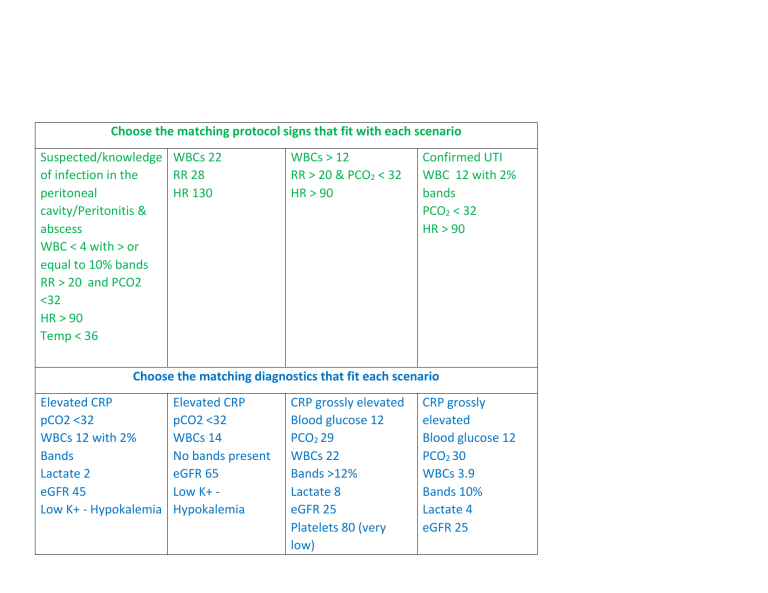
Choose the matching protocol signs that fit with each scenario Suspected/knowledge WBCs 22 of infection in the RR 28 peritoneal HR 130 cavity/Peritonitis & abscess WBC < 4 with > or equal to 10% bands RR > 20 and PCO2 <32 HR > 90 Temp < 36 WBCs > 12 RR > 20 & PCO2 < 32 HR > 90 Confirmed UTI WBC 12 with 2% bands PCO2 < 32 HR > 90 Choose the matching diagnostics that fit each scenario Elevated CRP pCO2 <32 WBCs 12 with 2% Bands Lactate 2 eGFR 45 Low K+ - Hypokalemia Elevated CRP pCO2 <32 WBCs 14 No bands present eGFR 65 Low K+ Hypokalemia CRP grossly elevated Blood glucose 12 PCO2 29 WBCs 22 Bands >12% Lactate 8 eGFR 25 Platelets 80 (very low) CRP grossly elevated Blood glucose 12 PCO2 30 WBCs 3.9 Bands 10% Lactate 4 eGFR 25 Low K+ Hypokalemia Low Mg+, PO4 hypomagnesia, hypophosphatemia Platelets 80 (very low) Low K+ Hypokalemia Low Mg+, PO4 hypomagnesia, hypophosphatemia Choose the expected assessment findings that fit each scenario BP 109/65 mmHg HR 108 bpm O 2 Sat 90% on 4L NP T 38.5 po RR 20/min A&O time 1, pain 9/10, Disorientated to place and time Decreased a/e bilateral bases, SOB Edema noted bilateral ankles Left > Right, Peripheral pulses weak, limbs cool to touch and pale, cap refill > 3 seconds Abd soft, BS present U/O 25 cc/hr BP 75/55 HR 130 O 2 Sat 91% on highflow 50% oxygen Temp 39 po RR 28 and shallow Disorientated Decreased a/e bilateral bases with coarse breath sounds bilateral mid lobe, O2sat 91% via face mask with 50% oxygen. Use of accessory muscles to breath Tachycardia, hypotension BP 110/60 mmHg HR 96 bpm O2 Sat 94% on 2L NP T 37.9 po RR 24/min A&O times 3, pain 9/10 Coarse crackles bilateral bases, slightly SOB Slight generalized peripheral edema, cap refill < 3 seconds, peripheral pulses bounding Abd firm and tender, no BS, no flatus U/O 40 cc/hr Skin flushed and warm to touch BP 80/64 mmHg HR 115 bpm O 2 Sat 91% on 5L NP T 35.4 po RR 24/min A&O time 2, pain 9/10 No a/e bilateral bases, a/e upper lobes only, SOB when trying to speak Family notice his hands and feet are swollen. Weak peripheral pulses, cap refill sluggish > 3 seconds, limbs cool despite major fluid resuscitation Peripheral mottling to lower limbs, cap refill > 3 seconds, pulses weak Abd frim and distended, BS absent, no flatus no urine output Skin cold and clammy, chills and rigorous (shaking with fever) to touch with peripheral mottling from knees to lower limbs bilateral Abd firm and distended with rebound tenderness, no BS, no flatus U/O 20 cc/hr Choose the best course of treatment that fit each scenario 1. Call RT and switch patient to O2 via face mask 2. Elevated HOB to maximize oxygenation 3. Monitor O2sat > Q1H 4. NS bolus 500 cc immediately 1. Call RT and physician 2. Continuously monitor O2sat & be ready to oxygenate via bag-valve mask 3. Another bolus of NS 500 cc and 1. Elevate HOB 30 degrees or >, Incentive spirometer and DB exercises 2. Reorient patient 3. Administer IV NS bolus 250 cc for low circulating volume 1. Continue to monitor oxygenation and support to keep O2 > 92% 2. Administer IV NS bolus 500cc for low circulating volume 5. Call physician for possible colloid (Albumin) administration & assessment for CT scan/surgery 6. Administer antibiotics 7. Change IV to NS with 20mEq KCL 8. Call ICU outreach for possible inotropic support if bolus doesn’t help BP & U/O or if oxygenation does not improve. call ICU outreach for inotropic medication 4. Balance elevation of HOB to maximize oxygenation but supine to support BP. 5. Administer antibiotics 6. IV would already have 20mEq KCL 4. Change IV to NS with 20mEq KCL 5. Administer antibiotics 6. Administer acetaminophen for fever 7. Assess Q1H for hypoxia, hypovolemia, fever, & oliguria 3. Assess Q1H for hypoxia, hypovolemia, fever, & oliguria 4. Change IV to NS with 20mEq KCL @150 cc/hr 5. Administer antibiotics as ordered