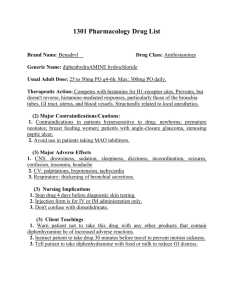
Study Guide for Pharmacology Exam 1: Test tips for all Anti-biotics in general: 1. Finish the whole medication – do not stop when the symptoms stop, and do not stop until all meds are gone 2. Accidental Pregnancies – the 3 C’s c – Child Care c – “-cillins” – Penicillin, Amoxicillin c – “-cyclines” – Doxycycline, Tetracycline *USE OTHER CONTRACEPTIVES* Oral contraceptives are ineffective 3. No Alcohol – ABX are hard on the liver, no added stress 4. No Food – MTF “Move The Food” M – Macrolids (Azithromycin) T – Tetracyclines (Doxycycline) F – Fluoroquinolones (Levofloxacin) Take on an empty stomach, increase fluids, and take one FULL glass of water on administration* 5. No Sun – Avoid “Fun The Sun” F – Fluoroquinolones – Levofloxacin’s T – Tetracyclines – Doxycycline’s S – Sulfa Drugs – SUN Burns 6. No Sun Sulfonylureas (Glyburide) Diuretics (thiazide/loops) Keys Words: Photosensitivity, Avoid “direct Sun exposure”, Wear sun block 7. Super Toxic (Kidneys + Ears) Vancomycin Gentamicin Neomycin *if too HIGH= KIDNEYS DIE Must draw a peak and trough *if too LOW = infections grow *MUST REPORT* Vertigo, tinnitus, Creatine over 1.3, BUN over 20, urine output less than 30* Sulfonamides: Fluoroquinolones: (Quinolones): Ex. Trimethoprim, Sulfamethoxazole (Bactrim) Ex. Levofloxacin (Levaquin), Ciprofloxacin, Norfloxacin MOA: Stops bacteria folic acid synthesis (Bacteriostatic) Indications: Frequently used for UTI’s Contraindications: Renal Disease, Pregnant women, and young children Adverse Effects: Steven Johnson Syndrome, Photosensitivity, Kidney Stone Development Memory Trick: S: Sun Burn (Sunblock & Avoid the sun) U: Urine (Crystals & Specific Gravity) (High and Drive) L: Lots of fluids (Water, 2 – 3L a day) F: Folic Acid (take this daily) Contraindications: - Allergies Glyburide (oral diabetic drug) Indications: Pneumonias & UTI (bactericidal) Contraindications: Children <18, Hx of tendonitis Memory Trick: -Floxacin = Fall – xacin, -floxacin= flex-acin Adverse Effects: GI upset, Tendon Rupture, Report Thrush Key points: - Avoid sun “direct sun exposure” Achilles tendons RUPTURES Report any and all muscle pain Contraindications: Tendonitis Not the same as a -MYCIN drug 1 hour BEFORE or AFTER meal Key Points: Not Pregnant safe, Increase Fluids, urine specific low, N/V/D Penicillin’s: Cephalosporins: Ex. Cephalexin (Keflex), Cefazolin, Ceftriaxone (Rocephin) -Cillin endings Ex. Cephalexin (Keflex), Cefazolin, Ceftriaxone (Rocephin) Indications for use: Broad spectrum, pregnancy and breast feeding safe Interactions: Alcohol, Antacids, Iron: Decreased absorption of ABX, take all separately Interactions: Methotrexate – increased electrolyte levels d/t decreased elimination Birth controls pills Warfarin – enhanced anticoagulation effects Will inactivate aminoglycoside Side Affects: GI Upset, Avoid use w/ patients who have hx of bleeding disorder or anticoagulant, Side Affects: N/V/D, Steven Johnson Syndrome, hives renal impairment, hypernatremia, hyperkalemia, superinfection, low platelets Nursing Implications: Take with water, Increased bleeding risk, use secondary birth control, take full dose Memory Trick: 3 C’s – Cross sensitivity, Ceph/Cef, Cillin During a Reaction: Stop, assess, epi - Diarrhea or other reaction: STOP DRUG Nursing Implications: Assess for allergy to Penicillin’s, give with food if stomach is upset, NO ALCOHOL up to 72 hours (Cefazolin and Cefotetan) Key points: Question the provider if they order a cephalosporin and they patient is allergic to penicillin’s, or other way around Macrolides: