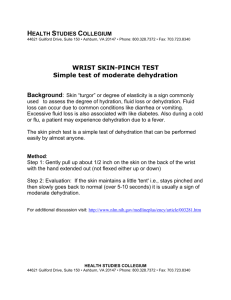
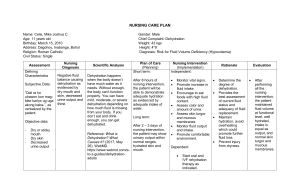
MOST COMMON TREATMENTS: 1. Increasing Fluid Intake 2. Clear fluids, water, clear - broths, frozen water/ice pops, sports drinks 3. Avoid Caffeine - INTERVENTIONS: 1. 2. 3. 4. 5. Hydration management involves both acute and ongoing management of oral intake Oral rehydration therapy is the first treatment approach Calculate daily fluid goal Compare current intake to fluid goal to evaluate hydration status Plan for at risk individuals - Serum osmolarity reading >300 mOsmol/L Elevated BUN (can also be elevated from other may other causes. Not always accurate) Urine color and osmolarity should not be used to determine dehydration in the elderly because they are no specific enough Changes in urine pattern and color should be noted DEHYDRATION IN ELDERLY WHAT SHOULD YOU DO! 1. Plan to drink at least a cup of fluid SHOULD every 1-2 hours WHAT YOU DO! 2. 1. 3. 2. 4. 3. Drink a total of 8-12 cups per day Plan to drink at least a cup of Keep water1-2 bottle throughout fluid every hours the day Drink a total of 8-12 cups per Avoid day alcohol and caffeine Keep water bottle throughout the day NISA HASKELL, STEPHANIE MARTIN, VALERIE MURPHY, ASMA NAIMI Age Related Changes That Affect Hydration Thirst sensation diminishes Loss of muscle mass in proportion to fat cells. (Fat cells have less water than muscle cells.) - Total body water decreases Kidneys can’t concentrate urine - In the elderly dehydration is commonly associated with other underlying diseases. (Ex. Diabetes, heart conditions, respiratory diseases) Studies show 1/2 of long-term care patients are dehydrated as well - Signs and Symptoms of Dehydration 1. 2. 3. 4. 5. 6. Dry mucous membranes in mouth & nose Speech incoherence Rapid pulse Sunken eyes Extremity weakness Decrease in skin turgor - not always reliable in the elderly for checking dehydration because of the thinning and decrease in elasticity of skin Difficulties with communicating needs and wants, immobility, and decreased appetites contribute to dehydration in long term care facilities Risk Factors for Dehydration in Elders 1. Use of more medications 2. Delirium 3. Thromboembolic complications 4. Infections 5. Kidney stones 6. Constipation 7. Falls 8. Renal failure 9. Seizures Dehydration - Dehydration – A condition caused by loss of too much fluid from the body. - Occurs when you lose more fluids than you are taking in, and your body does not have enough fluids to work properly. Types of Dehydration 1. Water-loss Results from insufficient fluid intake which leads to elevation of serum osmolarity and drop in extracellular fluid volume 2. Volume depletion Salt loss Occurs from excess fluid loss (diarrhea/vomiting) Serum osmolarity – stable or decreases slightly 10. Delayed wound healing