Fluids, Electrolytes, & Acid-Base Balance: Nursing Assessment & Interventions
advertisement

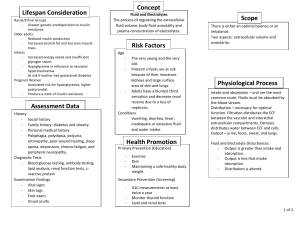
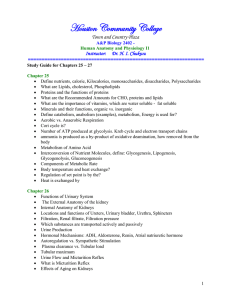
Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance Assessment Factors affecting fluid, electrolyte, & acid-base balance o Age Infants & elderly more susceptible to fluid imbalances Infants have a higher metabolic rate – creates more toxins, can’t concentrate urine, water lost to evaporation r/t high body surface area Elderly more prone to hypokalemia r/t wasting potassium with diuretics Elderly generally don’t drink enough water Subcutaneous tissue loss in elderly leads to increased moisture loss Gender Hormonal fluctuations in Men have a greater total body women water percentage o Stress – increased fluid retention from aldosterone production, decreased renal excretion o Weight – total body fluid disproportionate weight in people that are obese o Surgery – pre-op NPO, blood loss, stress, fluid drainage, post-op vomiting o Medical conditions – cardiac, hepatic, renal & respiratory Vital signs o Pay close attention to prolonged fever, tachycardia, changes in respirations, & alterations in BP o Monitor q4 Weight o I&O record isn’t always an accurate reflection of changes in fluid balance o Daily weights are the more precise method Same gown/clothing, same scale, same time of day, before breakfast, after voiding o A change of 1kg (2.2lb) = 1L (1000mL) of fluid Skin turgor & mucous membranes o Skin turgor can provide an indicator of fluid volume imbalance o Deficit Skin remains pulled upright Furrows in the tongue (severe (tented) after release deficit) Mucous membranes are dry & Common to see dry, cracked lips sticky Neurologic assessment o Deep tendon reflexes o Confusion, agitation, coma o Tremors Cardiovascular assessment o Irregular heart rate o Blood pressure o Palpitations o Peripheral pulses o Grading of pulses o Presence of edema Significant & visible sign of fluid volume excess Usually found in dependent areas of the body Late indicator of fluid volume excess Pitting edema – characterized by a lasting indentation in the skin when pressure is applied Brawny edema – obvious swelling; tissue is too firm & hard to be indented Respiratory assessment o Abnormal lung sounds (crackles) o Respiratory rate o Diminished lung sounds Musculoskeletal assessment o Muscle strength o Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance GI & GU assessment o Intake (PO, IV fluids) o Frequency & characteristics of stool – constipation or diarrhea o o Nausea & vomiting Amount of urine output Nursing Interventions Monitoring fluid balance o The nurse should evaluate the impact of disease or effect of treatment on an ongoing basis Fluid replacement – pt may need to increase fluid intake to offset losses Electrolyte replacement o 2 most commonly prescribed supplements are K+ and Ca+ Intake & Output (I&Os) o Oral intake includes all fluids & foods that become liquid at room temperature Ice chips, ice cream, popsicles/water ice, soup, jello o Output consists of any body fluid that can be measured o Nurse notes whether I&Os balance in a 24 hour period Nurse is responsible for confirming that ordered tests have been completed & results are communicated to the HCP o Labs often ordered to monitor fluid, electrolytes, & acid-base balance; also to assess effectiveness of prescribed meds Restricting electrolyte intake o Sodium restrictions are classified as mild, moderate, or severe o Na+ restrictions Mild – 3000-4000 mg/day “no added salt” Moderate – 2000 mg/day “low sodium” Severe – 500 mg/day o Instruct pt on the dietary restrictions & common foods to avoid Maintaining fluid & electrolyte balance o Restricting fluid intake – use 50% of the o Amount of fluid is divided further into fluid amount during the day when the fluid with meals, between meals, & with pt is most active & consumes two meals med admin Restricting electrolyte intake Education o Buy fresh or frozen, not canned o Salt substitutes & herbs are okay o No cured meats allowed o Some OTC meds have high sodium contents Mechanisms Body fluid is either intracellular (ICF) or extracellular (ECF) o Majority of fluid is ICF – within the cell o Extracellular fluid – fluid outside of the cell Interstitial, intravascular, or transcellular Extracellular fluid imbalances o Correct the underlying