateral 1/3rd of lower orbital margin DIRECTION OF NEEDLE : backward , upwards and medially towards apex of orbit VOLUME: 2 – 4 ml usually ADVANTAGES: • Complete akinesia • Dilatation of pupil • Adequate and quicker anaesthesia • Minimal amount of agent required Complications : Retrobulbar haemorrhage Globe penetration Optic nerve sheath injury Optic nerve atrophy Decrease visual acuity Retinal vascular occlusion Cont… Brain stem anaesthesia Frank convulsion Extra ocular muscle palsy Trigeminal nerve block Oculo-cardiac reflex Respiratory arrest Contraindication : • Bleeding disorder ( risk of retrobulbar haemorrhage) • Extreme myopia ( globe perforation) • An open eye injury (may cause expulsion of intraocular contents) • Posterior staphyloma PARABULBAR OR SUB-TENON BLOCK DRUG : LIGNOCAINE Conjunctival incision 2-3 mm Halfway between inf. limbus & fornix to open sub-tenon space Blunt canulla or needle is inserted to post. Sub-tenon space Bathing the nerves & muscles within the cone Infiltration Dissection ADVANTAGES: • Avoid vascular and optic nerve injury • Requires lower volume of anaesthetics • Better anaesthesia to iris and ant.segment DISADVANTAGES: • Subconjunctival haemorrhage • More post-operative morbidity FRONTAL BLOCK AIM: to block supra-orbital and supra-trochlear nerve supplying the upper lid. USE: ptosis surgery SITE OF INSERTION: just below mid-point of supra- orbital margin transcutaneously directed towards roof of orbit VOLUME: about 2 mlw INTRACAMERAL ANAESTHESIA AGENT: lignocain 1% (without preservative or adrenaline) USE: used for phacoemulsification FACIAL BLOCK AIM: blocking the action of orbicularis oculi. USE : as an adjunct to retrobulbar block. TYPES: 1. Van lint 2. O’Brien 3. Nadbath & Rehman 4. Atkinson Major sight and life-threatening complications A. Retrobulbar orbital haemorrhage SIGNS & SYMPTOMS • rapid intraorbital and intraocular pressure elevation • increasing proptosis • marked pain • ecchymoses in the eyelids • Chemosis • vision down to poor perception or no perception of light MANAGEMENT: Evaluation: Indirect ophthalmoscopy - for evidence of central retinal artery perfusion compromise. Immediate medical treatment: intravenous osmotic agents such as – • acetazolamide • mannitol Surgery: Surgical decompression such as - • Canthotomy, • Cantholysis • Orbital decompression B. Globe perforation: (Exceptionally soft eye ; myopic eye is more prone) • Occurred with retrobulbar and peribulbar anaesthesia • suspected if – marked pain during the delivery of local an aesthesia hypotony with inability to secure a stable globe - intraoperative signs of perforation reduced red reflex due to vitreous haemorrhage Serious sight threatening vitreoretinal complications may result **** seek the advice of a specialist vitreoretinal surgeon C. Nerve Injury Optic nerve may be damaged by: ●● direct trauma by needle ●● ischaemic damage from intrasheath injection or haemorrhage ●● pressure from retrobulbar haemorrhage ●● pressure from excess local anaesthetic injection into the retrobulbar space ●● excessive applied external pressure. NEED TO CARE : • avoiding deep injections into the orbit and • injecting with the eye in the primary position D. Brain stem anaesthesia Due to spread of local anaesthetic along the optic nerve sheath SYMPTOMS & SIGNS: • drowsiness • light-headedness • confusion • loss of verbal contact • cranial nerve palsies • convulsions • respiratory depression or respiratory arrest • cardiac arrest ONSET OF SYMPTOMS: within 10-20 mins of LA injection SYMPTOMS LASTS FOR: Hours E. Muscle palsy Diplopia and ptosis are common for 24–48 hours post-operatively when large volumes of long-acting local anaesthetics are used. If this persists or fails to recover, it may be due to muscle damage as a result of : • intramuscular injection of local anaesthetics • local anaesthetic myotoxicity • ischaemic contracture following haemorrhage/trauma F. Oculocardiac Reflex (Trigeminovagal reflex) Trigeminal nerve – afferent and vagal efferent pathway CAUSES: • Traction on extra-ocular muscle • Pressure on globe RESULT: Bradycardia Ventricular ectopy Ventricular fibrilation AFFERENT PATHWAY Impulses Long & short cilliary nerve Cilliary ganglion Trigeminal gasserian ganglion main trigeminal sensory nucleus in the floor of the 4th ventricle EFFERENT PATHWAY Cardiovascular center of medulla afferent LCN Vagus nerve Heart SCN CG TGG VN efferent Treatment • Stop the surgical stimulus immediately. • Ensure adequate ventilation . • Ensure sufficient anesthetic depth. Atropine / Glycopyrrolate (anti-cholinergic): often helpful immediately or prior surgery TAKE HOME MESSAGES • All local anaesthetic agents are myotoxic • Direct injection into a muscle should be avoided • No LA technique is entirely free of severe systemic adverse events • short, fine needle should be used • the eye in the primary gaze position (looking straight ahead) • Gentle aspiration after insertion of needle should be done to alleviate possible entry to blood vessel. • Bevel of the needle facing the globe and tangenital to sclera. • All occular surgery with LA should be treated as GA.