Fungal Infections: Actinomycosis & Aspergillosis Lecture Notes
advertisement
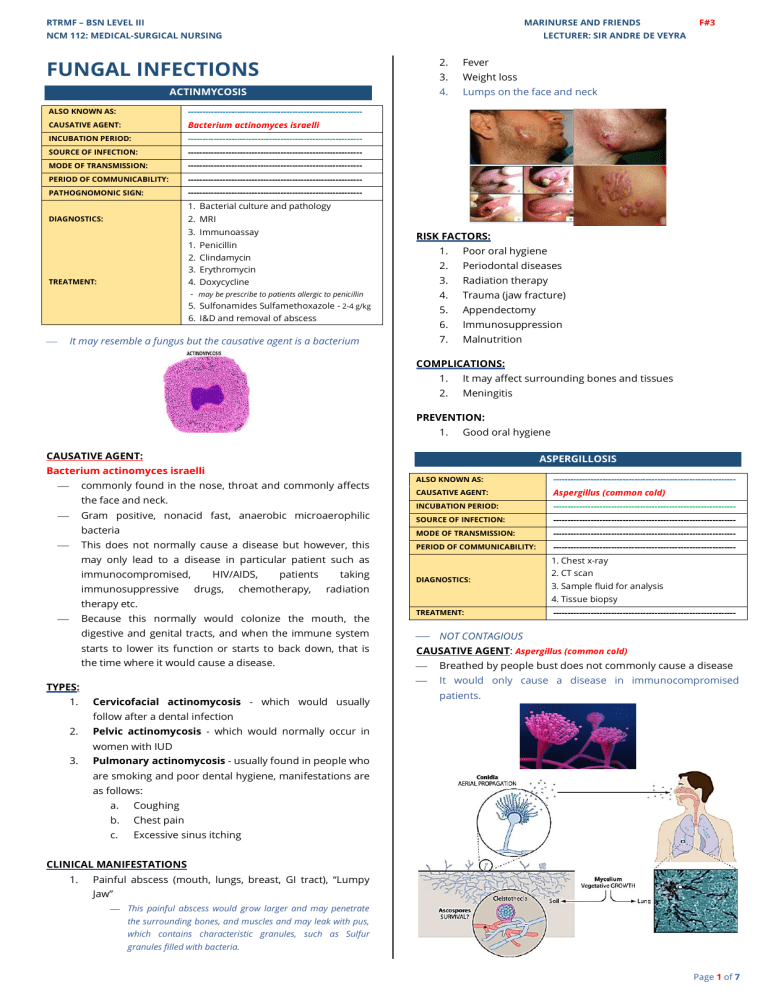
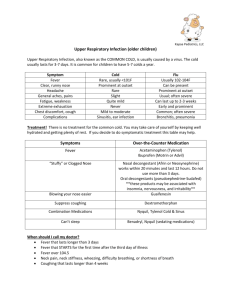
RTRMF – BSN LEVEL III MARINURSE AND FRIENDS NCM 112: MEDICAL-SURGICAL NURSING F#3 LECTURER: SIR ANDRE DE VEYRA FUNGAL INFECTIONS ACTINMYCOSIS ALSO KNOWN AS: ------------------------------------------------------------ CAUSATIVE AGENT: Bacterium actinomyces israelli INCUBATION PERIOD: ------------------------------------------------------------ SOURCE OF INFECTION: ------------------------------------------------------------ MODE OF TRANSMISSION: ------------------------------------------------------------ PERIOD OF COMMUNICABILITY: ------------------------------------------------------------ PATHOGNOMONIC SIGN: ------------------------------------------------------------ 2. Fever 3. Weight loss 4. Lumps on the face and neck 1. Bacterial culture and pathology 2. MRI DIAGNOSTICS: 3. Immunoassay 1. 2. 3. 4. 5. 6. TREATMENT: RISK FACTORS: Penicillin Clindamycin Erythromycin Doxycycline may be prescribe to patients allergic to penicillin Sulfonamides Sulfamethoxazole - 2-4 g/kg I&D and removal of abscess It may resemble a fungus but the causative agent is a bacterium ⎯ 1. Poor oral hygiene 2. Periodontal diseases 3. Radiation therapy 4. Trauma (jaw fracture) 5. Appendectomy 6. Immunosuppression 7. Malnutrition COMPLICATIONS: 1. It may affect surrounding bones and tissues 2. Meningitis PREVENTION: 1. Good oral hygiene CAUSATIVE AGENT: ASPERGILLOSIS Bacterium actinomyces israelli commonly found in the nose, throat and commonly affects ⎯ the face and neck. Gram positive, nonacid fast, anaerobic microaerophilic ⎯ bacteria This does not normally cause a disease but however, this ⎯ ALSO KNOWN AS: --------------------------------------------------------------- CAUSATIVE AGENT: Aspergillus (common cold) INCUBATION PERIOD: --------------------------------------------------------------- SOURCE OF INFECTION: --------------------------------------------------------------- MODE OF TRANSMISSION: --------------------------------------------------------------- PERIOD OF COMMUNICABILITY: may only lead to a disease in particular patient such as immunocompromised, immunosuppressive HIV/AIDS, drugs, patients chemotherapy, taking radiation therapy etc. Because this normally would colonize the mouth, the ⎯ digestive and genital tracts, and when the immune system starts to lower its function or starts to back down, that is the time where it would cause a disease. TYPES: 1. Cervicofacial actinomycosis - which would usually --------------------------------------------------------------1. Chest x-ray DIAGNOSTICS: 2. CT scan 3. Sample fluid for analysis 4. Tissue biopsy TREATMENT: ⎯ --------------------------------------------------------------- NOT CONTAGIOUS CAUSATIVE AGENT: Aspergillus (common cold) ⎯ Breathed by people bust does not commonly cause a disease ⎯ It would only cause a disease in immunocompromised patients. follow after a dental infection 2. Pelvic actinomycosis - which would normally occur in women with IUD 3. Pulmonary actinomycosis - usually found in people who are smoking and poor dental hygiene, manifestations are as follows: a. Coughing b. Chest pain c. Excessive sinus itching CLINICAL MANIFESTATIONS 1. Painful abscess (mouth, lungs, breast, GI tract), “Lumpy Jaw” ⎯ This painful abscess would grow larger and may penetrate the surrounding bones, and muscles and may leak with pus, which contains characteristic granules, such as Sulfur granules filled with bacteria. Page 1 of 7 RTRMF – BSN LEVEL III MARINURSE AND FRIENDS NCM 112: MEDICAL-SURGICAL NURSING LECTURER: MR. ANDRE CARLO DE VEYRA TYPES: 1. 