cause & replace water & electrolytes – orally, with blood products, or through balanced IV solutions Osmotic pressure Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance o Amount of pressure required to stop o Determined by the concentration of osmotic flow of water solutes in solution Hypovolemia & BP decrease stimulate the release of renin by the kidneys o Converts angiotensinogen to o Angiotensin II – vasoconstriction angiotensin I through body to increase BP, o ACE (angiotensin converting enzyme) reabsorption of water, stimulate adrenal cortex to produce aldosterone, secrete form the lungs kidneys changes angiotensin I to angiotensin II ADH, stimulates thirst mechanism Homeostasis – maintenance of fluid balance o Monitored by the kidneys through balance through vasoconstriction & excretion or reabsorption of Na+ changes in blood pressure o ADH (released by the pituitary gland) – o Renin-angiotensin-aldosterone maintain serum osmolality by mechanism o Controlled by several mechanisms: controlling the amount of water secreted in the urine renin-angiotensin regulates BP & fluid ECF & ICF ICF o Prevalent cation is K+ o Prevalent anion is PO43- ECF o Prevalent cation is Na+ o Prevalent anion is ClHypovolemia (ECF volume deficit) – abnormal loss of normal body fluids, inadequate intake, or plasma to interstitial fluid shift o Clinical manifestations r/t loss of vascular volume as well as CNS effects o Treatment: replace water & electrolytes with balanced IV solution o Use of hypotonic IV fluids o Diagnoses used Deficient fluid imbalance Acute confusion Electrolyte imbalance Imbalanced nutrition: less than Decreased cardiac output body requirements o Hypovolemic shock is a potential complication o Nursing diagnoses – deficient fluid imbalance, electrolyte imbalance, decreased cardiac output, acute confusion, imbalanced nutrition Dehydration – loss of water without corresponding loss of sodium o Assessment Chvostek’s sign, Trousseau’s sign, deep tendon reflexes, tremors, confusion, agitation, coma, jugular vein distension, ECG waveforms, pulses, BP, crackles, diminished lung sounds, respiratory rate, frequency & characteristics of stool, N/V, amt of urine output Hypervolemia (ECF volume excess) o Excess intake of fluids, abnormal retention of fluids, or interstitial to plasma fluid shift o Clinical manifestations r/t excess volume Weight gain is the most common o Edema (see assessment) o Care Remove fluid without changing electrolyte composition or osmolality of ECF Diuretics, fluid restriction, restriction of sodium intake, removal of fluid to treat ascites or pleural effusion o Nursing diagnoses – excess fluid volume, electrolyte imbalance, impaired gas exchange, impaired tissue integrity, activity intolerance Document continues below Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance Fluid Tonicity Isotonic, hypotonic, hypertonic Effects of water on RBCs Hypotonic – water excess; solutes less o Hypertonic – water deficit; solutes more concentrated than in cells concentrated than in cells Results in cellular swelling Results in cellular shrinking o Isotonic – normal water level Regulation of water balance o Renal regulation Primary organs for regulating fluid & electrolyte balance Adjusting urine volume Selective reabsorption of water & electrolytes Renal tubules are site of action of ADH & aldosterone Hydrostatic pressure o Force of fluid in a compartment o BP generated by heart’s contraction Oncotic pressure o Colloid osmotic pressure o Osmotic pressure caused by plasma proteins Fluid movement in capillaries – amount & direction of movement determined by o o Capillary hydrostatic pressure o Plasma oncotic pressure Fluid spacing o First spacing – normal distribution o Second spacing – abnormal accumulation of interstitial fluid (edema) o o Interstitial hydrostatic pressure Interstitial oncotic pressure o Third spacing – fluid is trapped where it’s difficult or impossible for it to move back into cells or blood vessels Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance Regulation of Water Balance Hypothalamic-pituitary regulation o Osmoreceptors in hypothalamus sense fluid deficit or increase o Deficit stimulates thirst & ADH release Renal regulation o Primary organs for regulating fluid & electrolyte balance o Adjusting urine volume Selective reabsorption of water & electrolytes Adrenal