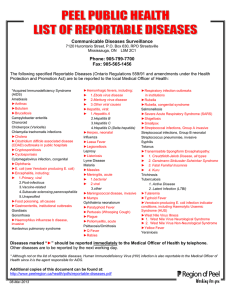
Family Nurse Practitioner Examination Certification Review Copyright © 2017 Edifying Publishing All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior permission of Edifying Publishing. Edifying Publishing 137-40 Laurelton Parkway Rosedale, NY 11422 ISBN: 978-0-9988163-0-2 (print book) e-book ISBN: 978-0-9988163-1-9 Library of Congress Control Number: 2017905673 The author and the publisher of this work have made every effort to use sources believed to be reliable to provide information that is accurate and compatible with standards generally accepted at the time of publication. However, medical science and the recommendations of healthcare agencies and associations can change at any moment. Therefore, a reader of this book should always be aware of current medical research, as well as new guidelines and recommendations by authoritative agencies. Special discounts on bulk quantities of our books are available to corporations, professional associations, healthcare organizations, and other qualifying groups. For details, please contact Edifying Publishing at: E-mail: contact@npreviewbook.com Preface This is a review book for the Family Nurse Practitioner Certification Examination that is offered by either the American Nurses Credentialing Center (ANCC) or the American Academy of Nurse Practitioners Certification Board (AANPCB). This book contains thousands of practice review questions, as well as images and reference charts, to help you learn the material needed to pass the FNP certification examination and become a certified Family Nurse Practitioner. This book has been created to be as streamlined as possible to contain only information on the FNP syllabus, without any, or much, extraneous information, to prevent you from studying material that is unlikely to be on the exam. Even though we believe this to be a good study guide for the FNP examination, we do not recommend that you use only one book for any test preparation. No one study guide will contain all of the information that will appear on the exam. Use as many professional study guides as you can manage in the time that you have allotted before you take the test. There are other great FNP certification examination study guides currently on the market. We recommend that you use at least 2-3 other study guides for the test to get a well-rounded, well-versed review for the test. The official website for this book is www.npreviewbook.com. All effort has been made to ensure that this book is as accurate as possible and contains no errors, but errors may still exist. If any errata are found for this book, they will be listed at www.npreviewbook.com/Errata. If you see any errors or inconsistencies, please email contact@npreviewbook.com so that the quality of this book can be improved; this will be much appreciated. About the Author David Hylton is a board-certified family nurse practitioner who wrote this book in collaboration with a nurse practitioner and a medical doctor. Contributors/Reviewers NP Crystal Rogers, RN, MSN, ANP Internal Medicine Hunter College New York MD Geuka Delva, M.D. Hospitalist of Internal Medicine American University of Antigua of Medicine New York/Antigua Table of Contents Chapter 1- About the Exam and Exam Tips Chapter 2- Pharmacology Pharmacology answers Chapter 3- Hematology and Lab Values Hematology and Lab Values answers Chapter 4- Integumentary and HEENT Integumentary and HEENT answers Chapter 5- Endocrine System Endocrine System answers Chapter 6- Gastrointestinal System Gastrointestinal System answers Chapter 7- Liver, Kidneys, Gallbladder, Appendix, Intestines, and Rectum Liver, Kidneys, Gallbladder, Appendix, the Intestines, and Rectum answers Chapter 8- Cardiology Cardiology answers Chapter 9- Musculoskeletal, Nerves & Vessels Musculoskeletal, Nerves, & Vessels answers Chapter 10- Respiratory System Respiratory System answers Chapter 11- Neurological System Neurological System answers Chapter 12- Oncology Oncology Answers Chapter 13- Maternity Maternity answers Chapter 14- Pediatrics Pediatrics answers Chapter 15- Men’s Health Men’s Health answers Chapter 16- Women’s Health Women’s Health answers Chapter 17- Sexual Health and STDs Sexual Health and STDs answers Chapter 18- Geriatrics Geriatrics answers Chapter 19- Psychiatry Psychiatry answers Chapter 20- Biochemical Attacks/Illicit Drugs/Accidents Biochemical Attacks/Illicit Drugs/Accidents answers Chapter 21- Health Promotion/Prevention Health Promotion/Prevention answers Chapter 22- Legal Aspects, Insurance, and Culture Legal Aspects, Insurance, and Culture answers Chapter 23- Statistics Statistics Answers Appendix Chapter 1- About the Exam and Exam Tips Who is eligible to take the exam? To qualify for the FNP certification examination, applicants must have completed an accredited NP program in the U.S. or an approved Canadian NP program. NP programs in the U.S. must be accredited by either the Commission on Collegiate Nursing Education (CCNE) or the Accreditation Commission for Education in Nursing, Inc. (ACEN) (formerly known as the NLNAC). Who are the certifying bodies for the Nurse Practitioner examination? The American Nurses Credentialing Center (ANCC) is the independent credentialing body of the American Nurses Association (ANA). It is the largest nurse credentialing organization in the United States. For more information about this credentialing body, visit their official website at www.nursecredentialing.org The American Academy of Nurse Practitioners Certification Board (AANPCB) was established under the direction of Dr. Jan Towers PhD, NP-C, CRNP, FAAN, FAANP in 1993. The AANPCB was established for the purpose of evaluation of individuals wishing to enter, continue, and/or advance in the NP profession through the certification process. AANPCB is a separately incorporated, nonprofit, independent organization overseen by a Commission composed of dedicated, knowledgeable, experienced, nurse practitioners representative of the certificants. The mission of the American Academy of Nurse Practitioners Certification Board is to provide excellence in testing and certification for nurse practitioners who adhere to and uphold the highest standards for Nurse Practitioners in the realm of certification. For more information about the AANPCB, visit their official website at http://www.aanpcert.org How many questions are on the FNP examination? For the test offered by the ANCC, each exam contains between 150 to 175 scored test items plus 25 pilot test items that do not count towards the final score. For the AANPCB exam, there are 150 questions. Of the 150 questions, 15 are pretest questions. A candidate’s score is based solely on the 135 scored questions. Pretest questions, or pilot questions, are questions developed during the process of Item Writing. Pretest questions are piloted on examinations to obtain statistical information for determining how well each question will perform prior to vetting them for use on the scored portion of an examination. Pretest questions are not distinguished from those that are scored. Performance on pretest questions does not affect the final score. What examination results are returned? For test scores, candidates view a Pass or Fail status on the computer upon completion of the examination. A preliminary report received of Pass at the testing site is not official notification, does not indicate active certification status, and may not be used for employment or licensure as an NP. A candidate's examination score is considered confidential information and will not be disclosed to anyone other than the candidate without specific written instructions from the candidate indicating to whom and why the information is to be disclosed. Results will not be given out by telephone, email, or fax. What happens if a person fails the exam? Candidates who do not pass the certification examination receive an official score letter indicating failure to pass with the score, areas of strength and areas of weakness. Candidates may apply to retake the examination after completion of a general review course or additional advanced practice continuing education. Topics to Know for the FNP Examination This isn’t an exhaustive list of all topics by subject for the FNP exam, but serves as a general indicator of topics and concepts that you should know and be familiar with. The questions in this book tests you on all these topics (and goes into more specifics). Pharmacology Alternative medicine Area Under the Curve (AUC) graph Cytochrome P450 enzymes Dipeptidyl peptidase-4 (DPP-4) inhibitors First-pass metabolism Half-life Minimum Inhibitory Concentration (MIC) Narrow Therapeutic Index (NTI) Hematology and Lab Values Alanine Transaminase (ALT) Ankle Brachial Index (ABI) Aspartate Transaminase (AST) Anisocytosis Aplastic anemia Alkaline phosphatase Bilirubin (conjugated and unconjugated) C-reactive protein (CRP) Creatinine clearance Creatine Kinase (CK) Erythrocyte Sedimentation Rate (ESR) Ferritin Gamma-glutamyl Transferase (GGT) Glucose-6-phosphate Dehydrogenase (G6PD) deficiency Hematocrit Hemoglobin Hemoglobin electrophoresis Iron-deficiency anemia Macrocytic/megaloblastic anemia Microcytic anemia Mean Corpuscular Volume (MCV) Mean Corpuscular Hemoglobin (MCH) Mean Corpuscular Hemoglobin Concentration (MCHC) Pernicious anemia Poikilocytosis Polycythemia Red Cell Distribution Width (RDW) Sickle cell anemia Thalassemia Total Iron Binding Capacity (TIBC) Integumentary and HEENT Acanthosis nigricans Acne Actinic keratosis Age-related macular degeneration (AMD) Allergic rhinitis Arcus senilis Blepharitis Burns (first degree, second degree, third degree) Cataracts Cellulitis Chalazion Cherry angioma Cholesteatoma Conjunctivitis Corneal ulcer Cutaneous larva migrans Dacryocystitis Dacryostenosis Dermatitis (atopic, contact, intertriginous, diaper, stasis) Diphtheria Ehlers-Danlos syndrome Ehrlichiosis Enterobiasis Erysipelas Erythema infectiosum Folliculitis Glaucoma (angle-closure, open-angle) Herpes keratitis Herpetic whitlow Hidradenitis suppurativa Hordeolum Hyperhidrosis Hyphema Impetigo (bullous, non-bullous) Lichen sclerosus Lipoma Lyme disease Lymphogranuloma venereum Melasma Meniere’s disease Molluscum contagiosum Mononucleosis Myringitis Nail disorders (onychomycosis, paronychia, koilonychia) Optic neuropathy Otitis infections (externa, media) Papilledema Peritonsillar abscess Pharyngitis Pinguecula Pityriasis rosea Pressure ulcers (stages) Psoriasis Pterygium Rheumatic fever Rocky Mountain Spotty Fever (RMSF) Rosacea Roseola Sarcoidosis Scabies Scarlet Fever Seborrheic dermatitis Seborrheic keratosis Sjögren’s Syndrome Stevens-Johnson syndrome (SJS) Strabismus (esotropia, exotropia, hypertropia, hypotropia) Strep throat Tinea infections (capitis, corporis, pedis, versicolor, etc.) Verruca vulgaris Vitiligo Xanthelasma Xerophthalmia Xerosis Endocrine System Diabetes Metabolic syndrome Addison’s disease Cushing’s disease Hyperthyroidism Hypothyroidism Gastrointestinal System Celiac disease Clostridium difficile colitis Diverticulosis (and diverticulitis) Dumping syndrome Esophageal spasms Gastritis Gastroenteritis Gastroesophageal Reflux Disease (GERD) Gastroparesis Inflammatory bowel disease (ulcerative colitis, Crohn’s disease) Irritable bowel syndrome (IBS) Pancreatitis Peritonitis Traveler’s diarrhea Ulcerative colitis Ulcers (gastric, duodenal) Zollinger-Ellison syndrome Liver, Kidneys, Gallbladder, Appendix, the Intestines, and Rectum Biliary colic Cirrhosis Fatty liver disease Hepatitis (A, B, C, D) Nephrolithiasis Polycystic kidney disease Pyelonephritis Renal artery stenosis Renal failure Cardiology Acute coronary syndrome Aortic dissection Arrhythmias (atrial fibrillation, ventricular fibrillation, etc.) Carotid sinus hypersensitivity Congestive heart failure Diastolic murmurs (mitral stenosis, aortic regurgitation) Hypertension Myocardial infarction Orthostatic hypotension Pulsus paradoxus Systolic murmurs (mitral regurgitation, aortic stenosis) Musculoskeletal, Nerves, & Vessels Ankylosing spondylitis Arthritis Bone spur Bursitis Carpal tunnel syndrome Cauda equina syndrome Chondromalacia patellae Colles’ fracture Dual X-ray absorptiometry Epicondylitis (medial, lateral) Fibromyalgia Genu recurvatum Genu valgum Genu varum Gout Herniated disc Mastoiditis Morton’s neuroma Navicular fracture Osteoarthritis Osteomyelitis Osteoporosis Phalen test Plantar fasciitis Polymyositis Sciatica Scoliosis Spinal compression fracture Spondylolisthesis Supraspinatus tendonitis Raynaud’s disease Rheumatoid arthritis Thoracic outlet syndrome Tibial torsion Tinel test Respiratory System Asthma COPD (emphysema, chronic bronchitis) Pertussis Pneumomediastinum Sleep apnea Tuberculosis Neurological System Amyotrophic lateral sclerosis (ALS) Aneurysms Aphasia (Broca’s, Wernicke’s, global) Apraxia Basilar skull fracture Bell’s palsy Benign paroxysmal positional vertigo (BPPV) Cranial nerves Delirium Dementia (Alzheimer’s, vascular dementia, dementia with lewy bodies) Essential tremor Guillain-Barré syndrome (GBS) Headaches (migraine, cluster, tension) Multiple sclerosis Parkinson’s disease Reflexes (deep tendon, primitive) Restless leg syndrome (RLS) Seizures (absence, atonic, tonic-clonic, etc.) Subdural hematoma Transient ischemic attacks Trigeminal neuralgia Oncology Bladder cancer Breast cancer Cervical cancer Colon cancer Liver cancer Lung cancer Lymphomas (Hodgkin’s, non-Hodgkin’s) Multiple myeloma Ovarian cancer Pheochromocytoma Prostate cancer Skin cancer (basal cell carcinoma, squamous cell carcinoma, melanoma) Strokes (hemorrhagic, ischemic) Thyroid cancer Uterine cancer Maternity Abortion (threatened, complete, incomplete, missed) Abruptio placentae Amniocentesis Breastfeeding Chorionic villus sampling (CVS) Coombs test Eclampsia Ectopic pregnancy Fetal alcohol syndrome (FAS) Gestational diabetes HELLP syndrome Hyperemesis gravidarum Mastitis Molar pregnancy Physiologic changes in pregnancy Placenta previa Preeclampsia Rh compatibility RhoGAM Shaken baby syndrome (SBS) Signs of pregnancy (positive, probable, presumptive) Teratogens Pediatrics Autism Child abuse Chromosomal abnormalities (Down syndrome, Fragile X syndrome, etc.) Bronchiolitis Hand-foot-mouth disease Hyperbilirubinemia Infant colic Kawasaki disease Milestones Nephroblastoma Phenylketonuria Reflexes (tonic neck, Moro, Babinski, etc.) Tanner stages Tay-Sachs disease Men’s Health Balanitis Benign prostatic hypertrophy Epididymitis Epispadias Erectile dysfunction Hydrocele Hypospadias Orchitis Peyronie’s disease Phimosis Priapism Prostatitis Testicular torsion Torsion of the appendix testis Varicocele Women’s Health Atrophic vaginitis Bacterial vaginosis Bartholin’s abscess Birth control (Combination pills, progestin-only pills, Depo-Provera, etc.) Candidal vaginitis Cervical ectropion Cervicitis Cystocele Fibrocystic breasts Labial adhesions Mammary duct ectasia Pelvic inflammatory disease Polycystic ovarian syndrome (PCOS) Salpingitis Trichomonas vaginitis Vulvodynia Sexual Health and STDs Chlamydia Fitz-Hugh-Curtis syndrome Gonorrhea HIV Jarisch-Herxheimer reaction Reactive arthritis Syphilis Trichomoniasis Urethritis (nongonococcal and gonococcal) Geriatrics Elder abuse Elder assessment Physiological changes Psychiatry Acute serotonin syndrome Depression (major, minor) Neuroleptic malignant syndrome Post-traumatic stress syndrome (PTSD) Seasonal affective disorder (SAD) Biochemical Attacks/Illicit Drugs Anthrax Carbon monoxide poisoning Delirium tremens Illicit drugs (cocaine, methamphetamine, ecstasy) Korsakoff syndrome Lead poisoning Rabies Ricin poisoning Wernicke encephalopathy Health Promotion/Prevention Bereavement care Diadochokinesia Graphesthesia Hyperesthesia Immunity Immunizations (primary, secondary, tertiary) Stereognosis Vaccines Legal Aspects, Insurance, and Culture Consolidated Omnibus Budget Reconciliation Act (COBRA) Emancipated minor Genetic symbols Health Insurance Portability and Accountability Act (HIPAA) Health Maintenance Organization (HMO) Hospice Institutional Review Board (IRB) Mature minor Medicare Medicaid Preferred Provider Organization (PPO) Respite care Statistics Hypothesis (alternative, null) Mean Median Mode Significance level Professional Guidelines to Follow for the Exam The following are major professional guidelines to follow for the exam. Follow the U.S. Preventive Services Task Force (USPSTF) guidelines for the screening recommendations of various medical conditions such as prostate cancer, lung cancer, diabetes, etc. The USPSTF offers recommendations for screening for various diseases based on a variety of factors including but not limited to a person’s age and medical history. Follow the Joint National Committee (JNC) guidelines for the management of hypertension in adults. The JNC’s latest guidelines are expressed in the JNC 8 Guidelines. Follow the Adult Treatment Panel (ATP) IV for guidelines for cholesterol management. Chapter 2- Pharmacology 1) Why should warfarin (Coumadin) not be prescribed along with Bactrim (trimethoprimsulfamethoxazole)? A) It causes a severe rash to break out B) It causes the warfarin to be less effective C) It increases serum warfarin levels D) It can cause respiratory arrest 2) What lab value should be monitored most closely when a person is taking warfarin (Coumadin)? A) B) C) D) CBC INR WBCs with differential Liver function Tests (LFTs) 3) What will normally occur if a person develops persistent side effects from ACE inhibitors such as a persistent dry, hacking cough? A) The person will have no choice but to keep taking the drug and endure these side effects B) The person will likely be placed on an angiotensin II receptor blocker C) The person will be taken off all antihypertensive medications D) The person will be placed on an additional ace inhibitor medication 4) Which antihypertensive medication may mask symptoms of hypoglycemia? A) B) C) D) Beta blockers Angiotensin II receptor blockers ACE inhibitors Calcium channel blockers 5) What is the first-line treatment for hypertension in a male with benign prostatic hypertrophy? A) B) C) D) ACE inhibitors Beta blockers Alpha blockers Calcium channel blockers 6) Which adverse effect can allopurinol cause? A) B) C) D) Peptic ulcers Diverticulosis Tendonitis Bone marrow suppression 7) What is the therapeutic serum level of digoxin? A) B) C) D) 0.1 – 0.4 ng/mL 0.5 – 2.0 ng/mL 2.0 – 3.5 ng/mL 4.0 – 6.0 ng/mL 8) Which of the following is beta blockers not used for? A) During an acute myocardial infarction B) For prophylaxis of migraine headaches C) To lower blood sugar before meals D) To reduce intraocular pressure 9) All of the following medications are hepatotoxic except for: A) B) C) D) Acetaminophen Ibandronate Isoniazid Atorvastatin 10) What is the first-pass metabolism of a drug? A) The amount of a drug that reaches the liver B) The amount of a drug that gets destroyed before reaching systemic circulation C) The amount of a drug that gets broken down by the digestive system D) The half-life of a drug 11) Antihistamines can be used to prevent or lessen all of the following except for: A) B) C) D) Allergy Inflammation Headaches Itchiness 12) Which antihistamine should not be given to a person who is about to undergo an activity where there is a risk for accident or injury? A) B) C) D) Diphenhydramine (Benadryl) Loratadine (Claritin) Cetirizine (Zyrtec) Fexofenadine (Allegra) 13) Which of the following diuretics is the most potent of all diuretics? A) B) C) D) Thiazide diuretics Loop diuretics Potassium sparing diuretics All diuretics are of equal potency 14) Taking a loop diuretic puts a patient at risk for all of the following except for: A) B) C) D) Hypokalemia Hyponatremia Hypertension Hypochloremia 15) All of the following are loop diuretics except for: A) B) C) D) Furosemide Bumetanide Triamterene Torsemide 16) When taking a loop diuretic, which lab value should the healthcare provider monitor most closely? A) B) C) D) White blood cell count Red blood cell count Potassium level Magnesium level 17) A patient taking spironolactone is at risk for which of following? A) B) C) D) Hypokalemia Hyperkalemia Hypercalcemia Hypermagnesemia 18) What medication is contraindicated when taking nitrates? A) B) C) D) Sildenafil Aspirin Acetaminophen Furosemide 19) What should not be taken along with statins? A) B) C) D) Orange juice Cranberry juice Grapefruit juice Milk 20) What is a possible side effect of sildenafil (Viagra) on vision? A) B) C) D) It can cause cataracts It can cause temporary blindness It can cause a decline in central vision It can cause blue-tinted vision 21) A patient taking triamterene should eat a diet that is: A) B) C) D) High in potassium Low in potassium High in fiber Low in fiber 22) A patient taking furosemide and digoxin complains of blurred vision and seeing green and yellow halos. The nurse suspects digoxin toxicity. Which of the following tests is least likely to be performed to check the patient’s status for digoxin toxicity? A) B) C) D) EKG Serum digoxin level Electrolyte levels Urine sample 23) What is the therapeutic serum level for theophylline in adults for the treatment of asthma? A) B) C) D) 1-3 µg/mL 5-15 µg/mL 20-30 µg/mL 30-50 µg/mL 24) All of the following can be taken with calcium channel blockers except for: A) B) C) D) Grapefruit juice Milk Juice Water 25) Niacin is prescribed primarily to lower: A) B) C) D) HDL cholesterol LDL cholesterol Triglyceride levels Blood sugar levels 26) What do fibrates primarily work to lower? A) B) C) D) Triglyceride levels HDL levels LDL levels Blood sugar levels 27) Which of the following statements is false regarding statins? A) Statins are the best pharmaceutical agents for lowering LDL cholesterol levels B) Besides lowering LDL levels, statins also increase HDL levels C) Statins pose a risk of rhabdomyolysis D) Patients with very high LDL cholesterol levels should be started on 80mg of simvastatin 28) A patient taking amiodarone with simvastatin is at increased risk for: A) B) C) D) A coma A myocardial infarction Cholelithiasis Acute renal failure 29) Statins increase the risk for all of the following except: A) B) C) D) Type II diabetes Rhabdomyolysis Liver damage A heart attack 30) Finasteride (Proscar) is used to treat: A) B) C) D) Urinary tract infections Balanitis Benign prostatic hypertrophy Erectile dysfunction 31) Alendronate, ibandronate, and risedronate are all examples of: A) B) C) D) Narcotics Bisphosphonates Proton pump inhibitors H2 receptor blockers 32) Isotretinoin is used to treat: A) B) C) D) Vitiligo Melasma Acne Tinea pedis 33) Bisphosphonates can lead to all of the following complications except for: A) B) C) D) Peptic ulcer disease Kidney stones Atypical fractures Esophagitis 34) What organ is the most active organ in the body for the metabolism of drugs? A) B) C) D) Kidneys Liver Lungs Stomach 35) What are the 2 main organs in the body responsible for drug excretion? A) B) C) D) The liver and lungs The liver and stomach The liver and kidneys The liver and gallbladder 36) What is the minimum inhibitory concentration (MIC)? A) The lowest concentration of a chemical (drug) needed to inhibit the growth of bacteria B) The lowest concentration of a chemical (drug) needed to kill bacteria C) The lowest concentration of a chemical (drug) needed to inhibit the growth of viruses D) The lowest concentration of a chemical (drug) needed to kill viruses 37) The area under the curve (AUC) graph for a drug has the drug plasma concentration as the dependent variable and: A) Time as the independent variable B) Bacteriostatic effect as the independent variable C) Bactericidal effect as the independent variable D) The serum bacteria count as the independent variable 38) What is the enzyme(s), principally found in the liver cells, that is primarily responsible for drug metabolism? A) B) C) D) ALT AST Cytochrome P450 enzymes Alkaline phosphatase 39) All of the following medications are responsible for many drug-to-drug interactions except for: A) B) C) D) Diphenhydramine Isoniazid Cimetidine Acetaminophen 40) Which of the following statements is false regarding Pregabalin (Lyrica)? A) Pregabalin is a Schedule II controlled substance B) Pregabalin is used for many nerve conditions such as fibromyalgia C) Pregabalin may be used in combination with other medications to treat certain types of seizures D) Pregabalin may cause drowsiness 41) The most commonly used reason for the use of herb saw palmetto is for: A) B) C) D) Prostate cancer Benign Prostatic Hypertrophy Colds Sore throat 42) Which of the following statements is false regarding tetracycline? A) Tetracycline is the first-line treatment for moderate to severe acne or rosacea B) Tetracycline can cause permanent discoloration of the teeth C) Tetracycline is classified by the FDA as a category B drug D) Tetracycline is best taken on an empty stomach 43) Quinolones are a type of: A) B) C) D) Antibiotic Antiviral Steroid Bronchodilator 44) Which of the following statements is false regarding quinolones? A) Quinolones are bactericidal antibacterial agents with broad-spectrum activity B) Quinolones should not be used on children (less than 18 years) because of their possible effect on growth inhibition C) Quinolones increase a person’s risk for developing asthma D) Quinolones are associated with an increased risk for tendonitis and tendon rupture 45) Which of the following drugs is not associated with potentially damaging ophthalmic effects and doesn't warrant regular eye examinations during periods of its administration? A) B) C) D) Ethambutol (Myambutol) Hydroxychloroquine (Plaquenil) Prednisone (Deltasone) Lorazepam (Ativan) 46) Besides being used to terminate a pregnancy, what is the other major use of misoprostol? A) It decreases the risk for stomach ulcers B) It is used as an antibiotic for certain bacterial infections C) It is used as an oral bronchodilator D) It is used as an anti-inflammatory drug for asthma as long-term treatment 47) All of the following drugs puts a patient at risk for hyperkalemia except for: A) B) C) D) Hydrochlorothiazide Losartan Captopril Spironolactone 48) What is the most common prescription drug class for fatal overdoses in the United States? A) B) C) D) Analgesics Benzodiazepines Antidepressants Statins 49) What is the second most common prescription drug class for fatal overdoses in the United States? A) B) C) D) Analgesics Benzodiazepines Antidepressants Statins 50) What is the most dangerous type of antidepressant in terms of overdosing of it? A) B) C) D) Atypical antidepressants Tricyclic antidepressants SSRIs MAOIs 51) What is the safest of all antidepressants? A) B) C) D) Atypical antidepressants Tricyclic antidepressants SSRIs MAOIs 52) What is most common drug poisoning seen in incoming patients arriving at emergency rooms in the United States? A) B) C) D) Analgesics Antidepressants Statins Antipsychotics 53) What is the most commonly prescribed drug class in America? A) B) C) D) Analgesics Antidepressants Benzodiazepines Statins 54) Akathisia is an adverse effect of: A) B) C) D) Antihistamines Beta blockers Antipsychotics Antidepressants 55) Amoxicillin should not be given as treatment for mononucleosis because it can cause: A) B) C) D) A rash Bronchoconstriction Renal failure Alopecia 56) Bitter orange is an herbal supplement that is used as a(n): A) B) C) D) Sedative Appetite Suppressor Antidepressant Antipyretic 57) Black cohosh is an herb that is used for: A) B) C) D) Appetite Suppression Depression Menopausal symptoms Fatigue 58) Which of the following is one of the uses of evening primrose oil? A) B) C) D) Skin disorders Depression Seizure disorders Insomnia 59) Ginseng is believed to have all of the following health benefits except for the ability to: A) B) C) D) Lower blood sugar Improve joint pain Fight colds and flus Suppress cancer growth 60) What class of drugs do dipeptidyl peptidase-4 (DDP-4) inhibitors belong to? A) B) C) D) Antihypertensive drugs Hyperlipidemic drugs Antidepressants Oral hypoglycemic drugs 61) Dipeptidyl peptidase-4 (DPP-4) inhibitors are used to treat: A) B) C) D) Type I diabetes Type II diabetes Hyperinsulinemia Diabetic ketoacidosis 62) Guggulipid is a plant extract that is used to lower: A) Blood sugar B) Cholesterol and triglycerides C) Fever D) Inflammatory markers such as ESR and CRP 63) Which of the following statements is false regarding dehydroepiandrosterone (DHEA)? A) DHEA is a hormone made naturally by the human body B) DHEA is precursor for insulin C) DHEA levels decrease after age 30, more steeply in women than in men D) Synthetic DHEA is taken for a variety of different purposes, where its effectiveness is unproven 64) High-intensity statin therapy is designed to lower LDL cholesterol levels by: A) B) C) D) 20% or greater 30% or greater 50% or greater 70% or greater 65) Which of the following vital signs should be monitored most closely when a person is taking nitrates? A) B) C) D) Pulse Blood pressure Temperature Respirations 66) Sustained-release, extended-release, and other time-release forms of nitroglycerin are used for: A) B) C) D) Episodes of acute angina Prophylaxis of angina Hypotension Prophylaxis of headaches 67) Which of the following statements is false regarding coenzyme Q10? A) Coenzyme Q10 (CoQ10) is found in every cell in the body B) CoQ10 is naturally present in small amounts in a variety of foods C) CoQ10 is available in the United States as a dietary supplement D) CoQ10 is proven by scientific studies to significantly help patients with heart failure 68) All of the following conditions require a person to take medications for life except for: A) B) C) D) Addison’s disease Pernicious anemia Glaucoma Guillain-Barré syndrome 69) Echinacea is an herb that may possibly be effective for: A) B) C) D) A common cold Depression Energy boost Dry skin 70) Melatonin is used to treat: A) B) C) D) Depression Insomnia Menopausal symptoms Upset stomach 71) Caffeine can cause all of the following symptoms if taken in a high enough dose except for: A) B) C) D) Insomnia Bradycardia GI disturbance Jitteriness 72) Besides acting as an antiemetic, metoclopramide also acts as a(n): A) B) C) D) Laxative Antidiarrheal GI stimulant Blood pressure lowering medication 73) Which of the following is considered an alternative medicine in the United States? A) B) C) D) Levothyroxine Hydrocortisone Glucosamine Isosorbide 74) Valerian root is an herb that is used chiefly for: A) B) C) D) Anxiety and insomnia Arthritis Bone pain Benign prostatic hypertrophy 75) Which of the following statements is false regarding isoflavones? A) Isoflavones are a class of phytoestrogens, which are plant-derived compounds of estrogenic activity B) Isoflavones come from soybeans C) Isoflavones mimic the activity of the hormone estrogen in the body D) Isoflavones have been proved in scientific studies to be a highly effective treatment for the reduction of hot flashes in post-menopausal women 76) Which of the following statements is false regarding the herb kava kava? A) Kava kava is used to calm anxiety, stress, and restlessness, and to treat insomnia B) Kava kava is native to the western Pacific Islands C) Kava kava has no reported side effects or safety issues D) Kava kava has been banned in Europe and Canada, but is still available in the United States 77) Ginkgo biloba may be taken for: A) B) C) D) The flu or common cold Dementia Menstrual symptoms Appetite suppression 78) Which of the following statements is false regarding homeopathy? A) Homeopathy is an alternative medical system in which remedies are derived from substances that come from plants, minerals, or animals B) There is little evidence to support homeopathy as an effective treatment for any specific condition C) Homeopathic remedies, due to the high dilution rates, do not have any side effects D) Homeopathic remedies are regulated by the U.S. Food and Drug Administration (FDA) 79) Which drug can precipitate acute renal failure in a patient with bilateral renal artery stenosis? A) Beta blockers B) Calcium channel blockers C) ACE inhibitors D) Thiazide diuretics 80) The maximum amount of acetaminophen that can be taken per day is: A) B) C) D) 1 gram 2 grams 4 grams 5 grams 81) What is antidote for acetaminophen? A) B) C) D) Calcium gluconate Magnesium sulfate Acetylcysteine Acetylsalicylic acid 82) Which medication is used to help a person quit smoking by decreasing cravings? A) B) C) D) Lorazepam Bupropion Escitalopram Citalopram 83) Taking metformin puts a patient at risk for: A) B) C) D) B1 deficiency B3 deficiency B6 deficiency B12 deficiency 84) Which disease should never be treated with just one medication? A) Lyme disease B) Tuberculosis C) Acute otitis media D) Rocky Mountain Spotted Fever 85) Which of the following benzodiazepines has the shortest half-life? A) B) C) D) Triazolam Alprazolam Clonazepam Diazepam 86) Which of the following benzodiazepines has the longest half-life? A) B) C) D) Lorazepam Clonazepam Midazolam Diazepam 87) Which antihypertensive drug is the least likely to cause erectile dysfunction in men with erectile dysfunction disorder? A) B) C) D) Beta blockers Calcium channel blockers Thiazides Alpha blockers 88) All of the following medications are linked to weight gain except for: A) B) C) D) Famotidine Megestrol acetate Mirtazapine Risperidone 89) All of the following conditions are contraindications for the use of bupropion except for: A) B) C) D) Peptic ulcer disease Seizure disorder Anorexia nervosa Bulimia nervosa 90) How long does it take SSRIs to work once a person starts taking them? A) B) C) D) 1-2 hours 2-3 days 4-6 weeks 3-4 months 91) Excessive amounts of loop diuretics can cause: A) B) C) D) Profuse vomiting Profound diuresis Lactic acidosis Pulmonary fibrosis 92) What is the recommended antihypertensive for a patient who has concurrent hypertension and osteoporosis? A) B) C) D) Thiazides Beta blockers ACE inhibitors Calcium channel blockers 93) Which of the following patients should not take nitrofurantoin? A) B) C) D) A patient with osteoporosis A patient with gallbladder disease A patient with G6PD deficiency A patient with pneumonia 94) Which of the following statements is false regarding cephalosporins? A) Cephalosporins are bacteriostatic B) Cephalosporins block bacteria from making their cell wall C) Cephalosporins enter breast milk and may alter the bowel flora of an infant; thus, use during breastfeeding is often discouraged D) The mechanism of action of cephalosporins is the same as penicillins 95) Which type of cephalosporin is most effective against gram-positive bacteria but is not very effective against gram-negative bacteria? A) B) C) D) First-generation cephalosporins Second-generation cephalosporins Third-generation cephalosporins Fourth-generation cephalosporins 96) Side effects of thiazide diuretics may include all of the following except for: A) B) C) D) Hyperkalemia Hyperuricemia Hypercalcemia Hyperglycemia 97) Which of the following conditions is Tamsulosin (Flomax) used for? A) B) C) D) Prostate cancer Bladder cancer Benign prostatic hypertrophy Urinary tract infections 98) Tamsulosin is approved for use only in: A) B) C) D) Infants Children Men Women 99) What instructions should a woman be given who is to take Isotretinoin (Accutane)? A) Take 81mg of aspirin with each dose to prevent facial flushing B) Use 2 forms of reliable birth control when taking this drug C) Alcoholic drinks must be limited to 1 drink per day as an absolute maximum D) Doxycycline is a safe antibiotic to take while taking Isotretinoin 100) Isotretinoin can safely be given to which of the following people? A) A 12-year-old girl with mild acne B) A 11-year-old boy with severe cystic acne C) A 20-year-old girl with moderate acne D) A 21-year-old pregnant woman with severe acne 101) What is the only liquid that should be taken with bisphosphonates? A) B) C) D) Juice Milk Water Lime 102) When should bisphosphonates be taken? A) First thing in the morning before breakfast B) In the morning, along with breakfast C) In the evening D) At nighttime, right before sleep 103) What special instruction should be given to a patient taking bisphosphonates? A) Make sure to take it with food B) Aspirin can’t be taken while on bisphosphonates C) Do not lie down a half an hour after taking the bisphosphonate D) Do not drink alcohol while on this medication 104) Alendronate can be given: A) B) C) D) Only daily Daily or weekly Daily or biweekly Daily or monthly 105) All of the following drugs have a narrow therapeutic index (NTI) except for: A) B) C) D) Theophylline Lorazepam Lithium Carbamazepine 106) Which of the following is a long-acting benzodiazepine? A) B) C) D) Midazolam (Versed) Alprazolam (Xanax) Lorazepam (Ativan) Diazepam (Valium) 107) St. John’s wort is an herb that is used for: A) B) C) D) Psychosis Depression Anxiety Seizures 108) St. John’s wort has drug interactions with all of the following drug classes except for: A) B) C) D) SSRIs Tricyclic antidepressants Opioids MAOIs 109) What is the most commonly prescribed medication used to treat the pain that accompanies sickle cell disease? A) B) C) D) Aspirin Acetaminophen Ibuprofen Morphine 110) What laboratory value is monitored during treatment with griseofulvin? A) B) C) D) BUN and creatinine CBC Erythrocyte sedimentation rate (ESR) Liver Function Tests (LFTs) 111) Very-high-potency steroids can be used: A) B) C) D) On the face On the groin On the arms With occlusive dressings Pharmacology answers 1) (C) Warfarin should not be prescribed along with Bactrim (trimethoprim-sulfamethoxazole) because it can increase serum warfarin levels, presenting a high risk for bleeding in a patient (source: drugs.com) 2) (B) The INR should be monitored closely when a person is taking warfarin. 3) (B) If a person is getting persistent side effects from ACE inhibitors such as a persistent, dry, hacking cough, the likely alternative is the person will be taken off of the ACE inhibitor and be placed on an angiotensin II receptor blocker (ARB) such as losartan, candesartan, or valsartan. ARBs don’t produce symptoms such as a dry, hacking cough (source: patient.info). 4) (A) Beta blockers may mask symptoms of hypoglycemia. What this means is that if a person has hypoglycemia who is taking beta blockers, the beta blockers may mask symptoms of the hypoglycemia, so that a person who has hypoglycemia doesn’t show the common symptoms of hypoglycemia. Common symptoms of hypoglycemia include tremors, sweating, palpitations, anxiety and a feeling of dread, and restlessness. Beta blockers may blunt the effects of epinephrine, so a person may not show all of these symptoms of hypoglycemia. In this way, beta blockers can mask hypoglycemia. 5) (C) The presence of benign prostatic hypertrophy (BPH) with coexisting hypertension is a compelling indication for the use of an alpha blocker for treatment. Alpha blockers are first-line therapy for men with lower urinary tract symptoms (LUTS) and benign prostatic hypertrophy (BPH). Typically, alpha blockers improve LUTS by 30–40% and maximum urinary flow rates by 16-25%, with clinical improvement within two weeks (source: bjcardio.co.uk) 6) (D) Allopurinol can cause bone marrow suppression, which is a reduction in bone marrow activity that results in decreased production of red blood cells, white blood cells, and/or platelets. Other adverse effects include a rash, hepatotoxicity, and severe hypersensitivity reactions. While on allopurinol therapy, liver tests, blood counts, and renal function should be monitored (source: hopkinsarthritis.org). 7) (B) The therapeutic serum level of digoxin is 0.5-2.0 ng/mL (source: drugguide.com) 8) (C) Beta blockers are not used to lower blood sugar before meals. Uses of beta blockers include use during an acute myocardial infarction and post myocardial infarction to reduce mortality, for prophylaxis of migraine headaches, for reduction of intraocular pressure (Timolol), for reduction of heart rate (tachycardia), and to treat symptoms of angina pectoris. 9) (B) Ibandronate isn’t associated with hepatotoxicity. Acetaminophen, isoniazid, and atorvastatin are all hepatotoxic. 10) (B) The first-pass metabolism of a drug is a phenomenon of drug metabolism in which the concentration of a drug is greatly reduced before it reaches systemic circulation. It is the amount of the drug that is lost due metabolism of the drug by the liver and the digestive system. When a drug is swallowed, it is absorbed by the digestive system and enters the hepatic portal system. It is carried through the portal vein into the liver before it reaches the rest of the body. The liver is responsible for metabolizing many drugs and is, in fact, the most active organ in the body for metabolizing drugs. Once the drug reaches the liver, the liver, for many drugs, metabolizes it to such an extent that only a small amount of the active drug emerges from the liver to the rest of the circulatory system (for systemic circulation). Drugs that have a high first-pass metabolism either have to be taken in very large doses or have to be taken another way other than orally such as intramuscularly or intravenously. The half-life of a drug is the amount of time in which the drug concentration decreases by 50% in the body (once taken). 11) (C) Antihistamines are not used to treat headaches. In fact, a possible side effect of antihistamines is headaches. Antihistamines are indicated for allergies, inflammation, and to decrease itchiness. 12) (A) If a person is going to undergo an activity that requires careful attention or where the risk for accident or injury is present, the person should take a second-generation antihistamine, such as loratadine, cetirizine, or fexofenadine. Second-generation antihistamines do not cause the drowsiness that first-generation antihistamines such as diphenhydramine (Benadryl) do. Because second-generation antihistamines do not readily cross the blood-brain barrier, they do not cause sedation like first-generation antihistamines and are the choice antihistamine to be taken when a person needs to remain vigilant. 13) (B) The most potent of all diuretics are loop diuretics. Loop diuretics excrete the most fluids out of the body than all other diuretics. 14) (C) A loop diuretic wastes away fluid, thereby decreasing blood pressure, so it would put a patient at risk for hypotension rather than hypertension. A loop diuretic is the most potent type of diuretic that wastes away practically every type of electrolyte including potassium, sodium, and chloride, putting a patient at risk for hypokalemia, hyponatremia, and hypochloremia. 15) (C) Triamterene is a potassium-sparing diuretic. Furosemide, bumetanide, and torsemide are all loop diuretics. 16) (C) When taking a loop diuretic, the potassium level should be monitored closely. Loop diuretics are a potassium-wasting diuretic that can lower potassium levels, leading to hypokalemia. The red blood cell or white blood cell count are not directly related to loop diuretics. Though magnesium can be decreased somewhat by loop diuretics, potassium is the electrolyte that can be shifted most radically; thus, it should be watched the closest. 17) (B) Spironolactone is a potassium-sparing diuretic. Therefore, a person taking spironolactone is at risk for hyperkalemia, especially if eating potassium-rich foods or taking potassium supplements. 18) (A) Sildenafil is contraindicated when taking nitrates. Taking sildenafil with nitrates can cause life-threatening hypotension (source: circ.ahajournals.org/) 19) (C) When taking statins, grapefruit juice should not be taken, because grapefruit juice can increase the statin drug level in the body. The grapefruit juice blocks special enzymes in the wall of the small intestine that break down many medications. This can lead to increased side effects due to the increased amount of the drug in the body. Statins that particularly have this interaction are Simvastatin (Zocor) and Atorvastatin (Lipitor) (source: fda.gov). 20) (D) Sildenafil (Viagra) can cause a person to have blue-tinged vision; this is vision in which there is blue shade to a person’s vision. The medical term for seeing everything tinted with blue is cyanopsia. 21) (B) Triamterene is a potassium-sparing diuretic. Therefore, a person taking triamterene should eat a diet that is low in potassium. A person should not eat a diet rich in potassium while taking triamterene. 22) (D) If a patient is suspected of having digoxin toxicity, tests to check the patient’s health status include checking the patient’s serum digoxin level. If the level is greater than 2 ng/mL, the patient has a toxic level. An EKG should be done on the patient, because digoxin toxicity can cause heart arrhythmias such as ventricular tachycardia and ventricular fibrillation. The patient’s electrolytes should also be taken, because digoxin toxicity can be made worse by electrolyte imbalances such as hypokalemia. A urine sample isn’t directly specific to digoxin toxicity. 23) (B) The therapeutic level of theophylline is 5-15 µg/mL in adults for the treatment of asthma. For children, the reference range is 5-10 µg/mL. 24) (A) Just like with statins, grapefruit juice should not be taken with calcium channel blockers. This is because grapefruit juice has a mechanism of action in which it inhibits an enzyme in the body (CYP3A4) that breaks down the calcium channel blocker drug. Therefore, the medication builds up in the body to higher-than-intended amounts. This can cause the blood pressure to drop more than intended, which can be dangerous for a patient. 25) (C) Niacin is used primarily to lower triglyceride levels as well as elevate HDL levels. Though niacin does modestly lower LDL cholesterol, it’s used primarily to lower triglyceride levels and boost HDL levels. To decrease LDL cholesterol, niacin is often prescribed in combination with statins. 26) (A) Fibrates, like niacin, work to lower triglyceride levels and raise HDL levels. Fibrates are not effective in lowering LDL cholesterol (source: medicinenet.com). 27) (D) Statins are among the best pharmaceutical agents for lowering LDL cholesterol levels. Besides lowering LDL levels, statins also increase HDL levels. Statins pose the risk of muscle injury and rhabdomyolysis. At one time, patients with very high LDL cholesterol levels would be started on the highest possible dose of statins such as 80mg of simvastatin. However, the FDA has tightened its rule on who should take the highest approved dose of the statin drug simvastatin. Due to the possible risk of muscle injury, the FDA now recommends that no new patients should start taking that dose (80mg of simvastatin). However, those who have been on statins for a while and have taken the 80mg dose of simvastatin for 12 months or more without signs of muscle injury can continue taking the dose. The FDA also recommends that patients who are unable to adequately lower their LDL cholesterol on 40mg of simvastatin should not be given the higher 80mg dose; instead, the FDA says that practitioners should give those patients another treatment to lower their LDL cholesterol (source: fda.gov). 28) (D) A patient taking amiodarone with simvastatin is at increased risk for rhabdomyolysis, which can cause acute renal failure (source: ncbi.nlm.nih.gov). 29) (D) Statins help to prevent heart attacks by decreasing a person’s LDL cholesterol levels but in the process of doing so increase the risk of a person developing type II diabetes, muscle damage, rhabdomyolysis, and liver damage. 30) (C) Finasteride (Proscar) is used to treat benign prostatic hypertrophy (BPH). Finasteride is an antiandrogen that shrinks the prostate by up to 50%. This causes less symptoms of BPH such as postvoid dribbling and nocturia. Finasteride, being an antiandrogen, is also used sometimes for prostate cancer because it is believed by many in the medical community that testosterone fuels prostate cancer. Finasteride is not used for balanitis, erectile dysfunction, or for UTIs. 31) (B) Alendronate, ibandronate, and risedronate are all examples of bisphosphonates. 32) (C) Isotretinoin is used to treat moderate to severe acne. 33) (B) Possible complications of bisphosphonates include peptic ulcer disease, esophagitis, esophageal perforation, and atypical fractures (seen rarely in long-term use). Bisphosphonates are not linked to kidney stones. 34) (B) The liver is the most active organ in the body for the metabolism of drugs. The other organs involved include the kidneys, organs of the gastrointestinal tract, and the lungs. 35) (C) The main organs in the body responsible for drug excretion are the liver and kidneys. 36) (A) The minimum inhibitory concentration (MIC) is the lowest concentration of a chemical (drug) needed to inhibit the growth of bacteria. The minimum bactericidal concentration (MBC) is the lowest concentration of a chemical (drug) that results in microbial death (in other words, the lowest concentration of the drug needed to kill bacteria). 37) (A) The area under the curve (AUC) graph for a drug has the drug plasma concentration as the dependent variable and time as the independent variable. You will see based on the graph below that the drug concentration peaks at a certain level and then after this decreases steadily from this point. This is because after the point where the drug concentration peaks, the body (mostly the liver and kidneys for most drugs) excretes the drug from the system. Image: Area under the curve (AUC) graph for a drug 38) (C) Cytochrome P450 enzymes are the enzymes that are most responsible for drug metabolism, accounting for 70% to 80% of enzymes involved in drug metabolism. Cytochrome P450 enzymes are primarily found in liver cells but are also located in cells throughout the body. Enzymes produced from the cytochrome P450 genes are involved in the formation (synthesis) and breakdown (metabolism) of various molecules and chemicals within cells. Cytochrome P450 enzymes play a role in the synthesis of many molecules including steroid hormones, certain fats (cholesterol and other fatty acids), and acids used to digest fats (bile acids). Additional cytochrome P450 enzymes metabolize external substances, such as medications that are ingested, and internal substances, such as toxins that are formed within cells (source: ghr.nlm.nih.gov). 39) (D) Antifungals such as ketoconazole, itraconazole, metronidazole, and fluconazole are all potent inhibitors of the cytochrome P450 enzymes. Therefore, they cause a lot of drug-to-drug interactions in that they allow other drugs to build up in the system, creating the potential for drug toxicity. Other drugs that are cytochrome P450 inhibitors are macrolide antibiotics which include clarithromycin, erythromycin, and telithromycin, calcium channel blockers such as verapamil and diltiazem, and SSRIs such as fluoxetine and paroxetine. Other drugs that are also potent cytochrome P450 inhibitors include amiodarone, cimetidine, diphenhydramine, isoniazid, and trimethoprim sulfamethoxazole. Even grapefruit juice is a potent cytochrome P450 inhibitor and must be avoided when taking certain medications. Acetaminophen is not a potent cytochrome P450 inhibitor. So, when thinking of drugs that cause frequent drug-to-drug interactions, think of antifungals, macrolide antibiotics, SSRIs and calcium channel blockers as some of the major classes of drugs that cause them (source: ncbi.nlm.nih.gov). 40) (A) Pregabalin is both a neuropathic pain agent used to treat many painful nerve conditions such as fibromyalgia and an anticonvulsant. Pregabalin may be used in combination with other medicines to treat certain types of seizures. Pregabalin is a schedule V controlled substance, which is the lowest class for any controlled substance narcotics. Pregabalin may cause drowsiness, so a person taking it should avoid alcohol. Also, because of the drowsiness, it should be used cautiously with the elderly. 41) (B) Saw palmetto is best known for its use in decreasing symptoms of an enlarged prostate (benign prostatic hypertrophy). Even though it is also used for prostate cancer, colds, and a sore throat, its best-known use is for BPH (source: webmd.com). 42) (C) Tetracycline is classified by the FDA as a category D drug, meaning there is positive evidence of risk to the fetus. Tetracycline has been linked to skeletal malformations in the fetus. Since it’s a category D drug, in some cases, the benefits may outweigh the risks. Tetracycline is used to treat many different types of bacterial infections such as urinary tract infections. It is also used often to treat acne and rosacea, as a first-line treatment. Tetracycline can cause yellowbrown to gray discoloration of the teeth. Tetracycline is best taken on an empty stomach 1 hour before a meal or 2 hours after a meal, because tetracycline binds to some minerals (calcium, iron, magnesium, zinc), making it less effective. Besides all this, know that tetracycline may decrease the effectiveness of oral contraceptives. 43) (A) Quinolones are a type of broad-spectrum antibiotic. 44) (C) Quinolones, which include drugs such as ciprofloxacin and levofloxacin, are bactericidal antibacterial agents with broad-spectrum activity. Quinolones should not be used on children (less than 18 years) because of their effect on growth inhibition (even though some studies dispute this fact). Quinolones are associated with an increased risk of tendonitis and tendon rupture. Quinolones are not associated with an increased risk for asthma. 45) (D) There are several types of medications that can potentially damage a person’s eyes in various ways. Digoxin can cause yellow to green vision, blurred vision, and halos, if toxicity is present. Ethambutol can cause optic neuropathy. Corticosteroids such as prednisone can cause cataracts and glaucoma. Fluoroquinolones can cause retinal detachment. Isotretinoin (Accutane) can cause cataracts and decreased night vision. Topiramate can cause acute angle-closure glaucoma and mydriasis. Hydroxychloroquine (Plaquenil) can cause optic neuropathy and permanent loss of vision. Sildenafil can cause blue-tinged vision. Lorazepam isn’t linked to any serious vision problems and does not require regular eye examinations during periods of its administration. 46) (A) Besides being used to terminate a pregnancy, misoprostol is used to decrease the risk of stomach ulcers. 47) (A) Hydrochlorothiazide is a thiazide diuretic, which is a diuretic that wastes potassium. Therefore, it does not put a patient at risk for hyperkalemia, but hypokalemia. Angiotensin II receptor blockers (such as Losartan), ACE inhibitors (such as Captopril), and potassium-sparing diuretics (such as Spironolactone) all put a patient at risk for developing hyperkalemia. 48) (A) Analgesics are the most commonly overdosed type of prescription medication which leads to the most deaths. Opioids are the type of analgesics that causes the most deaths. 49) (C) Antidepressants are the second most abused type of drug which leads to fatal overdoses. Most of the deaths associated with antidepressants are caused by tricyclic antidepressants. 50) (B) Tricyclic antidepressants are the most dangerous of all of the antidepressants in terms of overdosing on them. Overdosing on tricyclic antidepressants are linked to cardiac dysrhythmias, respiratory arrest, coma, and death. Tricyclic antidepressants are the second leading cause of deaths from prescription drug overdoses in the United States. 51) (C) SSRIs, by many standards, are the safest of all antidepressants. This is why they are so commonly prescribed. 52) (B) Antidepressants are the most common drug poisoning seen in emergency rooms in the United States. 53) (D) Statins are the most commonly prescribed drug class in America. 54) (C) Akathisia is an adverse effect of antipsychotics. Akathisia is one of the most prevalent and distressful antipsychotic-induced adverse effects. 55) (A) Amoxicillin should not be given as treatment for mononucleosis because it can cause a rash that is difficult to differentiate from a rash caused by an allergic reaction. Image: Rash associated with taking amoxicillin as treatment for mononucleosis 56) (B) Bitter orange is an herbal supplement that is used as an appetite suppressor and for weight loss. Some groups advocate that people avoid using it because it has been linked to a number of serious side effects such as stroke, myocardial infarction, dysrhythmias, and death (source: webmd.com). 57) (C) Black cohosh is an herb that is used for menopausal symptoms (source: webmd.com). 58) (A) Evening primrose oil is the oil from the seed of the evening primrose plant. Evening primrose oil is used for a variety of illnesses including skin disorders such as eczema, psoriasis, and acne. It is also used for rheumatoid arthritis, osteoporosis, Raynaud’s syndrome, multiple sclerosis, Sjögren’s syndrome, cancer, high cholesterol, heart disease, dyspraxia, intermittent claudication, alcoholism, Alzheimer’s disease, and schizophrenia. Some people use evening primrose oil for chronic fatigue syndrome, asthma, diabetic neuropathy, neurodermatitis, hyperactivity in children and ADHD, obesity and weight loss, whooping cough, and GI disorders including ulcerative colitis, irritable bowel syndrome, and peptic ulcer disease. Women use evening primrose oil in pregnancy for preventing high blood pressure, shortening labor, starting labor, and preventing late deliveries. Women also use evening primrose oil for premenstrual syndrome, breast pain, endometriosis, and symptoms of menopause such as hot flashes. In foods, evening primrose oil is used as a dietary source of essential fatty acids (source: webmd.com). 59) (B) Ginseng is an herb that has been used in various systems of medicine for many centuries. There is at least some evidence that the herb has the ability to support overall health, including boosting the immune system as to help people overcome common illnesses such as colds, as well as cancers. There is also at least some evidence that ginseng can increase a person’s sense of well-being, improve mental and physical performance, and lower blood glucose levels (source: webmd.com). 60) (D) Dipeptidyl peptidase-4 inhibitors are a type of oral hypoglycemic drug. Oral hypoglycemic medications that block DPP-4 are called DPP-4 inhibitors or gliptins. The mechanism of DPP-4 inhibitors is to increase incretin levels. Incretin is a natural hormone that a person’s body produces that tells the body to release insulin after a person has eaten something. When the body makes incretin, an enzyme called dipeptidyl peptidase-4 (DPP-4) removes it from the body. This is a normal, healthy process for people without diabetes. Some people with type 2 diabetes do not make enough incretin. This is where DDP-4 inhibitors are helpful. Inhibiting DPP-4 helps the incretin that is in the body to stay there longer. This triggers insulin to be released, which lowers blood sugar (source: webmd.com). 61) (B) Dipeptidyl peptidase-4 (DPP-4) inhibitors are used to treat type II diabetes. 62) (B) Guggulipid is a plant extract that is used lower cholesterol and triglyceride levels. Guggulipid is an extract from a tree that is found in India known as the mukul myrrh tree (source: medscape.com). 63) (B) DHEA is a hormone that is naturally made by the human body. DHEA is a precursor to male and female sex hormones (androgens and estrogens). DHEA levels in the body begin to decrease after age 30. This decrease occurs more quickly in women than men. Synthetic DHEA is taken for a whole host of reasons, where its effectiveness is unproven. Athletes and bodybuilders take DHEA to improve physical performance (though it’s banned by the NFL, MLB, and NCAA). DHEA is also taken for depression, sexual dysfunction, psoriasis, aging skin, and a host of other reasons, but its efficacy is unknown (source: webmd.com). 64) (C) High-intensity statin therapy is designed to lower LDL cholesterol levels by 50% or greater. High-intensity statin therapy includes atorvastatin 40-80mg or rosuvastin 20-40mg daily dosage. Moderate-intensity statin therapy is designed to lower LDL cholesterol levels by approximately 30-49%; this includes atorvastatin 10-20mg, rosuvastatin 5-10mg, simvastatin 2040mg, pravastatin 40-80mg, lovastatin 40mg, fluvastatin XL 80mg, fluvastatin 40 mg bid, or pitivastiatin 2-4mg. Low-intensity statin therapy decreases LDL cholesterol by 21-29% of its current level; this includes simvastatin 5-10mg or atorvastatin 10mg. 65) (B) Blood pressure should be monitored closely when a person is taking nitrates because nitrates cause vasodilation, which lowers blood pressure, which could possibly cause hypotension. 66) (B) Sustained-release, extended-release, and other time-release forms of nitroglycerin can be used for the prophylaxis of angina; they should not be used in episodes of acute angina. Nitroglycerin lowers blood pressure further, so it would never be used in cases of hypotension; it would worsen hypotension. Nitroglycerin is not used for the prophylaxis of headaches; in fact, a side effect of nitroglycerin is headaches. 67) (D) Coenzyme Q10 is a substance that is found in every cell in the body. The body makes CoQ10, and the cells use it to produce energy that the body needs for cell growth and maintenance. It also functions as an antioxidant, which protects the body from damage caused by harmful molecules. CoQ10 is naturally present in small amounts in a wide variety of foods; CoQ10 levels are especially high in organ meats, as well as beef, sardines, mackerel and peanuts. CoQ10 is available in the United States for purchase as a dietary supplement. CoQ10 is used for many conditions such as heart failure, cancer, muscular dystrophy, and periodontal disease; however, scientific studies do not conclude how useful it is for these conditions; its efficacy is either weak, uncertain, or nonexistent (source: webmd.com). 68) (D) Addison’s disease requires a person take hydrocortisone (synthetic cortisone) for life. Pernicious anemia requires a person to take vitamin B12 shots for life. Glaucoma requires eye drops for life. Guillain-Barré syndrome is a temporary condition of paralysis; it doesn’t require lifelong medication. 69) (A) Echinacea is an herb that may possibly be effective for a common cold, according to some studies. There is insufficient evidence for echinacea being effective for anything else (source: webmd.com). 70) (B) Melatonin is a hormone made naturally by the pineal gland in the brain which helps to control sleep and wake cycles. Synthetic melatonin can be taken as a supplement and is widely available; it is helpful for treating insomnia (source: webmd.com). 71) (B) Caffeine, with doses of 250mg/day or higher, can cause tachycardia, not bradycardia. High amounts can also cause insomnia, GI disturbance, and jitteriness. 72) (C) Besides acting as an antiemetic, metoclopramide also acts as a GI stimulant, increasing the peristalsis of the GI system. 73) (C) Glucosamine (with or without chondroitin) is considered an alternative medicine in the United States (used for osteoarthritis). Levothyroxine, hydrocortisone, and isosorbide are traditional Western medicines. 74) (A) Valerian root is an herb that is used chiefly for anxiety and insomnia. It is an anti-anxiety herb (source: webmd.com). 75) (D) Isoflavones are a class of phytoestrogens, which are plant-derived compounds of estrogenic activity. Isoflavones are produced almost exclusively by the members of the bean family, soy beans being a rich source of isoflavones. Isoflavones mimic the activity of the hormone estrogen in the body. Isoflavones are commonly used by postmenopausal women to reduce the occurrence of hot flashes. Though there is some indication of the benefit of isoflavones on hot flashes, there is no conclusive scientific evidence of its efficacy. There is also no conclusive evidence of its safety. 76) (C) Kava kava is a beverage or extract that is made from a plant native to the western Pacific Islands. It is taken by mouth to calm anxiety, stress, and restlessness, and to treat insomnia. Kava kava has some big safety concerns. Many cases of liver damage and even deaths have been traced to kava use. As a result, kava has been banned from markets in Europe and Canada; however, kava still remains available in the United States (source: webmd.com). 77) (B) Ginkgo biloba is an herb that may help with memory and sharp thinking. This is because ginkgo biloba improves blood flow to the brain and acts an antioxidant. Therefore, it may improve the thinking ability and memory of people with dementia. However, the benefits of ginkgo biloba regarding memory and sharp thinking isn’t conclusive. Some studies show that ginkgo biloba may modestly boost memory and cognitive speed, while other studies have not found this benefit (source: webmd.com). 78) (C) Homeopathy, also known as homeopathic medicine, is an alternative medical system that was developed in Germany. Homeopathic remedies are derived from substances that come from plants, minerals, or animals, such as red onion, arnica, (mountain herb), and belladonna (deadly nightshade). According to the 2012 National Health Interview Survey (NHIS), which included a comprehensive survey on the use of complementary health approaches by Americans, an estimated 5 million adults and 1 million children used homeopathy in the previous year. The 2012 survey also reported that although about 1.8 percent of children used homeopathy, only 0.2 percent of children went to a homeopathic practitioner. There is little evidence to support homeopathy as an effective treatment for any specific condition. Although people sometimes assume that all homeopathic remedies are highly diluted and therefore unlikely to cause harm, some products labeled as homeopathic can contain substantial amounts of active ingredients and therefore could cause side effects and drug interactions. Homeopathic remedies are regulated by the U.S. Food and Drug Administration (FDA); the FDA does not rate their effectiveness, though (source: nccih.nih.gov). 79) (C) ACE inhibitors should not be prescribed to patients with bilateral renal artery stenosis because ACE inhibitors can precipitate renal failure. 80) (C) The maximum amount of acetaminophen that can be taken per day is 4 grams. 81) (C) The antidote for acetaminophen is acetylcysteine. Calcium gluconate is the antidote for magnesium sulfate. Acetylsalicylic acid is the generic name for aspirin. 82) (B) Bupropion is used for smoking cessation by decreasing a person’s cravings for smoking. Bupropion can also be used to treat depression. 83) (D) Taking metformin places a patient at risk for B12 deficiency and, thus, for B12 deficiency anemia. This is referred to as metformin-induced vitamin B12 deficiency. 84) (B) Tuberculosis should never be treated with just one tuberculosis drug, because this increases the chance of microbial resistance. 2 or 3 drugs should be used to treat tuberculosis. 85) (A) Triazolam has the shortest half-life out of any of the other benzodiazepines; it has a halflife of 2 hours. Alprazolam (Xanax) has a half-life of 12 hours. Clonazepam has a half-life of 34 hours. Diazepam has a half-life of 100 hours. 86) (D) Diazepam has the longest half-life, which is 100 hours. Lorazepam has a half-life of 15 hours. Clonazepam has a half-life of 34 hours. Midazolam has a half-life of 1.5-2.5 hours. 87) (D) Alpha blockers are the antihypertensive class that is least likely to cause erectile dysfunction in men with erectile dysfunction disorder (or, in other words, they are the most likely to preserve erectile function). The next most effective antihypertensive to preserve erectile function is ACE inhibitors. The next most effective antihypertensive after this is calcium channel blockers (source: ncbi.nlm.nih.gov). 88) (A) Famotidine is not linked to weight gain. Megestrol acetate, mirtazapine, and risperidone can all cause weight gain. 89) (A) The use of bupropion is contraindicated in patients with a seizure disorder. Bupropion may trigger seizures, with the risk being greater at higher dosage prescriptions. The use of bupropion is also contraindicated in patients with a current or prior diagnosis of anorexia nervosa or bulimia nervosa because of the higher reported incidence of seizures in patients treated with the drug. Peptic ulcer disease is not a contraindication for the use of bupropion (source: rxlist.com). 90) (C) On average, it takes about 4-6 weeks for SSRIs to work and take effect once a person starts taking them. Some people may experience results quicker or a little later than this time period. This is important to teach patients, because they will not see immediate results from SSRIs. 91) (B) Excessive amounts of loop diuretics can cause profound diuresis. 92) (A) Thiazides are the recommended antihypertensive for a patient who has concurrent hypertension and osteoporosis. Thiazides lower urinary calcium excretion; this effect is associated with positive calcium balance and an increase in bone mineral density and reductions in fracture rates attributable to osteoporosis. The calcium-lowering effect also makes them useful in preventing calcium-containing kidney stones (source: ncbi.nlm.nih.gov). 93) (C) A patient with glucose-6-phosphate dehydrogenase (G6PD) deficiency should not take nitrofurantoin due to the link between nitrofurantoin-induced hemolytic anemia and G6PD deficiency. 94) (A) Cephalosporins are bactericidal, which means they kill bacteria. They are not bacteriostatic, which is something that inhibits the growth of bacteria. Cephalosporins block bacteria from making their cell wall. Cephalosporins have the same mechanism of action as penicillins (which are also bactericidal and block bacteria from making their cell wall). Cephalosporins enter breast milk and may alter the bowel flora of an infant; thus, use during breastfeeding is often discouraged, but, if used, the infant should be monitored for any adverse effects. 95) (A) First-generation cephalosporins are most effective against gram-positive cocci. They have modest gram-negative bacteria coverage. Second-generation cephalosporins have a greater gram-negative spectrum while retaining some activity against gram-positive bacteria. The thirdgeneration cephalosporins have a marked increase of activity against gram-negative bacteria. Fourth-generation cephalosporins have the broadest spectrum of activity, with similar activity against gram-positive organisms as first-generation cephalosporins. Fifth-generation cephalosporins are very broad-spectrum cephalosporins with activity against gram-positive cocci including MRSA, as well as many gram-negative bacilli. Fifth generation cephalosporins are unique in its activity against certain multidrug-resistant organisms (source: merckmanuals.com). 96) (A) Potential side effects of thiazide diuretics include hyperglycemia, hyperlipidemia, hyperuricemia, hypercalcemia, hypokalemia, hyponatremia, and hypomagnesemia. A way to remember this is that a thiazide diuretic is a potassium-wasting diuretic, so it gets rid of potassium; therefore, a potential side effect is hypokalemia. Because it’s a diuretic, it also wastes sodium (hyponatremia) and magnesium (hypomagnesemia). Thiazides reduce the clearance of uric acid since they compete for the same transporter, and therefore raise the levels of uric acid in the blood, so they are prescribed with caution in patients with gout or hyperuricemia. Chronic administration of thiazides is associated with hyperglycemia. Thiazides conserve calcium (promote calcium retention) by lowering urinary calcium excretion. This makes them useful for a number of conditions. One is they are useful in preventing calcium-containing kidney stones. Another is they are useful for increasing bone mineral density (due to the positive calcium balance) and reducing fracture rates attributable to osteoporosis. Thiazides also directly stimulate osteoblast differentiation and bone mineral formation, further slowing the course of osteoporosis. They are also used in the treatment of hypocalcemia. 97) (C) Tamsulosin is used to treat benign prostatic hypertrophy (BPH). Tamsulosin is used in BPH to improve urination in men. Tamsulosin is an alpha-blocker that relaxes the muscles in the prostate and bladder neck, making it easier for men to urinate. 98) (C) Tamsulosin is only approved for use in men. It is not approved for use by infants, children, or women. 99) (B) When a woman is taking Isotretinoin, she should avoid pregnancy, because Isotretinoin is a category X drug, which means it is teratogenic to a fetus. She should use 2 forms of reliable birth control when taking this drug. She also must sign consent forms pledging not to get pregnant. Isotretinoin is not associated with facial flushing, so there is no need to take medication to prevent flushing. It is recommended by manufacturers to avoid alcohol while on this drug. This is because isotretinoin is hepatotoxic, so taking it with another hepatotoxic substance (such as alcohol) increases the risk of liver damage. Doxycycline is an antibiotic that has a major drug interaction with Isotretinoin. Using some retinoids and tetracyclines together may increase the risk of a person developing a condition called pseudotumor cerebri. Another medical term for this condition is benign intracranial hypertension. In this condition, the brain swells around the optic nerve (the nerve connecting the eyes to the brain). Early symptoms include headaches, nausea, vomiting, and changes in vision. 100) (C) Isotretinoin can safely be given to a 20-year-old girl with moderate acne. Isotretinoin is not given to anyone younger than 13 years of age and is not given to pregnant women. Additionally, it is only given for moderate to severe acne, not mild acne. 101) (C) When taking a bisphosphonate such as alendronate (Fosamax), only plain water should be taken. This excludes any type of juice, carbonated beverage, mineral water, sparkling water, or any liquid other than plain water (source: medlineplus.gov). 102) (A) Bisphosphonates should be taken first thing in the morning before breakfast with a full glass of water on an empty stomach (source: medlineplus.gov). 103) (C) A person taking a bisphosphonate should not lie down for a half an hour after taking the bisphosphonate. A person also should not eat, drink, or take any other medications (including vitamins or antacids) for at least 30 minutes (source: medlineplus.gov). 104) (B) Alendronate (Fosamax) is given either daily or weekly. To prevent osteoporosis in adults, 5mg is given once daily or 35mg once weekly. To treat osteoporosis in adults, 10mg is given once daily or 70mg once weekly (source: drugs.com). 105) (B) Theophylline, lithium, and carbamazepine all have a narrow therapeutic index (NTI). Drugs with a narrow therapeutic index have a narrow therapeutic range and usually require frequent blood tests to check that the serum level is within the therapeutic range. If below the therapeutic range, the drug will not be very effective. If above the therapeutic range, toxic side effects may take place. Other drugs that have a narrow therapeutic range are digoxin and warfarin. 106) (D) Diazepam (Valium) is a long-acting benzodiazepine. Midazolam is an ultra-short acting benzodiazepine. Alprazolam and lorazepam are both medium-acting benzodiazepines. 107) (B) St. John’s wort is an herb that is primarily used for depression. 108) (C) St. John’s wort does not have a drug interaction with opioids. It does have drug interactions with SSRIs, tricyclic antidepressants, and MAOIs. 109) (D) Morphine is the most commonly prescribed pain medication for sickle cell disease. 110) (D) Griseofulvin is hepatotoxic, so liver function tests should be taken for a baseline level before treatment and, during treatment, the LFTs should be rechecked to monitor for liver damage (source: drugs.com). 111) (C) Very-high-potency steroids can be used on the arms. They should not be used on the face, groin, or with occlusive dressings. Chapter 3- Hematology and Lab Values 1) A person who cannot produce intrinsic factor has what condition? A) Pernicious anemia B) Indigestion C) GERD D) Superior mesenteric artery Syndrome 2) Which type of white blood cell is most specific to allergic reactions and sees a great increase in count during allergic reactions? A) B) C) D) Neutrophils Lymphocytes Eosinophils Basophils 3) Which type of white blood cell is most specific to bacterial infections and sees a great increase in count during bacterial infections? A) B) C) D) Neutrophils Lymphocytes Eosinophils Basophils 4) What percentage of white blood cells is made up of neutrophils? A) B) C) D) 10% - 20% 20% - 40% 40% - 60% 65% - 80% 5) What percentage of white blood cells is made up of lymphocytes? A) 10% - 20% B) 20% - 40% C) 40% - 60% D) 65% - 80% 6) What percentage of white blood cells is made up of monocytes? A) B) C) D) 0.5% - 1% 1% - 2% 2% - 8% 8% - 10% 7) What percentage of white blood cells is made up of eosinophils? A) B) C) D) 0.5% -1% 1% - 4% 4% - 8% 8% - 10% 8) What percentage of white blood cells is made up of basophils? A) B) C) D) 0.5% - 1% 1% - 2% 2% - 8% 8% - 10% 9) Which of the following would most likely cause an elevation in eosinophils? A) B) C) D) A parasitic infection A period of anemia A period of hypoxia A period of inflammation 10) A viral infection would cause the greatest elevation in which type of white blood cell? A) Lymphocytes B) Neutrophils C) Eosinophils D) Basophils 11) What would cause an elevation in C-reactive protein? A) B) C) D) Hyperlipidemia Inflammation in the body Hypercalcemia Hypermagnesemia 12) Which of the following is most specific to causing an elevation in B-type natriuretic peptide? A) B) C) D) Heart attack Heart failure Hypoxia Pulsus paradoxus 13) What does the mean corpuscular volume (MCV) correlate to? A) B) C) D) The weight of red blood cells The size of red blood cells The color of red blood cells The shape of red blood cells 14) Macrocytic anemia has a mean corpuscular volume of what value? A) B) C) D) 60 fL or greater 80 fL or greater 100 fL or greater 120 fL or greater 15) What diagnosis does a mean corpuscular volume of 72 fL indicate? A) B) C) D) Microcytic anemia Macrocytic anemia Normal RBC count Pernicious anemia 16) Microcytic anemia has a mean corpuscular volume of what value? A) B) C) D) 20 fL or below 60 fL or below 80 fL or below 100 fL or below 17) What might a mean corpuscular volume of 102 fL indicate? A) B12 deficiency B) Folate overload C) Iron deficiency D) Calcium overload 18) What might a mean corpuscular volume of 75 fL indicate? A) B) C) D) B12 deficiency Iron deficiency Folate deficiency Calcium deficiency 19) What type of anemia can lead toxicity lead to? A) Microcytic anemia B) Macrocytic anemia C) Pernicious anemia D) Lead toxicity has no effect on red blood cells 20) B6 deficiency can lead to all of the following symptoms except for: A) B) C) D) Peripheral neuropathy Cheilosis Depression Thrombocytopenia 21) Neutropenia is defined as an absolute neutrophil count (ANC) below what value? A) B) C) D) 500/mm3 1000/mm3 1500/mm3 2500/mm3 22) Vitamin B12 deficiency can cause all of the following symptoms except for: A) B) C) D) Impaired memory Peripheral neuropathy Joint pain Ataxia 23) What is the normal serum range for vitamin B12? A) B) C) D) 10-50 pg/mL 50-100 pg/mL 100-200 pg/mL Greater than 250 pg/mL 24) A woman walks into a clinic and has blood work done. Her serum B12 levels are found to be 200 pg/mL. What does this value signify? A) B) C) D) Normal B12 level Her B12 level is low Her B12 level is elevated Her B12 level is critically elevated 25) A man has trouble walking, keeping his balance, and has a gradual onset of paresthesia. He also has glossitis and pallor. The man is a strict vegan who takes no supplements. He is suspected of having a B12 deficiency. What values are expected when this man does a 24-hour urine test for methylmalonic acid (MMA) and gets his homocysteine level checked? A) MMA and homocysteine levels will both be elevated B) MMA and homocysteine levels will both be low C) MMA and homocysteine levels will be normal D) The MMA level will be high and the homocysteine level will be low 26) Vitamin B12 deficiency, if severe enough, can cause which symptom? A) B) C) D) Irreversible brain damage Heart failure Kidney failure Respiratory arrest 27) What would a healthcare professional expect to see in the peripheral blood smear of a person with vitamin B12 deficiency? A) Schistocytes and dacrocytes B) Leukopenia and thrombocytopenia C) Macroovalocytes and hypersegmented neutrophils D) Heinz bodies 28) Which of the following is not one of the classic triad symptoms of pernicious anemia? A) B) C) D) Weakness Shoulder pain Paresthesia Beefy, red tongue 29) Which of the following is not a cause of pernicious anemia? A) B) C) D) Dietary insufficiency of vitamin B12 A gastrectomy Bariatric surgery Gastric cancer 30) What is the treatment for pernicious anemia? A) Monthly B12 injections for life B) Intrinsic factor supplementation C) A gastrectomy D) Oral B12 supplementation 31) What condition does a deficiency of B12 or folate lead to? A) B) C) D) Microcytic anemia Macrocytic anemia Pernicious anemia Thalassemia 32) What is the normal range for serum folate in adults? A) B) C) D) 0.2 - 1.0 ng/mL 1.1 - 1.8 ng/mL 2 - 20 ng/mL 20 - 50 ng/mL 33) A woman comes into a clinic and is found to have a serum folate level of 4.5 ng/mL. What should the health care provider do based on this level? A) Rule out folate deficiency. The level is normal B) Start the woman on folate supplementation C) Tell this woman to decrease her consumption of foods high in folate D) Tell this woman to increase her consumption of foods high in folate 34) What does a deficiency in folate cause? A) Damage to the DNA of RBCs B) Damage to the makeup of neutrophils C) Damage to the makeup of platelets D) Damage to the makeup of eosinophils 35) A woman has a low serum folate level and has anemia due to this folate deficiency. What is a reasonable folic acid dosage that she should take daily? A) B) C) D) 1-5 mg 10-50 mg 50-100 mg 100-200 mg 36) A blood test is done in which a patient has elevated antiparietal antibodies and intrinsic factor antibodies. What is this patient’s diagnosis? A) B) C) D) GERD Pernicious anemia Gastric ulcers Duodenal ulcers 37) What is the normal range for platelet count? A) B) C) D) 75,000 – 150,000/µL 100,000 – 200,000 /µL 150,000 – 400,000/µL 200,000 – 300,000/µL 38) Thrombocytopenia is defined as a platelet count less than what value? A) B) C) D) 75,000/µL 100,000/µL 150,000/µL 400,000/µL 39) At which level of platelets can spontaneous bleeding occur? A) B) C) D) < 100,000/µL < 50,000/µL < 20,000/µL < 1000/µL 40) What is the normal range of hemoglobin for men? A) B) C) D) 10 – 12 g/dL 12 – 16 g/dL 14 – 18 g/dL 16 – 20 g/dL 41) What is the normal range of hemoglobin for women? A) B) C) D) 10 – 12 g/dL 12 – 16 g/dL 14 – 18 g/dL 16 – 20 g/dL 42) What does the hematocrit value represent? A) B) C) D) The proportion of white blood cells in 1 mL of plasma The proportion of platelets in 1 mL of plasma The proportion of red blood cells in 1 mL of plasma The proportion of hemoglobin in 1 mL of plasma 43) What is normal hematocrit for men? A) B) C) D) 37% to 47% 42% to 52% 48% to 54% 52% to 62% 44) What is normal hematocrit for women? A) B) C) D) 37% to 47% 42% to 52% 48% to 54% 52% to 62% 45) As a general rule, normally the hematocrit is how many times larger than the hemoglobin? A) Hematocrit = Hgb x 2 B) Hematocrit = Hgb x 3 C) Hematocrit = Hgb x 4 D) Hematocrit = Hgb x 5 46) What does the mean corpuscular hemoglobin concentration (MCHC) represent? A) The average size of RBCs in a sample of blood B) The average weight of hemoglobin per unit volume of red blood cell C) The average thickness of RBCs in a sample of blood D) The average shape of RBCs in a sample of blood 47) What is the normal range for the mean corpuscular hemoglobin concentration (MCHC)? A) B) C) D) 10-20 g/dL 20-30 g/dL 32-36 g/dL 40-47 g/dL 48) The mean corpuscular hemoglobin (MCH) represents: A) The variance in size of RBCs in a sample of blood B) The average size of RBCs in a sample of blood C) The average mass of hemoglobin per red blood cell in a sample of blood D) The average shape of RBCs in a sample of blood 49) Out of the body’s total iron supply, the majority of the iron (65%) is found in: A) B) C) D) The liver The bone marrow Hemoglobin Myoglobin 50) What is the major protein that transports iron in the blood? A) B) C) D) Fibrinogen Transferrin Albumin Globulin 51) Serum iron is: A) The total amount of iron in the blood B) The amount of iron in the blood that is unbound to transferrin C) The amount of iron in the blood that is bound to transferrin D) The amount of iron that is stored in tissues in the body 52) Which is the most sensitive test to check for iron-deficiency anemia? A) B) C) D) Ferritin level TIBC Serum iron level Hemoglobin and Hematocrit 53) Iron-deficiency anemia causes: A) B) C) D) Microcytic and hypochromic cells Microcytic and normochromic cells Macrocytic and hypochromic cells Macrocytic and normochromic cells 54) What is the normal range of serum iron? A) B) C) D) 10 - 30 µg/dL 40 - 120 µg/dL 60 - 170 µg/dL 300 - 450 µg/dL 55) What does the ferritin level represent? A) The amount of iron stored in red blood cells B) The amount of dietary iron that is consumed C) The amount of iron that the body excretes D) The amount of iron that is stored throughout tissues in the body 56) A man goes to a clinic and gets labs done. He has a ferritin level of 450 ng/mL. Which of the following is a likely diagnosis? A) Iron-deficiency anemia B) Hemochromatosis C) Wilson’s disease D) This represents a normal, healthy level 57) In iron-deficiency anemia, the ferritin level is low. How is the total iron-binding capacity? A) B) C) D) Decreased Normal Elevated Indeterminate 58) What does the Total Iron-Binding Capacity (TIBC) represent? A) A measure of the iron in the blood B) A measure of available transferrin that is bound to iron C) A measure of available transferrin that is unbound to iron D) A measure of the amount of iron that binds to red blood cells 59) What is the normal range for Total Iron-Binding Capacity (TIBC)? A) B) C) D) 100-200 µg/dL 200-300 µg/dL 240-450 µg/dL 400-600 µg/dL 60) What does the Red Cell Distribution Width (RDW) represent? A) B) C) D) The variability of the size of RBCs The average size of RBCs The average weight of red blood cells The proportion of red blood cells in 1 mL of plasma 61) Which statement is true regarding red blood cell distribution width (RDW)? A) Elevated RDW is characteristic of all anemias B) RDW has no correlation with anemia C) An elevated RDW is the hallmark sign of iron deficiency anemia D) Vitamin B12 deficiency anemia has no effect on the RDW 62) What is the normal range of RDW(-CV) in adults? A) B) C) D) 5-7% 8-10% 11.6-14.6% 15.2-18.2% 63) What are reticulocytes? A) B) C) D) Immature red blood cells Immature white blood cells Immature platelets A type of macrophage 64) What type of incident would most likely cause an increase in reticulocyte production? A) B) C) D) An infection Intense joint pain Severe Inflammation Severe hemorrhage 65) What is the normal range for reticulocytes in the body of a healthy adult? A) B) C) D) 0.5% - 1.5% of total red blood cells 2.5% - 5% of total red blood cells 5% - 10% of total red blood cells 10% - 15% of total red blood cells 66) What is the average lifespan of red blood cells in a healthy individual? A) B) C) D) 15-30 days 30-50 days 60-90 days 90-120 days 67) What part of the body sequesters red blood cells after their life cycle ends? A) B) C) D) Liver Spleen Kidneys Adrenal glands 68) What is thalassemia? A) A blood disorder in which the body produces too few red blood cells B) A blood disorder in which the red blood cells are abnormally shaped C) A blood disorder in which the body produces an abnormal form of hemoglobin D) A blood disorder in which the body produces too many red blood cells 69) What type of red blood cells does thalassemia produce? A) Microcytic and hypochromic red blood cells B) Macrocytic and hypochromic red blood cells C) Microcytic and normochromic red blood cells D) Macrocytic and normochromic red blood cells 70) The main treatment for thalassemia is: A) B) C) D) Epogen Iron supplements Regular blood transfusions Filgrastim 71) Which test is used to definitively diagnose thalassemia? A) CBC B) Mean Corpuscular Hemoglobin Concentration C) Hemoglobin electrophoresis D) RDW 72) Iron-deficiency anemia and thalassemia both produce a state of anemia. All of the following tests can be used to differentiate iron-deficiency anemia from thalassemia except for: A) B) C) D) Ferritin level The presence of microcytic cells RDW Hemoglobin electrophoresis 73) What level should also be checked when a practitioner is checking a person’s B12 levels? A) B) C) D) Iron Folate Calcium Magnesium 74) What disorder would a healthcare provider most suspect if a patient has anemia and a normal RDW? A) B) C) D) Iron deficiency anemia Vitamin B12 deficiency anemia Folate deficiency anemia Thalassemia 75) Triglycerides are a type of blood: A) B) C) D) Protein Carbohydrate Fat Sugar 76) Which of the following statements is false regarding triglycerides? A) The body converts any calories it doesn’t need to use right away into triglycerides B) Triglycerides are released for energy between meals C) Eating healthier and exercising can lower high triglyceride levels D) Proteins cause the greatest rise in triglyceride levels than any other macronutrient 77) All of the following have a potent effect in raising triglyceride levels except for: A) B) C) D) Alcohol Omega 3 fatty acids Trans fats Refined carbohydrates 78) Triglycerides are considered elevated when they are above: A) B) C) D) 100 mg/dL 150 mg/dL 200 mg/dL 240 mg/dL 79) A healthcare provider looks at a lab and sees a triglyceride level of 1100 mg/dL. The provider knows that this increases the patient’s risk for: A) B) C) D) Cholecystitis Acute pancreatitis Cirrhosis Neuropathy 80) All of the following are normal findings in a urine sample if found in small amounts except for: A) B) C) D) Nitrites Epithelial cells White blood cells Red blood cells 81) Hyaline casts are: A) Normal and may be seen in concentrated urine B) Abnormal and benign C) Abnormal and may indicate a UTI D) Abnormal and may indicate an aggressive cancer of the prostate 82) All of the following are true regarding hyaline casts except: A) Hyaline casts are produced in the renal tubules B) Hyaline casts are cylinder shaped C) Hyaline casts are composed mostly of fatty tissue D) Hyaline casts seen in high numbers are normally indicative of a significant renal disease 83) Which of following indicates that a urine sample is a contaminated sample and should be retaken? A) A large amount of red blood cells is present in the urine sample B) A large amount of epithelial cells is present in the urine sample C) A large amount of white blood cells is present in the urine sample D) A large amount of nitrites is present in the urine sample 84) At which level is there is a marked level of proteinuria? A) B) C) D) > 0.5g/day > 1 g/day > 3 g/day > 10 g/day 85) What are bands? A) B) C) D) Immature red blood cells Immature platelets Immature lymphocytes Immature neutrophils 86) Hematuria is defined as: A) B) C) D) No RBCs in the blood > 3 RBCs/hpf > 5 RBCs/hpf > 10 RBCs/hpf 87) All of the following illnesses can cause hematuria except for: A) B) C) D) Glomerulonephritis Syphilis Kidney stones Benign prostatic hypertrophy 88) Which of the following is the body's response to infection? A) B) C) D) Bandemia Reticulocytosis Hypercalcemia Hypermagnesemia 89) What is the normal range for band forms in the body? A) B) C) D) 1-2% 3-5% 6-9% 11-14% 90) All of the following statements are true regarding creatinine except: A) Creatinine is the end product of creatine metabolism B) Men produce more creatinine than women C) Elevated levels of serum creatinine are seen with liver damage or failure D) Elevated levels of serum creatinine are seen in people with more muscle mass 91) Which of the following statements is false regarding blood urea nitrogen (BUN) and creatinine? A) BUN and serum creatinine levels increase with renal failure B) Serum creatinine increases with dehydration, while BUN remains normal C) BUN decreases with starvation or a low-protein diet D) A normal BUN/creatinine ratio is between 10:1 to 20:1 92) A BUN/creatinine ratio of 5 would likely indicate which of the following conditions? A) B) C) D) Kidney disease Liver disease Prostate cancer Urethritis 93) Which of the following conditions below causes hypochromic cells? A) B) C) D) Thalassemia Folate deficiency anemia Sickle cell anemia B12 deficiency anemia 94) Which lab value is correlated with the color of the red blood cells? A) Mean corpuscular volume (MCV) B) Mean corpuscular hemoglobin concentration (MCHC) C) Red Cell Distribution Width (RDW) D) Hematocrit (HCT) 95) What substance is responsible for giving red blood cells their red color? A) B) C) D) Mitochondria Cell wall Ribosomes Hemoglobin 96) What is the medical term for red blood cells that are of unequal size? A) B) C) D) Poikilocytosis Anisocytosis Microcytosis Leukocytosis 97) What is the medical term for red blood cells that are of abnormal shape? A) B) C) D) Poikilocytosis Anisocytosis Microcytosis Leukocytosis 98) Which of the following would indicate anisocytosis? A) CBC with an abnormal hemoglobin level B) CBC with a high RDW value C) CBC with a low RBC count D) CBC with hypochromic cells 99) What is a normal creatine kinase (CK) level in men? A) B) C) D) 0-50 U/L 52-336 U/L 350-550 U/L 600-800 U/L 100) During an episode of rhabdomyolysis, what can the creatine kinase level elevate to? A) B) C) D) 400 – 500 U/L 600-700 U/L 800- 900 U/L Greater than 10,000 U/L 101) With rhabdomyolysis, dark-colored urine is due to the presence of what in the urine? A) B) C) D) Hyaline casts Myoglobin Red blood cells Sodium 102) Which medication class puts a person at greatest risk for developing rhabdomyolysis? A) B) C) D) NSAIDs Statins Atypical antipsychotics Quinolones 103) Myoglobin is a protein that is found in the heart muscles and the: A) B) C) D) Liver Kidneys Skeletal muscles Skin 104) The parathyroid hormone (PTH) produced by the parathyroid gland regulates: A) B) C) D) Calcium levels Testosterone levels Magnesium levels Sodium levels 105) What is the most common anemia in the world? A) B) C) D) Iron-deficiency anemia B12-deficiency anemia Folate-deficiency anemia Sickle cell anemia 106) Chvostek’s sign is seen in: A) B) C) D) Hypocalcemia Hypercalcemia Hyponatremia Hypernatremia 107) What test can be used to diagnose hyperprolactinemia? A) B) C) D) MRI Ultrasound Blood test Urine sample and urinalysis 108) Calcium has an inverse relationship with: A) B) C) D) Magnesium Phosphorus Potassium Sodium 109) All of the following increases a person’s risk for developing a deep vein thrombosis except for: A) B) C) D) Prolonged bed rest or inactivity Factor V Leiden deficiency Anemia Pregnancy 110) What is the most serious complication of a deep vein thrombosis? A) B) C) D) Post-thrombotic syndrome Pulmonary embolism Heart attack Stroke 111) What is the optimal level for LDL cholesterol? A) B) C) D) 70 mg/dL or less 100 mg/dL or less 130 mg/dL or less 190 mg/dL or less 112) Which of the following statements is false regarding HDL cholesterol? A) Low HDL alone, with normal LDL and total cholesterol, is not a risk factor for heart disease B) Target HDL is 40 mg/dL or greater for men and 50 mg/dL or greater for women C) HDL is referred to as “good cholesterol” D) HDL cholesterol scavenges the bloodstream and removes LDL cholesterol 113) At what levels of primary elevations of LDL cholesterol is it recommended that individuals, age 40 to 75, be treated with statin therapy? A) B) C) D) LDL ≥ 130 mg/dL LDL ≥ 160 mg/dL LDL ≥ 190 mg/dL LDL ≥ 220 mg/dL 114) According to the ATP IV guidelines, an individual, age 40 to 75, who has diabetes with an LDL cholesterol of what range would benefit from moderate- to high-intensity statin therapy? A) B) C) D) 30-69 mg/dL 70-189 mg/dL Greater than 190 mg/dL Greater than 220 mg/dL 115) According to the ATP IV, which individual would benefit from moderate to high-dose statin therapy? A) A nondiabetic individual with an LDL of 170 mg/dL B) A nondiabetic individual with an LDL of 185 mg/dL C) A diabetic individual with a LDL of 65 mg/dL D) A diabetic individual with an LDL of 110 mg/dL 116) What is the first-line treatment for hyperlipidemia? A) Lifestyle changes such as exercise and diet B) Statins C) Fibrates D) Bile acid sequestrants 117) Smoking increases all of the following except for: A) B) C) D) Total cholesterol LDL cholesterol HDL cholesterol Triglycerides 118) What is the normal total serum protein level? A) B) C) D) 2-4 g/dL 4-6 g/dL 6-8 g/dL 8-10 g/dL 119) Most of the body’s total serum protein is a combination of: A) B) C) D) Albumin and globulins Albumin and transferrin Transferrin and fibrinogen Albumin and fibrinogen 120) What is normal range of ammonia in the body? A) B) C) D) 1-5µg/dL 15-45 µg/dL 60-100 µg/dL 150-250 µg/dL 121) High levels of ammonia in the body would most likely indicate a problem with the: A) B) C) D) Kidneys Liver Gallbladder Red blood cells 122) What is the major type of hemoglobin found in healthy newborns? A) B) C) D) Hemoglobin A Hemoglobin E Hemoglobin F Hemoglobin S 123) What is the dominant type of hemoglobin in a healthy adult? A) B) C) D) Hemoglobin A Hemoglobin E Hemoglobin F Hemoglobin S 124) How much of a healthy adult’s hemoglobin can be made up of hemoglobin F? A) Absolutely none of an adult’s hemoglobin should be composed of hemoglobin F B) Less than 2% C) Less than 10% D) Less than 20% 125) What test is used to determine the composition of the types of hemoglobin in an individual? A) B) C) D) MCHC MCV RDW Hemoglobin electrophoresis 126) All of the following can cause aplastic anemia except for: A) B) C) D) B12 deficiency Radiation Adverse drug effect Viral infection 127) What is the definitive test to confirm aplastic anemia? A) B) C) D) Complete Blood Count (CBC) Bone marrow biopsy Hemoglobin electrophoresis Stool sample examination 128) What is the definitive test for the diagnosis of sickle cell anemia? A) B) C) D) Hematocrit value Hemoglobin value RDW Hemoglobin electrophoresis 129) What is the average lifespan of red blood cells in a person with sickle cell anemia? A) B) C) D) 5-7 days 10-20 days 30-60 days 90-120 days 130) People with sickle cell anemia are at increased risk for all of the following except: A) B) C) D) Frequent infections Splenic sequestration Priapism Cystic fibrosis 131) What will the results of hemoglobin electrophoresis show for a person who has sickle cell anemia? A) 80-100% Hb S, elevated Hb F, no Hb A B) 80-100% Hb A, elevated Hb F, no Hb S C) 80-100% Hb F, elevated Hb A, no Hb S D) 20-40% Hb S, 60-80% Hb A, no Hb F 132) Alkaline phosphatase may be elevated for all of the following conditions except for: A) B) C) D) Biliary obstruction Lung disease Bone disease Liver disease 133) Which statement is true regarding alkaline phosphatase? A) Alkaline phosphatase levels are higher in children than adults B) Alkaline phosphatase is an enzyme found only in the bones C) Malnutrition causes elevated levels of alkaline phosphatase D) Alkaline phosphatase levels are tested for more often in children than in adults 134) What are titers? A) Vaccines given to an individual B) Medications given to an individual C) Blood levels to check if an individual is immune to an illness D) Urine tests done to check for an illness 135) Which of the following may cause a falsely high body mass index (BMI) level? A) A person with high body fat content B) A person with a high muscular content C) A person who has chronic edema D) A person who has hyperaldosteronism 136) What is the normal range for AST in a healthy individual? A) B) C) D) 0 to 22 mg/dL 0 to 45 mg/dL 0 to 75 mg/dL 0 to 100 mg/dL 137) The AST value is specific to: A) B) C) D) The heart The brain The liver The AST value is nonspecific 138) What is the normal range for ALT in a healthy individual? A) B) C) D) 0 to 22 mg/dL 0 to 40 mg/dL 0 to 75 mg/dL 0 to 100 mg/dL 139) Serum ALT is specific to which organ in the body? A) B) C) D) The kidneys The liver The gallbladder The pancreas 140) What is the normal AST/ALT ratio in healthy conditions? A) B) C) D) 1:1 2:1 3:1 8:1 141) An AST/ALT ratio of 4:1 is most likely indicative of: A) Infectious hepatitis B) Alcohol-related body damage C) A growth spurt D) A bone disorder 142) Which body organ is the gamma-glutamyl transferase (GGT) enzyme most specific to? A) B) C) D) The gallbladder The pancreas The stomach The liver 143) Isolated elevated levels of gamma-glutamyl transferase (GGT) compared to other liver enzymes is most suggestive of: A) B) C) D) Cirrhosis Alcohol abuse Hepatitis Fatty liver disease 144) A practitioner gets lab results for a patient and observes that the alkaline phosphatase level is elevated and the gamma-glutamyl transferase (GGT) level is also elevated. This most likely signals: A) B) C) D) A bone disorder A liver disorder A lung condition A muscle condition 145) A nurse practitioner views labs for a patient and observes that the alkaline phosphatase level is elevated, the bilirubin is elevated, the GGT is elevated, the ALT is normal, and AST is slightly elevated. What is the most likely condition of this patient? A) B) C) D) A bone disorder A liver disorder Biliary obstruction A muscle condition 146) What are schistocytes? A) Red blood cells that are tear shaped B) Red blood cells that are abnormally large (high MCV) C) Red blood cells that are abnormally small (low MCV) D) Fragmented red blood cells 147) Which of the following disorders would schistocytes not likely be found in? A) Disseminated Intravascular Coagulation B) Systemic lupus erythematosus C) Thrombotic thrombocytopenic purpura D) Hemolytic uremic syndrome 148) Schistocytes are caused by: A) Chemical damage to the red blood cells B) Mechanical damage to the red blood cells C) White blood cells attacking and damaging the red blood cells D) Red blood cells that are self-destroying due to defective DNA makeup 149) Which of the following statements is false regarding nucleated red blood cells? A) Nucleated red blood cells are often present in adults in large numbers without any pathological findings B) Nucleated red blood cells are very immature forms of red blood cells C) Nucleated red blood cells are seen when there is a severe demand for red blood cells D) Nucleated red blood cells can be normal in infants for a short time after birth 150) Which of the following if seen in small amounts in adults is a normal finding that indicates no pathology? A) B) C) D) Holly jolly bodies Nucleated red blood cells Reticulocytes Heinz bodies 151) What is the most common type of cerebral aneurysm? A) B) C) D) Pseudoaneurysm Fusiform aneurysm Saccular aneurysm Dissecting aneurysm 152) In which type of aneurysm does blood collect under an intact outer layer of the blood vessel? A) B) C) D) Saccular aneurysm Pseudoaneurysm Fusiform aneurysm Dissecting aneurysm 153) An aneurysm is widening or ballooning of a blood vessel that is: A) 10% or more of the normal blood vessel diameter B) 30% or more of the normal blood vessel diameter C) 50% or more of the normal blood vessel diameter D) 75% or more of the normal blood vessel diameter 154) Which type of aneurysm balloons out from all sides of the blood vessel? A) B) C) D) Saccular aneurysm Pseudoaneurysm Fusiform aneurysm Dissecting aneurysm 155) Which type of aneurysm is characterized by a hematoma that forms on a blood vessel as a result of an injury to the blood vessel wall? A) B) C) D) Saccular aneurysm Pseudoaneurysm Fusiform aneurysm Dissecting aneurysm 156) Where is the most common place in the body for an aneurysm to occur? A) B) C) D) In a cerebral artery In the aorta In the mesenteric artery In the splenic artery 157) What is the most common type of aneurysm? A) Thoracic aortic aneurysm B) Abdominal aortic aneurysm C) Popliteal aneurysm D) Femoral aneurysm 158) What metric does the ankle brachial index (ABI) measure? A) B) C) D) Pulse Temperature Blood pressure Pulse oximetry 159) The ankle brachial index is a metric that is specific to determine if a patient has: A) B) C) D) Hypertension Diabetic neuropathy Atherosclerosis Peripheral arterial disease 160) Ankle brachial index monitoring is recommended for all of the following groups except for: A) Every smoker over 50 years old B) All pregnant women over 35 years old C) Every diabetic over 50 years old D) All patients over 70 years old 161) What is a positive finding for the ankle brachial index test? A) The blood pressure in the ankle is greater than the blood pressure in the arm B) The blood pressure in the ankle is the same as the blood pressure in the arm C) The blood pressure in the ankle is less than the blood pressure in the arm D) The blood pressure in the ankle and arm are both highly elevated 162) What score on the ankle brachial index is indicative of peripheral arterial disease? A) B) C) D) 3 or less 2 or less 0.9 or less 0.1 or less 163) Vitamin C deficiency is also referred to as: A) B) C) D) Scurvy Rickets Beriberi Cobalamin deficiency 164) Symptoms of vitamin C deficiency include all of the following except for: A) B) C) D) Bruising Osteomalacia Bleeding gums Fatigue 165) Myelodysplastic syndromes are a group of disorders that directly affects the: A) B) C) D) Kidneys Heart Liver Bone marrow 166) Which of the following statements is false regarding myelodysplastic syndromes? A) Myelodysplastic syndromes are primarily found in the elderly B) Myelodysplastic syndromes affect only the red blood cells C) About 30% of patients with myelodysplastic syndromes develop acute myeloid leukemia (AML) D) Myelodysplastic syndromes are an acquired illness 167) Which is the most common and accurate way of diagnosing acute pancreatitis? A) B) C) D) Serum amylase level Serum lipase level CRP level ESR level 168) With acute pancreatitis, serum amylase and lipase levels are at least how many times above their normal level: A) B) C) D) 2 3 4 5 169) A positive antinuclear antibody titer is most specific to which of the following conditions? A) B) C) D) Gout Osteoarthritis Diabetes Systemic lupus erythematosus 170) Which of the following statements is false regarding inflammatory markers in the body? A) C-reactive protein (CRP) is the amount of protein called C-reactive protein in the blood and it measures general levels of inflammation in the body B) The erythrocyte sedimentation rate (ESR) is the rate at which blood cells sediment (sink to the bottom of the test tube) in a period of 1 hour and it is used to detect inflammation in the body C) ESR changes more quickly than C-reactive protein as the patient’s condition improves or worsens D) C-reactive protein changes more quickly than ESR as the patient’s condition improves or worsens 171) What is the normal range for erythrocyte sedimentation rate in men? A) B) C) D) 0-22 mm/hour 0-40 mm/hour 0-60 mm/hour 0-80 mm/hour 172) What is the normal range for erythrocyte sedimentation rate in women? A) B) C) D) 0-29 mm/hour 0-40 mm/hour 0-60 mm/hour 0-80 mm/hour 173) High-sensitivity C-reactive protein (hs-CRP) levels which represent low risk for cardiovascular disease are below: A) B) C) D) 1.0 mg/L 3.0 mg/L 10.0 mg/L 30.0 mg/L 174) What is the most important lab value to monitor in a patient who is receiving statin therapy who has complaints of muscle pains? A) B) C) D) Creatine kinase ESR AST C-reactive protein 175) Which of the following markers can be used to screen for bone disease? A) Alkaline phosphatase levels B) Gamma-glutamyl transferase levels C) ALT levels D) Bilirubin levels 176) Which of the following statements is false regarding idiopathic thrombocytopenic purpura (ITP)? A) ITP is a disorder that can lead to easy or excessive bruising and bleeding B) ITP is caused by a problem that originates in the bone marrow of a person C) Children often develop ITP after a viral infection and usually recover fully without treatment, while in adults the disorder is often long term D) ITP is caused by an autoimmune response 177) What is the difference between an embolus and a thrombus? A) A thrombus is a broad term of any blockage material in a blood vessel; an embolus is a blood clot that acts as a blockage in a blood vessel B) An embolus is a broad term of any blockage material in a blood vessel; a thrombus is a blood clot that acts as a blockage in a blood vessel C) A thrombus is a broad term of any blockage material in a blood vessel; an embolus is a fat globule that acts as a blockage in a blood vessel D) An embolus is a broad term of any blockage material in a blood vessel; a thrombus is a bubble of air that acts as a blockage in a blood vessel 178) Which of the following tests would be the most useful and specific for diagnosing disseminated intravascular coagulation? A) B) C) D) CBC D-dimer Erythrocyte sedimentation rate C-reactive protein 179) What does proteinuria represent? A) Nothing, it is normal to have some protein in the urine B) Damage to the kidneys C) Damage to the liver D) Damage to the gallbladder 180) Creatinine clearance is the: A) Measure of the amount of creatinine in the blood at any given time B) Measure of the amount of creatinine in the blood in a 24-hour period C) Measure of the amount of creatinine that the kidneys are able to clear from the body in a 12-hour period D) Measure of the amount of creatinine that the kidneys are able to clear from the body in a 24-hour period 181) Creatinine clearance is a measure of: A) B) C) D) Liver function Kidney function Gallbladder function Pancreas function 182) Which of the following lab results would explain the peripheral neuropathy that a patient is feeling? A) B) C) D) Vitamin B12 500 pg/mL Vitamin B6 4.1 ng/mL Calcium 9.5 mg/dL Magnesium 1.9 mg/dL 183) Bilirubin is a breakdown product of: A) B) C) D) Platelets White blood cells Red blood cells Fat molecules 184) Conjugated bilirubin is bilirubin that is attached to: A) B) C) D) Protein Fat Sugar Bile 185) A woman is found to have a ferritin level of 100 ng/mL and a TIBC of 300 µg/dL. What would this be indicative of? A) Iron-deficiency anemia B) Hemochromatosis C) Normal value D) Hemosiderosis 186) Which macronutrient most affects blood urea nitrogen (BUN) levels? A) B) C) D) Carbohydrates Protein Fat They all equally affect BUN levels 187) A patient taking warfarin is found to have an INR of 7 without any visible signs of bleeding. Based on this, what should be done? A) The person should keep taking the regular dose of warfarin B) The person should take a reduced dosage of warfarin C) 1 or 2 doses of warfarin should be held D) Warfarin should be stopped and discontinued permanently 188) Glucose-6-phosphate dehydrogenase (G6PD) deficiency causes: A) B) C) D) Iron-deficiency anemia Folate-deficiency anemia B12-deficiency anemia Hemolytic anemia 189) Which of the following statements is false regarding glucose-6-phosphate dehydrogenase (G6PD) deficiency? A) G6PD deficiency is an inherited condition B) G6PD deficiency is more common among men than women C) G6PD deficiency is more common among blacks and people of Middle Eastern descent D) Those with G6PD deficiency usually have regular attacks daily 190) Symptoms of G6PD deficiency anemia include all of the following except for: A) B) C) D) Bradycardia Jaundice Pallor Splenomegaly 191) A person with G6PD deficiency must: A) Take erythropoietin daily B) Receive regular monthly blood transfusions C) Strictly avoid things that can trigger an episode of hemolytic anemia D) Carefully monitor his or her blood glucose levels daily 192) Which of the following drugs can a person with G6PD deficiency take safely? A) B) C) D) Nitrofurantoin Acetaminophen Trimethoprim sulfamethoxazole Aspirin 193) Polycythemia vera is characterized by: A) A hematocrit value greater than 47% in men or 42% in women B) A hematocrit value greater than 52% in men or 47% in women C) A hematocrit value greater than 60% in men or 50% in women D) A hematocrit value greater than 65% in men or 57% in women 194) All of the following are symptoms associated with polycythemia vera except for: A) B) C) D) Dyspnea Poor concentration Nystagmus Dizziness 195) Which of the following statements is false regarding polycythemia vera? A) Polycythemia vera is a type of cancer B) In polycythemia vera, the person’s bone marrow makes too many red blood cells C) Polycythemia vera develops very slowly, usually over many years D) Most people with polycythemia only live to about their mid-40s, even when treatment is given 196) Polycythemia vera is: A) B) C) D) Genetic Transmitted sexually Transmitted through blood Transmitted through saliva 197) Complications of polycythemia vera include all of the following except for: A) B) C) D) The formation of blood clots Chronic lymphocytic leukemia Stroke Heart attack 198) All of the following are true regarding polymyalgia rheumatica except: A) Mostly women are affected with polymyalgia rheumatica B) People with polymyalgia rheumatica are at high risk for rheumatoid arthritis C) Polymyalgia rheumatica causes muscle pain and stiff joints, especially in the shoulders and hips D) Polymyalgia rheumatica mostly affects those 50 years or older 199) Which of the following statements is false regarding temporal arteritis? A) Temporal arteritis is an inflammation of arteries in and around the scalp B) Temporal arteritis is an autoimmune disease C) Temporal arteritis is the most common form of vasculitis in patients over the age of 50 years D) Giant cell arteritis is 2 to 3 times more common in men than in women 200) What is the definitive test to confirm temporal arteritis? A) B) C) D) Temporal artery biopsy MRI Erythrocyte sedimentation rate (ESR) Lumbar puncture 201) What is the main class of medication used to treat temporal arteritis? A) B) C) D) DMARDs Tumor necrosis factor inhibitors Antihypertensives Steroids 202) All of the following are common symptoms of temporal arteritis except for: A) B) C) D) Headache Hypertension Vision changes Fever 203) What patient is most likely to have temporal arteritis based on its incidence in demographic populations? A) B) C) D) A 4-year-old boy A 2-year-old girl A 74-year-old man A 66-year-old woman 204) What would a healthcare provider expect the erythrocyte sedimentation rate (ESR) to be for a person with giant cell arteritis? A) 10 mm/h or higher B) 20 mm/h or higher C) 50 mm/h or higher D) 100mm/h or higher 205) Upon palpating the scalp of a person with temporal arteritis, what finding would the healthcare provider expect to find? A) Tenderness of the temporal artery B) Increased throbbing of the temporal artery C) Firmness of the temporal artery D) Large round nodules on the surface of the temporal artery 206) Besides affecting the temporal artery, which artery does giant cell arteritis also commonly affect? A) B) C) D) Superior mesenteric artery Facial artery Lingual artery Ophthalmic artery 207) An elderly lady comes into a clinic and displays all the classic signs of temporal arteritis. The healthcare provider performs a scalp examination which further gives evidence to this. The most appropriate next step for the healthcare provider to do for the management of this patient is to start therapy with: A) B) C) D) Metoprolol Acetaminophen Prednisone Adalimumab 208) All of the following are conditions that are commonly found in hyperaldosteronism except for: A) B) C) D) Hypertension Metabolic acidosis Hypokalemia Hypernatremia 209) What is the most common cause of primary hyperaldosteronism? A) B) C) D) Chronic alcoholism High triglyceride levels Adrenal adenoma Common cold 210) All of the following medications are used in the treatment of hyperaldosteronism except for: A) B) C) D) Antihypertensives Potassium-sparing diuretics Potassium supplements Loop diuretics 211) What is cavernous sinus thrombosis? A) A blood clot that travels to the lungs B) A blood clot at the base of the brain C) Hemorrhage that takes place at the pulmonary artery D) Hemorrhage that takes place at the base of the brain 212) What is the most common etiology of cavernous sinus thrombosis? A) B) C) D) Bacterial infection Viral infection Temporal arteritis Headaches 213) Cavernous sinus thrombosis is a: A) B) C) D) Benign condition Serious but nonfatal condition Serious condition that can be fatal Condition that is always fatal 214) Symptoms of cavernous sinus thrombosis include all of the following except for: A) A bulging eyeball B) Inability to move the eye in a certain direction, especially in the lateral direction C) Ptosis D) Low-grade fever 215) Cavernous sinus thrombosis is treated primarily with: A) B) C) D) High-dose salicylate therapy High-dose acetaminophen High-dose antibiotics High-dose heparin 216) Which of the following RDW(-CV) values is most suggestive of iron-deficiency anemia? A) 9.8% B) 11.8% C) 12.9% D) 14.9% Hematology and Lab Values answers 1) (A) A person who cannot produce intrinsic factor has pernicious anemia. Intrinsic factor is a glycoprotein produced by the parietal cells in the stomach which allow a person to absorb vitamin B12 in the small intestine. 2) (D) Basophils are a type of white blood cell that is most specific to allergic reactions and sees a great increase in count during allergic reactions. 3) (A) Neutrophils are most specific to bacterial infections and see a great increase in count during bacterial infections. 4) (C) Neutrophils normally make up 40-60% of white blood cells without any type of infection being present. During bacterial infections, they are more elevated (source: medlineplus.gov). 5) (B) Lymphocytes normally make up 20%-40% of white blood cells without any type of infection being present. During viral infections, they are more elevated (source: medlineplus.gov). 6) (C) Monocytes normally make up 2%-8% of white blood cells. They are a type of white blood cell that differentiates into macrophages. Macrophages surround and kill microorganisms, remove dead cells, and stimulate the action of other immune system cells (source: medlineplus.gov). 7) (B) Eosinophils make up 1-4% of white blood cells without any type of infection being present. They elevate during infections, most commonly in parasitic infections (source: medlineplus.gov). 8) (A) Basophils normally make up 0.5%-1.0% of white blood cells without any type of infection or inflammation being present. Basophils typically elevate when an allergic reaction occurs (source: medlineplus.gov). 9) (A) An infection, most typically a parasitic infection, would cause an elevation in eosinophils. 10) (A) A viral infection would cause the greatest elevation in lymphocytes. 11) (B) Inflammation in the body would cause an elevation in C-reactive protein. 12) (B) An elevated B-type natriuretic peptide would be suggestive of heart failure. 13) (B) The mean corpuscular volume (MCV) correlates to the average volume of red blood cells. Being that volume capacity correlates with size, the MCV is representative of the size of red blood cells. A low MCV number indicates smaller-than-normal RBCs. A high MCV number indicates larger-than-normal RBCs. 14) (C) Macrocytic anemia has a mean corpuscular volume of 100 fL or greater. The normal range for the mean corpuscular volume of red blood cells is 80-100 fL (femoliters). A MCV below 80 fL indicates microcytic anemia. A MCV above 100 fL indicates macrocytic anemia. 15) (A) A mean corpuscular volume (MCV) of 72 fL would indicate microcytic anemia. 16) (C) Microcytic anemia has a mean corpuscular volume below 80 fL. The normal range for the MCV is 80-100 fL. Anything below 80 fL is indicative of microcytic anemia. Anything above 100 fL is indicative of macrocytic anemia. 17) (A) A mean corpuscular volume of 102 fL may indicate B12 deficiency. Since B12 deficiency produces a type of macrocytic anemia, the MCV will be above 100 fL. Iron deficiency produces a type of microcytic anemia, in which case the MCV will be below 80 fL. 18) (B) A mean corpuscular volume of 75 fL may indicate iron deficiency anemia (a type of microcytic anemia). Both B12 deficiency anemia and folate deficiency anemia are macrocytic anemias, so with these conditions the MCV would be elevated above 100 fL. 19) (A) Lead toxicity can lead to microcytic anemia. 20) (D) B6 deficiency is not linked to thrombocytopenia. A B6 deficiency is associated with cheilosis, depression, and peripheral neuropathy. 21) (C) Neutropenia is defined as an absolute neutrophil count (ANC) less than 1500/mm3. The normal range for the ANC is 1500-8000/mm3 (source: medicinenet.com). 22) (C) Vitamin B12 deficiency mostly causes neurological and nervous system symptoms. However, it also does cause hematological symptoms such as anemia. Symptoms of B12 deficiency include gradual onset of symmetrical peripheral neuropathy starting in the feet and/or arms, numbness, ataxia (positive Romberg test), loss of vibration and position sense, impaired memory, and dementia (in severe cases). B12 is essential for good neurological, nervous system, and hematological health. 23) (D) In the United States, the normal serum range for vitamin B12 is greater than 250 pg/mL. Any value below this is a low vitamin B12 level (source: ods.od.nih.gov). 24) (B) A vitamin B12 level of 200 pg/mL is low. In the United States, vitamin B12 levels must be greater than 250 pg/mL for a person not to be clinically diagnosed with a B12 deficiency. 25) (A) With vitamin B12 deficiency, the MMA and the homocysteine levels will both be elevated. Increased methylmalonic acid levels are a sensitive indicator of mild vitamin B12 deficiency and elevated homocysteine levels denote vitamin B12 or folate deficiency (source: ncbi.nlm.nih.gov). 26) (A) Vitamin B12 deficiency, if severe enough, can cause irreversible brain damage and dementia. Heart failure, kidney failure, and respiratory arrest aren’t associated with vitamin B12 deficiency. 27) (C) A healthcare professional would expect to see macroovalocytes and hypersegmented neutrophils in the peripheral blood smear of a person with vitamin B12 deficiency. Normal neutrophils only contain 3 or 4 nuclear lobes (segments); hypersegmented neutrophils contain 6 or more lobes. Macroovalocytes are enlarged, oval-shaped red blood cells. They are not seen in healthy blood, and are most commonly seen in megaloblastic anemia (such as B12 deficiency anemia). A good way to think of macroovalocytes is just to break down the word. Macro- means large. Oval- means oval. And cytes means cells. So, it’s large oval cells. Though hypersegmented neutrophils may also be seen in iron-deficiency anemia, the appearance of hypersegmented neutrophils and macroovalocytes are unique to vitamin B12 or folate deficiency anemia. Image: Hypersegmented neutrophils seen in vitamin B12 or folate deficiency 28) (B) The classic triad symptoms of pernicious anemia is weakness, paresthesia, and a beefy, red tongue. Shoulder pain is not associated with pernicious anemia. 29) (A) Dietary insufficiency of vitamin B12 is not a cause of pernicious anemia. Pernicious anemia causes low vitamin B12 levels due to a lack of intrinsic factor needed to absorb vitamin B12 in the small intestine. A gastrectomy (removal of the stomach), either partial or total, bariatric surgery, and gastric cancer can all be causes of pernicious anemia. 30) (A) The treatment for pernicious anemia is monthly B12 injections for life. Being that a person who has pernicious anemia lacks the intrinsic factor needed to absorb vitamin B12, any oral intake of vitamin B12 will not be absorbed from the small intestine into the bloodstream. Therefore, the person needs regular B12 injections (that goes straight into the bloodstream) in order to have healthy serum B12 levels. 31) (B) Vitamin B12 or folate deficiency leads to macrocytic anemia. 32) (C) The normal range of serum folate in adults is 2 - 20 ng/mL (source: emedicine.medscape.com). 33) (A) The healthcare provider can rule out folate deficiency, since 4.5 ng/mL is a normal folate level. 34) (A) Folate deficiency causes damage to the DNA of RBCs. 35) (A) A reasonable amount of folic acid that can be supplemented for a person with anemia due to folate deficiency is 1-5 mg PO. 1-5 milligrams should be taken by mouth daily until recovery. This should be taken until the anemia is resolved and levels are normal. Then a diet with good sources of folate is recommended (source: mayoclinic.org). 36) (B) With pernicious anemia, there is an elevation of antiparietal antibodies and intrinsic factor antibodies. 37) (C) 150,000 – 400,000/µL is the normal platelet count. 38) (C) Thrombocytopenia is defined as a platelet count less than 150,000/µL (platelets per microliter of blood). 39) (C) Platelet counts below 20,000/µL are associated with spontaneous bleeding. People with platelet counts below 20,000/µL are at high risk for bleeding (source: merckmanuals.com). 40) (C) The normal range of hemoglobin for men is 14-18 g/dL. 41) (B) The normal range of hemoglobin for women is 12-16 g/dL. 42) (C) The hematocrit is the proportion of red blood cells in 1 mL of plasma. 43) (B) The normal hematocrit for men is 42% to 52%. 44) (A) The normal hematocrit for women is 37% to 47%. 45) (B) As a general rule, normally hematocrit is 3 times the value of the hemoglobin. 46) (B) The mean corpuscular hemoglobin concentration (MCHC) represents the average weight of hemoglobin per unit volume of red blood cell (source: emedicine.medscape.com). 47) (C) The normal range for mean corpuscular hemoglobin concentration (MCHC) is 32-36 g/dL. Numbers below this range are representative of hypochromic cells. Numbers above this range are representative of hyperchromic cells (source: medlineplus.gov). 48) (C) The mean corpuscular hemoglobin (MCH), or mean cell hemoglobin, is the average mass of hemoglobin per red blood cell in a sample of blood. Along with the MCHC, the MCH is reported as part of a standard complete blood count. The normal range for MCH is 27-31 picograms/cell. The MCH value is diminished in hypochromic anemias and increased in hyperchromic anemias (source: emedicine.medscape.com & medlineplus.gov). 49) (C) Out of the body’s total iron supply, the majority of the iron (65%) is found in hemoglobin. This shows how vital iron is for hemoglobin synthesis. 3% of the body’s iron is found in myoglobin (Schnell, M., & Kranpitz, 2003). 50) (B) Transferrin is the major iron-transport protein, carrying 60%-70% of the body’s iron. Transferrin is not the only protein in the body that transports iron; there are other proteins but transferrin is the major one. Transferrin contributes to the total iron-binding capacity (TIBC), as do the other proteins. As transferrin (and the other proteins) increase, the TIBC increases. Transferrin is the body’s counter mechanism against unbound iron in the blood. Unbound iron in the blood is highly toxic in the human body, but generally there is an excess of transferrin available to prevent the buildup of unbound iron in circulation (Schnell, M., & Kranpitz, 2003). 51) (C) Serum iron is the amount of circulating iron in the blood that is bound to transferrin. 52) (A) Ferritin is a protein manufactured in the liver, spleen, and bone marrow that consists of a protein shell and an iron core. Ferritin levels parallel the amount of iron stored in the body, so elevated levels of ferritin indicate excess iron in the body while decreased levels indicate a deficiency of iron in the body. Levels vary according to gender and age, but they are not affected by external intake of iron or subject to diurnal variations. This is why compared to iron and total iron-binding capacity, ferritin is a more sensitive and specific test for diagnosing iron-deficiency anemia. Normal levels of ferritin in adults is 12-300 ng/mL in men and 12-150 ng/mL in women. Iron-deficiency anemia in adults is indicated at ferritin levels less than 10 ng/mL. Hemochromatosis or hemosiderosis is indicated at ferritin levels greater than 400 ng/mL (source: medlineplus.gov) & (Schnell, M., & Kranpitz, 2003). 53) (A) Iron-deficiency anemia causes microcytic and hypochromic cells. 54) (C) The normal range of serum iron is 60 - 170 µg/dL (source: medlineplus.gov). 55) (D) The ferritin level represents the amount of iron that is stored throughout tissues in the body. 56) (B) Ferritin levels parallel the amount of iron stored in the body, so elevated levels of ferritin indicate excess iron in the body. Normal levels of ferritin in adults is 12-300 ng/mL in men and 12-150 ng/mL in women. Iron-deficiency anemia in adults is indicated at ferritin levels less than 10 ng/mL. Hemochromatosis or hemosiderosis is indicated at ferritin levels greater than 400 ng/mL (source: medlineplus.gov & (Schnell, M., & Kranpitz, 2003)). 57) (C) With iron-deficiency anemia, the ferritin and serum iron levels are low and the total ironbinding capacity (TIBC) is elevated. 