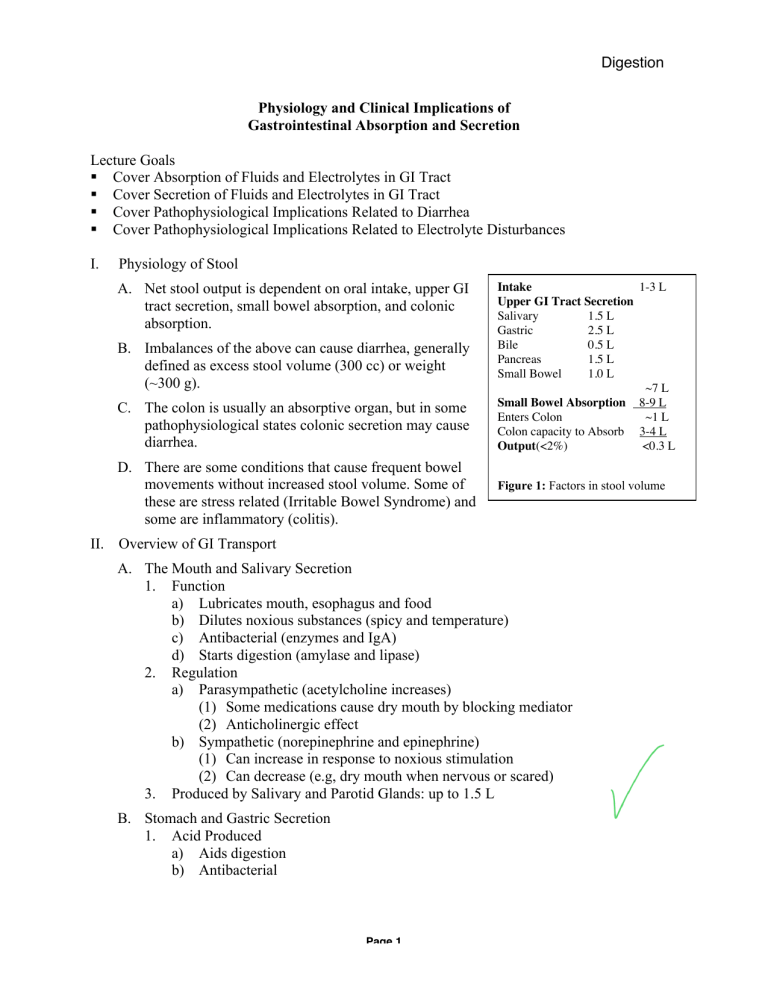
Physiology Digestion December 2, 2010 Joseph Awad, MD Physiology and Clinical Implications of Gastrointestinal Absorption and Secretion Lecture Goals Cover Absorption of Fluids and Electrolytes in GI Tract Cover Secretion of Fluids and Electrolytes in GI Tract Cover Pathophysiological Implications Related to Diarrhea Cover Pathophysiological Implications Related to Electrolyte Disturbances I. Physiology of Stool A. Net stool output is dependent on oral intake, upper GI tract secretion, small bowel absorption, and colonic absorption. B. Imbalances of the above can cause diarrhea, generally defined as excess stool volume (300 cc) or weight (~300 g). C. The colon is usually an absorptive organ, but in some pathophysiological states colonic secretion may cause diarrhea. D. There are some conditions that cause frequent bowel movements without increased stool volume. Some of these are stress related (Irritable Bowel Syndrome) and some are inflammatory (colitis). Intake 1-3 L Upper GI Tract Secretion Salivary 1.5 L Gastric 2.5 L Bile 0.5 L Pancreas 1.5 L Small Bowel 1.0 L ~7 L Small Bowel Absorption 8-9 L Enters Colon ~1 L Colon capacity to Absorb 3-4 L Output(<2%) <0.3 L Figure 1: Factors in stool volume II. Overview of GI Transport A. The Mouth and Salivary Secretion 1. Function a) Lubricates mouth, esophagus and food b) Dilutes noxious substances (spicy and temperature) c) Antibacterial (enzymes and IgA) d) Starts digestion (amylase and lipase) 2. Regulation a) Parasympathetic (acetylcholine increases) (1) Some medications cause dry mouth by blocking mediator (2) Anticholinergic effect b) Sympathetic (norepinephrine and epinephrine) (1) Can increase in response to noxious stimulation (2) Can decrease (e.g, dry mouth when nervous or scared) 3. Produced by Salivary and Parotid Glands: up to 1.5 L B. Stomach and Gastric Secretion 1. Acid Produced a) Aids digestion b) Antibacterial Page 1 Physiology December 2, 2010 Digestion Joseph Awad, MD 2. 3. Isoosmolarity is the Goal of the GI Tract a) The stomach empties liquids best when the osmolarity is equal to plasma (~300 mOsm). b) Solid contents are ground up and dissolved. Some starches and proteins are partially digested. c) Contents diluted by fluid secretion Implications for Rehydration When providing a fluid for rehydration, the fluid will enter the small bowel most rapidly if it is provided in an isoosmotic form. C. Small Intestine 1. Goals of Duodenum a) Neutralize acid (1) Pancreatic ductal cells and duodenum (2) HCO3- secretion (Na+-H+ exchange) (3) Stimuli (a) Lower duodenal pH causes secretin release (b) Vagal influences promote secretion b) Addition of bile and pancreatic enzymes Hormonal control discussed in other lectures (CCK) c) Iron absorption: mostly in duodenum 2. The Jejunum and Ileum are High Flux Areas a) Key Concept: Absorption and secretion are fairly independent processes. b) Maintaining Isoosmolarity (1) Digestion (by creating smaller more osmotically active particles) increases the osmotic load. This would tend to cause water to leave the the circulation to dilute the lumen, but . . . (2) Nutrient absorption drags these solutes and water out of the lumen. (3) The net effect should be for more fluid to leave the lumen than enters. (4) Given the tremendous bidirectional flow of fluid and solutes there is great potential for pathophysiological disturbance (more later). D. Colon: The Dehydrator 1. The colon normally receives 500 to 1500 ml chyme daily. 