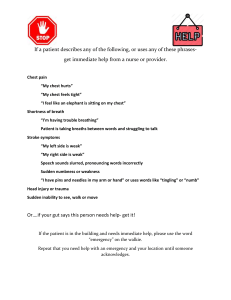
RESPIRATORY ASSESSMENT 1. 2. 3. 4. INSPECT PALPATE PERCUSS AUSCULTATE Past medical history. Medications. Vitals; O2 saturation, ABGs, capnography New or persisting respiratory symptoms. Are changes bilateral? TUBERCULOSIS Infectious disease most commonly affecting the lungs. Caused by mycobacterium tuberculosis. Rates are increasing due to HIV infection and antibiotic resistant strains. Affects the homeless, poor, disadvantaged. Forms in crowd settings (shelters, dorms, prisons, the immunosuppressed). ETIOLOGY ● airborne precautions (talking, sneezing, singing, etc.) ● infection influenced by size of space, concentration of bacteria, immune system of those in the area ● bacteria lodge in the bronchioles and alveoli and cause inflammation; Ghon lesion of focus ● most immunocompetent adults can complete kill of the bacteria ● can spread to bone, kidneys, lymph, adrenal glands CLASSIFICATION ● Active: Patient’s body cannot kill off bacteria; patient is symptomatic, infectious. ● Latent: Infection is there, but not active. Patient is asymptomatic and not infectious, but passes the skin test. Stress on the body can reactivate the disease. CLINICAL MANIFESTATIONS ● ● ● ● dry cough with mucoid or mucopurulent sputum fever, malaise, chills, unexplained weight loss dyspnea abscess formation, captitivation DIAGNOSIS ● tuberculin skin test (Mantoux test) ● interferon-Y release assay (blood test) ● chest X ray ● sputum cultures TREATMENT ● initial and continued antibiotic therapy (3 months of initial, 4 antibiotics, 5 if MDR) ● direct observation therapy is important public health measure; TB drugs are administered and healthcare professionals watch the patient swallow ● isoniazid for 9 months in patients with latent TB ● PREVENTION: BCG vaccine NURSING INTERVENTIONS DIAGNOSES Impaired breathing, ineffective airway clearance, risk for infection, lack of knowledge ● ● ● ● ● ● screening, address social determinants of TB infection in hospital, negative pressure room on respiratory precautions (N95) cover nose and mouth when sneezing, proper hand washing if sent home: isolate from family members, ventilation, pt. should sleep alone report to DPH, direct observation therapy teach patient signs and symptoms of a reemerging infection; stop smoking CHEST TRAUMA Can be blunt or penetrating. Fractured ribs are the most common blunt force chest injury. Splintered, displaced broken ribs can damage other organs. Sx. include pain at site, specially during inspiration, shallow breaths, atestlaciss, pneumonia. Flail chest is a fracture of 3 or more ribs in 2 different places. Causes paradoxical movement during breathing. Rapid, shallow breaths and tachycardia. Ensure O2 therapy and assistance with ventilation. Intubation and mechanical ventilation may be needed. ASSESSMENT FINDINGS ● audible air escaping chest ● tachycardia, shallow breathing ● paradoxical breathing ● cyanosis ● decreased O2 sat ● frothy secretions ● tracheal deviation ● decreased heart sounds ● asymmetrical BPs ● rapid, thready pulse ● dysrhythmias ● distended veins INTERVENTIONS ● establish and monitor ABCs ● high flow O2 ● establish 2 IV sites ● remove clothing to assess wound ● vent 3-way dressings, thick dressing over penetrating object ● Semi-Fowler’s once spinal cord injury is ruled out ● pain meds ● prepare for intubation, surgery TREATMENT: ● binding chest not recommended ● IS, TCDB ● NSAIDS, opiods, nerve blocks PNEUMOTHORAX Air enters the pleural cavity, disrupting negative pressure. Positive pressure causes the lung to fully or partially collapse. Can be open (caused by a wound) or closed. Penetrating wounds cause suction on inspiration. ETIOLOGY ● Spontaneous: rupture of blebs (air sacs) on surface of lungs, can happen in healthy young adults (tall, skinny boys with growth spurts) or secondary to COPD, asthma, pneumonia ● Iatrogenic: lacteration, puncture from a medical procedure (ex. esophageal procedures, mechanical ventilation, gastric tube → chest X ray will identify) ● Tension: medical emergency; affects both respiratory and cardiovascular systems → clamped chest tube, mechanical ventilation, open wound; dyspnea, tracheal deviation, absent lung sounds on affected side ● Hemothorax: blood in the pleural space; chest tube insertion necessary ● Chylothorax: lymph fluid fills space TREATMENT ● ventilation dressing (sealed on 3 sides); prevents air from entering pleural space on inspiration, and allows air to leave on expiration ● if an object stabbed the chest, do not remove it and stabilize with bulky dressing ● chest tube insertion ● tension pneumothorax: needle decompression followed by chest tube insertion CHEST SURGERY Indicated for