corticol regulation o Releases hormones to regulate water & electrolytes Cardiac regulation o Natriuretic peptides are antagonists to the RAAS o Hormones made by cardiomyocytes in response to increased atrial pressure GI regulation o Oral intake accounts for most water o Small amounts of water are eliminated by the GI tract in feces IV Fluids & Electrolyte Replacement Purpose o Maintenance – when oral intake isn’t adequate o Assess ability to obtain adequate fluid independently, express thirst & swallow efficiently Parenteral fluid & electrolyte replacements o Blood transfusions (regarding volume) o Central venous access devices (CVAD) o Permit frequent, continuous, rapid, or intermittent admin of fluids & meds Types of fluids categorized by tonicity Hypotonic – lower osmolality than plasma o Dilutes ECF o Decreased plasma osmolality (water excess) suppressed ADH release Renal tubules are sites of action of ADH & aldosterone o o Glucorticoids (cortisol) Mineralcorticoids (aldosterone) o They suppress secretion of aldosterone, renin, & ADH to decrease blood volume and pressure o Diarrhea & vomiting can lead to significant fluid & electrolyte loss o o Assist those with physical limitations Replacement – when losses have occurred o Allow for giving drugs that are potentially vesicants Used to admin blood/blood products & parenteral nutrition o Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance o Water moves from ECF to ICF by osmosis Isotonic – osmolality similar to plasma o Similar osmolality to ECF (only expands ECF); no net loss or gain from ICF Hypertonic – higher osmolality when compared to plasma o Draws water out of cells into ECF o Requires frequent monitoring of BP, lung sounds, & serum Na+ levels D5W (5% dextrose in water) – isotonic o Dextrose metabolizes quickly, net result of free water o Provides 170kcal/L D5 ½ NS (5.5% dextrose in normal saline) – hypertonic o Common maintenance fluid o Replaces fluid loss D10W (10% dextrose in water) – hypertonic o Provides 340 kcal/L o Provides free water but no electrolytes NS (normal saline) – isotonic o 0.9% saline, slightly more NaCl than ECF o Used when both fluid & sodium is lost Lactated Ringer’s – isotonic o Contains Na+, K+, Cl-, Ca2+, & lactate o Expands ECF – treats burns & GI losses Colloids – stay in vascular space & increase oncotic pressure o Human plasma products [albumin, FFP (fresh frozen plasma), blood] o o Usually maintenance fluids Monitor for changes in mentation o o Ideal to replace ECF volume deficit Fluids: D5W, NS, LR o Fluids: D5 ½ NS o Used to replace water loss, prevents ketosis o KCl added for maintenance or replacement o Limits dextrose concentration that may be infused peripherally o Only solution used with blood o Contraindicated with liver dysfunction, hyperkalemia, & severe hypovolemia o Semisynthetics (dextran, starches, Hespan) Sodium (Na) Responsible for o ECF volume & concentration o o Generating & transmitting nerve o impulses Imbalances typically associated with parallel changes in osmolality Hypernatremia Causes Inadequate water intake, excessive water loss, sodium gain S/S Thirst, AMS (drowsiness, restlessness, confusion, lethargy), S/S fluid volume deficit Interventions Seizures & coma possible - treat the underlying cause - replace fluids orally or via IV with isotonic fluids or hypotonic fluids (water deficit) - dilute with Na-free IV fluids & give diuretics (excess sodium) - monitor carefully Muscle contractility Regulating acid-base balance Hyponatremia Loss of sodium-containing fluids, water excess Headache, irritability, difficulty concentrating Severe – confusion, vomiting, seizures, coma - fluid restriction may be only treatment (water excess) - loop diuretics & demeclocycline - small amounts of IV hypertonic saline solution 3% NaCl (for seizures) - fluid replacement with isotonic sodium-containing solution Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance -encourage oral intake (abnormal fluid loss) Potassium (K) Responsible for o Resting membrane potential of nerve & o Maintenance of cardiac rhythms muscle cells o Acid-base balance o Cellular growth Dietary sources o Protein-rich foods o Salt substitutes o Fruits & vegetables o Potassium meds (PO or IV) Regulated by the kidneys Hypokalemia can enhance the effect of digitalis & lead to digitalis toxicity & subsequent cardiac arrest Always