58) (C) The Total Iron-Binding Capacity (TIBC) is a measure of available transferrin that is left unbound (to iron). Transferrin is used to transport iron in the body. To compensate for low amounts of iron in the body, transferrin levels increase in an attempt to try to transport more iron throughout the body; this increase in transferrin levels correlates with an increase in the TIBC (since the two are directly correlated). Therefore, the TIBC is elevated if there are low reserves of iron in the body, as seen in iron-deficiency anemia. In cases of excess iron in the body, the TIBC would be low. 59) (C) The normal range for Total Iron-Binding Capacity (TIBC) is 240-450 µg/dL. 60) (A) The Red Cell Distribution Width (RDW) represents the variability of the size of RBCs in the body. 61) (C) An elevated RDW is a hallmark sign of iron deficiency anemia. Deficiencies of vitamin B12 or folate produce a macrocytic anemia (large cell anemia) in which the RDW is elevated in roughly two-thirds of all cases. However, an elevated RDW is seen in virtually all cases of irondeficiency anemia. An elevated RDW has a correlation with many types of anemia but is not characteristic of all anemias. Anemia due to acute blood loss, aplastic anemia, and thalassemia minor may all present with a normal RDW. 62) (C) The normal range for RDW(-CV) in adults is 11.6-14.6% (source: emedicine.medscape.com). 63) (A) Reticulocytes are immature red blood cells. 64) (D) A severe hemorrhage is directly associated with an increase in reticulocyte production. In an effort to increase the amount of red blood cells, to compensate for the loss that occurs due to the severe hemorrhage, the body produces reticulocytes, immature red blood cells, which eventually become mature red blood cells. These red blood cells replace the red blood cells lost in the hemorrhage. 65) (A) The normal range of reticulocytes in the body of a healthy adult, without any acute distress such as hemorrhage, is 0.5%-1.5% of total red blood cells. This means that in a healthy adult, reticulocytes make up 0.5%-1.5% of total red blood cells (source: medlineplus.gov). 66) (D) The average life of red blood cells in a healthy individual is 90-120 days. 67) (B) The spleen sequesters red blood cells once their life cycle ends. The liver then breaks down the red blood cells into iron and globulin and bilirubin. 68) (C) Thalassemia is a blood disorder in which the body produces an abnormal form of hemoglobin. Hemoglobin is the protein in red blood cells that carries oxygen. This disorder results in large numbers of red blood cells being destroyed, causing anemia. A blood disorder in which the body produces too few red blood cells is anemia. A blood disorder in which the red blood cells are abnormally shaped is sickle cell anemia. A blood disorder in which the body produces too many red blood cells is polycythemia vera. 69) (A) Thalassemia produces microcytic and hypochromic red blood cells (source: patient.info). 70) (C) The main treatment for thalassemia is regular blood transfusions. Epogen wouldn’t be effective for thalassemia, because red blood cells would still get destroyed. With thalassemia, the person doesn’t have a problem making red blood cells. They have a problem making normal red bloods with normal hemoglobin. Therefore, regular blood transfusions (of the correct match) is the treatment. A person with thalassemia should not get iron supplements because regular blood transfusions cause excess iron in the blood. The person instead needs chelation therapy to reverse high iron levels. Filgastrim use is not for thalassemia; thalassemia is a not a disorder of white blood cells. 71) (C) Though tests such as the ferritin level and the RDW can be used to differentiate thalassemia from other disorders that have similar symptoms such as iron-deficiency anemia, hemoglobin electrophoresis is the definitive test to diagnose thalassemia. Hemoglobin electrophoresis is also the definitive test to diagnose other hemoglobinopathies such as sickle cell disorder. 72) (B) Both iron-deficiency anemia and thalassemia produce states of anemia. To differentiate between the two, several tests or examinations can be done. One test that can be done is to check the ferritin level of the person. In iron-deficiency anemia, this level will be low. If the level is normal to high, this is suggestive of thalassemia. Another test that can be done is to check the red cell distribution width (RDW). The RDW is a value that compares the size of red blood cells within a person’s body. If there is a great variance in the size of red blood cells, the person has a high RDW. If there is little variance of the size of red blood cells within the body, the person has a low or normal RDW. With thalassemia, a person may or may not have elevated levels of RDW (elevated RDW is present about 50% of the times). With iron-deficiency, the vast majority of cases (over 90%) have elevated RDW values. With iron-deficiency anemia, as the patient’s serum iron level drops lower and lower, the new successive red blood cells that are made get smaller and smaller. So, the new red blood cells created are smaller than the previous ones. This creates a high RDW, since there is a lot of variance in the size of red blood cells. Therefore, if there are microcytic, hypochromic cells and the RDW is normal, this is suggestive of thalassemia. Another test that can be done, the definitive test to diagnose thalassemia, is hemoglobin electrophoresis, which will show abnormal hemoglobin (which is definitive of thalassemia). Microcytic cells do not differentiate thalassemia from iron-deficiency anemia, because both conditions produce microcytic cells. Both cells are also hypochromic. 73) (B) When checking serum B12 levels, folate levels should also be checked, because folate and B12 deficiencies produce very similar symptoms. So, unless a practitioner checks both levels, s/he wouldn't know which (deficiency) is producing the symptoms. 74) (D) If a patient has anemia and a normal RDW value, the healthcare provider should most suspect thalassemia. Iron-deficiency anemia will cause high RDW values in virtually all cases. Vitamin B12 or folate deficiency anemia will cause a high RDW in roughly two-thirds of all cases. Thalassemia produces a high RDW in about half of its cases, so about half of people with thalassemia will have normal RDW. 75) (C) Triglycerides are a type of fat (lipid) found in the blood. 76) (D) The body converts any calories it doesn’t need to use right away into triglycerides. Triglycerides are released for energy between meals. Eating healthier and exercising can lower high triglyceride levels. Simple carbohydrates (like refined sugars) and saturated and trans fats are linked to rises in triglyceride levels (source: mayoclinic.org). 77) (B) Foods that have a potent effect on increasing triglyceride levels are alcohol, bad fats such as saturated fats and trans fats, and refined/simple carbohydrates such as foods made with white flour or sugary drinks such as soda (source: webmd.com). 78) (B) Triglycerides are considered elevated when they are above 150 mg/dL (source: webmd.com). 79) (B) Very high triglyceride levels (above 1000 mg/dL) put a person at risk for acute pancreatitis. High levels of triglycerides also put a person at risk for heart disease (source: ncbi.nlm.nih.gov). 80) (A) Nitrites found in the urine is an abnormal finding and is indicative of a bacterial infection. Nitrites are produced due to breakdown of nitrates (to nitrites) by certain bacteria. A few epithelial cells, white blood cells, or red blood cells in the urine are normal findings (source: webmd.com). 81) (A) Hyaline casts are normal and may be seen in concentrated urine. 82) (C) Hyaline casts are produced in the renal tubules and are cylinder-shaped because of this reason. Hyaline casts seen in high numbers is normally indicative of a significant renal disease. The common matrix of a hyaline casts is a mucoprotein known as Tamm-Horsfall protein (source: hopkinslupus.org). 83) (B) Large amounts of epithelial cells mean that the skin cells near the end of the urethra has fallen off into the urine sample (probably due to it not being a midcatch urine specimen). This is a contaminated sample of urine and should be retaken. Multiple different bacteria found in the urine sample is also indicative of a contaminated urine sample, and it should be discarded and retaken. A large amount of red blood cells is indicative of hematuria, not contamination. A large amount of white blood cells or nitrites is indicative of an infection, not contamination. 84) (C) A marked level of protein in the urine is an amount that is greater than 3g/day. A normal (healthy) amount is less than 0.5g/day. Levels near the high end of the normal range (near 0.5g) can be seen with exercise or concentrated urine in a healthy individual. A moderate amount of protein is 0.5 – 3g; this can be seen with chronic kidney conditions such as with chronic glomerulonephritis. Elevated levels above 3g/day may indicate aggressive acute kidney disorders such as lupus nephritis. 85) (D) Bands are immature neutrophils. 86) (C) Hematuria is defined as more than 5 red blood cells per high-powered field in the urine (source: emedicine.medscape.com). 87) (B) A number of conditions can cause hematuria, including urinary traction infections, kidney infections such as pyelonephritis, bladder or kidney stones, benign prostatic hypertrophy, kidney disease such as glomerulonephritis, advanced cancer of either the kidney, bladder, or prostate, inherited disorders such as sickle cell anemia, and kidney injury. Certain medications can cause hematuria such as cyclophosphamide and penicillin, as well as anticoagulants such as heparin and aspirin. Although it’s rare, even strenuous exercise can cause hematuria (source: mayoclinic.org). 88) (A) Bandemia refers to excess production of bands (immature neutrophils). Bandemia would occur as a response to infection in the body. 89) (B) The normal range for band forms (immature neutrophils) in the body is 3-5%. Band forms greater than this range is indicative of severe infection. A high band count is also referred to as a shift to the left. The band form is the percentage of the total white blood cell count that is composed of bands (immature WBCs). 90) (C) Creatinine is the end product of creatine metabolism. Men and people with more muscle mass produce higher levels of creatinine. Elevated levels of creatinine are seen with kidney damage or failure. 91) (B) Blood urea nitrogen is a product of body metabolism. The liver produces ammonia from the breakdown of protein. Ammonia is then transformed into urea, which is excreted out of the body by the kidneys. The kidneys are responsible for excreting BUN and creatinine out of the body, so both BUN and serum creatinine will increase in renal failure. BUN also increases with dehydration, blood loss, and a high-protein diet, but creatinine remains about normal. Overhydration can cause decreased BUN levels. BUN levels also decrease with starvation (since the person consumes less protein, there is less ammonia produced, which would be converted into BUN in the body). BUN also decreases with liver failure, since the liver converts ammonia into blood urea nitrogen. A normal BUN/creatinine ratio is between 10:1 to 20:1. 92) (B) A normal BUN/creatinine ratio is between 10:1 to 20:1. A lowered ratio may indicate liver disease. An increased level may indicate kidney disease. 93) (A) Thalassemia causes hypochromic cells (less red than normal). Since thalassemia produces abnormal hemoglobin and hemoglobin is what gives red blood cells their red color, then this is a way to remember that thalassemia produces hypochromic cells. Another disorder that causes hypochromic cells is iron-deficiency anemia. Since iron is needed to created hemoglobin (heme consists of iron molecules), iron-deficiency anemia causes a lack of hemoglobin, which creates hypochromic cells. Other types of anemias such as folate deficiency anemia, vitamin B12 deficiency anemia, and sickle cell anemia produce normochromic cells. 94) (B) The mean corpuscular hemoglobin concentration (MCHC) is correlated with the color of red blood cells. Since hemoglobin gives red blood cells their red color, a low MCHC would produce hypochromic cells. A high MCHC would produce hyperchromic cells. The mean corpuscular volume correlates with the volume (and, thus, size) of red blood cells. The Red Cell Distribution Width (RDW) correlates with the variance in size of red blood cells in the body. The hematocrit is the proportion of red blood cells in 1 mL of plasma. 95) (D) The hemoglobin, particularly the heme aspect, is responsible for giving red blood cells their red color. This is why cells that have a low concentration of hemoglobin (low MCHC) are pale in color (hypochromic). 96) (B) Anisocytosis is the medical term for red blood cells that are of unequal size. 97) (A) Poikilocytosis is the medical term for red blood cells that are abnormally shaped. A poikilocyte is an abnormally shaped red blood cell. Poikilocytosis refers to the presence of poikilocytes in the blood. Poikilocytosis is a blood disorder in which 10% or more of red blood cells are abnormally shaped. 98) (B) A CBC with a high RDW value indicates anisocytosis. Anisocytosis is red blood cells of unequal size. A CBC showing a high RDW value means there is great variation in the size of red blood cells (anisocytosis). 99) (B) In men, the normal range for creatine kinase is 52-336 U/L. In women, the normal range for creatine kinase is 38-176 U/L (source: mayomedicallaboratories.com). 100) (D) During episodes of rhabdomyolysis, the creatine kinase levels can be dramatically elevated. The normal creatine kinase is 52-336 U/L in men and 38-176 U/L in women. During episodes of rhabdomyolysis, depending on the severity, creatine kinase levels can easily rise over 10,000 U/L to even over 100,000 U/L. Creatine kinase levels have been documented to rise over 1,000,000 U/L in severe cases of rhabdomyolysis. 101) (B) The dark-colored urine that occurs with rhabdomyolysis is due to the presence of excess myoglobin in the urine. Myoglobin is a protein in heart and skeletal muscles. Normally, myoglobin in the urine is less than 5 ng/mL. When myoglobin is greater than 25 µg/mL, urine gets a dark brown red color (source: ncbi.nlm.nih.gov). 102) (B) Statins are the main type of medication that puts a person at risk for developing rhabdomyolysis. Other medications/drugs that put a person at risk for rhabdomyolysis include cyclosporine, erythromycin, colchicine, amphetamines, ecstasy, and LSD (source: healthline.com). 103) (C) Myoglobin is a protein that is found in the heart and skeletal muscles. If there is a breakdown of muscles of the heart or skeleton, this can cause excess myoglobin in the urine (myoglobinuria). 104) (A) The parathyroid hormone (PTH) regulates calcium levels in the body. 105) (A) The most common type of anemia in the world for all races, ages, and genders is irondeficiency anemia. 106) (A) Chvostek’s sign is seen with hypocalcemia. Chvostek’s sign is a clinical sign of existing nerve hyperexcitability seen in hypocalcemia. It is a spasm of the facial muscles elicited by tapping the facial nerve in the region of the parotid gland. 107) (C) Hyperprolactinemia is a condition of elevated serum prolactin. A simple blood test is all that is needed to determine whether a person has high levels of prolactin or not. High levels of prolactin may indicate a prolactinoma, a condition in which a noncancerous tumor (adenoma) of the pituitary gland in the brain overproduces the hormone prolactin. However, other things can cause hyperprolactinemia such as certain medications. 108) (B) Calcium has an inverse relationship with phosphorus. As one goes up, the other one goes down. 109) (C) Factor V Leiden is a mutation of one of the clotting factors in the blood called factor V. This mutation can increase a person’s chance of developing abnormal blood clots, usually in the veins. Pregnancy is a hypercoagulable state, so pregnancy increases a woman’s risk of developing a DVT. Prolonged bed rest or inactivity can increase a person’s disposition for DVTs due to this stasis. Anemia does not increase a person’s risk of having a DVT. 110) (B) The most serious complication of a deep vein thrombosis (DVT) is a pulmonary embolism (PE). Pulmonary embolisms can be fatal if the clot is large enough. Another (lesser) complication of DVTs is a disorder called post-thrombotic syndrome (PTS). Nearly one-third of people who have a DVT will have this long-term complication. PTS is characterized by damage caused by the clot to the valves in the vein. People with PTS have symptoms such as swelling, pain, and discoloration; in severe cases, ulcers can appear in the affected part of the body. It can even be so severe, the person can become disabled. A DVT does not cause a heart attack or stroke. A blood clot in an artery, usually in the heart or brain, is called an arterial thrombosis. This is the type of blood clot that can cause a heart attack or stroke. 111) (B) The optimal level for LDL cholesterol is 100 mg/dL or less (source: nhlbi.nih.gov). 112) (A) HDL cholesterol is referred as the “good cholesterol”, while LDL cholesterol is referred to as the “bad cholesterol”. HDL cholesterol scavenges the bloodstream and removes LDL cholesterol. Target HDL cholesterol is 40 mg/dL or greater for men and 50 mg/dL or greater for women. Low HDL alone, with normal LDL and total cholesterol, is a risk factor for heart disease; HDL alone, not taking into account LDL or total cholesterol, can increase or decrease a person’s risk for heart disease based on its level. 113) (C) According to the ATP IV guidelines, individuals (age 40 to 75) with primary elevations of LDL cholesterols greater than or equal to 190 mg/dL should be treated with moderate to highdose statin therapy. 114) (B) According to the ATP IV, individuals who have diabetes and an LDL cholesterol level of 70-189 mg/dL would benefit from treatment with moderate to high-dose statin therapy. 115) (D) According to the ATP IV, a diabetic individual with an LDL of 110 mg/dL would benefit from moderate to high-dose statin therapy. The ATP IV identified 4 major benefit groups of moderate to high-dose statin therapy. These include individuals who have clinical atherosclerotic cardiovascular disease (ASCVD), individuals with primary elevations of LDL ≥ 190 mg/dL, individuals 40 to 75 years of age with diabetes and an LDL of 70-189 mg/dL without clinical ASCVD, and individuals without clinical ASCVD or diabetes who are 40 to 75 years of age with an LDL of 70-189 mg/dL and a 10-year ASCVD risk of 7.5% or higher. The ASCVD risk is calculated according to the Pooled Cohort Equations. You don’t have to calculate it for the exam but realize that a level of 7.5% or higher is elevated and the ATP IV recommends that this individual will benefit from statin therapy. 116) (A) The first-line treatment for hyperlipidemia is lifestyle changes including exercise, diet, and smoking cessation. If these are not enough, then antilipidemic medications may be considered. 117) (C) Smoking increases total cholesterol, LDL cholesterol, and triglycerides. Smoking decreases HDL cholesterol levels. 118) (C) The normal total serum protein level is 6-8 g/dL. In normal, healthy conditions, albumin makes up 3.5-5.0 g/dL, and the remainder is the total globulins (source: ncbi.nlm.nih.gov). 119) (A) Most of the body’s total serum protein is a combination of albumin and globulins. Albumin, the protein present in the highest concentrations, is the main transport protein in the body. Albumin also maintains plasma oncotic pressure. Globulins make up the second majority of serum proteins. Fibrinogen, which is a protein essential for the conversion of fibrinogen to insoluble fibrin, makes up the third greatest amount. 120) (B) The normal range for ammonia in the human body is 15-45 µg/dL (source: medlineplus.gov). 121) (B) The liver is the organ that converts ammonia into urea. So, if there are high levels of ammonia in the body, this is indicative of a liver problem, such as cirrhosis or severe hepatitis. 122) (C) Hemoglobin F is the dominant type of hemoglobin found in newborns. From 1 day to 3 weeks, hemoglobin F makes up 70-77% of all hemoglobin. From 6-9 weeks, the amount drops to 42-64%. By 3-4 months, hemoglobin F drops further to 7-39%. By 6 months, hemoglobin F makes up only 3-7%. Hemoglobin S is found in sickle cell disease. Hemoglobin E is found in thalassemia-like conditions (Schnell, M., & Kranpitz, 2003). 123) (A) The dominant type of hemoglobin in a healthy adult is hemoglobin A (Schnell, M., & Kranpitz, 2003). 124) (B) An adult can still have some hemoglobin F in small amounts (less than 2%) without any type of pathology (Schnell, M., & Kranpitz, 2003). 125) (D) Hemoglobin electrophoresis is used to determine the composition of hemoglobin in an individual. Hemoglobin electrophoresis is a separation process used to identify normal and abnormal forms of hemoglobin (Schnell, M., & Kranpitz, 2003). 125) (D) Hemoglobin electrophoresis is the definitive test used for diagnosing sickle cell anemia. 126) (A) B12 deficiency does not cause aplastic anemia; it causes macrocytic anemia. Aplastic anemia can be caused by radiation, adverse drug effects, and viral infections. 127) (B) The definitive test to confirm aplastic anemia is a bone marrow biopsy. 128) (D) Hemoglobin electrophoresis is the definitive test used for diagnosing sickle cell anemia. 129) (B) The average lifespan of red blood cells in a person with sickle anemia is 10-20 days. This compares with 90-120 days for a healthy person with normal red blood cells. 130) (D) Cystic fibrosis is a hereditary disorder that one must be born with. Therefore, a person with sickle cell anemia is not at increased risk for developing or acquiring cystic fibrosis. A person with sickle cell anemia is at greater risk for priapism (prolonged erection of the penis), splenic sequestration (an acute condition of intrasplenic pooling of large amounts of blood), and frequent infections. 131) (A) The hemoglobin electrophoresis of a person with sickle cell anemia will show a composition of 80-100% hemoglobin S, elevated hemoglobin F (2% to 20%) and no hemoglobin A (which is the dominant type in healthy individuals) (source: patient.info). 132) (B) Alkaline phosphatase (ALP) may be elevated for several reasons. Alkaline phosphatase may be elevated due to liver disease or bone disorders. Alkaline phosphatase may also be elevated due to biliary obstruction (blocked bile ducts) because ALP is especially high in the edges of cells that join to form bile ducts. Any conditions that affect bone growth or causes increased activity of bone cells can affect serum ALP levels. An example of a bone disorder, for instance, that causes an increased ALP level is Paget’s disease. ALP is also found in the intestines and the kidneys and could be indicative of problems with these organs as well (source: emedicine.medscape.com). 133) (A) Alkaline phosphatase levels are higher in children than adults. This is because alkaline phosphatase is found in bones. Bones that are still growing produce higher levels of ALP. The normal level for alkaline phosphatase (in adults) is 20-140 IU/L. In children, levels can be as high as 500 IU/L. For this reason, this test is usually not done in children (since the levels are so high due to growth spurts). Alkaline phosphatase is not just found in bones. ALP is also found in the liver, bile ducts, kidneys, and intestines. Certain conditions such as malnutrition and protein deficiency can cause lower-than-normal levels of alkaline phosphatase. 134) (C) Titers are blood levels to check to see if an individual is immune to an illness. For example, varicella titers would check to see if an individual is immune to varicella. 135) (B) A person who is very muscular may have a falsely high body mass index (BMI). This is because muscle contains more weight than fat. All of the other conditions are indicative of a truly high BMI level. 136) (B) 0 to 45 mg/dL is the normal range for AST in a healthy individual. 137) (D) The AST value can be seen as a kind of non-specific indicator for damage or inflammation in the body. It is not specific to any one organ. 138) (B) 0 to 40 mg/dL is the normal range for ALT in a healthy individual. 139) (B) Serum ALT is specific to the liver. This enzyme is found mainly in the liver. An elevated ALT value is indicative of liver damage or inflammation. 140) (A) In a healthy individual, the normal AST/ALT ratio is 1:1. 141) (B) An AST/ALT ratio of 4:1 is most likely indicative of alcohol-related damage to organs. Because alcohol is damaging to many organs in the body and AST is found more widespread compared to ALT (which is more specific to the liver), AST/ALT ratios of 3:1 to 8:1 may indicate alcohol-related body damage. If the ALT is greater than the AST, this normally indicates a condition that is specific to the liver such as infectious hepatitis. 142) (D) Although GGT is found in many parts of the body such as the gallbladder, spleen, pancreas, and kidneys, it is most concentrated in the liver. GGT is predominantly used as a diagnostic marker for liver disease. The GGT test is the most sensitive enzyme indicator of liver damage and disease; therefore, the GGT level will rise even before other liver enzymes do. 143) (B) Isolated levels of gamma-glutamyl transferase (GGT) compared to other liver enzymes such as alanine transaminase (ALT) can indicate alcohol abuse or alcoholic liver disease. For other liver conditions such as where the liver is structurally damaged or inflamed such as cirrhosis or hepatitis, there will usually also be a marked elevation in liver enzymes such as ALT. It is important to know that GGT levels are not specific to acute alcohol intoxication. It is used for chronic alcohol abuse; it can indicate excess alcohol consumption up to 3 to 4 weeks prior to the test, but not shorter than this. 144) (B) If the alkaline phosphatase level is elevated and the gamma-glutamyl transferase (GGT) level is also elevated, this most likely signals a liver disorder, because both ALP and GGT elevate with a liver (or bile duct) disorder. With the presence of a bone disorder, the GGT level would not be elevated; only the ALP would be elevated. GGT is often measured relative to alkaline phosphatase (ALP). If GGT and ALP are both elevated, doctors will suspect that a person has a problem with his or her liver or bile ducts. If GGT is normal and ALP is elevated, this could indicate bone disease. ALP and GGT levels aren’t associated with the lungs or muscles (source: healthline.com). 145) (B) Based on the lab values, the most likely condition is a biliary obstruction. The bilirubin level is elevated, which may either signal liver damage or a biliary obstruction. The GGT is elevated, which it would be for either a liver disorder or biliary obstruction. However, the ALT is normal, signaling there likely is no liver involvement. The AST is just marginally elevated. Therefore, based on the data, this is likely a biliary obstruction. If the ALP level was elevated by itself, without the GGT, then this would likely signal bone involvement. 146) (D) Schistocytes are fragmented red blood cells. They are also referred to helmet cells, being that they resemble helmets for the regular, normal red blood cells. Image: Schistocytes 147) (B) Schistocytes would not likely be found in systemic lupus erythematosus. Schistocytes are commonly found in disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, hemolytic uremic syndrome, and can also be caused by an artificial heart valve. 148) (B) Schistocytes are caused by mechanical damage. For conditions such as disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, and hemolytic uremic syndrome, schistocytes are caused by excess fibrin in the bloodstream, which causes damage to the red blood cells (fragmentation) by the severing of the RBCs by the excess fibrin strands. Schistocytes can also be caused by artificial heart valves, which can cause shearing of red blood cells. 149) (A) Nucleated red blood cells are very immature forms of red blood cells that are often seen when there is a severe demand for red blood cells to be released by the bone marrow or there is some type of malfunction or abnormality of the bone marrow such as a tumor or fibrosis of the bone marrow. It may also be seen with chronically low oxygen levels. Nucleated red blood cells are normal in infants for a short time after birth. Nucleated red blood cells in adults in large numbers would definitely indicate a pathological finding such as a bone tumor, for example, and usually indicates a relatively poor prognosis. 150) (C) Reticulocytes seen in small amounts in the body in adults is normal. They are simply immature red blood cells which will mature. Holly jolly bodies, nucleated red blood cells, and Heinz bodies all indicate pathological findings. 151) (C) The most common type of cerebral aneurysm is a saccular aneurysm. Saccular aneurysms account for 80% to 90% of all intracranial aneurysms. Image: Types of aneurysms 152) (D) In a dissecting aneurysm, blood collects under an intact outer layer of the blood vessel. The outer layer of a blood vessel is called the adventitia. The middle layer is called the media. The inner layer is called the intima. In a dissecting aneurysm, blood pours through the 2 inner layers and collects in the outer layer, the adventitia. 153) (C) An aneurysm is widening or ballooning of a blood vessel that is 50% or more of the normal blood vessel diameter (source: patient.info). 154) (C) A fusiform aneurysm balloons out from all sides of the blood vessel. 155) (B) A pseudoaneurysm is a false aneurysm. The blood vessel itself is not actually ballooned out. Instead, there is just a hematoma that forms on the blood vessel as a result of injury to the blood vessel wall. This hematoma gives the appearance of an aneurysm, though it is not. 156) (B) The most common place in the body for an aneurysm to occur is in the aorta; this type of aneurysm is called an aortic aneurysm. 157) (B) The most common type of aneurysm is an abdominal aortic aneurysm. 158) (C) The ankle brachial index measures the ratio of the blood pressure of the ankle over the blood pressure of the arm. 159) (D) The ankle brachial index is a metric that is used to determine if a person has peripheral arterial disease (PAD). 160) (B) All the major cardiovascular societies advise that the ankle brachial index should be measured in every smoker over 50 years old, every diabetic over 50 years old, and all patients over 70 years old. 161) (C) A positive finding for the ankle brachial index test is the blood pressure in the ankle is less than the blood pressure in the arm. This shows that there is narrowing of the arteries in the lower extremities of the body, which indicates peripheral arterial disease. 162) (C) A score of 0.9 or less is indicative of peripheral arterial disease. The ankle brachial index is a metric of the ratio of the blood pressure of the ankle over the blood pressure of the arm. In healthy conditions, the blood pressures should be about equal, meaning there should be a 1:1 ratio. If the blood pressure at the ankle is less than the blood pressure at the arm, then this means there is narrowing of the arteries in the lower extremities (peripheral arterial disease). A score of 0.9 or less is indicative of peripheral arterial disease (source: webmd.com). 163) (A) Vitamin C deficiency is also referred to as scurvy. 164) (B) Symptoms of vitamin C deficiency include easy bruising, bleeding gums, weakness, and fatigue. Vitamin D deficiency, not C, would lead to osteomalacia, which is a poorly mineralized skeletal matrix (source: patient.info). 165) (D) Myelodysplastic syndromes are a group of bone marrow disorders in which the bone marrow does not produce enough healthy blood cells. It is often referred to as a “bone marrow failure disorder” (source: mds-foundation.org). 166) (B) Myelodysplastic syndromes (MDS) can affect all types of blood cells produced by the bone marrow. Low blood cell counts, referred to as cytopenias, are a hallmark feature of myelodysplastic syndromes. This includes low red blood cells (anemia), low white blood cells (leukopenia), and low platelets (thrombocytopenia). Thus, a person with MDS is at risk for anemia, infection, and easy bruising and spontaneous bleeding. In addition, about 30% of patients with MDS will progress to acute myeloid leukemia (AML). Most people with MDS are the elderly population. MDS is an acquired illness; it is not inherited (source: mdsfoundation.org). 167) (B) Though both serum amylase and lipase are normally examined when diagnosing a patient with pancreatitis, serum lipase is the more common and accurate of the 2 tests. Serum amylase determination is routinely available, but it is not as specific for pancreatitis; elevations of amylase are common in a host of other conditions. Elevated lipase levels are more specific to the pancreas. And lipase stays elevated in the body longer than amylase. While amylase levels generally decrease in a few days (normally around 5 days), lipase levels can stay elevated much longer (about 12 days). With acute pancreatitis, both serum amylase and lipase levels are at least 3 times above the normal reference range. 168) (B) With acute pancreatitis, serum amylase and lipase levels are typically at least 3 times the normal reference range. 169) (D) A positive antinuclear antibody (ANA) titer is specific to systemic lupus erythematosus (SLE), as well as other types of autoimmune diseases. However, an ANA titer isn’t diagnostic of SLE; other tests must also be conducted to definitively diagnose it. 170) (D) C-reactive protein (CRP) is the amount of protein called C-reactive protein in the blood; it measures general levels of inflammation in the body. The erythrocyte sedimentation rate (ESR) is the rate at which blood cells sediment (sink to the bottom of the test tube) in a period of 1 hour; it is also used to detect inflammation in the body. CRP changes more quickly than ESR as the patient’s condition improves or worsens, so it’s a timelier source of data. 171) (A) The normal ESR for men is 0-22 mm/hour. 172) (A) The normal ESR for women is 0-29 mm/hour. 173) (A) A normal CRP test cannot detect CRP levels below 10.0 mg/L. A high sensitivity CRP test can detect levels below 10.0 mg/L. This kind of test is performed to determine a person’s risk for cardiovascular disease. High-sensitivity C-reactive protein (hs-CRP) levels that represent a low risk for developing cardiovascular disease are those below 1.0 mg/L. A person is at average risk for developing cardiovascular disease if the levels are between 1.0 mg/L and 3.0 mg/L. A person is at high risk for cardiovascular disease if the hs-CRP levels are higher than 3.0 mg/L. 174) (A) Creatine kinase (CK) is the most important lab value to monitor for a patient who is taking statins and who has complaints of muscle pains. ESR, AST, and CRP are non-specific indicators of inflammation. Creatine kinase is more specific to the muscles and high levels would indicate muscle damage. 175) (A) Alkaline phosphatase levels are elevated in bone disease. Gamma-glutamyl transferase levels, ALT levels, and bilirubin levels will not be elevated in bone disease. 176) (B) Idiopathic thrombocytopenic purpura (ITP) is a disorder that can lead to easy or excessive bruising and bleeding. The bleeding results from an unusually low level of platelets (thrombocytopenia). Children often develop ITP after a viral infection and usually recover fully without treatment. In adults, the disorder is often long term. ITP is caused by the immune system attacking and destroying platelets. Why this happens is unknown, so this is why this disorder is considered idiopathic. In people with ITP, the bone marrow will be normal because a low platelet count is caused by the destruction of platelets in the bloodstream and spleen — not by a problem with the bone marrow. Women are two to three times more likely to develop ITP than men are. A rare complication of idiopathic thrombocytopenic purpura is bleeding into the brain, which can be fatal (source: mayoclinic.org). 177) (B) An embolus is a broad term of any blockage material in a blood vessel, which includes thrombi, fat globules, air bubbles, gas embolisms, or foreign materials. A thrombus is a blood clot that forms a blockage in a blood vessel. An embolism that is a piece of thrombus is termed a thromboembolism. 178) (B) D-dimer is the most useful and specific test for diagnosing disseminated intravascular coagulation (DIC). A positive test gives strong evidence for DIC. D-dimer is a test that detects a protein that results from clot break-down; it is often markedly elevated with DIC. If the D-dimer is normal, then DIC is unlikely. Other lab values that are useful in DIC is prothrombin time (PT), which is often prolonged with DIC. PTT may also be prolonged. The serum fibrinogen level may also be checked; fibrinogen is a protein that helps the blood clot. In DIC, fibrinogen is often decreased (source: patient.info). 179) (B) Although it can be normal to have some protein in the urine without any pathology being present, proteinuria is the term that refers to the presence of excess proteins in the urine. Proteinuria occurs due to damage to the kidneys. Because the kidneys are responsible for filtering the urine, it is the organ responsible for not allowing proteins to be filtered into the urine. If they are (in excessive amounts), this is indicative of kidney damage. 180) (D) Creatinine clearance is the measure of the amount of creatinine the kidneys are able to clear in a 24-hour period. 181) (B) The kidneys are the organs that are responsible for removing creatinine from the body; so, creatinine clearance is a measure of kidney function. 182) (B) A vitamin B6 level of 4.1 ng/mL would explain a patient’s peripheral neuropathy. The normal reference range for vitamin B6 is 5-30 ng/mL. A value of 4.1 ng/mL is low and normally manifests as peripheral neuropathy in a person. A vitamin B12 value of 500 pg/mL is normal; above 250 pg/mL in the United States is considered normal. The calcium and magnesium levels are also normal. 183) (C) Bilirubin is a breakdown product of red blood cells. 184) (C) Bilirubin that is attached to sugar is called direct or conjugated bilirubin. Bilirubin without sugar attached is called indirect or unconjugated bilirubin. All of the bilirubin in a person’s blood (conjugated and unconjugated) is called the total bilirubin. If bilirubin is not being attached to sugars or is not being adequately removed from the blood, it can mean that there is damage to the liver or liver disease (source: healthline.com). 185) (C) The woman having a ferritin level of 100 ng/mL and a TIBC of 300 µg/dL represents a normal range. Normal levels of ferritin for adults is 12-150 ng/mL in women (12-300 ng/mL in men). The normal range for Total Iron-Binding Capacity (TIBC) is 240-450 µg/dL. 186) (B) Protein or foods that are high in protein most affect blood urea nitrogen levels. Eating foods such as meats (high in protein) would elevate BUN levels more than a predominantly carbohydrate food (such as potatoes) or a predominantly fat food (such as avocadoes). 187) (C) If a patient’s INR is between 5 and 9, without any evidence of bleeding, then the next 1 to 2 doses of warfarin should be omitted and the patient’s INR should be evaluated in 24-48 hours. When the INR is < 5, warfarin should be resumed at an appropriate maintenance dose and then the INR should be reevaluated in 3-5 days. 188) (D) G6PD deficiency, standing for glucose-6-phosphate dehydrogenase deficiency, causes hemolytic anemia. The enzyme, G6PD, helps protect red blood cells from damage and premature destruction. With a deficiency of this enzyme, the red blood cells are more prone to premature destruction. The condition is triggered when the body is exposed to certain drugs, severe stress, infections, or certain foods (such as fava beans) (source: medlineplus.gov). 189) (D) People with G6PD deficiency have attacks when they are exposed to triggers. This can include being exposed to drugs such as aspirin or nitrofurantoin. This also can include infections, stress, or certain foods. The attacks are not regular or daily (unless exposed to triggers daily). G6PD deficiency is an inherited condition. It is seen more in men than in women. And it is most commonly seen in blacks and people of Middle Eastern descent (source: medlineplus.gov). 190) (A) Symptoms of G6PD deficiency anemia include tachycardia, shortness of breath, pallor, fatigue, jaundice, enlarged spleen (splenomegaly) and dark urine (source: medlineplus.gov). 191) (C) A person with G6PD deficiency must strictly avoid things that can trigger an episode of hemolytic anemia. This can include certain drugs, severe stress, infections, or certain types of foods. Being exposed to triggers can cause episodes of hemolytic anemia. Usually hemolytic episodes go away on their own. Rarely, kidney failure or death may occur following a severe hemolytic event (source: medlineplus.gov). 192) (B) A person with G6PD deficiency can safely take acetaminophen. Drugs that have been linked to hemolytic episodes associated with G6PD deficiency are antimalarial drugs, NSAIDs, quinidine, quinine, and sulfa drugs (source: medlineplus.gov). 193) (B) Polycythemia vera is characterized by a hematocrit value greater than 52% in men or 47% in women. 194) (C) Symptoms of polycythemia vera include headaches, poor concentration, fatigue, dizziness, and dyspnea. 195) (D) Polycythemia vera is a blood cancer that begins in the marrow of the bones. With polycythemia vera, the bone marrow makes too many red blood cells, which causes the blood to get too thick. This makes it more likely to develop blood clots, a stroke, or a heart attack. This disease develops very slowly, usually over many years. Most people find out that they have this condition when they’re 60 or older. This condition is more common among men than women. Although it can be life-threatening if the proper treatment isn’t given, most people have a good chance of living a long life when given the right care (source: webmd.com). 196) (A) Polycythemia vera is a genetic condition. Polycythemia vera cannot be transmitted sexually, through blood, or through saliva. It’s something that’s obtained when a gene called JAK2 doesn’t work right. This gene is responsible for making sure the bone marrow doesn’t make too many blood cells. The bone marrow makes three types of blood cells: red blood cells, white blood cells, and platelets. Most people with polycythemia vera have too many red blood cells. But the disease can also cause a person to have too many white blood cells and/or platelets as well. It’s rare, but parents can pass this broken gene to children at birth. More likely, however, a problem develops with the JAK2 gene over the course of the person’s life (not a problem obtained directly at birth) (source: webmd.com). 197) (B) Complications of polycythemia vera make it more likely for a person to form blood clots, have a stroke, or a heart attack. Polycythemia vera may develop into acute myelogenous leukemia (AML) or idiopathic myelofibrosis (source: webmd.com & cancer.ca). 198) (B) People with polymyalgia rheumatica are at high risk for temporal arteritis. There is no direct link between polymyalgia rheumatica and rheumatoid arthritis. Polymyalgia rheumatica is a condition that causes muscle pain and stiff joints, especially in the shoulders and hips. Polymyalgia rheumatica mostly affects those 50 years or older. Mostly women are affected with polymyalgia rheumatica. Women are about two times more likely to develop the disorder. 199) (D) Temporal arteritis, also known as giant cell arteritis, is an autoimmune disease. In temporal arteritis, immune cells are involved in an inflammatory reaction in large arteries of the body, mainly branches of the aorta and, often, the aorta itself. The inflammation damages the affected blood vessels. Thus, temporal arteritis is a type of vasculitis (vasculitis is defined as a condition in which blood vessels, particularly arteries, become inflamed). At present, the exact cause of temporal arteritis is unknown. Temporal arteritis is the most common form of vasculitis in patients over the age of 50 years. For reasons that are not clear, temporal arteritis is 2 to 3 times more common in women than in men. The condition is most commonly seen in people of northern European descent (source: vasculitisfoundation.org). 200) (A) A temporal artery biopsy is the definitive test used to confirm temporal arteritis. If signs of inflammation are seen in the sample of the temporal artery taken, this is a positive sign for temporal arteritis. 201) (D) Steroids is the main medication class used to treat temporal arteritis. Since temporal arteritis is an autoimmune disorder, steroids help to suppress the immune response, thereby decreasing symptoms. 202) (B) Hypertension is not a common symptom of temporal arteritis. Common symptoms of temporal arteritis include headaches, jaw pain, vision loss, fever, and fatigue. 203) (D) Temporal arteritis is seen most commonly in elderly women. It rarely affects people aged under 50 years. Women are more commonly affected than men. 204) (C) The laboratory hallmark of giant cell arteritis (GCA) is an elevation in the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level. The ESR usually exceeds 50 mm/h and may exceed 100 mm/h, but may be normal in 7-20% of patients with GCA. Therefore (when diagnosing GCA), a normal ESR does not rule out the condition, and the level of elevation of ESR does not correlate reliably with the severity of the disease (when monitoring the disease). This is because normal values of ESR are known to increase with age and are higher in women, so the ESR should be adequately adjusted. Other studies must be taken into consideration for monitoring GCA (source: emedicine.medscape.com). 205) (A) Upon palpating the scalp of a person with temporal arteritis, an expected finding would be tenderness of the temporal artery. There would be decreased throbbing of the temporal artery. 206) (D) Besides affecting the temporal artery, temporal arteritis may also affect the ophthalmic artery, causing vision problems. In fact, the most severe complication of temporal arteritis is blindness. GCA may affect also the occipital, vertebral, posterior ciliary, and proximal vertebral arteries (source: vasculitisfoundation.org & emedicine.medscape.com). 207) (C) Once there is strong supporting evidence that a person has temporal arteritis, treatment should be given right away. Being that temporal arteritis is an autoimmune disorder, prednisone, a steroid, is given to calm the immune response. This can halt damage to the temporal and ophthalmic arteries, as well as other arteries that temporal arteritis may affect. 208) (B) Hyperaldosteronism causes metabolic alkalosis, not metabolic acidosis. This is because aldosterone helps to reabsorb sodium and excretes potassium and hydrogen. The loss of hydrogen ions causes metabolic alkalosis. Being that aldosterone causes sodium retention, sodium (along with water) are retained. This extra fluid retention causes an increase in blood pressure. The sodium retention causes hypernatremia. Again, aldosterone causes the excretion of potassium (along with hydrogen), so this causes hypokalemia. 209) (C) The most common cause of primary hyperaldosteronism is an adrenal adenoma. An adrenal adenoma is a benign tumor on the adrenal gland (epithelial cells of the adrenal gland) that causes the adrenal gland to produce too much aldosterone. This causes symptoms like high blood pressure, hypernatremia, and hypokalemia. 210) (D) There are a few medications that are used to treat hyperaldosteronism. Antihypertensive medications will be used because hyperaldosteronism causes hypertension. Calcium channel blockers are normally used to control the blood pressure. Because hyperaldosteronism causes hypokalemia, potassium supplements are normally prescribed. Also, due to the hypokalemia, potassium-sparing diuretics are often used. Spironolactone is a potassium-sparing diuretic, so it increases the potassium levels of the person, while wasting away the excess sodium. Potassiumwasting diuretics such as loop diuretics would make the client’s condition worse and should not be given; this would further increase the risk of hypokalemia in the patient, which could cause heart arrhythmias. A thing to note is that the patient’s potassium levels should be checked regularly, because the combination of potassium supplements and potassium-sparing diuretics could cause hyperkalemia. 211) (B) Cavernous sinus thrombosis is a blood clot inside the cavernous sinus. The cavernous sinus is a cavity at the base of the brain that contains veins and nerves, as well as other structures. 212) (A) A bacterial infection is the most likely cause of cavernous sinus thrombosis. Cavernous sinus thrombosis is typically caused by a sinus infection that has spread from beyond its origin to the cavernous sinus. To contain the infection, the body’s immune system creates a clot to prevent bacteria or other pathogens from spreading. The clot leads to a backup of blood outflow from the brain and causes increased pressure inside of the brain. This increased pressure can damage the brain and can cause death. 213) (C) Cavernous sinus thrombosis is a serious condition that can be fatal. In fact, it is fatal up to about 30% of the time. The blood clot that forms in the cavernous sinus can cause a backup of blood in the brain, which causes increased intracranial pressure. This can damage the brain and can cause death. 214) (D) Possible symptoms of cavernous sinus thrombosis include severe headaches accompanied by a high fever, a bulging eye ball, inability to move the eye in a certain direction, especially in the lateral direction, vision loss, pain, and numbness around the face and eyes. It can also cause seizures. The fever associated with cavernous sinus thrombosis is generally a high-grade fever, as most of the times the etiology is an acute bacterial infection. 215) (C) Cavernous sinus thrombosis is treated primarily with high-dose antibiotics. Most of the times, a bacterial infection, usually staphylococcus aureus, is the cause of cavernous sinus thrombosis. Therefore, high-dose antibiotics are used for treatment. The antibiotics are normally given through an IV drip. Corticosteroids may be used to reduce swelling. And sometimes anticoagulants may be given. However, the primary treatment is high-dose antibiotics. 216) (D) In iron-deficiency anemia, RDW values are elevated in virtually all cases. The normal range for RDW(-CV) is 11.6-14.6%. A value above this range, such as 14.9%, suggests irondeficiency anemia. Chapter 4- Integumentary and HEENT 1) What is herpes keratitis? A) B) C) D) A viral infection of the mouth A viral infection of the eye A viral infection of the eyebrows A viral infection of the throat 2) All of the following are symptoms of herpes keratitis except for: A) B) C) D) Eye pain Retinal detachment Photophobia Blurred vision 3) Which of the following can be used to diagnose herpes keratitis? A) B) C) D) Tonometry Fluorescein eye stain Snell’s vision test Red Light Reflex test 4) Which of the following is false regarding acute angle-closure glaucoma? A) Acute angle-closure glaucoma is an ophthalmic emergency B) The patient should assume the supine position for as long as possible C) Treatment of acute angle-closure glaucoma consists of reducing the intraocular pressure (IOP) of the patient D) Acute angle-closure glaucoma causes painless vision loss 5) Which of the following symptoms is associated with acute angle-closure glaucoma? A) Sudden increase in eye pain and intraocular pressure B) Sudden increase in intraocular pressure without pain C) Gradual increase in intraocular pressure with increasing pain D) Gradual increase in intraocular pressure without pain 6) Which of the following symptoms is associated with open-angle glaucoma? A) Sudden increase in eye pain and intraocular pressure B) Sudden increase in intraocular pressure without pain C) Gradual increase in intraocular pressure with increasing pain D) Gradual increase in intraocular pressure without pain 7) Which of the following is false regarding open-angle glaucoma? A) Open-angle glaucoma occurs gradually B) Open-angle glaucoma initially leads to a loss of central vision C) Open-angle glaucoma makes up over 80% of all cases of glaucoma D) Screening for open-angle glaucoma can be done with tonometry 8) What is a peritonsillar abscess? A) A condition in which the tonsils are inflamed B) A condition in which pus collects around the tonsils C) A condition in which the blood supply to the tonsils decrease D) A condition in which the white blood cells of a person’s body attacks the tonsils, damaging it 9) What is the most common causative agent of a peritonsillar abscess? A) B) C) D) E. coli Haemophilus influenza Group A strep bacteria Group B strep bacteria 10) All of the following are symptoms of a peritonsillar abscess except for: A) Vomiting B) Sore throat C) Fever D) Odynophagia 11) What is the first-line treatment for a peritonsillar abscess? A) B) C) D) Antibiotics Antivirals Incision and drainage Lemon glycerin swabs 12) A peritonsillar abscess is a complication of: A) B) C) D) Laryngitis Acute otitis media Acute otitis externa Tonsillitis 13) What is diphtheria? A) A benign viral infection usually affecting the mucous membranes of the nose and throat B) A serious viral infection usually affecting the mucous membranes of the nose and throat C) A benign bacterial infection usually affecting the mucous membranes of the nose and throat D) A serious bacterial infection usually affecting the mucous membranes of the nose and throat 14) All of the following are symptoms of diphtheria except for: A) B) C) D) Sore throat Sunken lymph nodes Fever Markedly swollen neck (bullneck) 15) Which of the following statements regarding diphtheria is false? A) Diphtheria is very contagious B) Diphtheria is common in the United States C) Diphtheria normally coats the posterior pharynx, tonsils, uvula, and soft palate with a gray-to-yellow-colored pseudomembrane that is hard to displace D) Diphtheria normally produces a low-grade fever in a person 16) Molluscum contagiosum is mostly seen in: A) B) C) D) Children Adolescents Young adults The elderly 17) Which statement is false regarding leukoplakia? A) Leukoplakia is a definitive sign of oral cancer B) Patients with a history of chewing tobacco are at high risk for having leukoplakia C) Leukoplakia produces white patches that form on the gums, insides of the cheeks, bottom of the mouth, or tongue that cannot be scraped off D) Alcohol is a risk factor for leukoplakia 18) What should be done with an avulsed tooth? A) B) C) D) Store it in water at room temperature Store it on a very cold surface such as ice Store it by itself in a plastic bag Store it in milk 19) All of the following are causes of papilledema except for: A) B) C) D) A brain tumor A brain abscess A head injury Cluster headaches 20) All of the following are risk factors for cataracts except for: A) B) C) D) Chronic steroid use Long-term statin use Anorexia nervosa Diabetes 21) Which of the following statements is false regarding a pterygium? A) A pterygium is an overgrowth of scar tissue that forms over the conjunctiva of the eye B) A pterygium is non-cancerous C) A pterygium is normally triangular-shaped D) A pterygium is typically found on the area of the eyes closest to the ears 22) Common symptoms of a pterygium include all of the following except for: A) B) C) D) A gritty feeling in the eye Temporary blindness Blurred vision Eye itching 23) Which person would be at highest risk for getting a pterygium? A) B) C) D) Surfer Receptionist Nurse Dentist 24) Treatment for pterygia may include all of the following except for: A) B) C) D) Artificial tears Topical antibiotics Lubricating ointments Topical corticosteroids 25) Which of the following statements is false regarding a pinguecula? A) Dust exposure is the most common cause of pingueculas B) A pinguecula is a yellowish patch on the conjunctiva of the eye C) Pterygia are often preceded by pingueculas D) A pinguecula is a change in the normal tissue of the eye that results in a deposit of protein, fat and/or calcium on the eye 26) Pingueculas and pterygia are both most often caused by: A) B) C) D) Ultraviolet light damage Cataracts Bacterial infection Viral infection 27) What is the normal range for intraocular pressure (IOP)? A) B) C) D) 5 to 10 mmHg 12 to 21 mmHg 21 to 27 mmHg 27 to 34 mmHg 28) What is dacryostenosis? A) B) C) D) Blocked sweat glands in the skin Nasolacrimal obstruction A blocked pituitary gland A blocked pineal gland 29) Which statement is false regarding congenital dacryostenosis? A) Congenital dacryostenosis often resolves spontaneously by about age 6 to 9 months B) Reflux of saline or fluorescein dye when flushing the lacrimal drainage system confirms the diagnosis of dacryostenosis C) Green-colored purulent eye discharge is a common symptom of dacryostenosis D) Manual compression of the lacrimal sac 4 or 5 times a day may relieve the obstruction 30) What is dacryocystitis? A) B) C) D) Infection of the eye Infection of the sweat glands located near the eyes Infection of the lacrimal sac Infection of the nasal passages 31) What is the most common treatment for acute dacryocystitis? A) B) C) D) Antibiotics Dacryocystorhinostomy Cold compresses Antivirals 32) What is the most common cause of dacryocystitis? A) B) C) D) Chlamydial conjunctivitis Sinusitis Dacryostenosis Rhinorrhea 33) All of the following are common in the early and middle stages of age-related macular degeneration except for: A) B) C) D) Painless central vision loss Straight lines appear distorted Peripheral vision deteriorates rapidly Blurred vision 34) All of the following statements are true regarding age-related macular degeneration (AMD) except: A) Macular degeneration is the third most common cause of vision loss in the United States after glaucoma and cataracts B) The dry form of age-related macular degeneration is more common C) The wet form of age-related macular degeneration accounts for about 80% of vision loss in cases of macular degeneration D) Smoking is a major risk factor for age-related macular degeneration 35) What is blepharitis? A) Inflammation of the iris of the eye B) Inflammation of the cornea of the eye C) Inflammation of the lacrimal duct D) Inflammation of the eyelids 36) Which of the following is false regarding blepharitis? A) Blepharitis is most often a chronic condition B) Blepharitis usually does not cause permanent vision problems C) Blepharitis is highly contagious D) Blepharitis commonly occurs when tiny oil glands located near the base of the eyelashes become clogged 37) Symptoms of blepharitis include all of the following except: A) B) C) D) Red, swollen eyelids Eyelashes that grow abnormally A burning sensation in the eyes Less frequent blinking 38) All of the following may be used to treat blepharitis except for: A) B) C) D) Eyelid scrubs Steroid eye drops or ointments Topical antibiotics Alcohol swabs 39) All of the following are true regarding strep throat except: A) Strep throat is caused by group A strep bacteria B) Strep throat can lead to either rheumatic fever or scarlet fever C) Strep throat can lead to impetigo D) Strep throat can lead to hemolytic uremic syndrome 40) Treatment for a strep throat may include all of the following except for: A) Prednisone B) Penicillin as a first-line treatment C) Ibuprofen or acetaminophen for throat pain and fever D) Throat lozenges 41) All of the following statements are true about otitis externa except: A) Otitis externa is more common during warm and humid weather B) Otitis externa is usually a fungal infection C) Otitis externa normally involves swimming or any activities in which the ears get wet D) Otitis externa is usually a short-term condition that resolves within days to weeks 42) All of the following are common symptoms of otitis externa except for: A) Ear pain with manipulation of the external ear or tragus B) Rhinitis C) Some hearing loss D) Erythematous and swollen ear canal 43) What is the most common treatment for otitis externa? A) B) C) D) Cortisporin otic drops Normal saline ear irrigation Oral griseofulvin Oral acyclovir 44) Which of the following statements is false regarding otitis media with effusion (OME)? A) OME is a type of ear infection of the middle ear B) OME occurs most often in children under age 2, but is rare in newborns C) OME often does not have obvious symptoms D) OME most often goes away on its own over a few weeks or months; however, treatment may speed up this process 45) All of the following are common symptoms of infectious mononucleosis except for: A) B) C) D) Fatigue Paroxysmal coughing Acute pharyngitis Lymphadenopathy 46) Mononucleosis is most often spread through: A) B) C) D) Blood Respiratory secretions Saliva Stool 47) Treatment for mononucleosis includes all of the following except for: A) B) C) D) Rest Antibiotics Fluids OTC PRN fever and pain medication 48) All of the following tests are indicated for checking for suspected infectious mononucleosis except for: A) B) C) D) Heterophile antibody test CBC Palpation of cervical nodes Rapid Plasma Reagin 49) Infectious mononucleosis can produce all of the following complications except for: A) Splenomegaly/splenic rupture B) Hepatomegaly C) Heart failure D) Blood dyscrasias 50) All of the following statements are true regarding Lyme disease except: A) Lyme disease is spread by the bite of a deer tick B) Lyme disease produces flu-like symptoms C) Lyme disease can produce a “bulls-eye” rash that usually appears within 1-2 weeks after infection D) Lyme diseases produces a soft-textured rash 51) All of the following are prevention methods to prevent Lyme disease except for: A) Wearing long sleeve clothing B) Avoiding areas of known tick infestation C) Wearing bright colors D) Putting on insect repellant containing deet 52) Lyme disease is treated with: A) B) C) D) Antibiotics Antivirals Antifungals Antiparasitics 53) All of the following drugs are commonly associated with the onset of Stevens-Johnson syndrome except for: A) B) C) D) Sulfas Penicillins Proton pump inhibitors Barbiturates 54) All of the following statements regarding Stevens-Johnson syndrome are true except for: A) Stevens-Johnson syndrome has a mortality rate of 25% or higher B) Although Stevens-Johnson syndrome can be caused by viral infections and malignancies, the most common cause is medications C) Stevens-Johnson syndrome is a life-threatening skin condition in which cell death causes the epidermis to separate from the dermis D) Once the underlying cause is removed, Stevens-Johnson syndrome normally resolves within 24 hours 55) All of the following are common offenders in contact dermatitis except for: A) B) C) D) Poison ivy Perfumes or colognes Cotton Nickel 56) All of the following are common treatments for contact dermatitis except: A) B) C) D) Stopping exposure to the substance Calamine lotion Deodorants Oatmeal baths 57) What is the most common skin condition in the world? A) B) C) D) Rosacea Acne Eczema Psoriasis 58) What is hidradenitis suppurativa? A) A chronic skin condition of the sebaceous glands that produces small painful lumps commonly in the armpits or groin B) A chronic skin condition that is characterized by small circular red macules throughout the body C) A chronic skin condition of the epidermis that produces small black rashes throughout the body D) A chronic skin condition characterized by yellow plaques that appear around the eyelids 59) What is a chalazion? A) A condition characterized by yellow flat plaques over the upper or lower eyelids. B) A benign, painless bump or nodule inside the upper or lower eyelid C) Inflammation of the eyelid that affects the eyelashes or tear production D) Irritation and swelling of the mucous membrane in the nose 60) Which of the following statements is false regarding a chalazion? A) The bump that characterizes a chalazion is caused by a blockage of the Meibomian gland on the eyelid B) Chalazia are typically very painful C) Most chalazia heal within one month, either with no treatment or simple home care D) A chalazion may cause blurry or blocked vision 61) What is a cholesteatoma? A) An abnormal skin growth in the middle ear behind the eardrum B) An abnormal skin growth in the middle of the nose C) An abnormal skin growth in the eye pouch D) An abnormal skin growth in the eyebrow 62) What is a risk factor for cholesteatomas? A) History of chronic otitis media infections B) History of frequent conjunctivitis infections C) History of frequent episodes of rhinitis D) History of laryngitis 63) Treatment for cholesteatomas includes: A) Antiviral medications and surgical removal B) Antifungal medications and surgical removal C) Antibiotics and surgical removal D) Antiparasitic medications and surgical removal 64) What is Sjögren’s Syndrome? A) A type of cancer that attacks the adrenal glands B) An autoimmune disease that attacks the kidneys C) An autoimmune disease characterized by decreased function of the lacrimal and salivary glands D) A gastrointestinal illness that destroys the parietal cells in the stomach 65) What is hordeolum? A) A painful canker sore normally found in the roof of the mouth B) An acute infection of either the external or internal eyelid C) An acute infection of the eyebrows that causes painful red rashes D) An acute infection of nose that makes breathing difficult 66) All of the following are common symptoms of a hordeolum except: A) B) C) D) Watery eyes Puffy eyes Darkened eyelids Eyelid tenderness 67) All of the following are treatments for a hordeolum except for: A) B) C) D) Warm soaks or compresses Drainage Cold compresses Eyelid hygiene (lid scrubs) 68) What type of medication is used to treat a hordeolum? A) B) C) D) Antivirals Topical antibiotics Antifungals Antiparasitic drugs 69) How long does a hordeolum normally last? A) A hordeolum is a lifelong illness B) A hordeolum normally resolves in 1-2 days C) A hordeolum is self-limiting and normally resolves spontaneously in 1-2 weeks D) A hordeolum is self-limiting and normally resolves in 2-3 months 70) What is impetigo? A) A highly contagious bacterial infection that affects the superficial layers of the epidermis of the skin B) A noncontagious bacterial infection that affects the superficial layers of the epidermis of the skin C) A highly contagious bacterial infection that affects the subcutaneous layer of the skin D) A noncontagious bacterial infection that affects the subcutaneous layer of the skin 71) What bacteria make up the vast majority cases of impetigo? A) Listeria monocytogenes B) E. coli C) Clostridium botulinum D) Streptococcus pyogenes and Staphylococcus aureus 72) What is bullous impetigo? A) Impetigo that is characterized by red rashes B) Impetigo that is characterized by bubblelike cavities filled with air or fluid C) Impetigo that is characterized by pressure ulcers D) Impetigo that is characterized by black stretch marks 73) What group is impetigo most commonly seen in? A) B) C) D) Toddlers Teenagers Middle-aged adults The elderly 74) What is onychomycosis? A) A bacterial infection of the toenail or fingernail B) A viral infection of the toenail or fingernail C) A fungal infection of the toenail or fingernail D) A parasitic infection of the toenail or fingernail 75) What is the common and preferred treatment for onychomycosis? A) B) C) D) Topical antifungals Topical antibiotics Oral antifungals Oral antibiotics 76) Which of the following statements is false regarding hordeola and chalazia? A) A hordeolum and a chalazion are both lumps that are formed in or on the eyelid B) A hordeolum is an infected lump, while a chalazion is a noninfected lump C) Both chalazia and hordeola are usually very painful conditions D) A hordeolum is usually caused by a bacterial infection, while a chalazion is caused by a clogged oil gland 77) Rocky Mountain Spotty Fever is caused by the bite of what? A) B) C) D) Mosquito Tick Wasp Dragonfly 78) All of the following are common symptoms of Rocky Mountain Spotted Fever except for: A) B) C) D) Headache Myalgia Weight gain Malaise 79) Rocky Mountain Spotted Fever is most common during: A) B) C) D) The late fall to early winter The late winter to early spring The spring to early summer The summer to early fall 80) How is Rocky Mountain Spotted Fever diagnosed? A) B) C) D) Cerebrospinal fluid Muscle biopsy Serum antibody titers Liver function tests 81) What question is most pertinent for a healthcare provider to ask a person who is suspected of having Rocky Mountain Spotted Fever? A) Did you eat any raw meat in the last few days? B) Have you traveled to any foreign countries recently? C) Have you been sexually active with multiple partners recently? D) Have you been camping or in the woods recently? 82) What type of infection is Rocky Mountain Spotted Fever? A) B) C) D) Viral Bacterial Fungal Parasitic 83) What is the first-line treatment for Rocky Mountain Spotted Fever? A) B) C) D) Amoxicillin Penicillin Erythromycin Doxycycline 84) What is paronychia? A) An infection of the tissue folds around the nails B) An infection of the tissue around the eyebrows C) An infection of the tissue around the eyes D) An infection of the tissue around the mouth 85) Paronychia can be described as all of the following except for: A) B) C) D) Red Swollen Painless Painful 86) All of the following statements are true regarding paronychia except: A) Paronychia is most often caused by injury or trauma to the affected surrounding nail tissue, which can create a break in the skin that allows the entry of pathogens B) Paronychia can be caused by bacteria or fungi C) Paronychia may cause pus-filled blisters in the infected area D) Paronychia doesn’t affect the nail itself but only the tissue folds around the nail 87) Treatment for paronychia may include all of the following except for: A) Cold soaks of affected parts for 20 minutes 3 times a day B) Topical antibiotic application to the affected area C) Incision and drainage if an abscess is present D) Warm soaks of affected parts for 20 minutes 3 times a day 88) Chronic cases of paronychia are associated with coexisting: A) B) C) D) Subconjunctival hemorrhage Onychomycosis Subungual hematoma Tinea manuum 89) Herpetic whitlow is a viral infection of the: A) B) C) D) Fingers Toes Eyebrows Eyelids 90) Which of the following viruses causes most cases of herpetic whitlow? A) B) C) D) Herpes simplex virus I Herpes simplex virus II Cytomegalovirus (CMV) Astrovirus 91) All of the following statements are true regarding chickenpox (varicella) and herpes zoster (shingles) except: A) Both chickenpox (varicella) and herpes zoster (shingles) are caused by the same virus, the varicella-zoster virus B) Primary infection of the varicella-zoster virus is called varicella C) The reactivation of the varicella-zoster viral infection is known as shingles D) After primary infection, the varicella-zoster virus becomes latent within the subcutaneous tissue 92) All of the following statements are true regarding chickenpox except: A) The prodromal period of chickenpox in adults is characterized by fever and malaise B) The rashes in chickenpox progresses from red bumps (papules) to fluid-filled blisters (vesicles) to vesicles that drain and scab over (scabbed lesions) C) The rashes start on the head/face and quickly spread to the trunk and extremities D) The rashes in chickenpox are all at the same stage and all crust over together 93) Varicella is contagious from 1 to 2 days before the onset of rash up until: A) 1 week after the prodromal period B) 2 weeks after the prodromal period C) 1 week after the onset of rash D) All lesions have crusted over 94) All of the following can be potential complications of shingles except for: A) B) C) D) Huntington disease Post-herpetic neuralgia (PHN) Herpes zoster ophthalmicus Ramsay Hunt syndrome 95) Postherpetic neuralgia is best described as: A) A complication of shingles that causes such damage to nerve fibers that pain can’t be felt long after the rash and blisters of shingles disappear B) A complication of shingles that affects nerve fibers and skin, causing burning pain that lasts long after the rash and blisters of shingles disappear C) A complication of shingles that affects the myelin sheath of the central nervous system, causing demyelination D) A complication of shingles that causes extensive damage to muscles in the arms 96) Who is post-herpetic neuralgia (PHN) more likely to be seen in? A) B) C) D) Children Teenagers Middle age adults The elderly 97) All of the following medications are commonly used to treat post-herpetic neuralgia (PHN) except for: A) B) C) D) Amitriptyline Diazepam Depakote Gabapentin 98) Symptoms of herpes zoster ophthalmicus may involve all of the following except for: A) B) C) D) A painful forehead rash Severe ocular pain Xanthelasma Eyelid edema 99) Herpes zoster ophthalmicus affects cranial nerve: A) B) C) D) II IV V VII 100) Herpes zoster ophthalmicus can lead to: A) B) C) D) Dry eye syndrome Retinal detachment Age-related macular degeneration Corneal blindness 101) Ramsay Hunt syndrome affects primarily cranial nerves: A) B) C) D) VII & VIII VIII & X X & XI XI & XII 102) What is scabies? A) B) C) D) An infection of the hair Ringworm of the scalp An infection of the skin A fungal infection of the foot 103) The causative agent of scabies is a: A) B) C) D) Wasp Mite Tick Bee 104) Which of the following statements is false regarding scabies? A) Most people get scabies from direct, skin-to-skin contact B) Anyone from any age group can get scabies C) Scabies is a chronic illness that can last for months even with treatment D) Scabies can be diagnosed by scraping off a tiny bit of skin onto a glass slide from a person and examining it under a microscope 105) What is the primary treatment for scabies? A) B) C) D) Miconazole cream Griseofulvin Permethrin 5% Isotretinoin 106) Which of the following statements is false regarding Norwegian scabies? A) Norwegian scabies is a mild form of scabies B) Norwegian scabies is referred to as crusted scabies C) Norwegian scabies is characterized by a heavy infestation of mites D) The itching is generally less with Norwegian scabies 107) How is tinea capitis (ringworm of the scalp) spread? A) B) C) D) Spread by direct contact Spread by droplets Spread by blood exchange Spread through evaporation 108) What demographic is most at risk for contracting and spreading tinea capitis? A) B) C) D) Infants School-aged children College students The elderly in a nursing home 109) Which of the following will tinea capitis not cause? A) B) C) D) Kerion Scalp itchiness Low-grade fever Whitening of the hair 110) What is the gold standard treatment for tinea capitis? A) B) C) D) Miconazole cream Griseofulvin Permethrin 5% Isotretinoin 111) What is the preferred treatment for human and animal bite wounds? A) B) C) D) Amoxicillin clavulanate Trimethoprim sulfamethoxazole Doxycycline Cephalexin 112) What is erysipelas? A) An infection of the upper dermis that typically presents with a reddened skin rash B) An infection of the subcutaneous tissue that produces lumps in various parts of the body C) An infection of the epidermis of the skin that causes psoriatic plaques on the surface of the skin D) An infection of the subcutaneous tissue that causes deeply ulcerated skin 113) Which statement is false regarding erysipelas? A) Erysipelas is more superficial than cellulitis B) Erysipelas is more raised than cellulitis C) Erysipelas is less demarcated than cellulitis D) Infected individuals with erysipelas normally develop flu-like symptoms within 48 hours of infection 114) Erysipelas is most often caused by: A) B) C) D) Group A strep bacteria Group B strep bacteria Staphylococcus aureus E. coli 115) Purple striae on the abdomen may be indicative of: A) B) C) D) Cholelithiasis Hepatitis Cholecystitis Cushing’s disease 116) What is the most common cause of blindness in the United States? A) B) C) D) Macular degeneration Cataracts Diabetic retinopathy Glaucoma 117) Which of the following statements is false regarding arcus senilis? A) Arcus senilis causes progressive deterioration in vision B) Arcus senilis is a narrow opaque band encircling the cornea C) Arcus senilis is common in old age D) Arcus senilis is caused by a deposition of fat 118) If arcus senilis is found in young adults, it is usually caused by: A) B) C) D) Cataracts Early onset glaucoma Familial hyperlipidemia Early onset glaucoma 119) What is tinea versicolor? A) B) C) D) A bacterial infection of the skin A fungal infection of the skin A viral infection of the skin A parasitic infection of the skin 120) Which statement is false regarding tinea versicolor? A) Tinea versicolor is a chronic skin condition B) Tinea versicolor is most common in cold environments such as the Great North C) Tinea versicolor is most common in adolescent boys and young adult men D) Tinea versicolor is caused by a fungus called Pityrosporum ovale which is normally found on the human skin and causes problems only in certain circumstances. 121) What is the main symptom of tinea versicolor? A) Yellowish skin with dark, scattered papules B) Blistered skin with oozing pus C) Patches of discolored skin D) Painful skin lesions 122) Tinea versicolor is treated with: A) B) C) D) Antibiotics Antifungals Antivirals Corticosteroids 123) Changes to the skin caused by tinea versicolor: A) Normally last for a few days B) Normally lasts for about 2 weeks C) Can last all year D) Are permanent; the skin changes are irreversible 124) Risk factors for tinea versicolor include all of the following except for: A) B) C) D) Hot weather Lots of sweating Oily skin Non-humid weather 125) Which statement is false regarding senile purpura? A) Senile purpura is caused by increased vessel fragility due to connective tissue damage to the dermis B) Senile purpura is a benign condition C) Senile purpura causes purple ecchymoses most commonly located on the dorsum of the forearms and hands D) Senile purpura is a precancerous condition that is a precursor to skin cancer 126) Meniere’s disease is a disorder of: A) B) C) D) The eyes The inner ear The outer ear The hypothalamus 127) Symptoms of Meniere’s disease include all of the following except for: A) B) C) D) Vertigo Tinnitus Hearing loss Tension headaches 128) Which of the following statements is false regarding Meniere’s disease? A) Meniere’s disease is an acute illness that typically lasts for a few months and then disappears B) Meniere’s disease usually starts between the ages of 20 and 50 C) Meniere’s disease can cause permanent hearing loss D) The cause of Meniere’s disease is unknown. 129) All of the following medications may be prescribed for Meniere’s disease except for: A) B) C) D) Meclizine Promethazine Hydrochlorothiazide Aspirin 130) What type of diet is often recommended for people with Meniere’s disease? A) B) C) D) A low-fat diet A high-fiber diet A low-salt diet A low-purine diet 131) What is xanthelasma? A) Purplish macules that appear on the nose B) Raised, red bumps that appear mostly near the eyelids C) Yellow plaques that occur most commonly on the eyelids D) Pink, ulcerated skin that is present on the cheeks 132) When there is no family history of xanthelasma, it is most likely due to: A) B) C) D) High blood pressure High cholesterol High serum protein High uric acid 133) Which is true regarding xanthelasma? A) It is a harmful condition that often causes secondary skin infections B) It is a very painful skin condition C) It is seen most often in children rather than adults D) It is most common with people of Asian or Mediterranean descent 134) What is xerosis? A) A skin condition in which the face is covered with yellow plaques B) A condition in which the sweat glands are overactive, causing excess amounts of sweat on the skin C) A condition in which the skin is abnormally dry D) A condition in which many red, painless bumps exist on the face 135) Xerosis is most common during the: A) B) C) D) Fall months Winter months Spring months Summer months 136) What is a cherry angioma? A) A benign red papule containing a proliferation of blood vessels B) A benign red papule containing no blood vessels C) A precancerous red papule containing a proliferation of blood cells D) A cancerous papule containing no blood vessels 137) Which is true regarding cherry angiomas? A) Cherry angiomas are unlikely to cause any health problems B) Cherry angiomas, if untreated, often lead to ulcerations in the skin C) Cherry angiomas often lead to basal cell carcinoma D) Cherry angiomas are often cancerous 138) Which of the following statements is false regarding cherry angiomas? A) Cherry angiomas are most often found in adults age 30 or older B) The exact cause of cherry angiomas is unknown C) Cherry angiomas are prone to bleeding if irritated D) Cherry angiomas are self-limiting 139) What is acanthosis nigricans? A) A skin condition causing rough, sandpaper-textured rashes throughout the body B) A skin condition characterized by cherry angiomas throughout the body C) A skin condition characterized by small black bumps mostly on the torso and groin D) A skin disorder characterized by areas of dark, velvety discoloration in body folds and creases 140) Common areas affected by acanthosis nigricans include all of the following except for the: A) B) C) D) Neck Skinfolds of the fingers Groin Armpits 141) Acanthosis nigricans is most often found in people who have: A) High cholesterol and triglyceride levels B) Diabetes or who are obese C) Hyperuricemia D) Anemia and thrombocytopenia 142) Which statement is false regarding acanthosis nigricans? A) Skin changes are the only symptom associated with acanthosis nigricans B) With acanthosis nigricans, the skin affected is very painful and inflamed C) With acanthosis nigricans, the skin may have an odor D) With acanthosis nigricans, the skin may itch 143) What treatment is used to help improve acanthosis nigricans? A) B) C) D) Antibacterial topical cream Surgical debridement of the skin Improved skin hygiene Treating the underlying condition 144) What is actinic keratosis? A) A benign skin condition characterized by scaly, crusty lesions B) A precancerous skin condition characterized by scaly, crusty lesions C) A precancerous skin condition characterized by a proliferation of ulcerations throughout the body D) A cancerous condition characterized by scaly, crusty lesions 145) What is the cause of actinic keratosis? A) B) C) D) Certain types of medications Xerosis Acanthosis nigricans UV rays 146) What is the most common type of skin cancer that actinic keratosis can lead to? A) B) C) D) Basal cell carcinoma Melanoma Squamous cell carcinoma Dermatofibrosarcoma protuberans 147) Which of the following is a risk factor for actinic keratosis? A) B) C) D) Being fair-skinned Being dark-skinned Being between the ages of 20 and 30 Eating a high-fat diet 148) Which of the following statements is false regarding a lipoma? A) A lipoma is a fatty lump most often situated between the skin and muscle layer B) A lipoma is a precancerous skin condition C) Lipomas are usually found in middle age D) A lipoma is slow-growing 149) What is the cause of lipomas? A) B) C) D) High serum triglyceride levels Diabetes Obesity The cause is unknown 150) What age group are lipomas most common in? A) B) C) D) 2 to 5 years old 10 to 20 years old 20 to 40 years old 40 to 60 years old 151) What is vitiligo? A) A chronic skin condition characterized by patches of skin losing their pigment and becoming white B) A chronic skin condition characterized by rough, tan-to-brown, sandpaper-textured rashes throughout the body C) An acute skin condition characterized by patches of skin losing their pigment and becoming white D) An acute skin condition characterized by rough, tan-to-brown, sandpaper-textured rashes throughout the body 152) Which of the following statements is false regarding vitiligo? A) Typically, with vitiligo, both sides of the body are affected B) The cause of vitiligo is unknown C) Segmental vitiligo typically gets worse over time D) There is no known cure for vitiligo 153) Globally, vitiligo affects about: A) B) C) D) 0.01% of the population 1% of the population 5% of the population 10% of the population 154) The color of the hair, skin and eyes is determined by: A) B) C) D) Testosterone Estrogen Melatonin Melanin 155) Which statement is true regarding vitiligo? A) Vitiligo affects only dark-skinned individuals B) Vitiligo is not a contagious skin disorder C) Vitiligo can be life threatening D) Vitiligo only affects the skin 156) Vitiligo is a type of: A) B) C) D) Precancerous condition Cancerous condition Autoimmune disease Skin ulcer 157) Symptoms of cellulitis include all of the following except: A) B) C) D) Swelling of the skin Inflamed, red skin Vomiting Fever 158) A subungual hematoma is: A) Bleeding underneath the conjunctiva of the eye B) Bleeding underneath the fingernail or toenail C) Bleeding underneath the eyelashes D) Bleeding in areas of the joints 159) What is a furuncle? A) A bacterial or fungal infection of the skin B) A bacterial or fungal infection of the hair follicles C) A bacterial infection of the eyelids D) A viral infection of the mucous membranes of the nose 160) What is a carbuncle? A) A skin condition characterized by a cluster of boils coalescing together B) A skin condition characterized by patches of red skin with white scales C) A skin condition characterized by brown discoloration of the skin D) A skin condition characterized by a lack of pigmentation of the skin, forming white spots in the skin 161) Which statement is false regarding carbuncles? A) Staphylococcus aureus is the most common bacteria that causes carbuncles B) Carbuncles are filled with pus - a mixture of dead white blood cells, bacteria, and dead skin cells C) Carbuncles is a chronic skin condition D) Carbuncles are contagious and can be spread either to other parts of the body or to other people through direct contact 162) What is seborrheic keratosis? A) A benign skin condition that causes flat pinkish-colored macules on the skin B) A benign skin condition that causes an overgrowth of tissue on the skin that has a waxy, scaly appearance C) A precancerous skin condition that causes flat pinkish-colored macules on the skin D) A precancerous skin condition that causes an overgrowth of tissue on the skin that has a waxy, scaly appearance 163) Which of the following statements is false regarding seborrheic keratosis? A) Seborrheic keratosis is normally painless B) Seborrheic keratosis is found most commonly in children C) Seborrheic keratosis normally doesn’t require any treatment D) Seborrheic keratosis is not contagious 164) Seborrheic keratosis can mimic other skin conditions including skin cancers such as melanoma. What is the only definitive test that can be done to make sure that it is not in fact cancer? A) A full visual examination of the lesion must be done B) A wood lamp must be used to examine the lesion C) A biopsy of the lesion must be done D) There are no tests that can differentiate it from cancer 165) What is the medical term for a mole? A) B) C) D) Nevus Papule Macule Pustule 166) What is melasma? A) A skin condition that causes black bumps on the face B) A skin condition that causes white discolored patches on the face C) A skin condition that causes brown to gray-brown patches on the face D) A skin condition that causes intense acne near the eyebrows 167) Which of the following statements is false regarding melasma? A) Melasma is much more common in women than in men B) Melasma is very common during pregnancy C) Sun exposure is a risk factor for melasma D) Hormone replacement therapy is one of the treatments for melasma 168) What is psoriasis? A) A skin condition that causes brown discoloration of the skin B) A skin condition that causes small red, smooth bumps throughout the body C) A skin condition that causes scaly, itchy, dry rashes D) A skin condition that causes black discoloration of the skin, especially in the skin creases 169) Which of the following statements is false regarding psoriasis? A) Psoriasis changes the life cycle of the skin cells B) Psoriasis is a type of autoimmune disease C) Psoriasis is an acute illness typically lasting less than 4 weeks D) Between 10% and 30% of people with psoriasis develop psoriatic arthritis 170) The Koebner phenomenon refers to: A) Deeply ulcerated skin that appears over areas of skin trauma in a person with psoriasis B) New psoriatic lesions that form over areas of skin trauma in a person with psoriasis C) Heavy bleeding that occurs over areas of psoriatic plaques with skin trauma in a person with psoriasis D) Black lesions that occur over areas of psoriatic plaques with skin trauma in a person with psoriasis 171) Auspitz’s sign refers to: A) Pinpoint areas of bleeding that remain in the skin when a psoriatic plaque is scraped off B) Areas of psoriasis that are especially silvery and scaly C) New psoriatic plaques that form over areas of traumatized skin D) Black lesions that occur over areas of psoriatic plaques with skin trauma 172) All of the following may be symptoms of nail psoriasis except for: A) The nails may change to a green, yellow, or brown color B) The nails may develop ridges, grooves, or there may be pitting on the nail surface C) The nails may loosen or separate from the nail bed D) The nails may become thinner 173) Which of the following statements is false regarding guttate psoriasis? A) Guttate psoriasis is a type of psoriasis that is characterized by larger-than-normal psoriatic plaques that are extremely itchy B) Guttate psoriasis is not contagious C) Guttate psoriasis usually occurs on the trunk, arms, or legs, but it may cover a large portion of the body D) The trigger of guttate psoriasis is usually a streptococcus bacterial infection 174) What type of infection is cutaneous larva migrans? A) B) C) D) Bacterial Viral Fungal Parasitic 175) Which of the following statements is false regarding cutaneous larva migrans? A) The hookworm larvae that causes cutaneous larva migrans usually infest cats, dogs, and other animals, not humans B) Antibiotics are the treatment of choice for cutaneous larva migrans to shorten the duration of the illness C) Cutaneous larva migrans is self-limiting D) The larvae migrate under the skin’s surface and cause itchy red lines or tracks 176) Which of the following statements is false regarding Fordyce spots? A) Fordyce spots appear as small, painless, raised, pale, red or white spots or bumps B) Fordyce spots appear on the face, in the mouth, or on the genitals C) Fordyce spots are a sign of neurofibromatosis D) Fordyce spots are not associated with any type of disease or illness 177) What is rosacea? A) A skin disorder characterized by facial redness B) A skin disorder characterized by pruritic red rashes C) A skin disorder characterized by periorbital edema D) A skin disorder characterized by yellow-colored plaques that are located near the eyebrows 178) Which statement is false regarding rosacea? A) The cause of rosacea is unknown B) A biopsy is necessary in order to diagnose rosacea C) Rosacea can affect the eyes, causing dry, red, irritated eyes D) There is no cure for rosacea 179) Which of the following individuals is rosacea most likely to affect? A) B) C) D) A 13-year-old black male A 4-year-old white boy A 70-year-old black woman A 50-year-old white woman 180) What is the main class of medications used to treat rosacea? A) B) C) D) Antibiotics Steroids NSAIDs Antifungals 181) What is a comedo? A) An infected hair follicle (pore) on the skin B) A clogged hair follicle (pore) on the skin C) A type of psoriatic plaque that builds up on the skin D) A type of tan to brown discoloration of the skin 182) Which statement is false regarding comedones? A) Comedones may be open, in which case they are referred to as blackheads B) Comedones may be closed, in which case they are referred to as whiteheads C) The follicles in open comedones are completely blocked D) Comedones can occur with or without acne 183) What of the following best characterizes acne? A) A skin condition characterized by facial redness B) A skin condition usually characterized by comedones and papules and pustules C) A skin condition that causes tan to brown discoloration of the skin D) A skin condition that causes blackened skin on certain parts of the body 184) Acne is graded in stages from 1 to: A) B) C) D) 2 3 4 5 185) Isotretinoin is used for what type of acne? A) B) C) D) Mild Moderate Severe Moderate to severe 186) What initial monotherapy is most often used for acne? A) B) C) D) Benzoyl peroxide Topical retinoid Antibiotics Regular body lotion 187) All of the following are standard treatments for mild to moderate acne except for: A) Benzoyl peroxide gel B) Topical retinoid C) Acyclovir D) Antibiotics 188) What kind of acne is the most likely to be treated only with topical treatments? A) B) C) D) Mild acne Moderate acne Severe acne All forms of acne 189) What is another term used for pimples? A) B) C) D) Rashes Papules Pustules Furuncles 190) An examiner is examining the skin of a patient. There is a discolored area of skin that is flat, distinct and less than 1 cm wide that does not cause any changes to the texture or thickness of the skin. This is referred to as a: A) B) C) D) Macule Papule Pustule Rash 191) A benign bony protrusion on the hard palate of the mouth, that is usually midline on the palate is referred to as a: A) B) C) D) Torus palatinus Cleft palate Nicotinic stomatitis Split uvula 192) What is pityriasis rosea? A) A skin condition characterized by facial redness B) A skin condition that is characterized by patches (rashes) on the chest, belly, or back C) A skin condition characterized by black discoloration in the creases of the body such as the back of the neck D) A skin condition characterized by red pimples on the face 193) Which of the following is false regarding pityriasis rosea? A) Pityriasis rosea usually goes away on its own B) Pityriasis rosea is a benign condition C) Pityriasis rosea is usually caused by a bacterial infection D) Pityriasis rosea is not believed to be a contagious condition 194) Which of the following statements is false regarding meningococcemia? A) Meningococcemia is an acute and potentially life-threatening infection of the bloodstream B) Meningococcemia is caused by bacteria called Neisseria meningitides C) Meningococcemia can be spread from person to person only through direct contact D) Family members and those closely exposed to someone with meningococcemia are at increased risk 195) What is the difference between meningitis and meningococcemia? A) Meningococcemia is caused by the bacteria Neisseria meningitidis, while meningitis is caused by Fusobacterium B) Only meningitis causes a fever and headache; these symptoms are not present with meningococcemia C) Meningitis is an infection of the membranes that cover the brain and spinal cord; meningococcemia is when the infection remains in the blood and does not affect the membranes that cover the brain and spinal cord D) Meningococcemia is considered a medical emergency, while meningitis is not 196) Fulminant meningococcemia can cause changes in the skin that are characterized by: A) Deeply ulcerated skin throughout the body B) Purpuric skin lesions that are diffuse throughout the body C) Brown papules spread throughout the body D) Yellow macules that are present throughout the body 197) The meningococcal vaccination is recommended for all: A) Farm workers B) Healthcare professionals C) Tattoo parlor workers D) College students living in a dormitory 198) What medication is used as prophylaxis for those who may have been in close contact with a person with meningococcemia? A) B) C) D) Isoniazid Rifampin Ethambutol Erythromycin 199) Which of the following burns is painless? A) B) C) D) Superficial thickness (First Degree) Partial thickness (Second Degree) Full thickness (Third Degree) All types of burns are painful 200) Which is the only type of burn that never forms blisters? A) B) C) D) Superficial thickness (First Degree) Partial thickness (Second Degree) Full thickness (Third Degree) All types of burns form blisters 201) A man has been burned on his entire torso (chest and back). He has also sustained burns to his entire right leg. According to the rule of nines, what percentage of total body surface area (TBSA) has been burned? A) 36% B) 45% C) 54% D) 63% 202) Another name for enterobiasis is: A) B) C) D) Ringworm Pinworms Head lice Athlete’s foot 203) Which statement is false regarding enterobiasis? A) Enterobiasis is the most common worm infection in the United Sates B) Enterobiasis is spread most commonly through the use of swimming pools C) Hand hygiene is the most effective means for the prevention of enterobiasis D) The infected person and all household contacts and caretakers of the infected person should all be treated at the same time 204) What is a common test used to check for enterobiasis? A) B) C) D) Stool sample examination Tape test Rectal biopsy Urine test 205) Which medication is commonly prescribed to treat enterobiasis? A) B) C) D) Metronidazole Mebendazole Erythromycin Ketoconazole 206) Enterobiasis mainly occurs in: A) Children B) Adolescents C) Middle aged adults D) Elderly 207) What is main symptom of enterobiasis? A) B) C) D) Fever Headache Rectal itching Vomiting 208) Which of the following suggests that a child may have pinworms? A) Intense itching during the night B) Profuse vomiting during the night C) Intense headaches during the night D) Fever that persists throughout the day and night 209) All of the following conditions can cause uveitis except for: A) B) C) D) Rheumatoid arthritis Osteoarthritis Ankylosing spondylitis Bechet’s disease 210) What is intertriginous dermatitis? A) An inflammatory condition of the hair follicles of the chest B) An inflammatory condition of the skin folds C) An inflammatory condition of the eyelids D) An inflammatory condition of the eyebrows 211) Which of the following is the least common area where intertriginous dermatitis (intertrigo) would be found? A) Between the toes B) Armpits C) Beneath the breasts D) Abdomen 212) Which of the following is not a risk factor for intertrigo? A) B) C) D) Dry skin Obesity Diabetes Excessive sweating 213) Rheumatic fever is caused by: A) B) C) D) Group A streptococcus Group B streptococcus E. coli Streptococcus pyogenes 214) What is the most likely scenario of a child getting rheumatic fever? A) The child was playing outside and got bit by a tick B) The child was playing outside and scraped his knee against a rusty nail C) The child was at school and got severe food poisoning from a meal at lunch D) The child had a sore throat that was left untreated 215) What part of the body can rheumatic fever cause permanent damage to? A) B) C) D) The joints The brain The nerves The heart 216) What age is rheumatic fever most common in? A) 2-4 years old B) 5-15 years old C) 16-25 years old D) 25-40 years old 217) All of the following are major criteria used to diagnose rheumatic fever except for: A) B) C) D) Arthritis Fever Carditis Sydenham’s chorea 218) What is the main medication used to treat rheumatic fever? A) B) C) D) Cephalexin Penicillin Trimethoprim-sulfamethoxazole Ciprofloxacin 219) Diagnostic tests for rheumatic fever may include all of the following except for: A) B) C) D) Antistreptolysin titers EKG Urinalysis ESR 220) A person who has had rheumatic fever can get it again. What medication is the drug of choice to be given prophylactically before procedures such as dental procedures? A) B) C) D) Cephalexin Penicillin Trimethoprim-sulfamethoxazole Ciprofloxacin 221) What is the causative agent of scarlet fever? A) Group A strep B) Group B strep C) E. coli D) Staphylococcus pyogenes 222) All of the following are symptoms of scarlet fever except for: A) Sore throat B) Photophobia C) Bright sandpaper-textured rashes throughout the body D) Strawberry tongue 223) Seborrheic dermatitis causes all of the following conditions on the skin except for: A) B) C) D) Red skin Scaly patches Dandruff Deposits of yellow mucus 224) Where does seborrheic dermatitis most frequently occur? A) B) C) D) The chest The scalp The armpits The legs 225) Which of the following statements is false regarding acral lentiginous melanoma? A) Acral lentiginous melanoma is the most common type of melanoma in dark-skinned individuals B) Acral lentiginous melanoma arises on the soles of the feet, the palms of the hands, or beneath the nails C) Acral lentiginous melanoma is more common on the feet than on the hands D) Acral lentiginous melanoma affects primarily women 226) Which statement is true about the diameter of a mole that is melanoma? A) Diameter > 2mm B) Diameter > 4mm C) Diameter > 6mm D) Diameter > 8mm 227) What is the most common type of allergen that causes allergic rhinitis? A) B) C) D) Pollen Cigarette smoke Grass Dust mites 228) When an allergen comes into contact with a person’s body, the body releases: A) B) C) D) Cortisol Epinephrine Histamine Renin 229) Perennial allergic rhinitis is that which occurs: A) B) C) D) Seasonally One month out of the year 6 months out of the year All year round 230) What is rhinitis medicamentosa? A) Excess tearing of the eyes brought on by extended use of steroid eye drops or ointment B) Dry eyes brought on by extended use from steroid eye drops or ointments C) Rebound nasal congestion brought on by extended use of topical decongestants and certain oral medications D) Oral thrush brought on by extended use of oral steroids 231) Which of the following individuals is the most typical profile of a person with Systemic Lupus Erythematosus (SLE) based on its occurrence in demographic populations? A) A black or Hispanic woman in her 20s B) An elderly white woman in her 70s C) An Asian man in his 30s D) A black man in his 50s 232) All of the following are common symptoms of systemic lupus erythematosus except for: A) B) C) D) Butterfly malar rash Photophobia Endocarditis Raynaud’s phenomenon 233) What is stasis dermatitis? A) Inflammation of the skin of the lower legs caused by chronic arterial insufficiency B) Inflammation of the skin of the lower legs caused by chronic venous insufficiency C) Inflammation of the skin of the hands that is accompanied with generalized edema D) Inflammation of the skin of the hands caused by arterial insufficiency 234) Risk factors for stasis dermatitis include all of the following except for: A) B) C) D) Hypertension Venous insufficiency Being male Varicose veins 235) Which statement is false regarding stasis dermatitis? A) Stasis dermatitis occurs as a direct consequence of venous insufficiency B) Stasis dermatitis is an acute condition that can last as long as 2 weeks C) Stasis dermatitis most often affects middle-aged adults and elderly patients D) Stasis dermatitis can occur in one or both legs 236) What is lentigo? A) A condition characterized by red psoriatic plaques on the skin B) A condition characterized by yellow plaques around the eyelids C) A condition characterized by small pigmented macules that are well defined and that are surrounded by normal-appearing skin D) A condition characterized by small pigmented papules that are well defined and that are surrounded by normal-appearing skin 237) What is the cause of lentigo? A) B) C) D) Bacterial infection Fungal infection Sun exposure Autoimmune response 238) Which of the following statements is false regarding lentigo? A) Lentigo is a precursor for squamous cell carcinoma B) Lesions associated with lentigo tend to increase in number with age C) Lentigines are more common in light-skinned people D) Lentigines are also referred to as liver spots 239) Which disorder is characterized by spoon-shaped nails? A) B) C) D) Nail psoriasis Koilonychia Paronychia Onychomycosis 240) What is the most common cause of koilonychia? A) B) C) D) Fungal infection of the nails Trauma to the nail Peripheral arterial disease Iron-deficiency anemia 241) What is faun tail nevus? A) A condition in which many bumps appear near the rectum, most often due to hemorrhoids B) A posterior midline cutaneous lesion that involves localized hair on the spine C) A red rash on the popliteal area that is intensely itchy and painful D) A patch of clogged hair follicles on the scalp that can cause huge pus-filled blisters 242) Café-au-lait spots are: A) B) C) D) Macules Papules Pustules Rashes 243) Café-au-lait spots are: A) B) C) D) Pink Brown Black Red 244) Café-au-lait spots are usually an early sign of: A) Psoriasis B) Acanthosis nigricans C) Neurofibromatosis D) Café-au-lait spots are benign and are not associated with any disease or illness 245) Presbyopia is: A) Age-related nearsightedness B) Age-related farsightedness C) Age-related deterioration in central vision D) Age-related deterioration in peripheral vision 246) Which of the following statements is false regarding presbyopia? A) Presbyopia is a natural part of the aging process B) People with presbyopia have difficulty focusing on objects far away C) Presbyopia is a very common condition, with millions of cases in the United States each year D) Presbyopia normally begins in the early to mid-40s 247) Strabismus is a condition in which: A) B) C) D) There is misalignment of the feet There is cataracts of one eye There is blindness in one eye There is misalignment of the eyes 248) Which of the following statements is false regarding strabismus? A) Strabismus is caused by poor eye muscle control B) Strabismus is a very rare condition C) Strabismus is also referred to as crossed eyes D) The misalignment of the eyes can be inward, outward, upward, or downward 249) Esotropia is: A) A form of strabismus in which one or both eyes turn inward B) A form of strabismus in which one or both eyes turn outward C) A form of strabismus in which one eye is deviated upwards in comparison to the other eye D) A form of strabismus in which one eye is deviated downwards in comparison to the other eye 250) Which of the following statements is true regarding esotropia? A) Esotropia is a normal and common finding in infants B) Esotropia is a normal and common finding in adults C) Esotropia is abnormal if found in children or adults D) Esotropia puts a person at higher risk for developing blindness later in life 251) Which eye condition is referred to as lazy eye? A) B) C) D) Esotropia Amblyopia Hypertropia Hypotropia 252) Which test is a screening test for strabismus? A) B) C) D) Snellen’s eye chart Red reflex test Single cover test Fluorescein eye stain 253) Which eye problem would tonometry be most useful and specific for? A) B) C) D) Cataracts Glaucoma Retinal detachment Macular degeneration 254) Which part of the eye is most responsible for central vision? A) B) C) D) Cones Macula Rods Sclera 255) Which part of the eye is most responsible for bright color vision? A) B) C) D) Cones Macula Rods Sclera 256) Which part of the eye is most responsible for night vision? A) B) C) D) Cones Macula Rods Sclera 257) The fluorescein eye stain is used to check for: A) B) C) D) Cataracts Glaucoma Corneal abrasions Diabetic retinopathy 258) Which represents the normal sequence regarding the eyes and light exposure? A) Normally the pupil constricts in the presence of bright light and dilates in dim light or darkness B) Normally the pupil dilates in the presence of bright light and constricts in dim light or darkness C) Normally the pupil constricts in the presence of bright light and in dim light or darkness D) Normally the pupil dilates in the presence of bright light and in dim light or darkness 259) Which represents the normal sequence regarding the eyes and focus? A) Normally the pupils constrict when focusing on a nearby object and dilates when focusing on an object far away B) Normally the pupils dilate when focusing on a nearby object and constricts when focusing on an object far away C) Normally the pupils constrict when focusing on a nearby or far away object D) Normally the pupils dilate when focusing on a nearby or far away object 260) What is the outermost layer of the eye? A) B) C) D) Cornea Iris Pupil Lens 261) Which part of the eye is responsible for sharp vision such as that of 20/20 vision? A) B) C) D) Choroid Fovea Ciliary body Sclera 262) Which statement is false regarding Adie’s pupil? A) Adie’s pupil is a neurological disorder affecting the pupil of the eye B) In most cases, with Adie’s pupil, the affected pupil is smaller than normal (constricted) C) Usually, with Adie’s pupil, the pupil is slow to react in response to direct light D) Adie’s pupil may be the result of a post viral infection 263) Which describes Argyll Robertson pupils? A) Pupils that are large and constrict poorly to direct light and accommodation B) Pupils that are large and constrict poorly to direct light and briskly to accommodation C) Pupils that are small and constrict poorly to direct light and accommodation D) Pupils that are small and constrict poorly to direct light and briskly to accommodation 264) Which of the following statements is false regarding Marcus Gunn pupil? A) Marcus Gunn pupil is a medical sign whereupon the patient’s pupils constrict less than normal when a bright line is shone on it B) Marcus Gunn pupil is a medical sign whereupon the patient’s pupils dilate more than normal when a bright line is shone on it C) Marcus Gunn pupil is a medical sign whereupon the patient’s pupils do not dilate or constrict all when a bright line is shone on it D) Marcus Gunn pupil is a medical sign whereupon the patient’s pupils dilate with accommodation 265) Anisocoria refers to a condition in which: A) Both pupils are dilated B) Both pupils are constricted C) The pupils are of unequal size D) The pupils are both discolored a grayish color 266) A practitioner asks a patient to follow her finger with his eyes, as she moves her finger horizontally, back and forth. Which of the following conditions could the practitioner be checking for? A) B) C) D) Marcus Gunn Pupil Argyll Robertson pupil Dysconjugate gaze Anisocoria 267) The elliptical space between the open eyelids are referred to as the: A) B) C) D) Pupils Palpebral fissure Inner canthus Outer canthus 268) Which eye condition causes a decreased palpebral fissure in the affected eye? A) B) C) D) Nystagmus Ptosis Marcus Gunn Pupil Adie’s pupil 269) Which of the following eye conditions is characterized by involuntary, rapid, oscillating eye movements? A) B) C) D) Nystagmus Strabismus Esotropia Ptosis 270) Which of the following statements is false regarding ocular rosacea? A) Ocular rosacea is inflammation that causes redness, burning and itching of the eyes B) Ocular rosacea often develops in people who have rosacea but sometimes can be the first sign that a person may later develop the facial type C) Ocular rosacea is cured through a course of oral doxycycline antibiotics D) Ocular rosacea can affect vision 271) Corneal light reflex is a test that is done to check for: A) B) C) D) Visual acuity Ocular alignment Cataracts Glaucoma 272) Which of the following is a description of supernumerary nipples? A) A condition in which a person has no nipples B) A condition in which a person has only 1 nipple C) A condition in which a person has 2 nipples D) A condition in which a person has more than 2 nipples 273) Sarcopenia is the loss of: A) B) C) D) Epidermal tissue Subcutaneous tissue Muscle tissue Blood vessels 274) Cachexia is characterized by all of the following except for: A) B) C) D) Marked weight loss Marked weight gain Ill health Muscle loss 275) Cachexia is also referred to as: A) B) C) D) Syndrome X Wasting syndrome Trisomy 21 Trisomy 18 276) Where would cachexia most likely be found? A) In a person with diabetes B) In a person with glaucoma C) In a person with advanced cancer D) In a person with end-stage renal disease 277) Ceruminosis is: A) The inability of the body to create cerumen B) Excessive accumulation of cerumen C) Cerumen that is infected D) Cerumen that is irreversibly bound to the ear canal 278) What is orbital cellulitis? A) Inflammation of the eye anterior to the orbital septum B) Inflammation of the eye posterior to the orbital septum C) Gangrene of the eye anterior to the orbital septum D) Gangrene of the eye posterior to the orbital septum 279) What is the most common cause of orbital cellulitis? A) B) C) D) Trauma to the eye Ear infection Tonsillitis Sinus infection 280) Symptoms of orbital cellulitis include all of the following except: A) Painful swelling of the upper and lower eyelid B) Bulging eyes C) Unaffected vision D) Fever 281) All of the following are possible complications of orbital cellulitis except for: A) B) C) D) Brain aneurysm Hearing loss Cavernous sinus thrombosis Loss of vision 282) What type of infection most commonly causes orbital cellulitis? A) B) C) D) Bacterial Viral Parasitic Fungal 283) Which of the following statements is false regarding periorbital cellulitis and orbital cellulitis? A) Orbital cellulitis is an ophthalmic emergency, while periorbital cellulitis is a much less severe condition B) Periorbital cellulitis does not produce bulging of the eye, limited eye movement, or pain on eye movement, as does orbital cellulitis C) Both orbital cellulitis and periorbital cellulitis cause loss of vision D) Staphylococcus and streptococcus bacteria are the most common causes of both orbital and preorbital cellulitis 284) What is atopic dermatitis? A) A skin condition that is characterized by dry, itchy rashes B) A skin condition that is characterized by furuncles C) A skin condition that is characterized by white patches on the skin D) A skin condition that is characterized by brown to tan discoloration of the skin, mainly on the face 285) Atopic dermatitis is also called: A) B) C) D) Psoriasis Eczema Acne Athlete’s foot 286) Triggers that may exacerbate atopic dermatitis include all of the following except: A) Allergens, such as dust mites and animal dander B) Stress C) Pork D) Allergic reaction 287) Common areas of atopic dermatitis on the body include all of the following except for the: A) B) C) D) Cheeks Knees Elbows Buttocks 288) Which of the following is false regarding atopic dermatitis? A) Most people who get atopic dermatitis do so before age 5 B) Atopic dermatitis rarely starts when a person is an adult C) Atopic dermatitis is a very common skin disorder D) Atopic dermatitis is always a lifelong disease 289) Ptosis involves the: A) B) C) D) Upper eyelid Lower eyelid Eyebrows Lacrimal ducts 290) Which of the following is false regarding a fishtail uvula? A) A fishtail uvula is a benign condition B) The fishtail uvula is split into 2 sections C) The fishtail uvula’s split may be a partial or complete division D) Infants with tonsillitis are at higher risk for having a split uvula 291) Which of the following statements is false regarding optic neuropathy? A) Optic neuropathy refers to damage to the retina B) The main symptom of optic neuropathy is a loss of vision, with poor color vision in the affected eye C) Optic neuropathy is common in multiple sclerosis D) With optic neuropathy, the pupillary response to light is abnormal 292) What is the most common cause of optic neuropathy? A) Inflammation of the optic nerve B) Insufficient blood flow to the optic nerve C) Compression of the optic nerve such as by a tumor D) Direct trauma to the optic nerve 293) Which of the following statements is false regarding optic atrophy? A) Optic atrophy causes a loss of some or most of the nerve fibers in the optic nerve B) Optic atrophy can cause abnormal vision and, in cases, severe vision loss C) Optic atrophy is a reversible condition D) Many diseases such as glaucoma and tumors can cause optic atrophy 294) What is the cause of roseola? A) B) C) D) Herpes simplex virus 1 Epstein-Barr Virus Human herpesvirus 6 Streptococcus pneumoniae 295) Roseola is also called: A) Fifth disease B) Sixth disease C) Rosacea D) Slapped cheeks 296) All of the following are symptoms associated with roseola except for: A) B) C) D) High fever Febrile seizures Headaches Red rash 297) Which of the following is true regarding erythema infectiosum? A) Erythema infectiosum is a common, mild rash illness B) It is caused by the norovirus C) Symptoms may include fever, runny nose, and headache D) The rash that is associated with erythema infectiosum appears on the face 298) Lymphogranuloma venereum is a type of: A) B) C) D) Cancer Precancerous condition Autoimmune disease STD 299) Which of the following statements is false regarding lymphogranuloma venereum? A) Lymphogranuloma venereum may involve small, painless sores on the genital area B) Lymphogranuloma venereum is a long-term (chronic) infection of the lymphatic system C) Lymphogranuloma venereum is transmitted through respiratory secretions D) Lymphogranuloma venereum is caused by any of 3 different types of Chlamydia trachomatis bacteria 300) What is the main risk factor for contracting lymphogranuloma venereum? A) Diabetes B) Hypertension C) Pneumonia D) HIV-positive status 301) Koplik spots are seen with: A) B) C) D) Measles Mumps Varicella Lymphogranuloma venereum 302) Which of the following regions of the body would koplik spots most likely be found? A) B) C) D) In the genital area On the nose In the mouth In the axillary region 303) What color is koplik spots? A) B) C) D) White Brown Red Green 304) Which of the following statements is false regarding a corneal ulcer? A) A corneal ulcer is an open sore on the cornea B) Contact lens wearers are at an increased risk for corneal ulcers C) Fluorescein dye is used to diagnose corneal ulcers D) Timolol eye drops are the mainstay treatment for corneal ulcers 305) Which of the following is not a symptom of a corneal ulcer? A) Eye pain B) Lack of tearing C) Sensation of a foreign body in the eye D) Worsening or blurry vision 306) Most cases of a corneal ulcer are due to: A) B) C) D) Cataracts Glaucoma Bacterial infection Fungal infection 307) Which of the following statements is false regarding ehrlichiosis? A) Ehrlichiosis is a bacterial infection B) Ehrlichiosis is transmitted through the bite of a mosquito C) Ehrlichiosis usually causes flu-like symptoms D) Most cases of ehrlichiosis occur in the spring and summer months 308) Which medication is highly effective against ehrlichiosis? A) B) C) D) Tetracyclines Penicillins Macrolides Fluoroquinolones 309) Folliculitis is: A) B) C) D) Inflammation of the lacrimal sac Inflammation of the hair follicles Inflammation of the fallopian tubes Inflammation of the phalanges 310) Which statement is true regarding folliculitis? A) Folliculitis takes place only on the hair follicles of the scalp B) Folliculitis takes place only on the hair follicles of the face C) Folliculitis takes place only on the hair follicles on the abdomen D) Folliculitis can take place on any hair follicles in the body 311) What is usually the cause of folliculitis? A) Viral or parasitic infection B) Bacterial or fungal infection C) Excess dirt on the skin due to poor hygiene D) An autoimmune disease in which white blood cells attack and inflame hair follicles 312) All of the following are risk factors for folliculitis except for: A) B) C) D) Trimming hair with scissors Having diabetes Having open scrapes or wounds Wearing makeup 313) How does folliculitis usually manifest? A) Red pustules with a hair in the center of each one B) Brown macules with a hair in the center of each one C) Small psoriatic plaques with intermittent hairs in them D) Blackheads with a hair in the center of each one 314) Which of the following is characteristic of fire ant stings? A) They produce a round, bluish discoloration on the skin B) They produce several round, bluish-discolored macules on the skin C) They produce a single, large bullseye’s rash on the skin D) They produce groups of swollen red spots on the skin that develop a blister on the top 315) Where are fire ants most commonly found in the United States? A) B) C) D) The Northern United Sates The Western United States The Eastern United States The Southern United States 316) All of the following provide protection against fire ants except: A) Wearing DEET-containing insect repellant B) Staying away from fire ant nests C) Wearing socks and shoes when outside D) Wearing gloves when gardening 317) All of the following illnesses are spread through tick bites except for: A) B) C) D) Rocky Mountain Spotted Fever Ehrlichiosis Malaria Lyme disease 318) Which of the following statements is false regarding keratoacanthoma? A) Keratoacanthoma is a fast-spreading cancer B) Keratoacanthoma is a benign tumor C) Keratoacanthoma is most commonly seen in those over the age of 60 D) Ultraviolet rays are one of the contributing factors to developing keratoacanthoma 319) Which type of skin cancer does keratoacanthoma most closely resemble in appearance? A) B) C) D) Basal cell carcinoma Squamous cell carcinoma Melanoma Dermatofibrosarcoma protuberans 320) Risk factors for keratoacanthoma include all of the following except for: A) B) C) D) Prolonged sun exposure Fair skin Age over 60 Dark skin 321) Verruca vulgaris is a type of: A) B) C) D) Mole Wart Macule Pustule 322) Which of the following statements is false regarding verruca vulgaris? A) Verruca vulgaris is a benign condition B) Verruca vulgaris is caused by one of many types of human papillomavirus C) Verruca vulgaris is especially common among children and adolescents D) Verruca vulgaris only occurs on the hands 323) Diastasis recti is also known as: A) B) C) D) Abdominal separation Cleft palate Split leg Hirschsprung disease 324) Which statement is true regarding diastasis recti in newborns? A) Most children with diastasis recti die within the first year of life B) Most children with diastasis recti die within the first 2 years of life C) Most children with diastasis recti die within the first 5 years of life D) Diastasis recti is not associated with morbidity or mortality 325) Which of the following statements is false regarding diastasis recti? A) Diastasis recti is a common condition in newborns B) Diastasis recti is seen more in premature newborns C) Diastasis recti in infants usually resolves with age D) Diastasis recti is common in men 326) Cotton wall spots can be seen in: A) Diabetic retinopathy B) Hypertensive retinopathy C) Diabetic retinopathy and hypertensive retinopathy D) Neither diabetic retinopathy nor hypertensive retinopathy 327) What is the most common type of uveitis? A) B) C) D) Anterior uveitis Intermediate uveitis Posterior uveitis Diffuse uveitis 328) The uvea is the: A) B) C) D) Outer layer of the eye Middle layer of the eye Inner layer of the eye Fibers that make up the optic nerve 329) Punch biopsies are used to obtain: A) B) C) D) Hairs on the skin Epidermal tissue Epidermal and dermal tissue Full-thickness skin specimens 330) The West Nile virus is transmitted to humans most commonly through: A) B) C) D) Livestock Mosquitoes Contaminated swimming pools Person-to-person contact 331) Which of the following statements is false regarding West Nile virus? A) Most people (70-80%) who become infected do not develop any symptoms B) About 20% of people develop flu-like symptoms such as fever, headache, body aches, and joint pain C) Less than 1% of people infected develop serious neurological illnesses such as meningitis or encephalitis D) Vaccination is widely available for West Nile virus to prevent its spread 332) When do most people get infected with the West Nile virus? A) B) C) D) Spring months Summer months Fall months Winter months 333) Where has the West Nile virus been reported? A) In the northeastern part of the United States B) In the Southern United States C) In the lower 48 states (excluding Hawaii and Alaska) D) In all 50 states 334) Which of the following statements is false regarding skin tags? A) Skin tags are usually benign B) Skin tags are a painful condition C) Skin tags are most common in middle age D) Skin tags are more common in overweight individuals 335) What is a hyphema? A) A bacterial infection of the eye that causes swelling and puffiness B) Inflammation of the eyelids caused by a bacterial or viral infection C) A collection of blood in the anterior chamber of the eye D) A yellow triangular-shaped growth on the eye due to UV rays 336) What is usually the cause of a hyphema? A) B) C) D) Hypertensive retinopathy Diabetic retinopathy Trauma Neovascularization 337) Which of the following statements is false regarding hyphemas? A) With a hyphema, blood collects between the cornea and the iris B) A hyphema can only fill up the bottom half of the anterior chamber of the eye C) A hyphema can cause partial or total vision blockage in the affected eye D) A hyphema is generally painful 338) Which of the following statements is false regarding a subconjunctival hemorrhage? A) Subconjunctival hemorrhages are usually harmless B) A subconjunctival hemorrhage is due to broken blood vessels underneath the conjunctiva of the eye C) A subconjunctival hemorrhage only occurs with significant force to the conjunctiva of the eye D) Subconjunctival hemorrhages normally heal within about 2 weeks 339) Which of the following symptoms is a person with a subconjunctival hemorrhage most likely to experience? A) B) C) D) Eye pain Eye discharge Scratchy feeling on the eye Change in vision 340) Virchow’s node is a: A) A lymph node in the cervical region B) A lymph node in the left supraclavicular fossa C) A lymph node in the axillary region D) A lymph node in the femoral region 341) Where does the virchow’s node gets its blood supply from? A) B) C) D) Cranial cavity Thoracic cavity Abdominal cavity Spinal cavity 342) Trosier’s sign most likely indicates which of the following conditions? A) B) C) D) Brain cancer Oral cancer Lung cancer Gastric cancer 343) Which of the following statements is false regarding Von Recklinghausen’s disease? A) Von Recklinghausen’s disease is a genetic disease B) Von Recklinghausen’s disease is a disorder characterized by the growth of tumors on nerves C) Von Recklinghausen’s disease is a disorder that is limited to nerve involvement D) The tumors associated with Von Recklinghausen’s disease are usually benign 344) What vitamin deficiency is often linked to dysconjugate gaze? A) B) C) D) Riboflavin Thiamine Pyridoxine Cobalamin 345) Which of the following is false regarding urticaria? A) Urticaria is characterized by the transient eruption of papular lesions B) Urticaria can appear anywhere on the body C) Urticaria usually results due to an allergic reaction to something D) Urticaria normally isn’t pruritic 346) Which of the following statements is false regarding diaper dermatitis? A) Diaper dermatitis is entirely specific to infants B) The usual cause of diaper dermatitis is irritation due to urine or stool C) Treatment includes frequent diaper changes D) The most common microbial infecting agent is candida albicans 347) Which of the following statements is false regarding hyperhidrosis? A) The most common sites of hyperhidrosis are in the axillary region or the palms of the hands and soles of the feet B) Most cases of hyperhidrosis begin to occur in adolescence or young adulthood C) Hyperhidrosis occurs at predictable periods of time each day D) Hyperhidrosis is a chronic condition 348) Which ethnicity is most likely to be affected with hyperhidrosis? A) B) C) D) Italians Ashkenazi Jews Hispanic Japanese 349) What is hyperhidrosis most associated with? A) B) C) D) Mortality Heart problems Dehydration Diminished quality of life 350) Rhinophyma is associated with which disorder? A) B) C) D) Acne Acanthosis nigricans Melasma Rosacea 351) Which of the following conditions is referred as “jock’s itch”? A) B) C) D) Tinea capitis Tinea cruris Tinea pedis Tinea corporis 352) Which of the following is false regarding epidermoid cysts? A) Epidermoid cysts are small bumps beneath the skin B) Epidermoid cysts are usually painful C) Epidermoid cysts can appear on any part of the body, but are most common on the face, neck and trunk D) In most cases, epidermoid cysts cause no long-term problems 353) Which eye condition is known as pinkeye? A) B) C) D) Blepharitis Pterygium Uveitis Conjunctivitis 354) Tinea cruris is a: A) A fungal infection of the groin and the adjacent skin B) A bacterial infection of the groin and the adjacent skin C) A fungal infection of the chest D) A bacterial infection of the chest 355) A tinea infection is also referred to as a ringworm or a: A) B) C) D) Lipomas Dermatophytosis Macule Viral rash 356) Tinea cruris is often seen concomitantly with: A) B) C) D) Tinea capitis Tinea pedis Acne Rosacea 357) Which of the following statements is false regarding tinea cruris? A) The rash associated with tinea cruris is usually scaly, raised, and red B) Tinea cruris is most often seen in adult women C) Tinea cruris can be very pruritic D) Infection causing tinea cruris often comes from the feet or nails originally 358) Lichen sclerosus is known as: A) B) C) D) White spot disease Mask of pregnancy Red man syndrome Elastic skin 359) Which of the following statements is false regarding lichen sclerosus? A) Lichen sclerosus creates skin that is thinner than normal B) Lichen sclerosus is most common on the face C) Lichen sclerosus is a chronic condition that cannot be cured D) Lichen sclerosus can cause easy bruising or tearing of the skin 360) Which group is at highest risk for obtaining lichen sclerosus? A) B) C) D) Infants Pregnant women Postmenopausal women Sexually active middle-aged men 361) Which of the following statements is true regarding lichen sclerosus? A) Bacterial infections are the cause of lichen sclerosus B) Lichen sclerosus is a highly contagious skin condition that can be spread through direct contact C) Lichen sclerosus is an uncommon STD D) In women, lichen sclerosus usually involves the vulva 362) What is the mainstay treatment for lichen sclerosus? A) B) C) D) Antivirals Antibiotics Corticosteroids DMARDs 363) Which condition is also known as hay fever? A) B) C) D) Allergic conjunctivitis Allergic rhinitis Sinusitis Rocky Mountain Spotted fever 364) Which of the following statements is false regarding conjunctivitis? A) Both bacterial and viral conjunctivitis are highly contagious B) Viral conjunctivitis is usually distinguished due to its purulent exudate C) In adults, viral conjunctivitis is the most common type of conjunctivitis D) Both viral and bacterial conjunctivitis can be spread through direct contact or respiratory droplets 365) Which of the following bacteria would be least likely to cause bacterial conjunctivitis? A) B) C) D) Staphylococcus aureus Streptococcus pneumoniae Pseudomonas aeruginosa Moraxella catarrhalis 366) Chronic bacterial conjunctivitis often develops with which other inflammatory condition? A) B) C) D) Dacryocystitis Blepharitis Scleritis Iritis 367) Which of the following statements is false regarding hyperacute bacterial conjunctivitis? A) Hyperacute bacterial conjunctivitis is a severe form of bacterial conjunctivitis that develops rapidly B) Hyperacute bacterial conjunctivitis is accompanied by a large amount of yellow-green discharge that returns even after being wiped away from the eye(s) C) Hyperacute bacterial conjunctivitis most often occurs in children D) Hyperacute bacterial conjunctivitis can lead to vision loss if not treated promptly 368) Which type of conjunctivitis would be most commonly found in a newborn? A) B) C) D) Allergic conjunctivitis Bacterial conjunctivitis Hyperacute bacterial conjunctivitis Chlamydial conjunctivitis 369) Which type of viruses are the most common causative agents of viral conjunctivitis? A) B) C) D) Adenoviruses Herpesviruses Picornaviruses Rubella virus 370) Which past history would be most important when evaluating a man who is suspected of having adult chlamydial conjunctivitis? A) B) C) D) History of multiple sex partners History of swimming pool use History of recent colds History of alcohol abuse 371) Which of the following is not an allergic disease or is not a disease triggered by allergic reactions? A) B) C) D) Allergic conjunctivitis Bacterial conjunctivitis Asthma Eczema 372) Which of the following eye conditions doesn’t lead to blindness? A) B) C) D) Glaucoma Subconjunctival hemorrhage Corneal ulceration Macular degeneration 373) Which of the following statements is false regarding epistaxis? A) Hypertension and the use of anticoagulants are risk factors for epistaxis B) Epistaxis occurs with the greatest frequency in adolescents C) The most common causes of epistaxis are dryness and nose picking D) Anterior epistaxis is epistaxis that bleeds down the nares, while posterior epistaxis is epistaxis that bleeds down the throat 374) All of the following measures are recommended to be taken during a nosebleed except: A) The patient should pinch the nares together for 10 to 15 minutes B) The patient should sit in the upright position leaning forward C) The patient should apply a heat pack to the nose D) If bleeding is uncontrolled or if the patient’s status is questionable, the patient should be referred to the ED 375) All of the following are prevention methods for epistaxis except for: A) Avoiding hot showers B Avoiding forceful nose blowing C) Use of a humidifier D) Use a water-based lubricant in the nares 376) Which of the following statements is false regarding pharyngitis? A) Pharyngitis is referred to often as “sore throat” B) Pharyngitis can be viral or bacterial C) Most cases of pharyngitis are bacterial D) Pharyngitis often causes a scratchy throat and difficulty swallowing 377) Which of the following viruses is least likely to cause pharyngitis? A) B) C) D) RSV Common cold Influenza Mononucleosis 378) What is the most common bacteria that causes bacterial pharyngitis? A) B) C) D) Group A streptococcus Gonorrhea Chlamydia Corynebacterium 379) Which of the following tests can be used to differentiate viral and bacterial pharyngitis? A) B) C) D) Fluorescein eye stain test Antinuclear Antibody Testing Rapid strep test Rheumatoid Factor testing 380) What is the most commonly prescribed antibiotic for bacterial pharyngitis? A) B) C) D) Erythromycin Penicillin Cephalexin Trimethoprim-sulfamethoxazole 381) Which of the following statements is false regarding scleritis? A) Scleritis is an eye condition characterized by severe pain and tenderness in the eye B) Scleritis does not affect vision C) The 2 main types of scleritis are anterior scleritis and posterior scleritis D) In almost half the cases, scleritis is associated with an underlying autoimmune disorder 382) Black dots present on the scalp (the black dot sign) is indicative of: A) B) C) D) Onset of male baldness An advanced stage of cancer Tinea capitis Psoriasis 383) Which of the following conditions is least likely to be life threatening? A) B) C) D) Meningococcemia Erysipelas Tuberculosis Rocky Mountain Spotted Fever 384) Tinea infections thrive the best in: A) B) C) D) Cold, moist environments Cold, dry environments Warm, moist environments Warm, dry environments 385) Which of the following statements is false regarding tinea pedis? A) Tinea pedis causes peeling skin between the toes B) Tinea pedis can affect one or both feet C) Tinea pedis is more common in children than adults D) Walking barefoot on a communal floor is a common transmission of tinea pedis 386) Tinea pedis is found with the greatest frequency in: A) B) C) D) Young adult men Young adult women Older adult women Older adult men 387) Tinea infections are caused by: A) B) C) D) Dermatophytes Gram-positive bacteria Gram-negative bacteria Parasites 388) What type of infections are all tinea infections? A) B) C) D) Bacterial Viral Fungal Parasitic 389) What is the diagnostic test for all tinea infections? A) B) C) D) Blood test Skin biopsy KOH slide Wood’s lamp 390) Which of the following is false regarding tinea barbae? A) Tinea barbae is a fungal infection of the beard and moustache areas of the face B) Tinea barbae is more common than tinea capitis C) Tinea barbae generally affects only adult men D) Tina barbae most often affects farmers 391) A kerion is a complication of what condition? A) B) C) D) Tinea capitis Tinea cruris Tinea pedis Tinea manuum 392) Acanthosis nigricans can be a sign of underlying: A) B) C) D) Rheumatoid arthritis Hypocalcemia Hypokalemia Diabetes 393) Amaurosis fugax is a: A) Temporary loss of vision in one or both eyes due to a lack of blood flow to the retina B) Permanent loss of vision in one or both eyes due to a lack of blood flow to the retina C) Temporary loss of hearing in one or both ears due to damage to the tympanic membrane D) Permanent loss of hearing in one or both ears due to damage to the tympanic membrane 394) Amaurosis fugax may occur due to all of the following disorders except for: A) B) C) D) Temporal arteritis Migraine headaches Head injury A chalazion 395) Which of the following statements is false regarding amaurosis fugax? A) Amaurosis fugax can cause sudden loss of vision in one or both eyes B) The loss of vision associated with amaurosis fugax can last for days C) After the temporary blindness, vision returns to normal D) Amaurosis fugax increases a person’s risk for stroke 396) Myringitis is a form of: A) B) C) D) Otitis media Otitis externa A cholesteatoma Rhinitis 397) Myringitis is inflammation of the: A) B) C) D) External ear canal Tympanic membrane Temporal lobe of the brain Throat 398) All of the following skin conditions are benign except for: A) B) C) D) Seborrheic keratosis Cherry angioma Keratoacanthoma Basal cell carcinoma 399) A patient has a pressure ulcer that is erythematosus without any break in the skin. The pressure ulcer does not blanch. What stage would this pressure ulcer be classified as? A) B) C) D) Stage 1 Stage 2 Stage 3 Stage 4 400) A patient has a deep decubitus pressure ulcer that reaches into the subcutaneous tissue underneath the dermis but does not reach the muscles and bones. What stage would this pressure ulcer be classified as? A) Stage 1 B) Stage 2 C) Stage 3 D) Stage 4 401) Which of the following statements is false regarding presbycusis? A) Presbycusis is age-related hearing loss with gradually progressive inability to hear B) Presbycusis is most often caused by conductive hearing loss C) Presbycusis refers especially to a loss of hearing high-frequency sounds D) Presbycusis is seen with the greatest frequency in the elderly 402) Which of the following is most suggestive of hearing loss? A) B) C) D) Air conduction > Bone conduction Bone conduction > Air conduction Air conduction = Bone conduction None of the following 403) Which of the following statements is false regarding the herpes simplex virus? A) Herpes simplex virus type 1 mainly causes oral herpes B) Herpes simplex virus type 2 causes genital herpes C) Symptoms of herpes include painful blisters or ulcers at the site of infection D) Both herpes simplex virus type 1 and 2 infections are usually short-lived and last for less than 6 weeks 404) Ehlers-Danlos syndrome is a disorder of: A) B) C) D) Bones Connective tissue Red blood cells White blood cells 405) Common symptoms of Ehlers-Danlos syndrome include all of the following except for: A) Frequent dislocations B) Thrombocytopenia C) Easy bruising D) Hypermobility of the joints 406) A woman comes into a clinic. What makes a practitioner suspect that she has Ehlers-Danlos syndrome? A) She can lift extremely heavy objects B) She has extreme hirsutism C) She can bend her fingers much beyond the normal range of motion D) Her voice is extremely deep and raspy 407) What type of disorder is Ehlers Danlos syndrome? A) Inherited B) Acquired through years of smoking C) Acquired through years of repetitive joint stress D) Acquired through years of poor nutritional intake 408) Xerophthalmia is a medical condition in which: A) The axillary regions produce no sweat B) The salivary glands produce no saliva C) The eyes produce no tears D) The sebaceous glands produce no oil 409) Xerophthalmia can be caused by a deficiency of: A) B) C) D) Vitamin A Vitamin D Vitamin E Vitamin K 410) If untreated, xerophthalmia can lead to: A) Glaucoma B) Cataracts C) Corneal ulceration D) Macular degeneration 411) Which demographic group would xerophthalmia most likely be found in? A) Children under 9 years old in Africa B) Children under 9 years old in the United States C) Adults over 60 years old in Africa D) Adults over 60 years old in the United States 412) Which of the following statements is false regarding geographic tongue? A) Geographic tongue is a condition that is characterized by a map-like appearance on the tongue B) Geographic tongue is caused by a candidal infection C) Geographic tongue can occur at any age, but is most common in middle-aged adults and older adults D) Certain triggers such as hot, spicy foods may trigger pain or discomfort in those with geographic tongue 413) Which of the following statements is false regarding waist-to-hip ratio (WHR)? A) Waist-to-hip ratio is the ratio of the circumference of the waist to that of the hips B) The waist-to-hip ratio can be used as an indicator or measure of health and the risk for developing serious health conditions C) People with “pear-shaped” bodies (more weight around the hips) face more health risks than people with “apple-shaped” bodies (more weight around the waist) D) The World Health Organization states that abdominal obesity is defined as a waist-tohip ratio above 0.90 for men and 0.85 for females 414) Where is the inframammary crease? A) The human anatomical point where the bottom of the breast and the chest meet B) The human anatomical point where the inner thigh meets the groin C) The human anatomical point where the chin meets the neck D) The human anatomical point where the wrist meets the arm 415) Cheilosis affects the: A) B) C) D) Throat Corners of the mouth Eyes Nose 416) Sarcoidosis is common in all of the following body parts except for the: A) B) C) D) Lungs Lymph nodes Eyes Nose 417) Which of the following statements is false regarding sarcoidosis? A) In half of cases of sarcoidosis, it goes away on its own B) Many people with sarcoidosis have no symptoms C) Sarcoidosis does not cause any health complications or long-term health problems D) There is no cure for sarcoidosis 418) A patient has a fever, chills, headache, fatigue and muscle and joint aches. He claims recently that he has been camping out in the woods without any protection. Upon examination, the practitioner discovers a circular red rash with central clearing on his back that is warm to touch. The patient denies knowing it was there and says that he has had no pain or itching in the area. Of all the following, what is the most likely diagnosis for this patient? A) B) C) D) Rocky Mountain Spotted Fever Erythema migrans Contact dermatitis Psoriasis 419) A patient has a fever, headache, abdominal pain, muscle pain, and has been vomiting. The patient tells the nurse that rashes first appeared on his wrists a few days ago and now has spread to his chest. The patient said that he does a lot of outdoor activities including hunting. Of all the following, what is the most likely diagnosis for this patient? A) Contact dermatitis B) West Nile Virus C) Rocky Mountain Spotted Fever D) Ehrlichiosis 420) A patient, a 40-year-old white woman, comes into a clinic with facial redness apparent around her nose, cheeks, forehead, and chin. In the redness are many scattered pimples. The patient’s eyes are also red and irritated, with the eyelids being swollen. Of all the following, what is the most likely diagnosis for this patient? A) B) C) D) Contact dermatitis Atopic dermatitis Psoriasis Rosacea 421) A patient comes into a clinic. Upon complete body examination, the practitioner finds several lumps on the patient’s underarms and groin. The patient complains that for the last few days, the lumps have been painful. The patient denies the lumps being itchy. Of all the following, what is the most likely diagnosis for this patient? A) B) C) D) Psoriasis Hidradenitis suppurativa Intertriginous dermatitis Pityriasis rosea 422) A patient comes into a clinic and complains of extreme itching on his arms. The patient believes that he may have come into contact with poison ivy when out on a camping trip. The practitioner examines his arms and sees reddened areas with skin peeling off along with blisters. The patient has no fever, denies nausea and vomiting, and any muscle aches. What is the patient’s likely diagnosis? A) B) C) D) Erythema migrans Rocky Mountain Spotted Fever Contact dermatitis Rosacea 423) Which disorder requires that all members of the household be treated? A) B) C) D) Scarlet fever Scabies Ehrlichiosis Lichen sclerosus 424) A child with his parent comes into a clinic. The parent complains that the child has had a sore throat for about 3 weeks now, which she has been treating with fluids, rest, throat lozenges, and herbal supplements. However, the sore throat hasn’t gotten better. The parent said she decided to bring her child in after noting a red rough, sandpaper-textured rash on the child’s face which has now spread to the child’s trunk. The practitioner checks the child’s temperature and notes that it is 104°F. Upon examination, the practitioner also notes that the child’s tongue is red and bumpy. Of all the following, what is the most likely diagnosis for this patient? A) B) C) D) Rheumatic fever Scarlet fever Kawasaki disease Mumps Integumentary and HEENT answers 1) (B) Herpes keratitis is a viral infection of the eye caused by the herpes simplex virus. 