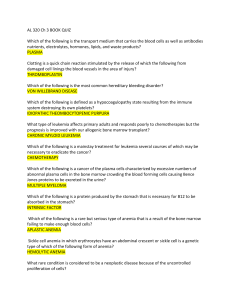
Anemia Mazin Abdelgadir General features 1. 2. 3. 4. 5. 6. Decrase RBCs Pallor Hypoxia Peripheral blood changes BM hyperplasia Extra medullary hematopoiesis Process of RBCs production iron Vit b12 Folic acid BM (Aplastic anemia) RBCs (hemolysis) Iron deficiency anemia • Very common • 25% to 50% of people in developing countries . • Causes: 1. Chronic blood loss is the most important cause :peptic ulcers, colonic cancer, hemorrhoids,menorrhagia, metrorrhagia, cancers). 2. low intake 3. Increased demands (pregnancy and infancy.) 4. Malabsorption (celiac disease or after gastrectomy) • iron deficiency develops insidiously. • Iron stores are depleted , marked by : 1. a decline in serum ferritin 2. and the absence of stainable iron in the bone marrow. 3. decrease in serum iron and 4. a rise in the serum transferrin. 5. Microcytic hypochromic anemia, 6. impaired work and cognitive performance, 7. reduced immunocompetence. Clinical feature: 1. weakness, and pallor, 2. figernails, thinning, flttening, and “spooning,” 3. pica, the compunction to consume non food stuffs such as dirt or clay. 4. In peripheral smears red cells are microcytic and hypochromic Diagnostic criteria: 1. anemia, hypochromic and microcytic 2. low serum ferritin and iron levels, 3. low transferrin saturation, 4. increased total iron-binding capacity, 5. For unclear reasons, the platelet count often is elevated. 6. Erythropoietin levels are increased, but marrow cellularity usually is only slightly increased. Microcytosis hypochromia There is also increased anisocytosis (variation in size) and poikilocytosis (variation in shape). Aplastic anemia • Aplastic anemia is a disorder in which multipotent myeloid stem cells are suppressed, leading to bone marrow failure and pancytopenia. • pure red cell aplasia, :only erythroid progenitors are affected and anemia is the only manifestation. Causes 1. 50% is idiopathic. 2. a drug or a chemical,( alkylating agents, antimetabolites), benzene, and chloramphenicol. 3. viral hepatitis. 4. Cancer affecting the bone marrow 5. Chemotherapy Pathogenesis • autoreactive T cells play an important role. • 5% to 10% of patients with “acquired” aplastic anemia have inherited defects in telomerase,. Morphology • The bone marrow in aplastic anemia is markedly hypocellular, with greater than 90% of the intertrabecular space being occupied by fat. • Thrombocytopenia and granulocytopenia may result in hemorrhages and bacterial infections, respectively. • The requirement for transfusions may eventually lead to hemosiderosis. Clinical course • The slowly progressive anemia causes the insidious development of weakness, pallor, and dyspnea. • Thrombocytopenia often manifests with petechiae and ecchymoses. • Granulocytopenia may be manifested by frequent and persistent minor infections or by the sudden onset of chills, fever, and prostration. • Aplastic anemia does not cause splenomegaly • the red cells are normochromic and normocytic • Reticulocytes are reduced in number(reticulocytopenia) Tx & Px • The prognosis is unpredictable. • Withdrawal of drugs sometimes leads to remission, • Bone marrow transplantation often is curative, particularly in nontransfused patients younger than 40 years of age. • Transfusions sensitize patients to alloantigens, producing a high rate of engraftment failure Myelophthisic Anemia • anemia is caused by extensive infitration of the marrow by tumors or other lesions. • It most commonly is associated with metastatic breast, lung, or prostate cancer. • Other tumors, advanced tuberculosis, lipid storage disorders, and osteosclerosis • . The principal manifestations include anemia and thrombocytopenia. • the white cell series is less affected. • Characteristically misshapen red cells, some resembling teardrops, are seen in the peripheral blood. • Immature granulocytic and erythrocytic precursors also may be present (leukoerythroblastosis) Thank you