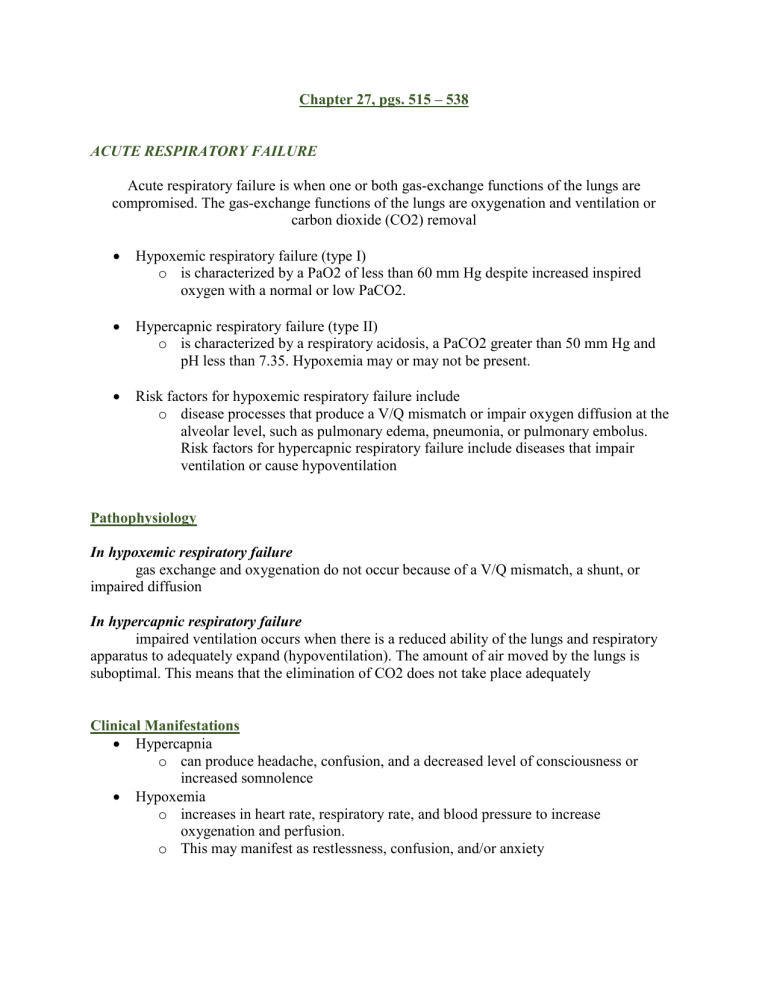
Chapter 27, pgs. 515 – 538 ACUTE RESPIRATORY FAILURE Acute respiratory failure is when one or both gas-exchange functions of the lungs are compromised. The gas-exchange functions of the lungs are oxygenation and ventilation or carbon dioxide (CO2) removal Hypoxemic respiratory failure (type I) o is characterized by a PaO2 of less than 60 mm Hg despite increased inspired oxygen with a normal or low PaCO2. Hypercapnic respiratory failure (type II) o is characterized by a respiratory acidosis, a PaCO2 greater than 50 mm Hg and pH less than 7.35. Hypoxemia may or may not be present. Risk factors for hypoxemic respiratory failure include o disease processes that produce a V/Q mismatch or impair oxygen diffusion at the alveolar level, such as pulmonary edema, pneumonia, or pulmonary embolus. Risk factors for hypercapnic respiratory failure include diseases that impair ventilation or cause hypoventilation Pathophysiology In hypoxemic respiratory failure gas exchange and oxygenation do not occur because of a V/Q mismatch, a shunt, or impaired diffusion In hypercapnic respiratory failure impaired ventilation occurs when there is a reduced ability of the lungs and respiratory apparatus to adequately expand (hypoventilation). The amount of air moved by the lungs is suboptimal. This means that the elimination of CO2 does not take place adequately Clinical Manifestations Hypercapnia o can produce headache, confusion, and a decreased level of consciousness or increased somnolence Hypoxemia o increases in heart rate, respiratory rate, and blood pressure to increase oxygenation and perfusion. o This may manifest as restlessness, confusion, and/or anxiety Diagnosis Arterial blood gases o assess the adequacy of both oxygenation and ventilation in the lungs o SpO2 greater than 94% (which correlates to a PaO2 of approximately 80 mm Hg). Hypercarbic respiratory failure results in ABGs with a pH of less than 7.35 and a PaCO2 of greater than 45 mm Hg Venous oxygen saturation measures the amount of oxygenated blood returning to the heart to determine the adequacy of perfusion at the tissue level A normal venous oxygen saturation is 60% to 80%. A decreased venous oxygen saturation indicates inadequate cardiac output; the tissues are extracting more oxygen than normal because of the decreased oxygen delivery hemoglobin and hematocrit should be analyzed to make certain that there are enough binding sites for oxygen to ensure adequate oxygen-carrying capacity A chest x-ray may show such as heart failure, pulmonary congestion, pneumonia, or pneumothorax, that can explain the respiratory failure A sputum culture should be obtained to rule out a pathogenic (i.e., bacterial or viral) cause of the failure. Treatment Respiratory failure is not a disease—it is a condition caused by another disease or disorder begins with oxygen The use of a nasal cannula or Venturi mask may provide adequate support. This is not the case when a patient is suffering from respiratory failure. The patient in acute respiratory failure who has not responded to traditional methods of oxygen administration may be placed on a nonrebreather mask with 100% FIO2. The mask is placed over the patient’s nose and mouth and then secured to the patient using the elastic band. The oxygen flow meter is then turned on to its maximum setting. The reservoir bag of the mask should be inflated to ensure that the patient is receiving 100% oxygen. noninvasive or invasive positive-pressure ventilation may be necessary to open the alveoli to allow gas exchange. Noninvasive positive-pressure ventilation (NPPV), such as bilevel positive airway pressure (BiPAP) or continuous positive airway pressure (CPAP), administered via a tight-fitting face mask, can be used to help increase oxygenation. In BiPAP, the patient receives two different pressures. A higher pressure during inhalation assists with the opening of the alveoli, and a lower pressure during exhalation keeps the alveoli from collapsing during/at the end of exhalation but also allows ease of exhalation. In contrast, CPAP maintains one continuous pressure throughout the respiratory cycle to help keep the alveoli open through inspiration and