2) (B) Herpes keratitis involves an acute onset of severe eye pain, photophobia, and blurred vision in the affected eye. Retinal detachment is not a symptom associated with herpes keratitis (source: aao.org). 3) (B) Herpes keratitis can be diagnosed through the use of fluorescein dye. The fluorescein eye stain is used to check for corneal abrasions. The fluorescein eye stain uses an orange dye (fluorescein) to stain the eye and then a blue light to detect for either abrasions or foreign bodies in the eye. How the test is performed is that a piece of blotting paper containing fluorescein dye is touched to the surface of the eye. The person is then asked to blink. Blinking spreads the dye throughout the eye. The practitioner then shines a blue light into the eye. Any problems on the surface of the cornea will be stained by the dye and appear green under the blue light. A normal result would be that the dye remains in the tear film on the surface of the eye and does not stick to the eye itself (source: medlineplus.gov). 4) (D) Acute angle-closure glaucoma is a condition that causes increased intraocular pressure (IOP) and painful vision loss. It is an ophthalmic emergency. The patient should assume the supine position for as long as possible to decrease IOP. Treatment consists of reducing the IOP. 5) (A) Acute angle-closure glaucoma is associated with a sudden increase in eye pain and intraocular pressure. 6) (D) Open-angle glaucoma is associated with a gradual onset of increased intraocular pressure that is painless. This gradual increase in intraocular pressure leads to damage of the optic nerve. 7) (B) Open-angle glaucoma makes up over 80% of all cases of glaucoma. It has a gradual onset, unlike angle-closure glaucoma which has a sudden onset. All types of glaucoma initially lead to a loss of peripheral vision. After, if left untreated and progresses, it can lead to a loss of central vision and blindness. Screening for open-angle glaucoma can be done with tonometry. 8) (B) A peritonsillar abscess is a condition in which pus collects around the tonsils. It is a complication of tonsillitis. 9) (C) Though a peritonsillar abscess may involve several organisms (it can be a polymicrobial infection), most often it is caused by streptococcal bacteria, specifically group A strep bacteria; it can also be caused by other organisms as well, such as Staphylococcus aureus or Fusobacterium (source: aafp.org). 10) (A) Vomiting is a not a common symptom of a peritonsillar abscess. Common symptoms of a peritonsillar abscess include fever, odynophagia (difficulty swallowing), and severe throat pain. 11) (C) The first-line treatment for a peritonsillar abscess is incision and drainage of the abscess. 12) (D) A peritonsillar abscess is a complication of tonsillitis. 13) (D) Diphtheria is a serious bacterial infection usually affecting the mucous membranes of the nose and throat. 14) (B) Common symptoms of diphtheria include a sore throat, fever, weakness, swollen lymph nodes, and a markedly swollen neck (sometimes referred to as a “bullneck”). 15) (B) Diphtheria is very rare in the United States today, one of the reasons attributable to the widespread use of vaccination. Diphtheria is a condition that is very contagious. Diphtheria normally coats the posterior pharynx, tonsils, uvula, and soft palate with a gray-to-yellowcolored pseudomembrane that is hard to displace. It normally produces a low-grade fever in a person. 16) (A) Molluscum contagiosum is a skin infection that is caused by a virus. The virus, called the Molluscum contagiosum virus, produces benign raised lesions, or bumps, on the upper layers of the skin. The virus is easily spread but is not harmful. Molluscum contagiosum is mostly seen in children. The most common ages to see it is 1 to 10 years of age (source: cdc.gov). 17) (A) Leukoplakia is not a definitive sign of oral cancer. Most leukoplakia patches are noncancerous (benign), though some do indicate early signs of cancer. Leukoplakia produces white patches that form on the gums, insides of the cheeks, bottom of the mouth, or tongue that cannot be scraped off. Patients with a history of chewing tobacco are at high risk for leukoplakia. Alcohol consumption is also another risk for developing leukoplakia (source: mayoclinic.org). 18) (D) An avulsed tooth is a tooth that has been completely displaced from its socket in the mouth, usually occurring due to trauma. Milk is an appropriate storage medium for an avulsed tooth. Water and ice have been shown to damage the tooth root cells, and as such, an avulsed tooth should never be stored in them. 19) (D) Papilledema is optic disc swelling (swelling in the back of the eye) due to increased intracranial pressure (ICP). Conditions that may increase intracranial pressure and, thus, lead to papilledema are a brain tumor, a brain abscess, a head injury, bleeding in the brain, inflammation of the brain (such as encephalitis) or its tissues (meningitis), and idiopathic intracranial hypertension. Cluster headaches would not cause papilledema. 20) (C) Risk factors for cataracts include ultraviolet radiation from the sun or other sources, diabetes, hypertension, obesity, smoking, chronic use of steroids, statin medications, previous eye injury or inflammation, previous eye surgery, hormone replacement therapy, significant alcohol consumption, and family history. Anorexia nervosa is not a risk factor for cataracts. 21) (D) A pterygium is an overgrowth of scar tissue on the conjunctiva of the eye. The conjunctiva is a thin clear membrane over the ‘whites’ of the eye (sclera). The pterygium (scar tissue) is present over this conjunctiva and can extend across the cornea and affect vision. Pterygia are normally triangular-shaped in appearance. They are non-cancerous overgrowths. They are normally present on the side of the eye near the nose, not the ear. Pterygia are most often caused by UV damage from the sun. The part of the eye closest to the nose gets a double dosage of UV radiation. This is because it gets UV exposure directly from the sun and UV exposure from the UV rays reflected off the bridge of the nose to the eye. This can damage the tissue of the eye, resulting in scar tissue (pterygium). Image: Pterygium Credit: Photograph by Jmvaras José Miguel Varas, MD, licensed under the Creative Commons Attribution 3.0 Unported license 22) (B) Common symptoms of a pterygium include eye itchiness, burning in the eye, a gritty feeling in the eye (such as the feeling you have when sand gets into your eyes), and just the general feeling of having a foreign object in the eye. Pterygia commonly can cause blurred vision. It does not cause temporary blindness. 23) (A) A pterygium is also referred to as surfer’s eye, because it is common among surfers and other people who spend long amounts of hours in the sun. Landscapers also tend to get pterygia often due to spending long hours out in the sun. 24) (B) Treatments used for a pterygium include artificial tears, sometimes lubricating ointments in more severe cases, and topical corticosteroids which are used for a short period of time to reduce inflammation of the eye. If unresponsive to medication or if very severe, surgery may be done to remove the pterygium. A surgical excision is done under local or topical anesthesia and is an outpatient procedure. 25) (A) The most common cause of pingueculas is sun exposure (UV rays). Dust exposure is another cause. A pinguecula is a yellowish patch on the conjunctiva of the eye. It is a change in normal tissue that results in a deposit of protein, fat, and/or calcium on the eye. Pterygia are almost always preceded by pingueculas. Image: Pinguecula Credit: Photograph by Red eye2008, licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license 26) (A) Pingueculas and pterygia are most often caused by UV radiation from the sun. 27) (B) The normal range for intraocular pressure is 12 to 21 mmHg (source: allaboutvision.com). 28) (B) Dacryostenosis is nasolacrimal obstruction found in newborns, causing excess tearing. Nasolacrimal obstruction can be congenital or acquired. Normally tears would go down the nasal passages and down to the back of throat. However, with dacryostenosis, the lacrimal duct(s) (can be unilateral or bilateral) is blocked. Therefore, the newborn presents with excessive tearing and crusting in the morning. When dacryostenosis is congenital, it is called congenital dacryostenosis or congenital nasolacrimal obstruction. When dacryostenosis is acquired, it is called acquired dacryostenosis. 29) (C) Green-colored purulent discharge is abnormal and is indicative of a bacterial infection. It is not part of the normal process of dacryostenosis. Diagnosis for dacryostenosis includes a healthcare provider flushing the lacrimal drainage system with either saline or fluorescein dye. Reflux of the solution indicates dacryostenosis. Congenital dacryostenosis often resolves spontaneously by about age 6 to 9 months; before 1 year of age, manual compression of the lacrimal sac 4 to 5 times per day may relieve the obstruction. After the age of 1 year, the nasolacrimal duct may need probing, usually under general anesthesia; if obstruction is recurrent, a temporary plastic tube may be inserted. In acquired dacryostenosis, the underlying disorder is treated when possible. If treatment is not possible or is ineffective, a passage between the lacrimal sac and the nasal cavity can be created surgically (dacryocystorhinostomy). 30) (C) Dacryocystitis is an infection of the lacrimal sac, secondary to obstruction of the nasolacrimal duct. The lacrimal (or tear) sac is a small chamber into which tears drain. In healthy conditions, these tears would then go (from the lacrimal sac) through the nasolacrimal duct and then into the nasal passages. When there is an obstruction of the nasolacrimal duct at the lacrimal sac junction, pathogens such as bacteria can build up in the lacrimal sac and cause infection (dacryocystitis). With dacryocystitis, the area may be painful, red, and swollen. Sometimes a collection of pus may form. Image: Dacryocystitis 31) (A) The most common treatment for acute dacryocystitis is antibiotics. For chronic dacryocystitis, a procedure called a dacryocystorhinostomy is normally done. This is a procedure which involves fistulization of the lacrimal sac into the nasal cavity, which is done to restore the flow of tears from the lacrimal sac into the nose. This prevents the buildup of bacteria in the lacrimal sac, helping to prevent future cases of dacryocystitis. 32) (C) The most common cause of dacryocystitis is dacryostenosis. Dacryostenosis is a condition in which the lacrimal duct is blocked. Due to this blockage, tears do not flow out through the lacrimal sac normally as they would. Therefore, pathogens such as bacteria can build up, causing an infection of the lacrimal sac called dacryocystitis. 33) (C) Normally in age-related macular degeneration (AMD), peripheral vision is unaffected. Central vision is what is lost. Central vision becomes blurry and straight lines seem distorted. Only toward the late stages leading to blindness does a person also lose peripheral vision. 34) (A) Age-related macular degeneration (or just macular degeneration) is the leading cause of vision loss in the United States, affecting more people than glaucoma and cataracts combined. There are 2 forms of age-related macular degeneration (AMD), the dry form and the wet form. The dry form of AMD is more common. The wet form, however, is more aggressive and accounts for about 80% of vision loss in people with AMD. Smoking is a major risk factor for AMD. Other risk factors include age (most common in people over 65), family history and genetics, race (more common in whites than other races), obesity, and cardiovascular disease. 35) (D) Blepharitis is inflammation of the eyelids. Blepharitis typically affects the part of the eyelid where the eyelashes grow. The condition usually affects both eyelids. Image: Blepharitis Credit: Photograph by clubtable, released into the public domain 36) (C) Blepharitis is not contagious. Blepharitis is inflammation of the eyelids. Blepharitis commonly occurs when tiny oil glands located near the base of the eyelashes become clogged. Blepharitis usually does not cause permanent damage to a person’s vision. It is often a chronic condition that is difficult to treat. 37) (D) Symptoms of blepharitis include red eyes, a gritty burning sensation in the eyes, red, swollen eyelids, itchy eyelids, crusted eyelashes upon waking up, eyelid sticking, light sensitivity, eyelashes that grow abnormally, loss of eyelashes, and more frequent blinking. 38) (D) Alcohol swabs are not used to treat blepharitis. Treatment for blepharitis includes a topical antibiotic (since blepharitis may be due to a bacterial infection), steroid eye drops (to help control inflammation), and eyelid scrubs (for cleansing the eyelids). Blepharitis is not just caused by infections of the eyelids. Blepharitis may be caused by other ailments such as seborrheic dermatitis or rosacea. In these cases, treating the underlying conditions may help to improve the blepharitis. Even with good treatment, blepharitis doesn’t really completely go away. It is a chronic illness that is characterized by recurrent flare-ups. Therefore, it is a difficult ailment to treat and may require daily treatment such as with daily eyelid scrubs. 39) (D) Hemolytic uremic syndrome is caused by E. coli, not group A strep bacteria that causes strep throat. A strep throat, if left untreated, can progress to rheumatic fever, scarlet fever, impetigo, or glomerulonephritis. 40) (A) Steroids such as prednisone are not used to treat strep throat. Treatment for strep throat includes penicillin as a first-line treatment, ibuprofen or acetaminophen for throat pain and fever, and throat lozenges. 41) (B) Otitis externa is usually a bacterial infection. It is rarely a fungal infection. In North America, over 90% of otitis externa cases are caused by bacteria. It is estimated that the number is actually around 98% (caused by bacteria). Pseudomonas aeruginosa and Staphylococcus aureus are common causative agents. Otitis externa can be caused by other pathogens, though, such as fungi. So, this is why antifungals may be used to treat certain cases of otitis externa. Otitis externa is more common during warm and humid weather. Cases normally involve swimming or any activity in which the ears get wet. Otitis externa is usually a short-term condition that resolves within days to weeks (source: aafp.org). 42) (B) Otitis externa typically does not cause rhinitis, which is a stuffy nose. Common symptoms of otitis externa include ear pain with manipulation of the external ear or tragus, redness and swelling of the outer ear and ear canal, a feeling of pressure or fullness in the ear, discharge from the ear, tenderness upon moving the ear or jaw, and some hearing loss. 43) (A) The most common treatment for otitis externa is cortisporin otic drops. Cortisporin otic solution (neomycin and polymyxin B sulfates and hydrocortisone otic solution) is a combination of two antibiotics and an anti-inflammatory corticosteroid in an ear drop used to treat outer ear infections caused by bacteria. 44) (A) Otitis media with effusion (OME) is fluid behind the eardrum in the middle ear that is most often thick or sticky (though it can be thin and watery). It occurs without an ear infection. OME is a condition that occurs after most ear infections have been treated. After most ear infections have been treated, fluid (an effusion) remains in the middle ear for a few days or weeks. OME can also precede an ear infection. When the Eustachian tube is partially blocked (for whatever reason), fluid builds up in the middle ear. Bacteria, then, inside the ear become trapped and begin to grow, which can lead to an ear infection. OME most often occurs in children under age 2, but is rare in newborns. Younger children get OME more often than older children or adults because their eustachian tube is shorter, more horizontal, and straighter, making it easier for bacteria to enter. The tube is also floppier, with a tinier opening that's easy to block. Another reason young children get OME with greater frequency is because young children get more colds, since it takes time for their immune system to be able to recognize and ward off cold viruses. Unlike children with an ear infection, children with OME do not act sick. OME often does not have obvious symptoms. Older children and adults often complain of muffled hearing or a sense of fullness in the ear. Younger children may turn up the television volume because of hearing loss. OME is most often not life threatening. Most children do not have longterm damage to their hearing or speaking ability, even when the fluid remains for many months. Otitis media with effusion most often goes away on its own over a few weeks or months. Treatment may speed up this process (source: medlineplus.gov). 45) (B) The classic triad symptoms of infectious mononucleosis include fatigue, acute pharyngitis, and lymphadenopathy. Paroxysmal coughing is not associated with infectious mononucleosis. 46) (C) Mononucleosis is most often spread through saliva. This is why it is called the kissing disease. It can be spread by intimate kissing. 47) (B) Treatment for mononucleosis includes rest, fluids, and OTC PRN fever and pain medications. Being that mononucleosis is caused by a virus, antibiotics are not used for its treatment. 48) (D) The heterophile antibody test is positive for a person who has infectious mononucleosis. A complete blood count will be done. Normally with infectious mononucleosis, atypical lymphocytes and lymphocytosis (greater than 50%) will be present. Since mononucleosis often presents with lymphadenopathy, it causes enlarged cervical nodes that may be tender to palpation. This is a common area that is checked. The Rapid Plasma Reagin test is a test that is done to screen for syphilis, not mononucleosis. 49) (C) Infectious mononucleosis can lead to splenomegaly/splenic rupture, airway obstruction, neurologic conditions such as Guillain-Barré syndrome, aseptic meningitis, optic neuritis, and blood dyscrasias such as atypical lymphocytes. Infectious mononucleosis is not linked to heart failure. 50) (D) Lyme disease is spread by the bite of a deer tick. It produces flu-like symptoms. Lyme disease can produce a “bulls-eye” rash that usually appears within 1-2 weeks after infection. Lyme disease produces a rash that feels hot to touch and has a rough texture. The rash is not softtextured. 51) (C) Wearing bright colors is not a preventative measure for Lyme disease. Preventative measures include avoiding areas of known tick infestation, wearing long sleeve clothing, and putting on insect repellant containing deet. 52) (A) Lyme disease is treated with antibiotics. Patients treated with appropriate antibiotics in the early stages of Lyme disease usually recover rapidly and completely. Oral antibiotics commonly used include doxycycline, amoxicillin, or cefuroxime axetil. Patients with certain neurological or cardiac illnesses may require intravenous treatment with drugs such as ceftriaxone or penicillin (source: cdc.gov). 53) (C) More than 100 drugs are linked to the causation of Stevens-Johnson syndrome. Some of the most common are medicines for gout such as allopurinol, pain relievers such as acetaminophen, ibuprofen, and naproxen, antibiotics such as sulfas and penicillins, and antiseizure medications such as barbiturates. Proton pump inhibitors aren’t known to be associated with the onset of Stevens-Johnson syndrome. 54) (D) Stevens-Johnson syndrome is a potentially life-threatening skin condition in which cell death causes the epidermis to separate from the dermis. Stevens-Johnson syndrome has a mortality rate of 25% or higher. Although Stevens-Johnson syndrome can be caused by viral infections and malignancies, the most common cause is medications. Once the underlying cause is removed, SJS is normally short-term and heals within days to weeks, though in severe cases, it can take months to heal. 55) (C) Contact dermatitis is a red rash that appears at the site of contact of the skin with an irritant. Common irritants include poison ivy, jewelry such as nickel or gold, various perfumes and colognes, and other chemicals in cosmetics. 56) (C) Deodorant can be a cause, not a treatment, of contact dermatitis. Common irritants causing contact dermatitis include solvents, rubbing alcohol, bleach, personal care products, such as soaps, deodorants, and cosmetics, airborne substances, such as sawdust or wool dust, and burdock, a plant used in alternative medicine therapies. Treatments for contact dermatitis include stopping exposure to the offending substance(s), oatmeal baths, and calamine lotion. 57) (B) Acne is the most common skin condition in the world. 58) (A) Hidradenitis suppurativa is a chronic skin condition of the sebaceous glands that produces small painful lumps commonly in the armpits or groin. Image: Hidradenitis suppurativa 59) (B) A chalazion is a benign, painless bump or nodule inside the upper or lower eyelid. Image: Chalazion 60) (B) Chalazia typically aren’t painful. The bump that characterizes a chalazion is caused by a blockage of the Meibomian gland on the eyelid. Symptoms of a chalazion include a hard lump on the eyelid, increased tearing, blurry or blocked vision, and sensitivity to light. Most chalazia heal within one month, either with no treatment or simple home care. 61) (A) A cholesteatoma is an abnormal skin growth in the middle ear behind the eardrum. Repeated infections and/or a tear or pulling inward of the eardrum can allow skin into the middle ear. This skin builds up in the middle ear and over time can increase in size. It can damage the surrounding delicate bones of the middle ear, leading to hearing loss. The hearing loss is usually temporary and treatment (surgery) can often improve it. However, if the cholesteatoma continues its growth and is left untreated, permanent hearing loss can result. Cholesteatomas are most often acquired, though they can be congenital. 62) (A) A risk factor for cholesteatomas is a history of chronic otitis media infections. 63) (C) Generally, the only way to truly get rid of a cholesteatoma that has formed is through surgery. A cholesteatoma is removed surgically. Cholesteatomas don’t go away naturally. They usually continue to grow, in which case the symptoms normally get more severe over time. A cholesteatoma can grow so much that it can damage bones in the middle ear. This can, at times, lead to permanent hearing loss in the affected ear. Once a cholesteatoma has been diagnosed, a regimen of antibiotics, ear drops, and careful cleansing of the ear will most likely be prescribed. The healthcare provider will then be able to draft up a plan for its surgical removal. In most cases, surgery is done as an outpatient procedure. 64) (C) Sjögren’s syndrome is an autoimmune disease characterized by decreased function of the lacrimal and salivary glands. 65) (B) A hordeolum (also called stye) is a localized infection or inflammation of the eyelid margin involving hair follicles of the eyelashes (external hordeolum) or Meibomian glands (internal hordeolum). Image: Hordeola 66) (C) A hordeolum is a common disorder of the eyelid characterized by an acute focal infection. Its symptoms commonly include puffy eyes, watery eyes, a lump on the eyelid, and eyelid tenderness. Most times, the site appears pinkish; it rarely appears darkened (or blackened). Hordeola are normally painful. 67) (C) Treatments used for a hordeolum include warm compresses to the eyes, drainage, eyelid hygiene such as using lid scrubs to clean the eyes, massages of the lesions a few times a day, and topical antibiotic ointment. Warm compresses, not cold compresses, are used. 68) (B) The majority of the times, a hordeolum is caused by staphylococcal bacteria. Therefore, a hordeolum is treated with topical antibiotics applied to the site. Systemic antibiotics may be indicated if the hordeolum is complicated by preseptal cellulitis. 69) (C) A hordeolum is a temporary acute infection. It is not a lifelong problem. It normally is self-limiting and resolves spontaneously within 1-2 weeks. 70) (A) Impetigo is a highly contagious bacterial infection that affects the superficial layers of the epidermis of the skin. 71) (D) The vast majority of cases of impetigo are caused by either Streptococcus pyogenes or Staphylococcus aureus. Listeria monocytogenes, E. coli, and Clostridium botulinum aren’t linked to impetigo. 72) (B) Bullous impetigo is impetigo that is characterized by bubblelike cavities filled with air or fluid. 73) (A) Impetigo is most commonly seen in toddlers and is mostly a pediatric disorder. It is rarely seen in the older population, though it can still occur. 74) (C) Onychomycosis is a fungal infection of the nail (fingernail or toenail). Image: Onychomycosis Credit: Photograph by James Heilman, MD, distributed under the Creative Commons Attribution-Share Alike 3.0 Unported license 75) (C) Oral (systemic) antifungals are the treatment of choice for onychomycosis. Systemic antifungal agents are the most effective treatment for onychomycosis. Topical treatment has proven to be of little value because the nails are too thick and hard for external applications to penetrate to the site of infection. The use of topical agents is normally limited to cases involving less than half of the distal nail plate or for patients unable to tolerate systemic treatment; it may also be used as an adjunct to oral antifungals. 76) (C) A hordeolum and a chalazion are both lumps that are formed in or on the eyelid. A hordeolum is an infected lump, while a chalazion is a noninfected lump. A hordeolum is usually caused by a bacterial infection, while a chalazion is caused by a clogged oil gland. A hordeolum (also called a stye) is very painful. A chalazion is not usually painful. So, in summary, a chalazion is basically a noninfected lump that forms on the eyelid that is usually not painful, while a hordeolum is an infected lump formed in or on the eyelid that is very painful. 77) (B) Rocky Mountain Spotted Fever is caused by the bite of a dog tick or wood tick. 78) (C) Weight gain is not a symptom of Rocky Mountain Spotted Fever. Common symptoms of Rocky Mountain Spotted Fever include fever, rash (which occurs 2-5 days after the fever in about 90% of people), headache, nausea, vomiting, abdominal pain, muscle pain, lack of appetite, and conjunctival infection of the eyes. 79) (C) Rocky Mountain Spotted Fever has been reported at all times during the year, but the time where most cases occur is during the spring to early summer months. 80) (C) Rocky Mountain Spotted Fever (RMSF) is diagnosed through serum antibody titers. If a person is positive for RMSF, in the blood will be antibody titers to R. rickettsii (the bacteria carried by the infected tick). 81) (D) Going camping or being in the woods presents the most likely scenario of how a person could come into contact with an infected tick that can cause Rocky Mountain Spotted Fever. 82) (B) Rocky Mountain Spotted Fever is a bacterial infection caused by Rickettsia rickettsii, a gram-negative bacterium. A tick can carry this bacterium and can spread it to humans. 83) (D) Doxycycline is the first-line treatment for Rocky Mountain Spotted Fever. 84) (A) Paronychia is an infection of the tissue folds around the nails, either the fingernails or toenails. 85) (C) Paronychia is normally described as a red, swollen, and painful infection around the nails. Image: Paronychia Credit: Photograph by Chris Craig 86) (D) Paronychia, many times, does affect the nail and its appearance. The nail may look detached, abnormally shaped, or have an unusual color. Paronychia can be caused by bacteria or fungi. There are really 2 types of paronychia: acute and chronic. Acute paronychia is normally caused by staphylococcus bacteria. Chronic paronychia is usually caused by a fungal infection. Paronychia is most often caused by injury or trauma to the affected surrounding nail tissue; this can cause a break in the skin, which allows pathogens to enter. There may be pus-filled blisters that form in the infected area, especially with a bacterial infection. 87) (A) Treatment of paronychia include warm soaks of affected parts for 20 minutes 3 times a day and topical antibiotic application to the affected area. An incision and drainage may be done if an abscess is present. Cold soaks are not used for treatment of paronychia. 88) (B) Chronic cases of paronychia are associated with coexisting onychomycosis. 89) (A) Herpetic whitlow is a viral skin infection of the finger(s) that is caused by herpes simplex virus (type 1 or type 2), from direct contact with either a cold sore or genital herpes lesion. Image: Herpetic whitlow 90) (A) Herpes simplex virus I (HSV-1) causes 60% of cases of herpetic whitlow. The other 40% is caused by herpes simplex virus 2 (HSV-2). Cytomegalovirus and astrovirus are not causes of herpetic whitlow (source: emedicine.medscape.com). 91) (D) Both chickenpox (varicella) and herpes zoster (shingles) are caused by the same virus, the varicella-zoster virus. The primary infection of the varicella-zoster virus is called varicella. The reactivation of the varicella-zoster viral infection is known as shingles. After primary infection (chickenpox), the virus becomes latent within a dermatome (sensory ganglia) and is kept under control by an intact immune system. If the person becomes immunocompromised (for whatever reason), this can cause reactivation of the infection, which causes shingles. 92) (D) Most adults who get chickenpox experience prodromal symptoms for up to 48 hours before breaking out in a rash. These prodromal symptoms include fever and malaise prior to the rash onset, but in children the rash is often the first sign of disease. The rashes in chickenpox progresses from red bumps (papules) to fluid-filled blisters (vesicles) to vesicles that drain and scab over (scabbed lesions). The rashes in chickenpox are in different stages of development and do not all crust over at the same time. New bumps (papules) may continue appearing while others have transformed already to vesicles and others have crusted over and formed scabs. As a result, a person may have all three stages of the rash- bumps (papules), fluid-filled blisters (vesicles), and scabbed lesions- at the same time (source: cdc.gov & mayoclinic.org). 93) (D) Varicella is contagious from 1 to 2 days before the onset of rash to the period until all lesions have crusted over. 94) (A) Huntington disease is an inherited disorder. Post-herpetic neuralgia, herpes zoster ophthalmicus, and Ramsay Hunt syndrome are all potential complications of shingles. 95) (B) Post-herpetic neuralgia is a complication of shingles that affects nerve fibers and skin, causing burning pain that lasts long after the rash and blisters of shingles disappear (source: mayoclinic.org). 96) (D) The elderly and the immunocompromised are most at risk for post-herpetic neuralgia. 97) (B) Amitriptyline, Depakote, and Gabapentin are all medications used to treat post-herpetic neuralgia. Diazepam is not a medication prescribed for post-herpetic neuralgia. 98) (C) Xanthelasma is not a symptom that would be produced by herpes zoster ophthalmicus. During the acute phase of the disease, symptoms may include a painful forehead rash, severe ocular pain, eyelid edema, conjunctival hyperemia (excess of blood vessels), corneal edema, and photophobia. 99) (C) Herpes zoster ophthalmicus affects cranial nerve V, the trigeminal nerve. 100) (D) Herpes zoster ophthalmicus can lead to corneal blindness. 101) (A) Ramsay Hunt syndrome primarily affects cranial nerves VII (the facial nerve) and VIII (the vestibulocochlear nerve). This can cause facial paralysis and hearing loss on the affected side (source: patient.info). 102) (C) Scabies is an infection of the skin. It is a contagious, intensely itchy skin condition caused by a tiny, burrowing mite. 103) (B) The causative agent of scabies is a mite, called the human itch mite, which is an eightlegged bug that is so small that it cannot be seen on the skin. People get scabies when the mite burrows into the top layer of the skin to live and feed. A female mite often burrows into the human skin to lay her eggs. When the skin reacts to the mite, an extremely itchy rash develops. This itching is mainly at night. Itching is the most common symptom of scabies. Itching can be so intense that it can keep a person awake at night. Scratching the itchy rash can cause sores and infection to develop in the sores (source: aad.org). 104) (C) Scabies can be transmitted from infected person to another person. Most people get scabies from direct, skin-to-skin contact. Less often, people pick up mites from infested items such as bedding, clothes, and furniture. The mite can survive for about 48 to 72 hours without human contact. Anyone from any age group or race can get scabies. People who are very clean and neat can get scabies. It tends to spread easily in nursing homes and extended-care facilities. A dermatologist can successfully diagnose and treat scabies. To check if the person has scabies, a dermatologist may scrape off a tiny bit of skin on a glass slide and look at the slide under a microscope. If scabies mites or their eggs are seen, then scabies can be definitively diagnosed. Scabies is a short-term condition that can resolve completely with treatments today (source: aad.org). 105) (C) The primary treatment for scabies is permethrin 5% cream. 106) (A) Norwegian scabies is a rare, severe form of scabies. It is extremely contagious because of the larger number of mites in and on the skin. People who have crusted scabies have 100s or even 1,000s of mites in their skin. By comparison, most people who get scabies have 15 to 20 mites on their skin. Characteristics of this form of scabies include scaly, crusted sores on the hands, feet, scalp, face, torso and pressure-bearing areas such as the elbows. Facial skin may flake off, and significant hair loss can result. The itching is generally mild despite the heavy infestation of mites. Crusted scabies develops in people who have a weak immune system due to a medical condition, the elderly, and people who are living in institutions. Crusted scabies develops when the person’s body cannot develop any resistance to the mites. Without resistance, the mites quickly multiply (source: webmd.com & aad.org). Image: Norwegian scabies 107) (A) Tinea capitis (ringworm of the scalp) is spread by direct contact such as through sharing contaminated objects such as a hairbrush. 108) (B) School-aged children are the highest risk demographic group for contracting and spreading tinea capitis (ringworm of the scalp) due to the fact that they commonly share personal items such as hats, combs, brushes, etc. College students are more aware of this and are less likely to do so. Therefore, tinea capitis is seen most often in children. 109) (D) The key clinical symptom of tinea capitis is loss of scalp hair (alopecia). Tinea capitis is the single greatest cause of alopecia in children. Areas that are infected appear bald with small black dots, due to hair that has broken off. The person may have round, scaly areas of skin that are red or inflamed. A person may have kerion, a condition in which there are inflamed areas of pus-filled sores on the scalp. A person with tinea capitis almost always has itching of the scalp. A person may have a low-grade fever around 100-101°F or swollen lymph nodes in the neck. Tinea capitis can cause lasting scars on the scalp. Tinea capitis does not cause whitening of the hair. 110) (B) Griseofulvin is the gold standard treatment for tinea capitis. 111) (A) Amoxicillin clavulanate (Augmentin) is the preferred antibiotic for both human and animal bites. If there is a penicillin allergy, doxycycline is an acceptable alternative, except for children younger than eight years and pregnant women. Other acceptable combinations include clindamycin and a fluoroquinolone in adults or clindamycin and trimethoprim-sulfamethoxazole in children (source: aafp.org). 112) (A) Erysipelas is an infection of the upper dermis and superficial lymphatics that typically presents with a reddened skin rash. Image: Erysipelas Credit: Photograph by CDC/Dr. Thomas F. Sellers/Emory University, released in the public domain 113) (C) Erysipelas is more demarcated than cellulitis. Erysipelas is more superficial (nearer to the outer surface of the skin), more raised, and more demarcated than cellulitis. Demarcated means that it has a clear, cut area of infection. Cellulitis is more generalized and doesn’t have such demarcation. Infected individuals with erysipelas normally develop flu-like symptoms within 48 hours of infection. 114) (A) Erysipelas is most often caused by group A strep bacteria. The group A strep infects the person through breaks in the skin such as through scratches. 115) (D) Purple striae on the skin would be most indicative of Cushing’s disease. 116) (A) Macular degeneration is the most common cause of blindness in the United States. 117) (A) Arcus senilis is a narrow opaque band encircling the cornea, common in older adults. It develops gradually and is not associated with any vision changes. It is caused by a deposition of fat on the cornea. It doesn’t require treatment (source: mayoclinic.org). 118) (C) Arcus senilis is a narrow plaque band encircling the cornea. It is common in older adults. It is caused by a deposition of fat. If it is found in young adults (typically seen in people less than 45 years old), it can be a sign of familial hyperlipidemia, a condition in which younger people have severe cases of high cholesterol and high triglycerides passed down through family (hence, why it’s called familial hyperlipidemia). 119) (B) Tinea versicolor is a common fungal infection of the skin that causes patches of discolored skin. The fungus interferes with the normal pigmentation of the skin, resulting in small, discolored patches. These patches may be lighter or darker in color than the surrounding skin and most commonly affect the trunk and shoulders. Image: Tinea versicolor 120) (B) Tinea versicolor is common in hot environments such as tropical and subtropical environments, not cold environments. Tinea versicolor is a chronic fungal infection of the skin. It is most common in adolescent boys and young adult men due to the fact that they have oily skin. Tinea versicolor is caused by a fungus called Pityrosporum ovale, which is normally found on the human skin and causes problems only in certain circumstances 121) (C) The main symptom of tinea versicolor is patches of discolored skin. The patches normally have sharp borders (edges) and is often reddish to tan in color. The patches may be scaly in appearance. The patches do not darken in the sun, so they may appear lighter than the surrounding healthy skin, but they can be darker. The patches may produce itching. Tinea versicolor is not a painful condition; it normally produces no pain at all. 122) (B) Tinea versicolor is treated with antifungals. It is a fungal infection caused by Pityrosporum ovale, a fungus which is normally found on the skin. In certain conditions, this fungus can cause tinea versicolor. 123) (C) Changes to skin caused by tinea versicolor can last for months or even all year round. Tinea versicolor is a chronic skin condition. The spots may disappear when the temperature drops and return when the air gets warm and humid. Or they may remain the duration of the year if the weather is constantly hot. Though it may persist for a long period of time, the skin changes associated with tinea versicolor aren’t irreversible. People who live in non-tropical areas often see tinea versicolor disappear during the cool, dry months. 124) (D) Tinea versicolor is caused by the fungus Pityrosporum ovale. It is a type of yeast (a yeast is a type of fungus). Risk factors that cause of an overgrowth of this yeast include hot weather and moist, oily skin. This why skin with a lot of sweat on it increases the risk for overgrowth of this yeast. This is also the reason why humid weather is a risk factor for overgrowth as well. Non-humid weather is a not risk factor for the overgrowth of Pityrosporum ovale. 125) (D) Senile purpura is a benign skin condition that is common in older adults. It is caused by increased vessel fragility due to connective tissue damage to the dermis. It causes purple ecchymoses commonly located on the dorsum of the forearms and hands. It is not a precancerous condition. Image: Senile purpura 126) (B) Meniere’s disease is a disorder of the inner ear. 127) (D) Symptoms of Meniere’s disease include vertigo, fluctuating hearing loss that ultimately leads to permanent hearing loss, tinnitus (ringing in the ears), and sometimes a feeling of fullness or pressure in the ear. It can also lead to problems with balance, creating a higher risk for falls. Meniere’s disease can affect both ears, but most commonly affects one ear. Tension headaches are not associated with Meniere’s disease. 128) (A) Meniere’s disease is a chronic illness. It is not an acute illness that comes and goes. There is no cure for Meniere’s disease, but symptoms can be managed through lifestyle changes and medications. Meniere’s disease usually starts between the ages of 20 and 50. Meniere’s disease causes fluctuating hearing loss, ultimately leading to permanent hearing loss. The cause of Meniere’s disease is unknown. 129) (D) Aspirin and medications that can contain aspirin generally should be avoided in people who have Meniere’s disease. This is because aspirin can cause tinnitus or in the case of Meniere’s disease worsen the existing tinnitus. Meclizine is taken to help with the vertigo that a person with Meniere’s disease experiences. Promethazine is taken to help decrease the nausea and vomiting a person with Meniere’s disease may have, especially during episodes of vertigo. Since Meniere’s disease is believed to be due to excess endolymphatic fluid in the inner ear, diuretics such as hydrochlorothiazide may be prescribed to decrease excess fluid from the body. 130) (C) A low-salt diet is recommended for people who have Meniere’s disease due to the fact that salt causes fluid retention. Since Meniere’s disease is believed to be caused by an excess of fluid in the inner ear, excess salt consumption (which causes fluid retention) is discouraged. Some people with Meniere’s disease reports that a low-salt diet helps; others do not. But this diet is often recommended by healthcare professionals. 131) (C) Xanthelasma are yellow plaques that occur most commonly on or near the upper or lower eyelids, though they are more common on the upper eyelids (source: emedicine.medscape.com). Image: Xanthelasma 132) (B) When there is no family history of xanthelasma, it is most likely due to high cholesterol levels. The yellow plaques that form are made up of deposits of cholesterol. If there is a family history, it may simply be genetic, since there is a genetic component to xanthelasma. In this case with a family history, it may or may not be due to high cholesterol levels. And in some cases of xanthelasma, even if there is no family history, it may not be due to high cholesterol but most times it is. 133) (D) Xanthelasma is condition which causes yellow plaques to appear most often on or near the eyelids. It is neither a harmful nor painful condition. It does not often cause secondary skin infections. Xanthelasma is seen with most frequency in adults over age 40 and the elderly. It can still be found in children, but occur most often in people who are middle age or in the elderly. It is most common with people of Asian or Mediterranean descent. 134) (C) Xerosis is a condition in which the skin is abnormally dry. It is the medical term for abnormally dry skin. Xerosis is common, especially in the elderly. As the body ages, it becomes harder for the skin to retain moisture. Image: Xerosis 135) (B) Xerosis is most common during the winter months. 136) (A) A cherry angioma is a benign red papule containing a proliferation of blood vessels. Image: Cherry angioma 137) (A) Cherry angiomas are often not treated and are unlikely to cause any health problems. 138) (D) Cherry angiomas are not self-limiting, so they may never go away. In fact, they tend to increase in number and size as one gets older. Though they don’t lead to further health problems, some people want them removed for better cosmetic appearance. There are a number of surgeries to get rid of cherry angiomas, if one chooses. These include electrocauterization (an electric current to burn the angioma), cryosurgery (freezing the angioma with liquid nitrogen), laser surgery (a pulsed dye laser is used to get rid of the cherry angioma), and shave excision (removing the cherry angioma from the top portion of the skin). Cherry angiomas are most often found in adults age 30 or older. The exact cause of cherry angiomas is unknown. Cherry angiomas are prone to bleeding if irritated (due to the fact that they contain a proliferation of blood vessels). 139) (D) Acanthosis nigricans is a skin disorder characterized by areas of dark, velvety discoloration in body folds and creases. It is a very common condition affecting millions of people in the United States. Image: Acanthosis nigricans 140) (B) Acanthosis nigricans is a skin disorder characterized by areas of dark, velvety discoloration in body folds and creases. Common body parts affected include the armpits, groin, and neck. The skinfolds of the fingers are not commonly affected. 141) (B) Acanthosis nigricans is found most often in people who have diabetes and/or who are obese. If people do not have diabetes who have acanthosis nigricans, they are at higher risk for developing type II diabetes. Rarely, acanthosis nigricans can be caused by a cancerous tumor in the body, such as the stomach or liver. 142) (B) Pain is not associated with acanthosis nigricans. It is not normally painful or inflamed. The only symptom associated with acanthosis nigricans is skin changes. It does not have any other effects on the body. The skin may have an odor and may itch. 143) (D) The treatment for acanthosis nigricans is to treat the underlying condition causing it. If it is obesity, then the condition may be reversed by losing weight. If the condition is caused by a tumor, then treatment of the tumor such as surgically removing it may clear up the skin. 144) (B) Actinic keratosis is a precancerous condition characterized by scaly, crusty lesions (growths) on the skin that are caused by damage from the sun’s ultraviolet (UV) rays. The lesions are often elevated, rough in texture, and resemble warts. Image: Actinic keratosis 145) (D) The cause of actinic keratosis is UV rays, either from the sun or from tanning beds. As with most skin cancers, chronic, prolonged sun exposure is linked to actinic keratosis. 146) (C) The most common type of skin cancer that actinic keratosis leads to is squamous cell carcinoma. The second most common form of skin cancer actinic keratosis can lead to is basal cell carcinoma, which is the most common form of skin cancer. 147) (A) Being fair or pale skinned is a risk factor for actinic keratosis. Fair-skinned people tend to have a lower tolerance to the sun’s ultraviolet (UV) rays; as a result, they are more likely to obtain skin damage from sun exposure. Dark-skinned people tend to have a higher tolerance to how much UV rays they can take before their skin is damaged. Age 40 or older is a risk factor for actinic keratosis, not ages 20 to 30. There is no direct association between a high-fat diet and actinic keratosis. 148) (B) A lipoma is a slow-growing fatty lump (composed of adipose tissue) that is most often situated between the skin and muscle layer. A lipoma is not precancerous or cancerous and is usually harmless. A lipoma rarely is a serious medical condition. Unless it is painful or bothers a person, treatment generally is not necessary. Image: Lipoma 149) (D) The cause of lipomas is unknown. The greatest link that causes lipomas seems to be genetic, as lipomas tend to run in families. 150) (D) Lipomas can occur at any age, but they are most common in middle age (age 40 to 60 years old). 151) (A) Vitiligo is a chronic skin condition characterized by patches of skin losing their pigmentation and becoming white (pale). Image: Vitiligo 152) (C) There is no known cause for vitiligo. It is believed to be due to genetic susceptibility, that when triggered by an environmental factor(s), causes the body’s immune system to destroy skin pigment cells. Vitiligo is classified into 2 main types: segmental and non-segmental vitiligo. Non-segmental vitiligo is vitiligo that affects both sides of the body. This is the more “severe” form of vitiligo and usually gets worse over time. Segmental vitiligo is vitiligo that affects mostly one side of the body. Segmental vitiligo is seen as the more “mild” form of vitiligo and typically does not worsen over time. About 90% of vitiligo cases are nonsegmental (affects both sides of the body) and about 10% are segmental (affects mostly one side of the body). 153) (B) Globally, vitiligo affects about 1% of the population. Males and females are equally affected. About half show signs of this skin disorder before the age of 20 and most develop it before the age of 40. 154) (D) Melanin is the pigment produced by cells in our body (called melanocytes) that gives human skin, hair, and eyes their color. In people with vitiligo, there is a deficiency in the amount of melanin produced, which causes a loss of pigmentation of the skin; this causes white patches of skin. Vitiligo occurs because the cells that produce melanin (melanocytes) die or stop functioning. 155) (B) Vitiligo is not a contagious disorder. Vitiligo affects people of all skin colors, light or dark. It is most prominent and easily noticed in individuals with darker skin, because the contrast of the white patches versus the dark skin makes it more noticeable; however, it occurs in people of all skin colors. Vitiligo may not just affect the skin. It can also affect the tissue that lines the inside of the mouth and nose or the inner layer of the eyeball (the retina). Vitiligo is not a lifethreatening condition. 156) (C) Vitiligo is a type of autoimmune disease in which the immune system dysfunctions and attacks melanocytes in the body. This causes loss of pigmentation in the skin and white patches. 157) (C) Vomiting is not a common symptom of cellulitis. Common symptoms of cellulitis include swelling of the skin, inflamed, red skin, and a fever. 158) (B) A subungual hematoma is bleeding underneath the fingernail or toenail. 159) (B) A furuncle, also called a boil, is a bacterial or fungal infection of hair follicles. The infected hair follicles can be on any part of the body. When the hair follicles become infected, the skin around it becomes inflamed. The furuncle looks like a red, raised bump on the skin that can be filled with pus. Image: Furuncle 160) (A) A carbuncle is a skin condition characterized by a cluster of boils coalescing together. These boils are connected subcutaneously. Image: Carbuncle 161) (C) Most carbuncles are caused by staphylococcus aureus bacteria, which inhabit the skin surface, throat, and nasal passages. These bacteria can cause infection by entering the skin through a point of entry such as a hair follicle, small scrape, or puncture. Carbuncles are filled with pus- a mixture of dead white blood cells, bacteria, and dead skin cells. Active carbuncles are contagious and can be spread either to other parts of the body or to other people from direct contact. Carbuncles is not a chronic illness. Depending on the severity, most carbuncles heal within 2 to 3 weeks after medical treatment (source: webmd.com). 162) (B) Seborrheic keratosis is a benign skin condition that causes an overgrowth of tissue on the skin that has a waxy, scaly appearance. Image: Seborrheic keratosis 163) (B) Seborrheic keratosis is found most commonly in middle age adults and the elderly, not children (children rarely have these growths). Seborrheic keratosis is a common skin growth that is comprised of layers of dead skin cells. This usually gives them a waxy, scaly texture. Though some people have just one, it is more common to have many. The number of lesions varies according to person. Seborrheic keratosis is a benign condition; it is not precancerous or cancerous. The lesions can vary widely in color but most are tan or brown. The lesions are normally painless. Seborrheic keratosis normally doesn’t require any treatment, as the condition is harmless. However, some people may opt to have them surgically removed for reasons such as for better cosmetic appearance. 164) (C) Seborrheic keratosis can mimic many other skin conditions including skin cancers such as melanoma. The only way to differentiate it definitively is through a biopsy of the lesion; this will show whether it is cancerous or not. 165) (A) The medical term for a mole is a nevus. 166) (C) Melasma is a skin condition that causes brown to gray-brown patches on the face. Image: Melasma 167) (D) Hormone replacement therapy or patch contraceptives are risk factors for melasma, not treatments. Melasma is common in women, especially pregnant women and those who are taking oral or patch contraceptives or hormone replacement medications. It is believed to be common in pregnancy due to the hormonal changes that occur in pregnancy. Melasma is thought to occur due to the stimulation of melanocytes by the female sex hormones estrogen and progesterone to produce more melanin when the skin is exposed to the sun. This results in the brown to graybrown discoloration in the skin. Women with a light brown skin type who are living in regions with intense sun exposure are particularly susceptible to developing melasma. 168) (C) Psoriasis is a skin condition that causes scaly, itchy, dry rashes. It is characterized by skin cells that multiply up to 10 times faster than normal. As underlying cells reach the skin’s surface and die, their large volume causes raised, red plaques covered with white scales. Image: Psoriasis 169) (C) Psoriasis is a common skin condition that changes the cycle of skin cells. Psoriasis causes skin cells to undergo rapid mitotic division and the skin cells build up rapidly on the surface of the skin. These extra skin cells form thick, silvery scales and itchy, dry, red patches that are sometimes painful. The dry, cracked skin may bleed at times. Besides itching, there may also be burning or soreness. Psoriasis is a persistent, chronic disease that can be characterized by periods of relief, with times of psoriasis flare-ups. Treatment for psoriasis consists of nonprescription cortisone cream and light therapy. It is estimated by the National Psoriasis Foundation that 10% to 30% of people with psoriasis have psoriatic arthritis, a type of inflammatory arthritis that is seen in association with skin psoriasis. 170) (B) Koebner phenomenon refers to new psoriatic lesions or plaques that develop over areas of skin trauma (in people who have psoriasis). Koebner’s phenomenon (or Koebnerisation) is named after German dermatologist Heinrich Koebner who found that the skin of people who have psoriasis which had become traumatized following an injury often developed a psoriatic lesion (or plaque) in the area where psoriasis had not previously affected. This could be any type of skin trauma such as cuts, scrapes, bruises, needle sticks, etc. Image: Koebner phenomenon 171) (A) Auspitz’s sign is a type of diagnostic test is done that is characteristic of psoriasis. When the psoriatic lesion (or plaque) is scraped off such as with a glass slide, underneath the lesion will show pinpoint areas of bleeding that remain. This is characteristic of a psoriatic lesion and thus can be used to differentiate psoriasis from other skin conditions that may mimic it. Image: Auspitz’s sign 172) (D) If a person has psoriasis, changes may occur with the person’s nails, referred to as nail psoriasis. Nail psoriasis can alter the appearance of the nails in several ways. The nails may change color and turn green, yellow or brown. They may also have small red or white spots beneath them. The surface appearance of the nails may develop ridges or grooves, or there may be pitting (small pinprick holes) on the nail surface. Chalky white material can gather under the nail, causing the nail to lift away from the skin; this can cause the nail to loosen and separate from the nail bed, which can be very painful. About a third of people with nail psoriasis can also get a fungal infection that can cause their nails to thicken. They may also get brittle and break. The nails, in general, even without separation from the nailbed, can get tender and hurt with nail psoriasis. Image: Pitted nails seen with psoriasis 173) (A) Guttate psoriasis is a type of psoriasis that looks like small, salmon-pink drops on the skin. The word guttate is derived from the Latin word gutta, meaning drop. Usually there is a fine scale on the drop-like lesion that is much finer than the scales in plaque psoriasis, which is the most common type of psoriasis. The drop-like lesions usually itch. Guttate psoriasis is not contagious. It usually occurs on the trunk, arms, or legs. However, it may cover a large portion of the body. The trigger of the disease is usually a streptococcal (bacterial) infection. As many as 80% of people with guttate psoriasis have a streptococcal infection, usually in the form of tonsillopharyngitis, before the outbreak. The eruption of the skin lesions usually happens about two to three weeks after a person has strep throat. This type of psoriasis can also be chronic. Besides streptococcal bacteria, guttate psoriasis can be triggered by other types of infections as well. For example, the chicken pox or colds can trigger the psoriasis. The guttate form of psoriasis is relatively uncommon. Fewer than 2% of those with psoriasis have the guttate type. Guttate psoriasis is more common in children and adults younger than 30 years. Boys and girls are equally affected. Usually, guttate psoriasis goes away in a few weeks without treatment. Simple reassurance and moisturizers to soften the skin may be sufficient care (source: emedicinehealth.com). Image: Guttate psoriasis 174) (D) Cutaneous larva migrans is a parasitic infection caused by the larvae of various nematode parasites of the hookworm family (Ancyloostomatidae). 175) (B) Cutaneous larva migrans is a parasitic skin infection caused by hookworm larvae that usually infest cats, dogs, and other animals. Humans normally become infected by walking barefoot on sandy beaches or contacting soil that have been contaminated with animal feces. It is also known as creeping eruption as once infected, the larvae migrate under the skin’s surface and cause itchy red lines or tracks. Cutaneous larva migrans is self-limiting. Humans are an unintended dead-end host, so to speak, so the hookworm larvae eventually die. The disease usually takes a few weeks to heal, though it can take months or up to a year in certain cases. To shorten the duration of the disease, effective treatments are available. Anthelmintics are the treatment of choice. Antihistamines and topical corticosteroids may also be used with anthelminthics to provide relief from the itching (source: dermnetnz.org). Image: Cutaneous larva migrans 176) (C) Fordyce spots are a benign condition. They are not associated with any disease or illness, nor are they infectious. They appear on the face, in the mouth, or on the genitals of a person (man or woman). They appear as small, painless, raised, pale, red or white spots or bumps. Image: Fordyce spots 177) (A) Rosacea (roh-ZAY-shuh) is a skin disorder characterized by facial redness. It causes redness on the nose, cheeks, chin, and forehead. Some people may get pimples on the red parts of their faces (referred to as acne rosacea). Rosacea can also cause burning and soreness in the eyes (referred to as ocular rosacea). Image: Rosacea 178) (B) A biopsy is not necessary in order to diagnose rosacea. The pattern of redness on a person’s face that rosacea causes makes it easy for a doctor to diagnose. The cause of rosacea is unknown. Rosacea tends to run in families, so there is possibly a genetic link, but experts don’t definitively know its cause. Besides the skin, rosacea can also affect the eyes, causing dry, red, irritated eyes. There is no cure for rosacea. Treatment is centered around controlling and managing the disorder. 179) (D) Rosacea can occur in anyone but it most commonly affects middle-aged women who have fair skin. 180) (A) The main class of medications used to treat rosacea is antibiotics. Low-dose antibiotics like doxycycline may be used. Skin creams may also be used that contain antibiotics such as topical metronidazole gel or azelaic acid. 181) (B) A comedo is a clogged hair follicle (pore) on the skin. 182) (C) Comedones may be open, in which case they are referred to as blackheads. Or they may be closed, in which case they are referred to as whiteheads. The follicles in closed comedones (whiteheads) are completely blocked. Comedones can occur with or without acne. Image: Comedones 183) (B) Acne is a skin condition that is usually characterized by comedones and papules and pustules. Comedones are clogged hair follicles (pores) on the skin. Hair follicles get clogged due to keratin (skin debris) and oil combining to block the hair follicle (pore). Comedones can be open (blackhead) or closed (whitehead). So, acne is a condition that is usually characterized by comedones (blackheads and/or whiteheads) along with papules and pustules (pimples). Papules are raised lesions (like bumps) that contain no visible fluid. Pustules are raised lesions that contain pus-filled fluid. Acne may also be composed of cysts or nodules. Image: Acne 184) (C) Acne is graded on a scale of 1 to 4. Grade 1 is considered mild acne. Grade 1 acne is characterized by the appearance of open comedones, or blackheads. Grade 2 acne is considered moderate acne. In moderate acne, blemishes appear in greater numbers. It is marked by the presence of whiteheads, which are closed comedones; there may be some slight swelling with mild inflammation in this stage. With Grade 2 acne, there will also be occasional papules and pustules. Grade 3 acne is considered severe acne. Acne moves to Grade 3 when blemishes occur in larger numbers and inflammation is more pronounced. Blemishes may be so dense that they spread and merge together, resulting in an entire area of skin being infected rather than just a single pore. There is a greater incidence of papules and pustules in grade 3 acne. Grade 4 acne is considered cystic acne. Cystic acne is characterized by large blemishes on the face and jaw line which can also affect the upper body, neck, arms, shoulders and back. The aggravated nature of Grade 4 acne often results in cysts, which are deep blemishes more than 5 mm in diameter. Their appearance is similar to that of a boil, with a smooth, tender surface that is painful to the touch. Nodules are hard, painful bumps that are similar to cysts but contain no pus or other fluids. They can last for weeks or months and even go dormant only to reappear later on (source: myclaritymd.com). 185) (D) Isotretinoin, a type of oral retinoid, is used for moderate to severe acne. 186) (A) Initial monotherapy for acne normally is benzoyl peroxide gel. 187) (C) Standard treatments for mild to moderate acne include benzoyl peroxide gel, topical retinoids, and antibiotics. 188) (A) Mild acne may be treated only with topical treatments. This may include topical retinoids (vitamin A), benzoyl peroxide gel, and topical antibiotics (such as clindamycin or erythromycin). Moderate to severe acne may involve the use of oral medications such as isotretinoin and oral antibiotics. 189) (C) Another term used for pimples is pustules. A pustule (pimple) is a small, inflamed skin swelling that is filled with pus. 190) (A) A macule is a flat, distinct, discolored area of skin less than 1cm wide that does not involve any changes to the texture or thickness of the skin. Papules are raised lesions (like bumps) that contain no visible fluid. A pustule (pimple) is a small, inflamed skin swelling that is filled with pus. Image: Macule 191) (A) A torus palatinus is a benign bony protrusion on the hard palate of the mouth, that is usually midline on the palate. Image: Torus palatinus Credit: Photograph distributed under the Creative Commons Attribution-Share Alike 3.0 Unported license 192) (B) Pityriasis rosea is a skin condition that is characterized by patches (rashes) on the chest, belly, or back. These patches are referred to as herald patches. Pityriasis rosea can also lead to a classic “Christmas tree” pattern on a person’s back. Image: Pityriasis rosea herald patches Image: “Christmas tree” arrangement of patches with pityriasis rosea 193) (C) Pityriasis rosea, unlike many other skin conditions, is not caused by a fungus or bacteria and it is not caused by an allergic reaction. It is believed to be possibly caused by a virus. Pityriasis rosea is a benign condition. It’s usually harmless. It is not believed to be a contagious skin disorder. Pityriasis rosea usually goes away on its own. It usually lasts for about 6-8 weeks. 194) (C) Meningococcemia can be spread from person to person through direct contact with bodily secretions (such as nasal secretions) and through respiratory droplets. 195) (C) Both meningococcemia and meningitis may be caused by the same Neisseria meningitidis bacteria. When the bacteria infect the membranes that cover the brain and spinal cord, it is meningitis. When the infection remains in the blood but does not infect the membranes that cover the brain or spinal cord, it is meningococcemia. Both have similar symptoms such as fever, headache, nausea, and a stiff neck. And both are medical emergencies that need to be treated right away. 196) (B) Fulminant meningococcemia can cause changes in the skin that are characterized by diffuse purpuric skin lesions throughout the body. Image: Purpura fulminans associated with meningococcemia 197) (D) The meningococcal vaccination is recommended for all college students living in a dormitory. 198) (B) Rifampin is used as prophylaxis for those who have been in close contact with someone with meningococcemia. Rifampin is taken every 12 hours for 2 days for prophylaxis in adults (source: cdc.gov). 199) (C) A full thickness (third degree) burn is the only type of burn that is painless. This is because the burn penetrates so deeply into the skin that the nerves (which sense pain) are damaged. Therefore, the client feels no sensation. 200) (A) Superficial thickness (first degree) burns are the only type of burns that never forms blisters. First-degree burns are the only burns that don’t penetrate the skin. They affect only the outermost part of the epidermis. Therefore, they don’t create blisters on the skin. 201) (C) The entire torso (chest and back) represents 36% of TBSA, the entire right leg represents 18% of TBSA. Adding these together gives a TBSA of 54%. 202) (B) Another name for enterobiasis is pinworms. 203) (B) Enterobiasis is most commonly spread through the fecal-oral route. The fecal-oral route is the transfer of infective pinworm eggs from the anus to someone’s mouth, either directly by hand or indirectly through contaminated objects. Pinworm infections are rarely spread through the use of swimming pools. Although chlorine levels found in pools are not high enough to kill pinworm eggs, the presence of a small number of pinworm eggs in a large swimming pool makes the chance of infection unlikely. Enterobiasis is the most common worm infection in the United States. When a person has been infected with pinworms, all household contacts and caretakers should be treated at the same time. Hand hygiene is the most effective means for the prevention of enterobiasis. Pinworms commonly affect children with the greatest frequency, who place their hands on many surfaces without washing them. Hand hygiene is vital. Another prevention method is trimming and scrubbing the fingernails. Since enterobiasis causes itching, this can cause pinworms to accumulate in the fingernails when a person scratches. Shortened nails lessen the chance of having pinworms accumulate underneath the nails (since they’re short). 204) (B) The tape test is a common test that is done to check for enterobiasis (pinworms). How pinworms generally work is that they most commonly live in the colon and rectum of humans. While an infected person sleeps, female pinworms leave the intestine through the anus and deposit their eggs on the surrounding skin. Therefore, placing tape on the anus area firmly and lifting up the tape will remove these eggs. If eggs are present, they will usually stick to the tape. The tape can then be placed on a slide and examined under a microscope. Because activities such as washing/bathing or having a bowel movement can remove eggs from the skin, this test should be done either hours into the night or as soon as the person wakes up before engaging in any morning activities. The tape test should be done on 3 consecutive mornings to increase the chance of finding pinworm eggs. Because itching and scratching is common in pinworm infections, samples taken from underneath the fingernails may also contain eggs. Pinworm eggs are rarely found in routine stool or urine samples. 205) (B) Mebendazole is an anthelmintic (anti-parasitic) used to treat worm infections such as pinworms, roundworms, and hookworms. Other drugs that can be used are pyrantel pamoate and albendazole. Pyrantel pamoate is available without the need for prescription. 206) (A) Enterobiasis mainly occurs in school-aged and preschool-aged children (source: cdc.gov). 207) (C) The main symptom of enterobiasis is rectal itching. When the pinworm infection is heavy, there can be a secondary bacterial infection due to the irritation and scratching of the anal area (source: cdc.gov). 208) (A) Intense itching during the night is strongly suggestive of enterobiasis (pinworms). 209) (B) Osteoarthritis is not associated with uveitis. Rheumatoid arthritis, ankylosing spondylitis, and Bechet’s disease can cause uveitis. 210) (B) Intertriginous dermatitis (also known as intertrigo) is an inflammatory condition of skin folds. Intertrigo is induced or aggravated by heat, moisture, maceration, friction, and lack of air circulation. Intertrigo commonly affects the axilla, perineum, inframammary creases, and abdominal folds. (Intertriginous areas refer to skin folds, such as underneath the breasts. Intertriginous dermatitis is dermatitis affecting the skinfolds.) Image: Intertriginous dermatitis 211) (A) The most common areas affected by intertrigo include larger skin-fold areas including the armpits, beneath the breasts, the genital area, and the abdomen. However, intertrigo may appear in any of the skin folds that rub together and trap moisture. So, this also includes between the toes and fingers, in the inner thighs, in the crease of the neck, and between the buttocks. 212) (A) Moisture, not dryness, is a risk factor for intertrigo. There are several risk factors for intertrigo. A person is more likely to develop intertrigo who has diabetes or is obese. A person who is wearing a brace or splint is also at higher risk because braces and splints trap moisture. This is also why being exposed to high heat and humidity is a risk factor. Other risk factors include incontinence, excessive sweating, poor hygiene, malnutrition, and a suppressed immune system. 213) (A) Rheumatic fever is caused by infection with group A streptococcus bacteria. Group A strep can also cause scarlet fever, impetigo, and glomerulonephritis. 214) (D) The most likely scenario of a child getting rheumatic fever is getting infected with group A strep bacteria and first getting a sore throat. If the sore throat is not treated (normal treatment would be antibiotics), the infection could spread to other parts of the body and cause systemic effects such as joint pain. Rheumatic fever is infamous for heart involvement and can damage the heart, particularly the mitral valve. All of this stems from the fact that the child’s group A strep infection was left untreated. 215) (D) Rheumatic fever can cause permanent damage to the heart. It can cause inflammation of the heart called carditis. It tends to particularly affect the valves of the heart, most typically the mitral valve. Even after the rheumatic fever is resolved, the heart, especially the valves, may be damaged and need surgical repair. 216) (B) Though rheumatic fever can occur in younger children and adults, it is most common in children ages 5-15 years old. 217) (B) In order to diagnose rheumatic fever, a person must have either 2 major criteria or they must have 1 major criterion and 2 minor criteria. The major criteria of rheumatic fever can be memorized by the J♥NES criteria. J stands for joints, particularly arthritis, which is inflammation. ♥ stands for carditis, inflammation of the heart. Rheumatic fever particularly affects the valves of the heart; most commonly, the mitral valve becomes inflamed and damaged. N stands for nodules, particularly subcutaneous nodules that can occur with rheumatic fever. Subcutaneous nodules are lumps that are found underneath a person’s skin. E stands for erythema marginatum, which are slightly raised, red, painless rashes that can occur. S stands for Sydenham’s chorea, which are neurological in origin. They are rapid, involuntary, uncontrollable jerking movements affecting the face, hands, and feet. It is a major sign of acute rheumatic fever. So, in summary, the major signs of rheumatic fever are arthritis, carditis, subcutaneous nodules, erythema marginatum, and Sydenham’s chorea. There are 4 minor criteria. The minor criteria include fever, arthralgia (pain in the joint), elevated erythrocyte sedimentation rate (ESR) or Creactive protein (CRP), and a prolonged PR interval on an EKG. Again, if a person has 2 major criteria or the person has 1 major criterion and 2 minor criteria, this is sufficient to make a diagnosis of rheumatic fever. Of course, there must be group A strep cultured as the etiology. Image: Subcutaneous nodule that may be seen in Rheumatic fever 218) (B) Penicillin is the drug of choice used to treat rheumatic fever. If a person is allergic to penicillin or otherwise cannot tolerate it, then erythromycin can be used as an alternative. 219) (C) Urinalysis typically is not done for rheumatic fever. Tests for rheumatic fever include a culture (through a swab of the throat) or antistreptolysin O titers (to identify the group A strep organism), ESR and CRP (to identify the level of inflammation in the body), and an EKG to identify any heart abnormalities such as a prolonged PR interval, which can be found in rheumatic fever. 220) (B) Illnesses such as rheumatic fever can recur later in life. Therefore, antibiotics should be given prophylactically before procedures such as surgeries and dental procedures. Just like when treating the acute illness, penicillin is the choice drug given prophylactically before procedures. If the patient is allergic to penicillin, erythromycin can be used as an alternative. 221) (A) Just like rheumatic fever, scarlet fever is caused by group A strep bacteria. 222) (B) Photophobia is not a common symptom of scarlet fever. Common symptoms of scarlet fever include a bright red, sandpaper-textured rash that covers most of the body, a sore throat, a strawberry tongue, and a high fever. Image: Scarlet fever bright sandpaper-textured rashes Image: Strawberry tongue seen with scarlet fever 223) (D) Seborrheic dermatitis is a skin condition that frequently causes red skin, scaly patches, and dandruff. Deposits of yellow mucus on the skin is not associated with seborrheic keratosis. 224) (B) Seborrheic dermatitis most frequently occurs on the scalp. 225) (D) Acral lentiginous melanoma affects women and men about equally. Acral lentiginous melanoma is a type of melanoma that affects the soles of the feet, the palms of the hands, or beneath the nails. More rarely, it can be found in the oral mucosa. It is more common on the feet than on the hands. Acral lentiginous melanoma is the most common type of melanoma in darkskinned individuals as well as Asians. It accounts for less than 1% of melanoma in fair-skinned individuals. The type of acral lentiginous melanoma that affects the nails may present as a longitudinal tan, black, or brown streak on the finger underneath the nailbed (source: dermnetnz.org & ncbi.nlm.nih.gov). Image: Acral lentiginous melanoma seen underneath a fingernail 226) (C) A mole that is melanoma has a diameter that is greater than 6mm. The criteria to determine if a mole is melanoma is the “A, B, C, D, E” criteria of melanoma. The “A, B, C, D, E” criteria of melanoma involve A (asymmetry), B (border irregular), C (color varies in the same region), D (diameter > 6mm), E (enlargement or change in size). 227) (A) Though there are many allergens that cause allergic rhinitis, the most common type of allergen that causes it is pollen. Other possible triggers include grass, dust mites, cockroaches, cigarette smoke, and perfume. 228) (C) When an allergen comes into contact with a person’s body, the body releases histamine in response. Histamine is secreted by basophils and mast cells as part of a local immune response to the presence of invading bodies (such as allergens). The basophils and mast cells are found in nearby connective tissue. This histamine release causes capillaries to become more permeable to white blood cells and other proteins, which proceed to target and attack foreign bodies in the affected tissue (source: news-medical.net). 229) (D) There are 2 types of allergic rhinitis- seasonal and perennial. Perennial allergic rhinitis is that which occurs all year round. Pollen-based allergies are usually seasonal (strongest during the summer and fall). 230) (C) Rhinitis medicamentosa is rebound nasal congestion brought on by extended use of topical decongestants and certain oral medications. Examples of topical decongestants include oxymetazoline, phenylephrine, xylometazoline, and naphazoline nasal sprays. 231) (A) SLE is most commonly found in women rather than men with a 9:1 ratio. Out of the races, it is most commonly found in black or Hispanic women. 232) (C) SLE typically is not associated with endocarditis. The most common way that lupus affects the heart is pericarditis, inflammation of the pericardium (the sac that surrounds the heart). Symptoms accompanying pericarditis are typically a sharp pain the chest and at times shortness of breath. Other common symptoms of lupus include fatigue, joint pain, anemia, fever, malaise, red ashes, alopecia (hair loss), major depression, photophobia, Raynaud’s syndrome, and weight loss. 233) (B) Stasis dermatitis is inflammation of the skin of the lower legs caused by chronic venous insufficiency. Image: Stasis dermatitis 234) (C) Women are slightly more likely to get stasis dermatitis than men. This is most likely due to the fact that pregnancy results in significant stress on the lower-extremity venous system. Risk factors for stasis dermatitis include high blood pressure, venous insufficiency (occurs when a person’s veins have difficulty sending blood from the legs to the heart), varicose veins (swollen and enlarged veins that are visible under the skin), congestive heart failure, kidney failure, injury to the lower legs, multiple pregnancies, a DVT in the leg, obesity, prolonged standing or sitting, and an age greater than 50 years old. 235) (B) Stasis dermatitis occurs as a direct consequence of venous insufficiency. The loss of valvular function in the veins of the lower legs to bring blood back up to the heart (due to agerelated decrease in valve competency) is the most common cause of stasis dermatitis. However, it can be a result also of events such as deep vein thrombosis, surgery such as vein stripping, total knee arthroplasty, harvesting of saphenous veins for coronary bypass, or traumatic injury; all of these can severely damage the function of the lower leg venous system and result in pooling of fluid in the lower extremity, which can lead to stasis dermatitis. Stasis dermatitis typically affects middle-aged adults and elderly patients and rarely occurs before the fifth decade of life. An exception would be patients with acquired venous insufficiency due to surgery, trauma, or thrombosis. Stasis dermatitis can occur in one or both legs. Stasis dermatitis is a chronic condition that can’t be cured but can be managed. 236) (C) Lentigo is a skin condition that is characterized by small pigmented macules (that are tan to brown-colored) on the skin that are well defined and that are surrounded by normalappearing skin. Image: Lentigines (plural for lentigo) 237) (C) Lentigines are caused by sun exposure. 238) (A) Lentigo is a benign skin condition; it is not a precursor to any cancerous condition. Lesions associated with lentigo tend to increase in number with age. Lentigines are more common in light-skinned people. Lentigines are also referred to as liver spots. 239) (B) Koilonychia is characterized by spoon-shaped nails. This is why koilonychia is also known as spoon nails. It refers to abnormally thin nails (usually of the hand) which have lost their convexity, becoming flat or even concave in shape. Image: Koilonychia 240) (D) The most common cause of koilonychia (spoon-shaped nails) is chronic iron-deficiency anemia. Koilonychia is more a sign of systemic problems (hypochromic anemia) than it is a localized problem. 241) (B) A faun tail nevus is a posterior midline cutaneous lesion that involves localized hair on the spine. It is a sign of a spinal anomaly such as spina bifida. 242) (A) Café-au-lait spots are hyperpigmented macules that may vary in color from light brown to dark brown. Café-au-lait spots are called referred to as café-au-lait macules. 243) (B) Café-au-lait spots are either light to dark brown in color. Image: Café-au-lait spots 244) (C) Café-au-lait skin spots are usually the earliest manifestations of neurofibromatosis. Café-au-lait macules are observed in 95% of patients with neurofibromatosis type 1 (NF1), which is the most frequently occurring neurocutaneous syndrome. 245) (B) Presbyopia is age-related farsightedness. It is a gradual, age-related loss of the eyes' ability to focus actively on nearby objects. 246) (B) People with presbyopia have difficulty seeing objects that are nearby. Presbyopia normally occurs beginning in the early to mid-40s and worsens until about age 65. On onset, people experience blurred near vision during activities that require close vision such as reading or working at a computer. Presbyopia occurs due to the natural aging process. Presbyopia is a very common condition, with millions of new cases in the United States each year. According to the World Health Organization, more than a billion people in the world were presbyopic as of 2005. 247) (D) Strabismus is a condition in which there is misalignment of the eyes. With this condition, the person’s eyes do not look in exactly the same direction at the same time. 248) (B) Strabismus is a common condition, with millions of cases in the United States per year. Strabismus is a condition that is caused due to poor eye muscle control. It is also referred to as crossed eyes. The misalignment of the eyes can be inward, outward, upward, or downward. 249) (A) Esotropia is a form of strabismus in which one or both eyes turn inward. Exotropia is a form of strabismus in which one or both eyes turn outward. Hypertropia is a form of strabismus in which one eye is deviated upwards in comparison to the other eye. Hypotropia is a form of strabismus in which one eye is deviated downwards in comparison to the other eye. 250) (A) Esotropia is a normal and common finding in infants. Most infants are born with eyes that are not aligned at birth. It is common in infancy for an infant to appear as if s/he has esotropia, because the bridge of the nose is not fully developed. 251) (B) Amblyopia is the medical term for lazy eye. Amblyopia can result from any condition that prevents the eye from focusing clearly. 252) (C) The single cover (cover/uncover) test is a test that is used to screen for strabismus. During the cover test, each of the eyes are covered one at a time. The first eye is covered for approximately 1-2 seconds. As this eye is covered, the uncovered eye is observed for any shift in fixation. The same is done next with the other eye. In this way, strabismus can be discovered by looking for shifts in fixation of the eyes. 253) (B) Tonometry would be most useful for testing for glaucoma. Since glaucoma is an eye condition characterized by increased intraocular pressure, tonometry is useful for measuring the intraocular pressure to determine if a person has glaucoma. 254) (B) The macula are most responsible for central vision. This is why in macular degeneration, there is loss of central vision. 255) (A) The cones of the eye are most responsible for color vision, particularly of bright colors. The rods function best with in dim light. 256) (C) The rods of the eye function best for night vision and for conditions of low light. The cones of the eye function best in bright color vision. 257) (C) The fluorescein eye stain is used to check for corneal abrasions. The fluorescein eye stain uses an orange dye (fluorescein) to stain the eye and then a blue light to detect for either abrasions or foreign bodies in the eye. How the test is performed is that a piece of blotting paper containing fluorescein dye is touched to the surface of the eye. The person is then asked to blink. Blinking spreads the dye throughout the eye. The practitioner then shines a blue light into the eye. Any problems on the surface of the cornea will be stained by the dye and appear green under the blue light. A normal result would be that the dye remains in the tear film on the surface of the eye and does not stick to the eye itself (source: medlineplus.gov). 258) (A) Normally the pupil constricts in the presence of bright light and dilates in dim light or darkness. 259) (A) Normally the pupils constrict when focusing on a nearby object and dilates when focusing on an object far away. 260) (A) The cornea is the outermost layer of the eye. 261) (B) The fovea is the part of the eye that is responsible for sharp central vision such as that of 20/20 vision. Also, the fovea is the part of the eye that has the greatest concentration of cones; therefore, it is the location of the greatest color perception in the eye. 262) (B) Adie’s pupil is a neurological disorder affecting the pupil of the eye. In most cases, the affected pupil is larger than normal (dilated) and is slow to react in response to direct light. Adie’s pupil may be the result of a post viral infection. The term Adie syndrome is used when both abnormalities of the pupil and loss of deep tendon reflexes are present. 263) (D) Argyll Robertson pupils are pupils that are small and constrict poorly to direct light and briskly to accommodation. 264) (A) Marcus Gunn pupil is a medical sign whereupon the patient’s pupil constricts less than normal when a bright line is shone upon it. 265) (C) Anisocoria refers to a condition in which the pupils of the eyes are of unequal size. As a rule, whenever you see the prefix aniso-, know that it means unequal. Aniso comes from the Greek word, anisos, meaning unequal, from an-, not, + isos, equal. The opposite of aniso- is iso-. The eyes of a person with anisocoria are both reactive to light and accommodation. If the difference is less than 1mm, it may be a normal variant. Greater than that would be indicative of anisocoria. 266) (C) Dysconjugate gaze is the failure of the eyes to turn together in the same direction. Dysconjugate gaze can be tested by a practitioner asking a patient to follow his or her finger horizontally. Failure of both eyes to follow the finger indicates dysconjugate gaze. Marcus Gunn pupil would be tested with either a pen light or some type of shining light. It is a medical sign whereupon the patient’s pupil constricts less than normal when a bright line is shone on it. Argyll Robertson pupils would be checked for through a test checking for a person’s response to accommodation (bringing an object near a patient) and whether the persons’s eyes constrict in the presence of bright light. With Argyll Robertson pupils, the pupils constrict due to accommodation (object brought close) but do not constrict when a bright light is shone on it. 267) (B) The elliptical space between the open eyelids is referred to as the palpebral fissure. In normal, healthy adults, this measures about 10mm vertically and 30mm horizontally. Image: Palpebral fissure 268) (B) Ptosis causes a decreased palpebral fissure in the affected eye. Nystagmus causes involuntary, uncontrolled, rapid, repetitive movement of the eyes; it doesn’t affect the eyelids, so it doesn’t affect the palpebral fissure. Marcus Gunn pupil and Adie’s pupil only affects the pupils, not the eyelids, so it doesn’t affect the palpebral fissure. 269) (A) Nystagmus is an eye condition characterized by involuntary, rapid, oscillating eye movements. 270) (C) Ocular rosacea is inflammation that causes redness, burning, and itching of the eyes. It often develops in people who have rosacea, a chronic skin condition that affects the face. Sometimes ocular rosacea can be the first sign that a person may later develop the facial type. Symptoms may include dry eyes, burning or stinging in the eyes, itchy eyes, grittiness or feeling of having a foreign body in the eye(s), blurred vision, photophobia, redness, swollenness, and tearing. Ocular rosacea primarily affects adults between the ages of 30 and 50. Treatment is available but it does not cure ocular rosacea. 271) (B) The corneal light reflex test (also called the Hirschberg test) is a test done to check for ocular alignment. It checks to see if there is an uneven gaze in the patient’s eyes (strabismus). It can be used to check for esotropia, exotropia, hypertropia, and hypotropia. It is performed by shining a light in the person's eyes and observing where the light reflects off the corneas. When doing the test, the light reflexes of both eyes are compared, and will be symmetrical in an individual with normal fixation. In an abnormal result, based on where the light lands on the corneas, the examiner can detect if there is an esotropia, exotropia, hypertropia, or hypotropia. 272) (D) Supernumerary nipples is a benign condition in which a person has more than the 2 usual nipples on his or her chest. Image: Supernumerary nipples Credit: Photograph by Zureks, licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license 273) (C) Sarcopenia is the loss of muscle tissue as a natural part of the aging process. 274) (B) Cachexia is a condition characterized by ill health, marked weight loss, and muscle loss. 275) (B) Cachexia is also referred to as wasting syndrome. 276) (C) Cachexia is found in about 80% of people with advanced cancer. People with advanced cancer tend to lose their appetite, which then causes marked weight loss, muscle loss, and ill health. 277) (B) Ceruminosis is excessive accumulation of cerumen. 278) (B) Orbital cellulitis is inflammation of the eye posterior to (behind) the orbital septum. Periorbital cellulitis refers to inflammation of the eye anterior to (in front of) the orbital septum. 279) (D) A sinus infection is the most common cause of orbital cellulitis. 280) (C) Symptoms of orbital cellulitis include painful swelling of the upper and lower eyelids (and also possibly the eyebrow and cheek), a bulging eye, decreased vision, eye pain (especially when moving the eye), fever (generally 102°F or higher), general malaise, painful or difficult eye movements, and a shiny, discolored eyelid (red or purple). The vision is affected; orbital cellulitis will result in decreased vision. 281) (A) Possible complications of orbital cellulitis include cavernous sinus thrombosis, hearing loss, septicemia, meningitis, and optic nerve damage and loss of vision. This is why orbital cellulitis is considered an ophthalmic emergency which needs to be treated right away. 282) (A) Orbital cellulitis is most commonly caused by a bacterial infection. Staphylococcus aureus, streptococcus pneumonia and beta-hemolytic streptococcus are the 3 types of bacteria that are responsible for most cases of orbital cellulitis. Therefore, orbital cellulitis is usually treated with antibiotics. If a severe abscess forms that can threaten the vision or neurological status of a person, surgical intervention may be necessary. Surgical intervention requires drainage of the sinuses. 283) (C) Orbital cellulitis causes a loss in vision, while periorbital cellulitis doesn’t cause decreased vision. Orbital cellulitis is a more severe form of cellulitis of the eye. Unlike periorbital cellulitis, which is more superficial, orbital cellulitis occurs in the posterior of the orbital septum (periorbital cellulitis takes place in the anterior of the orbital septum). Orbital cellulitis is considered an ophthalmic emergency, unlike periorbital cellulitis. Periorbital cellulitis does not produce bulging of the eye, limited eye movement, or pain on eye movement. If these signs are seen, then the cellulitis is most likely orbital cellulitis. 284) (A) Atopic dermatitis is a skin condition that is characterized by dry, itchy rashes. Unlike psoriasis, it is generally not covered with scales. Image: Atopic dermatitis 285) (B) Atopic dermatitis is also called eczema. 286) (C) Common triggers that may exacerbate atopic dermatitis include allergens, such as dust mites or animal dander, harsh soaps and detergents, weather changes, stress, allergic reactions, and skin infections. Pork is not a common allergen that triggers atopic dermatitis. 287) (D) Common areas of atopic dermatitis include the cheeks, the entire trunk of the body, the elbows, and the knees. It may also appear on the neck, wrists and ankles. Although the rash may commonly appear in the crease between the buttocks, the buttocks itself is not an area that is commonly affected. 288) (D) Atopic dermatitis is a chronic disorder that may or may not be a lifelong disease. Sometimes atopic dermatitis may completely go away. Other times it remains. There is no way of knowing yet in the medical community whether atopic dermatitis will go away or be a lifelong disease. This makes managing the disease and stopping the atopic dermatitis from getting worse a priority. Atopic dermatitis is a very common skin disorder, with millions of new cases a year in the United States. Most people who get atopic dermatitis do so before the age of 5 (over 90%). It is rare for atopic dermatitis to start in adulthood. 289) (A) Ptosis is a drooping of the upper eyelid(s). 290) (D) A fishtail uvula is a uvula that is split, either partially or completely, into 2 sections. A fishtail uvula is a benign condition. Newborns with a cleft palate are at higher risk of having a split uvula. Image: Fishtail uvula 291) (A) Optic neuropathy refers to damage to the optic nerve. The main symptom of optic neuropathy is a loss of vision, with poor color vision in the affected eye. The condition is common in people who have multiple sclerosis (MS). With optic neuropathy, the pupil always appears abnormal (afferent pupillary defect). This means that the pupil constricts less in the presence of bright light. Depending on the severity of optic neuropathy, the optic nerve may appear normal or swollen. 292) (B) The most common cause of optic neuropathy is insufficient blood flow to the optic nerve referred to as ischemic optic neuropathy. Inflammation of the optic nerve (termed optic neuritis), compression on the optic nerve such as by lesions (termed compressive optic neuropathy), infiltration of the optic nerve such as by infections (termed infiltrative optic neuropathy), and trauma to the optic nerve (termed traumatic optic neuropathy) each account for less cases of optic neuropathy than ischemic optic neuropathy. 293) (C) The optic nerve is a bundle of nerve fibers that carry images from the retina to the brain. Each fiber carries a part of the visual information to the brain, including aspects such as color, side vision, etc. If these nerve fibers get damaged, which they do in optic atrophy, the brain doesn’t receive all of this information. This can cause a host of vision changes including blurred vision, abnormal side vision, and abnormal color vision. Depending on the damage, effects can range from minor vision changes to severe vision loss. Many conditions can lead to optic atrophy or damage to the optic nerve. It can be due to inflammation of the optic nerve (called optic neuritis), glaucoma (due to high intraocular pressure), improper development of the optic nerve, tumors, and other possibilities. Damage to the optic nerve is irreversible. Once the nerve fibers in the optic nerve are damaged or destroyed, they do not heal or grow back. This is why early diagnosis and treatment is important. 294) (C) The cause of roseola (also called roseola infantum) is primary infection with human herpesvirus 6. Roseola can also be caused by human herpesvirus 7. 295) (B) Roseola is also called sixth disease. It is also referred to as exanthem subitum and roseola infantum. 296) (C) The classic presentation of roseola is an infant or young toddler who acutely develops a high fever and often a febrile seizure. The fever often spikes higher than 103°F or 39.5°C; this fast-rising fever causes febrile seizures in about 10-15% of children. After 3 days, the fever rapidly goes down and a rash develops. The rash is normally a pinkish-reddish color and can be flat or raised. The rash usually spreads to many areas of the body, including the neck, face, arms, and legs. Image: Roseola 297) (B) Erythema infectiosum is a viral illness caused by parvovirus B19 that is characterized by a red rash. This disease is also called fifth disease because it was fifth in a list of historical classifications of common skin rash illnesses in children. It is more common in children than adults. A person usually gets sick with erythema infectiosum within 4 to 14 days after getting infected with the parvovirus B19. The first symptoms of erythema infectiosum are usually mild and may include fever, runny nose, and a headache. Then a person may get a rash on the face and body. The red rash that appears on the face is called a “slapped cheek” rash. This rash is the most recognized feature of erythema infectiosum. Some people may get a second rash a few days later on their chest, back, buttocks, arms, or legs. Image: Erythema infectiosum Credit: Photograph by Sandyjameslord, distributed under the Creative Commons AttributionShare Alike 4.0 International license 298) (D) Lymphogranuloma venereum is a type of STD caused by either 1 of 3 types of Chlamydia trachomatis bacteria. 299) (C) Lymphogranuloma venereum (LGV) is an STD (spread through sexual transmission). It is caused by any of 3 different types of the Chlamydia trachomatis bacteria. LGV is more common in Central and South America than in North America. LGV is more common in men than in women. Symptoms of LGV can begin a few days to a month after coming in contact with the bacteria. Symptoms include drainage from the skin through the lymph nodes in the groin, painful bowel movements, blood or pus from the rectum, small painless sores on the genital area, swelling and redness of the skin in the groin area, swelling of the labia (in women), and swollen groin lymph nodes on one or both sides. Image: Lymphogranuloma venereum 300) (D) The main risk factor for contracting lymphogranuloma venereum is being HIV positive. 301) (A) Koplik spots are seen with measles. 302) (C) Koplik spots would most likely be found in the mouth, on the inside of the cheeks early in the course of measles. 303) (A) Koplik spots are white in color. Image: Koplik spots 304) (D) A corneal ulcer is an open sore on the cornea. People at risk for corneal ulcers include contact lens wearers, people who have or have had cold sores, chicken pox, or shingles, people who use steroid eyedrops, people with dry eye, people with eyelid disorders that prevent proper functioning of the eyelid, and people who suffer injury or burns to the cornea. If a person wears contact lenses, safe handling, storage and cleaning of the lenses are key steps to reduce the risk of a corneal ulcer. To diagnose a corneal ulcer, the ophthalmologist will use a special dye called fluorescein dye to illuminate any damage to the cornea and then examine the cornea using a special microscope called a slit lamp. The slit-lamp exam will allow the ophthalmologist to see the damage to the cornea and determine if it is a corneal ulcer. If the ophthalmologist suspects that an infection is responsible for the corneal ulcer, a tiny tissue sample may be taken so that the infection can be identified and properly treated. Antibiotics, antifungal or antiviral eyedrops are the mainstay of treatment for corneal ulcers. Sometimes antifungal tablets will be prescribed. In other cases, an injection of medication is given near the eye for treatment. Oral pain medication may be prescribed to reduce pain. If corneal ulcers cannot be treated with medication, surgery may be needed to keep a person’s vision. A corneal transplant can replace the damaged cornea with a healthy donor cornea to restore vision (source: aao.org). Image: Corneal ulcer 305) (B) Common symptoms of a corneal ulcer include eye redness, eye pain, excessive tearing, sensation of a foreign body in the eye, and worsening or blurry vision. 306) (C) Most cases of a corneal ulcer are due to a bacterial infection that invades the cornea, often following eye injury, trauma, or damage. 307) (B) Ehrlichiosis is a bacterial infection that is transmitted through the bite of a tick (called the Lone Star tick) transmitted in the southeastern and south-central United States. Ehrlichiosis usually causes flu-like symptoms including fever, headache, fatigue, and muscle aches. Usually, these symptoms occur within 1-2 weeks following the tick bite. The tick bite is usually painless, and about half of the people who develop ehrlichiosis may not even remember being bitten by a tick. Most cases of ehrlichiosis occur in the spring and summer months when populations of the Lone Star tick are at their peak, and people are outside more often (source: cdc.gov). 308) (A) Tetracycline antibiotics are highly effective against ehrlichiosis. Doxycycline is the first-line treatment for adults and children of all ages and should be initiated immediately whenever ehrlichiosis is suspected. 309) (B) Folliculitis is inflammation of the hair follicles. Basically, folliculitis is infected hair follicles. 310) (D) Folliculitis can take place on any hair follicles in the body. Image: Folliculitis 311) (B) Usually, the cause of folliculitis is a bacterial or fungal infection. Bacterial infections are more common, with staphylococcus aureus being the most common organism causing the infection. 312) (A) Trimming the hair with scissors is unlikely to cause folliculitis because usually the hair is clipped off and the follicle itself is left undamaged. Shaving is much more likely to cause folliculitis because the razor is placed directly against the skin and it is more likely to irritate the hair follicle. Other risk factors include wearing tight clothes (since it can cause the fabric to rub across the follicle, irritating it), using or working with substances that can irritate or block hair follicles (such as makeup, cocoa butter, motor oil, etc.), having a cut, scrape, or wound (if bacteria or fungi get in, it can spread to nearby hair follicles), use of a hot tub, whirlpool, or swimming pool not properly treated with chlorine, having a disease such as diabetes or HIV (lowers the body’s ability to fight infection), having hyperhidrosis (excessive sweating), and having certain skin conditions such as dermatitis and acne. 313) (A) Folliculitis usually manifests as red pustules (pus-filled lesions) with a hair in the center of each one. Folliculitis is infected hair follicles. So, each of the follicles affected appears red and raised with the usual hair sprouting from it in the center. 314) (D) Fire ant stings are characterized by groups of swollen red spots on the skin that have a blister on top of each red spot. Fire ants attack in swarms and are aggressive. Each fire ant can sting several times. This is why usually there are groups of red spots on the skin, as opposed to 1 or 2. They usually attack when their nest (their residence) is disturbed; this is when they are most aggressive. Image: Fire ant Image: Fire Ant Stings 315) (D) Fire ants are mostly found in the Southern states of the United States. Imported fire ants originally came from South America. In the United Sates, fire ants currently inhabit all or parts of Alabama, Arkansas, California, Florida, Georgia, Louisiana, Mississippi, New Mexico, North Carolina, Oklahoma, South Carolina, Tennessee, and Texas. They are even found in Virginia and are discovered sporadically in Kentucky, Missouri and Maryland. However, they’re a greater threat in Southern states. 316) (A) Wearing DEET-containing insect repellant does not repel fire ants. Fire ants are not deterred from stinging by a wide variety of insect repellents and chemical substances. If fire ants are disturbed by their nests being disturbed, chemical repellants do not matter. The best protection against fire ants is to stay away from fire ant nests. Look around for mounds and avoid stepping on them. Wear socks and shoes when outside and gloves when gardening to avoid giving the fire ants direct access to your skin. 317) (C) Malaria is spread to humans through mosquito bites. Rocky Mountain Spotted Fever, ehrlichiosis, and Lyme disease are all spread through tick bites. 318) (A) Keratoacanthoma is a benign tumor despite its similarities to squamous cell carcinoma. For this reason, keratoacanthoma is termed a pseudocancer, occurring as an isolated nodule and mimicking squamous cell carcinoma. Keratoacanthoma (KA) originates in the skin’s hair follicles and rarely spreads to other cells. KA is commonly found on sun-exposed areas of the skin such as the face, neck, hands, arms, and legs. Though the exact cause of KA is unknown, ultraviolet rays from the sun or elsewhere is one of the contributing factors to KA. Other contributing factors include chemical carcinogens, smoking, infection with some strains of a wart virus such as HPV, trauma, and genetic factors. 319) (B) Keratoacanthoma most closely resembles squamous cell carcinoma (SCC) in appearance. Since it strongly resembles SCC, a practitioner may do a biopsy to differentiate the two. Like SCC, it resembles a dome or crater. Image: Keratoacanthoma 320) (D) Just like with all the major skin cancers, the risk factors for keratoacanthoma are similar. Older age, prolonged sun exposure, fair skin, immunocompromised status, and the frequent use of tanning beds are risk factors. 321) (B) Verruca vulgaris (also called a common wart) is a raised wart with a roughened surface. It is most common on the hands but can grow anywhere on the body. Image: Verruca vulgaris 322) (D) Verruca vulgaris is a benign condition that is caused by one of many types of human papillomavirus. It is especially common among children and adolescents. Though it most frequently occurs on the hands, it can occur anywhere on the body. 323) (A) Diastasis recti is also known as abdominal separation. Diastasis recti is commonly defined as a separation of roughly 2.7 cm or greater of the 2 sides of the rectus abdominis muscle. 324) (D) Diastasis recti is not associated with morbidity or mortality. 325) (D) Diastasis recti is a common condition that is most commonly seen in 2 populations, newborns and pregnant women. It is known to occur in men, but not frequently. It is seen more in premature and black newborns. Diastasis recti in infants usually resolves with age; in certain circumstances, surgery may be indicated. 326) (C) Cotton wall spots can be seen in either diabetic retinopathy or hypertensive retinopathy. Image: Cotton wool spots 327) (A) Anterior uveitis is the most common type of uveitis. The type of uveitis a person has is classified by where the inflammation occurs in the uvea. Anterior uveitis is inflammation of the iris (iritis) or inflammation of the iris and ciliary body. Intermediate uveitis is inflammation of the ciliary body. Posterior uveitis is inflammation of the choroid. Diffuse uveitis (also called panuveitis) is inflammation of all areas of the uvea. 328) (B) The uvea is the middle layer of the eye that consists of the iris, ciliary body, and choroid. 329) (D) Punch biopsies are considered the primary technique for obtaining diagnostic fullthickness skin specimens. The technique involves using a circular blade that is rotated down through the epidermis and dermis and into the subcutaneous tissue, yielding a 3- to 4-mm cylindrical core of tissue sample. Punch biopsies are useful for diagnostic tests for various skin disorders. With local anesthesia used, this procedure is generally painless. 330) (B) The West Nile Virus is transmitted to humans most commonly through mosquitoes. In rare instances, it can be spread through blood transfusions, organ transplants, exposure in a laboratory setting, and from mother to baby during pregnancy, delivery, or breastfeeding (source: cdc.gov). 331) (D) West Nile Virus is a viral illness spread most commonly to humans through mosquitoes. Most people (70-80%) who become infected with West Nile virus do not develop any symptoms. About 20% of people infected will develop flu-like symptoms such as a fever, headache, body aches, joint pain, vomiting, diarrhea, or rash. Most people with the West Nile virus disease recover completely, but fatigue and weakness can last for weeks or months. Less than 1% of people who are infected will develop a serious neurologic illness such as encephalitis or meningitis. About 10% of these cases will be fatal. There is no vaccine or specific antiviral treatments for West Nile virus (as of 2017). 332) (B) Most people get infected with the West Nile virus in the summer months. The most common times of infection is from June through September. 333) (C) West Nile virus has been reported in all 48 lower states. The only states that have not had reported cases of West Nile virus are Alaska and Hawaii. Outbreaks have been occurring every summer since 1999. The risk of infection is highest for people who work outside or who participate in outdoor activities due to increased exposure to mosquitoes. 334) (B) Skin tags (the medical name being acrochordons) are benign growths on the skin that are generally painless. Skin tags are generally acquired (not present at birth) and can occur in any age group; however, they arise most often in adulthood and are most common in middle age. Skin tags are more common in overweight individuals. They are seen with greater frequency in pregnancy, as hormone elevations likely play a role in their prevalence. Image: Skin tags 335) (C) A hyphema is a collection of blood in the anterior chamber of the eye. Image: Hyphema 336) (C) Usually, trauma is the cause of hyphemas. This is termed traumatic hyphemas. It is usually the result of a projectile (such as a soccer ball, rock, air gun pellet, BB gun pellet, hockey puck, or paintball) or a deliberate punch striking the exposed portion of the eye despite the protection of the bony orbital rim. Due to the aggressive nature of hyphemas, males account for about 75% of all cases. 337) (B) With a hyphema, blood collects between the cornea and the iris. Blood from a hyphema can cover part or all of the iris and pupil. Depending on the level, there can be a partial or total vision blockage in the affected eye. Hyphemas are generally painful. 338) (C) A subconjunctival hemorrhage occurs when a tiny blood vessel(s) breaks just underneath the conjunctiva (the clear surface of the eye). The conjunctiva can’t absorb blood quickly, so the blood gets trapped. A subconjunctival hemorrhage can occur without any obvious trauma to the eye. Because the arterioles are so small and delicate, even something minor such as coughing can cause a blood vessel to break in the eye. A person may be totally unaware of having a subconjunctival hemorrhage until visually examining the eye. On examining the eye, the person will see a bright red patch of blood on the white (sclera) of the eye. Image: Subconjunctival hemorrhage 339) (C) A subconjunctival hemorrhage is unlikely to produce any symptoms. If a symptom is experienced, it is usually a scratchy feeling on the eye due to the blood leakage. A subconjunctival hemorrhage is unlikely to produce eye pain, eye discharge, or any change in vision. 340) (B) A virchow’s node (also called a signal node or sentinel node) is a lymph node in the left supraclavicular fossa (which is the area above the left clavicle). 341) (C) The virchow’s node gets its blood supply from the abdominal cavity. 