cardiac, lung, esophageal disorders. TYPES ● Thoracotomy: gives access to heart, lungs, anterior spine, thoracic aorta, esophagus. - median: splits sternum, primarily used for heart surgery - posterolateral: 4-5-6 intercostal space from front to back, used for lung surgeries - anterolateral: 4-5 intercostal space at midaxillary line, for surgery/trauma ● VATS: minimally invasive, removal of masses and nodules, biopsy PREOPERATIVE CARE ● assess cardiopulmonary status ● get EKG, ABGs, CBCs, anesthesia consult ● stop smoking, relieve anxiety ● inform patient about intubation, blood, IV medications; teach breathing exercises POSTOPERATIVE CARE ● chest tube monitoring and management ● pain management, PCA ● TCDB, IS ● assess breathing rate and effort, vitals, sputum, chest tube drainage, pain ● assess surgical site CHEST TUBES Chest tubes restore negative pressure to the lungs, allowing them to inflate. It is inserted by a HCP and attached to a drainage system. It is covered with an occlusive dressing (petroleum) to prevent airflow, and placement is confirmed by X ray. The drainage system collects fluid, blood, and air. DRAINAGE SYSTEM ● ● ● first compartment: collects air, fluid from pleural space of patient second compartment: has 2 cm of fluid, air comes from the collection chamber and the water prevents backflow to the patient; bubbling will occur until the air leak is resolved; tidaling is the normal fluctuation of water → if it stops, check for an occlusion. Tidaling with slow and resolve as the pneumothorax resolves. third compartment; provides gentle suction, usually at -20 NURSING CARE ● keep chest tube loosely coiled below chest level ● ensure dressing is air occulsive ● do not clamp tube during patient transfers ● notify team if drainage exceeds 200ml in first hour, 100ml/hr in other scenarios; report signs of respiratory distress; note color of drainage ● assess cause for a new or worsening air leak: patient or drainage system? ● encourage IS, TCDB ● if tube is disconnected, first priority is to establish water-seal ATELECTASIS Collapsed, airless alveoli. Common occurrence after surgeries and in bedridden patients if proper interventions are not performed; airways are closed off by secretions. CLINICAL MANIFESTATIONS ● hallmark is low grade fever ● dim lung sounds at bases ● low O2 saturation, SOB PREVENTION, TREATMENT ● keep patients mobile, ROM exercises ● TCBD ● IS use ● chest physiotherapy AIRWAY OBSTRUCTION Priority medical emergency. Can be partial or complete. CAUSES ● aspiration ● asthma attack ● edema and inflammation;infection, trauma,cancer, abscess, allergic reaction CLINICAL MANIFESTATIONS ● stridor ● nasal flaring ● use of accessory muscles ● cyanosis ● tachycardia ● restlessness, changes in LOC, anxiety PRIORITIES AND TREATMENT #1 priority is reestablishing air flow and preventing permanent brain damage (4 minutes). ● ● ● ● Heimlich maneuver, suctioning albuterol corticosteroids epinephrine ● advanced airway (ETT, tracheostomy) LARYNGEAL CANCER Cancer of the head and neck. Associated with smoking, HPV in patients > 50 years old. CLINICAL MANIFESTATIONS ● early: lump in throat, voice changes, hoarseness, one-sided sore throat or ear pain, coughing up blood ● late: difficulty swallowing and moving neck, tongue, and jaw; weight loss, pain DIAGNOSIS, TREATMENT ● laparoscopy, bronchoscopy, CAT scan ● biopsy ● TNM staged ● radiation, chemo, surgery NURSING INTERVENTIONS ● proper nutrition, G/PEG tube care; evaluate ability to swallow ● monitor incision ● proper oral care (dental guard during radiation to prevent mouth sores) ● ETT, tracheostomy care (sterile procedure, suctioning) TRACHEOSTOMY Surgically constructed opening in the anterior trachea. Used to establish a patent airway, bypass an obstruction, wean off mechanical ventilation. Less damage to vocal cords than an ETT. NURSING INTERVENTIONS ● Monitor vitals, lung sounds, start an IV line, ensure suctioning and ambu bag are present at bedside ● assess trach site each shift; dressing change every 12 hours ● suctioning; dispose inner cannula if disposable, clean once a shift if nondisposable ● change tapes with 2 people present ● if tube is dislodged, immediately call for help; insert obstrutor into spare tubing, lubricate, insert, and remove the ob. SUCTIONING ● ● ● ● ● ● ● ● sterile procedure hyperoxygenate for 30 seconds before insert catheter without suctioning, turn suctioning on once you hit resistance twisting motion hold breath assess for changes in patients status during suctioning LPN can determine need for suctioning, suction, and provide trach care UAPs can be overseen in providing oral care PULMONARY EMBOLUS (PE) Blockage of 1 or more pulmonary