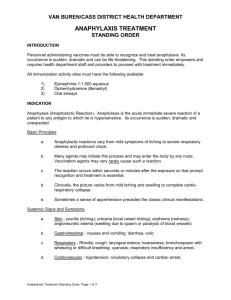
ANAPHYLAXIS COPYRIGHT © 2017, ELSEVIER INC. ALL RIGHTS RESERVED. ANAPHYLACTIC SHOCK Acute, life-threatening hypersensitivity (allergic) reaction ▪ Massive vasodilation ▪ Release of vasoactive mediators ▪ ↑ Capillary permeability ANAPHYLACTIC SHOCK Clinical manifestations ▪ Anxiety, confusion, dizziness ▪ Sense of impending doom ▪ Chest pain ▪ Incontinence ANAPHYLACTIC SHOCK Clinical manifestations Depends of the mediators ▪ Localized mediators- cutaneous response ( Wheal-and-flare reaction) ▪ Systemically released mediators – anaphylaxis ▪ Occurs within minutes ▪ Can be life threatening: ▪ Bronchial constriction ▪ Airway obstruction ▪ Vascular collapse ▪ ▪ ▪ ▪ Swelling of lips and tongue, angioedema Wheezing, stridor due to laryngeal edema Flushing, pruritus, urticaria Respiratory distress and circulatory failure INITIAL SYMPTOMS OF ANAPHYLAXIS Edema and itching of the site of exposure to the allergen Shock can occur rapidly and is manifested by: ▪ Rapid, weak pulse ▪ Hypotension ▪ Dilated pupils ▪ Dyspnea ▪ Bronchial edema ▪ Angioedema ▪ Possibly cyanosis ▪ Death - if emergency treatment is not initiated ASSESSMENT Subjective ▪ Feeling of uneasiness, apprehension, weakness, and impending doom Objective ▪ On auscultation crackles & wheezes, with reduced breath sounds, ▪ Erythema, angioedema of eyes, lips, tongue, ▪ Intensely itchy skin, hives large blotches ▪ Increased mucous production ▪ Stridor, suffocation ▪ Tachycardia ▪ Hypotension ▪ Laryngeal edema MEDICAL INTERVENTIONS Depends on severity Typically epinephrine is administered Oxygen therapy Antihistamines, corticosteroids Intravenous fluids - Normal Saline(NS) or Lactated Ringers (LR) Vasopressor agents and volume expanders INTERPROFESSIONAL CARE ANAPHYLACTIC SHOCK Epinephrine, diphenhydramine, ranitidine Maintain a patent airway ▪ Nebulized bronchodilators ▪ Aerosolized epinephrine ▪ Endotracheal intubation or cricothyroidotomy may be necessary EPINEPHRINE AUTO-INJECTOR No absolute contraindications Usual dose 0.3mg ▪ may need additional if person is large or not getting better after one dose Injecting ▪ into middle third of outer portion of thigh ▪ can go through clothes Give if patient feels ▪ SOB, throat tightening or pre-syncopal INTERPROFESSIONAL CARE ANAPHYLACTIC SHOCK Aggressive fluid replacement IV corticosteroids if significant hypotension persists after 1–2 hours of aggressive therapy NURSING INTERVENTION Head to toe assessment Assist with medical management- FOCUS is getting the medicines quickly Regular vital sign and follow-up assessments post reaction ▪ Reaction could be biphasic or protracted or delayed (in case where there was a known exposure) Education Prevention teaching