342) (D) Trosier’s sign is the finding of an enlarged, hard node on the left side of the neck due to an enlarged lymph node in the left supraclavicular fossa (enlargement of virchow’s node). Trosier’s sign has been regarded as strongly indicative of the presence of cancer in the abdomen, specifically gastric cancer that has spread through the lymph vessels. This is because virchow’s node is supplied blood through vessels from the abdomen. If there is an enlargement of virchow’s node, this likely is caused by a cancer in the abdomen. Image: Trosier’s sign 343) (C) Von Recklinghausen’s disease is a genetic disorder that is characterized by the growth of tumors on nerves (called neurofibromas). The tumors are usually benign; in rare instances, the tumors can become cancerous. The disease can also affect the skin. On the skin, it may cause light brown spots called café-au-lait spots. Von Recklinghausen’s disease can also cause bone deformities (source: healthline.com). 344) (B) Dysconjugate gaze is often linked to thiamine (B1) deficiency. It is common in alcoholics, because alcohol leeches the body of thiamine. 345) (D) Urticaria, also called hives, is a vascular reaction of the skin marked by the transient appearance of erythematous papules that are often accompanied by severe pruritus. Urticaria can occur anywhere on the body. Urticaria is usually an allergic reaction to a food, medication, insect bite or other substance. Most cases are self-limiting and are of short duration. In rare cases, the eruptions can last for several days and can happen recurrently over weeks. Chronic urticaria is defined as urticaria with recurrent episodes over a period lasting longer than 6 weeks. Image: Urticaria 346) (A) Though most cases of diaper dermatitis include infants, it is not limited to infants but to anyone who uses diapers or incontinence diapers/pads, which is frequently found in the elderly population. Diaper dermatitis is confined to the area of the diaper (or padding). Increased wetness in the diaper area makes the skin more susceptible to breakdown. This can be wetness from any source but the most common is from urine or stool. Candida albicans is another possible cause of diaper dermatitis. It is the most common microbial infecting agent of diaper dermatitis. The peak incidence of diaper dermatitis is 9-12 months of age in infants. It is a very common condition. Treatment consists of frequent diaper changes, performing skin care and keeping the diaper area dry, using barrier cream/ointment with each diaper change, and using antifungals if diaper dermatitis is due to Candida infection. Image: Diaper dermatitis 347) (C) Hyperhidrosis is a common disorder in which there is excessive sweating. An estimated 2-3% of Americans suffer from this condition. It affects men and women about equally. There are 2 types of hyperhidrosis: generalized or localized. With generalized hyperhidrosis, excessive sweating can be present in multiple areas (usually the axillary, palmar, and soles of the feet). Localized hyperhidrosis typically has excessive sweating in one part of the body. Of the localized hyperhidrosis, the 2 most common types are excessive sweating of the underarms (called axillary hyperhidrosis) and of the palms of the hands and soles of the feet (called palmoplantar hyperhidrosis). Both localized forms of hyperhidrosis tend to begin in adolescence. Generalized hyperhidrosis tends to start in adulthood. Hyperhidrosis is a chronic condition that can be difficult to treat. The sweating associated with hyperhidrosis is unpredictable, which can be a source of embarrassment in social situations for a person suffering from the condition. 348) (D) All races can be affected by hyperhidrosis; however, the Japanese are reportedly affected more than 20 times more frequently than other ethnic groups. 349) (D) Hyperhidrosis is most associated with a decreased quality of life. The frequent excessive sweating can cause embarrassment and anxiety in social situations. In fact, for this reason, hyperhidrosis is sometimes labelled the “silent handicap”. Hyperhidrosis is not associated with mortality, heart problems, or dehydration. 350) (D) Rhinophyma is a large, red-colored, bulby nose that is considered to be a symptom of severe rosacea. The cause of a rhinophyma is unknown. It occurs more frequently in men than women. Image: Rhinophyma 351) (B) Tinea cruris is referred to as “jock’s itch”. It is also referred to as “ringworm of the groin”. 352) (B) Epidermoid cysts are benign (noncancerous) small bumps beneath the skin. Epidermoid cysts can appear on any part of the body, but are most common on the face, neck and trunk. They are slow growing and are often painless. In most cases, epidermoid cysts cause no long-term problems. Image: Epidermoid cyst 353) (D) Conjunctivitis is also known as pinkeye. 354) (A) Tinea cruris is a fungal infection of the groin and its adjacent skin. Image: Tinea cruris 355) (B) Ringworm is a common skin infection that is caused by a fungus. It’s called ringworm because it can cause a circular rash (which is shaped like a ring). The rash is usually red and itchy. Ringworm goes by many names. The medical terms used for ringworm are “tinea” or “dermatophytosis”. 356) (B) Tinea cruris is often seen concomitantly with tinea pedis. 357) (B) Tinea cruris is a fungal infection of the groin and adjacent skin. The rash associated with tinea cruris is usually scaly, raised and red; it can be very pruritic in nature. It is most often seen in adult men. Tinea cruris often comes from a fungal infection of the feet (tinea pedis) or a fungal infection of the nails (onychomycosis), spread by scratching or the use of an infected towel. 358) (A) Lichen sclerosus is also known as white spot disease; this is because of the white patches that appear on the skin. Image: Lichen sclerosus 359) (B) Lichen sclerosus is an uncommon condition that creates patchy, white skin that’s thinner than normal. This can cause easy bruising or tearing of the skin. Though lichen sclerosus can occur anywhere on the body, it is most common in the genital and anal areas. It is a chronic (long-term) condition that can be managed but not cured. 360) (C) Though anyone can get lichen sclerosus, postmenopausal women have the highest risk of obtaining it (source: mayoclinic.org). 361) (D) The exact cause of lichen sclerosus is unknown. An overactive immune system and hormonal imbalances are believed to play a role. Lichen sclerosus isn’t contagious and cannot be spread through sexual intercourse; lichen sclerosus is not an STD. In women, lichen sclerosus usually involves the vulva. In boys and men, uncircumcised males are most at risk, because the condition generally affects the foreskin (source: mayoclinic.org). 362) (C) Corticosteroid ointments or creams are commonly prescribed for lichen sclerosus. Generally, these creams are applied daily initially. After several weeks, the practitioner will likely recommend that these creams only be used twice a week (source: mayoclinic.org). 363) (B) Allergic rhinitis is also called hay fever. 364) (B) Bacterial conjunctivitis is usually distinguished from viral conjunctivitis due to the purulent exudate that it produces. Viral conjunctivitis is much less likely to produce purulent exudate. Both bacterial and viral conjunctivitis are highly contagious and can be spread through direct contact or respiratory droplets. In adults, viral conjunctivitis is the most common type of conjunctivitis, while bacterial conjunctivitis may have a higher incidence in children. 365) (D) Moraxella Catarrhalis would be least likely to cause bacterial conjunctivitis. The most common types of bacteria that causes bacterial conjunctivitis include Staphylococcus aureus, Haemophilus influenza, Streptococcus pneumoniae, and Moraxella catarrhalis. 366) (B) Chronic bacterial conjunctivitis often develops along with blepharitis, an inflammation of the eyelids. The chronic bacterial conjunctivitis promotes bacterial growth on the eyelid. 367) (C) Hyperacute bacterial conjunctivitis is a severe form of bacterial conjunctivitis that occurs suddenly and develops rapidly. It is accompanied by a large amount of yellow-green discharge that returns even after being wiped away from the eye(s). It is most often caused by Neisseria gonorrhea in sexually active adults. The infection can lead to vision loss if not treated promptly. 368) (D) Chlamydial conjunctivitis (also known as inclusion conjunctivitis) is more common in newborns. It includes redness of the eye(s), swelling of the eyelids, and discharge of pus, usually 5 to 12 days after birth. 369) (A) Viral conjunctivitis can be caused by several types of viruses, with adenoviruses being the most common cause. Other viruses that can cause viral conjunctivitis include rubella virus, rubeola (measles) virus, Herpesviruses, varicella-zoster virus (which also causes chickenpox and shingles), Epstein-Barr virus (which also causes infectious mononucleosis), and picornaviruses (which includes coxsackievirus A24 and enterovirus 70). 370) (A) A history of multiple sex partners is the most relevant and frequent cause of chlamydial conjunctivitis in adults. Usually, with cases, patients have acquired a new sex partner in the preceding 2 months. Even though chlamydial conjunctivitis can be caused by swimming pool use and it is sometimes referred to as swimming pool conjunctivitis, it is uncommon; rarely is adult chlamydial conjunctivitis acquired from contaminated swimming pool water. 371) (B) Bacterial conjunctivitis is not a condition caused or triggered by allergies. Asthma, eczema, and allergic conjunctivitis are all caused or triggered by allergic reactions. 372) (B) A subconjunctival hemorrhage is a mostly benign eye condition; it does not lead to blindness. Glaucoma, corneal ulceration, and macular degeneration can all progress to blindness, especially if not treated appropriately. Corneal ulceration (also called peripheral ulcerative keratitis) can quickly produce progressive necrosis of the corneal stroma, leading to perforation and blindness. 373) (B) The most common causes of epistaxis are dryness (often caused by indoor heat in the winter) and nose picking. The two often work together because nose picking occurs more often when the mucus in the nose is dry and crusty. Risk factors for epistaxis include hypertension and the use of anticoagulants. Epistaxis is divided into 2 categories: anterior epistaxis (epistaxis that bleeds down the nares) and posterior epistaxis (epistaxis that bleeds down the throat). Epistaxis is usually benign, self-limiting and spontaneous. It has peaks of incidence at age 2-10 and 50-80 years. Both sexes are equally affected. Children with migraines have a higher incidence of recurrent epistaxis than children without migraines. 374) (C) Measures that should be taken during a nosebleed is the patient should sit in the upright position, leaning forward, as to not aspirate blood. The patient should pinch the nares together for 10 to 15 minutes to stop the bleeding. An ice pack can be applied to the nose and cheeks; the cold will constrict the blood vessels and help stop the bleeding. If the bleeding is uncontrolled or if the patient’s status is questionable, the patient should be referred to the ED. 375) (A) Hot showers aren’t linked to epistaxis; in fact, showers, because of the moist air, can be used as a form of relief. Avoiding forceful nose blowing, using a humidifier (to keep the nares moist), and using a water-based lubricant in the nares (if an environment is dry) are all prevention methods for epistaxis. 376) (C) Pharyngitis is often referred to as “sore throat”. Pharyngitis can be viral or bacterial; however, most cases are viral. A sore throat is the chief symptom of pharyngitis. Other symptoms include a dry, scratchy throat and difficulty swallowing. Also, there may be sneezing, a runny nose, headache, cough, fatigue, body aches, chills, and fever. 377) (A) The most common causative viral agents of pharyngitis include viruses of the common cold, influenza, and mononucleosis. 378) (A) Less common than viral pharyngitis is bacterial pharyngitis. The most common bacterial infection of the throat is strep throat, which is caused by Group A streptococcus bacteria (it’s called strep throat because it’s caused by Group A strep bacteria). Rare causes of bacterial pharyngitis include gonorrhea, chlamydia, and Corynebacterium. 379) (C) A rapid strep test is an easy test that can be done by most practitioners in an office that will tell within a few minutes if the person is positive for strep bacteria. If positive, this is indicative of bacterial pharyngitis. If not, this is indicative of viral pharyngitis. 380) (B) Penicillin is the most commonly prescribed antibiotic for bacterial pharyngitis, which is most often strep throat caused by group A strep bacteria. Just like with all conditions caused by group A strep bacteria, such as rheumatic fever and scarlet fever, penicillin is normally prescribed. 381) (B) Scleritis is a painful inflammation of the sclera (the white part of the eye, composed of tough fibrous tissues and that forms a protective layer of the eye). Scleritis is characterized by severe pain and tenderness in the eye. Scleritis can affect vision; it can cause blurred vision, tearing, and extreme sensitivity to light. In some cases, partial or complete loss of vision is possible. The 2 main types of scleritis are anterior scleritis (affecting the front portion of the sclera) and posterior scleritis (affecting the back portion of the sclera). In almost half the cases, scleritis is associated with an underlying autoimmune disorder such as rheumatoid arthritis. 382) (C) Black dots present on the scalp (the black dot sign) is indicative of tinea capitis. Tinea capitis is a fungal infection that involves the scalp. It may involve only parts of the scalp or the entire scalp. Areas that are infected appear bald with small black dots, due to the hair that has broken off. Image: Tinea capitis 383) (B) Erysipelas is seldom a life-threatening illness because it’s an infection that is restricted to the upper dermis and superficial layers of the skin; therefore, it’s doesn’t present a high risk for septicemia. 384) (C) Tinea infections such as tinea pedis (athlete’s foot) thrives the best in warm, moist environments, because fungi grow best in warm, moist environments. This is why it’s encouraged to keep the skin as dry as possible to prevent tinea infections. 385) (C) Tinea pedis affects all ages but is more common in adults than in children. Walking bare foot on a communal floor or sharing a towel can result in infection. The fungal spores found on bathroom floors or locker rooms can persist for months or years. Tinea pedis can affect one or both feet. It causes peeling skin between the toes on the foot. Image: Tinea pedis 386) (A) Tinea pedis (athlete’s foot) is found most often in young adult men. 387) (A) Tinea infections are caused by tiny fungi known as dermatophytes. 388) (C) All tinea infections are fungal infections. They are caused by dermatophytes. Tinea versicolor, tinea cruris, tinea capitis, tinea corporis, tinea pedis, etc. are all fungal infections. 389) (C) The diagnostic test for all tinea infections is the KOH (potassium hydroxide) slide. KOH microscopy is the easiest and most cost-effective method used to diagnose fungal infections of the hair, skin, and nails. KOH dissolves keratinocytes to allow easy viewing of hyphae, which is characteristic of fungi. A specimen is collected from the person and placed on a glass slide. A drop of KOH is added and the slide is heated gently with flame to adequately dissolve the keratin. The sample is then looked under microscopy to locate hyphae (source: aad.org). 390) (B) Tinea barbae is a fungal infection of the beard and moustache areas of the face with a dermatophyte fungus. It is less common than tinea capitis and generally affects only adult men. Tinea barbae most often affects farmers and is due to direct contact with an infected animal. It is rarely passed from one person to another (source: dermnetnz.org). Image: Tinea barbae 391) (A) A kerion is a complication of tinea capitis. A kerion appears on the scalp as an inflamed, thickened, pus-filled area, which is sometimes accompanied by a fever. Image: Kerion 392) (D) Acanthosis nigricans can be a sign of underlying diabetes. 393) (A) Amaurosis fugax is a temporary loss of vision in one or both eyes due to a lack of blood flow to the retina. It isn’t a disease but rather a symptom or sign of other disorders. 394) (D) When you think about amaurosis fugax, think of lack of blood flow to the retina— anything that can cause a lack of blood flow to the retina. This includes causes such as a blood clot in an artery in the eye. This blood clot usually travels from a larger artery, such as the carotid artery in the neck, to an artery in the eye. Plaque buildup also can restrict blood flow to the retina and cause temporary blindness. Other disorders that can cause amaurosis fugax include optic neuritis, migraine headaches, a brain tumor, a head injury, multiple sclerosis, temporal arteritis, and systemic lupus erythematosus. 395) (B) Amaurosis fugax is a condition in which a person experiences sudden vision loss in one or both eyes due to restricted blood flow to the retina. The loss of vision usually lasts for a few seconds to several minutes; it does not last for days. Afterward, vision returns to normal. Some people describe the loss of vision as a gray or black shade coming down over the eye. Because something, many times a blood clot in an artery, causes blockage, amaurosis fugax increases a person’s risk for having a stroke. 396) (A) Myringitis is a form of otitis media. 397) (B) Myringitis is inflammation of the tympanic membrane. The extremely thin and delicate tympanic membrane (TM) is the first component of the middle ear conductive system. The TM is easily traumatized, and diseases of the TM deprive patients of their ability to work and to enjoy life. Myringitis, or inflammation of the TM, may be accompanied by hearing impairment and a sensation of congestion and earache. A fever may be present. Bullous myringitis is myringitis that is composed of small fluid-filled blisters on the eardrum and can cause severe pain. Treatment includes antibiotics and pain medication (source: emedicine.medscape.com). 398) (D) Basal cell carcinoma is a cancerous skin condition. Seborrheic keratosis, cherry angiomas, and keratoacanthoma are all benign (noncancerous) skin conditions. 399) (A) A pressure ulcer that does not cause a break in the skin and does not blanch is classified as a stage 1 pressure ulcer. 400) (C) A pressure ulcer that extends into the subcutaneous tissue but does not reach the muscles or bones would be classified as a stage 3 pressure ulcer. 401) (B) Presbycusis is the loss of hearing that gradually occurs in most individuals as they grow older. Hearing loss is a common disorder associated with aging. About 30-35% of adults between the ages of 65 and 75 years have hearing loss. It is estimated that 40-50% of people 75 and older have hearing loss. Presbycusis is most often caused by sensorineural hearing loss. Sensorineural hearing loss is caused by disorders of the inner ear or auditory nerve. Presbycusis is most commonly caused by gradual changes in the inner ear. The cumulative effects of repeated exposure to daily traffic sounds or construction work, noisy offices, equipment that produces noise, and loud music can cause sensorineural hearing loss. Sensorineural hearing loss is most often due to a loss of hair cells (sensory receptors in the inner ear). This can occur as a result of hereditary factors as well as aging, various health conditions, and side effects of some medications (aspirin and certain antibiotics). The hearing loss associated with presbycusis is usually greater for high-pitched sounds. A person may hear low-pitched sounds normally but may not hear higher-pitched sounds as well. Although less common, presbycusis can also be caused by conductive hearing disorder, meaning the loss of sound sensitivity is caused by abnormalities of the outer ear and/or middle ear. Such abnormalities may include reduced function of the tympanic membrane (the eardrum) or reduced function of the three tiny bones in the middle ear that carry sound waves from the tympanic membrane to the inner ear. 402) (B) Though bone conduction equaling air conduction represents an abnormality, bone conduction being greater than air conduction would be suggestive of the greatest amount of hearing loss. In normal hearing, air conduction is greater than bone conduction. 403) (D) The herpes simplex virus, or herpes, is categorized into 2 types: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). HSV-1 is mainly transmitted by oral- to-oral contact to cause oral herpes (which can include symptoms known as “cold sores”), but can also cause genital herpes. Symptoms of herpes include painful blisters or ulcers at the site of infection. HSV-2 is a sexually transmitted infection that causes genital herpes. Herpes infections are most contagious when symptoms are present but can still be transmitted to others in the absence of symptoms. Infection with HSV-2 increases the risk of acquiring HIV infection. Both HSV-1 and HSV-2 infections are lifelong. Antiviral medications such as acyclovir, famciclovir, and valaciclovir are the most effective medications available for people infected with HSV. These can help to reduce the severity and frequency of symptoms, but cannot cure the infection (source: who.int). 404) (B) Ehlers-Danlos syndrome is a disorder of the connective tissue. With Ehlers-Danlos syndrome, the connective tissue throughout the body lacks collagen (collagen is said to form the glue of connective tissue). So, people with Ehlers-Danlos syndrome have extremely stretchy skin, often have dislocations due to the lack of collagen in the connective tissue of the joints, and have blood vessels that rupture easily, causing easy bruising. Since almost all of the body is made up of connective tissue, Ehlers-Danlos syndrome can affect practically every joint in the body as well as internal body organs. 405) (B) Thrombocytopenia is not a symptom associated with Ehlers-Danlos syndrome. Symptoms of Ehlers-Danlos syndrome include frequent dislocations, hypermobility of the joints, and skin that’s translucent, elastic, and bruises easily; this is why Ehlers-Danlos syndrome is also called elastic skin. The skin may also wrinkle and there is usually poor wound healing with this condition. 406) (C) A practitioner may suspect a person has Ehlers-Danlos syndrome if s/he is able to bend his/her fingers way beyond the normal range of motion. 407) (A) Ehlers-Danlos syndrome is an inherited disorder. It is defective genes passed from parent to child. This is the only way a person can get Ehlers-Danlos syndrome; it is not acquired through lifestyle or environment. There are many various types of Ehlers-Danlos syndrome. Depending on the type, it may be autosomal dominant, autosomal recessive, or X-linked. 408) (C) Xerophthalmia is a medical condition in which the eyes produce no tears. This is why xerophthalmia is referred to as dry eyes or dry eye syndrome or conjunctivitis arida. 409) (A) Xerophthalmia may be caused by a deficiency of vitamin A. There are other causes of xerophthalmia including systemic autoimmune disorders (such as Sjögren’s syndrome) and medications (such as antihistamines), but the most common cause of xeropthalmia is a vitamin A deficiency. Prophylaxis of xerophthalmia consists of administration of periodic vitamin A (when caused by vitamin A deficiency) or a change in diet to include (more) vitamin A-rich foods. 410) (C) Xerophthalmia is described by pathologic dryness of the conjunctiva and cornea. The conjunctiva becomes dry, thick, and wrinkled. If untreated, it can lead to corneal ulceration and ultimately to blindness as a result of corneal damage. 411) (A) Xerophthalmia mainly affects children under 9 years old and accounts for 20,000 – 100,000 new cases of childhood blindness each year in developing countries. The condition is largely found in developing countries like many of those in Africa and Southern Asia. Vitamin A deficiency is relatively rare in developed countries. The condition is not congenital and develops over the course of a few months as the lacrimal glands fail to produce tears. 412) (B) Geographic tongue is a condition that is characterized by a map-like appearance on the tongue. It is a benign condition that is not linked to any type of infection or illness. It can occur at any age, but is most common in middle-aged adults and older adults. It appears to occur more in women than in men. About 10% of people with geographic tongue may have mild discomfort or a burning or painful sensation; this is often from sensitivity to substances such as hot, spicy, or acidic foods, cigarette smoke, or toothpaste (source: webmd.com). Image: Geographic tongue Photograph by Bim im Garten, distributed under the Creative Commons Attribution-Share Alike 3.0 Unported license 413) (C) Waist-to-hip ratio (WHR) is the ratio of the circumference of the waist to that of the hips. The WHR can be used as an indicator or measure of health and the risk for developing serious health conditions. People with “apple-shaped” bodies (more weight around the waist) face more health risks than people with “pear-shaped” bodies (more weight around the hips). The World Health Organization states that abdominal obesity is defined as a WHR above 0.90 for men and 0.85 for females. The National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK) states that women with waist-hip ratios greater than 0.8 and men with waist-hip ratios greater than 1.0 are at increased health risk because of their fat distribution. Image: Waist-to-hip ratio Credit: Photograph by Mikael Häggström, license under the Creative Commons AttributionShare Alike 3.0 Unported license 414) (A) The inframammary crease is the human anatomical point where the bottom of the breast and chest meet. 415) (B) Cheilosis is a common inflammatory condition affecting the corners of the mouth (also known as the oral commissures). Depending on the underlying causes, it may last for a few days or persist indefinitely. Cheilosis is also known as angular cheilitis or angular stomatitis. Image: Cheilosis Credit: Photograph by Matthew Ferguson 57, distributed under the Creative Commons Attribution-Share Alike 3.0 Unported license 416) (D) Sarcoidosis is the growth of tiny collections of inflammatory cells (granulomas) in different parts of the body- most commonly the lungs, lymph nodes, eyes, and skin. 417) (D) Signs and symptoms of sarcoidosis vary depending on which organs are affected. Sarcoidosis sometimes develops gradually and can produce symptoms that last for years. Other times, symptoms appear suddenly and then disappear just as quickly. Many people with sarcoidosis have no symptoms, so the disease may be discovered only when a person has a chest X-ray done for another reason. For most people, sarcoidosis resolves on its own with no lasting consequences. But sometimes it can cause long-term problems. Depending on which organ(s) is affected determines what type of health complications may result. Untreated pulmonary sarcoidosis can lead to permanent scarring of the lungs, making it difficult to breathe. Sarcoidosis of the eyes can eventually cause blindness. Sarcoidosis of the kidneys can lead to kidney failure. Sarcoidosis of the heart can cause abnormal heart rhythms and in certain instances can lead to death. There is no cure for sarcoidosis, but most people do very well with little or only modest treatment. 418) (B) The most likely diagnosis for this patient is erythema migrans (Lyme disease). About 70-80% of people who get erythema migrans develop an expanding red circular rash. The rash begins at the site of the tick bite after a delay of 3 to 30 days, with the average being 7 days after the tick bite. The rash expands gradually over a period of days reaching up to 12 inches or more across. Sometimes the rash clears as it enlarges, resulting in a target or “bull’s-eye” appearance. The rash may feel warm to touch but is rarely itchy or painful. This rash may appear on any area of the body (source: cdc.gov). Image: “Bulls-eye” rash seen with erythema migrans 419) (C) The patient most likely has Rocky Mountain Spotted Fever (RMSF). RMSF is spread through the bite of an infected tick. The tick bite is usually painless and about half of the people who develop RMSF do not remember being bitten. The disease frequently begins as a sudden onset of fever and headache during the first few days of symptoms. The person may also have nausea and vomiting, abdominal pain, muscle pain, and a lack of appetite. Most people with RMSF (90%) have some type of rash during the course of illness. A classic case of RMSF involves a rash that first appears 2-5 days after the onset of fever as small, flat, pink, non-itchy spots (macules) on the wrists, forearms, and ankles and spreads to the trunk and sometimes the palms and soles. Approximately 10% of people with RMSF never develop a rash; these people are at increased risk for being misdiagnosed. Some also develop an atypical rash; these people are also at increased risk for misdiagnosis (source: cdc.gov). Image: Rash seen with Rocky Mountain Spotted Fever 420) (D) The most likely diagnosis for this patient is rosacea. Rosacea is a common condition that affects fair-skinned women with the greatest frequency. Because rosacea often has pimples accompanied with the facial redness, it is often referred to as acne rosacea. About half of people who have rosacea also experience eye dryness, irritation and swollen, reddened eyelids. In some people, rosacea's eye symptoms precede the skin symptoms. 421) (B) The patient’s likely diagnosis is hidradenitis suppurativa. Hidradenitis suppurativa produces small, usually painful lumps on the body, especially in the underarms and groin regions. Intertriginous dermatitis is a skin condition that is characterized by inflammation of the skin at skin folds such as the armpits and groin, like hidradenitis suppurativa; however, the inflammation manifests mainly as redness and not lumps. Psoriasis is a skin condition characterized by dry, itchy, rashes with white scales; psoriasis is normally a very itchy condition. Pityriasis rosea is characterized by large patches (rashes) on the chest, belly or back. 422) (C) The patient’s likely diagnosis is contact dermatitis. Both erythema migrans and rocky mountain spotted fever would create flu-like symptoms like fever, myalgia, nausea and vomiting; since these are not present, it is unlikely to be one of these. Rosacea is characterized by redness on the face. All of the symptoms given for the patient are consistent with contact dermatitis. The main symptom of contact dermatitis is a red rash wherever the skin came into contact with the irritant, in this case poison ivy. There may be blisters, fissures, hives, peeling or ulcers on the contact site. It is also very common that there would be itching or swelling at the site. Contact dermatitis can but does not necessarily cause systemic effects such as fever, generalized malaise and nausea and vomiting. 423) (B) Scabies is a condition that is highly contagious and that requires all members of a household be treated. All clothes and sheets should be washed in hot water and ironed at a high temperature. If a person gets treatment and the people with whom he or she lives or has close contact do not get treatment, the person can get scabies again. A person can have scabies and not readily display any active symptoms of the illness. A person can have scabies and not have any symptoms for 2 to 6 weeks. 424) (B) The child’s likely diagnosis is scarlet fever. Also known as scarlatina, scarlet fever features a bright red rash that covers most of the body. The rash looks like a sunburn and feels like sandpaper. It typically begins on the face or neck and spreads to the trunk, arms, and legs. If pressure is applied to the reddened skin, it will turn pale. The tongue generally looks red and bumpy, and it’s often covered with a white coating early in the disease. Scarlet fever is almost always accompanied by a sore throat and a high fever. It is most common in children 5 to 15 years of age. Scarlet fever is a bacterial illness caused by the same type of bacteria that causes a strep throat (group A streptococcus bacteria). In scarlet fever, the bacteria release a toxin that produces the rash and red tongue. Kawasaki disease also features a strawberry tongue and a high fever; however, it does not produce a red, sandpaper-textured rash. Instead it produces a rash that is usually on the main part of the body and the genitals. With Kawasaki disease, the child may have red, dry cracked lips, swollen lymph nodes in the neck, conjunctivitis without thick discharge, and peeling skin on the hands and feet. Rheumatic fever, also as the name implies, produces a fever. However, the rash is also not sandpaper-textured. Normally the rash associated with rheumatic fever is a flat or slightly raised, painless rash with a ragged edge (erythema marginatum). Mumps is a viral infection (caused by the paramyxovirus) that may produce swollen, painful salivary glands, fever, headache, fatigue, muscle aches, and appetite loss. Rashes are not associated with mumps (source: mayoclinic.org). Chapter 5- Endocrine System 1) What of the following statements is false regarding diabetes? A) Most cases of diabetes (85% to 90%) are type I diabetes B) American Indians/Alaskan Natives have the highest rates of diagnosed diabetes out of any other race/ethnic group C) People with type 1 diabetes are most at risk for diabetic ketoacidosis D) Hyperosmolar hyperglycemic nonketotic syndrome (HHNS) occurs more often in people with type 2 diabetes 2) Which of the following statements is false regarding type I diabetes? A) In most people with type 1 diabetes, the body's own immune system destroys the insulin-producing (islet) cells in the pancreas B) The first-line treatment for type I diabetes is oral hypoglycemic drugs C) There is no cure for type I diabetes despite active research D) There's no known way to prevent type 1 diabetes 3) Any random blood glucose above what level is indicative of diabetes? A) B) C) D) 120 mg/dL 150 mg/dL 180 mg/dL 200 mg/dL 4) A patient comes in and takes the 2-hour oral glucose tolerance test (OGTT) ingesting a 75g glucose load. 2 hours later, the person's blood glucose level is taken. What blood glucose level is indicative of diabetes? A) B) C) D) > 140 mg/dL > 160 mg/dL > 180 mg/dL > 200 mg/dL 5) What is the first-line treatment for most cases of type II diabetes? A) B) C) D) Meglitinides Biguanides Insulin Sulfonylureas 6) What are meglitinides indicated for? A) As the first-line treatment against type II diabetes B) For type 2 diabetics with postprandial hyperglycemia C) For abatement of hypoglycemia symptoms D) For type 1 diabetes before meals 7) What is the mechanism of action of sulfonylureas (used for type II diabetes)? A) It stimulates the beta cells of the pancreas to secrete more insulin B) It decreases the amount of glucose storage (glycogen) in the body C) It increases the renal clearance of glucose D) It decreases the absorption of sugar in the small intestines 8) Diabetes can cause all of the following complications except for: A) B) C) D) Vision loss Renal failure Epilepsy Limb amputation 9) A fasting blood sugar of 100-125 mg/dL is considered: A) B) C) D) Hypoglycemia Normal Prediabetes Diabetes 10) Which of the following does not represent one of the cardinal signs of diabetes? A) B) C) D) Extreme thirst Frequent headaches Extreme hunger Frequent urination 11) In order to diagnose diabetes through fasting blood glucose levels (FBG), what must be achieved? A) A FBG level ≥ 100 mg/dL on one occasion B) A FBG level ≥ 100 mg/dL on 2 occasions C) A FBG level ≥ 126 mg/dL on one occasion D) A FBG level ≥ 126 mg/dL on 2 occasions 12) Which of the following statements is false regarding hemoglobin A1C? A) Fasting is required prior to HbA1c testing B) The HbA1c test gives a long-term view (about 2-3 months) of blood sugar levels C) The HbA1c test monitors glycated hemoglobin levels D) A HbA1c value of 6.5% or greater is indicative of diabetes 13) What HbA1c value is indicative of prediabetes? A) B) C) D) 4.0% - 5.6% 5.7% - 6.4% 6.5% - 7.4% 7.5% - 8.4% 14) Every point increase in hemoglobin A1c corresponds roughly to an increase in blood sugar of: A) B) C) D) 20 mg/dL 30 mg/dL 40 mg/dL 50 mg/dL 15) Newly diagnosed diabetics should have their hemoglobin A1c level checked every: A) B) C) D) Month 3 months 6 months Year 16) Severe hypoglycemia includes all of the following symptoms except for: A) B) C) D) Clammy hands Cheilosis Lightheadedness Weakness 17) Which of the following is the preferred treatment for a hypoglycemic patient who is conscious? A) B) C) D) Glucose 15 to 20g Orange juice Soft drink Hard candy 18) Which describes the Somogyi effect? A) Rebound hypoglycemia that occurs in the morning following a nocturnal spike in blood sugar B) Rebound hyperglycemia that occurs in the morning following a nocturnal drop in blood sugar C) An elevation in the fasting blood sugar in the morning due to increased insulin resistance in the early morning hours D) A decrease in the fasting blood sugar in the morning due to decreased insulin resistance in the early morning hours 19) What is one of the ways to counter the Somogyi effect? A) Give a snack before bedtime B) Give a snack in the morning C) Raise the amount of regular insulin given at bedtime D)Raise the amount of NPH insulin given with dinner 20) What is the Dawn Phenomenon? A) Rebound hypoglycemia that occurs in the morning following a nocturnal spike in blood sugar B) Rebound hyperglycemia that occurs in the morning following a nocturnal drop in blood sugar C) An elevation in the fasting blood sugar in the morning due to increased insulin resistance in the early morning hours D) A decrease in the fasting blood sugar in the morning due to decreased insulin resistance in the early morning hours 21) All of the following instructions should be given to a diabetic except for: A) “Never go barefoot” B) “Trim nails rounded” C) “Wear shoes that fit properly” D) “Check your feet daily, especially the soles of your feet” 22) Insulin is a: A) B) C) D) Enzyme Hormone Blood component Substrate 23) Which type of insulin covers meals eaten within 30 to 60 minutes? A) B) C) D) Rapid acting insulin Short-acting insulin Intermediate-acting insulin Long-acting insulin 24) Which type of insulin covers needs for about half the day or overnight? A) B) C) D) Rapid acting insulin Short-acting insulin Intermediate-acting insulin Long-acting insulin 25) Long-acting insulin or intermediate-acting insulin are often combined with: A) Rapid-acting insulin B) Short-acting insulin C) Rapid or short-acting insulin D) Neither rapid nor short-acting insulin 26) Which type of insulin covers one meal at a time? A) B) C) D) Rapid-acting insulin Regular insulin NPH insulin Long-acting insulin 27) A basal insulin is insulin that has: A) B) C) D) A rapid onset No peak A short duration A long duration 28) Which diabetic medication is held on the day of a procedure using IV contrast dye and for 48 hours after the procedure? A) B) C) D) Rosiglitazone Chlorpropamide Repaglinide Metformin 29) What does exercise do in the body to help those with diabetes? A) Exercise increases the amount of insulin secreted by the body B) Exercise increases cellular glucose uptake in the body C) Exercise increases the renal clearance of glucose from the body D) Exercise decreases the amount of glucose absorbed into the bloodstream 30) A diabetic should do all of the following during a sick day except: A) Stop taking insulin or antidiabetic medications B) Check ketones with each urination C) Frequently self-monitor blood sugar levels D) Contact his or her HCP if blood glucose is greater than 300 mg/dL 31) What is metabolic syndrome? A) A group of risk factors that raises a person’s risk for heart disease, stroke, and diabetes B) A group of risk factors that raises a person’s risk for seizures C) A group of risk factors that raises a person’s risk for obesity D) A group of risk factors that raises a person’s risk for hypertension 32) All of the following are criteria for metabolic syndrome except for: A) B) C) D) Peak expiratory flow Abdominal obesity Hypertension Hyperlipidemia 33) Waist circumference diagnostic of metabolic syndrome is: A) > 30 inches for men and > 25 inches for women B) > 35 inches for men and > 30 inches for women C) > 40 inches for men and > 35 inches for women D) > 50 inches for men and > 40 inches for women 34) In order to be diagnosed with metabolic syndrome, a person must have: A) B) C) D) 2 out of the 5 criteria 3 out of the 5 criteria 4 out of the 7 criteria 5 out of the 10 criteria 35) What blood sugar level represents a metabolic risk factor? A) B) C) D) 80 mg/dL or greater 100 mg/dL or greater 110 mg/dL or greater 126 mg/dL or greater 36) What HDL cholesterol level represents a metabolic risk factor? A) HDL less than 60 mg/dL in men and less than 70 mg/dL in women B) HDL less than 50 mg/dL in men and less than 60 mg/dL in women C) HDL less than 40 mg/dL in men and less than 50 mg/dL in women D) HDL less than 30 mg/dL in men and less than 40 mg/dL in women 37) What is the normal range of thyroid-stimulating hormone (TSH)? A) B) C) D) 0.1 - 2.0 mIU/L 0.2- 3.0 mIU/L 0.4 - 4.0 mIU/L 0.04 - 12.0 mIU/L 38) What might the TSH be for a person who has (untreated) hypothyroidism? A) B) C) D) 0.001 1.2 5.6 9.1 39) What finding will be present in hypothyroidism? A) High TSH and low free T4 levels B) High TSH and high free T4 levels C) Low TSH and low free T4 levels D) Low TSH and high free T4 levels 40) A patient is found to have an elevated TSH level. What should the practitioner do next? A) Diagnose hypothyroidism B) Put the patient right away on levothyroxine daily C) Order free T3 and T4 labs D) Recheck the levels in 3 weeks to see if it’s still elevated 41) What is the gold standard for diagnosing Hashimoto’s thyroiditis? A) B) C) D) TSH level Free T3 levels Free T4 levels Antithyroid microsomal antibody 42) What is the most common cause of hypothyroidism? A) B) C) D) Hashimoto’s thyroiditis Pituitary disorders Congenital defect Medication reactions 43) Which medication is most commonly prescribed for hypothyroidism? A) B) C) D) Montelukast Levothyroxine Prednisone Repaglinide 44) What is the most common cause of hyperthyroidism? A) Grave’s disease B) Estrogen overdosing C) Uncontrolled diabetes D) Viral infection 45) All of the following symptoms are commonly seen in hyperthyroidism except for: A) B) C) D) Weight loss Tachycardia Hypotension Fine tremors 46) Which of the following would be laboratory findings for hyperthyroidism? A) High TSH and low free T3 and T4 levels B) High TSH and high free T3 and T4 levels C) Low TSH and low free T3 and T4 levels D) Low TSH and high free T3 and T4 levels 47) All of the following are true regarding radioactive iodine except: A) Radioactive iodine leads to permanent destruction of the thyroid gland B) Radioactive iodine results in hypothyroidism for life C) Radioactive iodine is contraindicated in pregnancy and lactation D) Using radioactive iodine causes an increased risk for cancer 48) Which of the following statements is false regarding glands? A) A gland is a group of cells that produces and secretes a chemical(s) B) Exocrine glands, such as sweat and salivary glands, release secretions onto an epithelial surface by way of a duct C) Endocrine glands release hormones directly into the bloodstream where they can be transported to cells in other parts of the body D) Most glands in the body are exocrine glands 49) Which gland in the body controls and regulates the thyroid? A) Thymus gland B) Pituitary gland C) Pineal gland D) Adrenal glands 50) Which gland is body is responsible for producing melatonin? A) B) C) D) Hypothalamus Pituitary gland Pineal gland Thyroid gland 51) Addison’s disease is a disorder in which the body produces too little: A) B) C) D) Epinephrine Cortisol ADH Insulin 52) Addison’s disease is also called: A) B) C) D) Hashimoto’s thyroiditis Grave’s disease Adrenal insufficiency Pheochromocytoma 53) All of the following are symptoms of Addison’s disease except for: A) B) C) D) Weight gain Low blood pressure Fatigue Salt craving 54) Which of the following is a frequent skin change associated with Addison’s disease? A) Acne B) Rosacea C) Vitiligo D) Hyperpigmentation of the skin 55) All of the following hematological conditions are associated with Addison’s disease except for: A) B) C) D) Hyperglycemia Hypoglycemia Hyperkalemia Hyponatremia 56) Untreated (un-medicated) Addison’s disease can trigger: A) B) C) D) A hypertensive crisis An addisonian crisis Ventricular fibrillation Status epilepticus 57) If a patient with Addison’s disease has low aldosterone levels, what may the practitioner prescribe to replace aldosterone? A) B) C) D) Hydrocortisone Fludrocortisone Prednisone Cortisone 58) Which of the following statements is false regarding Addison’s disease? A) Addison’s disease is a chronic, progressive disorder that cannot be cured B) Addison’s disease can be life-threatening C) A person with Addison’s disease will need to take medications daily for life as treatment D) People with Addison’s disease have a much shorter life expectancy than the rest of the population 59) A person with Addison’s disease often has cravings for: A) B) C) D) Potassium Salt Meat Spices 60) What is the cause of Cushing’s disease? A) A tumor or hyperplasia of the pituitary gland B) A tumor or hyperplasia of the adrenal gland C) A tumor or hyperplasia of the thyroid gland D) A tumor or hyperplasia of the spleen 61) All of the following are symptoms associated with Cushing’s disease except for: A) Weight gain B) Purple striae on various parts of the body C) Easy bruising D) Thickening of the skin 62) All of the following hematological conditions are associated with Cushing’s disease except for: A) B) C) D) Hyperglycemia Anemia Hypernatremia Hypokalemia 63) The most common enzyme defect in humans involves: A) B) C) D) Alpha glucosidase Glucose-6-phosphate dehydrogenase Lipase Protease 64) A patient comes in with an elevated TSH level and normal T4 levels. She has fatigue and cold intolerance. What is the diagnosis? A) B) C) D) Normal finding Subclinical hypothyroidism Hypothyroidism Hyperthyroidism 65) The thymus gland is responsible for: A) B) C) D) Metabolism Red blood cell production Cellular immunity Breathing rate 66) The anterior pituitary gland is responsible for the production of all of the following hormones except for: A) B) C) D) ADH LH TSH FSH 67) The adrenal glands sit on top of the: A) B) C) D) Liver Kidneys Gallbladder Pancreas 68) All of the following are catecholamines except for: A) B) C) D) Cortisol Epinephrine Norepinephrine Dopamine 69) Catecholamines are produced by the: A) B) C) D) Adrenal cortex Adrenal medulla Kidneys Liver 70) Which of the following statements is false regarding catecholamines? A) Catecholamine levels fluctuate constantly throughout the day B) Blood measurement of catecholamines is not as reliable as a 24-hour timed urine test C) Stress does not affect catecholamine levels D) Catecholamine levels can be used to help diagnose pheochromocytoma 71) In which disease process is too much adrenocorticotropic hormone (ACTH) produced by the body? A) B) C) D) Addison’s disease Cushing’s disease Hypothyroidism Hyperthyroidism 72) What is the earliest clinical signs of diabetic retinopathy? A) B) C) D) Cotton wall spots Hard exudates Microaneurysms Proliferation of blood vessels 73) What do hard exudates in retinopathy represent? A) Splotches of blood leaked from damaged capillaries B) Broken proteins from damaged capillaries C) Leakage of lipid residues from damaged capillaries D) Fragments of sugar molecules from damaged capillaries 74) On an eye examination, hard exudates appear as: A) B) C) D) Blue spots or flecks Yellow spots or flecks A large black area Red spots or flecks 75) What is the best way to prevent diabetic retinopathy? A) B) C) D) Daily eye hygiene Regular visits to the ophthalmologist Aggressive control of blood sugar levels Proper blood pressure control 76) How many stages comprise diabetic retinopathy? A) B) C) D) 1 2 3 4 77) Which of the following statements is true regarding diabetic retinopathy? A) Diabetic retinopathy is usually present within 3 months of a person having diabetes B) Diabetic retinopathy is usually present within 6 months of a person having diabetes C) Diabetic retinopathy is usually present within 1 year of a person having diabetes D) Diabetic retinopathy can take decades to develop from the time of the onset of diabetes 78) Proliferation of blood vessels seen in proliferative diabetic retinopathy can cause all of the following except for: A) B) C) D) Vitreous hemorrhage Retinal detachment Pingueculas Glaucoma 79) Diabetic retinopathy is best diagnosed using: A) B) C) D) The Snellen Chart Tonometry The dilated eye exam The red reflex test 80) Which statement is false regarding diabetic retinopathy? A) Diabetic retinopathy causes progressive damage to the retina, the light-sensitive lining at the back of the eye B) Diabetic retinopathy usually affects both eyes C) Diabetic retinopathy is only specific to type II diabetes D) Diabetic retinopathy can lead to total blindness 81) The proliferative stage of diabetic retinopathy refers to a proliferation of: A) B) C) D) Hard exudates Cotton wall spots Blood vessels Microaneurysms Endocrine System answers 1) (A) Most cases of diabetes (85% to 90%) are type II diabetes. American Indians/Alaskan natives have the highest rates of diagnosed diabetes out of any other race/ethnic background. According to statistics from the American Diabetes Association, the rates of diagnosed diabetes by race/ethnic background are 15.9% of American Indians/Alaskan Natives, 13.2% of nonHispanic blacks, 12.8% of Hispanics, 9.0% of Asian Americans, and 7.6% of non-Hispanic whites. Complications of diabetes include diabetic ketoacidosis, which is most common in type 1 diabetes and hyperosmolar hyperglycemic nonketotic syndrome, which is more common in type 2 diabetes (source: diabetes.org). 2) (B) The first-line treatment for type I diabetes is insulin. The first-line treatment for type II diabetes is oral hypoglycemic drugs. The exact cause of type 1 diabetes is unknown. In most people with type 1 diabetes, the body's own immune system — which normally fights harmful bacteria and viruses — mistakenly destroys the insulin-producing (islet) cells in the pancreas. Genetics may play a role in this process, and exposure to certain environmental factors, such as viruses, may trigger the disease. Despite active research, type 1 diabetes has no cure. But it can be managed. With proper treatment, people with type 1 diabetes can expect to live longer, healthier lives than they could have in the past. There's no known way to prevent type 1 diabetes. But researchers are working on preventing the disease or further destruction of the islet cells in people who are newly diagnosed (source: mayoclinic.org). 3) (D) Any random blood glucose above 200 mg/dL at any point in the day, whether a person has just eaten or not, is indicative of diabetes. Blood sugar levels should not exceed 200 mg/dL in healthy individuals. 4) (A) With the 2-hour oral glucose tolerance test (OGTT) with 75g of ingested glucose load, if the blood glucose is greater than 200 mg/dL 1 hour after the ingestion, this is indicative of diabetes. If the blood glucose is greater than 140 mg/dL 2 hours after ingestion, this is indicative of diabetes. Note that, in a healthy adult, the postprandial glucose level should not exceed 180 mg/dL after a meal. Exceeding over 200 mg/dL at any time is indicative of diabetes. 5) (B) Biguanides, chiefly metformin, is the first-line treatment for most cases of type II diabetes. 6) (B) Meglitinides are indicated for type 2 diabetics with postprandial hyperglycemia. Meglitinides such as nateglinide (Starlix) and repaglinide (Prandin) help stop the rapid rise in blood sugar levels that can occur immediately after a person with type 2 diabetes eats (source: webmd.com). 7) (A) Sulfonylureas work by stimulating the pancreas to release more insulin and are only effective when there is some pancreatic beta-cell activity still present in an individual. 8) (C) Diabetes can cause a variety of complications including hypertension, stroke, eye problems and blindness, kidney disease and kidney failure, and limb amputations. Diabetes does not cause epilepsy. 9) (C) A fasting blood sugar of less than 70 mg/dL is considered low blood sugar. A fasting blood sugar of 70-99 mg/dL is considered normal. A fasting blood sugar of 100-125 mg/dL is considered prediabetes. And a fasting blood sugar of 126 mg/dL or greater is considered diabetes. 10) (B) The 3 cardinal signs of diabetes are polydipsia (extreme thirst), polyphagia (extreme hunger), and polyuria (frequent urination). 11) (D) In order to diagnose diabetes, a fasting blood glucose of 126 mg/dL or higher must be met on 2 separate occasions. 12) (A) Fasting is not required prior to hemoglobin A1c testing. Hemoglobin A1c (HgbA1c) gives a long-term view of 2-3 months of a person’s blood sugar levels. It monitors glycated hemoglobin levels, which means hemoglobin covered with sugar. A HbA1c value of 6.5% or greater is indicative of diabetes. Converting this to mg/dL, this is approximately equal to a trailing 3-month average of 140mg/dL. 13) (B) A HbA1c value of 5.7% to 6.4% is indicative of prediabetes. 14) (B) For every point increase there is in a person’s hemoglobin A1c value, this correlates roughly to an increase of about 30mg/dL. 15) (B) Newly diagnosed diabetics should have their hemoglobin A1c levels checked every 3 months until their blood glucose levels are well controlled. After this, hemoglobin A1c level should be checked twice a year (every 6 months). 16) (B) Cheilosis, inflammation and small cracks in one or both corners of the mouth, is caused by various vitamin deficiencies, not hypoglycemia. Symptoms of severe hypoglycemia include stupor, seizures, visual disturbances such as loss of vision, and confusion (source: mayoclinic.org). 17) (A) 15 to 20 grams of glucose is the preferred treatment for a hypoglycemic patient who is conscious. Other options include orange juice, a soft drink, and hard candy. 18) (B) The Somogyi effect is rebound hyperglycemia that occurs in the morning following a nocturnal drop in blood sugar. The somogyi effect is due to overtreatment of diabetics in the evening hours and/or at bedtime (bedtime insulin dose is too high). The overtreatment of bloodlowering medication causes severe nocturnal hypoglycemia. In response, the body stimulates counterregulatory hormones such as glucagon to be released from the liver. The high levels of glucagon raise the blood sugar levels, resulting in high fasting blood glucose by 7:00am. This is more common in type 1 diabetics. 19) (A) The Somogyi effect is rebound hyperglycemia that occurs in the morning following a nocturnal drop in blood sugar. The somogyi effect is due to overtreatment of diabetics in the evening hours and/or at bedtime (bedtime insulin dose is too high). The overtreatment of bloodlowering medication causes severe nocturnal hypoglycemia. Since the underlying reason for this is overmedicating patients, a patient can either be given a snack at bedtime to raise the blood sugar or the diabetic medications that a patient receives in the evening or bedtime hours should be lowered. 20) (C) Dawn Phenomenon is a normal physiologic event in which there is an elevation in the fasting blood sugar that occurs daily early in the morning. This is due to the body’s physiology in which there is an increase in insulin resistance between 4am and 8am. This is caused by the physiologic spike in growth hormone, glucagon, epinephrine, and cortisol. 21) (B) Diabetics should trim their nails squarely, not rounded. This can prevent injury to the toenails. Diabetics should never go barefoot, should wear shoes that fit properly, and check their feet daily, especially the soles. 22) (B) Insulin is a hormone. Insulin does not catalyze any reaction, so it’s not considered an enzyme. As a messenger (a hormone), it regulates the activities of proteins that do catalyze reactions. 23) (B) Short-acting insulin such as regular (R) humulin covers insulin needs for meals eaten within 30 to 60 minutes. 24) (C) Intermediate-acting insulin covers needs for about half the day or overnight. 25) (C) Long-acting or intermediate-acting insulin are often combined with rapid-acting or shortacting insulin. 26) (A) Rapid-acting insulin covers one meal at a time. If a person eats 3 meals a day, it would be given once per each meal to cover the meal. 27) (B) A basal insulin is insulin that has no peak. 28) (D) Metformin should be held on the day of a procedure using IV contrast and for 48 hours after the procedure (after 48 hours, it may be resumed again). If not, this can cause lactic acidosis. This can lead to major medical issues, including multiorgan failure. 29) (B) Exercise increases cellular glucose uptake in the body, thereby decreasing blood glucose levels. 30) (A) When sick, a diabetic should not stop taking antidiabetic medicine or insulin. The person should frequently self-monitor blood glucose levels, eat small amounts of food every 3 to 4 hours to keep the blood sugar as normal as possible, and contact the HCP if there is vomiting or persistent diarrhea, the blood glucose level is greater than 300 mg/dL, or if there are changes in the level of consciousness. 31) (A) Metabolic syndrome is a group of risk factors that raises a person’s risk for heart disease, stroke, and diabetes. 32) (A) Peak expiratory flow is not one of the criteria for metabolic syndrome. The 5 characteristics that comprise metabolic syndrome are abdominal obesity (waist circumference greater than 40 inches for men or greater than 35 inches for women), hypertension (130/85 mmHg or higher), a high triglyceride level (greater than 150 mg/dl), a low HDL cholesterol level (less than 40 mg/dl in men or less than 50 mg/dl in women), and high fasting blood sugar (100 mg/dl or higher). In order for metabolic syndrome to be diagnosed, the person must meet at least 3 of these criteria. If a person just has 1 or 2, for instance, a diagnosis of metabolic syndrome will not be made. 3 or more of these criteria must be present. 33) (C) Waist circumference diagnostic of metabolic syndrome is a waist circumference greater than 40 inches for men and greater than 35 inches for women. 34) (B) In order to be diagnosed with metabolic syndrome, a person must have 3 out of the 5 criteria. Metabolic syndrome is a group of risk factors that increases a person’s risk for heart disease, stroke, and diabetes. The 5 criteria are abdominal obesity, hypertension, a high triglyceride level, a low HDL cholesterol level, and a high fasting blood sugar. A person with 3 or more of these 5 criteria will be diagnosed with metabolic syndrome. 35) (B) A blood sugar of 100 mg/dL or greater represents a metabolic risk factor. 36) (C) An HDL cholesterol level less than 40 mg/dL in men or less than 50 mg/dL in women is a metabolic risk factor. 37) (C) 0.4 - 4.0 mIU/L is the normal range of thyroid-stimulating hormone (source: medlineplus.gov). 38) (D) The TSH will be elevated in hypothyroidism. The normal range of TSH is 0.4 – 4.0 mIU/L. The TSH will be above this reference range in hypothyroidism. A TSH of 9.1 may be seen in hypothyroidism. TSH stands for thyroid-stimulating hormone. If a person has hypothyroidism, this means s/he is not producing sufficient levels of thyroid hormones that the body needs. Therefore, the pituitary gland sends out more TSH (thyroid-stimulating hormone) in an attempt to increase the production of thyroid hormones. This is why TSH is elevated in hypothyroidism. 39) (A) In hypothyroidism, there will be high TSH and low free T4 levels. 40) (C) If a patient is found to have an elevated TSH level, the next step is to order free T3 and T4 labs. If these levels are low, then the person can be diagnosed with hypothyroidism. Hypothyroidism should not be diagnosed based on TSH level alone, because the TSH level can transiently elevate due to external circumstances such as the person recently taking iodine supplements. When it’s due to transient increase, levels go back to normal; it is not indicative of hypothyroidism. Positive confirmation of hypothyroidism depends on an elevated TSH level with low free T3 and T4 levels. 41) (D) The gold standard for diagnosing hashimoto’s thyroiditis is antimicrosomal antibodies, which will be elevated. Antimicrosomal antibodies are also referred to as TSH-receptor antibodies. 42) (A) The most common cause of hypothyroidism is Hashimoto’s thyroiditis (or autoimmune hypothyroidism), a form of thyroid inflammation caused by a person’s own immune system response. This causes the thyroid's tissue to gradually decay, which directly impacts the thyroid's ability to produce hormones. This will eventually result in hypothyroidism when the thyroid is unable to make the amounts of thyroid hormones that the body needs. Hashimoto's thyroiditis is a common disorder. It affects as many as 10 million people in the US alone, and approximately 10% of women over age 30 have Hashimoto's thyroiditis (the disease affects women ten times more than men). Other causes of hypothyroidism include partial or complete thyroidectomy, radiation treatment either for cancer or for hyperthyroidism with radioactive iodine (I-131), congenital defects (congenital hypothyroidism), certain medications such as amiodarone, lithium, interferon alpha, and interleukin-2, too much or too little iodine, damage to the pituitary gland, and rare disorders that infiltrate the thyroid such as amyloidosis (can deposit amyloid protein on the thyroid), sarcoidosis (which can deposit granulomas) and hemochromatosis (which can deposit iron). 43) (B) Levothyroxine (Synthroid) is most commonly prescribed for hypothyroidism. Levothyroxine is a synthetic thyroid hormone that is chemically identical to thyroxine (T4), which is naturally secreted by the thyroid gland. 44) (A) The most common cause for hyperthyroidism is a chronic autoimmune disease called Grave’s disease. Grave’s disease accounts for around 75% of all cases of hyperthyroidism (source: patient.info). 45) (C) Symptoms of hyperthyroidism may include weight loss (even when the person has the same appetite and eats the same amount of food or even increases the amount of food eaten), increased appetite, nervousness, anxiety, irritability, tachycardia, tremor (usually a fine trembling in the hands and fingers), sweating, heat intolerance, changes in bowel patterns, especially more frequent bowel movements, an enlarged thyroid (goiter), fatigue, muscle weakness, difficulty sleeping, skin thinning, and fine, brittle hair. Hypertension would be seen in hyperthyroidism, not hypotension. Uncommon conditions of hyperthyroidism include exophthalmos (protruding out of the eye balls); the chance of this occurring increases if the person smokes (source: mayoclinic.org). 46) (D) In hyperthyroidism, there will be very low TSH (< 0.4 mIU/L) and high free T3 and T4 levels. 47) (D) Radioactive iodine is not linked to an increased risk for cancer. Radioactive treatment of hyperthyroidism results in the permanent destruction of the thyroid gland and the person having hypothyroidism for life. The person will be placed on hormone therapy for life, most commonly levothyroxine (Synthroid). Radioactive iodine is contraindicated in pregnancy and lactation. Using radioactive iodine during pregnancy or lactation can lead to damage of the child’s thyroid. 48) (D) A gland is a group of cells that produces and secretes a chemical(s). Exocrine glands, such as sweat and salivary glands, release secretions onto an epithelial surface by way of a duct. Endocrine glands release hormones directly into the bloodstream where they can be transported to cells in other parts of the body. The majority of glands in the body are endocrine glands. 49) (B) The pituitary gland (also called the “Master Gland”) controls and regulates thyroid function. Therefore, damage to the pituitary gland can affect thyroid hormone production. 50) (C) The pineal gland is responsible for the production of melatonin, which helps regulate a person’s sleep-wake cycle. 51) (B) Addison’s disease is a disorder in which the body produces too little cortisol. Besides cortisol, often there are insufficient levels of aldosterone as well. 52) (C) Addison’s disease is also called adrenal insufficiency. It is called this because the adrenal glands produce too little cortisol and often insufficient levels of aldosterone as well. 53) (A) Symptoms of Addison’s disease include extreme fatigue, weight loss and decreased appetite, hyperpigmentation of the skin (bronzing of the skin), low blood pressure that may cause episodes of fainting, salt craving, gastrointestinal problems such as nausea, vomiting, and diarrhea, hypoglycemia, nausea, and depression. 54) (D) Addison’s disease is associated with hyperpigmentation of the skin (bronzing of the skin). Image: Hyperpigmentation (bronzing) of the skin seen with Addison’s disease 55) (A) Addison’s disease is associated with hypoglycemia, hyperkalemia, and hyponatremia. 56) (B) Untreated (un-medicated) Addison’s disease can trigger an addisonian crisis. During an addisonian crisis, a person may have severe vomiting and diarrhea (leading to dehydration), hypotension which may include fainting, loss of consciousness, and hyperkalemia and hyponatremia. 57) (B) If a patient with Addison’s disease has low aldosterone levels, the practitioner may prescribe fludrocortisone to replace aldosterone. Hydrocortisone, prednisone, or cortisone would be prescribed to replace cortisol. 58) (D) Addison’s disease is a chronic, progressive, incurable disorder characterized by the lack of production of adrenal hormones, specifically cortisone and many times also aldosterone. Addison’s disease, left untreated, can trigger an addisonian crisis which can be life threatening. To manage Addison’s disease, a person will need to take synthetic cortisol (and possibly also synthetic aldosterone) to replace the lack of cortisol (and aldosterone) produced naturally by the adrenal glands. This is done by taking the medication(s) every day for life. With good management (daily medications), people with Addison’s disease have a normal life expectancy. 59) (B) A person with Addison’s disease often has cravings for salt due to the underlying hyponatremia that the disease process causes. 60) (A) Cushing’s disease is caused by a tumor or hyperplasia of the pituitary gland. A type of pituitary tumor called an adenoma is the most common cause. An adenoma is almost always benign (noncancerous). 61) (D) Common symptoms of Cushing’s disease include weight gain and fatty tissue deposits, particularly around the midsection and upper back, in the face (moon face) and between the shoulders (buffalo hump), pink or purple stretch marks (striae) on the skin of the abdomen, thighs, breasts, and arms, thinning, fragile skin that bruises easily, slow healing of cuts, infections, and acne. Women with Cushing syndrome may experience thicker or more visible body and facial hair (hirsutism) and irregular or absent menstrual periods. Men with Cushing syndrome may experience decreased libido, decreased fertility, and erectile dysfunction. Other signs and symptoms of Cushing’s disease may include severe fatigue, muscle weakness, depression, anxiety and irritability, loss of emotional control, cognitive difficulties, new or worsened high blood pressure, headache, bone density loss, leading to fractures over time, and, in children, impaired growth (source: mayoclinic.org). Image: Purple striae seen in Cushing’s disease 62) (B) Anemia is not associated with Cushing’s disease. Hyperglycemia, hypokalemia, and hypernatremia are associated with Cushing’s disease. 63) (B) Glucose-6-phosphate dehydrogenase (G6PD) is the most common enzyme defect in humans. It leads to a common condition called G6PD deficiency, which can cause episodes of hemolytic anemia, which at times could prove fatal. 64) (B) Subclinical hypothyroidism is a mild form of hypothyroidism in which a person has an elevated TSH level but T4 levels within the normal range. The person with subclinical hypothyroidism may have no symptoms or mild symptoms such as fatigue, cold intolerance, consistent weight gain, depression, or memory problems. 65) (C) The thymus gland, located in the anterior aspect of the chest at the base of the heart, is responsible for cellular immunity. Cellular immunity (or cell-mediated immunity) is an immune response that does not involve antibodies, but rather involves the activation of phagocytes, antigen specific cytotoxic T-lymphocytes, and the release of various cytokines in response to an antigen. 66) (A) The anterior pituitary gland is responsible for the production of ACTH (adrenocorticotropic hormone), TSH (thyroid-stimulating hormone), FSH (follicle-stimulating hormone), LH (luteinizing hormone), GH (growth hormone), and prolactin. The posterior pituitary gland is responsible for the production of oxytocin and ADH (antidiuretic hormone). 67) (B) The adrenal glands sit on top of the kidneys. There are 2 adrenal glands, one on the top of each kidney. Image: Adrenal glands 68) (A) The major catecholamines are epinephrine, norepinephrine, and dopamine. 69) (B) Catecholamines are produced by the adrenal medulla. 70) (C) Catecholamine levels fluctuate constantly throughout the day. Blood measurement of catecholamines is not as reliable as a 24-hour timed urine test for this reason. Because catecholamine levels fluctuate, obtaining a blood sample can at given point may not represent the average level for a person. Instead, a 24-hour timed urine test is used most often, which allows for more accurate measurement. Many things can affect catecholamine levels. High levels can indicate an adrenal gland tumor (such as pheochromocytoma) or other type of tumor is present. Any major stress, such as burns, sepsis, illness, surgery, or traumatic injury can cause high levels. Also, blood pressure medications can cause high levels of catecholamines (source: webmd.com). 71) (B) In Cushing’s disease, too much ACTH is produced. This causes excess cortisol in the body. 72) (C) The earliest clinical signs of diabetic retinopathy are microaneurysms. Microaneurysms are focal dilated areas of weakened blood vessel walls. 73) (C) Hard exudates in retinopathy represent the leakage of lipid residues from damaged capillaries. 74) (B) On an eye examination, hard exudates appear as yellow spots or flecks on the eye. This is due to the leakage of lipid residues from damaged capillaries secondary to the disease process. Image: Hard exudates seen in diabetic retinopathy 75) (C) The best way to prevent diabetic retinopathy is through aggressive control of diabetes. Since the pathologic mechanism of diabetic retinopathy is directly related to the underlying cause, which is hyperglycemia, the best way to prevent or delay further damage caused by diabetic retinopathy is by aggressive control of one’s blood sugar. 76) (C) Diabetic retinopathy is composed of 3 stages. The first stage is diabetes without retinopathy. The second stage is the nonproliferative stage of diabetic retinopathy. The third stage is the proliferative stage of diabetic retinopathy. Usually, the first stage is characterized by either mild symptoms or no symptoms at all. However, damage is occurring to retinal pericytes, which are cells in the retina that are specialized contractile cells that surround the retinal vasculature and are very important for regulating blood flow throughout the retina. The second stage, the nonproliferative stage, is characterized by microaneurysms and hard exudates in the retina. The third stage, the proliferative stage, is characterized by a proliferation of blood vessels in the retina, which can have damaging effects on the eye. 77) (D) Diabetic retinopathy is a slow-progressing disease. It usually takes many years, even decades, for diabetic retinopathy to develop and progress in stages, especially to the point of complete blindness. Diabetic retinopathy is not something that happens in a few months. 78) (C) Pingueculas is a condition that is caused by UV rays damaging the cornea of the eye. It is unrelated to proliferative diabetic retinopathy. Diabetic retinopathy in the proliferative stage involves abnormal growth of blood vessels in the retina. These abnormal blood vessels can be damaging in many ways to the body; they shouldn’t be seen as the helpful types of blood vessels. One complication they can lead to vitreous hemorrhage. The new blood vessels may bleed into the clear, jelly-like substance that fills the center of the eye called the vitreous cavity. Depending on the severity, it may cause mild symptoms such as just dark spots (floaters) or severe symptoms such as complete vision blockage if the blood fills the whole vitreous cavity. The blood often clears from the eye within a few weeks to months, so the vision loss associated with vitreous hemorrhage is usually temporary. The abnormal blood vessels associated with proliferative diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye (causing retinal detachment). The new blood vessels may grow in the front of the eye and interfere with the normal flow of fluid out of the eye, causing an increased intraocular pressure (glaucoma). Eventually, the effects seen with diabetic retinopathy can cause complete and permanent vision loss. 79) (C) Diabetic retinopathy is best diagnosed using the dilated eye exam. During this dilated eye exam, the practitioner can see clinical signs of diabetic retinopathy such as microaneurysms (appearing as red spots), hard exudates (appearing as yellow spots or flecks), and a proliferation of blood vessels. The downside of a dilated eye exam is that it can’t pick up on the first stage of diabetic retinopathy (diabetes without retinopathy); only through microscopic examination can damage to the retinal pericytes be seen. So, a dilated eye exam is more specific to the second and third stages of diabetic retinopathy. 80) (C) Diabetic retinopathy can occur with any type of diabetes (type I or type II). Diabetic retinopathy causes progressive damage to the retina, which is the light-sensitive lining at the back of the eye and can lead to total blindness. It usually affects both eyes. 81) (C) The proliferative stage of diabetic retinopathy refers to a proliferation of blood vessels within the eye. Because of all the microvascular damage done to the eye in the previous stages, as a restorative mechanism, the body creates a proliferation of blood vessels in an attempt to supply blood to the eye. Chapter 6- Gastrointestinal System 1) A person with GERD should avoid all of the following except for: A) B) C) D) Caffeine Alcohol NSAIDs Acetaminophen 2) GERD can lead to all of the following complications except for: A) B) C) D) Gastric ulcers Barrett’s esophagus Zollinger-Ellison syndrome Tooth decay 3) All of the following medications are commonly prescribed for GERD except for: A) B) C) D) Proton pump inhibitors H2 blockers Antispasmodics Antacids 4) All of the following statements are true regarding ulcers except: A) Duodenal ulcers are more common than gastric ulcers B) Helicobacter pylori is the most common cause for both duodenal and gastric ulcers C) Gastric ulcers are relieved by eating food D) Chronic NSAID use is a common cause for duodenal and gastric ulcers 5) A patient goes to a clinic who has been found to have gastric ulcers that are H. pylori positive. Besides being prescribed proton pump inhibitors and H2 blockers, which medication class will also be prescribed to this patient? A) Antivirals B) Antibiotics C) Antifungals D) Antiparasitics 6) Which of the following statements is false regarding helicobacter pylori bacteria? A) H. pylori is not a normal flora of the human body B) H. pylori can cause peptic ulcers and stomach cancer C) H. pylori is found in over half of the world’s population D) Over 90% of people with H. pylori bacteria develop a peptic ulcer 7) All of the following might make a healthcare provider suspect that a patient has gastric ulcers except: A) Anemia shown in CBC B) Elevated H. pylori immunoglobulin (IgG) levels C) Pain hours after eating a meal D) Serology shows low iron levels 8) All of the following are elevated in acute pancreatitis except for: A) B) C) D) Amylase Lipase Glycogen Trypsin 9) All of the following are symptoms that can be seen in acute pancreatitis except for: A) Nausea and vomiting B) Abdominal epigastric pain that radiates to the midback C) Fever D) Gastric ulcers 10) All of the following are common causes of acute pancreatitis except for: A) Cholelithiasis B) Elevated triglyceride levels C) Alcohol abuse D) Diabetes 11) All of the following are common symptoms of clostridium difficile colitis except for: A) B) C) D) 10 to 15 stools a day Fever Cramping Red rashes on the groin 12) What test is used to diagnose C. difficile colitis? A) B) C) D) Sputum sample Stool assay Serology Colon biopsy 13) What is the most likely scenario of how a person becomes ill with C. difficile colitis? A) The person had unprotected sex with several partners B) The person had a recent episode of a head cold C) The person just completed a course of antibiotics D) The person recently camped out in the woods without much protection 14) Which of the following statements is false regarding gastroenteritis? A) The main symptom of gastroenteritis is severe constipation B) Gastroenteritis is inflammation of the lining of the intestines C) The most common cause of gastroenteritis is norovirus infection D) Gastroenteritis can be caused by a virus, bacteria, or parasites 15) What is the most common complication of gastroenteritis? A) Internal hemorrhaging B) Dehydration C) Rhinitis D) Sinusitis 16) Symptoms of gastroenteritis include all of the following except: A) B) C) D) Abdominal cramping Hematemesis Vomiting Diarrhea 17) What is the most common causative agent of diarrhea in infants and young children in the world? A) B) C) D) Norovirus Rotavirus Epstein-Barr virus Varicella zoster virus 18) Cullen’s sign is specific to checking for: A) B) C) D) Cholecystitis Pyelonephritis Appendicitis Acute pancreatitis 19) Cullen’s sign is: A) Pain elicited when the left lower quadrant of the abdomen is palpated B) Pain elicited when the right lower quadrant of the abdomen is palpated C) Superficial edema and bruising in the subcutaneous fatty tissue around the umbilicus D) Bruising and bluish discoloration of the flanks 20) Grey Turner’s sign is: A) Pain elicited when the left lower quadrant of the abdomen is palpated B) Pain elicited when the right lower quadrant of the abdomen is palpated C) Superficial edema and bruising in the subcutaneous fatty tissue around the umbilicus D) Bruising and bluish discoloration of the flanks 21) Zollinger-Ellison syndrome is a syndrome in which the body produces too much: A) B) C) D) Myoglobin Gastrin Insulin Amylase 22) Which test is entirely specific to Zollinger-Ellison syndrome? A) B) C) D) Amylase levels Fasting gastrin level Protease levels Antiparietal cell antibody level 23) Zollinger-Ellison syndrome, if left untreated, can ultimately lead to: A) B) C) D) Liver failure Kidney failure Ulcerations in the GI tract Lung collapse 24) Serum gastrin levels are considered elevated if they are above: A) B) C) D) 50 pg/mL 100 pg/mL 200 pg/mL 500 pg/mL 25) Which of the following statements is false regarding celiac disease? A) The definitive test to diagnose celiac disease is a biopsy of the small intestine B) The only solution to celiac disease is a strict, lifelong adherence to a gluten-free diet C) The symptoms associated with a person with celiac disease eating foods containing gluten are mostly neurological manifestations D) Patients diagnosed with celiac disease should be examined for nutritional deficiencies, which can cause health problems such as low bone density 26) Which of the following should be avoided with a person who has celiac sprue? A) B) C) D) Corn Rice Beer Potatoes 27) What type of infection is giardiasis? A) B) C) D) Bacterial Viral Fungal Parasitic 28) What is the most prominent symptom that giardiasis causes? A) B) C) D) Vomiting Heartburn Diarrhea Fever 29) What is the most common situation of how a person contracts giardiasis? A) The person drank some local water while on vacation B) The person ate raw beef at a local restaurant C) The person sat next to someone who was sneezing incessantly D) The person got pricked with a needle that had blood on it 30) What is the method through which giardiasis is diagnosed? A) Blood tests B) Nasal swab C) Stool samples D) Urine samples 31) What is proctitis? A) Inflammation of the anus and the lining of the rectum B) Inflammation of the prostate gland C) Inflammation of the small intestine D) Inflammation of the pituitary gland 32) What’s the most common cause of proctitis? A) B) C) D) Constipation Irritable bowel syndrome STDs Ulcerative colitis 33) Hypoactive bowel sounds are normal in all of the following conditions except: A) During exercise B) During sleep C) After surgery D) They are never normal and are a sign of an underlying condition 34) Decreased or absent bowel sounds would likely cause all of the following except for: A) B) C) D) Abdominal distention Diarrhea Constipation Abdominal bloating 35) With bowel obstruction, what type of bowel sounds would likely be heard? A) Constant, monotonous, low-pitched sounds B) High-pitched bowel sounds C) Gurgling sounds D) No bowel sounds 36) Which of the following conditions is least likely to cause projectile vomiting? A) B) C) D) Gastric outlet syndrome Superior mesenteric artery syndrome Appendicitis Pyloric stenosis 37) All of the following conditions cause right upper quadrant pain except for: A) B) C) D) Pyelonephritis of the right kidney Cholecystitis Appendicitis Hepatitis 38) Dumping syndrome is a condition that can be caused by: A) B) C) D) Eating too fast Bariatric surgery Gastric ulcers Pyloric stenosis 39) Which of the following statements is false? A) Diverticula are pouches that form in the wall of the colon in diverticulosis B) Diverticulosis is the formation of diverticula, while diverticulitis is a condition in which the diverticula become inflamed or infected C) It is believed that a low-fiber diet plays a role in the formation of diverticula D) Diverticulosis and diverticulitis are both painful conditions 40) Which of the following statements is false regarding diverticulitis? A) Diverticulitis can cause diarrhea or constipation B) Diverticulitis usually causes pain in the right lower quadrant C) Diverticulitis can cause nausea and sometimes vomiting and anorexia D) Diverticulitis can cause bloating and gas 41) Which of the following statements is false regarding diverticula? A) Diverticula are found most often in the lower part of the large intestine (colon) B) Diverticula are common, especially after the age of 40 C) Diverticula seldom cause problems D) Diverticula are caused due to autoimmune dysfunction in which the body attacks part of the colon 42) All of the following are risk factors for diverticulitis except for: A) B) C) D) Being thin Aging Smoking Lack of exercise 43) What diet is recommended for diverticulitis? A) B) C) D) A high-fiber diet A low-fiber diet A high-protein diet A low-protein diet 44) Complications that can result from diverticulitis include all of the following except for: A) B) C) D) Abscess formation Pyelonephritis Colon or small intestine blockage Peritonitis 45) Treatments for uncomplicated diverticulitis include all of the following measures except for: A) Antibiotics B) A liquid diet for a few days while the bowel heals before gradually returning to solid food C) Motrin for pain relief D) Rest 46) Which of the following statements is false regarding gastritis? A) Gastritis is inflammation of the lining of the stomach B) Gastritis can occur acutely or chronically C) Gastritis is not associated with any increased risk for stomach cancer D) If untreated, gastritis can lead to severe blood loss 47) All of the following are causes or contributors to gastritis except for: A) B) C) D) Crohn’s disease Excessive alcohol use Bile reflux Infections 48) All of the following are common symptoms of gastritis except for: A) B) C) D) Indigestion Projectile vomiting Abdominal pain Loss of appetite 49) Which of the following drugs would not be prescribed for those suffering from gastritis? A) B) C) D) Antacids NSAIDs Proton pump inhibitors H2 blockers 50) Which of the following statements is true regarding irritable bowel syndrome? A) Irritable bowel syndrome causes changes in bowel tissue B) Irritable bowel syndrome increases a person’s risk for colorectal cancer C) Irritable bowel syndrome can cause diarrhea or constipation D) Irritable bowel syndrome is an inflammatory condition 51) Which of the following statements is false regarding irritable bowel syndrome (IBS)? A) Irritable bowel syndrome is a chronic disease B) Females tend to have IBS at about twice the incidence as males C) Irritable bowel syndrome tends to occur in the elderly D) Diagnosing irritable bowel syndrome depends largely on a complete medical history and physical exam 52) Common symptoms of irritable bowel syndrome include all of the following except: A) B) C) D) Abdominal pain or cramping A bloated feeling Blood in the stool Diarrhea or constipation 53) Which of the following statements is false regarding irritable bowel syndrome (IBS)? A) The cause of IBS is not known exactly B) Episodes of IBS or aggravation of IBS is believed to be caused by certain triggers C) IBS can aggravate hemorrhoids D) Steroids are the main type of medication used to treat IBS 54) Which of the following statements is false regarding ulcerative colitis? A) Ulcerative colitis is a non-inflammatory bowel disease that causes ulcers in the digestive tract B) Ulcerative colitis affects the large intestine and rectum C) Symptoms of ulcerative colitis usually develop over time rather than suddenly D) Ulcerative colitis can potentially lead to life-threatening complications 55) Symptoms of ulcerative colitis include all of the following except for: A) Diarrhea, often with blood or pus B) Abdominal pain and cramping C) Rectal bleeding D) Dysuria 56) Which of the following drugs would be least likely to be prescribed for ulcerative colitis? A) B) C) D) Antidiarrheals Anti-inflammatory drugs Laxatives Pain relievers 57) Besides ulcerative colitis, what is the other type of inflammatory bowel disease (IBD)? A) B) C) D) Irritable bowel syndrome Crohn’s disease Diverticulosis Zollinger-Ellison syndrome 58) All of the following symptoms are associated with peritonitis except for: A) B) C) D) Polyuria Decreased or absent bowel sounds Fever Abdominal distension 59) Which of the following is least likely to cause peritonitis? A) B) C) D) Diverticulitis Peritoneal dialysis Renal failure Appendicitis 60) If peritonitis is left untreated, it can lead to: A) Gastric ulcers B) Zollinger-Ellison syndrome C) Sepsis D) Abdominal aortic aneurysm 61) Salmonella infection is normally transmitted by: A) B) C) D) Pigeons and other birds Turtles and other amphibians Mice and other rodents Cats and other felines 62) Barrett’s esophagus is: A) A benign illness B) A precancer for esophageal cancer C) A malignant cancer of the esophageal lining D) A tumor in the lower esophagus 63) How is Barrett’s esophagus diagnosed? A) B) C) D) MRI Barium swallow Manual throat examination Upper endoscopy with biopsy 64) In order to diagnose anorexia nervosa, how much weight loss from the ideal body weight must there be? A) B) C) D) 5% 10% 15% 25% 65) The majority of people with anorexia nervosa are between the ages of: A) 6 and 12 B) 13 and 20 C) 21 and 28 D) 30 and 35 66) A person with anorexia nervosa is at risk for all of the following complications except for: A) B) C) D) Cardiac complications Osteoporosis Anemia Dysmenorrhea 67) A practitioner places his fingers on the approximate location of the gallbladder while the patient takes a deep breath. The practitioner is checking for which sign? A) B) C) D) Rovsing’s sign Murphy’s sign Obturator sign Psoas sign 68) An atonic colon is also called: A) B) C) D) Hirschsprung disease Lazy colon Hemorrhoids Intussusception 69) What is the most common symptom of an atonic colon? A) B) C) D) Constipation Vomiting Nausea Fever 70) An atonic colon is caused by: A) Lack of fiber in the diet B) Injury to the colon C) Loss of muscle tone D) Decreased blood supply to the colon 71) Which of the following is most likely to cause an atonic colon? A) B) C) D) Chronic use of steroids Trauma to the colon Prostatitis Chronic use of laxatives 72) Oliguria is defined as urinary output less than: A) B) C) D) 1500 mL/day 1000 mL/day 500 mL/day 400 mL/day 73) Which of the following statements is false regarding amebiasis? A) Amebiasis is a disease caused by the parasite Entamoeba histolytica B) Amebiasis is most common in people who live in tropical areas with poor sanitary conditions C) Amebiasis is characterized by severe, debilitating pain, nausea, and vomiting D) Amebiasis is diagnosed through stool sample examination 74) Which of the following conditions is referred to as the stomach flu? A) B) C) D) Pyloric stenosis Irritable bowel syndrome GERD Gastroenteritis 75) Which of the following statements is false regarding esophageal spasms? A) Esophageal spasms typically occur only occasionally B) The contractions associated with esophageal spasms are irregular and uncoordinated C) The spasms can prevent food and liquids from travelling down the esophagus D) Esophageal spasms are a very common condition that affects mostly middle-age adults 76) Which of the following is not a symptom of esophageal spasms? A) Squeezing pain in the chest B) Pain in the stomach C) Difficulty swallowing D) Regurgitation of contents that have been swallowed 77) A person who has esophageal spasms may during acute episodes think he is having: A) B) C) D) A concussion A seizure Angina Amnesia 78) Which of the following statements is false regarding traveler’s diarrhea? A) Traveler’s diarrhea is a stomach and intestinal infection that occurs as a result of unsanitary handling of food B) Traveler’s diarrhea is a bacterial illness that is usually caused by Salmonella C) Traveler’s diarrhea is the most common illness affecting international travelers D) Traveler’s diarrhea is usually self-limiting 79) Sources of traveler’s diarrhea include all of the following except for: A) B) C) D) Local water Salads Peeled fruit Crowded pools 80) Which of the following statements is false regarding bulimia? A) Bulimia nervosa is a condition characterized by recurrent episodes of binge eating that is often accompanied by purging B) Usually a person with bulimia is very thin C) A person with bulimia has extreme concern for body weight and image D) Russell’s sign is associated with bulimia 81) Which of the following statements is false regarding anorexia nervosa and bulimia? A) Anorexia nervosa is characterized by self-starvation, while bulimia is characterized by binge eating most often followed by purging B) Anorexics and bulimics are both extremely concerned about body weight and selfimage C) Anorexics are thin, while bulimics tend to be normal weight D) Anorexia nervosa is most often found in females, while bulimia is most often found in males 82) Obesity increases the risk of a person developing all of the following disorders except for: A) B) C) D) Fatty liver disease Osteoporosis Diabetes Hypertension 83) Gastroparesis a condition that causes: A) The indigestion of carbohydrates in the stomach B) The indigestion of proteins in the stomach C) Delayed gastric emptying of food contents from the stomach into the small intestine D) Rapid gastric emptying of food contents from the stomach into the small intestine Gastrointestinal System answers 1) (D) A person with GERD should avoid mints (relaxes the gastric sphincter), caffeine, chocolate (contains caffeine), alcohol, NSAIDs such as aspirin, and all types of aggravating foods. Acetaminophen (not a gastric irritant) can be safely taken with GERD. 2) (C) Zollinger-Ellison syndrome isn’t associated with GERD. It is a rare syndrome that is usually caused by a gastrinoma, or tumor, that originates from the pancreas, or less commonly, the small intestine. The tumor secretes a hormone known as gastrin, which results in the overproduction of hydrochloric acid in the stomach. Complications of GERD include gastric ulcers, esophagitis, esophageal ulcers, esophageal stricture, Barrett’s esophagus, and tooth decay (source: webmd.com). 3) (C) Common medications prescribed for GERD include proton pump inhibitors, H2 blockers, and antacids. Antispasmodics are not prescribed for GERD. 4) (C) Duodenal ulcers are more common than gastric ulcers. The most common cause of gastric and duodenal ulcers is helicobacter pylori bacteria. This bacterium damages the mucus that protects the stomach and small intestine, allowing for stomach acid to burn through. Chronic NSAID use is another common cause of peptic ulcers. Stress and spicy foods do not cause ulcers, but can make them worse. Duodenal ulcers are often relieved by eating foods; the pain associated with gastric ulcers is made worse through eating food. 5) (B) H. pylori are bacteria that commonly are the cause of gastric or duodenal ulcers. If the ulcers that a patient has is found to have been caused by H. pylori bacteria, then besides the typical acid-lowering or acid-neutralizing medications such as H2 blockers and proton pump inhibitors, the patient will also get prescribed antibiotics to destroy the H. pylori bacteria. For H. pylori negative ulcers, antibiotics will not normally be prescribed. 6) (D) Helicobacter pylori is a type of bacteria that can enter the body and live in the digestive tract. H. pylori are adapted to live in the harsh, acidic environment of the stomach. It is present in over half of the world’s population. It may be spread by unclean food or water. H. pylori are usually harmless but they can cause stomach issues including peptic ulcers and stomach cancer; they’re responsible for the majority of ulcers in the stomach and small intestine. Even though many people are infected with H. pylori bacteria, only about 10% develop a peptic ulcer. H. pylori is not a natural flora present in the body. 7) (C) A person who has a gastric ulcer usually complains of pain right after a meal. This is because the food goes directly into the stomach once eaten. The body secretes hydrochloric acid to break down the food and this acid secreted on top of the gastric ulcers causes pain. With duodenal ulcers, eating usually relieves pain. People with duodenal ulcers usually have pain hours after eating a meal. With duodenal ulcers, a person may also have pain at nighttime. A healthcare provider might suspect gastric ulcers if there is anemia shown in the CBC because gastric ulcers cause internal bleeding from the ulcerated site. A healthcare provider might also suspect gastric ulcers if there is a serology of low iron levels. Iron deficiency anemia can occur with bleeding (such as with ulcers). Folate or vitamin B12 deficiency don’t result from bleeding episodes as does iron deficiency anemia. 8) (C) In acute pancreatitis, amylase, lipase, and trypsin enzymes are all elevated. Glycogen, the storage form of glucose in the liver, is not elevated in acute pancreatitis. 9) (D) Gastric ulcers are not directly associated with acute pancreatitis. Common symptoms of acute pancreatitis include nausea and vomiting, abdominal pain originating in the epigastric region that radiates to the midback, abdominal bloating or swelling, and fever. 10) (D) Diabetes is not a known risk factor for acute pancreatitis. Risk factors for pancreatitis include alcohol abuse, a family history of pancreatitis, high triglyceride levels (high level of fat in the blood), cholelithiasis (which can block the bile duct, which blocks the flow of pancreatic enzymes into the small intestine), cystic fibrosis, smoking cigarettes, pancreatic structural anomalies such as pancreas divisum, and certain medications such as estrogen therapy. 11) (D) Clostridium difficile is a bacterium that can cause symptoms ranging from diarrhea to life-threatening inflammation of the colon (colitis). Clostridium difficile colitis symptoms include 10 to 15 stools a day, fever, nausea, loss of appetite, and abdominal cramping. Red rashes on the groin are not found in clostridium difficile colitis. 12) (B) In order to diagnose C. difficile colitis, a stool assay (by enzyme-linked immunosorbent assay) is done for clostridium difficile bacteria. Serology studies may be done but these will give general, rather than specific, indicators of illness such as elevated white blood cells and inflammatory markers. 13) (C) The most likely scenario or situation for a person becoming ill with clostridium difficile colitis is the person currently on a course of antibiotics or having just completed a course of antibiotics. After antibiotics are taken, this can cause changes in the intestinal flora, killing good bacteria and potentially allowing for harmful bacteria to flourish. 14) (A) Gastroenteritis, also referred to as the stomach flu, is a very common illness and causes inflammation of the lining of the intestines. The main symptoms of gastroenteritis are watery diarrhea and vomiting. The most common type of gastroenteritis is viral gastroenteritis, and the norovirus is the most common cause of serious gastroenteritis and also of foodborne disease outbreaks in the United States. Although not as common, bacteria such as E. coli, salmonella and campylobacter bacteria can also trigger gastroenteritis. Parasites can also cause gastroenteritis but it’s not common; organisms such as giardia and cryptosporidium can be picked up by drinking contaminated water or from contaminated swimming pools. 15) (B) The most common complication of gastroenteritis is dehydration secondary to frequent episodes of diarrhea and vomiting that may occur. 16) (B) Symptoms of gastroenteritis include diarrhea, vomiting, abdominal pain, headache, and fever and chills. 17) (B) The rotavirus is the world’s most common cause of diarrhea in infants and young children. 18) (D) Cullen’s sign is specific to checking for acute hemorrhagic pancreatitis. 19) (C) Cullen’s sign is positive if there is superficial edema and bruising in the subcutaneous fatty tissue around the umbilicus. It is a predictive sign for acute hemorrhagic pancreatitis. Image: Cullen’s sign Credit: Photograph by Herbert L. Fred, MD and Hendrik A. van Dijk, licensed under the Creative Commons Attribution License (CC-BY 2.0) 20) (D) Grey Turner’s sign is bruising and bluish discoloration of the flanks. It is a predictive sign of severe acute pancreatitis. Image: Grey Turner’s sign Credit: Photograph by Herbert L. Fred, MD and Hendrik A. van Dijk, licensed under the Creative Commons Attribution 2.0 Generic license 21) (B) Zollinger-Ellison syndrome is a syndrome in which the body produces too much gastrin. 22) (B) Fasting gastrin levels are entirely specific to Zollinger-Ellison syndrome. ZollingerEllison syndrome produces gastrin levels that are higher than normal. 23) (C) Zollinger-Ellison syndrome is a syndrome in which the body produces too much gastrin. Gastrin is a peptide hormone that stimulates the secretion of gastric acid (hydrochloric acid, or HCL) by the parietal cells of the stomach. This overproduction of gastrin, in turn, leads to the overproduction of hydrochloric acid, which can ulcerate the stomach or small intestine. 24) (B) Serum gastrin levels are considered elevated once they are above 100 pg/mL. Reference levels for gastrin range from 0-100 pg/mL. 25) (C) The definitive test to diagnose celiac disease is a biopsy of the small intestine. Antibody testing, especially for tissue transglutaminase (tTG)-IgA antibodies, is the best first test and can be used as a screening test for celiac disease; however, a biopsy is needed for definitive confirmation. The only solution to celiac disease is a strict, lifelong adherence to a gluten-free diet. The most common symptom associated with a person with celiac disease eating foods containing gluten is diarrhea. Other symptoms include bloating, gas, fatigue, anemia, and osteoporosis. Atypically, there can be neurological implications such as seizures and hallucinations. Many people with celiac disease have no symptoms. Patients diagnosed with celiac disease should be examined for nutritional deficiencies, which can cause health problems such as a low bone density; this is brought on by the fact that celiac disease is a malabsorption syndrome (which can cause nutritional deficiencies). 26) (C) Beer contains barley, which contains gluten. A person with celiac sprue needs to avoid barley, rye, and wheat. 27) (D) Giardiasis is caused by the parasite giardia. Giardiasis is a parasitic illness that causes rampant diarrhea. 28) (C) The most prominent symptom that giardiasis causes is diarrhea. Giardiasis causes rampant diarrhea. 29) (A) The most common way of contracting giardiasis is through contaminated water. Though giardiasis can be transmitted through uncooked food, contaminated water is the most common way giardiasis is transmitted. 30) (C) Giardiasis is diagnosed by obtaining multiple stool samples. This is because once giardia has entered the body, it can be excreted out through the feces intermittently. Intermittently is the reason multiple stool samples need to be collected. It may not be excreted out in one stool sample, so various stool samples collected on separate days are more accurate than a single sample. 31) (A) Proctitis is inflammation of the anus and the lining of the rectum. 32) (C) The most common cause of proctitis is STDs. Gonorrhea, syphilis, herpes, anal warts, and chlamydia are the most common causes of sexually transmitted proctitis. Proctitis is increasingly more common in homosexual men and in people engaging in oral-anal or anal intercourse with many partners. 33) (A) Hypoactive bowel sounds are normal after certain conditions such as during sleep or after a surgery using general anesthesia. During waking hours, hypoactive bowel sounds would be a cause for concern. 34) (B) Decreased or absent bowels would likely cause abdominal bloating, abdominal distention, and constipation. Diarrhea is associated with hyperactive intestinal activity, or hyperactive bowel sounds. 35) (B) With bowel obstruction, high-pitched bowel sounds would likely be heard. Gurgling sounds or clicks are normal sounds heard over the bowels. 36) (C) Appendicitis is least likely to cause projectile vomiting. Projectile vomiting usually occurs when there is a blockage or obstruction somewhere in the GI tract, preventing food from going down its normal course. Since the food can’t progress, the body forces it up (projectile vomiting). Gastric outlet syndrome, superior mesenteric artery syndrome, and pyloric stenosis are all conditions that create obstructions in the GI tract. 37) (C) Appendicitis causes right lower quadrant pain. Pyelonephritis of the right kidney, cholecystitis, and hepatitis all cause right upper quadrant pain. 38) (B) Dumping syndrome is a condition that can develop after surgery to remove all or part of the stomach or after surgery to bypass the stomach to aid in losing weight. Also called rapid gastric emptying, dumping syndrome occurs when food, especially sugar, moves from the stomach into the small intestines too quickly. Most people with dumping syndrome develop signs and symptoms, such as abdominal cramps and diarrhea, 10 to 30 minutes after eating. Other people have symptoms 1-3 hours after eating, and still others have both early and late symptoms. Generally, the effects of dumping syndrome can be prevented by changing one’s diet after the surgery. Changes include eating smaller meals and limiting high-sugar foods (source: mayoclinic.org). 39) (D) Diverticulosis is a condition characterized by diverticula, pouches that form in the wall of the colon. When these diverticula become inflamed or infected, the condition is called diverticulitis. The cause of diverticulosis is unknown, but it is believed in the medical community that a low-fiber plays a role. Without fiber to add bulk to the stool, the colon has to work harder than normal to push the stool forward. The pressure from this may cause pouches to form in weak spots along the colon. Diverticulosis is generally not a painful condition, as the diverticula aren’t inflamed or infected. Diverticulitis can be a painful condition. 40) (B) Symptoms of diverticulitis include belly pain, usually in the lower left quadrant (LLQ), that is sometimes worse when a person moves; this is the most common symptom. This pain may be constant and persist for several days. Other symptoms can include fever and chills, bloating and gas, diarrhea or constipation, nausea and sometimes vomiting, and not feeling like eating (anorexia). 41) (D) Diverticula are common, especially after the age of 40. They are found most often in the lower part of the large intestine (colon). They seldom cause problems. The cause of diverticula is unknown. Diverticula usually develop when naturally weak places in the colon give way under pressure. This causes marble-sized pouches to protrude through the colon wall. The cause of diverticulosis is unknown, but it is believed in the medical community that a low-fiber plays a role. Without fiber to add bulk to the stool, the colon has to work harder than normal to push the stool forward. The pressure from this may cause pouches to form in weak spots along the colon. 42) (A) Aging (incidence of diverticulitis increases with age), obesity (being obese increases the odds of developing diverticulitis), smoking (people who smoke cigarettes have a higher risk than nonsmokers), a lack of exercise (exercise increases peristalsis in the bowels), a diet high in animal fat and low in fiber, and certain medications such as steroids, opiates, and NSAIDs all put a person at higher risk for developing diverticulitis. 43) (A) A high-fiber diet is recommended for diverticulitis. High-fiber foods such as fresh fruits and vegetables soften waste material and help it pass more quickly through the colon. A diet high in animal fat and low in fiber is linked to an increased risk for diverticulitis. Image: Diverticula 44) (B) Pyelonephritis isn’t a complication associated with diverticulitis. Complications of diverticulitis include abscess formation (which occurs when pus collects in the pouch), a blockage in the colon or small intestine caused by scarring, a fistula (abnormal passageway) between sections of the bowel and bladder, and peritonitis, which can occur if the diverticula rupture and the infected contents spill into the abdominal cavity. About 25% of people with diverticulitis develop complications. 45) (C) Treatment for uncomplicated diverticulitis include antibiotics (to treat the infection), a liquid diet for a few days while the bowel heals before gradually returning to solid food, an OTC pain reliever such as acetaminophen, and rest. Motrin would not be used because it is an NSAID and can irritate the bowels. Instead a non-NSAID analgesic such as acetaminophen would be used. For complicated diverticulitis, a person may need intravenous antibiotics and insertion of a tube to drain an abscess, if one has formed. Depending on the complication, surgery may be needed; for example, if a segment of the colon is very diseased, a bowel resection may be need to be done to remove this diseased portion and reconnect the healthy segments (an anastomosis). If so much of the colon has been damaged, an anastomosis may not be able to be done; instead the surgeon will perform a colostomy by creating an opening (called a stoma) in the abdominal wall connected to a healthy part of the colon and waste will pass into the colostomy bag. Once the inflammation has been eased, the colostomy may be reversed and the bowel reconnected. 46) (C) Gastritis is inflammation of the lining of the stomach. Gastritis can occur suddenly (acutely) or gradually (chronically). If left untreated, gastritis can lead to severe blood loss and an increased risk for stomach cancer. 47) (A) Causes or contributors to gastritis include excessive alcohol use, stress, the use of certain medications such NSAIDs, bile reflux, and infections. Crohn’s disease is a disease of the intestines and is not associated with gastritis. 48) (B) Though vomiting is a common symptom of gastritis, the vomiting would not be projectile in nature. Symptoms of gastritis include nausea, vomiting, recurrent upset stomach, abdominal pain, abdominal bloating, indigestion, burning or gnawing feeling in the stomach between meals or at night, hiccups, loss of appetite, and black, tarry stools. 49) (B) NSAIDs would not be prescribed for someone suffering from gastritis because NSAIDs are a stomach irritant. For pain for those suffering from gastritis, a non-NSAID would be taken such as acetaminophen. Antacids, proton pump inhibitors, and H2 blockers may be prescribed because they reduce or neutralize stomach acid. 50) (C) Irritable bowel syndrome can cause a person to have diarrhea or constipation. Irritable bowel syndrome is a common disorder that affects the large intestine (colon). Irritable bowel syndrome can cause cramping, abdominal pain, bloating, gas, diarrhea, and constipation. Unlike ulcerative colitis and Crohn’s disease, irritable bowel syndrome does not cause changes in the bowel tissue and is not an inflammatory condition, though it may produce discomfort. Irritable bowel syndrome does not increase a person’s risk for colorectal cancer. 51) (C) Irritable bowel syndrome is a chronic disease. Females tend have IBS at about twice the incidence as men. Irritable bowel syndrome tends to occur in people under the age of 45, so it mostly affects the younger population. Diagnosing IBS depends largely on a complete medical history and physical exam. Because there are usually no physical signs to definitively diagnose IBS, diagnosis is often a process of ruling out other conditions. Researchers have developed two sets of diagnostic criteria for IBS and other functional gastrointestinal disorders in which the bowel appears normal but doesn’t function normally. Both criteria are based on the symptoms a person is experiencing after other conditions have been ruled out. One is the Rome criteria; according to the Rome criteria, a person must have abdominal pain and discomfort lasting at least three days a month in the last three months, associated with two or more of the following: improvement with defecation, altered frequency of stool or altered consistency of stool. The Manning criteria focus on pain relieved by defecation, having incomplete bowel movements, mucus in the stool, and changes in stool consistency; the more symptoms present, the greater the likelihood of it being IBS. The practitioner may do additional testing on top of this. 52) (C) The signs and symptoms of irritable bowel syndrome can vary widely from person to person and often resemble that of other conditions. This is why it’s called a syndrome; it can produce a widely varying set of symptoms for different people. Common symptoms of irritable bowel syndrome include abdominal pain or cramping, a bloated feeling, gas, diarrhea or constipation (sometimes alternating bouts of constipation and diarrhea), and mucus in the stool. Blood in the stool would not be a typical symptom of IBS and can indicate a more serious condition. 53) (D) The cause of IBS is not known exactly, but a variety of factors play a role, such as stronger-than-normal contractions in the intestines and abnormalities in the GI nervous system. Episodes of IBS or aggravation of IBS is believed to linked to certain triggers, which vary from person to person. Common triggers include food (common ones include chocolate, spices, fats, milk, carbonated beverages, alcohol), stress (during periods of high stress, symptoms are either worse or more frequent), hormones (the higher incidence in women is believed to be due to hormones and many women find that symptoms are worse during or around their menstrual periods), and other illnesses (such as gastroenteritis). Because a common symptom of IBS is constipation, IBS can aggravate (make worse) hemorrhoids. Steroids typically are not used to treat IBS, as IBS is not an inflammatory condition. Because it’s not clear what causes irritable bowel syndrome, treatment focuses on relief of symptoms. Fiber supplements such as psyllium husk may be given to control constipation, antidiarrheals may be given to help control diarrhea, and anticholinergic and antispasmodic medications may be given to relieve painful bowel spasms. 54) (A) Ulcerative colitis is an inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in the digestive tract. Ulcerative colitis affects the innermost lining of the large intestine (colon) and rectum. Symptoms usually develop over time, rather than suddenly. Ulcerative colitis can be debilitating and sometimes can lead to life-threatening complications such as peritonitis. While it has no known cure, treatment can greatly reduce signs and symptoms of the disease and even bring about long-term remission (source: mayoclinic.org). 55) (D) Ulcerative colitis symptoms can vary, depending on the severity of inflammation and where it occurs. Therefore, doctors often classify ulcerative colitis according to its location. Symptoms of ulcerative colitis include diarrhea (often with blood or pus), abdominal pain and cramping, rectal pain, rectal bleeding (passing a small amount of blood with stool), urgency to defecate, inability to defecate despite urgency, weight loss, fatigue and fever. Most people with ulcerative colitis have mild to moderate symptoms. The course of ulcerative colitis may vary, with some people having long periods of remission (source: mayoclinic.org). 56) (C) Of all the medications, laxatives would least likely be prescribed for ulcerative colitis. This is because though ulcerative colitis can cause constipation, it usually causes diarrhea. Therefore, antidiarrheals are much more likely to be prescribed. Anti-inflammatory drugs are often the first step in the treatment of inflammatory bowel disease. Anti-inflammatory drugs such as sulfasalazine and corticosteroids are used to reduce inflammation. Immune system suppressors may also be prescribed, as they reduce inflammation by suppressing the immune system response that starts the process. Other drugs that may be used for ulcerative colitis are antibiotics (if an infection and fever is present), pain relievers, and iron supplements (if there is chronic intestinal bleeding) (source: mayoclinic.org). 57) (B) Besides ulcerative colitis, the other type of inflammatory bowel disease is Crohn’s disease. The symptoms of Crohn’s disease are similar to that of ulcerative colitis, but the areas affected in the gastrointestinal (GI) tract are different. Crohn’s disease most commonly affects the end of the small bowel (the ileum) and the beginning of the colon, but it may affect any part of the gastrointestinal (GI) tract, from the mouth to the anus. Ulcerative colitis is limited to the colon, also called the large intestine. Crohn’s disease can also affect the entire thickness of the bowel wall, while ulcerative colitis only involves the innermost lining of the colon. Finally, in Crohn’s disease, the inflammation of the intestine can “skip”- leaving normal areas in between patches of diseased intestine. In ulcerative colitis, this does not occur (source: ccfa.org). 58) (A) Symptoms of peritonitis include fever, nausea and vomiting, abdominal distention, decreased or absent bowel sounds, low urine output, thirst, and inability to pass stool or gas. 59) (C) Renal failure would be the least likely to cause peritonitis. Rupture of the diverticula in diverticulitis, peritoneal dialysis, and rupture of the appendix in appendicitis are all risk factors for peritonitis. An infection may occur during peritoneal dialysis due to unclean surroundings, poor hygiene, or contaminated equipment; symptoms may include cloudy dialysis fluid. Peritonitis is common among people undergoing peritoneal dialysis therapy. Other risk factors include cirrhosis, Crohn’s disease, stomach ulcers, pancreatitis, and a history of peritonitis. 60) (C) If peritonitis is left untreated, it can lead to severe, potentially life-threatening infection throughout the body (sepsis). Treatment usually involves antibiotics and in some cases surgery depending on the underlying condition. 61) (B) Salmonella infection is normally transmitted by turtles and other amphibians. 62) (B) Barrett’s esophagus is a precancer for esophageal cancer. 63) (D) Barrett’s esophagus is diagnosed via an upper endoscopy with biopsy. The diagnosis of Barrett's esophagus rests upon seeing (at endoscopy) a pink esophageal lining that extends a short distance (usually less than 2.5 inches) up the esophagus from the gastroesophageal junction and finding intestinal type cells (goblet cells) on biopsy of the lining (source: medicinenet.com). 64) (C) Weight loss of at least 15% from the ideal body weight is required for a diagnosis of anorexia nervosa. Anorexia nervosa is diagnosed when a person drops to 85% or less of the ideal body weight. 65) (B) The majority of people with anorexia nervosa are between the ages of 13 and 20, with 17 and 18 being the peak ages for the condition. 66) (D) A person with anorexia nervosa is likely to have irregular periods or amenorrhea (no menstrual cycle at all) rather than dysmenorrhea, which are painful menstrual cycles. Other complications of anorexia nervosa include cardiac complications including arrhythmias and heart failure, anemia, osteoporosis, kidney problems, electrolyte imbalances, gastrointestinal problems such as constipation, and depression (source: mayoclinic.org). 67) (B) Murphy’s sign is a sign of gallbladder disease consisting of pain on taking a deep breath when the examiner’s fingers are on the approximate location of the gallbladder. 68) (B) An atonic colon is also called lazy colon or atonic bowel or colon stasis. Atonic colon occurs when there is a lack of normal muscle tone or strength in the colon. It can result in chronic constipation. 69) (A) The most common symptom of an atonic colon is constipation. Besides constipation, a person may also experience stomach pains, bloating, nausea, vomiting and fever. 70) (C) An atonic colon is caused by a loss of muscle tone. This results in colon stasis and constipation. 71) (D) An atonic colon is linked to the chronic use of laxatives. Laxatives work by stimulating the bowel muscles with irritants. However, when they are used repeatedly, the muscles build up a tolerance and larger quantities of the irritants are needed to get the same effect. This causes low muscle tone, which can result in an atonic colon. 72) (D) Oliguria is defined as urinary output less than 400 mL/day (source: emedicine.medscape.com). 73) (C) Amebiasis is a disease caused by the one-celled parasite Entamoeba histolytica. It is most common in people who live in tropical areas with poor sanitary conditions. In the United States, amebiasis is most common in people who have traveled to tropical places that have poor sanitary conditions, immigrants from tropical countries that have poor sanitary conditions, people who live in institutions that have poor sanitary conditions, and men who have sex with men. Only about 10% to 20% of people who are infected with E. histolytica become sick from infection. The symptoms are often quite mild and can include loose stools, stomach pain, and stomach cramping. Amebiasis is diagnosed through stool sample examination. Because E. histolytica is not always found in every stool sample, a person may have to submit several stool samples from several different days (source: cdc.gov). 74) (D) Gastroenteritis is also referred to as the stomach flu. 75) (D) Esophageal spasms are painful contractions that occur within the esophagus that are irregular, uncoordinated and sometimes powerful (in healthy conditions, contractions are regular and coordinated). Esophageal spasms typically occur only occasionally and may not need treatment. At times, the spasms are frequent and can prevent food and liquids from travelling down the esophagus. Esophageal spasms is a rare condition that tends to occur in people between the ages of 60 and 80 years old. 76) (B) Esophageal spasms are not associated with stomach pain. Symptoms of esophageal spasms include difficulty swallowing specific foods or drinks (such as red wine or extremely hot or cold liquids), the feeling that an object is stuck in the throat, and regurgitation of contents swallowed. 77) (C) A person experiencing esophageal spasms may mistake it for angina (chest pain), since esophageal spasms can cause a squeezing pain in the chest area. The pain is often intense. 78) (B) Traveler's diarrhea is a stomach and intestinal infection that occurs as a result of unsanitary handling of food. Traveler’s diarrhea is the most common illness affecting international travelers. Areas where there are the highest risks of contracting traveler's diarrhea include the developing countries of Africa, the Middle East, Latin America, and Asia. The risk of infection varies depending on the type of eating establishment visited -- from fairly low risk in private homes to high risk in food from street vendors. A person typically develops traveler's diarrhea after ingesting food or water that's contaminated with organisms from feces. These organisms are infectious agents — including various bacteria, viruses and parasites — that enter the digestive tract and overpower a person’s defense mechanisms, resulting in signs and symptoms of traveler's diarrhea. The most common culprit is E. coli bacteria. Typical symptoms include abrupt onset of diarrhea, fever, nausea and vomiting, bloating, malaise, cramps, and loss of appetite. Because of the loss of fluid from diarrhea, dehydration can be a complication of traveler’s diarrhea. Traveler's diarrhea is usually self-limiting and goes away on its own within a few days (usually lasts 3 to 7 days) and is rarely life threatening (source: webmd.com & mayoclinic.org). 79) (C) Sources of traveler’s diarrhea include local water, salads, fruits (unless peeled), and crowded pools. Peeled fruit would unlikely be a source of traveler’s diarrhea. 80) (B) Bulimia nervosa is a condition characterized by recurrent episodes of binge eating, most often accompanied by purging such as through inducing vomiting, taking diuretics, or laxatives. Usually the person is of normal weight. There are few outward signs of bulimia; behavior usually occurs in secret. Therefore, behavior may go unnoticed for years. Signs and symptoms of bulimia may include sneaking food, making excuses to use the bathroom after meals, eating large amounts of food on the spur of the moment, taking laxatives, vomiting and/or over-exercising to “purge” food, extreme concern with body weight and image, wearing away of the enamel on teeth (due to vomiting), and Russell’s sign (which are teeth marks on the knuckles from selfinducing vomiting). Image: Russell’s sign seen in bulimia nervosa Credit: Photograph by User: Kyukyusha, released into the public domain 81) (D) Anorexia nervosa is characterized by self-starvation, while bulimia is characterized by binge eating most often followed by purging. Anorexics and bulimics are both extremely concerned about body weight and self-image. Anorexics are thin (less than 85% of ideal body weight), while bulimics are most often normal weight. Anorexics relentlessly pursue thinness. Anorexia nervosa and bulimia nervosa are most often found in females. 82) (B) Obesity increases the risk of a person developing fatty liver disease, diabetes, and hypertension. Obesity does not increase the risk of developing osteoporosis. 