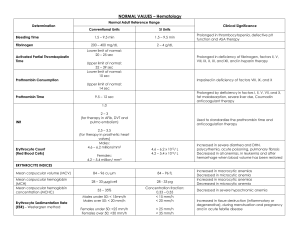
General and colorectal CASE 2: RIGHT ILIAC FOSSA PAIN History A 19-year-old man presents with a 2-day history of abdominal pain. The pain started in the central abdomen and has now become constant and has shifted to the right iliac fossa. The patient has vomited twice today and is off his food. His motions were loose today, but there was no associated rectal bleeding. Examination The patient has a temperature of 37.8°C and a pulse rate of 110/min. On examination of his abdomen he has localized tenderness and guarding in the right iliac fossa. Urinalysis is clear. INVESTIGATIONS Haemoglobin Mean cell volume White cell count Platelets Sodium Potassium Urea Creatinine C-reactive protein 14.2 g/dL 86 fL 19 ⫻ 109/L 250 ⫻ 109/L 136 mmol/L 3.5 mmol/L 5.0 mmol/L 62 µmol/L 20 mg/L Normal 11.5–16.0 g/dL 76–96 fL 4.0–11.0 ⫻ 109/L 150–400 ⫻ 109/L 135–145 mmol/L 3.5–5.0 mmol/L 2.5–6.7 mmmol/L 44–80 µmol/L ⬍5 mg/L Questions • What is the likely diagnosis? • What are the differential diagnoses for this condition? • How would you manage this patient? • What are the complications of any surgical intervention that may be required? 3