expiration. Invasive positive-pressure ventilation requires an advanced airway, such as an endotracheal tube (ETT) or a tracheostomy tube, and mechanical ventilation. As with CPAP, during mechanical ventilation, positive pressure is maintained throughout the ventilatory cycle in the form of positive end-expiratory pressure (PEEP). The pressure is measured at the end of expiration, thus the name, but as stated, the positive pressure is maintained throughout the cycle. Mechanical ventilation is discussed in detail in Chapter 7. Medications inhaled bronchodilators o open the airways by stimulating beta-2 receptors within the lungs inhaled steroids o decrease the inflammatory response, decreasing bronchoconstriction and increasing the airway diameter diuretics o are used to decrease pulmonary congestion, especially in cases where pulmonary edema is the underlying cause of failure. sedation o used to control agitation and anxiety that increase the work of breathing and oxygen consumption, and it is especially needed if the patient requires mechanical ventilation antibiotics o may be initially broad spectrum to treat a suspected pneumonia and are adjusted if the sputum culture is positive for a bacterial infection Complications ABGs o Hypoventilation of type II failure results in CO2 retention, acidosis, and ultimately, decreased PaO2; V/Q mismatch or diffusion defects of type 1 failure result in a decreased PaO2. Hypoxia and increased oxygen demand due to tachycardia may lead to dysrhythmias. A change in mental status may be an early indication of impending respiratory failure. Agitation is caused by hypoxemia. Somnolence is caused by hypercapnia. crackles (pulmonary edema) or rhonchi (pneumonia, COPD) or diminished or absent breath sounds (hypoventilation). Cyanosis may be visible in the nail beds and around the mouth in the initial stages of hypoxemia; as central cyanosis sets in, the body may take on a blue or gray tinge. A deep pink coloration to the skin is highly indicative of increased CO2 levels. Actions Administer oxygen (with humidity) as ordered. Supplemental oxygen is necessary to treat hypoxemia. Humidity helps to prevent mucosal drying and helps keep secretions thin so that they can be more easily coughed or suctioned up. Medication administration Administer bronchodilating medications as ordered. o Bronchial smooth muscle relaxants help open the airways. Administer steroids as ordered o Reduce inflammation; synergistic effect with bronchodilating agents (administer bronchodilator medications first, then inhaled steroids to allow the steroids to be inhaled more easily into the bronchial tree) Administer diuretics as ordered o Diuretics help decrease the pulmonary congestion that impairs ventilation. Administer sedation as ordered (typically only in mechanically ventilated patients) o Sedation helps decrease anxiety and agitation, helping to decrease the work of breathing and oxygen consumption. Elevate the head of the bed; sit the patient up in a chair. Position patient with the “good lung down. o positioning with the good lung down improves gas exchange by optimizing the V/Q ratio; gravity ensures the healthy lung maintains adequate blood flow to optimize ventilation to perfusion. Chest physical therapy and suctioning; ambulate as able o assisted coughing or suctioning help mobilize and clear secretions. Administer IV fluids/hydration o Decreases viscosity of secretions; helps maintain intravascular volume. Administer nutritional support o The patient’s metabolic needs must be met to promote healing. Be prepared for noninvasive or invasive positive-pressure ventilatory support. A severe V/Q mismatch may require the addition of positive pressure to adequately promote gas exchange. Teaching The patient should understand the risk factors and causes of acute respiratory failure and how to avoid future occurrences. Techniques such as pursed-lip breathing and diaphragmatic breathing allow for better alveolar ventilation and improve gas exchange. Aerobic exercise helps improve respiratory status. Hand washing and pneumococcal and influenza vaccinations help decrease the likelihood of infection adequate hydration helps ensure thin secretions. Smoking cessation