83) (C) Gastroparesis, also called delayed gastric emptying, is a disorder that slows or stops the movement of food from the stomach into the small intestine. Normally, the muscles of the stomach, which are controlled by the vagus nerve, contract to break up food and move it through the gastrointestinal (GI) tract. The GI tract is a series of hollow organs joined in a long, twisting tube from the mouth to the anus. The movement of muscles in the GI tract, along with the release of hormones and enzymes, allows for the digestion of food. Gastroparesis can occur when the vagus nerve is damaged by illness or injury, which causes the stomach muscles to stop working normally. Food then moves slowly from the stomach to the small intestine or stops moving altogether. Most people diagnosed with gastroparesis have idiopathic gastroparesis, which means a health care provider cannot identify the cause. The most common symptoms of gastroparesis are nausea, a feeling of fullness after eating only a small amount of food, and vomiting undigested food—sometimes several hours after a meal (source: niddk.nih.gov). Chapter 7- Liver, Kidneys, Gallbladder, Appendix, Intestines, and Rectum 1) Nonalcoholic fatty liver disease is caused due to: A) Alcohol poisoning B) Triglyceride fat deposits in the hepatocytes of the liver C) A viral infection D) A bacterial infection 2) Which of the following is false regarding fatty liver disease (steatosis)? A) Fatty liver disease may cause a liver that is smaller than normal B) A person with fatty liver disease may be asymptomatic C) If fat makes up more than 5-10% of the liver’s weight, this may be indicative of fatty liver disease D) Fatty liver disease increases the risk of a person developing cirrhosis 3) What is the definitive diagnostic test for fatty liver disease? A) ALT serum levels B) Enlargement and bulging of the liver seen on an MRI scan C) Liver biopsy D) Elevated levels of serum bilirubin 4) What is the most common hepatitis infection? A) B) C) D) Hepatitis A Hepatitis B Hepatitis C Hepatitis D 5) How is hepatitis A most commonly transmitted? A) Through the fecal oral route B) Through sexual transmission C) Through blood exposure D) Through droplet exposure 6) Which of the following vaccines is used for hepatitis A? A) B) C) D) Hiberix Gardasil Havrix Tenivac 7) All of the following can be causes or contributors to hepatitis except for: A) B) C) D) Excessive alcohol intake High-protein diet Viral infection Hepatotoxic drugs 8) Which of the following statements is false regarding hepatitis A? A) Presence of the hepatitis A IgG antibodies indicates immunity from the hepatitis A virus B) Presence of the hepatitis A IgM antibodies indicates active infection of hepatitis A virus C) Hepatitis A vaccination causes production of IgM antibodies D) In most cases of hepatitis A, the liver heals within 6 months with no lasting damage 9) Which of the following is not a transmission method of hepatitis C? A) B) C) D) IV drug use Breastfeeding Blood transfusion Sexual intercourse 10) A hepatitis C antibody test checks to see: A) If a person has ever been exposed to the hepatitis C virus B) If a person has active hepatitis C infection C) How much hepatitis C viral load is present in a person’s body D) How much hepatitis C antigens are present on red blood cells 11) A patient is tested for hepatitis C antibody and tests positive for antibodies. What should the practitioner do next? A) Diagnose the patient with hepatitis C and start treatment B) Repeat the hepatitis C antibody test C) Order the hepatitis C RNA test D) Order the ALT and AST labs 12) A person has a positive hepatitis C antibody test and a negative HCV RNA. Which is true? A) The person has never been exposed to the hepatitis C virus B) The person has been exposed to the hepatitis C virus but has been cured of the viral illness C) The person has been exposed to the hepatitis C virus and the disease is moderately destroying the liver D) The person has been exposed to the hepatitis C virus and the disease is aggressively destroying the liver 13) A hepatitis C antibody test can produce a false negative if: A) The person has coexisting hepatitis B infection B) The person has cirrhosis C) The person has recently contracted the hepatitis C virus in the last 6 months D) The person regularly receives blood transfusions 14) Which of the following statements is false regarding hepatitis C? A) A positive hepatitis C antibody test means the person has been infected with hepatitis C virus at some point in his or her life B) Once a person has been infected, he/she will always have antibodies present in the blood C) A person’s immune system can clear the hepatitis C virus without any treatment D) The hepatitis C antibody test is also referred to as the polymerase chain reaction test (PCR) 15) Which type of testing checks to see how a person with hepatitis C is responding to treatment? A) B) C) D) Anti-HCV antibody test HCV quantitative test HCV viral genotyping Alkaline phosphatase levels 16) What is the screening test for active hepatitis B infection? A) B) C) D) Hepatitis B surface antigen Hepatitis B surface antibody Liver biopsy Serum ALT levels 17) Which of the following statements is false regarding the hepatitis B surface antibody? A) Presence of the hepatitis B surface antibody indicates immunity from hepatitis B B) Presence of the hepatitis B surface antibody may be due to a past infection that has resolved or hepatitis B vaccination C) The hepatitis B surface antibody can determine active infection D) The body forms the hepatitis B surface antibody due to being exposed to the hepatitis B surface antigen 18) Which of the following antibodies are produced in response to the hepatitis B vaccination? A) Hepatitis B surface antibodies B) Hepatitis B core antibodies C) Hepatitis B e antibodies D) Hepatitis B surface antibodies and hepatitis B core antibodies 19) Which statement is false regarding the hepatitis B core antibody (anti-HBc)? A) Hepatitis B core antibody appears at the onset of symptoms in acute hepatitis B and persists for life B) The presence of hepatitis B core antibody (anti-HBc) indicates previous or ongoing infection with hepatitis B virus in an undefined time frame C) Hepatitis B core antibody will always be present if a person has ever had a hepatitis B infection D) Hepatitis B core antibody is only present for acute cases of hepatitis B infection 20) Presence of the hepatitis B e antigen (HBeAg) indicates: A) The person does not have hepatitis B B) The person’s hepatitis B is mild and decreasing C) The person has recovered from the hepatitis B infection D) The virus is replicating and the infected person has high levels of the hepatitis B virus 21) The IgM antibody to the hepatitis B core antigen (IgM anti-HBc) indicates: A) An acute hepatitis B infection B) A chronic hepatitis B infection C) That a previous hepatitis B infection has resolved D) That a person has been successfully vaccinated against the hepatitis B infection 22) Which of the following indicates that a person is susceptible to the hepatitis B infection? A) HBsAg negative, anti-HBc negative, anti-HBs negative B) HBsAg negative, anti-HBc negative, anti-HBs positive C) HBsAg negative, anti-HBc positive, anti-HBs positive D) HBsAg positive, anti-HBc positive, anti-HBs positive 23) A negative HBsAg, a positive anti-HBc, and a positive anti-HBs would indicate: A) Susceptibility to the hepatitis B infection B) Immunity to hepatitis B due to natural infection C) Immunity to hepatitis B due to vaccination D) Acute hepatitis B infection 24) Which of the following would indicate that a person is chronically infected with hepatitis B? A) Negative HBsAg, negative anti-HBc, and positive anti-HBs B) Negative HBsAg, positive anti-HBc, and positive anti-HBs C) Positive HBsAg, positive anti-HBc, positive IgM anti-HBc, and negative anti-HBs D) Positive HBsAg, positive anti-HBc, negative IgM anti-HBc, and negative anti-HBs 25) All of the following statements are true about hepatitis D except: A) A person must have hepatitis B in order to contract hepatitis D B) Hepatitis D can be acute or chronic C) Infection with both hepatitis B and D increases a person’s risk for cirrhosis D) Hepatitis D is very common in the United States 26) How are the AST and ALT values during acute hepatitis infection? A) ALT and AST levels decrease during the acute phase of hepatitis B) ALT and AST levels stay the same as normal C) ALT and AST levels can go as high as 3x the normal levels during the acute phase of hepatitis D) ALT and AST levels can be elevated up to 10x the normal levels during the acute phase of hepatitis 27) All of the following are symptoms of acute drug-induced hepatitis except for: A) Jaundice B) Abdominal tenderness in the left upper quadrant C) Fatigue D) Anorexia 28) For which hepatitis is there no vaccine for? A) B) C) D) Hepatitis A Hepatitis B Hepatitis C Hepatitis D 29) Which of the following statements is false regarding fulminant hepatitis? A) People who have fulminant hepatitis typically develop symptoms seen in viral hepatitis and then rapidly develop severe, often life-threatening liver failure B) Symptoms of fulminant hepatitis include hepatic encephalopathy and blood-clotting defects C) Only hepatitis B and C infections can lead to fulminant hepatitis D) For some people, a liver transplant is the only lifesaving option for fulminant hepatitis 30) Where is the gallbladder located? A) Right upper quadrant of the abdomen B) Left upper quadrant of the abdomen C) Right lower quadrant of the abdomen D) Left lower quadrant of the abdomen 31) Which duct is directly connected to the gallbladder? A) B) C) D) The cystic duct The common bile duct The right hepatic duct The left hepatic duct 32) Bile is: A) Made in the liver and stored in the gallbladder B) Made in the gallbladder and stored in the liver C) Both made in the liver and stored in the liver D) Both made in the gallbladder and stored in the gallbladder 33) What is the most common reason for biliary colic? A) B) C) D) Inflamed bile duct Pancreatitis Gallstones Nephrolithiasis 34) Biliary colic is most likely to cause pain in the: A) Upper left quadrant B) Upper right quadrant C) Lower left quadrant D) Lower right quadrant 35) When would symptoms of biliary colic most likely be the most severe? A) B) C) D) On an empty stomach At night during sleep After a fatty meal After drinking a very cold beverage 36) What is true regarding the anatomical position of the kidneys? A) The left and right kidneys are both at the same level B) The right kidney is lower than the left kidney due to displacement by the liver C) The left kidney is lower than the right kidney due to displacement by the liver D) The left kidney is lower than the right kidney due to displacement by the gallbladder 37) What is the most specific indicator of kidney function? A) B) C) D) Serum creatinine levels Blood urea nitrogen Urine output Sodium levels 38) How many nephrons does each kidney contain? A) B) C) D) 100 1,000 10,000 1,000,000 39) What is the glomerular filtration rate? A) The amount of fluid that passes through the kidneys in a given unit of time B) The amount of fluid that is filtered by the glomeruli in the kidneys in a given unit of time C) The amount of glucose that passes through the kidneys in a given unit of time D) The amount of sodium that passes through the kidneys in a given unit of time 40) What is considered a normal glomerular filtration rate in a healthy individual? A) B) C) D) 60 mL/min or greater 70 mL/min or greater 80 mL/min or greater 90mL/min or greater 41) What glomerular filtration rate (GFR) would constitute stage 5 chronic kidney disease? A) B) C) D) Less than 60 mL/min Less than 50 mL/min Less than 30 mL/min Less than 15 mL/min 42) What is the number one cause of chronic renal failure in the United States? A) B) C) D) Hypertension Diabetes Viral illness Pyelonephritis 43) All of the following are symptoms associated with renal failure except for: A) B) C) D) Nausea and lethargy Decreased urinary output Rhabdomyolysis Edema and weight gain 44) The majority of kidney stones are made up of: A) Calcium oxalate stones B) Struvite stones C) Uric acid stones D) Cystine stones 45) What is the best and most commonly used way of finding the size and location of kidney stones? A) B) C) D) MRI Barium enema Renal ultrasound Manual palpation 46) Which of the following statements is false regarding renal artery stenosis? A) Renal artery stenosis is a condition that can lead to progressive worsening hypotension B) Renal artery stenosis is seen most often in older adults C) Renal artery stenosis can lead to kidney damage and kidney failure D) Most cases of renal artery stenosis are asymptomatic 47) Renal artery stenosis is most often caused by: A) B) C) D) Hypertension Diabetes Chronic kidney disease Atherosclerosis 48) What is polycystic kidney disease? A) A disease in which the kidneys become scarred and fibrotic B) A disease in which the kidneys bleed often due to superficial vessels breaking on the kidneys C) A disease in which clusters of cysts develop within the kidneys D) A disease in which the kidneys shrink substantially and are less able to filter fluids 49) Polycystic kidney disease is: A) Inherited B) Acquired through years of uncontrolled diabetes C) Acquired through years of uncontrolled hypertension D) Acquired through years of smoking 50) Common complications of polycystic kidney disease include all of the following except: A) B) C) D) Infective endocarditis Kidney failure Hypertension Kidney stones 51) All of the following are true about pyelonephritis except: A) Pyelonephritis is an infection of the kidney B) Pyelonephritis is caused the majority of times by E. coli C) Pyelonephritis is uncommon during pregnancy D) Pyelonephritis is usually caused by an untreated UTI or bladder infection 52) Which of the following is not a function of the spleen? A) The spleen sequesters and recycles old red blood cells B) Platelets are stored in the spleen C) White blood cells in the spleen screen the blood flowing through D) The spleen converts ammonia into urea 53) Splenic injury such as splenic rupture most often occurs due to: A) B) C) D) Infection Renal failure Blunt trauma Dehydration 54) Which statement is true regarding the spleen? A) A person can live without a spleen without any health consequences at all B) A person will die in a matter of days without a spleen C) A person can live without a spleen, though he or she may have poor blood sugar control D) A person can live without a spleen, but this puts the person at risk for possible lifethreatening infections 55) Which of the following statements is false regarding a splenic injury? A) The spleen is the most frequent organ to be damaged in blunt trauma injuries involving the abdomen, regardless of age B) A ruptured spleen is an emergency medical condition C) A ruptured spleen poses a risk of internal hemorrhage D) A ruptured spleen is not life-threatening 56) Which of the following is not a risk factor for developing gallstones? A) B) C) D) Female gender Obesity Being pregnant High-carbohydrate diet 57) What is the main risk factor for developing cholecystitis? A) B) C) D) Gallstones Kidney stones Hypertension Diabetes 58) What is the most common complication of acute cholecystitis? A) B) C) D) Acute gastric ulcers Gangrene of the gallbladder Intussusception Crohn’s disease 59) All of the following signs are specific to appendicitis except for: A) Psoas sign B) Obturator sign C) Murphy’s sign D) Rovsing’s test 60) An examiner wants to check whether a patient may have acute appendicitis. She deeply palpates the left lower quadrant of the patient’s abdomen which results in referred pain to the right lower quadrant. This test is characteristic of: A) B) C) D) Obturator sign Rovsing’s sign Markle test Murphy’s sign 61) What is rhabdomyolysis? A) An acute breakdown of skeletal muscle in the body B) An acute breakdown of red blood cells in the body C) An acute breakdown of bones within the body D) An acute breakdown of platelets in the body 62) Symptoms of rhabdomyolysis include all of the following except: A) B) C) D) Muscle pain and aches Urinary frequency Dark urine Generalized weakness 63) What is the most sensitive and reliable test for diagnosing rhabdomyolysis? A) B) C) D) Serum myoglobin levels Serum creatine kinase levels Lactate dehydrogenase Potassium levels 64) A nurse practitioner would expect to find all of the following in the urinalysis of a person with rhabdomyolysis except: A) B) C) D) Albuminuria Myoglobinuria Bacteriuria Acidic pH 65) Which of the following is the most common potential complication of rhabdomyolysis? A) B) C) D) Liver failure Kidney failure Heart failure Prostate failure 66) Which of the following may be a sign that a patient taking statins is suffering from rhabdomyolysis? A) B) C) D) Muscle pain with cloudy urine Muscle pain with dark-colored urine Muscle pain with hematemesis Muscle pain with frequent coughing 67) An obese woman comes into a clinic complaining of vague right upper quadrant pain and general malaise. Her hepatitis A, B, and C profile are negative. Her ALT and AST levels are slightly elevated. Which of the following is the likely diagnosis? A) B) C) D) Fatty Liver Hepatitis Pancreatitis Diverticulitis 68) All of the following statements are true regarding urinary tract infections (UTIs) except: A) UTIs are more common in women than in men B) The highest incidence of UTIs in women is during the nonreproductive years C) UTIs are caused the majority of the times by E. coli D) Diabetes is a risk factor for developing UTIs 69) All of the following are risk factors for developing UTIs except for: A) B) C) D) Female gender Catheterization Hypertension Pregnancy 70) Encopresis is sometimes called: A) B) C) D) Urinary incontinence Fecal incontinence Uncontrolled hypertension Uncontrolled sneezing 71) The cause of encopresis is associated with: A) B) C) D) Emotional or psychiatric disorder Digestive disorder Urethral disorder Rectal disorder 72) The feeling of needing to pass stools, even though the bowel is empty, is termed: A) B) C) D) Tenesmus Incontinence Dysuria Dystonia 73) Which of the following demographic groups would be most at risk for hepatitis A? A) Travelers to underdeveloped countries B) Farmers C) Campers D) Healthcare workers 74) Which of the following statements is false regarding anal fissures? A) An anal fissure is tear in the lining of the lower rectum that causes no pain B) Anal fissure generally doesn’t lead to further serious health problems C) Anal fissures are caused by injury or trauma to the anal canal D) Anal fissures affect people of all ages Liver, Kidneys, Gallbladder, Appendix, the Intestines, and Rectum answers 1) (B) Nonalcoholic fatty liver disease is caused due to triglyceride fat deposits in the hepatocytes in the liver. Experts don't know exactly why some people accumulate fat in the liver while others do not. 2) (A) Fatty liver disease is a subtle condition. Fatty liver disease may cause a liver that is a little larger than normal which a practitioner may notice during a physical examination, which could raise suspicion of this condition. If fat makes up more than 5-10% of the liver’s weight, this may be indicative of fatty liver. A person may have no symptoms at first. As time goes on, often years or even decades, a person may develop problems such as fatigue, pain in the right upper quadrant, loss of weight or appetite, weakness, nausea, confusion, poor judgment, or trouble with concentration. The main complication of nonalcoholic fatty liver disease is cirrhosis, which is late-stage scarring (fibrosis) of the liver (source: webmd.com and mayoclinic.org). 3) (C) A liver biopsy is the definitive test to diagnose fatty liver disease. 4) (B) Hepatitis B is the most common type of hepatitis infection. Hepatitis B is the most common serious liver infection in the world. 5) (A) Hepatitis A is transmitted most commonly through the fecal oral route. 6) (C) Havrix is a vaccine used for hepatitis A produced by GlaxoSmithKline. The other vaccine currently available for hepatitis A is Vaqta produced by Merck. Hiberix is a vaccine for Haemophilus influenza type B. Gardasil is a vaccine for human papillomavirus. Tenivac is a vaccine used for tetanus. 7) (B) Excessive alcohol intake, hepatotoxic drugs, and a viral infection are possible causes or contributors to hepatitis. A high-protein diet isn’t associated with hepatitis. 8) (C) The presence of the hepatitis A IgM antibodies indicates acute hepatitis A infection. The patient, in this case, is contagious and the hepatitis A infection is present. There is no immunity established yet by the body. The presence of the hepatitis A IgG antibodies indicates that immunity to hepatitis A has been established. In this case, the person is not infectious or contagious. Hepatitis A vaccination produces immunity to hepatitis A, so it produces hepatitis A IgG antibodies. The hepatitis A vaccination (Havrix) is an inactivated vaccine; therefore, it does not cause acute hepatitis A infection. 9) (B) Hepatitis C cannot be transmitted through breastfeeding. IV drug use (blood exchange), blood transfusion, and sexual intercourse can all transmit the hepatitis C virus (source: cdc.gov). 10) (A) The hepatitis C antibody test checks to see if a person has ever been exposed to the hepatitis C virus. If the hepatitis C antibody test is positive, this means that the person has been exposed to the hepatitis C virus and has made antibodies. It cannot determine if the virus is latent or active. To determine if a patient is actively or chronically infected, the person should be tested for hepatitis C RNA (source: hepatitis.va.gov). 11) (C) If a person tests positive for the hepatitis C antibody, this means that the person has been exposed to the hepatitis C virus. However, this test does not tell if the person is actively infected with hepatitis C. To check to see if the person is actively, or chronically, infected, the practitioner should order a hepatitis C RNA test. If the hepatitis C is undetectable, the person does not have active hepatitis C infection. 12) (B) A person with a positive hepatitis C antibody test and a negative HCV RNA test has been exposed to the hepatitis C virus but has been cured of the viral illness either by their own immune system or through treatment. 13) (C) A hepatitis C antibody test can produce a false negative if the person has recently contracted the hepatitis C virus in the last 6 months. If a person believes he or she may have been exposed to hepatitis C in the last 6 months, the person will need to be tested again. This is because it takes the body’s immune system time to produce antibodies to the hepatitis C virus. This is the same case for the HIV virus. 14) (D) The hepatitis C antibody test is also referred to as the anti-HCV test. The hepatitis C RNA test, which checks to see if a person is actively, or chronically, infected with hepatitis C is also referred to as the polymerase chain reaction (PCR) test. A positive hepatitis C antibody test means the person has been infected with hepatitis C virus at some point in his or her life. Once a person has been infected, s/he will always have antibodies present in the blood. Therefore, a person who has ever been exposed to the hepatitis C virus will test positive for life for hepatitis C antibodies. A person’s immune system can clear the hepatitis C virus without any treatment. According to the CDC, approximately 15%–25% of people who are infected with hepatitis C are able to clear the virus on their own. 15) (B) The HCV quantitative test checks the level of virus (called viral load) in a patient’s blood. A decreasing viral load would mean that the virus is being destroyed and that the patient is getting better. HCV viral genotyping is a test used to find out which genotype of the HCV virus is present. HCV has six genotypes, and some are easier to treat than others. It is important to know that the HCV quantitative test and the HCV viral genotyping test are all part of the HCV RNA test; the HCV RNA test is composed of 2 subtests, the HCV quantitative test and the HCV viral genotyping test. The anti-HCV antibody (also called a hepatitis C antibody test) checks only to see if a person has ever been exposed to the hepatitis C virus. Alkaline phosphatase levels are not directly related to hepatitis C treatment. 16) (A) The screening test for active hepatitis B infection is checking for the hepatitis B surface antigen. If a patient is positive for the hepatitis B surface antigen, the patient has the hepatitis B virus and is infectious. The presence of the hepatitis B surface antigen (HBsAg) indicates that the person is currently and actively infectious with hepatitis B. Checking for the hepatitis B surface antibody would not function as a screening test for active hepatitis B infection because the surface antibody only checks to see if a person has ever been exposed to the hepatitis B virus but cannot differentiate whether the infection is latent or active. If a person has been vaccinated or had a previous (resolved) hepatitis B infection, the surface antibody test will always test positive. To screen for active hepatitis B infection, the hepatitis B surface antigen must be checked for. 17) (C) The body forms the hepatitis B surface antibody (anti-HBs) due to being exposed to the hepatitis B surface antigen, either from natural infection or vaccination; therefore, the presence of the hepatitis B surface antibody indicates immunity from hepatitis B. The hepatitis B surface antibody test cannot be used to determine active infection. All that the hepatitis B surface antibody test can reveal is if the person has immunity or not to hepatitis B. To determine active infection, the hepatitis B surface antigen test would be conducted. 18) (A) Hepatitis B surface antibodies are the antibodies produced in response to the hepatitis B surface antigen (HbsAg), a protein present on the surface of the hepatitis B virus. Hepatitis B surface antibodies appear due to convalescence from acute infection or from receiving hepatitis B vaccination. The antibodies can last for many years and be lifelong. Hepatitis B core antibodies are only formed if the person has obtained the actual hepatitis B infection. Hepatitis B e antibodies are antibodies that are produced by the immune system temporarily during acute hepatitis B virus infection or consistently during or after a burst in viral replication. Spontaneous conversion from e antigen to e antibody (a change known as seroconversion) is a predictor of long-term clearance of the hepatitis B virus in patients undergoing antiviral therapy and indicates lower levels of hepatitis B virus. 19) (D) Hepatitis B core antibody appears at the onset of symptoms in acute hepatitis B and persists for life. The presence of hepatitis B core antibody (anti-HBc) indicates previous or ongoing infection with hepatitis B virus in an undefined time frame. Hepatitis B core antibody will always be present if a person has ever had a hepatitis B infection. 20) (D) Hepatitis B e antigen (HBeAg) is a secreted product of the nucleocapsid gene of the hepatitis B virus (HBV) that is found in the blood during acute and chronic hepatitis B infection. Its presence indicates that the virus is replicating and the infected person has high levels of the hepatitis B virus (HBV) (source: cdc.gov). 21) (A) Presence of the IgM antibody to the hepatitis B core antigen (IgM anti-HBc) indicates an acute hepatitis B infection. Positivity indicates recent infection with the hepatitis B virus in the last 6 months (≤ 6 months). So, if the IgM antibody to the hepatitis B core antigen is positive, think acute hepatitis B infection (for the patient). 22) (A) A negative HBsAg, a negative anti-HBC, and a negative anti-HBs indicate that a person is susceptible (isn’t immune) to the hepatitis B virus. The HBsAg means that the person does not have the surface hepatitis B antigen, so the person isn’t currently and actively infected with the hepatitis B virus. Negative anti-HBc and anti-HBs serological markers mean that the person has not produced any antibodies to the hepatitis B virus. Therefore, the person isn’t immune to hepatitis B and, therefore, is susceptible. 23) (B) A negative HBsAg, a positive anti-HBc, and a positive anti-HBs would indicate immunity to hepatitis B due to natural infection. A negative HBsAg means that the person isn’t actively infected with the hepatitis B infection. A positive anti-HBc and a positive anti-HBs means that the person has produced antibodies to the hepatitis B virus; thus, the person has developed immunity. Production of both the hepatitis B surface antibody (anti-HBs) and the hepatitis B core antibody (anti-HBc) indicates immunity due to a natural infection (that the person had and recovered from). If the person only produced the hepatitis B surface antibody (anti-HBs), this would indicate immunity due to hepatitis B vaccination; the hepatitis B vaccination does not let a person produce anti-HBc. 24) (D) A positive HBsAg, positive anti-HBc, negative IgM anti-HBc, and negative anti-HBs indicates that a person is chronically infected with hepatitis B. A positive HBsAg means that the person is actively infected. So, the first 2 options can be eliminated, as they indicate the person isn’t actively affected, since the HBsAg is negative. In a chronic infection, the anti-HBc will be positive, because anti-HBc appears at the onset of symptoms in acute hepatitis B (and persists for life). The IgM anti-HBc will be negative in chronic hepatitis B infection, because the IgM antibody to hepatitis B core antigen signifies a recent infection with hepatitis B virus (<6 months). The IgM anti-HBc would be positive in an acute infection of hepatitis B, which is shown in option C. In chronic or acute hepatitis B infection, the anti-HBs is negative, because the person has not developed immunity to the viral infection; it is currently active. Anti-HBs is only positive when a person has developed immunity to the hepatitis B infection. 25) (D) Hepatitis D is of low prevalence in the United States. A person must have hepatitis B in order to contract hepatitis D, which can be acute or chronic. Infection with both hepatitis B and D increases a person’s risk for cirrhosis. 26) (D) During the acute phase of hepatitis, ALT and AST levels can be elevated up to 10x the normal values; if ALT and AST levels are elevated 10 times the normal range, this is usually indicative of acute hepatitis infection. ALT levels are usually not as high in chronic hepatitis, often less than 4 times the normal. 27) (B) Acute-drug induced hepatitis would cause pain the right upper quadrant, since the liver is located in the right upper quadrant. Common symptoms of drug-induced hepatitis include abdominal pain, dark urine, fatigue, fever, headache, jaundice, anorexia, nausea and vomiting, and white or clay-colored stools. 28) (C) Although it is under current development, there is no vaccine yet available for hepatitis C. Vaccines for hepatitis A and B are widely available. Since hepatitis D cannot be obtained without the presence of hepatitis B, getting the hepatitis B vaccine prevents hepatitis D. 29) (C) People who have fulminant hepatitis typically develop symptoms seen in viral hepatitis and then rapidly develop severe, often life-threatening liver failure. This can happen within hours, days, or sometimes weeks. Symptoms can include hepatic encephalopathy, blood-clotting defects, extreme irritability, and a buildup of fluid in the abdominal cavity, arms, and legs. Any viral hepatitis infection, either A, B, C, or D, can lead to fulminant hepatitis; hepatitis D actually poses a greater risk due to its dual-nature infection (B & D). The only known way to prevent fulminant viral hepatitis is to prevent viral hepatitis infection. People who have fulminant hepatitis need to be hospitalized in an intensive care unit. While there, they can be cared for until their condition becomes more stable. For some people, a liver transplant is the only lifesaving option. 30) (A) The gallbladder is located in the right upper quadrant of the abdomen, right below the liver. Knowing the positions of various organ is very important because if a person has a disease of the gallbladder, it will manifest as pain in the region where the gallbladder is located. Therefore, if a person has a biliary obstruction, for example, it will manifest as right upper quadrant pain. Image: Gallbladder 31) (A) The cystic duct is the duct that directly connects to the gallbladder. Image: Cystic duct 32) (A) Bile is made in the liver and stored in the gallbladder. It is a substance whose purpose is to digest fats. 33) (C) Gallstones are the most common cause of biliary colic. If gallstones block the cystic duct or the common bile duct, the normal flow of bile into the intestine is disrupted. The muscle cells in the bile duct contract vigorously to try to move the stone, causing the pain of biliary colic. 34) (B) Biliary colic is most likely to cause pain in the upper right quadrant. The gallbladder, along with the cystic duct and the common bile duct, are located in the upper right quadrant; therefore, pain would most likely occur in this region. 35) (C) Because symptoms of biliary colic usually are triggered by the digestive system’s demand for bile, they are especially common after fatty meals. 36) (B) The right kidney is lower than the left kidney due to displacement by the liver. 37) (A) The most specific indicator of kidney function is serum creatinine levels. Though the BUN level is also an indicator of kidney function, the serum creatinine level is the most sensitive test of kidney function because kidney impairment is almost the only cause of elevated serum creatinine levels. 38) (D) Each kidney contains 1,000,000 nephrons. Each nephron contains a glomerulus, a tubule, and a collecting duct. Nephrons filter waste products from the blood. 39) (B) The glomerular filtration rate is the amount of fluid that is filtered by the glomeruli in the kidneys in a given unit of time. 40) (D) A normal glomerular filtration rate (GFR) in a healthy individual is 90 mL/min or greater. 41) (D) A glomerular filtration rate (GFR) of less than 15 mL/min would constitute stage 5 chronic kidney disease, which is also referred to as end-stage chronic kidney disease. 42) (B) The number one cause of chronic renal failure in the United States is diabetes. 43) (C) Rhabdomyolysis may be a cause of renal failure, but it is not a symptom seen because of renal failure. Symptoms associated with renal failure include nausea, vomiting, loss of appetite, lethargy and weakness, decreased urinary output, sleep problems, decreased mental sharpness, edema and weight gain, and hypertension. 44) (A) The majority of kidney stones are made up of calcium oxalate. 45) (C) A renal ultrasound is the best and most common way to find the size and location of kidney stones. 46) (A) Renal artery stenosis is a narrowing of the arteries that carry blood to one or both of the kidneys. It is most often seen in older adults with atherosclerosis (the most common cause of renal artery stenosis). Renal artery stenosis can worsen over time and often leads to hypertension and kidney damage and can lead to kidney failure. It can lead to high blood pressure because the body senses less blood reaching the kidneys and misinterprets this as low blood pressure; this signals the release of hormones from the kidney that leads to an increase in blood pressure. Over time, due to this high blood pressure, the kidneys can become damaged and this can lead to kidney failure. Most cases of renal artery stenosis are asymptomatic; if symptomatic, the main problem is high blood pressure that cannot be controlled with medication. 47) (D) Renal artery stenosis is seen most frequently in people with atherosclerosis. The atherosclerotic plaque buildup causes narrowing in one or both renal arteries that carries blood to the kidneys. More than 90% of the time, renal artery stenosis is caused by atherosclerosis. 48) (C) Polycystic kidney disease is a disease in which clusters of cysts develop within the kidneys. Cysts are fluid-filled sacs. Although the kidneys usually are the most severely affected organs, polycystic kidney disease can cause cysts to develop also in the liver and elsewhere in the body. Image: Polycystic kidney Credit: CDC 49) (A) Polycystic kidney disease is an inherited disorder. It is not acquired. 50) (A) Common complications of polycystic kidney disease include hypertension, kidney failure, pregnancy complications (such as preeclampsia), growth of cysts in the liver, development of a brain aneurysm, mitral valve prolapse, colon problems, and chronic pain in the side or back. Regarding heart involvement, as many as 25% of people with polycystic kidney disease develop mitral valve prolapse, not infective endocarditis. 51) (C) Pyelonephritis, an infection of the renal pelvis, is not uncommon in pregnancy. Pyelonephritis is the most common urinary tract complication in pregnant women, occurring in approximately 2% of all pregnancies. Pyelonephritis is usually caused by an untreated UTI or bladder infection. Pyelonephritis is caused the majority of times by E. coli. 52) (D) Functions of the spleen include sequestering and recycling old red blood cells, storing platelets, and screening the blood flowing through for pathogens (done by the white blood cells in the spleen). The liver converts ammonia into urea. 53) (C) Splenic injury such as splenic rupture is most often observed in blunt trauma. This may include sports injuries, motor vehicle crashes, gunshot wounds, knife wounds, or with explosive injuries, as seen in warfare and civilian bombing. Although protected under the rib cage, the spleen is the most frequent organ to be damaged in blunt trauma injuries involving the abdomen. That’s true regardless of age. 54) (D) The spleen is a delicate, fist-sized organ under the left rib cage near the stomach. It contains special white blood cells that destroy bacteria and help the body fight infections. The spleen also helps remove, or filter, old red blood cells from the body’s circulation. It also stores platelets. A person can live without the spleen but it would put the person at risk for lifethreatening infections, as the spleen plays a crucial role in the body’s immune system. 55) (D) A ruptured spleen is an emergency medical condition that occurs when the capsule-like covering of the spleen, called the splenic capsule, breaks open, pouring blood into the abdominal area. The spleen is the most frequent organ to be damaged in blunt trauma injuries involving the abdomen, regardless of age. Depending on the size of the rupture, a large amount of internal bleeding can occur. Internal bleeding can cause shock-like symptoms including a dropped blood pressure, light-headedness, fainting, restlessness, and anxiety. With a splenic rupture, pain may be felt in the left side of the abdomen under the rib cage and the left side of the shoulder (because nerves of the left shoulder and the left side of the diaphragm originate from the same location). Deaths caused by splenic rupture are possible and do still occur, even at trauma centers. 56) (D) Risk factors for developing gallstones include being female, being overweight or obese, being pregnant, eating a high-fat or high-cholesterol diet, a family history of gallstones, and having diabetes (source: mayoclinic.org). 57) (A) Having gallstones is the main risk factor for developing cholecystitis (which is inflammation of the gallbladder) (source: mayoclinic.org). 58) (B) The most common complication of acute cholecystitis is gangrene of the gallbladder, if left untreated. Acute cholecystitis requires hospitalization. 59) (C) The psoas sign is a medical sign that indicates irritation to the iliopsoas group of hip flexors in the abdomen, which can indicate an inflamed appendix. The psoas sign is elicited by passively extending the thigh of a patient lying on his side with knees extended, or asking the patient to actively flex his thigh at the hip. If abdominal pain results, it is a positive psoas sign. The obturator sign is an indicator of irritation to the obturator internus muscle, which can indicate appendicitis. The technique for detecting the obturator sign, called the obturator test, is carried out on each leg in succession. The patient lies on her/his back with the hip and knee both flexed at ninety degrees. The examiner holds the patient's ankle with one hand and knee with the other hand. The examiner rotates the hip by moving the patient's ankle away from the patient's body while allowing the knee to move only inward. This is flexion and internal rotation of the hip. In the clinical context, it is performed when acute appendicitis is suspected. The appendix may come into physical contact with the obturator internus muscle, which will be stretched when this maneuver is performed on the right leg. This causes pain and is evidence in support of an inflamed appendix. Rovsing's sign is a sign of appendicitis. If palpation of the left lower quadrant of a person's abdomen increases the pain felt in the right lower quadrant, the patient is said to have a positive Rovsing's sign and may have appendicitis. The Markle sign can be another test that can suggest appendicitis. The Markle sign (also called the heel jar test) is a clinical sign that suggests appendicitis if pain in the right lower quadrant of the abdomen is elicited by dropping from standing on the toes to the heels with a jarring landing. It is found in patients with localized peritonitis due to acute appendicitis. Abdominal pain while walking or running is an equivalent sign. McBurney's point is the name given to the point over the right side of the abdomen that is one-third of the distance from the anterior superior iliac spine to the umbilicus (navel). This point roughly corresponds to the most common location of the base of the appendix where it is attached to the cecum. Deep tenderness at McBurney's point, known as McBurney's sign, is a sign of acute appendicitis. Involuntary guarding and rebound tenderness on the right-side of the abdomen is also indicative of appendicitis. 60) (B) Rovsing’s sign involves deep palpation of the left lower quadrant. If it results in referred pain to the right lower quadrant, this is a positive finding for acute appendicitis. 61) (A) Rhabdomyolysis is an acute breakdown of skeletal muscle in the body. It can be due to direct or indirect muscle injury. It results from the death of muscle fibers and release of their contents into the bloodstream. 62) (B) The classic triad symptoms of rhabdomyolysis include myalgia (muscle pain and aches), generalized weakness, and darkened urine (dark red-brownish urine). Other symptoms of rhabdomyolysis include abdominal pain, nausea or vomiting, fever, tachycardia, confusion, dehydration, reduced level of consciousness, and reduced or no urine output. Rhabdomyolysis would not cause urinary frequency, but little to no urine output. The breakdown of skeletal muscle puts the body in a state of toxicity (dehydration), so that the body conserves fluids. Myoglobin is a protein in heart and skeletal muscles. Normally, myoglobin in the urine is less than 5 ng/mL. When myoglobin is greater than 25 µg/mL, urine gets a dark brown red color (source: ncbi.nlm.nih.gov). 63) (B) The serum creatine kinase level is the most reliable and sensitive indicator for diagnosing rhabdomyolysis, since it’s the most reliable indicator of muscle injury. Creatine kinase levels elevate immediately after muscle injury. The CK levels rise within 12 hours of muscle injury, peak in 24-36 hours, then decrease by 30-40% each day. This long period of time that the CK level is elevated gives ample time for medical professionals to assess for muscle injury. Plasma myoglobin measurements are not as reliable, because myoglobin has a half-life of 1-3 hours and is cleared from the plasma within 6 hours. So, myoglobin levels not measured at the right time can produce a false-negative result, though a positive finding can help confirm the diagnosis. For this reason, urine myoglobin measurements are preferable than serum measurements. Hyperkalemia, which can pose an immediate threat to a patient due to the cardiac arrhythmias it can cause, occurs only in about 10-40% of cases of rhabdomyolysis; and hyperkalemia can be due to a number of causes other than muscle injury. Therefore, it is not a test used as a sole determination for rhabdomyolysis, but its levels help to confirm that there is acute renal failure when used in conjunction with other labs. Elevated levels of lactate dehydrogenase (LDH) levels may be detected, but it is not as specific as creatine kinase levels. 64) (C) Though a urinalysis by itself is inadequate to diagnose rhabdomyolysis, its results can give further evidence to whether a person has the condition. In the urinalysis of a patient with rhabdomyolysis, there will be elevated levels of albumin (protein) and myoglobin, with an acidic pH. The decreased (more acidic) pH of the urine is due to damaged muscle cells releasing acids. Rhabdomyolysis is not associated with an elevated level of bacteria in the urine. 65) (B) The most common potential complication of rhabdomyolysis is kidney failure. 66) (B) If a patient is taking statins and has muscle pain with dark-colored urine, this is a strong sign that the patient may be suffering from rhabdomyolysis. Cloudy urine would more indicate an infection such as a UTI. Hematemesis and frequent coughing are not associated with rhabdomyolysis. Any time a patient has muscle pain, especially with dark-colored urine, who is taking statins, rhabdomyolysis should be suspected. Creatine kinase levels should be measured. If the CK level is highly elevated, this is indicative of rhabdomyolysis. 67) (A) The woman’s likely diagnosis is fatty liver disease (steatosis). Since the hepatitis A, B, and C profiles are negative, hepatitis can be ruled out. In steatosis, there is either no pain or a vague pain. Since the liver is in the right upper quadrant, pain would be felt in this region. Steatosis can cause general malaise. Steatosis either causes normal ALT and AST levels or levels that are slightly elevated. Fatty liver disease is most often found in overweight or obese individuals. Pancreatitis is more likely to cause left upper quadrant pain. Diverticulitis is more likely to cause left lower quadrant pain. 68) (B) The highest incidence of UTIs in women is during the reproductive years. UTIs are much more common in women than in men due to the fact that women have shorter urethras. Men having UTIs can always be seen as abnormal. In boys, however, it can be seen with more incidence. Diabetes is one of several risk factors for developing UTIs. The majority of UTIs are caused by E. coli. 69) (C) Hypertension is not a risk factor for developing UTIs. Risk factors for developing UTIs include female gender (shorter urethras), catheterization, pregnancy, being sexually active, and urinary tract abnormalities. 70) (B) Encopresis is sometimes called fecal incontinence or soiling. Encopresis is the repeated passing of stool (usually involuntarily) into clothing. Typically, it happens when impacted stool collects in the colon and rectum; the colon becomes too full and liquid stool leaks around the retained stool, staining underwear. Stool retention, especially chronic, can cause distention of the bowels and loss of control over bowel movements. Encopresis is caused by the deliberate withholding of stool by the individual. 71) (A) The cause of encopresis is associated with an emotional or psychiatric disorder. 72) (A) Tenesmus is the feeling of needing to pass stools, even though the bowel is empty. Tenesmus may involve straining to defecate; tenesmus refers especially to ineffectual and painful straining for an extended period of time. 73) (A) Travelers to underdeveloped countries would be at the highest risk for hepatitis A. 74) (A) An anal fissure is a tear in the lining of the lower rectum that causes pain during bowel movements. Anal fissures generally don’t lead to more serious health problems. Most anal fissures heal with home treatment after a few days or weeks. Anal fissures are a common problem that affects people of all ages, including young and otherwise healthy people. Anal fissures are caused by injury or trauma to the anal canal. This can be when a person is constipated and tries to pass a hard stool, during birth (which can cause trauma to the anal canal), during a rectal exam, during anal intercourse, or by a foreign object. Anal fissures may cause pain during bowel movements that can be severe and can last several hours after the bowel movement. Chapter 8- Cardiology 1) What does the S1 heart sound represent? A) The opening of the tricuspid and mitral valves (the atrioventricular valves) B) The opening of the aortic and pulmonic valves (the semilunar valves) C) The closure of the tricuspid and mitral valves (the atrioventricular valves) D) The closure of the aortic and pulmonic valves (the semilunar valves) 2) What does the S2 heart sound represent? A) The opening of the tricuspid and mitral valves (the atrioventricular valves) B) The opening of the aortic ad pulmonic valves (the semilunar valves) C) The closure of the tricuspid and mitral valves (the atrioventricular valves) D) The closure of the aortic and pulmonic valves (the semilunar valves) 3) S3 is an abnormal heart sound heard in: A) B) C) D) Congestive heart failure A heart attack Pulsus paradoxus Pericarditis 4) What does an S4 heart sound normally represent? A) B) C) D) Heart failure Left aortic hypertrophy Right ventricular hypertrophy Left ventricular hypertrophy 5) What does a split S2 heart sound represent? A) Closure of the tricuspid and mitral valves are not synchronized normally B) Closure of the aortic and pulmonic valves are not synchronized normally C) Heart failure D) Left ventricular hypertrophy 6) Where is a benign split S2 heart sound best heard? A) The second intercostal space (ICS) at the right of the sternum B) The second intercostal space (ICS) at the left of the sternum C) The fifth intercostal space (ICS) at the right of the sternum D) The fifth intercostal space (ICS) at the left of the sternum 7) Atrial fibrillation is a type of: A) B) C) D) Bradycardia Tachycardia Ventricular arrhythmia Normal heart rhythm 8) All of the following are common symptoms of symptomatic atrial fibrillation except for: A) B) C) D) Dizziness Syncope Hypertension Dyspnea 9) The EKG of atrial fibrillation will show an absence of: A) B) C) D) P waves QRS cycles T waves ST segments 10) Treatment for atrial fibrillation may include all of the following except for: A) B) C) D) Lidocaine Digoxin Anticoagulants Synchronized cardioversion 11) All of the following are common causes of paroxysmal atrial tachycardia (PAT) except for: A) B) C) D) Digitalis toxicity Caffeine intake Hyperthyroidism Hyperkalemia 12) What is the target INR for a patient who has atrial fibrillation? A) B) C) D) 1.0-2.0 2.0-3.0 3.0-4.0 4.0-5.0 13) What is the desired INR for a patient with synthetic/prosthetic valves? A) B) C) D) 1.0-2.0 2.0-3.0 2.5-3.5 3.5-4.5 14) Symptoms of a myocardial infarction include all of the following with the exception of: A) Midsternal chest pain that feels like heavy pressure on the chest B) Diaphoresis C) Numbness in the left jaw D) Jugular vein distention 15) Which of the following statements is false regarding a myocardial infarction? A) The EKG shows ST segment elevation or depression B) There is an elevation in levels of cardiac enzymes, specifically Troponin T and CKMB C) Women are more likely to have an MI than men D) Women are more likely to have atypical symptoms than men 16) What is the most common type of arrhythmia in the United States? A) B) C) D) Ventricular fibrillation Atrial fibrillation Ventricular tachycardia Atrial flutter 17) All of the following are common symptoms of an abdominal aortic aneurysm except for: A) B) C) D) Chest pain Abdominal pain Pulsating abdominal mass Low back pain 18) All of the following are risk factors for developing an abdominal aortic aneurysm except for: A) B) C) D) Smoking Anemia Hypertension Being male 19) All of the following are symptoms of right ventricular failure except for: A) B) C) D) Pulmonary edema Splenomegaly Hepatomegaly Jugular venous distention 20) All of the following puts a person at high risk for developing bacterial endocarditis except for: A) B) C) D) Prosthetic heart valves Damaged heart valves Congenital heart defects Atherosclerosis 21) All of the following can be seen in bacterial endocarditis except for: A) B) C) D) Subungual hemorrhages Costochondritis Osler nodes Janeway lesions 22) A healthcare provider would expect all of the following findings in a patient suspected of having bacterial endocarditis except for: A) Fever B) Profuse vomiting C) Elevated WBCs D) Elevated erythrocyte sedimentation rate (ESR) 23) All of the following statements are true regarding mitral valve prolapse except: A) Asymptomatic mitral valve prolapse does not need treatment B) Mitral valve prolapse is most commonly diagnosed by cardiac echocardiogram with a Doppler flow study C) Mitral valve prolapse produces an abnormal S4 heart sound. D) Mitral valve prolapse may put some patients at a higher risk for the formation of thromboemboli 24) All of the following medical conditions can produce episodes of severe hypertension except for: A) B) C) D) Pheochromocytoma Atrial fibrillation Hyperaldosteronism Autonomic dysreflexia 25) A systolic murmur is a murmur that occurs when: A) The heart contracts B) The heart relaxes C) The atrioventricular valves close D) The semilunar valves close 26) A diastolic murmur is a murmur that occurs when: A) B) C) D) The heart contracts The heart relaxes The atrioventricular valves close The semilunar valves close 27) Heart murmurs are graded based on the Levine scale with a grading scale of: A) B) C) D) 1 to 3 1 to 4 1 to 5 1 to 6 28) Which grade of heart murmurs is the loudest? A) B) C) D) Grade I Grade IV Grade V Grade VI 29) Which grade of the Levine scale produces a sound that is about equal to the S1 and S2 (lubdub) heart sounds? A) B) C) D) Grade II Grade III Grade IV Grade V 30) Which grade on the Levine scale does a murmur first produce a thrill that can be palpated? A) B) C) D) Grade II Grade III Grade IV Grade V 31) Whether a murmur occurs during the systolic period or diastolic period refers to the murmur’s: A) B) C) D) Timing Location Intensity Radiation 32) Which of the following statements is true regarding diastolic murmurs? A) All diastolic murmurs are benign B) Some diastolic murmurs are abnormal C) All diastolic murmurs are abnormal D) A diastolic murmur occurs with aortic stenosis 33) Which of the following heart murmurs can be described as an early diastolic murmur? A) B) C) D) Aortic regurgitation Mitral regurgitation Aortic stenosis Mitral stenosis 34) Causes of aortic stenosis include all of the following except for: A) B) C) D) Congenital heart defect Calcification of the aortic valve History of rheumatic fever Hypertension 35) Aortic stenosis is most common in: A) B) C) D) Children Adolescents Middle-aged adults Older adults 36) Low-pitched sounds are best heard with the: A) Bell of a stethoscope B) Diaphragm of a stethoscope 37) High-pitched sounds are best heard with the: A) Bell of a stethoscope B) Diaphragm of a stethoscope 38) Which of the following describes the sound of aortic stenosis? A) B) C) D) Low-pitched and harsh Low-pitched and blowing High-pitched and harsh High-pitched and blowing 39) Where is aortic stenosis murmur best heard? A) The second intercostal space (ICS) at the right of the sternum B) The second intercostal space (ICS) at the left of the sternum C) The fifth intercostal space (ICS) at the right of the sternum D) The fifth intercostal space (ICS) at the left of the sternum 40) Aortic stenosis is best heard with the: A) Bell of a stethoscope B) Diaphragm of a stethoscope 41) Which of the following is best heard through the bell of a stethoscope? A) B) C) D) Aortic regurgitation Mitral regurgitation Mitral stenosis Aortic stenosis 42) All of the following are systolic murmurs except for: A) B) C) D) Mitral regurgitation Aortic stenosis Mitral stenosis Mitral valve prolapse 43) Where is the murmur produced by mitral stenosis best heard? A) The second intercostal space (ICS) at the right of the sternum B) The second intercostal space (ICS) at the left of the sternum C) The fifth intercostal space (ICS) at the right of the sternum D) The fifth intercostal space (ICS) at the left of the sternum 44) All of the following may cause cardiac murmurs except for: A) B) C) D) Valvular stenosis Valvular insufficiency Bradycardia A septal defect 45) Which statement is false regarding cardiac murmurs? A) Systolic murmurs occur between the S1 and S2 heart sounds B) Diastolic murmurs occur between the S2 and S1 heart sounds C) The pitch of a heart sound is influenced most by the amount of blood flow there is D) The shape of a cardiac murmur can be described as crescendo, descrescendo, crescendo-descrescendo, or uniform. 46) Systolic murmurs can be classified by all of the following except for: A) B) C) D) Early systolic Midsystolic Pansystolic Late systolic 47) Diastolic murmurs can be classified by all of the following except for: A) B) C) D) Early diastolic Mid diastolic Late diastolic Pandiastolic 48) Where do most aortic stenosis murmurs radiate to? A) B) C) D) Axilla Neck Stomach Liver 49) Where do most mitral regurgitation murmurs radiate to? A) B) C) D) Axilla Neck Stomach Liver 50) Which type of murmur is a pansystolic murmur that is high-pitched and uniform in shape? A) B) C) D) Aortic stenosis Mitral regurgitation Mitral stenosis Aortic regurgitation 51) Which type of a murmur is typically a mid-systolic murmur, that is high-pitched, with a crescendo-decrescendo shape? A) B) C) D) Aortic stenosis Mitral regurgitation Mitral stenosis Aortic regurgitation 52) Mitral valve prolapse causes: A) B) C) D) An early systolic murmur A mid or late systolic murmur An early diastolic murmur A mid or late diastolic murmur 53) In which of the following cardiac murmurs would it be easiest to hear the S2 heart sound? A) B) C) D) Pansystolic murmur Late systolic murmur Midsystolic murmur None of these murmurs 54) A systolic blood pressure of 135/88 mmHg is classified as: A) B) C) D) Normal Prehypertension Stage I hypertension Stage II hypertension 55) According to the Eighth Joint National Committee (JNC-8), initial hypertensive treatment for the black community includes either a calcium channel blocker or a: A) B) C) D) ACE inhibitor Thiazide diuretic Angiotensin II receptor blocker Beta blocker 56) The JNC-8 recommends that pharmacological antihypertensive treatment be started on adults 60 years of age or older that have a blood pressure of: A) B) C) D) 150/90 mmHg or higher 140/90 mmHg or higher 130/90 mmHg or higher 120/80 mmHg or higher 57) The JNC-8 recommends that pharmacological antihypertensive treatment be started on adults less than 60 years that have a blood pressure of: A) B) C) D) 150/90 mmHg or higher 140/90 mmHg or higher 130/90 mmHg or higher 120/80 mmHg or higher 58) According to the JNC-8, there is moderate evidence of improved kidney outcome for people with chronic kidney disease (CKD) if there is initial antihypertensive therapy of either ACE inhibitors or: A) B) C) D) Thiazide diuretics Beta blockers Angiotensin II receptor blockers Calcium channel blockers 59) Which of the following drugs should not be taken in combination with ACE inhibitors? A) B) C) D) Calcium channel blockers Angiotensin II receptor blockers Beta blockers Thiazide diuretics 60) According to the JNC-8, if pharmacological treatment is started and the blood pressure is not lowered to the target level, what should be done? A) The person should continue the pharmacological regimen and increase exercise B) The person should continue the pharmacological regimen and go on a strict DASH diet C) The dose of the initial drug should be increased or a second drug from another class should be prescribed D) Two more drugs should be added from other antihypertensive classes to lower the blood pressure 61) Either ACE inhibitors or angiotensin II receptor blockers put a patient at risk for: A) B) C) D) Hyperuricemia Hyperkalemia Hypercalcemia Hypomagnesemia 62) Other than sinus tachycardia, what is the next most common type of arrhythmia with people who have hyperthyroidism? A) B) C) D) Ventricular tachycardia Premature ventricular contractions Atrial fibrillation Atrial flutter 63) What is essential hypertension? A) Hypertension without any known secondary cause B) Hypertension caused by a tumor located somewhere in the body C) Hypertension caused by injury to the spinal cord D) Hypertension caused by renal failure 64) All of the following conditions cause secondary hypertension except for: A) B) C) D) Pheochromocytoma Hyperaldosteronism Chronic kidney disease Addison’s disease 65) Which of the following is the correct way of measuring orthostatic hypotension? A) Have the patient lie down for 5 minutes, then measure the blood pressure and pulse rate; then have the patient sit up and repeat blood pressure and pulse rate measurement after 1 minute; then have the patient stand and repeat blood pressure and pulse rate measurement after 1 minute B) Have the patient lie down for 5 minutes, then measure the blood pressure and pulse rate; then have the patient stand and repeat blood pressure and pulse rate measurement after standing 1 and 3 minutes C) Have the patient lie down for 5 minutes, then measure the blood pressure and pulse rate; then have the patient stand up and repeat blood pressure and pulse rate measurement after 3 minutes D) Have the patient lie down for 5 minutes, then measure the blood pressure and pulse rate; then have the patient sit up and repeat blood pressure and pulse rate measurement after 3 minutes 66) Orthostatic hypotension can be diagnosed if there is a drop in systolic or diastolic blood pressure of: A) B) C) D) SBP ≥ 10 mmHg or DBP ≥ 5 mmHg SBP ≥ 20 mmHg or DBP ≥ 10 mmHg SBP ≥ 30 mmHg or DBP ≥ 20 mmHg SBP ≥ 40 mmHg or DBP ≥ 30 mmHg 67) Orthostatic hypotension is most commonly found in: A) B) C) D) Children Adolescents Middle-aged adults The elderly 68) Which is diagnostic of pulsus paradoxus? A) A drop in SBP > 5 mmHg with inspiration B) A drop in SBP > 10 mmHg with inspiration C) A drop in SBP > 20 mmHg with inspiration D) A drop in SBP > 30 mmHg with inspiration 69) A nurse practitioner is examining a patient for pulsus paradoxus. Which of the following would make the NP suspect that the patient has pulsus paradoxus? A) During inspiration, the NP auscultates a cardiac beat that cannot be palpated at the radial pulse B) During inspiration, the NP palpates a radial pulse that cannot be auscultated as a cardiac beat C) During inspiration, the NP cannot auscultate a cardiac beat or a palpate a radial pulse D) During inspiration, the NP auscultates a cardiac beat and palpates a radial pulse 70) What equipment does a practitioner need to measure pulsus paradoxus? A) B) C) D) Blood pressure cuff only Stethoscope only Blood pressure cuff and stethoscope Ultrasound machine 71) All of the following conditions may cause pulsus paradoxus except for: A) B) C) D) Cardiac tamponade Pericarditis Endocarditis COPD 72) During inspiration, normally blood pressure: A) B) C) D) Increases Decreases Remains the same Is immeasurable 73) All of the following could cause inaccurate blood pressure readings except for: A) Sitting with the back and arm supported B) Sitting with the legs crossed C) Smoking or caffeine intake within 30 minutes before the measurement D) Taking the blood pressure right after a strenuous activity 74) In hypertensive retinopathy, the arterioles: A) B) C) D) Stiffen and the lumen gets wider Stiffen and the lumen narrows Stretch and the lumen gets wider Stretch and the lumen narrows 75) Common symptoms of hypertensive retinopathy include all of the following except for: A) Cotton wool spots B) Arteriovenous nicking C) Macular degeneration D) Copper wire arterioles and silver wire arterioles 76) Which statement is false regarding the point of maximal impulse (PMI)? A) The PMI represents the area of greatest apical pulsation B) Frequently the PMI is located at the 5th intercostal space at the left midclavicular line C) The PMI should always be visible in a person D) The PMI is best felt when the patient is sitting upright or leaning forward 77) Where is Erb’s point located? A) 2nd intercostal space in the left sternal region B) 3rd intercostal space in the left sternal region C) 4th intercostal space in the left sternal region D) 5th intercostal space in the left sternal region 78) Where is the best listening post for the tricuspid valve? A) At the 2nd intercostal space on the right side of the sternal area B) At the 2nd intercostal space on the left side of the sternal area C) At the 4th or 5th intercostal space on the right side of the sternal area D) At the 4th or 5th intercostal space on the left side of the sternal area 79) The aortic and pulmonic valves are best heard at the A) B) C) D) 2nd intercostal space 3rd intercostal space 4th intercostal space 5th intercostal space 80) Which of the following below is not a type of paroxysmal atrial tachycardia? A) B) C) D) Atrial fibrillation Atrial flutter Premature ventricular contractions Wolff-Parkinson White syndrome 81) Normal jugular vein distention is A) B) C) D) 2 cm or less 4 cm or less 5 cm or less 6 cm or less 82) All of the following are risk factors for heart disease except for: A) B) C) D) HDL levels below 60 mg/dL Diabetes Hypertension Cigarette smoking 83) A man who suffered an episode of heart failure a month ago was hospitalized and treated for 2 weeks. Now at home, he has symptoms of fatigue and dyspnea even while at rest. According to the New York Heart Association Functional Capacity Ratings, what class in the classification system would this man fall under? A) B) C) D) I II III IV 84) Which of the following is false regarding mitral stenosis? A) Mitral stenosis is narrowing of the mitral valve B) Mitral stenosis can be congenital or acquired C) Adults may have mitral stenosis and be asymptomatic D) Symptoms of mitral stenosis are more severe at rest than with activity 85) What is the most common cause of mitral stenosis in adults? A) Radiation treatment to the chest B) Buildup of calcium deposits forming around the mitral valves C) Rheumatic fever D) Certain medications 86) Acute coronary syndrome is any condition in which: A) The heart stops pumping B) There is a sudden reduction or blockage of blood flow to the heart C) Enzymes of the heart are dramatically increased D) There is a buildup of atherosclerotic plaque in the coronary vessels 87) Which of the following conditions would most likely cause acute coronary syndrome? A) B) C) D) Pericarditis Myocardial infarction Endocarditis Atrial fibrillation 88) Carotid sinus hypersensitivity can result in: A) Marked tachycardia and a drop in blood pressure B) Marked tachycardia and an increase in blood pressure C) Marked bradycardia and a drop in blood pressure D) Marked bradycardia and an increase in blood pressure 89) Which symptoms is carotid sinus hypersensitivity associated with? A) B) C) D) Nausea and vomiting Headache and hypertension Stiffness and paralysis Dizziness or syncope 90) Which of the following statements is false regarding carotid sinus hypersensitivity? A) Mild stimulation to the neck can trigger episodes of carotid sinus hypersensitivity B) Carotid sinus hypersensitivity episodes are not linked to falls in the elderly C) Carotid sinus hypersensitivity is found mostly in older males D) Carotid sinus hypersensitivity episodes are caused by transient diminished cerebral perfusion 91) The carotid sinus is a type of: A) B) C) D) Artery Vein Capillary Baroreceptor site 92) The carotid sinus is associated with: A) B) C) D) Respirations Temperature Blood pressure Blood glucose 93) Which of the following will likely not prevent carotid sinus hypersensitivity attacks? A) Avoiding massaging of the carotid sinus B) Avoiding wearing tight fitting collars around the neck C) Shaving gently in the front of the neck region when trimming hair D) Keeping the neck nonvertical as much as possible 94) An aortic dissection is a tear of the: A) B) C) D) Inner layer of the aorta Middle layer of the aorta Outer layer of the aorta All layers of the aorta 95) Aortic dissection most frequently occurs with: A) B) C) D) Women in their 40s and 50s Women in their 60s or older Men in their 40s and 50s Men in their 60s or older 96) Symptoms of aortic dissection include all of the following except for: A) Sudden severe chest or upper back pain B) Loss of consciousness C) Shortness of breath D) Hypertension 97) Which of the following statements is false regarding an aortic dissection? A) An aortic dissection can be fatal B) An aortic dissection is divided into 2 groups, type A and type B C) An aortic dissection is a relatively uncommon condition D) With an aortic dissection, there is a narrowing of the aorta on a chest X-ray 98) Which of the following statements is false regarding holiday heart syndrome? A) Holiday heart syndrome is an irregular heartbeat pattern present in individuals who are otherwise healthy B) Holiday heart syndrome is a temporary condition in which symptoms usually resolve within 24 hours C) Ventricular fibrillation is the most common arrhythmia in holiday heart syndrome D) Holiday heart syndrome is associated with binge alcohol drinking 99) Angina is chest pain caused by: A) Too much blood flow to the heart B) Reduced blood flow to the heart C) Infection of the outer layer of the heart D) Infection of the inner layer of the heart 100) Which of the following statements is false regarding supraventricular tachycardia? A) Supraventricular tachycardia has a sudden onset B) Supraventricular tachycardia produces narrow QRS complexes C) The rate of supraventricular tachycardia is usually greater than 150 bpm D) With supraventricular tachycardia, there are absent T waves 101) Which of the following blood pressures represents isolated systolic hypertension? A) B) C) D) 152/88 165/100 185/120 142/95 102) Blood pressure readings at doctors’ offices higher than in other settings is termed: A) B) C) D) Isolated systolic hypertension White Coat Hypertension Prehypertension Stage I hypertension 103) All of the following are common medications used in congestive heart failure except for: A) B) C) D) Digoxin Prednisone Furosemide Metoprolol 104) What does potassium do to the heart? A) Potassium inhibits the beating of the heart B) Potassium accelerates the beating of the heart C) Potassium has no effect on the heart rate D) Potassium strengthens the contraction of the heart but doesn’t affect the heart rate 105) What is preload? A) The end diastolic volume that stretches either the right or left atrium of the heart to its greatest dimensions B) The end diastolic volume that stretches either the right or left ventricle of the heart to its greatest dimensions C) The pressure against which the heart must work to eject blood during systole D) The force that the left atrium contracts with 106) What is afterload? A) The amount of blood pumped out from the left ventricle of the blood B) The pressure against which the heart must work to eject blood during systole C) The force that the left ventricle contracts with D) The amount of blood that enters the left ventricle 107) Which factor can cause a drop in afterload? A) B) C) D) Increased preload Increased peripheral resistance Decreased peripheral resistance Increased blood pressure 108) A nurse practitioner examines a patient’s pulses and notices that the dorsalis pedis pulse on the right foot is diminished. How should she grade this pulse? A) B) C) D) 0 1+ 2+ 3+ 109) The New York Heart Association (NYHA) Functional Classification system is a system that is used for: A) Patients who have suffered a myocardial infarction recently B) Patients who have had heart failure C) Patients who have right or left ventricular hypertrophy D) Patients who have stents in place 110) What effect does alcohol have on blood pressure? A) It decreases blood pressure B) It doesn’t affect blood pressure C) It increases blood pressure D) It may increase or decrease blood pressure 111) All of the following are symptoms of congestive heart failure except for: A) B) C) D) Dyspnea Swollen feet and ankles S4 heart sound Crackles 112) Which is the most common type of diuretic used to treat heart failure? A) Thiazide diuretic B) Loop diuretic C) Potassium-sparing diuretic D) They are all used equally for heart failure 113) All of the following statements are true regarding coarctation of the aorta (COA) except for: A) COA is a narrowing of the aorta B) COA produces higher blood pressure in the arms than in the legs C) Atherosclerosis is a huge risk factor in developing COA D) COA may produce delayed or diminished femoral pulses 114) What is the gold standard for diagnosing peripheral arterial disease? A) B) C) D) MRI CT scan Angiography Barium swallow 115) What is the most common arrhythmia caused by digoxin toxicity? A) B) C) D) Atrial fibrillation Atrial flutter Ventricular fibrillation Premature ventricular contractions 116) What is thromboangiitis obliterans (Buerger’s disease)? A) A disease in which blood vessels of the hands and feet become blocked B) A disease in which the blood vessels of the hands and feet break easily, leading to internal bleeding and bruising C) A disease in which blood vessels throughout the body dilate greatly, leading to hypotension D) A disease in which blood vessels throughout the body develop numerous aneurysms 117) What is the biggest risk factor for thromboangiitis obliterans (Buerger’s disease)? A) B) C) D) Diet high in fat Smoking Smog exposure Atherosclerosis Cardiology answers 1) (C) The S1 heart sound represents the closure of the tricuspid and mitral valves (the atrioventricular valves). 2) (D) The S2 heart sound represents the closure of the aortic and pulmonic valves (the semilunar valves). 3) (A) An S3 heart sound is heard in congestive heart failure. The third heart sound or S3 is a rare extra heart sound that occurs soon after the normal "lub-dub" heart sounds (S1 and S2). The S3 heart sound produces a rhythm classically compared to the cadence of the word "Kentucky" with the final syllable ("-CKY") representing S3. S3 may be normal in people under 40 years of age and some trained athletes but should disappear before middle age. Re-emergence of this sound late in life is abnormal and may indicate serious problems such as heart failure. The sound of S3 is lower in pitch than the normal S1 and S2 sounds, usually faint, and best heard with the bell of a stethoscope. It is a type of gallop rhythm by virtue of having an extra sound. 4) (D) An S4 heart sound normally represents left ventricular hypertrophy. 5) (B) A split S2 heart sound represents that closure of the aortic and pulmonic valves are not synchronized normally. This could be a normal phenomenon (physiologic splitting), as is what occurs during inspiration. 6) (B) A benign split S2 heart sound is best heard over the pulmonic area, which is the located at the second intercostal space on the left side of the sternum. 7) (B) Atrial fibrillation is a type of supraventricular tachycardia. 8) (C) Atrial fibrillation may manifest no symptoms in a patient. However, when it is symptomatic, it may present with a patient having heart palpitations, weakness, dizziness, syncope, hypotension, and dyspnea. 9) (A) The EKG of a person with atrial fibrillation will show an absence of P waves. Instead of there being P waves, there will be fibrillatory waves. The QRS cycles (representing ventricular depolarizations) and the T waves (representing ventricular repolarizations) will still be present in atrial fibrillation. 10) (A) Lidocaine is used for ventricular arrhythmias, not for supraventricular arrhythmias such as atrial fibrillation. Digoxin is used many times as a treatment for atrial fibrillation. Because the atria quiver and fail to properly pump blood to the ventricles, a person with atrial fibrillation is at risk for developing blood clots. To prevent this, anticoagulants such as warfarin may be prescribed. Synchronized cardioversion may be done for atrial fibrillation. Synchronized cardioversions are done for unstable atrial fibrillation, atrial flutter, and atrial tachycardia. It attempts to shock the heart back into normal rhythm. 11) (D) Paroxysmal atrial tachycardia is a type of arrhythmia. Paroxysmal means that the episode of arrhythmia begins and ends abruptly. Atrial means that arrhythmia starts in the atria, or upper chambers of your heart. Tachycardia means that the heart is beating abnormally fast. Common causes of paroxysmal atrial tachycardia (PAT) include digitalis toxicity, alcohol, hyperthyroidism, caffeine intake, and certain illegal drugs. Hyperkalemia would cause bradycardia, not tachycardia. 12) (B) The target INR for a patient with atrial fibrillation is 2.0-3.0. 13) (C) The desired INR for a patient with synthetic/prosthetic valves is 2.5-3.5. Due to the fact that blood clots can easily accumulate on the valves, the INR should be kept in the 2.5-3.5 range. 14) (D) Jugular vein distention is more commonly seen in heart failure. Common symptoms of a myocardial infarction include pressure or tightness in the chest, pain in the chest, back, jaw, and other areas of the upper body that lasts more than a few minutes or that goes away and comes back, shortness of breath, diaphoresis (profuse sweating), nausea, vomiting, anxiety, cough, dizziness, and tachycardia (source: healthline.com). 15) (C) Men are more likely to have an MI than women. There are several ways to diagnose an MI. On an EKG, there will be either be ST segment elevation or depression. Levels of cardiac enzymes, specifically Troponin T and CK-MB, will increase. Women are more likely to have atypical symptoms of an MI than men. A woman may have upper back pain and lightheadedness. In fact, some women who have had a heart attack report that their symptoms felt like symptoms of the flu. 16) (B) Atrial fibrillation is the most common type of arrhythmia in the United States. 17) (A) Chest pain is not a common symptom of an abdominal aortic aneurysm. Common symptoms of an abdominal aortic aneurysm include a pulsating feeling near the navel, a deep constant pain in the abdomen or the side of the abdomen, and low back pain (source: mayoclinic.org). 18) (B) Smoking, hypertension, and being male all are risk factors for an abdominal aortic aneurysm. Other risk factors include an age of 65 or older, a family history of abdominal aortic aneurysms, atherosclerosis, and people who have aneurysms in other parts of the body. 19) (A) Pulmonary edema is a common finding in left ventricular failure, not right ventricular failure. Common symptoms of right ventricular failure include peripheral edema, anorexia, nausea, abdominal pain related to congestion, jugular vein distention, hepatomegaly, splenomegaly, fatigue, and dyspnea. 20) (D) Risk factors for developing bacterial endocarditis include prosthetic heart valves, damaged heart valves, a history of endocarditis, certain congenital heart defects and IV drug users, since needles many times are contaminated with bacteria. 21) (B) Costochondritis, chest pain with respiration, isn’t directly associated or commonly seen with bacterial endocarditis. Osler’s nodes are red, raised lesions found on the hands and feet often in people who have bacterial endocarditis. They are caused by immune complex deposition and are painful. Osler’s nodes are tender to touch; Janeway lesions, also seen with bacterial endocarditis, on the other hand, are nontender. Subungual hemorrhages, tiny blood clots that tend to run vertically under the nails, are also seen many times with bacterial endocarditis. Image: Osler’s nodes 22) (B) Profuse vomiting is not a common finding in bacterial endocarditis. A person will likely feel general malaise but frequent vomiting is not expected. Findings in bacterial endocarditis include a fever, elevated WBCs, an elevated ESR, a new or changed heart murmur, fatigue, aching joints and muscles, night sweats, shortness of breath, persistent cough, paleness, swelling in the feet, legs, or abdomen, unexplained weight loss, Osler’s nodes, and Janeway lesions. 23) (C) Mitral valve prolapse produces the classic finding of an S2 “click” followed by a systolic murmur. In other words, there is a murmur which begins right after a mid-systolic click and runs to the end of the systolic period. Mitral valve prolapse does not produce an S4 heart sound. 24) (B) Atrial fibrillation can cause hypotension. Pheochromocytoma, hyperaldosteronism, and autonomic dysreflexia can all cause episodes of severe hypertension. 25) (A) A systolic murmur is heard when the heart contracts. The period between the heart contracting and relaxing is the systolic period; this is where a systolic murmur is heard. 26) (B) A diastolic murmur is heard when the heart relaxes. The period of time from when the heart relaxes to the time when the heart contracts is the diastolic period; this is where a diastolic murmur is heard. Image: Systolic murmur and diastolic murmur 27) (D) Heart murmurs are graded on a scale called the Levine scale which has grading system of I to VI. Grade I is a very soft murmur that can only be heard under optimal conditions. Grade VI is a heart murmur that is so loud, it can be heard without a stethoscope; the thrill it produces is also easily palpated. 28) (D) Grade VI is the loudest heart murmur on the Levine scale. 29) (B) A grade III heart murmur produces a sound that is about equal to the S1 and S2 (lub-dub) heart sounds. 30) (C) A murmur first produces a thrill that can be palpated at a grade of IV on the Levine scale. 31) (A) Whether a heart murmur occurs during the systolic cycle or the diastolic cycle refers to the murmur’s timing. The 7 classifications for murmurs are timing, shape, location, radiation, intensity, pitch, and quality. Timing refers to whether the murmur is a systolic or diastolic murmur. Shape refers to the intensity of the murmur over time. Murmurs can be crescendo (progressively increase in intensity), decrescendo (progressively decrease in intensity), crescendo-decrescendo (a progressive increase in intensity followed by a progressive decrease), or uniform (stays constant throughout the cycle). Location refers to where the heart murmur is usually heard best. There are 4 places on the anterior chest wall to listen for heart murmurs; each of the locations roughly corresponds to a specific part of the heart and should be listened to (through the stethoscope) with the patient supine. The 4 locations are the aortic region, pulmonic region, tricuspid region, and the mitral region. Radiation refers to where the sound of the murmur radiates to (generally the sound radiates in the direction of blood flow). Intensity refers to the Levine scale which is graded on a scale of I to VI, with I being the faintest sound and VI being the loudest. Pitch refers to whether the murmur is low-pitched, medium-pitched or high-pitched. The quality refers to characteristics of the murmur, such as whether it’s blowing, harsh, rumbling, etc. 32) (C) All diastolic murmurs are abnormal and are indicative of some type of heart disorder. With systolic murmurs, some murmurs may be benign. 33) (A) Aortic regurgitation can be described as an early diastolic murmur that is decrescendo. It is present during the early part of the diastolic cycle. Mitral regurgitation is a pansystolic murmur. Aortic stenosis is a mid-systolic murmur. Mitral stenosis is a diastolic murmur that normally has early and late components in the diastolic period. Image: Aortic regurgitation 34) (D) Hypertension, by itself, is not linked to the causation of aortic stenosis. Common causes of aortic stenosis include a congenital heart defect, calcification of the aortic valve, and a history of rheumatic or scarlet fever. The most common cause of aortic stenosis is calcification of the aortic valve, referred to as calcific aortic stenosis; this affects mostly older people. 35) (D) Aortic stenosis is most common in older adults. The most common cause of aortic stenosis is calcification of the aortic valve, which is seen most commonly in older adults (men older than 65 or women older than 75). 36) (A) Low-pitched sounds are best heard with the bell of a stethoscope. 37) (B) Mid to high-pitched sounds are best heard with the diaphragm of a stethoscope. 38) (C) Aortic stenosis is described as high-pitched and harsh. 39) (A) The aorta is located most closely near the second intercostal space (ICS) at the right of the sternum. So, this is where the murmur produced by aortic stenosis can best be heard. 40) (B) Aortic stenosis is best heard with the diaphragm of a stethoscope. Mid to high-pitched sounds are best heard through the diaphragm of a stethoscope. 41) (C) Mitral stenosis is best heard through the bell of a stethoscope because it is produces a low-pitched sound. Aortic regurgitation, mitral regurgitation, and aortic stenosis all produce high-pitched sounds, so they are best heard through the diaphragm of a stethoscope. 42) (C) Mitral stenosis is a diastolic murmur, not a systolic murmur. It’s hard to remember which heart abnormalities are systolic and which are diastolic, so use these mnemonics. MR AS(S) can be used for common systolic murmurs. In MR AS(S), MR stands for mitral regurgitation. AS stands for aortic stenosis. The last S just stands for systolic. In the mnemonic MS AR(D), MS stands for mitral stenosis. AR stands for aortic regurgitation. The D stands for diastolic. So, to remember which murmurs are systolic and which are diastolic, think of MR AS(S) and MS AR(D). Though it is not part of the mnemonic, remember that mitral valve prolapse (MVP) produces the classic finding of an S2 “click” followed by a systolic murmur; thus, MVP is a systolic murmur. 43) (D) Mitral stenosis is best heard at the apex of the heart, which is at the fifth intercostal space (ICS) at the left of the sternum. 44) (C) There are 4 major causes of cardiac murmurs. If blood is forced through a tight area, turbulent blood flow occurs. This is why valvular stenosis causes cardiac murmurs. The worse the stenosis, usually the louder the murmur. But the intensity of a murmur still cannot be used to indicate the severity of a disease, because if heart failure ensues (due to an issue such as stenosis), there is inadequate pumping in order to create blood flow, which would lessen the effects of the murmur. A second major cause of a murmur is valvular insufficiency in which an incompetent valve causes blood to abnormally travel backwards which meets normal, forward blood flow; this creates turbulence and, thus, a cardiac murmur. A third major cause of cardiac murmurs is a congenital heart defect such as atrial septal defect (ASD) or ventricular septal defect (VSD); this murmur is again created because of turbulence when blood crosses abnormally into another chamber with normal blood flow. A fourth cause of cardiac murmurs is increased blood flow through a normal valve in high output states, such as a crisis such as thyrotoxicosis. 45) (C) The pitch of a heart sound is influenced most by the pressure gradient across the pathologic area of the heart. With aortic stenosis, for example, there is usually a large pressure gradient between the left ventricle and the aorta; thus, the murmur of aortic stenosis is high pitched. Conversely, the murmur of mitral stenosis is low pitched, since there is a lower pressure gradient between the left atrium and the left ventricle during diastole. 46) (A) Systolic murmurs can be classified as either midsystolic, late systolic, or pansystolic murmurs. A midsystolic murmur begins just after the S1 heart sound and terminates just before the S2 heart sound. A pansystolic cardiac murmur begins with or immediately after the S1 heart sound and extends up to the S2 heart sound. A late systolic murmur begins significantly after the S1 heart sound and may or may not extend up to the S2 heart sound. 47) (D) Diastolic murmurs can be classified as early, mid, or late diastolic murmurs. 48) (B) Most aortic stenosis murmurs radiate to the neck. 49) (A) Most mitral regurgitation murmurs radiate to the axilla. Systolic murmurs are the only types of murmurs that really radiate. Diastolic murmurs aren’t likely to radiate (as to the same effect as systolic murmurs). 50) (B) Mitral regurgitation is a pansystolic murmur that is high-pitched and uniform in shape throughout the cycle. 51) (A) Aortic stenosis is typically a mid-systolic murmur that is high-pitched with a crescendodecrescendo shape. 52) (B) Mitral valve prolapse causes a mid or late systolic murmur. 53) (C) It would be easiest to hear the S2 heart sound with a midsystolic cardiac murmur. This is because midsystolic murmurs begins just after the S1 heart sound and terminates just before the S2 heart sound, so S1 and S2 sound are distinctly audible. With pansystolic murmurs, the intensity of the murmur is high immediately after the onset of the S1 heart sound and it extends to just before the S2 heart sound; so, the S1 and S2 heart sounds may be drowned out and difficult to hear. A late systolic murmur begins significantly after the S1 heart sound and may or may not extend up to the S2 heart sound, so the S2 heart sound may or may not be able to be heard. 54) (B) A systolic BP between 120-139 mmHg or a diastolic BP between 80-89 mmHg is classified as prehypertension. A systolic BP less than 120 mmHg or a diastolic BP less than 80 mmHg is classified as normal. A systolic BP of 140-159 mmHg or a diastolic BP of 90-99 is classified as stage I hypertension. A systolic BP of 160-179 mmHg or a diastolic BP of 100-109 is classified as stage II hypertension. A systolic BP of 180 mmHg or greater or a diastolic BP of 110 mmHg or greater is classified as stage III hypertension. 55) (B) According to the Eighth Joint National Committee (JNC-8), initial hypertensive treatment in the general black population should be either a calcium channel blocker or a thiazide diuretic, taken alone or in combination with another drug. Blacks are known to respond better to these 2 choices. For the general nonblack population, initial hypertensive treatment includes either a thiazide diuretic, calcium channel blocker, ACE inhibitor, or an angiotensin II receptor blocker (ARB), taken alone or in combination. 56) (A) The JNC-8 recommends that pharmacological antihypertensive treatment be started on adults 60 years of age or older who have a blood pressure of 150/90 mmHg or greater. The BP goal for adults 60 years of age or older should be below 150/90 mmHg. 57) (B) The JNC-8 recommends that pharmacological treatment be started on adults less than 60 years old who have a blood pressure of 140/90 mmHg or greater. 58) (C) According to the JNC-8, there is moderate evidence of improved kidney outcome for people with chronic kidney disease (CKD) if initial antihypertensive therapy consists of ACE inhibitors or angiotensin II receptor blockers (ARBs), either taken alone or in combination with another class. This applies to all CKD patients without regard to race or diabetes status. An ACE inhibitor should not be combined with an ARB. 59) (B) According to the JNC-8, angiotensin II receptor blockers (ARBs) should not be taken in combination with ACE inhibitors. 60) (C) According to the JNC-8, if pharmacological treatment is initiated and the target blood pressure is not reached within a month, the dose of the initial drug should be increased or a second drug from another antihypertensive drug class should be added and given to the patient. The clinician should then continue to assess the blood pressure and adjust the treatment regimen until the target blood pressure is reached. 61) (B) Either ACE inhibitors or angiotensin II receptor blockers can place a patient at risk for hyperkalemia. 62) (C) Besides sinus tachycardia, the next most common type of arrhythmia seen in hyperthyroidism is atrial fibrillation. Atrial flutter is uncommon, as are premature ventricular contractions (PVCs) and ventricular tachycardia. 63) (A) Essential hypertension is hypertension without any known secondary cause. Essential hypertension is also called primary hypertension. Secondary hypertension is hypertension that is caused by a known source such as a tumor. 64) (D) Addison’s disease is a condition that causes secondary hypotension, not hypertension. People with Addison’s disease are likely to have episodes of low blood pressure and may faint due to this low blood pressure. Pheochromocytoma is a tumor, most commonly located in the adrenal medulla, that causes excess catecholamine production, which raises blood pressure. Hyperaldosteronism is a tumor of the adrenal cortex which causes excess production of aldosterone, which raises blood pressure. 65) (B) The correct way to measure orthostatic hypotension is to have the patient lie down for 5 minutes; then take the blood pressure and pulse rate. After this, have the patient stand. Repeat the blood pressure and pulse rate measurements after standing for 1 minute and repeat again at 3 minutes. If there is a drop of systolic blood pressure of 20 mmHg or a drop of the diastolic blood pressure of 10 mmHg or greater after 3 minutes of standing, this is a positive sign of orthostatic hypotension. 66) (B) If there is a drop of systolic blood pressure of 20 mmHg or greater or a drop of the diastolic blood pressure of 10 mmHg or greater from the person being in the supine position (lying down) to after 3 minutes of standing, this is a positive sign of orthostatic hypotension. 67) (D) Orthostatic hypotension is most commonly found in the elderly. 68) (B) A drop in systolic blood pressure (SBP) greater than 10 mmHg is diagnostic of pulsus paradoxus. 69) (A) A practitioner would suspect a patient has pulsus paradoxus if during inspiration (when the patient breathes in), the practitioner can auscultate a heartbeat that cannot be palpated at the radial pulse. This is because the blood pressure has dropped by more than 10 mmHg. So even though the examiner can hear a heartbeat, the examiner cannot palpate it at the radial pulse because the blood pressure has fallen so much (greater than 10 mmHg) that it cannot be palpated. 70) (C) To measure pulsus paradoxus (PP), the practitioner needs a blood pressure cuff and a stethoscope. PP is quantified using a blood pressure cuff and a stethoscope (Korotkoff sounds), by measuring the variation of the systolic pressure during expiration and inspiration. The practitioner should inflate cuff until no sounds are heard (as is normally done when taking a BP), then slowly decrease the cuff pressure until systolic sounds are first heard during expiration but not during inspiration (note this reading), and slowly continue decreasing the cuff pressure until sounds are heard throughout the entire respiratory cycle (inspiration and expiration). Note this second reading. If the pressure difference between the two readings is >10mmHg, the patient can be classified as having pulsus paradoxus. 71) (C) Pulsus paradoxus may be indicative of many disorders such as cardiac tamponade, pericarditis, chronic sleep apnea, croup, asthma, and COPD. Endocarditis is not associated with cardiac tamponade. 72) (B) During inspiration, blood pressure normally decreases; it usually decreases by 10 mmHg or less. If blood pressure decreases by more than 10 mmHg, this is indicative of pulsus paradoxus. 73) (A) Several things could cause inaccurate blood pressure readings. These include a person sitting with the legs crossed, smoking or caffeine intake within 30 minutes before the measurement, and taking the blood pressure right after a strenuous activity. The person should have at least 5 minutes of rest before taking the blood pressure. Mercury sphygmomanometer readings are preferred over digital machine readings. 74) (B) Moderately sustained hypertension (systolic BP above 160 mmHg and/or diastolic BP above 100 mmHg) over at least 5 years stiffens the wall and narrows the lumen of retinal arterioles. 75) (C) Macular degeneration is not associated with hypertensive retinopathy. Common symptoms of hypertensive retinopathy include cotton wool spots (fluffy, white patches on the retina due to ischemia), arteriovenous nicking, and copper wire arterioles and silver wire arterioles. Moderately sustained hypertension (systolic BP above 160 mmHg and/or diastolic BP above 100 mmHg) over at least 5 years stiffens the wall and narrows the lumen of retinal arterioles. Arteriovenous nicking is a condition in which as the stiffened arteriole crosses a retinal vein, it indents the vein and causes a slight deviation in its path. With hypertensive retinopathy, there is also an increase in light reflection from vessel walls. The arteriole vessel walls are normally a flat red color in normal states. Hypertensive retinopathy makes the arterioles develop a shiny, glistening reflection. As the vessel wall thickens and the blood column narrows, the reflection shifts toward a bronze color ("copper-wiring") and eventually toward gray ("silverwiring"). Arteriovenous nicking and an increased light reflex are reliable as signs of chronic hypertension only in patients aged less than 70 years, because advanced age can produce these abnormalities even in a normotensive state. Other changes that can be seen with hypertensive retinopathy include hard exudates (due to leakage of lipids from the blood vessels), flame-shaped hemorrhages (also known as superficial retinal hemorrhages), and optic disc edema. 76) (C) The point of maximal impulse represents the area on the anterior chest wall (called the precordium) where the apical pulsation is felt the strongest. The apical impulse is not always visible in a person; it is more easily seen in patients who are thin or who have enlarged hearts. The PMI is best felt when the patient is sitting upright or leaning forward. Frequently the PMI is located at the 5th intercostal space at the midclavicular line; however, conditions such as left ventricular hypertrophy could make this variable. 77) (B) Erb’s point is located at the 3rd intercostal space in the left sternal region. Erb’s point does not reflect sound from any one particular heart valve, but is a common listening post, lying halfway between the base and the apex of the heart. 78) (D) The tricuspid valve is best heard at either the 4th or 5th intercostal space on the left side of the sternal area. 79) (A) The aortic and pulmonic valves are both best heard at the 2nd intercostal space. While the aortic valve is heard at the right of the sternum, the pulmonic valve is heard at the left of the sternum. 80) (C) Premature ventricular contractions are a type of heart arrhythmia that has origins in the ventricles; PVCs are normally due to some type of ventricular irritant. Atrial fibrillation, atrial flutter, and Wolff-Parkinson White syndrome are all types of paroxysmal atrial tachycardia heart rhythms. Realize that paroxysmal atrial tachycardia is also known as supraventricular atrial tachycardia, heart arrhythmias whose origins are above the ventricles. 81) (B) Normal jugular vein distention is 4 cm or less. In a condition such as right ventricular failure, jugular vein distention can be elevated above this level. 82) (A) An HDL level below 40 mg/dL in men or below 50 mg/dL in women is considered a risk factor for heart disease. Other risk factors include hypertension, a family history of premature heart disease (women with a myocardial infarction before the age of 65 or men with a myocardial infarction before the age of 55), diabetes, hyperlipidemia or dyslipidemia, age (men older than 45 years old or women older than 55), cigarette smoking, and obesity. 83) (D) According to the New York Heart Association Functional Capacity Ratings, a heart failure patient who has symptoms even while at rest falls under class IV of functional capacity ratings. A class of I means the person has no limitation of physical activity. Ordinary physical activity does not cause fatigue, palpitation, or dyspnea. A class of II means a person has slight limitation of physical activity. The person is comfortable at rest but ordinary physical activity results in fatigue, palpitation, or dyspnea. A class of III means a person has marked limitation of physical activity. The person is comfortable at rest but less than ordinary activity causes fatigue, palpitation, or dyspnea. A class of IV means the person is unable to carry on any physical activity without discomfort. The person has symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. See the Appendix Reference Table XVIII for the chart of the New York Heart Association (NYHA) Functional Classification. 84) (D) Mitral stenosis is narrowing of the mitral valve. It can be congenital (there from birth) or acquired (such as through rheumatic fever). Adults who have mitral stenosis may be asymptomatic (have no symptoms). However, symptoms may appear or get worse with exercise or any other activity that raises the heart rate. 85) (C) In adults, the most common cause of mitral stenosis is rheumatic fever. The valve problems normally develop 5 to 10 years after having rheumatic fever. Because rheumatic fever is becoming rare in the United States because most strep infections are treated, mitral stenosis is less common today than in the past. 86) (B) Acute coronary syndrome is any condition in which there is a sudden reduction or blockage of blood flow to the heart. This is a common condition with over 200,000 US cases per year. Acute coronary syndrome is most often caused by plaque buildup or clot formation in the heart’s arteries. Symptoms may include heart attack-like chest pressure, chest pressure while resting or activity, or sudden heart stoppage. 87) (B) Acute coronary syndrome is any condition in which there is a sudden reduction or blockage of blood flow to the heart. Acute coronary syndrome is usually caused by either myocardial infarction or unstable angina. 88) (C) Carotid sinus hypersensitivity can result in marked bradycardia and a drop in blood pressure. 89) (D) Carotid sinus hypersensitivity is an exaggerated response to carotid sinus baroceptor stimulation. It results in dizziness or syncope due to transient diminished cerebral perfusion. Although baroreceptor function usually diminishes with age, some people experience hypersensitive carotid baroreflexes. For these individuals, even mild stimulation to the neck results in marked bradycardia and a drop in blood pressure. In severe cases, a loss of consciousness or convulsions and seizures may occur when a buildup of pressure occurs in these arteries due to manual stimulation. 90) (B) Carotid sinus hypersensitivity is a potent contributory factor in the cause of unexplained falls and syncopal episodes in elderly people. Carotid sinus hypersensitivity episodes are caused by transient diminished cerebral perfusion when pressure is applied to the carotid sinus. It is mostly found in older adult males. Even mild stimulation to the neck can trigger episodes of syncope and hypotension. 91) (D) The carotid sinus is a type of baroreceptor site in the human body. It is present in the dilated area at the base of the internal carotid artery just superior to the bifurcation of the internal carotid and external carotid arteries. 92) (C) The carotid sinus is a major baroreceptor site in humans; therefore, blood pressure balance and homeostatic balance are the 2 major functions of the carotid sinus reflex found in the carotid artery. Because of the nature of the autonomic system, blood pressure changes affect heart rate. So, the carotid sinus can both affect blood pressure and heart rate. 93) (D) Carotid sinus hypersensitivity is independent of the position of the neck. It doesn’t matter which orientation the neck is in, putting pressure on the carotid sinus can result in episodes of bradycardia and hypotension, which can lead to syncope. If a person is lying down, it may put them at less risk for falls, since they are not standing up, but falls are not the only risk of carotid sinus hypersensitivity attacks; loss of consciousness, convulsions, and seizures can also occur, if severe enough. Avoiding pressure on the carotid sinus prevents attacks, such as avoiding massaging of the carotid sinus, avoiding tight fitting collars around the neck, and shaving the front of the neck region gently when trimming hair. 94) (A) An aortic dissection is a tear of the inner layer of the aorta. Blood surges through the tear, causing the inner layer to separate from the middle layer. If the blood-filled channel ruptures through the outside aortic wall, aortic dissection is often fatal. 95) (D) Aortic dissection most frequently occurs with men who are in their 60s or older. Men have about double the incidence of aortic dissection than women. 96) (D) Symptoms of aortic dissection may be similar to those of other heart problems such as a heart attack. Typical signs and symptoms include sudden severe chest or upper back pain, often described as a tearing, ripping or shearing sensation, that radiates to the neck or down the back, loss of consciousness, shortness of breath, sudden difficulty speaking, loss of vision, weakness or paralysis of one side of the body, and a weak pulse in one arm compared with the other. Hypotension, not hypertension, would result. 97) (D) An aortic dissection is a medical emergency which can be life threatening. It is a relatively uncommon condition. An aortic dissection is divided into 2 groups, type A and type B. Type A is a tear in the upper aorta (at or near the heart); this is the more common and dangerous type. Type B is a tear in the lower aorta. Detecting an aortic dissection can be a difficult thing because it mimics many other health conditions. A practitioner may suspect an aortic dissection if the patient describes the incident as a sudden tearing or ripping chest pain, there is widening of the aorta on the chest X-ray, and there is a blood pressure difference between right and left arms. Because the aorta tears and the inner and middle layer separates, it widens, not narrows. 98) (C) Holiday heart syndrome is an irregular heartbeat pattern present in individuals who are otherwise healthy. It is a temporary condition and is coined “holiday heart syndrome” due to heart abnormalities that occur due to excessive alcohol consumption, although it can also occur due to stress or dehydration. In certain cases, even moderate amounts of alcohol can trigger this condition. Atrial fibrillation is the most common arrhythmia in holiday heart syndrome. Symptoms usually resolve within 24 hours. 99) (B) Angina is chest pain caused by reduced blood flow to the heart. 100) (D) Supraventricular tachycardia is a type of tachycardia located above the ventricles. Atrial fibrillation is the most common type of supraventricular tachycardia. It produces narrow QRS complexes with a heart rate that is generally greater than 150 bpm. It has a sudden onset. T waves are present. 101) (A) Isolated systolic hypertension is defined as a blood pressure where the systolic blood pressure is greater than 140 mmHg and the diastolic blood pressure is less than 90 mmHg. Therefore, the blood pressure of 152/88 is the only blood pressure that represents isolated systolic hypertension. 102) (B) White coat hypertension is high blood pressure that occurs at doctors’ offices but that are lower in other settings. 103) (B) Common medications used for congestive heart failure include blood pressure medications (such as beta blockers, ACE inhibitors, angiotensin II receptor blockers), diuretics such as loop diuretics, and digitalis glycosides such as digoxin (source: American Heart Association). 104) (A) Potassium inhibits the beating of the heart. This is why low potassium leads to tachycardia. And why high potassium leads to bradycardia. 105) (B) Preload is the end diastolic volume that stretches the right or left ventricle of the heart to its greatest dimensions. In other words, preload is the volume of blood in the ventricle at the end of diastole. 106) (B) Afterload is the pressure against which the heart must work to eject blood during systole. 107) (C) Decreased peripheral resistance in the body can cause a drop in afterload. Increased preload, increased peripheral resistance, and increased blood pressure all cause increases in the afterload. 108) (B) A pulse that is barely palpable or that is diminished should be graded 1+. A pulse that is completely absent is graded as a 0. A pulse that is normal is charted as a 2+. A pulse that is increased is charted as a 3+. A pulse that is bounding is charted as a 4+. 109) (B) The New York Heart Association (NYHA) Functional Classification system is a system that is used to classify patients who have had heart failure. It categorizes them into certain classes according to the severity of their symptoms. 110) (C) Drinking too much alcohol can increase blood pressure. The Dietary Guidelines for Americans recommends that men limit alcohol to no more than two drinks a day and women to one or less a day (source: mayoclinic.org). 111) (C) Common symptoms of congestive heart failure include dyspnea (shortness of breath), lung congestion that produces crackles, a dry, hacking cough, fluid retention that can cause swollen feet and ankles, nocturia, dizziness, fatigue, and weakness. 112) (B) Loop diuretics are the type of diuretic most commonly used to treat heart failure. Loop diuretics are the most potent type of diuretic and are especially useful for acute heart failure. 113) (C) Coarctation of the aorta (COA) is a congenital heart defect. It is not acquired through any lifestyle factors such as atherosclerosis. COA is a narrowing of the aorta, which produces higher blood pressure in the arms than in the legs. COA may produce delayed or diminished femoral pulses. 114) (C) The gold standard for diagnosing peripheral arterial disease is angiography, normally through a Doppler ultrasound flow study. 115) (D) The most common type of arrhythmia caused by digoxin toxicity is premature ventricular contractions (PVCs). Digoxin does not cause atrial fibrillation or atrial flutter. In fact, digoxin is used many times in the treatment of atrial fibrillation and atrial flutter. Besides atrial fibrillation and atrial flutter, digoxin (toxicity) can cause virtually any other type of arrhythmia. 116) (A) Thromboangiitis obliterans is a rare disease in which blood vessels of the hands and feet become blocked. Thromboangiitis obliterans (Buerger’s disease) is caused by small blood vessels that become inflamed and swollen. The blood vessels then narrow or get blocked by blood clots (thrombosis). Blood vessels of the hands and feet are mostly affected. Arteries are more affected than veins. Average age when symptoms begin is around 35. This condition mostly affects young men ages 20 to 45 who are heavy smokers or chew tobacco. There is no cure for thromboangiitis obliterans. The goal of treatment is to control symptoms and prevent the disease from getting worse (source: medlineplus.gov). 117) (B) Smoking is the biggest risk factor for thromboangiitis obliterans. Chapter 9- Musculoskeletal, Nerves & Vessels 1) What is polymyositis? A) An inflammatory condition characterized by one-sided facial paralysis B) An inflammatory condition characterized by muscle weakness that affects both sides of the body C) An inflammatory condition characterized by muscle weakness in the face D) An inflammatory condition characterized by the frequent occurrence of muscle rigidity 2) What is the most defining characteristic of polymyositis? A) B) C) D) Aphonia Atonic seizures Muscle weakness Facial paralysis 3) Which demographic group has the highest occurrence of polymyositis? A) B) C) D) White men White women Black men Black women 4) Which age group does polymyositis most commonly affect? A) B) C) D) 10-20 years of age 20-50 years of age 60-80 years of age 80-90 years of age 5) All of the following are symptoms of polymyositis except for: A) Muscle weakness B) Median nerve compression C) Elevated serum creatine kinase (CK) levels D) Inflammation of the muscles 6) A possible complication of polymyositis is: A) B) C) D) Seizures Arthritis Dysphagia Parkinson’s 7) Polymyositis is largely believed to be a: A) B) C) D) Precancerous condition Cancerous condition Bacterial illness Autoimmune disease 8) Which medication can be very effective at controlling symptoms of polymyositis? A) B) C) D) NSAIDs Narcotics Corticosteroids Folic acid 9) Which of the following statements is false regarding Raynaud’s disease? A) Raynaud’s disease is characterized by vasospasms in certain areas of the body such as the fingers and toes, which causes these areas to feel numb and cold, in response to certain triggers such as cold weather and stress B) Women are more likely than men to have Raynaud’s disease C) Raynaud’s disease is more common for those who live in tropical climates D) Raynaud’s disease can be primary or secondary 10) All of the following are common triggers of Raynaud’s phenomenon except: A) Warm weather B) Emotional stress C) Nicotine D) Cold weather 11) Which of the following is not a secondary cause of Raynaud’s disease? A) B) C) D) Carpal tunnel syndrome Plantar fasciitis Systemic lupus erythematosus Scleroderma 12) What type of medication is most commonly given for Raynaud’s disease? A) B) C) D) Beta blockers Ace inhibitors Loop diuretics Calcium channel blockers 13) What is fibromyalgia? A) A disorder characterized by frequent headaches with extreme hypersensitivity to sound and light B) A disorder characterized by easy bruising and bone fractures C) A disorder characterized by widespread muscle pain and tenderness D) A disorder characterized by anemia and extreme hypermobility of the joints 14) All of the following are common symptoms of fibromyalgia except: A) B) C) D) Widespread body pain or aches Thick respiratory secretions Brain fog Nonrefreshing sleep 15) Which statement is true regarding fibromyalgia? A) Fibromyalgia affects men more so than women B) Fibromyalgia is a temporary condition that lasts for a few years C) Fibromyalgia is a chronic condition D) Fibromyalgia doesn’t affect sleep 16) How is fibromyalgia diagnosed? A) A muscle biopsy B) The presence of tender points throughout the body C) Electromyography D) Widespread pain for more than 3 months with no explanatory medical condition 17) All of the following are risk factors for osteoarthritis except for: A) B) C) D) Obesity Old age Female gender Diabetes 18) Which of the following statements is false regarding rheumatoid arthritis? A) Rheumatoid arthritis is the most common type of autoimmune arthritis B) Rheumatoid arthritis affects men more than it does women C) Rheumatoid arthritis is a chronic disease that causes pain, stiffness, swelling and limited motion of many joints D) Rheumatoid arthritis can affect organs, as well as joints 19) The stiffness seen in rheumatoid arthritis is most often worst: A) B) C) D) In the morning During the day In the evening At night during sleep 20) The presence of all of the following in a person’s serology would be suggestive of rheumatoid arthritis except for: A) Anemia B) Rheumatoid factor C) CA-125 serum marker D) Elevated ESR 21) Which medication would likely be prescribed for a mild case of rheumatoid arthritis? A) B) C) D) Acetaminophen NSAIDs DMARDs Opioids 22) Which of the following statements is false regarding rheumatoid arthritis and osteoarthritis? A) Rheumatoid arthritis is more likely to affect the body symmetrically (on both sides) than osteoarthritis B) Rheumatoid arthritis is more likely to develop at any time in life than osteoarthritis C) Rheumatoid arthritis is more common than osteoarthritis D) Rheumatoid arthritis is more likely to cause fatigue and a general feeling of malaise 23) Ankylosing spondylitis is a type of: A) B) C) D) Muscle disease Arthritis Deformity of the foot Deformity of the skull 24) All of the following statements are true regarding ankylosing spondylitis except: A) Ankylosing spondylitis is more common in males B) Ankylosing spondylitis produces a positive rheumatoid factor C) The average age of onset of ankylosing spondylitis is in the early 20s D) Ankylosing spondylitis affects mainly the spine and the sacroiliac joints and can affect other joints 25) All of the following are common symptoms of ankylosing spondylitis except for: A) Uveitis B) Marked loss of range of motion such as forward bending and rotational ability C) Muscle weakness D) Stiffness in the morning 26) Ankylosing spondylitis is: A) B) C) D) Limited to localization in the spine Limited to localization in the sacrum Limited to localization in the feet Systemic 27) During HLA typing for a person suspected of having ankylosing spondylitis, what gene will more than likely to be found if the diagnosis is confirmed? A) B) C) D) HLA-B27 gene HLA-B57 gene HLA-DR3 gene HLA-DR4 gene 28) Which of the following complications is most likely to occur in a person with ankylosing spondylitis? A) B) C) D) Costochondritis Heart failure Renal failure Autonomic dysreflexia 29) What is a common radiographic finding of a person with ankylosing spondylitis? A) B) C) D) Greenstick fractures Spinal fusion Oblique fractures Comminuted fractures 30) What is the first-line treatment for ankylosing spondylitis? A) Corticosteroids B) NSAIDs C) Opioids D) Disease-modifying agents for rheumatoid disease (DMARDs) 31) All of the following statements are true regarding lateral epicondylitis except: A) Lateral epicondylitis produces pain on the outside of the elbow on the forearm B) Lateral epicondylitis normally causes peripheral neuropathy on the affected forearm C) Lateral epicondylitis is a type of tendon injury D) The symptoms of lateral epicondylitis develop gradually over time 32) Which tests are specific to carpal tunnel syndrome? A) B) C) D) Chvostek's sign and Trousseau's sign McMurray’s test and Thessaly Test Phalen’s sign and Tinel's sign Ortolani’s sign and Barlow’s sign 33) Pain and tingling in carpal tunnel syndrome is due to compression of the: A) B) C) D) Radial nerve Ulnar nerve Axillary nerve Median nerve 34) Phalen's sign consists of A) Full flexion of the wrist for 30 seconds B) Full flexion of the wrist for 60 seconds C) Full flexion of the wrist for 5 minutes D) Full flexion of the wrist for 10 minutes 35) What is a positive finding for Phalen's sign? A) Tingling sensation of “pins and needles” in the hand B) Bluish, cyanotic appearance of the hand C) A cold sensation over the hand D) A feeling of intense warmth occurring over the hand 36) Tinel's sign consists of: A) B) C) D) Tapping the anterior wrist briskly Squeezing the wrist briskly Tapping the posterior wrist briskly Squeezing the wrist for 15 seconds 37) What is a positive finding for Tinel's sign? A) Tingling sensation of “pins and needles” in the hand B) Bluish, cyanotic appearance of the hand C) A cold sensation over the hand D) A feeling of intense warmth occurring over the hand 38) What is the most common cause of cauda equina syndrome? A) B) C) D) A bulging herniated disc Spinal stenosis Tumors Injury to the spine 39) Acute cauda equina syndrome is treated by: A) B) C) D) Corticosteroid shots NSAIDs Decompression surgery Laser excision 40) All of the following are risk factors for plantar fasciitis except for: A) Obesity B) Diabetes C) Prolonged standing D) Prolonged sitting 41) Which of the following is true regarding plantar fasciitis? A) Plantar fasciitis is always bilateral B) Plantar fasciitis can only be healed surgically C) Weight bearing commonly is prescribed to help heal plantar fasciitis D) Plantar fasciitis is aggravated by walking 42) What is the most common medication used for plantar fasciitis? A) B) C) D) Opioids NSAIDs Quinolones Corticosteroids 43) Gout has a disposition for the: A) B) C) D) Great toe Small toe Third toe Second toe 44) What is considered an elevated uric acid level? A) B) C) D) 3 mg/dL or greater 5 mg/dL or greater 7 mg/dL or greater 11 mg/dL or greater 45) Which types of foods should be avoided in people who have gout? A) High phenylalanine foods B) High oxalate foods C) High purine foods D) High sodium foots 46) All of the following foods should be avoided for a person with gout except for: A) B) C) D) Potatoes Sardines Beer Meats 47) Which medication is used for the long-term treatment of gout? A) B) C) D) Cholestyramine Colchicine Allopurinol Atorvastatin 48) What is Morton’s neuroma? A) A painless condition in which the nerves in the hands thicken B) A painless condition in which the nerves in the feet thicken C) A painful condition in which the nerves in the hands thicken D) A painful condition in which the nerves in the feet thicken 49) Morton’s neuroma is most commonly between: A) B) C) D) The first and second toe The second and third toe The third and fourth toe The fourth and fifth toe 50) Risk factors for Morton’s neuroma include all of the following except for: A) Wearing high heel shoes B) Wearing tight shoes C) Running D) Smoking 51) The NP suspects, based on patient’s symptoms and risk factors, that a client may have Morton’s neuroma. Which test would the NP perform to confirm these suspicions? A) B) C) D) Lachman test Mulder test McMurray’s test Psoas sign 52) All of the following are risk factors for osteoporosis except for: A) B) C) D) Obesity Female gender Chronic steroid use Alcohol use 53) Which race/ethnicities of women are at highest risk for osteoporosis? A) Whites and Asians B) Blacks and Native Americans C) Hispanics and Blacks D) Pacific Islanders and Eastern Europeans 54) Osteoporosis can increase the likelihood for all of the following except for: A) B) C) D) Loss of height over time Stooped posture Bone fractures Decreased serum calcium levels 55) Which test is the best and most commonly used test to measure a person’s bone mineral density (BMD)? A) X-ray B) Dual-energy x-ray absorptiometry (DEXA) scan C) CAT scan D) Serum calcium levels 56) A patient went for a DEXA scan to measure his bone mineral density. The results showed a score of -1.8 SD. This patient would be classified as having: A) B) C) D) Normal, healthy bones Osteopenia Osteoporosis Indeterminate 57) A patient went for a DEXA scan to measure his bone mineral density. The results showed a score of -2.6 SD. This patient would be classified as having: A) B) C) D) Normal, healthy bones Osteopenia Osteoporosis Indeterminate 58) A man comes into a clinic and complains of midfoot pain. The pain worsens with activity and improves with rest. Which of the following disorders listed below could be responsible for these symptoms? A) B) C) D) Colles’ fracture Navicular fracture Smith’s fracture Femur fracture 59) The Adams Forward Bend Test is used to check for: A) B) C) D) Spinal irritation/inflammation Scoliosis Back pain Carpal tunnel syndrome 60) Supraspinatus tendonitis involves the: A) B) C) D) Foot Knee Shoulder Hand 61) Which of the following activities puts a person at higher risk for supraspinatus tendonitis? A) B) C) D) Running Swimming Tennis Hockey 62) What are bursae? A) Fluid-filled sacs that act as cushions between muscles, tendons, and bones near the joints B) A flexible but inelastic cord of strong fibrous collagen tissue attaching a muscle to a bone C) A short band of tough, flexible, fibrous connective tissue that connects two bones or cartilages, or holds together a joint D) A band or bundle of fibrous tissue that has the ability to contract, producing movement or maintaining the position of parts of the body 63) Which of the following statements is false regarding bursitis? A) Bursitis is a condition that occurs when the bursae become inflamed B) The most common causes of bursitis are repetitive motions or positions that irritate the bursa around a joint C) The occurrence of bursitis is highest among adolescents and young adults D) Being overweight is a risk factor for bursitis 64) All of the following are common locations of bursitis except for the: A) B) C) D) Shoulder Heel Elbow Hip 65) Sites of bursitis include all of the following symptoms except for: A) Achy or stiff joints B) Joints that hurt when a person moves or the joint is pressed on C) Swollen joints D) Necrotic joints 66) What is the most common type of bursitis in the hip region? A) B) C) D) Gluteus medius bursitis Trochanteric bursitis Ischial bursitis Iliopsoas bursitis 67) All of the following are treatments used for bursitis except: A) B) C) D) OTC pain medication Corticosteroid shots Cold therapy Diuretics 68) Which procedure may be done to remove fluid from a site of bursitis? A) B) C) D) Lumbar puncture Fasciotomy Fine needle aspiration Stitches 69) Where is a baker’s cyst located? A) B) C) D) In the feet Underneath the knees Above the knee Behind the knee 70) The anterior cruciate ligament (ACL) is the ligament that attaches: A) B) C) D) The femur to the tibia The fibula to the tibia The ulnar to the radius The humerus to the radius 71) What is the most common cause of hip fractures in the elderly? A) Elderly abuse B) Falls C) Osteoporosis D) Unexplained spontaneous hip fractures 72) Which of the following tests checks for the presence of an ACL injury? A) B) C) D) Mulder test Ortolani test Lachman’s test McMurray’s test 73) All of the following are common symptoms of an ACL injury except for: A) Knee pain B) Knee swelling C) Loss of full range of motion in the knee D) The absence of pain while walking 74) A phalanx refers to: A) B) C) D) A bone of the finger A bone of the toe A bone of either the finger or toe A bone of the knee 75) What is the gold standard for checking for joint damage? A) B) C) D) X-ray CT scan Palpation MRI 76) McMurray’s test is most sensitive for detection of a(n): A) B) C) D) ACL injury Tibial fracture Meniscus tear Fracture of the patella 77) What is the difference between tendons and ligaments? A) Tendons connect bone to bone; ligaments connect muscles to bones B) Tendons connect muscles to bone; ligaments connect bone to bone C) Tendons and ligaments connect bone to bone but ligaments allow for more flexibility D) Tendons and ligaments connect muscles to bone but tendons allow for more flexibility 78) What is the meniscus? A) A type of crescent-shaped cartilage in the knee B) A type of ligament that attaches the lateral aspect femur to the lateral aspect of the fibula C) A type of ligament that attaches the medial aspect femur to the medial aspect of the fibula D) A type of tendon that attaches the patella to the tibia 79) The meniscus is found: A) B) C) D) Between the tibia and fibula Between the femur and tibia At the top of the femur At the bottom of the fibula 80) Which statement is false regarding meniscus tears? A) Meniscus tears often occur at the same time as other knee injuries such as an ACL injury B) Older people are at higher risk for developing meniscus tears than younger people C) Meniscus tears are painless and may go unnoticed initially D) Meniscus tears can cause locking of the knees 81) Colles’ fracture is a fracture of the: A) B) C) D) Distal radius in the forearm Proximal radius in the forearm Distal ulna in the forearm Proximal ulna in the forearm 82) Falling with the wrists in a flexed position would most likely lead to what type of fracture? A) B) C) D) Colles’ fracture Navicular fracture Smith’s fracture Proximal humerus fracture 83) A spinal disorder in which a bone (vertebra) slips forward over the bone below it is called: A) B) C) D) Spinal stenosis Herniated disc Degenerative disc disease Spondylolisthesis 84) What is the single largest nerve in the human body? A) B) C) D) Saphenous nerve Trigeminal nerve Ulnar nerve Sciatic nerve 85) Spondylolisthesis most commonly occurs in the: A) B) C) D) Cervical vertebrae Upper thoracic vertebrae Lower thoracic vertebrae Lumbosacral vertebrae 86) How is spondylolisthesis definitively diagnosed? A) B) C) D) X-ray Spinal tap Ultrasound Physical examination 87) A spinal compression fracture is: A) Compression of the nerve roots in the spinal cord B) Osteoporosis specifically in the vertebrae of the spinal cord C) A fracture of a vertebra D) Wearing and tearing of the intervertebral disc 88) What is the most common reason for a spinal compression fracture? A) B) C) D) Contact sports Heavy lifting Osteoporosis Bone cancer 89) Which of the following statements is false regarding a herniated disc? A) A herniated disc is also referred to as a slipped disc or a ruptured disc B) A herniated disc can irritate nearby nerves and result in pain, numbness, or weakness in an arm or leg C) Most herniated discs occur in the thoracic region of the spine D) Most people with herniated discs do not need surgery 90) What is the most common cause of a ruptured disc? A) B) C) D) Disk degeneration Traumatic injury Osteoporosis Spondylolisthesis 91) Which of the following is a risk factor for a herniated disc? A) B) C) D) Hypertension Osteoporosis Obesity Diabetes 92) Which of the following is false regarding sciatica? A) Sciatica is caused by an underlying medical condition B) Sciatica normally begins before the age of 20 years old C) Sciatica normally takes place on one side of the body D) Sciatica involves pain that radiates from the back, through the buttocks, and down the leg 93) Causes of sciatica may include all of the following except for: A) B) C) D) Lumbar herniated disc Degenerative disc disease Spondylolisthesis Hypertension 94) Which of the following is not a risk factor for sciatica? A) B) C) D) Obesity Diabetes Prolonged standing Prolonged sitting 95) Which is true regarding sciatica? A) Sciatica is normally a chronic issue that never resolves B) Most cases of sciatica resolve with non-surgical treatment in a few weeks C) Sciatica, even in severe cases, always resolves itself without any need for surgical treatment D) Sciatica, for all cases, needs surgical treatment for it to resolve 96) Which of the following statements is false regarding internal tibial torsion? A) Internal tibial torsion is commonly known as intoeing B) Internal tibial torsion is a benign condition C) Internal tibial torsion usually causes a lot of pain for a child D) Most children outgrow their internal tibial torsion without any treatment 97) Internal tibial torsion may lead to: A) B) C) D) Extreme pain Frequent falls Osteomyelitis Failure to thrive 98) Bone spurs are associated with: A) B) C) D) Normal bone development Osteoarthritis Osteosarcoma Ankylosing spondylitis 99) What is main symptom associated with bone spurs? A) B) C) D) Bone pain Tendonitis Ataxia Most bone spurs cause no symptoms 100) Chondromalacia patellae is a condition in which: A) There are small cracks in the patella bone B) The patella bone splits in half vertically C) The cartilage on the undersurface of the patella deteriorates and softens D) The cartilage on top of the patella deteriorates and softens 101) Chondromalacia patellae is also known as: A) B) C) D) Runner’s knee Swimmer’s knee Football knee Gymnastics knee 102) Which age group is most at risk for chondromalacia patellae? A) B) C) D) Infants Adolescents Older Adults Elderly 103) Which of the following statements is false regarding chondromalacia patellae? A) Chondromalacia patellae affects females more than males B) Chondromalacia patellae presents as a painless condition C) Swelling and tenderness may be present in the knee region D) Rest, stabilizing, and icing the joint may be the first line of treatment 104) Which of the following conditions would least likely not aggravate pain in a person with chondromalacia patella? A) Running B) Prolonged standing C) Prolonged sitting with bent knees D) Prolonged resting with the legs straight 105) Which sign is most specific to chondromalacia patellae? A) B) C) D) Anterior drawer sign Posterior drawer sign Theater sign Murphy’s sign 106) Most pain that is elicited in chondromalacia patellae is due to: A) Fractures of the femur B) Fractures of the patella C) Bone-to-bone grating of the patella and femur bones D) Fractures of the medial condyles 107) Genu varum is also known as: A) B) C) D) Bow-leggedness Knock knees Tennis’s elbow Golfer’s elbow 108) What is the most common cause of genu varum? A) B) C) D) Infection Tumors Rickets Physical trauma 109) Which of the following statements is false regarding genu varum? A) Genu varum is a physical deformity marked by the outward bowing of the lower leg in relation to the thigh B) It is normal for a child to have a degree of genu varum until about the age of 3 C) Genu varum that persists into later childhood and that is untreated increases the risk of a person’s chances of developing arthritis later in life D) Most cases of genu varum causes severe immobility 110) Genu valgam is also known as: A) B) C) D) Bow-leggedness Knock knees Tennis’s elbow Golfer’s elbow 111) Genu valgam is a condition in which: A) A child has deformed feet in which the feet are internally rotated at the ankle B) A child has deformed feet in which the feet are externally rotated at the ankle C) There is outward protruding of the lower leg in relation to the thigh D) The knees angle in and touch one another when the legs are straightened 112) It is normal for children to have genu valgam between the ages of: A) B) C) D) 2-5 years 6-9 years 10-12 years Genu valgam is always abnormal 113) Pes planus is also known as: A) B) C) D) Flat feet Bow-leggedness Knock knees Arched feet 114) Which of the following statements is false regarding pes planus? A) Pes planus can be inherited or acquired B) Children or adults can be affected C) Most infants are flat-footed until they are between the ages 3 and 5 when their longitudinal arch develops normally D) Most people with pes planus have severe pain when walking 115) What is the usual treatment for pes planus in adults? A) There is no treatment B) Comfortable shoes with good arch support C) Bisphosphonates D) Surgery 116) Pectus excavatum is a condition in which: A) A person’s breastbone is sunken into his or her chest B) A person’s breastbone has small fractures throughout it C) A person’s breastbone doesn’t form at all at birth D) A person’s breastbone is characterized by a protrusion of the sternum and ribs 117) Which of the of the following statements is false regarding pectus excavatum? A) Pectus excavatum is a congenital chest wall deformity B) Pectus excavatum, even in mild conditions, causes severe respiratory issues C) Pectus excavatum produces a concave, or caved-in, appearance in the anterior chest wall D) Pectus excavatum occurs most often in males in about a 3:1 ratio 118) Pectus carinatum is a condition in which: A) A person’s breastbone is sunken into his or her chest B) A person’s breastbone has small fractures throughout it C) A person’s breastbone doesn’t form at all at birth D) A person’s breastbone characterized by a protrusion of the sternum and ribs 119) What is the most common type of congenital chest wall deformity? A) B) C) D) Pectus carinatum Pectus excavatum Cleft sternum Pentalogy of Cantrell 120) Nursemaid’s elbow is a type of: A) B) C) D) Congenital defect Strained tendon in the arm Dislocation of the elbow joint Greenstick fracture of the elbow 121) Nursemaid’s elbow is also called: A) B) C) D) Broken elbow Pulled elbow Twisted elbow Knee lag 122) Nursemaid’s elbow is most common in: A) B) C) D) Children 1-4 years old Children 6-10 years old Adolescents 13-18 years Young adults in their 20s 123) What is the treatment for nursemaid’s elbow? A) B) C) D) Surgery Reduction NSAIDs No treatment available 124) Which of the following signs are highly suspicious that a child has endured nursemaid’s elbow? A) There is enormous swelling in the arm B) There is an easily noticeable bone deformity of the arm C) There is numbness and tingling in the hand of the affected arm D) The child limits use of the affected arm and mostly keeps it in a fixed, straight position on his/her side 125) A painful condition of the big toe caused by gout is called: A) B) C) D) Tendonitis Podagra Bunions Hammertoes 126) What is torticollis? A) A condition in which a child, due to muscle abnormalities, cannot open the jaw B) A condition in which the neck muscles contract, causing the head to twist to one side C) A condition in which a child suffers partial paralysis and is unable to move the lower limbs D) A condition in which the child suffers from muscle stiffness, which makes it impossible to move the arms 127) Carnett’s sign is a test that checks for: A) B) C) D) Intra-abdominal pain Abdominal wall pain Chest pain Spinal cord pain 128) A patient comes into a clinic, complaining of abdominal pain. The healthcare practitioner elicits the Carnett’s sign and the pain gets worse when the patient lifts his legs. What condition would most likely cause this pain? A) B) C) D) Appendicitis Rectus sheath hematoma Cholecystitis Nephrolithiasis 129) The first cervical vertebra is called the: A) B) C) D) The atlas The axis Transverse foramen Posterior tubercle 130) The second cervical vertebra is called the: A) B) C) D) The atlas The axis Transverse foramen Posterior tubercle 131) How many vertebrae make up the spine? A) B) C) D) 10 18 33 51 132) Which of the following statements is false regarding a rectus muscle tear? A) A rectus muscle tear is rare B) A rectus muscle tear manifests as bleeding, swelling and pain C) A rectus muscle tear is normally caused by appendicitis D) A rectus muscle tear can be diagnosed by a CT scan 133) Atlantoaxial instability is defined as: A) Inability to move the first and second cervical vertebrae B) Excessive movement between the first and second cervical vertebrae C) Fractures of the first and second cervical vertebrae D) Spinal fusion of the first and second cervical vertebrae 134) In the majority of the cases (95%) of thoracic outlet syndrome, pain is due to compression of: A) B) C) D) Arteries Veins Nerves Muscles 135) Which of the following statements is false regarding thoracic outlet syndrome? A) Thoracic outlet syndrome is a group of disorders that occur when blood vessels or nerves in the space between the collar bone and the first rib are compressed B) Thoracic outlet syndrome can cause pain in the legs and feet C) Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures D) Poor posture can cause compression in the thoracic outlet area 136) Common causes of thoracic outlet syndrome include all of the following except: A) B) C) D) Physical trauma Certain anatomical defects Rheumatoid arthritis Pregnancy 137) Which of the following demographic populations does thoracic outlet syndrome most commonly occur in? A) B) C) D) Young adult males Young adult females Older adult males Older adult females 138) A condition in which the knees hyperextend backwards is called: A) B) C) D) Genu valgum Genu varum Genu recurvatum Chondromalacia patellae 139) Which of the following statements is false regarding genu recurvatum? A) It is a deformity in the knee joint B) It decreases the normal range of motion of the knee joint C) It causes a backwards-bending knee D) The development of genu recurvatum may lead to knee pain and knee osteoarthritis 140) Which of the following statements is true regarding tandem gait? A) Tandem gait is a method of walking where the toes of the back foot touch the heel of the front foot with each step B) Tandem gait is a method of walking where the legs are kept as far apart as possible C) Tandem gait is a method of walking where a person takes steps as far backwards as possible with each step D) Tandem gait is a method of walking where the person’s feet criss cross with each step taken 141) Roos Stress test is also called the: A) B) C) D) Foot Stress Test Neck Stress Test Elevated Arm Stress Test Leg Stress Test 142) What is the most common cause for lower limb amputations in the United States? A) B) C) D) Cancer Traumatic injury Vascular disease Unexplained causes 143) The Tinetti Gait and Balance Instrument is designed to determine: A) A child’s risk for falls B) An elder’s risk for falls C) The risk for falls for a person with muscular dystrophy D) The risk for falls for a person with orthostatic hypotension 144) Which of the following statements is false regarding the Ottawa Ankle Rules? A) The examination consists of the practitioner palpating the entire distal 6cm of the fibula and tibia B) The examination consists of the patient taking steps C) An ankle x-ray series is required even if there is no bone tenderness or inability to bear weight on the ankles D) The Ottawa Ankles Rules should not be used on patients younger than 18 years old 145) Mastoiditis produces pain: A) B) C) D) In the front of the ear Behind the ear On the front of the nose On the side of the nose 146) Mastoiditis is most often caused by: A) B) C) D) Traumatic injury Acute otitis media Osteomyelitis Rhinitis 147) Which of the following statements is false regarding septic arthritis? A) Septic arthritis is also known as infectious arthritis B) Septic arthritis is usually caused by bacteria C) Septic arthritis usually affects all joints in the body to some degree D) Septic arthritis is diagnosed by an arthrocentesis 148) Common bacteria that cause acute septic arthritis include all of the following except: A) B) C) D) Haemophilus influenza E. coli Staphylococcus bacteria Streptococcus bacteria 149) Treatment for septic arthritis usually consists of: A) Antibiotics and corticosteroids B) Antibiotics and arthrocentesis C) Antibiotics, antivirals, and antifungals D) High-dose morphine 150) Tenosynovitis is inflammation of: A) B) C) D) Joint Tendon Synovium Muscle 151) Heberden’s nodes and Bouchard’s nodes are seen in: A) B) C) D) Osteoarthritis Rheumatoid arthritis Ankylosing spondylitis Gout 152) Which of the following statements is false regarding osteomyelitis? A) Osteomyelitis is an infection of a bone B) Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue C) In children, osteomyelitis most often affects the spine D) Osteomyelitis is most often treated by surgery followed by strong antibiotics 153) What type of bacteria most often causes osteomyelitis? A) B) C) D) Staphylococcus bacteria Streptococcus bacteria E. Coli Salmonella 154) What is the gold standard for diagnosing osteomyelitis? A) B) C) D) X-ray Bone biopsy CT scan CBC 155) All of the following conditions are systemic except for: A) B) C) D) Rheumatoid arthritis Ankylosing spondylitis Osteoarthritis Lupus 156) Which condition is swan neck deformity and boutonnière deformity most often seen in? A) B) C) D) Osteoarthritis Rheumatoid arthritis Ankylosing spondylitis Gout 157) Which type of arthritic disease is most likely to have an onset after the age of 60? A) B) C) D) Osteoarthritis Rheumatoid arthritis Ankylosing spondylitis Gout 158) Which statement is true regarding scoliosis and kyphosis? A) Scoliosis is the anterior-posterior curvature of the spine, while kyphosis is the lateral curvature of the spine B) Kyphosis is the anterior-posterior curvature of the spine, while scoliosis is the lateral curvature of the spine C) Scoliosis and kyphosis both refer to the anterior-posterior curvature of the spin, with kyphosis being more severe D) Scoliosis and kyphosis both refer to the lateral curvature of the spine, with kyphosis being more severe 159) Acute limb ischemia occurs whenever there is: A) An acute infection in the body B) Sudden lack of blood flow to a limb C) Severe hemorrhage in the body D) Osteonecrosis 160) Symptoms of peripheral arterial disease may include all of the following except for: A) Intermittent claudication B) Gangrene on one or more toes C) Decreased or absent dorsalis pedis pulse D) Decreased capillary refill time 161) All of the following are skin changes associated with peripheral arterial disease except for: A) B) C) D) Shiny skin Hairless skin Skin that is warm to touch A change in color of the skin Musculoskeletal, Nerves, & Vessels answers 1) (B) Polymyositis is an inflammatory condition characterized by muscle weakness that affects both sides of the body. Polymyositis can be summed up by its name. Poly means many. Myo means muscle. And itis means inflammation. So many muscles are inflamed and, thus, are weak. Polymyositis affects the muscles closest to the trunk, such as those in the hips, thighs, shoulders, upper arms, and neck. Polymyositis can make it difficult for a woman to walk up stairs, rise from a seated position, or reach for something overhead. Polymyositis develops gradually over weeks or months (source: mayoclinic.org). 