Tetracyclines: “-Thromycin” endings Ex. Tetracyclines, Doxycycline Ex. Azythromycin, Erythromycin Indications: Treatment of Rikettsia, Chlamydia, Lyme Disease, Syphilis, PID, Acne Indications: Broad Spectrum, URI/LRI, Lyme Disease, STI’s, Chlamydia, Mycoplasma, Pneumonia, Strep. Infections Interactions: Inhibits metabolism of digoxin = toxicity, monitor the levels, should not be taken clarithromycin & erythromycin = prolonged QT = malignant dysrhythmias Adverse Side Effects: Prolonged QT = could be cardiac arrest, Hepatotoxicity = monitor AST, ALT Nursing Implications: No Juice, only water, make sure that they have baseline cardiac and liver function tests, MONITOR EKG - Don’t give Tylenol = affects the liver double time Memory Tricks: Thromycin = throws ECG waves = “prolonged QT intervals” Interactions/Adverse Side Effects: Tooth Discoloration, superinfection (C. Diff), GI Upset, Photosensitivity, Hepatotoxicity Nursing Implications: Use second form of Birth control, take on empty stomach, MUST STI UP AFTER 30 MINS OF ADMINISTRATION – do not take dairy products, antacids, iron Memory Tricks: Cycling is dangerous – Not safe for a pregnant mother, BUGs in their teeth = discoloration, use sun block while on the cycling trip Key Points: - NOT pregnancy safe MUST USE OTHER BIRTH CONTORL Tooth Discoloration Sun Burns – Wear Sun Common Side Effects: N/V/D. Fever, Decreasing WBC = infection is working Aminoglycosides: Vancomycin: “-Mycin” Indications: Given for a serious infection like MRSA and C. Diff Ex. Gentamycin, Tobramycin, Neomycin Indications: Often used with other antibiotics, given parenterally, Cystic Fibrosis Interactions: Increased Nephrotoxicity, with other nephrotoxic drug, Increased ototoxicity with loop diuretics Side Effects: Nephrotoxicity (reversible), Ototoxicity (irreversible), tinnitus, feeling of fullness in ears, headache, skin rash Nursing Implications: Encourage Fluids, (> 3L/day unless contraindications), Assessment of baseline hearing and renal test, IMMEDIATELY REPORT S/S OF OTOTOXICITY, NEPHROTOXICITY = stop the drug - Draw serum levels 15 – 30 mins before next does Never mix with Penicillin’s/ Vancomycin Monitor the BUN and Creatinine Interactions: Renal Dysfunction, hearing loss, elderly & neonates - ETOH, Benzos, Ca Channel Blockers, Cyclosporine Side Effects: Rapid infusions can cause: Hypotension, Red Man’s Syndrome, ototoxicity, nephrotoxicity Nursing Implications: Adequate Hydration (2 L/24 hrs) = prevents nephrotoxicity, burns during admission, can cause thrombophlebitis – monitor IV site closely, may extravasate Key Points: Check 15 -30 mins before “next dose” or “administration” - Report and hold over 20 = vancomycin If the patient is having anaphylaxis o STOP, EPI RED MAN SYNDROME IS NOT ANAPHYLAXIS Metronidazole: Ex. Flagyl Indication: Anaerobic organism, GYN infections, P.O. to treat C. Diff, STI Interactions: ETOH, Lithium, Benzo, Cyclosporin, Ca+ Channel Blocker, Phenytoin, Phenobarbital (Seizures meds) Adverse Effects: Headache, Dizziness, NVD, Thrombocytopenia Nursing Implications: Baseline CNS, GI, GU, and ETOH Assessments Contraindications: Allergy, 1st trimester, caution in renal/cardiac/seizure disorders Key Points: Avoid ETOH during and 3 days after treatment, if patients do have ETOH = will have violent vomiting & cramping Normal Side Affects: - Dark Urine “Discoloration”, metallic tasting Deadly Side Affect: - Report any new rash or skin peeling Report Steven’s Johnson Syndrome Memory Trick: M – Metallic tasting (normal) E – ETOH AVOID T – Treats C .Diff & STI (Trichomoniasis) R – Rash or Skin Peeling