2. Sodium and chloride generally absorbed a) Ileal effluent is close to isotonic, ~140 mEq/L Na+) b) Colonic effluent effluent is usually < 50 mEq/L Na+) 3. Water is absorbed 4. Net excretion of K+ and HCO3- Page 2 Physiology December 2, 2010 Digestion Joseph Awad, MD III. Mechanisms of Secretion and Absorption A. Duodenal/Pancreatic Secretion H2O Cl1. The primary driver in this cell CO2 + and every such cell is the Na C.A. K+ ATPase (not shown). HCO32. Plasma flowing by the cells is H20 OH- + H + H+ + HCO 3+ acidified by ATP dependent K Cl H+ pumps and Na+-H+ exchange Na+ H+ (facilitated transport) resulting ATP in CO2 production from HCO3 . The CO2 diffuses into the cell. K+ 3. Carbonic anhydrase converts Lumen (neg) Capillary the CO2 into bicarbonate that flows down an electrochemical potential gradient in exchange Na+ + for Cl . H is pumped back out Figure 2: Bicarbonate Secretion into the blood. 4. To facilitate increased bicarbonate secretion, Cl- is pumped back into the lumen under the influence of secretin. 5. The lumen is electronegative dragging Na+ paracellularly. Water also follows sodium and other ions to maintain isoosmolarity of the lumen. B. Intestinal Absorption 1. Absorption takes place primarily in the villi, especially towards the tip, as opposed K+ + Na to secretion that is primarily a crypt ATP H+ phenomenon (see below). There is a net Na+ + absorption of nutrients, Na+, Cl-, HCO3Na and water. Glucose/AA 2. There are transporters of amino acids and simple sugars that are powered by the Na+ gradient (out>in). These molecules are cotransporters. Lumen Capillary 3. Na+ also powers the excretion of H+. The K+ (neg). result is the reverse of the III-A above Clwith absorption of any excess bicarbonate Figure 3: Small intestinal absorption. in the jejunum. + 4. The absorption of Na tends to at least transiently leave anions behind in the lumen making it electronegative pushing the absorption of Cl- and water paracellularly. C. Intestinal Secretion 1. Secretion is primarily a function of crypt cells. 2. Again the primary driver is the gradient set up by the Na+-K+ ATPase. 3. CFTR (cystic fibrosis transporter) is a chloride pump that plays a major role in regulating secretion. Page 3 Physiology December 2, 2010 Digestion Joseph Awad, MD 4. 5. 6. 7. The Na+ gradient is used to drive K+ and Clinto the cell. CFTR pushes Cl- into the lumen making it electronegative. K+ leaves the cell passively into the blood helping to maintain the gradient from blood to lumen (pos to neg). Na+ and water flow follow this gradient. The total flow can be controlled by the activity of CFTR. More Cl- transport equals more secretion. CFTR turn-ons a) Increased cAMP (VIP and PGs) b) Increased Ca++ (Acetylcholine) K+ Cl- CFTR K+ 2 ClNa+ Lumen Na+ Capillary H 20 Figure 4: Intestinal secretion. D. Colonic Absorption and Ion Fluxes 1. Net effects a) Net absorption of Na+ and Cl- with K+ reduction in concentrations in effluent. 3 K+ Na+ b) Net absorption of water. ATP H+ c) Loss of K+ / HCO3H2CO3 2 Na+ 2. Again the primary driver is the gradient set HCO3+ + up by the Na -K ATPase. In addition there Cl? is an electrogenic Na+ pump on the luminal side. This pump causes the lumen to be Na+ negative. a) Drives Cl- absorption (in exchange for Lumen Capillary HCO3- and paracellularly) + (neg) b) Drives K excretion Figure 5: Colonic absorption and ion 3. The presence of tight junctions in the colon + fluxes. allows Na and Cl to be removed and concentrations in lumen decreased. 4. Aldosterone can increase absorption by causing increased production of Na+ pumps on both luminal and capillary sides. IV. Pathophysiology of Diarrhea: Four Primary Mechanisms A. Osmotic Load 1. Poorly digested or absorbed sugars a) Lactose intolerance b) Sorbitol (1) Prunes and some other fruits (2) Diet/diabetic candies 2. Mucosal disease with malabsorption 3. Medications e.g.,Magnesium hydroxide (Milk of Magnesia, MOM) Page 4 Physiology December 2, 2010 Digestion Joseph Awad, MD B. Enhanced Proximal GI Secretion 1. Cholera and cholera-like toxins a) Gs protein ADP-ribosylation and activation b) cAMP increased with increased CFTR activity 2. Hormones a) Hormone secreting tumors like VIPoma (rare) b) Prostaglandin analogs (misoprostol) C. Impaired Colonic Absorption or Stimulated Secretion 1. Bile acids cause secretion. Terminal ileal disease or resection can cause bile acids to enter colon. 