2) (C) The hallmark feature of polymyositis is muscle weakness. 3) (D) Black women have the highest occurrence of polymyositis. Polymyositis is more common in blacks than in whites, and women are affected more often than men. 4) (B) Polymyositis most commonly affects adults in their 20s to 50s. 5) (B) Polymyositis is not associated with median nerve compression; carpal tunnel syndrome is. Common symptoms of polymyositis include muscle weakness and inflammation and elevated serum creatine kinase levels. 6) (C) A possible complication of polymyositis is dysphagia, or difficulty swallowing (if the muscles of the esophagus are affected). This dysphagia can lead to choking episodes and aspiration pneumonia. Another complication of polymyositis is breathing problems (if the chest muscles are affected by the disease) (source: mayoclinic.org). 7) (D) Polymyositis is largely believed to be an autoimmune disease. 8) (C) Corticosteroids can be very effective at controlling symptoms of polymyositis. Since polymyositis is linked to an overactive immune system, corticosteroids can be used to quiet down the immune response, so that less muscles are damaged. 9) (C) Raynaud’s disease is characterized by vasospasms in certain areas of the body such as the fingers and toes in response to certain triggers such as cold weather and stress. Doctors don’t completely understand the cause of Raynaud’s attacks, but blood vessels in the hands and feet appear to overreact to cold temperatures or stress. With Raynaud’s disease, arteries to the fingers and toes go into vasospasms when exposed to cold or stress, narrowing the vessels and temporarily limiting blood supply. Women are more likely than men to have Raynaud’s disease. Raynaud’s is more common in those who live in cold climates. Raynaud’s can be primary (no cause) or secondary (caused by other underlying medication conditions) (source: mayoclinic.org). 10) (A) Cold weather, not warm weather, is a common trigger of Raynaud’s phenomenon. Other triggers for Raynaud’s phenomenon include emotional stress, nicotine, and caffeine. 11) (B) Plantar fasciitis is not associated with Raynaud’s disease. Secondary causes of Raynaud’s phenomenon include connective tissue diseases such as scleroderma, lupus, rheumatoid arthritis, and Sjögren’s syndrome, arterial diseases such as atherosclerosis and Buerger’s disease, carpal tunnel syndrome, repetitive actions such as typing or playing the piano, smoking (constricts blood vessels), injuries to the hands or feet such as wrist fractures, and certain medications such as beta blockers. 12) (D) Calcium channel blockers are the medication most commonly prescribed for Raynaud’s phenomenon. Calcium channel blockers such as nifedipine and amlodipine are commonly prescribed. 13) (C) Fibromyalgia is a common and chronic disorder characterized by widespread pain, diffuse tenderness, and a number of other symptoms, including fatigue and sleep problems. 14) (B) Thick respiratory secretions are not a common symptom of fibromyalgia. Common symptoms of fibromyalgia include musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. The pain associated with fibromyalgia is described as a constant dull ache that has lasted for at least 3 months. The pain occurs on both sides of the body, above and below the waist (widespread pain). People with fibromyalgia often awaken tired, even with reporting long periods of sleep. And their sleep can be disrupted by pain. People with fibromyalgia often have cognitive difficulties, suffering from what is referred to “fibro fog”, which impairs a person of the ability to focus, pay attention, and concentrate. People with fibromyalgia may also experience headaches and depression. 15) (C) Fibromyalgia is a chronic condition. It affects women with much more prevalence than men; in fact, women account for about 90% of cases of fibromyalgia. Fibromyalgia can affect sleep in many ways, including sleep awakening because of pain and nonrefreshing sleep, even after a long period of sleep. 16) (D) Fibromyalgia is diagnosed by the presence of widespread pain that lasts for more than 3 months—with the person having no underlying medical condition that could cause the pain. In the past, fibromyalgia was diagnosed by a practitioner checking for tender points in the body. 11 tender points in the body were needed to diagnose fibromyalgia. Newer guidelines don’t require a tender point exam. Instead, a fibromyalgia diagnosis can be made if a person has had widespread pain for more than 3 months, with no underlying medical condition that could cause the pain. 17) (D) Risk factors for osteoarthritis include older age (risk of osteoarthritis increases with age), female gender, obesity (increased weight puts added stress on weight-bearing joints such as the hips and knees), joint injuries (such as from playing sports), certain occupations (that place repetitive stress on a particular joint), genetics (some people inherit a tendency to develop osteoarthritis), and bone deformities (some people are born with malformed joints or defective cartilage which increases the risk of osteoarthritis). 18) (B) Rheumatoid arthritis (RA) is the most common form of autoimmune arthritis, affecting more than 1.3 million Americans. Of these, about 75 percent are women. In fact, 1–3 percent of women may get rheumatoid arthritis in their lifetime. The disease most often begins between the fourth and sixth decades of life. However, RA can start at any age. RA is a chronic (long-term) disease that causes pain, stiffness, swelling and limited motion and function of many joints. While RA can affect any joint, the small joints in the hands and feet tend to be involved the most often. Inflammation sometimes can affect organs as well, for instance, the eyes or lungs (since it is a systemic disorder) (source: rheumatology.org). 19) (A) The stiffness seen in rheumatoid arthritis is most often worst in the morning. The stiffness may last one to two hours (or even the whole day). Stiffness for a long time in the morning is a clue that a person may have RA, since few other arthritic diseases behave this way. For instance, osteoarthritis most often does not cause prolonged morning stiffness (source: rheumatology.org). 20) (C) There is no single test that confirms a rheumatoid arthritis diagnosis for most patients with this disease. Rather, a doctor makes the diagnosis by looking at the symptoms and results from a physical examination, lab tests and radiology findings. One of the factors that a diagnosis of rheumatoid arthritis depends on is symptoms and results of a physical exam, such as the presentation of warmth, swelling and pain in the joints. Some blood tests also can help confirm RA. Telltale signs include anemia, the presence of rheumatoid factor (not definitive, though, because rheumatoid factor can also be present in other disorders), antibodies to cyclic citrullinated peptides (pieces of protein found in 60-70% of patients with RA), and elevated ESR (indicating inflammation). Besides blood work, X-rays can help in detecting RA, but may not show anything abnormal in the early stages. Even so, these first X-rays may be useful later to show if the disease is progressing. Often, MRI and ultrasound scanning are done to help judge the severity of RA. CA-125 serum marker is not specific to rheumatoid arthritis (source: rheumatology.org). 21) (B) For mild cases of rheumatoid arthritis, NSAIDs are most often prescribed. Acetaminophen would not be used in most cases because it doesn’t have the anti-inflammatory effect that NSAIDS have. For severe cases of rheumatoid arthritis, DMARDs are often prescribed. 22) (C) The main difference between osteoarthritis and rheumatoid arthritis is the cause behind the joint symptoms. Osteoarthritis is caused by mechanical wear and tear on joints. Rheumatoid arthritis is an autoimmune disease in which the body's own immune system attacks the body's joints. Osteoarthritis is the most common form of arthritis. Rheumatoid arthritis affects about onetenth as many people as osteoarthritis. Rheumatoid arthritis is more likely to begin any time in life, while osteoarthritis usually begins later in life. Rheumatoid arthritis usually has a relatively rapid onset (over weeks to months), while osteoarthritis usually has slow development (over years). With RA, joints are painful, swollen and stiff, while with OA, joints ache and may be tender but have little to no swelling. RA often affects small and large joints on both sides of the body (symmetrically), such as both hands, both wrists or elbows, or the balls of both feet; with OA, symptoms often begin on one side of the body (they may spread gradually to the other side over time). Most often, with OA, symptoms are limited to one set of joints, usually the joints in the fingers, large weight-bearing joints such as the hips and knees, or the spine. With RA, morning stiffness usually lasts longer than 1 hour; with OA, morning stiffness usually lasts less than 1 hour, with stiffness returning at the end of the day or after periods of activity. With RA, frequent fatigue and a general feeling of malaise are present, while with OA, whole-body symptoms are not present (source: webmd.com). 23) (B) Ankylosing spondylitis is a type of arthritis that affects mainly the spine and the sacroiliac joints. 24) (B) Ankylosing spondylitis does not produce a positive rheumatoid factor. Ankylosing spondylitis is more prevalent in males than in females. The average age of onset is in one’s early 20s. Ankylosing spondylitis affects mainly the spine and the sacroiliac joints and can affect other joints. 25) (C) Common symptoms of ankylosing spondylitis include pain and stiffness, uveitis, and marked loss of range of motion such as forward bending and rotational ability. Constant pain and stiffness are normally in the low back, buttocks, and hips that continue for more than 3 months. Ankylosing spondylitis can also cause an overgrowth of bones, which may lead to abnormal joining of bones called bony fusion. Fusion affecting bones of the neck, back, or hips may impair a person’s ability to perform routine daily activities. Fusion of the ribs to the spine or breastbone may limit a person’s ability to expand his or her chest when taking a deep breath. Muscle weakness is not a symptom directly related to ankylosing spondylitis. Image: Uveitis 26) (D) Ankylosing spondylitis is a systemic disorder. Though it may only affect the spine and sacroiliac joints, it is not contained to this area. People with this condition may also have a fever, fatigue, and loss of appetite. There may also be eye involvement, frequently uveitis. In rare cases, lung and heart problems may also develop. 27) (A) HLA testing stands for human leukocyte antigen testing. It tests white blood cells to see if certain antigens are attached to them. It is used to match organ and tissue transplant recipients with compatible donors. It is also used to see if certain individuals have a disposition for certain autoimmune disorders such as ankylosing spondylitis. The presence of the HLA-B27 gene puts a person at increased risk for ankylosing spondylitis. Just having the gene doesn’t automatically mean the person has the illness but just has a great disposition for it. About 90% of the people who are carriers of this gene have symptoms of ankylosing spondylitis. 28) (A) A person with ankylosing spondylitis may develop costochondritis, which is chest pain with respiration. If the thoracic spine is involved with the person’s ankylosing spondylitis, this can put pressure on the lungs, which can cause pain on respiration. 29) (B) Spinal fusion is a common radiographic finding of a person with ankylosing spondylitis. Ankylosing spondylitis is an inflammatory disease that, over time, can cause some of the vertebrae in the spine to fuse. This fusing makes the spine less flexible and can result in a hunched-forward posture. If the ribs are affected, this can make it difficult for a person to breathe deeply (source: mayoclinic.org). 30) (B) The first-line treatment for ankylosing spondylitis is NSAIDs. NSAIDs — such as naproxen (Naprosyn) and indomethacin (Indocin) — are the medications doctors most commonly use to treat ankylosing spondylitis. They can relieve inflammation, pain and stiffness (source: mayoclinic.org). 31) (B) Lateral epicondylitis (also called tennis elbow) is a painful condition of the outside of the elbow on the forearm caused by overuse. Playing tennis or other racquet sports can cause this condition; however, several other sports and activities can put a person at risk. Lateral epicondylitis is an inflammation of tendons that join the forearm muscles on the outside of the elbow. The forearm muscles and tendons become damaged from overuse—repeating the same motions again and again. This leads to pain and tenderness on the outside of the elbow. The symptoms of lateral epicondylitis develop gradually. In most cases, the pain begins as mild pain and slowly worsens over weeks and months. There is usually no specific injury associated with the start of symptoms. Common symptoms include pain or burning on the outer part of the elbow and/or a weak grip strength (such as when holding the tennis racquet). Lateral epicondylitis is not associated with peripheral neuropathy on the affected arm (source: aaos.org). Image: Site of lateral epicondylitis 32) (C) Phalen’s sign and Tinel’s sign are specific to carpal tunnel syndrome. 33) (D) Pain and tingling in carpal tunnel syndrome is due to compression of the median nerve. 34) (B) Phalen’s sign consists of full flexion of the wrist for 60 seconds (1 minute). Image: Phalen’s sign 35) (A) A positive finding for Phalen’s sign is a tingling sensation of “pins and needles” in the hand. This is due to the median nerve being compressed. 36) (A) Tinel’s sign consists of tapping the anterior wrist briskly. Image: Tinel’s sign 37) (A) A positive finding for Tinel’s sign, just like with Phalen’s sign, is a tingling sensation of “pins and needles” in the hand. This is due to the median nerve being compressed. 38) (A) Cauda equina syndrome is a condition in which the cauda equina, a bundle of nerve roots located at the lower end of the spinal cord, are compressed. The most common cause of cauda equina syndrome is a bulging herniated disc that protrudes out and puts compression on the cauda equina nerves. 39) (C) Acute cauda equina syndrome is treated by decompression surgery. Cauda equina syndrome is a medical emergency that calls for urgent surgical intervention. If patients with cauda equina syndrome do not receive treatment quickly, adverse results can include paralysis, impaired bladder and/or bowel control, difficulty walking, and/or other neurological and physical problems. Cauda equina syndrome is a condition in which the cauda equina, a bundle of nerve roots located at the lower end of the spinal cord in the lumbosacral spine, are compressed. This may damage the nerve roots, leading to lasting damage, which can cause incontinence and possibly permanent paralysis of the legs. The cauda equina send and receive messages to and from the legs, feet, and pelvic organs. 40) (D) Prolonged sitting is not a risk factor for plantar fasciitis. Risk factors for plantar fasciitis include obesity, diabetes, flat feet, and prolonged standing. 41) (D) Plantar fasciitis is aggravated by walking. Plantar fasciitis is acute or recurrent pain on the bottom of the feet caused by microtears in the plantar fascia. Plantar fasciitis can be in one foot (unilateral) or both feet (bilateral). Plantar fasciitis is usually a self-limiting condition that heals within a year. Under certain circumstances, however, surgical intervention may need be done. Weight bearing worsens plantar fasciitis, especially when the person is standing, because it puts increased pressure on the plantar fascia. Image: Plantar fasciitis 42) (B) NSAIDs are most commonly prescribed for plantar fasciitis. Drugs such as naproxen (Aleve) or ibuprofen (Advil) are commonly prescribed. 43) (A) Gout has a disposition for the great toe. 44) (C) Serum uric acid levels are considered elevated when above 7 mg/dL. Be aware that lab levels frequently vary according to different sources, whether it be different hospitals, facilities, or clinics. You will almost never see lab values be the same across many different sources. Some sources do say that uric acid levels can go as high as 8 mg/dL, but others say that levels above 7 mg/dL is elevated, such as webmd.com. So, you just have to choose the values that are as close to the normal range as possible when selecting appropriate lab values. According to webmd.com, normal uric acid levels in men is 3.4-7.0 mg/dL; normal uric acid levels in women is 2.46.0 mg/dL. So, the first 2 options of 3 mg/dL and 5 mg/dL do not represent elevated values. The last option of 11 mg/dL is very high. The closest correct value would then be 7 mg/dL. 45) (C) High purine foods should be avoided in people who have gout. Eating foods high in purines will increase uric acid levels further, worsening the gout. 46) (A) Potatoes can be safely eaten by a gout patient, because it’s a low-purine food. Foods high in purines include beer, sugary soft drinks, organ meats such as liver from many different animal sources, all types of meats, various types of fish including anchovies, sardines, herring, mussels, codfish, trout, and haddock, and gravy. 47) (C) Allopurinol (Zyloprim) is used for the long-term treatment of gout. Colchicine is used in acute episodes of high uric acid levels in the body. 48) (D) Morton’s neuroma is a painful condition in which the nerves in the feet thicken. Morton's neuroma affects the ball of the foot, most commonly the area between the third and fourth toes. Morton's neuroma may feel as if a person is standing on a pebble in his or her shoe or on a fold in his or her sock. Image: Morton’s neuroma 49) (C) Morton’s neuroma is most commonly present in between the third and fourth toe. 50) (D) Risk factors for Morton’s neuroma include wearing high heel shoes, tight shoes, and doing certain high-impact activities such as running or jogging. Smoking is not directly associated with Morton’s neuroma. 51) (B) The Mulder test is specific to checking for Morton’s neuroma. During this test, the healthcare practitioner squeezes together the two metatarsal heads with one hand while applying pressure to the interdigital spaces with the other hand. Pain and a clicking sound is a positive finding for Morton’s neuroma. 52) (A) Risk factors for osteoporosis include age (bone density peaks after age 30; after this age, a person will begin losing bone mass), gender (women over the age of 50 are the most likely group to develop osteoporosis; the condition is 4 times as common in women than in men), family history, body structure and body weight (petite, thin people are at greater risk), previous history of broken bones, certain diseases such as rheumatoid arthritis, certain medications such as long-term use of steroids, smoking, and heavy alcohol consumption (source: webmd.com). 53) (A) White and Asian women are at highest risk for osteoporosis. 54) (D) Osteoporosis can increase the likelihood for loss of height over time, stooped posture, and bone fractures. Osteoporosis can cause hypercalcemia (not hypocalcemia) if the person’s bones continue to release calcium into the circulating bloodstream. 55) (B) A dual-energy x-ray absorptiometry (DEXA) scan is the best and most commonly used test to measure a person’s bone mineral density. 56) (B) A score of -1.8 SD (standard deviations) would be classified as osteopenia. Any score between -1 and -2.5 is classified as osteopenia. Any score greater than -1 would mean the person has normal, healthy bone mineral density. Any score below -2.5 would indicate osteoporosis. 57) (C) A score of -2.6 SD (standard deviations) would be classified as osteoporosis. Any score between -1 and -2.5 would be classified as osteopenia. Any score greater than -1 would mean the person has normal, healthy bone mineral density. Any score below -2.5 would indicate osteoporosis. 58) (B) Out of all the fractures listed, a navicular fracture is the only fracture that takes place near the middle of the foot, so it’s the only fracture that would cause midfoot pain. Smith’s fracture and Colles’ fracture are fractures of the wrist. A femur fracture is a fracture of the femur, the long bone in the upper leg. Image: Navicular fracture 59) (B) The Adam’s Forward Bend Test is a test used to check for scoliosis. During this test, a person bends forward with both arms hanging free. The examiner will look for asymmetry of the spine. 60) (C) Supraspinatus tendonitis involves the shoulder. Supraspinatus tendonitis is inflammation of the tendon underneath the acromion bone. Image: Supraspinatus muscle Credit: Photograph by Anatomography, licensed under the Creative Commons Attribution-Share Alike 2.1 Japan license 61) (C) Any activities that require repetitive throwing or overhead motions can irritate the supraspinatus tendon, causing supraspinatus tendonitis. This includes pitching in baseball, volleyball, and tennis. 62) (A) Bursae are fluid-filled sacs that act as cushions between muscles, tendons, and bones near the joints. 63) (C) The most common causes of bursitis are repetitive motions or positions that irritate the bursa around a joint. Examples include throwing a baseball overhead repeatedly, leaning on one’s elbows for long periods of time, extensive kneeling such as in carpet work, and prolonged sitting, particularly on hard surfaces. Other causes include injury or trauma to the affected area, inflammatory arthritis such as rheumatoid arthritis, gout, and infection. Being overweight is a risk factor for bursitis, because being overweight places more stress on the joints. The occurrence of bursitis becomes more common with aging (source: mayoclinic.org). 64) (B) The most common locations for bursitis are in the shoulder, elbow and hip. But bursitis can also exist in the knee, heel and the base of the big toe. Bursitis often occurs near joints that perform frequent repetitive motions (source: mayoclinic.org). 65) (D) Bursitis does not cause necrotic joints. Common symptoms of bursitis include pain (joints that hurt when a person moves or the joint is pressed on), swelling and stiffness of the joints. 66) (B) The most commonly affected bursa in the hip region is the trochanteric bursa (trochanteric bursitis). 67) (D) Diuretics are not used to treat bursitis. OTC pain medications include nonsteroidal antiinflammatory drugs such as aspirin, ibuprofen, and naproxen. Corticosteroid injections are injected into the bursa to reduce inflammation and, therefore, improve symptoms. Cold therapy is used to reduce the inflammation and pain. 68) (C) A fine needle aspiration may be done to remove excess fluid buildup from a site of the body with bursitis. During this procedure, a fine needle is inserted into the site of bursitis and fluid is aspirated out. This helps to relieve pressure and discomfort from the site. 69) (D) A baker’s cyst is located behind the knee. A baker’s cyst is a fluid-filled cyst that causes a bulge and a feeling of tightness behind the knee. Since it is located behind the knee, it is also called a popliteal cyst. 70) (A) The anterior cruciate ligament (ACL) is the ligament that attaches the femur to the tibia. Image: Anterior cruciate ligament (ACL) 71) (B) Falls are the most common cause of hip fractures in the elderly. About 90% of hip fractures in the elderly are due to falls. 72) (C) The Lachman test checks for ACL injury. To perform the Lachman test on a patient, the patient’s knee is flexed to 20 to 30 degrees. The examiner should grasp the femur with one hand and the other hand is placed behind the proximal tibia. Then the examiner firmly pulls, as if attempting to displace the tibia from the femur. The examiner looks for the amount of anterior displacement from this pulling and checks the firmness of the end point. It’s always good to compare this with the other knee. If there is an increased displacement or a soft end point, this can be indicative of an ACL injury. Image: Lachman test 73) (D) Signs and symptoms of an ACL injury usually include a loud “pop” or a “popping” sensation in the knee (at the time of the injury), severe pain and the inability to continue activity, swelling that begins within a few hours, a feeling of instability or “giving way”, and a loss of range of motion. Walking, placing weight on the knee, would cause pain. Image: ACL injury 74) (C) A phalanx (plural: phalanges) refers to a bone of either the finger or toe. The phalanges are the bones that make up the fingers of the hands and the toes of the feet. There are 56 phalanges in the human body, with fourteen in each hand and foot. Each finger or toe has 3 phalanges, with the exception of the thumb and large toe, which contain only 2 phalanges. 75) (D) The MRI is the gold standard for checking for soft tissue injuries in the body, such as joint injury. X-rays are used for bone injuries such as bone fractures. Physical palpation would suggest injury but isn’t conclusive. 76) (C) There are 2 types of meniscus classifications: the medial meniscus and the lateral meniscus. The medial meniscus is the meniscus that is closer to the midline of the body. The lateral meniscus is the meniscus that is closer to the lateral part of the body (the extremities). McMurray’s test is a test that can check for a meniscus tear. It can be performed in 2 ways such that it can check for damage to the medial meniscus or the lateral meniscus. The test is performed by a combination of flexion and rotation of the knee. A positive finding for McMurray’s test is pain, or a clicking or a popping sound that occurs during examination. Image: Lateral and medial meniscus 77) (B) Tendons connect muscles to bone. Ligaments connect bone to bone. 78) (A) The meniscus is a type of rubbery, C-shaped cartilage disc that helps to cushion and stabilize the knees. Each knee has 2 menisci- one at the outer edge of the knee (the lateral meniscus) and the other at the inner edge of the knee (the medial meniscus). Besides acting to cushion the knees, the menisci help to keep the knee steady by balancing a person’s weight across the knee. It protects the bones from wear and tear. 79) (B) The meniscus, the C-shaped cartilage that provides cushioning and stability to the knee, is found between the femur and tibia bones. 80) (C) Meniscus tears are often characterized by pain and can be quite debilitating. Meniscus tears are common in contact sports and sports that require jumping such as volleyball and basketball. They happen often when a person changes direction suddenly while running and often occur at the same time as other knee injuries such as an ACL tear. Older athletes are at a higher risk for meniscus tears, since the meniscus weakens with age. A popping sensation is normally heard at the time of the injury. Symptoms of a meniscus tear include pain in the knee, swelling, and a tendency for the knee to lock up. The locking up of the knee is due to the shredded pieces of the meniscus (cartilage) that move into the knee joint, not allowing for full range of motion. 81) (A) Colles’ fracture is a fracture of the distal radius in the forearm with posterior displacement of the wrist. It is commonly seen in people with osteoporosis. It usually occurs due to a fall with outstretched hands. Falling with the wrists flexed would cause a Smith’s fracture. Image: Colles’ fracture 82) (C) Falling with the wrists in a flexed position would most likely lead to a Smith’s fracture. A Smith's fracture, also sometimes known as a reverse Colles’ fracture, is a fracture of the distal radius. It is caused by a direct blow to the dorsal forearm or falling onto flexed wrists, as opposed to a Colles' fracture which occurs as a result of falling onto wrists in extension. Smith's fractures are less common than Colles' fractures. The distal fracture fragment is displaced ventrally (forward toward the palm), as opposed to a Colles' fracture in which the fragment is displaced dorsally. Depending on the severity of the impact, there may be one or many fragments of broken bones. Image: Smith’s fracture 83) (D) Spondylolisthesis is a spinal disorder in which a vertebra slips forward over the bone below it. 84) (D) The sciatic nerve is the single largest nerve in the human body. 85) (D) Spondylolisthesis most commonly occurs in the lumbosacral vertebrae. 86) (A) Spondylolisthesis is definitively diagnosed through X-ray. X-rays will show one of the vertebrae displaced forward. CT scans and MRIs can also be done, but an X-ray is the simplest and most cost-effective way to diagnose spondylolisthesis. 87) (C) A spinal compression fracture is a fracture of a vertebra. 88) (C) The most common reason for a spinal compression fracture is osteoporosis. 89) (C) A herniated disk refers to a problem with one of the rubbery cushions (disks) between the individual bones (vertebrae) that stack up to make up the spine. A spinal disk is a disk with a softer center encased within a tougher exterior. Sometimes called a slipped disk or a ruptured disk, a herniated disk occurs when some of the disk protrudes out. Many people experience no symptoms from a herniated disk, but it can irritate nearby nerves and result in pain, numbness, or weakness in an arm or leg. Most herniated disks occur in the lower back (lumbar spine), although they can also occur in the thoracic or cervical spine. Most people who have a herniated disk don’t need surgery to correct the problem. 90) (A) Disk herniation is most often the result of a gradual, age-related wear and tear called disk degeneration. As a person ages, the spinal disks lose some of their water content; this makes them less flexible and more prone to tearing or rupturing with even a minor strain or twist. Most people can't pinpoint the exact cause of their herniated disk. Sometimes, using the back muscles instead of the leg and thigh muscles to lift large, heavy objects can lead to a herniated disk, as can twisting and turning while lifting. Rarely, a traumatic event such as a fall or a blow to the back can cause a herniated disk (source: mayoclinic.org). 91) (C) Factors that increase the risk of a herniated disk include being overweight or obese (excess body weight causes extra stress on the disks in the lower back), occupation (people with jobs that require repetitive lifting, pulling, pushing, bending sideways and twisting are at an increased risk for a herniated disk), and genetics (some people inherit a genetic predisposition to developing a herniated disk) (source: mayoclinic.org). 92) (B) Sciatica is really a medical symptom of an underlying medical condition and is not itself a diagnosis. Sciatica occurs when the sciatic nerve becomes pinched, usually by a herniated disc in the spine or by an overgrowth of bone (bone spur) on the vertebrae. More rarely, the nerve can be compressed by a tumor or damaged by a disease such as diabetes. Sciatica is pain radiating along the sciatic nerve, which is the nerve that starts from the lower back and runs down the leg. Sciatica causes pain from the lower back, through the buttocks, down the leg, and possibly into the foot and toes. It may be a sharp pain that may make it difficult to stand up or walk. It may cause weakness, numbness, burning, or searing pain. The pain may be worse when sitting due to the fact that the nerve is compressed in this position. The symptoms associated with sciatica normally takes place on one side of the body; rarely is it bilateral. Sciatica is most likely to develop around age 40 or 50; sciatica rarely occurs before age 20. 93) (D) Common causes of sciatica include a lumbar herniated disc, degenerative disc disease, spondylolisthesis, and spinal stenosis. More rarely, the nerve can be compressed by a tumor or damaged by a disease such as diabetes. Hypertension is not a cause of sciatica. 94) (C) Risk factors for sciatica include age (which can cause age-related changes in the spine such as herniated discs and bone spurs), obesity (increases stress on the spine which can trigger spinal changes), prolonged sitting, and diabetes (diabetes is notorious for nerve damage, which may include the sciatic nerve). Prolonged standing is not a risk factor for sciatica. 95) (B) Most cases of sciatica resolve with non-surgical treatment in a few weeks. Most often, only in severe cases does sciatica need surgical intervention. 96) (C) Internal tibial torsion is inward twisting of the tibia bone, which leads to intoeing of the foot. Internal tibial torsion is diagnosed in young children and is a common gait abnormality. Most children outgrow their internal tibial torsion without any treatment. In rare cases in which the condition doesn’t improve over time, surgery may be recommended to treat internal tibial torsion. There is no pain associated with internal tibial torsion. However, it may lead to a child having more frequent falls than normal due to the gait abnormality it causes. Image: Internal tibial torsion 97) (B) Internal tibial torsion may lead to a child having frequent falls due to the gait abnormality that it creates. Internal tibial torsion is not a condition characterized by pain. 98) (B) Bone spurs are associated with osteoarthritis. The main cause of bone spurs is joint damage associated with osteoarthritis. 99) (D) Most bone spurs cause no symptoms and may go undetected for years. If it does produce symptoms, it’s dependent on the place of the bone spurs. Bone spurs in the knee can make it painful to extend and bend the leg. Bone spurs in the spine can pinch the spinal cord or its nerve roots and can cause weakness or numbness in the arms or legs. Bone spurs in the hips can make it painful to move the hips. Bone spurs in the shoulders can make shoulder movements painful. 100) (C) Chondromalacia patellae is a condition in which the cartilage on the undersurface of the patella deteriorates and softens. Image: Chondromalacia patellae 101) (A) Chondromalacia patellae is also known as “runner’s knee”. It is a condition where the cartilage on the undersurface of the patella (kneecap) deteriorates and softens. It is common among young, athletic individuals, but may also occur in older adults who have arthritis of the knee. Chondromalacia patellae is often seen as an overuse injury in sports. Other times, it can be caused by improper knee alignment. Chondromalacia patella has also been called patellofemoral syndrome. 102) (B) Adolescents and young adults are at high risk for chondromalacia patellae. During growth spurts, the muscles and bones develop rapidly, which may contribute to short-term muscle imbalances. These imbalances can cause the kneecap to rub up against the thigh bone rather than against the cartilage of the thigh bone at the knee. This abnormal rubbing can lead to deterioration in the patella, resulting in chondromalacia patellae. 103) (B) Chondromalacia patellae typically presents with pain in the knee region (patellofemoral pain). In fact, the most common symptom of chondromalacia patellae is knee pain that worsens when walking up or down stairs, kneeling, or squatting. There may be sensation of grinding or cracking when bending or extending the knee. Pain may worsen after activities that apply extreme pressure on the knees, such as standing for an extended period of time or exercising. Swelling and tenderness may be present, as there is often friction between the patella and the femur. Chondromalacia patellae affects females more than males; this is because women possess less muscle mass than males, which can cause abnormal knee positioning. First-line treatment may include resting, stabilizing, and icing the joint. Since many times chondromalacia patellae is due to overuse such as from activity in sports, simply resting the knee can result in self-repair. 104) (D) Prolonged rest with the legs straight is least likely to aggravate pain in a person with chondromalacia patellae. Running will very likely aggravate pain. Pain may also be aggravated with prolonged standing, as there is great pressure on the knees. Prolonged sitting with the knees bent also will likely aggravate pain, as the knees being bent is a source of pressure. Resting with the legs straight puts the least pressure on the knees. 105) (C) Pain may be exacerbated by sitting with the knees flexed for a prolonged period of time, such as while watching a movie, hence leading to the terms "theater sign" and "movie-goer's knee." Patients with this condition often may prefer to sit at an aisle seat, where they may more frequently keep the knee extended. 106) (C) Most of the pain that is elicited in chondromalacia patellae is due to bone-to-bone grating or rubbing of the patella and femur bones. If the cartilage on the undersurface of the patella bone wears away, this presents direct bone-on-bone grating between the patella bone and the femur bone, which causes pain and discomfort. 107) (A) Genu varum is also known as bow-leggedness. Image: Genu varum 108) (C) The most common cause of genu varum (bow-leggedness) is rickets, a condition that prevents ossification of the bones. 109) (D) Genu varum (bow-leggedness) is a condition marked by the outward bowing of the lower leg in relation to the thigh. With genu varum, the knees stay wide apart when a person stands with the feet and ankles together. It is considered normal in children under the age of 18 months. Infants are born bowlegged because of their folded position in the mother’s womb. Bowed legs begin to straighten once the child starts to walk and the legs begin to bear weight (at about 12 to 18 months). If it persists after a child’s 3rd birthday, the child is called bowlegged. No treatment is recommended for bowed legs unless the condition is extreme. Special shoes, braces, or casts can be tried if the condition is severe. In most cases of genu varum, the outcome is good and most have no difficulties walking. Genu varum that persists and is left untreated leads to an increased risk for developing arthritis in the knees or hips over time. 110) (B) Genu valgam is also known as knock knees. This is because the knees are very close together when standing and often knock against each other. Image: Genu valgam 111) (D) Genu valgam is a condition in which the knees angle in and touch one another when the legs are straightened. 112) (A) It is normal for children to have genu valgam between the ages of 2 to 5. Almost all cases of genu valgam resolve as the child grows older naturally without treatment. If symptoms persist or worsen, treatment may be necessary. 113) (A) Pes planus is also known as flat feet. Image: Pes planus 114) (D) Pes planus (flat foot or flat feet) is a condition in which the longitudinal arch in the foot, which runs lengthwise along the sole of the foot (feet), has not developed normally and is lowered or flattened out. People who have flat feet rarely have symptoms or problems. Some people may have pain due to minor injury or excessive standing, walking, running, or poorly fitted footwear, but most have no symptoms. Pes planus can be inherited (condition existing at birth) or acquired such as through injury or conditions such as rheumatoid arthritis, stroke, or diabetes. Children as well as adults may be flat-footed. Most children are flat-footed until they are between the ages of 3 and 5 when their longitudinal arch develops normally. 115) (B) Pes planus is rarely treated in young children, since the foot arch usually develops normally by the age of 5. Treatment in adults generally consists of wearing spacious, comfortable shoes with good arch support. Padding for the heel (a heel cup) or orthotic shoe devices, which are molded pieces of rubber, leather, metal, plastic, or other synthetic material, are inserted into the shoe. They balance the foot in a neutral position and cushion the foot from excessive pounding. Surgery is rarely needed for pes planus. 116) (A) Pectus excavatum is a condition in which a person’s breastbone is sunken into his or her chest. For this reason, pectus excavatum is also referred to as sunken chest or funnel chest. Image: Pectus excavatum 117) (B) Pectus excavatum is a congenital chest wall deformity in which several ribs and the sternum grow abnormally, producing a concave, or caved-in, appearance in the anterior chest wall. Pectus excavatum is a common condition that occurs in an estimated 1 in 300-400 births, with a higher rate in males than females (in about a 3:1 ratio). The condition is typically noticed at birth, and more than 90% of cases are diagnosed within the first year of life. Pectus excavatum can progress in severity with growth spurts during adolescence and into adulthood in some cases. In mild cases, the only physical symptom of pectus excavatum is normally just a slight indentation in the chest (however, emotionally, it can cause self-image problems). Only in severe cases of pectus excavatum can the breastbone compress the lungs and/or the heart; this can reduce the amount of room the lungs have to expand and reduce the heart’s ability to pump efficiently. In this case, surgery may be done (source: emedicine.medscape.com). 118) (D) Pectus carinatum is a condition characterized by a protrusion of the sternum and ribs (which causes outward bulging). Because of this, pectus carinatum is also called pigeon chest. Image: Pectus carinatum 119) (B) Pectus excavatum is the most common type of congenital chest wall abnormality. About 90% of chest wall abnormalities are pectus excavatum. The second most common chest wall deformity is pectus carinatum, which makes up about 5-7% of congenital chest wall deformities (source: emedicine.medscape.com). 120) (C) Nursemaid’s elbow is a type of dislocation of the elbow joint in children. Nursemaid’s elbow is a partial dislocation of the elbow joint that happens when a ligament slips out of place near the elbow. 121) (B) Nursemaid’s elbow is also called pulled elbow, because the injury occurs due to pulling on the child’s arm. The medical term for the injury is radial head subluxation. Nursemaid's elbow often occurs when a caregiver holds a child's hand or wrist and pulls suddenly on the arm to avoid a dangerous situation or to help the child onto a step or curb. The injury may also occur during play when an older friend or family member swings a child around holding just the arms or hands. 122) (A) Nursemaid’s elbow is a common early childhood injury. It usually happens in children 1 to 4 years of age, but can happen any time from birth up to age 6 or 7 years old. This is because their ligaments (the muscle that holds bones together) are loose and their bones are not yet fully formed; this makes it easier for dislocation to occur. 123) (B) The treatment for nursemaid’s elbow is a procedure in which the doctor moves the bones back into the correct position (called reduction or reduction maneuver). 124) (D) Nursemaid’s elbow can be somewhat complex to detect, because it doesn’t really have any signs except for the child having pain and this pain doesn’t trigger off that a dislocation has necessarily occurred. The pain may be thought to be possibly due to a fall. There is no swelling or deformity, which would likely be present with a fracture. Therefore, if a child refuses to use the arm because the pain associated with its use and usually keeps it in a fixed straight position on his/her side (to minimize pain), this could be a sign that the child has suffered nursemaid’s elbow. 125) (B) Podagra is a painful condition of the big toe caused by gout. Gout is referred to at times as podagra when it affects the big toe joint. Podagra is a Greek work that translates to “foot trap”. 126) (B) Torticollis is a condition in which the neck muscles contract, causing the head to twist to one side. 127) (B) Carnett’s sign is a test that checks for pain in the abdominal wall. For this test, the patient is asked to lift the head and shoulders from the examination table or, as an alternative, to raise both legs with straight knees. If the pain gets worse, this is a positive Carnett’s sign, which increases the likelihood that the abdominal wall and not the abdominal cavity is the source of pain. A negative Carnett’s sign is said to occur when the abdominal pain decreases when the patient is asked to lift the head likely points to intra-abdominal cause of the pain. 128) (B) If the Carnett’s sign is elicited and it is positive, this is a sign that the source of pain is in the abdominal wall, rather than intra-abdominally. The rectus sheath is a muscle in the abdominal wall. A rectus sheath hematoma is the result of bleeding into the rectus sheath from damage to the superior or inferior epigastric arteries or their branches or from a direct tear of the rectus muscle. 129) (A) The first cervical vertebra is called the atlas (C1). 130) (B) The second cervical vertebra is called the axis (C2). 131) (C) The spine is made up of 33 vertebrae divided into 4 sections—the cervical vertebrae, the thoracic vertebrae, the lumbar vertebrae, and the sacrum and coccyx. The cervical vertebrae are composed of 7 vertebrae (C1-C7), the thoracic vertebrae are composed of 12 vertebrae (T1T12), the lumbar vertebrae are composed of 5 vertebrae (L1-L5), the sacral vertebrae are composed of 5 vertebrae (S1-S5) that are fused together, and the coccyx (also called the tailbone) is located at the base of the spine and is composed of four fused vertebrae. 132) (C) A rectus muscle tear is not caused by appendicitis. It is normally caused due to a vigorous workout or a sudden movement. Its happening is rare. A torn rectus muscle manifests as bleeding, swelling, and pain. A rectus muscle tear can be diagnosed by a CT scan. 133) (B) Atlantoaxial instability is defined as excessive movement between the first and second cervical vertebrae. 134) (C) In the majority of cases of thoracic outlet syndrome, pain is due to compression of nerves in the space between the collarbone and the first rib (thoracic outlet). This is type of thoracic outlet syndrome is referred to as neurogenic thoracic outlet syndrome (nTOS). 135) (B) Thoracic outlet syndrome is a group of disorders that occur when blood vessels or nerves in the space between the collar bone and the first rib (thoracic outlet) are compressed. This can cause pain in the shoulders and neck and numbness in the fingers. Causes of thoracic outlet syndrome include congenital anatomical defects (such as an extra rib above the first rib), poor posture (drooping of the shoulders or holding the head in a forward position), trauma (such as a car accident that causes internal changes that can compress the nerves in the thoracic outlet), repetitive activity (such as pitching in baseball or swimming), pressure on the joints (such as from obesity), and pregnancy (which can loosen the joints). Treatment for thoracic outlet syndrome usually involves physical therapy and pain relief measures. Most people improve with these approaches. In some cases, however, the doctor may recommend surgery. Credit: Photograph by BruceBlaus, distributed under the Creative Commons Attribution-Share Alike 4.0 International license 136) (C) Common causes of thoracic outlet syndrome include physical trauma (such as car accidents, sports-related injuries, etc.), certain anatomical defects (such as having an extra rib), and pregnancy. Rheumatoid arthritis is not associated with thoracic outlet syndrome. 137) (B) Thoracic outlet syndrome is most likely to occur in young adult females between the ages of 20 and 40 years old. Being female (females are far more likely to be diagnosed with thoracic outlet syndrome than males) and being between the ages of 20 and 40 years old are risk factors for thoracic outlet syndrome. 138) (C) A condition in which the knees hyperextend backwards is called genu recurvatum. Image: Genu recurvatum 139) (B) Genu recurvatum is a deformity in the knee joint that causes a backwards-bending knee. This causes an increased range of motion of the knee joint that can be mild, moderate or severe. The development of genu recurvatum may lead to knee pain and knee osteoarthritis. Genu recurvatum can be due to an injury that an athlete sustains that causes excessive backwards motion of the knee. It can be a difficult problem to treat. It can be caused by a congenital defect, certain diseases such as multiple sclerosis and muscular dystrophy, and irregularities in musculoskeletal structures such as joints, ligaments, and limbs around the knee area. 140) (A) Tandem gait is a method of walking where the toes of the back foot touch the heel of the front foot with each step. If a person is unable to do this, this can be a positive sign for many conditions such as a state of drunkenness. 141) (C) The Roos Stress test is also called the Elevated Arm Stress test. This test is specific to thoracic outlet syndrome. 142) (C) Among those with limb loss, the main causes are vascular disease (54%) including diabetes and peripheral arterial disease, trauma (45%), and cancer (less than 2%) (source: amputee-coalition.org). 143) (B) The Tinetti Gait and Balance Instrument is designed to determine an elderly person’s risk for falls within the next year. 144) (C) The Ottawa Ankle Rules is used to determine whether a patient needs radiographs of the injured ankle in the emergency department. The examination consists of a practitioner palpating the entire distal 6cm of the fibula and tibia. The examination also consists of the patient trying to walk. If there is bone tenderness at certain points on palpation or the patient is unable to take 4 complete steps (immediately after the injury and in the ED), then an ankle x-ray series is required. If there is no bone tenderness and the patient is able to bear weight, then an x-ray series is not warranted. The Ottawa Ankles Rules should not be used on patients younger than 18 years of age. 145) (B) Mastoiditis is an infection of the mastoid bone of the skull. The mastoid is located just behind the ear. Image: Mastoiditis Credit: Photograph by B. Welleschik, distributed under the Creative Commons Attribution-Share Alike 3.0 Unported license 146) (B) Mastoiditis is most often caused by a middle ear infection (acute otitis media). The infection may spread from the ear to the mastoid bone. The bone has a honeycomb-like structure that fills with infected material and may break down. The condition is most common in children. Before antibiotics, mastoiditis was one of the leading causes of death in children. This condition does not occur very often today and is also much less dangerous (source: medlineplus.gov). 147) (C) Septic arthritis, also known as infectious arthritis, is a condition characterized by the inflammation of a joint. It is usually caused by pathogens, such bacteria, fungi, or viruses, with bacteria being the most common causative agent. Typically, septic arthritis affects one large joint in the body, such as the knee or hip. Less frequently, septic arthritis can affect multiple joints. Septic arthritis is usually caused by an infection that spreads through the bloodstream from another area of the body. Young children and the elderly are most likely to develop septic arthritis. Septic arthritis is diagnosed through a procedure called an arthrocentesis. An arthrocentesis is a surgical procedure of the joint to draw a sample of joint fluid, known as synovial fluid. Normally this fluid is sterile and acts as a lubricant. With septic arthritis, the synovial fluid will have a high white blood cell count. The lab will also try to culture bacteria or other organisms from the synovial fluid to determine what pathogen is affecting the individual (if it is in fact septic arthritis) (source: webmd.com). 148) (B) Common bacteria that causes septic arthritis include Haemophilus influenza, staphylococcus bacteria, and streptococcus bacteria. Viruses that cause septic arthritis include hepatitis A, B, and C, parvovirus B19, herpes viruses, HIV, adenovirus, coxsackie viruses, and mumps. Fungi that can cause septic arthritis include Histoplasma, coccidiomyces, and blastomyces (source: webmd.com). 149) (B) Treatment for septic arthritis usually consists of antibiotics and arthrocentesis. Since septic arthritis is usually bacterial in origin, a combination of powerful antibiotics and drainage of the infected synovial fluid from the joint is used. Initially, empiric antibiotics are chosen to cover a wide range of infections. If the bacteria can be identified, antibiotics specific to that organism are used. It may take 4 to 6 weeks of treatment with antibiotics to ensure complete eradication of the infectious agents. Drainage of the infected area is critical for rapid clearing of the infection (source: webmd.com). 150) (C) Tenosynovitis is the inflammation of the fluid-filled sheath (called the synovium) that surrounds a tendon (the cord that joins muscle to bone). It is not inflammation of the tendon itself (that would be tendonitis). Inflammation of both often occurs simultaneously. 151) (A) Heberden’s nodes and Bouchard’s nodes are seen in osteoarthritis. 152) (C) Osteomyelitis is an infection of the bone. Infections can reach a bone by traveling through the bloodstream or spreading from nearby tissue. Infections can also begin in the bone itself if an injury exposes the bone to germs. In children, osteomyelitis most commonly affects the long bones of the legs and upper arms. Adults are more likely to develop osteomyelitis in the bones that make up the spine (the vertebrae). People who have diabetes may develop osteomyelitis in their feet if they have foot ulcers. Most people with osteomyelitis require surgery to remove parts of the bones that have died—followed by strong antibiotics, often delivered intravenously, typically for at least 4 to 6 weeks (source: mayoclinic.org). 153) (A) Most cases of osteomyelitis are caused by staphylococcus bacteria, types of germs commonly found on the skin or in the nose (source: mayoclinic.org). 154) (B) A bone biopsy is the gold standard for diagnosing osteomyelitis. If the source of the osteomyelitis is the bloodstream, blood tests can reveal elevated levels of white blood cells as well as what germs are to blame. However, the blood test would need to do be done in combination with other tests such as X-rays, CT scans, or MRIs, to see if there is involvement with bone. A bone biopsy is the gold standard because it reveals the extent of damage to the bone and what organisms are causing osteomyelitis directly from the source. 155) (C) Osteoarthritis is not a systemic infection. It is localized only to the affected areas (joints in the body). It will not cause systemic effects such as fever or involvement of other organs in the body. All of the other conditions listed- rheumatoid arthritis, ankylosing spondylitis, and lupus- are systemic and can have multiple organ involvement in the body. 156) (B) Swan neck deformity is a deformed position of the finger, in which the joint closest to the fingertip is permanently bent toward the palm, there is a straightening out (extension) of the middle joint, and the nearest joint to the palm is bent away from the palm. Swan neck deformity is seen most often in rheumatoid arthritis. The boutonnière deformity is very similar to the swan neck deformity, in that the joint closest to the fingertip is permanently bent toward the palm, while the nearest joint to the palm is bent away from the palm; however, with boutonnière deformity, there is no straightening out of the middle joint. Image: Swan neck deformity Credit: Photograph by User: Phoenix119, licensed under the Creative Commons AttributionShare Alike 3.0 Unported license Image: Boutonnière Deformity 157) (A) Osteoarthritis is most likely to have an onset in older adults after the age of 60. Osteoarthritis is caused by wear and tear on the joints, usually over several decades. Meanwhile, ankylosing spondylitis, rheumatoid arthritis, and gout normally have onsets before the age of 60. 158) (B) Kyphosis is the anterior-posterior curvature of the spine, while scoliosis is the lateral curvature of the spine. 159) (B) Acute limb ischemia occurs whenever there is a sudden lack blood flow to a limb. By definition, acute limb ischemia is a sudden lack of blood flow to a limb. 160) (D) Symptoms of peripheral arterial disease (PAD) may include intermittent claudication (leg pain when walking that is relieved by rest), gangrene on one or more toes (in severe situations), decreased or absent pulses in the leg and/or foot, increased capillary refill time, and bruits over partially blocked arteries. 161) (C) Skin changes associated with peripheral arterial disease include hair loss or slower hair growth on the legs and feet, shiny skin on the legs, skin that is cold to touch (the affected side is colder than the nonaffected side, if only one side is affected). Due to the lower-than-normal amount of blood flow, the color of the skin may change. Chapter 10- Respiratory System 1) What of the following statements is true regarding tuberculosis (TB)? A) TB is not a reportable disease. The CDC does not have to be contacted B) TB is a reportable disease and CDC should be notified C) A patient who has TB will be told to start medications STAT at home D) A person who is suspected of having TB will have to undergo comprehensive blood work for definitive confirmation 2) Which of the following is the most common site for a tuberculosis infection caused by the Mycobacteria tuberculosis? A) B) C) D) Kidneys Brain Lungs Adrenals 3) What action can be taken against noncompliant patients who refuse treatment for tuberculosis? A) Nothing. A person is free to refuse treatment B) The person can be fined for noncompliance by government agencies C) The person can be quarantined to protect the public D) The person will generally heal on his own over time from TB 4) Why is a person with tuberculosis normally started on multiple antitubercular drugs? A) Each drug has a different mechanism of action on the Mycobacteria tuberculosis B) Multiple drugs are used due to the high rates of resistance the bacteria have C) Multiple drugs speed up the time in which a person recovers from the illness D) Multiple drugs together produce less side effects than if one drug was used 5) What blood work should be done prior to a patient starting the antitubercular drug Isoniazid? A) WBC count with differential B) Platelet count C) RBC count D) Liver function test 6) All of the following are true about the Mantoux test except: A) The Mantoux test injects 0.1mL of purified protein derivative (PPD) into a person B) The Mantoux test is done subdermally C) The redness that the Mantoux test produces is the most important indicator of whether tuberculosis is present D) The Mantoux test should be assessed 48-72 hours after the injection to assess for tuberculosis 7) A diabetic has taken the Mantoux test to check for tuberculosis. In order to be considered a positive finding, the induration must be: A) B) C) D) ≥ 1mm ≥ 5mm ≥ 10mm ≥ 15mm 8) A Mantoux test with an induration of 5mm will be considered positive for tuberculosis in all of the following groups except for: A) Injection drug users B) Those with HIV C) Organ transplant receivers D) People who have been in close contact with a person who has active TB 9) A healthy person with no risk factors for tuberculosis has a positive finding for tuberculosis if the induration from the Mantoux test is: A) B) C) D) 5mm or greater 10mm or greater 15mm or greater 20 mm or greater 10) Which of the following individuals will be positive for tuberculosis only if the induration produced from the Mantoux test is 10mm or greater? A) A person who is HIV+ B) A person who is immunocompromised C) A person who has had a recent contact with infectious tuberculosis D) A homeless person 11) Which test is a blood test that is specific to check to see if a person is infected with the tuberculosis bacteria? A) B) C) D) Mantoux test QuantiFERON-TB Gold Antinuclear Antibody panel Rapid plasma regain test 12) Which of the following statements is false regarding miliary tuberculosis? A) Miliary TB is a potentially life-threatening type of tuberculosis that occurs when a large number of bacteria travel through the bloodstream and spread throughout the body B) Miliary TB is most common in children under 4 years of age, the elderly, and the immunocompromised C) A chest X-ray may show innumerable small white spots, which is typical of miliary TB D) Patients with miliary TB will always need a lung transplant in order to survive due to the scarring and degeneration that occurs in the lungs 13) All of the following are risk factors for developing pulmonary emboli except for: A) B) C) D) Atrial fibrillation COPD Estrogen use Prolonged inactivity 14) What is the gold standard for diagnosing pneumonia? A) Sputum culture B) Chest X-ray C) Urine sample D) Formation of mycobacterium antibodies 15) Which of the following statements is true regarding asthmatic patients? A) Every asthmatic patient should be on long-acting beta2-agonists B) Every asthmatic should be on some form of corticosteroids C) Every asthmatic should be on a leukotriene modifier D) Every asthmatic should be on a PRN short-acting beta2-agonist 16) Which of the following statements is false regarding the green zone of spirometer usage? A) The green zone is the zone that represents 80%-100% of expected volume a person should reach B) A person in the green zone will most likely need an increase in asthma medications C) The green zone is the desired zone where an asthma patient should be D) A person in the green zone does not have any symptoms of an asthma attack 17) Which of the following peak expiratory flow values puts a person in the yellow zone? A) B) C) D) 80% - 100% of expected volume 50% - 80% of expected volume 20% - 50% of expected volume 10% - 20% of expected volume 18) Which of the following peak expiratory flow values puts a person in the red zone? A) B) C) D) 80% - 100% of expected volume 50% - 80% of expected volume Below 50% of expected volume 10% - 20% of expected volume 19) Which of the following is not one of the factors used to calculate the expected peak expiratory flow? A) Weight B) Age C) Height D) Gender 20) Which type of asthma is the only one that doesn’t require the use of corticosteroids? A) B) C) D) Mild intermittent asthma Mild persistent asthma Moderate persistent asthma Severe persistent asthma 21) Which type of asthma has symptoms that occur more than twice a week but not daily? A) B) C) D) Mild intermittent asthma Mild persistent asthma Moderate persistent asthma Severe persistent asthma 22) Which type of asthma requires a daily oral corticosteroid? A) B) C) D) Mild intermittent asthma Mild persistent asthma Moderate persistent asthma Severe persistent asthma 23) Manufacturing of mast cell stabilizer drugs has been discontinued in the United States. What is now the recommended treatment instead? A) B) C) D) Short-acting beta2 agonists Inhaled corticosteroids Long-acting beta2 agonists Methylxanthines 24) Leukotriene antagonists are a type of: A) Long-acting bronchodilator B) Short-acting bronchodilator C) Anti-inflammatory agent D) Corticosteroid 25) All of the following are true regarding long-acting beta2-agonists except: A) Long-acting beta2-agonists are taken twice a day B) Long-acting beta2-agonists can be taken as rescue inhaler drugs C) Drugs that are long-acting beta2-agonists include Salmeterol and Formoterol D) Long-acting beta2-agonists are used daily for moderate to persistent asthma 26) Besides albuterol, what is another short-acting bronchodilator that can be used in emergency situations by asthmatics? A) B) C) D) Salmeterol Formoterol Levalbuterol Arformoterol 27) Long-acting beta2-agonists belong to what drug class? A) B) C) D) Corticosteroids Bronchodilators Leukotriene modifiers Methylxanthines 28) Mesothelioma that affects the lungs involves the: A) B) C) D) Bronchi Bronchioles Alveoli Pleural lining of the lungs 29) In which of the following populations would seeing a barrel chest be most abnormal in? A) Healthy children B) Healthy adults C) People with emphysema D) People with chronic bronchitis 30) What is the etiology of over 90% of cases of COPD? A) B) C) D) Inhaling dust Smoking Radon Asbestos 31) With emphysema, which type of percussion sound would most likely be heard over the lungs? A) B) C) D) Resonance Hyperresonance Flatness Nothing 32) Which is the most common form of sleep apnea? A) B) C) D) Obstructive sleep apnea Central sleep apnea Complex sleep apnea syndrome All are equally common 33) All of the following are common symptoms of sleep apnea except for: A) B) C) D) Loud snoring Episodes of breathing cessation Insomnia Nocturnal hypoglycemia 34) All of the following are risk factors for obstructive sleep apnea except for: A) Obesity B) Being female C) Older age D) Smoking 35) A doctor may recommend all of the following for cases of mild sleep apnea to improve symptoms except for: A) B) C) D) Prescribing treatment for allergies Sleeping earlier Losing weight Smoking cessation 36) During periods of breathing cessation of sleep apnea, all of the following occur except for: A) B) C) D) Oxygen saturation plummets Blood pressure increases Heart rate increases Blood pressure decreases 37) Which of the following will a sleep partner most likely observe in a person who has sleep apnea? A) Incessant talking and mumbling during sleep B) Periods of sleepwalking during the night C) Loud grunting noises through the night D) Loud snoring with periods of breathing cessation 38) The FEV1 represents the: A) Volume of air inhaled during the first second of forced inhalation B) Volume of air exhaled during the first second of forced expiration started from the level of total lung capacity C) Volume of air inhaled during maximum inhalation D) Volume of air exhaled during maximum expiration after taking the deepest breath possible 39) The maximum amount of air a person can expel from the lungs after a maximum inhalation is the: A) B) C) D) Tidal volume Inspiratory reserve volume Expiratory reserve volume Vital capacity 40) The FEV1/FVC ratio represents: A) The proportion of a person’s vital capacity that he or she is able to expire in the first second of forced expiration B) The maximum amount of oxygen a person can expel from the lungs after maximum inhalation C) The maximum amount of oxygen a person can inhale in a forced breath in 1 second D) The proportion of a person’s vital capacity that he or she is able to expire in the first 3 seconds of forced expiration 41) The FEV1/FVC ratio is used to: A) Stage lung cancer B) Diagnose obstructive and restrictive lung disease C) Predict mortality from lung disease D) Differentiate the types of COPD 42) In an individual with healthy lungs, what sound is heard over the lower lobes? A) B) C) D) Vesicular breath sounds Bronchial breath sounds Bronchovesicular breath sounds Nothing 43) In a healthy individual, what breath sounds are heard over the large airways? A) B) C) D) Vesicular breath sounds Bronchial breath sounds Bronchovesicular breath sounds Nothing 44) Which of the following statements is false regarding stridor? A) Stridor is caused by obstruction of the lower airway B) Stridor is a sign of respiratory distress C) Stridor is a high-pitched, harsh sound D) Stridor requires immediate treatment 45) Which adventitious sound can often be cleared through coughing? A) B) C) D) Rales Rhonchi Wheezing Stridor 46) A pneumomediastinum is a condition characterized by: A) B) C) D) A collapsed lung Air in between the lungs Fluid buildup in the lungs Pneumonia in one of the lungs 47) Which of the following statements is false regarding a pneumomediastinum? A) A pneumomediastinum is a normal finding B) A pneumomediastinum is caused by injury or disease C) The primary symptom of a pneumomediastinum is substernal chest pain D) The diagnosis of a pneumomediastinum is a chest X-ray 48) Which of the following statements is false regarding pertussis? A) Pertussis a respiratory disorder characterized by uncontrollable, violent coughing which often makes it difficult to breathe B) Pertussis is a highly contagious respiratory disease C) Pertussis can be very serious and even can be deadly D) No vaccination is currently available for pertussis 49) What is the most commonly used antibiotic for pertussis? A) B) C) D) Macrolides Penicillins Fluoroquinolones Cephalosporins 50) Which of the following statements is false? A) Bronchitis can be acute or chronic B) In most cases, acute bronchitis is viral in nature, but sometimes can be bacterial C) Chronic bronchitis and asthma are the two main types of COPD D) Smoking is a risk factor for developing chronic bronchitis 51) Which of the following statements is false regarding the Bacillus Calmette–Guérin (BCG) vaccine? A) BCG is a vaccine for tuberculosis B) BCG vaccination is used in many countries with a high prevalence of tuberculosis C) BCG vaccination is unlikely to cause a false-positive reaction to the Mantoux test D) BCG vaccination is unlikely to cause a false-positive reaction to the QuantiFERONTB test 52) A man comes into a clinic and says that he has had the BCG vaccine from his home country a few years ago. Which statement is true regarding the next steps that may be taken? A) The man can take the Mantoux test to test whether he is negative or positive for tuberculosis B) The man should not take the Mantoux test, as this will always produce positive results in those who have had the BCG vaccination C) The man should not take the Mantoux test and should instead just have a chest X-ray done to check for any signs of tuberculosis D) The man should take the Mantoux test, the QuantiFERON-TB test, and have a chest Xray done, since he had the BCG vaccine 53) For exercise-induced asthma conditions, what type of medication should be given 10 to 15 minutes before exercise? A) B) C) D) Short-acting beta2-agonist Long-acting beta2-agonist High-dose inhaled corticosteroid Leukotriene antagonist Respiratory System answers 1) (B) Tuberculosis is a communicable disease that must be reported to the CDC so that it doesn’t spread and lead to an outbreak. A person with TB is put on airborne precautions. This is why a healthcare worker entering the room of a person with TB must wear a fitted N95 mask for protection from transmission. A person with TB does not start medications at home. The person must go and receive treatment at a hospital. The most common definitive way of diagnosing tuberculosis is through a sputum culture. Therefore, comprehensive bloodwork is not a typical procedure for diagnosing TB. 2) (C) The lungs (85%) is the most common site of infection for the Mycobacteria tuberculosis. 3) (C) A person who is noncompliant and refuses treatment for tuberculosis can be quarantined to protect the public. Tuberculosis is a highly communicable disease that can lead to an outbreak with the public. Aggressive action must be taken to curb its spread. 4) (B) Multiple drugs are used to fight against tuberculosis because of the high rates of resistance that the Mycobacteria tuberculosis have. 5) (D) Before a person is started on any antitubercular drugs, s/he should have a baseline liver function test (LFT) done. All antitubercular drugs, including isoniazid, are hepatotoxic. Therefore, a person should have a baseline LFT done. And when treatment begins, further LFTs should be done to see if the liver is being affected by the drugs. 6) (C) The redness that the Mantoux test produces at the site is not an important indication of tuberculosis. The more important factor is the induration produced. 7) (C) A person with diabetes is at higher risk for active TB than a person with no known risk factors. So, while a person with no known risk factors must have an induration ≥ 15mm in order to be considered positive, a person with diabetes only needs an induration ≥ 10mm to be considered positive for TB. 8) (A) Injection drug users are considered positive for tuberculosis if they have an induration ≥ 10mm. People considered positive for tuberculosis with an induration ≥ 5mm are people with HIV, people who have received an organ transplant, those who are immunosuppressed (including those on steroid therapy), those who have been in close contact with a person who has active TB, and people who have changes on a chest X ray that looks like past TB. Those who are considered positive for TB with an induration ≥ 10mm are healthcare workers, injection drug users, people with a known negative test in the past 2 years, people with conditions that increase the risk of getting active TB such as those with diabetes or kidney failure, immigrants who have moved from a country with a high TB rate in the past 5 years, children under the age of 4, children or adolescents who are exposed to high-risk adults, and students and employees of certain group living settings, such as prisons, nursing homes, and homeless shelters. Those who are considered positive with an induration ≥ 15mm are individuals with no known risk factors for TB. 9) (C) A healthy individual with no risk factors for tuberculosis has a positive finding for tuberculosis if the induration from the Mantoux test is 15mm or greater. 10) (D) A homeless person without any other risk factors for TB would have a positive finding for TB if the induration from the Mantoux test is greater than or equal to 10mm. All the other options will be positive if the induration from the Mantoux test is greater than or equal to 5mm. 11) (B) The QuantiFERON-TB Gold test is a blood test that checks if a person is infected with mycobacterium tuberculosis bacteria. Realize that the QuantiFERON-TB test only detects if a person is infected with tuberculosis and cannot distinguish between latent and active infection. The Mantoux test is specific to tuberculosis, but it isn’t a blood test; it, too, like the QuantiFERON-TB test, cannot distinguish between latent and active infection. For these reasons, these tests are only used to screen for TB infection and cannot be used to diagnosis active infection. The Mycobacterium tuberculosis bacteria must be cultured from the patient, most often done through a sputum sample in order to make a definitive diagnosis of active TB infection. The Antinuclear Antibody (ANA) panel is a test that checks for certain autoimmune disorders such as systemic lupus erythematosus. 12) (D) Miliary tuberculosis is a potentially life-threatening type of tuberculosis that occurs when a large number of bacteria travel through the bloodstream and spread throughout the body. It is a contagious infection caused by the bacteria, Mycobacteria tuberculosis. Miliary tuberculosis is so named because of the innumerable tiny spots that form in the lungs that are the size of millets, the small round seeds in bird food. It is also referred to as disseminated tuberculosis, because it is often widespread throughout the entire body. Miliary TB occurs most often in children under 4 years of age, the elderly, and the immunocompromised. Though miliary TB can affect all organs of the body, it often affects the lungs, liver, and bone marrow; in certain cases, it can affect the meninges (tissues that cover the brain and spinal cord) and the pericardium (the outer layer of the heart). Symptoms are wide ranging and depend on which body organs are involved. General symptoms of TB may be present such as weight loss, night sweats, weakness, malaise, and difficulty breathing. If the bone marrow is involved, anemia and other hematological abnormalities may be present, which can mimic leukemia. Treatment for miliary TB is similar to that of pulmonary tuberculosis. Antibiotics are given for 6 to 9 months. If the meninges are affected, antibiotics are given for 9 to 12 months. Other drugs such as corticosteroids may be used. Surgery may also be necessary for certain complications. Image: Miliary tuberculosis 13) (B) Having COPD isn’t directly correlated with an increased risk for developing a pulmonary embolism. Risk factors for developing pulmonary emboli include atrial fibrillation, estrogen use, and prolonged inactivity. 14) (B) The gold standard for diagnosing pneumonia is through chest X-ray. The chest X-ray will show consolidation in the affected part of the lung. 15) (D) Every asthmatic should be on a PRN short-acting beta2-agonist such as albuterol sulfate. This is what is referred to as an asthma rescue drug. Every asthmatic should have it, whether the person has mild intermittent asthma, mild persistent asthma, moderate persistent asthma, or severe persistent asthma. 16) (B) A person in the green zone will either need to maintain his or her current medications or reduce medications. A person in the green zone is managing his or her asthma very well; therefore, medications either need to simply be maintained or may be reduced. An asthma action plan is based on zones defined either by a person’s symptoms, peak flow, or both. The green zone of the asthma action plan is where a person with asthma wants to be every day. The green zone represents a peak expiratory flow of 80% to 100% of the expected volume for the person. The expected volume is calculated based on a person’s height, age, and gender. If the person meets at least 80% of that expected outcome, that puts him or her in the green zone. Symptoms also factor into whether an asthmatic is in the green zone. Symptoms befitting of the green zone include the person not having any symptoms of an asthma attack, the person being able to do his or her usual activities, and the person being able to sleep without having symptoms. So, if a person has these qualifications and a peak expiratory flow of 80%-100%, the person is in the green zone of the asthma action plan. 17) (B) A peak expiratory flow of 50% - 80% puts a person in the yellow zone of the asthma action plan. The yellow zone is characterized by an acute exacerbation of asthma symptoms (asthma worsening) or that the asthma medications likely need to be increased (to keep the asthma in control, as the previous medications likely are not enough). Symptoms in the yellow zone may keep the person from doing his or her usual activities and may disturb sleep. Symptoms include coughing and wheezing, shortness of breath and chest tightness. 18) (C) A peak expiratory flow below 50% puts a person in the red zone of the asthma action plan. The red zone is characterized by severe asthma symptoms. Symptoms include shortness of breath while walking, talking, or at rest, retractions (using chest muscles to breathe), and wheezing. If a person is showing symptoms of the red zone, after all medications have been administered, 911 should be called. 19) (A) Weight is not considered when calculating the expected peak expiratory flow for a person. The factors considered to calculate the expected peak expiratory flow (PEF) are height, age, and gender (HAG). The following chart below, by no means, needs to be memorized but helps to remember and visualize peak expiratory flow and the factors that make it up. Image: Peak Expiratory Flow (Based on Height, Age, and Gender) (No need to memorize) Credit: By Mikael Häggström, used with permission 20) (A) Mild intermittent asthma (step 1) is the only type of asthma that doesn’t require the use of corticosteroids. The only medication used for mild intermittent asthma (the least severe type of asthma) is a rescue inhaler (a short-acting beta2-agonist such as albuterol). 21) (B) Mild intermittent asthma is characterized by symptoms (such as coughing and wheezing) 2 days or fewer a week. Mild persistent asthma is characterized by symptoms more than 2 times a week but not daily. Moderate persistent asthma is characterized by daily symptoms. Severe persistent asthma is characterized by symptoms that occur frequently throughout the entire day. 22) (D) Severe persistent asthma requires the use of an oral corticosteroid daily, usually prednisone, in addition to a high-dose inhaled corticosteroid. Mild intermittent asthma doesn’t require any corticosteroids. Mild persistent asthma usually has a low-dose inhaled corticosteroid prescribed. Moderate persistent asthma usually has a low-to-medium-dose inhaled corticosteroid. 23) (B) Mast cell stabilizer drugs have been discontinued in the United States. They were previously used for mild persistent asthma but now are unavailable. The recommended treatment now instead is inhaled corticosteroids, which are deemed superior anti-inflammatory drugs than mast cell stabilizers. This includes inhaled corticosteroids, such as fluticasone and budesonide. 24) (C) Leukotriene antagonists are a type of anti-inflammatory agent. It inhibits the action of leukotrienes (an inflammatory mediator) by blocking select receptor sites. 25) (B) Long-acting beta2-agonists are not used as rescue drugs for asthma. They are for longterm treatment. For short-term bronchodilation, a short-acting drug such as albuterol should be used. Long-acting beta2-agonists are taken twice a day and are used daily for moderate to persistent asthma. 26) (C) Besides albuterol, another short-acting bronchodilator that can be used by asthmatics in rescue situations is levalbuterol. Salmeterol, formoterol, and arformoterol are all long-acting bronchodilators and are not used as rescue drugs. 27) (B) Long-acting beta2-agonists are bronchodilators. Many times, they are combined with corticosteroids to produce a combination drug such as Advair and Symbicort. But the long-acting beta2-agonist by itself is a bronchodilator. 28) (D) Mesothelioma that affects the lungs affects the pleural lining of the lungs. It is a rare, aggressive type of cancer that can affect many parts of the body, though the lungs are the most commonly affected body part. 29) (B) A barrel chest would be most abnormal in a healthy adult. A barrel chest is a normal finding in a child. People who have COPD such as emphysema may develop a slight barrel chest in the later stages of the disease. It occurs because the lungs are chronically overinflated with air, so the rib cage stays partially expanded all of the time. 30) (B) Smoking is the leading cause of COPD and is linked to over 90% of COPD cases. 31) (B) With emphysema, the type of percussion sound that would most likely be heard over the lungs is hyperresonance. Hyperresonance results when there is too much air in the lungs. Resonance is the normal sound heard in health over air-filled lungs. Flatness would be heard over the lungs when there is presence of fluid or a solid mass, such as in pleural effusion, pneumonia, or with a tumor. 32) (A) The most common form of sleep apnea is obstructive sleep apnea, which occurs when the airway is blocked; this may be caused by the throat muscles relaxing and blocking the airway or something physically blocking the airways such as enlarged tonsils. Central sleep apnea is another form of sleep apnea that occurs when the brain doesn’t send proper signals to the muscles that control breathing. Complex sleep apnea syndrome is another form that occurs when someone has both obstructive sleep apnea and central sleep apnea. These are the 3 major forms of sleep apnea; all have common symptoms. The major difference is how they’re caused. 33) (D) Common symptoms of sleep apnea include loud snoring, episodes of breathing cessation during sleep, abrupt awakenings accompanied by shortness of breath, difficulty staying asleep (insomnia), daytime sleepiness (hypersomnia), and irritability. Nocturnal hypoglycemia is not associated with sleep apnea. 34) (B) Being male is a risk factor developing sleep apnea. Males are twice as likely to have sleep apnea than females. However, women increase their risk if they’re overweight and their risk appears to increase after menopause. Risk factors for sleep apnea include obesity (those who are obese are 4 times more at risk for sleep apnea than those with normal weight), neck circumference (people with thicker necks may have narrower airways), narrowed airway (may be naturally inherited or caused by enlarged tonsils or adenoids), being older (sleep apnea occurs significantly more often in older adults), family history, use of alcohol, sedatives, or tranquilizers (can relax the muscles of the throat), smoking (smokers have 3 times the risk of developing obstructive sleep apnea than nonsmokers), and nasal congestion (whether it’s an anatomical problem or allergies). 35) (B) Sleeping earlier is not an intervention that would improve the symptoms of sleep apnea. Instead, the underlying cause(s) needs to be addressed. For mild cases of sleep apnea, a practitioner may recommend lifestyle-only changes. These include losing weight, smoking cessation, and treatment of allergies so that the nasal passages are less congested. For moderate to severe cases of sleep apnea, the practitioner may recommend an airway pressure device such as CPAP or BIPAP. 36) (D) During an episode of breathing cessation during sleep apnea, oxygen saturation plummets, because the person isn’t breathing (taking in oxygen). As a mechanism to counter the low levels of oxygen, the body increases the blood pressure to pump blood throughout the body. For the same reason, the heart rate increases (to pump oxygen throughout the body). 37) (D) A partner of someone who has sleep apnea will most likely report loud snoring during sleep accompanied by periods of breathing cessation that typically last 10 to 20 seconds. 38) (B) The FEV1, standing for the forced expiratory volume, is the volume of air exhaled during the first second of a forced expiratory maneuver started from the level of total lung capacity. Image: Forced Expiratory Volume in 1 second (FEV1) 39) (D) The maximum amount of air a person can expel from the lungs after a maximum inhalation is the vital capacity. The vital capacity is equal to the sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume. A person’s vital capacity can be measured by a spirometer and can help make a diagnosis of an underlying lung disease, the severity of a lung disease, and monitor the progress of a lung disease. A normal adult has a vital capacity between 3 and 5 liters. 40) (A) The FEV1/FVC ratio is the proportion of a person’s vital capacity that s/he is able to expire in the first second of forced expiration. The FEV1 (forced expiratory volume) is the amount of air that a person can exhale during a forced breath in the first second. The FVC (forced vital capacity) is the total amount of air exhaled. Therefore, the FEV1/FVC ratio represents the air exhaled during the first second over the total amount of air exhaled (during the entire exhalation process). 41) (B) The FEV1/FVC ratio is used in the diagnosis of obstructive and restrictive lung disease. 42) (A) In an individual with healthy lungs, vesicular breath sounds are heard over the lower lobes of the respiratory system. With vesicular breath sounds, inspiration lasts longer than expiration. And sounds are louder with inspiration than at expiration. 43) (B) In a healthy individual, bronchial breath sounds are heard over the large airways. With bronchial breath sounds, expiration lasts longer than inspiration. With bronchovesicular breath sounds, inspiration and expiration are about the same in length. Bronchovesicular breath sounds are normal sounds heard in the mid-chest area or in the posterior chest between the scapula. Image: Respiratory sounds 44) (A) Stridor is caused by an obstruction of the upper airway. Stridor is a high-pitched harsh sound that is heard on inspiration. It is a sign of respiratory distress that requires immediate intervention. 45) (B) Rhonchi are adventitious breath sounds that can often be cleared through coughing. Rales (or crackles) are sounds associated with fluid in the airways or with fibrosis. Stridor is a high-pitched, inspiratory sound associated with upper airway obstruction. Wheezing are lowpitched sounds associated with bronchospasms. 46) (B) A pneumomediastinum is a condition characterized by air in between in the lungs (the mediastinum). The mediastinum is the space in the middle of the chest, between the lungs. 47) (A) A pneumomediastinum is air in the mediastinum. It is not a normal finding and indicates some type of injury or disease. It is most commonly caused by either esophageal rupture, alveolar rupture, or bowel rupture (where air in the abdominal cavity tracts up into the chest). The primary symptom is substernal chest pain. The diagnosis is confirmed by a chest X-ray, which will show air in the mediastinum. The condition can result from physical trauma or other situations that lead to air escaping from the lungs, airways, or bowel into the chest cavity. Treatment for a pneumomediastinum is based on the underlying cause. If caused by esophageal, bowel or tracheal perforation, surgery may be needed to repair the holes. For simpler cases, treatment is conservative. The tissues in the mediastinum will slowly resorb the air in the cavity. 48) (D) Pertussis is a respiratory disorder characterized by uncontrollable, violent coughing which often makes it difficult to breathe. It is a highly contagious disorder caused by the bacterium Bordetella pertussis. These bacteria attach to the cilia that line the part of the upper respiratory system. These bacteria release toxins, which damage the cilia and cause the airways to swell. After fits of many coughs, someone with pertussis often needs to take deep breaths which result in a “whooping” sound. Pertussis can affect people of all ages, but can be very serious, even deadly, for babies less than a year old. Pertussis is spread from person to person. People with pertussis usually spread the disease to another person by coughing or sneezing. Vaccination does exist for pertussis. In the United States, the recommended pertussis vaccine for babies and young children is called DTaP. This is a combination vaccine that helps protect against three diseases: diphtheria, tetanus and pertussis. Then there is a booster (called TDaP) for preteens, teens, and adults that provides protection against tetanus, diphtheria and pertussis. 49) (A) Macrolides are the most commonly prescribed antibiotic for pertussis. 50) (C) Often developing from a cold or other respiratory infection, acute bronchitis is very common. In most cases, acute bronchitis is viral in nature, but sometimes can be bacterial. Chronic bronchitis, a more serious condition, is a constant irritation or inflammation of the lining of the bronchial tubes, often due to smoking. People who have bronchitis often cough up thickened mucus. Emphysema and chronic bronchitis are the two main types of COPD (source: medlineplus.gov). 51) (C) BCG is a vaccine for tuberculosis. BCG vaccination is used in many countries with a high prevalence of tuberculosis to prevent childhood tuberculous meningitis and miliary disease. However, BCG is not generally recommended for use in the United States because of the low risk of infection with Mycobacterium tuberculosis, the variable effectiveness of the vaccine against adult pulmonary tuberculosis, and the vaccine’s potential interference with tuberculin skin test (TST) reactivity (the Mantoux test). The tuberculin skin test and blood tests to detect TB infection are not contraindicated for persons who have been vaccinated with BCG. BCG vaccination may cause a false-positive reaction to the TST. Blood tests to detect TB infection, unlike the TST, are not affected by prior BCG vaccination and are less likely to give a falsepositive result (source: cdc.gov). 52) (A) The man can take the Mantoux test to test whether he is negative or positive for tuberculosis. The BCG vaccine does not last forever and those who have gotten the BCG vaccine may test negative for tuberculosis through the Mantoux test. 53) (A) For exercise-induced asthma, the asthmatic should be pre-medicated 10 to 15 minutes before exercise with a short-acting beta2-agonist such as albuterol or levalbuterol. Chapter 11- Neurological System 1) Guillain-Barré syndrome directly affects the: A) B) C) D) Brain Central nervous system Peripheral nervous system Muscles 2) What is the definitive test done to check for Guillain-Barré syndrome? A) B) C) D) Blood test MRI Lumbar Puncture CT scan 3) How long does it normally take for a person to recover from Guillain-Barré Syndrome? A) About a week B) A few months to 1 year C) 2 years D) Never, Guillain-Barré is a permanent disease 4) Amyotrophic lateral sclerosis (ALS) is: A) B) C) D) Easily curable Difficult to cure Incurable and fatal Incurable but not fatal 5) What is normally the cause of death of a person who has amyotrophic lateral sclerosis (ALS)? A) Heart failure B) Respiratory arrest C) Liver dysfunction D) Sepsis 6) How long do people with amyotrophic lateral sclerosis (ALS) normally live once the disease has set in? A) B) C) D) They normally die within 6 months They normally die within 1 year They normally die within 5 years They normally die within 20 years 7) Which of the following statements is false regarding multiple sclerosis? A) Multiple sclerosis is a disabling condition involving the central nervous system B) Multiple sclerosis involves the demyelination of neurons C) Men are affected more than women D) There is no cure for multiple sclerosis 8) All of the following symptoms are associated with multiple sclerosis except for: A) Double vision B) Left ventricular hypertrophy C) Fatigue D) Tingling sensations in parts of the body 9) Parkinson’s disease is characterized by a lack of production of: A) B) C) D) Dopamine Acetylcholine Epinephrine Norepinephrine 10) All of the following are commonly seen in Parkinson’s disease except for: A) Shuffling gait B) Bradykinesia C) Microglia D) Seizures 11) What is the first-line medication for Parkinson’s disease? A) B) C) D) Interferon beta-1a Natalizumab Carbidopa-Levodopa Baclofen 12) Which of the following statements is true regarding the diagnosis of Parkinson’s disease? A) An MRI can be used to definitively diagnose Parkinson’s disease B) A CT scan can be used to definitively diagnose Parkinson’s disease C) A blood test can be used to definitively diagnose Parkinson’s disease D) There is no single test that is used to diagnose Parkinson’s disease 13) For a patient with chronic subdural hematoma, a likely finding would be: A) B) C) D) Previous ischemic stroke History of heart attack History of renal failure History of head trauma 14) All of the following are common symptoms of a chronic subdural hematoma except for: A) B) C) D) Headaches Gradual loss of cognitive ability Somnolence Deafness 15) Chronic subdural hematoma is most commonly found in: A) B) C) D) Children Adolescents Middle age adults Elderly 16) The Romberg test checks for: A) B) C) D) Balance and coordination Hearing Vision Knee stability 17) All of the following are positive signs of the Romberg test except for: A) The person falls down B) The person excessively sways C) The person keeps his feet close together to keep balance D) The person keeps his feet far apart to keep balance 18) Which of the following demonstrates Kernig’s sign? A) The NP flexes the patient’s knees at 90 degrees compared to the hips and then attempts to straighten the legs B) The NP flexes the patient’s neck toward the chest C) The NP tells the patient to touch his chest with the chin D) The NP taps the facial nerve of the patient 19) Which of the following demonstrates Brudzinski’s sign? A) The NP flexes the patient’s knees at 90 degrees compared to the hips and then attempts to straighten the legs B) The NP flexes the patient’s neck toward the chest C) The NP tells the patient to touch his chest with the chin D) The NP taps the facial nerve of the patient 20) What causes essential tremor? A) Parkinson’s disease B) Multiple sclerosis C) A problem originating in the nervous system D) Huntington disease 21) Which of the following statements is false regarding essential tremor? A) Essential tremor causes involuntary and rhythmic shaking B) It can affect almost any part of the body but occurs most often in the hands C) It occurs mostly when the person is at rest D) Essential tremor is usually not a dangerous condition 22) What is the first-line treatment for essential tremor? A) B) C) D) Beta blockers Corticosteroids Benzodiazepines DMARDs 23) What is the difference between the tremors associated with essential tremor and the tremors associated with Parkinson’s disease? A) Essential tremor usually occurs with purposeful activity, while Parkinson’s tremor usually occurs at rest B) Essential tremor usually occurs at rest, while Parkinson’s tremor usually occurs with purposeful activity C) Essential tremor and Parkinson’s tremor usually both occur at rest D) Essential tremor and Parkinson’s tremor usually both occur with purposeful activity 24) The Mini-Mental Status Examination (MMSE) is used to assess: A) B) C) D) Intelligence Creative thinking The cranial nerves Cognitive impairment 25) The Mini-Mental Status Examination (MMSE) is commonly used to assess for: A) Parkinson’s disease B) Multiple sclerosis C) Dementia D) B12 deficiency 26) Which of the following statements is false regarding seizures? A) Seizures occur when the electrical activity within the brain slows B) Focal or partial seizures occur when seizure activity is limited to a part of one hemisphere of the brain C) Generalized seizures occur when there is widespread seizure activity in the left and right hemispheres of the brain D) Atonic seizures are also known as drop attacks 27) Which of the following seizures most often results in falls? A) B) C) D) Absence seizures Atonic seizures Tonic-clonic seizures Myoclonic seizures 28) Which type of seizures is referred to as generalized seizures? A) B) C) D) Tonic-clonic seizures Clonic seizures Tonic seizures Myoclonic seizures 29) Which of the following statements is false regarding febrile seizures? A) Febrile seizures are seizures that are triggered by a fever B) Febrile seizures affect the adolescents ages 13-17 with the greatest frequency C) Febrile seizures aren’t linked to other health problems such as epilepsy or brain damage D) Children often lose consciousness during a febrile seizure 30) Which statement is true regarding tonic and clonic seizures? A) Tonic seizures are comprised of rigidity, while clonic seizures are comprised of jerking movements B) Clonic seizures are comprised of jerking movements, while tonic seizures are comprised of rigidity C) Tonic seizures are comprised of atony, while clonic seizures are comprised of jerking movements D) Clonic seizures are comprised of atony, while tonic seizures are comprised of jerking movements 31) All of the following medications may be used for status epilepticus except for: A) B) C) D) Levetiracetam Lorazepam Phenytoin Diazepam 32) Most transient ischemic attacks last: A) B) C) D) Less than 5 minutes Less than 15 minutes Less than 30 minutes Less than 60 minutes 33) Which of the following statements is false regarding a transient ischemic attack (TIA)? A) When a TIA is over, it usually causes no permanent injury to the brain B) Most strokes that occur are preceded by a transient ischemic attack C) A transient ischemic attack can be looked at as a warning that a stroke may happen at some point in the future D) A transient ischemic attack is a medical emergency 34) All of the following are symptoms of a stroke except for: A) B) C) D) Face drooping Facial twitching Arm weakness Speech difficulty 35) All of the following are risk factors for a stroke except for: A) B) C) D) Diabetes Hypertension Anemia Obesity 36) Which of the following statements is false regarding strokes? A) Blacks are at higher risk for strokes than whites B) Men are at higher risk for strokes than women C) Strokes are most common in the elderly D) A family history of strokes may put a person at higher risk for having a stroke 37) Tissue plasminogen activator (tPA) is given for: A) B) C) D) Hemorrhagic strokes Ischemic strokes Hyperlipidemia Hypertensive crisis 38) When should tissue plasminogen activator (tPA) be given for a stroke? A) Before the stroke begins B) As soon as possible after the onset of the stroke C) 12 hours after the onset of the stroke D) 24 hours after the onset of the stroke 39) A carotid endarterectomy: A) Removes a blood vessel that is blocked by a clot B) Adds a stent to a blood vessel C) Staples a ruptured vessel D) Removes plaque from a blood vessel 40) Which statement is false regarding hemorrhagic strokes? A) Hemorrhagic strokes account for about 15 percent of all strokes B) Hemorrhagic strokes account for about 40 percent of deaths from strokes C) An ultrasound will normally be used to determine whether the stroke is hemorrhagic or not D) The 2 types of hemorrhagic strokes are intracerebral hemorrhage and subarachnoid hemorrhage 41) Risk factors for a hemorrhagic stroke include all of the following except for: A) B) C) D) Hypercholesterolemia Hypertension Anticoagulant therapy Excessive alcohol consumption 42) All of the following statements are true regarding cerebrovascular accidents (CVA) except for: A) Most strokes are hemorrhagic strokes B) Atrial fibrillation is a risk factor for a stroke C) Symptoms include one-side facial paralysis, speech disturbances, and hemiparesis D) The 2 types of strokes are ischemic and hemorrhagic strokes 43) Homonymous hemianopsia is the: A) Complete loss of vision in one eye B) Complete loss of vision in both eyes C) Loss of vision in half of the visual fields of both eyes on the same side D) Clouding of vision of the eyes 44) The “ABCD2” stroke scoring system is a system used to calculate the risk of stroke in people who: A) Have high cholesterol and triglyceride levels B) Recently have had a transient ischemic attack (TIA) C) Have a high fall risk D) Have concurrent neuropathic pathologies 45) Which of the following is not one of the criteria used in the “ABCD2” stroke scoring system? A) B) C) D) Age Blood pressure Cholesterol Diabetes 46) All of the following are symptoms of attention deficit disorder (ADD) except for: A) B) C) D) Inattention Decreased cognitive ability Hyperactivity Impulsivity 47) Based on symptoms, a nurse practitioner suspects a patient may have cavernous sinus thrombosis. The nurse practitioner should refer the patient: A) B) C) D) To the ophthalmologist To the neurologist To the hematologist To the emergency room 48) An examiner asks a woman to shrug her shoulder. This examiner is checking the function of the patient’s cranial nerve: A) B) C) D) VIII IX X XI 49) Which cranial nerve is responsible for a person’s sense of smell? A) I B) II C) III D) V 50) Which cranial nerves are responsible for swallowing? A) B) C) D) V & VII VII & IX IX, X, & XII IX & VII 51) An examiner asks a patient to stick out her tongue. What cranial nerve is the examiner checking the function of? A) B) C) D) V VII IX XII 52) The examiner asks a patient to chew. The examiner is checking the function of cranial nerve: A) B) C) D) V VII IX XII 53) Which 3 cranial nerves are responsible for eye movement? A) B) C) D) I, II, III III, V, VI III, IV, V III, IV, VI 54) An examiner takes a cotton applicator and wisps it slightly across the patient’s eye to elicit the corneal reflex. The examiner is testing the patient’s cranial nerve: A) III B) IV C) V D) VI 55) Which cranial nerve is the cranial nerve of facial expressions such as smiling and frowning? A) B) C) D) V VII X XI 56) Which cranial nerve is responsible for sweet, sour, and bitter taste to the anterior tongue? A) B) C) D) VII IX X XII 57) An examiner tests the reflex of a patient’s leg and gets a very brisk response. The examiner should chart this reflex as: A) B) C) D) 1+ 2+ 3+ 4+ 58) Which of the following statements is false regarding trigeminal neuralgia? A) Trigeminal neuralgia is characterized by the onset of sudden, sharp pain B) Trigeminal neuralgia is usually unilateral C) Trigeminal neuralgia primarily affects adolescents D) The pain associated with trigeminal neuralgia is normally set off by triggers such as touching certain parts of the face, chewing, or laughing 59) Trigeminal neuralgia is caused most often due to: A) History of frequent, chronic headaches B) A traumatic head injury C) Brain tumor D) Compression of the trigeminal nerve by an artery 60) Which statement is true about the trigeminal nerve? A) The trigeminal nerve has 1 branch: the ophthalmic nerve B) The trigeminal nerve has 2 branches: the ophthalmic nerve and the maxillary nerve C) The trigeminal nerve has 3 branches: the ophthalmic nerve, the maxillary nerve, and the mandibular nerve D) The trigeminal nerve has 4 branches: the ophthalmic nerve, the maxillary nerve, the olfactory nerve, and the mandibular nerve 61) Symptoms of trigeminal neuralgia typically begin between the ages of: A) B) C) D) 10-20 years 20-40 years 40-60 years 60-80 years 62) What is the main drug class used to treat trigeminal neuralgia? A) B) C) D) Steroids Anticonvulsants DMARDs Benzodiazepines 63) Kernicterus is a serious condition in which a child can have irreversible brain damage due to excess: A) B) C) D) Uric acid Bilirubin Ammonia Creatinine 64) The weber or rinne test is used to check cranial nerve: A) B) C) D) I II IV VIII 65) The Snellen test is used to check cranial nerve: A) B) C) D) I II III IV 66) What is aphasia? A) A disorder characterized by the inability to perform particular, purposeful actions, as a result of brain damage B) A language disorder that affects a person's ability to communicate, as a result of brain damage C) A disorder characterized by an inability to recognize and identify objects or persons D) A partial or total loss of memory 67) What is apraxia? A) A disorder characterized by the inability to perform particular, purposeful actions, as a result of brain damage B) A language disorder that affects a person's ability to communicate, as a result of brain damage C) A disorder characterized by an inability to recognize and identify objects or persons, typically as a result of brain damage D) A partial or total loss of memory 68) What is Broca’s aphasia? A) A type of aphasia in which an individual has difficulty understanding language in its written or spoken form B) A type of aphasia in which an individual has trouble speaking fluently C) A type of aphasia in which an individual has trouble speaking fluently and trouble understanding language in its written or spoken form D) A type of aphasia in which a person has the lost the ability to communicate in his or her native language 69) Broca’s aphasia is also known as: A) B) C) D) Fluent aphasia Receptive aphasia Expressive aphasia Wernicke’s aphasia 70) What is Wernicke’s aphasia? A) A type of aphasia in which an individual has difficulty understanding language in its written or spoken form B) A type of aphasia in which an individual has trouble speaking fluently C) A type of aphasia in which an individual has trouble speaking fluently and trouble understanding language in its written or spoken form D) A type of aphasia in which a person has the lost the ability to communicate in his or her native language 71) Wernicke’s aphasia is also known as: A) B) C) D) Non-fluent aphasia Receptive aphasia Expressive aphasia Broca’s aphasia 72) What is global aphasia? A) A type of aphasia in which an individual has difficulty understanding language in its written or spoken form B) A type of aphasia in which an individual has trouble speaking fluently C) A type of aphasia in which an individual has trouble speaking fluently and trouble understanding language in its written or spoken form D) A type of aphasia in which a person has the lost the ability to communicate in his or her native language 73) Which of the following statements is false regarding aphasia? A) Aphasia occurs with damage to the left hemisphere of the brain B) Damage to the frontal lobe of the left hemisphere can result in receptive aphasia C) Damage to the front and back regions of the left hemisphere of the brain can cause global aphasia D) Aphasia results in language deficits 74) Bell’s palsy is a type of: A) B) C) D) Leg paralysis Facial paralysis Neck paralysis Shoulder paralysis 75) In Bell’s Palsy, there is damage to cranial nerve: A) B) C) D) IV V VII IX 76) What is the cause of Bell’s palsy? A) Bell’s palsy occurs when cerebellum of the brain becomes inflamed B) Bell’s palsy occurs when the 7th cranial nerve becomes swollen or compressed C) Bell’s palsy occurs when the pineal gland in the brain becomes overactive D) Bell’s palsy occurs when the pituitary gland becomes overactive 77) All of the following are common symptoms of Bell’s palsy except for: A) B) C) D) Drooping on one half of the face Altered sense of taste Decreased mental acuity Drooling 78) Which of the following statements is true about Bell’s palsy? A) Most people with Bell’s palsy recover completely without treatment in a few months B) Bell’s Palsy is usually a permanent, lifelong disability C) Bell’s palsy usually requires antibiotics for a person to make a full and quick recovery D) Bell’s palsy can alter a person’s taste but doesn’t affect a person’s hearing 79) How can Bell’s palsy affect a person’s eyes? A) It frequently leads to retinal detachment B) It frequently leads to cataracts C) It frequently leads to glaucoma D) It can cause abnormal tear production, causing either excessive tear production or a lack of tear production 80) Which is the most commonly prescribed and effective medication for treating Bell’s palsy? A) B) C) D) Ibuprofen Meloxicam Prednisone Acyclovir 81) What is the most common artery in the brain where aneurysms occur? A) B) C) D) Anterior cerebral artery Middle cerebral artery Posterior cerebral artery Inferior parietal artery 82) What is the most common trigger for benign paroxysmal positional vertigo (BPPV)? A) Standing up B) Lifting one’s hands C) Specific changes in the position of the head D) Specific changes in the position of the legs 83) Benign paroxysmal positional vertigo is characterized by: A) Brief episodes of mild to intense dizziness B) Episodes of mild to intense dizziness that last about 30 minutes at a time C) Episodes of mild to intense dizziness that last normally an hour D Episodes of mild to intense dizziness that is chronic and lasts all day long 84) Benign paroxysmal positional vertigo may present with: A) B) C) D) Cholesteatomas Nystagmus Increased intracranial pressure Cluster headaches 85) What complication can benign paroxysmal positional vertigo lead to? A) B) C) D) Deafness Damage to the inner ear Blindness Falls 86) Which of the following statements is false regarding restless leg syndrome (RLS)? A) RLS is characterized by a nearly irresistible urge to move the legs B) By moving their legs, people with RLS relieve their discomfort C) RLS is characterized by throbbing, pulling, creeping, or other unpleasant sensations in the legs D) RLS is an acute condition, normally lasting less than a month 87) Symptoms of restless leg syndrome occur primarily: A) B) C) D) In the morning In the afternoons During the day At night 88) Which of the following statements is false regarding restless leg syndrome? A) It occurs about twice as often in women than in men B) It is a very common condition C) It can occur at any age, though symptoms tend to be more severe in middle age or later D) In most cases, restlessness leg syndrome is caused due to traumatic brain injury 89) People with restless leg syndrome often have: A) B) C) D) High blood sugar High blood pressure Hyperlipidemia Sleep problems 90) How is restless leg syndrome diagnosed? A) B) C) D) MRI of the brain Serum markers Review of symptoms Cranial nerves examination 91) Which of the following statements is false regarding clonus? A) Clonus is a series of involuntary, rhythmic, muscular contractions and relaxations B) Clonus is usually initiated by a reflex C) Clonus is a sign of an underlying heart problem D) Clonus is most commonly found at the ankle, specifically with a dorsiflexion/plantar flexion movement 92) Which of the following patients would clonus be least likely to be seen in? A) A patient who has suffered a stroke B) A patient who has varicella C) A patient who has multiple sclerosis D) A patient with a severed spinal cord 93) What is the most common type of dementia? A) B) C) D) Alzheimer’s Dementia with Lewy bodies Vascular dementia Dementia from Parkinson's disease 94) Dementia caused by conditions that block or reduce blood flow to the brain is termed: A) B) C) D) Vascular dementia Dementia from Parkinson's disease Dementia with Lewy bodies Creutzfeldt-Jakob disease. 95) Which of the following statements is false regarding Alzheimer’s disease? A) Alzheimer’s disease occurs due to physical changes in the brain, including a buildup of certain proteins, which causes damage to the nerve cells B) Those with Alzheimer’s live an average of 8 years after diagnosis of the illness C) Alzheimer’s is part of the normal aging process D) Alzheimer’s is a progressive disease 96) Alzheimer’s disease is chiefly caused due to: A) B) C) D) Demyelination of nerves Destruction of nerve cells Lack of production of nerve cells Proliferation of nerve cells 97) Which of the following statements is false regarding Alzheimer’s disease? A) There is no cure for Alzheimer’s disease B) Current drugs used to treat Alzheimer’s disease can slow the progression of the disease C) The greatest known risk factor for Alzheimer’s is increasing age D) The most common early symptom of Alzheimer's is difficulty remembering newly learned information 98) Which of the following statements is true regard delirium and dementia? A) Delirium is reversible, while most cases of dementia are irreversible B) Delirium is irreversible, while most cases of dementia are reversible C) Both delirium and dementia are reversible D) Both delirium and dementia are irreversible 99) Delirium is referred to as the: A) B) C) D) Acute confusional state Chronic confusional state Acute hyperactive state Chronic hyperactive state 100) Sundowning in an individual with dementia produces: A) B) C) D) Complete tiredness and a sleepy state Increased agitation or confusion An acute state of diaphoresis Acute panic attacks 101) Which of the following statements is false regarding the sundowning syndrome seen with dementia? A) Having rooms well-lit can combat the effects of sundowning B) Sundowning usually resolves by the morning C) Sundowning recurs commonly D) Changing the environment frequently can help lessen the severity of sundowning syndrome 102) Which of the following is true about a patient in the late stage of Alzheimer’s disease? A) Patients need partial or complete care for activities of daily living B) Patients lose the ability to talk C) Patients usually need a pacemaker to be inserted D) Patient are usually intubated and hooked up to ventilators 103) People with dementia normally die due to: A) B) C) D) Respiratory arrest Stroke Renal failure Pneumonia 104) Cholinesterase inhibitors, such as donepezil, for Alzheimer’s work to increase the amount of: A) B) C) D) Dopamine in the brain Serotonin in the brain Norepinephrine in the brain Acetylcholine in the brain 105) Which of the following is true about diagnosing dementia? A) Dementia can be diagnosed with an MRI of the brain B) Dementia can be diagnosed by certain serum markers C) Dementia is diagnosed by a neurological exam D) Dementia is diagnosed based on a range of medical tests and a person’s medical history 106) Common symptoms of dementia with Lewy bodies include all of the following except: A) B) C) D) Visual hallucinations Parkinsonism Seizures Markedly fluctuating cognition 107) The heel-to-shin test tests the: A) Frontal lobe function B) Parietal lobe function C) Brainstem function D) Cerebellar function 108) All of the following are common symptoms of a basilar skull fracture except for: A) B) C) D) Raccoon eyes Rhinorrhea Autonomic dysreflexia Battle sign 109) Deep tendon reflexes are controlled by the: A) B) C) D) Brainstem Spinal nerves Cranial nerve X Cranial nerve XI 110) Which of the following statements is false regarding reflexes? A) Primitive reflexes are also called stretch reflexes B) Primitive reflexes are present at birth in full-term newborns and most disappear in the first few months of life C) In premature infants, some primitive reflexes may not be present or may be weak D) Primitive reflexes are controlled by the brainstem 111) Which statement is false about deep tendon reflexes? A) Deep tendon reflexes are voluntary movements that occur in response a stimulus B) Deep tendon reflexes provide information about the communication between the central nervous system and the peripheral nervous system C) A decreased reflex response usually indicates a problem with the peripheral nervous system D) A brisk or exaggerated reflex response indicates a problem with the central nervous system 112) Which of the following statements is false regarding the Achilles reflex? A) The Achilles reflex can be checked by tapping the Achilles tendon while the foot is dorsiflexed B) A positive result for the Achilles reflex would be the jerking of the foot towards its plantar surface C) The Achilles reflex checks the spinal nerves L1 and L2 D) The Achilles reflex is also known as the ankle jerk reflex 113) Which of the following statements is false regarding the patellar reflex? A) The patellar reflex can be checked with a person being in the sitting position and tapping right below the kneecap B) The sharp tap on the patellar tendon slightly stretches the quadriceps C) The patellar reflex checks the spinal nerves L2, L3, and L4 D) The patellar reflex is also known as the plantar reflex 114) Which reflex checks spinal nerves L5, S1, and S2? A) B) C) D) Biceps reflex Triceps reflex Babinski reflex Patellar reflex 115) Reflexes of the arms and fingers test spinal nerves in the: A) B) C) D) Cervical plexus Thoracic plexus Lumbar plexus Sacral plexus 116) Which is the most severe type of spina bifida? A) B) C) D) Myelomeningocele Meningocele Spina bifida occulta They are all equally severe 117) Which of the following is a condition in which most of the brain does not develop? A) B) C) D) Spina bifida Anencephaly Microcephaly Encephalocele 118) Which of the following is false regarding cluster headaches? A) Cluster headaches often cause vomiting B) Cluster headaches occur more commonly in males than in females C) Cluster headaches typically cause pain around the eye D) The pain from cluster headaches is one-sided 119) What treatment is used for cluster headaches? A) B) C) D) Tylenol Ibuprofen High-dose oxygen No treatment available 120) Migraine headaches typically last anywhere from: A) B) C) D) 2 to 4 hours 8 to 12 hours 12 to 24 hours 4 to 72 hours 121) Which of the following statements is false regarding migraine headaches? A) Migraine headaches affect men about 3 times as much as women B) Migraine headaches are one of the most common problems seen in ERs and doctor’s offices C) Classic migraines are usually more severe than common migraines D) Common migraines are migraines that have no aura before the headache 122) Which of the following statements is false regarding migraine headaches? A) Migraine headaches are always preceded by an aura B) Migraine headaches are described as pounding, throbbing headaches C) Migraine headaches may be accompanied by nausea, vomiting, and extreme sensitivity to light or sound D) Migraine attacks can cause significant pain and last for hours to days 123) Common precipitating factors for migraine headaches include all of the following except for: A) B) C) D) Monosodium glutamate (MSG) Milk Caffeine Aspartame 124) Which of the following medications may be used for prophylaxis of migraine headaches? A) B) C) D) Prednisone Propranolol Pseudoephedrine Lorazepam 125) All of the following drug classes may be used for migraine headache prophylaxis except for: A) B) C) D) Beta blockers Benzodiazepines Anticonvulsants Tricyclic antidepressants 126) Status migrainosus is a migraine headache that lasts longer than A) B) C) D) 1 day 2 days 3 days 5 days 127) Which type of headache is commonly described as the most painful type of headache? A) B) C) D) Migraine headaches Tension headaches Sinus headaches Cluster headaches 128) What is the most common trigger for muscle tension headaches? A) B) C) D) Stress Smoking Certain foods Loud noises 129) All of the following characterize tension headaches except for: A) Dull, aching head pain B) Sharp, stabbing pain behind the eye C) Sensation of tightness or pressure across the forehead or on the sides and back of the head D) Tenderness of the scalp, neck, and shoulder muscles 130) Which of the following statements is false regarding tension headaches? A) It is usually bilateral B) It is usually accompanied by nausea and vomiting C) It isn’t usually associated with visual disturbances D) Physical activity does not make tension headaches worse 131) A woman comes into a clinic and complains of a headache that is characterized by a throbbing pain on both sides of her head. Which type of headache is she most likely suffering from? A) Migraine headaches B) Tension headaches C) Cluster headaches D) Sinus headaches 132) Which type of headache may be accompanied by tearing, eye drooping, and nasal congestion? A) B) C) D) Migraine headaches Tension headaches Sinus headaches Cluster headaches 133) What is the most common type of headache? A) B) C) D) Migraine headaches Tension headaches Cluster headaches Sinus headaches 134) Which type of headache is usually mild or moderate? A) B) C) D) Migraine headaches Tension headaches Cluster headaches Sinus headaches 135) Sumatriptan is used for: A) The prophylaxis of migraine headaches B) During an acute episode of a migraine headache C) For the prophylaxis and an acute episode of a migraine headache D) For the prophylaxis of tension headaches 136) Basilar migraines originate in the: A) Frontal lobe B) Temporal lobe C) Occipital lobe D) Brainstem 137) Which of the following statements is false regarding a basilar migraine? A) Symptoms of a basilar migraine include dizziness, double vision, and lack of coordination B) Basilar migraines are preceded by an aura that can occur about 10 to 45 minutes before the onset of head pain C) This type of migraine is very fleeting and usually lasts less than 5 minutes D) This migraine may mimic more serious conditions, such as seizures, stroke, meningitis or brain tumors 138) Which of the following conditions is characterized by trouble with reading despite normal intelligence? A) B) C) D) Agraphia Alexia Aphasia Agnosia 139) Which of the following statements is false regarding Munchausen syndrome? A) Munchausen syndrome is a mental disorder in which a person repeatedly and deliberately acts as if he/she has a physical or mental illness when really not sick B) Munchausen is considered a mental illness C) Most of the symptoms that a person with Munchausen syndrome complains of are mental disorders D) Munchausen syndrome is most often found in young adults 140) Factitious disorder by proxy is a condition in which a person: A) Fakes a physical illness B) Fakes a mental illness C) Lies that s/he is healthy when s/he is really ill D) Acts as if a person in his or her care has an illness when the person really does not Neurological System answers 1) (C) Guillain-Barré syndrome (GBS) is a disorder in which the body's immune system attacks part of the peripheral nervous system. The first symptoms of this disorder include varying degrees of weakness or tingling sensations in the legs. In many instances, the symmetrical weakness and abnormal sensations spread to the arms and upper body. These symptoms can increase in intensity until certain muscles cannot be used at all and, when severe, the person is almost totally paralyzed. In these cases, the disorder is life threatening - potentially interfering with breathing and, at times, with blood pressure or heart rate - and is considered a medical emergency (source: ninds.nih.gov). 