O – Oh Not Dazzling (“Dazole”ing) Immunosuppressants: (Selectively Suppresses T Lymphocytes) Azathioprine (Imuran)/ Cyclosporine (Sandimmune): Methotrexate: MOA: Blocks cell regrowth, and proliferation MOA: Stops folic acid metabolism which stops cell reproduction Indications: To prevent Organ Transplant Rejection Indications: Rheumatoid Arthritis (Body attacking its own joints) Precaution: Before giving this med: Adverse Effects: Low Immunity = Infections, Low Platelets = Serious Bleeding, Fetal Death while pregnant Nursing Implications: - No pregnancy No crowds or LIVE vaccines No Razors or brushing teeth hard Key Points: - - Infection Risk o Avoid Crowds o Avoid Fresh Fruit and Flowers Thrombocytopenia (Platelets under 100,000) Men … no trying for a baby until 3 months after treatment is complete - Check WBC & Platelet Report Leukopenia (<4000) Monitor for bleeding (Thrombocytopenia) No babies (use other contraceptives) Common Side Effects: Cyclosporine, Gingival Hyperplasia Nursing Implications: - Avoid Crowds No Live Vaccines (Herpes + Shingles) Soft Bristles toothbrush Use contraceptives Immunomodulators: Monoclonal Antibodies: Varied throughout the types of antibodies (ends in -mab’s) Adverse Effects: Hypersensitivity, Flu like symptoms – Flu like, Capillary Leak syndrome = low BP, Black Box Warning: Serious infection, lymphoma, malignancy, allergic reaction is common - Uncommon: Hepatotoxicity, Bone Marrow Suppression, CNS effects Nursing Implications: Pre-medicate with Benadryl, and Antihistamine Ex. Adalimumab - Acts on the TNF [Tumor Necrosis Factor] (Crohn’s, RA, and Psoriasis) Ex. Certolizumab (Crohn’s, RA) - TNF antagonist Ex. Infliximab - Acts on the TNF (Crohn’s, RA, and Psoriasis, Ulcerative Colitis) - Contraindicated: Heart Failure - Black Box Warning: Fatal = TB, Fungal Interactions Ex. Natalizumab - Blocks proteins on WBC (MS) Ex. Rituximab - Binds to B cells and causes lysis - MUST PREMEDICATE w/ Benadryl, and antihistamine Monoclonal Antibodies: Nursing Implications: - Assess for cautions (infections), and other contraindications first Assess for hypersensitivity o See if it is necessary to pre-medicate first TB Test first INFECTION IS KEY Systemic Lupus: Chronic Multisystem inflammatory autoimmune disease Affects: Skin, Joins, Serous Membranes (Pleural spaces around the lungs, and the heart), Renal System, Hematologic system, Neurologic system Etiology: UV Light, Stress, Chemicals, Toxins, Infections Pathophysiology: Autoimmune reaction – autoantibodies attack nucleic acids, erythrocytes, coagulation proteins lymphocytes, platelets, & other cells (Type III hypersensitivity reaction) Treatment: NSAIDS = arthritis Antimalarial Agents: Hydroxychloroquine (Plaquenil) Used to treat fatigue, skin and joint complications May take months to see (+) effects May prevent flares Side effects: Retinopathy and visual changes (Blurry, Vision changes) Must have eye exams Q6 months Immunosuppressants: Methotrexate (meth-no-trexate) Prescribed in combination with folic acid to help decrease the side effects of corticosteroid therapy Side Effects: Infection Azathioprine (Imuran) Cyclophosphamide (Cytoxan) Belimumab Monoclonal antibodies – work on the B lymphocytes Must premedicate with reaction Contraindications: Cannot use if: Breastfeeding, severe renal disease, CNS manifestations of SLE, depression, active infection (like TB infection) (No live vaccines) Active vs. Passive Immunity: Active: Passive: Definition: Exposure of the body to the associate disease antigen Definition: The host is given the ability to fight off an invading