2. Bacterial digestion products (many osmotically active substances are digested to products that stimulate colonic secretion) a) Fatty acids (1) Pancreatic insufficiency (a) Chronic pancreatitis – decreased enzyme production (b) Zollinger-Ellison Syndrome (gastrinoma) – inactivated enzymes (2) Intestinal dysfunction (e.g., gluten sensitive enteropathy) 3. Inflammation 4. Infection D. Motility Disorders 1. Stasis with small bowel bacterial overgrowth, leading to bacterial digestion products as above. These compounds can also stimulate motility. 2. A, B, and C above are often associated with stimulation of motility. 3. Excessive motility alone is rarely a cause of diarrhea. E. Summing it All Up 1. Problems affecting the small bowel have the greatest potential to cause large volumes of stool a) Inhibition of small bowel absorption b) Stimulation of small bowel secretion (cholera) 2. The colon tries to make up, and can make up for a fair amount of extra contents dumped from the small bowel. 3. Diseases affecting the colon exacerbate problems higher up. 4. Diseases of the colon alone more often cause frequent BMs than markedly increased stool volume. V. Assorted Clinical Topics A. Oral Rehydration Therapy for Secretory Diarrhea 1. Absorption is not impaired 2. Glucose facilitates Na+ transport which facilitates water absorption 3. Glucose provides energy 4. Replaces other electrolytes including increased K+ and HCO3- losses induced by the colon’s attempt to absorb more NaCl and water. Page 5 Oral Rehydration Recipe 1/2 tsp. Baking soda Na HCO31/2 tsp. Salt (NaCl) Juice 2 lemons 1/2 tsp KCl 2 - 3 Tbsp. Karo syrup 2 Tbsp. glucose 1 liter water (clean) Physiology December 2, 2010 Digestion Joseph Awad, MD B. Nasogastric Suction especially Secretion Na+ ClK+ with gastric outlet obstruction Gastric 60 100 10 H+ rich 1. Gastric acid production Pancreatic 140 30-75 10 HCO3- rich causes HCO3- to be pumped New ileostomy 130 110 20 into blood that is usually Ileostomy 50 60 10 balanced by pancreatic Diarrhea 60 45 30 HCO3- rich HCO3 production with acid pumped into blood. Table 1: Electrolyte concentrations of various GI fluids. 2. Removal of gastric acid creates an unopposed process. NG tube 3. The patient will develop a Acid - Base Imbalance metabolic alkalosis with chloride depletion. H2O + CO2 + C. Pancreatic Fistula 1. Loss of bicarbonate and sodium. 2. Replacement with Na bicarbonate containing fluid. H GI HCO3- Pancreatic Duct Cell Parietal Cell D. Ileostomy (small bowel surgically Blood connected to skin) Losses 1. Patients with ileostomies are at H2O + CO2 HCO3H risk for dehydration (no colon to help retain sodium and fluid. Figure 6: Illustration of acid-base imbalance resulting from 2. Patients with new ostomies are at nasogastric suction. greater risk. After the small bowel adapts, takes over some colonic-type functions, the risk decreases. + E. Diarrhea 1. When the colon has to work overtime K+ and HCO3- losses increase as the colon attempts to absorb more NaCl and water. VI. Bowel Movements Rule A. Having good, comfortable, conveniently-timed bowel movements is very important. B. Normal: 3 a day to 3 a week C. Constipation 1. Infrequent stools 2. Difficult to pass 3. Painful D. Diarrhea 1. More than 300 ml (g) per day 2. Frequent urgent bowel movements E. Understanding the pathophysiology of bowel movements will help you treat these conditions. More in years to come. Page 6