2) (C) A lumbar puncture is the definitive test to check for Guillain-Barré syndrome. 3) (B) It normally takes a few months to a year for a person to recover from Guillain-Barré syndrome. Most individuals, however, have good recovery from even the most severe cases of Guillain-Barré syndrome, although some continue to have a certain degree of weakness (source: ninds.nih.gov). 4) (C) ALS is incurable and fatal. Amyotrophic lateral sclerosis (ALS), also called Lou Gehrig's disease, is a rapidly progressive, invariably fatal neurological disease that attacks the nerve cells (neurons) responsible for controlling voluntary muscles (muscle action we are able to control, such as those in the arms, legs, and face). The disease belongs to a group of disorders known as motor neuron diseases, which are characterized by the gradual degeneration and death of motor neurons. Eventually, all muscles under voluntary control are affected, and individuals lose their strength and the ability to move their arms, legs, and body. When muscles in the diaphragm and chest wall fail, people lose the ability to breathe without ventilation support. Most people with ALS die from respiratory failure, usually within 3 to 5 years from the onset of symptoms. However, about 10 percent of those with ALS survive for 10 or more years (source: ninds.nih.gov). 5) (B) Normally the cause of death of a person who has ALS is respiratory arrest. Due to the fact that ALS causes degeneration of all the muscles in the body, people with ALS lose the ability to breathe and die of respiratory arrest. 6) (C) Most people with ALS die from respiratory failure, usually within 3 to 5 years from the onset of symptoms (source: ninds.nih.gov). 7) (C) Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system). In MS, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between the brain and the rest of the body. Eventually, the disease can cause the nerves themselves to deteriorate or become permanently damaged. Signs and symptoms of MS vary widely and depend on the amount of nerve damage done and which nerves are affected. It can affect a variety of things from a person’s gait to a person’s vision. Women are about twice as likely as men are to develop MS. There's no cure for multiple sclerosis. However, treatments can help speed recovery from attacks, modify the course of the disease and manage symptoms (source: mayoclinic.org). 8) (B) MS symptoms can vary widely and depend on the amount of nerve damage done and which nerves are affected. Symptoms may include numbness or weakness in one or more limbs, partial or complete loss of vision (usually in one eye at a time, often with pain during eye movement), double vision, tingling or pain in parts of the body, electric-shock sensations that occur with certain neck movements, especially bending the neck forward (Lhermitte sign), tremor, lack of coordination or unsteady gait, slurred speech, fatigue, dizziness, and problems with bowel and bladder function. Most people with MS have a relapsing-remitting disease course. They experience periods of symptoms or relapses that develop over days or weeks. These relapses are followed by quiet periods of disease remission that can last months or even years (source: mayoclinic.org). 9) (A) Parkinson’s disease is a progressive disorder of the nervous system that affects movement; it is characterized by a lack of dopamine. 10) (D) Symptoms of Parkinson’s disease include a tremor (especially in the hands or fingers and especially when the hand is at rest), bradykinesia (over time, Parkinson’s disease may reduce the ability to move and slow one’s movement), rigidity (muscle stiffness), impaired posture and balance (posture may become stooped and a person may develop balance problems as a result of Parkinson’s disease), loss of movements (such as decreased ability to blink or smile, which can cause a blank affect), speech changes (that can produce monotone speech), and writing changes (can cause small handwriting called microglia). 11) (C) The first-line medication for Parkinson’s disease is carbidopa-levodopa (Sinemet). 12) (D) No specific test exists to diagnose Parkinson's disease. A neurologist will diagnose Parkinson's disease based on a person’s medical history, a review of his/her signs and symptoms, and a neurological and physical examination. The neurologist may order tests, such as blood tests, to rule out other conditions that may be causing the symptoms. Imaging tests — such as MRI, ultrasound of the brain, SPECT and PET scans — may also be used to help rule out other disorders. In addition to the examination, the doctor may give the person carbidopa-levodopa, a Parkinson's disease medication. A sufficient dose may be given to show the benefit, as low doses for a day or two aren't reliable. Significant improvement with this medication will often confirm the diagnosis of Parkinson's disease. Sometimes it takes time to diagnose Parkinson's disease. Regular follow-up appointments may be recommended with neurologists trained in movement disorders to evaluate a person’s condition and symptoms over time to diagnose Parkinson's disease (source: mayoclinic.org). 13) (D) A history of head trauma would be the most likely finding for a patient with chronic subdural hematoma. In most cases, head trauma, such as from a fall that results in a head injury, creates the hematoma that can bleed slowly over time. 14) (D) Common symptoms of a chronic subdural hematoma include headaches, gradual loss of cognitive ability, somnolence, confusion, change in behavior, dizziness, and weakness. Seizures, nausea and vomiting may also be seen. 15) (D) Chronic subdural hematomas are most commonly found in the elderly. 16) (A) The Romberg test checks for balance and coordination ability. 17) (C) During the Romberg test, the patient is told to stand with his arms/hands straight on each side and with the feet together first with his eyes open and then with his eyes closed. If the patient is able to keep his balance without falling down or excessively swaying, while keeping his feet close together, it is a negative Romberg test. If the person has to keep his feet far apart to maintain balance, it is a positive Romberg test. 18) (A) Kernig’s sign is performed by flexing the patient’s knees at 90 degrees with the hips and attempting to straighten the legs. Resistance to leg straightening is a positive sign of meningeal irritation. 19) (B) Brudzinski’s sign is performed by the NP flexing the patient’s neck toward the chest. The NP will take his or her hand and place it behind the patient’s head and move it slowly toward the chest. If the patient reflexively flexes the hips in response to this movement (to relieve pain), this is a positive sign of meningeal irritation. The first option is Kernig’s sign, which also checks for meningeal irritation. The third option, telling the patient to touch his chest with his chin, is a test to check for nuchal rigidity. If the person is unable to touch the chest secondary to pain, this is a positive sign of nuchal rigidity. The fourth option, tapping the facial nerve of a patient, is Chvostek’s sign, which checks for hypocalcemia. 20) (C) Essential tremor is caused by a problem originating in the nervous system. Other medical conditions don’t cause essential tremor. 21) (C) Essential tremor is a nervous system disorder that causes involuntary and rhythmic shaking. It can affect almost any part of the body but trembling most often occurs in the hands. Tremors most often occur when the person is doing purposeful activity, not at rest; it is an action tremor. It is usually not a dangerous condition, but it typically worsens over time and can be severe in some people. Essential tremor can occur at any age but is most common in people age 40 and older. 22) (A) The first-line treatment for essential tremor is beta blockers. The most common beta blocker prescribed for essential tremor is propranolol. 23) (A) The tremors associated with essential tremor usually occur with purposeful activity, while the tremors associated with Parkinson’s disease usually occur at rest. 24) (D) The MMSE is used to test for cognitive impairment. 25) (C) The Folstein Mini-Mental Status Examination (MMSE) is commonly used to assess for dementia. It is a brief screening test to assess for cognitive impairment. Six subject areas are tested for. These include orientation, attention and calculation, recall, writing a sentence, following a three-stage command, and copying a design. 26) (A) Seizures occur when the electrical activity of the brain is abnormal and rapid. Focal or partial seizures occur when seizure activity is limited to a part of one hemisphere of the brain. Generalized seizures occur when there is widespread seizure activity in the left and right hemispheres of the brain. Atonic seizures are also known as drop attacks because the person suddenly loses muscle tone and, thus, drops (falls) down. 27) (B) Atonic seizures (also called akinetic seizures) are characterized by a few seconds in which muscle tone is lost. The loss of muscle tone frequently results in falls. The prefix a- means without. Tonic means tone. So, without tone means the person loses muscle tone and can easily fall. 28) (A) Tonic-clonic seizures are referred to as generalized seizures. 29) (B) Febrile seizures are seizures that occur in young children and are triggered by a fever. It affects children between the ages of 6 months and 5 years old the most frequently. The fever may accompany common childhood illnesses such as a cold or the flu. Febrile seizures most often occur while a child has a fever above 101°F (38.3°C); however, in some cases, a child may not have a fever at the time of the seizure but will develop one a few hours later. Most often during a febrile seizure, a child loses consciousness and his arms and legs will shake uncontrollably. Most febrile seizures last only for a few minutes. They do not cause any long-term health problems such as epilepsy or brain damage. 30) (A) Tonic seizures are comprised of rigidity, while clonic seizures are comprised of rhythmic jerking of the extremities. Generalized seizures, also known as tonic-clonic seizures, are comprised of both (tonic) rigidity and jerking (clonic) movements. 31) (A) Antiepileptic drugs such as lorazepam, diazepam, phenytoin, and phenobarbital may be used for status epilepticus. Levetiracetam would not be used in status epilepticus. 32) (A) Most transient ischemic attacks (TIAs) last less than 5 minutes; the average is about a minute. 33) (B) The vast majority of strokes that occur are not preceded by a transient ischemic attack, though about a third of people who experience a transient ischemic attack go on to have a stroke within a year. Therefore, a TIA can be looked at as a warning sign that a stroke may happen at some point in the future. A TIA usually doesn’t cause any permanent injury to the brain due to its fleeting nature. Any time a person exhibits stroke-like symptoms, whether from a TIA or a stroke, it should be viewed as a medical emergency. There is no way of knowing during an episode whether it’s a TIA or a stroke; therefore, there should no difference in response in how TIAs and strokes are handled. 34) (B) Facial twitching is not a symptom associated with strokes. The mnemonic FAST is an easy way to remember the symptoms of a stroke and the action to take. “F” stands for face drooping. “A” stands for arm weakness. “S” stands for speech difficulty. “T” stands for time to call 911 (since all strokes and TIAs are medical emergencies). Other signs can include weakness, especially on one side of the body, sudden confusion, trouble seeing in one or both eyes, sudden trouble with walking and balance and coordination, and a sudden severe headache with no known cause. 35) (C) Risk factors for a stroke include hypertension, diabetes, heart disease, smoking, old age, personal or family history of a stroke or TIA, brain aneurysms or arteriovenous malformations (AVMs), alcohol and illegal drug use, certain medical conditions such as sickle cell disease, vasculitis, or bleeding disorders, lack of physical activity, obesity, stress, hypocholesteremia, and unhealthy diet (source: National Heart, Lung, and Blood Institute). 36) (B) Each year, women have more strokes than men, and women die more often than men from strokes. Factors that influence this include pregnancy, use of birth control pills, history of preeclampsia/eclampsia, gestational diabetes, oral contraceptive use, smoking, and postmenopausal hormone therapy. Blacks are at higher risk for strokes than whites. Strokes are most common in the elderly population. A family history of strokes may put a person at higher risk for having a stroke. 37) (B) Tissue plasminogen activator (tPA) is given for ischemic strokes. It is given through an IV in the arm. tPA works by dissolving the clot (causing the blockage), thus, improving blood flow to the part of the brain that previously was deprived of blood. 38) (B) A tissue plasminogen activator (tPA) should be given as soon as possible after the onset of a stroke. It should be given no more than 3 hours after the onset of a stroke. Certain patients, however, those under 80 years of age who aren’t taking anticoagulants and have no history of stroke and diabetes, may benefit from tPA up to 4.5 hours after the onset of the stroke. tPA is not given before a stroke begins, since it is not given prophylactically. 39) (D) A carotid endarterectomy removes atherosclerotic plaque built up on the walls of the carotid artery, as a way of preventing a future stroke. 40) (C) Usually, a CT scan or an MRI will be done to check whether the stroke is a hemorrhagic stroke or not. An angiogram also may be ordered. A CT scan is the fastest way for a facility to check whether the stroke is hemorrhagic or not, so that is usually what is ordered. Hemorrhagic strokes occur in about 15 percent of all strokes, yet make up 40 percent of all stroke deaths. The 2 types of hemorrhagic strokes are intracerebral hemorrhage and subarachnoid hemorrhage. Intracerebral hemorrhage, which is bleeding within the brain, is more common. Subarachnoid hemorrhage is bleeding on top of the brain (between the brain and the tissues that cover the brain). 41) (A) Hypercholesterolemia is a risk factor for ischemic stroke, not hemorrhagic stroke. Risk factors for hemorrhagic strokes include hypertension, excessive alcohol and drug use, anticoagulant therapy, and certain blood disorders such as sickle cell anemia. 42) (A) The 2 types of strokes are ischemic (also called embolic) strokes and hemorrhagic strokes. The majority of strokes are ischemic strokes (about 80%). Hemorrhagic strokes account for the minority of strokes (about 20%). Atrial fibrillation is a risk factor for a stroke, because it increases the risk for the formation of blood clots. Symptoms of a stroke include one-sided facial paralysis, speech disturbances, and hemiparesis. 43) (C) Homonymous hemianopsia is a loss of vision in half of the visual fields of both eyes on the same side. It is most frequently caused in stroke and traumatic brain injuries. Image: Left-sided hemianopsia Credit: Photograph by Nunh-huh, licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license 44) (B) The “ABCD2” stroke scoring system is a system used to calculate the risk of stroke in people who recently have had a transient ischemic attack (TIA). The system is used to predict the risk of the patient having a stroke in the following days of the TIA. 45) (C) Cholesterol is not one of the criteria used in the “ABCD2” stroke scoring system. “A” stands for age. If the person is 60 years or older, this person is at a higher risk for stroke. “B” stands for blood pressure. If the systolic blood pressure is greater than 140 mmHg or the diastolic blood pressure is greater than 90 mmHg, the person is at an increased risk for a stroke. “C” stands for clinical features. These features include unilateral weakness and speech disturbance, which put a patient at an increased risk for a stroke. The first “D” stands for diabetes, which is another risk factor for a stroke. The second “D” stands for the duration of the transient ischemic attack which took place. Depending on how long the TIA occurred for determines the risk for having a stroke. A TIA which lasted for 60 minutes or longer represents the greatest risk for having a stroke for this category. 46) (B) The 3 cardinal signs of attention deficit disorder (ADD) include inattention, hyperactivity, and impulsivity. 47) (D) Cavernous sinus thrombosis is a medical emergency. The patient should be referred to the emergency room (ER) if a practitioner suspects a patient has it. It is an illness that requires high-dose antibiotics and may require surgery. Surgery may be needed to drain the site of the initial infection. 48) (D) By asking the woman to shrug her shoulders, the examiner is checking the function of the patient’s cranial nerve XI, the spinal accessory nerve. 49) (A) Cranial nerve I (the olfactory nerve) is responsible for a person’s sense of smell. One very popular mnemonic for cranial nerves is Oh Oh Oh, To Touch And Feel Very Good Velvet, Such Heaven. The first 3 words in this mnemonic begin with an “O”. So how can you differentiate them? Remember that we have 1 nose; therefore, cranial nerve I is the olfactory nerve. We have 2 eyes; therefore, cranial nerve II is the optic nerve. Therefore, the last cranial nerve that begins with the letter “O” must be the oculomotor nerve (cranial nerve III), which aids in eye movement. Cranial nerve IV is the trochlear nerve, which controls the inward and downward movement of the eye. Cranial nerve V is the trigeminal nerve. The trigeminal nerve is responsible for sensations in the face and motor functions such as biting and chewing. Cranial nerve VI is the abducens nerve, which controls the lateral movement of the eyes away from the nose (lateral abduction of the eyes). Cranial nerve VII is the facial nerve, which controls the muscles of facial expression and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue and oral cavity. Cranial nerve VIII is the vestibulocochlear nerve, which is responsible for the sense of hearing and balance. Cranial nerve IX is the glossopharyngeal nerve, which is the nerve that conveys taste sensations from the posterior one-third of the tongue, aids in swallowing, and senses carotid blood pressure. Cranial nerve X is the vagus nerve, which is the nerve that senses aortic blood pressure, slows heart rate, stimulates digestive organs, and aids in swallowing. Cranial nerve XI is the spinal accessory nerve, which controls muscles responsible for moving the shoulders. Cranial nerve XII is the hypoglossal nerve, which controls tongue movements. 50) (C) Cranial nerves IX (the glossopharyngeal nerve), the X (the vagus nerve), and XII (the hypoglossal nerve) are responsible for swallowing. 51) (D) By asking a patient to stick out her tongue, the examiner is checking cranial nerve XII (the hypoglossal nerve). The hypoglossal nerve is responsible for movement of the tongue such as sticking the tongue out of the mouth. 52) (A) Cranial nerve V (the trigeminal nerve) is responsible for facial movements such as biting and chewing. 53) (D) Cranial nerves III (oculomotor), IV (trochlear), and VI (abducens) are responsible for eye movement. The oculomotor nerve innervates muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the muscles that enable pupillary constriction and accommodation (ability to focus on near objects as in reading). The oculomotor nerve is responsible for the majority of eye and eyelid movements, although the trochlear nerve and abducens nerve also contribute to eye movement. The trochlear nerve is a motor nerve which controls the downward and inward movement of the eye. The abducens nerve is a motor nerve, which moves the eyes laterally away from the nose. 54) (C) The corneal reflex (also referred to as the blink reflex) is an involuntary blinking of the eyelids elicited by stimulation of the cornea (i.e., touching the surface of the cornea such as with a cotton applicator). The purpose of this reflex is to protect the eyes from foreign bodies as well as bright light. This reflex is elicited due to cranial nerve V (the trigeminal nerve). Therefore, the examiner is testing cranial nerve V. 55) (B) Cranial nerve VII, the facial nerve, is the nerve of facial expressions; this includes expressions such as smiling and frowning. 56) (A) Cranial nerve VII, the facial nerve, is responsible for taste on the anterior 2/3rd of the tongue. The glossopharyngeal nerve is responsible for taste on the posterior 1/3rd of the tongue. 57) (D) According to the grading response of reflexes, no reflex response is a score of 0, a slight response is a score of 1+, a normal response is a score of 2+, a very brisk response is a score of 3+, and a repeating reflex, or clonus, is a score of 4+. 58) (C) Trigeminal neuralgia primarily affects older adults, typically peaking in the 60s (7th decade of life). Trigeminal neuralgia is more common in older adults due to the fact that it is caused most often due to elongation of the arteries. This elongation causes compression against the trigeminal nerve. This elongation takes time to occur, which is why it’s seen most often in older adults. The compression against the trigeminal nerve causes the nerve to become degraded; it degrades the insulation of the nerve, allowing for the nerve to short circuit. This is what causes the sudden, sharp, electric shock-like pain of trigeminal neuralgia. Trigeminal neuralgia is a disorder characterized by attacks of sudden, sharp, stabbing pain. In between attacks, the person is normally asymptomatic. Some people with trigeminal neuralgia can have hundreds of attacks within the course of one day. Trigeminal neuralgia was once called the “suicide disease” because of the numerous numbers of people taking their own lives before (more) effective treatments were discovered. 59) (D) Trigeminal neuralgia is caused most often due to some compression on the trigeminal nerve. Usually this compression is caused by an artery compressing on the trigeminal nerve. Usually this artery is the superior cerebellar artery. Less commonly, trigeminal neuralgia can be caused by compression due to a tumor in the head. Image: Artery compressing trigeminal nerve 60) (C) The trigeminal nerve has 3 branches or divisions. These are nerves that branch off of the trigeminal nerve: the ophthalmic nerve, the maxillary nerve, and the mandibular nerve. Simplified, the ophthalmic nerve involves the eyes and the forehead. The maxillary nerve involves the cheeks. And the mandibular nerve involves the jaw. Most times, the pain starts in the 2nd or 3rd division. Credit: Photograph by Madhero88, licensed under the Creative Commons Attribution 3.0 Unported license 61) (C) Typically, the onset of symptoms of trigeminal neuralgia begin between the ages of 40 and 60, peaking in the 60s. 62) (B) The main drug class used to treat trigeminal neuralgia is anticonvulsants. This includes drugs such as carbamazepine (Tegretol), phenytoin (Dilantin), and pregabalin (Lyrica). Usually, the patient is started on a low dose that is increased over time. 63) (B) Kernicterus is a serious condition due to excess bilirubin that can cause irreversible brain damage in a child. 64) (D) The weber or rinne test is used to check cranial nerve VIII, the vestibulocochlear nerve. Weber and rinne tests check a person’s hearing. 65) (B) The Snellen test is used to check cranial nerve II, the optic nerve. The Snellen test is a test to check a person’s vision. 66) (B) Aphasia is a language disorder that affects a person’s ability to communicate, either to understand language or formulate language. This can be spoken or written language. 67) (A) Apraxia is a disorder characterized by the inability to perform particular, purposeful actions, as a result of brain damage. 68) (B) Broca’s aphasia is a type of aphasia in which an individual has trouble speaking fluently. For this reason, it is also referred to as expressive aphasia. 69) (C) Broca’s aphasia is also known as expressive aphasia. It is called expressive aphasia because the person has problems expressing him or herself, but no problem understanding someone’s speech. 70) (A) Wernicke’s aphasia is a type of aphasia in which an individual has difficulty understanding language in its written or spoken form. For this reason, Wernicke’s aphasia is also referred to as receptive aphasia. 71) (B) Wernicke’s aphasia is also known as receptive aphasia. This is because a person is unable to receive (or understand) language (either written or spoken). 72) (C) Global aphasia is a type of aphasia in which an individual has trouble speaking fluently and trouble understanding language in its written or spoken form. So, basically, global aphasia includes both Broca’s and Wernicke’s aphasia. 73) (B) Damage to the frontal lobe of the left hemisphere of the brain can result in expressive aphasia. Broca’s area is located in the frontal lobe of the left hemisphere. Wernicke’s area is located in the back end of the temporal lobe on the left hemisphere. Damage to Wernicke’s area can result in receptive aphasia. And damage to both the front and back regions of the brain on the left hemisphere can cause global aphasia. Image: Areas of Broca’s and Wernicke’s aphasia 74) (B) Bell’s palsy is a type of facial paralysis characterized by muscle weakness on one side of the face. 75) (C) In Bell’s palsy, there is damage to cranial nerve VII, the facial nerve. 76) (B) Bell’s palsy is a condition that occurs when the 7th cranial nerve, the facial nerve, becomes swollen or compressed; this results in facial weakness and paralysis. Why the 7th cranial nerve becomes inflamed is unknown, but the medical community believes that bell’s palsy is triggered by a viral infection. 77) (C) Bell’s palsy is caused by damage or compression to the 7th cranial nerve, not the brain; so, it is not associated with any mental deficits. Common symptoms of Bell’s palsy include drooping on one side of the face, inability to open or close the eye on the affected side, difficulty eating and drinking, inability to make facial expressions such as smiling and frowning, facial weakness, muscle twitching on the face, abnormal tear production (either too much or too little) in the affected eye, headache, and sensitivity to sound. 78) (A) Most people with Bell’s palsy recover completely, without treatment, in a few months. Though people who have a severe case of Bell’s palsy may have permanent damage such as permanent facial muscle weakness, the majority recover completely within a few months. The origin of Bell’s palsy is usually linked to viral infections, so antibiotics are not effective in treating it. Bell’s palsy can cause altered taste and cause an increased sensitivity to sound. 79) (D) Bell’s palsy can cause abnormal tear production, causing either excessive tear production or a lack of tear production. A lack of tear production can cause the eye to be dry. Therefore, in this case, an eye lubricant would be given to prevent corneal drying. 80) (C) Prednisone is commonly prescribed and is the medication that is most effective for treating Bell’s palsy. This is especially true when it is given soon after the onset of symptoms (within 3 days). Acyclovir, though sometimes prescribed for Bell’s palsy, has been shown to be of little effectiveness. 81) (A) The anterior cerebral artery is the most common artery where aneurysms occur in the brain. Images: Arteries of the brain 82) (C) Benign paroxysmal positional vertigo (BPPV) is vertigo that occurs due to changes in position. BPPV is usually triggered by specific changes in the position of the head. This might occur when the head is tipped up or down, when a person lies down, or when a person turns over or sits up in bed. 83) (A) Benign paroxysmal positional vertigo is characterized by brief episodes of mild to intense dizziness. The episodes are very short in duration. This is why it’s called paroxysmal, which means fleeting or temporary. Episodes come quickly and go quickly. 84) (B) Benign paroxysmal positional vertigo may present with nystagmus, involuntary movements of the eyes from side to side. 85) (D) Benign paroxysmal positional vertigo (BPPV) is rarely serious and rarely leads to health complications. However, due to the vertigo, it puts a person at risk for falls. 86) (D) Restless leg syndrome (RLS) is a neurological disorder characterized by throbbing, pulling, creeping or other unpleasant sensations in the legs and an uncontrollable, sometimes overwhelming, urge to move them. It is a chronic condition that can last for years or be lifelong. RLS can be managed but there is no cure. The person moving their legs relieves the discomfort associated with this syndrome. 87) (D) Symptoms of restless leg syndrome occur primarily at night when a person is relaxing or increase in severity during the night if symptoms are occurring during the day. The most distinctive aspect of this syndrome is that lying down and trying to relax triggers symptoms (restlessness). Symptoms of RLS are generally absent or negligible in the morning. 88) (D) In most cases, the cause of restless leg syndrome is unknown. It is believed to have a genetic component, as restless leg syndrome is often found in families where the onset of symptoms is before age 40. Other evidence suggests that a low level of iron in the brain may be responsible for RLS. RLS is a very common condition, affecting millions of adults in the United States and about 1 million children. RLS occurs with about twice as much frequency in women than in men. RLS can occur at any age, though symptoms tend to be more severe in middle age or later. 89) (D) People with restless leg syndrome often have sleep problems. Most people with RLS have difficulty falling asleep and staying asleep. This can cause exhaustion and daytime fatigue. Thus, it can have a big impact on a person’s personal life, such as their work life and activities of daily living. It can also lead to concentration problems and impaired memory. More than 80% of people experience periodic limb movement of sleep (PLMS). PLMS is characterized by involuntary leg twitching or jerking movements during sleep that happen less than every minute, sometimes throughout the night; this can cause repeated awakening and sleep disturbance. 90) (C) Restless leg syndrome is diagnosed through a review of symptoms. There is no specific test conducted such as an MRI or a blood test that can be used to diagnose RLS. The practitioner will look for 4 basic criteria: if symptoms are worse at night and are absent or negligible in the morning, if there is a strong and often overwhelming need or urge to move the affected limb(s), often associated with paresthesia (abnormal sensations) or dysesthesia (unpleasant abnormal sensations), sensory symptoms that are triggered by rest, relaxation, or sleep, and sensory symptoms that are relieved with movement and the relief persists as long as the movement continues. The presence of these symptoms in a person is a strong indicator of RLS. 91) (C) Clonus is a series of involuntary, rhythmic, muscular contractions and relaxations. Clonus is a sign of certain neurological conditions, particularly associated with upper motor neuron lesions involving descending motor pathways. Clonus is normally initiated by a reflex. When started, clonus can last for a few seconds or several minutes depending on the severity of the person’s condition. Clonus is most commonly found at the ankle, specifically with dorsiflexion and plantar flexion movement. So, when clonus is tested for, normally the ankle is flexed and extended to determine whether clonus exists or not. 92) (B) Varicella isn’t linked to clonus, as it doesn’t directly affect the brain or spinal cord. The major causes of clonus include multiple sclerosis, strokes, brain tumors, and trauma to the spinal cord or head. Multiple sclerosis causes demyelination of the nerve cells, disrupting communication between the brain and the spinal cord; the miscommunication can result in clonus depending on the sites of the body present with this demyelination. With a stroke, the brain cells do not receive enough oxygen either due to ischemia or hemorrhage. During this period of oxygen starvation, the brain’s motor nerve cells get injured. Since these motor neurons control body movements, clonus can result. Similarly, brain tumors, located near the brain’s motor neurons, can compress the motor neurons and this can result in clonus. Trauma to the brain or spinal cord can cause clonus because of the disruption of communication. If a spinal cord injury occurs, any area below the level of the injury no longer receives signals from above the site to inhibit activity. Trauma to the brain can damage motor neurons, which can result in clonus. 93) (A) Alzheimer’s is the most common type of dementia. Alzheimer's disease accounts for 60 to 80 percent of cases of dementia. The second most common type of dementia is vascular dementia, which is dementia that occurs after a stroke. 94) (A) Vascular dementia is a decline in thinking skills caused by conditions that block or reduce blood flow to the brain, depriving brain cells of vital oxygen and nutrients. 95) (C) Alzheimer’s disease occurs due to physical changes in the brain, including a buildup of certain proteins, which cause damage to nerve cells. Alzheimer’s is a progressive disease, which means that it worsens over time. Those with the illness live an average of 8 years after diagnosis, though survival can range from 4 to 20 years depending on the person’s age and other health conditions. Although the greatest known risk factor for Alzheimer’s disease is increasing age and the majority of people with Alzheimer’s are 65 and older, Alzheimer’s is not a normal part of aging. In certain cases, up to 5 percent of people with the disease have early onset of Alzheimer’s, which often appears in one’s 40s or 50s. 96) (B) Although some evidence points to a link of Alzheimer’s with demyelination of the axons of nerve cells, Alzheimer’s disease is caused chiefly due to destruction of nerve cells in the brain. Two abnormal structures called plaques and tangles are responsible for damage and death of nerve cells. Plaques are deposits of a protein fragment called beta-amyloid that build up in the spaces between nerve cells. Tangles are twisted fibers of another protein called tau that build up inside of cells. Though most people develop some plaques and tangles as they age, those with Alzheimer’s tend to develop far more. Most experts believe that plaques and tangles block communication among nerve cells and disrupt processes that cells need to survive. So, it’s the destruction and death of nerve cells that causes the memory failure, personality changes, and inability to perform daily tasks associated with Alzheimer’s disease. 97) (B) Currently, there is no cure for Alzheimer’s disease. Current drugs used to treat Alzheimer’s can help improve the symptoms of the disease; however, they do not slow the progression of the disease. Alzheimer’s is a disease where the greatest known risk factor is increasing age. The most common early symptom of Alzheimer’s disease is difficulty remembering newly learned information; this is because Alzheimer’s disease typically begins in the frontal lobe of the brain, which is the part of the brain that affects learning. As Alzheimer’s disease progresses, it can lead to increasingly severe symptoms, including personality changes, confusion, unfounded suspicion of family members, friends, and caregivers, worsening memory loss, difficulty speaking, swallowing, and walking. 98) (A) Delirium is reversible, while most cases of dementia are irreversible. 99) (A) Delirium is referred to as the acute confusional state. 100) (B) Sundowning is an event that occurs late in the evening when a person with dementia has increased agitation or confusion. This is why sundowning is also referred to as “late-day confusion”. The sundowning syndrome can also occur with delirium. 101) (D) The sundowning syndrome is a syndrome that brings on agitation and confusion late in the evening in a person with dementia or delirium. Symptoms usually resolve by the morning. Sundowning typically recurs commonly. Having rooms well-lit with a source of sound such as music playing can combat the effects of the syndrome. Familiar surroundings are important. Most people with dementia like to keep to a certain routine and love familiar surroundings. Changing the environment such as adding, removing, or moving around furniture can increase agitation and discomfort in a person with dementia. 102) (A) In the late stages of Alzheimer’s disease, patients need either partial or complete care in regard to completion of activities of daily living (ADLs). Although patients can still verbally talk, they lose the ability to carry on a conversation and respond to their environment. They may have a loss of physical capabilities such walking, ability to swallow, and control of bladder and bowel function. 103) (D) Most people with dementia such as Alzheimer’s disease die from pneumonia. Pneumonia is listed as the ultimate cause of death in up to two-thirds of people with dementia. Death due to pneumonia can be attributed to many things. For one, many in late-stage dementia are put to live in care homes and, due to their illness, may go to hospitals frequently; this puts them at risk for hospital-acquired pneumonia, which tends to be more resistant to antibiotic treatment. Also, many people with dementia are very immobile due to the disease process; immobility is a risk factor for pneumonia. Besides immobility, people with dementia may develop problems chewing due to the disease process; this puts them at a greater risk for developing aspiration pneumonia. Death can also occur due to other infections and sepsis. 104) (D) Cholinesterase inhibitors such as donepezil, galantamine, and rivastigmine work to increase the amount of acetylcholine in the brain. Cholinesterase inhibitors prevent the breakdown of acetylcholine, a chemical messenger that supports communication among nerve cells. This allows acetylcholine levels to remain high in the brain. This improves communication among nerve cells and improves symptoms of the disease (i.e., such as the person having improved cognitive function). However, it does not stop the progression of the disease and eventually symptoms will worsen. It simply delays the worsening of symptoms for 6 to 12 months, on average, for people who take them. After this time, a person may experience no benefits taking them; at this point, the drug can be stopped. Donepezil (Aricept) is the only cholinesterase inhibitor approved to treat all stages of Alzheimer’s disease. Besides cholinesterase inhibitors, memantine is another medication prescribed for dementia, which improves symptoms, but, again, does not delay the progression of the disease. 105) (D) No single test can determine whether a person has dementia. Diagnosis is based on a range of medical tests and the person’s medical history. Tests include a physical exam, a neurological exam, a mental status exam, and other laboratory tests to rule out other conditions such as thyroid problems. 106) (C) While specific symptoms vary in a person with lewy body dementia, core features of lewy body dementia include fluctuating cognition with great variations in attention and alertness from day to day and hour to hour, visual hallucinations, and motor features of Parkinson’s disease. Parkinsonian features include shuffling gait, reduced arm-swing during walking, blank expression (reduced range of facial expression), ratchet-like cogwheeling movements, low speech volume, and difficulty swallowing. Seizures are not associated with lewy body dementia. 107) (D) The heel-to-shin test tests cerebellar function. During the heel-to-shin test, the patient should place the heel of his (or her) right foot just below his left knee, and pass it straight down the shin and back up again. The patient should then demonstrate the same thing on the opposite side (the heel of his left foot just below his right knee and pass it straight down the shin and up again). Inability to perform heel-to-shin maneuvers appropriately is suggestive of cerebellar dysfunction. 108) (D) Common symptoms of a basilar skull fracture include raccoon eyes, rhinorrhea, and battle sign. 109) (B) Deep tendon reflexes are controlled by the spinal nerves. Deep tendon reflexes occur at the level of the spinal cord. 110) (A) Primitive reflexes are also called survival reflexes or newborn reflexes. Deep tendon reflexes are also called stretch reflexes. Primitive reflexes are controlled by the brainstem; deep tendon reflexes are controlled by spinal nerves. Primitive reflexes are automatic, stereotyped movements in infants. Primitive reflexes (such as the rooting reflex or the Moro reflex) are present at birth in full-term newborns and most disappear in the first few months of life; some like the blink reflex remain throughout life. In premature infants, some primitive reflexes may not be present or may be weak. An example of this is the rooting reflex. This reflex does not begin until about the 32nd week of pregnancy and is not fully developed until about 36 weeks. Due to their early birth, which causes this reflex not to fully develop, premature babies may have a weak or immature sucking ability ((Rudd & Kocisko, 2014) & stanfordchildrens.org)). 111) (A) Reflexes, whether primitive or deep tendon, are involuntary movements that occur in response a stimulus. Deep tendon reflexes provide information about the communication between the central nervous system and the peripheral nervous system. A decreased deep tendon reflex usually indicates a problem with the peripheral nervous system. A brisk or exaggerated reflex indicates a problem with the central nervous system (Rudd & Kocisko, 2014). 112) (C) The Achilles reflex is also known as the ankle jerk reflex. It occurs when the Achilles tendon is tapped while the foot is dorsiflexed. A positive result would be the jerking of the foot towards its plantar surface. The Achilles reflex checks the spinal nerves, S1 and S2. Image: Achilles reflex 113) (D) The patellar reflex is also called the knee-jerk response. This is because the knee moves (jerks) in response to the tendon being tapped. The patellar reflex can be checked by a person being in the sitting position and sharply tapping on the patellar tendon, which lies just below the kneecap. The sharp tap on the tendon slightly stretches the quadriceps, the complex of muscles at the front of the upper leg. In reaction, these muscles contract, and the contraction tends to straighten the leg in a kicking motion. The patellar reflex checks spinal nerves L2, L3, and L4 (L2-L4). Image: Patellar reflex 114) (C) The Babinski reflex (also called the plantar reflex) is a reflex that tests spinal nerves L5, S1, and S2. This reflex is tested by stroking the foot with an object from the heel all the way up to the toes. An abnormal sign would be that the toes would fan out; this would be abnormal in adults. If the toes plantar flex, this is a normal finding. 115) (A) Reflexes of the arms and fingers test spinal nerves in the cervical plexus. These include the brachioradialis reflex (C5-C6), extensor digitorum reflex (C6-C7), biceps reflex (C5-C6), and triceps reflex (C6-C8). All areas of the arms and fingers have their source from nerves in the cervical plexus. 116) (A) Myelomeningocele is the most severe type of spina bifida. 117) (B) Anencephaly is a condition in which most of the brain does not develop. Those affected are usually stillborn or die shortly after birth. Spina bifida does not affect the brain. Microcephaly is a condition in which a child is born with a small head. Encephalocele is a condition in which a portion of the brain protrudes through an opening in the skull. 118) (A) Cluster headaches are not associated with queasiness or vomiting. They are characterized most often by the excruciating pain that is so bad it has been referred to as “suicide headaches”. The pain is typically around the eye and is always one-sided. Cluster headaches are named so because they occur in clusters at a time. They normally occur several times a day for weeks or months and then don’t show up for months or even years again. Then they may come back again in clusters. Cluster headaches occur more often in males than in females with about a 5:1 ratio. Cluster headaches are often accompanied by tearing, eye drooping, and nasal congestion. 119) (C) High-dose oxygen is most commonly prescribed for cluster headaches. 120) (D) Migraine headaches typically last anywhere from 4 to 72 hours. 121) (A) Migraine headaches affect women about 3 times as much as men. Migraine headaches are one of the most common problems seen in ERs and doctor’s offices. It is known to affect over 30 million Americans. There are 2 types of migraine headaches, common migraines and classic migraines. Common migraines are migraines that have no aura before the headache. Classic migraines are migraines that have an aura present before the headaches. Common migraines, as the name suggests, are more common and account for about 80% of all migraines. Classic migraines (that have an aura) tend to be more severe than common migraines. 122) (A) Migraine headaches may or may not be preceded by an aura. Migraine headaches are described as pounding, throbbing headaches. They may be accompanied by nausea, vomiting, and extreme sensitivity to light or sound; tension headaches, for instance, tend not to have these characteristics. Migraine attacks can cause significant, debilitating pain that can last for hours to days. 123) (B) Milk is not a common precipitating factor for migraines. Common precipitating factors for migraines include red wine, MSG, aspartame, chocolate, beer, stress, and sleep changes. 124) (B) Propranolol is used commonly for the prophylaxis of migraine headaches. 125) (B) There are a number of drug classes that are used for migraine headache prophylaxis. These include beta blockers (such as propranolol and timolol), anticonvulsants (such as divalproex sodium), tricyclic antidepressants (such as amitriptyline), calcium antagonists (such as flunarizine), and MAOIs (such as phenelzine). Being that flunarizine and MAOIs have more adverse effects than other drug classes, they are used as second-line treatments for migraine prophylaxis (though their efficacy is high). Benzodiazepines are not used for migraine headache prophylaxis. 126) (C) Status migrainosus is a migraine headache that lasts longer than 3 days (72 hours). Normally, migraines last anywhere from 4-72 hours. If the migraine headache persists past 72 hours, this is considered status migrainosus. 127) (D) A cluster headache is commonly described as the most painful type of headache. 128) (A) The most common trigger for muscle tension headaches is stress. 129) (B) A tension headache is described as a dull, aching head pain. It is described as a sensation of tightness or pressure across the forehead or on the sides and back of the head, as if someone is squeezing the person’s head or there is a tight band around the head. It is also described as being characterized by tenderness of the scalp, neck, and shoulder muscles. Cluster headaches are headaches that are described as being comprised of a sharp, stabbing pain behind the eye. 130) (B) Tension headaches are usually bilateral. Unlike migraines, they are not usually accompanied by visual disturbances, nausea, or vomiting. While physical activity normally aggravates migraine pain, it doesn’t make tension headache pain worse. 131) (A) Migraine headaches are generally described as headaches that produce a throbbing pain on both sides of the head. Tension headaches produce a dull to moderate type of headache usually. Cluster headaches can be very severe and cause a sharp, stabbing pain behind the eye, usually on one side of the face. Sinus headaches usually produce a deep and constant pain in the cheekbones, forehead, or bridge of the nose. 132) (D) Cluster headaches are the only type of headache accompanied by tearing, eye drooping, and nasal congestion. 133) (B) Tension headaches are the most common type of headache. 134) (B) Tension headaches are usually mild or moderate. This is comparison to migraine headaches, which can cause throbbing pain on both sides of the head or cluster headaches, which can be very severe and cause a sharp, stabbing pain behind the eye. Sinus headaches usually produce a deep and constant pain in the cheekbones, forehead, or bridge of the nose. 135) (B) Sumatriptan is used during an acute episode of a migraine headache. Apart from sumatriptan, NSAIDs may also be used during acute episodes of migraine headaches for pain management. 136) (D) Basilar migraines, also referred to as basilar artery migraines or brainstem migraines, are migraines that originate in the lower part of the brain, the brainstem. 137) (C) Basilar migraines are headaches that start in the lower part of the brain, called the brainstem. A basilar migraine is a migraine composed of symptoms including dizziness, double vision, and a lack of coordination. Basilar migraines are preceded by an aura that typically occurs about 10 to 45 minutes before the onset of head pain. This type of migraine can last anywhere from 4 to 72 hours and can take a long time to recover from. A person suffering from a basilar migraine may feel drained for up to 24 hours after it’s over. Symptoms of a basilar migraine may mimic more serious conditions such as seizure disorders, stroke, meningitis, or brain tumors. To differentiate these conditions from basilar migraines, doctors may perform comprehensive examinations. 138) (B) Alexia is characterized by trouble with reading despite normal intelligence. It is a condition that occurs with someone who previously could read who loses the ability to. The difficulties are involuntary and people with this disorder have a normal desire to learn. Agraphia is an acquired neurological disorder causing a loss in the ability to communicate through writing. Aphasia is a neurological disorder characterized by the inability to comprehend and/or formulate language. Agnosia is a neurological disorder that causes an inability to recognize common objects, people, or sounds. 139) (C) Munchausen syndrome is a factitious disorder, which is a condition in which a person deliberately and consciously acts as if he or she has physical or mental illness when there really is no illness. Munchausen syndrome is considered a mental illness because it is associated with severe emotional difficulties. Most of the symptoms feigned in people with Munchausen syndrome are related to physical illness (i.e., symptoms such as chest pain, stomach problems, fever), rather than a mental disorder. People with Munchausen syndrome may deliberately produce or exaggerate symptoms or just flat out lie. Munchausen syndrome is considered a rare syndrome that is most often found in young adults. 140) (D) Factitious disorder by proxy is a condition in which a person acts as if a person in his/her care is sick when the person really isn’t sick. Chapter 12- Oncology 1) What is the most common type of cancer in women in the United States? A) B) C) D) Cervical cancer Uterine cancer Lung cancer Breast cancer 2) What is the most common type of cancer overall in men in the United States? A) B) C) D) Lung cancer Skin cancer Prostate cancer Stomach cancer 3) What is the most common type of gynecological cancer? A) B) C) D) Ovarian cancer Uterine cancer Breast cancer Cervical cancer 4) Which cancer has the highest mortality rate? A) B) C) D) Colon cancer Lung cancer Breast cancer Stomach cancer 5) What type of skin cancer has the highest mortality rate? A) Basal cell carcinoma B) Squamous cell carcinoma C) Melanoma D) Dermatofibrosarcoma protuberans 6) What is the most common type of skin cancer? A) B) C) D) Basal cell carcinoma Squamous cell carcinoma Melanoma Merkel cell carcinoma 7) All of the following are common characteristics of melanoma except for: A) B) C) D) Moles are dark-colored Moles have diameters of 3 mm or less Moles have irregular borders Moles are asymmetric 8) What is the current recommendation schedule for a woman to receive a mammogram? A) Start at 30 years of age and then every year until 80 years old B) Start at 30 years of age and then every 2 years until 74 years old C) Start at 50 years of age and then every year until 74 years old D) Start at 50 years of age and then every 2 years until 74 years old 9) What is the current recommendation schedule for a woman to receive a pap smear/liquid cytology for cervical cancer? A) Start at 12 years old and continue every 3 years until 65 years old B) Start at 18 years old and continue every 3 years until 65 years old C) Start at 21 years old and continue every 3 years until 65 years old D) Start at 40 years old and continue every 3 years until 65 years old 10) Which of the following cancers is recommended for routine screening? A) Colon cancer B) Skin cancer C) Prostate cancer D) Pancreatic cancer 11) Which population of people should be routinely screened for lung cancer? A) All people older than 65 years B) People from age 55 to 80 years who have smoked at any time in their lives C) People from age 55 to 80 years who have a 30 pack-year smoking history D) Anyone from any age who is a current smoker 12) All of the following are risk factors for breast cancer except for: A) B) C) D) Early menarche Late menopause Late menarche Nulliparity 13) All of the following are risk factors for cervical cancer except for: A) B) C) D) Older age onset of sex Multiple sex partners Immunosuppression Smoking 14) What is multiple myeloma? A) A cancer that causes the overproduction of the plasma cells within the bone marrow B) A cancer that causes the overproduction of immature lymphocytes within the bone marrow C) A cancer that causes the overproduction of red blood cells within the bone marrow D) A cancer that causes the overproduction of platelets within the bone marrow 15) Common symptoms of multiple myeloma include all of the following except for: A) Hypercalcemia B) Bone fractures C) Thrombocytosis D) Anemia 16) What age group is multiple myeloma most commonly seen in? A) B) C) D) Teenagers Young adults Middle-aged population Elderly population 17) Which demographic population is most at risk for multiple myeloma? A) B) C) D) People of Eastern European descent People of Eastern Asian descent People of African descent People of Hispanic descent 18) All of the following statements are true regarding pheochromocytoma except for: A) Pheochromocytoma is a tumor of the adrenal gland B) Pheochromocytoma causes excess production of catecholamines in the body C) If left untreated, pheochromocytoma can be a life-threatening condition D) Pheochromocytoma is managed primarily through blood-pressure lowering medication 19) Pheochromocytoma is a condition in which there are transient episodes of: A) B) C) D) Hypertension Hypotension Hypoglycemia Hyperglycemia 20) A patient should be referred to a urologist if the patient’s prostate specific antigen (PSA) is greater than: A) 2.0 ng/mL B) 4.0 ng/mL C) 6.0 ng/mL D) 8.0 ng/mL 21) What test normally accompanies the PSA for screening for prostate cancer? A) B) C) D) A digital rectal exam (DRE) An ultrasound of the prostate An X-ray of the prostate An MRI of the prostate 22) What is the definitive test to diagnose prostate cancer? A) B) C) D) PSA level Digital Rectal Exam (DRE) Biopsy of the prostatic tissue An ultrasound of the prostate 23) What objective finding discovered by a healthcare provider during a digital rectal exam leads the examiner to believe that the patient has prostate cancer? A) The prostate feels very soft and is movable B) There is a hard, fixed nodule on the prostate gland that can be felt C) The prostate contains a soft nodule on top of it that feels waxy D) Small tears can be felt across the prostate gland 24) What is the number one leading cause of lung cancer? A) B) C) D) Smoking Asbestos Radon Air pollution 25) What is the second leading cause of lung cancer? A) Smoking B) Asbestos C) Radon D) Air pollution 26) All of the following are risk factors for lung cancer except for: A) B) C) D) Smoking Tuberculosis Radiation therapy to the chest Radon 27) The risk of developing lung cancer for a past smoker who has quit begins to equal that of a nonsmoker after smoking cessation of: A) B) C) D) 5 years 10 years 15 years 20 years 28) What part of the body does mesothelioma most commonly affect? A) B) C) D) The lining of the abdomen The lining of the lungs The exterior lining of the heart The lining of the testicles 29) Mesothelioma is caused by exposure to: A) B) C) D) Cigarette smoke Lead Mercury Asbestos 30) Which of the following is true about mesothelioma? A) It usually has an excellent prognosis B) It has a prognosis of about 50% C) It usually has a very poor prognosis D) It is always 100% fatal 31) Where is the most likely scenario in which a person would be exposed to asbestos? A) Eating fish for years from a local fish farm B) A person having unprotected sex for many years C) A person working as a nurse for many decades D) A person living in an older home for decades 32) All of the following are common symptoms of pleural mesothelioma except for: A) B) C) D) Dyspnea Hemoptysis Weight loss Petechiae 33) Which demographic population has the highest incidence for bladder cancer? A) B) C) D) White men Black men White women Black women 34) All of the following are symptoms of bladder cancer except for: A) B) C) D) Hematuria Dysuria Pelvic pain Inflamed ureters 35) All of the following are risk factors for bladder cancer except for: A) Smoking B) Exposure to certain types of workplace chemicals C) Benign prostatic hypertrophy D) Use of cyclophosphamide 36) Modifiable lifestyle risk factors for colon cancer include all of the following except: A) B) C) D) A diet low in fruits and vegetables Obesity Lack of regular physical activity A low-protein diet 37) All of these medical conditions place a patient at a higher risk for colon cancer except: A) Ulcerative colitis B) Duodenal ulcers C) Crohn’s disease D) Familial adenomatous polyposis (FAP) 38) When is it recommended that adults without any high-risk factors for colorectal cancer begin to get screened for colorectal cancer? A) B) C) D) 40years old 45 years old 50 years old 55 years old 39) Which of the following is a widely-used screening test for colorectal cancer? A) B) C) D) Barium enema MRI Digital rectal examination Colonoscopy 40) How often is it recommended that men get a colonoscopy for colorectal cancer screening? A) Every year B) Every 2 years C) Every 5 years D) Every 10 years 41) How often should a sigmoidoscopy be performed when screening for colon cancer? A) B) C) D) Every year Every 2 years Every 5 years Every 10 years 42) How often should a high-sensitivity fecal occult blood test be performed when screening for colon cancer? A) B) C) D) Every year Every 2 years Every 5 years Every 10 years 43) All of the following are risk factors for liver cancer except for: A) B) C) D) Hypercalcemia Hemochromatosis Heavy alcohol consumption Hepatitis 44) All of the following are current recommendations to lower a person’s risk of liver cancer except: A) B) C) D) Get vaccinated against hepatitis B Get tested for hepatitis C Avoid drinking too much alcohol Eat a low-fat diet 45) Common symptoms of ovarian cancer include all of the following except: A) Vaginal bleeding or discharge that that is not normal for a person B) Facial flushing C) Pain in the pelvic or abdominal area D) Bloating in the stomach 46) Which of the following statements is false regarding lymphomas? A) A lymphoma is a cancer that develops in the lymph nodes and lymphatic system B) The 2 main types of lymphoma are non-Hodgkin’s lymphoma and Hodgkin’s lymphoma C) Hodgkin’s lymphoma occurs much more frequently than non-Hodgkin’s lymphoma D) The main symptom of a lymphoma is enlargement of the lymph nodes that does not go away 47) Where are the majority of breast cancer cases located? A) B) C) D) Right near the nipples Lower inner quadrant Lower outer quadrant Upper outer quadrant 48) What is an adenoma? A) A benign tumor that grows on fibrous or connective tissue B) A benign tumor formed by glandular structures in epithelial tissue C) A malignant tumor that grows on fibrous or connective tissue D) A malignant tumor formed by glandular structures in epithelial tissue 49) Which statement is false regarding tumors? A) A tumor is also called a neoplasm B) A tumor is an abnormal mass of tissue which may be solid or fluid-filled C) A tumor is always cancerous D) Benign tumors cannot spread 50) What is a fibroid? A) A benign tumor that grows on fibrous or connective tissue B) A benign tumor formed by glandular structures in epithelial tissue C) A malignant tumor that grows on fibrous or connective tissue D) A malignant tumor formed by glandular structures in epithelial tissue 51) What is another term for a precancerous state? A) B) C) D) Benign Premalignant Malignant Terminal 52) A benign tumor that consists of a proliferation of blood vessels is called a: A) B) C) D) Lipoma Adenoma Fibroma Hemangioma 53) Which of the following statements is false regarding leukoplakia? A) A leukoplakia is characterized by thick white patches that form in the mouth B) A leukoplakia cannot be scraped off C) Tobacco smoking and/or chewing is believed to be the main cause of leukoplakia D) Most cases of leukoplakia are malignant 54) What is a carcinoma? A) A cancer arising in the epithelial tissue of the skin or lining of the organs B) A cancer arising in the connective or nonepithelial tissue such as bones or muscles C) A cancer that affects the immune system, specifically the lymphatic system D) A cancer of the blood or bone marrow 55) What is a sarcoma? A) A cancer arising in the epithelial tissue of the skin or lining of the organs B) A cancer arising in the connective or nonepithelial tissue such as bones or muscles C) A cancer that affects the immune system, specifically the lymphatic system D) A cancer of the blood or bone marrow 56) The Pel-Ebstein sign may be seen at times with: A) B) C) D) Esophageal cancer Stomach cancer Hodgkin’s lymphoma Leukemia 57) All of the following conditions are benign states except for: A) B) C) D) Fibroma Lipoma Actinic keratosis Hemangioma 58) Which of the following is false regarding skin cancer? A) Basal cell carcinoma is the most common type of skin cancer B) Both basal cell carcinoma and squamous cell carcinoma are much more common than melanoma C) Squamous cell carcinoma is more likely to spread than basal cell carcinoma D) Actinic keratosis is a risk factor for melanoma 59) All of the following conditions represent precancerous states except for: A) B) C) D) Barrett’s esophagus Actinic keratosis Seborrheic keratosis Cervical dysplasia 60) Which of the following statements is false regarding thyroid cancer? A) Often, the first sign of thyroid cancer is a thyroid nodule B) Symptoms of thyroid cancer include a hoarse voice, neck pain, and enlarged lymph nodes C) A nodule that is hot on scan is more likely to be malignant D) Most thyroid cancers are very curable 61) Which is the greatest risk for developing thyroid cancer? A) Hypothyroidism B) Hyperthyroidism C) Iodide supplementation D) External radiation of the head, neck or chest in childhood 62) Which of the following statements is false regarding basal cell carcinoma? A) Basal cell carcinomas are lesions that arise in the deepest layer of the epidermis B) Basal cell carcinomas are most frequently found in the buttocks and genital areas C) Basal cell carcinoma rarely metastasizes beyond the original tumor site D) Basal cell carcinomas are usually caused by prolonged, intense sun exposure 63) All of the following are measures to prevent skin cancer except: A) Seek the shade, especially between 6AM-9AM B) Avoid tanning and never use UV tanning beds C) Self-examine your skin head-to-toe every month D) See your doctor every year for a professional skin exam 64) What is the second most common form of skin cancer? A) B) C) D) Basal cell carcinoma Squamous cell carcinoma Melanoma Dermatofibrosarcoma protuberans 65) What is the most common type of cancer in childhood and teenagers? A) B) C) D) Hodgkin’s lymphoma Leukemia Wilm’s tumor Osteosarcoma 66) Acute leukemia is defined as leukemia in which: A) Greater than 10% of the cells in the bone marrow are blasts B) Greater than 20% of the cells in the bone marrow are blasts C) Greater than 30% of the cells in the bone marrow are blasts D) Greater than 50% of the cells in the bone marrow are blasts 67) Myeloid line of cells means cells that: A) Are immature red blood cells B) Are immature platelets C) Are immature white blood cells D) Non-lymphoid cells that arise from the bone marrow 68) Which of the following statements is false regarding leukemia? A) Acute myeloid leukemia is the most common type of acute leukemia in adults B) Acute myeloid leukemia is mostly found in older adults C) The prognosis for children with acute lymphocytic leukemia is poor D) Chronic types of leukemia are rare in children 69) Which cancer does the pap test check for? A) B) C) D) Uterine Cervical Ovarian Vaginal Oncology Answers 1) (D) Breast cancer is the most common type of cancer in women in the United States. 2) (C) Prostate cancer is the most common type of cancer overall in men in the United States. 3) (B) Uterine cancer (endometrial cancer) is the most common type of gynecological cancer. 4) (B) Lung cancer has the highest mortality rate for both genders. The 5-year survival rate for lung cancer is 16%, giving it a mortality rate of 84%. The cancer with the second highest mortality rate is colon cancer, with a 5-year survival of 65%, giving it a mortality rate of 35%. 5) (C) Melanoma has the highest mortality rate out of the 3 major skin cancers. Though melanoma only accounts for about 1% of skin cancers, it makes up 75% of skin cancer deaths. Dermatofibrosarcoma protuberans rarely spreads, so therefore this cancer has a high survival rate. 6) (A) Basal cell carcinoma is the most common type of skin cancer. The second most common type of skin cancer is squamous cell carcinoma. Melanoma is the third most common type. Skin cancers such as Merkel cell carcinoma are very rare. 7) (B) The “A, B, C, D, E” of melanoma involve A (asymmetry), B (border irregular), C (color varies in the same region), D (diameter > 6mm), and E (enlargement or change in size). Melanoma moles have a diameter greater than 6mm, not 3mm or less. 8) (D) The current recommendation schedule set by the United States Preventive Services Task Force (USPSTF) is for a woman to receive a mammogram starting at the age of 50 years old and receive one every 2 years until the age of 74. 9) (C) The current recommendation schedule by the USPSTF (March 2012) for a woman to receive a pap smear/liquid cytology for cervical cancer is to start at the age of 21 and continue every 3 years until 65 years old. 10) (A) Colon cancer is the only cancer of the above choices that are recommended for routine screening. Screening for colon cancer starts at age 50. The United States Preventive Services Task Force (USPSTF) does not recommend screening for skin cancer (2016), prostate cancer (2012), or pancreatic cancer (2004). The dates shown with the cancers are when the USPSTF released their recommendations. Be aware that these recommendations, though usually constant, are subject to change by the USPSTF. As you can see, some haven’t changed for many years such as pancreatic cancer, and others have changed within the last few years. To see a full, up-todate list of the USPTFS recommendations, visit their website at https://www.uspreventiveservicestaskforce.org/ 11) (C) The United States Preventive Task Force Services (USPTFS) recommends annual screening for lung cancer (December 2013) with low-dose computed tomography in adults ages 55 to 80 years who have a 30 pack-year smoking history and currently smoke or who have quit within the past 15 years. Screening should be discontinued once a person has not smoked for 15 years or develops a health problem that limits life expectancy or the ability or willingness to have curative lung surgery. 12) (C) Late menarche is not a risk factor for breast cancer. Risk factors for breast cancer include early menarche (a girl’s first period), late menopause, and nulliparity (a woman never having children). All these conditions expose a woman to more estrogen over her lifetime, increasing the risk for breast cancer. Other risk factors for breast cancer include being female (99% of breast cancer cases are with women), age greater than 50 years, certain inherited genes (the most common being inherited mutations in the BRCA1 and BRCA2 genes), having a family history or personal history of breast cancer, being white (white women have slightly higher risk than black women), having dense breast tissue, having a history of radiation therapy (such as to treat another type of cancer), alcohol consumption, obesity (adipose tissue can make small amounts of estrogen), and hormone replacement therapy. 13) (A) Older age onset of sex is not a risk factor for cervical cancer. Risk factors for cervical cancer include HPV infection, younger age onset of sex (immature cervix easier to infect), multiple sex partners (defined as greater than 4 lifetime partners), immunodeficiency, genital herpes, smoking (doubles the risk of cervical cancer), age, race/ethnicity (more common among black, Hispanic, and American Indian women), and use of oral contraceptives. 14) (A) Multiple myeloma is a cancer that cause overproduction of plasma cells within the bone marrow. 15) (C) Common symptoms of multiple myeloma include bone pain (which can be in any bone but is most often in the back, hips and skull), bone weakness, fractures, anemia, leukopenia, thrombocytopenia, hypercalcemia (which can cause extreme thirst, severe constipation, and kidney problems), and kidney damage (due to damage from the myeloma protein). 16) (D) Multiple myeloma is mostly seen in the elderly population. It is rarely seen in younger people. 17) (C) People of African descent are the demographic group at highest risk for getting multiple myeloma; they have the highest incidence of multiple myeloma. 18) (D) Pheochromocytoma is a tumor of the adrenal gland that causes excess production of catecholamines in the body. Pheochromocytoma can result in episodes of severe hypertension. If left untreated, pheochromocytoma can be a life-threatening condition. Pheochromocytoma is managed or cured primarily through surgery. The tumor must be removed from the adrenal gland. 19) (A) Pheochromocytoma is a condition in which there are transient episodes of hypertension. This is caused because pheochromocytoma is a condition characterized by a tumor mostly found in the adrenal medulla. This causes excess secretions of catecholamines such as epinephrine and norepinephrine, which causes potent vasoconstriction. This can cause episodes of very high blood pressure. 20) (B) A patient should be referred to see a urologist if the PSA is greater than 4.0 ng/mL. Anything above 4.0 ng/mL is an elevated number that needs further investigation. Be aware that the United States Preventive Task Force Service does not recommend routine screening for prostate cancer (in asymptomatic individuals). However, if a practitioner has suspicion that a person may have prostate cancer (or any other prostate condition), s/he will likely screen for it. 21) (A) A digital rectal exam (DRE) normally accompanies a PSA during prostate cancer screening. 22) (C) The definitive test for diagnosing prostate cancer is a biopsy of the prostatic tissue. A PSA level and a digital rectal exam are used for screening for prostate cancer. If findings are positive, then a biopsy of the prostatic tissue can confirm the diagnosis. 23) (B) During a digital rectal exam, if the examiner feels a hard, fixed nodule on the prostate gland, this is a positive finding that needs further examination. The hard, fixed nodule produces high suspicion of prostate cancer. The nodule is painless to the patient. 24) (A) Smoking is the leading cause of lung cancer. In the United States, anywhere from 80% to 90% of lung cancer cases are linked to tobacco use. 25) (C) Radon is the second leading cause of lung cancer. Radon gas is a natural, chemically inert gas that is a natural decay product of uranium. It decays to form products that emit a type of ionizing radiation. Radon gas can travel up through soil and enter homes through gaps in the foundation, pipes, drains, or other openings. The U.S. Environmental Protection Agency estimates that one out of every 15 homes in the U.S. contains dangerous levels of radon gas. Radon gas is invisible and odorless, but can be detected with simple test kits. Radon gas is estimated to cause 12% of lung cancer deaths. 26) (B) Tuberculosis has not been found to increase the risk for lung cancer. Risk factors for lung cancer include smoking, exposure to secondhand smoke, exposure to radon gas, exposure to asbestos and other carcinogens, family history of lung cancer, and radiation therapy to the chest. Smoking is the number one risk factor. In the United States, smoking is linked to about 80% to 90% of lung cancers. Radon is a naturally occurring gas that comes from rock and dirt and can get trapped in houses and buildings. It cannot be detected by our senses. According to the U.S. Environmental Protection Agency (EPA), radon causes about 20,000 cases of lung cancer each year in the United States. Cancer survivors who had radiation therapy to the chest are at higher risk of lung cancer (source: cdc.gov & webmd.com). 27) (C) In the medical community, it is purported that the risk of developing lung cancer for a past smoker who has quit begins to approach that of a nonsmoker after about 15 years of smoking cessation. The risk of developing lung cancer decreases each year following smoking cessation, as normal cells grow and replace damaged cells in the lung. After about 15 years, past smokers are at about equal risk to individuals who have never smoked. 28) (B) There are a few different types of mesothelioma. The most common type is pleural mesothelioma. Pleural mesothelioma affects the lining of the lungs known as the pleura of the lungs. Pleural mesothelioma comprises about 75 percent of all mesothelioma cases. The second most common type of mesothelioma is peritoneal mesothelioma. This is a type of mesothelioma of the peritoneum, the lining of the abdomen. Other types include pericardial mesothelioma (affecting the exterior lining of the heart known as the pericardium) and testicular mesothelioma (affecting the lining of the testicles). Pleural and peritoneal mesothelioma, however, are the 2 most common types, comprising nearly 90 percent of all mesothelioma diagnoses. 29) (D) Mesothelioma is caused by exposure to asbestos, normally over a period of many years (decades). 30) (C) Mesothelioma usually has a very poor prognosis. Mesothelioma is a rare, aggressive cancer. When diagnosed with mesothelioma, the prognosis is usually very poor, as there is no cure for the disease, and typically it is discovered at a late stage of development. Generally, the earlier mesothelioma is diagnosed, the better the prognosis a patient has. It is not always 100% fatal, especially if caught early. 31) (D) A person living in an older home is the most likely scenario for a person being exposed chronically to asbestos. Asbestos fibers are known to be extremely strong and resistant to heat and fire. Before asbestos was found to have carcinogenic properties, it was seen as a safe fire retardant. So, it was used freely without any type of regulations on its use until the 1970s and 1980s. So, they may be found in insulation, drywall, ceiling and floor tiles, cements, paint and more. Many homes and buildings built before 1980 contain asbestos products. When these products are left undisturbed, they rarely pose any risks to a person’s health. But if they are disturbed such as through drilling the walls, tearing down the walls, uplifting the tiles on the floor, and in general renovating a house, this can cause the asbestos particles to become airborne, in which case they can be breathed in by a person. By law, only qualified professionals can test for asbestos or remove asbestos materials from a home. Once these particles are inhaled, they become trapped in the respiratory tract and lungs, where they may remain for life. A person living in a home is not the only way a person can be exposed. Another exposure is occupationalrelated exposure. Any occupation dealing with products with asbestos puts a person at risk. Occupations include construction workers, drywall tapers, electricians, firefighters, auto mechanics, and many other professions. 32) (D) Common symptoms of pleural mesothelioma include persistent dry or raspy cough, hemoptysis (coughing up blood), shortness of breath (dyspnea), difficulty swallowing (dysphagia), night sweats or fever, pain in the lower back or rib area, painful breathing, unexplained weight loss, fatigue, and lumps that may be present under the skin on the chest. Petechiae are not associated with pleural mesothelioma. 33) (A) White men have the highest incidence of bladder cancer than any other demographic population. 34) (D) Inflamed ureters aren’t associated with bladder cancer. Common symptoms of bladder cancer include hematuria (blood in the urine), urinary frequency, dysuria (pain while urinating), back pain, and pelvic pain. 35) (C) Risk factors for bladder cancer include tobacco use (smokers are four to seven times more likely to develop bladder cancer than nonsmokers), age (bladder cancer increases with age, with more than 70% of people with bladder cancer being older than 65 years old), being male (men are 3-4 times more likely to develop bladder cancer than women), white race (white people are more than twice as likely to be diagnosed with bladder cancer than black people), exposure to chemicals used in the textile, rubber, leather, dye, paint, and print industries, chronic bladder problems such as bladder stones and infections, use of cyclophosphamide (a chemotherapy drug), a personal history of bladder cancer, and arsenic exposure (a naturally occurring substance that can be found in drinking water) (source: cdc.gov). 36) (D) Low-protein diets aren’t directly associated with colon cancer. Instead a low-fiber and a high-fat diet are linked to colon cancer. Risk factors that contribute to the development of colon cancer include a diet low in fruits and vegetables, a low-fiber and high-fat diet, lack of regular physical activity, obesity, alcohol consumption, and tobacco use. 37) (B) Medical conditions that are considered risk factors for colorectal cancer include inflammatory bowel disease such as Crohn’s disease or ulcerative colitis, a personal or family history of colorectal cancer or colorectal polyps, or a genetic syndrome such as familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer (also known as Lynch syndrome). Duodenal ulcers are not directly associated with colon cancer. 38) (C) The U.S. Preventive Services Task Force (USPSTF) recommends that adults ages 50 to 75 be screened for colorectal cancer, and that adults ages 76 to 85 ask their doctor if they should be screened. So, age 50 is the age when a man or woman without any high-risk factors should begin getting screened for colorectal cancer. It is recommended that individuals with risk factors for colorectal cancer (i.e., such as family history, those with inflammatory bowel disease) get screened at an earlier age. Colorectal cancer can be screened for every year by the highsensitivity FOBT, every 5 years via sigmoidoscopy, or every 10 years via colonoscopy. 39) (D) A colonoscopy is a widely-used screening test to check for colorectal cancer. During screening, the examiner is looking for precancerous polyps, which are abnormal growths located in the colon. These precancerous polyps can then be removed before they turn into cancer. Colorectal cancer almost always develops from precancerous polyps. 40) (D) The recommendation is that men get a colonoscopy every 10 years starting from age 50. The U.S. Preventive Services Task Force (USPSTF) recommends that adults ages 50 to 75 be screened for colorectal cancer, and that adults ages 76 to 85 ask their doctor if they should be screened. 41) (C) If a person chooses to screen for colon cancer using a sigmoidoscopy, it should be performed every 5 years. 42) (A) If a person chooses to screen for colon cancer through a high-sensitivity fecal occult blood test, it should be performed annually. 43) (A) Many liver cancer cases are related to the hepatitis B or C virus. Millions of people live with chronic hepatitis B or C in the United States and don’t know they have the virus. Other risk factors for liver cancer include heavy alcohol use, cirrhosis, obesity, diabetes, and having hemochromatosis, a condition in which the body takes up and stores excess iron; too much iron in the liver can cause an enlarged liver, liver failure, and liver cancer, or cirrhosis. Eating foods contaminated with aflatoxin, a known hepatotoxic substance, is also a risk factor for liver disease. Aflatoxin is a fungus that can grow on foods. It commonly contaminates maize and other types of crops. Exposure to aflatoxin is known to cause hepatocellular injury, both chronic and acute. Nonalcoholic fatty liver disease, an accumulation of fat in the liver, also increases the risk of liver cancer. Hypercalcemia is more likely to affect the kidneys (such as kidney stones) rather than the liver. 44) (D) A low-fat diet, though healthier than a high-fat diet, isn’t linked to a decreased risk for liver cancer. 45) (B) Common symptoms of ovarian cancer include vaginal bleeding from a woman’s vagina or discharge that is not considered normal for her, pain in the pelvic or abdominal area, back pain, bloating, feeling full quickly while eating, and a change in bathroom habits, such as urinary frequency or dysuria. Facial flushing is not directly associated with ovarian cancer. 46) (C) Non-Hodgkin’s lymphoma makes up about 90% of cases of lymphoma, while Hodgkin’s lymphoma represents about 10% of cases. So, non-Hodgkin’s lymphoma makes up the bulk of lymphoma cases. The main symptom of a lymphoma is enlargement of the lymph nodes that does not go away. 47) (D) The majority of breast cancer cases are located in the upper outer quadrant called the “Tail of Spence”. Image: Tail of Spence 48) (B) An adenoma is a benign tumor formed by glandular structures in epithelial tissue. Even though the tumor itself is benign (noncancerous and does not spread), this does not mean it doesn’t cause health problems in the body. An adrenal adenoma (benign tumor of the adrenal gland) can stimulate the adrenal glands to produce too much aldosterone, which can cause health issues such as hypertension, hypokalemia, and hypernatremia. 49) (C) Tumors are not always cancerous. Benign tumors are not cancerous. A tumor, also called a neoplasm, is an abnormal mass of tissue which may be solid or fluid-filled. An adenoma, for example, is a type of benign tumor that forms on the epithelial tissue of glandular structures in the body. Benign tumors cannot spread. Besides being benign, tumors can also be classified as being pre-malignant (precancerous) and malignant (cancerous). 50) (A) A fibroid (also referred to as a fibroma) is a benign tumor that grows on fibrous or connective tissue of any organ in the body. An example is uterine fibroids. Even though a fibroid is benign, it can grow and compress against other body structures and cause symptoms. Uterine fibroids, for example, can cause vaginal bleeding, pelvic pain or discomfort. Image: Uterine fibroids 51) (B) Another term for a precancerous state is a premalignant state. A benign state is a noncancerous state. A malignant state is a cancerous state. 52) (D) A hemangioma is a benign tumor that consists of a proliferation of blood vessels. Hemangiomas can many times be seen on the surface of the skin. The majority of hemangiomas appear at birth and gradually go away after some months to years. Image: Hemangioma 53) (D) Most cases of leukoplakia are benign. A small percentage of cases are premalignant or malignant. Leukoplakia is a condition characterized by thickened white patches that form on the gums, the insides of the cheek, the bottom of the mouth, and less commonly the tongue. The patches cannot be scraped off. The medical community aren’t sure about the exact cause of leukoplakia but consider tobacco- whether smoked, dipped, or chewed- to be the main culprit. 54) (A) A carcinoma is a cancer arising in the epithelial tissue of the skin or lining of the organs. A sarcoma is a cancer arising in the connective or nonepithelial tissue such as bones, muscles, and cartilage. A lymphoma is a cancer that affects the immune system, specifically the lymphatic system. Leukemia is a cancer of the blood or bone marrow. 55) (B) A sarcoma is a cancer arising in the connective or nonepithelial tissue such as bones or muscles. An osteosarcoma, also called an osteogenic sarcoma, is a type of cancer that starts in the bones. 56) (C) The Pel-Ebstein sign (or Pel-Ebstein fever) may be seen at times with Hodgkin’s lymphoma. The Pel-Ebstein sign is a high-grade fever that keeps rising and falling every 7-10 days or so. The fever rises abruptly, stays high for a week or so and then falls abruptly down, staying down for about a week. Then it rises again and falls again. This rise and fall pattern is repeated. Thus, practitioners need to know what a person’s temperature has been doing over several weeks in order to identify Pel-Ebstein fever. Not all patients with Hodgkin’s lymphoma have this pattern of fever. In fact, only a minority have this exact pattern. However, when it’s present, it can be a strong clue that Hodgkin’s lymphoma may be the culprit. 57) (C) Actinic keratosis is a precancerous growth of crusty, scaly, thick patches of skin. Fibromas, lipomas, and hemangiomas are all benign states. 58) (D) Actinic keratosis is a risk factor for squamous cell carcinoma. The majority of the times actinic keratosis leads to squamous cell carcinoma (SCC). However, in rarer circumstances, it can lead to basal cell carcinoma (BCC). There is no direct association between actinic keratosis and melanoma. Basal cell carcinoma is the most common type of skin cancer. Both basal cell carcinoma and squamous cell carcinoma are much more common than melanoma. Squamous cell carcinoma is more likely to spread than basal cell carcinoma, so doctors will typically offer a much more urgent referral for a squamous cell carcinoma than a basal cell carcinoma. A basal cell carcinoma is unlikely to spread. 59) (C) Seborrheic keratosis is a benign skin condition. Barrett’s esophagus is a precancer for esophageal cancer. Actinic keratosis is a precancer either for squamous cell carcinoma or basal cell carcinoma. Cervical dysplasia is a precancerous state for cervical cancer. 60) (C) According to the National Cancer Institute, there are about 56,000 new cases of thyroid cancer in the US each year. Thyroid cancer does not always cause symptoms; often, the first sign of thyroid cancer is a thyroid nodule. Other symptoms of thyroid cancer include a hoarse voice, neck pain, and enlarged lymph nodes. A nodule that is cold on scan is more likely to be malignant than hot on scan. Most thyroid cancers are very curable. 61) (D) Thyroid cancer is a rare type of cancer. The greatest risk for getting thyroid cancer is external radiation to the head, neck, or chest in childhood. 62) (B) Basal cell carcinomas (BCC) are the most frequently occurring form of skin cancer. Basal cell carcinomas are abnormal, uncontrolled growths or lesions that arise in the skin’s basal cells, which line the deepest layer of the epidermis (the outermost layer of the skin). BCCs often look like open sores, red patches, pink growths, shiny bumps, or scars. They are usually caused by prolonged, intense sun exposure over a period of time. Almost all BCCs occur on parts of the body excessively exposed to the sun—especially the face, ears, neck, scalp, shoulders, and back. BCC rarely metastasizes beyond the original tumor site. Only in very rare cases can it spread to other parts of the body and become life-threatening. Nonetheless, BCCs should always be taken seriously (source: skincancer.org). Image: Basal cell carcinoma 63) (A) Prevention guidelines to prevent skin cancer include seeking shade, especially between 10AM-4PM (when the sun’s rays are the strongest), avoiding tanning and never using UV tanning beds, covering up with clothing including using a broad-brimmed hat and UV-blocking sunglasses, using a broad spectrum sunscreen with an SPF of 15 or higher every day, using a water-resistant, broad spectrum sunscreen with an SPF of 30 or higher for extended outdoor activity, examining one’s skin from head-to-toe every month, and seeing a doctor every year for a professional skin exam. Regarding the sunscreen, it should be placed on the entire body 30 minutes before going outside and reapplied every two hours or after swimming or excessive sweating (source: skincancer.org). 64) (B) Squamous cell carcinoma (SCC) is an uncontrolled growth of abnormal cells arising in the squamous cells, which compose most of the skin’s upper layers (the epidermis). SCCs often look like elevated growths with central depression. They may crust or bleed. Like other types of skin cancers, SCC is mainly caused by cumulative ultraviolet (UV) exposure over the course of a lifetime (source: skincancer.org). Image: Squamous cell carcinoma 65) (B) Leukemia is the most common cancer in children and teenagers, accounting for almost 33% of cancers. Most childhood leukemias are acute lymphocytic leukemia (ALL). Most of the remaining cases are acute myeloid leukemia (AML). Chronic leukemias are rare in children (source: American Cancer Society). 66) (B) Acute leukemia is defined by the World Health Organization as leukemia in which greater than 20% of the cells in the bone marrow are blasts. Once blasts reach this threshold, the leukemia can progress rapidly. Chronic leukemia is defined as having less than 20% blasts in the bone marrow. 67) (D) Myeloid line of cells means cells that arise from the bone marrow. It refers to blood cells that become granulocytes, monocytes, erythrocytes, or platelets. Although all blood cells, even lymphocytes, are born in the bone marrow, myeloid cells in the narrowest sense of the term can be distinguished from lymphoid cells, that is, lymphocytes, which come from common lymphoid progenitor cells that give rise to B cells and T cells. On the other hand, lymphocytic leukemia affects cells that are lymphocytes, causing a proliferation of immature lymphocytes. Thus, myeloid is associated with the innate immune system (which can be seen as the non-specific immune system) that comprises the cells and mechanisms that defend the host from infection from other organisms but does not offer memory against the pathogens or confer long-last or protective immunity to the host. In contrast, lymphoid is associated with the adaptive immune system (which is comprised of highly specialized, systemic cells and processes that eliminate pathogens or prevent their growth and that creates immunological memory after an initial response to a pathogen so that future encounters with that pathogen creates an enhanced response). However, like myeloid leukemia, lymphocytic leukemia affects all red blood cells because the proliferation of lymphocytic cells crowds out the bone marrow, preventing the other cells from being produced in normal amounts. 68) (C) Acute myeloid leukemia is the most common type of acute leukemia in adults, mostly found in older adults. Acute lymphocytic leukemia (ALL) is the most common type of leukemia found in children. ALL has a good prognosis. The 5-year survival rate for children with ALL is over 85%. AML also has a good 5-year survival rate for children and is in the range of 60-70%. Chronic types of leukemia are rare in children (source: American Cancer Society). 69) (B) The pap test checks for cervical cancer. Cervical cancer is the only cancer that a pap test checks for. Maternity Chapter 13- Maternity 1) What is caput succedaneum? A) Diffused edema of the scalp that crosses the midline B) Traumatic subperiosteal hemorrhage where there is a collection of blood that does not cross the midline or suture lines C) A bruise where there is outward bleeding from the infant’s scalp D) Internal bleeding of an infant’s kidneys 2) What causes caput succedaneum? A) A frank breech position during pregnancy B) A woman having a bicornuate uterus C) Intrauterine and vaginal pressure from a prolonged or difficult vaginal labor D) An oblique position during pregnancy 3) What is a cephalhematoma? A) Diffused edema of the scalp that crosses the midline B) Traumatic subperiosteal hemorrhage where there is a collection of blood that does not cross the midline or suture lines C) A bruise where there is outward bleeding from the infant’s scalp D) Internal bleeding of an infant’s kidneys 4) What is colostrum? A) A type of mucus that forms in the cervix to protect against pathogens that may enter through the vagina B) A greasy type of fluid that is found on the placenta during its removal C) A fluid that leaks from the vagina late in pregnancy D) The first milk produced by the breasts in pregnancy 5) It is recommended that RhoGAM be given: A) To all pregnancies of Rh positive mothers with the exclusion of abortions, miscarriages, or ectopic pregnancies B) To all pregnancies of Rh negative mothers with the exclusion of abortions, miscarriages, or ectopic pregnancies C) To all pregnancies of Rh positive mothers regardless of whether it results in abortions, miscarriages, or ectopic pregnancies D) To all pregnancies of Rh negative mothers regardless of whether it results in abortions, miscarriages, or ectopic pregnancies 6) RhoGAM should be given at: A) 24 weeks of gestation and within 72 hours of birth B) 24 weeks of gestation and within 2 weeks after birth C) 28 weeks of gestation and within 72 hours after birth D) 28 weeks of gestation and within 2 weeks after birth 7) How long does the first trimester of pregnancy last? A) B) C) D) Weeks 1 - 8 Weeks 1 - 10 Weeks 1 - 12 Weeks 1 - 14 8) What is a miscarriage? A) The spontaneous loss of a fetus before the 20th week of pregnancy B) The spontaneous loss of a fetus before the 24th week of pregnancy C) The spontaneous loss of a fetus before the 28th week of pregnancy D) The spontaneous loss of a fetus before the 32nd week of pregnancy 9) What is a threatened abortion? A) An abortion in which the fetus dies or was never formed but the body does not recognize the pregnancy loss or expel the pregnancy products B) Vaginal bleeding that occurs in the first 20 weeks of pregnancy C) An abortion in which the body has expelled part of the tissue and products of pregnancy D) An abortion in which the body has expelled all pregnancy contents 10) What is the term referring to an abortion in which all of the products (tissues) of conception leave the body? A) Incomplete abortion B) Complete abortion C) Infected abortion D) Missed abortion 11) What is a missed abortion? A) An abortion in which the fetus dies or was never formed but the body does not recognize the pregnancy loss or expel the pregnancy products B) Vaginal bleeding that occurs in the first 20 weeks of pregnancy C) An abortion in which the body has expelled part of the tissue and products of pregnancy D) An abortion in which the body has expelled all pregnancy contents 12) Which of the following statements is false regarding missed abortions? A) The placenta may still continue to release hormones and a woman may still continue to experience signs of pregnancy B) The fetus, if formed, dies in utero C) The unviable fetus and pregnancy products stay retained inside the woman’s body D) There is vaginal bleeding 13) A woman has increased constipation during pregnancy due to the effects of: A) B) C) D) Progesterone Prolactin Estrogen Human chorionic gonadotropin 14) A Coombs test checks for: A) The presence of antibodies that may destroy granulocytes B) The presence of antibodies that may destroy agranulocytes C) The presence of antibodies that may destroy red blood cells D) The presence of antibodies that may destroy platelets 15) What does the direct Coombs test measure? A) Antibodies that are stuck to the surface of red blood cells. B) Antibodies that are floating in the blood C) Antibodies that are stuck to the surface of white blood cells D) Antibodies that are stuck to the surface of platelets 16) What does the indirect Coombs test measure? A) Antibodies that are stuck to the surface of red blood cells. B) Antibodies that are floating in the blood C) Antibodies that are stuck to the surface of white blood cells D) Antibodies that are stuck to the surface of platelets 17) Which type of test is most specific to checking for autoimmune hemolytic anemia? A) B) C) D) Direct Coombs test Indirect Coombs test CBC Erythrocyte sedimentation rate 18) Which of the following is not a risk factor for abruptio placentae? A) B) C) D) Cocaine use Hypertension Preeclampsia Asthma 19) HELLP syndrome is a serious but rare complication of: A) Placenta previa B) Preeclampsia C) Hyperemesis gravidarum D) Abruptio placentae 20) Which of the following is not a symptom of HELLP syndrome? A) B) C) D) Hemolysis Elevated liver enzymes Low platelets Pressure ulcers 21) Which of the following lab values decrease during pregnancy? A) B) C) D) Alkaline phosphatase Hemoglobin White blood cell count Erythrocyte sedimentation rate 22) Alkaline phosphatase levels rise in pregnancy due to: A) B) C) D) The increased blood volume The growth of the fetal bones Increased kidney size Increased estrogens levels 23) Low alpha-fetoprotein (AFP) could be an indicator of: A) B) C) D) Multiple gestation pregnancy Down Syndrome Spina bifida Anencephaly 24) What supplement is commonly prescribed to women to prevent neural tube defects? A) B) C) D) Folic acid Thiamine Niacin Magnesium 25) A nurse practitioner notes that a patient’s alpha-fetoprotein (AFP) is low and suspects it may possibly be Down syndrome. The practitioner orders a quadruple screen test. All of the following are components of the quadruple screen test except for: A) B) C) D) Luteinizing hormone Human chorionic gonadotropin Estriol Inhibin-A 26) Which of the following is the greatest risk factor for a woman having a baby with Down syndrome? A) B) C) D) Poor diet Smoking Advanced maternal age Obesity 27) Which of the following symptoms is not part of the classic triad symptoms of preeclampsia? A) B) C) D) Proteinuria Glucosuria Hypertension Edema 28) All of the following are risk factors for preeclampsia except for: A) A first pregnancy B) A woman being underweight C) A woman having a new sexual partner D) A multiple gestation pregnancy 29) To diagnose preeclampsia based on the blood pressure level, on 2 separate occasions, the blood pressure must be: A) Systolic BP ≥ 140 mmHg or Diastolic BP ≥ 90 mmHg B) Systolic BP ≥ 140 mmHg or Diastolic BP ≥ 110 mmHg C) Systolic BP ≥ 160 mmHg or Diastolic BP ≥ 90 mmHg D) Systolic BP ≥ 160 mmHg or Diastolic BP ≥ 110 mmHg 30) When do most cases of preeclampsia occur? A) B) C) D) First trimester Early second trimester Late second trimester Late third trimester 31) Which medication is commonly prescribed if a woman has preeclampsia with contractions? A) B) C) D) Metoprolol Calcium gluconate Magnesium sulfate Pregabalin 32) If preeclampsia causes seizures, what is this condition referred to as? A) B) C) D) Epilepsy Eclampsia Placenta previa Kernicterus 33) The only cure for preeclampsia or eclampsia is: A) B) C) D) Magnesium sulfate Calcium gluconate Lorazepam Delivery 34) Which of the following is the most definitive sign of pregnancy? A) Positive sign B) Probable sign C) Presumptive sign D) None of these 35) Which of the following is the least definitive sign of pregnancy? A) B) C) D) Positive sign Probable sign Presumptive sign None of these 36) Which of the following is not a positive sign of pregnancy? A) Palpation of the fetus by the healthcare provider B) Ultrasound and visualization of the fetus C) Fetal heart tones auscultated by the healthcare provider D) Positive blood pregnancy test (testing for hCG) 37) The nurse inspects a woman’s vaginal area and observes cervical softening. This is referred to as: A) B) C) D) Goodell’s sign Chadwick’s sign Hegar’s sign Tinel’s sign 38) All of the following are presumptive signs of pregnancy except for: A) B) C) D) Amenorrhea Enlarged uterus Swollen and tender breasts Urinary frequency 39) Goodell’s sign, Chadwick’s sign, and Hegar’s sign are all: A) Positive signs of pregnancy B) Probable signs of pregnancy C) Presumptive signs of pregnancy D) Not signs of pregnancy 40) Quickening is a: A) B) C) D) Positive sign of pregnancy Probable sign of pregnancy Presumptive sign of pregnancy It is not a sign of pregnancy 41) When can quickening first be observed in pregnancy? A) B) C) D) At 12 weeks At 16 weeks At 20 weeks At 24 weeks 42) When can the fetal heart rate first be first heard? A) B) C) D) 6-8 weeks 10 to 12 weeks 16 to 18 weeks 20-22 weeks 43) Melasma, blotchy hyperpigmentation of the skin, is due to elevated levels of: A) B) C) D) Estrogen Alpha-fetoprotein Prolactin Progesterone 44) What is the normal range for fetal heart rate (FHR)? A) 90-120 bpm B) 100-140 bpm C) 110-160 bpm D) 130-200 bpm 45) What are Mongolian spots? A) Malignant, cancerous skin legions that can aggressively attack a child’s immune system B) Blue to black colored patches or stains that are benign and usually fade by 2 to 3 years C) Red spots that are rash-like in appearance and that are benign D) Blue to black colored patches that can either be malignant or benign and that are permanent for life 46) Which body part does the fetus receive nourishment through? A) B) C) D) Umbilical cord Placenta Fallopian tube Uterus 47) What is the safe amount of alcohol that a woman can drink during pregnancy? A) B) C) D) 2 drinks a day 1 drink a day A half of drink a day There is no safe level of alcohol consumption in pregnancy 48) Which of the following statements is false regarding alcohol consumption during pregnancy? A) Alcohol can increase the risk of miscarriage B) Alcohol easily passes through the placenta C) Though alcohol can cause damage to the fetus during any time in pregnancy, it is especially damaging during the third trimester, carrying the risk of major birth defects D) A woman should not drink if she is trying to get pregnant or think that she is pregnant 49) All of the following are common symptoms of fetal alcohol poisoning except for: A) Microcephaly B) Formation of tumors on various body organs C) Low birth weight D) Learning disabilities 50) What does chorionic villus sampling test for? A) To check a fetus’s bone density B) To check whether the fetus has chromosomal abnormalities C) To check a fetus’s heart health D) To check a fetus’s lung maturation 51) Performing chorionic villus sampling increases the risk of: A) B) C) D) Maternal hemorrhage Ascites Birth defects Miscarriage 52) Which statement is false regarding chorionic villus sampling (CVS)? A) CVS takes a sample of tissue from the placenta B) A CVS is normally performed between 6-8 weeks of pregnancy C) CVS testing is optional and completely dependent on the woman D) Before a CVS test is done, a woman will have an ultrasound performed 53) Besides chorionic villus sampling, what is the only other test that can check for chromosomal abnormalities? A) B) C) D) Transvaginal ultrasound Maternal blood test Amniocentesis Nuchal translucency test 54) Most miscarriages occur in which trimester? A) First trimester B) Second trimester C) Third trimester D) Any trimester 55) What is the leading cause of preventable birth defects and developmental disabilities in the United States? A) B) C) D) Advanced maternal age in pregnancy Cocaine use during pregnancy Alcohol use during pregnancy Junk food eating during pregnancy 56) Hyperemesis gravidarum is characterized primarily by: A) B) C) D) Orthostatic hypotension Nausea and vomiting Headaches Cramps 57) Hyperemesis gravidarum is believed to be caused by rising levels of: A) B) C) D) Estrogen Progesterone Luteinizing hormone Human chorionic gonadotropin 58) Hyperemesis gravidarum almost exclusively occurs in the: A) B) C) D) First trimester Second trimester Early part of the third trimester Late part of the third trimester 59) Home pregnancy tests that check to see whether a woman is pregnant checks to see if what substance is present in the urine? A) Human chorionic gonadotropin B) Estrogen C) Progesterone D) Prolactin 60) What drug is misoprostol used in combination with to terminate a pregnancy? A) B) C) D) Tetracycline Mifepristone Thalidomide Methotrexate 61) Drugs that have adequate and well-controlled human studies that have failed to demonstrate a risk to the fetus in the first trimester (and later trimesters) are of: A) B) C) D) Category A Category B Category C Category D 62) A woman can safely take all of the following in pregnancy except for: A) B) C) D) Levothyroxine Single dose of vitamin A Megadose of vitamin A Single dose of folic acid 63) Prolactin is produced by the: A) B) C) D) Liver Kidneys Pituitary gland Pineal gland 64) What is the primary function of prolactin in females? A) It thickens the coating of the uterus B) It enlarges a woman’s breasts and prepares them for milk production C) It triggers ovulation and development of the corpus luteum D) It stimulates the synthesis and secretion of FSH and LH 65) All of the following cause high levels of serum prolactin in the body except for: A) B) C) D) Pregnancy Prolactinoma Certain medications Hyperthyroidism 66) What hormone is responsible for uterine stimulation in labor? A) B) C) D) Prolactin Estrogen Progesterone Oxytocin 67) What is the main function of progesterone? A) It lubricates the vagina, making it comfortable for a woman to have sex B) It stimulates the ovaries to ovulate C) It stimulates the ovaries, enabling growth of the eggs D) It thickens the lining of the uterus each month to receive and nourish a fertilized egg 68) Which statement is false regarding luteinizing hormone? A) In females, an acute rise of luteinizing hormone triggers ovulation B) In females, an acute rise of luteinizing hormone triggers the development of the corpus luteum C) Luteinizing hormone works inversely with follicle-stimulating hormone (FSH) D) In males, luteinizing hormone works to stimulate the production of testosterone 69) Which of the following is false regarding a woman’s physiology during pregnancy? A) A woman has increased peristalsis during pregnancy B) Varicose veins become more severe during pregnancy C) A woman’s kidneys increase in size during pregnancy (physiologic hydronephrosis) D) A woman’s blood clotting factors increase during pregnancy especially after labor 70) A newborn is defined as anyone who is equal to or less than: A) B) C) D) 14 days old 28 days old 1 year old 2 years old 71) What supplementation is recommended for all breastfed infants in the first few days of life? A) B) C) D) Vitamin A Vitamin B12 Vitamin C Vitamin D 72) Which statement is false regarding erythema toxicum? A) Erythema toxicum is characterized by a rash of small yellow-to-white-colored papules surrounded by red skin B) Erythema toxicum is a benign condition C) Erythema toxicum is rare in newborns D) Erythema toxicum usually clears within 2 weeks and is usually gone by age 4 months without any treatment 73) Which of the following statements is false about milia? A) Milia are white bumps B) They typically appear on the arms and legs C) They are harmless D) They can occur in people of all ages, but are most common in newborns 74) What test is used to check for congenital cataracts? A) Eye drainage examination B) Red reflex test C) Snell’s vision test D) Rosenbaum chart test 75) Which statement is false regarding vernix caseosa? A) It is a protective substance secreted from sebaceous glands that covers the fetus during pregnancy B) Vernix caseosa looks like a whitish, cheesy substance C) Full-term neonates usually a lot of vernix caseosa D) The presence and amount of vernix caseosa can assist in estimating the gestational age of a newborn 76) Which statement is false regarding lanugo? A) Lanugo is fine, downy hair that develops after 16 weeks of gestation B) The amount of lanugo increases as the fetus ages C) The presence and amount of lanugo can assist in estimating the gestational age of a newborn D) The lanugo gradually falls out 77) When does the posterior fontanel usually close by? A) B) C) D) 1 month 3 months 6 months 12-18 months 78) When does the anterior fontanel usually close by? A) B) C) D) 1-3 months 3-5 months 6-9 months 12-18 months 79) All of the following conditions are benign in a newborn just delivered except for: A) B) C) D) Circumoral cyanosis Cephalhematoma Erythema toxicum Milia 80) During pregnancy, plasma volume increases up to: A) B) C) D) 10% 20% 25% 50% 81) The increased blood plasma volume in pregnancy is most attributable to increased levels of: A) B) C) D) Erythropoietin Aldosterone Cortisone Prolactin 82) What is the only immunoglobulin that crosses the placenta during pregnancy? A) B) C) D) IgA IgE IgG IgD 83) Group B strep bacteria is tested for in a pregnant woman between: A) B) C) D) 20 and 24 weeks 24 and 28 weeks 30 and 34 weeks 35 and 37 weeks 84) How is Group B strep bacteria tested for in a pregnant woman? A) B) C) D) Oral swab Vaginal and rectal swab Blood test Vaginal and rectal biopsy 85) If a woman is found positive for Group B strep, what is the treatment? A) B) C) D) Erythromycin Penicillin Cephalexin Levofloxacin 86) Which of the following is false regarding group B strep? A) Group B strep is naturally found in the intestines and urinary and genital tracts B) Most women carrying group B strep bacteria have no symptoms C) Group B strep bacteria is carried in less than 1% of women D) Group B strep bacteria can be transmitted to a fetus and cause harm to the fetus 87) White blood cells are most elevated in pregnancy during: A) B) C) D) The first trimester The second trimester The third trimester The first and third trimesters 88) During pregnancy, what level can hemoglobin drop to without any pathology being present? A) B) C) D) 10. 5 g/dL 10 g/dL 9.5 g/dL 9 g/dL 89) During pregnancy, what level can hematocrit drop to without any type of pathology being present? A) B) C) D) 30% 28% 26% 24% 90) Which of the following is false regarding pregnancy? A) During pregnancy, the alkaline phosphatase level decreases B) During pregnancy, the ALT, AST, and GGT values stay the same C) During pregnancy, the platelet count stays the same D) During pregnancy, the glomerular filtration rate (GFR) increases 91) Which of the following statements is true regarding drugs and pregnancy? A) All bisphosphonates are category X drugs and should be avoided during pregnancy B) All hormonal drugs, natural or synthetic, are category X drugs and should be avoided in pregnancy C) All vaccines are contraindicated in pregnancy D) Lithium is safe to take in pregnancy 92) Which statement is true regarding a woman’s heartbeat during pregnancy? A) It decreases by about 15 to 20 beats per minute B) It remains unchanged C) It increases by about 5 beats per minute D) It increases by about 15 to 20 beats per minute 93) Which statement is true regarding preload and afterload in pregnancy? A) The preload and afterload both decrease in pregnancy B) The preload and afterload both increase in pregnancy C) The preload increases and the afterload decreases D) The preload decreases and the afterload increases 94) Which of the following is false regarding a mammary souffle? A) It is a murmur heard over the breasts in pregnancy B) It can occur in one or both breasts C) It occurs only early in pregnancy D) It can exist during lactation 95) Which statement is false regarding edema in pregnancy? A) Mild edema of the lower extremities and the feet is normal in pregnancy B) Edema is most noticeable in the third trimester C) The edema is caused by the additional blood and fluid created during pregnancy D) Sudden, severe swelling of the face and hands could be indicative of placenta previa 96) Which statement is true regarding asymptomatic bacteriuria in pregnant women? A) Asymptomatic bacteriuria does not need to be treated until a woman exhibits symptoms B) Asymptomatic bacteriuria should only be treated in the first trimester C) Asymptomatic bacteriuria should only be treated if it occurs in the third trimester D) Asymptomatic bacteriuria should always be treated at any part of pregnancy 97) What happens to the kidneys during pregnancy? A) The kidneys decrease in size B) The glomerular filtration rate decreases C) The kidneys increase in size D) The ureters of the kidneys become more constricted 98) A woman who has been previously diagnosed with bipolar disorder is contemplating pregnancy. What instructions should the nurse practitioner give regarding lithium usage during pregnancy? A) Lithium is completely safe to use during pregnancy and should be continued to keep the bipolar disorder symptoms in control B) Lithium may increase the frequency of headaches during pregnancy due to an unknown cause, so its use should be taken with caution C) Lithium may interfere with hormones during pregnancy and may cause frequent nausea D) Lithium is a teratogen that is linked to cardiac defects in fetuses and should not be taken during pregnancy 99) What is placenta previa? A) A condition in which the placenta is partially or completely implanted against the lower part of the uterus B) A condition in which blood supply to the placenta diminishes and causes necrosis of the placental tissue C) An autoimmune condition in which the body mistakenly attacks the placenta, identifying it as foreign to the body D) A condition in which the placenta gets detached from the fetus, causing the fetus imminent distress 100) What is the most prominent symptom of placenta previa? A) Painful abdominal cramps B) Painless vaginal bleeding C) Intermittent seizures that occur during late pregnancy D) Uncontrolled hypertension 101) How is placenta previa diagnosed? A) B) C) D) Through a vaginal examination Through elevated levels of AFP Through a CT scan Through ultrasound 102) A woman comes to a clinic for a pregnancy checkup at 20 weeks and gets a sonogram that shows partial placenta previa. What is the most likely outcome of this condition? A) Regardless of whether the placenta previa improves or not, the mother will have to deliver by C-section B) The woman’s placenta previa will most likely worsen during pregnancy to complete placenta previa C) The woman’s placenta previa likely will resolve as the pregnancy progresses D) The woman’s placenta previa, whether it worsens or not, will allow for a natural vaginal birth 103) When are most women routinely screened for gestational diabetes? A) B) C) D) Between 16 and 20 weeks Between 20 and 24 weeks Between 24 and 28 weeks Between 28 and 32 weeks 104) A pregnant woman undergoes the 1-hour oral glucose tolerance test (OGTT). 1 hour after she drinks the solution, her blood sugar is taken and is found to be 132 mg/dL. How does the nurse practitioner interpret this result? A) B) C) D) Low Normal High Indeterminate 105) A pregnant woman undergoes the 1-hour oral glucose screening test. 1 hour after she drinks the 50-gram glucose solution, her blood sugar is taken and is found to be 160 mg/dL. What is the next step that the nurse practitioner takes? A) Tell the patient to take in more dietary glucose B) Tell the patient the result is normal and that gestational diabetes is not present C) Diagnose the patient with gestational diabetes D) Have the patient undergo the 3-hour oral glucose tolerance test (OGTT) 106) A pregnant woman undergoes a 3-hour glucose tolerance test (OGTT). 1 hour after the test, the blood sugar is 190 mg/dL. 2 hours after the test, the blood sugar is 160 mg/dL. 3 hours after the test, the blood sugar is 150 mg/dL. How does the nurse practitioner interpret these results? A) The results show low blood sugar B) The results show normal blood sugar C) The woman has a diagnosis of gestational diabetes D) The woman now needs to undergo a 5-hour oral glucose tolerance test (OGTT) 107) What hormone is responsible for the onset of gestational diabetes? A) Estrogen B) Progesterone C) Human placental lactogen D) Human chorionic gonadotropin 108) Women who get gestational diabetes are at high risk for: A) B) C) D) Death Unexplained seizure disorders Type II diabetes Pneumonia 109) According to Bartholomew’s rule of fourths, where would the fetus be at 36 weeks into the pregnancy? A) Symphysis pubis B) Midway between the symphysis pubis and the umbilicus C) Umbilicus D) Xiphoid process 110) A molar pregnancy is also known as: A) B) C) D) An ectopic pregnancy A viable pregnancy Hydatidiform mole A stillbirth 111) What is the treatment for a molar pregnancy? A) Early delivery of the fetus B) C-section C) Removal of all of the growth from the uterus D) Megestrol Acetate 112) What is a potential complication of a molar pregnancy? A) Sterility B) Cancer C) Abruptio placentae D) Eclampsia 113) Which statement is false regarding a molar pregnancy? A) In a complete molar pregnancy, there is no embryo or normal placental tissue B) In a partial molar pregnancy, there is an abnormal embryo and possibly some normal placental tissue C) A molar pregnancy may seem like a normal pregnancy in the early stages D) Molar pregnancies produce no symptoms that would alarm a woman to think there may be an abnormality 114) What is the cause of a molar pregnancy? A) Nutritional deficiencies during pregnancy B) An abnormally fertilized egg C) Taking teratogens during pregnancy D) In vitro fertilization 115) After a molar pregnancy, it is recommended that: A) A woman wait 3 months before getting pregnant again B) A woman wait 6-12 months before getting pregnant again C) A woman wait 3-5 years before getting pregnant again D) A woman never get pregnant again 116) Which of the following statements is false regarding an ectopic pregnancy? A) An ectopic pregnancy is a pregnancy that takes place outside of the uterus B) Symptoms include pelvic pain and vaginal bleeding C) The baby survives about 50% of the time D) Ectopic pregnancies can be fatal to the mother 117) What is the most common place for an ectopic pregnancy? A) The fallopian tubes B) The ovaries C) The cervix D) The abdomen 118) Which of the following statements is false regarding ectopic pregnancy? A) About 1-2% of all pregnancies are ectopic pregnancies B) In an ectopic pregnancy, the fertilized egg can be transplanted into the uterus successfully about half of the time C) Most ectopic pregnancies take place in some part of the fallopian tube, which are also referred to as “tubal pregnancies” D) Most women who have an ectopic pregnancy have normal pregnancies and births in the future 119) All of the following are risk factors for an ectopic pregnancy except for: A) Use of a cervical cap B) Current use of an intrauterine device (IUD) C) History of pelvic inflammatory disease D) History of ectopic pregnancy 120) Human chorionic gonadotropin is produced by the: A) B) C) D) Uterus Fetus Placenta Fallopian tubes 121) When does the umbilical cord usually separate from the newborn after birth? A) B) C) D) 1 day 1 week 3 weeks 1 month 122) A woman has had 4 pregnancies. In her first pregnancy, she gave birth to twins. In her second pregnancy, the fetus died in utero at 12 weeks. In her third pregnancy, the fetus died in utero at 14 weeks. She is currently in the 16th week of a healthy pregnancy. What is this woman’s obstetric history? A) B) C) D) G4P2A2 G4P1A2 G4P2A1 G4P1A1 123) What is the estimated date of delivery (EDD) for a woman in which the first day of her last menstrual period was January 7, 2015? A) B) C) D) October 7, 2015 November 7, 2015 October 14, 2015 November 14, 2015 124) The first day of the last menstrual period that a woman had was March 10, 2016. Based on this date, when is her expected date of delivery (EDD)? A) B) C) D) November 10, 2016 December 10, 2016 November 17, 2016 December 17, 2016 125) Which of the following is false regarding meconium? A) Meconium is the first feces of a newborn B) Meconium is usually a dark green color C) If an infant passes meconium in the womb, it can meconium aspiration syndrome D) Preterm neonates are most at risk for meconium aspiration 126) How much weight does a healthy woman typically gain during pregnancy? A) A healthy woman gains no weight during pregnancy B) 5-10 lbs C) 15-25 lbs D) 30-50 lbs 127) Mittelschmerz is pain associated with: A) Proliferation of sperm into a woman’s body during sex B) Hyperactive fetus in the womb C) Ovulation D) Fertilization of an egg 128) How should a pregnant woman wear her seatbelt? A) With the lap belt above the uterine fundus B) With the lap belt below the uterine fundus C) Either above or below the uterine fundus; it doesn’t matter D) A pregnant woman should not wear a seatbelt 129) Smoking during pregnancy increases the fetus’s risk of: A) B) C) D) Fetal alcohol syndrome Cardiac defects Deafness Intrauterine growth restriction 130) The vast majority of victims of Shaken Baby Syndrome are: A) B) C) D) Less than 1-year old 1-2 years old 2-3 years old 4-5 years old 131) Which demographic group is most likely to be the cause of Shaken Baby Syndrome? A) B) C) D) Teenage mothers Teenage fathers Mothers in their 40s Fathers in their 40s 132) All of the following are common symptoms of Shaken Baby Syndrome except for: A) B) C) D) Hemolytic anemia Detached retina Serious brain injury Skull fractures 133) Which of the following statements is false regarding Shaken Baby Syndrome? A) Shaken Baby Syndrome is considered a form of child abuse B) Permanent brain damage can result from Shaken Baby Syndrome C) Shaken Baby Syndrome is most often caused by rough play with the child or the child falling due to inattention from the caregiver D) Death can result from Shaken Baby Syndrome 134) Which type of contraception should a woman not use if she wants to get pregnant within the next 9 months? A) B) C) D) Intrauterine device Cervical cap Diaphragm Depo-Provera 135) Nitrofurantoin is used in pregnancy to treat: A) B) C) D) Headaches UTIs Leg cramps It should not be used in pregnancy 136) Which of the following statements is true regarding the use of nitrofurantoin? A) It is safe to use during any stage in pregnancy B) It is safe to use only during the first 12 weeks of pregnancy C) It is safe to use up until the end of the 37th week of pregnancy D) It should not be used in pregnancy 137) A pregnant woman is in her 18th week of pregnancy. Which of the following antibiotics would be least likely to be prescribed? A) B) C) D) Nitrofurantoin Amoxicillin Trimethoprim-sulfamethoxazole Cephalexin 138) Which of the following statements is false regarding breastfeeding? A) Clicking noises during breastfeeding is normal and indicates that the baby is feeding well B) The baby should have the entire nipple and areola inside of his or her mouth C) Breastfeeding should be on demand throughout the day and night D) The tip of the infant’s nose, cheeks and chin should be touching the breast 139) Which of the following statements is true regarding a woman breastfeeding and having sore nipples? A) The woman should start breastfeeding on the less painful breast first B) The first should start breastfeeding on the more painful breast first C) A woman should stop breastfeeding if she has sore nipples D) A woman should breastfeed only sparingly if she has sore nipples 140) Which of the following statements is false regarding mastitis? A) Mastitis is inflammation of the breast B) Mastitis most often occurs during the first 6 months of a woman beginning breastfeeding C) If a woman has mastitis, she should stop breastfeeding as to not pass the infection to the baby D) Mastitis can be a painful condition 141) What is the most common causative agent of mastitis? A) Group A streptococcus B) Group B streptococcus C) Staphylococcus aureus D) E. coli 142) All of the following are risk factors for mastitis except for: A) Poor latching of the infant on the breast B) Infrequent breast feeding C) Previous history of mastitis D) Taking hot showers 143) How long is breastfeeding recommended for according to the American Academy of Pediatrics (AAP)? A) B) C) D) The first 6 months of life The first 9 months of life The first year of life The first 2 years of life 144) Breastfeeding should be done: A) B) C) D) Every hour Every 2 hours Every 4 hours On demand 145) All of the following are contraindications for a woman breastfeeding except: A) The mother is hepatitis B positive B) The baby has galactosemia C) The mother is HIV positive D) The mother is actively taking chemotherapy drugs 146) Maternal benefits of breastfeeding include all of the following except: A) Breastfeeding promotes weight loss B) Breastfeeding causes the release of oxytocin, which helps the woman’s uterus return to its pre-pregnancy size C) Breastfeeding lowers a woman’s risk of breast and ovarian cancer D) Breastfeeding helps a woman’s ability to form blood clots 147) All of these drugs are categorized as Category X drugs and should never be taken in pregnancy except for: A) B) C) D) Isotretinoin (Accutane) Metoprolol Warfarin sodium (Coumadin) Thalidomide 148) In a newborn: A) The chest circumference is about 1 to 2 cm more than the head circumference B) The head circumference is about 1 to 2 cm more than the chest circumference C) The chest circumference is about 3 to 4 cm more than the head circumference D) The head circumference is about 3 to 4 cm more than the head circumference 149) What may cause bulging fontanels in a newborn? A) B) C) D) Dehydration Sleeping Blinking Crying 150) A sunken fontanelle can be an indicator of: A) B) C) D) Dehydration Fluid overload Atrial septal defect Tetralogy of Fallot 151) A mother gives birth to a newborn who is 10 hours old. The newborn’s bilirubin level is 8 mg/dL. This represents a: A) B) C) D) Decreased level Normal level Slightly elevated level Critically elevated level 152) Preterm infants are those born before: A) B) C) D) 34 weeks 36 weeks 37 weeks 38 weeks Maternity answers 1) (A) Caput succedaneum is diffused edema of the scalp that crosses the midline. It disappears without treatment. It is not a pathological finding. Image: Caput succedaneum 2) (C) Caput succedaneum is caused by intrauterine and vaginal pressure from a prolonged or difficult vaginal labor 3) (B) A cephalhematoma is traumatic subperiosteal hemorrhage where there is a collection (swelling) of blood that does not cross the midline or suture lines. Image: Cephalhematoma 4) (D) Colostrum is the first milk produced by the breasts in pregnancy. 