6. Cutaneous or Skin Aspergillosis - which may enter in Allergic bronchopulmonary aspergillosis (ABPA) the break of skin integrity. - undergone surgery, burns Inflammation of the lungs and allergy symptoms such as: 7. a. Coughing F#3 Examples: People who Invasive Aspergillosis ⎯ serious infection b. Wheezing ⎯ affects immunocompromised people c. SOB ⎯ Affects the lungs but also spread to other parts of d. Fever the body • RISK FACTORS: a. Fever a. Cystic fibrosis b. Chest pain b. Asthma c. Cough • Aspergilloma- is a fungus ball that colonizes in a d. Hemoptysis healed lung scar or abscess from a previous disease. e. SOB • AT RISK: a. Chemotherapy b. Organ transplant c. High doses of corticosteroids 2. Allergic Aspergillus Sinusitis - causes inflammation in the sinuses and symptoms such as: a. Drainage b. Stuffiness c. Rhinorrhea d. Headache e. Reduced ability to smell 3. Azole-Resistant Aspergillus Fumigatus - One species of aspergillus fumigatus will become resistant to certain medicine used in the treatment 4. Aspergilloma - ball of aspergillus grown in lungs or sinuses, does not spread to other part of the body a. Cough b. Hemoptysis c. SOB DIAGNOSTIC TESTS • Risk factor: TB 5. Chronic Pulmonary Aspergillosis ⎯ Causes cavities in the lungs ⎯ Aside from formation the found in ball the lungs, there may be, or it may lead to cavities in the lungs. This happens in commonly long term aspergillosis (3 months or more)”. Aspergilloma may also be present. a. Weight loss b. Cough c. Hemoptysis 1. Chest x-ray 2. CT scan 3. Sample fluid for analysis 4. Tissue biopsy - for microscopic exam or fungal culture MANAGEMENT: 1. Discontinue immunosuppressive drugs 2. Severe cases may need surgery PREVENTION: 1. Avoid areas with a lot of dust 2. Avoid activities with close contact to soil or dust (wear mask or gloves) 3. Clean injury with soap and water d. Fatigue e. SOB • RISK FACTORS: a. TB b. COPD c. Sarcoidosis Page 2 of 7 RTRMF – BSN LEVEL III MARINURSE AND FRIENDS NCM 112: MEDICAL-SURGICAL NURSING LECTURER: MR. ANDRE CARLO DE VEYRA BLASTOMYCOSIS ALSO KNOWN AS: --------------------------------------------------------------- CAUSATIVE AGENT: Blastomyces INCUBATION PERIOD: 3 weeks – 3 months SOURCE OF INFECTION: --------------------------------------------------------------- F#3 • Severe blastomycosis - Can spread to the skin, bones, joints, CNS (brain and spinal cord) Breathing microscopic fungal spores from the MODE OF TRANSMISSION: air after participating in activities that disturb the soil, exposed to decomposing material such as wood, leaves etc. PERIOD OF COMMUNICABILITY: --------------------------------------------------------------- PATHOGNOMONIC SIGN: --------------------------------------------------------------History, symptoms, and PE; Chest X-ray; CT DIAGNOSTICS: scan of