dilute IV KCl (potassium chloride) Never give KCl via IV push or as a bolus Major ICF cation Hyperkalemia Hypokalemia Increase of K+ via the kidneys or GI Causes Impaired renal excretion, shift from ICF to ECF, massive intake of K+, some tract, increased shift of K+ from ECF to ICF, dietary K+ deficiency, renal losses drugs, renal failure from diuresis Cardiac issues, skeletal muscle S/S Dysrhythmias, fatigue, confusion, tetany, muscle cramps, weak or weakness, weakness of respiratory paralyzed skeletal muscles, ABD muscles, decreased GI motility, cramps hyperglycemia Interventions - stop K+ intake - KCl supplements PO or IV - should not exceed 10 mEq/hr - increase K+ excretion – diuretics, dialysis, Veltessa, Kayexalate - use an infusion pump - force K+ from ECF to ICF by IV insulin with dextrose (severe hyperkalemia) Calcium (Ca) Responsible for o Formation of teeth & bones o Blood clotting o Transmission of nerve imoulses Obtained from dietary intake; need vitamin D to absorb Present in bones & plasma o Ionized Ca2+ is biologically active Changes in pH & serum albumin affects Ca2+ levels Balance controlled by o Parathyroid hormone (PTH) – increases bone resorption, GI absorption, 7 renal tubule reabsorption of Ca2+ o o Myocardial contractions Muscle contractions o Calcitonin – increases Ca2+ deposition into bone, increases renal Ca2+ excretion, & decreases GI absorption Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance Chvostek’s sign – contraction of face muscles after light tap over the facial nerve in front of the ear Hypercalcemia Causes Hyperparathyroidism, cancer S/S Interventions Trousseau’s sign – carpal spasm induced by inflating a BP cuff above the systolic pressure for a few minutes Hypocalcemia Decreased production of PTH, multiple blood trnasfusions, alkalosis, increased Ca2+ loss Fatigue, lethargy, weakness, Positive Trousseau’s or Chvostek’s confusion, hallucinations, seizures, sign, laryngeal stridor, dysphagia, coma, dysrhythmias, bone pain, numbness & tingling around the fractures, nephrolithiasis, polyuria, mouth or in the extremities, dehydration dysrhythmias - low Ca2+ diet - treat the cause - Ca2+ & vitamin D supplements - increased weight-bearing activity - increase fluid intake - IV Ca2+ gluconate - rebreathe into paper bag - hydration with isotonic saline infusion - treat pain & anxiety to prevent - calcitonin hyperventilation-induced alkalosis Phosphate (P) Responsible for o o Function of muscle o RBCs Primary anion in ICF Involved in acid-base balance buffering system, ATP production, cellular uptake of glucose, & metabolism of macros (carbs, proteins, fats) Causes S/S Interventions o Nervous system Serum levels controlled by parathyroid hormone (PTH) Maintenance requires adequate renal functioning Reciprocal relationship with Ca2+ Hyperphosphatemia Hypophosphatemia Malnourishment/malabsorption, AKI, chronic kidney disease, excess intake of phosphate or vitamin D, diarrhea, use of phosphate-binding hypoparathydroidism agents, inadequate replacement during parenteral nutrition Tetany, muscle cramps, paresthesia, CNS depression, muscle weakness & hypotension, dysrhythmias, seizures pain, respiratory failure, HF, rickets, (hypocalcemia) osteomalacia - ID & treat underlying cause - oral supplements Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance - restrict food/fluids containing phosphorus - hemodialysis - volume expansion & forced diuresis - correct any hypocalcemia - ingestion of high phosphorus foods IV admin Na+ or K+ phosphate Magnesium (Mg) Cofactor in enzyme for metabolism of carbs Required for DNA & protein synthesis Responsible for o Blood glucose control o Needed for ATP production o BP regulation Acts directly on myoneural junction 50-60% contained in bone Important for normal cardiac function Absorbed in GI tract, excreted by kidneys Hypermagnesia Hypomagnesia Prolonged fasting, chronic Causes Increased intake of products containing Mg, renal insufficiency, alcoholism, fluid loss from GI tract, excess IV Mg admin prolonged parenteral nutrition without supplementation, diuretics, PPI drugs, hyperglycemia osmotic diuresis S/S Hypotension, facial flushing, lethargy, Resembles hypocalcemia** N/V, impaired deep tendon reflexes, muscle paralysis, respiratory & Muscle crampls, tremors, hyperactive cardiac arrest deep tendon reflexes, Chvostek’s & Trousseau’s