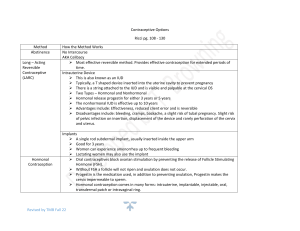
Case: 25 year old with irregular cycles, hirsutism, and with BMI: 30 (obese) Reason for prescription and additional notes Copper IUD ● Copper IUD is highly effective in long-term contraception even when used as EC, and effectiveness does not depend on weight ● Candidates: ○ Nulliparous ○ Adolescents ○ Immunocomprom ised women ● Contraindications: ○ Pregnancy (or just suspicion) ○ Acute PID ○ Postpartum endometritis or infected abortion ○ Known or suspected uterine or cervical malignancy ○ Genital bleeding of unknown origin ○ Previously inserted IUD that has not been removed ● Avoid using levonorgestrel because it is more Mechanism of action ● ● Induce local inflammation → environment hostile for the sperm → fertilization will not occur Copper: increases extent of inflammation → accumulation of the uterine lumen → penetrates the fallopian tube and cervix → ○ affects the viability of the gametes ○ prevents fertilization ○ Lowers chance of development of zygote ○ ALSO impedes sperm transportation and viability in the cervical mucus Benefits ● ● ● ● ● Effectiveness can last for 10 Tier 1 contraceptive Reduction in the risk of the development of cervical and endometrial carcinoma Effectiveness equivalent t tubal sterilization Improvement pf symptoms of endometriosis and adenomyosis Risk and Adverse Effects ● Uterine bleeding: heavy or prolonged menses or intermenstrual bleeding. ○ Due to increased release of prostaglandin ○ Rarely leads to anemia ○ Occurs in the first few months → reassurance and supplemental iron for these patients ● Perforation at the fundus is caused by the insertion process ○ Rare ● Complications Relation to Pregnancy: extrauterine location (ectopic pregnancy) ● androgenic in formulation Copper allergy and Wilson Disease ○ In the event of intrauterine pregnancy, whether or not the pregnancy is desired or not, device should be removed ○ If pregnancy is not desired: manual vacuum aspiration Infection: PID ● Due to the placement process ● Routine prophylaxis is not effective ● If IUD is still not implanted: delay implantation if infection is suspected ● If px is already positive with gonorrhea or chlamydia with an IUD implanted, give antibiotics without removing it. ○ If condition will not improve (72 hours) and it progresses into an tubo-ovarian abscess: device should be removed ● Actinomycosis (PID) ○ Associated with the use of IUD Vaginal Ring/ Condoms ● It is a flexible polymer ring with a 54-mm outer diameter and a 50-mm inner ● ● Its core releases a daily dose of 15 ug ethinyl estradiol and 120 ug of the progestin etonogestrel. These doses effectively inhibit ovulation, ● ● A ring may be used concurrently with vaginal medications or with a tampon. One ring provides ● However this will not produce protection for stds so it is still advisable to use condoms. ● ● OCP: mainly by suppressing the ovulation thru interference of the GnRH ● diameter. These are highly effective and failure rate is reported to be 0.65 pregnancies per 100 woman-years (Mulders, 2001; Roumen, 2001). I.e, < 1 per 100 Tier 2: (6-12 pregnancies per 100 women in 1 year ● It also thickens the cervical mucus, which makes it more difficult for sperm to move through the cervix, and thins the lining of the womb so a fertilised egg is less likely to implant itself. ● ● Progestin ● Inhibit ovulation ● Thickening of the cervical mucus ● Thinning of the endometrium ● contraception for a month, so you don't have to think about it every day. Unlike the pill, the ring still works if you have sickness (vomiting) or diarrhoea. period-type bleeding usually becomes lighter, more regular and less painful. Decrease acne (with decreased androgens/dose) ● it may cause temporary side effects, such as increased vaginal discharge, headaches, nausea, breast tenderness and m Adverse Effects: (dosage and potency dependent) ● Nausea ● Breast tenderness ● Weight gain (contradicting studies) ● headache Estrogen ● Maintain the endometrium → prevent unscheduled bleeding ● Inhibit follicular development Ethinyl estradiol ● Severe adverse cardiovascular effects ● Minor adverse symptoms without increasing the failure rate Combination: ● Suppress the gonadotropins ● Estrogen: prevents the rise in FSH and enhances the progestin component ● Progestin: inhibits ovulation and Increased risk ● Venous and arterial thrombosis ○ Obesity is a risk factor for this (BMI >40) ● specifically the LH surge (Lowest amount to suppress: ovulation inhibition dose) Overall suppression of follicular development Secondary (changes in): ● Cervical mucus ● Fallopian tube ● Endometrium ○ ● Women who smoke older than 35 yrs Breast cancer