the lungs; Tissue biopsy; Culture of fluid from respiratory tract; Blastomyces Urine Antigen TREATMENT: ⎯ 1. Itraconazole- for mild to moderate cases (200 mg tid for 3 days, 200 mg OD or bid for 6-12 mos) 2. Antifungal- may last 6 mos-1 year 3. Amphotericin B- for severe cases Like aspergillosis, it is NOT CONTAGIOUS. COMPLICATIONS: 1. Brain abscess 2. Epidural abscess 3. Meningitis 4. Bone lesions 5. Genital lesions (epididymal swelling, deep perineal discomfort, and prostatic tenderness) CAUSATIVE AGENT: BLASTOMYCOSIS Blastomyces ⎯ commonly live in moist soil and commonly found in ALSO KNOWN AS: SAN Joaquin Fever, Valley Fever decomposing matters such as wood or leaves. CAUSATIVE AGENT: Coccidiodes immitis, Coccidiodes posadassii INCUBATION PERIOD: 1-3 weeks SOURCE OF INFECTION: --------------------------------------------------------------Breathing microscopic fungal spores from the MODE OF TRANSMISSION: air after participating in activities that disturb the soil TRANSMISSION: Breathing microscopic fungal spores from air after participating in activities that disturb the soil, exposed to PERIOD OF COMMUNICABILITY: --------------------------------------------------------------- PATHOGNOMONIC SIGN: --------------------------------------------------------------Enzyme immunoassay, Immunodiffusion, DIAGNOSTICS: 1. Fever (common) 2. Cough 3. Night sweats 4. Myalgia 5. Arthralgia 6. Chest pain 7. Fatigue 8. Extrapulmonary (disseminated blastomycosis) painless abscess (1 mm diameter or more, as lesion enlarge the center of the lesion will heal forming “Atrophic scar’, which would lead to elevated patch more than or equal to 2 cm wide with an abruptly slopping purplish red abscess scalded border.) Culture- tissue & respiratory specimens, Urinary antigen detection, PCR decomposing material such as wood, leaves etc. CLINICAL MANIFESTATIONS Complement fixation (CF), Lateral flow assay, TREATMENT: ⎯ ⎯ ⎯ ⎯ Antifungal (Disseminated) Fluconazole Amphotericin B History: It was first found in San Joaquin Valley (California) May spread via pulmonary or hematogenous route; inhalation of airborne arthroconidia Endemic to the US, Mexico, South America, Arizona, California’s Southern San Joaquin Valley Usually it may be benign, asymptomatic, self-limiting respiratory infection RISK FACTORS: 1. Immunocompromised 2. Pregnant 3. Diabetes Mellitus 4. Filipino or a person of color DIAGNOSTIC TESTS 1. Enzyme immunoassay- wherein we will be able to detect specific IgM and IgG antibodies 2. Immunodiffusion- through this we are able to identify IgM antibodies, which are positive during the early course of infection. Helpful in detecting infection during its early stage. Not definitive. 3. Complement fixation (CF)- where you can find IgG 4. Lateral flow assay 5. Culture - tissue and respiratory specimens 6. Urinary antigen detection 7. Polymerase Chain Reaction (PCR) CLINICAL MANIFESTATIONS Page 3 of 7 RTRMF – BSN LEVEL III MARINURSE AND FRIENDS NCM 112: MEDICAL-SURGICAL NURSING LECTURER: MR. ANDRE CARLO DE VEYRA F#3 1. Fatigue DIAGNOSTICS 2. Cough 1. Antigen detection in urine and serum 3. Dyspnea 2. Antibody test – (2 to 6 weeks after acquiring) 4. Headache 3. Culture - (Tissue, Blood, Body Fluids. It takes 6 weeks to 5. Night sweats 