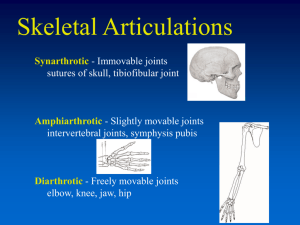
Anterior Cruciate Ligament Injury Yabut & Geografo BASIC ANATOMY 3 Bones: Femur, Tibia & Patella 3 Joints: Tibiofemoral Joint (Knee joint) Patellofemoral Joint Superior Tibiofibular Joint 2 Condyles: Lateral Femoral Condyle Medial Femoral Condyle 2 Meniscus: Medial Meniscus Lateral Meniscus Ligaments 1. Arcuate Ligament 2. Oblique Popliteal Ligament 3. Patellar Ligament 4. Coronary Ligament 5. Ligament of Humphrey(Anterior Meniscofemoral ligament) 6. Ligament of Wrisberg(Posterior Meniscofemoral ligament) Anterior Cruciate Ligament Origin: Anterior spine Insertion: Lateral condyle Description: Oblique & longer Orientation: Posterior, lateral, superior Location: Intracapsular Extrasynovial CKC: Prevent anterior displacement of tibia on the femur; posterior displacement of femur on the tibia Injuries: Hyperextension, Loading on extended knee Kinesiology Screw home mechanism (SHM) of knee joint is a critical mechanism that plays an important role in terminal extension of the knee. 1. There is an observable rotation of the knee during flexion and extension. 2. This rotation is important for healthy movement of the knee. 3. During the last 30 degrees of knee extension, the tibia (open chain) or femur (closed chain) must externally or internally rotate, respectively, about 10 degrees. 4. This slight rotation is due to inequality of the articular surface of femur condyles. 5. Rotation must occur to achieve full extension and then flexion from full extension. UNHAPPY TRIAD OF O’DONOGHUE 1. Rupture of the ACL 2. Tear of the medial meniscus 3. Rupture of the superficial tibial collateral ligament and the deep capsular ligament / medial collateral ligament injury Muscles Knee Extensors ● ● ● ● Rectus femoris Vastus lateralis Vastus medialis Vastus intermedius Knee Flexors ● ● ● Biceps Femoris Semimembranosus Semitendinosus Knee Rotators(Medial) ● ● Popliteus SGT Sartorius, Gracilis, Semitendinosus Knee Rotators(Lateral) ● ● Biceps Femoris Tensor Fascia Latae Epidemiology Very common disabling event among athlete or worker 70% ACL tears during sports 15-45 yr - highest risk, active people especially in sports Women > Men Etiology >Anterior blow to tibia, resulting in knee extension >Torn by extreme valgus or varus forces after failure of the medial/lateral ligament complex has occurred. >Non-contact 70% of the cases: by doing a wrong movement. >Sudden pivoting or cutting maneuver during sporting activity, which is commonly seen in football, basketball and soccer >Landing awkwardly from a jump >Tear due to work injuries or automobile accidents. Mechanism: combination of hyperextension and rotation. Pathophysiology The ACL receives a rich blood supply, primarily from the middle geniculate artery, so when the ACL is ruptured, a haemarthrosis usually develops rapidly. However, despite its intra-articular location, the ACL is actually extrasynovial. Due to the poor intrinsic healing properties of the ACL, a torn ACL will not heal on its own. Over time, the damaged fibres may scar down to the posterior cruciate ligament or to the intercondylar notch Signs and symptoms - Hear a “pop” accompanied by sharp lateral pain Minimal swelling because the ligament is not attached to the joint capsule. Subtle instability (+) varus test 30 of flexion should confirm damage to the ligament (+)avulsion fx of peroneal nerve injury if tenderness is detected on head of fibula. - Usually associated with abnormal forward movement of the tibia on the femur - Loss of ROM Possible Complication anterior knee pain extensor mechanism/patellar dysfunction long-term quads weakness patellar fx patellar tendon rupture. Differential Dx ● ● ● ● Knee dislocations. Meniscal injuries. Collateral ligaments injury. Posterolateral corner injuries to the knee. Diagnostic procedure MRI Radiographs Laxity Testing Dynamic Ultrasonography SPECIAL TESTS - LACHMAN TEST, ANTERIOR DRAWER TESTS PROGNOSIS MEDICAL / SURGICAL MANAGEMENT >Non-operative: Lifestyle changes and avoid activities that cause recurrent instability Aggressive rehab. Functional knee brace >Surgical Arthroscopic Reconstruction Graft options • Autografts (patellar tendon & hamstring tendon) • Allografts • synthetic > Medical Management Nonsteroidal anti-inflammatory drugs (NSAIDs)- ibuprofen Opioid analgesics-codeine Interventions Maximum protection phase (early days, 1-4 days) PRICE, gait training, PROM/AAROM, patellar mobilization, muscle setting, assisted SLRs, ankle pumps. (Late, weeks 2-4) Continue early interventions, progress to full weight-bearing, SLRs in 4 planes, low load PRE, initiate open-chain knee extension, trunk/pelvis stabilization and aerobic conditioning. Moderate protection phase (early: weeks 5-6) multiple angle isometrics, advanced closed chain strengthening and PRE, LE stretching program, endurance training, proprioceptive training, stabilization exercises (late: weeks 7-10) continue early interventions, advance strengthening, endurance and flexibility, advance proprioceptive training to high speed stepping drills, unstable surface challenge drills, and balance beam, initiate a walk/jog program at the end of this phase, initiate plyometric drills. Minimum protection phase (weeks 11-24) continue LE stretching program, advance PRE/initiate isokinetic training, advance closed-chain exercise, plyometric drills, advance proprioceptive training, progressive agility drills, simulated work or sport-specific endurance training, progress running program. Return to activity phase Continue to progress PRE drills and flexibility exercises, advance agility drills, advance running drills, implement drills specific to sport or occupation, determine the need for protective bracing prior to return to sport or work.