signs, confusion, vertigo, seizures - treat underlying cause Interventions - prevention first!! IV CaCl or calcium gluconate if - oral supplements symptomatic - increase dietary intake Fluids & IV furosemide to promote - parenteral IV or IM MG when severe urinary excretion - dialysis Acid-Base Regulation pH level – measure of H+ (hydrogen) ion concentration o Normal range – 7.35 to 7.45 o Acidosis - < 7.35 Increased H+ concentration o Alkalosis - > 7.45 Decreased H+ concentration o Death results in a pH level under 6.8 or over 7.8 3 mechanisms to regulate acid-base balance o Respiratory regulation The lungs control the amount of carbonic acid available by retaining or exhaling CO2 CO2 + H2O > H2CO3 > H+ + HCO3- Respiratory center in the medulla controls breathing Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance Increased respirations lead to decreased CO2 in blood increased CO2 elimination & o Renal regulation The kidneys neutralize acid & base by excreting or retaining H+ ions & excreting or forming bicarbonate ions Conserves bicarbonate & excretes acid 3 mechanisms for acid elimination Excrete weak acids Secrete free H+ Combine H+ with ammonia (NH3) o Buffer system Shifts H+ in & out of the cell Act chemically to change strong acids to weak acids or bind Primary regulator of acidthem balance Carbonic acid – bicarbonate, phosphate, protein, hemoglobin buffers CVAD (central venous access devices) Catheters placed in large blood vessels o Subclavian, jugular 3 main types o Centrally inserted catheters (central lines) Peripherally inserted central catheters (PICC line) o Implanted ports Useful for patients with limited peripheral vascular access or need for long-term vascular access Hemodynamic monitoring Venous blood samples Injection of radiopaque contract media o Permits frequent, continuous, rapid, or intermittent admin of fluids & meds Allows for giving drugs that are potentially vesicants Used to admin blood or blood products & parenteral nutrition Advantages o Immediate access o o Reduced venipunctures Disadvantages o Increased risk of systemic infection o o Invasive procedure o o Clamped or kinked catheter o o Tip against wall of vessel o o Thrombosis o Interventions o Inspect catheter & insertion site o o Change dressing & clear according to policy Transparent semipermeable dressing or gauze dressing Chlorhexidine preferred cleansing agent o Change injection caps o Centrally inserted catheter o Inserted into a vein in the chest or ABD o wall with the tip resting in the distal end o of superior vena cava Decreased risk of extravasation Precipitate buildup in lumen Embolism Risk of infection Pneumothorax Catheter migration Assess for pain Flushing is IMPORTANT! Non-tunneled or tunneled Dacron cuff anchors catheter & decreases incidence of infection Class 16 (Chp. 16) – Fluids, Electrolytes, & Acid-Base Balance o Single, double, or triple lumen o Examples of long-term tunneled catheters Hickman Broviac Groshong PICC lines o Central venous catheter inserted into a o For patients who need vascular access vein in arm for 1 week to 6 months o Single or multi lumen, non-tunneled o Can’t use arm for BP or blood draws o Advantages Lower infection rate Decreased cost Fewer insertion-related complications o Disadvantages Deep vein thrombosis (DVT) Phlebitis Implanted port o Central venous catheter connect to an implanted, single or double subcutaneous injection port o Port is titanium or plastic with self-sealing silicone septum o Drugs are injected through skin into port o Advantages Good for long-term therapy Cosmetic discretion Low risk of infection Midline catheters o Peripheral catheters 3-8” long Single or double lumen o Use & care similar to PICC lines o May stay in place up to 4 weeks Vocabulary Diffusion – movement of molecules across a permeable membrane from high to low concentration o Facilitated diffusion – uses carrier to help move molecules Active transport – process in which molecules move against concentration gradient o External energy is needed for this process o Sodium-potassium pump – as Na+ diffuses into the cell & K+ diffuses out of the cell, the active transport system supplied with energy delivers Na + back to ECF & K+ back to ICF Osmosis – movement of water down a concentration gradient from low solute concentration to high solute concentration, across a semi-permeable membrane