6. Myalgia 7. Rash be positive after acquiring the disease, initially it will not be positive, the wait for 6 weeks) 4. Microscopy – (low sensitivity, but can provide quick diagnosis) 5. PCR CLINICAL MANIFESTATIONS 1. HISTOPLASMOSIS ALSO KNOWN AS: --------------------------------------------------------------- CAUSATIVE AGENT: Histoplasma capsulatum INCUBATION PERIOD: 3 – 17 days RESERVOIR: MODE OF TRANSMISSION: Soil, heavily contaminated with bird or bat droppings Inhalation of airborne microconidia after disturbance of contaminated material PERIOD OF COMMUNICABILITY: --------------------------------------------------------------DIAGNOSTICS: TREATMENT: Antigen detection in urine and serum; Antibody test- (2-6 weeks after acquiring); Culture; Microscopy; PCR 1. Mild to moderate cases – may resolve without treatment 2. Amphotericin B (severe acute pulmonary or chronic disseminated cases, with CNS involvement) 3. Itraconazole (mild to moderate cases or as step down) A. Primary pulmonary – self-limiting B. Disseminated – bones, joints, soft tissue and meninges involvement COMPLICATIONS 1. Progressive, chronic, or disseminated disease 2. Meningitis 3. Diffuse lung disease- HIV patients - People who developed Coccidiomycosis might develop immunity after Acute pulmonary histoplasmosis a. Fever b. Malaise c. Cough d. Headache e. Chest pain f. Chills g. Myalgia ⎯ Patients with history of pulmonary disease are at risk for Chronic Histoplasmosis and that may lead to Disseminated Histoplasmosis – which involve already other parts of the body COMPLICATIONS 1. Pericarditis 2. Broncholithiasis 3. Pulmonary nodules 4. Mediastinal granuloma 5. Mediastinal fibrosis - Those with history of pulmonary disease may develop pulmonary or disseminated histoplasmosis TREATMENT 1. Mild to moderate cases – may resolve without treatment 2. Amphotericin B (severe acute pulmonary or chronic disseminated cases, with CNS involvement) 3. Itraconazole (mild to moderate cases or as step down) (Step Down meaning tapos na sya sa Amphotericin B then we want to continue the treatment for a longer period of time, then we will step down from infection. Amphotericin B to Itraconazole) MUCORMYCOSIS ALSO KNOWN AS: Previously called Zygomycosis Molds belonging to the order Mucorales CAUSATIVE AGENT: Rhizopus species. mucor species Cunninghamella bertholletiae, Apophysomyces INCUBATION PERIOD: 3 – 17 days RESERVOIR: Soil MODE OF TRANSMISSION: PERIOD OF COMMUNICABILITY: ⎯ Inhaled, then got into the lungs and travels to the lymph. DIAGNOSTICS: HIV 2. Organ transplant 3. Immunosuppression 4. Infants 5. More than 55 years old from the Environment --------------------------------------------------------------Histopathological evidence culture specimen from a or positive culture of nonsterile sites (sputum) – DEFINITIVE RISK FACTORS 1. Inhalation, Inoculation, Ingestion of Spores TREATMENT: 1. Amphotericin B - first line treatment 2. Posaconazole, isavunconaxole 3. Surgical debridement or resection of infected tissue Page 4 of 7 RTRMF – BSN LEVEL III MARINURSE AND FRIENDS NCM 112: MEDICAL-SURGICAL NURSING LECTURER: MR. ANDRE CARLO DE VEYRA HEALTH CARE RELATED OUTBREAKS ⎯ From Adhesive Bandage, b. wooden F#3 Secondary tongue depressors, ⎯ Pathogen spread