microorganism Type of: Toxoid or vaccine Type of: Immunoglobulin or Antitoxin Artificial: Exposure to the vaccine Artificial: Person is inoculated with serum containing immunoglobulins obtained from other humans or animals- antibodies already prepared for the host, the host doesn’t always have to make them Ex. Flu, Herpes Zoster, Chickenpox, rubella Natural: Immunity by surviving the disease Ex. Hep B, Rabies, tetanus, Varicella, Antivenin Natural: Mom to baby via breast milk, or bloodstream via placenta First line of defense – Innate immunity (Physical, mechanical, biomechanical barriers) Second line of defense – Inflammation (Mast cells continuously searching – which if they find something they then release an antihistamine or WBC to the site) Third line of defense – Adaptive (acquired) (Specific) immunity HIV: Hard virus to kill due to the virus living within the cell itself Key Characteristics of antiviral drugs: - Able to enter the cells infected with virus Some drugs stimulate the body’s immune system Antiviral drugs are in patients with competent immune systems A health immune system works synergistically with the drug to eliminate or suppress viral activity Best Medications never fully eradicate the virus: - Host immune system has a better chance of controlling or eliminating when virus cannot replicate Pathophysiology of HIV: 1. Virus bends to specific CD4 receptors to enter the T-cell (Fusion) 2. Reverse transcriptase (which is the enzyme that is brought along with the HIV virus) assists to make viral DNA from RNA a. Viral DNA enters host cell nucleus and splices itself into genome permanently (Integrase) b. Protease, puts “pieces together” for the final viral cell 3. Consequences of integration into genetic structure a. All daughter cells are infected, viral DNA will direct cell to make HIV Antiretroviral Drugs: Fusion Inhibitors - Inhibit viral fusion, preventing viral replication o Ex. Enfuvirtide (Fuzeon) MOA: Supress the fusion process Contraindication: Severe Allergy or intolerable toxicity Form: Injectables Entry Inhibitor – CCR5 - Block entry into the cell o Ex. Maracviroc (Selzentry) MOA: Block entry into cell wall Contraindications: Severe Drug allergy ADE: Hepatotoxicity (Assess LFT’s) Form: PO only Reverse Transcriptase inhibitors (RTI’s) - - Blocks activity of the enzyme reverse transcriptase, preventing production of new viral DNA Nucleoside reverse transcriptase inhibitors (NRTI’s) o Ex. Zidovudine (Retrovir) (Azidothymidine) *FIRST LINE OF TREATMENT* MOA: Block the enzyme ADE: Bone Marrow Suppression (high risk for infection) (May need to switch the drug) Patient Education: given during pregnancy to prevent transmission to fetus/infants MUST SIT UPRIGHT AFTER 30 MINS AFTER TAKING THE MEDICATION o Ex. Tenofovir (Viread) MOA: Block the enzyme (Reverse transcriptase) Contraindications: Liver dx, Bone marrow suppression (Decrease RBC, Decrease WBC, Decrease Platelets) ADE: Lactic acidosis, hepatomegaly Form: Oral Nonnucleoside Reverse Transcriptase Inhibitors (NNRTI’s) o Ex. Nevirapine (Viramune) MOA: Inhibit the action of reverse transcriptase ADE: Rash, Fever, Nausea, Headache, LFT Elevation (Hepatoxicity) Patient Education: Use with NRTI’s Form: PO Protease Inhibitors (PI’s) - Inhibit the protease retroviral enzyme, preventing viral replication o Ex. Indinavir (Cixivan) & Ritonavir (Norvir) MOA: Inhibits protease enzyme, which prevents viral replication Contraindications: Pancreatitis, Liver Dx, diabetes Adverse Desired Effects: Nephrolithiasis (Drinks lots of fluids), N/V/D, Lipodystrophy (Insulin Resistance) Form: PO, EMPTY