5) (D) It is recommended that RhoGAM be given to all pregnancies of Rh negative mothers, regardless of whether they result in abortions, miscarriages, or ectopic pregnancies. 6) (C) RhoGAM should be given at 28 weeks of gestation and within 72 hours after birth. 7) (C) The first trimester of pregnancy is the first 12 weeks of pregnancy, taking place from weeks 1-12. The second trimester then takes place from weeks 13-27. The third trimester takes place from week 28 to birth. 8) (A) A miscarriage is defined as the loss of a fetus before the 20th week of pregnancy. 9) (B) A threatened abortion is vaginal bleeding that occurs in the first 20 weeks of pregnancy that is sometimes accompanied by abdominal cramps. A threatened abortion means that an abortion has not yet occurred but can possibly occur (source: healthline.com). 10) (B) A complete abortion is an abortion in which all of the products (tissue) of conception leave the body. 11) (A) A missed abortion is an abortion in which the fetus dies or was never formed but the body does not recognize the pregnancy loss or expel the pregnancy products. 12) (D) A missed abortion is an abortion in which the fetus dies or was never formed—this occurs before there are any external signs of abortion such as vaginal bleeding. The unviable fetus (if formed) and pregnancy products stay retained inside the woman’s body. The placenta may still continue to release hormones and a woman may still continue to experience signs of pregnancy. 13) (A) The effects of progesterone are believed to cause constipation during pregnancy. 14) (C) A Coombs test is a test that checks for the presence of antibodies that may destroy red blood cells. The direct Coombs test involves looking directly at red blood cells found in a sample of blood. The indirect Coombs test looks at the liquid part of the blood (the plasma). 15) (A) A direct Coombs test measures antibodies that are stuck to the surface of red blood cells. An indirect Coombs test measures antibodies that are floating in the blood that could act against red blood cells. 16) (B) The indirect Coombs test measures antibodies that are floating in the blood that could act against red blood cells. 17) (A) The direct Coombs test is the most specific test to check for autoimmune hemolytic anemia. The direct Coombs test involves looking directly at red blood cells found in a sample of blood to see if there are any antibodies attached to the red blood cells that may be causing their destruction. Autoimmune hemolytic anemia is a condition in which there is low red blood count due to destruction of red blood cells by the immune system. The direct Coombs test can be used to determine if it is the immune system that is responsible for the destruction of the red blood cells. Though the indirect Coombs test may be used to check for autoimmune hemolytic anemia also, the direct coombs test is more specific, since it checks to see if antibodies are directly attached to the red blood cells. The indirect coombs test is most used often for blood transfusion compatibility and Rh compatibility. 18) (D) Asthma is not a risk factor for abruptio placentae. Risk factors for abruptio placentae include previous placental abruption, high blood pressure, abdominal trauma, smoking, cocaine use, premature rupture of the membranes, blood clotting disorders, multiple gestation pregnancy, and maternal age greater than 40 years old. 19) (B) HELLP syndrome is a serious but rare complication of preeclampsia. 20) (D) The HELLP in HELLP syndrome is really an acronym that stands for Hemolysis, Elevated Liver enzymes, and Low Platelets. Pressure ulcers is a not associated with HELLP syndrome. 21) (B) Hemoglobin, as well as hematocrit, levels decrease during pregnancy. This is because a woman’s plasma volume increases 30%-50% during pregnancy. This causes hemodilution, which causes a drop in hemoglobin and hematocrit values. Alkaline phosphatase levels increase during pregnancy due to the growth of the fetal bones; the values are even higher in multiple gestation pregnancies. White blood cell count rises dramatically, especially near the end of pregnancy, to protect the mother during delivery in which her vagina opens widely, potentially allowing bacteria and pathogens to get in. Erythrocyte sedimentation rate (ESR) also rises during pregnancy. 22) (B) Alkaline phosphatase levels increase in pregnancy due to the growth of fetal bones in the woman’s body. 23) (B) Low alpha-fetoprotein ( AFP) level may possibly indicate Down syndrome. High AFP levels may indicate a multiple gestation pregnancy or neural tube defects such as spina bifida or anencephaly. 24) (A) Women taking folic acid have been found to have lower incidences of neural tube defects. 25) (A) A quadruple screen test is composed of alpha fetoprotein (AFP), human chorionic gonadotropin (hCG), estriol, and inhibin-A. In Down syndrome, the AFP will be low, the estriol will be low, the hcG will be high, and the inhibin-A will be high. 26) (C) The biggest risk factor for a woman having a baby with Down syndrome is advanced maternal age. As a woman gets older, her chance of conceiving a baby with Down syndrome increases. According to statistics, at 25 years of age, a woman has a 1 in 1200 chance of having a baby with Down syndrome. By age 35, a woman has a 1 in 350 chance of conceiving a baby with Down syndrome. By age 40, the chance is 1 in 100. By age 45, there is a 1 in 30 chance. By age 49, there is a 1 in 10 chance. This is due to the fact that older eggs have a greater risk of improper chromosome division. 27) (B) Glucosuria is not a symptom directly associated with preeclampsia. The classic triad symptoms of preeclampsia are hypertension, proteinuria, and edema. 28) (B) Risk factors for preeclampsia include a personal or family history of preeclampsia, a first pregnancy (the risk of developing preeclampsia is highest during the first pregnancy), a new partner (each pregnancy with a new partner increases the risk of preeclampsia greater than it would be with a second or third pregnancy with the same partner), age (pregnancy at an age greater than 40 puts a woman more at risk), obesity, multiple gestation pregnancy, an interval between pregnancies either less than 2 years or greater than 10 years, and a history of certain conditions such as hypertension, diabetes, clotting disorders, or lupus. 29) (A) To diagnose preeclampsia based on the blood pressure, the systolic blood pressure must be greater than 140 mmHg or the diastolic blood pressure must be greater than 90 mmHg on 2 separate occurrences. 30) (D) Most cases of preeclampsia occur in the late third trimester, at about 34 weeks of gestation or later. 31) (C) If a woman’s preeclampsia has progressed to the point where she is having contractions, magnesium sulfate is commonly given in this situation. 32) (B) If preeclampsia causes seizures, this condition is referred to as eclampsia. 33) (D) The only cure for preeclampsia or eclampsia is delivery. 34) (A) A positive sign is the most definitive sign of pregnancy. A positive sign is the only sign that is a definite, absolute sign of pregnancy. 35) (C) A presumptive sign is the least definitive sign of pregnancy. Presumptive signs are the least objective and the least accurate to predict a state of pregnancy. 36) (D) A positive blood pregnancy test testing for hCG (human chorionic gonadotropin) is not a positive sign of pregnancy; it is a probable sign of pregnancy. hCG can also be elevated in cases of nonpregnancy, such as in a molar pregnancy and in ovarian cancer. So, it’s not a definite sign of pregnancy. There are only 3 positive signs of pregnancy. These include palpation of the fetus by the healthcare provider, ultrasound and visualization of the fetus, and fetal heart tones auscultated by the healthcare provider. 37) (A) Goodell’s sign represents cervical softening. 38) (B) An enlarged uterus is a probable sign of pregnancy. Presumptive signs of pregnancy include amenorrhea, nausea/vomiting, breast changes such as the breasts becoming swollen and tender, fatigue, and urinary frequency. 39) (B) Goodell’s sign (cervical softening), Chadwick’s sign (blue discoloration of the cervix and vagina), and Hegar’s sign (softening of the uterine isthmus) are all probable signs of pregnancy. 40) (B) Quickening is a probable sign of pregnancy. It isn’t a positive sign of pregnancy, because even though a woman may feel like a fetus is inside of her moving around, it could be misinterpreted. Probable signs of pregnancy include Goodell’s sign, Chadwick’s sign, Hegar’s sign, an enlarged uterus, ballottement, positive urine or blood pregnancy tests, and quickening. 41) (B) Quickening, the phenomenon in which a pregnant woman feels the baby’s movement for the first time, starts at about week 16. 42) (A) The fetal heart rate can first be heard at 6-8 weeks via ultrasound and 10-12 weeks via Doppler. 43) (A) Melasma (the mask of pregnancy), also called chloasma, is due to high levels of estrogen in the body. 44) (C) The normal fetal heart rate (FHR) is 110-160 bpm. 45) (B) Mongolian spots are blue to black colored patches or stains that are benign and usually fade by 2 to 3 years. 46) (B) It is through the placenta that the fetus receives nourishment during pregnancy. 47) (D) There is no safe amount of alcohol that woman can drink during pregnancy. Any alcohol consumption during pregnancy is discouraged. This includes even occasional alcohol such as a glass of wine during dinner or a mug of beer while out with friends. Alcohol is easily passed along to the baby, who is less able to eliminate it than the mother (source: kidshealth.org). 48) (C) There is no known safe amount of alcohol to drink during pregnancy. Any amount of alcohol can harm a developing fetus and increase the risk of miscarriage. Alcohol easily passes through the placenta, the organ that nourishes a fetus during pregnancy. Alcohol exposure during the first trimester (while a woman may not even know she is pregnant yet) is especially hazardous and can cause major birth defects. Later in pregnancy, drinking alcohol can cause poor growth and brain damage that could lead to learning and behavioral problems. These problems can be prevented by not drinking any alcohol during pregnancy. A woman should not drink if she is trying to get pregnant or think that she may be pregnant (source: kidshealth.org). 49) (B) Fetal alcohol syndrome (FAS) has various physical defects, along behavioral, and learning disabilities. Physical disabilities include certain facial features such as small eye openings, a thin upper lip, and a smooth philtrum (the groove between the nose and upper lip). FAS babies may have poor growth and may have low birth weight and a small head size. They may not grow or gain weight as well as other children and may be short as adults. They may have birth defects such as heart, bone, and kidney problems. Vision problems and hearing loss are common. They may have seizures and other neurological problems, such as poor balance and coordination. They may have delayed development such as not reaching milestones at the expected time. They also may have trouble sleeping. Behavioral problems may include fussiness and jitteriness. They may have poor social skills, hyperactivity, poor attention and concentration, learning disabilities, stubbornness, impulsiveness, and anxiety (source: kidshealth.org). 50) (B) Chorionic villus sampling (CVS) is a test done to check whether the baby has chromosomal abnormalities such as Down syndrome, Edward’s syndrome, Patau syndrome, Turner syndrome, etc. It does not check the health status of a fetus’s organs. 51) (D) Performing a chorionic villus sampling slightly increases the risk of a miscarriage. Maternal hemorrhage (CVS only poses the risk for slight bleeding), ascites, and birth defects are not risks associated with chorionic villus sampling. 52) (B) A CVS is normally performed between weeks 10-14 weeks of pregnancy. Doing a CVS before this time increases the risk for complications. A CVS is a procedure that takes a sample of tissue from the placenta. Since the placenta contains fetal cells, the cells can be tested for chromosomal abnormalities. CVS testing is completely optional and dependent on the woman who is pregnant. It is not mandated for any reasons at all. Before a CVS is performed, an ultrasound is done to determine the location of the placenta. This can determine whether it’s best for a doctor to take a sample of the placenta through the abdomen (transabdominal CVS) or through the cervix (transcervical CVS). A transabdominal CVS is more commonly used. 53) (C) Besides chorionic villus sampling, the only other test done to check for chromosomal abnormalities is an amniocentesis. An advantage that chorionic villus sampling has over an amniocentesis is that it can be done earlier in pregnancy. While chorionic villus sampling can be done between 10 and 14 weeks, an amniocentesis is performed between 15 and 18 weeks. While a CVS can be done earlier, an amniocentesis is safer, offering less risk of a possible miscarriage. A maternal blood test cannot show fetal chromosomal abnormalities. A standard ultrasound cannot determine chromosomal abnormalities. A nuchal translucency test is a type of ultrasound that measures the thickness of the fluid buildup at the back of the developing baby's neck. Though this test can be suggestive of Down syndrome, if this area is thicker than normal, it does not directly check a fetus’s chromosomes. 54) (A) Most miscarriages occur during the first trimester, specifically between the 7th and 12th weeks of pregnancy. 55) (C) Alcohol such as beer, wine, and hard liquor consumption during pregnancy is the leading cause of preventable birth defects and developmental disabilities in the United States. 56) (B) Hyperemesis gravidarum is characterized primarily by nausea and vomiting. The vomiting can be so severe that dehydration and weight loss can occur. 57) (D) Hyperemesis gravidarum is believed to be caused by rising levels of human chorionic gonadotropin (hCG). hCG is a hormone made by the placenta during pregnancy. Women with multiple gestation pregnancy are at higher risk for having elevated levels of hCG. 58) (A) Hyperemesis gravidarum occurs almost exclusively in the first trimester of pregnancy. 59) (A) Home pregnancy tests that check to see if a woman is pregnant use test strips to test a urine sample for human chorionic gonadotropin (hCG). It is important to know that even if hCG is detected in the urine sample, it is not a positive sign of pregnancy but a probable sign. This is because in certain circumstances, hCG may be produced in the body due to other conditions such as a tumor being present in the body. The only positive signs of pregnancy are palpation of the fetus by the healthcare provider, ultrasound and visualization of the fetus, and fetal heart tones auscultated by the healthcare provider. 60) (B) Misoprostol is used in combination with mifepristone to end a pregnancy (abortion). The woman first takes mifepristone followed 2 days later by misoprostol. This is a nonsurgical option for women who opt to terminate a pregnancy. Mifepristone works by blocking the action of progesterone, damaging uterine blood vessels. This vascular damage causes embryo detachment. Misoprostol then completes the process by inducing cervical dilation to expel all the contents from the uterus out of the body. 61) (A) Category A drugs are drugs that have adequate and well-controlled human studies that have failed to demonstrate a risk to the fetus in the first trimester (and later trimesters). Category B drugs are drugs that have shown no risk in animal studies, for where there are no adequate and well-controlled studies in pregnant women. Category C drugs are drugs in which animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. Category D drugs are drugs in which there is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but in certain cases potential benefits may warrant use of the drug in pregnant women despite potential risks. Category X drugs are drugs that are contraindicated in pregnancy. Studies in animals or humans have demonstrated fetal abnormalities and/or there is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience, and the risks involved in use of the drug in pregnant women clearly outweigh potential benefits. Category N drugs are drugs that have not yet been classified by the FDA (source: drugs.com). See the Pregnancy Category Chart in the reference section at the back of this book for this chart. 62) (C) Taking megadoses of vitamins in pregnancy is to be avoided. Megadoses of vitamin A has the probability of causing teratogenic effects to the fetus, so it should be avoided. Taking single doses of vitamins are safe in pregnancy; single doses of vitamins are categorized by the FDA as being of type category A, meaning that adequate and well-controlled human studies have failed to demonstrate a risk to the fetus in the first trimester of pregnancy (or later trimesters). Levothyroxine, likewise, is safe and is categorized by the FDA as a category A drug. 63) (C) Prolactin is produced by the pituitary gland. 64) (B) The primary function of prolactin in females is it enlarges a woman’s breasts and prepares them for milk production. The main function of progesterone is that it thickens the coating of the uterus. The main function of luteinizing hormone is it triggers ovulation and development of the corpus luteum. The main function of gonadotropin-releasing hormone is that is stimulates the synthesis and secretion of the gonadotropins, FSH and LH. 65) (D) Prolactin levels elevate during pregnancy, as it enlarges the breasts and prepares them for milk production. A prolactinoma s a noncancerous tumor of the pituitary gland in the brain, which causes the overproduction of the hormone prolactin. Certain medications such as metoclopramide can cause high levels of prolactin in the body. Hyperthyroidism is not linked to high levels of prolactin in the body. 66) (D) Oxytocin is the hormone responsible for uterine stimulation in labor. Oxytocin is also responsible for stimulation of milk ejection (milk letdown). 67) (D) One of the main and most important functions of progesterone is that it thickens the lining of the uterus each month. The enriched endometrial lining is prepared to receive and nourish a fertilized egg. If pregnancy occurs, progesterone is produced by the placenta and levels remain elevated throughout pregnancy. Estrogen lubricates the vagina, making sex more comfortable for a woman. Luteinizing hormone stimulates the ovaries to ovulate. Folliclestimulating hormone (FSH) stimulates the ovaries, enabling growth of the follicles (or eggs). 68) (C) Luteinizing hormones work synergistically (together) with FSH during the menstrual cycle. LH and FSH both rise and fall together in the menstrual cycle. They are inversely related. In females, an acute rise in LH triggers ovulation and the development of corpus luteum. The corpus luteum is the structure that produces progesterone, which thickens the lining of the endometrium in preparation for a fertilized egg. In males, LH works to stimulate the production of testosterone. 69) (A) A woman has decreased peristalsis during pregnancy, which can cause constipation; this is due to the effects of progesterone. Progesterone is also known to cause heartburn during pregnancy in a woman. Varicose veins become more severe during pregnancy. A woman’s kidneys increase in size during pregnancy (physiologic hydronephrosis), due to the increased blood volume in her body. A woman’s blood clotting factors increase during pregnancy especially after labor, to prevent massive blood loss. 70) (B) A newborn is defined as anyone who is 28 days old or younger. 71) (D) It is recommended that all breastfed infants receive vitamin D supplementation in the first few days of life. According to the American Academy of Pediatrics, a supplement of 400 IU per day of vitamin D is recommended for all breastfed infants (source: cdc.gov). 72) (C) Erythema toxicum is common in newborns, occurring in up to half of all healthy newborns. Erythema toxicum is a benign skin condition characterized by a rash of small yellowto-white-colored papules surrounded by red skin. Erythema toxicum usually disappears without any treatment or changes in skin care. It usually clears within 2 weeks of life and is usually gone by 4 months. Image: Erythema toxicum 73) (B) Milia most often appear on the nose and cheeks, not the arms and legs. Milia are white bumps that are benign in nature. They can occur in people of all ages, but are most common in newborns. Milia occurs in about 40% of newborns. Milia normally do not require any treatment and usually disappear on their own. Image: Milia 74) (B) The red reflex test is used to check for congenital cataracts. During the red reflex test, a red light is shone into the eyes. If the red reflex is present in both eyes, this is a normal finding. If the red reflex is diminished or absent in one or both eyes, this is indicative of cataracts. Because the eyes are so clouded in cataracts, the red light does not pass through; therefore, there is an absent red light reflex. In normal healthy eyes, the red light transmission will pass right through without obstruction. Image: Red reflex 75) (C) Vernix caseosa is a protective substance secreted from sebaceous glands that covers the fetus during pregnancy. It looks like a whitish, cheesy substance. Full-term neonates usually have little to no vernix caseosa. The presence and amount of vernix caseosa can assist in estimating the gestational age of a newborn. The more preterm the birth, the more vernix caseosa is present on the newborn. 76) (B) The amount of lanugo, just like the amount of vernix caseosa, decreases as the fetus ages, not increases. Lanugo is fine, downy hair that develops on a fetus after 16 weeks of gestation. The presence and amount of lanugo can assist in estimating the gestational age of a newborn. The lanugo gradually falls out. 77) (B) The posterior fontanel usually closes by 2-3 months. 78) (D) The anterior fontanel usually closes by 12-18 months. 79) (B) A cephalhematoma is abnormal and could be a sign of serious bodily harm. Circumoral cyanosis, erythema toxicum, and milia are common, benign conditions. If circumoral cyanosis persists past 24 hours, this is a sign of concern. 80) (D) Blood plasma volume increases in pregnancy up to 50%. 81) (B) The increased blood plasma volume in pregnancy is most attributable to the increased levels of aldosterone. 82) (C) IgG is the only immunoglobulin that crosses the placenta during pregnancy and makes up 75% to 85% of all antibodies in the infant. 83) (D) Group B strep bacteria is tested for in a pregnant woman between 35 and 37 weeks. Studies show that testing done within 5 weeks of delivery is the most accurate at predicting the GBS status at birth. 84) (B) Group B strep bacteria is tested for in a pregnant woman through a vaginal and rectal swab. The sample is then taken to a lab where culture & sensitivity testing is done for any presence of GBS. Test results are usually available within 24 to 48 hours. 85) (B) IV penicillin is the primary treatment for group B strep given to a woman who is positive for group B strep bacteria. Another antibiotic, ampicillin, can also be used. 86) (C) Group B strep is found in approximately 25% of all healthy women. Group B strep is naturally found in the intestines and urinary and genital tracts. Most women carrying group B strep bacteria have no symptoms. The reason group B strep bacteria is tested for in pregnancy (between weeks 35 and 37) is because it can be transmitted to a fetus and can cause harm to the fetus. Therefore, if a woman is found to be a carrier of group B strep, she will be treated with IV antibiotics, with penicillin being the treatment of choice. 87) (C) White blood cells, particularly neutrophils, are elevated all throughout pregnancy but they elevate the most during the third trimester, especially the last part of the third trimester close to delivery. A few hours after delivery, healthy women have been documented as having WBC counts varying from 9,000 to 25,000/mm. By 4 weeks post-delivery, typical WBC ranges are similar to those in healthy non-pregnant women. 88) (C) The normal hematocrit in a healthy, nonpregnant woman is 12-16 g/dL. During pregnancy hemoglobin can drop as low as 9.5 g/dL without any type of pathology being present. This is because plasma volume increases during pregnancy, causing hemodilution. A hemoglobin below 9.5 g/dL is likely indicative of iron-deficiency anemia or some other type of pathology. 89) (B) The normal hematocrit level in a healthy, non-pregnant woman is 37% - 47%. During pregnancy (by the third trimester), the hematocrit can drop as low as 28% without any type of pathology present. This is because plasma volume increases during pregnancy, causing hemodilution. 90) (A) During pregnancy, the alkaline phosphatase level increases; this is due to the growth of the fetal bones in pregnancy. Multiple gestation pregnancies are likely to have even more elevated values. During pregnancy, the ALT, AST, and GGT values remain unchanged, as does the platelet count. During pregnancy, to deal with the significant increase in blood plasma levels, the kidneys are more active and the glomerular filtration rate increases by 50%. The kidneys increase in length and volume, and physiologic hydronephrosis occurs in up to 80% of women. Since the kidneys are more active, this decreases serum creatinine, urea, and uric acid levels. 91) (B) All hormonal drugs, whether natural or synthetic, are category X drugs in pregnancy. This includes estrogen, progesterone, testosterone, etc. Any drug also that blocks hormone synthesis or binding is also category X; this includes antithyroid drugs such as methimazole and propylthiouracil (PTU). Not all bisphosphonates are category X drugs. Raloxifene (Evista) is. However, alendronate (Fosamax) is category C, as is ibandronate. All live vaccines are contraindicated during pregnancy, but there are vaccines that can be given safely during pregnancy such as the inactivated influenza vaccine (non-live). Lithium a teratogen which is linked to cardiac defects in a fetus known as Ebstein’s anomalies and should not be taken. 92) (D) A woman’s pulse during pregnancy increases by about 15 to 20 beats per minute. 93) (C) In pregnancy, the preload increases because there is a much higher blood volume in pregnancy. The afterload decreases because there is decreased peripheral vascular resistance in pregnancy. 94) (C) Mammary souffle is a murmur heard over the breasts in pregnancy or during lactation (when a woman is lactating). It can occur in one or both breasts. When occurring in pregnancy, it occurs late in pregnancy, not early. 95) (D) Sudden, severe swelling of the face and hands could be indicative of preeclampsia. Mild edema of the lower extremities and the feet is normal in pregnancy due to the additional blood and fluid created during pregnancy. Edema is most noticeable during the third trimester. 96) (D) Asymptomatic bacteriuria should always be treated in pregnancy because women with asymptomatic bacteriuria are more likely to deliver premature or low birth weight infants and have an increased risk of developing pyelonephritis during pregnancy compared to women without bacteriuria. The evidence is so strong that the United States Preventive Services Task Force (USPSTF) recommends screening (as of July 2008) for asymptomatic bacteriuria with urine culture for pregnant women at 12 to 16 weeks’ gestation or their first prenatal visit, if later. So, the rule is, asymptomatic bacteriuria should always be treated in pregnancy. 97) (C) The kidneys increase in size during pregnancy. The ureters and renal pelvis become dilated. The glomerular filtration rate (GFR) increases due to the fact that a woman has increased blood volume during pregnancy. 98) (D) Lithium is a known teratogen and the woman should not take lithium during pregnancy due to the fact that is linked to cardiac defects in fetuses called Ebstein’s anomalies. 99) (A) Placenta previa is a condition in which the placenta is partially or completely blocking the lower part of the uterus. In other words, the placenta is covering the top of the cervix. It is a condition that can cause severe bleeding. Image: Placenta previa 100) (B) The most prominent symptom of placenta previa is it causes painless vaginal bleeding that can be light to severe. 101) (D) Placenta previa is diagnosed through ultrasound. Routine vaginal exams are avoided because doing them may cause further bleeding. 102) (C) The woman’s placenta previa will most likely resolve as the pregnancy progresses. 103) (C) Most women are routinely screened for gestational diabetes between 24 and 28 weeks of pregnancy. The test may be done earlier if the woman has high glucose levels in the urine during routine prenatal visits or is at high risk for diabetes. Women who have a low risk for diabetes may not have any testing done at all for gestational diabetes. 104) (B) A blood sugar of 132 mg/dL is normal after a 1-hour oral glucose tolerance test (OGTT). A normal result for the glucose screening test is a blood sugar that is equal to or less than 140 mg/dL 1 hour after drinking the glucose solution. 105) (D) If the blood sugar following the 1-hour oral glucose screening test is above 140 mg/dL, this is an elevated number. The practitioner should then have the patient undergo a 3-hour oral glucose tolerance test. 106) (C) The woman has a diagnosis of gestational diabetes. If fasting blood glucose before the woman drinks the 3-hour oral glucose tolerance test (OGTT) is greater than 95 mg/dL, or 1 hour after the test the blood glucose is greater than 180 mg/dL, or if 2 hours after the test the blood glucose is greater than 155 mg/dL, or if 3 hours after the test the blood glucose is greater than 140 mg/dL, all of these conditions are diagnostic of gestational diabetes. If only one of these values are elevated, the healthcare provider may just ask a patient to modify his or her diet and then repeat the test. If 2 or more of these values are elevated, the woman will be diagnosed with gestational diabetes. 107) (C) Human placental lactogen (hPL) is a hormone produced by the placenta, the organ that develops during pregnancy to help feed the growing baby. This hormone breaks down fats from the mother to provide fuel for the growing baby. It can lead to insulin resistance and the onset of gestational diabetes (due to this insulin resistance). 108) (C) Women who get gestational diabetes are at higher risk for type II diabetes. 109) (D) According to Bartholomew’s rule of fourths, the fetus would be at the mother’s xiphoid process 36 weeks into the pregnancy. At 12 weeks, the fetus would be at the symphysis pubis. At 16 weeks, the fetus would be halfway between the symphysis pubis and the umbilicus. At 20 weeks, the fetus would be at the umbilicus. At 36 weeks, the fetus would be at the xiphoid process. 110) (C) A molar pregnancy is also known as hydatidiform mole. A molar pregnancy occurs when tissue that normally becomes a fetus instead becomes an abnormal growth in the uterus. Even though it isn’t an embryo, this growth triggers symptoms of pregnancy, such as increased levels of human chorionic gonadotropin (hCG). 111) (C) The treatment for a molar pregnancy is removal of all of the growth from the uterus. This is normally done through a procedure called vacuum aspiration. 112) (B) A potential complication of a molar pregnancy is that the abnormal growth in the uterus becomes cancerous. Most abnormal growths are benign (noncancerous) but they can become cancerous. Rarely, a cancerous form of gestational trophoblastic disease known as choriocarcinoma develops and spreads to other organs. Choriocarcinoma is usually successfully treated with multiple cancer drugs. 113) (D) There are 2 types of molar pregnancies, a complete molar pregnancy and a partial molar pregnancy. In a complete molar pregnancy, there is no embryo or normal placental tissue. In a partial molar pregnancy, there is an abnormal embryo and possibly some normal placental tissue. The embryo begins to develop but is malformed and cannot survive. A molar pregnancy may seem like a normal pregnancy in the early stages, but most molar pregnancies present alarming symptoms that alerts a woman to the possibility that there is something wrong. These symptoms include dark brown to bright red vaginal bleeding during the first trimester, severe nausea and vomiting, possible vaginal passage of grape-like cysts, and rarely pelvic pain or pressure. Other signs include rapid uterine growth (the uterus is too large for the stage of pregnancy), hypertension, preeclampsia, ovarian cysts, anemia, and hyperthyroidism. 114) (B) The cause of a molar pregnancy is an abnormally fertilized egg. In a complete molar pregnancy, all of the fertilized egg’s chromosomes come from the father. Shortly after fertilization, the chromosomes from the mother’s egg are lost or inactivated and the father’s chromosomes are duplicated. The egg may have had an inactive nucleus or no nucleus. In a partial molar pregnancy, the mother’s chromosomes remain but the father provides 2 sets of chromosomes. As a result, the embryo has 69 chromosomes instead of the normal 46. This can happen when the father’s chromosomes are duplicated or if 2 sperm fertilize a single egg. Risk factors that cause a molar pregnancy include maternal age greater than 35 or younger than 20 and a previous molar pregnancy. 115) (B) After a molar pregnancy, it is recommended that a woman wait 6-12 months before trying to get pregnant again. During this 6-12 month-period, the woman’s practitioner will monitor her hCG levels to see that they are decreasing, to make sure there’s no remaining molar tissue. 116) (C) An ectopic pregnancy is a pregnancy that takes place outside of the uterus; for this reason, it is called an extrauterine pregnancy. It occurs when a woman’s ovum (egg), that has been fertilized, implants outside the uterus (gets stuck there). Symptoms include pelvic pain and abnormal vaginal bleeding. Normally, in ectopic pregnancies, the baby doesn’t survive in most cases. Ectopic pregnancies can also be fatal to the mother. 117) (A) The most common place for an ectopic pregnancy is the fallopian tubes. Over 95% of ectopic pregnancies take place in the fallopian tube. Within the fallopian tube, most (about 80%) occur in the ampullary (middle part of the fallopian tube). About 15% takes place in the isthmus (upper part of the fallopian tube near the uterus). About 5% are fimbrial (at the end of the tube). About 2% are interstitial (inside the part of the fallopian tube that crosses into the uterus. Outside of the fallopian tube, less than 1% are cervical and less than 1% are abdominal. Image: Places of ectopic pregnancies 118) (B) About 1-2% of all pregnancies are ectopic pregnancies; an ectopic pregnancy occurs about 1 in every 80 pregnancies. Most ectopic pregnancies take place in some part of the fallopian tube; these pregnancies are referred to as “tubal pregnancies”. In an ectopic pregnancy, there is no way to transplant the fertilized egg into the uterus, so ending the pregnancy is the only option. Most women who have an ectopic pregnancy have normal pregnancies and births in the future; this is true even if a fallopian tube has been removed. As long as a woman has one working fallopian tube, she can get pregnant. 119) (A) The use of a cervical cap is not a risk factor for an ectopic pregnancy. Risk factors for ectopic pregnancies include current use of an intrauterine device (IUD) (a form of a birth control), history of pelvic inflammatory disease (which can scar organs in the pelvis), STDs such as chlamydia and gonorrhea, congenital abnormalities of the fallopian tube, history of pelvic surgery, history of ectopic pregnancy, unsuccessful tubal ligation (surgical sterilization) or tubal ligation reversal, use of fertility drugs, and infertility treatments such as in vitro fertilization. 120) (C) Human chorionic gonadotropin (hCG) is a hormone produced by the placenta. 121) (B) The umbilical cord usually separates from the newborn by 1 week after birth. 122) (B) The woman has had 4 pregnancies, so she has a gravidity of 4 (G4). A live birth is considered a successful pregnancy. The woman gave birth to twins in her first pregnancy and has yet to have another live birth; therefore, she has a parity of 1. It does not matter that she gave birth to twins, triplets, or any other multiples. One pregnancy is always one live birth, regardless if it’s a multiple gestation birth. She then had 2 fetuses who died in utero before 20 weeks; thus, she had 2 abortions. Therefore, her obstetric history is G4P1A2. If she had had a fetus die in utero after 20 weeks, this would count as a stillbirth, which counts as parity, not an abortion. An abortion is death in utero before the age of 20 weeks, while a stillbirth is death in utero after 20 weeks or at delivery. 123) (C) In order to calculate the expected date of delivery (EDD), you can either add 9 months + 7 days to the current date or another way of doing it is by adding a year and subtracting 3 months and then adding 7 days. In the case of the first day of the last menstrual period being January 7, 2015, the expected date of delivery is October 14, 2015. 124) (D) Using Naegele’s rule to calculate a woman’s expected date of delivery, you add 9 months and 7 days (or add a year and subtract 3 months and add 7 days) to the first day of the last menstrual period that the woman had. Adding 9 months and 7 days to March 10, 2016 yields December 17, 2016. 125) (D) Meconium is the first feces of a newborn. Unlike later feces, meconium is composed of materials ingested during the time the infant spent in the uterus: intestinal epithelial cells, lanugo, mucus, amniotic fluid, bile, and water. Unlike later feces, meconium is viscous and sticky, normally a dark green color. Meconium should be completely passed by the end of the first few days after birth, with the stools progressing to a yellow color (digested milk). Though meconium is normally retained in the infant’s bowels until after birth, sometimes it is expelled into the amniotic fluid in utero. The infant can breathe in this meconium-stained fluid, which can cause meconium aspiration syndrome. Post-term, not preterm, babies are most at risk for meconium aspiration syndrome, because they spend a longer time in the uterus during pregnancy. 126) (C) A healthy woman (normal weight) typically gains 15-25 lbs during the course of a pregnancy. 127) (C) Mittelschmerz is pain associated with ovulation. It is usually one-sided, lower abdominal pain associated with normal ovulation. It occurs midway through a menstrual cycle— about 14 days before a woman’s next menstrual period. In most cases, mittelschmerz does not require medical attention. For minor pain, OTC pain relievers and home remedies are often effective (source: mayoclinic.org). 128) (B) A pregnant woman should wear her seatbelt with the lap belt below the uterine fundus. 129) (D) Smoking during pregnancy increases the fetus’s risk of intrauterine growth restriction (IUGR). 130) (A) The vast majority of victims from Shaken Baby Syndrome are less than 1 year old. The average age of victims is between the age of 3 and 8 months (Rudd & Kocisko, 2014). 131) (B) Research shows that teenage fathers are most likely to cause shaken baby syndrome. Risk factors for shaken baby syndrome include unrealistic expectations of babies, young or single parenthood, stress, domestic violence, alcohol or substance abuse, unstable family situations, depression, and a history of mistreatment as a child. Men are more likely to inflict shaken baby syndrome than women (source: mayoclinic.org). 132) (A) Shaken baby syndrome (SBS), also known as abusive head trauma, is a diagnosis that may include a combination of findings including broken bones, skull fractures, brain bleeding, retinal hemorrhages, and detached retina. SBS occurs when a baby is shaken repeatedly, often by a frustrated caretaker in an effort to quiet an inconsolable baby. A baby’s head is disproportionately large and the blood vessels are fragile, which makes the brain and eyes more susceptible to bleeding from a shaking injury. Most children who are victims of SBS are under 1 year of age, with many of them being under six months of age. Injuries from SBS can lead to permanent visual and developmental disabilities, or even death (source: aapos.org). 133) (C) Shaken baby syndrome- also known as abuse head trauma, shaken impact syndrome, inflicted head injury, or whiplash shake syndrome- is a serious brain injury resulting from forcefully shaking an infant or toddler. Shaken baby syndrome is a form of child abuse that can result in permanent brain damage or death. Shaken baby syndrome occurs when a parent or caregiver severely shakes a baby or toddler due to frustration or anger- often because the child won’t stop crying. Shaken baby syndrome isn’t usually caused by rough play with a child or minor falls. Approximately 25% of victims of shaken baby syndrome die. Shaken baby syndrome is the leading cause of physical child abuse in the US (source: mayoclinic.org & dontshake.org). 134) (D) A woman can get pregnant very soon after removing an IUD, cervical cap, or diaphragm. Because Depo Provera is long lasting, it can take a long time to get pregnant after getting the last shot—anywhere from 6-10 months. So, Depo-Provera is not a good birth control method if a woman is thinking of getting pregnant soon. 135) (B) Nitrofurantoin is an antibiotic that can be used in pregnancy to treat UTIs. 136) (C) Nitrofurantoin is safe to use up until the end of the 37th week of pregnancy. Nitrofurantoin is contraindicated in pregnant patients at term (38 to 42 weeks' gestation), during labor and delivery, or when the onset of labor is imminent because of the possibility of hemolytic anemia due to immature erythrocyte enzyme system of the child (source: drugs.com). 137) (B) Amoxicillin is least likely to be prescribed because of the high resistance bacteria has to it. 138) (A) When breastfeeding, the baby should have the entire nipple and areola inside of his or her mouth. The tip of the infant’s nose, cheeks, and chin should be touching the breast. The breast should be aligned with the infant’s nose. Breastfeeding should be on demand throughout the day and night. Usually it’s every 2-3 hours, so it’s normally given 8-12 times in a 24-hour period. Breastfeeding is a quiet event. Swallowing noises are normal, but not clicking noises. Clicking noises indicate improper latching of the baby on the breast. 139) (A) If a woman has sore nipples, she should start breastfeeding on the less painful breast first. She should continue to breastfeed because cessation of breastfeeding can cause breast engorgement. 140) (C) Mastitis is breast inflammation usually caused by infection; it can be a painful condition. It can happen to a woman at any time, although mastitis is most common during the first 6 months of breastfeeding. Mastitis most often happens when bacteria enter the breast through the nipple. This can happen when a nursing mother has a cracked or sore nipple. If a woman has mastitis, she can continue to nurse her baby. In fact, breastfeeding usually helps to clear up the infection, and nursing will not harm the baby. Going for long stretches between nursing or failing to empty the breast completely may also contribute to mastitis (because it causes stasis which can make it easier for bacteria to grow). Using different breastfeeding techniques and making sure the baby is latched on properly when nursing will help with emptying the breast and avoiding cracked nipples (source: webmd.com). 141) (C) The most common causative agent of mastitis is staphylococcus aureus. 142) (D) Risk factors for mastitis include poor latching of the infant on the breast (this can cause a break of skin on the breast which can be an entry point for bacteria), infrequent breastfeeding (causes stasis which can let bacteria grow in the breast), and previous history of mastitis. Taking hot showers is not a risk factor; in fact, it is used as a remedy for mastitis, since it helps to let milk flow out to the nipple and out of the breast. 143) (C) The American Academy of Pediatrics (AAP) recommends that an infant be breastfed for the first full year of life. 144) (D) Breastfeeding should be given on demand. 145) (A) Health professionals agree that human milk provides the most complete form of nutrition for infants. However, there are rare exceptions when human milk is not recommended. Breastfeeding is not advisable if an infant is diagnosed with galactosemia (a rare genetic metabolic disorder that affects how the body processes a simple sugar called galactose), the mother has HIV, is taking antiretroviral medications, has untreated, active tuberculosis, is infected with human T-cell lymphotropic virus type I or type II, is using or is dependent upon an illicit drug, is taking prescribed cancer chemotherapy agents (such as antimetabolites that interfere with DNA replication and cell division), or is undergoing radiation therapies (source: cdc.gov). 146) (D) Breastfeeding burns extra calories, so it can help a woman lose pregnancy weight faster. It releases the hormone oxytocin, which helps the uterus return to its pre-pregnancy size and may reduce uterine bleeding after birth. Breastfeeding also lowers a woman’s risk of breast and ovarian cancer. While breastfeeding can prevent postpartum bleeding due to the fact that it causes the uterus’s size to decrease back to pre-pregnancy level (prevents uterine atony which is a risk for bleeding), there is no direct associated link with it helping a woman’s ability to form blood clots. Another benefit is that since a woman doesn’t have to buy formula, it saves money and time (shopping) (source: webmd.com). 147) (B) Drugs that are classified by the FDA as category X drugs are found to be teratogenic to a fetus and should never be taken during pregnancy. These drugs include finasteride, isotretinoin, warfarin, misoprostol, androgenic hormones (birth control pills, HRT, testosterone), thalidomide, DES, methimazole, and others. Live virus vaccines (MMR, varicella, rotavirus, FluMist) should also not be given in pregnancy. 148) (B) The head circumference is about 1 to 2 cm more than the chest circumference in a newborn. 149) (D) Crying or increased intracranial pressure may cause bulging fontanels. Dehydration causes sunken fontanels. 150) (A) A sunken (or flattened) fontanelle can be an indicator of dehydration. Bulging fontanelles can be an indicator of fluid overload. 151) (B) For a newborn less than 24 hours old, a bilirubin level of 8mg/dL represents a normal level. An elevated level that may require treatment would be one above 10mg/dL. 152) (C) Preterm infants are those born before 37 weeks of pregnancy. An average full-term baby is born between 38 and 42 weeks of pregnancy. Post-term infants are those born after 42 weeks of pregnancy. Chapter 14- Pediatrics 1) Why should a child avoid milk for the first year of life? A) It can cause gastrointestinal (GI) bleeding B) It is more likely to cause lactose intolerance later in life C) It is likely to cause food allergies D) It weakens the child’s immune system 2) In a normal healthy person, the amino acid phenylalanine is converted into: A) B) C) D) Blood urea nitrogen Proteins Tyrosine Ammonia 3) What is the treatment for phenylketonuria (PKU)? A) A phenylalanine-free diet B) A diet with restricted amounts of phenylalanine C) Injections of the enzyme phenylalanine hydroxylase at each meal D) Surgical repair of the parietal cells in the stomach 4) What can phenylketonuria (PKU) lead to if it is left untreated? A) B) C) D) Severe mental retardation Kidney failure Liver failure Ulcerated intestines 5) When should newborns be tested for phenylketonuria? A) Immediately after birth B) 12 hours after birth C) 48 hours after birth D) 2 weeks after birth 6) When is it recommended to start solid food in an infant? A) B) C) D) At 3-4 months At 4-6 months At 6-8 months At 8-10 months 7) What is the most common renal malignancy in children? A) B) C) D) Rhabdoid Tumor of the Kidney Congenital Mesoblastic Nephroma Multilocular Cystic Nephroma Nephroblastoma 8) Why should the abdomen of a child suspected of having Wilm’s tumor (nephroblastoma) not be palpated rigorously? A) It can cause the tumor to grow B) It can cause the tumor to rupture and spread its seeds throughout the body, causing metastasis of the cancer C) It causes tremendous pain and discomfort in the child D) It causes the kidney to be compressed, halting its blood supply 9) All of the following are symptoms of Kawasaki disease except for: A) B) C) D) Vasculitis Peeling of the skin on the hands Fever Ecchymoses 10) What treatment is used for Kawasaki disease? A) B) C) D) High-dose aspirin and IVIG High-dose acetaminophen and IVIG High-dose corticosteroids and IVIG High-dose penicillin and IVIG 11) By 6 months of age, the infant’s weight should be: A) B) C) D) The same as the birth weight Double the birth weight Triple the birth weight Quadruple the birth weight 12) By 12 months of age, the infant’s weight should be: A) B) C) D) The same as the birth weight Double the birth weight Triple the birth weight Quadruple the birth weight 13) What is the only vaccine given at birth? A) B) C) D) IPV Hepatitis B Hepatitis A MMR 14) How long does it take a child to produce antibodies following an influenza vaccination? A) B) C) D) 2-3 days 1 week 2 weeks 1 month 15) Which of the following is true about the HPV vaccine? A) It should only be given to girls B) It can be first given at 11 or 12 years of age C) It is given as a single shot D) The HPV vaccine protects against pancreatic cancer 16) What can hyperbilirubinemia cause in infants? A) B) C) D) Liver damage Kidney damage Kernicterus Carbuncles 17) Ortolani and Barlow maneuvers are tests used to check for: A) Acute appendicitis B) ACL tear C) Meniscus tear D) Developmental dysplasia of the hip (DDH) 18) All of the following are common symptoms of kernicterus in an infant except for: A) B) C) D) Seizures Lethargy Renal failure Severe mental retardation 19) What is a noninvasive way to check a newborn’s bilirubin? A) B) C) D) Serum bilirubin level Using a bilirubinometer Using a wood’s lamp Using a thermometer 20) All of the following are commonly seen in autism except for: A) Poor eye contact B) Talkativeness C) Lack of social interaction D) Repetitive behaviors 21) Which of the following statements is false regarding autism? A) Autism occurs in every racial and ethnic group, across all socioeconomic levels B) Girls are significantly more likely to develop autism than boys C) Children with Fragile X syndrome have an increased risk for autism D) People with ASD have a higher than average risk of having epilepsy 22) Which of the following statements is true regarding autism? A) Autism can be easily diagnosed at birth B) Autism is very apparent by 1 year of age C) Autism is hard to diagnose before 18 months of age D) Autism cannot be diagnosed before the age of three 23) All of the following are common features of fragile X syndrome except for: A) B) C) D) Long face with a prominent forehead Intellectual disability Autism Hypoactive behavior 24) Which of the following is necessary to definitively diagnose Fragile X syndrome? A) B) C) D) Physical examination Neurological examination Blood test Hair analysis 25) Which of the following is false regarding hand-foot-mouth disease? A) It is an acute bacterial illness B) It is most contagious during the first week of illness C) It is spread through direct contact with nasal discharge, saliva, blister fluid, or stool D) It is self-limiting 26) What is the most common causative agent of hand-foot-mouth disease? A) B) C) D) E. coli Coxsackievirus A16 Human papillomavirus Moraxella catarrhalis 27) Common symptoms of hand-foot-mouth disease include all of the following except for: A) B) C) D) Acute onset of fever Diarrhea Small blister formations Sore throat 28) What is the number one cause of death in adolescents in the United States? A) B) C) D) Homicide Suicide Accidents/injuries Cancer 29) Hemolytic uremic syndrome is a condition characterized by which of the following? A) Hemolytic anemia, leukopenia, and thrombocytopenia B) Hemolytic anemia, thrombocytopenia, and liver failure C) Hemolytic anemia, thrombocytopenia, and kidney failure D) Hemolytic anemia, leukopenia, and severe brain damage 30) A kid with hemolytic uremic syndrome is having a hemolytic episode. What would be expected? A) Reticulocytosis B) Reticulocytes will be unchanged C) Reticulocytopenia D) Reticulocytes will be unmeasurable 31) What is the treatment for hemolytic uremic syndrome? A) B) C) D) Antibiotics Viral drugs Blood transfusions and dialysis Sodium bicarbonate 32) What is the most likely way that a person contracts hemolytic uremic syndrome? A) The person went out to a restaurant and ate a raw beef dish B) The person had unprotected sex C) The person obtained a tattoo at a tattoo parlor D) The person shared toothbrushes with roommates 33) Bronchiolitis is: A) Infection and inflammation of the alveoli B) Infection and inflammation of the bronchus C) Infection and inflammation of the bronchioles D) Infection and inflammation of the trachea 34) Bronchiolitis is caused the vast majority of the times by: A) B) C) D) A virus Bacteria A fungus A parasite 35) What is the peak time of the year that young children and infants get bronchiolitis? A) Spring B) Summer C) Fall D) Winter 36) How is bronchiolitis most often diagnosed? A) B) C) D) Through blood tests Through a nose swab Through X-ray Through ultrasound 37) All of the following are common symptoms of bronchiolitis except: A) B) C) D) Runny nose A cough Sleep apnea Wheezing 38) Which of the following statements is false regarding bronchiolitis? A) Most cases of bronchiolitis require hospitalization B) Bronchiolitis occurs most often during the first 2 years of life, especially ages 3 to 6 months C) Bronchiolitis typically lasts for about 1-2 weeks D) Bronchiolitis is more common in children who have not been breastfed 39) Which of the following is an effective treatment for bronchiolitis? A) B) C) D) Antibiotics Bronchodilators Chest physiotherapy Humidified air 40) Which drug is used prophylactically for respiratory syncytial virus (RSV)? A) B) C) D) Palivizumab Adalimumab Infliximab Golimumab 41) What is the difference between anorexia and anorexia nervosa? A) Anorexia is a lack of lack of appetite for food, while anorexia nervosa is an eating disorder characterized by self-starvation and excessive weight loss B) Anorexia nervosa is a lack of appetite for food, while anorexia is an eating disorder characterized by self-starvation and excessive weight loss C) Anorexia is more a severe form of anorexia nervosa D) Anorexia is a less severe form of anorexia nervosa 42) An adolescent with adolescent idiopathic scoliosis is determined to have a spinal curvature of about 30 degrees. What is the usual treatment for this degree of curvature? A) The practitioner would observe and monitor the curvature B) Bracing C) Surgical correction such as with Harrington rods used on the spine D) Spinal fusion 43) What type of infection is molluscum contagiosum? A) B) C) D) A viral infection of the skin A viral infection of the mouth A bacterial infection of the skin A bacterial infection of the mouth 44) Molluscum contagiosum is characterized by: A) B) C) D) Yellow papules Boils Black, non-raised, painless lesions Round, firm, painless bumps 45) Which is true regarding molluscum contagiosum? A) The bumps that appear with molluscum contagiosum only go away with surgical intervention B) The bumps that appear with molluscum contagiosum only go away with medical intervention C) The bumps that appear with molluscum contagiosum usually go away on their own D) The bumps that appear with molluscum contagiosum never go away 46) Molluscum contagiosum normally resolves within: A) B) C) D) A few days 2-3 weeks 6-12 months It doesn’t resolve 47) Which of the following statements is false regarding molluscum contagiosum? A) Molluscum contagiosum can appear anywhere on the body B) Molluscum contagiosum is a precancerous skin condition C) Immunocompromised individuals are at higher risk for obtaining molluscum contagiosum D) Molluscum contagiosum is contagious and can spread from direct person-to-person contact and through contaminated fomites 48) People with molluscum contagiosum should be careful: A) To apply antifungal cream to the skin each night to decrease the severity of the condition B) To take griseofulvin each night C) Not to scratch or pick at molluscum lesions D) When shaving areas of the skin with lesions 49) The Tanner stages describe stages of: A) B) C) D) Intellectual development Social maturation Pubertal maturation Psychological development 50) At which stage of the Tanner scale do the breasts begin to bud and the areola start to develop? A) B) C) D) Stage I Stage II Stage III Stage IV 51) During which Tanner stage does the nipple and areola separate from the breast, forming a secondary mound? A) B) C) D) Stage II Stage III Stage IV Stage V 52) What is stage of the Tanner scale that represents full, mature, adult breasts? A) B) C) D) Stage II Stage III Stage IV Stage V 53) In which Tanner stage do the scrotum and testes begin to enlarge? A) B) C) D) Stage I Stage II Stage III Stage IV 54) During which Tanner stage does the penis begin to enlarge? A) B) C) D) Stage II Stage III Stage IV Stage V 55) During which Tanner stage is there is a distinct darkening of the scrotum? A) B) C) D) Stage II Stage III Stage IV Stage V 56) When does the stepping reflex usually disappear by? A) B) C) D) 1-2 weeks 1-2 months 3-4 months 6-8 months 57) A nurse practitioner checks for the rooting reflex in a newborn. She does this by: A) Standing the newborn up and suddenly making him drop B) Standing the newborn up and making his feet touch the surface of the floor C) Stroking the corner of the newborn’s mouth with her finger D) Making a loud noise to startle the newborn 58) When does the rooting reflex disappear? A) B) C) D) 1-2 months 3-4 months 6-8 months 9-12 months 59) A practitioner is testing an infant’s blinking reflex. She does this by placing a light puff of air over each of the infant’s eyes. What is a normal response? A) B) C) D) The child’s pupils will constrict The child’s pupils will dilate The child will keep his eyes open The child will close his eyes 60) A practitioner places a 5-month-old baby supine on a bed with the head turned to one side. Which of the following reflexes is the practitioner checking? A) B) C) D) Rooting reflex Moro reflex Tonic neck reflex Babinski’s sign 61) A practitioner has a baby in the standing position and then suddenly drops the baby to a lower position. Which reflex is the practitioner testing? A) B) C) D) Rooting reflex Tonic neck reflex Moro reflex Stepping response 62) Babinski’s reflex is normal in children up to: A) B) C) D) 3 months 6 months 1 year 2 years 63) What is a normal (healthy) response to the anal wink reflex test? A) Contraction of the external anal sphincter B) Dilation of the external anal sphincter C) The baby crying D) The baby stretching out both of his legs 64) At what age should a child’s reflexes be the same as like adults? A) B) C) D) 2 years 3 years 5 years 8 years 65) A child should be able to sit unsupported by: A) B) C) D) 4-5 months 7-8 months 9-10 months 11-12 months 66) What age does an infant start babbling? A) B) C) D) 3 months 6 months 9 months 11 months 67) By what age should a child be able to hold a crayon and mark on paper? A) B) C) D) 4-6 months 7-8 months 1 year 2 years 68) At what age does the child begin using the pincer grasp? A) B) C) D) 4-5 months 7-8 months 10-11 months 2 years 69) By what age can a child roll from his back to his stomach and from his stomach to his back? A) B) C) D) 3 months 6 months 8 months 10 months 70) At what should a child be able to draw circles and squares? A) B) C) D) 2 years 3 years 4 years 5 years 71) By what age should a child be able to dress him or herself? A) B) C) D) 4 years 5 years 6 years 7 years 72) At what age does a child begin walking? A) B) C) D) 8 months 12 months 15 months 18 months 73) What age can children normally ride a tricycle by? A) B) C) D) 2 years 3 years 4 years 5 years 74) At about what age can most children ride a bicycle? A) B) C) D) 3 years old 6 years old 8 years old 10 years old 75) At what age does a child begin thinking abstractly? A) B) C) D) 4 years old 7 years old 11 years old 13 years old 76) To examine the ear canal of an infant, the auricle should be pulled: A) B) C) D) Backward and frontward Frontward and upward Backward and downward Frontward and downward 77) It is normal for infants to have periods of apnea lasting up to A) B) C) D) 5 seconds 10 seconds 15 seconds 30 seconds 78) What age can ibuprofen be given to a child? A) B) C) D) 3 months 6 months 1 year 2 years 79) Which of the following statements is false regarding intoeing? A) Intoeing means that the feet turn inward instead of pointing straight ahead when a child walks B) Intoeing is commonly referred as being “pigeon-toed” C) Intoeing will almost always correct itself without any type of treatment D) Intoeing increases the risk for a child obtaining arthritis 80) Which group accounts for the majority of perpetrators in child abuse cases? A) B) C) D) The parents Close relatives Daycare workers School teachers 81) Which of the following is not a risk factor for child abuse? A) B) C) D) Lack of extended family support Very low socioeconomic status Two-parent households Drug abuse 82) Which of the following groups of kids are most at risk for child abuse? A) Children under the age of 3 B) Children who are between the ages of 4 and 5 C) Children who are between the ages of 8-10 D) Adolescents between the ages of 12 and 15 83) Which of the following conditions would least likely be an indicator of child physical abuse? A) Various fractures in various stages of healing B) Bruises on the hands C) Femur fracture in a non-ambulating infant D) Bite marks 84) Which of the following is true about healthcare providers and abuse? A) Healthcare providers aren’t mandatory reporters, so it isn’t necessary for them to report suspected abuse B) Healthcare providers are mandatory reporters of abuse, so they are obligated to report abuse to the authorities or a child abuse hotline C) Healthcare providers should confront suspected abusers directly when there is suspicion of abuse and interrogate D) Healthcare providers are only required to report cases of suspected physical abuse 85) Which of the following signs is least likely a sign of sexual abuse? A) A child acting out in sexually inappropriate ways B) A child with complaints of pain in the genital area C) A girl with complaints of vaginal discharge or bleeding D) A girl with complaints of malodorous urine 86) Which of the following statements is false regarding infant colic? A) Colic is a term that applies to any healthy, well-fed infant who cries more than 3 hours a day, more than 3 days a week, for more than 3 weeks B) Colic is likely to start around age 2 weeks if the infant is full-term or later if premature C) Kids who are colic babies are more likely to have autism than kids who are not D) Colic almost always goes away on its own by 3 or 4 months 87) Infant colic is essentially: A) B) C) D) Unexplained vomiting Unexplained crying Crying due to excess pain Unexplained coughing 88) Which of the following statements is false regarding jaundice? A) The most common type of jaundice is physiologic jaundice which affects up to 60% of full term babies in the first week of life B) Physiologic jaundice is normal C) Jaundice is caused by elevated bilirubin levels D) Jaundice normally resolves within 5-6 months after birth 89) Which of the following statements is false regarding spermarche? A) Spermarche refers to the beginning of development of sperm in boys’ testicles at puberty B) Spermarche is one of the first events in the life of a male leading to sexual maturity C) Spermarche occurs at the time when the boy develops secondary sexual characteristics D) Spermarche occurs between the ages of 8 and 10 years of age 90) What is the number one reason for hospitalization among children? A) B) C) D) Common cold RSV Asthma Injuries 91) What is the leading cause of infant mortality in the United States? A) B) C) D) Unintentional injury Sudden infant death syndrome Birth defects Prematurity and low birth weight 92) Adolescent children range in age from: A) B) C) D) 6-18 6-12 10-18 13-18 93) What age can sunscreen be applied on a child? A) B) C) D) 3 months 6 months 9 months 12 months 94) During phototherapy for hyperbilirubinemia, what parts of the body should be covered? A) B) C) D) Arms and legs Arms and chest Eyes and mouth Eyes and genitalia 95) What is considered normal urine output for infants? A) B) C) D) 1-3 wet diapers a day 3-6 wet diapers a day 6-10 wet diapers a day 12-15 wet diapers a day 96) Infants who are fed solid food too early are at an increased risk for developing: A) B) C) D) Diabetes Osteoporosis Food allergies Erythroblastosis fetalis 97) When is a child’s immune system fully developed? A) B) C) D) At birth 3 months 6 months 1 year 98) According to the American Dental Association, a child should have his or her first dental visit by: A) B) C) D) 6 months 1 year 18 months 2 years 99) Which of the following statements is false regarding an infant’s teeth? A) Teething is the eruption of the teeth through the gums B) Teeth erupt at 4 to 10 months of age, usually around 6 months C) Usually the first 2 teeth to erupt are the upper center teeth D) Natal teeth can be present at birth and can interfere with breastfeeding 100) None of the following foods should be given to a child under 1 year of age except for: A) B) C) D) Cow’s milk Honey Corn syrup Bacon 101) What is the primary reason for low birth weight? A) B) C) D) Prematurity of birth Inadequate maternal nutrition Low maternal weight A child being in the breech position 102) According to the American Academy of Pediatrics (AAP), how should an infant be seated in a car? A) In the front seat in a forward-facing seat B) In the front seat in a rear-facing seat C) In the back seat in a front-facing seat D) In the back seat in a rear-facing seat 103) All of the following are signs of respiratory distress in children except for: A) B) C) D) Nose breathing Nasal flaring Retractions Tripod positioning 104) Enuresis is: A) B) C) D) Getting up at night to urinate Constipation Urinary incontinence Fecal incontinence 105) Which of the following statements is false regarding sudden infant death syndrome (SIDS)? A) SIDS is the sudden, unexpected death of a child under 1 year of age, usually occurring while the child is awake B) SIDs can occur at any time from 1 week old to 1 year old, but the peak incidence of SIDS is 2 to 4 months of age C) The autopsy of a child who has died from SIDS reveals pulmonary edema D) Placing an infant to sleep on his or her back is an important measure to prevent SIDS 106) Which is true regarding blood pressure readings in children? A) Normal systolic blood pressure in infants is between 70 and 90 mmHg B) Adolescents reach adult levels in term of blood pressure readings C) Routine monitoring of blood pressure should begin at age 5 D) Diagnosis of hypertension cannot be made from a single reading 107) What age do most babies start crawling? A) B) C) D) 4 months 6 months 8 months 10 months 108) When should a parent take his child to his first thorough eye examination? A) B) C) D) 3 months 6 months 12 months 2 years 109) Which of the following statements is true regarding the vision of newborns? A) Babies are born with 20/40 vision B) From birth to 4 months, babies’ primary focus is on objects 16 to 20 inches from their face or the distance to the parent’s face C) Any eye crossing occurring at any time during infancy is abnormal D) Babies should begin to follow moving objects with their eyes and reach for things at around 3 months of age 110) Aspirin should not be used in children under the age of 16 years old due to risk of developing: A) B) C) D) Pneumonia Reye’s syndrome Meningitis Internal bleeding 111) What type of disease is Tay-Sachs? A) Autosomal recessive disorder B) Autosomal dominant disorder C) Acquired disorder through malnutrition D) Acquired disorder through allergies 112) Which enzyme do children with Tay-Sachs disease lack? A) B) C) D) Alpha glucosidase Lipase Amylase Hex A 113) Tay-Sachs is a disease that makes a child unable to break down: A) B) C) D) Proteins Lipids Carbohydrates Bilirubin 114) Tay-Sachs leads to all of the following except for: A) Deafness B) Blindness C) Epidermal necrolysis D) Hypotonia 115) Most children with Tay-Sachs disease die: A) B) C) D) Shortly after birth By 2 years old By 5 years old By 17 years old 116) Which demographic population is most at risk for Tay-Sachs disease? A) B) C) D) People of African descent Eastern European Jews Eastern Asian descent Native American descent 117) Patau syndrome is also referred to as: A) B) C) D) Trisomy 13 Trisomy 18 Trisomy 21 XXY syndrome 118) Common symptoms of Patau syndrome include all of the following except for: A) B) C) D) Multiple organ defects Hydrocephalus Severe intellectual disability Cleft lip and palate 119) Most people born with Patau syndrome die within: A) The first year of life B) The first five years of life C) By age 10 D) By age 20 120) Edward’s syndrome is also referred to as: A) B) C) D) Trisomy 13 Trisomy 18 Trisomy 21 XXY syndrome 121) Common symptoms of Edward’s syndrome include all of the following except for: A) B) C) D) Multiple organ defects Severe learning disability Bone abnormalities Macrocephaly 122) Most people born with Edward’s syndrome die within: A) B) C) D) The first year of life The first five years of life By age 10 By age 20 123) A mother in her past pregnancy gave birth to a child with Edwards syndrome who died after 3 days of life. What should the practitioner tell this mother about a future pregnancy? A) The chances of you having another child with Edward syndrome is 0% B) The chance of you having another child with Edwards syndrome is no greater than 1% C) The chance of you having another child with Edwards syndrome is about 50% D) The chance of you having another child with Edwards syndrome is 100% 124) Which is the most severe type of trisomy? A) Trisomy 13 B) Trisomy 18 C) Trisomy 21 D) They’re all equally severe 125) Down Syndrome may include all of the following symptoms except for: A) B) C) D) High-set ears Some degree of mental retardation Flattened facial features A short neck 126) Children with Down Syndrome with atlantoaxial instability: A) Need wheelchairs to get around B) Are restricted from any type of contact sports C) Are restricted from oral intake D) Are limited in talking ability 127) All of the following are common symptoms of Marfan syndrome except for: A) B) C) D) Tall stature Bulging or indented chest Abnormally long fingers Dystonia 128) Which is of the following statements is false regarding separation anxiety? A) Separation anxiety is distress caused by a fear of abandonment B) Separation anxiety can begin as early as 8 months of age and end as late as 7 years of age C) Separation anxiety peaks between 10 and 18 months D) Separation anxiety is a normal stage of development 129) The Oedipus complex refers to: A) A child’s desire for sexual involvement with the opposite sex parent B) A child’s first spoken words C) A child’s inclination to touch and play with his/her own feces D) A child’s first steps walking 130) What is the most common type of convulsions in infants and young children? A) B) C) D) Tonic-clonic seizures Myoclonic seizures Clonic seizures Febrile seizures 131) Which type of seizure, most commonly seen in children, is characterized by a blank stare that normally lasts between 10 and 15 seconds? A) B) C) D) Absence seizure Tonic seizure Clonic seizure Status epilepticus Pediatrics answers 1) (A) A child should avoid milk for the first year of life because drinking milk can cause gastrointestinal bleeding. 2) (C) In a normal, healthy person, the amino acid phenylalanine is converted into tyrosine. 3) (A) The treatment for phenylketonuria is a phenylalanine-free diet. Phenylalanine needs to be avoided, even in small amounts. 4) (A) Phenylketonuria, if left untreated, mostly has neurological repercussions and can cause severe mental retardation. 5) (C) A newborn should be tested for phenylketonuria approximately 48 hours after birth. This is because the child needs to eat first and adequate time needs to be given to see how his or her body reacts to phenylalanine. 48 hours is the recommended period of waiting time. Screening for it earlier than this can cause missed cases of phenylketonuria. 6) (B) It is recommended that an infant start solid food at 4-6 months of age. 7) (D) The most common renal malignancy in children is a nephroblastoma, which is also called Wilm’s tumor. It is a fast-growing tumor on the kidney. 8) (B) The abdomen of a child suspected of having Wilm’s tumor (nephroblastoma) should not be palpated rigorously because it can cause the tumor to rupture and spread throughout the body, causing metastasis of the cancer. 9) (D) Symptoms of Kawasaki disease include high fever that lasts for at least 5 days, swollen lymph nodes, conjunctivitis, a rash on the main part of the body (trunk) and in the genital area, red, dry, cracked lips, a strawberry tongue, and irritability. Ecchymoses on the body is not associated with Kawasaki disease. 10) (A) The treatment for Kawasaki disease is high-dose salicylate therapy (aspirin) and IVIG. 11) (B) By 6 months of age, an infant’s weight should be double the birth weight. 12) (C) By 12 months of age, an infant’s weight should be triple the birth weight. 13) (B) Hepatitis B is the only vaccine given at birth. 14) (C) It takes 2 weeks for a child to produce antibodies for influenza after vaccination. 15) (B) The HPV vaccine should be given to girls and boys. Both can get infected by the human papillomavirus (HPV). HPV is a very common virus. HPV infection can cause cervical, vaginal, and vulvar cancers in women; penile cancer in men; and anal cancer, cancer of the back of the throat (oropharynx), and genital warts in both men and women. The HPV vaccine is recommended for preteen boys and girls at age 11 or 12, so they are protected before ever being exposed to the virus. The HPV vaccine can be given up to age 21 in males and up to age 26 in females. All kids who are 11 or 12 years old should get 2 shots of HPV vaccine 6-12 months apart. Adolescents who receive their 2 shots less than 5 months apart will require a third dose of HPV vaccine. 16) (C) Hyperbilirubinemia can cause kernicterus, a condition in which the child suffers neurological damage (due to the excess bilirubin) that can lead to mental retardation. 17) (D) Ortolani and Barlow maneuvers are tests used to check for developmental dysplasia of the hip. 18) (C) Symptoms of kernicterus include lethargy, poor feeding habits, fever, and vomiting. Affected infants may also experience the absence of certain reflexes and mild to severe muscle spasms. A severe buildup of bilirubin can cause brain damage, including severe mental retardation. Kernicterus can be a life-threatening condition (source: rarediseases.org). 19) (B) A noninvasive way of checking a newborn’s bilirubin level is through the use of a bilirubinometer. Checking the bilirubin through the serum level would be an invasive test. Wood’s lamp is used to check for abnormalities of the skin, not for bilirubin levels. A thermometer checks a person’s temperature. 20) (B) Autism spectrum disorder (ASD) refers to a group of complex neurodevelopment disorders characterized by repetitive and characteristic patterns of behavior and difficulties with social communication and interaction. The symptoms are present from early childhood and affect daily functioning. Even as infants, children with autism may seem different, especially when compared to children their own age. They may become overly focused on certain objects, rarely make eye contact, and fail to engage in typical babbling with their parents. 21) (B) Autism occurs in every racial and ethnic group, across all socioeconomic levels. Boys are significantly more likely to develop autism than girls. Children with certain genetic disorders such as Fragile X syndrome have an increased risk for autism. People with ASD also have a higher than average risk of having epilepsy. Children whose language skills regress early in life — before age 3 — appear to have a greater risk of developing epilepsy or seizure-like brain activity. About 20 to 30 percent of children with ASD develop epilepsy by the time they reach adulthood. Additionally, people with both ASD and intellectual disability (such as Fragile X syndrome) have the greatest risk of developing a seizure disorder. 22) (C) Diagnosing autism spectrum disorder (ASD) can be difficult, since there is no medical test, like a blood test, that can be used for diagnosis. Doctors look at the child’s behavior and development to make a diagnosis. Autism is hard to diagnose before 18 months of age. By age 2, a diagnosis by an experienced professional can be considered very reliable. However, many children do not receive a final diagnosis until much older (source: cdc.gov). 23) (D) Fragile X syndrome (FXS) is a genetic disorder that includes mild to moderate intellectual disability, as well as physical and behavioral abnormalities. Physical abnormalities include an elongated and narrow face, large ears, flexible fingers, and large testicles. About a third of people with FXS have features of autism such as withdrawn social interaction. Hyperactivity, not hypoactivity, is commonly seen with Fragile X syndrome. Image: Boy with Fragile X syndrome Credit: Photograph by Peter Saxon, distributed under the Creative Commons Attribution-Share Alike 4.0 International license 24) (C) A blood test is used to definitively diagnose a person with having Fragile X syndrome. Fragile X syndrome is a genetic disorder which occurs as a result of a mutation of the fragile X mental retardation 1 (FMR1) gene on the X chromosome. The X chromosome is one of 2 types of sex chromosomes. Women have 2 X chromosomes, while men have 1 X chromosome. Analysis of the chromosomes, through a blood sample, can determine Fragile X syndrome. 25) (A) Hand-foot-mouth disease is an acute viral illness. It is spread through direct contact with nasal discharge, saliva, blister fluid or stool. It is most contagious during the first week of illness. It is a self-limiting illness. 26) (B) The most common causative agent of hand-foot-mouth disease is coxsackievirus A16 (source: mayoclinic.org). 27) (B) Hand-foot-mouth disease typically is not associated with diarrhea. Hand-foot-mouth disease is a common viral illness that usually affects infants and children younger than 5 years old. However, it can sometimes occur in adults. Symptoms of hand-foot-mouth disease include an acute onset of fever, a sore throat, mouth sores (small blister formations), and skin rash. 28) (C) The number one leading cause of death in adolescents in the United States is accidents/injuries. The second leading cause of death in adolescents is homicide. The third leading cause of death in adolescents is suicide. These are followed by cancer (4th) and heart disease (5th) (source: cdc.gov). 29) (C) Hemolytic uremic syndrome is a condition characterized by hemolytic anemia (anemia caused by destruction of red blood cells), low platelet count (thrombocytopenia), and acute kidney failure (uremia). 30) (A) During a hemolytic episode, a practitioner would expect reticulocytosis, an increase in reticulocytes, which are immature red blood cells. There is an increase in reticulocytes to replace all of the red blood cells that have been destroyed due to the hemolytic episode. 31) (C) Blood transfusions and dialysis are the first-line treatments for hemolytic uremic syndrome. Antibiotics are not given because they can actually worsen hemolytic uremic syndrome. 32) (A) Hemolytic uremic syndrome is normally contracted by a person eating a raw dish containing the E. coli strain which causes hemolytic uremic syndrome. 33) (C) Bronchiolitis is a common lung infection in young children and infants. It causes inflammation and congestion in the small airways (bronchioles) of the lung. Bronchiolitis is almost always caused by a virus. Typically, the peak time for bronchiolitis is during the winter months. Bronchiolitis starts out with symptoms similar to those of a common cold but then progresses to coughing, wheezing and sometimes difficulty breathing. Symptoms of bronchiolitis can last for several days to weeks, even a month (source: mayoclinic.org). 34) (A) Bronchiolitis is caused the vast majority of the time by a virus. The most common virus that causes bronchiolitis is respiratory syncytial virus (RSV) (source: healthline.com). 35) (D) The peak time for bronchiolitis is during the winter months. 36) (B) Bronchiolitis is most commonly diagnosed through a nose swab sample. The healthcare provider takes a sample of mucus from the child’s nose. The sample is then tested for the virus that may be affecting the child. 37) (C) Sleep apnea isn’t associated directly with bronchiolitis. Common symptoms of bronchiolitis include a runny nose, a stuffy nose, a cough, wheezing, and difficulty breathing. A slight fever may also be present. Bronchiolitis occurs when a virus infects the bronchioles, which are small airways in the lungs. The infection makes the bronchioles swell and become inflamed. Mucus collects in these airways, which makes it difficult for air to flow freely in and out of the lungs (hence, causing wheezing at times). 38) (A) Most cases of bronchiolitis are treated at home. Only in severe cases does bronchiolitis require hospitalization. Bronchiolitis occurs most often during the first 2 years of life, especially ages 3 to 6 months. The illness typically lasts for about 1-2 weeks. Bronchiolitis is more common in children who have not been breastfed (source: emedicine.medscape.com & medlineplus.gov). 39) (D) Because viruses cause bronchiolitis, antibiotics (which are used to treat bacterial infections) aren’t effective against it. Bronchodilators (drugs that open the airways) haven’t been found to be routinely helpful. But a person’s doctor may try nebulized albuterol treatment to see if it helps. Oral corticosteroid medications and chest physiotherapy (to loosen mucus) have not been shown to be effective treatments for bronchiolitis and are not recommended. In severe cases of infection, a child may be admitted to the hospital, where treatment includes oxygen, humidified air, suctioning of nasal secretions, and IV fluids. 40) (A) Palivizumab is a medication used to prevent RSV in children who are at high risk for RSV. The drug is injected into a large muscle such as the thigh once a month for several months during the RSV season (source: medlineplus.gov). 41) (A) Anorexia is a lack of appetite for food, while anorexia nervosa is an eating disorder characterized by self-starvation and excessive weight loss. 42) (B) For spinal curvatures of 20 to 40 degrees, bracing is the usual treatment. For spinal curvatures less than 20 degrees, the practitioner would usually just observe and monitor for changes in curvature. For curvatures greater than 40 degrees, surgical correction is usually done such as with Harrington rods used on the spine. 43) (A) Molluscum contagiosum is a viral infection of the skin. It is caused by an infection of the poxvirus (molluscum contagiosum virus) (source: cdc.gov). 44) (D) Molluscum contagiosum is characterized by round, firm, painless bumps. Image: Molluscum contagiosum 45) (C) The bumps that appear with molluscum contagiosum usually go away on their own. Only in rare cases are the bumps removed using medications or other procedures. 46) (C) Molluscum contagiosum is a medium-term disorder. It normally resolves within a few months (6-12 months). In certain cases, however, it may take years to resolve (up to about 4 years). 47) (B) Molluscum contagiosum is not a precancerous skin condition. It is largely a benign condition that is self-limiting. The bumps associated with molluscum contagiosum usually disappear without treatment. The round, firm, painless bumps that are associated with molluscum contagiosum can appear anywhere on the body. Immunocompromised individuals such as those with HIV are at higher risk for this skin disorder. The bumps on people who are immunocompromised may be more numerous, larger, and more difficult to treat. Molluscum contagiosum is contagious and spreads either from direct person-to-person contact or through contaminated fomites. Fomites are inanimate objects that are contaminated with the virus that causes molluscum contagiosum. 48) (C) People with molluscum contagiosum should be careful not to scratch or pick at molluscum lesions. This is because this can spread lesions from the infected part(s) of the body to other areas of the body; this is called autoinoculation. Therefore, the person should either not scratch the area or enclose the area, such as with a watertight bandage, to contain the infection to that area. Molluscum contagiosum is a viral infection; therefore, antifungals, such as Griseofulvin, are not used. Areas of skin with lesions should not be shaved at all, because this can be spread the infection to other parts of the body. 49) (C) The Tanner stages describe stages of pubertal maturation. Boys are rated for genital development and pubic hair growth, while girls are rated for breast development and pubic hair growth. Tanner Stages range from Stage I to Stage V, so it’s a 5-point scale. 50) (B) With the Tanner scale, the breasts begin to bud and the areola begin to develop at Stage II. So, with the Tanner scale, stage I represents the prepubertal pattern (the breasts before puberty occurs). In Stage II, the breasts begin to bud and the areolae start to enlarge (widen). During this stage, there is one mound formed (the mound of the breasts extended from the chest). In Stage III, the breasts continue to grow, along with the nipples and areolae. In Stage IV, the nipples and areolae become elevated, forming a secondary mound (the mound of the nipple and areola extending from each of the breasts). Stage V is the adult pattern of full-grown mature breasts. Image: Tanner Stages of Breast Development in Girls 51) (C) During Stage IV, the nipple and areola begin to separate from the breasts. This is the secondary mound. The first mound formed during Stage II is the breast protruding from the chest. The second mound formed is the nipple and areola protruding from the breast. 52) (D) Stage V of the Tanner scale represents full, mature, adult breasts. The 2 easiest stages to represent during the Tanner Scale is Stage I and Stage V. Stage I is the prepubertal stage. This is the stage before puberty has hit, so breast development has not begun yet. Stage V is the full adult stage, in which the breasts have reached full maturation. Then you just have to think of the middle 3 stages. In Stage II, just remember that breast development begins and the areolae begin to enlarge (widen in size). The first mound is formed (the breast protruding from the chest). In Stage III, the breasts along with the nipples and areolae simply increase in size. In Stage IV, the nipple and areola separate from the chest, forming a secondary mound. 53) (B) During Tanner Stage II, there is enlargement of the scrotum and testes. Also, during this stage, the scrotal skin reddens and changes in texture. So, with males regarding the external genitalia, Stage I represents the prepubertal stage (before a boy hits puberty). During this stage, the testes, scrotal sac, and penis have a size and proportion similar to those seen in early childhood. In Stage II, there begins to be an enlargement of the scrotum and testes; the scrotal skin reddens and changes in texture (more rugae). In Stage III, the penis increases in size, initially in length, but also with some increase in circumference as well. The testes and scrotum also continue to become larger. During Stage IV, the penis enlarges in length and circumference. The testes and scrotum continue to enlarge, and there is a distinct darkening of the scrotal skin. In Stage V, the genitalia are adult with regard to size and shape. Image: Tanner Stages of External Genitalia in Boys 54) (B) During Stage III, the penis begins to enlarge, initially in length, but with some circumference increase as well. During Stage IV, the penis continues to enlarge. By Stage V, the boy has full adult genitalia. Stage II is an increase in size of the testes and scrotum. 55) (C) During Tanner Stage IV, there is a distinct darkening of the scrotal sac. 56) (B) The stepping reflex is a reflex in which the neonate steps up and down in place when held upright. It usually disappears by 1-2 months. 57) (C) To check for the rooting reflex, a nurse practitioner strokes the corner of the newborn’s mouth with her finger. A normal response (seen in children under 4 months) is for the child to turn toward the finger and attempt to suckle on it. 58) (B) The rooting reflex disappears around 3-4 months. 59) (D) The blinking reflex is a permanent reflex that should be present from birth. To test this reflex, a light puff of air is placed over the infant’s eyes. A normal result is the infant closing his or her eyes. 60) (C) The practitioner is checking the tonic neck reflex. When the baby lies flat (supine) on the bed with the head turned to one side, the normal response is extension of the extremities to the side that the head is facing and flexion of the other side of the extremities. It is also known as the fencing reflex because of the characteristic position of the infant’s arms and head, which resemble that of a classically trained fencer. Image: Tonic neck reflex Credit: Photograph by Mjlissner, distributed under the Creative Commons CC0 1.0 Universal Public Domain Dedication 61) (C) Lowering a baby suddenly from a neutral position to a lower position elicits the Moro reflex. A normal finding for the Moro reflex would be the baby’s arms flail outward and then are brought into the body. The hands will open and the infant will usually cry out. The Moro reflex disappears by 6 months of age. 62) (D) The Babinski reflex occurs after the sole of the foot has been firmly stroked. A positive finding would be the big toe then moves upward or toward the top surface of the foot and the other toes fan out. Though Babinski’s reflex may disappear as early as 1 year, it is normal in children up to 2 years of age (source: medlineplus.gov). 63) (A) The "anal wink" is a contraction of the external anal sphincter when the skin near the anal opening is scratched. 64) (C) By 5 years of age, a child’s reflexes should be the same as like an adult. 65) (B) A child should be able to sit unsupported by 7-8 months. 66) (B) An infant starts babbling at around 6 months of age. 67) (C) A child should be able to hold a crayon and may make marks on a paper by the age of 12 months (1 year). 68) (B) A child begins using the pincer grasp at about 7-8 months of age. The pincer grasp is a grasp where a child holds an object in between the thumb and the index finger. Image: Pincer grasp 69) (B) By 6 months of age, a child should be able to roll from his back to his stomach and from his stomach to his back. 70) (C) A child should be able to draw circles and squares by 4 years of age. 71) (B) By 5 years of age, a child should be able to dress him or herself. 72) (B) A child begins walking (taking steps), with or without support, usually between 9 and 12 months. By 18 months of age, the child should be able to walk independently. 73) (B) Children normally can ride a tricycle by the age of 3 years. So when you see tricycle, think of tri for (three). A child should be able to ride a tricycle by the age of 3. 74) (B) By the age of 6, most children have the balance and coordination to be able to ride a bicycle. 75) (C) A child begins thinking abstractly at about 11 years of age. 76) (C) To examine the ear canal of an infant, the auricle should be pulled backward and downward. To examine the ear canal on older children and adults, the auricle is pulled backward and upward. 77) (C) It is normal for infants to have periods of apnea lasting up to 15 seconds. 78) (C) Ibuprofen (Motrin) can be given to a child after 6 months of age. Ibuprofen should never be given to infants less than 6 months of age. 79) (D) Intoeing means that the feet turn inward instead of pointing straight ahead when a child walks. It is commonly referred to as being pigeon-toed. In the vast majority of cases in children younger than 8 years of age, intoeing will almost always correct itself without any type of treatment. Intoeing does not increase a child’s risk of obtaining arthritis and does not cause pain. 80) (A) Parents account for the majority of perpetrators in child abuse cases. 81) (C) Risk factors for child abuse include a history of domestic violence in a family, poverty or very low socioeconomic status, immature parents, single-parent status, lack of extended family support, social isolation, a situation of financial difficulty, and drug abuse. 82) (A) Children under the age of 3 are most at risk for abuse because of the total reliance they have on their caregiver for all needs. 83) (B) Bruises on the hands of a child would be least likely to be a sign of physical abuse in a child. This is because the hands are a high-impact area that is frequently used to shield the body in times of falls. Signs of physical abuse in a child include repeated visits to a healthcare facility where there are either questionable causes for the injury that has taken place or whose stories or descriptions of what occurred don’t match. Injuries to areas of the body that don’t frequently receive impact such as from falls could be a sign of child abuse; these include the head, chest, genital area, and buttocks. Any patterned marks on the body such as a belt buckle or an iron is suspicious of child abuse, especially if the child can name the object when asked about the mark. Injuries such as burns, bruising, lacerations, or bite marks may indicate abuse. For burns, children do pull out pans from hot stoves, but these burns typically affect the chest and abdomen; they wouldn’t involve areas such as the buttocks or head. Other signs of abuse include multiple fractures in the body, especially if they are in various stages of healing. Femur fractures in a nonambulating infant is also a possible sign of child abuse. 84) (B) Healthcare providers are mandatory reporters of abuse, so they are obligated to report abuse to the authorities or a child abuse hotline. This includes all forms of abuse. They do not confront and interrogate suspected abusers directly but report the information to the appropriate authorities. 85) (D) A girl with complaints of malodorous urine most likely has a UTI, which is common in young girls. Signs of sexual abuse include vaginal discharge, vaginal bleeding, vaginal itching or swelling, a child acting out sexually in inappropriate ways, and pain in the genital area. 86) (C) Colic is a condition that is a bit of a mystery; its cause is unknown. Colic is a term that applies to any healthy, well-fed infant who cries more than 3 hours a day, more than 3 days a week, for more than 3 weeks. Things we know about colic is that it is likely to start around the age of 2 weeks if the infant is full-term or later if premature. It almost always goes away on its own by 3 or 4 months. The baby’s gender or whether it’s breast or bottle fed doesn’t matter. Kids who had colic as babies are no different from those who didn’t (source: webmd.com). 87) (B) Infant colic is essentially unexplained crying (crying for which no cause can be found). Colic is a term that applies to any healthy, well-fed infant who cries more than 3 hours a day, more than 3 days a week, for more than 3 weeks. 88) (D) Jaundice, a yellowing of the skin or sclera of the eyes, is caused by elevated bilirubin levels. The most common type of jaundice is physiologic jaundice which affects up to 60% of full term babies in the first week of life; physiologic jaundice is a normal occurrence. Jaundice develops when a baby’s liver is not efficient enough to remove the bilirubin from the bloodstream. Once the baby begins to mature and red blood cells diminish, the jaundice will subside with no lasting effects on the body. This usually happens about 1-2 weeks after birth. Besides physiologic (normal) jaundice, jaundice can also occur due to prematurity (jaundice due to the fact that premature babies have even less developed livers to eliminate bilirubin and thus are at higher risk), blood incompatibility with the mother, medical conditions such as blood clotting issues, excessive bruising during birth, and issues with breastfeeding. 89) (D) Spermarche refers to the beginning of development of sperm in boys’ testicles at puberty. It is one of the first events in the life of a male leading to sexual maturity. It occurs at the time when the body develops secondary sexual characteristics. Although it is not 100% known, it appears that spermarche occurs between the ages of 11-15 years of age. 90) (C) Asthma is the number one reason for hospitalization among children. It is also worthy to note that asthma is the most chronic disease of childhood (Rudd & Kocisko, 2014). 91) (C) According to the CDC, the most common cause of infant mortality in the United States is birth defects, followed by prematurity/low birth weight, then sudden infant death syndrome, then complications of pregnancy, and then unintentional injury. 92) (D) Adolescents are children who range in age from 13-18 years. Newborns are those less than 28 days old. Infants are those from the age of 1 month to 1 year old. Toddlers are those 1 to 3 years old. Preschool children are those ages 3 to 5. School-age children are those 6-12 years old. 93) (B) Sunscreen can be applied on a child starting at 6 months of age. 94) (D) When a newborn or infant is being treated with phototherapy for hyperbilirubinemia, the eyes and genitalia should be covered. Covering the infant’s eyes is done to prevent cataracts. Eye patches are removed and the infant is held only during feedings. In phototherapy, blue-green fluorescent light is absorbed into the skin, mixes with bilirubin, and converts bilirubin into lumirubin, which is water soluble and thereby allows the infant to excrete bilirubin in the stool and urine (Rudd & Kocisko, 2014). 95) (C) 6-10 wet diapers/day is considered normal urine output for infants (Rudd & Kocisko, 2014). 96) (C) Infants who are fed solid food too early have a higher incidence of developing food allergies as a result of exposure to proteins in the food (Rudd & Kocisko, 2014). 97) (C) The infant’s immune system is not fully developed until 6 months of age, and begins to produce antibodies around 2 to 3 months of age. Infants are at increased risk for infection who are younger than 6 months because of immature immune responses (Rudd & Kocisko, 2014). 98) (B) According to the American Dental Association, a child should have his or her first dental visit by 1 year of age. 99) (C) Teething is the eruption of the teeth through the gums. Teeth erupt at 4 to 10 months, usually around 6 months. Usually the first 2 teeth that erupt are the two lower center teeth. 100) (D) Bacon can safely be given to a child under 1 year of age. Cow’s milk should not be given to a child under 1 year of age because it can cause gastrointestinal bleeding. Honey or corn syrup should never be given to a child less than 1 year of age because this may result in the ingestion of Clostridium botulinum bacteria (Rudd & Kocisko, 2014). 101) (A) The primary reason for low birth weight in a newborn is prematurity of birth (born < 37 weeks of gestation). 102) (D) According to guidelines from the American Academy of Pediatrics (AAP), rear-facing seats in the back seat are used from birth to 2 years of age, or until the child has reached the height and weight limits for the car seat. 103) (A) Nose breathing is normal; mouth breathing would be a sign of respiratory distress. Signs of respiratory distress in a child include tachypnea (breathing rapidly), retractions (ability to see ribs during inhalation), nasal flaring (nares flare out in an effort to take in air), accessory muscle use (use of shoulders and abdomen to breathe), tripod positioning (sitting with head up and out to stent the airway open), stridor (high-pitched sound indicative of upper airway obstruction), and wheezing (Rudd & Kocisko, 2014). 104) (C) Enuresis is a condition of urinary incontinence. 105) (A) Sudden infant death syndrome (SIDS) is the unexplained death, usually during sleep, of a seemingly healthy baby less than a year old. SIDS is sometimes known as crib death because the infants often die in their cribs. SIDs can occur at any time from 1 week old to 1 year old, but the peak incidence of SIDS is 2 to 4 months of age. With SIDS, the cause of death is unknown, but autopsy reveals pulmonary edema. Placing an infant to sleep on his or her back is an important measure to prevent SIDS. 106) (C) Normal systolic blood pressure in infants is between 70 and 90 mmHg. In adolescence, blood pressure reaches adult levels. Routine monitoring of blood pressure should begin around age 3. Diagnosis of hypertension cannot be made from one reading; it requires at least 2 high readings on separate occasions (Rudd & Kocisko, 2014). 107) (C) Most babies begin crawling around the age of 8 months. 108) (B) A child should be taken to his or her first thorough eye examination at 6 months of age. 109) (D) A baby is born with 20/400 vision at birth, which improves steadily during maturation. From birth to 4 months, babies’ primary focus is on objects 8 to 10 inches from their face or the distance to the parent’s face. For the first two months of life, an infant’s eyes are not well coordinated and may appear to wander or to be crossed. This is usually normal. However, if an eye appears to turn in or out constantly, an evaluation is warranted. Babies should begin to follow moving objects with their eyes and reach for things at around 3 months of age (source: allaboutvision.com & aoa.org). 110) (B) Aspirin should not be used in children under the age of 16 years old due to the risk of developing Reye’s syndrome. 111) (A) Tay-Sachs is an autosomal recessive disorder. Both parents must be carriers of TaySachs in order for a child to inherit it. 112) (D) Hexosaminidase A, or hex-A, is the enzyme that children with Tay-Sachs disease lack. Hex-A is needed for the body to break down a fatty waste substance found in brain cells. Without Hex-A, fatty waste substances accumulate abnormally and cause progressive damage until the central nervous system can no longer sustain life. 113) (B) Tay-Sachs is a disease that makes a child unable to break down certain kinds of lipids. The lipids, in turn, build up in the body and damage the nerve cells in the brain and spinal cord. 114) (C) Tay-Sachs is a progressive degenerative disease that is fatal and leads to death. While symptoms vary from one child to the next, there is always a slowing down of development. Gradually, Tay-Sachs children lose motor skills (hypotonia) and mental functions. Over time, the child becomes blind, deaf, mentally retarded, paralyzed and nonresponsive to the environment (source: tay-sachs.org). 115) (C) Tay-Sachs is a fatal disease in which most children die by the age of 5 years. 116) (B) Tay-Sachs disease affects Eastern European Jews (such as Ashkenazi Jews) with the greatest frequency. 117) (A) Babies born with Patau syndrome have an extra chromosome on the 13th pair of chromosomes. Therefore, Patau syndrome is also referred to as trisomy 13. Illustration: Karyotype of a girl born with Patau syndrome 118) (B) Common symptoms of Patau syndrome include multiple organ defects such as kidney and heart abnormalities, severe intellectual disabilities, other conditions such as cleft lip and cleft palate, microcephaly (abnormally small head), microphthalmia (abnormally small eyeballs), and blindness. 119) (A) About 80% of people born with Patau syndrome die within the first year of life. Patau syndrome has a very poor prognosis. In fact, most infants with this condition don’t live past their first week of life. 120) (B) With Edward’s syndrome, there is an extra chromosome on the 18th pair of autosomes. Therefore, Edward’s syndrome is also referred to as trisomy 18. 121) (D) Symptoms of Edward’s syndrome are very similar to symptoms of Patau syndrome. Symptoms of Edward’s syndrome include multiple organ defects such as heart and kidney problems, severe learning disability, bone abnormalities such as scoliosis, feeding problems, breathing problems, and frequent infections of the lungs and urinary system. Like Patau syndrome, Edward’s syndrome commonly causes microcephaly, not macrocephaly. 122) (A) Just like Patau syndrome, most people born with Edward’s syndrome die within the first year of life. Only about 12% of babies born with Edward’s syndrome survive past the first year of life. 123) (B) A mother should be comforted knowing that if she has had a child with Edwards syndrome, the chance of her having another child with Edwards syndrome is no greater than 1%. This is also true for Patau syndrome. If a woman had a baby born with Patau syndrome, the chance of having another child with Patau syndrome is no greater than 1%. 124) (A) Trisomy 13 (Patau syndrome) is the least common and most severe of the viable autosomal trisomys. 125) (A) Common features of children with Down syndrome include flattened facial features, a small head, a short neck, protruding tongue, upward slanting eyes (unusual for the child’s ethnic group), unusually shaped or small ears, low set ears, poor muscle tone, broad, short hands with a single crease in the palm, relatively short fingers and small hands and feet, excessive flexibility, tiny white spots on the colored part (iris) of the eye called Brushfield spots, and short height. Intellectual and developmental problems range from mild to moderate. Infants with Down syndrome may be of average size, but typically they grow slowly and remain shorter than other children the same age. In general, developmental milestones, such as sitting and crawling, occur at about twice the age of children without impairment (source: mayoclinic.org). 126) (B) Children with Down Syndrome with atlantoaxial instability are restricted from playing any type of contact sports. 127) (D) Marfan syndrome is a genetic disorder that affects the body’s connective tissue. People with Marfan syndrome are tall and thin with long arms, legs, fingers, and toes. They usually have either a bulging or a sunken chest. Regarding the heart, people with Marfan syndrome may have an enlarged or bulging aorta, which could be life-threatening. Dystonia, a movement disorder in which a person's muscles contract uncontrollably, is not associated with Marfan syndrome (source: marfan.org). 128) (B) Separation anxiety is distress caused by a fear of abandonment. Separation anxiety can begin as early as 8 months of age and end as late as 3 years of age. Separation anxiety peaks between 10 and 18 months. It is a normal stage of development. When this fear occurs in a child over the age of 6 years, is excessive, and lasts longer than four weeks, the child may have separation anxiety disorder. 129) (A) The Oedipus complex refers to a child’s desire for sexual involvement with the opposite sex parent (i.e., males being attracted to their mothers and females being attracted to their fathers). It is one of Sigmund Freud’s authorships and he claimed that this occurs between the ages of 3-6 years of age. 130) (D) Febrile seizures are the most common type of convulsions in infants and young children. During febrile seizures, usually both the arms and the legs will shake uncontrollably. 131) (A) An absence seizure is a seizure most commonly found in children that is characterized by a blank stare that normally lasts between 10 and 15 seconds. Chapter 15- Men’s Health 1) Spermatogenesis occurs in the: A) B) C) D) Testes Epididymis Prostate gland Vas deferens 2) How long does it take approximately for sperm to fully mature from conception? A) B) C) D) 1 week 1 month 3 months 6 months 3) Where do sperm mature? A) B) C) D) In the testes In the epididymis In the vas deferens In the prostate gland 4) Ideal temperature for sperm production is: A) 1 to 2 °C above core body temperature B) 1 to 2 °C below core body temperature C) 5 to 6 °C below core body temperature D) 5 to 6 °C above core body temperature 5) What is the function of prostatic fluid (the fluid secreted by the prostate gland)? A) Prostatic fluid makes the sperm more active and mobile to penetrate the vagina B) Prostatic fluid is of alkaline pH and helps the sperm survive in the vagina (an acidic pH) C) Prostatic fluid destroys immobile sperm D) Prostatic fluid is of acidic pH and helps the sperm survive in the vagina (an alkaline pH) 6) What is the cremasteric reflex? A) A reflex in which the testicle elevates toward the body in response to stroking or lightly pinching the ipsilateral inner thigh (thigh on the same side as the affected testicle) B) A reflex in which the testicle goes further into the scrotum in response to stroking or lightly pinching the ipsilateral inner thigh C) A reflex in which the vas deferens is pushed toward the prostate gland upon touching the ipsilateral inner thigh D) A reflex in which the vas deferens is pushed toward the epididymis upon touching the ipsilateral inner thigh 7) What is testicular torsion? A) A condition in which the testicle adheres to the scrotum wall B) A condition in which the testicle bursts due to inner inflammation C) A condition in which the two testicles get stuck and connected together D) A condition in which the spermatic cord of the testicle becomes twisted, interrupting the blood supply to the testicle 8) All of the following are symptoms of testicular torsion except for: A) Sudden onset of severe testicular pain B) Absent cremasteric reflex C) Nausea and vomiting D) Internal bleeding of the testicle 9) Which statement is false regarding testicular torsion? A) Usually only one testicle is affected B) In most cases, testicular torsion requires immediate surgery in order to save the testicle C) Most cases of testicular torsion come from men who have bell clapper deformity D) A man has about 72 hours from the onset of testicular torsion to have a high probability of saving the testicle 10) What test is most often done to diagnose testicular torsion? A) B) C) D) Urethral swab Urine culture Color doppler ultrasound Blood test 11) What demographic population does testicular torsion occur most frequently in? A) B) C) D) 12 to 18 year olds 20 to 39 year olds 40 to 59 year olds 60 to 79 year olds 12) What is Peyronie’s disease? A) A condition in which a man cannot achieve an erection without great pain B) A condition in which a man cannot urinate without great pain C) A condition in which fibrous scar tissue called plaque forms within the penis which causes curved, painful erections D) A condition in which an erection produces moderate to severe bleeding from the penis 13) All of the following are risk factors for priapism except for: A) Taking high doses of erectile dysfunction drugs B) Diabetes C) Having sickle cell anemia D) Cocaine use 14) What tubes are cut during a vasectomy? A) B) C) D) The ureters The urethra The epididymis The vas deferens 15) Which of the following statements is false regarding the testicular self-examination (TSE)? A) The TSE should be performed on a monthly basis B) The TSE is best performed while a male is taking a warm shower C) A male should gently roll each testicle between his fingers, feeling for any irregularities on the surface or texture of the testicle D) If a male notices one testicle is slightly larger than the other or one testicle hangs lower than the other, he should contact his health provider immediately 16) What is the definitive diagnosis for testicular cancer? A) Ultrasound of the testicle B) Blood test checking for tumor markers C) Testicular biopsy D) A manual digital exam of the testicles 17) How can the testicle be described for a male with testicular cancer? A) B) C) D) A shrunken testicle A softened testicle A testicle that is like a solid mass A testicle that is very bumpy 18) All of the following are common symptoms of benign prostatic hypertrophy (BPH) except for: A) B) C) D) Postvoid dribbling Nocturia Feelings of incomplete emptying Bacteriuria 19) What does finasteride (Proscar) do to the prostate? A) Vascularizes it B) Enlarges it C) Shrinks it D) Destroys bad tissue on the prostate 20) A patient with benign prostatic hypertrophy has been taking finasteride (Proscar) for several months and has recently got blood drawn to measure his prostate-specific antigen (PSA) levels. His baseline PSA was 3 ng/mL when measured before the finasteride treatment. After receiving his lab results, his PSA levels are now 2.5 ng/mL. This shows that the man’s PSA has: A) B) C) D) Gotten worse Has remained unchanged Has improved slightly Has improved dramatically 21) Which of the following statements is false regarding acute prostatitis? A) Acute prostatitis is a serious infection and swelling of the prostate gland B) Acute prostatitis is a medical emergency C) Acute prostatitis can be caused by sexually transmitted infections D) Acute prostatitis increases the risk for prostate cancer 22) A nurse practitioner suspects that a patient has acute prostatitis based on symptoms and history. Upon performing a digital rectal exam (DRE) of the prostate, the nurse would expect the prostate to feel: A) B) C) D) Rubbery and of normal size Extremely tender and boggy Like a hard mass Enlarged and rubbery 23) All of the following would be observed in a healthy prostate gland during a digital rectal exam (DRE) except: A) The prostate would feel symmetrical (the same on both sides) B) The prostate would feel rubbery C) The prostate would feel hard D) The prostate would be heart-shaped 24) What is balanitis? A) Inflammation of the scrotum B) Inflammation of the testes C) Inflammation of the epididymis D) Inflammation of the glans of the penis 25) What is the most common cause of balanitis? A) B) C) D) Bacterial infection Candida yeast infection Chemical irritant Psoriasis 26) All of the following are common symptoms of balanitis except for: A) B) C) D) Redness Gangrene Soreness Irritation 27) Which statement is true concerning balanitis? A) It occurs most often in men and rarely affects young boys B) It more commonly affects uncircumcised males C) Balanitis is a rare condition D) Balanitis is treated by washing the area thoroughly with soap and water each day 28) What is varicocele? A) An enlargement of veins in the scrotum B) A painless buildup of watery fluid around one or both testicles that causes the scrotum or groin area to swell C) A painful buildup of watery fluid around one or both testicles that causes the scrotum or groin area to swell D) Inflammation of the glans of the penis 29) A varicocele is often described as a scrotum that feels like it contains: A) B) C) D) A heavy ball A bag of worms A hammer A stick 30) The NP is examining a patient who she suspects has varicocele. What can help the NP visualize the veins on the scrotum better? A) Rub the area gently a few times B) Tap the area with the fingernail C) Ask the patient to take a deep breath and hold it while bearing down (the Valsalva maneuver) D) Ask the patient to sit in the high fowler’s position during inspection 31) Varicocele commonly causes the testes to: A) B) C) D) Enlarge in size Shrink in size Become gangrenous Have a bumpy texture 32) What complication can varicocele cause? A) B) C) D) Benign prostatic hypertrophy Acute bacterial epididymitis UTIs Infertility 33) Which of the following is the most common cause of epididymitis in young adult males? A) B) C) D) UTIs Testicular cancer STDs Testicular torsion 34) All of the following symptoms are common in epididymitis except for: A) B) C) D) Low-grade fever Chills Painless ejaculation Scrotal pain 35) What is the most commonly prescribed treatment for epididymitis? A) B) C) D) Antibiotics Antivirals Antifungals Antiparasitics 36) Epididymitis is most commonly found in males age: A) B) C) D) 2 to 5 years 12 to 18 years 20 to 39 years 60-80 years 37) Which medication poses a high risk for a patient developing epididymitis? A) B) C) D) Erythromycin Amiodarone Penicillin Furosemide 38) Which test is specific to epididymitis? A) B) C) D) Prehn’s sign Lachman test Blue dot sign McMurray’s test 39) All of the following tests may be conducted to diagnose epididymitis except for a: A) B) C) D) Complete blood count Muscle biopsy Urethral culture Urine culture 40) Any time there is severe scrotal pain from a condition such as epididymitis, what condition should be ruled out due to the fact that it is a urologic emergency? A) B) C) D) Testicular cancer Prostatitis Testicular torsion Orchitis 41) When a testicle is inflamed along with the epididymis, this is called: A) B) C) D) Testicular torsion Orchitis Epididymo-orchitis Urethritis 42) The epididymis connects the: A) B) C) D) Prostate to the urethra Testicles to the vas deferens Kidneys to the bladder Ureters to the bladder 43) What is orchitis? A) B) C) D) Inflammation of the vas deferens Inflammation of the epididymis Inflammation of the testicles Inflammation of the prostate 44) What type of infection precedes most cases of reactive arthritis? A) B) C) D) UTIs Common cold STDs Pneumonia 45) What is a hydrocele? A) An accumulation of fluid in the testicles B) An accumulation of fluid surrounding the testicles C) An accumulation of fluid in the epididymis D) An accumulation of fluid in the vas deferens 46) Which statement is false regarding a hydrocele? A) A hydrocele is generally painless B) Hydroceles occur due to a defect in how the kidneys filter fluids C) A hydrocele causes the scrotum or groin area to swell D) Hydroceles can occur at any age 47) Erectile dysfunction is also called: A) B) C) D) Priapism Sterility Impotence Proctitis 48) Which of the following statements is false regarding erectile dysfunction? A) Erectile dysfunction is the inability to get and keep an erection firm enough for sex B) Erectile dysfunction does not interfere with a man’s ability to impregnate a woman C) Erectile dysfunction can be caused due to physical or psychological issues D) Smoking is a risk factor for erectile dysfunction 49) Which of the following drugs is most effective for erectile dysfunction? A) B) C) D) Phosphodiesterase inhibitors Nitrates Beta blockers ACE inhibitors 50) Which of the following is false regarding torsion of the appendix testis? A) Torsion of the appendix is a twisting of the vestigial appendage that is located along the testicle B) The appendix testis is present in about 90% of males C) This condition can cause sterility in a man later in life D) The condition can be painful 51) Which sign is indicative of torsion of the appendix testis? A) B) C) D) Prehn’s sign Blue dot sign Murphy’s sign McMurray’s sign 52) The urethral opening being present on the ventral surface of the penis is referred to as: A) B) C) D) Hypospadias Epispadias Peyronie’s disease Balanitis 53) The urethral opening being present on the dorsal surface of the penis is referred to as: A) B) C) D) Hypospadias Epispadias Peyronie’s disease Balanitis 54) What is the difference between gynecomastia and pseudogynecomastia? A) Gynecomastia is a buildup of excessive growth tissue, while pseudogynecomastia is a buildup of fat behind, around, and under the nipples B) Pseudogynecomastia is a buildup of fat behind, around, and under the nipples, while gynecomastia is a buildup of excessive growth tissue C) Gynecomastia is a buildup of excessive growth tissue, while pseudogynecomastia is a proliferation of lipomas around the nipples D) Gynecomastia is a proliferation of lipomas around the breast tissue, while pseudogynecomastia is excessive growth tissue. So, with gynecomastia, the underlying matter is breast tissue; with pseudogynecomastia, the underlying matter is fat. 55) Which of the following disorders can transillumination be used in order to help diagnose it? A) B) C) D) Cataracts Tendonitis Glaucoma Hydrocele 56) For men with erectile dysfunction, sildenafil (Viagra) should be taken: A) B) C) D) 5 to 10 minutes before sex 30 to 60 minutes before sex 2 hours before sex 4 hours before sex 57) All of the following statements are true concerning sildenafil (Viagra) except: A) Sildenafil should be taken on an empty stomach because foods and fats delay its action B) Sildenafil can be taken up to 3 times a day before sexual activity C) Sildenafil should not be taken with nitrates D) Sildenafil side effects include headache, nasal congestion, and facial flushing 58) A condition in which foreskin of the penis cannot be pulled back is termed: A) B) C) D) Phimosis Balanitis Peyronie’s disease Epispadias 59) For which condition is the cremasteric reflex absent? A) B) C) D) Testicular cancer Hydrocele Prostatitis Testicular torsion 60) Klinefelter syndrome is also known as: A) B) C) D) Trisomy 13 Trisomy 18 XYY syndrome XXY syndrome 61) All of the following are common symptoms of Klinefelter syndrome except for: A) B) C) D) Small testicles Gynecomastia Osteoporosis Excess hair on the skin 62) Most men with Klinefelter syndrome: A) B) C) D) Have seizure disorders Are shorter than average height Are sterile Are severely mentally retarded 63) Men with Klinefelter syndrome produce low amounts of: A) B) C) D) Red blood cells White blood cells Platelets Testosterone Men’s Health answers 1) (A) Spermatogenesis, the process in which sperm are created, occur in the testes. 2) (C) It takes sperm around 2 ½ - 3 months to fully mature from conception. 3) (B) Sperm are created in the testes but mature in the epididymis. 4) (B) Ideal temperature for sperm production in the testicles is 1 to 2 °C below core body temperature. 5) (B) Prostatic fluid is of alkaline pH and helps the sperm survive in the vagina (which has an acidic pH). 6) (A) The cremasteric reflex is a reflex in which the testicle elevates toward the body in response to stroking or lightly pinching the ipsilateral thigh (thigh on the same side as the affected testicle). With testicular torsion, the cremasteric reflex is absent. 7) (D) Testicular torsion is a condition in which the spermatic cord of the testicle becomes twisted, interrupting the blood supply to the testicle. 8) (D) Symptoms of testicular torsion include sudden onset of severe testicular or scrotal pain, nausea and vomiting, scrotal edema, and an absent cremasteric reflex. 9) (D) From the onset of testicular torsion, time is critical. The longer the time that passes without medical treatment, the greater the chance a man has of losing his testicle. 72 hours is much too long. By this time, the chance of saving the testicle is practically zero. The rule is, if a man gets surgery done within 4-6 hours from onset of the testicular torsion, the testicle has a 90% chance of being saved. This chance drops to 50% by hour 12. By 24 hours, it drops to 10%. And the longer the time after this that passes, the chances decrease further. With testicular torsion, timely treatment is vital. Testicular torsion is usually unilateral (affects only one testicle). Bilateral testicular torsion is extremely rare. In most cases, testicular torsion requires immediate surgery in order to save the testicle. Most cases of testicular torsion come from men who have bell clapper deformity. In most males, the testicles are attached to the scrotum, making it difficult for the spermatic cord to twist. In males who have bell clapper deformity, the testicles are unsecured and can move and twist in the scrotum. 10) (C) A color doppler ultrasound, specifically a color Doppler, is most often used to diagnose a testicular torsion. Although a urethral swab or urine culture will rule out other disorders such as epididymitis, testicular torsion is a time-critical emergency. Urethral swabs or urine cultures would be too time-expensive; it would take too long to get results from them. A blood test wouldn’t show any specific indicators that would definitively show that a person has testicular torsion. 11) (A) Testicular torsion can occur at any age but it is most common during the ages of 12 to 18. 12) (C) Peyronie’s disease is a condition in which fibrous scar tissue called plaque forms within the penis which causes curved, painful erections. Image: Peyronie’s disease Credit: Photograph by SugarMaple, licensed under the Creative Commons Attribution-Share Alike 3.0 Unported license 13) (B) Certain medications such as erectile dysfunction drugs, certain medical conditions such as sickle cell anemia, and the use of certain types of drugs such as cocaine are risk factors for priapism. Diabetes isn’t directly associated with priapism. 14) (D) The vas deferens are cut during a vasectomy. This makes a man be unable to have kids. 15) (D) It is recommended that testicular self-examinations be done on a monthly basis. Most testicular cancers are found by men themselves or their partner. Very few are found by a physician, so it is important for a male to be acquainted with this self-exam. It is best to do the testicular self-exam during or right after a warm shower or bath. The warmth relaxes the scrotum, making the exam easier. If possible, the male should stand in front of a mirror. He should first check for any swelling on the scrotal skin. Then he should examine each testicle with both hands. He should place his index and middle fingers under the testicle with the thumbs placed on top. He should gently roll the testicle between the thumbs and fingers to feel for any irregularities on the surface or any irregularities in the texture of the testicle. He should then find the epididymis, a soft rope-like structure on the back of the testicle. Being familiar with this structure won’t make him mistake it for a suspicious lump. It is normal for one testicle to seem slightly larger than the other and it’s also normal for one testicle to hang lower than the other. If any testicular lumps, bumps, or irregularities are noted, he should see a doctor. Not all lumps are cancerous, but he should be further evaluated by his health care provider. 16) (C) The definitive diagnosis for testicular cancer is a testicular biopsy. 17) (C) The testicle of a male with testicular cancer is often described as a testicle that is like a solid mass. 18) (D) Bacteriuria is not a common symptom of benign prostatic hypertrophy and would require further investigation. Common symptoms of benign prostatic hypertrophy are postvoid dribbling, nocturia, feelings of incomplete emptying, urinary urgency, and weak urinary stream. 19) (C) Finasteride, an antiandrogen drug, shrinks the prostate gland by about 50%. It is used for benign prostatic hypertrophy (BPH). It may also be used for prostate cancer, being that is an antiandrogen (prostate cancer is believed to be fueled by testosterone). 20) (A) This shows that the man’s PSA count has gotten worse. Finasteride shrinks a man’s prostate by about 50% throughout the course of its therapy; this decreases the PSA