artery by a blood clot, fat, or air. Most derive from deep vein thrombosis (DVT) of the lower limbs. Other causes include long bone and pelvis fractures, improperly administered IV, bacterial vegetation. RISK FACTORS ● recent surgery ● use of hormonal birth control ● air travel ● HF ● clotting disorders ● cigarette smoking, cancer ● obesity CLINICAL MANIFESTATIONS ● vague ● SOB is most common ● hypoxemia ● crackles, wheezing, tachycardia, hypotension, cough, chest pain ● pulmonic heart sounds emphasized COMPLICATIONS ● pulmonary infarction ● pulmonary hypertension; occurs with recurrent PEs; hypoxia causes dilation and hypertrophy of right ventricle DIAGNOSTIC STUDIES ● D-dimer test: measures presence of clots, but is nonspecific. If recent surgery or other thrombi, patient will test positive ● spiral CT: gold standard (note if patient can’t have contrast dye) TREATMENT ● immediate anticoagulation therapy (LMWH); bridge to warfarin (for at least 3 months) ● IVC filter if risk for multiple clots or unable to receive anticoagulants ● embolectomy if obstruction is large enough NURSING INTERVENTIONS ● PREVENTION: anti-embolism stockings, early ambulation, ROM exercises, anticoagulation ● apply O2, continue until anticoagulant therapy is provided; administer morphine for pain and anxiety ● keep patient in Semi-Fowler’s ● carefully monitor vital signs ● monitor pTT/INR, watch for signs of bleeding ● educate; tell patient what is happening ● fall precautions ● post-surgical care ASTHMA Bronchial hyperreactivity to a stimulus; results in an exaggerated inflammatory response. If left untreated, airway remodeling may occur. TRIGGERS ● air pollutants, such as exhaust fumes, cigarette smoke, and perfumes ● allergens, such as pollen, cockroaches, dust, and mold ● drugs, such as NSAIDs, aspirin, some beta blockers (propranolol) ● occupational exposures (agriculture, construction, paints) ● viruses, such as rhinitis and upper respiratory infections ● cold/hot air, hormones, stress ● exercise CLINICAL MANIFESTATIONS ● wheezing, especially on expiration ● cough, dyspnea, chest tightness ● “silent chest” on severe exacerbations ● hyperventilation COMPLICATIONS Status asthmaticus. Severe form of asthma attack characterized by hypoxia, hypercapnia, and acute respiratory failure. Mechanical ventilation is indicated; hemodynamic monitoring, sedation, and analgesics are essential. DIAGNOSIS, TREATMENT ● peak flow rate is observed and monitored ● spirometry (cease bronchodilators for 6-12 hours prior) ● IgE levels ● goal is to identify triggers, prevent exacerbations ● during acute exacerbation, O2 therapy is administered ● SABA (albuterol), ipratropium, corticosteroids (maintenance) ● MDI; wait 1 minute between puffs ● DPI INTERVENTIONS ● primarily prevention of acute attacks and exacerbations ● how to use peak flow meter ● proper nutrition and sleep ● go to ED if in “red zone”, call HCP if in the yellow ● relieve anxiety during acute attacks, provide O2, cardiac monitoring ● rescue plan is 2-4 puffs of a SABAq 20 mins, up to 3 times ● Semi Fowler’s ● pursed lip breathing COPD Progressive airflow limitation; this is a slow process. The inflammatory response results in structural changes and air trapping. This disease is highly correlated with tobacco use, and is largely preventable. CLINICAL MANIFESTATIONS ● bronchitis: persistent coug w/ sputum for 3 months for 2 consecutive years ● emphysema: structural change in lungs that are not reversible, enlarged air spaces ● slow progression; chronic cough, sputum, dyspnea ● chest heaviness ● barrel chest, anorexia COMPLICATIONS ● pulmonary hypertension and cor pulmonale → right sided heart failure, NVD, peripheral edema; treated with O2 therapy, anticoagulants and sometimes diuretics ● exacerbations: acute dyspnea, cough, sputum, respiratory acidosis; increase in frequency as COPD progresses TREATMENT AND NURSING INTERVENTIONS ● drug therapy (SABA, LABA, corticosteroids) ● smoking cessation ● oxygen therapy (maintain saturation of 88-90%) ● PLB, huff coughing, CPT, postural drainage, proper nutrition PNEUMONIA Infection of the lung parenchyma. Can be CAP, HAP, aspiration, necrotizing, opportunistic. CLINICAL MANIFESTATIONS ● cough, chills, dyspnea ● pleural chest pain ● colored sputum ● ecophony, exaggerated fremitus, crackles ● confusion in older patients COMPLICATIONS ● atelectasis ● bacteremia, sepsis ● pleurisy, pneumothorax ● respiratory failure DIAGNOSIS ● chest x-ray ● sputum culture ● ABGs TREATMENT AND INTERVENTIONS ● empirical antibiotic therapy, PO as soon as possible ● post-surgical preventative measures ● position changes, postural drainage, CPT, TCDB ● nutritional therapy and fluids ABG INTERPRETATION