hematogenously hospital linens, negative pressure rooms, water leaks, poor ⎯ Lesions are erythematous, indurated, painful air filtration, non-sterile medical devices cellulitis, then progress to an ulcer covered with black eschar COMMUNITY ONSET OUTBREAKS 4. ⎯ Trauma associated with Natural Disasters (meaning after bagyo, hurricane, etc. then this may erupt) GI Mucormycosis ⎯ Less common ⎯ Non-specific abdominal pain, distention, nausea and vomiting, GI bleeding RISK FACTORS ⎯ It is common on patients who are malnourished and 1. Uncontrolled DM 2. Malignancy 3. Organ or hematopoietic transplant 4. Prolong corticosteroid therapy 5. Skin trauma 6. IV drug use 7. Malnourishment Pulmonary 8. Premature and LBW infants mucormycosis, then may proceed to Disseminated premature infants. Affected parts are the stomach, colon, and most of all the ileum is the most affected 5. Disseminated ⎯ Common in neutropenic patients with pulmonary infection ⎯ It may start first as Rhinocerebral Mucormycosis, Mucormycosis or any forms of Mucormycosis CLINICAL FORMS 1. ⎯ Rhinocerebral mucormycosis ⎯ Common site of spread: a. Brain renal b. Spleen patients, c. Heart hematopoietic stem cell transplant or solid organ d. Skin Most common transplant, form in pts. neutropenic with cancer DM, transplant recipient a. Unilateral swelling b. Headaches c. Nasal or sinus congestion/pain d. Serosanguinous nasal discharge e. Fever f. Ptosis, loss of EOM function g. Vision disturbance h. Necrotic black lesions on hard palate, nasal turbinates i. 2. Drainage of black pus from eyes Pulmonary mucormycosis ⎯ Common in patients with hematologic malignancy or profound neutropenia a. Fever b. Cough c. Chest pain d. Dyspnea e. Angioinvasion (Refer to Picture above) ❖ LUQ of the Picture – Necrotic Black Lesions of the Hard Palate ❖ RUQ of the Picture – Rhinocerebral Mucormycosis affecting the Nasal Turbinates PREVENTION 1. Avoid areas with a lot of dust (construction, excavation sites) 2. Avoid direct contact with water damaged building and flood water 3. Avoid activities that involve close contact to soil or dust NORCADOSIS ALSO KNOWN AS: CAUSATIVE AGENT: 3. Primary ⎯ Direct inoculation of fungus to disrupted skin ⎯ Acute inflammatory response with pus, abscess Nocardia nova, N. farcinica, N. cyrincigeorgica, N. brasiliensis INCUBATION PERIOD: ------------------------------------------------------------ RESERVOIR: ------------------------------------------------------------ MODE OF TRANSMISSION: ------------------------------------------------------------ PERIOD OF COMMUNICABILITY: ------------------------------------------------------------ DIAGNOSTICS: ------------------------------------------------------------ TREATMENT: 1. Antimicrobial Susceptibility Testing (AST) should be performed. 