STOMACH Patient Education: Use other forms of contraception’s HIV integrase strand transfer inhibitors (Integrase inhibitors) - Blocks the function of integrase o Ex. Raltegravir (Isentress) MOA: Bind with integrase enzyme and prevent HIV from incorporating its genetic material into the host Contraindications: Severe Allergy and intolerable toxicity ADE: Muscle myopathy, rhabdo Form: PO Nursing Implications for all HAART Drugs: - Patients will require lifelong therapy o If the patient develops resistance -> change the combo of drugs up All drugs must be given at evenly spaced intervals, Around the clock to ensure a steady state Asses for contraindications, conditions that may indicate cautious use, and potential drug interactions THESE DRUGS ARE NOT CURES; THEY ARE ONLY TO HELP MANAGE SYMPTOMS Cancer: Malfunction of genes that control growth/differentiation Stages: Initiation – DNA mess up w/ radicals, Chemicals, sun, Tabaco products Tumor must reach a critical mass that can be detected (1 cm on palpation, 0.5 cm by radiologic test) Promotion – Proliferation w/ growth of cells, and substation of apoptosis (programmable cell death) Reversible proliferation of altered cells, and this gets promoted by: Dietary fats, obesity, tobacco, ETOH This means they person needs lifestyle medications Progression – Cancer cells are good with angiogenesis (creating their own vascular system/ blood supply) Increase in growth rate & invasiveness, metastasis Tumor develops its own blood supply Cells detach from the tumor and invade surrounding tissues Penetrate lymph & blood vessels = metastasis o Common Areas: Liver Bone Brain Lung Adrenal Glands TNM Classification of Cancer: Chemotherapy Treatment: - Chemotherapy is a combination of multiple drugs The most affected drugs are those that are rapidly dividing cells o Hair Follicles o Lining of the GI tract o Bone Marrow Contraindications - Very rare to have absolute contraindications Premedication is relevant for people with allergies Low WBC (Infections) Severe nutritional compromises & dehydration Impaired renal, hepatic, or other major organ functions Having a high neutrophil count (<500 cells) o No fresh flowers, fruits, crowds Caring for patients that have chemo drugs in their system: - Double flushing of bodily fluids in the commode Special hampers for disposal of all objects that encounter patients’ bodily fluids Personal Protective equipment Special procedure if liquid spills Common ADE: - Women need to use other forms of contraception’s that are not drugs Erythema/hyperpigmentation Alopecia Monitor weight loss SMALL, FREQUENT, HIGH PROTEIN, HIGH CALORIC MEALS N/V/D (Puts the patient in metabolic alkalosis) (give the patient an antiemetic) BONE MARROW SUPRESSION o Anemia o Leukopenia o Thrombocytopenia o NADIR (first 7 – 10 days after initiation of treatment, the patient is most immunosuppressant EXTRAVASATION: If suspected: Stop the infusion immediately, but do not remove the IV, some IV antidotes will be given in that same space that the catheter was in Cell Cycle Specific Drugs: Methotrexate (Antidote – Leucovorin) MOA: inhibit cell growth through interfering with folic acid synthesis Contraindications: NO PREGNANCY ADE: Sever Bone Marrow Suppression Cell Cycle Non-Specific Drugs: Cyclophosphamide (Cytoxan) – Bone Marrow Suppression, increased risk of bleeding (monitor Urine output), and H&H [hemorrhagic cystitis] Cisplatin (Platinol) = Renal Toxicity (monitor kidney damage, Creatine <1.3, BUN <20, Urine output >30), ototoxicity (vertigo, balance problems) ADE: Alopecia, GI effects, BMS, Extravasation