2. N. Farcinica – resistant to multiple antimicrobial agents including TrimethoprimSulfamethoxazole (TMP-SMX) 3. Abscess – Surgically drained Cutaneous mucormycosis a. ------------------------------------------------------------ formation, tissue swelling, necrosis, lesions Page 5 of 7 RTRMF – BSN LEVEL III MARINURSE AND FRIENDS NCM 112: MEDICAL-SURGICAL NURSING LECTURER: MR. ANDRE CARLO DE VEYRA ⎯ Routine culture must be held for at least 14 days tissue F#3 MANIFESTATIONS: samples from lungs, mucus from lower airways, skin, brain Pneumonia-like illness – cough, fever, chest pain, weight loss tissues COMPLICATIONS: 1. Meningoencephalitis – fever, headache, lethargy, mental status changes 2. Permanent neurologic damage CLINICAL MANIFESTATIONS ⎯ Invasive pulmonary infection 1. Fever 2. Cough 3. Chest pain 4. Pneumonia 5. Lung abscesses 6. Cavitary lesions ⎯ Disseminated infection ⎯ CNS involvement – Brain abscess 1. Headache Infected meninges: where you can see that there is an infected cerebral spinal fluid and there are swollen tissues that occupies the 2. Lethargy space which may lead to your signs and symptoms; your headache, 3. Confusion fever. And the problem there is upon its healing it may leave 4. Seizures 5. Sudden onset of neurologic deficit permanent neurologic damage TREATMENT: 1. Fluconazole – for asymptomatic, mild-moderate pulmonary infections before it grows out in terms of level, early detection and - prompt treatment is important. Before it reaches the meninges and affects the CNS, you - know that the disadvantage there is even if it leads to severe CNS infection it may lead to permanent neurologic damage. There may be mental status changes. PREVENTION: how do we prevent this from occurring? Boost your immune - 1. Wear shoes. 2. Protect open wounds and cuts. system. 2. Amphotericin B – severe pulmonary and CNS infections CRYPTOCOCCOSIS ALSO KNOWN AS: ------------------------------------------------------------ CAUSATIVE AGENT: Cryptococcus neoformans INCUBATION PERIOD: -----------------------------------------------------------Soil, decaying wood, tree hollows, RESERVOIR: bird droppings MODE OF TRANSMISSION: PERIOD OF COMMUNICABILITY: Inhalation of basidiospores or desiccated yeast cells TNIEA VERSOCOLOR ALSO KNOWN AS: Pityriasis Versicolor CAUSATIVE AGENT: Malassezia (Alapao) INCUBATION PERIOD: ------------------------------------------------------------ RESERVOIR: ------------------------------------------------------------ MODE OF TRANSMISSION: ------------------------------------------------------------ ------------------------------------------------------------ 1. Culture DIAGNOSTICS: ------------------------------------------------------------ 3. Antigen detection (CSF or serum) a. Latex agglutination 1. Selenium sulfide TREATMENT: b. Enzyme immunoassay c. Lateral flow assay TREATMENT: yeast cells PERIOD OF COMMUNICABILITY: 2. Microscopy DIAGNOSTICS: Inhalation of basidiospores or desiccated 1. Fluconazole 2. Amphotericin B RISK FACTORS: 1. Advanced HIV/AIDS (CD4 count of less than 200 cells/mm) 2. Organ transplant recipients 3. Immunosuppressive treatment ⎯ 2. Ketoconazole (gel/cream) 3. Itraconazole 4. Fluconazole the fungus will alter the pigmentation of the skin resulting in discolored patches CONTRIBUTING FACTORS: 1. Hot humid weather 2. Oily skin 3. Hormonal changes 4. Weakened immune system Page 6 of 7 RTRMF – BSN LEVEL III MARINURSE AND FRIENDS NCM 112: MEDICAL-SURGICAL NURSING LECTURER: MR. ANDRE CARLO DE VEYRA CLINICAL MANIFESTATION: 1. F#3 CANDIDIASIS (Moniliasis) Patches of skin discoloration (back, chest, neck, and upper arms) ALSO KNOWN AS: Moniliasis CAUSATIVE AGENT: Candida albicans 2. Mild itching INCUBATION PERIOD: 12 hrs – 5 days 3. Scaling RESERVOIR: ------------------------------------------------------------ MODE OF TRANSMISSION: Sexual contact PERIOD OF COMMUNICABILITY: -----------------------------------------------------------1. Stool culture 2. Gram DIAGNOSTICS: staining of skin, vaginal discharge, scrapings 1. Nystatin- for oral thrush 2. Clitrimazole, fluconazole, ketoconazole, for mucous membrane and vaginal infection TREATMENT: 3. Fluconazole or amphotericin for systemic infection TINEA (Ringworm) ALSO KNOWN AS: Ringworm CAUSATIVE AGENT: ----------------------------------------------------------- INCUBATION PERIOD: ------------------------------------------------------------ RESERVOIR: ------------------------------------------------------------ MODE OF TRANSMISSION: Fomites PERIOD OF COMMUNICABILITY: ------------------------------------------------------------ CLINICAL MANIFESTATIONS: 1. Hx and PE 2. Microscopy – KOH Potassium Hydroxide DIAGNOSTICS: Stain 3. UV light (Wood's lamp) 1. Scaly skin, erythematous & popular rash sometimes covered with exudates 2. Nails red, swollen, nailbeds darkened, occasionally purulent discharge & separation of pruritic nails from nailbeds 3. Oral thrush - cream or bluish white patches on tongue, mouth, pharynx (bloody engorgement when scraped) 4. Retrosternal pain & regurgitation 5. Vaginal mucosa - white or yellowish discharge with 4. Culture pruritus, and local excoriation; white or gray raised 1. Tinea pedis (athlete’s foot) on vaginal walls - Antifungal terbinafine - Chronic - oral antifungal: a) terbinafine b) itraconzole c) fluconazole - TREATMENT: Adjunctive therapy: foot powder, talcum powder 2. Tinea capitis - Topical antifungal - Griseofulvin (DOC) - Terbinafine (for px >4 y/o) - Selenium sulfide shampoos COMPLICATIONS: 1. Renal system: Fever, flank pain, dysuria, hematuria, Pulmonary system: hemoptysis, fever and cough 2. Brain: headache, seizure 3. Endocardium: may lead to systolic/ diastolic murmur, fever, chest pain. 4. Eye: Blurred vision, orbital and periorbital pain. COMPLICATIONS: 1. Onchomycosis (nails) 2. Tinea corporis 3. Tinea pedis 4. Vaginitis 5. Aseptic meningitis Lesion is erythematous, missed, scaly ring with central 6. Paronychia clearing 7. Malabsorption syndrome 2. Multiple lesions present 8. Myocarditis 3. Mild to exudative lesions. 9. Endocarditis 10. Granuloma 3. Tinea corporis/cruris CLINICAL MANIFESTATION: 1. PREVENTION: 1. Keep skin clean and dry 2. Wear shoes that allow air to circulate freely around your feet 3. Don't walk barefoot on areas like locker room, public showers 4. Cut fingernails and toenails short 5. Change socks, underwear at least once a day 6. Don't share clothing, towel, sheets and other personal items 7. Wash hands with soap and running water after playing with pets 8. Shower after practice session (for athletes) patches TREATMENT: 1. Nystatin- for oral thrush 2. Clitrimazole, fluconazole, ketoconazole, for mucous membrane and vaginal infection 3. Fluconazole or amphotericin for systemic infection • Practice universal precaution • Apply cream and lotion or oil on pruritic site • Advise client not to scrape the oral thrush • Check vaginal discharge & note the color, odor and amount • Check high risk patients daily END Page 7 of 7